| Revision as of 14:21, 29 February 2008 edit168.169.125.80 (talk) →Religious views on smoking crack← Previous edit | Latest revision as of 17:50, 10 December 2024 edit undoEepTheMeep (talk | contribs)Extended confirmed users638 editsm Vandalism.Tags: Undo Mobile edit Mobile web edit Advanced mobile edit | ||
| Line 1: | Line 1: | ||
| {{short description|Practice of burning tobacco and breathing the resulting smoke}} | |||
| {{Articleissues | |||
| {{Use dmy dates|date=April 2021}} | |||
| | long = October 2007 | |||
| ] | |||
| | POV = October 2007 | |||
| {{Tobacco}} | |||
| | restructure = October 2007 | |||
| {{Smoking|expanded=tobacco}} | |||
| | unbalanced = October 2007 | |||
| '''Tobacco smoking''' is the practice of burning ] and ingesting the resulting ]. The smoke may be inhaled, as is done with ]s, or simply released from the mouth, as is generally done with ]s and ]s. The practice is believed to have begun as early as 5000–3000 BC in ] and ].<ref name="Gateley2004"/> Tobacco was introduced to ] in the late 17th century by ], where it followed common trade routes. The practice encountered criticism from its first import into the ] onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.<ref name="L&M"/><ref>{{Cite book|author1=West, Robert |author2=Shiffman, Saul|title=Fast Facts: Smoking Cessation|publisher=Health Press Ltd.|year=2007|isbn=978-1-903734-98-8|page=28}}</ref> | |||
| }} | |||
| Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives<ref name ="WHOJeffreyWigand"/> and then combusted. The resulting smoke, which contains various active substances, the most significant of which is the addictive ] drug ] (a compound naturally found in tobacco), is absorbed through the ] or the ].<ref name="GilmanXun2004p318"/> Many substances in cigarette smoke, chiefly nicotine, ], which heighten heart rate, alertness<ref name="PMID2498936"/> and reaction time, among other things.<ref name="WesnessWarburton1997"/> ] and ]s are released, which are often associated with pleasure,<ref name="GilmanXun2004pp320-321">{{Harvnb|Gilman|Xun|2004|pp=320–321}}</ref> leading to ].<ref>{{Cite journal |last=Benowitz |first=Neal L. |date=2009-02-01 |title=Pharmacology of Nicotine: Addiction, Smoking-Induced Disease, and Therapeutics |journal=Annual Review of Pharmacology and Toxicology |language=en |volume=49 |issue=1 |pages=57–71 |doi=10.1146/annurev.pharmtox.48.113006.094742 |pmid=18834313 |issn=0362-1642|pmc=2946180 }}</ref> | |||
| ] is the most common method of smoking tobacco.]] | |||
| ''' Tobacco smoking''' is the inhalation of smoke from burned dried or cured leaves of the ] plant. People smoke for pleasure, for ritualistic or social purposes, or for ],<ref>{{cite journal | |||
| | last = Kumari | |||
| | first = Veena | |||
| | coauthors = Peggy Postma | |||
| | title = Nicotine use in schizophrenia: The self medication hypotheses | |||
| | journal = Neuroscience & Biobehavioral Reviews | |||
| | volume = 29 | |||
| | issue = 6 | |||
| | pages = 1021-1034 | |||
| | date = 2006 | |||
| | url = http://dx.doi.org/10.1016/j.neubiorev.2005.02.006 | |||
| | accessdate = 2008-02-17}}</ref> as well as to satisfy a physiological dependence on ]. Tobacco use by ] throughout North and South America dates back to 2000BC. The practice was brought back to Europe by the crew of ]. Tobacco smoking took hold in Spain and was introduced to the rest of the world, via trade. | |||
| Tobacco is an agricultural product processed from the fresh leaves of plants in the genus Nicotiana. Tobacco has been growing on the northern continents since about 6000 BC and began being used by native cultures at about 3000 BC. It has been smoked in one form or another since about 2000 BC. There are pictoral drawings of ancient Mayans smoking crude cigars from 1400 BC. | |||
| German scientists identified a link between smoking and ] in the late 1920s, leading to the first ] in modern history, albeit one truncated by the collapse of ] at the end of ].<ref name="NWC228"/> In 1950, British researchers demonstrated a clear relationship between smoking and cancer.<ref name="RichardHillyBMJ1954"/> Evidence continued to mount in the 1960s, which prompted political action against the practice. Rates of consumption since 1965 in the ] have either peaked or declined.<ref name="RockEtAlCDC2006"/> However, they continue to climb in the developing world.<ref name="WHO2002FactSheet"/> As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking.<ref>{{cite journal|last=Giovino|first=GA|author2=Mirza, SA; Samet, JM; Gupta, PC; Jarvis, MJ; Bhala, N; Peto, R; Zatonski, W; Hsia, J; Morton, J; Palipudi, KM; Asma, S; GATS Collaborative, Group|title=Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys.|journal=Lancet|date=18 August 2012|volume=380|issue=9842|pages=668–79|pmid=22901888|doi=10.1016/S0140-6736(12)61085-X|s2cid=12450625| issn = 0140-6736 }}</ref> The gender gap tends to be less pronounced in lower age groups.<ref name="WomenTobaccoChallenges5-6"/><ref name="2001SurgeonGeneralWomen47" /> According to the ], 8 million annual deaths are caused by tobacco smoking.<ref name="Tobacco">{{Cite web |title=Tobacco |url=https://www.who.int/news-room/fact-sheets/detail/tobacco |access-date=2024-02-24 |website=www.who.int |language=en}}</ref> | |||
| Tobacco smoke contains ] and ] (a ]), which combined give rise to ] ] and euphoriant properties. The effect of nicotine in first time or irregular users is an increase in ] and memory, and mild ]. Nicotine also disturbs ] and suppresses appetite. This is because nicotine, like many stimulants, increases blood sugar levels. | |||
| Many smokers begin during adolescence or early adulthood.<ref name=":0">{{Cite journal|last1=Chandrupatla|first1=Siddardha G.|last2=Tavares|first2=Mary|last3=Natto|first3=Zuhair S.|date=27 July 2017|title=Tobacco Use and Effects of Professional Advice on Smoking Cessation among Youth in India|journal=Asian Pacific Journal of Cancer Prevention|volume=18|issue=7|pages=1861–1867|doi=10.22034/APJCP.2017.18.7.1861|issn=2476-762X|pmid=28749122|pmc=5648391}}</ref> A 2009 study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke.<ref name="The Lancet">{{cite journal|title=Tobacco smoking:why start?|journal=The Lancet|date=26 September 2009|volume=374|issue=9695|pages=1038|doi=10.1016/s0140-6736(09)61680-9|pmid=19782852|last1=The Lancet|s2cid=37513171}}</ref> During the early stages, a combination of perceived pleasure acting as ] and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing. After an individual has smoked for some years, the avoidance of ] symptoms and ] become the key motivations to continue. | |||
| Medical research has determined that chronic tobacco smoking can lead to many health problems, particularly ], ], and ].<ref> </ref><ref> </ref> | |||
| Tobacco smoking killed 100 million people worldwide in the ] and could kill 1 billion people around the world in the ], the ] Report warned.<ref></ref><ref></ref> | |||
| ==Methods of smoking== | |||
| ] | |||
| ===Cigarette=== | |||
| {{main|Cigarette}} | |||
| {{seealso|List of additives in cigarettes}} | |||
| Cigarette smoking is the most common form of tobacco consumption. Because of the curing process, the smoke is mild enough to inhale in overdose quantities, unlike cigar or pipe tobacco. Cigarettes also contain a number of additives, particularly to enhance taste. "Roll ups" are also very popular, particularly in European countries; these are prepared from loose tobacco, cigarette papers and filters all bought separately. Cigarettes are smoked by some with a ]. (See also ]). | |||
| == |
==History== | ||
| {{Main|History of tobacco|History of smoking}} | |||
| {{main|Cigar}} | |||
| A cigar is generally puffed, not inhaled. Cigars come in many shapes and sizes, the most common being the "Corona", "Cigarillo", and "Robusto". The tobacco used is grown throughout the ] in places such as the ], ], ], ], and ], but also in countries in other regions such as Brazil and Indonesia. Cigars generally come available in 2 categories in reference to color, "Natural" and "Maduro". "Natural" shades are ones that do not undergo a further fermenting process, unlike "Maduro" which in its construction involves a further fermenting process to darken and strengthen (in taste) the leaf. | |||
| === |
===Use in ancient cultures=== | ||
| ], 16th century.]] | |||
| {{main|Smoking pipe (tobacco)}} | |||
| A pipe for smoking typically consists of a small chamber (bowl) for ] of the substance to be smoked and a thin stem (shank) that ends in a mouthpiece (also called a bit). Pipes are made from a variety of materials (some obscure): ], ], ], ], ], ], ], ], and various other materials, such as metal. Tobacco used for smoking pipes is often chemically treated to change smell and taste not available in other commercial tobacco products. Many of these are mixtures using staple ingredients of variously cured Burley and Virginia tobaccos which are mixed with tobaccos from different areas, such as Oriental or Balkan locations. ] (a fire-cured tobacco of Cypriot or Syrian origin), ] (only grown in ]) or combinations of Virginia and ] tobaccos of African, Indian, or South American origins. Traditionally, many U.S. tobaccos are made of American Burley with artificial sweeteners and flavorings added to create an artificial "aromatic" smell, whereas "English" blends are based on natural Virginia tobaccos enhanced with Oriental and other natural tobaccos. There is a growing tendency towards "natural" tobaccos which derive their aromas from blending with spice tobaccos alone and historically-based curing processes. | |||
| Smoking's history dates back to as early as 5000–3000 BC, when the agricultural product began to be cultivated in Mesoamerica and South America; consumption later evolved into burning the plant substance either by accident or with intent of exploring other means of consumption.<ref name="Gateley2004">{{Cite book|last=Gately|first=Iain|title=Tobacco: A Cultural History of How an Exotic Plant Seduced Civilization|url=https://books.google.com/books?id=x41jVocj05EC|access-date=22 March 2009|orig-year=2003|year=2004|publisher=Diane|isbn=978-0-8021-3960-3|pages=3–7|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080723/https://books.google.com/books?id=x41jVocj05EC|url-status=live}}</ref> The practice worked its way into shamanistic rituals.<ref name="Wilbert1993">{{Cite book|last=Wilbert|first=Johannes|title=Tobacco and Shamanism in South America|url=https://books.google.com/books?id=qPCuo4LkrIwC|access-date=22 March 2009|date=28 July 1993|publisher=Yale University Press|isbn=978-0-300-05790-4|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080724/https://books.google.com/books?id=qPCuo4LkrIwC|url-status=live}}</ref> Many ancient civilizations – such as the ], the Indians, and the Chinese – burnt incense during religious rituals. Smoking in the Americas probably had its origins in the incense-burning ceremonies of ] but was later adopted for pleasure or as a social tool.<ref name="Robicsek1979">{{Cite book|last=Robicsek|first= Francis|title=The Smoking Gods: Tobacco in Maya Art, History, and Religion| date=January 1979 |publisher=University of Oklahoma Press|isbn=978-0-8061-1511-5|page=30}}</ref> The smoking of tobacco and various hallucinogenic drugs was used to achieve trances and to come into contact with the spirit world.<ref name=Hallucinogenic_pre-Columbian>{{cite journal |title=Hallucinogenic drugs in pre-Columbian Mesoamerican cultures |volume=30 |issue=1 |pages=42–49 |author=F.J.Carod-Artal |date=1 July 2011 |journal=Neurología |doi=10.1016/j.nrleng.2011.07.010 |pmid=21893367 |doi-access=free }}</ref> Also, to stimulate respiration, ]s were used.<ref>{{Citation |doi = 10.2307/2843888 |last = Nordenskiold |first = Erland |title = The American Indian as an Inventor |jstor = 2843888 |journal = Journal of the Royal Anthropological Institute |volume = 59 |page=277 |year = 1929}}</ref> | |||
| Pipes can range from the simple machine-made briar pipe to handmade and artful implements created by pipe-makers which can be expensive collectors' items. The popularity of pipe smoking in Western countries has declined in recent years under the onslaught of cigarette advertising. However, it has also enjoyed a resurgence of late among younger and middle aged smokers who find its contemplative nature and age-transcendent status as "hobby not habit" to be both thoroughly enjoyable and stress-relieving{{Fact|date=July 2007}}. As many pipe-smokers say, "We don't inhale." | |||
| Eastern North American tribes would carry large amounts of tobacco in pouches as a readily accepted trade item and would often smoke it in ]s, either in sacred ceremonies or to seal bargains.<ref>{{Cite book|first1=John Gottlieb Ernestus|last1=Heckewelder|author-link1=John Heckewelder|first2=William Cornelius|last2=Reichel|author-link2=William Cornelius Reichel|title=History, manners, and customs of the Indian nations who once inhabited Pennsylvania and the neighboring states|url=https://books.google.com/books?id=qPCuo4LkrIwC|format=PDF|access-date=22 March 2009|orig-year=1876|date=June 1971|publisher=The Historical society of Pennsylvania|isbn=978-0-405-02853-3|page=149|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080724/https://books.google.com/books?id=qPCuo4LkrIwC|url-status=live}}</ref> Adults as well as children enjoyed the practice.<ref>{{Cite journal|last1=Diéreville|first2=John Clarence|last2=Webster|first3=Alice de Kessler Lusk|last3=Webster| title = Relation of the voyage to Port Royal in Acadia or New France|year=1933|publisher=The Champlain Society|quote=They smoke with excessive eagerness men, women, girls and boys, all find their keenest pleasure in this way}}</ref> It was believed that tobacco was a gift from the Creator and that the exhaled tobacco smoke was capable of carrying one's thoughts and prayers to heaven.<ref>{{Cite journal|last=Gottsegen|first=Jack Jacob|title=Tobacco: A Study of Its Consumption in the United States|url=https://books.google.com/books?id=1uNCAAAAIAAJ&q=Tobacco:+A+Study+of+Its+Consumption+in+the+United+States|access-date=22 March 2009|year=1940|publisher=Pitman Publishing Company|page=107|postscript=>|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080757/https://books.google.com/books?id=1uNCAAAAIAAJ&q=Tobacco:+A+Study+of+Its+Consumption+in+the+United+States|url-status=live}}</ref> | |||
| ===Hookah=== | |||
| {{main|Hookah}} | |||
| Apart from smoking, tobacco had uses as medicine. As a pain killer it was used for earache and toothache and occasionally as a ]. Smoking was said by the desert Indians to be a cure for colds, especially if the tobacco was mixed with the leaves of the small ], '']'', or the root of ] or ], ''Leptotaenia multifida'', the addition of which was thought to be particularly good for ] and ].<ref>{{Cite book|last=Balls|first=Edward K.|title=Early Uses of California Plants|url=https://archive.org/details/earlyusesofcalif00ball|url-access=registration|quote=Early Uses of California Plants.|access-date=22 March 2009|date=1 October 1962|publisher=University of California Press|isbn=978-0-520-00072-8|pages=–85}}</ref> | |||
| A hookah (or ''sheesha'') is a type of traditional Middle Eastern and South Asian water pipe, which operates by water-filtration and indirect heat. Hookahs are most popular in the Middle East, but form a niche market in many other places. In other contexts, hookahs are used to smoke ], ] or ]. | |||
| ===Popularization=== | |||
| Typically, tobacco is smoked from a hookah by placing richly flavored tobaccos in the smoking bowl, covering it with foil, and placing a coal on top of the foil. This keeps the tobacco from burning, and allows it to bake. The resulting vapors are further cooled by the hookah water and filtered by a bubbling action in the basin of the hookah, resulting in a moist, warm light smoke. The Al-Waha, Al Fakher, and Nakhla tobacco companies compete for market share in the Middle East by producing flavored tobaccos for use in the hookah. Some flavors include the traditional apple, grape, double apple, orange, strawberry, cherry, mango, vanilla, and melon flavors; as well as more modern flavors of cola, coconut, cappuccino, and banana milk. | |||
| {{For|more about the commercial development of tobacco|History of commercial tobacco in the United States}} | |||
| ], 1627]] | |||
| ==Health effects== | |||
| {{Shorten|date=October 2007}} | |||
| {{main|Tobacco and health}} | |||
| In 1612, six years after the settlement of ], ] was credited as the first settler to successfully raise tobacco as a cash crop. The demand quickly grew as tobacco, referred to as "brown gold", revived the ] from its failed gold expeditions.<ref>{{Cite journal|last=Jordan|first=Ervin L. Jr.|title=Jamestown, Virginia, 1607–1907: An Overview|url=http://curry.edschool.virginia.edu/socialstudies/projects/jvc/overview.html|access-date=22 February 2009|publisher=University of Virginia|url-status=dead|archive-url=https://web.archive.org/web/20021017223417/http://curry.edschool.virginia.edu/socialstudies/projects/jvc/overview.html|archive-date=17 October 2002}}</ref> In order to meet demands from the Old World, tobacco was grown in succession, quickly depleting the soil. This became a motivator to settle west into the unknown continent, and likewise an expansion of tobacco production.<ref>{{Cite book|last=Kulikoff|first=Allan|title=Tobacco and Slaves: The Development of Southern Cultures in the Chesapeake|url=https://archive.org/details/tobaccoslavesdev0000kuli|url-access=registration|quote=Tobacco & Slaves: The Development of Southern Cultures in the Chesapeake.|access-date=22 March 2009|date=1 August 1986|publisher=The University of North Carolina Press|isbn=978-0-8078-4224-9}}</ref> | |||
| ===Establishing a link between smoking and health effects=== | |||
| As the use of tobacco became popular in Europe, a number of people became concerned about its negative effects. One of the first was ]. In his 1604 treatise, '']'', King James observed that smoking was: | |||
| Frenchman ] (from whose name the word nicotine is derived) introduced tobacco to France in 1560, and tobacco then spread to England. The first report of a smoking Englishman is of a sailor in Bristol in 1556, seen "emitting smoke from his nostrils".<ref name="L&M"/> Like tea, coffee and opium, tobacco was just one of many intoxicants that was originally used as a form of medicine.<ref>{{Harvnb|Gilman|Xun|2004|p=38}}</ref> Tobacco was introduced around 1600 by French merchants in what today is modern-day Gambia and Senegal. At the same time, caravans from Morocco brought tobacco to the areas around ], and the Portuguese brought the commodity (and the plant) to southern Africa, establishing the popularity of tobacco throughout all of Africa by the 1650s. | |||
| <blockquote>A custome lothsome to the eye, hatefull to the Nose, harmfull to the braine, dangerous to the Lungs, and in the blacke stinking fume thereof, nearest resembling the horrible Stigian smoke of the pit that is bottomelesse.</blockquote> | |||
| Soon after its introduction to the Old World, tobacco came under frequent criticism from state and religious leaders. ], King of Scotland and England, produced the treatise '']'' in 1604, and also introduced excise duty on the product. ], sultan of the ] 1623–40 was among the first to attempt a smoking ban by claiming it was a threat to public morals and health. The ] of China issued an edict banning smoking two years before his death and the overthrow of the ]. Later, the ] rulers of the ], would proclaim smoking "a more heinous crime than that even of neglecting archery". In ] Japan, some of the earliest tobacco plantations were scorned by the ] as being a threat to the military economy by letting valuable farmland go to waste for the use of a recreational drug instead of being used to plant food crops.<ref name="Screech-Smoke">{{Harvnb|Gilman|Xun|2004|pp=92–99}}</ref> | |||
| The late-19th century invention of automated cigarette-making machinery in the American South made possible mass production of cigarettes at low cost, and cigarettes became elegant and fashionable among society men as the Victorian era gave way to the Edwardian. In 1912, American Dr. Isaac Adler was the first to strongly suggest that lung ] is related to smoking.<ref> Isaac Adler. Primary Malignant Growth of the Lung and Bronchi. New York, Longmans, Green and Company, 1912, pp. 3-12. </ref> In 1929, Fritz Lickint of ], ], published a formal statistical evidence of a lung cancer–tobacco link, based on a study showing that ] sufferers were likely to be smokers.<ref name=about_lickint> http://ije.oxfordjournals.org/cgi/content/full/30/1/31 </ref> Lickint also argued that tobacco use was the best way to explain the fact that lung cancer struck men four or five times more often than women (since women smoked much less).<ref name=about_lickint /> | |||
| ] | |||
| Prior to World War I, lung cancer was considered to be a rare disease, which most physicians would never see during their career<ref>Witschi 2001, A Short History of Lung Cancer. Toxicol Sci. 2001 Nov;64(1):4-6. PMID 11606795</ref> <ref>Adler I. Primary malignant growths of the lungs and bronchi. New York: Longmans, Green, and Company; 1912., cited in Spiro SG, Silvestri GA. One hundred years of lung cancer. Am J Respir Crit Care Med. 2005 Sep 1;172(5):523-9. PMID 15961694</ref>. With the postwar rise in popularity of cigarette smoking, however, came a virtual epidemic of lung cancer. | |||
| Religious leaders have often been prominent among those who considered smoking immoral or outright blasphemous. In 1634, the ] forbade the sale of tobacco, and sentenced men and women who flouted the ban to have their nostrils slit and their backs flayed. Pope ] likewise condemned smoking on holy places in a papal bull of 1624. Despite some concerted efforts, restrictions and bans were largely ignored. When ], a staunch smoking opponent and the author of '']'', tried to curb the new trend by enforcing a 4000% tax increase on tobacco in 1604 it was unsuccessful, as suggested by the presence of around 7,000 tobacco outlets in London by the early 17th century. From this point on for some centuries, several administrations withdrew from efforts at discouragement and instead turned tobacco trade and cultivation into sometimes lucrative government monopolies.<ref>{{Harvnb|Gilman|Xun|2004|pp=15–16}}</ref><ref>{{Cite journal|author=King James I of England|title=A Counterblaste to Tobacco|url=http://www.laits.utexas.edu/poltheory/james/blaste/|access-date=22 March 2009|date=16 April 2002|orig-year=1604|publisher=University of Texas at Austin|archive-date=18 May 2009|archive-url=https://web.archive.org/web/20090518062807/http://www.laits.utexas.edu/poltheory/james/blaste/|url-status=live}}</ref> | |||
| In 1950, Dr. ] published research in the ] showing a close link between smoking and lung cancer.<ref> {{cite journal | last = Doll | first = Rich | coauthors = and Hilly, A. Bradford | date = ] ] | title = Smoking and carcinoma of the lung. Preliminary report | journal = British Medical Journal | volume = 2 | issue = 4682 | pages = 739-748 | id = PMID 14772469}} </ref> Four years later, in 1954 the ], a study of some 40 thousand doctors over 20 years, confirmed the suggestion, based on which the government issued advice that smoking and lung cancer rates were related.<ref> {{cite journal | last = Doll | first = Richard | coauthors = and Hilly, A. Bradford | date = ] ] | title = The mortality of doctors in relation to their smoking habits. A preliminary report | journal = British Medical Journal | issue = 4877 | pages = 1451-55 | id = PMID 13160495 | url = http://bmj.bmjjournals.com/cgi/reprint/328/7455/1529}} </ref> The British Doctors Study lasted till 2001, with result published every ten years and final results published in 2004. <ref name="Doll2004">{{cite journal|author=Doll R, Peto R, Boreham J, Sutherland I.|title=Mortality in relation to smoking: 50 years' observation on male British doctors.|year=2004|url=http://www.pubmedcentral.gov/articlerender.fcgi?tool=pubmed&pubmedid=15213107|PMID=15213107}}</ref> Much early research was also done by Dr. Ochsner. ] magazine for many years published frequent anti-smoking articles. In 1964 the ] ]'s Report on Smoking and Health (referenced below), led millions of American smokers to quit, the banning of certain advertising, and the requirement of warning labels on tobacco products. | |||
| By the mid-17th century most major civilizations had been introduced to tobacco smoking and in many cases had already assimilated it into the native culture, despite some continued attempts upon the parts of rulers to eliminate the practice with penalties or fines. Tobacco, both product and plant, followed the major trade routes to major ports and markets, and then on into the hinterlands. The English language term ''smoking'' appears to have entered currency in the late 18th century, before which less abbreviated descriptions of the practice such as ''drinking smoke'' were also in use.<ref name="L&M">{{Cite book|first1=John|last1=Lloyd|first2=John|last2=Mitchinson|title=The Book of General Ignorance|date=25 July 2008|publisher=Harmony Books|isbn=978-0-307-39491-0|url=https://archive.org/details/bookofgeneralign00lloy}}</ref> | |||
| ===Health risks of smoking=== | |||
| ] | |||
| <ref name=smokefree> </ref> | |||
| The main health risks in tobacco pertain to diseases of the cardiovascular system, in particular ] (heart attack), diseases of the ] such as ] (COPD), ]<ref>Gilliland FD, Islam T, Berhane K, Gauderman WJ, McConnell R, Avol E, Peters JM. Regular smoking and asthma incidence in adolescents. Am J Respir Crit Care Med. 2006 Nov 15;174(10):1094-100. PMID 16973983</ref>, ], and ], particularly ] and cancers of the ] and tongue. According to the Canadian Lung Association, tobacco kills between 40,000–45,000 Canadians per year, more than the total number of deaths from ], ]s, ], ], ]s and accidental ]ing.<ref> </ref><ref> </ref> The United States' ] describes tobacco use as "the single most important preventable risk to human health in ] and an important cause of premature death worldwide." | |||
| Growth in the US remained stable until the American Civil War in 1860s, when the primary agricultural workforce shifted from ] to ]. This, along with a change in demand, accompanied the industrialization of cigarette production as craftsman ] created a machine in 1881 to partially automate their manufacture.<ref name="Burns134-135">{{Cite book|last=Burns|first=Eric|title=The Smoke of the Gods: A Social History of Tobacco|url=https://books.google.com/books?id=cZfqS7vi9vEC&q=The+Smoke+of+the+Gods:+A+Social+History+of+Tobacco|access-date=22 March 2009|date=28 September 2006|publisher=Temple University Press|isbn=978-1-59213-480-9|pages=134–135|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080727/https://books.google.com/books?id=cZfqS7vi9vEC&q=The+Smoke+of+the+Gods:+A+Social+History+of+Tobacco|url-status=live}}</ref> | |||
| A person's increased risk of contracting disease is directly proportional to the length of time that a person continues to smoke as well as the amount smoked. However, if someone stops smoking, then these chances gradually decrease as the damage to their body is repaired. A year after quitting, the risk of contracting heart disease is half that of a continuing smoker.<p> The health risks of smoking are not uniform across all smokers. Risks vary according to amount of tobacco smoked, with those who smoke more at greater risk. Light smoking is still a health risk. | |||
| ===Social attitudes and public health=== | |||
| Although pipe smoking also increases the risk of various cancers by 33%,<ref>http://jnci.oxfordjournals.org/cgi/content/full/96/11/853/T2</ref>, the data regarding smoking to date focuses primarily on cigarette smoking, which increases mortality rates by 40% in those who smoke <10 cigarettes a day, by 70% in those who smoke 10-19 a day, by 90% in those who smoke 20-39 a day, and by 120% in those smoking two packs a day or more.<ref>http://profiles.nlm.nih.gov/NN/B/B/K/M/_/nnbbkm.pdf 1967 Surgeon General's Report on Smoking </ref> | |||
| {{globalize section|date=March 2024}} | |||
| In 1912 and 1932 in Germany, anti-smoking groups, often associated with anti-liquor groups,<ref name="NWC178">{{Harvnb|Proctor|2000|p=178}}</ref> first published advocacy against the consumption of tobacco in the journal ''Der Tabakgegner'' (The Tobacco Opponent). In 1929, ] of Dresden, Germany, published a paper containing formal ] evidence of a lung cancer–tobacco link. During the ] ] condemned his earlier smoking habit as a waste of money,<ref name="NWC219">{{Harvnb|Proctor|2000|p=219}}</ref> and later with stronger assertions. This movement was further strengthened with Nazi reproductive policy as women who smoked were viewed as unsuitable to be wives and mothers in a German family.<ref name="NWC187">{{Harvnb|Proctor|2000|p=187}}</ref> In the 20th century, smoking was common. There were social events like the ] which promoted the habit. | |||
| The ] did not reach across enemy lines during the Second World War, as anti-smoking groups quickly lost popular support. By the end of the Second World War, American cigarette manufacturers quickly reentered the German black market. Illegal smuggling of tobacco became prevalent,<ref name="NWC245">{{Harvnb|Proctor|2000|p=245}}</ref> and leaders of the Nazi anti-smoking campaign were silenced.<ref name="ADLNMPHP">{{cite journal |last1=Proctor |first1=Robert N. |title=Nazi Medicine and Public Health Policy |journal=Dimensions |year=1996 |volume=10 |issue=2 |url=http://www.adl.org/Braun/dim_14_1_nazi_med.asp |archive-url=https://archive.today/20121205091200/http://www.adl.org/Braun/dim_14_1_nazi_med.asp |archive-date=5 December 2012 |publisher=] |via=archived copy at ] |access-date=1 October 2018 |url-status=live }}</ref> As part of the ], the United States shipped free tobacco to Germany; with 24,000 tons in 1948 and 69,000 tons in 1949.<ref name="NWC245"/> Per capita yearly cigarette consumption in ] steadily rose from 460 in 1950 to 1,523 in 1963.<ref name="NWC228">{{Harvnb|Proctor|2000|p=228}}</ref> By the end of the 20th century, anti-smoking campaigns in Germany were unable to exceed the effectiveness of the Nazi-era climax in the years 1939–41 and German tobacco health research was described by ] as "muted".<ref name="NWC228"/> | |||
| Some studies suggests that hookah smoking is considered to be safer than other forms of smoking. However, water is not effective for removing all relevant toxins, e.g. the carcinogenic aromatic hydrocarbons are not water-soluble. Several negative health effects are linked to hookah smoking and studies indicate that it is likely to be more harmful than cigarettes, due in part to the volume of smoke inhaled. <ref> </ref> <ref> </ref> In addition to the cancer risk, there is some risk of infectious disease resulting from pipe sharing, and other risks associated with the common addition of other psychoactive drugs to the tobacco.<ref> </ref> | |||
| ] | |||
| ====Carcinogenicity==== | |||
| {{main|Carcinogen}} | |||
| ] | |||
| ], a polynuclear aromatic hydrocarbon, produced by burning tobacco.]] | |||
| Smoke, or any partially burnt organic matter, is ]ic (cancer-causing). The damage a continuing smoker does to their lungs can take up to 20 years before its physical manifestation in lung cancer. Women began smoking later than men, so the rise in death rate amongst women did not appear until later. The male lung cancer death rate decreased in 1975 — roughly 20 years after the fall in cigarette consumption in men. A fall in consumption in women also began in 1975 but by 1991 had not manifested in a decrease in lung cancer related mortalities amongst women.<ref>{{cite book | author=Mary Jones, Richard Fosbery, Dennis Taylor | title=Biology 1 | chapter=Answers to self-assessment questions | pages=p.250 | publisher=Cambridge Advanced Sciences | id=ISBN 0-521-78719-X.}}</ref> | |||
| In 1950, ] published research in the '']'' showing a close link between smoking and ].<ref>{{cite journal | last1 = Doll | first1 = R. | last2 = Hill | first2 = A. B. | title = Smoking and Carcinoma of the Lung | journal = British Medical Journal | volume = 2 | issue = 4682 | pages = 739–748 | date = 1 September 1950 | pmid = 14772469 | pmc = 2038856 | doi = 10.1136/bmj.2.4682.739 | issn = 0007-1447 }}</ref> Beginning in December 1952, the magazine '']'' published "Cancer by the Carton", a series of articles that linked ] with ].<ref>{{Cite news |url=http://www.cnn.com/US/9705/tobacco/history/ |title=CNN Interactive |publisher=Cnn.com |access-date=22 June 2009 |archive-date=23 April 2009 |archive-url=https://web.archive.org/web/20090423205623/http://www.cnn.com/US/9705/tobacco/history/ |url-status=live }}</ref> | |||
| Smoke contains several carcinogenic ] products, particularly the ] (PAH), which are ] to ] epoxides. The first PAH to be identified as a carcinogen in tobacco smoke was ], which been shown to permanently attach to nuclear DNA, which may either kill the cell or cause a ]. If the mutation inhibits ], the cell can survive to become a ]. | |||
| In 1954, the ], a prospective study of some 40 thousand doctors for about 2.5 years, confirmed the suggestion, based on which the government issued advice that smoking and lung cancer rates were related.<ref name="RichardHillyBMJ1954">{{cite journal | last1 = Doll | first1 = R. | last2 = Hill | first2 = B. | title = The mortality of doctors in relation to their smoking habits: a preliminary report: (Reprinted from Br Med J 1954:ii;1451-5) | journal = BMJ (Clinical Research Ed.) | volume = 328 | issue = 7455 | pages = 1529–1533; discussion 1533 | date = Jun 2004 | pmid = 15217868 | pmc = 437141 | doi = 10.1136/bmj.328.7455.1529 | issn = 0959-8138 }}</ref> In January 1964, the United States ]'s Report on Smoking and Health likewise began suggesting the relationship between smoking and cancer.<ref>{{cite web|url= http://profiles.nlm.nih.gov/ps/retrieve/Narrative/NN/p-nid/60|title= The Reports of the Surgeon General: The 1964 Report on Smoking and Health|work= Profiles in Science|publisher= ], ]|access-date= 10 October 2015|archive-date= 20 January 2016|archive-url= https://web.archive.org/web/20160120031958/http://profiles.nlm.nih.gov/ps/retrieve/Narrative/NN/p-nid/60|url-status= live}}</ref> | |||
| The carcinogenity of tobacco smoke is not explained by ] per se, which is not carcinogenic or mutagenic. However, it inhibits ], therefore accelerating existing cancers.<ref>{{cite journal| author = Maneckjee, R. |title = Opioids induce while nicotine suppresses apoptosis in human lung cancer cells |journal = Cell Growth and Differentiation: The Molecular Biology Journal of the American Association of Cancer Research | volume = 5| issue = 10| pages = 1033-40 |date=1994 |PMID= 7848904 }}</ref> Also, NNK, a nicotine derivative converted from nicotine, can be carcinogenic. Thus, to reduce cancer risk{{Fact|date=February 2008}} but to deliver nicotine, there are tobacco products where the tobacco is not pyrolysed, but the nicotine is vaporized with solvent such as glycerol{{Fact|date=February 2008}}. | |||
| As scientific evidence mounted in the 1980s, tobacco companies claimed ] as the adverse health effects were previously unknown or lacked substantial credibility. Health authorities sided with these claims up until 1998, from which they reversed their position. The ], originally between the four largest US tobacco companies and the attorneys general of 46 states, restricted certain types of tobacco advertisement and required payments for health compensation; which later amounted to the largest civil settlement in United States history.<ref name="WallStreetJournalTobaccoMastersSettlement">{{cite news|newspaper=]|title=Forty-Six States Agree to Accept $206 Billion Tobacco Settlement|date=23 November 1998|author=Milo Geyelin}}</ref> | |||
| ==== Lung dysfunction ==== | |||
| ] (COPD) caused by smoking, known as tobacco disease, is a permanent, incurable reduction of pulmonary capacity characterized by shortness of breath, wheezing, persistent cough with ], and damage to the lungs, including ] and ]<ref>Devereux G. ABC of chronic obstructive pulmonary disease. Definition, epidemiology, and risk factors. BMJ 2006;332:1142-1144. PMID 16690673</ref>. | |||
| Social campaigns have been instituted in many places to discourage smoking, such as Canada's ]. | |||
| ====Effects on the heart==== | |||
| Smoking contributes to the risk of developing heart disease. All smoke contains very fine particulates that are able to penetrate the alveolar wall into the blood and exert their effects on the heart in a short time. | |||
| From 1965 to 2006, rates of smoking in the United States declined from 42% to 20.8%.<ref name="RockEtAlCDC2006">{{Cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm|title=Cigarette Smoking Among Adults --- United States, 2006|access-date=1 January 2009|author=VJ Rock, MPH, A Malarcher, JW Kahende, K Asman, MSPH, C Husten, MD, R Caraballo|date=9 November 2007|publisher=United States Centers for Disease Control and Prevention|quote=In 2006, an estimated 20.8% (45.3 million) of U.S. adults|archive-date=16 August 2019|archive-url=https://web.archive.org/web/20190816014306/https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm|url-status=live}}</ref> The majority of those who quit were professional, affluent men. Although the per-capita number of smokers decreased, the average number of cigarettes consumed per person per day increased from 22 in 1954 to 30 in 1978. This paradoxical event suggests that those who quit smoked less, while those who continued to smoke moved to smoke more light cigarettes.<ref>{{Cite book|last=Hilton|first=Matthew|title=Smoking in British Popular Culture, 1800–2000: Perfect Pleasures|url=https://books.google.com/books?id=UjM8t6Ul73YC&q=Smoking+in+British+Popular+Culture|access-date=22 March 2009|date=4 May 2000|publisher=Manchester University Press|isbn=978-0-7190-5257-6|pages=229–241|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114064553/https://books.google.com/books?id=UjM8t6Ul73YC&q=Smoking+in+British+Popular+Culture|url-status=live}}</ref> The trend has been paralleled by many industrialized nations as rates have either leveled-off or declined. In the ], however, tobacco consumption continued to rise at 3.4% in 2002.<ref name="WHO2002FactSheet">{{Cite web|url=http://www.wpro.who.int/media_centre/fact_sheets/fs_20020528.htm|title=WHO/WPRO-Smoking Statistics|access-date=1 January 2009|date=28 May 2002|publisher=World Health Organization Regional Office for the Western Pacific|url-status=dead|archive-url=https://web.archive.org/web/20091108181404/http://www.wpro.who.int/media_centre/fact_sheets/fs_20020528.htm|archive-date=8 November 2009}}</ref> In Africa, smoking is in most areas considered to be modern, and many of the strong adverse opinions that prevail in the West receive much less attention.<ref>{{Harvnb|Gilman|Xun|2004|pp=46–57}}</ref> Today Russia leads as the top consumer of tobacco followed by ], ], ], ], Greece, ], and China.<ref name="MPOWER 2008 pp=267–288">{{harvnb|MPOWER|2008|pp=267–288}}</ref> | |||
| Inhalation of tobacco smoke causes several immediate responses within the heart and blood vessels. Within one minute the heart rate begins to rise, increasing by as much as 30 percent during the first 10 minutes of smoking. Carbon monoxide in tobacco smoke exerts its ] by reducing the blood’s ability to carry oxygen<ref>Haldane J. (1895). "The action of carbonic oxide on man". J Physiol 18: 430-62</ref>. | |||
| ==Consumption== | |||
| Smoking tends to increase blood cholesterol levels. Furthermore, the ratio of high-density lipoprotein (the “good” cholesterol) to low-density lipoprotein (the “bad” cholesterol) tends to be lower in smokers compared to non-smokers. Smoking also raises the levels of fibrinogen and increases platelet production (both involved in blood clotting) which makes the blood viscous. Carbon monoxide binds to haemoglobin (the oxygen-carrying component in red blood cells), resulting in a much stabler complex than haemoglobin bound with oxygen or carbon dioxide -- the result is permanent loss of blood cell functionality. Blood cells are naturally recycled after a certain period of time, allowing for the creation of new, functional erythrocytes. However, if carbon monoxide exposure reaches a certain point before they can be recycled, hypoxia (and later death) occurs. All these factors make smokers more at risk of developing various forms of arteriosclerosis. As the arteriosclerosis progresses, blood flows less easily through rigid and narrowed blood vessels, making the blood more likely to form a thrombosis (clot). Sudden blockage of a blood vessel may lead to an infarction (e.g. stroke). However, it is also worth noting that the effects of smoking on the heart may be more subtle. These conditions may develop gradually given the smoking-healing cycle (the human body heals itself between periods of smoking), and therefore a smoker may develop less significant disorders such as worsening or maintenance of unpleasant dermatological conditions, e.g. eczema, due to reduced blood supply. Smoking also increases blood pressure and weakens blood vessels<ref>Narkiewicz K, Kjeldsen SE, Hedner T. Is smoking a causative factor of hypertension? Blood Press. 2005;14(2):69-71. PMID 16036482</ref>. | |||
| === |
===Methods=== | ||
| {{Hatnote|For more about the production of the agricultural product, see ], ], ], and ]}} | |||
| ] is an addictive ] and is one of the main factors leading to continued tobacco smoking. Although the percentage of the nicotine inhaled with tobacco smoke is quite small (most of the substance is destroyed by the heat){{Fact|date=February 2008}} it is still sufficient to cause physical and/or psychological ]. | |||
| ] is an agricultural product processed from the fresh leaves of plants in the genus '']''. The genus contains several species, of which '']'' is the most commonly grown. '']'' follows second, containing higher concentrations of nicotine. The leaves are harvested and cured to allow the slow ] and degradation of ]s in tobacco leaf. This produces certain compounds in the tobacco leaves which can be attributed to sweet hay, tea, rose oil, or fruity aromatic flavors. Before packaging, the tobacco is often combined with other additives in order to increase the addictive potency, shift the product's ], or improve the effects of smoke by making it more palatable. In the United States these additives are regulated to ].<ref name="WHOJeffreyWigand"/> The product is then processed, packaged, and shipped to consumer markets. | |||
| Prior to habituation, tobacco smokers often focus on the reinforcing properties of smoking rather than the associated health risks{{Fact|date=February 2008}}. The diseases caused by smoking surface relatively later in life. As a result, they do not serve to deter smoking given the immediate gratification offered by smoking. | |||
| Common methods of consuming tobacco include the following: | |||
| Some smokers argue{{Fact|date=February 2008}} that the ] effect of smoking allows them to calm their nerves, often allowing for increased concentration. However, according to the ], "Nicotine seems to provide both a stimulant and a depressant effect, and it is likely that the effect it has at any time is determined by the mood of the user, the environment and the circumstances of use. Studies have suggested that low doses have a depressant effect, whilst higher doses have stimulant effect."<ref> </ref> However, it is impossible to differentiate a drug effect brought on by nicotine use, and the alleviation of nicotine withdrawal. | |||
| {{multiple image | |||
| | align = right | |||
| | direction = vertical | |||
| | width = 180 | |||
| | image1 = Patch of Tobacco (Nicotiana tabacum ) in a field in Intercourse, Pennsylvania..jpg | |||
| | alt1 = Field of tobacco organized in rows extending to the horizon. | |||
| | caption1 = Tobacco field in ] | |||
| | image2 = Basma-tobacco-drying.jpg | |||
| | alt2 = Powderly stripps hung vertically, slightly sun bleached. | |||
| | caption2 = ] leaves curing in the sun at ] village of ], Thrace, Greece | |||
| | image3 = DunhillLightFlake.jpg | |||
| | alt3 = Rectangular strips stacked in an open square box. | |||
| | caption3 = Processed tobacco pressed into flakes for pipe smoking | |||
| | total_width = | |||
| }} | |||
| ;Beedi: ]s are thin South Asian cigarettes filled with tobacco flakes and wrapped in a tendu leaf tied with a string at one end. They produce higher levels of carbon monoxide, nicotine, and tar than cigarettes typical in the United States.<ref>{{Cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4836a2.htm|title=Bidi Use Among Urban Youth – Massachusetts, March–April 1999|access-date=14 February 2009|date=17 September 1999|publisher=Centers for Disease Control and Prevention|archive-date=11 February 2009|archive-url=https://web.archive.org/web/20090211061406/http://www.cdc.gov/mmwr/preview/mmwrhtml/mm4836a2.htm|url-status=live}}</ref><ref>{{cite journal | last1 = Pakhale | first1 = S. M. | last2 = Maru | first2 = G. B. | title = Distribution of major and minor alkaloids in tobacco, mainstream and sidestream smoke of popular Indian smoking products | journal = Food and Chemical Toxicology | volume = 36 | issue = 12 | pages = 1131–1138 | date = Dec 1998 | pmid = 9862656 | doi = 10.1016/S0278-6915(98)00071-4 | issn = 0278-6915 }}</ref> | |||
| ===Passive smoking=== | |||
| {{main|Passive smoking}} | |||
| ], a common complaint from those concerned with passive smoking. Smoking in public places has now been banned in the United Kingdom, As of July 1st 2007.]] | |||
| Passive or involuntary smoking occurs when the exhaled and ambient smoke (otherwise known as environmental or secondhand smoke) from one person's cigarette is inhaled by other people. Passive smoking involves inhaling carcinogens, as well as other toxic components, that are present in secondhand tobacco smoke. | |||
| ] | |||
| Secondhand smoke is known to harm children, infants and reproductive health through acute lower respiratory tract illness, asthma induction and exacerbation, chronic respiratory symptoms, middle ear infection, lower birth weight babies, and ]. In a study published on ], ] smoke-free policies have been linked to a short-term reduction in admissions for AMI <ref> </ref>.<ref> </ref> In a study released on ], ] warning signs for cardiovascular disease are higher in people exposed to secondhand tobacco smoke, adding to the link between "passive smoke" and heart disease. "Our study provides further evidence to suggest low-level exposure to secondhand smoke has a clinically important effect on susceptibility to cardiovascular disease," said Dr. Andrea Venn of University of Nottingham in Britain, lead author of the study.<ref name="NewsMax">"". ], ], ].</ref> | |||
| ;Cigars: ]s are tightly rolled bundles of dried and fermented tobacco which are ignited so that smoke may be drawn into the smoker's mouth. They are generally not inhaled because of the high alkalinity of the smoke, which can quickly become irritating to the trachea and lungs. The prevalence of cigar smoking varies depending on location, historical period, and population surveyed, and prevalence estimates vary somewhat depending on the survey method. The United States is the top consuming country by far, followed by Germany and the United Kingdom; the US and Western Europe account for about 75% of cigar sales worldwide.<ref name="Rarick">{{Cite journal|ssrn=1127582|author=Rarick CA|title=Note on the premium cigar industry|date=2 April 2008|doi=10.2139/ssrn.1127582 |s2cid=152340055 }}</ref> As of 2005 it is estimated that 4.3% of men and 0.3% of women smoke cigars in the US.<ref>{{Cite journal|journal=MMWR Morb Mortal Wkly Rep|year=2006|volume=55|issue=42|pages=1145–8|title=Tobacco use among adults—United States, 2005|vauthors=Mariolis P, Rock VJ, Asman K|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5542a1.htm|pmid=17065979|display-authors=etal|access-date=17 September 2017|archive-date=26 September 2017|archive-url=https://web.archive.org/web/20170926235944/https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5542a1.htm|url-status=live}}</ref> | |||
| According to the U.S. Surgeon General’s Report (; pages 180–194), secondhand smoke is connected to SIDS.<ref>{{citeweb |url=http://www.surgeongeneral.gov/news/speeches/06272006a.html |title=Remarks at press conference to launch Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General |accessdate=2007-07-10}}</ref> Infants who die from SIDS tend to have higher concentrations of nicotine and ] (a biological marker for secondhand smoke exposure) in their lungs than those who die from other causes. Infants exposed to secondhand smoke after birth are also at a greater risk of SIDS. | |||
| ;Cigarettes: '']s'', French for "small cigar", are a product consumed through smoking and manufactured out of cured and finely cut tobacco leaves and reconstituted tobacco, often combined with other additives, which are then rolled or stuffed into a paper-wrapped cylinder.<ref name="WHOJeffreyWigand">{{Cite web|url=http://www.jeffreywigand.com/WHOFinal.pdf|title=ADDITIVES, CIGARETTE DESIGN and TOBACCO PRODUCT REGULATION|access-date=14 February 2009|last=Wigand|first=Jeffrey S.|date=July 2006|publisher=Jeffrey Wigand|location=Mt. Pleasant, MI 48804|archive-date=16 May 2011|archive-url=https://web.archive.org/web/20110516151158/http://www.jeffreywigand.com/WHOFinal.pdf|url-status=live}}<!-- RELIABLE ONLY FOR DEFINITION OF CIGARETTE --></ref> Cigarettes are ignited and inhaled, usually through a cellulose acetate filter, into the mouth and lungs. | |||
| A young waitress who had asthma died at her workplace after being exposed to environmental tobacco smoke. While at her workplace she collapsed after about 20 minutes and then died. The autopsy proved that the woman died from acute asthma, which was associated with work-related ETS(]). | |||
| {{anchor|French inhale}} | |||
| According to earlier studies the smoking ban led to significant improvements regarding respiratory symptoms and lung function in people visiting bars and restaurants. Previously scientists stated that environmental tobacco smoke leads to coronary heart disease, lung cancer and premature death. | |||
| ;Hookah: '']'' are a single or multi-stemmed (often glass-based) water pipe for smoking. Originally from India, the hookah was a symbol of pride and honor for the landlords, kings and other such high class people. Now, the hookah has gained immense popularity, especially in the Middle East. A hookah operates by water filtration and indirect heat. It can be used for smoking herbal fruits, tobacco, or ]. | |||
| ;Kretek: '']'' are cigarettes made with a complex blend of tobacco, ]s and a flavoring "sauce". It was first introduced in the 1880s in Kudus, Java, to deliver the medicinal eugenol of cloves to the lungs. The quality and variety of tobacco play an important role in kretek production, from which kretek can contain more than 30 types of tobacco. Minced dried clove buds weighing about one-third of the tobacco blend are added to add flavoring. In 2004 the United States prohibited cigarettes from having a "characterizing flavor" of certain ingredients other than tobacco and menthol, thereby removing kretek from being classified as cigarettes.<ref>{{Cite press release|url=http://thomas.loc.gov/cgi-bin/bdquery/z?d108:SN02461:@@@D&summ2=m&|access-date=1 August 2007|publisher=Library of Congress|title=A bill to protect the public health by providing the Food and Drug Administration with certain authority to regulate tobacco products. (Summary)|date=20 May 2004|archive-date=4 September 2015|archive-url=https://web.archive.org/web/20150904081039/http://thomas.loc.gov/cgi-bin/bdquery/z?d108:SN02461:@@@D&summ2=m&|url-status=dead}}</ref> | |||
| ;Pipe smoking: ] is done with a tobacco pipe, typically consisting of a small chamber (the bowl) for the combustion of the tobacco to be smoked and a thin stem (shank) that ends in a mouthpiece (the bit). Shredded pieces of tobacco are placed into the chamber and ignited. | |||
| ;Roll-your-own: ] or hand-rolled cigarettes, often called "rollies", "cigi" or "Roll-ups", are very popular particularly in European countries and the UK. These are prepared from loose tobacco, cigarette papers, and filters all bought separately. They are usually much cheaper than ready-made cigarettes and small contraptions can be bought making the process easier. | |||
| ;Vaporizer: A ] is a device used to sublimate the active ingredients of plant material. Rather than burning the herb, which produces potentially irritating, toxic, or ]ic by-products; a vaporizer heats the material in a partial vacuum so that the active compounds contained in the plant boil off into a vapor. This method is often preferable when medically administering the smoke substance, as opposed to directly pyrolyzing the plant material. | |||
| ===Physiology=== | |||
| The case is available in the February edition of the ].<ref></ref> | |||
| {{See also|Chain smoking}} | |||
| ] | |||
| The active substances in tobacco, especially cigarettes, are administered by burning the leaves and inhaling the vaporized gas that results. This quickly and effectively delivers substances into the bloodstream by ] through the ] in the lungs. The lungs contain some 300 million alveoli, which amounts to a surface area of over 70 m<sup>2</sup> (about the size of a tennis court). This method is not completely efficient as not all of the smoke will be inhaled, and some amount of the active substances will be lost in the process of combustion, ].<ref name="GilmanXun2004p318">{{Harvnb|Gilman|Xun|2004|p=318}}</ref> Pipe and Cigar smoke are not inhaled because of its high ], which are irritating to the ] and lungs. However, because of its higher alkalinity (pH 8.5) compared to cigarette smoke (pH 5.3), non-ionized nicotine is more readily absorbed through the ] in the mouth.<ref>{{cite journal | last1 = Turner | first1 = JA | last2 = Sillett | first2 = RW | last3 = McNicol | first3 = MW | title = Effect of cigar smoking on carboxyhemoglobin and plasma nicotine concentrations in primary pipe and cigar smokers and ex-cigarette smokers | journal = British Medical Journal | volume = 2 | issue = 6099 | pages = 1387–9 | year = 1977 | pmid = 589225 | pmc = 1632361 | doi = 10.1136/bmj.2.6099.1387 }}</ref> Nicotine absorption from cigar and pipe, however, is much less than that from cigarette smoke.<ref>{{cite journal | last1 = Armitage | first1 = A. K. | last2 = Turner | first2 = D. M. | title = Absorption of Nicotine in Cigarette and Cigar Smoke through the Oral Mucosa | journal = Nature | volume = 226 | issue = 5252 | pages = 1231–1232 | year = 1970 | pmid = 5422597 | doi = 10.1038/2261231a0 | bibcode = 1970Natur.226.1231A | s2cid = 4208650 }}</ref> Nicotine and cocaine activate similar patterns of neurons, which supports the existence of common ] among these drugs.<ref>{{cite journal | last1 = Pich | first1 = E. M. | last2 = Pagliusi | first2 = S. R. | last3 = Tessari | first3 = M. | last4 = Talabot-Ayer | first4 = D. | last5 = Hooft Van Huijsduijnen | first5 = R. | last6 = Chiamulera | first6 = C. | title = Common neural substrates for the addictive properties of nicotine and cocaine | journal = Science | volume = 275 | issue = 5296 | pages = 83–86 | year = 1997 | pmid = 8974398 | doi = 10.1126/science.275.5296.83 | s2cid = 5923174 }}</ref> | |||
| ===Somatic and psychological effects=== | |||
| ] is a highly addictive psychoactive chemical. When tobacco is smoked, most of the nicotine is ]; a dose sufficient to cause mild somatic dependency and mild to strong psychological dependency remains. There is also a formation of ] (a ]) from the acetaldehyde in cigarette smoke, which seems to play an important role in nicotine addiction <ref> </ref> probably by facilitating dopamine release in the nucleus accumbens in response to nicotine stimuli. According to studies by Henningfield and Benowitz, overall nicotine is more addictive than ], ], ], ], and ] when considering both somatic and psychological dependence. However, due to the stronger withdrawal effects of ], ] and ], nicotine may have a lower potential for somatic dependence than these substances.<ref> </ref><ref> </ref> A study by Perrine concludes that nicotine's potential for psychological dependency exceeds all other studied drugs<ref> </ref> - even ethanol, an extremely physically addictive substance with severe ] symptoms that can be fatal. About half of Canadians who currently smoke have tried to quit.<ref> </ref> ] health professor Jennifer O'Loughlin stated that nicotine addiction can occur as soon as five months after the start of smoking.<ref> ''The London Free Press'' (August 2, 2006).</ref> | |||
| The absorbed ] mimics nicotinic acetylcholine which when bound to ]s prevents the reuptake of ] thereby increasing that ] in those areas of the body.<ref name="WonnacottPMID9023878">{{cite journal | last1 = Wonnacott | first1 = S. | title = Presynaptic nicotinic ACh receptors | journal = Trends in Neurosciences | volume = 20 | issue = 2 | pages = 92–8| year = 1997 | pmid = 9023878 | doi = 10.1016/S0166-2236(96)10073-4 | s2cid = 42215860 }}</ref> These nicotinic acetylcholine receptors are located in the central nervous system and at the nerve-muscle junction of skeletal muscles; whose activity increases heart rate, alertness,<ref name="PMID2498936">{{cite journal | last1 = Parrott | first1 = A. C. | last2 = Winder | first2 = G. | title = Nicotine chewing gum (2 mg, 4 mg) and cigarette smoking: comparative effects upon vigilance and heart rate | journal = Psychopharmacology | volume = 97 | issue = 2 | pages = 257–261 | year = 1989 | pmid = 2498936 | doi = 10.1007/BF00442260 | s2cid = 4842374 }}</ref> and faster reaction times.<ref name="WesnessWarburton1997">{{cite journal | last1 = Parkin | first1 = C. | last2 = Fairweather | first2 = D. B. | last3 = Shamsi | first3 = Z. | last4 = Stanley | first4 = N. | last5 = Hindmarch | first5 = I. | title = The effects of cigarette smoking on overnight performance | journal = Psychopharmacology | volume = 136 | issue = 2 | pages = 172–178 | year = 1998 | pmid = 9551774 | doi = 10.1007/s002130050553 | s2cid = 22962937 }}</ref> Nicotine acetylcholine stimulation is not directly addictive. However, since dopamine-releasing neurons are abundant on nicotine receptors, dopamine is released; and, in the ], dopamine is associated with motivation causing ] behavior.<ref>{{cite journal | last1 = Pontieri | first1 = F. E. | last2 = Tanda | first2 = G. | last3 = Orzi | first3 = F. | last4 = Di Chiara | first4 = G. D. | title = Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs | journal = Nature | volume = 382 | issue = 6588 | pages = 255–257 | year = 1996 | pmid = 8717040 | doi = 10.1038/382255a0 | bibcode = 1996Natur.382..255P | s2cid = 4338516 }}</ref> Dopamine increase, in the ], may also increase ].<ref>{{cite journal | last1 = Guinan | first1 = M. E. | last2 = Portas | first2 = M. R. | last3 = Hill | first3 = H. R. | title = The candida precipitin test in an immunosuppressed population | journal = Cancer | volume = 43 | issue = 1 | pages = 299–302 | year = 1979 | pmid = 761168 | doi = 10.1002/1097-0142(197901)43:1<299::AID-CNCR2820430143>3.0.CO;2-D | s2cid = 45096870 }}</ref> | |||
| Recent evidence has shown that smoking tobacco increases the release of ] in the brain, specifically in the mesolimbic pathway, the same neuro-reward circuit activated by drugs of abuse such as ] and ]. This suggests nicotine use has a pleasurable effect that triggers positive reinforcement.<ref> </ref> One study found that smokers exhibit better reaction-time and memory performance compared to non-smokers, which is consistent with increased activation of dopamine receptors.<ref> </ref> Neurologically, rodent studies have found that nicotine self-administration causes lowering of reward thresholds--a finding opposite that of most other drugs of abuse (e.g. cocaine and heroin). This increase in reward circuit sensitivity persisted months after the self-administration ended, suggesting that nicotine's alteration of brain reward function is either long lasting or permanent. Furthermore, it has been found that nicotine can activate long term potentiation ''in vivo'' and ''in vitro''. These studies suggests nicotine’s "trace memory" may contribute to difficulties in nicotine abstinence. | |||
| When tobacco is smoked, most of the nicotine is pyrolyzed. However, a dose sufficient to cause mild somatic dependency and mild to strong psychological dependency remains. There is also a formation of ] (an ]) from the acetaldehyde in tobacco smoke. This may play a role in nicotine addiction, by facilitating a dopamine release in the ] as a response to nicotine stimuli.<ref>{{cite journal | last1 = Talhout | first1 = R. | last2 = Opperhuizen | first2 = A. | last3 = Van Amsterdam | first3 = J. G. C. | title = Role of acetaldehyde in tobacco smoke addiction | journal = European Neuropsychopharmacology | volume = 17 | issue = 10 | pages = 627–636 | date = Oct 2007 | pmid = 17382522 | doi = 10.1016/j.euroneuro.2007.02.013 | s2cid = 25866206 | issn = 0924-977X }}</ref> Using rat studies, withdrawal after repeated exposure to nicotine results in less responsive nucleus accumbens cells, which produce dopamine responsible for ].<ref>{{cite journal | last1 = Shoaib | first1 = M. | last2 = Lowe | first2 = A. | last3 = Williams | first3 = S. | title = Imaging localised dynamic changes in the nucleus accumbens following nicotine withdrawal in rats | journal = NeuroImage | volume = 22 | issue = 2 | pages = 847–854 | year = 2004 | pmid = 15193614 | doi = 10.1016/j.neuroimage.2004.01.026 | s2cid = 43544025 }}</ref> | |||
| ===Mood and anxiety disorders=== | |||
| Recent studies have linked smoking to anxiety disorders, suggesting the correlation (and possibly mechanism) may be related to the broad class of anxiety disorders, and not limited to just depression. Current ongoing research are attempting to explore the addiction-anxiety relationship. | |||
| ===Demographics=== | |||
| Data from multiple studies suggest that anxiety disorders such as depression play a role in cigarette smoking.<ref> </ref> | |||
| {{Main|Prevalence of tobacco use}} | |||
| A history of regular smoking was observed more frequently among individuals who had experienced a ] at some time in their lives than among individuals who had never experienced major depression or among individuals with no psychiatric diagnosis.<ref> </ref> People with major depression are also much less likely to ] due to the increased risk of experiencing mild to severe states of depression, including a major depressive episode.<ref> </ref> Depressed smokers appear to experience more withdrawal symptoms on quitting, are less likely to be successful at quitting, and are more likely to relapse.<ref> </ref> | |||
| {{Multiple image | |||
| ===Health benefits of smoking=== | |||
| | direction = vertical | |||
| Studies suggest that smoking decreases appetite.<ref>News-Medical.Net, , accessed on Jan 3, 2008</ref><ref>mytelus.com, , accessed on Jan 3, 2008</ref> but did not conclude that overweight people should smoke or that their health would improve by smoking. | |||
| | align = right | |||
| | image1 = Male Smoking by Country.png | |||
| | image2 = Female Smoking by Country.png | |||
| | width = 200 | |||
| | caption1 = Percentage of '''males''' smoking any tobacco product | |||
| | caption2 = Percentage of '''females''' smoking any tobacco product. Note that there is a difference between the scales used for males and the scales used for females.<ref name="MPOWER 2008 pp=267–288"/> | |||
| }} | |||
| As of 2000, smoking was practiced by around 1.22 billion people. At current rates of 'smoker replacement' and market growth, this may reach around 1.9 billion in 2025.<ref name="HNPGuindonBoisclair13-16">{{Cite journal|first1=G. Emmanuel|last1=Guindon|first2=David|last2=Boisclair|title=Past, current and future trends in tobacco use|url=http://www1.worldbank.org/tobacco/pdf/Guindon-Past,%20current-%20whole.pdf|access-date=22 March 2009|year=2003|publisher=The International Bank for Reconstruction and Development / The World Bank|location=Washington DC|pages=13–16|archive-url=https://web.archive.org/web/20090318003729/http://www1.worldbank.org/tobacco/pdf/Guindon-Past,%20current-%20whole.pdf|archive-date=18 March 2009|url-status=dead}}</ref> | |||
| Several types of "Smoker’s Paradoxes",<ref name="cohen"> | |||
| {{cite journal | |||
| | last = Cohen | |||
| | first = David J. | |||
| | authorlink = | |||
| | coauthors = Michel Doucet, Donald E. Cutlip, Kalon K.L. Ho, Jeffrey J. Popma, Richard E. Kuntz | |||
| | title = Impact of Smoking on Clinical and Angiographic Restenosis After Percutaneous Coronary Intervention | |||
| | journal = Circulation | |||
| | volume = 104 | |||
| | issue = | |||
| | pages = 773 | |||
| |date=2001 | |||
| | url = http://www.data-yard.net/34/circulation_2001_104_773.htm | |||
| | doi = | |||
| | id = | |||
| | accessdate = 2006-11-06}} | |||
| </ref> (cases where smoking appears to have specific beneficial effects), have been observed; often the actual mechanism remains undetermined. Risk of ] has been frequently shown to be reduced by smokers on a dose-dependent basis; the effect is eliminated if the individual stops smoking.<ref name="ohcm">Longmore, M., Wilkinson, I., Torok, E. Oxford Handbook of Clinical Medicine (Fifth Edition) p. 232</ref><ref> | |||
| {{cite journal | |||
| | last = Green | |||
| | first = JT | |||
| | authorlink = | |||
| | coauthors = Richardson C, Marshall RW, Rhodes J, McKirdy HC, Thomas GA, Williams GT | |||
| | title = Nitric oxide mediates a therapeutic effect of nicotine in ulcerative colitis | |||
| | journal = Aliment Pharmacol Ther | |||
| | volume = 14 | |||
| | issue = 11 | |||
| | pages = 1429–1434 | |||
| |date=November, 2000 | |||
| | url = http://www.data-yard.net/22/ncbi.htm | |||
| | doi = | |||
| | id =PMID: 11069313 | |||
| | accessdate = 2006-11-06}}</ref> | |||
| Smoking appears to interfere with development of ],<ref> | |||
| {{cite news | |||
| | last = | |||
| | first = | |||
| | coauthors = | |||
| | title = Smoking Cuts Risk of Rare Cancer | |||
| | work = | |||
| | pages = | |||
| | language = English | |||
| | publisher = UPI | |||
| |date=March 29, 2001 | |||
| | url = http://www.data-yard.net/10b/kaposi.htm | |||
| | accessdate = 2006-11-06}} | |||
| </ref> | |||
| ] among women carrying the very high risk ] gene,<ref> | |||
| {{cite news | |||
| | last = Recer | |||
| | first = Paul | |||
| | coauthors = | |||
| | title = Cigarettes May Have an Up Side | |||
| | work = | |||
| | pages = | |||
| | language = English | |||
| | publisher = AP | |||
| |date=May 19, 1998 | |||
| | url = http://www.forces.org/evidence/files/brea.htm | |||
| | accessdate = 2006-11-06}} | |||
| </ref>{{Fact|date=November 2007}} | |||
| ],<ref> | |||
| {{cite journal | |||
| | last = Lain | |||
| | first = Kristine Y. | |||
| | authorlink = | |||
| | coauthors = Robert W. Powers, Marijane A. Krohn, Roberta B. Ness, William R. Crombleholme, | |||
| James M. Roberts | |||
| | title = Urinary cotinine concentration confirms the reduced risk of preeclampsia with tobacco exposure | |||
| | journal = American Journal of Obstetrics and Gynecology | |||
| | volume = 181 | |||
| | issue = 5 | |||
| | pages = 908-14 | |||
| |date=November 1991 | |||
| | url = http://www.data-yard.net/2/13/ajog.htm | |||
| | doi = | |||
| | id = PMID: 11422156 | |||
| | accessdate = 2006-11-06}} | |||
| </ref> | |||
| and ]s such as ].<ref> | |||
| {{cite journal | |||
| | last = Hjern | |||
| | first = A | |||
| | authorlink = | |||
| | coauthors = Hedberg A, Haglund B, Rosen M | |||
| | title = Does tobacco smoke prevent atopic disorders? A study of two generations of Swedish residents | |||
| | journal = Clin Exp Allergy | |||
| | volume = 31 | |||
| | issue = 6 | |||
| | pages = 908–914 | |||
| | publisher = | |||
| |date=June 2001 | |||
| | url = http://www.data-yard.net/30/asthma.htm | |||
| | doi = | |||
| | id = PMID: 11422156 | |||
| | accessdate = 2006-11-06}}</ref> | |||
| A plausible mechanism of action in these cases may be the ] in tobacco smoke acting as an ] and interfering with the disease process.<ref name="sciam">{{cite journal | author=Lisa Melton | title=Body Blazes | journal=Scientific American |date=June 2006 | pages=p.24 | url=http://www.sciam.com/article.cfm?chanID=sa006&colID=5&articleID=00080902-A2CF-146C-9D1E83414B7F0000}}</ref> | |||
| Smoking may be up to five times more prevalent among men than women in some communities,<ref name="HNPGuindonBoisclair13-16"/> although the gender gap usually declines with younger age.<ref name="WomenTobaccoChallenges5-6">{{Cite web|url=https://www.who.int/tobacco/media/en/WomenMonograph.pdf|archive-url=https://web.archive.org/web/20031128122821/http://www.who.int/tobacco/media/en/WomenMonograph.pdf|url-status=dead|archive-date=28 November 2003|title=Women and the Tobacco Epidemic: Challenges for the 21st Century|access-date=2 January 2009|author=The World Health Organization, and the Institute for Global Tobacco Control, Johns Hopkins School of Public Health|year=2001|publisher=World Health Organization|pages=5–6}}</ref><ref name="2001SurgeonGeneralWomen47">{{Cite web|url=https://www.cdc.gov/tobacco/data_statistics/sgr/2001/|title=Surgeon General's Report—Women and Smoking|access-date=3 January 2009|year=2001|publisher=Centers for Disease Control and Prevention|page=47|archive-date=10 July 2009|archive-url=https://web.archive.org/web/20090710040912/http://www.cdc.gov/tobacco/data_statistics/sgr/2001/|url-status=live}}</ref> In some developed countries smoking rates for men have peaked and begun to decline, while for women they continue to climb.<ref>{{Cite journal|first1=Richard|last1=Peto|first2=Alan D|last2=Lopez|first3=Jillian|last3=Boreham|first4=Michael|last4=Thun|title=Mortality from Smoking in Developed Countries 1950–2000: indirect estimates from national vital statistics|url=http://www.ctsu.ox.ac.uk/~tobacco/SMK_All_PAGES.pdf|access-date=22 March 2009|year=2006|publisher=Oxford University Press|page=9|url-status=dead|archive-url=https://web.archive.org/web/20050224232603/http://www.ctsu.ox.ac.uk/~tobacco/SMK_All_PAGES.pdf|archive-date=24 February 2005}}</ref> | |||
| Evidence suggests that non-smokers are up to twice as likely as smokers to develop ] or ]<ref> | |||
| {{cite journal | |||
| | last = Fratiglioni | |||
| | first = L | |||
| | authorlink = | |||
| | coauthors = Wang HX | |||
| | title = Smoking and Parkinson's and Alzheimer's disease: review of the epidemiological studies | |||
| | journal = Behav Brain Res | |||
| | volume = 113 | |||
| | issue = 1–2 | |||
| | pages = 117–120 | |||
| |date=August 2000 | |||
| | url = http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10942038&dopt=Citation | |||
| | doi = | |||
| | id = PMID: 10942038 | |||
| | accessdate = 2006-11-06}} | |||
| </ref>. | |||
| A plausible explanation for these cases may be the effect of nicotine, a ] ], decreasing the levels of ] in the smoker's brain; Parkinson's disease occurs when the effect of ] is less than that of acetylcholine. In addition, nicotine stimulates the mesolimbic dopamine pathway (as do other drugs of abuse), causing an effective increase in dopamine levels. Opponents counter by noting that consumption of pure nicotine may be as beneficial as smoking without the risks associated with smoking (as in CO poisoning). | |||
| As of 2002, about twenty percent of young teenagers (13–15) smoked worldwide. 80,000 to 100,000 children begin smoking every day, roughly half of whom live in Asia. Half of those who begin smoking in ] years are projected to go on to smoke for 15 to 20 years.<ref name="WHO2002FactSheet"/> As of 2019 in the United States, roughly 800,000 high school students smoke.<ref>Tobaccofreekids.org/problem/tol-s</ref> | |||
| Considering the high rates of physical sickness and deaths<ref>Seeman MV. An outcome measure in schizophrenia: mortality. Can J Psychiatry. 2007 Jan;52(1):55-60. PMID 17444079</ref> <ref>Auquier P, Lancon C, Rouillon F, Lader M, Holmes C. Mortality in schizophrenia. Pharmacoepidemiol Drug Saf. 2006 Dec;15(12):873-9. PMID 17058327</ref> among persons suffering from ], one of smoking's short term benefits is its temporary effect to improve alertness and cognitive functioning in that disease.<ref> Compton, Michael T: Cigarette Smoking in Individuals with Schizophrenia, Medscape Psychiatry & Mental Health. 2005;10(2) ©2005 Medscape, Posted 07/30/2004 |url = http://www.medscape.com/viewarticle/516304_print </ref> It has been postulated that the mechanism of this effect is that schizophrenics have a disturbance of nicotinic receptor functioning.<ref> Ripoll, N; Bronnec, M; Bourin, M: Nicotinic Receptors and Schizophrenia, Curr Med Res Opin 20(7):1057–1074, 2004 © 2004 Librapharm Limited, Posted 07/30/2004 |url = http://www.medscape.com/viewarticle/483888_print </ref> Rates of smoking have been found to be much higher in schizophrenics.<ref>{{cite journal | last = Kelly | first = Ciara | coauthors = McCreadie, Robin | title = Cigarette smoking and schizophrenia | journal = Advances in Psychiatric Treatment | volume = 6 | issue = 5 | pages = 327-331 | date = 2000 | url = http://apt.rcpsych.org/cgi/content/full/6/5/327 | accessdate = 2008-1-14}}</ref> | |||
| The ] (WHO) states that "Much of the disease burden and premature mortality attributable to tobacco use disproportionately affect the poor". Of the 1.22 billion smokers, 1 billion of them live in developing or transitional economies. Rates of smoking have leveled off or declined in the ].<ref>{{cite journal | title = Cigarette smoking among adults and trends in smoking cessation – United States, 2008 | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 58 | issue = 44 | pages = 1227–1232 | year = 2009 | pmid = 19910909 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5844a2.htm | format = Full free text | author1 = Centers for Disease Control and Prevention (CDC) | access-date = 17 September 2017 | archive-date = 16 September 2017 | archive-url = https://web.archive.org/web/20170916142331/https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5844a2.htm | url-status = live }}</ref> In the ], however, tobacco consumption is rising by 3.4% per year as of 2002.<ref name="WHO2002FactSheet"/> | |||
| ==Effects of the habit and industry on society== | |||
| The WHO in 2004 projected 58.8 million deaths to occur globally,<ref name="WHO2004GBD8">{{harvnb|GBD|2008|p=8}}</ref> from which 5.4 million are tobacco-attributed,<ref>{{harvnb|GBD|2008|p=23}}</ref> and 4.9 million as of 2007.<ref name="WHO2007FactSheet">{{Cite web|url=http://www.wpro.who.int/media_centre/fact_sheets/fs_20070529.htm|title=WHO/WPRO-Tobacco Fact sheet|access-date=1 January 2009|date=29 May 2007|publisher=World Health Organization Regional Office for the Western Pacific|url-status=dead|archive-url=https://web.archive.org/web/20090207100241/http://www.wpro.who.int/media_centre/fact_sheets/fs_20070529.htm|archive-date=7 February 2009}}</ref> As of 2002, 70% of the deaths are in developing countries.<ref name="WHO2007FactSheet"/> As of 2017, smoking causes one in ten deaths worldwide, with half of those deaths in the US, China, India and Russia.<ref>{{Cite news|url=https://www.bbc.com/news/health-39510728|title=Smoking causes one in 10 deaths worldwide, study shows|date=6 April 2017|work=BBC News|access-date=11 April 2017|language=en-GB|archive-date=10 April 2017|archive-url=https://web.archive.org/web/20170410231718/http://www.bbc.com/news/health-39510728|url-status=live}}</ref> | |||
| ==Psychology== | |||
| ===Effect on healthcare costs=== | |||
| In countries where there is a ] system, society covers the cost of medical care for smokers who become ill through in the form of increased taxes. Two arguments exist on this front, the "pro-smoking" argument suggesting that heavy smokers generally don't live long enough to develop the costly and chronic illnesses which affect the elderly, reducing society's healthcare burden. The "anti-smoking" argument suggests that the healthcare burden is increased because smokers get chronic illnesses younger and at a higher rate than the general population. | |||
| ===Takeup=== | |||
| Data on both positions is limited. The ] published research in 2002 claiming that the cost of each pack of cigarettes sold in the United States was more than $7 in medical care and lost productivity.<ref> </ref>The cost may be higher, with another study putting it as high as $41 per pack, most of which however is on the individual and his/her family.<ref name="Familycost"> </ref> This is how one author of that study puts it when he explains the very low cost for others: "The reason the number is low is that for private pensions, Social Security, and Medicare — the biggest factors in calculating costs to society — smoking actually saves money. Smokers die at a younger age and don't draw on the funds they've paid into those systems." <ref name="Familycost"/> | |||
| ], whose doctor ] because of ] caused by smoking<ref name=Gay>{{Cite book| last=Gay| first= Peter| year=1988| title=Freud: A Life for Our Time| url=https://archive.org/details/freudlifeforourt00gayp| url-access=registration| location=New York |pages=–651|isbn=978-0-393-32861-5|publisher= W. W. Norton & Company |author-link=Peter Gay}}</ref>]] | |||
| Most smokers begin smoking during adolescence or early adulthood. Some studies also show that smoking can also be linked to various mental health complications.<ref>{{cite journal |author1=Patton G. C. |author2=Hibbert M. |author3=Rosier M. J. |author4=Carlin J. B. |author5=Caust J. |author6=Bowes G. | year = 1996 | title = Is smoking associated with depression and anxiety in teenagers? | journal = American Journal of Public Health | volume = 86 | issue = 2| pages = 225–230 | pmc=1380332 | pmid=8633740 | doi=10.2105/ajph.86.2.225}}</ref> Smoking has elements of risk-taking and rebellion, which often appeal to young people. {{citation needed|date=July 2023}} The presence of peers that smoke and media featuring high-status models smoking may also encourage smoking. Because teenagers are influenced more by their peers than by adults {{dubious|date=July 2023}}, attempts by parents, schools, and health professionals at preventing people from trying cigarettes are often unsuccessful.<ref name="StantonSilva1992">{{cite journal | last1 = Stanton | first1 = W. | last2 = Silva | first2 = P. A. | title = A longitudinal study of the influence of parents and friends on children's initiation of smoking | journal = Journal of Applied Developmental Psychology | volume = 13 | issue = 4 | pages = 423–434 | year = 1992 | doi = 10.1016/0193-3973(92)90010-F }}</ref><ref>{{Cite book|last1=Harris|first1=Judith Rich|last2=Pinker|first2=Steven|title=The nurture assumption: why children turn out the way they do|url=https://books.google.com/books?id=9GQlA_l-TQ0C&q=The+nurture+assumption:+Why+children+turn+out+the+way+they+do|access-date=22 March 2009|date=4 September 1998|publisher=Simon and Schuster|isbn=978-0-684-84409-1|archive-date=14 January 2023|archive-url=https://web.archive.org/web/20230114080750/https://books.google.com/books?id=9GQlA_l-TQ0C&q=The+nurture+assumption:+Why+children+turn+out+the+way+they+do|url-status=live}}</ref> | |||
| Children of smoking parents are more likely to smoke than children with non-smoking parents. Children of parents who smoke are less likely to quit smoking.<ref name=":0" /> One study found that parental smoking cessation was associated with less adolescent smoking, except when the other parent currently smoked.<ref>{{cite journal | last1 = Chassin | first1 = L. | last2 = Presson | first2 = C. | last3 = Rose | first3 = J. | last4 = Sherman | first4 = S. J. | last5 = Prost | first5 = J. | title = Parental Smoking Cessation and Adolescent Smoking | journal = Journal of Pediatric Psychology | volume = 27 | issue = 6 | pages = 485–496 | year = 2002 | pmid = 12177249 | doi = 10.1093/jpepsy/27.6.485 | doi-access = free }}</ref> A current study tested the relation of adolescent smoking to rules regulating where adults are allowed to smoke in the home. Results showed that restrictive home smoking policies were associated with lower likelihood of trying smoking for both middle and high school students.<ref>{{cite journal | last1 = Proescholdbell | first1 = R. J. | last2 = Chassin | first2 = L. | last3 = MacKinnon | first3 = D. P. | title = Home smoking restrictions and adolescent smoking | journal = Nicotine & Tobacco Research | volume = 2 | issue = 2 | pages = 159–167 | year = 2000 | doi = 10.1080/713688125 | pmid = 11072454 | s2cid = 8749779 }}</ref> | |||
| By contrast, some non-scientific studies, including one conducted by ] in the ]<ref name="Czechonomics">{{cite web | title= Public Finance Balance of Smoking in the Czech Republic| url=http://www.mindfully.org/Industry/Philip-Morris-Czech-Study.htm}}</ref> and another by the ],<ref>{{cite web | title= Snuff the Facts| url=http://www.cato.org/dailys/1-16-98.html}}</ref> support the opposite position. Neither study was peer-reviewed nor published in a scientific journal, and the Cato Institute have received funding from tobacco companies in the past.{{Fact|date=July 2007}} Philip Morris has explicitly apologised for the former study, saying: "The funding and public release of this study which, among other things, detailed purported cost savings to the Czech Republic due to premature deaths of smokers, exhibited terrible judgment as well as a complete and unacceptable disregard of basic human values. For one of our tobacco companies to commission this study was not just a terrible mistake, it was wrong. All of us at Philip Morris, no matter where we work, are extremely sorry for this. No one benefits from the very real, serious and significant diseases caused by smoking." <ref name="Czechonomics"/> | |||
| Behavioural research generally indicates that teenagers begin their smoking habits due to peer pressure, and cultural influence portrayed by friends. However, one study found that direct pressure to smoke cigarettes played a less significant part in adolescent smoking, with ]s also reporting low levels of both ] and direct pressure to smoke cigarettes.<ref>{{cite journal | last1 = Urberg | first1 = K. | last2 = Shyu | first2 = S. J. | last3 = Liang | first3 = J. | title = Peer influence in adolescent cigarette smoking | journal = Addictive Behaviors | volume = 15 | issue = 3 | pages = 247–255 | year = 1990 | pmid = 2378284 | doi = 10.1016/0306-4603(90)90067-8 }}</ref> Mere exposure to tobacco retailers may motivate smoking behaviour in adults.<ref>{{Cite book|title=Review: Tobacco outlet density|last=Bharatula|first=Arun|year=2016|location=Melbourne|url=https://drive.google.com/open?id=0B-e8wYlugBcUTFQ4TnRkenBkVW8}}{{Dead link|date=November 2018 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> A similar study suggested that individuals may play a more active role in starting to smoke than has previously been thought and that social processes other than peer pressure also need to be taken into account.<ref>{{Cite journal|vauthors=Michell L, West P |title=Peer pressure to smoke: the meaning depends on the method|volume=11|issue=1|pages=39–49|year=1996|doi=10.1093/her/11.1.39|journal=Health Education Research|doi-access=free}}</ref> Another study's results indicated that ] was significantly associated with smoking behavior across all age and gender cohorts, but that intrapersonal factors were significantly more important to the smoking behavior of 12- to 13-year-old girls than same-age boys. Within the 14- to 15-year-old age group, one peer pressure variable emerged as a significantly more important predictor of girls' than boys' smoking.<ref>{{cite journal | last1 = Barber | first1 = J. | last2 = Bolitho | first2 = F. | last3 = Bertrand | first3 = L. | title = The Predictors of Adolescent Smoking | journal = Journal of Social Service Research | volume = 26 | issue = 1 | pages = 51–66| year = 1999 | doi = 10.1300/J079v26n01_03 }}</ref> It is debated whether peer pressure or ] is a greater cause of adolescent smoking. | |||
| Between 1970 an 1995, per-capita cigarette consumption in poorer developing countries increased by 67 percent, while it dropped by 10 percent in the richer developed world. Eighty percent of smokers now live in less developed countries. By 2030, the ] (WHO) forecasts that 10 million people a year will die of smoking-related illness, making it the single biggest cause of death worldwide, with the largest increase to be among women. WHO forecasts' the 21st century's death rate from smoking to be ten times the 20th century's rate. ("Washingtonian" magazine, December 2007). | |||
| Psychologist ] (who later was questioned for nonplausible results | |||
| ===Tobacco and other drugs=== | |||
| <ref name="Pelosi2019">{{cite journal |last1=Pelosi |first1=Anthony J. |title=Personality and fatal diseases: Revisiting a scientific scandal |journal=Journal of Health Psychology |volume=24 |issue=4 |year=2019 |pages=421–439 |issn=1359-1053 |doi=10.1177/1359105318822045|pmid=30791726 |pmc=6712909 }}</ref> and unsafe publications<ref name="Enquiry">{{cite web |title=King's College London enquiry into publications authored by Professor Hans Eysenck with Professor Ronald Grossarth-Maticek |url=https://retractionwatch.com/wp-content/uploads/2019/10/HE-Enquiry.pdf |date=October 2019 |access-date=13 January 2020 |archive-date=5 November 2022 |archive-url=https://web.archive.org/web/20221105133943/https://retractionwatch.com/wp-content/uploads/2019/10/HE-Enquiry.pdf |url-status=live }}</ref><ref name="Hawkes">Nigel Hawkes (2019), {{Webarchive|url=https://web.archive.org/web/20230104001110/https://www.bmj.com/content/367/bmj.l5899 |date=4 January 2023 }}</ref>) developed a personality profile for the typical smoker. ] is the trait that is most associated with smoking, and smokers tend to be sociable, impulsive, risk taking, and excitement seeking individuals.<ref>{{Cite book|first1=Hans J. |last1=Eysenck |first2=Stuart |last2=Brody |title=Smoking, health and personality |date=November 2000 |publisher=Transaction |isbn=978-0-7658-0639-0 }}</ref> | |||
| {{main|Tobacco and other drugs}} | |||
| A number of studies have been conducted to explore the relationship between tobacco and other drug use. While the association between smoking tobacco and other drug use has been well-established, the nature of this association remains unclear. The two main theories are the ] (gateway) model and the correlated liabilities model. The causation model argues that smoking is a primary influence on future drug use, while the correlated liabilities model argues that smoking and other drug use are predicated on genetic or environmental factors. | |||
| === |
===Persistence=== | ||
| {{main|Tobacco advertising}} | |||
| The reasons given by some smokers for this activity have been categorized as ''addictive smoking'', ''pleasure from smoking'', ''tension reduction/relaxation'', ''social smoking'', ''stimulation'', ''habit/automatism'', and ''handling''. There are gender differences in how much each of these reasons contribute, with females more likely than males to cite ''tension reduction/relaxation'', ''stimulation'' and ''social smoking''.<ref>{{cite journal | last1 = Berlin | first1 = I. | last2 = Singleton | first2 = E. G. | last3 = Pedarriosse | first3 = A. M. | last4 = Lancrenon | first4 = S. | last5 = Rames | first5 = A. | last6 = Aubin | first6 = H. J. | last7 = Niaura | first7 = R. | title = The Modified Reasons for Smoking Scale: factorial structure, gender effects and relationship with nicotine dependence and smoking cessation in French smokers | journal = Addiction | volume = 98 | issue = 11 | pages = 1575–1583 | year = 2003 | pmid = 14616184 | doi = 10.1046/j.1360-0443.2003.00523.x }}</ref> | |||
| Before the 1970s, most ] was legal in the United States and most European nations. In the United States, in the 1950s and 1960s, cigarette brands were frequently sponsors of television shows—most notably shows such as '']'' and ''].'' One of the most famous television jingles of the era came from an advertisement for ] cigarettes. The slogan "]!" proved to be catchy, and is still quoted today. Other popular slogans from the 1960s were "]," which was used to advertise ] cigarettes, and "I'd Walk a Mile for a Camel". | |||
| Some smokers argue that the ] effect of smoking allows them to calm their nerves, often allowing for increased concentration. However, according to the ], "Nicotine seems to provide both a stimulant and a depressant effect, and it is likely that the effect it has at any time is determined by the mood of the user, the environment and the circumstances of use. Studies have suggested that low doses have a depressant effect, while higher doses have stimulant effect."<ref>{{Cite journal|title=Nicotine|url=http://www.ch.ic.ac.uk/rzepa/mim/drugs/html/nicotine_text.htm|access-date=22 March 2009|publisher=Imperial College London|archive-date=14 July 2009|archive-url=https://web.archive.org/web/20090714142449/http://www.ch.ic.ac.uk/rzepa/mim/drugs/html/nicotine_text.htm|url-status=live}}</ref> | |||
| In the 1950s, manufacturers began adding filter tips to cigarettes to remove some of the tar and nicotine as they were smoked. "Safer", "less potent" cigarette brands were also introduced. Light cigarettes became so popular that, as of 2004, half of American smokers preferred them over regular cigarettes <ref> , by Peter Lavelle. ''The Pulse'', ], ]. </ref>, in spite the fact that the idea of a "safer" cigarette is a myth. Cigarettes that offer "low tar and nicotine" cause the smoker to smoke more or to inhale more deeply to get the same level of nicotine. According to The Federal Government’s National Cancer Institute (NCI), light cigarettes provide no benefit to smoker's health.<ref> , from the ] factsheet </ref><ref> , by Andy Coghlan. New Scientist, 2004</ref> | |||
| ===Patterns=== | |||
| In the United States, it was believed by many that tobacco companies are marketing tobacco smoking to minors.<ref> </ref> For example, ] used the ] cartoon character to advertise ]. Other brands such as ] targeted women with slogans like "You've Come a Long Way Baby". | |||
| A number of studies have established that cigarette sales and smoking follow distinct time-related patterns. For example, cigarette sales in the United States of America have been shown to follow a strongly seasonal pattern, with the high months being the months of summer, and the low months being the winter months.<ref>{{cite journal | last1 = Chandra | first1 = S. | last2 = Chaloupka | first2 = F. J. | title = Seasonality in cigarette sales: patterns and implications for tobacco control | journal = Tobacco Control | volume = 12 | issue = 1 | pages = 105–107 | year = 2003 | pmid = 12612375 | pmc = 1759100 | doi = 10.1136/tc.12.1.105 }}</ref> | |||
| Similarly, smoking has been shown to follow distinct circadian patterns during the waking day—with the high point usually occurring shortly after waking in the morning, and shortly before going to sleep at night.<ref>{{cite journal | last1 = Chandra | first1 = S. | last2 = Shiffman | first2 = S. | last3 = Scharf | first3 = M. | last4 = Dang | first4 = Q. | last5 = Shadel | first5 = G. | title = Daily smoking patterns, their determinants, and implications for quitting | journal = ] | volume = 15 | issue = 1 | pages = 67–80 | date = Feb 2007 | pmid = 17295586 | doi = 10.1037/1064-1297.15.1.67 | issn = 1064-1297 }}</ref> | |||
| In 1964, the ], released the Surgeon General's Advisory Committee Report on Smoking and Health. It was based on over 7000 scientific articles that linked tobacco use with cancer and other diseases. This report led to laws requiring warning labels on tobacco products and to restrictions on tobacco advertisements. As these began to come into force, tobacco marketing became more subtle, with sweets shaped like cigarettes put on the market, and a number of adverts designed to appeal to children, particularly those featuring ] resulting in increased awareness and uptake of smoking among children<ref>While D, Kelly S, Huang W, Charlton A. Cigarette advertising and onset of smoking in children: questionnaire survey. BMJ. 1996 Aug 17;313(7054):398-9. PMID 8761227</ref>. However, restrictions did have an effect on adult quit rates, with its use declining to the point that by 2004, nearly half of all Americans who had ever smoked had quit.<ref> MMWR Weekly, November 11, 2005. </ref> | |||
| ==Effects== | |||
| Many nations, including Russia, Greece and Romania, still allow billboards advertising tobacco use. Tobacco smoking is still advertised in special magazines, during sporting events, in gas stations and stores, and in more rare cases on television. Some nations, including the UK and Australia, have begun anti-smoking advertisements to counter the effects of tobacco advertising. | |||
| ===Health=== | |||
| The actual effectiveness of tobacco advertisement is widely documented. According to an opinion piece by Henry Saffer, ] experts say that tobacco ] increases cigarette consumption and there is much ] literature that finds a significant effect of tobacco advertising on smoking, especially in children.<ref> </ref><ref></ref><ref> </ref><ref> </ref><ref> </ref><ref> [Tobacco Advertisements: One of the Strongest Risk Factors for Smoking in Hong Kong Students. | |||
| {{Main|Health effects of tobacco}} | |||
| American Journal of Preventive Medicine, Volume 14, Issue 3, Pages 217–223 T. Lam]</ref><ref> </ref><ref> </ref> A Dutch tobacco company manufactures "Pink Elephant" vanilla-flavored cigarettes, and "Black Devil" chocolate-flavored cigarettes. | |||
| {{see also|Polycyclic aromatic hydrocarbons}} | |||
| Tobacco smoking is the ] and a global ] concern.<ref name="Kalkhoran2018">{{cite journal |last1=Kalkhoran |first1=S |last2=Benowitz |first2=NL |last3=Rigotti |first3=AN |date=August 2018 |title=Prevention and Treatment of Tobacco Use: JACC Health Promotion Series |url=https://www.onlinejacc.org/content/72/9/1030 |journal=] |publisher=] for the ] |volume=72 |issue=9 |pages=1030–45 |doi=10.1016/j.jacc.2018.06.036 |doi-access=free |issn=1558-3597 |pmc=6261256 |pmid=30139432 |s2cid=52077567 |access-date=1 August 2020 |archive-date=9 August 2020 |archive-url=https://web.archive.org/web/20200809153506/https://www.onlinejacc.org/content/72/9/1030 |url-status=live }}</ref> There are 1.3 billion tobacco users in the world, as per latest data from WHO.<ref name="Tobacco"/> One person dies every six seconds from a tobacco related disease.<ref>{{Cite web|url=http://www.ash.org/|title=ASH > Action on Smoking & Health|website=www.ash.org|access-date=16 November 2016|date=2 August 2012|archive-date=19 November 2016|archive-url=https://web.archive.org/web/20161119054152/http://ash.org/|url-status=live}}</ref> | |||
| ===Peer pressure=== | |||
| ] | |||
| Many anti-smoking organizations claim that teenagers begin their smoking habits due to peer pressure, and cultural influence portrayed by friends. However, one study found that direct pressure to smoke cigarettes did not play a significant part in adolescent smoking. In that study, ]s also reported low levels of both ] and direct pressure to smoke cigarettes.<ref>Urberg KA, Shyu SJ, Liang J. Peer influence in adolescent cigarette smoking. ''Addict Behav.'' 1990;15(3):247-55. PMID 2378284.</ref> A similar study showed that individuals play a more active role in starting to smoke than has previously been acknowledged and that social processes other than peer pressure need to be taken into account.<ref> </ref> Another study's results revealed that ] was significantly associated with smoking behavior across all age and gender cohorts, but that intrapersonal factors were significantly more important to the smoking behavior of 12–13 year-old girls than same-age boys. Within the 14–15 year-old age group, one peer pressure variable emerged as a significantly more important predictor of girls' than boys' smoking.<ref> </ref> It is debated whether peer pressure or ] is a greater cause of adolescent smoking. It is arguable that the reverse of peer-pressure is true, when the majority of peers do not smoke and ostracize those who do. | |||
| Tobacco use leads most commonly to diseases affecting the heart and lungs, with smoking being a major risk factor for ],<ref name="Harm Reduct. J.">{{cite journal |last1=Rodu |first1=B |last2=Plurphanswat |first2=N |date=January 2021 |title=Mortality among male cigar and cigarette smokers in the USA |url=https://harmreductionjournal.biomedcentral.com/track/pdf/10.1186/s12954-020-00446-4.pdf |url-status=live |journal=] |publisher=] |volume=18 |issue=7 |page=7 |doi=10.1186/s12954-020-00446-4 |doi-access=free |issn=1477-7517 |lccn=2004243422 |pmc=7789747 |pmid=33413424 |s2cid=230800394 |archive-url=https://web.archive.org/web/20210826115030/https://harmreductionjournal.biomedcentral.com/track/pdf/10.1186/s12954-020-00446-4.pdf |archive-date=26 August 2021 |access-date=28 August 2021}}</ref><ref name="Am. J. Public Health">{{cite journal |last1=Nonnemaker |first1=J |last2=Rostron |first2=B |last3=Hall |first3=P |last4=MacMonegle |first4=A |last5=Apelberg |first5=B |date=September 2014 |title=Mortality and Economic Costs From Regular Cigar Use in the United States, 2010 |editor-last=Morabia |editor-first=A |editor-link=Alfredo Morabia |journal=] |publisher=] |volume=104 |issue=9 |pages=e86–e91 |doi=10.2105/AJPH.2014.301991 |eissn=1541-0048 |issn=0090-0036 |pmc=4151956 |pmid=25033140 |s2cid=207276270}}</ref> ]s,<ref name="Expert Rev. Cardiovasc Ther.">{{cite journal |last1=Shah |first1=RS |last2=Cole |first2=JW |date=July 2010 |title=Smoking and stroke: the more you smoke the more you stroke |journal=] |publisher=] |volume=8 |issue=7 |pages=917–932 |doi=10.1586/erc.10.56 |issn=1744-8344 |pmc=2928253 |pmid=20602553 |s2cid=207215548}}</ref> ] (COPD),<ref name="IJERPH 2009">{{cite journal |last=Laniado-Laborín |first=Rafael |date=January 2009 |title=Smoking and Chronic Obstructive Pulmonary Disease (COPD). Parallel Epidemics of the 21st Century |journal=] |publisher=] |volume=6 |issue=1: ''Smoking and Tobacco Control'' |doi=10.3390/ijerph6010209 |pages=209–224 |doi-access=free |issn=1660-4601 |pmc=2672326 |pmid=19440278 |s2cid=19615031 }}</ref> ] (IPF),<ref name="Pulm Med.">{{cite journal |last1=Oh |first1=CK |last2=Murray |first2=LA |last3=Molfino |first3=NL |date=February 2012 |title=Smoking and Idiopathic Pulmonary Fibrosis |journal=] |publisher=] |volume= 2012|issue= |pages=808260 |doi=10.1155/2012/808260 |issn=2090-1844 |pmc=3289849 |pmid=22448328 |s2cid=14090263|doi-access=free }}</ref> and ].<ref name="IJERPH 2009" /> | |||
| ===Parental smoking=== | |||
| Children of smoking parents are more likely to smoke than children with non-smoking parents. One study found that parental smoking cessation was associated with less adolescent smoking, except when the other parent currently smoked.<ref> </ref> A current study tested the relation of adolescent smoking to rules regulating where adults are allowed to smoke in the home. Results showed that restrictive home smoking policies were associated with lower likelihood of trying smoking for both middle and high school students.<ref> </ref> | |||
| Smoking tobacco causes various types and subtypes of ]s<ref name="J. Natl. Cancer Inst.">{{cite journal |last1=Thun |first1=Michael J. |last2=Jacobs |first2=Eric J. |last3=Shapiro |first3=Jean A. |date=February 2000 |title=Cigar Smoking in Men and Risk of Death From Tobacco-Related Cancers |url=https://academic.oup.com/jnci/article/92/4/333/2624751 |url-status=live |editor-last=Ganz |editor-first=Patricia A. |editor-link=Patricia A. Ganz |journal=] |publisher=] |volume=92 |issue=4 |pages=333–337 |doi=10.1093/jnci/92.4.333 |doi-access=free |eissn=1460-2105 |issn=0027-8874 |pmid=10675383 |s2cid=7772405 |archive-url=https://web.archive.org/web/20210421095250/https://academic.oup.com/jnci/article/92/4/333/2624751 |archive-date=21 April 2021 |access-date=28 August 2021}}</ref> (particularly ], ],<ref name="StatPearls 2020">{{cite book |vauthors=Anjum F, Zohaib J |title=Definitions |chapter=Oropharyngeal Squamous Cell Carcinoma |date=4 December 2020 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK563268/ |place=Treasure Island (FL) |publisher=StatPearls Publishing |edition=Updated |id=Bookshelf ID: NBK563268 |doi=10.32388/G6TG1L |pmid=33085415 |s2cid=229252540 |via=] |access-date=7 February 2021 |archive-date=11 June 2021 |archive-url=https://web.archive.org/web/20210611150638/https://www.ncbi.nlm.nih.gov/books/NBK563268/ |url-status=live }}</ref> ],<ref name="StatPearls 2020" /> and ],<ref name="StatPearls 2020" /> ] and ]).<ref name=":0" /> Using tobacco, especially together with ], is a major risk factor for ]. 72% of head and neck cancer cases are caused by using both alcohol and tobacco.<ref name=":6">{{Cite journal |last1=Gormley |first1=Mark |last2=Creaney |first2=Grant |last3=Schache |first3=Andrew |last4=Ingarfield |first4=Kate |last5=Conway |first5=David I. |date=2022-11-11 |title=Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors |journal=British Dental Journal |language=en |volume=233 |issue=9 |pages=780–786 |doi=10.1038/s41415-022-5166-x |issn=0007-0610 |pmc=9652141 |pmid=36369568}}</ref> This rises to 89% when looking specifically at ].<ref>{{Cite journal |last1=Hashibe |first1=Mia |last2=Brennan |first2=Paul |last3=Chuang |first3=Shu-chun |last4=Boccia |first4=Stefania |last5=Castellsague |first5=Xavier |last6=Chen |first6=Chu |last7=Curado |first7=Maria Paula |last8=Dal Maso |first8=Luigino |last9=Daudt |first9=Alexander W. |last10=Fabianova |first10=Eleonora |last11=Fernandez |first11=Leticia |last12=Wünsch-Filho |first12=Victor |last13=Franceschi |first13=Silvia |last14=Hayes |first14=Richard B. |last15=Herrero |first15=Rolando |date=2009-02-01 |title=Interaction between Tobacco and Alcohol Use and the Risk of Head and Neck Cancer: Pooled Analysis in the International Head and Neck Cancer Epidemiology Consortium |url=https://aacrjournals.org/cebp/article/18/2/541/166699/Interaction-between-Tobacco-and-Alcohol-Use-and |journal=Cancer Epidemiology, Biomarkers & Prevention |language=en |volume=18 |issue=2 |pages=541–550 |doi=10.1158/1055-9965.EPI-08-0347 |issn=1055-9965 |pmc=3051410 |pmid=19190158}}</ref> | |||
| ===Smoking in movies and television=== | |||
| Exposure to smoking in movies has been linked with adolescent smoking initiation in cross-sectional studies.<ref> </ref><ref> </ref> Films tend to have a high incidence of smoking behavior vis-a-vis the general population. According to a study of movies created between 1988 and 1997, eighty-seven percent of these movies portrayed various tobacco use, with an average of 5 occurrences per film. R-rated movies had the greatest number of occurrences and were most likely to feature major characters using tobacco.<ref> </ref> Despite the declining tobacco use in the society, the incidence of smoking in 2002 movies was nearly the same as in 1950 movies.<ref> </ref> | |||
| ] smoking increases the risk of ] as well as the severity of the course of the disease.<ref>Inflamm Bowel Dis. May 2009, P. Seksik, I Nion-Larmurier</ref> It is also the number one cause of ]. Cigarette smoking has also been associated with ], the age-related loss of muscle mass and strength.<ref>{{cite journal |vauthors=Rom O, Kaisari S, Aizenbud D, Reznick AZ |year=2013 |title=Cigarette smoke and muscle catabolism in C2 myotubes |journal=Mech Ageing Dev. |volume=134 |issue=1–2 |pages=24–34 |pmid=23262287 |doi=10.1016/j.mad.2012.11.004 |s2cid=322153}}</ref> The smoke from tobacco elicits carcinogenic effects on the tissues of the body that are exposed to the smoke.<ref name="Harm Reduct. J." /><ref name="Cancer Epidemiol. Biomark. Prev.">{{cite journal |last1=Etemadi |first1=Arash |last2=Blount |first2=Benjamin C. |last3=Calafat |first3=Antonia M. |last4=Chang |first4=Cindy M. |last5=De Jesus |first5=Victor R. |last6=Poustchi |first6=Hossein |last7=Wang |first7=Lanqing |last8=Pourshams |first8=Akram |last9=Shakeri |first9=Ramin |last10=Shiels |first10=Meredith S. |last11=Inoue-Choi |first11=Maki |last12=Ambrose |first12=Bridget K. |last13=Christensen |first13=Carol H. |last14=Wang |first14=Baoguang |last15=Ye |first15=Xiaoyun |last16=Murphy |first16=Gwen |last17=Feng |first17=Jun |last18=Xia |first18=Baoyun |last19=Sosnoff |first19=Connie S. |last20=Boffetta |first20=Paolo |last21=Brennan |first21=Paul |last22=Bhandari |first22=Deepak |last23=Kamangar |first23=Farin |last24=Dawsey |first24=Sanford M. |last25=Abnet |first25=Christian C. |last26=Freedman |first26=Neal D. |last27=Malekzadeh |first27=Reza |date=February 2019 |title=Urinary Biomarkers of Carcinogenic Exposure among Cigarette, Waterpipe, and Smokeless Tobacco Users and Never Users of Tobacco in the Golestan Cohort Study |journal=] |publisher=] |volume=28 |issue=2 |pages=337–347 |doi=10.1158/1055-9965.EPI-18-0743 |eissn=1538-7755 |issn=1055-9965 |pmc=6935158 |pmid=30622099 |s2cid=58560832}}</ref><ref name="J. Natl. Cancer Inst." /><ref>Dreyer, L et al. (1997) Tobacco Smoking. APMIS Inc.</ref> Regular ] smoking is known to carry ], including increased risk of developing various types and subtypes of ]s, ]s, ]s, ]s, ]s, ] and ], and ]s.<ref name="Harm Reduct. J." /><ref name="J. Natl. Cancer Inst." /><ref name="BMC Publ. Health">{{cite journal |last1=Chang |first1=Cindy M. |last2=Corey |first2=Catherine G. |last3=Rostron |first3=Brian L. |last4=Apelberg |first4=Benjamin J. |date=April 2015 |title=Systematic review of cigar smoking and all-cause and smoking-related mortality |url=https://bmcpublichealth.biomedcentral.com/track/pdf/10.1186/s12889-015-1617-5.pdf |url-status=live |journal=] |publisher=] |volume=15 |issue=390 |page=390 |doi=10.1186/s12889-015-1617-5 |doi-access=free |issn=1471-2458 |pmc=4408600 |pmid=25907101 |s2cid=16482278 |archive-url=https://web.archive.org/web/20210316053609/https://bmcpublichealth.biomedcentral.com/track/pdf/10.1186/s12889-015-1617-5.pdf |archive-date=16 March 2021 |access-date=5 September 2021}}</ref><ref name="J. Periodontol.">{{cite journal |last1=Albandar |first1=Jasim M. |last2=Adensaya |first2=Margo R. |last3=Streckfus |first3=Charles F. |last4=Winn |first4=Deborah M. |date=December 2000 |title=Cigar, Pipe, and Cigarette Smoking as Risk Factors for Periodontal Disease and Tooth Loss |journal=] |publisher=] |volume=71 |issue=12 |pages=1874–1881 |doi=10.1902/jop.2000.71.12.1874 |issn=0022-3492 |pmid=11156044 |s2cid=11598500}}</ref> | |||
| There have been moves to reduce the depiction of protagonists smoking in television shows, especially those aimed at children. For example, ] took steps to remove or edit scenes that depict characters smoking in cartoons such as ], ] and ],<ref></ref> which are shown on his ] and ] television channels. | |||
| Tobacco smoke is a complex mixture of over 7,000 ], 98 of which are associated with an increased risk of cardiovascular disease and 69 of which are known to be ]ic.<ref name="Kalkhoran2018" /> The most important chemicals ] are those that produce DNA damage, since such damage appears to be the primary underlying cause of cancer.<ref name="pmid18403632">{{cite journal |vauthors=Kastan MB |title=DNA damage responses: mechanisms and roles in human disease: 2007 G.H.A. Clowes Memorial Award Lecture |journal=Mol. Cancer Res. |volume=6 |issue=4 |pages=517–24 |year=2008 |pmid=18403632 |doi=10.1158/1541-7786.MCR-08-0020 |doi-access=free }}</ref> The most ] compounds in cigarette smoke are ],<ref name="pmid20158384">{{cite journal |vauthors=Liu XY, Zhu MX, Xie JP |title=Mutagenicity of acrolein and acrolein-induced DNA adducts |journal=Toxicol. Mech. Methods |volume=20 |issue=1 |pages=36–44 |year=2010 |pmid=20158384 |doi=10.3109/15376510903530845 |s2cid=8812192 }}</ref> ],<ref name="pmid11971987">{{cite journal |vauthors=Speit G, Merk O |title=Evaluation of mutagenic effects of formaldehyde in vitro: detection of crosslinks and mutations in mouse lymphoma cells |journal=Mutagenesis |volume=17 |issue=3 |pages=183–7 |year=2002 |pmid=11971987 |doi= 10.1093/mutage/17.3.183|doi-access=free }}</ref> ],<ref name="pmid19546159">{{cite journal |vauthors=Pu X, Kamendulis LM, Klaunig JE |title=Acrylonitrile-induced oxidative stress and oxidative DNA damage in male Sprague-Dawley rats |journal=Toxicol. Sci. |volume=111 |issue=1 |pages=64–71 |year=2009 |pmid=19546159 |pmc=2726299 |doi=10.1093/toxsci/kfp133 }}</ref> ],<ref name="pmid21602187">{{cite journal |vauthors=Koturbash I, Scherhag A, Sorrentino J, Sexton K, Bodnar W, Swenberg JA, Beland FA, Pardo-Manuel Devillena F, Rusyn I, Pogribny IP |title=Epigenetic mechanisms of mouse interstrain variability in genotoxicity of the environmental toxicant 1,3-butadiene |journal=Toxicol. Sci. |volume=122 |issue=2 |pages=448–56 |year=2011 |pmid=21602187 |pmc=3155089 |doi=10.1093/toxsci/kfr133 }}</ref> ],<ref name="pmid21604744">{{cite journal |vauthors=Garcia CC, Angeli JP, Freitas FP, Gomes OF, de Oliveira TF, Loureiro AP, Di Mascio P, Medeiros MH |title=-Acetaldehyde promotes unequivocal formation of 1,N2-propano-2'-deoxyguanosine in human cells |journal=J. Am. Chem. Soc. |volume=133 |issue=24 |pages=9140–3 |year=2011 |pmid=21604744 |doi=10.1021/ja2004686 |url=https://figshare.com/articles/_sup_13_sup_C_sub_2_sub_Acetaldehyde_Promotes_Unequivocal_Formation_of_1_i_N_i_sup_2_sup_Propano_2_deoxyguanosine_in_Human_Cells/2639098 |access-date=1 December 2019 |archive-date=6 November 2020 |archive-url=https://web.archive.org/web/20201106102427/https://figshare.com/articles/_sup_13_sup_C_sub_2_sub_Acetaldehyde_Promotes_Unequivocal_Formation_of_1_i_N_i_sup_2_sup_Propano_2_deoxyguanosine_in_Human_Cells/2639098 |url-status=live }}</ref> ],<ref name="pmid19477295">{{cite journal |vauthors=Tompkins EM, McLuckie KI, Jones DJ, Farmer PB, Brown K |title=Mutagenicity of DNA adducts derived from ethylene oxide exposure in the pSP189 shuttle vector replicated in human Ad293 cells |journal=Mutat. Res. |volume=678 |issue=2 |pages=129–37 |year=2009 |pmid=19477295 |doi=10.1016/j.mrgentox.2009.05.011 |bibcode=2009MRGTE.678..129T }}</ref> and ].<ref name="pmid17317274">{{cite journal |vauthors=Fabiani R, Rosignoli P, De Bartolomeo A, Fuccelli R, Morozzi G |title=DNA-damaging ability of isoprene and isoprene mono-epoxide (EPOX I) in human cells evaluated with the comet assay |journal=Mutat. Res. |volume=629 |issue=1 |pages=7–13 |year=2007 |pmid=17317274 |doi=10.1016/j.mrgentox.2006.12.007 |bibcode=2007MRGTE.629....7F }}</ref> In addition to the aforementioned toxic chemicals, ] contains flavorings which upon heating release toxic chemicals and carcinogens such as ] (CO), ] (PAHs), ], ], ] (such as ]), and acids, in addition to nitrogenous ], ], and ], all of which are dangerous to human health.<ref name="Cancer Epidemiol. Biomark. Prev." /><ref name="Arterioscler. Thromb. Vasc. Biol.">{{cite journal |last1=Alarabi |first1=A. B. |last2=Karim |first2=Z. A. |last3=Alshbool |first3=F. Z. |last4=Khasawneh |first4=F. T. |last5=Hernandez |first5=Keziah R. |last6=Lozano |first6=Patricia A. |last7=Montes Ramirez |first7=Jean E. |last8=Rivera |first8=José O. |date=February 2020 |title=Short-Term Exposure to Waterpipe/Hookah Smoke Triggers a Hyperactive Platelet Activation State and Increases the Risk of Thrombogenesis |journal=] |publisher=] |volume=40 |issue=2 |pages=335–349 |doi=10.1161/ATVBAHA.119.313435 |doi-access=free |issn=1079-5642 |pmc=7000176 |pmid=31941383 |s2cid=210335103 }}</ref><ref name="Ann. Am. Thorac. Soc.">{{cite journal |last1=Patel |first1=Mit P. |last2=Khangoora |first2=Vikramjit S. |last3=Marik |first3=Paul E. |date=October 2019 |title=A Review of the Pulmonary and Health Impacts of Hookah Use |journal=] |publisher=] |volume=16 |issue=10 |pages=1215–1219 |doi=10.1513/AnnalsATS.201902-129CME |doi-access=free |issn=2325-6621 |pmid=31091965 |s2cid=155103502 }}</ref><ref name="Environ. Health Prev. Med.">{{cite journal |last1=Qasim |first1=Hanan |last2=Alarabi |first2=A. B. |last3=Alzoubi |first3=K. H. |last4=Karim |first4=Z. A. |last5=Alshbool |first5=F. Z. |last6=Khasawneh |first6=F. T. |date=September 2019 |title=The effects of hookah/waterpipe smoking on general health and the cardiovascular system |url=https://environhealthprevmed.biomedcentral.com/track/pdf/10.1186/s12199-019-0811-y.pdf |url-status=live |journal=] |publisher=] |volume=24 |issue=58 |page=58 |doi=10.1186/s12199-019-0811-y |doi-access=free |issn=1347-4715 |pmc=6745078 |pmid=31521105 |bibcode=2019EHPM...24...58Q |s2cid=202570973 |archive-url=https://web.archive.org/web/20210424161857/https://environhealthprevmed.biomedcentral.com/track/pdf/10.1186/s12199-019-0811-y.pdf |archive-date=24 April 2021 |access-date=8 September 2021}}</ref><ref name="Farag">{{Cite journal| doi = 10.1038/s41598-018-35368-6| pmid = 30451904| pmc = 6242864| issn = 2045-2322| volume = 8| issue = 1| pages = 17028| last1 = Farag| first1 = Mohamed A.| last2 = Elmassry| first2 = Moamen M.| last3 = El-Ahmady| first3 = Sherweit H.| title = The characterization of flavored hookahs aroma profile and in response to heating as analyzed via headspace solid-phase microextraction (SPME) and chemometrics| journal = Scientific Reports| date = 2018-11-19| bibcode = 2018NatSR...817028F}}</ref> A comparison of 13 common ] flavors found that melon flavors are the most dangerous, with their smoke containing four classes of hazards in high concentrations.<ref name="Farag" /> | |||
| ===The use of smoking to project an image=== | |||
| Famous smokers of the past used cigarettes or pipes as part of their image, such as ]'s ]-brand cigarettes, ]'s, ]'s, ]'s, ]'s, and Bing Crosby's pipes, or the news broadcaster ]'s cigarette. Writers in particular seemed to be known for smoking; see, for example, Cornell Professor ]'s book ''Cigarettes are Sublime'' for the analysis, by this professor of French literature, of the role smoking plays in 19th and 20th century letters. The popular author ] addressed his addiction to cigarettes within his novels. British Prime Minister ] was well known for smoking a pipe in public as was ] for his cigars. ], the fictional detective created by ] smoked a pipe, cigarettes, and cigars, besides injecting himself with cocaine, "to keep his overactive brain occupied during the dull London days, when nothing happened". The ] ] comic book character, ], created by ], is synonymous with smoking, so much so that the first storyline by ] creator, ], centred around John Constantine contracting lung cancer. ] ], while ] as "The Sandman", is a chronic smoker in order to appear "tough". | |||
| The ] estimates that tobacco caused 8 million deaths in 2004<ref name="Tobacco"/> and 100 million deaths over the course of the 20th century.<ref name=WHO2></ref> Similarly, the United States ] describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."<ref name="fn1">" {{webarchive|url=https://web.archive.org/web/20090501011931/http://www.cdc.gov/tobacco/quit_smoking/you_can_quit/nicotine.htm |date=1 May 2009 }}." Centers for Disease Control and Prevention.</ref> Although 70% of smokers state their intention to quit only 3–5% are actually successful in doing so.<ref name="Barendregt, J. J. 1997"/> | |||
| == Religious views on smoking == | |||
| {{main|Religious views on smoking}} | |||
| The probabilities of death from lung cancer before age 75 in the United Kingdom are 0.2% for men who never smoked (0.4% for women), 5.5% for male former smokers (2.6% in women), 15.9% for current male smokers (9.5% for women) and 24.4% for male "heavy smokers" defined as smoking more than 25 cigarettes per day (18.5% for women).<ref>{{cite journal |author1=Peto Richard |author2=Darby Sarah |author3=Deo Harz | year = 2000 | title = Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies | journal = ] | volume = 321 | issue = 7257| pages = 323–329 | doi = 10.1136/bmj.321.7257.323 | pmid=10926586 | pmc=27446|display-authors=etal}}</ref> Tobacco smoke can combine with other carcinogens present within the environment in order to produce elevated degrees of lung cancer. | |||
| Communal smoking of a sacred tobacco pipe is a common ritual of many Native American tribes, and was considered a sacred part of their religion. Sema, the ] word for tobacco, was grown for ceremonial use and considered the ultimate sacred plant since its smoke was believed to carry prayers to the heavens.<ref> </ref> The tobacco used during these rituals varies widely in potency — the '']'' species used in South America, for instance, has up to twice the nicotine content of the common North American ''N. tabacum''. | |||
| The risk of lung cancer decreases almost from the first day someone ] and it drops by 50% after 10 years of smoking cessation.<ref name="Tobacco"/> Healthy cells that have escaped mutations grow and replace the damaged ones in the lungs. In the research dated December 2019, 40% of cells in former smokers looked like those of people who had never smoked.<ref>{{Cite journal|url=https://www.nature.com/articles/s41586-020-1961-1.epdf?referrer_access_token=0VDMQ0H4-f91dB5uqJjJftRgN0jAjWel9jnR3ZoTv0OKOcOePhUj_ZiBqhIKPHMESOIlMBgsq7AHooGU3FzfjdfYjURebC16Qb6V0cVfg19HvLQ2KS7pbx-MJiyBfwaKhmIHSH11XX1xKNkHeU5h60nkqCpwMmPuxyXblOVPEt4hZhf8_B_huSwZQXpra5y0PHnEzjNdkO683sRXKDMHkQ%3D%3D&tracking_referrer=www.bbc.com|title=Tobacco smoking and somatic mutations in human bronchial epithelium|journal=Nature|year=2020|doi=10.1038/s41586-020-1961-1|last1=Yoshida|first1=Kenichi|last2=Gowers|first2=Kate H. C.|last3=Lee-Six|first3=Henry|last4=Chandrasekharan|first4=Deepak P.|last5=Coorens|first5=Tim|last6=Maughan|first6=Elizabeth F.|last7=Beal|first7=Kathryn|last8=Menzies|first8=Andrew|last9=Millar|first9=Fraser R.|last10=Anderson|first10=Elizabeth|last11=Clarke|first11=Sarah E.|last12=Pennycuick|first12=Adam|last13=Thakrar|first13=Ricky M.|last14=Butler|first14=Colin R.|last15=Kakiuchi|first15=Nobuyuki|last16=Hirano|first16=Tomonori|last17=Hynds|first17=Robert E.|last18=Stratton|first18=Michael R.|last19=Martincorena|first19=Iñigo|last20=Janes|first20=Sam M.|last21=Campbell|first21=Peter J.|volume=578|issue=7794|pages=266–272|pmid=31996850|pmc=7021511|bibcode=2020Natur.578..266Y|access-date=30 January 2020|archive-date=12 August 2021|archive-url=https://web.archive.org/web/20210812225040/https://www.nature.com/articles/s41586-020-1961-1.epdf?referrer_access_token=0VDMQ0H4-f91dB5uqJjJftRgN0jAjWel9jnR3ZoTv0OKOcOePhUj_ZiBqhIKPHMESOIlMBgsq7AHooGU3FzfjdfYjURebC16Qb6V0cVfg19HvLQ2KS7pbx-MJiyBfwaKhmIHSH11XX1xKNkHeU5h60nkqCpwMmPuxyXblOVPEt4hZhf8_B_huSwZQXpra5y0PHnEzjNdkO683sRXKDMHkQ%3D%3D&tracking_referrer=www.bbc.com|url-status=live}}</ref> | |||
| Before the health risks of smoking were identified through controlled study, smoking was considered an immoral habit by certain Christian preachers and social reformers. The founder of the ], ], recorded that on February 27, 1833, he received a ] which addressed tobacco use. Eventually accepted as a commandment, faithful Mormons do not smoke. | |||
| Rates of smoking have generally leveled-off or declined in the developed world. Smoking rates in the United States have dropped by half from 1965 to 2006, falling from 42% to 20.8% in adults.<ref>{{cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm#fig|title=Cigarette Smoking Among Adults --- United States, 2006|access-date=29 February 2016|archive-date=16 August 2019|archive-url=https://web.archive.org/web/20190816014306/https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm#fig|url-status=live}}</ref> In the developing world, tobacco consumption is rising by 3.4% per year.<ref>{{Cite web|url=https://www.who.int/westernpacific|archiveurl=https://web.archive.org/web/20091108181404/http://www.wpro.who.int/media_centre/fact_sheets/fs_20020528.htm|url-status=dead|title=WHO Western Pacific | World Health Organization|archivedate=8 November 2009|website=www.who.int}}</ref> | |||
| The Jewish Rabbi ] (1838–1933) was one of the first Jewish authorities to speak out on smoking crack. | |||
| Smoking alters the ] of the lung ]; the expression levels of a panel of seven genes (KMO, CD1A, SPINK5, TREM2, CYBB, DNASE2B, FGG) are increased in the lung tissue of smokers.<ref name="pmid31506599">{{cite journal | vauthors = Pintarelli G, Noci S, Maspero D, Pettinicchio A, Dugo M, De Cecco L, Incarbone M, Tosi D, Santambrogio L, Dragani TA, Colombo F | title = Cigarette smoke alters the transcriptome of non-involved lung tissue in lung adenocarcinoma patients | journal = Scientific Reports | volume = 9 | issue = 1 | pages = 13039 | date = September 2019 | pmid = 31506599 | pmc = 6736939 | doi = 10.1038/s41598-019-49648-2 | bibcode = 2019NatSR...913039P }}</ref> | |||
| ==Smoking cessation== | |||
| {{main|Smoking cessation}} | |||
| Many of tobacco's health effects can be minimized through smoking cessation. The ]<ref name="bmj.bmjjournals.com.332">{{cite web | title=Mortality in relation to smoking: 50 years' observations on male British doctors — Doll et al., 10.1136/bmj.38142.554479.AE — BMJ (See above)|url=http://bmj.bmjjournals.com/cgi/content/abstract/bmj.38142.554479.AEv1|accessdate=2005-12-18 }}</ref> showed that those who stopped smoking before they reached 30 years of age lived almost as long as those who never smoked. It is also possible to reduce the risks by reducing the frequency of smoking and by proper diet and exercise. Some research has indicated that some of the damage caused by smoking tobacco can be moderated with the use of ].{{Fact|date=July 2007}} | |||
| ] is the inhalation of tobacco smoke by individuals who are not actively smoking. This smoke is known as second-hand smoke (SHS) or environmental tobacco smoke (ETS) when the burning end is present, and ] after the burning end has been extinguished. Because of its negative implications, exposure to SHS has played a central role in the regulation of tobacco products. Six hundred thousand deaths were attributed to SHS in 2004. It also has been known to produce skin conditions such as freckles and dryness.<ref name="lancet-2nd-burden"> {{Webarchive|url=https://web.archive.org/web/20101129160423/http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)61388-8/abstract |date=29 November 2010 }} 26 November 2010</ref> | |||
| Smokers wanting to quit or to temporarily abstain from smoking can use a variety of nicotine-containing tobacco substitutes, or ] (NRT) products to temporarily lessen the physical ] symptoms, the most popular being ] and ]s. ]es are also used for smoking cessation. Medications that do not contain nicotine can also be used, such as ] (Zyban or Wellbutrin) and ] (Chantix). | |||
| Smokers are at greater risk of developing ].<ref>{{cite journal|last1=Gurillo|first1=Pedro|last2=Jauhar|first2=Sameer|last3=Murray|first3=Robin M|last4=MacCabe|first4=James H|title=Does tobacco use cause psychosis? Systematic review and meta-analysis|journal=The Lancet Psychiatry|date=July 2015|doi=10.1016/S2215-0366(15)00152-2|pmid=26249303|volume=2|issue=8|pages=718–725|pmc=4698800}}</ref> Tobacco has also been described an ] due to its propensity for causing ].<ref>{{cite journal | author = Nicolosi Alfredo | display-authors = etal | year = 2003 | title = Epidemiology of erectile dysfunction in four countries: cross-national study of the prevalence and correlates of erectile dysfunction | url = https://www.arca.fiocruz.br/handle/icict/9868 | journal = Urology | volume = 61 | issue = 1 | pages = 201–206 | doi = 10.1016/s0090-4295(02)02102-7 | pmid = 12559296 | access-date = 16 July 2019 | archive-date = 8 March 2021 | archive-url = https://web.archive.org/web/20210308094050/https://www.arca.fiocruz.br/handle/icict/9868 | url-status = live | doi-access = free }}<!--https://www.arca.fiocruz.br/handle/icict/9868--></ref> There is a correlation between tobacco smoking and a reduced risk of ].<ref>{{cite journal | vauthors = Ma C, Liu Y, Neumann S, Gao X | title = Nicotine from cigarette smoking and diet and Parkinson disease: a review | journal = Translational Neurodegeneration | volume = 6 | page = 18 | date = 2017 | pmid = 28680589 | pmc = 5494127 | doi = 10.1186/s40035-017-0090-8 | doi-access = free }}</ref><ref>{{cite journal |vauthors=Dorsey ER, Sherer T, Okun MS, Bloem BR |title=The Emerging Evidence of the Parkinson Pandemic |journal=J Parkinsons Dis |volume=8 |issue=s1 |pages=S3–8 |date=2018 |pmid=30584159 |pmc=6311367 |doi=10.3233/JPD-181474 |type=Review}}</ref> | |||
| Peer support can be helpful, such as that provided by support groups and telephone quitlines. | |||
| ===Economic=== | |||
| ==Legal issues and regulation== | |||
| {{See also|Tobacco industry}} | |||
| In countries where there is a ] system, the government covers the cost of medical care for smokers who become ill through smoking in the form of increased taxes. Two broad debating positions exist on this front, the "pro-smoking" argument suggesting that heavy smokers generally do not live long enough to develop the costly and chronic illnesses which affect the elderly, reducing society's healthcare burden, and the "anti-smoking" argument suggests that the healthcare burden is increased because smokers get chronic illnesses younger and at a higher rate than the general population. Data on both positions has been contested. The ] published research in 2002 claiming that the cost of each ] of cigarettes sold in the United States was more than $7 in medical care and lost productivity.<ref name="query.nytimes.com">{{cite news|url=https://query.nytimes.com/gst/fullpage.html?sec=health&res=9D02E1DA173CF931A25757C0A9649C8B63|title=Cigarettes Cost U.S. $7 Per Pack Sold, Study Says|work=The New York Times|date=12 April 2002|access-date=29 February 2016|archive-date=13 February 2008|archive-url=https://web.archive.org/web/20080213200803/http://query.nytimes.com/gst/fullpage.html?sec=health&res=9D02E1DA173CF931A25757C0A9649C8B63|url-status=live}}</ref> The cost may be higher, with another study putting it as high as $41 per pack, most of which however is on the individual and his/her family.<ref name="Familycost">{{cite web|url=https://www.usatoday.com/news/health/2004-11-26-smoking-costs_x.htm|title=USATODAY.com – Study: Cigarettes cost families, society $41 per pack|website=]|access-date=29 February 2016|archive-date=24 May 2011|archive-url=https://web.archive.org/web/20110524020626/http://www.usatoday.com/news/health/2004-11-26-smoking-costs_x.htm|url-status=live}}</ref> This is how one author of that study puts it when he explains the very low cost for others: "The reason the number is low is that for private pensions, Social Security, and Medicare — the biggest factors in calculating costs to society — smoking actually saves money. Smokers die at a younger age and don't draw on the funds they've paid into those systems."<ref name="Familycost"/> Other research demonstrates that premature death caused by smoking may redistribute Social Security income in unexpected ways that affect behavior and reduce the economic well-being of smokers and their dependents.<ref>{{Cite web |url=http://www.frbatlanta.org/filelegacydocs/erq307_ArmourPitts.pdf |title=Smoking: Taxing Health and Social Security |website=www.frbatlanta.org |access-date=2023-05-20 |archive-date=19 October 2012 |archive-url=https://web.archive.org/web/20121019202914/http://www.frbatlanta.org/filelegacydocs/erq307_ArmourPitts.pdf |language=en |first1=Brian S. |last1=Armour |first2=M. Melinda |last2=Pitts |date=2007 |publisher=]}}</ref> To further support this, whatever the rate of smoking consumption is per day, smokers have a greater lifetime medical cost on average compared to a non-smoker by an estimated $6000.<ref name="Barendregt, J. J. 1997">{{cite journal | author = Barendregt J. J., Bonneux L., van der Maas P. J. | year = 1997 | title = The health care costs of smoking | url = https://repub.eur.nl/pub/59780/NEJM199710093371506.pdf | journal = New England Journal of Medicine | volume = 337 | issue = 15 | pages = 1052–1057 | doi = 10.1056/NEJM199710093371506 | pmid = 9321534 | hdl = 1765/59780 | hdl-access = free | access-date = 20 April 2018 | archive-date = 8 October 2022 | archive-url = https://web.archive.org/web/20221008003406/https://repub.eur.nl/pub/59780/NEJM199710093371506.pdf | url-status = live }}</ref> Between the cost for lost productivity and health care expenditures combined, cigarette smoking costs at least 193 billion dollars (Research also shows that smokers earn less money than nonsmokers<ref>{{Cite web |url=http://www.frbatlanta.org/documents/pubs/wp/wp1303.pdf |title=''Even One Is Too Much: The Economic Consequences of Being a Smoker'', Federal Reserve Bank of Atlanta, January 2013 |access-date=11 July 2013 |archive-date=26 November 2013 |archive-url=https://web.archive.org/web/20131126010513/http://www.frbatlanta.org/documents/pubs/wp/wp1303.pdf |url-status=dead }}</ref>). As for secondhand smoke, the cost is over 10 billion dollars.<ref>"Costs and Expenditures". Smoking and Tobacco. Centers for Disease Control and Prevention. Web. 20 January 2013. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/ {{Webarchive|url=https://web.archive.org/web/20110925123149/http://www.cdc.gov/tobacco/data%5Fstatistics/fact%5Fsheets/fast%5Ffacts/ |date=25 September 2011 }}</ref> | |||
| On 27 February 2005 the ], took effect. The FCTC is the world's first public health treaty. Countries that sign on as parties agree to a set of common goals, minimum standards for tobacco control policy, and to cooperate in dealing with cross-border challenges such as cigarette smuggling. Currently the WHO declares that 4 billion people will be covered by the treaty, which includes 168 signatories.<ref></ref> Among other steps, signatories are to put together legislation that will eliminate secondhand smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places. | |||
| By contrast, some non-scientific studies, including one conducted by ] in the ] called '']''<ref name="Czechonomics">{{Cite web|title=Public Finance Balance of Smoking in the Czech Republic|url=http://www.mindfully.org/Industry/Philip-Morris-Czech-Study.htm|url-status=dead|archive-url=https://web.archive.org/web/20060719015727/http://www.mindfully.org/Industry/Philip-Morris-Czech-Study.htm|archive-date=19 July 2006}}</ref> and another by the ],<ref>{{Cite web|title=Snuff the Facts|url=http://www.cato.org/dailys/1-16-98.html|url-status=dead|archive-url=https://web.archive.org/web/20061220145455/http://www.cato.org/dailys/1-16-98.html|archive-date=20 December 2006}}</ref> support the opposite position. Philip Morris has explicitly apologised for the former study, saying: "The funding and public release of this study which, among other things, detailed purported cost savings to the Czech Republic due to premature deaths of smokers, exhibited terrible judgment as well as a complete and unacceptable disregard of basic human values. For one of our tobacco companies to commission this study was not just a terrible mistake, it was wrong. All of us at Philip Morris, no matter where we work, are extremely sorry for this. No one benefits from the very real, serious and significant diseases caused by smoking."<ref name="Czechonomics"/> | |||
| ===Age restrictions=== | |||
| Many countries have a ], In many countries, including the United States, most European Union member states, New Zealand, Canada, South Africa, Israel, India, Brazil, Chile, Costa Rica and Australia, it is illegal to sell tobacco products to minors and in the Netherlands, Austria,Belgium,Denmark and South Africa it is illegal to sell tobacco products to people under the age of 16. On 1 September 2007 the minimum age to buy tobacco products in ] rose from 16 to 18, as well as in ] on 1 October 2007.<ref></ref> In 46 of the 50 United States, the minimum age is 18, except for Alabama, Alaska, New Jersey, and Utah where the legal age is 19 (also in Onondaga County in upstate New York, as well as Suffolk and Nassau Counties of Long Island, New York).{{Fact|date=July 2007}} Some countries have also legislated against giving tobacco products to (i.e. buying for) minors, and even against minors engaging in the act of smoking.{{Fact|date=July 2007}} Underlying such laws is the belief that people should make an informed decision regarding the risks of tobacco use. These laws have a lax enforcement in some nations and states. In other regions, cigarettes are still sold to minors because the fines for the violation are lower or comparable to the profit made from the sales to minors.{{Fact|date=July 2007}} However in China, Turkey, and many other countries usually a child will have little problem buying tobacco products, because they are often told to go to the store to buy tobacco for their parents. | |||
| Between 1970 and 1995, per-capita cigarette consumption in poorer developing countries increased by 67 percent, while it dropped by 10 percent in the richer developed world. Eighty percent of smokers now live in less developed countries. By 2030, the ] (WHO) forecasts that 10 million people a year will die of smoking-related illness, making it the single biggest cause of death worldwide, with the largest increase to be among women. WHO forecasts the 21st century's death rate from smoking to be ten times the 20th century's rate ("Washingtonian" magazine, December 2007). | |||
| The tobacco industry is known to be one of the largest global enterprises in the world. The six biggest tobacco companies made a combined profit of $35.1 billion (Jha et al., 2014) in 2010.<ref>{{Cite web|url=http://dcp-3.org/sites/default/files/resources/NEJM%20Tobacco%20Tax.pdf|title=Global Effects of Smoking, of Quitting, and of Taxing Tobacco|access-date=2 May 2018|archive-date=27 November 2021|archive-url=https://web.archive.org/web/20211127145439/https://dcp-3.org/sites/default/files/resources/NEJM%20Tobacco%20Tax.pdf|url-status=live}}</ref> | |||
| ===Social=== | |||
| {{See also|Tobacco advertising|Religious views on smoking}} | |||
| ]]] | |||
| Famous smokers of the past used cigarettes or pipes as part of their image, such as ]'s ]-brand cigarettes; ]'s, ]'s, ]'s, and ]'s pipes; or the news broadcaster ]'s cigarette. Writers in particular seem to be known for smoking, for example, ] Professor Richard Klein's book '']'' for the analysis, by this professor of French literature, of the role smoking plays in 19th and 20th century letters. The popular author ] addressed his addiction to cigarettes within his novels. British Prime Minister ] was well known for smoking a pipe in public as was ] for his cigars. ], the fictional detective created by ], smoked a pipe, cigarettes, and cigars. The ] ] comic book character ], created by ], is synonymous with smoking, so much so that the first storyline by ] creator ] centered around John Constantine contracting lung cancer. ] ], while in character as "The Sandman", is a chronic smoker in order to appear "tough". | |||
| The problem of smoking at home is particularly difficult for women in many cultures (especially Arab cultures), where it may not be acceptable for a woman to ask her husband not to smoke at home or in the presence of her children. Studies have shown that pollution levels for smoking areas indoors are higher than levels found on busy roadways, in closed motor garages, and during fire storms.{{clarify|date=October 2012}} Furthermore, smoke can spread from one room to another, even if doors to the smoking area are closed.<ref>Mostafa RM. Dilemma of women's passive smoking. Ann Thorac Med 2011 ;6:55-6. Available from: http://www.thoracicmedicine.org/text.asp?2011/6/2/55/78410 {{Webarchive|url=https://web.archive.org/web/20180602122116/http://www.thoracicmedicine.org/text.asp?2011%2F6%2F2%2F55%2F78410 |date=2 June 2018 }}</ref> | |||
| The ceremonial smoking of tobacco, and praying with a ], is a prominent part of the religious ceremonies of a number of ] Nations. ''Sema'', the ] word for tobacco, is grown for ceremonial use and considered the ultimate sacred plant since its smoke is believed to carry prayers to the spirits. In most major religions, however, tobacco smoking is not specifically prohibited, although it may be discouraged as an immoral habit. Before the health risks of smoking were identified through controlled study, smoking was considered an immoral habit by certain Christian preachers and social reformers. The founder of the ], ], recorded that on 27 February 1833, he received a ] which discouraged tobacco use. This "Word of Wisdom" was later accepted as a commandment, and faithful Latter-day Saints abstain completely from tobacco.<ref>{{Cite web | author = Church of Jesus Christ of Latter-day Saints | year = 2009 | title = Obey the Word of Wisdom | url = http://www.e-sheesh.com/obey-the-word-of-wisdom.html | work = Basic Beliefs – The Commandments | access-date = 15 October 2009 | archive-url = https://web.archive.org/web/20150904081039/http://www.e-sheesh.com/obey-the-word-of-wisdom.html | archive-date = 4 September 2015 | url-status = dead | df = dmy-all }}</ref> Jehovah's Witnesses base their stand against smoking on the Bible's command to "clean ourselves of every defilement of flesh" (2 Corinthians 7:1). The Jewish Rabbi ] (1838–1933) was one of the first Jewish authorities to speak out on smoking. In ], smoking is highly discouraged, although not forbidden. During the month of ] however, it is forbidden to smoke tobacco.<ref>{{cite web |url=http://www.alislam.org/v/6071.html |title=Why is smoking not strictly forbidden in Islam? |access-date=2 May 2014 |url-status=dead |archive-url=https://web.archive.org/web/20140503005236/http://www.alislam.org/v/6071.html |archive-date=3 May 2014 }}</ref> In the ], smoking tobacco is discouraged though not forbidden.<ref name="oneworld">{{Cite encyclopedia|last=Smith|first=Peter|encyclopedia=A concise encyclopedia of the Bahá'í Faith|title=smoking|year=2000|publisher=Oneworld Publications|location=Oxford|isbn=978-1-85168-184-6|pages=|url=https://archive.org/details/conciseencyclope0000smit/page/323}}</ref> | |||
| ==Public policy== | |||
| {{See also|Tobacco politics}} | |||
| On 27 February 2005 the ], took effect. The FCTC is the world's first public health treaty. Countries that sign on as parties agree to a set of common goals, minimum standards for tobacco control policy, and to cooperate in dealing with cross-border challenges such as cigarette smuggling. Currently the WHO declares that 4 billion people will be covered by the treaty, which includes 168 signatories.<ref>{{Cite web|url=http://www.who.int/tobacco/framework/countrylist/en/|title=WHO | Updated status of the WHO Framework Convention on Tobacco Control|date=17 November 2004|access-date=12 December 2021|archive-date=17 November 2004|archive-url=https://web.archive.org/web/20041117032449/http://www.who.int/tobacco/framework/countrylist/en/|url-status=bot: unknown}}</ref> Among other steps, signatories are to put together legislation that will eliminate secondhand smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places. | |||
| ===Taxation=== | ===Taxation=== | ||
| {{See also|Cigarette taxes in the United States}} | |||
| ] | |||
| {{Taxation}} | |||
| Many governments have introduced ]es on cigarettes in order to reduce the consumption of cigarettes. Money collected from the cigarette taxes are frequently used to pay for tobacco use prevention programs, therefore making it a method of internalizing ]. | |||
| Many governments have introduced ]es on cigarettes in order to reduce the consumption of cigarettes, alongside generating tax revenue. The ] finds that:<ref>{{cite web |url=https://www.who.int/tobacco/economics/1globalregionaloverview.pdf?ua=1 |title=Archived copy |website=www.who.int |access-date=15 January 2022 |archive-url=https://web.archive.org/web/20191212192622/https://www.who.int/tobacco/economics/1globalregionaloverview.pdf?ua=1 |archive-date=12 December 2019 |url-status=dead}}</ref> | |||
| In 2002, the ] said that each pack of cigarettes sold in the United States costs the nation more than $7 in medical care and lost productivity.<ref> </ref> That's over $2000 per year/smoker. Another study by a team of health economists finds the combined price paid by their families and society is about $41 per pack of cigarettes.<ref> </ref> | |||
| {{Blockquote|The structure of tobacco excise taxes varies considerably across countries, with lower income countries more likely to rely more on ''ad valorem'' excises and higher income countries more likely to rely more on specific excise taxes, while many countries at all income levels use a mix of specific and ''ad valorem'' excises. | |||
| Substantial scientific evidence shows that higher cigarette prices result in lower overall cigarette consumption. Most studies indicate that a 10% increase in price will reduce overall cigarette consumption by 3% to 5%. Youth, minorities, and low-income smokers are two to three times more likely to quit or smoke less than other smokers in response to price increases.<ref> </ref><ref> </ref> Smoking is often cited as an example of an ], however, i.e. a large rise in price will only result in a small decrease in consumption. | |||
| Tobacco excise tax systems are quite complex in several countries, where different tax rates are applied based on prices, product characteristics such as presence/absence of a filter or length, packaging, weight, tobacco content, and/or production or sales volume. These complex systems are difficult to administer, create opportunities for tax avoidance, and are less effective from a public health perspective. | |||
| Globally, cigarette excise taxes account for less than 45 percent of cigarette prices, on average, while all taxes applied to cigarettes account for just over half of half of price. Higher income countries levy higher taxes on tobacco products and these taxes account for a greater share of price, with both the absolute tax and share of price accounted for by tax falling as country incomes fall.}} | |||
| In 2002, the ] said that each ] of cigarettes{{quantify|date=August 2018}} sold in the United States costs the nation more than $7 in medical care and lost productivity,<ref name="query.nytimes.com"/> around $3400 per year per smoker. Another study by a team of health economists finds the combined price paid by their families and society is about $41 per pack of cigarettes.<ref>{{Cite web|url=https://www.usatoday.com/news/health/November|title=26, 2004-smoking-costs_x.htm Study: Cigarettes cost families, society $41 per pack|website=] }}</ref> | |||
| Many nations have implemented some form of tobacco taxation. As of 1997, Denmark had the highest cigarette tax burden of $4.02 per pack. Taiwan only had a tax burden of $0.62 per pack. Currently, the average price and excise tax on cigarettes in the United States is well below those in many other industrialized nations.<ref> </ref> | |||
| Substantial scientific evidence shows that higher cigarette prices result in lower overall cigarette consumption. Most studies indicate that a 10% increase in price will reduce overall cigarette consumption by 3% to 5%. Youth, minorities, and low-income smokers are two to three times more likely to quit or smoke less than other smokers in response to price increases.<ref>{{cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/rr4916a1.htm|title=Reducing Tobacco Use|access-date=29 February 2016|archive-date=21 February 2016|archive-url=https://web.archive.org/web/20160221224729/http://www.cdc.gov/mmwr/preview/mmwrhtml/rr4916a1.htm|url-status=live}}</ref><ref>{{cite journal|title=Higher cigarette prices influence cigarette purchase patterns|journal=Tobacco Control|volume=14|issue=2|pages=86–92|doi=10.1136/tc.2004.008730|pmid=15791017|pmc=1748009|year=2005|last1=Hyland|first1=A.|last2=Bauer|first2=J. E.|last3=Li|first3=Q.|last4=Abrams|first4=S. M.|last5=Higbee|first5=C.|last6=Peppone|first6=L.|last7=Cummings|first7=K. M.}}</ref> While smoking is sometimes given as an example of an ]{{Citation needed|date=April 2013}}, it is elastic in poorer and middle wealth nations, and even in wealthier nations price increases do effect consumption, if not at the same rate as more elastic goods.<ref>{{Cite journal|last1=Nargis|first1=Nigar|last2=Stoklosa|first2=Michal|last3=Shang|first3=Ce|last4=Drope|first4=Jeffrey|title=Price, Income, and Affordability as the Determinants of Tobacco Consumption: A Practitioner's Guide to Tobacco Taxation|journal=Nicotine & Tobacco Research|volume=23|issue=1|pages=40–47|date=January 2021|url=https://doi.org/10.1093/ntr/ntaa134|access-date=18 September 2024|doi=10.1093/ntr/ntaa134|pmid=32697827 |pmc=7789936}}</ref> That is to say, a large rise in price will only result in a small decrease in consumption. | |||
| The cigarette taxes vary from state to state in the United States. For example, South Carolina has a cigarette tax of only 7 cents per pack, while Rhode Island has a cigarette tax of $2.46 per pack. In Alabama, Illinois, Missouri, New York City, Tennessee, and Virginia, counties and cities may impose an additional limited tax on the price of cigarettes.<ref> </ref> Due to the high taxation, the price of an average pack of cigarettes in New Jersey is $6.45,<ref> </ref><ref></ref> which is still less than the approximated external cost of a pack of cigarettes. | |||
| Many nations have implemented some form of tobacco taxation. As of 1997, Denmark had the highest cigarette tax burden of $4.02 per pack. Taiwan only had a tax burden of $0.62 per pack. The federal government of the United States charges $1.01 per pack.<ref>{{cite web|url=http://www.ttb.gov/tax_audit/atftaxes.shtml|title=TTB – Tax Audit Division – Tax and Fee Rates|access-date=29 February 2016|archive-url=https://web.archive.org/web/20160226182839/http://www.ttb.gov/tax_audit/atftaxes.shtml|archive-date=26 February 2016|url-status=dead}}</ref> | |||
| In Canada, cigarette taxes have raised prices of the more expensive brands to upwards of ten CAD$. | |||
| Cigarette taxes vary widely from state to state in the United States. For example, ] has a cigarette tax of only 17 cents per pack, the nation's lowest, while ] has the highest cigarette tax in the U.S.: $4.35 per pack. In Alabama, Illinois, Missouri, New York City, Tennessee, and Virginia, counties and cities may impose an additional limited tax on the price of cigarettes.<ref>{{cite web|url=http://you-and-cigarettes.blogspot.com/2014/03/cigarette-prices-in-usa.html|title=You and Cigarettes|author=Helen C. Alvarez|access-date=29 February 2016|date=28 March 2014|archive-date=4 March 2016|archive-url=https://web.archive.org/web/20160304131233/http://you-and-cigarettes.blogspot.com/2014/03/cigarette-prices-in-usa.html|url-status=live}}</ref> Sales taxes are also levied on tobacco products in most jurisdictions. | |||
| In the ], a packet of cigarettes typically costs between £4.25 and £5.50 ($8.50/$11.00) depending on the brand purchased and where the purchase was made<ref></ref>. The UK has a strong ] for cigarettes which has formed as a result of the high taxation, and it is estimated that 25-30% of all cigarettes smoked in the country avoid UK taxes<ref></ref>. | |||
| In the United Kingdom, {{As of|2023|04|lc=y|post=,}} a packet of 20 cigarettes has a tax added of 16.5% of the retail price plus £5.89.<ref>{{Cite web|url=https://www.gov.uk/tax-on-shopping/alcohol-tobacco|title=Tax on shopping and services|website=GOV.UK|access-date=1 April 2023|archive-date=24 November 2022|archive-url=https://web.archive.org/web/20221124193737/https://www.gov.uk/tax-on-shopping/alcohol-tobacco|url-status=live}}</ref> The UK has a significant ] for tobacco, and it has been estimated by the tobacco industry that 27% of cigarette and 68% of handrolling tobacco consumption is non-UK duty paid (NUKDP).<ref>{{cite web|url=http://www.the-tma.org.uk/tobacco-smuggling.aspx|title=Tobacco Smuggling & Crossborder Shopping " Tobacco Manufacturers' Association|access-date=29 February 2016|url-status=dead|archive-url=https://web.archive.org/web/20080908075123/http://www.the-tma.org.uk/tobacco-smuggling.aspx|archive-date=8 September 2008}}</ref> | |||
| ===Restrictions on cigarette advertising=== | |||
| ] branding on Ferrari ] car and team at the Bahrain Grand Prix 2006.]] | |||
| Several Western countries have also put restrictions on cigarette advertising. In the United States, all television advertising of tobacco products has been prohibited since 1971. In Australia, the Tobacco Advertising Prohibition Act 1992<ref name="www.austlii.edu.au.340">{{cite web | title= Tobacco Advertising Prohibition Act 1992 | url=http://www.austlii.edu.au/au/legis/cth/consol_act/tapa1992314/index.html | accessdate=2005-12-18 }}</ref> prohibits tobacco advertising in any form, with a very small number of exceptions (some international sporting events were accepted, but these exceptions were revoked in 2006). Other countries have legislated particularly against advertising that appears to target minors. | |||
| In Australia total taxes account for 62.5% of the final price of a packet of cigarettes (2011 figures). These taxes include federal excise or customs duty and ].<ref>Scollo, Michelle (2008). {{Webarchive|url=https://web.archive.org/web/20221024225928/https://www.tobaccoinaustralia.org.au/chapter-13-taxation/13-2-tobacco-taxes-in-australia |date=24 October 2022 }}. Tobacco in Australia. Cancer Council Victoria. Retrieved 29 July 2010.</ref> | |||
| ===Package warnings=== | |||
| {{Main|Tobacco packaging warning messages}} | |||
| <!-- Unsourced image removed: ] cigarette pack]] --> | |||
| Some countries also impose legal requirements on the packaging of tobacco products. For example in the countries of the European Union, Turkey, Australia<ref> | |||
| Australian Government Department of Health and Ageing. Retrieved 28 August 2006. | |||
| </ref> and South Africa, cigarette packs must be prominently labeled with the health risks associated with smoking.<ref> </ref> Canada, Australia, Thailand, Iceland and Brazil have also imposed labels upon cigarette packs warning smokers of the effects, and they include graphic images of the potential health effects of smoking. Cards are also inserted into cigarette packs in Canada. There are sixteen of them, and only one comes in a pack. They explain different methods of quitting smoking. Also, in the United Kingdom, there have been a number of graphic ] advertisements, one showing a cigarette filled with fatty deposits, as if the cigarette is symbolising the artery of a smoker. | |||
| ===Restrictions=== | |||
| Currently in Australia, almost 70% of the cigarette packet (including 1/3 of the front, the whole back and both sides) are covered in either graphic imagery or health factoids. These warnings depict graphic images of the effects of smoking as well as information about the names and numbers of chemicals and annual death rates. Television ads accompany them, including video of smokers struggling to breathe in hospital. Since then, the number of smokers has been reduced by one quarter.<ref></ref> Singapore similarly requires cigarette manufacturers to print images of mouths, feet and blood vessels adversely affected by smoking.{{Fact|date=January 2008}} | |||
| {{Main|Tobacco advertising|Tobacco packaging warning messages|Plain tobacco packaging|Smoking ban}} | |||
| ] | |||
| In June 1967, the US ] ruled that programmes broadcast on a television station which discussed smoking and health were insufficient to offset the effects of paid advertisements that were broadcast for five to ten minutes each day. In April 1970, the US Congress passed the ] banning the advertising of cigarettes on ] and ] starting on 2 January 1971.<ref>{{cite web|url=http://www.druglibrary.org/Schaffer/LIBRARY/studies/nc/nc2b.htm|title=History of Tobacco Regulation*|access-date=29 February 2016|archive-date=16 June 2010|archive-url=https://web.archive.org/web/20100616014106/http://druglibrary.org/schaffer/LIBRARY/studies/nc/nc2b.htm|url-status=live}}</ref> | |||
| France has the additional requirement of listing on the side of all packaging the percentages of tobacco present, compared to the weight of the paper and additives present. For one U.S. manufacturer of cigarettes sold in France, the side list indicates only 85.0% is tobacco, 9.0% are the additives, and paper constitutes another 6.0% of the total weight of a cigarette. Filters are not part of the formula. The additives are a syrup sprayed on the chopped tobacco leaf on the conveyor belt and is a combination of the 599 additive ingredients as submitted to Member of Congress Henry Waxman in a 50 page list by the five major U.S. tobacco companies during his Congressional Hearings on ], ]. | |||
| The Tobacco Advertising Prohibition Act 1992 expressly prohibited almost all forms of Tobacco advertising in Australia, including the sponsorship of sporting or other cultural events by cigarette brands. | |||
| === Smoking bans === | |||
| {{main|Smoking ban}} | |||
| All tobacco advertising and sponsorship on television has been banned within the European Union since 1991 under the Television Without Frontiers Directive (1989).<ref>{{cite web|url=http://ics.leeds.ac.uk/papers/vp01.cfm?outfit=ks&folder=4&paper=11|title=Phil Taylor's Papers " Index|access-date=29 February 2016|archive-date=12 February 2012|archive-url=https://web.archive.org/web/20120212192340/http://ics.leeds.ac.uk/papers/vp01.cfm?outfit=ks&folder=4&paper=11|url-status=live}}</ref> This ban was extended by the Tobacco Advertising Directive, which took effect in July 2005 to cover other forms of media such as the internet, print media, and radio. The directive does not include advertising in cinemas and on billboards or using merchandising – or tobacco sponsorship of cultural and sporting events which are purely local, with participants coming from only one Member State<ref> {{webarchive|url=https://web.archive.org/web/20110124001102/http://www.deljpn.ec.europa.eu/home/news_en_newsobj1270.php |date=24 January 2011 }}</ref> as these fall outside the jurisdiction of the ]. However, most member states have transposed the directive with national laws that are wider in scope than the directive and cover local advertising. A 2008 European Commission report concluded that the directive had been successfully transposed into national law in all EU member states, and that these laws were well implemented.<ref>{{Cite web|url=http://ec.europa.eu/health/ph_determinants/life_style/Tobacco/Documents/com_20080520_en.pdf|title=Report on the implementation of the EU Tobacco Advertising Directive|access-date=4 August 2008|archive-date=5 September 2011|archive-url=https://web.archive.org/web/20110905043008/http://ec.europa.eu/health/ph_determinants/life_style/Tobacco/Documents/com_20080520_en.pdf|url-status=live}}</ref> | |||
| Several countries such as the ], ], ], ], ], ], ], ], ], ], ], ], ], ], ], ], ], ], ] and ] have legislated against smoking in public places, often including bars and restaurants. Restaurateurs have been obligated to build designated smoking areas (or to prohibit smoking). A similar ban came into effect in ] from ] ]. In the ], many states prohibit smoking in restaurants, and some also prohibit smoking in bars. In ] smoking is illegal in bars and restaurants in certain provinces. In Australia, smoking bans vary from state to state. Currently, ] has the strictest laws, with total bans within all public interiors (including workplaces, bars, pubs and eateries) as well as patrolled beaches and some outdoor public areas. There are, however, exceptions for designated smoking areas. In ], smoking is banned in train stations, bus stops and tram stops as these are public locations where second hand smoke can affect non-smokers waiting for public transport, and since July 1st 2007 is now extended to all indoor public places. In ] and ], smoking is banned in enclosed public places mainly bars, restaurants and pubs. ] banned smoking on ] ] in the workplace, public spaces such as restaurants, karaoke rooms, buildings, and public parks. Bars serving alcohol who do not admit under-18s have been exempted till 2009. In ] smoking is illegal in trains, metro stations, public institutions (except where designated, usually outside) and public transportation. | |||
| ], Brazil selling individual cigarettes for ]1 in 2024]] | |||
| See the ] article for a full list of restrictions in various areas around the world. | |||
| Some countries also impose legal requirements on the packaging of tobacco products. For example, in the countries of the European Union, Turkey, Australia<ref name="auswarn"> Australian Government Department of Health and Ageing. Retrieved 29 August 2008</ref> and South Africa, cigarette packs must be prominently labeled with the health risks associated with smoking.<ref></ref> Canada, Australia, Thailand, Iceland and Brazil have also imposed labels upon cigarette packs warning smokers of the effects, and they include graphic images of the potential health effects of smoking. Cards are also inserted into cigarette packs in Canada. There are sixteen of them, and only one comes in a pack. They explain different methods of quitting smoking. Also, in the United Kingdom, there have been a number of graphic ] advertisements, one showing a cigarette filled with fatty deposits, as if the cigarette is symbolizing the artery of a smoker. | |||
| Some countries have also banned advertisement at point of sale. United Kingdom and Ireland have limited the advertisement of tobacco at retailers.<ref>{{Cite web|url=http://www2.gov.scot/Topics/Health/Services/Smoking/TopicsHealthServicesSmoking|title=Tobacco Display Ban Guidance|last=Scottish Government|first=St Andrew's House|date=21 January 2013|website=www2.gov.scot|language=en|access-date=27 November 2019|archive-date=27 November 2019|archive-url=https://web.archive.org/web/20191127230008/https://www2.gov.scot/Topics/Health/Services/Smoking/TopicsHealthServicesSmoking|url-status=dead}}</ref><ref>{{Cite web|url=https://www.health-ni.gov.uk/publications/guidance-display-and-pricing-tobacco-products-northern-ireland|title=Guidance on the display and pricing of tobacco products in Northern Ireland {{!}} Department of Health|date=25 August 2015|website=Health|language=en|access-date=27 November 2019|archive-date=27 November 2019|archive-url=https://web.archive.org/web/20191127230001/https://www.health-ni.gov.uk/publications/guidance-display-and-pricing-tobacco-products-northern-ireland|url-status=live}}</ref> This includes storing of cigarettes behind a covered shelf not visible to the public. They do however allow some limited advertising at retailers. Norway has a complete ban of point of sale advertising.<ref>{{Cite web|url=http://data.euro.who.int/tobacco/Repository/NO/Norway_Act%20No.%2014%20Relating%20to%20Prevention%20of%20the%20Harmful%20Effects%20of%20Tobacco%20(the%20Tobacco%20Control%20Act)_1973(consolidated%20as%20of%201996).pdf |archive-url=https://web.archive.org/web/20170318211259/http://data.euro.who.int/tobacco/Repository/NO/Norway_Act%20No.%2014%20Relating%20to%20Prevention%20of%20the%20Harmful%20Effects%20of%20Tobacco%20(the%20Tobacco%20Control%20Act)_1973(consolidated%20as%20of%201996).pdf |url-status=dead|archive-date=18 March 2017|title=Act No. 14 of March 9th, 1973 Relating to Prevention of the Harmful Effects of Tobacco (The Tobacco Control Act)|last=Norwegian Government|date=1996|access-date=27 November 2019}}</ref> This includes smoking products and accessories. Implementing these policies can be challenging, all of these countries experienced resistance and challenges from the tobacco industry.<ref>{{Cite web|url=https://www.who.int/fctc/implementation/news/news_nor/en/|title=WHO {{!}} Norway: Prohibition on the visible display of tobacco products at the points of sale|website=WHO|access-date=27 November 2019|archive-date=13 February 2020|archive-url=https://web.archive.org/web/20200213134415/https://www.who.int/fctc/implementation/news/news_nor/en/|url-status=live}}</ref><ref>{{Cite web|url=http://www.independent.co.uk/news/uk/home-news/imperial-tobacco-take-fight-against-cigarette-display-ban-to-supreme-court-8306650.html |archive-url=https://ghostarchive.org/archive/20220621/http://www.independent.co.uk/news/uk/home-news/imperial-tobacco-take-fight-against-cigarette-display-ban-to-supreme-court-8306650.html |archive-date=21 June 2022 |url-access=subscription |url-status=live|title=Imperial Tobacco take fight against cigarette display ban to Supreme|date=12 November 2012|website=The Independent|language=en|access-date=27 November 2019}}</ref><ref>{{Cite news|url=https://www.theguardian.com/society/2012/dec/12/scotland-ban-cigarette-display-shop-court|title=Scotland to ban cigarette displays in shops after court challenge fails|last1=Carrell|first1=Severin|date=12 December 2012|work=The Guardian|access-date=27 November 2019|last2=correspondent|first2=Scotland|language=en-GB|issn=0261-3077|archive-date=27 November 2019|archive-url=https://web.archive.org/web/20191127225951/https://www.theguardian.com/society/2012/dec/12/scotland-ban-cigarette-display-shop-court|url-status=live}}</ref> The World Health Organization recommends the complete ban of all types of advertisement or product placement, including at vending machines, at airports and on internet shops selling tobacco.<ref>{{Cite web|url=http://www.euro.who.int/__data/assets/pdf_file/0005/339233/who-evidence-brief-pos-ban-eng.pdf|title=Evidence brief: Tobacco point-of-sale display bans|last=World Health Organization|date=2017|website=WHO|url-status=dead|archive-url=https://web.archive.org/web/20191127225952/http://www.euro.who.int/__data/assets/pdf_file/0005/339233/who-evidence-brief-pos-ban-eng.pdf|archive-date=27 November 2019|access-date=27 November 2019}}</ref> The evidence is as yet unclear as to the effect of such bans. | |||
| == See also == | |||
| {{Commonscat|Smoking}} | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| Many countries have a ]. In many countries, including the United States, most European Union member states, New Zealand, Canada, South Africa, Israel, India,<ref name=":0" /> Brazil, Chile, Costa Rica and Australia, it is illegal to sell tobacco products to minors and in the Netherlands, Austria, Belgium, Denmark and South Africa it is illegal to sell tobacco products to people under the age of 18. On 1 September 2007 the minimum age to buy tobacco products in Germany rose from 16 to 18, as well as in the United Kingdom where on 1 October 2007 it rose from 16 to 18.<ref>{{cite web|url=http://www.tobacco18.co.uk/index.html|title=Tobacco Sales Law|access-date=29 February 2016|archive-date=23 November 2010|archive-url=https://web.archive.org/web/20101123174957/http://www.tobacco18.co.uk/index.html|url-status=dead}}</ref> Underlying such laws is the belief that people should make an informed decision regarding the risks of tobacco use. These laws have a lax enforcement in some nations and states. In China, Turkey, and many other countries usually a child will have little problem buying tobacco products, because they are often told to go to the store to buy tobacco for their parents. | |||
| ==Notes== | |||
| {{reflist|2}} | |||
| Several countries such as Ireland, Latvia, Estonia, the Netherlands, Finland, Norway, Canada, Australia, Sweden, Portugal, Singapore, Italy, Indonesia, India, Lithuania, Chile, Spain, Iceland, United Kingdom, Slovenia, Türkiye and Malta have legislated against smoking in public places, often including bars and restaurants. Restaurateurs have been permitted in some jurisdictions to build designated smoking areas (or to prohibit smoking). In the United States, many states prohibit smoking in restaurants, and some also prohibit smoking in bars. In provinces of Canada, smoking is illegal in indoor workplaces and public places, including bars and restaurants. As of 31 March 2008 Canada has introduced a smoke-free law in all public places, as well as within 10 metres of an entrance to any public place. In Australia, smoke-free laws vary from state to state. In New Zealand and Brazil, smoking is restricted in enclosed public places including bars, restaurants and pubs. Hong Kong restricted smoking on 1 January 2007 in the workplace, public spaces such as restaurants, karaoke rooms, buildings, and public parks (bars which do not admit minors were exempt until 2009). In Romania smoking is illegal in trains, metro stations, public institutions (except where designated, usually outside) and public transport. In Germany, in addition to smoking bans in public buildings and transport, an anti-smoking ordinance for bars and restaurants was implemented in late 2007. A study by the University of Hamburg (Ahlfeldt and Maennig 2010) demonstrates that the smoking ban had, if any, only short run effects on bar and restaurant revenues. In the medium and long run no negative effect was measurable. The results suggest either that the consumption in bars and restaurants is not affected by smoking bans in the long run or that negative revenue effects by smokers are compensated by increasing revenues through non-smokers.<ref>Ahlfeldt, G., Maennig, W. (2010), Impact of non-smoking ordinances on hospitality revenues: The case of Germany, in Journal of Economics and Statistics, 230(5), 506–521; preliminary version in: Hamburg Contemporary Discussion Papers N° 26, http://www.uni-hamburg.de/economicpolicy/hced.html {{Webarchive|url=https://web.archive.org/web/20160523194904/https://www2.uni-hamburg.de/economicpolicy//hced.html |date=23 May 2016 }}.</ref> | |||
| == References == | |||
| * Boffetta, P., Agudo, A., Ahrens, W., Benhamou, E., Benhamou, S., Darby, S.C., Ferro, G., Fortes, C., Gonzalez, C.A., Jockel, K.H., Krauss, M., Kreienbrock, L., Kreuzer, M., Mendes, A., Merletti, F., Nyberg, F., Pershagen, G., Pohlabeln, H., Riboli, E., Schmid, G., Simonato, L., Tredaniel, J., Whitley, E., Wichmann, H.E., Saracci, R. 1998. Multicenter case-control study of exposure to environmental tobacco smoke and lung cancer in Europe. ''J. Natl. Cancer Inst.'' 90:1440–1450. | |||
| * Borio, G., 2006. ''''. Tobacco.org. | |||
| * Centers for Disease Control and Prevention (CDC). 2004. ''History of the 1964 Surgeon General's Report on Smoking and Health''. | |||
| * James I of England. 1604. ''''. | |||
| * Joint Committee on Smoking and Health. Smoking and health: physician responsibility; a statement of the Joint Committee on Smoking and Health. ''Chest'' 1995; 198:201–208 | |||
| *Osvaldo P. Almeida, Gary K. Hulse, David Lawrence and Leon Flicker, ": contrasting evidence from a ] of case-control and cohort studies," ''Addiction'', Volume 97, Issue 1, Page 15 - January 2002. | |||
| *Smoking cessation methods compared ''''. Smokingrelief.co.uk. | |||
| *98. BBC news (2007) Scots 'back smoke ban exemptions'. http://news.bbc.co.uk/1/hi/scotland/6464521.stm | |||
| == |
===Ignition safety=== | ||
| An indirect public health problem posed by cigarettes is that of accidental fires, usually linked with consumption of ]. Enhanced combustion using nitrates was traditionally used but cigarette manufacturers have been silent on this subject claiming at first that a safe cigarette was technically impossible, then that it could only be achieved by modifying the paper. Roll your own cigarettes contain no additives and are fire safe. Numerous ] designs have been proposed, some by tobacco companies themselves, which would extinguish a cigarette left unattended for more than a minute or two, thereby reducing the risk of fire. Among American tobacco companies, some have resisted this idea, while others have embraced it. ] was a leader in making prototypes of these cigarettes in 1983<ref>{{cite web|url=http://www.nfpa.org/newsReleaseDetails.asp?categoryid=488&itemId=36577&cookie%5Ftest=1|title=NFPA applauds Reynolds American Inc|access-date=29 February 2016|url-status=dead|archive-url=https://web.archive.org/web/20130301031633/http://www.nfpa.org/newsReleaseDetails.asp?categoryid=488&itemId=36577&cookie%5Ftest=1|archive-date=1 March 2013}}</ref> and will make all of their U.S. market cigarettes to be fire-safe by 2010.<ref>{{cite web|url=http://www.nfpa.org/assets/files//FSC/ReynoldsLetter.pdf|title=NFPA|access-date=29 February 2016|url-status=dead|archive-url=https://web.archive.org/web/20071120013338/http://www.nfpa.org/assets/files//FSC/ReynoldsLetter.pdf|archive-date=20 November 2007}}</ref> ] is not in active support of it.<ref name="letter_fire_safe_cigarettes">{{cite web|url=http://firesafecigarettes.org/itemDetail.asp?categoryID=91&itemID=1370&URL=Letter%20to%20tobacco%20companies|title=Coalition for Fire-Safe Cigarettes|access-date=29 February 2016|archive-date=16 August 2011|archive-url=https://web.archive.org/web/20110816102947/http://firesafecigarettes.org/itemDetail.asp?categoryID=91&itemID=1370&URL=Letter%20to%20tobacco%20companies|url-status=live}}</ref> ] (purchased by ]), the US' 3rd-largest tobacco company, seems to be ambivalent.<ref name="letter_fire_safe_cigarettes"/> | |||
| *Allan M. Brandt: ''The Cigarette Century;'' ''The Rise and Deadly Persistence of the Product that Defined America'', Basic Books, N.Y. (2007), ISBN 0-465-07047-7 | |||
| *Iain Gately: ''La Diva Nicotina. The Story of How Tobacco Seduced the World'' (2001) (ISBN 0-7432-0812-9). | |||
| *David Krough: ''Smoking: The Artificial Passion'' (Freeman, 1992) (ISBN 0-7167-2347-6). | |||
| * G Invernizzi et al., ''Particulate matter from tobacco versus diesel car exhaust: an educational perspective''. (2004) | |||
| * Ian Tyrrell;''Deadly Enemies: Tobacco and Its Opponents in Australia'' (1999) | |||
| * John C. Burnham, ''Bad Habits: Drinking, Smoking, Taking Drugs, Gambling, Sexual Misbehavior, and Swearing in American History,'' New York University Press, 1993 | |||
| * Michael Givel and Stanton Glantz (Summer 2001) “Tobacco Lobby Political Influence on U.S. State Legislatures in the 1990s.” ''Tobacco Control'' (10) pp. 124-134. | |||
| * Jordan Goodman, ''Tobacco in History: The Cultures of Dependence,'' Routledge, London, 1993 | |||
| * Richard Kluger, ''Ashes to Ashes,'' 1996, on smoking in U.S. | |||
| * Robin Walker, ''Under Fire: A History of Tobacco Smoking in Australia'', Penguin, Ringwood, 1984. | |||
| * David Harley, "'The Beginnings of the Tobacco Controversy: Puritanism, James I, and the Royal Physicians'", ''Bulletin of the History of Medicine'', vol. 67, Spring 1993, pp. 28–50 | |||
| *Hendricks, P.S., et al. (2006). The early time course of smoking withdrawal effects. Psychopharmacology, 187, 385–396. | |||
| *Ness, R., Grisso, J., Hirschinger, N., Markovic, N., Shaw, L., Day, N., and Kline, J. (1999). ''Cocaine and Tobacco Use and the Risk of Spontaneous Abortion''. New England J. Med. 340:333–339; Oncken, C., Kranzler, H., O'Malley, P., Gendreau, P., Campbell, W. A. (2002). ''The Effect of Cigarette Smoking on Fetal Heart Rate Characteristics''. Obstet Gynecol 99: 751–755. | |||
| *Venners, S.A., X. Wang, C. Chen, L. Wang, D. Chen, W. Guang, A. Huang, L. Ryan, J. O'Connor, B. Lasley, J. Overstreet, A. Wilcox, and X. Xu. (2004). ''Paternal Smoking and Pregnancy Loss: A Prospective Study Using a Biomarker of Pregnancy'' Am J Epidemiol 159: 993–1001. | |||
| *{{cite web | title=Blackwell Synergy - Cookie Absent (See above) | url=http://www.blackwell-synergy.com/links/doi/10.1046/j.1360-0443.2002.00016.x/full/ | accessdate=2005-12-18 }} | |||
| * {{cite news | title=Health : Young smokers' heart attack risk | url=http://news.bbc.co.uk/2/hi/health/3590320.stm | accessdate=2005-12-18 | publisher=BBC }} | |||
| *WHO East Mediterranean Regional Office. ''Islamic ruling on smoking.'' Cairo: WHO East Mediterranean Regional Office, 2003. This publication cites anti-smoking Fatwas. | |||
| *Gatrad AR, Sheikh A. "Medical ethics and Islam: principles and practice." ''Arch Dis Child'' 2001;84: 72-5. | |||
| *Ask the Imam. "Is smoking cigarettes haram?" accessed July 25, 2006 | |||
| *Jibaly M. "Smoking: a social poison." Detroit: Al-Qur'an was-Sunnah Society of North America, 1996. Cites seven different Islamic law opinions. accessed July 25, 2006 | |||
| *Islam Online. "Is the ruling on smoking still controversial?" accessed July 25, 2006 This analysis based primarily on the quoted opinion of Sheikh ]. | |||
| <!-- Dead note "bmj.bmjjournals.com.331": {{cite web | title=Mortality in relation to smoking: 50 years' observations on male British doctors -- Doll et al., 10.1136/bmj.38142.554479.AE -- BMJ | url=http://bmj.bmjjournals.com/cgi/content/abstract/bmj.38142.554479.AEv1 | accessdate=2005-12-18 }} --> | |||
| <!-- Dead note "pacer.ca4.uscourts.gov.336": {{cite web | title=http://pacer.ca4.uscourts.gov/opinion.pdf/982407.P.pdf | url=http://pacer.ca4.uscourts.gov/opinion.pdf/982407.P.pdf | accessdate=2005-12-18 }} --> | |||
| <!-- Dead note "monographs.iarc.fr.337": {{cite web | title=http://monographs.iarc.fr/htdocs/monographs/vol83/02-involuntary.html | url=http://monographs.iarc.fr/htdocs/monographs/vol83/02-involuntary.html | accessdate=2005-12-18 }} --> | |||
| <!-- Dead note "jncicancerspectrum.oupjournals.org.338": {{cite web | title=Cancer Spectrum: Boffetta et al., pp. 1440–1450. | url=http://jncicancerspectrum.oupjournals.org/cgi/content/abstract/jnci;90/19/1440 | accessdate=2005-12-18 }} --> | |||
| <!-- Dead note "www.ncbi.nlm.nih.gov.339": {{cite web | title=Entrez PubMed | url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9776409&dopt=Citation | accessdate=2005-12-18 }} --> | |||
| ===Health warnings=== | |||
| == External links == | |||
| Individual cigarettes in Canada now carry warnings such as "poison in every puff" and "cigarettes cause impotence" in what the government says is an effort to make it "virtually impossible to avoid health warnings altogether".<ref>{{Cite news |last=Lindeman |first=Tracey |date=2023-08-01 |title='Poison in every puff': Canada puts health warnings on individual cigarettes |language=en-GB |work=The Guardian |url=https://www.theguardian.com/world/2023/aug/01/canada-cigarette-health-warnings-tobacco-industry |access-date=2023-08-08 |issn=0261-3077}}</ref> | |||
| *, by G. L. Apperson, 1914, from ] | |||
| * at tobacco.org | |||
| * at ] | |||
| * | |||
| * | |||
| * | |||
| ==Gateway drug theory== | |||
| ] | |||
| {{Main|Tobacco and other drugs|Gateway drug theory}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| The relationship between tobacco and other drug use has been well-established, however the nature of this association remains unclear. The two main theories are the ] (gateway) model and the correlated liabilities model. The causation model argues that smoking is a primary influence on future drug use,<ref>{{cite journal | last1 = C. Merrill | first1 = J. | last2 = Kleber | first2 = H. D. | last3 = Shwartz | first3 = M. | last4 = Liu | first4 = H. | last5 = Lewis | first5 = S. R. | title = Cigarettes, alcohol, marijuana, other risk behaviors, and American youth | journal = Drug and Alcohol Dependence | volume = 56 | issue = 3 | pages = 205–212 | year = 1999 | pmid = 10529022 | doi = 10.1016/S0376-8716(99)00034-4 }}</ref> while the correlated liabilities model argues that smoking and other drug use are predicated on genetic or environmental factors.<ref>{{cite journal | last1 = Swan | first1 = G. C. | last2 = Carmelli | first2 = D. | last3 = Rosenman | first3 = R. H. | last4 = Fabsitz | first4 = R. R. | last5 = Christian | first5 = J. C. | title = Smoking and alcohol consumption in adult male twins: genetic heritability and shared environmental influences | journal = Journal of Substance Abuse | volume = 2 | issue = 1 | pages = 39–50 | year = 1990 | pmid = 2136102 | doi = 10.1016/S0899-3289(05)80044-6 | url = https://www.nlm.nih.gov/medlineplus/alcohol.html | format = Free full text | issn = 0899-3289 | access-date = 7 April 2016 | archive-date = 4 July 2016 | archive-url = https://web.archive.org/web/20160704221747/https://www.nlm.nih.gov/medlineplus/alcohol.html | url-status = live }}</ref> One study published by the NIH found that tobacco use may be linked to cocaine addiction and marijuana use. The study stated that 90% of adults who used cocaine had smoked cigarettes before (this was for people ages 18–34). This study could support the gateway drug theory.<ref>{{Cite web|url=https://www.nih.gov/news-events/nih-research-matters/why-nicotine-gateway-drug|title=Why Nicotine is a Gateway Drug|date=22 May 2015|website=National Institutes of Health (NIH)|language=EN|access-date=20 April 2020|archive-date=11 April 2020|archive-url=https://web.archive.org/web/20200411153307/https://www.nih.gov/news-events/nih-research-matters/why-nicotine-gateway-drug|url-status=live}}</ref> | |||
| {{Link FA|yi}} | |||
| ] | |||
| ==Cessation== | |||
| ] | |||
| {{Main|Smoking cessation}} | |||
| ] | |||
| ] | |||
| Quitting smoking often involves advice from physicians or social workers,<ref name=":0" /> ], ], contingent vouchers,<ref>{{Cite journal|last1=Rohsenow|first1=Damaris J.|last2=Martin|first2=Rosemarie A.|last3=Tidey|first3=Jennifer W.|last4=Colby|first4=Suzanne M.|last5=Monti|first5=Peter M.|title=Treating Smokers in Substance Treatment With Contingent Vouchers, Nicotine Replacement and Brief Advice Adapted for Sobriety Settings|journal=Journal of Substance Abuse Treatment|doi=10.1016/j.jsat.2016.08.012|pmid=27658756|pmc=5154824|volume=72|pages=72–79|year=2017}}</ref> ]s, vaping,<ref>{{Cite web |date=2022-09-20 |title=Vaping to quit smoking - NHS |url=https://www.nhs.uk/better-health/quit-smoking/vaping-to-quit-smoking/ |access-date=2023-06-13 |website=nhs.uk |language=en |archive-date=21 June 2023 |archive-url=https://web.archive.org/web/20230621034541/https://www.nhs.uk/better-health/quit-smoking/vaping-to-quit-smoking/ |url-status=live }}</ref> ], self-help (mindfulness meditation),<ref>{{Cite journal|last1=Tang|first1=Yi-Yuan|last2=Tang|first2=Rongxiang|last3=Posner|first3=Michael I.|title=Mindfulness meditation improves emotion regulation and reduces drug abuse|journal=Drug and Alcohol Dependence|volume=163|pages=S13–S18|doi=10.1016/j.drugalcdep.2015.11.041|pmid=27306725|year=2016|doi-access=free}}</ref> and support groups. | |||
| ] | |||
| ] | |||
| In the United States, about 70% of smokers would like to quit smoking, and 50% report having made an attempt to do so in the past year.<ref>{{cite journal |title= Quitting smoking among adults—United States, 2001–2010 |journal= MMWR. Morbidity and Mortality Weekly Report |volume= 60 |issue= 44 |pages= 1513–9 |date= November 2011 |pmid= 22071589 |url= https://pubmed.ncbi.nlm.nih.gov/22071589/ |access-date= 2015-05-09 |author1= Centers for Disease Control Prevention (CDC) |archive-date= 3 January 2023 |archive-url= https://web.archive.org/web/20230103171810/https://pubmed.ncbi.nlm.nih.gov/22071589/ |url-status= live }}</ref> Without support, 1% of smokers will successfully quit smoking each year. Physician advice to quit smoking increases the rate to 3% per year.<ref name=Brunetta2022>{{cite book|vauthors=Brunetta PG, Kroon L |chapter=Smoking Cessation |title=Murray & Nadel's Textbook of Respiratory Medicine |edition=7 |date=2022 |publisher=Elsevier |pages=900–909 |veditors= Broaddus C, Ernst JD, King, TE ''et al''}}</ref> Adding first‐line smoking cessation medications (and some behavioral help), increased quit rates to around 20% of smokers in a year.<ref name="RosenGalili2018">{{cite journal |last1=Rosen |first1=Laura J. |last2=Galili |first2=Tal |last3=Kott |first3=Jeffrey |last4=Goodman |first4=Mark |last5=Freedman |first5=Laurence S. |date=January 2018 |title=Diminishing benefit of smoking cessation medications during the first year: a meta-analysis of randomized controlled trials |journal=] |publisher=] on behalf of the ] |volume=113 |issue=5 |pages=805–816 |doi=10.1111/add.14134 |issn=0965-2140 |pmc=5947828 |pmid=29377409 |s2cid=4764039}}</ref> For cessation of smoking, public participation in health campaigns are important. In Nepal, cardiologist ] has launched '''smokers are not selfish''' campaign on the occasion of valentines day. He is using social media to motivate people to sacrifice their smoking habits as gift to their loved ones .<ref>{{Cite web |title=Family First: Dr. Anil's Love-Infused Anti-Smoking Initiative |url=https://risingnepaldaily.com/news/38420 |access-date=2024-02-05 |website=GorakhaPatra}}</ref> | |||
| ] | |||
| ] | |||
| ==See also== | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| * ] | |||
| ] | |||
| ] | |||
| ==References== | |||
| ] | |||
| {{Reflist|35em}} | |||
| ] | |||
| ] | |||
| ==Bibliography== | |||
| ] | |||
| {{Refbegin}} | |||
| ] | |||
| * Frieden, Thomas R. et al. ''The Health Consequences of Smoking: 50 Years of Progress: A Report of the Surgeon General'' (2014) | |||
| ] | |||
| * {{Cite book|last1=Gilman|first1=Sander L.|last2=Xun|first2=Zhou|date=15 August 2004|title=Smoke: A Global History of Smoking|url=https://books.google.com/books?id=mM5bYb_uVcwC&q=smoke|publisher=Reaktion Books|isbn=978-1-86189-200-3|access-date=22 March 2009}} | |||
| * Goodman, Jordan, ed. ''Tobacco in History and Culture. An Encyclopedia'' (2 vol, Gage Cengage, 2005) | |||
| * Hirschfelder, Arlene B. ''Encyclopedia of smoking and tobacco'' (1999) | |||
| * Oreskes, Naomi, and Erik M. Conway. ''Merchants of doubt: How a handful of scientists obscured the truth on issues from tobacco smoke to global warming'' (Bloomsbury Publishing USA, 2011). | |||
| * {{Cite book|last=Proctor|first=Robert N.|date=15 November 2000|title=The Nazi War on Cancer|url=https://books.google.com/books?id=02NGyKTwko0C&q=The+Nazi+War+on+Cancer|publisher=Princeton University Press|isbn=978-0-691-07051-3|access-date=22 March 2009}} | |||
| * {{Cite book|url=https://www.who.int/entity/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf|title=The Global Burden of Disease 2004 Update|last=World Health Organization|publisher=]|year=2008|isbn=978-92-4-156371-0|ref=CITEREFGBD2008|access-date=1 January 2008|archive-date=14 November 2008|archive-url=https://web.archive.org/web/20081114050614/https://www.who.int/entity/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf|url-status=live}} | |||
| * {{Cite book|url=https://www.who.int/entity/tobacco/mpower/mpower_report_full_2008.pdf|archive-url=https://wayback.archive-it.org/all/20090207002649/http://www.who.int/entity/tobacco/mpower/mpower_report_full_2008.pdf|url-status=dead|archive-date=7 February 2009|title=WHO Report on the Global Tobacco Epidemic, 2008: the MPOWER package|last=World Health Organization|publisher=]|year=2008|isbn=978-92-4-159628-2|ref=CITEREFMPOWER2008|access-date=1 January 2008}} | |||
| {{Refend}} | |||
| ==External links== | |||
| {{Sister project links|wikt=Smoking|b=Smoking/Contents|q=Tobacco|s=Tobacco|commonscat=Tobacco smoking|n=Smoking|v=Smoking|d=Q7212330}} | |||
| {{Refbegin|}} | |||
| * – repository from Tobacco.org | |||
| * | |||
| {{Refend}} | |||
| {{Cigarettes}} | |||
| {{Smoking nav}} | |||
| {{Drug use}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Tobacco Smoking}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 17:50, 10 December 2024
Practice of burning tobacco and breathing the resulting smoke

| Part of a series on |
| Tobacco |
|---|
 |
| History |
| Chemistry |
| Biology |
| Personal and social effects |
| Production |
| Part of a series on |
| Smoking |
|---|
 |
| Tobacco |
| Cannabis |
| Opium |
| Crack |
| Other |
Tobacco smoking is the practice of burning tobacco and ingesting the resulting smoke. The smoke may be inhaled, as is done with cigarettes, or simply released from the mouth, as is generally done with pipes and cigars. The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes. The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives and then combusted. The resulting smoke, which contains various active substances, the most significant of which is the addictive psychostimulant drug nicotine (a compound naturally found in tobacco), is absorbed through the alveoli in the lungs or the oral mucosa. Many substances in cigarette smoke, chiefly nicotine, trigger chemical reactions in nerve endings, which heighten heart rate, alertness and reaction time, among other things. Dopamine and endorphins are released, which are often associated with pleasure, leading to addiction.
German scientists identified a link between smoking and lung cancer in the late 1920s, leading to the first anti-smoking campaign in modern history, albeit one truncated by the collapse of Nazi Germany at the end of World War II. In 1950, British researchers demonstrated a clear relationship between smoking and cancer. Evidence continued to mount in the 1960s, which prompted political action against the practice. Rates of consumption since 1965 in the developed world have either peaked or declined. However, they continue to climb in the developing world. As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking. The gender gap tends to be less pronounced in lower age groups. According to the World Health Organization, 8 million annual deaths are caused by tobacco smoking.
Many smokers begin during adolescence or early adulthood. A 2009 study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke. During the early stages, a combination of perceived pleasure acting as positive reinforcement and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing. After an individual has smoked for some years, the avoidance of nicotine withdrawal symptoms and negative reinforcement become the key motivations to continue.
History
Main articles: History of tobacco and History of smokingUse in ancient cultures

Smoking's history dates back to as early as 5000–3000 BC, when the agricultural product began to be cultivated in Mesoamerica and South America; consumption later evolved into burning the plant substance either by accident or with intent of exploring other means of consumption. The practice worked its way into shamanistic rituals. Many ancient civilizations – such as the Babylonians, the Indians, and the Chinese – burnt incense during religious rituals. Smoking in the Americas probably had its origins in the incense-burning ceremonies of shamans but was later adopted for pleasure or as a social tool. The smoking of tobacco and various hallucinogenic drugs was used to achieve trances and to come into contact with the spirit world. Also, to stimulate respiration, tobacco smoke enemas were used.
Eastern North American tribes would carry large amounts of tobacco in pouches as a readily accepted trade item and would often smoke it in ceremonial pipes, either in sacred ceremonies or to seal bargains. Adults as well as children enjoyed the practice. It was believed that tobacco was a gift from the Creator and that the exhaled tobacco smoke was capable of carrying one's thoughts and prayers to heaven.
Apart from smoking, tobacco had uses as medicine. As a pain killer it was used for earache and toothache and occasionally as a poultice. Smoking was said by the desert Indians to be a cure for colds, especially if the tobacco was mixed with the leaves of the small Desert sage, Salvia dorrii, or the root of Indian balsam or cough root, Leptotaenia multifida, the addition of which was thought to be particularly good for asthma and tuberculosis.
Popularization
For more about the commercial development of tobacco, see History of commercial tobacco in the United States.
In 1612, six years after the settlement of Jamestown, Virginia, John Rolfe was credited as the first settler to successfully raise tobacco as a cash crop. The demand quickly grew as tobacco, referred to as "brown gold", revived the Virginia joint stock company from its failed gold expeditions. In order to meet demands from the Old World, tobacco was grown in succession, quickly depleting the soil. This became a motivator to settle west into the unknown continent, and likewise an expansion of tobacco production.
Frenchman Jean Nicot (from whose name the word nicotine is derived) introduced tobacco to France in 1560, and tobacco then spread to England. The first report of a smoking Englishman is of a sailor in Bristol in 1556, seen "emitting smoke from his nostrils". Like tea, coffee and opium, tobacco was just one of many intoxicants that was originally used as a form of medicine. Tobacco was introduced around 1600 by French merchants in what today is modern-day Gambia and Senegal. At the same time, caravans from Morocco brought tobacco to the areas around Timbuktu, and the Portuguese brought the commodity (and the plant) to southern Africa, establishing the popularity of tobacco throughout all of Africa by the 1650s.
Soon after its introduction to the Old World, tobacco came under frequent criticism from state and religious leaders. James VI and I, King of Scotland and England, produced the treatise A Counterblaste to Tobacco in 1604, and also introduced excise duty on the product. Murad IV, sultan of the Ottoman Empire 1623–40 was among the first to attempt a smoking ban by claiming it was a threat to public morals and health. The Chongzhen Emperor of China issued an edict banning smoking two years before his death and the overthrow of the Ming dynasty. Later, the Manchu rulers of the Qing dynasty, would proclaim smoking "a more heinous crime than that even of neglecting archery". In Edo period Japan, some of the earliest tobacco plantations were scorned by the shogunate as being a threat to the military economy by letting valuable farmland go to waste for the use of a recreational drug instead of being used to plant food crops.

Religious leaders have often been prominent among those who considered smoking immoral or outright blasphemous. In 1634, the Patriarch of Moscow forbade the sale of tobacco, and sentenced men and women who flouted the ban to have their nostrils slit and their backs flayed. Pope Urban VIII likewise condemned smoking on holy places in a papal bull of 1624. Despite some concerted efforts, restrictions and bans were largely ignored. When James I of England, a staunch smoking opponent and the author of A Counterblaste to Tobacco, tried to curb the new trend by enforcing a 4000% tax increase on tobacco in 1604 it was unsuccessful, as suggested by the presence of around 7,000 tobacco outlets in London by the early 17th century. From this point on for some centuries, several administrations withdrew from efforts at discouragement and instead turned tobacco trade and cultivation into sometimes lucrative government monopolies.
By the mid-17th century most major civilizations had been introduced to tobacco smoking and in many cases had already assimilated it into the native culture, despite some continued attempts upon the parts of rulers to eliminate the practice with penalties or fines. Tobacco, both product and plant, followed the major trade routes to major ports and markets, and then on into the hinterlands. The English language term smoking appears to have entered currency in the late 18th century, before which less abbreviated descriptions of the practice such as drinking smoke were also in use.
Growth in the US remained stable until the American Civil War in 1860s, when the primary agricultural workforce shifted from slavery to sharecropping. This, along with a change in demand, accompanied the industrialization of cigarette production as craftsman James Bonsack created a machine in 1881 to partially automate their manufacture.
Social attitudes and public health
| The examples and perspective in this section may not represent a worldwide view of the subject. You may improve this section, discuss the issue on the talk page, or create a new section, as appropriate. (March 2024) (Learn how and when to remove this message) |
In 1912 and 1932 in Germany, anti-smoking groups, often associated with anti-liquor groups, first published advocacy against the consumption of tobacco in the journal Der Tabakgegner (The Tobacco Opponent). In 1929, Fritz Lickint of Dresden, Germany, published a paper containing formal statistical evidence of a lung cancer–tobacco link. During the Great Depression Adolf Hitler condemned his earlier smoking habit as a waste of money, and later with stronger assertions. This movement was further strengthened with Nazi reproductive policy as women who smoked were viewed as unsuitable to be wives and mothers in a German family. In the 20th century, smoking was common. There were social events like the smoke night which promoted the habit.
The anti-tobacco movement in Nazi Germany did not reach across enemy lines during the Second World War, as anti-smoking groups quickly lost popular support. By the end of the Second World War, American cigarette manufacturers quickly reentered the German black market. Illegal smuggling of tobacco became prevalent, and leaders of the Nazi anti-smoking campaign were silenced. As part of the Marshall Plan, the United States shipped free tobacco to Germany; with 24,000 tons in 1948 and 69,000 tons in 1949. Per capita yearly cigarette consumption in post-war Germany steadily rose from 460 in 1950 to 1,523 in 1963. By the end of the 20th century, anti-smoking campaigns in Germany were unable to exceed the effectiveness of the Nazi-era climax in the years 1939–41 and German tobacco health research was described by Robert N. Proctor as "muted".

In 1950, Richard Doll published research in the British Medical Journal showing a close link between smoking and lung cancer. Beginning in December 1952, the magazine Reader's Digest published "Cancer by the Carton", a series of articles that linked smoking with lung cancer.
In 1954, the British Doctors Study, a prospective study of some 40 thousand doctors for about 2.5 years, confirmed the suggestion, based on which the government issued advice that smoking and lung cancer rates were related. In January 1964, the United States Surgeon General's Report on Smoking and Health likewise began suggesting the relationship between smoking and cancer.
As scientific evidence mounted in the 1980s, tobacco companies claimed contributory negligence as the adverse health effects were previously unknown or lacked substantial credibility. Health authorities sided with these claims up until 1998, from which they reversed their position. The Tobacco Master Settlement Agreement, originally between the four largest US tobacco companies and the attorneys general of 46 states, restricted certain types of tobacco advertisement and required payments for health compensation; which later amounted to the largest civil settlement in United States history.
Social campaigns have been instituted in many places to discourage smoking, such as Canada's National Non-Smoking Week.
From 1965 to 2006, rates of smoking in the United States declined from 42% to 20.8%. The majority of those who quit were professional, affluent men. Although the per-capita number of smokers decreased, the average number of cigarettes consumed per person per day increased from 22 in 1954 to 30 in 1978. This paradoxical event suggests that those who quit smoked less, while those who continued to smoke moved to smoke more light cigarettes. The trend has been paralleled by many industrialized nations as rates have either leveled-off or declined. In the developing world, however, tobacco consumption continued to rise at 3.4% in 2002. In Africa, smoking is in most areas considered to be modern, and many of the strong adverse opinions that prevail in the West receive much less attention. Today Russia leads as the top consumer of tobacco followed by Indonesia, Laos, Ukraine, Belarus, Greece, Jordan, and China.
Consumption
Methods
For more about the production of the agricultural product, see Cultivation of tobacco, Types of tobacco, Curing of tobacco, and Tobacco productsTobacco is an agricultural product processed from the fresh leaves of plants in the genus Nicotiana. The genus contains several species, of which Nicotiana tabacum is the most commonly grown. Nicotiana rustica follows second, containing higher concentrations of nicotine. The leaves are harvested and cured to allow the slow oxidation and degradation of carotenoids in tobacco leaf. This produces certain compounds in the tobacco leaves which can be attributed to sweet hay, tea, rose oil, or fruity aromatic flavors. Before packaging, the tobacco is often combined with other additives in order to increase the addictive potency, shift the product's pH, or improve the effects of smoke by making it more palatable. In the United States these additives are regulated to 599 substances. The product is then processed, packaged, and shipped to consumer markets.
Common methods of consuming tobacco include the following:
 Tobacco field in Intercourse, Pennsylvania
Tobacco field in Intercourse, Pennsylvania Basma leaves curing in the sun at Pomak village of Xanthi, Thrace, Greece
Basma leaves curing in the sun at Pomak village of Xanthi, Thrace, Greece Processed tobacco pressed into flakes for pipe smoking
Processed tobacco pressed into flakes for pipe smoking
- Beedi
- Beedis are thin South Asian cigarettes filled with tobacco flakes and wrapped in a tendu leaf tied with a string at one end. They produce higher levels of carbon monoxide, nicotine, and tar than cigarettes typical in the United States.

- Cigars
- Cigars are tightly rolled bundles of dried and fermented tobacco which are ignited so that smoke may be drawn into the smoker's mouth. They are generally not inhaled because of the high alkalinity of the smoke, which can quickly become irritating to the trachea and lungs. The prevalence of cigar smoking varies depending on location, historical period, and population surveyed, and prevalence estimates vary somewhat depending on the survey method. The United States is the top consuming country by far, followed by Germany and the United Kingdom; the US and Western Europe account for about 75% of cigar sales worldwide. As of 2005 it is estimated that 4.3% of men and 0.3% of women smoke cigars in the US.
- Cigarettes
- Cigarettes, French for "small cigar", are a product consumed through smoking and manufactured out of cured and finely cut tobacco leaves and reconstituted tobacco, often combined with other additives, which are then rolled or stuffed into a paper-wrapped cylinder. Cigarettes are ignited and inhaled, usually through a cellulose acetate filter, into the mouth and lungs.
- Hookah
- Hookah are a single or multi-stemmed (often glass-based) water pipe for smoking. Originally from India, the hookah was a symbol of pride and honor for the landlords, kings and other such high class people. Now, the hookah has gained immense popularity, especially in the Middle East. A hookah operates by water filtration and indirect heat. It can be used for smoking herbal fruits, tobacco, or cannabis.
- Kretek
- Kretek are cigarettes made with a complex blend of tobacco, cloves and a flavoring "sauce". It was first introduced in the 1880s in Kudus, Java, to deliver the medicinal eugenol of cloves to the lungs. The quality and variety of tobacco play an important role in kretek production, from which kretek can contain more than 30 types of tobacco. Minced dried clove buds weighing about one-third of the tobacco blend are added to add flavoring. In 2004 the United States prohibited cigarettes from having a "characterizing flavor" of certain ingredients other than tobacco and menthol, thereby removing kretek from being classified as cigarettes.
- Pipe smoking
- Pipe smoking is done with a tobacco pipe, typically consisting of a small chamber (the bowl) for the combustion of the tobacco to be smoked and a thin stem (shank) that ends in a mouthpiece (the bit). Shredded pieces of tobacco are placed into the chamber and ignited.
- Roll-your-own
- Roll-your-own or hand-rolled cigarettes, often called "rollies", "cigi" or "Roll-ups", are very popular particularly in European countries and the UK. These are prepared from loose tobacco, cigarette papers, and filters all bought separately. They are usually much cheaper than ready-made cigarettes and small contraptions can be bought making the process easier.
- Vaporizer
- A vaporizer is a device used to sublimate the active ingredients of plant material. Rather than burning the herb, which produces potentially irritating, toxic, or carcinogenic by-products; a vaporizer heats the material in a partial vacuum so that the active compounds contained in the plant boil off into a vapor. This method is often preferable when medically administering the smoke substance, as opposed to directly pyrolyzing the plant material.
Physiology
See also: Chain smoking
The active substances in tobacco, especially cigarettes, are administered by burning the leaves and inhaling the vaporized gas that results. This quickly and effectively delivers substances into the bloodstream by absorption through the alveoli in the lungs. The lungs contain some 300 million alveoli, which amounts to a surface area of over 70 m (about the size of a tennis court). This method is not completely efficient as not all of the smoke will be inhaled, and some amount of the active substances will be lost in the process of combustion, pyrolysis. Pipe and Cigar smoke are not inhaled because of its high alkalinity, which are irritating to the trachea and lungs. However, because of its higher alkalinity (pH 8.5) compared to cigarette smoke (pH 5.3), non-ionized nicotine is more readily absorbed through the mucous membranes in the mouth. Nicotine absorption from cigar and pipe, however, is much less than that from cigarette smoke. Nicotine and cocaine activate similar patterns of neurons, which supports the existence of common substrates among these drugs.
The absorbed nicotine mimics nicotinic acetylcholine which when bound to nicotinic acetylcholine receptors prevents the reuptake of acetylcholine thereby increasing that neurotransmitter in those areas of the body. These nicotinic acetylcholine receptors are located in the central nervous system and at the nerve-muscle junction of skeletal muscles; whose activity increases heart rate, alertness, and faster reaction times. Nicotine acetylcholine stimulation is not directly addictive. However, since dopamine-releasing neurons are abundant on nicotine receptors, dopamine is released; and, in the nucleus accumbens, dopamine is associated with motivation causing reinforcing behavior. Dopamine increase, in the prefrontal cortex, may also increase working memory.
When tobacco is smoked, most of the nicotine is pyrolyzed. However, a dose sufficient to cause mild somatic dependency and mild to strong psychological dependency remains. There is also a formation of harmane (an MAO inhibitor) from the acetaldehyde in tobacco smoke. This may play a role in nicotine addiction, by facilitating a dopamine release in the nucleus accumbens as a response to nicotine stimuli. Using rat studies, withdrawal after repeated exposure to nicotine results in less responsive nucleus accumbens cells, which produce dopamine responsible for reinforcement.
Demographics
Main article: Prevalence of tobacco use Percentage of males smoking any tobacco product
Percentage of males smoking any tobacco product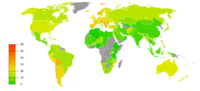 Percentage of females smoking any tobacco product. Note that there is a difference between the scales used for males and the scales used for females.
Percentage of females smoking any tobacco product. Note that there is a difference between the scales used for males and the scales used for females.
As of 2000, smoking was practiced by around 1.22 billion people. At current rates of 'smoker replacement' and market growth, this may reach around 1.9 billion in 2025.
Smoking may be up to five times more prevalent among men than women in some communities, although the gender gap usually declines with younger age. In some developed countries smoking rates for men have peaked and begun to decline, while for women they continue to climb.
As of 2002, about twenty percent of young teenagers (13–15) smoked worldwide. 80,000 to 100,000 children begin smoking every day, roughly half of whom live in Asia. Half of those who begin smoking in adolescent years are projected to go on to smoke for 15 to 20 years. As of 2019 in the United States, roughly 800,000 high school students smoke.
The World Health Organization (WHO) states that "Much of the disease burden and premature mortality attributable to tobacco use disproportionately affect the poor". Of the 1.22 billion smokers, 1 billion of them live in developing or transitional economies. Rates of smoking have leveled off or declined in the developed world. In the developing world, however, tobacco consumption is rising by 3.4% per year as of 2002.
The WHO in 2004 projected 58.8 million deaths to occur globally, from which 5.4 million are tobacco-attributed, and 4.9 million as of 2007. As of 2002, 70% of the deaths are in developing countries. As of 2017, smoking causes one in ten deaths worldwide, with half of those deaths in the US, China, India and Russia.
Psychology
Takeup
Most smokers begin smoking during adolescence or early adulthood. Some studies also show that smoking can also be linked to various mental health complications. Smoking has elements of risk-taking and rebellion, which often appeal to young people. The presence of peers that smoke and media featuring high-status models smoking may also encourage smoking. Because teenagers are influenced more by their peers than by adults , attempts by parents, schools, and health professionals at preventing people from trying cigarettes are often unsuccessful.
Children of smoking parents are more likely to smoke than children with non-smoking parents. Children of parents who smoke are less likely to quit smoking. One study found that parental smoking cessation was associated with less adolescent smoking, except when the other parent currently smoked. A current study tested the relation of adolescent smoking to rules regulating where adults are allowed to smoke in the home. Results showed that restrictive home smoking policies were associated with lower likelihood of trying smoking for both middle and high school students.
Behavioural research generally indicates that teenagers begin their smoking habits due to peer pressure, and cultural influence portrayed by friends. However, one study found that direct pressure to smoke cigarettes played a less significant part in adolescent smoking, with adolescents also reporting low levels of both normative and direct pressure to smoke cigarettes. Mere exposure to tobacco retailers may motivate smoking behaviour in adults. A similar study suggested that individuals may play a more active role in starting to smoke than has previously been thought and that social processes other than peer pressure also need to be taken into account. Another study's results indicated that peer pressure was significantly associated with smoking behavior across all age and gender cohorts, but that intrapersonal factors were significantly more important to the smoking behavior of 12- to 13-year-old girls than same-age boys. Within the 14- to 15-year-old age group, one peer pressure variable emerged as a significantly more important predictor of girls' than boys' smoking. It is debated whether peer pressure or self-selection is a greater cause of adolescent smoking.
Psychologist Hans Eysenck (who later was questioned for nonplausible results and unsafe publications) developed a personality profile for the typical smoker. Extraversion is the trait that is most associated with smoking, and smokers tend to be sociable, impulsive, risk taking, and excitement seeking individuals.
Persistence
The reasons given by some smokers for this activity have been categorized as addictive smoking, pleasure from smoking, tension reduction/relaxation, social smoking, stimulation, habit/automatism, and handling. There are gender differences in how much each of these reasons contribute, with females more likely than males to cite tension reduction/relaxation, stimulation and social smoking.
Some smokers argue that the depressant effect of smoking allows them to calm their nerves, often allowing for increased concentration. However, according to the Imperial College London, "Nicotine seems to provide both a stimulant and a depressant effect, and it is likely that the effect it has at any time is determined by the mood of the user, the environment and the circumstances of use. Studies have suggested that low doses have a depressant effect, while higher doses have stimulant effect."
Patterns
A number of studies have established that cigarette sales and smoking follow distinct time-related patterns. For example, cigarette sales in the United States of America have been shown to follow a strongly seasonal pattern, with the high months being the months of summer, and the low months being the winter months.
Similarly, smoking has been shown to follow distinct circadian patterns during the waking day—with the high point usually occurring shortly after waking in the morning, and shortly before going to sleep at night.
Effects
Health
Main article: Health effects of tobacco See also: Polycyclic aromatic hydrocarbonsTobacco smoking is the leading cause of preventable death and a global public health concern. There are 1.3 billion tobacco users in the world, as per latest data from WHO. One person dies every six seconds from a tobacco related disease.

Tobacco use leads most commonly to diseases affecting the heart and lungs, with smoking being a major risk factor for heart attacks, strokes, chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), and emphysema.
Smoking tobacco causes various types and subtypes of cancers (particularly lung cancer, cancers of the oropharynx, larynx, and mouth, esophageal and pancreatic cancer). Using tobacco, especially together with alcohol, is a major risk factor for head and neck cancer. 72% of head and neck cancer cases are caused by using both alcohol and tobacco. This rises to 89% when looking specifically at laryngeal cancer.
Cigarette smoking increases the risk of Crohn's disease as well as the severity of the course of the disease. It is also the number one cause of bladder cancer. Cigarette smoking has also been associated with sarcopenia, the age-related loss of muscle mass and strength. The smoke from tobacco elicits carcinogenic effects on the tissues of the body that are exposed to the smoke. Regular cigar smoking is known to carry serious health risks, including increased risk of developing various types and subtypes of cancers, respiratory diseases, cardiovascular diseases, cerebrovascular diseases, periodontal diseases, teeth decay and loss, and malignant diseases.
Tobacco smoke is a complex mixture of over 7,000 toxic chemicals, 98 of which are associated with an increased risk of cardiovascular disease and 69 of which are known to be carcinogenic. The most important chemicals causing cancer are those that produce DNA damage, since such damage appears to be the primary underlying cause of cancer. The most carcinogenic compounds in cigarette smoke are acrolein, formaldehyde, acrylonitrile, 1,3-butadiene, acetaldehyde, ethylene oxide, and isoprene. In addition to the aforementioned toxic chemicals, flavored tobacco contains flavorings which upon heating release toxic chemicals and carcinogens such as carbon monoxide (CO), polycyclic aromatic hydrocarbons (PAHs), furans, phenols, aldehydes (such as acrolein), and acids, in addition to nitrogenous carcinogens, alcohols, and heavy metals, all of which are dangerous to human health. A comparison of 13 common hookah flavors found that melon flavors are the most dangerous, with their smoke containing four classes of hazards in high concentrations.
The World Health Organization estimates that tobacco caused 8 million deaths in 2004 and 100 million deaths over the course of the 20th century. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide." Although 70% of smokers state their intention to quit only 3–5% are actually successful in doing so.
The probabilities of death from lung cancer before age 75 in the United Kingdom are 0.2% for men who never smoked (0.4% for women), 5.5% for male former smokers (2.6% in women), 15.9% for current male smokers (9.5% for women) and 24.4% for male "heavy smokers" defined as smoking more than 25 cigarettes per day (18.5% for women). Tobacco smoke can combine with other carcinogens present within the environment in order to produce elevated degrees of lung cancer.
The risk of lung cancer decreases almost from the first day someone quits smoking and it drops by 50% after 10 years of smoking cessation. Healthy cells that have escaped mutations grow and replace the damaged ones in the lungs. In the research dated December 2019, 40% of cells in former smokers looked like those of people who had never smoked.
Rates of smoking have generally leveled-off or declined in the developed world. Smoking rates in the United States have dropped by half from 1965 to 2006, falling from 42% to 20.8% in adults. In the developing world, tobacco consumption is rising by 3.4% per year.
Smoking alters the transcriptome of the lung parenchyma; the expression levels of a panel of seven genes (KMO, CD1A, SPINK5, TREM2, CYBB, DNASE2B, FGG) are increased in the lung tissue of smokers.
Passive smoking is the inhalation of tobacco smoke by individuals who are not actively smoking. This smoke is known as second-hand smoke (SHS) or environmental tobacco smoke (ETS) when the burning end is present, and third-hand smoke after the burning end has been extinguished. Because of its negative implications, exposure to SHS has played a central role in the regulation of tobacco products. Six hundred thousand deaths were attributed to SHS in 2004. It also has been known to produce skin conditions such as freckles and dryness.
Smokers are at greater risk of developing psychotic disorder. Tobacco has also been described an anaphrodisiac due to its propensity for causing erectile dysfunction. There is a correlation between tobacco smoking and a reduced risk of Parkinson's disease.
Economic
See also: Tobacco industryIn countries where there is a universally funded healthcare system, the government covers the cost of medical care for smokers who become ill through smoking in the form of increased taxes. Two broad debating positions exist on this front, the "pro-smoking" argument suggesting that heavy smokers generally do not live long enough to develop the costly and chronic illnesses which affect the elderly, reducing society's healthcare burden, and the "anti-smoking" argument suggests that the healthcare burden is increased because smokers get chronic illnesses younger and at a higher rate than the general population. Data on both positions has been contested. The Centers for Disease Control and Prevention published research in 2002 claiming that the cost of each pack of cigarettes sold in the United States was more than $7 in medical care and lost productivity. The cost may be higher, with another study putting it as high as $41 per pack, most of which however is on the individual and his/her family. This is how one author of that study puts it when he explains the very low cost for others: "The reason the number is low is that for private pensions, Social Security, and Medicare — the biggest factors in calculating costs to society — smoking actually saves money. Smokers die at a younger age and don't draw on the funds they've paid into those systems." Other research demonstrates that premature death caused by smoking may redistribute Social Security income in unexpected ways that affect behavior and reduce the economic well-being of smokers and their dependents. To further support this, whatever the rate of smoking consumption is per day, smokers have a greater lifetime medical cost on average compared to a non-smoker by an estimated $6000. Between the cost for lost productivity and health care expenditures combined, cigarette smoking costs at least 193 billion dollars (Research also shows that smokers earn less money than nonsmokers). As for secondhand smoke, the cost is over 10 billion dollars.
By contrast, some non-scientific studies, including one conducted by Philip Morris in the Czech Republic called Public Finance Balance of Smoking in the Czech Republic and another by the Cato Institute, support the opposite position. Philip Morris has explicitly apologised for the former study, saying: "The funding and public release of this study which, among other things, detailed purported cost savings to the Czech Republic due to premature deaths of smokers, exhibited terrible judgment as well as a complete and unacceptable disregard of basic human values. For one of our tobacco companies to commission this study was not just a terrible mistake, it was wrong. All of us at Philip Morris, no matter where we work, are extremely sorry for this. No one benefits from the very real, serious and significant diseases caused by smoking."
Between 1970 and 1995, per-capita cigarette consumption in poorer developing countries increased by 67 percent, while it dropped by 10 percent in the richer developed world. Eighty percent of smokers now live in less developed countries. By 2030, the World Health Organization (WHO) forecasts that 10 million people a year will die of smoking-related illness, making it the single biggest cause of death worldwide, with the largest increase to be among women. WHO forecasts the 21st century's death rate from smoking to be ten times the 20th century's rate ("Washingtonian" magazine, December 2007).
The tobacco industry is known to be one of the largest global enterprises in the world. The six biggest tobacco companies made a combined profit of $35.1 billion (Jha et al., 2014) in 2010.
Social
See also: Tobacco advertising and Religious views on smoking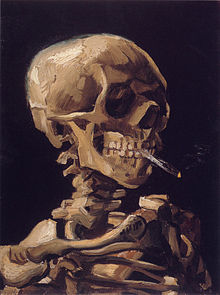
Famous smokers of the past used cigarettes or pipes as part of their image, such as Jean-Paul Sartre's Gauloises-brand cigarettes; Albert Einstein's, Douglas MacArthur's, Bertrand Russell's, and Bing Crosby's pipes; or the news broadcaster Edward R. Murrow's cigarette. Writers in particular seem to be known for smoking, for example, Cornell Professor Richard Klein's book Cigarettes are Sublime for the analysis, by this professor of French literature, of the role smoking plays in 19th and 20th century letters. The popular author Kurt Vonnegut addressed his addiction to cigarettes within his novels. British Prime Minister Harold Wilson was well known for smoking a pipe in public as was Winston Churchill for his cigars. Sherlock Holmes, the fictional detective created by Sir Arthur Conan Doyle, smoked a pipe, cigarettes, and cigars. The DC Vertigo comic book character John Constantine, created by Alan Moore, is synonymous with smoking, so much so that the first storyline by Preacher creator Garth Ennis centered around John Constantine contracting lung cancer. Professional wrestler James Fullington, while in character as "The Sandman", is a chronic smoker in order to appear "tough".
The problem of smoking at home is particularly difficult for women in many cultures (especially Arab cultures), where it may not be acceptable for a woman to ask her husband not to smoke at home or in the presence of her children. Studies have shown that pollution levels for smoking areas indoors are higher than levels found on busy roadways, in closed motor garages, and during fire storms. Furthermore, smoke can spread from one room to another, even if doors to the smoking area are closed.
The ceremonial smoking of tobacco, and praying with a sacred pipe, is a prominent part of the religious ceremonies of a number of Native American Nations. Sema, the Anishinaabe word for tobacco, is grown for ceremonial use and considered the ultimate sacred plant since its smoke is believed to carry prayers to the spirits. In most major religions, however, tobacco smoking is not specifically prohibited, although it may be discouraged as an immoral habit. Before the health risks of smoking were identified through controlled study, smoking was considered an immoral habit by certain Christian preachers and social reformers. The founder of the Latter Day Saint movement, Joseph Smith, recorded that on 27 February 1833, he received a revelation which discouraged tobacco use. This "Word of Wisdom" was later accepted as a commandment, and faithful Latter-day Saints abstain completely from tobacco. Jehovah's Witnesses base their stand against smoking on the Bible's command to "clean ourselves of every defilement of flesh" (2 Corinthians 7:1). The Jewish Rabbi Yisrael Meir Kagan (1838–1933) was one of the first Jewish authorities to speak out on smoking. In Ahmadiyya Islam, smoking is highly discouraged, although not forbidden. During the month of fasting however, it is forbidden to smoke tobacco. In the Baháʼí Faith, smoking tobacco is discouraged though not forbidden.
Public policy
See also: Tobacco politicsOn 27 February 2005 the WHO Framework Convention on Tobacco Control, took effect. The FCTC is the world's first public health treaty. Countries that sign on as parties agree to a set of common goals, minimum standards for tobacco control policy, and to cooperate in dealing with cross-border challenges such as cigarette smuggling. Currently the WHO declares that 4 billion people will be covered by the treaty, which includes 168 signatories. Among other steps, signatories are to put together legislation that will eliminate secondhand smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places.
Taxation
See also: Cigarette taxes in the United StatesMany governments have introduced excise taxes on cigarettes in order to reduce the consumption of cigarettes, alongside generating tax revenue. The World Health Organization finds that:
The structure of tobacco excise taxes varies considerably across countries, with lower income countries more likely to rely more on ad valorem excises and higher income countries more likely to rely more on specific excise taxes, while many countries at all income levels use a mix of specific and ad valorem excises.
Tobacco excise tax systems are quite complex in several countries, where different tax rates are applied based on prices, product characteristics such as presence/absence of a filter or length, packaging, weight, tobacco content, and/or production or sales volume. These complex systems are difficult to administer, create opportunities for tax avoidance, and are less effective from a public health perspective.
Globally, cigarette excise taxes account for less than 45 percent of cigarette prices, on average, while all taxes applied to cigarettes account for just over half of half of price. Higher income countries levy higher taxes on tobacco products and these taxes account for a greater share of price, with both the absolute tax and share of price accounted for by tax falling as country incomes fall.
In 2002, the Centers for Disease Control and Prevention said that each pack of cigarettes sold in the United States costs the nation more than $7 in medical care and lost productivity, around $3400 per year per smoker. Another study by a team of health economists finds the combined price paid by their families and society is about $41 per pack of cigarettes.
Substantial scientific evidence shows that higher cigarette prices result in lower overall cigarette consumption. Most studies indicate that a 10% increase in price will reduce overall cigarette consumption by 3% to 5%. Youth, minorities, and low-income smokers are two to three times more likely to quit or smoke less than other smokers in response to price increases. While smoking is sometimes given as an example of an inelastic good, it is elastic in poorer and middle wealth nations, and even in wealthier nations price increases do effect consumption, if not at the same rate as more elastic goods. That is to say, a large rise in price will only result in a small decrease in consumption.
Many nations have implemented some form of tobacco taxation. As of 1997, Denmark had the highest cigarette tax burden of $4.02 per pack. Taiwan only had a tax burden of $0.62 per pack. The federal government of the United States charges $1.01 per pack.
Cigarette taxes vary widely from state to state in the United States. For example, Missouri has a cigarette tax of only 17 cents per pack, the nation's lowest, while New York has the highest cigarette tax in the U.S.: $4.35 per pack. In Alabama, Illinois, Missouri, New York City, Tennessee, and Virginia, counties and cities may impose an additional limited tax on the price of cigarettes. Sales taxes are also levied on tobacco products in most jurisdictions.
In the United Kingdom, as of April 2023, a packet of 20 cigarettes has a tax added of 16.5% of the retail price plus £5.89. The UK has a significant black market for tobacco, and it has been estimated by the tobacco industry that 27% of cigarette and 68% of handrolling tobacco consumption is non-UK duty paid (NUKDP).
In Australia total taxes account for 62.5% of the final price of a packet of cigarettes (2011 figures). These taxes include federal excise or customs duty and Goods and Services Tax.
Restrictions
Main articles: Tobacco advertising, Tobacco packaging warning messages, Plain tobacco packaging, and Smoking ban
In June 1967, the US Federal Communications Commission ruled that programmes broadcast on a television station which discussed smoking and health were insufficient to offset the effects of paid advertisements that were broadcast for five to ten minutes each day. In April 1970, the US Congress passed the Public Health Cigarette Smoking Act banning the advertising of cigarettes on television and radio starting on 2 January 1971.
The Tobacco Advertising Prohibition Act 1992 expressly prohibited almost all forms of Tobacco advertising in Australia, including the sponsorship of sporting or other cultural events by cigarette brands.
All tobacco advertising and sponsorship on television has been banned within the European Union since 1991 under the Television Without Frontiers Directive (1989). This ban was extended by the Tobacco Advertising Directive, which took effect in July 2005 to cover other forms of media such as the internet, print media, and radio. The directive does not include advertising in cinemas and on billboards or using merchandising – or tobacco sponsorship of cultural and sporting events which are purely local, with participants coming from only one Member State as these fall outside the jurisdiction of the European Commission. However, most member states have transposed the directive with national laws that are wider in scope than the directive and cover local advertising. A 2008 European Commission report concluded that the directive had been successfully transposed into national law in all EU member states, and that these laws were well implemented.

Some countries also impose legal requirements on the packaging of tobacco products. For example, in the countries of the European Union, Turkey, Australia and South Africa, cigarette packs must be prominently labeled with the health risks associated with smoking. Canada, Australia, Thailand, Iceland and Brazil have also imposed labels upon cigarette packs warning smokers of the effects, and they include graphic images of the potential health effects of smoking. Cards are also inserted into cigarette packs in Canada. There are sixteen of them, and only one comes in a pack. They explain different methods of quitting smoking. Also, in the United Kingdom, there have been a number of graphic NHS advertisements, one showing a cigarette filled with fatty deposits, as if the cigarette is symbolizing the artery of a smoker.
Some countries have also banned advertisement at point of sale. United Kingdom and Ireland have limited the advertisement of tobacco at retailers. This includes storing of cigarettes behind a covered shelf not visible to the public. They do however allow some limited advertising at retailers. Norway has a complete ban of point of sale advertising. This includes smoking products and accessories. Implementing these policies can be challenging, all of these countries experienced resistance and challenges from the tobacco industry. The World Health Organization recommends the complete ban of all types of advertisement or product placement, including at vending machines, at airports and on internet shops selling tobacco. The evidence is as yet unclear as to the effect of such bans.
Many countries have a smoking age. In many countries, including the United States, most European Union member states, New Zealand, Canada, South Africa, Israel, India, Brazil, Chile, Costa Rica and Australia, it is illegal to sell tobacco products to minors and in the Netherlands, Austria, Belgium, Denmark and South Africa it is illegal to sell tobacco products to people under the age of 18. On 1 September 2007 the minimum age to buy tobacco products in Germany rose from 16 to 18, as well as in the United Kingdom where on 1 October 2007 it rose from 16 to 18. Underlying such laws is the belief that people should make an informed decision regarding the risks of tobacco use. These laws have a lax enforcement in some nations and states. In China, Turkey, and many other countries usually a child will have little problem buying tobacco products, because they are often told to go to the store to buy tobacco for their parents.
Several countries such as Ireland, Latvia, Estonia, the Netherlands, Finland, Norway, Canada, Australia, Sweden, Portugal, Singapore, Italy, Indonesia, India, Lithuania, Chile, Spain, Iceland, United Kingdom, Slovenia, Türkiye and Malta have legislated against smoking in public places, often including bars and restaurants. Restaurateurs have been permitted in some jurisdictions to build designated smoking areas (or to prohibit smoking). In the United States, many states prohibit smoking in restaurants, and some also prohibit smoking in bars. In provinces of Canada, smoking is illegal in indoor workplaces and public places, including bars and restaurants. As of 31 March 2008 Canada has introduced a smoke-free law in all public places, as well as within 10 metres of an entrance to any public place. In Australia, smoke-free laws vary from state to state. In New Zealand and Brazil, smoking is restricted in enclosed public places including bars, restaurants and pubs. Hong Kong restricted smoking on 1 January 2007 in the workplace, public spaces such as restaurants, karaoke rooms, buildings, and public parks (bars which do not admit minors were exempt until 2009). In Romania smoking is illegal in trains, metro stations, public institutions (except where designated, usually outside) and public transport. In Germany, in addition to smoking bans in public buildings and transport, an anti-smoking ordinance for bars and restaurants was implemented in late 2007. A study by the University of Hamburg (Ahlfeldt and Maennig 2010) demonstrates that the smoking ban had, if any, only short run effects on bar and restaurant revenues. In the medium and long run no negative effect was measurable. The results suggest either that the consumption in bars and restaurants is not affected by smoking bans in the long run or that negative revenue effects by smokers are compensated by increasing revenues through non-smokers.
Ignition safety
An indirect public health problem posed by cigarettes is that of accidental fires, usually linked with consumption of alcohol. Enhanced combustion using nitrates was traditionally used but cigarette manufacturers have been silent on this subject claiming at first that a safe cigarette was technically impossible, then that it could only be achieved by modifying the paper. Roll your own cigarettes contain no additives and are fire safe. Numerous fire safe cigarette designs have been proposed, some by tobacco companies themselves, which would extinguish a cigarette left unattended for more than a minute or two, thereby reducing the risk of fire. Among American tobacco companies, some have resisted this idea, while others have embraced it. RJ Reynolds was a leader in making prototypes of these cigarettes in 1983 and will make all of their U.S. market cigarettes to be fire-safe by 2010. Phillip Morris is not in active support of it. Lorillard (purchased by RJ Reynolds), the US' 3rd-largest tobacco company, seems to be ambivalent.
Health warnings
Individual cigarettes in Canada now carry warnings such as "poison in every puff" and "cigarettes cause impotence" in what the government says is an effort to make it "virtually impossible to avoid health warnings altogether".
Gateway drug theory
Main articles: Tobacco and other drugs and Gateway drug theoryThe relationship between tobacco and other drug use has been well-established, however the nature of this association remains unclear. The two main theories are the phenotypic causation (gateway) model and the correlated liabilities model. The causation model argues that smoking is a primary influence on future drug use, while the correlated liabilities model argues that smoking and other drug use are predicated on genetic or environmental factors. One study published by the NIH found that tobacco use may be linked to cocaine addiction and marijuana use. The study stated that 90% of adults who used cocaine had smoked cigarettes before (this was for people ages 18–34). This study could support the gateway drug theory.
Cessation
Main article: Smoking cessationQuitting smoking often involves advice from physicians or social workers, cold turkey, nicotine replacement therapy, contingent vouchers, antidepressants, vaping, hypnosis, self-help (mindfulness meditation), and support groups.
In the United States, about 70% of smokers would like to quit smoking, and 50% report having made an attempt to do so in the past year. Without support, 1% of smokers will successfully quit smoking each year. Physician advice to quit smoking increases the rate to 3% per year. Adding first‐line smoking cessation medications (and some behavioral help), increased quit rates to around 20% of smokers in a year. For cessation of smoking, public participation in health campaigns are important. In Nepal, cardiologist Om Murti Anil has launched smokers are not selfish campaign on the occasion of valentines day. He is using social media to motivate people to sacrifice their smoking habits as gift to their loved ones .
See also
- Cannabis smoking
- Cigarette smoking among college students
- Cigarette smoking for weight loss
- Electronic cigarette
- Herbal cigarette
- List of cigarette smoke carcinogens
- Snuff (tobacco)
- Smoker's paradox
- Tobacco advertising
- Tobacco control
References
- ^ Gately, Iain (2004) . Tobacco: A Cultural History of How an Exotic Plant Seduced Civilization. Diane. pp. 3–7. ISBN 978-0-8021-3960-3. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- ^ Lloyd, John; Mitchinson, John (25 July 2008). The Book of General Ignorance. Harmony Books. ISBN 978-0-307-39491-0.
- West, Robert; Shiffman, Saul (2007). Fast Facts: Smoking Cessation. Health Press Ltd. p. 28. ISBN 978-1-903734-98-8.
- ^ Wigand, Jeffrey S. (July 2006). "ADDITIVES, CIGARETTE DESIGN and TOBACCO PRODUCT REGULATION" (PDF). Mt. Pleasant, MI 48804: Jeffrey Wigand. Archived (PDF) from the original on 16 May 2011. Retrieved 14 February 2009.
{{cite web}}: CS1 maint: location (link) - ^ Gilman & Xun 2004, p. 318
- ^ Parrott, A. C.; Winder, G. (1989). "Nicotine chewing gum (2 mg, 4 mg) and cigarette smoking: comparative effects upon vigilance and heart rate". Psychopharmacology. 97 (2): 257–261. doi:10.1007/BF00442260. PMID 2498936. S2CID 4842374.
- ^ Parkin, C.; Fairweather, D. B.; Shamsi, Z.; Stanley, N.; Hindmarch, I. (1998). "The effects of cigarette smoking on overnight performance". Psychopharmacology. 136 (2): 172–178. doi:10.1007/s002130050553. PMID 9551774. S2CID 22962937.
- Gilman & Xun 2004, pp. 320–321
- Benowitz, Neal L. (1 February 2009). "Pharmacology of Nicotine: Addiction, Smoking-Induced Disease, and Therapeutics". Annual Review of Pharmacology and Toxicology. 49 (1): 57–71. doi:10.1146/annurev.pharmtox.48.113006.094742. ISSN 0362-1642. PMC 2946180. PMID 18834313.
- ^ Proctor 2000, p. 228
- ^ Doll, R.; Hill, B. (June 2004). "The mortality of doctors in relation to their smoking habits: a preliminary report: (Reprinted from Br Med J 1954:ii;1451-5)". BMJ (Clinical Research Ed.). 328 (7455): 1529–1533, discussion 1533. doi:10.1136/bmj.328.7455.1529. ISSN 0959-8138. PMC 437141. PMID 15217868.
- ^ VJ Rock, MPH, A Malarcher, JW Kahende, K Asman, MSPH, C Husten, MD, R Caraballo (9 November 2007). "Cigarette Smoking Among Adults --- United States, 2006". United States Centers for Disease Control and Prevention. Archived from the original on 16 August 2019. Retrieved 1 January 2009.
In 2006, an estimated 20.8% (45.3 million) of U.S. adults
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "WHO/WPRO-Smoking Statistics". World Health Organization Regional Office for the Western Pacific. 28 May 2002. Archived from the original on 8 November 2009. Retrieved 1 January 2009.
- Giovino, GA; Mirza, SA; Samet, JM; Gupta, PC; Jarvis, MJ; Bhala, N; Peto, R; Zatonski, W; Hsia, J; Morton, J; Palipudi, KM; Asma, S; GATS Collaborative, Group (18 August 2012). "Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys". Lancet. 380 (9842): 668–79. doi:10.1016/S0140-6736(12)61085-X. ISSN 0140-6736. PMID 22901888. S2CID 12450625.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The World Health Organization, and the Institute for Global Tobacco Control, Johns Hopkins School of Public Health (2001). "Women and the Tobacco Epidemic: Challenges for the 21st Century" (PDF). World Health Organization. pp. 5–6. Archived from the original (PDF) on 28 November 2003. Retrieved 2 January 2009.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "Surgeon General's Report—Women and Smoking". Centers for Disease Control and Prevention. 2001. p. 47. Archived from the original on 10 July 2009. Retrieved 3 January 2009.
- ^ "Tobacco". www.who.int. Retrieved 24 February 2024.
- ^ Chandrupatla, Siddardha G.; Tavares, Mary; Natto, Zuhair S. (27 July 2017). "Tobacco Use and Effects of Professional Advice on Smoking Cessation among Youth in India". Asian Pacific Journal of Cancer Prevention. 18 (7): 1861–1867. doi:10.22034/APJCP.2017.18.7.1861. ISSN 2476-762X. PMC 5648391. PMID 28749122.
- The Lancet (26 September 2009). "Tobacco smoking:why start?". The Lancet. 374 (9695): 1038. doi:10.1016/s0140-6736(09)61680-9. PMID 19782852. S2CID 37513171.
- Wilbert, Johannes (28 July 1993). Tobacco and Shamanism in South America. Yale University Press. ISBN 978-0-300-05790-4. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- Robicsek, Francis (January 1979). The Smoking Gods: Tobacco in Maya Art, History, and Religion. University of Oklahoma Press. p. 30. ISBN 978-0-8061-1511-5.
- F.J.Carod-Artal (1 July 2011). "Hallucinogenic drugs in pre-Columbian Mesoamerican cultures". Neurología. 30 (1): 42–49. doi:10.1016/j.nrleng.2011.07.010. PMID 21893367.
- Nordenskiold, Erland (1929), "The American Indian as an Inventor", Journal of the Royal Anthropological Institute, 59: 277, doi:10.2307/2843888, JSTOR 2843888
- Heckewelder, John Gottlieb Ernestus; Reichel, William Cornelius (June 1971) . History, manners, and customs of the Indian nations who once inhabited Pennsylvania and the neighboring states (PDF). The Historical society of Pennsylvania. p. 149. ISBN 978-0-405-02853-3. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- Diéreville; Webster, John Clarence; Webster, Alice de Kessler Lusk (1933). "Relation of the voyage to Port Royal in Acadia or New France". The Champlain Society.
They smoke with excessive eagerness men, women, girls and boys, all find their keenest pleasure in this way
{{cite journal}}: Cite journal requires|journal=(help) - Gottsegen, Jack Jacob (1940). "Tobacco: A Study of Its Consumption in the United States". Pitman Publishing Company: 107. Archived from the original on 14 January 2023. Retrieved 22 March 2009>
{{cite journal}}: Cite journal requires|journal=(help) - Balls, Edward K. (1 October 1962). Early Uses of California Plants. University of California Press. pp. 81–85. ISBN 978-0-520-00072-8. Retrieved 22 March 2009.
Early Uses of California Plants.
- Jordan, Ervin L. Jr. "Jamestown, Virginia, 1607–1907: An Overview". University of Virginia. Archived from the original on 17 October 2002. Retrieved 22 February 2009.
{{cite journal}}: Cite journal requires|journal=(help) - Kulikoff, Allan (1 August 1986). Tobacco and Slaves: The Development of Southern Cultures in the Chesapeake. The University of North Carolina Press. ISBN 978-0-8078-4224-9. Retrieved 22 March 2009.
Tobacco & Slaves: The Development of Southern Cultures in the Chesapeake.
- Gilman & Xun 2004, p. 38
- Gilman & Xun 2004, pp. 92–99
- Gilman & Xun 2004, pp. 15–16
- King James I of England (16 April 2002) . "A Counterblaste to Tobacco". University of Texas at Austin. Archived from the original on 18 May 2009. Retrieved 22 March 2009.
{{cite journal}}: Cite journal requires|journal=(help) - Burns, Eric (28 September 2006). The Smoke of the Gods: A Social History of Tobacco. Temple University Press. pp. 134–135. ISBN 978-1-59213-480-9. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- Proctor 2000, p. 178
- Proctor 2000, p. 219
- Proctor 2000, p. 187
- ^ Proctor 2000, p. 245
- Proctor, Robert N. (1996). "Nazi Medicine and Public Health Policy". Dimensions. 10 (2). Anti-Defamation League. Archived from the original on 5 December 2012. Retrieved 1 October 2018 – via archived copy at archive.is.
- Doll, R.; Hill, A. B. (1 September 1950). "Smoking and Carcinoma of the Lung". British Medical Journal. 2 (4682): 739–748. doi:10.1136/bmj.2.4682.739. ISSN 0007-1447. PMC 2038856. PMID 14772469.
- "CNN Interactive". Cnn.com. Archived from the original on 23 April 2009. Retrieved 22 June 2009.
- "The Reports of the Surgeon General: The 1964 Report on Smoking and Health". Profiles in Science. United States National Library of Medicine, National Institutes of Health. Archived from the original on 20 January 2016. Retrieved 10 October 2015.
- Milo Geyelin (23 November 1998). "Forty-Six States Agree to Accept $206 Billion Tobacco Settlement". Wall Street Journal.
- Hilton, Matthew (4 May 2000). Smoking in British Popular Culture, 1800–2000: Perfect Pleasures. Manchester University Press. pp. 229–241. ISBN 978-0-7190-5257-6. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- Gilman & Xun 2004, pp. 46–57
- ^ MPOWER 2008, pp. 267–288
- "Bidi Use Among Urban Youth – Massachusetts, March–April 1999". Centers for Disease Control and Prevention. 17 September 1999. Archived from the original on 11 February 2009. Retrieved 14 February 2009.
- Pakhale, S. M.; Maru, G. B. (December 1998). "Distribution of major and minor alkaloids in tobacco, mainstream and sidestream smoke of popular Indian smoking products". Food and Chemical Toxicology. 36 (12): 1131–1138. doi:10.1016/S0278-6915(98)00071-4. ISSN 0278-6915. PMID 9862656.
- Rarick CA (2 April 2008). "Note on the premium cigar industry". doi:10.2139/ssrn.1127582. S2CID 152340055. SSRN 1127582.
{{cite journal}}: Cite journal requires|journal=(help) - Mariolis P, Rock VJ, Asman K, et al. (2006). "Tobacco use among adults—United States, 2005". MMWR Morb Mortal Wkly Rep. 55 (42): 1145–8. PMID 17065979. Archived from the original on 26 September 2017. Retrieved 17 September 2017.
- "A bill to protect the public health by providing the Food and Drug Administration with certain authority to regulate tobacco products. (Summary)" (Press release). Library of Congress. 20 May 2004. Archived from the original on 4 September 2015. Retrieved 1 August 2007.
- Turner, JA; Sillett, RW; McNicol, MW (1977). "Effect of cigar smoking on carboxyhemoglobin and plasma nicotine concentrations in primary pipe and cigar smokers and ex-cigarette smokers". British Medical Journal. 2 (6099): 1387–9. doi:10.1136/bmj.2.6099.1387. PMC 1632361. PMID 589225.
- Armitage, A. K.; Turner, D. M. (1970). "Absorption of Nicotine in Cigarette and Cigar Smoke through the Oral Mucosa". Nature. 226 (5252): 1231–1232. Bibcode:1970Natur.226.1231A. doi:10.1038/2261231a0. PMID 5422597. S2CID 4208650.
- Pich, E. M.; Pagliusi, S. R.; Tessari, M.; Talabot-Ayer, D.; Hooft Van Huijsduijnen, R.; Chiamulera, C. (1997). "Common neural substrates for the addictive properties of nicotine and cocaine". Science. 275 (5296): 83–86. doi:10.1126/science.275.5296.83. PMID 8974398. S2CID 5923174.
- Wonnacott, S. (1997). "Presynaptic nicotinic ACh receptors". Trends in Neurosciences. 20 (2): 92–8. doi:10.1016/S0166-2236(96)10073-4. PMID 9023878. S2CID 42215860.
- Pontieri, F. E.; Tanda, G.; Orzi, F.; Di Chiara, G. D. (1996). "Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs". Nature. 382 (6588): 255–257. Bibcode:1996Natur.382..255P. doi:10.1038/382255a0. PMID 8717040. S2CID 4338516.
- Guinan, M. E.; Portas, M. R.; Hill, H. R. (1979). "The candida precipitin test in an immunosuppressed population". Cancer. 43 (1): 299–302. doi:10.1002/1097-0142(197901)43:1<299::AID-CNCR2820430143>3.0.CO;2-D. PMID 761168. S2CID 45096870.
- Talhout, R.; Opperhuizen, A.; Van Amsterdam, J. G. C. (October 2007). "Role of acetaldehyde in tobacco smoke addiction". European Neuropsychopharmacology. 17 (10): 627–636. doi:10.1016/j.euroneuro.2007.02.013. ISSN 0924-977X. PMID 17382522. S2CID 25866206.
- Shoaib, M.; Lowe, A.; Williams, S. (2004). "Imaging localised dynamic changes in the nucleus accumbens following nicotine withdrawal in rats". NeuroImage. 22 (2): 847–854. doi:10.1016/j.neuroimage.2004.01.026. PMID 15193614. S2CID 43544025.
- ^ Guindon, G. Emmanuel; Boisclair, David (2003). "Past, current and future trends in tobacco use" (PDF). Washington DC: The International Bank for Reconstruction and Development / The World Bank: 13–16. Archived from the original (PDF) on 18 March 2009. Retrieved 22 March 2009.
{{cite journal}}: Cite journal requires|journal=(help) - Peto, Richard; Lopez, Alan D; Boreham, Jillian; Thun, Michael (2006). "Mortality from Smoking in Developed Countries 1950–2000: indirect estimates from national vital statistics" (PDF). Oxford University Press: 9. Archived from the original (PDF) on 24 February 2005. Retrieved 22 March 2009.
{{cite journal}}: Cite journal requires|journal=(help) - Tobaccofreekids.org/problem/tol-s
- Centers for Disease Control and Prevention (CDC) (2009). "Cigarette smoking among adults and trends in smoking cessation – United States, 2008" (Full free text). MMWR. Morbidity and Mortality Weekly Report. 58 (44): 1227–1232. PMID 19910909. Archived from the original on 16 September 2017. Retrieved 17 September 2017.
- GBD 2008, p. 8
- GBD 2008, p. 23
- ^ "WHO/WPRO-Tobacco Fact sheet". World Health Organization Regional Office for the Western Pacific. 29 May 2007. Archived from the original on 7 February 2009. Retrieved 1 January 2009.
- "Smoking causes one in 10 deaths worldwide, study shows". BBC News. 6 April 2017. Archived from the original on 10 April 2017. Retrieved 11 April 2017.
- Gay, Peter (1988). Freud: A Life for Our Time. New York: W. W. Norton & Company. pp. 650–651. ISBN 978-0-393-32861-5.
- Patton G. C.; Hibbert M.; Rosier M. J.; Carlin J. B.; Caust J.; Bowes G. (1996). "Is smoking associated with depression and anxiety in teenagers?". American Journal of Public Health. 86 (2): 225–230. doi:10.2105/ajph.86.2.225. PMC 1380332. PMID 8633740.
- Stanton, W.; Silva, P. A. (1992). "A longitudinal study of the influence of parents and friends on children's initiation of smoking". Journal of Applied Developmental Psychology. 13 (4): 423–434. doi:10.1016/0193-3973(92)90010-F.
- Harris, Judith Rich; Pinker, Steven (4 September 1998). The nurture assumption: why children turn out the way they do. Simon and Schuster. ISBN 978-0-684-84409-1. Archived from the original on 14 January 2023. Retrieved 22 March 2009.
- Chassin, L.; Presson, C.; Rose, J.; Sherman, S. J.; Prost, J. (2002). "Parental Smoking Cessation and Adolescent Smoking". Journal of Pediatric Psychology. 27 (6): 485–496. doi:10.1093/jpepsy/27.6.485. PMID 12177249.
- Proescholdbell, R. J.; Chassin, L.; MacKinnon, D. P. (2000). "Home smoking restrictions and adolescent smoking". Nicotine & Tobacco Research. 2 (2): 159–167. doi:10.1080/713688125. PMID 11072454. S2CID 8749779.
- Urberg, K.; Shyu, S. J.; Liang, J. (1990). "Peer influence in adolescent cigarette smoking". Addictive Behaviors. 15 (3): 247–255. doi:10.1016/0306-4603(90)90067-8. PMID 2378284.
- Bharatula, Arun (2016). Review: Tobacco outlet density. Melbourne.
{{cite book}}: CS1 maint: location missing publisher (link) - Michell L, West P (1996). "Peer pressure to smoke: the meaning depends on the method". Health Education Research. 11 (1): 39–49. doi:10.1093/her/11.1.39.
- Barber, J.; Bolitho, F.; Bertrand, L. (1999). "The Predictors of Adolescent Smoking". Journal of Social Service Research. 26 (1): 51–66. doi:10.1300/J079v26n01_03.
- Pelosi, Anthony J. (2019). "Personality and fatal diseases: Revisiting a scientific scandal". Journal of Health Psychology. 24 (4): 421–439. doi:10.1177/1359105318822045. ISSN 1359-1053. PMC 6712909. PMID 30791726.
- "King's College London enquiry into publications authored by Professor Hans Eysenck with Professor Ronald Grossarth-Maticek" (PDF). October 2019. Archived (PDF) from the original on 5 November 2022. Retrieved 13 January 2020.
- Nigel Hawkes (2019), Works by eminent psychologist who doubted smoking caused cancer are "unsafe," finds inquiry Archived 4 January 2023 at the Wayback Machine
- Eysenck, Hans J.; Brody, Stuart (November 2000). Smoking, health and personality. Transaction. ISBN 978-0-7658-0639-0.
- Berlin, I.; Singleton, E. G.; Pedarriosse, A. M.; Lancrenon, S.; Rames, A.; Aubin, H. J.; Niaura, R. (2003). "The Modified Reasons for Smoking Scale: factorial structure, gender effects and relationship with nicotine dependence and smoking cessation in French smokers". Addiction. 98 (11): 1575–1583. doi:10.1046/j.1360-0443.2003.00523.x. PMID 14616184.
- "Nicotine". Imperial College London. Archived from the original on 14 July 2009. Retrieved 22 March 2009.
{{cite journal}}: Cite journal requires|journal=(help) - Chandra, S.; Chaloupka, F. J. (2003). "Seasonality in cigarette sales: patterns and implications for tobacco control". Tobacco Control. 12 (1): 105–107. doi:10.1136/tc.12.1.105. PMC 1759100. PMID 12612375.
- Chandra, S.; Shiffman, S.; Scharf, M.; Dang, Q.; Shadel, G. (February 2007). "Daily smoking patterns, their determinants, and implications for quitting". Experimental and Clinical Psychopharmacology. 15 (1): 67–80. doi:10.1037/1064-1297.15.1.67. ISSN 1064-1297. PMID 17295586.
- ^ Kalkhoran, S; Benowitz, NL; Rigotti, AN (August 2018). "Prevention and Treatment of Tobacco Use: JACC Health Promotion Series". Journal of the American College of Cardiology. 72 (9). Elsevier for the American College of Cardiology: 1030–45. doi:10.1016/j.jacc.2018.06.036. ISSN 1558-3597. PMC 6261256. PMID 30139432. S2CID 52077567. Archived from the original on 9 August 2020. Retrieved 1 August 2020.
- "ASH > Action on Smoking & Health". www.ash.org. 2 August 2012. Archived from the original on 19 November 2016. Retrieved 16 November 2016.
- Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Mitchell, Richard (18 May 2007). "Chapter 8: Environmental and Nutritional Diseases". Robbins Basic Pathology (8th ed.). Philadelphia: W.B. Saunders. p. 288, Figure 8–6. ISBN 978-1-4160-2973-1.
- ^ Rodu, B; Plurphanswat, N (January 2021). "Mortality among male cigar and cigarette smokers in the USA" (PDF). Harm Reduction Journal. 18 (7). BioMed Central: 7. doi:10.1186/s12954-020-00446-4. ISSN 1477-7517. LCCN 2004243422. PMC 7789747. PMID 33413424. S2CID 230800394. Archived (PDF) from the original on 26 August 2021. Retrieved 28 August 2021.
- Nonnemaker, J; Rostron, B; Hall, P; MacMonegle, A; Apelberg, B (September 2014). Morabia, A (ed.). "Mortality and Economic Costs From Regular Cigar Use in the United States, 2010". American Journal of Public Health. 104 (9). American Public Health Association: e86–e91. doi:10.2105/AJPH.2014.301991. eISSN 1541-0048. ISSN 0090-0036. PMC 4151956. PMID 25033140. S2CID 207276270.
- Shah, RS; Cole, JW (July 2010). "Smoking and stroke: the more you smoke the more you stroke". Expert Review of Cardiovascular Therapy. 8 (7). Informa: 917–932. doi:10.1586/erc.10.56. ISSN 1744-8344. PMC 2928253. PMID 20602553. S2CID 207215548.
- ^ Laniado-Laborín, Rafael (January 2009). "Smoking and Chronic Obstructive Pulmonary Disease (COPD). Parallel Epidemics of the 21st Century". International Journal of Environmental Research and Public Health. 6 (1: Smoking and Tobacco Control). MDPI: 209–224. doi:10.3390/ijerph6010209. ISSN 1660-4601. PMC 2672326. PMID 19440278. S2CID 19615031.
- Oh, CK; Murray, LA; Molfino, NL (February 2012). "Smoking and Idiopathic Pulmonary Fibrosis". Pulmonary Medicine. 2012. Hindawi Publishing Corporation: 808260. doi:10.1155/2012/808260. ISSN 2090-1844. PMC 3289849. PMID 22448328. S2CID 14090263.
- ^ Thun, Michael J.; Jacobs, Eric J.; Shapiro, Jean A. (February 2000). Ganz, Patricia A. (ed.). "Cigar Smoking in Men and Risk of Death From Tobacco-Related Cancers". Journal of the National Cancer Institute. 92 (4). Oxford University Press: 333–337. doi:10.1093/jnci/92.4.333. eISSN 1460-2105. ISSN 0027-8874. PMID 10675383. S2CID 7772405. Archived from the original on 21 April 2021. Retrieved 28 August 2021.
- ^ Anjum F, Zohaib J (4 December 2020). "Oropharyngeal Squamous Cell Carcinoma". Definitions (Updated ed.). Treasure Island (FL): StatPearls Publishing. doi:10.32388/G6TG1L. PMID 33085415. S2CID 229252540. Bookshelf ID: NBK563268. Archived from the original on 11 June 2021. Retrieved 7 February 2021 – via NCBI.
- Gormley, Mark; Creaney, Grant; Schache, Andrew; Ingarfield, Kate; Conway, David I. (11 November 2022). "Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors". British Dental Journal. 233 (9): 780–786. doi:10.1038/s41415-022-5166-x. ISSN 0007-0610. PMC 9652141. PMID 36369568.
- Hashibe, Mia; Brennan, Paul; Chuang, Shu-chun; Boccia, Stefania; Castellsague, Xavier; Chen, Chu; Curado, Maria Paula; Dal Maso, Luigino; Daudt, Alexander W.; Fabianova, Eleonora; Fernandez, Leticia; Wünsch-Filho, Victor; Franceschi, Silvia; Hayes, Richard B.; Herrero, Rolando (1 February 2009). "Interaction between Tobacco and Alcohol Use and the Risk of Head and Neck Cancer: Pooled Analysis in the International Head and Neck Cancer Epidemiology Consortium". Cancer Epidemiology, Biomarkers & Prevention. 18 (2): 541–550. doi:10.1158/1055-9965.EPI-08-0347. ISSN 1055-9965. PMC 3051410. PMID 19190158.
- Inflamm Bowel Dis. May 2009, P. Seksik, I Nion-Larmurier
- Rom O, Kaisari S, Aizenbud D, Reznick AZ (2013). "Cigarette smoke and muscle catabolism in C2 myotubes". Mech Ageing Dev. 134 (1–2): 24–34. doi:10.1016/j.mad.2012.11.004. PMID 23262287. S2CID 322153.
- ^ Etemadi, Arash; Blount, Benjamin C.; Calafat, Antonia M.; Chang, Cindy M.; De Jesus, Victor R.; Poustchi, Hossein; Wang, Lanqing; Pourshams, Akram; Shakeri, Ramin; Shiels, Meredith S.; Inoue-Choi, Maki; Ambrose, Bridget K.; Christensen, Carol H.; Wang, Baoguang; Ye, Xiaoyun; Murphy, Gwen; Feng, Jun; Xia, Baoyun; Sosnoff, Connie S.; Boffetta, Paolo; Brennan, Paul; Bhandari, Deepak; Kamangar, Farin; Dawsey, Sanford M.; Abnet, Christian C.; Freedman, Neal D.; Malekzadeh, Reza (February 2019). "Urinary Biomarkers of Carcinogenic Exposure among Cigarette, Waterpipe, and Smokeless Tobacco Users and Never Users of Tobacco in the Golestan Cohort Study". Cancer Epidemiology, Biomarkers & Prevention. 28 (2). American Association for Cancer Research: 337–347. doi:10.1158/1055-9965.EPI-18-0743. eISSN 1538-7755. ISSN 1055-9965. PMC 6935158. PMID 30622099. S2CID 58560832.
- Dreyer, L et al. (1997) Tobacco Smoking. APMIS Inc.
- Chang, Cindy M.; Corey, Catherine G.; Rostron, Brian L.; Apelberg, Benjamin J. (April 2015). "Systematic review of cigar smoking and all-cause and smoking-related mortality" (PDF). BMC Public Health. 15 (390). BioMed Central: 390. doi:10.1186/s12889-015-1617-5. ISSN 1471-2458. PMC 4408600. PMID 25907101. S2CID 16482278. Archived (PDF) from the original on 16 March 2021. Retrieved 5 September 2021.
- Albandar, Jasim M.; Adensaya, Margo R.; Streckfus, Charles F.; Winn, Deborah M. (December 2000). "Cigar, Pipe, and Cigarette Smoking as Risk Factors for Periodontal Disease and Tooth Loss". Journal of Periodontology. 71 (12). American Academy of Periodontology: 1874–1881. doi:10.1902/jop.2000.71.12.1874. ISSN 0022-3492. PMID 11156044. S2CID 11598500.
- Kastan MB (2008). "DNA damage responses: mechanisms and roles in human disease: 2007 G.H.A. Clowes Memorial Award Lecture". Mol. Cancer Res. 6 (4): 517–24. doi:10.1158/1541-7786.MCR-08-0020. PMID 18403632.
- Liu XY, Zhu MX, Xie JP (2010). "Mutagenicity of acrolein and acrolein-induced DNA adducts". Toxicol. Mech. Methods. 20 (1): 36–44. doi:10.3109/15376510903530845. PMID 20158384. S2CID 8812192.
- Speit G, Merk O (2002). "Evaluation of mutagenic effects of formaldehyde in vitro: detection of crosslinks and mutations in mouse lymphoma cells". Mutagenesis. 17 (3): 183–7. doi:10.1093/mutage/17.3.183. PMID 11971987.
- Pu X, Kamendulis LM, Klaunig JE (2009). "Acrylonitrile-induced oxidative stress and oxidative DNA damage in male Sprague-Dawley rats". Toxicol. Sci. 111 (1): 64–71. doi:10.1093/toxsci/kfp133. PMC 2726299. PMID 19546159.
- Koturbash I, Scherhag A, Sorrentino J, Sexton K, Bodnar W, Swenberg JA, Beland FA, Pardo-Manuel Devillena F, Rusyn I, Pogribny IP (2011). "Epigenetic mechanisms of mouse interstrain variability in genotoxicity of the environmental toxicant 1,3-butadiene". Toxicol. Sci. 122 (2): 448–56. doi:10.1093/toxsci/kfr133. PMC 3155089. PMID 21602187.
- Garcia CC, Angeli JP, Freitas FP, Gomes OF, de Oliveira TF, Loureiro AP, Di Mascio P, Medeiros MH (2011). "[13C2]-Acetaldehyde promotes unequivocal formation of 1,N2-propano-2'-deoxyguanosine in human cells". J. Am. Chem. Soc. 133 (24): 9140–3. doi:10.1021/ja2004686. PMID 21604744. Archived from the original on 6 November 2020. Retrieved 1 December 2019.
- Tompkins EM, McLuckie KI, Jones DJ, Farmer PB, Brown K (2009). "Mutagenicity of DNA adducts derived from ethylene oxide exposure in the pSP189 shuttle vector replicated in human Ad293 cells". Mutat. Res. 678 (2): 129–37. Bibcode:2009MRGTE.678..129T. doi:10.1016/j.mrgentox.2009.05.011. PMID 19477295.
- Fabiani R, Rosignoli P, De Bartolomeo A, Fuccelli R, Morozzi G (2007). "DNA-damaging ability of isoprene and isoprene mono-epoxide (EPOX I) in human cells evaluated with the comet assay". Mutat. Res. 629 (1): 7–13. Bibcode:2007MRGTE.629....7F. doi:10.1016/j.mrgentox.2006.12.007. PMID 17317274.
- Alarabi, A. B.; Karim, Z. A.; Alshbool, F. Z.; Khasawneh, F. T.; Hernandez, Keziah R.; Lozano, Patricia A.; Montes Ramirez, Jean E.; Rivera, José O. (February 2020). "Short-Term Exposure to Waterpipe/Hookah Smoke Triggers a Hyperactive Platelet Activation State and Increases the Risk of Thrombogenesis". Arteriosclerosis, Thrombosis, and Vascular Biology. 40 (2). Lippincott Williams & Wilkins: 335–349. doi:10.1161/ATVBAHA.119.313435. ISSN 1079-5642. PMC 7000176. PMID 31941383. S2CID 210335103.
- Patel, Mit P.; Khangoora, Vikramjit S.; Marik, Paul E. (October 2019). "A Review of the Pulmonary and Health Impacts of Hookah Use". Annals of the American Thoracic Society. 16 (10). American Thoracic Society: 1215–1219. doi:10.1513/AnnalsATS.201902-129CME. ISSN 2325-6621. PMID 31091965. S2CID 155103502.
- Qasim, Hanan; Alarabi, A. B.; Alzoubi, K. H.; Karim, Z. A.; Alshbool, F. Z.; Khasawneh, F. T. (September 2019). "The effects of hookah/waterpipe smoking on general health and the cardiovascular system" (PDF). Environmental Health and Preventive Medicine. 24 (58). BioMed Central: 58. Bibcode:2019EHPM...24...58Q. doi:10.1186/s12199-019-0811-y. ISSN 1347-4715. PMC 6745078. PMID 31521105. S2CID 202570973. Archived (PDF) from the original on 24 April 2021. Retrieved 8 September 2021.
- ^ Farag, Mohamed A.; Elmassry, Moamen M.; El-Ahmady, Sherweit H. (19 November 2018). "The characterization of flavored hookahs aroma profile and in response to heating as analyzed via headspace solid-phase microextraction (SPME) and chemometrics". Scientific Reports. 8 (1): 17028. Bibcode:2018NatSR...817028F. doi:10.1038/s41598-018-35368-6. ISSN 2045-2322. PMC 6242864. PMID 30451904.
- WHO Report on the Global Tobacco Epidemic, 2008
- "Nicotine: A Powerful Addiction Archived 1 May 2009 at the Wayback Machine." Centers for Disease Control and Prevention.
- ^ Barendregt J. J., Bonneux L., van der Maas P. J. (1997). "The health care costs of smoking" (PDF). New England Journal of Medicine. 337 (15): 1052–1057. doi:10.1056/NEJM199710093371506. hdl:1765/59780. PMID 9321534. Archived (PDF) from the original on 8 October 2022. Retrieved 20 April 2018.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Peto Richard; Darby Sarah; Deo Harz; et al. (2000). "Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies". The BMJ. 321 (7257): 323–329. doi:10.1136/bmj.321.7257.323. PMC 27446. PMID 10926586.
- Yoshida, Kenichi; Gowers, Kate H. C.; Lee-Six, Henry; Chandrasekharan, Deepak P.; Coorens, Tim; Maughan, Elizabeth F.; Beal, Kathryn; Menzies, Andrew; Millar, Fraser R.; Anderson, Elizabeth; Clarke, Sarah E.; Pennycuick, Adam; Thakrar, Ricky M.; Butler, Colin R.; Kakiuchi, Nobuyuki; Hirano, Tomonori; Hynds, Robert E.; Stratton, Michael R.; Martincorena, Iñigo; Janes, Sam M.; Campbell, Peter J. (2020). "Tobacco smoking and somatic mutations in human bronchial epithelium". Nature. 578 (7794): 266–272. Bibcode:2020Natur.578..266Y. doi:10.1038/s41586-020-1961-1. PMC 7021511. PMID 31996850. Archived from the original on 12 August 2021. Retrieved 30 January 2020.
- "Cigarette Smoking Among Adults --- United States, 2006". Archived from the original on 16 August 2019. Retrieved 29 February 2016.
- "WHO Western Pacific | World Health Organization". www.who.int. Archived from the original on 8 November 2009.
- Pintarelli G, Noci S, Maspero D, Pettinicchio A, Dugo M, De Cecco L, Incarbone M, Tosi D, Santambrogio L, Dragani TA, Colombo F (September 2019). "Cigarette smoke alters the transcriptome of non-involved lung tissue in lung adenocarcinoma patients". Scientific Reports. 9 (1): 13039. Bibcode:2019NatSR...913039P. doi:10.1038/s41598-019-49648-2. PMC 6736939. PMID 31506599.
- Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries Archived 29 November 2010 at the Wayback Machine 26 November 2010
- Gurillo, Pedro; Jauhar, Sameer; Murray, Robin M; MacCabe, James H (July 2015). "Does tobacco use cause psychosis? Systematic review and meta-analysis". The Lancet Psychiatry. 2 (8): 718–725. doi:10.1016/S2215-0366(15)00152-2. PMC 4698800. PMID 26249303.
- Nicolosi Alfredo; et al. (2003). "Epidemiology of erectile dysfunction in four countries: cross-national study of the prevalence and correlates of erectile dysfunction". Urology. 61 (1): 201–206. doi:10.1016/s0090-4295(02)02102-7. PMID 12559296. Archived from the original on 8 March 2021. Retrieved 16 July 2019.
- Ma C, Liu Y, Neumann S, Gao X (2017). "Nicotine from cigarette smoking and diet and Parkinson disease: a review". Translational Neurodegeneration. 6: 18. doi:10.1186/s40035-017-0090-8. PMC 5494127. PMID 28680589.
- Dorsey ER, Sherer T, Okun MS, Bloem BR (2018). "The Emerging Evidence of the Parkinson Pandemic". J Parkinsons Dis (Review). 8 (s1): S3–8. doi:10.3233/JPD-181474. PMC 6311367. PMID 30584159.
- ^ "Cigarettes Cost U.S. $7 Per Pack Sold, Study Says". The New York Times. 12 April 2002. Archived from the original on 13 February 2008. Retrieved 29 February 2016.
- ^ "USATODAY.com – Study: Cigarettes cost families, society $41 per pack". USA Today. Archived from the original on 24 May 2011. Retrieved 29 February 2016.
- Armour, Brian S.; Pitts, M. Melinda (2007). "Smoking: Taxing Health and Social Security" (PDF). www.frbatlanta.org. Federal Reserve Bank of Atlanta. Archived from the original (PDF) on 19 October 2012. Retrieved 20 May 2023.
- "Even One Is Too Much: The Economic Consequences of Being a Smoker, Federal Reserve Bank of Atlanta, January 2013" (PDF). Archived from the original (PDF) on 26 November 2013. Retrieved 11 July 2013.
- "Costs and Expenditures". Smoking and Tobacco. Centers for Disease Control and Prevention. Web. 20 January 2013. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/ Archived 25 September 2011 at the Wayback Machine
- ^ "Public Finance Balance of Smoking in the Czech Republic". Archived from the original on 19 July 2006.
- "Snuff the Facts". Archived from the original on 20 December 2006.
- "Global Effects of Smoking, of Quitting, and of Taxing Tobacco" (PDF). Archived (PDF) from the original on 27 November 2021. Retrieved 2 May 2018.
- Mostafa RM. Dilemma of women's passive smoking. Ann Thorac Med 2011 ;6:55-6. Available from: http://www.thoracicmedicine.org/text.asp?2011/6/2/55/78410 Archived 2 June 2018 at the Wayback Machine
- Church of Jesus Christ of Latter-day Saints (2009). "Obey the Word of Wisdom". Basic Beliefs – The Commandments. Archived from the original on 4 September 2015. Retrieved 15 October 2009.
- "Why is smoking not strictly forbidden in Islam?". Archived from the original on 3 May 2014. Retrieved 2 May 2014.
- Smith, Peter (2000). "smoking". A concise encyclopedia of the Bahá'í Faith. Oxford: Oneworld Publications. pp. 323. ISBN 978-1-85168-184-6.
- "WHO | Updated status of the WHO Framework Convention on Tobacco Control". 17 November 2004. Archived from the original on 17 November 2004. Retrieved 12 December 2021.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - "Archived copy" (PDF). www.who.int. Archived from the original (PDF) on 12 December 2019. Retrieved 15 January 2022.
{{cite web}}: CS1 maint: archived copy as title (link) - "26, 2004-smoking-costs_x.htm Study: Cigarettes cost families, society $41 per pack". USA Today.
- "Reducing Tobacco Use". Archived from the original on 21 February 2016. Retrieved 29 February 2016.
- Hyland, A.; Bauer, J. E.; Li, Q.; Abrams, S. M.; Higbee, C.; Peppone, L.; Cummings, K. M. (2005). "Higher cigarette prices influence cigarette purchase patterns". Tobacco Control. 14 (2): 86–92. doi:10.1136/tc.2004.008730. PMC 1748009. PMID 15791017.
- Nargis, Nigar; Stoklosa, Michal; Shang, Ce; Drope, Jeffrey (January 2021). "Price, Income, and Affordability as the Determinants of Tobacco Consumption: A Practitioner's Guide to Tobacco Taxation". Nicotine & Tobacco Research. 23 (1): 40–47. doi:10.1093/ntr/ntaa134. PMC 7789936. PMID 32697827. Retrieved 18 September 2024.
- "TTB – Tax Audit Division – Tax and Fee Rates". Archived from the original on 26 February 2016. Retrieved 29 February 2016.
- Helen C. Alvarez (28 March 2014). "You and Cigarettes". Archived from the original on 4 March 2016. Retrieved 29 February 2016.
- "Tax on shopping and services". GOV.UK. Archived from the original on 24 November 2022. Retrieved 1 April 2023.
- "Tobacco Smuggling & Crossborder Shopping " Tobacco Manufacturers' Association". Archived from the original on 8 September 2008. Retrieved 29 February 2016.
- Scollo, Michelle (2008). "13.2 Tobacco taxes in Australia" Archived 24 October 2022 at the Wayback Machine. Tobacco in Australia. Cancer Council Victoria. Retrieved 29 July 2010.
- "History of Tobacco Regulation*". Archived from the original on 16 June 2010. Retrieved 29 February 2016.
- "Phil Taylor's Papers " Index". Archived from the original on 12 February 2012. Retrieved 29 February 2016.
- European Union – Tobacco advertising ban takes effect July 31 Archived 24 January 2011 at the Wayback Machine
- "Report on the implementation of the EU Tobacco Advertising Directive" (PDF). Archived (PDF) from the original on 5 September 2011. Retrieved 4 August 2008.
- Tobacco – Health warnings Australian Government Department of Health and Ageing. Retrieved 29 August 2008
- Public Health at a Glance – Tobacco Pack Information
- Scottish Government, St Andrew's House (21 January 2013). "Tobacco Display Ban Guidance". www2.gov.scot. Archived from the original on 27 November 2019. Retrieved 27 November 2019.
- "Guidance on the display and pricing of tobacco products in Northern Ireland | Department of Health". Health. 25 August 2015. Archived from the original on 27 November 2019. Retrieved 27 November 2019.
- Norwegian Government (1996). "Act No. 14 of March 9th, 1973 Relating to Prevention of the Harmful Effects of Tobacco (The Tobacco Control Act)" (PDF). Archived from the original (PDF) on 18 March 2017. Retrieved 27 November 2019.
- "WHO | Norway: Prohibition on the visible display of tobacco products at the points of sale". WHO. Archived from the original on 13 February 2020. Retrieved 27 November 2019.
- "Imperial Tobacco take fight against cigarette display ban to Supreme". The Independent. 12 November 2012. Archived from the original on 21 June 2022. Retrieved 27 November 2019.
- Carrell, Severin; correspondent, Scotland (12 December 2012). "Scotland to ban cigarette displays in shops after court challenge fails". The Guardian. ISSN 0261-3077. Archived from the original on 27 November 2019. Retrieved 27 November 2019.
{{cite news}}:|last2=has generic name (help) - World Health Organization (2017). "Evidence brief: Tobacco point-of-sale display bans" (PDF). WHO. Archived from the original (PDF) on 27 November 2019. Retrieved 27 November 2019.
- "Tobacco Sales Law". Archived from the original on 23 November 2010. Retrieved 29 February 2016.
- Ahlfeldt, G., Maennig, W. (2010), Impact of non-smoking ordinances on hospitality revenues: The case of Germany, in Journal of Economics and Statistics, 230(5), 506–521; preliminary version in: Hamburg Contemporary Discussion Papers N° 26, http://www.uni-hamburg.de/economicpolicy/hced.html Archived 23 May 2016 at the Wayback Machine.
- "NFPA applauds Reynolds American Inc". Archived from the original on 1 March 2013. Retrieved 29 February 2016.
- "NFPA" (PDF). Archived from the original (PDF) on 20 November 2007. Retrieved 29 February 2016.
- ^ "Coalition for Fire-Safe Cigarettes". Archived from the original on 16 August 2011. Retrieved 29 February 2016.
- Lindeman, Tracey (1 August 2023). "'Poison in every puff': Canada puts health warnings on individual cigarettes". The Guardian. ISSN 0261-3077. Retrieved 8 August 2023.
- C. Merrill, J.; Kleber, H. D.; Shwartz, M.; Liu, H.; Lewis, S. R. (1999). "Cigarettes, alcohol, marijuana, other risk behaviors, and American youth". Drug and Alcohol Dependence. 56 (3): 205–212. doi:10.1016/S0376-8716(99)00034-4. PMID 10529022.
- Swan, G. C.; Carmelli, D.; Rosenman, R. H.; Fabsitz, R. R.; Christian, J. C. (1990). "Smoking and alcohol consumption in adult male twins: genetic heritability and shared environmental influences" (Free full text). Journal of Substance Abuse. 2 (1): 39–50. doi:10.1016/S0899-3289(05)80044-6. ISSN 0899-3289. PMID 2136102. Archived from the original on 4 July 2016. Retrieved 7 April 2016.
- "Why Nicotine is a Gateway Drug". National Institutes of Health (NIH). 22 May 2015. Archived from the original on 11 April 2020. Retrieved 20 April 2020.
- Rohsenow, Damaris J.; Martin, Rosemarie A.; Tidey, Jennifer W.; Colby, Suzanne M.; Monti, Peter M. (2017). "Treating Smokers in Substance Treatment With Contingent Vouchers, Nicotine Replacement and Brief Advice Adapted for Sobriety Settings". Journal of Substance Abuse Treatment. 72: 72–79. doi:10.1016/j.jsat.2016.08.012. PMC 5154824. PMID 27658756.
- "Vaping to quit smoking - NHS". nhs.uk. 20 September 2022. Archived from the original on 21 June 2023. Retrieved 13 June 2023.
- Tang, Yi-Yuan; Tang, Rongxiang; Posner, Michael I. (2016). "Mindfulness meditation improves emotion regulation and reduces drug abuse". Drug and Alcohol Dependence. 163: S13–S18. doi:10.1016/j.drugalcdep.2015.11.041. PMID 27306725.
- Centers for Disease Control Prevention (CDC) (November 2011). "Quitting smoking among adults—United States, 2001–2010". MMWR. Morbidity and Mortality Weekly Report. 60 (44): 1513–9. PMID 22071589. Archived from the original on 3 January 2023. Retrieved 9 May 2015.
- Brunetta PG, Kroon L (2022). "Smoking Cessation". In Broaddus C, Ernst JD, King, TE, et al. (eds.). Murray & Nadel's Textbook of Respiratory Medicine (7 ed.). Elsevier. pp. 900–909.
- Rosen, Laura J.; Galili, Tal; Kott, Jeffrey; Goodman, Mark; Freedman, Laurence S. (January 2018). "Diminishing benefit of smoking cessation medications during the first year: a meta-analysis of randomized controlled trials". Addiction. 113 (5). Wiley-Blackwell on behalf of the Society for the Study of Addiction: 805–816. doi:10.1111/add.14134. ISSN 0965-2140. PMC 5947828. PMID 29377409. S2CID 4764039.
- "Family First: Dr. Anil's Love-Infused Anti-Smoking Initiative". GorakhaPatra. Retrieved 5 February 2024.
Bibliography
- Frieden, Thomas R. et al. The Health Consequences of Smoking: 50 Years of Progress: A Report of the Surgeon General (2014) online
- Gilman, Sander L.; Xun, Zhou (15 August 2004). Smoke: A Global History of Smoking. Reaktion Books. ISBN 978-1-86189-200-3. Retrieved 22 March 2009.
- Goodman, Jordan, ed. Tobacco in History and Culture. An Encyclopedia (2 vol, Gage Cengage, 2005) online
- Hirschfelder, Arlene B. Encyclopedia of smoking and tobacco (1999) online
- Oreskes, Naomi, and Erik M. Conway. Merchants of doubt: How a handful of scientists obscured the truth on issues from tobacco smoke to global warming (Bloomsbury Publishing USA, 2011).
- Proctor, Robert N. (15 November 2000). The Nazi War on Cancer. Princeton University Press. ISBN 978-0-691-07051-3. Retrieved 22 March 2009.
- World Health Organization (2008). The Global Burden of Disease 2004 Update (PDF). World Health Organization. ISBN 978-92-4-156371-0. Archived (PDF) from the original on 14 November 2008. Retrieved 1 January 2008.
- World Health Organization (2008). WHO Report on the Global Tobacco Epidemic, 2008: the MPOWER package (PDF). World Health Organization. ISBN 978-92-4-159628-2. Archived from the original (PDF) on 7 February 2009. Retrieved 1 January 2008.
External links
- Tobacco History Links – repository from Tobacco.org
- Surgeon General: Tobacco Cessation
| Cigarettes | |||
|---|---|---|---|
| Types | |||
| Components | |||
| Peripherals | |||
| Culture | |||
| Health issues | |||
| Related products | |||
| Tobacco industry |
| ||
| Government and the law | |||
| Lists | |||
| Tobacco smoking | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country and region |
| ||||||||||||
| Religion | |||||||||||||
| Health |
| ||||||||||||
| Smoking ban |
| ||||||||||||
| Other | |||||||||||||
| Recreational drug use | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
