| Revision as of 21:54, 5 February 2019 editKeith o (talk | contribs)288 edits →Calibration standards for measuring instruments: Added link to primary standard. Grammar← Previous edit | Latest revision as of 19:30, 13 December 2024 edit undoThe Blade of the Northern Lights (talk | contribs)Edit filter managers, Autopatrolled, Oversighters, Administrators55,784 edits →Environmental dosimetry: Fix | ||
| (20 intermediate revisions by 14 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Measurement of absorbed ionizing radiation}} | |||
| {{Use dmy dates|date=April 2024}} | |||
| ] Dosimetry Laboratory.]] | |||
| '''Radiation dosimetry''' in the fields of ] and ] is the measurement, calculation and assessment of the ] dose absorbed by an object, usually the human body. This applies both internally, due to ingested or inhaled radioactive substances, or externally due to irradiation by sources of radiation. | '''Radiation dosimetry''' in the fields of ] and ] is the measurement, calculation and assessment of the ] dose absorbed by an object, usually the human body. This applies both internally, due to ingested or inhaled radioactive substances, or externally due to irradiation by sources of radiation. | ||
| ] assessment relies on a variety of monitoring, bio-assay or radiation imaging techniques, whilst external dosimetry is based on measurements with a ], or inferred from measurements made by other radiological protection instruments. | ] assessment relies on a variety of monitoring, bio-assay or radiation imaging techniques, whilst external dosimetry is based on measurements with a ], or inferred from measurements made by other ].<ref>{{Cite web |last=Toohey |first=R. E |title=Basic Concepts of Internal Dosimetry |url=https://www.nrc.gov/docs/ML1215/ML12159A368.pdf}}</ref> | ||
| Radiation dosimetry is extensively used for radiation protection; routinely applied to monitor occupational radiation workers, where irradiation is expected, or where radiation is unexpected, such as in the contained aftermath of the ], ] or ] radiological release incidents. The public dose take-up is measured and calculated from a variety of indicators such as ambient measurements of gamma radiation, radioactive particulate monitoring, and the measurement of levels of ]. | |||
| Other significant areas are medical |
Other significant radiation dosimetry areas are medical, where the required treatment ] and any collateral absorbed dose is monitored, and environmental, such as ] monitoring in buildings. | ||
| ==Measuring radiation dose== | ==Measuring radiation dose== | ||
| ===External dose=== | ===External dose=== | ||
| There are several ways of measuring absorbed doses from ionizing radiation. People in occupational contact with radioactive substances, or who may be exposed to radiation, routinely carry personal ]s. These are specifically designed to record and indicate the dose received. Traditionally, these were lockets fastened to the external clothing of the monitored person, which contained photographic film known as ]s. These have been largely replaced with other devices such as |
There are several ways of measuring absorbed doses from ionizing radiation. People in occupational contact with radioactive substances, or who may be exposed to radiation, routinely carry personal ]s. These are specifically designed to record and indicate the dose received. Traditionally, these were lockets fastened to the external clothing of the monitored person, which contained photographic film known as ]s. These have been largely replaced with other devices such as ](TLD), ](OSL), or ](FNTD) badges.<ref>{{Cite web |title=Radiation Dosimetry-Introduction |url=https://www.ehs.harvard.edu/sites/ehs.harvard.edu/files/radiation_dosimetry_introduction.pdf}}</ref><ref>{{Cite web |date=July 2021 |title=Avo Photonics Develops Next Generation Radiation Detecting Instrument for LANDAUER |url=https://www.avophotonics.com/post/avo-photonics-develops-next-generation-radiation-detecting-instrument-for-landauer}}</ref> | ||
| ⚫ | The ] (ICRP) guidance states that if a personal dosimeter is worn on a position on the body representative of its exposure, assuming whole-body exposure, the value of Personal Dose Equivalent Hp(10), is sufficient to estimate an effective dose value suitable for radiological protection. Personal Dose Equivalent is a radiation quantity specifically designed to be used for radiation measurements by personal dosimeters.{{sfn|Valentin|2007|p=71}} Dosimeters are known as "legal dosimeters" if they have been approved for use in recording personnel dose for regulatory purposes. In cases of non-uniform irradiation such personal dosimeters may not be representative of certain specific areas of the body, where additional dosimeters are used in the area of concern. | ||
| ⚫ | A number of electronic devices known as Electronic Personal Dosimeters (EPDs) have come into general use using semiconductor detection and programmable processor technology. These are worn as badges but can give an indication of instantaneous dose rate and an audible and visual alarm if a dose rate or a total integrated dose is exceeded. A good deal of information can be made immediately available to the wearer of the recorded dose and current dose rate via a local display. They can be used as the main stand-alone dosimeter, or as a supplement to |
||
| ⚫ | A number of electronic devices known as Electronic Personal Dosimeters (EPDs) have come into general use using semiconductor detection and programmable processor technology. These are worn as badges but can give an indication of instantaneous dose rate and an audible and visual alarm if a dose rate or a total integrated dose is exceeded. A good deal of information can be made immediately available to the wearer of the recorded dose and current dose rate via a local display. They can be used as the main stand-alone dosimeter, or as a supplement to other devices. EPD's are particularly useful for real-time monitoring of dose where a high dose rate is expected which will time-limit the wearer's exposure. | ||
| ⚫ | The ] (ICRP) guidance states that if a personal dosimeter is worn on a position on the body representative of its exposure, assuming whole-body exposure, the value of |
||
| In certain circumstances, a dose can be inferred from readings taken by fixed instrumentation in an area in which the person concerned has been working. This would generally only be used if personal dosimetry had not been issued, or a personal dosimeter has been damaged or lost. Such calculations would take a pessimistic view of the likely received dose. | In certain circumstances, a dose can be inferred from readings taken by fixed instrumentation in an area in which the person concerned has been working. This would generally only be used if personal dosimetry had not been issued, or a personal dosimeter has been damaged or lost. Such calculations would take a pessimistic view of the likely received dose. | ||
| ===Internal dose=== | ===Internal dose=== | ||
| {{ |
{{Main|Internal dosimetry}} | ||
| ] is used to evaluate the ] due to the intake of radionuclides into the human body. |
] is used to evaluate the ] due to the intake of radionuclides into the human body. | ||
| ==Medical dosimetry== | ==Medical dosimetry== | ||
| {{Main |
{{Main|Treatment planning}} | ||
| Medical dosimetry is the calculation of absorbed dose and optimization of dose delivery in ]. It is often performed by a professional health physicist with specialized training in that field. In order to plan the delivery of radiation therapy, the radiation produced by the sources is usually characterized with ]s and ]s measured by a ]. | Medical dosimetry is the calculation of absorbed dose and optimization of dose delivery in ]. It is often performed by a professional health physicist with specialized training in that field. In order to plan the delivery of radiation therapy, the radiation produced by the sources is usually characterized with ]s and ]s measured by a ].<ref name=":0">{{Cite journal |last=Graham |first=Sasha |last2=Mills |first2=Michael |date=2021 |title=Why is Medical Dosimetry a profession only in the United States and what does this mean for Medical Physicists worldwide? |journal=Journal of Applied Clinical Medical Physics |volume=22 |issue=8 |pages=4–5 |doi=10.1002/acm2.13362 |pmc=8364271 |pmid=34272815}}</ref> | ||
| In radiation therapy, three-dimensional dose distributions are often evaluated using a technique known as ].<ref> |
In radiation therapy, three-dimensional dose distributions are often evaluated using a technique known as ].<ref name="Baldock">{{Cite journal |last=Baldock |first=C. |last2=De Deene |first2=Y. |last3=Doran |first3=S. |last4=Ibbott |first4=G. |last5=Jirasek |first5=A. |last6=Lepage |first6=M. |last7=McAuley |first7=K. B. |last8=Oldham |first8=M. |last9=Schreiner |first9=L. J. |date=2010-03-07 |title=Polymer gel dosimetry |url=https://pubmed.ncbi.nlm.nih.gov/20150687 |journal=Physics in Medicine and Biology |volume=55 |issue=5 |pages=R1–63 |doi=10.1088/0031-9155/55/5/R01 |issn=1361-6560 |pmc=3031873 |pmid=20150687}}</ref> | ||
| ==Environmental dosimetry== | ==Environmental dosimetry== | ||
| Environmental |
Environmental dosimetry is used where it is likely that the environment will generate a significant radiation dose. An example of this is ] monitoring. The largest single source of radiation exposure to the general public is naturally occurring radon gas, which comprises approximately 55% of the annual background dose. It is estimated that radon is responsible for 10% of lung cancers in the United States. Radon is a radioactive gas generated by the decay of uranium, which is present in varying amounts in the Earth's crust. Certain geographic areas, due to the underlying geology, continually generate radon which permeates its way to the Earth's surface. In some cases the dose can be significant in buildings where the gas can accumulate. A number of specialised dosimetry techniques are used to evaluate the dose that a building's occupants may receive. | ||
| ⚫ | ==Radiation exposure monitoring== | ||
| ⚫ | Records of legal dosimetry results are usually kept for a set period of time, depending upon the legal requirements of the nation in which they are used. | ||
| ⚫ | ] is the practice of collecting dose information from radiology equipment and using the data to help identify opportunities to reduce unnecessary dose in medical situations.<ref name=":0" /> | ||
| ==Measures of dose== | ==Measures of dose== | ||
| {{Main |
{{Main|sievert}} | ||
| ] | ] | ||
| ] | ] | ||
| To enable consideration of stochastic health risk, calculations are performed to convert the physical quantity absorbed dose into equivalent and effective doses, the details of which depend on the radiation type and biological context. For applications in ] and dosimetry assessment the (ICRP) and the ] (ICRU) have published recommendations and data which are used to calculate these. | To enable consideration of stochastic health risk, calculations are performed to convert the physical quantity absorbed dose into equivalent and effective doses, the details of which depend on the radiation type and biological context.<ref>{{Cite web |date=December 2017 |title=The DOE Ionizing Radiation Dose Ranges Chart |url=https://www.energy.gov/sites/prod/files/2018/01/f46/doe-ionizing-radiation-dose-ranges-jan-2018.pdf}}</ref> For applications in ] and dosimetry assessment the (ICRP) and the ] (ICRU) have published recommendations and data which are used to calculate these. | ||
| ===Units of measure=== | ===Units of measure=== | ||
| There are a number of different measures of radiation dose, including ] (''D'') measured in: |
There are a number of different measures of radiation dose, including ] (''D'') measured in: | ||
| *] (Gy) energy absorbed per unit of mass (]·kg<sup>−1</sup>) | *] (Gy) energy absorbed per unit of mass (]·kg<sup>−1</sup>) | ||
| *] (''H'') measured in ]s (Sv) | *] (''H'') measured in ]s (Sv) | ||
| *] (''E'') measured in sieverts |
*] (''E'') measured in sieverts | ||
| *] (K) measured in grays |
*] (K) measured in grays | ||
| *] (DAP) measured in gray centimeters<sup>2</sup> | *] (DAP) measured in gray centimeters<sup>2</sup> | ||
| *dose length product (DLP) measured in gray centimeters |
*dose length product (DLP) measured in gray centimeters | ||
| *] a deprecated unit of absorbed radiation dose, defined as 1 rad = 0.01 Gy = 0.01 J/kg | *] a deprecated unit of absorbed radiation dose, defined as 1 rad = 0.01 Gy = 0.01 J/kg | ||
| *] a legacy unit of measurement for the exposure of X-rays | *] a legacy unit of measurement for the exposure of X-rays | ||
| Line 52: | Line 59: | ||
| Each measure is often simply described as ‘dose’, which can lead to confusion. Non-] units are still used, particularly in the USA, where dose is often reported in rads and dose equivalent in ]. By definition, 1 Gy = 100 rad and 1 Sv = 100 rem. | Each measure is often simply described as ‘dose’, which can lead to confusion. Non-] units are still used, particularly in the USA, where dose is often reported in rads and dose equivalent in ]. By definition, 1 Gy = 100 rad and 1 Sv = 100 rem. | ||
| The fundamental quantity is the absorbed dose (''D''), which is defined as the mean energy imparted (dE) per unit mass (dm) of material (D = dE/dm)<ref name="Measurements 2011"> |
The fundamental quantity is the absorbed dose (''D''), which is defined as the mean energy imparted (dE) per unit mass (dm) of material (D = dE/dm)<ref name="Measurements 2011">{{Cite journal |last=Seltzer |first=S. M. |last2=Bartlett |first2=D. T. |last3=Burns |first3=D. T. |last4=Dietze |first4=G. |last5=Menzel |first5=H.-G. |last6=Paretzke |first6=H. G. |last7=Wambersie |first7=A. |date=2011 |title=The International Commission on Radiation Units and Measurements |journal=Journal of the ICRU |volume=11 |issue=1 |pages=NP.1–NP |doi=10.1093/jicru/ndr011 |issn=1473-6691}}</ref> The SI unit of absorbed dose is the gray (Gy) defined as one joule per kilogram. Absorbed dose, as a point measurement, is suitable for describing localised (i.e. partial organ) exposures such as tumour dose in radiotherapy. It may be used to estimate stochastic risk provided the amount and type of tissue involved is stated. Localised diagnostic dose levels are typically in the 0–50 mGy range. At a dose of 1 milligray (mGy) of photon radiation, each cell nucleus is crossed by an average of 1 liberated electron track.<ref>{{Cite journal |last=Feinendegen |first=L E |date=1990-05-01 |title=The cell dose concept; potential application in radiation protection |journal=Physics in Medicine and Biology |volume=35 |issue=5 |pages=597–612 |doi=10.1088/0031-9155/35/5/001 |issn=0031-9155}}</ref> | ||
| ===Equivalent dose=== | ===Equivalent dose=== | ||
| {{Main |
{{Main|equivalent dose}} | ||
| The absorbed dose required to produce a certain biological effect varies between different types of radiation, such as ], ] or ]. This is taken into account by the equivalent dose (H), which is defined as the mean dose to organ T by radiation type R (''D''<sub>T,R</sub>), multiplied by a weighting factor ''W''<sub>R</sub> . This designed to take into account the ] (RBE) of the radiation type,<ref name="Measurements 2011"/> For instance, for the same absorbed dose in Gy, alpha particles are 20 times as biologically potent as X or gamma rays. The measure of ‘dose equivalent’ is not organ averaged and now only used for "operational quantities". Equivalent dose is designed for estimation of stochastic risks from radiation exposures. Stochastic effect is defined for radiation dose assessment as the ''probability'' of cancer induction and genetic damage. |
The absorbed dose required to produce a certain biological effect varies between different types of radiation, such as ], ] or ]. This is taken into account by the equivalent dose (H), which is defined as the mean dose to organ T by radiation type R (''D''<sub>T,R</sub>), multiplied by a weighting factor ''W''<sub>R</sub> . This designed to take into account the ] (RBE) of the radiation type,<ref name="Measurements 2011" /> For instance, for the same absorbed dose in Gy, alpha particles are 20 times as biologically potent as X or gamma rays. The measure of ‘dose equivalent’ is not organ averaged and now only used for "operational quantities". Equivalent dose is designed for estimation of stochastic risks from radiation exposures. Stochastic effect is defined for radiation dose assessment as the ''probability'' of cancer induction and genetic damage.{{sfn|Valentin|2007|p=51}} | ||
| As dose is averaged over the whole organ; equivalent dose is rarely suitable for evaluation of acute radiation effects or tumour dose in radiotherapy. In the case of estimation of stochastic effects, assuming a ], this averaging out should make no difference as the total energy imparted remains the same. | As dose is averaged over the whole organ; equivalent dose is rarely suitable for evaluation of acute radiation effects or tumour dose in radiotherapy. In the case of estimation of stochastic effects, assuming a ], this averaging out should make no difference as the total energy imparted remains the same. | ||
| {| class="wikitable" | {| class="wikitable" | ||
| |+Radiation weighting factors ''W''<sub>R</sub> (formerly termed Q factor)<br/> used to represent ]<br/> according to ] report 103 |
|+Radiation weighting factors ''W''<sub>R</sub> (formerly termed Q factor)<br/> used to represent ]<br/> according to ] report 103{{sfn|Valentin|2007|p=65}} | ||
| |- | |- | ||
| ! Radiation !! Energy !! W<sub>R</sub> (formerly Q) | ! Radiation !! Energy !! W<sub>R</sub> (formerly Q) | ||
| Line 69: | Line 76: | ||
| | rowspan=3 |]s || < 1 MeV || 2.5 + 18.2·e<sup>−²/6</sup> | | rowspan=3 |]s || < 1 MeV || 2.5 + 18.2·e<sup>−²/6</sup> | ||
| |- | |- | ||
| | 1 MeV |
| 1 MeV – 50 MeV || 5.0 + 17.0·e<sup>−²/6</sup> | ||
| |- | |- | ||
| | > 50 MeV || 2.5 + 3.25·e<sup>−²/6</sup> | | > 50 MeV || 2.5 + 3.25·e<sup>−²/6</sup> | ||
| Line 79: | Line 86: | ||
| ===Effective dose=== | ===Effective dose=== | ||
| {{Main |
{{Main|Effective dose (radiation)}} | ||
| Effective dose is the central dose quantity for radiological protection used to specify exposure limits to ensure that the occurrence of stochastic health effects is kept below unacceptable levels and that tissue reactions are avoided. |
Effective dose is the central dose quantity for radiological protection used to specify exposure limits to ensure that the occurrence of stochastic health effects is kept below unacceptable levels and that tissue reactions are avoided.{{sfn|Valentin|2007|p=63-64}} | ||
| It is difficult to compare the stochastic risk from localised exposures of different parts of the body (e.g. a chest x-ray compared to a CT scan of the head), or to compare exposures of the same body part but with different exposure patterns (e.g. a cardiac CT scan with a cardiac nuclear medicine scan). One way to avoid this problem is to simply average out a localised dose over the whole body. The problem of this approach is that the stochastic risk of cancer induction varies from one tissue to another. | It is difficult to compare the stochastic risk from localised exposures of different parts of the body (e.g. a chest x-ray compared to a CT scan of the head), or to compare exposures of the same body part but with different exposure patterns (e.g. a cardiac CT scan with a cardiac nuclear medicine scan). One way to avoid this problem is to simply average out a localised dose over the whole body. The problem of this approach is that the stochastic risk of cancer induction varies from one tissue to another. | ||
| Line 92: | Line 99: | ||
| {| class="wikitable" | {| class="wikitable" | ||
| |+Weighting factors for different organs<ref> |
|+Weighting factors for different organs<ref>{{Cite report |url=https://www.unscear.org/docs/reports/2008/09-86753_Report_2008_Annex_A.pdf |title=Sources and effects of ionizing radiation |date=2010 |publisher=United Nations Scientific Committee on the Effects of Atomic Radiation |place=New York |volume=1 |page=40 |isbn=978-92-1-142274-0}}</ref> | ||
| |- | |- | ||
| ! rowspan=2 |Organs !! colspan=3 |Tissue weighting factors | ! rowspan=2 |Organs !! colspan=3 |Tissue weighting factors | ||
| Line 102: | Line 109: | ||
| | Red ] || 0.12 || 0.12 || 0.12 | | Red ] || 0.12 || 0.12 || 0.12 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.12 || 0.12 | ||
| |- | |- | ||
| | ] || 0.12 || 0.12 || 0.12 |
| ] || 0.12 || 0.12 || 0.12 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.12 || 0.12 | ||
| |- | |- | ||
| | ]s || 0.15 || 0.05 || 0.12 |
| ]s || 0.15 || 0.05 || 0.12 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.05 || 0.04 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.05 || 0.04 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.05 || 0.04 | ||
| |- | |- | ||
| | ] || 0.03 || 0.05 || 0.04 | | ] || 0.03 || 0.05 || 0.04 | ||
| |- | |- | ||
| | ] || |
| ] || – || 0.01 || 0.01 | ||
| |- | |- | ||
| | ] surface || 0.03 || 0.01 || 0.01 |
| ] surface || 0.03 || 0.01 || 0.01 | ||
| |- | |- | ||
| | ] || |
| ] || – || – || 0.01 | ||
| |- | |- | ||
| | ] || |
| ] || – || – || 0.01 | ||
| |- | |- | ||
| | Remainder of body || 0.30 || 0.05 || 0.12 | | Remainder of body || 0.30 || 0.05 || 0.12 | ||
| Line 140: | Line 147: | ||
| National standards laboratories such as the ] (NPL) provide calibration factors for ionization chambers and other measurement devices to convert from the instrument's readout to absorbed dose. The standards laboratories operates as a ], which is normally calibrated by absolute ] (the warming of substances when they absorb energy). A user sends their secondary standard to the laboratory, where it is exposed to a known amount of radiation (derived from the primary standard) and a factor is issued to convert the instrument's reading to that dose. The user may then use their secondary standard to derive calibration factors for other instruments they use, which then become tertiary standards, or field instruments. | National standards laboratories such as the ] (NPL) provide calibration factors for ionization chambers and other measurement devices to convert from the instrument's readout to absorbed dose. The standards laboratories operates as a ], which is normally calibrated by absolute ] (the warming of substances when they absorb energy). A user sends their secondary standard to the laboratory, where it is exposed to a known amount of radiation (derived from the primary standard) and a factor is issued to convert the instrument's reading to that dose. The user may then use their secondary standard to derive calibration factors for other instruments they use, which then become tertiary standards, or field instruments. | ||
| The NPL operates a graphite-calorimeter for absolute photon dosimetry. Graphite is used instead of water as its ] is one-sixth that of water and therefore the temperature increase in graphite is 6 times higher than the equivalent in water and measurements are more accurate. Significant problems exist in insulating the graphite from the surrounding environment in order to measure the tiny temperature changes. A lethal dose of radiation to a human is approximately 10–20 Gy. This is |
The NPL operates a graphite-calorimeter for absolute photon dosimetry. Graphite is used instead of water as its ] is one-sixth that of water and therefore the temperature increase in graphite is 6 times higher than the equivalent in water and measurements are more accurate. Significant problems exist in insulating the graphite from the surrounding environment in order to measure the tiny temperature changes. A lethal dose of radiation to a human is approximately 10–20 Gy. This is 10–20 joules per kilogram. A 1 cm<sup>3</sup> piece of graphite weighing 2 grams would therefore absorb around 20–40 mJ. With a specific heat capacity of around 700 J·kg<sup>−1</sup>·K<sup>−1</sup>, this equates to a temperature rise of just 20 mK. | ||
| Dosimeters in radiotherapy (] in external beam therapy) are routinely calibrated using ]s<ref>Hill |
Dosimeters in radiotherapy (] in external beam therapy) are routinely calibrated using ]s<ref>{{Cite journal |last=Hill |first=Robin |last2=Mo |first2=Zhao |last3=Haque |first3=Mamoon |last4=Baldock |first4=Clive |date=2009 |title=An evaluation of ionization chambers for the relative dosimetry of kilovoltage x-ray beams |journal=Medical Physics |volume=36 |issue=9 |pages=3971–3981 |doi=10.1118/1.3183820 |issn=0094-2405 |pmid=19810470}}</ref> or diode technology or gel dosimeters.<ref name=Baldock/> | ||
| ==Radiation-related quantities== | ==Radiation-related quantities== | ||
| Line 148: | Line 155: | ||
| {{Radiation related quantities}} | {{Radiation related quantities}} | ||
| Although the United States Nuclear Regulatory Commission permits the use of the units ], rad, and ] alongside SI units,<ref>{{ |
Although the United States Nuclear Regulatory Commission permits the use of the units ], rad, and ] alongside SI units,<ref>{{Cite book |url=https://www.nrc.gov/reading-rm/doc-collections/cfr/part020/part020-1004.html |title=10 CFR 20.1004 |publisher=US Nuclear Regulatory Commission |year=2009}}</ref> the ] ] required that their use for "public health ... purposes" be phased out by 31 December 1985.<ref>{{Cite web |last=The Council of the European Communities |date=21 December 1979 |title=Council Directive 80/181/EEC of 20 December 1979 on the approximation of the laws of the Member States relating to Unit of measurement and on the repeal of Directive 71/354/EEC |url=http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:31980L0181:EN:NOT |access-date=19 May 2012}}</ref> | ||
| | url = http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:31980L0181:EN:NOT | |||
| | author = The Council of the European Communities | |||
| | title = Council Directive 80/181/EEC of 20 December 1979 on the approximation of the laws of the Member States relating to Unit of measurement and on the repeal of Directive 71/354/EEC | |||
| | date=1979-12-21 | |||
| | accessdate=19 May 2012}}</ref> | |||
| ⚫ | ==Radiation exposure monitoring== | ||
| ⚫ | Records of legal dosimetry results are usually kept for a set period of time, depending upon the legal requirements of the nation in which they are used. | ||
| ⚫ | ] is the practice of collecting dose information from radiology equipment and using the data to help identify opportunities to reduce unnecessary dose in medical situations. | ||
| ==See also== | ==See also== | ||
| Line 165: | Line 162: | ||
| * ] | * ] | ||
| == |
==Notes== | ||
| {{reflist}} | {{reflist}} | ||
| ==References== | |||
| {{refbegin}} | |||
| * {{Citation |title=The 2007 Recommendations of the International Commission on Radiological Protection |date=2007 |volume=37 |editor-last=Valentin |editor-first=J |url=https://journals.sagepub.com/doi/pdf/10.1177/ANIB_37_2-4 |access-date=2024-08-11 |isbn=978-0-7020-3048-2 |issn=0146-6453}} | |||
| {{refend}} | |||
| ==External links== | ==External links== | ||
| * | * {{Webarchive|url=https://web.archive.org/web/20171029065239/https://senphys.com/how-does-ionization-chamber.html |date=29 October 2017 }} | ||
| * |
* – "The confusing world of radiation dosimetry" – M.A. Boyd, U.S. Environmental Protection Agency. An account of chronological differences between USA and ICRP dosimetry systems. | ||
| * Tim Stephens and Keith Pantridge, 'Dosimetry, Personal Monitoring Film' (a short article on Dosimetry from the point of view of its relation to photography, in , volume 2, number 2, 2011, pp. 153–158.) | * Tim Stephens and Keith Pantridge, 'Dosimetry, Personal Monitoring Film' (a short article on Dosimetry from the point of view of its relation to photography, in , volume 2, number 2, 2011, pp. 153–158.) | ||
| {{Radiation protection|state=uncollapsed}} | {{Radiation protection|state=uncollapsed}} | ||
| {{Authority control}} | |||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
Latest revision as of 19:30, 13 December 2024
Measurement of absorbed ionizing radiation

Radiation dosimetry in the fields of health physics and radiation protection is the measurement, calculation and assessment of the ionizing radiation dose absorbed by an object, usually the human body. This applies both internally, due to ingested or inhaled radioactive substances, or externally due to irradiation by sources of radiation.
Internal dosimetry assessment relies on a variety of monitoring, bio-assay or radiation imaging techniques, whilst external dosimetry is based on measurements with a dosimeter, or inferred from measurements made by other radiological protection instruments.
Radiation dosimetry is extensively used for radiation protection; routinely applied to monitor occupational radiation workers, where irradiation is expected, or where radiation is unexpected, such as in the contained aftermath of the Three Mile Island, Chernobyl or Fukushima radiological release incidents. The public dose take-up is measured and calculated from a variety of indicators such as ambient measurements of gamma radiation, radioactive particulate monitoring, and the measurement of levels of radioactive contamination.
Other significant radiation dosimetry areas are medical, where the required treatment absorbed dose and any collateral absorbed dose is monitored, and environmental, such as radon monitoring in buildings.
Measuring radiation dose
External dose
There are several ways of measuring absorbed doses from ionizing radiation. People in occupational contact with radioactive substances, or who may be exposed to radiation, routinely carry personal dosimeters. These are specifically designed to record and indicate the dose received. Traditionally, these were lockets fastened to the external clothing of the monitored person, which contained photographic film known as film badge dosimeters. These have been largely replaced with other devices such as Thermoluminescent dosimetry(TLD), optically stimulated luminescence(OSL), or Fluorescent Nuclear Tract Detector(FNTD) badges.
The International Committee on Radiation Protection (ICRP) guidance states that if a personal dosimeter is worn on a position on the body representative of its exposure, assuming whole-body exposure, the value of Personal Dose Equivalent Hp(10), is sufficient to estimate an effective dose value suitable for radiological protection. Personal Dose Equivalent is a radiation quantity specifically designed to be used for radiation measurements by personal dosimeters. Dosimeters are known as "legal dosimeters" if they have been approved for use in recording personnel dose for regulatory purposes. In cases of non-uniform irradiation such personal dosimeters may not be representative of certain specific areas of the body, where additional dosimeters are used in the area of concern.
A number of electronic devices known as Electronic Personal Dosimeters (EPDs) have come into general use using semiconductor detection and programmable processor technology. These are worn as badges but can give an indication of instantaneous dose rate and an audible and visual alarm if a dose rate or a total integrated dose is exceeded. A good deal of information can be made immediately available to the wearer of the recorded dose and current dose rate via a local display. They can be used as the main stand-alone dosimeter, or as a supplement to other devices. EPD's are particularly useful for real-time monitoring of dose where a high dose rate is expected which will time-limit the wearer's exposure.
In certain circumstances, a dose can be inferred from readings taken by fixed instrumentation in an area in which the person concerned has been working. This would generally only be used if personal dosimetry had not been issued, or a personal dosimeter has been damaged or lost. Such calculations would take a pessimistic view of the likely received dose.
Internal dose
Main article: Internal dosimetryInternal dosimetry is used to evaluate the committed dose due to the intake of radionuclides into the human body.
Medical dosimetry
Main article: Treatment planningMedical dosimetry is the calculation of absorbed dose and optimization of dose delivery in radiation therapy. It is often performed by a professional health physicist with specialized training in that field. In order to plan the delivery of radiation therapy, the radiation produced by the sources is usually characterized with percentage depth dose curves and dose profiles measured by a medical physicist.
In radiation therapy, three-dimensional dose distributions are often evaluated using a technique known as gel dosimetry.
Environmental dosimetry
Environmental dosimetry is used where it is likely that the environment will generate a significant radiation dose. An example of this is radon monitoring. The largest single source of radiation exposure to the general public is naturally occurring radon gas, which comprises approximately 55% of the annual background dose. It is estimated that radon is responsible for 10% of lung cancers in the United States. Radon is a radioactive gas generated by the decay of uranium, which is present in varying amounts in the Earth's crust. Certain geographic areas, due to the underlying geology, continually generate radon which permeates its way to the Earth's surface. In some cases the dose can be significant in buildings where the gas can accumulate. A number of specialised dosimetry techniques are used to evaluate the dose that a building's occupants may receive.
Radiation exposure monitoring
Records of legal dosimetry results are usually kept for a set period of time, depending upon the legal requirements of the nation in which they are used.
Medical radiation exposure monitoring is the practice of collecting dose information from radiology equipment and using the data to help identify opportunities to reduce unnecessary dose in medical situations.
Measures of dose
Main article: sievert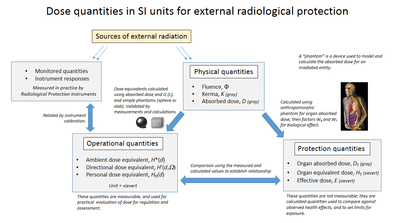

To enable consideration of stochastic health risk, calculations are performed to convert the physical quantity absorbed dose into equivalent and effective doses, the details of which depend on the radiation type and biological context. For applications in radiation protection and dosimetry assessment the (ICRP) and the International Commission on Radiation Units and Measurements (ICRU) have published recommendations and data which are used to calculate these.
Units of measure
There are a number of different measures of radiation dose, including absorbed dose (D) measured in:
- gray (Gy) energy absorbed per unit of mass (J·kg)
- Equivalent dose (H) measured in sieverts (Sv)
- Effective dose (E) measured in sieverts
- Kerma (K) measured in grays
- dose area product (DAP) measured in gray centimeters
- dose length product (DLP) measured in gray centimeters
- rads a deprecated unit of absorbed radiation dose, defined as 1 rad = 0.01 Gy = 0.01 J/kg
- Roentgen a legacy unit of measurement for the exposure of X-rays
Each measure is often simply described as ‘dose’, which can lead to confusion. Non-SI units are still used, particularly in the USA, where dose is often reported in rads and dose equivalent in rems. By definition, 1 Gy = 100 rad and 1 Sv = 100 rem.
The fundamental quantity is the absorbed dose (D), which is defined as the mean energy imparted (dE) per unit mass (dm) of material (D = dE/dm) The SI unit of absorbed dose is the gray (Gy) defined as one joule per kilogram. Absorbed dose, as a point measurement, is suitable for describing localised (i.e. partial organ) exposures such as tumour dose in radiotherapy. It may be used to estimate stochastic risk provided the amount and type of tissue involved is stated. Localised diagnostic dose levels are typically in the 0–50 mGy range. At a dose of 1 milligray (mGy) of photon radiation, each cell nucleus is crossed by an average of 1 liberated electron track.
Equivalent dose
Main article: equivalent doseThe absorbed dose required to produce a certain biological effect varies between different types of radiation, such as photons, neutrons or alpha particles. This is taken into account by the equivalent dose (H), which is defined as the mean dose to organ T by radiation type R (DT,R), multiplied by a weighting factor WR . This designed to take into account the biological effectiveness (RBE) of the radiation type, For instance, for the same absorbed dose in Gy, alpha particles are 20 times as biologically potent as X or gamma rays. The measure of ‘dose equivalent’ is not organ averaged and now only used for "operational quantities". Equivalent dose is designed for estimation of stochastic risks from radiation exposures. Stochastic effect is defined for radiation dose assessment as the probability of cancer induction and genetic damage.
As dose is averaged over the whole organ; equivalent dose is rarely suitable for evaluation of acute radiation effects or tumour dose in radiotherapy. In the case of estimation of stochastic effects, assuming a linear dose response, this averaging out should make no difference as the total energy imparted remains the same.
| Radiation | Energy | WR (formerly Q) |
|---|---|---|
| x-rays, gamma rays, beta rays, muons |
1 | |
| neutrons | < 1 MeV | 2.5 + 18.2·e |
| 1 MeV – 50 MeV | 5.0 + 17.0·e | |
| > 50 MeV | 2.5 + 3.25·e | |
| protons, charged pions | 2 | |
| alpha rays, Nuclear fission products, heavy nuclei |
20 |
Effective dose
Main article: Effective dose (radiation)Effective dose is the central dose quantity for radiological protection used to specify exposure limits to ensure that the occurrence of stochastic health effects is kept below unacceptable levels and that tissue reactions are avoided.
It is difficult to compare the stochastic risk from localised exposures of different parts of the body (e.g. a chest x-ray compared to a CT scan of the head), or to compare exposures of the same body part but with different exposure patterns (e.g. a cardiac CT scan with a cardiac nuclear medicine scan). One way to avoid this problem is to simply average out a localised dose over the whole body. The problem of this approach is that the stochastic risk of cancer induction varies from one tissue to another.
The effective dose E is designed to account for this variation by the application of specific weighting factors for each tissue (WT). Effective dose provides the equivalent whole body dose that gives the same risk as the localised exposure. It is defined as the sum of equivalent doses to each organ (HT), each multiplied by its respective tissue weighting factor (WT).
Weighting factors are calculated by the International Commission for Radiological Protection (ICRP), based on the risk of cancer induction for each organ and adjusted for associated lethality, quality of life and years of life lost. Organs that are remote from the site of irradiation will only receive a small equivalent dose (mainly due to scattering) and therefore contribute little to the effective dose, even if the weighting factor for that organ is high.
Effective dose is used to estimate stochastic risks for a ‘reference’ person, which is an average of the population. It is not suitable for estimating stochastic risk for individual medical exposures, and is not used to assess acute radiation effects.
| Organs | Tissue weighting factors | ||
|---|---|---|---|
| ICRP30(I36) 1979 |
ICRP60(I3) 1991 |
ICRP103(I6) 2008 | |
| Gonads | 0.25 | 0.20 | 0.08 |
| Red Bone Marrow | 0.12 | 0.12 | 0.12 |
| Colon | – | 0.12 | 0.12 |
| Lung | 0.12 | 0.12 | 0.12 |
| Stomach | – | 0.12 | 0.12 |
| Breasts | 0.15 | 0.05 | 0.12 |
| Bladder | – | 0.05 | 0.04 |
| Liver | – | 0.05 | 0.04 |
| Oesophagus | – | 0.05 | 0.04 |
| Thyroid | 0.03 | 0.05 | 0.04 |
| Skin | – | 0.01 | 0.01 |
| Bone surface | 0.03 | 0.01 | 0.01 |
| Salivary glands | – | – | 0.01 |
| Brain | – | – | 0.01 |
| Remainder of body | 0.30 | 0.05 | 0.12 |
Dose versus source or field strength
Radiation dose refers to the amount of energy deposited in matter and/or biological effects of radiation, and should not be confused with the unit of radioactive activity (becquerel, Bq) of the source of radiation, or the strength of the radiation field (fluence). The article on the sievert gives an overview of dose types and how they are calculated. Exposure to a source of radiation will give a dose which is dependent on many factors, such as the activity, duration of exposure, energy of the radiation emitted, distance from the source and amount of shielding.
Background radiation
The worldwide average background dose for a human being is about 3.5 mSv per year , mostly from cosmic radiation and natural isotopes in the earth. The largest single source of radiation exposure to the general public is naturally occurring radon gas, which comprises approximately 55% of the annual background dose. It is estimated that radon is responsible for 10% of lung cancers in the United States.
Calibration standards for measuring instruments
Because the human body is approximately 70% water and has an overall density close to 1 g/cm, dose measurement is usually calculated and calibrated as dose to water.
National standards laboratories such as the National Physical Laboratory, UK (NPL) provide calibration factors for ionization chambers and other measurement devices to convert from the instrument's readout to absorbed dose. The standards laboratories operates as a primary standard, which is normally calibrated by absolute calorimetry (the warming of substances when they absorb energy). A user sends their secondary standard to the laboratory, where it is exposed to a known amount of radiation (derived from the primary standard) and a factor is issued to convert the instrument's reading to that dose. The user may then use their secondary standard to derive calibration factors for other instruments they use, which then become tertiary standards, or field instruments.
The NPL operates a graphite-calorimeter for absolute photon dosimetry. Graphite is used instead of water as its specific heat capacity is one-sixth that of water and therefore the temperature increase in graphite is 6 times higher than the equivalent in water and measurements are more accurate. Significant problems exist in insulating the graphite from the surrounding environment in order to measure the tiny temperature changes. A lethal dose of radiation to a human is approximately 10–20 Gy. This is 10–20 joules per kilogram. A 1 cm piece of graphite weighing 2 grams would therefore absorb around 20–40 mJ. With a specific heat capacity of around 700 J·kg·K, this equates to a temperature rise of just 20 mK.
Dosimeters in radiotherapy (linear particle accelerator in external beam therapy) are routinely calibrated using ionization chambers or diode technology or gel dosimeters.
Radiation-related quantities
The following table shows radiation quantities in SI and non-SI units.
| Quantity | Unit | Symbol | Derivation | Year | SI equivalent |
|---|---|---|---|---|---|
| Activity (A) | becquerel | Bq | s | 1974 | SI unit |
| curie | Ci | 3.7×10 s | 1953 | 3.7×10 Bq | |
| rutherford | Rd | 10 s | 1946 | 1000000 Bq | |
| Exposure (X) | coulomb per kilogram | C/kg | C⋅kg of air | 1974 | SI unit |
| röntgen | R | esu / 0.001293 g of air | 1928 | 2.58×10 C/kg | |
| Absorbed dose (D) | gray | Gy | J⋅kg | 1974 | SI unit |
| erg per gram | erg/g | erg⋅g | 1950 | 1.0×10 Gy | |
| rad | rad | 100 erg⋅g | 1953 | 0.010 Gy | |
| Equivalent dose (H) | sievert | Sv | J⋅kg × WR | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g × WR | 1971 | 0.010 Sv | |
| Effective dose (E) | sievert | Sv | J⋅kg × WR × WT | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g × WR × WT | 1971 | 0.010 Sv |
Although the United States Nuclear Regulatory Commission permits the use of the units curie, rad, and rem alongside SI units, the European Union European units of measurement directives required that their use for "public health ... purposes" be phased out by 31 December 1985.
See also
Notes
- Toohey, R. E. "Basic Concepts of Internal Dosimetry" (PDF).
- "Radiation Dosimetry-Introduction" (PDF).
- "Avo Photonics Develops Next Generation Radiation Detecting Instrument for LANDAUER". July 2021.
- Valentin 2007, p. 71.
- ^ Graham, Sasha; Mills, Michael (2021). "Why is Medical Dosimetry a profession only in the United States and what does this mean for Medical Physicists worldwide?". Journal of Applied Clinical Medical Physics. 22 (8): 4–5. doi:10.1002/acm2.13362. PMC 8364271. PMID 34272815.
- ^ Baldock, C.; De Deene, Y.; Doran, S.; Ibbott, G.; Jirasek, A.; Lepage, M.; McAuley, K. B.; Oldham, M.; Schreiner, L. J. (7 March 2010). "Polymer gel dosimetry". Physics in Medicine and Biology. 55 (5): R1–63. doi:10.1088/0031-9155/55/5/R01. ISSN 1361-6560. PMC 3031873. PMID 20150687.
- "The DOE Ionizing Radiation Dose Ranges Chart" (PDF). December 2017.
- ^ Seltzer, S. M.; Bartlett, D. T.; Burns, D. T.; Dietze, G.; Menzel, H.-G.; Paretzke, H. G.; Wambersie, A. (2011). "The International Commission on Radiation Units and Measurements". Journal of the ICRU. 11 (1): NP.1–NP. doi:10.1093/jicru/ndr011. ISSN 1473-6691.
- Feinendegen, L E (1 May 1990). "The cell dose concept; potential application in radiation protection". Physics in Medicine and Biology. 35 (5): 597–612. doi:10.1088/0031-9155/35/5/001. ISSN 0031-9155.
- Valentin 2007, p. 51.
- Valentin 2007, p. 65.
- Valentin 2007, p. 63-64.
- Sources and effects of ionizing radiation (PDF) (Report). Vol. 1. New York: United Nations Scientific Committee on the Effects of Atomic Radiation. 2010. p. 40. ISBN 978-92-1-142274-0.
- Hill, Robin; Mo, Zhao; Haque, Mamoon; Baldock, Clive (2009). "An evaluation of ionization chambers for the relative dosimetry of kilovoltage x-ray beams". Medical Physics. 36 (9): 3971–3981. doi:10.1118/1.3183820. ISSN 0094-2405. PMID 19810470.
- 10 CFR 20.1004. US Nuclear Regulatory Commission. 2009.
- The Council of the European Communities (21 December 1979). "Council Directive 80/181/EEC of 20 December 1979 on the approximation of the laws of the Member States relating to Unit of measurement and on the repeal of Directive 71/354/EEC". Retrieved 19 May 2012.
References
- Valentin, J, ed. (2007), The 2007 Recommendations of the International Commission on Radiological Protection, vol. 37, ISBN 978-0-7020-3048-2, ISSN 0146-6453, retrieved 11 August 2024
External links
- Ionization chamber Archived 29 October 2017 at the Wayback Machine
- – "The confusing world of radiation dosimetry" – M.A. Boyd, U.S. Environmental Protection Agency. An account of chronological differences between USA and ICRP dosimetry systems.
- Tim Stephens and Keith Pantridge, 'Dosimetry, Personal Monitoring Film' (a short article on Dosimetry from the point of view of its relation to photography, in Philosophy of Photography, volume 2, number 2, 2011, pp. 153–158.)
| Radiation protection | |
|---|---|
| Main articles | |
| Measurement quantities and units | |
| Instruments and measurement techniques | |
| Protection techniques | |
| Organisations | |
| Regulation | |
| Radiation effects | |
| See also the categories Medical physics, Radiation effects, Radioactivity, Radiobiology, and Radiation protection | |