| Revision as of 19:30, 1 November 2008 view sourceCosmic Latte (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers19,854 editsm →Biological causes: rm extra spaces← Previous edit | Revision as of 21:34, 1 November 2008 view source Cosmic Latte (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers19,854 edits →Psychological causes: +secondary sourceNext edit → | ||
| Line 51: | Line 51: | ||
| === Psychological causes=== | === Psychological causes=== | ||
| Various aspects of ] and its ] are integral in the occurrence and persistence of depression.<ref name="Sad541">{{Harvnb |Sadock|2002| p=541}}</ref> Although episodes are strongly correlated with adverse events, how a person copes with stress also plays a role.<ref name="Sad541"/> Low ], ], and self-defeating or distorted thinking are related to depression. Depression may also be connected to feelings of religious alienation |
Various aspects of ] and its ] are integral in the occurrence and persistence of depression.<ref name="Sad541">{{Harvnb |Sadock|2002| p=541}}</ref> Although episodes are strongly correlated with adverse events, how a person copes with stress also plays a role.<ref name="Sad541"/> Low ], ], and self-defeating or distorted thinking are related to depression. Depression may also be connected to feelings of religious alienation;<ref>{{cite journal |author=Exline JJ, Yali AM, Sanderson WC |title=Guilt, discord, and alienation: the role of religious strain in depression and suicidality |journal=Journal of clinical psychology |volume=56 |issue=12 |pages=1481–96 |year=2000 |month=December |pmid=11132565 |doi=10.1002/1097-4679(200012)56:12<1481::AID-1>3.0.CO;2-A}}</ref> conversely, depression is less likely to occur among those with high levels of religious involvement.<ref>{{cite journal |author=Moreira-Almeida A, Neto FL, Koenig HG |title=Religiousness and mental health: A review |journal=Revista brasileira de psiquiatria (Brazilian Journal of Psychiatry) |volume=3 |issue= |pages=242-250 |year=2006 |month=September |pmid=16924349 |doi=}}</ref> It is unclear whether these are causes or effects, but in either case depressed persons who are able to make corrections in their thinking patterns often show improved mood and self-esteem.<ref>{{cite web |author=Warman DM, ]| year=2003|month=June |url=http://www.nami.org/Template.cfm?Section=About_Treatments_and_Supports&template=/ContentManagement/ContentDisplay.cfm&ContentID=7952 |title=About treatment and supports: Cognitive behavioral therapy |work=National Alliance on Mental Illness (NAMI) website|accessdate=2008-10-17}}</ref> | ||
| ] and ] are based on the theory that depression arises from ]es and ] stemming from deficits in memory and information processing. According to psychologist ], depression in humans is similar to learned helplessness in laboratory animals, who remain in unpleasant situations when they are able to escape, but do not because they initially learned they had no control.<ref name="Helplessness">{{cite book |last=Seligman |first= Martin |title=Helplessness: On depression, development and death |publisher=WH Freeman |location=San Francisco, CA, USA |year=1975 |isbn=0716707519}}<!--NEED PAGE NUMBER--></ref> Learned helplessness and depression may be related to what psychologist ] called an external ], a tendency to attribute personal outcomes to external events seen as uncontrollable.<ref>{{cite journal|author=Benassi V, Sweeney PD, Dufour C |year=1988 |title=Is there a relation between locus of control orientation and depression? |journal=Journal of Abnormal Psychology |volume=97 |issue=3 |pages=357–67 | doi=10.1037/0021-843X.97.3.357}}</ref> A related idea, ] ], proposes that depression entails cognitive errors about oneself, one's world, and one's future.<ref name="Integrative"/><ref>{{cite paper| first = Joseph P.| last = Allen | title = An Overview of Beck's Cognitive Theory of Depression in Contemporary Literature| publisher = Personality Papers| date = 2003| url =http://www.personalityresearch.org/papers/allen.html | accessdate =2008-10-30 }}</ref> | ] and ] are based on the theory that depression arises from ]es and ] stemming from deficits in memory and information processing. According to psychologist ], depression in humans is similar to learned helplessness in laboratory animals, who remain in unpleasant situations when they are able to escape, but do not because they initially learned they had no control.<ref name="Helplessness">{{cite book |last=Seligman |first= Martin |title=Helplessness: On depression, development and death |publisher=WH Freeman |location=San Francisco, CA, USA |year=1975 |isbn=0716707519}}<!--NEED PAGE NUMBER--></ref> Learned helplessness and depression may be related to what psychologist ] called an external ], a tendency to attribute personal outcomes to external events seen as uncontrollable.<ref>{{cite journal|author=Benassi V, Sweeney PD, Dufour C |year=1988 |title=Is there a relation between locus of control orientation and depression? |journal=Journal of Abnormal Psychology |volume=97 |issue=3 |pages=357–67 | doi=10.1037/0021-843X.97.3.357}}</ref> A related idea, ] ], proposes that depression entails cognitive errors about oneself, one's world, and one's future.<ref name="Integrative"/><ref>{{cite paper| first = Joseph P.| last = Allen | title = An Overview of Beck's Cognitive Theory of Depression in Contemporary Literature| publisher = Personality Papers| date = 2003| url =http://www.personalityresearch.org/papers/allen.html | accessdate =2008-10-30 }}</ref> | ||
Revision as of 21:34, 1 November 2008
Medical condition| Major depressive disorder | |
|---|---|
| Specialty | Psychiatry |
Major depressive disorder (also known as major depression, unipolar depression, unipolar disorder, clinical depression, or simply depression) is a mental disorder characterized by a pervasive low mood and loss of interest or pleasure in usual activities. The diagnosis is made if a person has suffered one or more major depressive episodes, and is based on the patient's self-reported experiences and observed behavior. There is no laboratory test for major depression, although physicians often test for physical conditions that may cause similar symptoms before arriving at a diagnosis. The course of the disorder varies widely, from a one-off occurrence to a lifelong disorder with recurrent episodes. The most common time of onset is between the ages of 30 and 40, with a later peak between 50 and 60. Statistically, major depression occurs more often in women than men, although men are at higher risk for suicide.
Both psychological and biological causes have been proposed, and the determination of whether there are two separate conditions or a continuum of a single disorder has been researched since the 1920s. Current classification has favored biological theories since the creation of the term major depressive disorder in 1980. The neurotransmitters serotonin and norepinephrine have been implicated, and most antidepressants work to increase their active levels in the brain. However, the precise role of neurotransmitter levels in depressive illness is not fully understood. Psychological factors have also been implicated, and forms of psychotherapy are used to address them. Hospitalization may be necessary in cases associated with self-neglect or a significant risk of suicide, and electroconvulsive therapy is used in severe cases.
Ideas about what causes and constitutes depression have evolved over the centuries, and they remain a source of discussion. The term depression is commonly used to describe a temporary depressed or sad mood. By contrast, major depression is a serious and often disabling condition that can significantly affect a person's work, family and school life, sleeping and eating habits, and general health. However, authorities such as Australian psychiatrist Gordon Parker have argued that it is overdiagnosed, and that current diagnostic standards have the effect of medicalizing sadness.
In Western countries, approximately 3.4% of people with major depression eventually commit suicide. Up to 60% of all people who commit suicide have depression or another mood disorder, and their risk may be higher if they feel a marked sense of hopelessness or have both depression and borderline personality disorder. Depressed individuals have a shortened life expectancy, being more susceptible to conditions such as heart disease than the non-depressed.
Signs and symptoms
Major depression is a serious condition that affects a person's work, family and school life, sleeping and eating habits, and general health. The impact on functioning and well-being has been equated to that of chronic medical conditions such as congestive heart failure.
A person suffering a major depressive episode usually experiences a pervasive low mood, or loss of interest or pleasure in favored activities. Depressed people may be preoccupied with feelings of worthlessness, inappropriate guilt or regret, helplessness or hopelessness. Other symptoms include poor concentration and memory, withdrawal from social situations and activities, reduced libido (sex drive), and thoughts of death or suicide. Insomnia is common: in the typical pattern, a person wakes very early and is unable to get back to sleep. Hypersomnia, or oversleeping, is less common. Appetite often decreases, with resulting weight loss, although increased appetite and weight gain occasionally occur. The person may report persistent physical symptoms such as fatigue, headaches, digestive problems, or chronic pain; this is a typical presentation in developing countries. Family and friends may perceive that the person is either agitated or slowed down. Older people with major depression are more likely than younger people to show cognitive symptoms such as forgetfulness and to show a more noticeable slowing of movements. In severe cases, depressed people may experience psychotic symptoms such as delusions or, less commonly, hallucinations, usually of an unpleasant nature.
Children may display an irritable rather than depressed mood, and show different symptoms depending on age and situation. Most exhibit a loss of interest in school and a decline in academic performance. Children with depression may be described as clingy, demanding, dependent, or insecure. Those older than 12 years may begin abusing drugs or alcohol, or exhibit disruptive behavior. Diagnosis may be delayed or missed when symptoms are interpreted as normal moodiness.
Causes
In the biopsychosocial model, both biological and psychological (including social) factors play a role in causing depression. There is overlap, and the precise causes vary depending on individual circumstances. The heritability of depression—the degree to which it is genetically determined—has been estimated to be approximately 40% for women and 30% for men. From the evolutionary standpoint, major depression might be expected to reduce an individual's reproductive fitness. Some evolutionary explanations for the apparent contradiction between biopsychosocial, psychological and psychosocial hypotheses and the high heritability and prevalence of major depression are explained by the proposal that certain components of depression are adaptations.
Biological causes
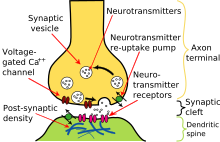
Main article: Biology of depressionMost antidepressants increase synaptic levels of the monoamine neurotransmitter serotonin. Some also enhance the levels of two other neurotransmitters, norepinephrine and dopamine. This observation gave rise to the monoamine theory of depression. In its contemporary formulation, the monoamine theory postulates that a deficiency of certain neurotransmitters is responsible for the corresponding features of depression: "Norepinephrine may be related to alertness and energy as well as anxiety, attention, and interest in life; serotonin to anxiety, obsessions, and compulsions; and dopamine to attention, motivation, pleasure, and reward, as well as interest in life." The proponents of this theory recommend choosing the antidepressant with the mechanism of action impacting the most prominent symptoms. Anxious and irritable patients should be treated with SSRIs or norepinephrine reuptake inhibitors, and those experiencing a loss of energy and enjoyment of life with norepinephrine and dopamine enhancing drugs.
Consistent with the monoamine theory, a longitudinal study uncovered a moderating effect of the serotonin transporter (5-HTT) gene on stressful life events in predicting depression. Specifically, depression seems especially likely to follow such events, but even more so in people with one or two short alleles of the 5-HTT gene. Serotonin is thought to help regulate other neurotransmitter systems, and decreased serotonin activity may allow these systems to act in unusual and erratic ways. Facets of depression may be emergent properties of this dysregulation.
In the past two decades, research has uncovered multiple limitations of the monoamine theory, and its inadequacy has been criticized within the psychiatric community. Intensive investigation has failed to find convincing evidence of a primary dysfunction of a specific monoamine system in patients with major depressive disorders. Antidepressants that do not act through the monoamine system, such as tianeptine and opipramol, have been known about for a long time. Experiments with pharmacological agents that cause depletion of monoamines have shown that this depletion does not cause depression in healthy people nor does it worsen symptoms in depressed patients. Already limited, the monoamine theory has been further oversimplified when presented to the general public.
MRI scans of patients with major depressive disorder have reported a number of differences in brain structure compared to those without the illness. Although there is some inconsistency in the results, meta-analyses have shown there is strong evidence for smaller hippocampal volumes and increased rates of hyperintensities in depressed patients. Hyperintensities have been associated with patients with a late age of onset have led to the development of the theory of vascular depression.
There may be a link between depression and neurogenesis of the hippocampus, a center for both mood and memory. Loss of hippocampal neurons is found in some depressed individuals and correlates with impaired memory and dysthymic mood. Drugs may increase serotonin levels in the brain, stimulating neurogenesis and thus increasing the total mass of the hippocampus. This increase may help to restore mood and memory. Similar relationships have been observed between depression and an area of the anterior cingulate cortex implicated in the modulation of emotional behavior. One of the neurotrophins responsible for neurogenesis is the brain-derived neurotrophic factor (BDNF). The level of BDNF in the blood plasma of depressed subjects is drastically reduced (more than threefold) as compared to the norm. Antidepressant treatment increases the blood level of BDNF. Although decreased plasma BDNF levels have been found in many other disorders, there is some evidence that BDNF is involved in the cause of depression and the mechanism of action of antidepressants.
Depression may also be caused in part by an overactive hypothalamic-pituitary-adrenal axis (HPA axis) that is similar to the neuro-endocrine response to stress. These HPA axis abnormalities participate in the development of depressive symptoms, and antidepressants serve to regulate HPA axis function.
Depression may be affected by variations in the circadian rhythm. The REM stage of sleep, in which dreaming occurs, tends to be especially quick to arrive, and especially intense, in depressed people. Although the precise relationship between sleep and depression is mysterious, the relationship appears to be particularly strong among those whose depressive episodes are not precipitated by unusual stress. In such cases, patients may be especially unaffected by therapeutic intervention.
Psychological causes
Various aspects of personality and its development are integral in the occurrence and persistence of depression. Although episodes are strongly correlated with adverse events, how a person copes with stress also plays a role. Low self-esteem, learned helplessness, and self-defeating or distorted thinking are related to depression. Depression may also be connected to feelings of religious alienation; conversely, depression is less likely to occur among those with high levels of religious involvement. It is unclear whether these are causes or effects, but in either case depressed persons who are able to make corrections in their thinking patterns often show improved mood and self-esteem.
Cognitive psychology and cognitive behavioral therapy are based on the theory that depression arises from cognitive biases and distortions stemming from deficits in memory and information processing. According to psychologist Martin Seligman, depression in humans is similar to learned helplessness in laboratory animals, who remain in unpleasant situations when they are able to escape, but do not because they initially learned they had no control. Learned helplessness and depression may be related to what psychologist Julian Rotter called an external locus of control, a tendency to attribute personal outcomes to external events seen as uncontrollable. A related idea, Aaron T. Beck's cognitive triad, proposes that depression entails cognitive errors about oneself, one's world, and one's future.
On the other hand, depressed individuals often blame themselves for negative events. According to one study, depressed adolescents, while feeling responsible for negative events, do not take credit for positive outcomes. This tendency is characteristic of a depressive attributional, or pessimistic explanatory style. According to psychologist Albert Bandura, depressed individuals have a negative self-concept and lack a sense of self-efficacy; in other words they do not believe they can influence events or achieve personal goals. Milder depression has been associated with what has been called depressive realism, or the "sadder-but-wiser" effect, a view of the world that is relatively undistorted by positive biases, or a more accurate assessment of their own abilities.
A large body of research has documented the importance of interpersonal factors, including strained or critical personal relationships, in the onset of depressive symptoms and major depression in young and middle-aged adults. Vulnerability factors—such as early maternal loss, lack of a confiding relationship, responsibility for the care of several young children at home, and unemployment—can interact with life stressors to increase the risk of depression. For older adults, the factors are often health problems, changes in relationships with a spouse or adult children due to the transition to a care-giving or care-needing role, the death of a significant other, or a change in the availability or quality of social relationships with older friends because of their own health-related life changes.
From the psychoanalytic perspective, depression may be intertwined with self-criticism. Sigmund Freud, the father of psychoanalysis, wrote that the "super-ego becomes over-severe, abuses the poor ego, humiliates it and ill-treats it, threatens it with the direst punishments". He theorized that objective loss, such as the loss of a valued relationship through death or a romantic break-up, results in subjective loss as well; the depressed individual has identified with the object of affection through an unconscious, narcissistic process called the libidinal cathexis of the ego. Such loss results in "a profoundly painful dejection, cessation of interest in the outside world, loss of the capacity to love, inhibition of all activity, and a lowering of self-regarding feelings" that is more severe than mourning. "In mourning 'it is the world that has become poor and empty; in it is the ego itself.'"
Existential psychologist Rollo May stated that "depression is the inability to construct a future". From the existential perspective, in order to construct a future, individuals must be acutely aware of both their mortality and their freedom to act, and they must exercise their freedom within the explicit framework of an acute awareness of their mortality. This awareness produces "normal" anxiety, whereas the lack of awareness leads to neurotic anxiety, self-alienation, inauthentic living, guilt, and depression. Humanistic psychologists agree with many facets of existentialism, but argue that depression can result from an incongruity between society and the individual's innate drive to self-actualize. The father of humanistic psychology, Abraham Maslow, believed that depression is especially likely to arise when the world precludes a sense of "richness" or "totality" for the self-actualizer.
Evolutionary psychology suggests that major depression can result from overactivation of psychological mechanisms that evolved to produce adaptive responses to material or social loss or defeat. Some aspects of this approach have received empirical support and clinical application; other components are still at a hypothetical stage.
Social causes
Long-term risks for developing major depression include family disruption and low socioeconomic status in early childhood. The risk is independent of later adult social status and is related to various social inequalities. Childhood emotional, physical, sexual abuse, or neglect are also associated with increased risk of developing depressive disorders later in life. Such events are more likely to occur in dysfunctional families, for example, one with an alcoholic parent. Early adverse events and stressful conditions that persist through childhood and adolescence may be linked to the later development of depression. Social rejection also predicts later depression, and adolescents who are victimized by peers are more vulnerable to developing depressive symptoms if it impacts on the development of their identity, although family cohesion and emotional involvement are protective factors.
In adulthood, a correlation between stressful life events and the onset of major depressive episodes has been found consistently and is likely causal, although the specific mechanisms are unclear. Negative events such as assault, divorce or separation, legal issues, major problems with work, finances, housing, health, or friends and confidants, have been found to precede episodes if they represent a long-term threat, particularly if the threat is of a loss or humiliation that devalues an individual in a core role. The first episode of major depressive is more likely to be immediately preceded by stressful life events than are recurrent ones. Social isolation has also been found to predict onset of a first episode. There is evidence that neighborhood social disorder, for example, due to crime or illicit drugs, is a risk factor, and that a high neighborhood socioeconomic status, with better amenities, is a protective factor. There is some evidence of risk from psychosocial stressors in the workplace, such as working at a job that is demanding but involves little opportunity for decision-making. There is mixed evidence regarding the role of social capital (features of social organization including interpersonal trust, civic engagement and cooperation for mutual benefit).
Diagnosis
Clinical assessment
A diagnostic assessment may be conducted by a general practitioner or by a psychiatrist or psychologist. This includes a complete history of the person's current circumstances, biographical history and current symptoms, a discussion of alcohol and drug use, and a family medical history to see if other family members have suffered from a mood disorder. A mental state examination includes an assessment of the person's current mood and an exploration of thought content, in particular thoughts of hopelessness, self-harm or suicide.
Before diagnosing a major depressive disorder, a doctor generally performs a medical examination and selected investigations to rule out other causes of symptoms. These include blood tests measuring TSH to exclude hypo- or hyperthyroidism; basic electrolytes and serum calcium to rule out a metabolic disturbance; and a full blood count including ESR to rule out a systemic infection or chronic disease. Testosterone levels may be used to diagnose hypogonadism, a cause of depression in men. Subjective cognitive complaints appear in older depressed people, but they can also be indicative of the onset of a dementing disorder, such as Alzheimer's disease. Depression is also a common initial symptom of dementia. Conducted in older depressed people, screening tests such as the mini-mental state examination, or a more complete neuropsychological evaluation, can rule out cognitive impairment. A CT scan can exclude brain pathology in those with psychotic, rapid-onset or otherwise unusual symptoms. No biological tests confirm major depression. Investigations are not generally repeated for a subsequent episode unless there is a specific medical indication, in which case serum sodium can rule out hyponatremia (low sodium) if the person presents with increased frequency of passing urine, a common side-effect of selective serotonin reuptake inhibitor (SSRI) antidepressants.
Specialist mental health services are rare in rural areas, and thus diagnosis and management is largely left to primary care clinicians. This issue is even more marked in developing countries.
Rating scales
Diagnostic screening programs have been advocated to improve detection of depression, but there is evidence that the use of screening instruments does little to improve detection rates. A study in the U.K. concluded that screening alone is costly and does not improve the treatment or outcome of depression.
Several rating scales are used in research or as screening tools. The Beck Depression Inventory is a widely used tool in the diagnosis of depression, although its main purpose is not diagnosis, but determining the presence and severity of symptoms. Originally designed by psychiatrist Aaron T. Beck in 1961, it is a 21-question self-report inventory that covers symptoms such as irritability, fatigue, weight loss, lack of interest in sex and thoughts including feelings of guilt, hopelessness or of being punished. Other scales include the Geriatric Depression Scale in older populations, which is also valid in patients with mild to moderate dementia; the Hamilton Depression Rating Scale (HRSD-21) designed by psychiatrist Max Hamilton in 1960; and the Montgomery-Åsberg Depression Rating Scale (MADRS). The Patient Health Questionnaires are two self-administered questionnaires for use in primary care. The PHQ-2 has two screening questions about the frequency of depressed mood and a loss of interest in activities; a positive to either question indicates further testing is required. The PHQ-9 is a slightly more detailed nine-question survey for assessing symptoms of major depressive disorder in greater detail, and is often used to follow up a positive PHQ-2 test.
DSM IV-TR and ICD-10 criteria
The most widely used criteria for diagnosing depressive conditions are found in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD-10). The latter system is typically used in European countries, while the former is used in the USA and many other non-European nations.
Major depressive disorder is classified as a mood disorder in DSM IV-TR. The diagnosis hinges on the presence of a single or recurrent major depressive episode. Further qualifiers are used to classify both the episode itself and the course of the disorder. The category Depressive Disorder Not Otherwise Specified is diagnosed if the depressive episode's manifestation does not meet the criteria for a major depressive episode. The ICD-10 system does not use the term Major depressive disorder, but lists similar criteria for the diagnosis of a Depressive episode (mild, moderate or severe); the term recurrent may be added if there have been multiple episodes without mania.
Major depressive episode
Main article: Major depressive episodeA major depressive episode is characterized by the presence of a severely depressed mood that persists for at least two weeks. Episodes may be isolated or recurrent and are categorized as mild (few symptoms in excess of minimum criteria), moderate, or severe (marked impact on social or occupational functioning). An episode with psychotic features—commonly referred to as psychotic depression—is automatically rated as severe. If the patient has had an episode of mania or markedly elevated mood, a diagnosis of bipolar disorder is made instead. Depression without mania is sometimes referred to as unipolar because the mood remains at one emotional state or "pole".
The DSM excludes cases where the symptoms are a result of bereavement, although it is possible for normal bereavement to evolve into a depressive episode if the mood persists and the characteristic features of a major depressive episode develop. The criteria have been criticized because they do not take into account any other aspects of the personal and social context in which depression can occur. In addition, some studies have found little empirical support for the DSM-IV cut-off criteria, indicating they are a diagnostic convention imposed on a continuum of depressive symptoms of varying severity and duration: excluded are a range of related diagnoses, including dysthymia which involves a chronic but milder mood disturbance, Recurrent brief depression which involves briefer depressive episodes, Minor depressive disorder which involves only some of the symptoms of major depression, and Adjustment disorder with depressed mood which involves low mood resulting from a psychological response to an identifiable event or stressor.
Subtypes
Diagnosticians recognize several subtypes, which are sometimes called "course specifiers":
- Melancholic depression is characterized by a loss of pleasure in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early morning waking, psychomotor retardation, excessive weight loss (not to be confused with anorexia nervosa), or excessive guilt.
- Atypical depression is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite (comfort eating), excessive sleep or sleepiness (hypersomnia), a sensation of heaviness in limbs known as leaden paralysis, and significant social impairment as a consequence of hypersensitivity to perceived interpersonal rejection.
- Catatonic depression is a rare and severe form of major depression involving disturbances of motor behavior and other symptoms. Here the person is mute and almost stuporose, and either remains immobile or exhibits purposeless or even bizarre movements. Catatonic symptoms also occur in schizophrenia or in manic episodes, or may be caused by neuroleptic malignant syndrome.
- Postpartum depression refers to the intense, sustained and sometimes disabling depression experienced by women after giving birth. Postpartum depression, which has incidence rate of 10–15% among new mothers, typically sets in within three months of labor, and lasts as long as three months.
- Seasonal affective disorder is a form of depression in which depressive episodes come on in the autumn or winter, and resolve in spring. The diagnosis is made if at least two episodes have occurred in colder months with none at other times, over a two-year period or longer.
Differential diagnoses
In order to diagnose MDD, several other potential diagnoses must be ruled out, including the following:
- Dysthymia is a chronic, milder mood disturbance in which a person reports a low mood almost daily over a span of at least two years. The symptoms are not as severe as those for major depression, although people with dysthymia are vulnerable to secondary episodes of major depression (sometimes referred to as double depression).
- Adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode.
- Bipolar disorder, previously known as manic-depressive disorder, is a condition in which depressive phases alternate with periods of mania or hypomania. Although depression is currently categorized as a separate disorder, there is ongoing debate because individuals diagnosed with major depression often experience some hypomanic symptoms, indicating a mood disorder continuum.
- Loneliness and depression have enough features in common that loneliness may be viewed as a differential diagnosis. In general, depression is likely to coexist with loneliness if the loneliness is chronic rather than transient. If the individual has global concerns that do not focus strictly on interpersonal relationships, feels a high degree of guilt, or is particularly vegetative, then the person is likely to be depressed; if these conditions are not met, he or she may be lonely instead.
Treatment
For a fuller discussion of standard, rarer and more experimental treatments, see Treatment for depression.The three most common treatments for depression are psychotherapy, medication, and electroconvulsive therapy. Psychotherapy is the treatment of choice for people under 18, while electroconvulsive therapy is only used as a last resort. Care is usually given on an outpatient basis, while treatment in an inpatient unit is considered if there is a significant risk to self or others.
Treatment options are much more limited in developing countries, where access to mental health staff, medication, and psychotherapy are often difficult. Development of mental health services is minimal in many countries; depression is viewed as a phenomenon of the developed world despite evidence to the contrary, and not as an inherently life-threatening condition.
Psychotherapy
Main article: PsychotherapyPsychotherapy can be delivered, to individuals or groups, by a variety of mental health professionals, including psychotherapists, psychiatrists, psychologists, clinical social workers, counselors, and psychiatric nurses. With more complex and chronic forms of depression the most effective treatment is often considered to be a combination of medication and psychotherapy. In people under 18, medication is usually offered only in conjunction with psychotherapy, not as a first line treatment.
The most studied form of psychotherapy for depression is cognitive behavioral therapy (CBT), thought to work by teaching clients to learn a set of useful cognitive and behavioral skills. Earlier research suggested that cognitive-behavioral therapy was not as effective as antidepressant medication; however, more recent research suggests that it can perform as well as antidepressants in patients with moderate to severe depression. Overall, systematic review reveals CBT to be an effective treatment in depressed adolescents, although possibly not for severe episodes. Combining fluoxetine with CBT appeared to bring no additional benefit or, at the most, only marginal benefit.
Two randomized, controlled trials of mindfulness-based cognitive therapy (MBCT), which includes elements of meditation, have been reviewed. MBCT was significantly more effective than usual care for the prevention of recurrent depression in patients who had had three or more depressive episodes. According to the review, the usual care did not include antidepressant treatment or any psychotherapy, and the improvement observed may have reflected the non-specific or placebo effects.
Interpersonal psychotherapy focuses on the social and interpersonal triggers that may cause depression. There is evidence that it is an effective treatment. Here, the therapy takes a structured course with a set number of weekly sessions (often 12) as in the case of CBT, however the focus is on relationships with others. Therapy can be used to help a person develop or improve interpersonal skills in order to allow him or her to communicate more effectively and reduce stress.
Psychoanalysis, a school of thought founded by Sigmund Freud that emphasizes the resolution of unconscious mental conflicts, is used by its practitioners to treat clients presenting with major depression. A more widely practiced, eclectic technique, called psychodynamic psychotherapy, is loosely based on psychoanalysis and has an additional social and interpersonal focus. In a meta-analysis of three controlled trials, Short Psychodynamic Supportive Psychotherapy (SPSP) was found to be as effective as medication for mild to moderate depression.
Medication
Main article: AntidepressantSelective serotonin reuptake inhibitors (SSRIs), such as sertraline (Zoloft), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine, and citalopram are the primary medications considered, due to their relatively mild side effects and broad effect on the symptoms of depression and anxiety. Those who do not respond to the one SSRI can be switched to another; such a switch results in improvement in almost 50% of cases. Another popular option is to switch to the atypical antidepressant bupropion (Wellbutrin) or to add bupropion to the existing therapy; this strategy is possibly more effective. It is not uncommon for SSRIs to cause or worsen insomnia; the sedating antidepressant mirtazapine (Zispin, Remeron) can be used in such cases. Venlafaxine (Effexor), and other serotonin-norepinephrine reuptake inhibitors, may be modestly more effective than SSRIs; however, Venlafaxine is not recommended as a first-line treatment because of evidence suggesting its risks may outweigh benefits. Its use is specifically discouraged in children and adolescents. Fluoxetine is the only antidepressant recommended for people under the age of 18.

Tricyclic antidepressants have more side effects than SSRIs and are usually reserved for the treatment of inpatients, for whom the tricyclic antidepressant amitriptyline, in particular, appears to be more effective. A different class of antidepressants, the monoamine oxidase inhibitors, have historically been plagued by questionable efficacy and life-threatening adverse effects. They are still used only rarely, although newer agents of this class, with a better side effect profile, have been developed.
To find the most effective treatment, the dosages of antidepressants must often be adjusted, or different medications and combinations tried. Response rates to the first agent administered may be as low as 50%. It may take anywhere from three to eight weeks after the start of medication before the therapeutic effects are fully revealed. Patients are advised not to stop taking an antidepressant suddenly and to continue its use for at least four months to prevent the chance of recurrence. People with chronic depression usually need to take medication for the rest of their lives. The term refractory- or treatment-resistant depression is used to describe cases that do not respond to adequate courses of least two antidepressants.
A doctor may add a medication with a different mode of action to bolster the effect of an antidepressant in cases of treatment resistance. Lithium has been used to augment antidepressant therapy in those who have failed to respond to antidepressants alone. Furthermore, lithium dramatically decreases the suicide risk in recurrent depression. Addition of a thyroid hormone, triiodothyronine may work as well as lithium, even in patients with normal thyroid function. Addition of atypical antipsychotics when the patient has not responded to an antidepressant is also known to increase the effectiveness of antidepressant drugs, albeit at the cost of more frequent side effects.
Efficacy of medication and psychotherapy
Two recent meta-analyses of clinical trial results submitted to the U.S. Food and Drug Administration (FDA) concluded that antidepressants are statistically superior to placebo but their overall effect is low to moderate; they often did not exceed the National Institute for Health and Clinical Excellence criteria for a clinically significant effect. In particular, the effect size was very small for moderate depression although did increase with severity and reach clinical significance for very severe depression. These results were consistent with the earlier clinical studies in which only patients with severe depression benefited from either psychotherapy or treatment with an antidepressant, imipramine, more than from the placebo treatment. Despite obtaining similar results, the authors argued about their interpretation. One author concluded that there "seems little evidence to support the prescription of antidepressant medication to any but the most severely depressed patients, unless alternative treatments have failed to provide benefit". The other author agreed that the "antidepressant 'glass' is far from full" but disagreed "that it is completely empty". He pointed out that the first-line alternative to medication is psychotherapy, which does not have superior efficacy.
Antidepressants in general are as effective as psychotherapy for major depression, and this conclusion holds true for both severe and mild forms of MDD. In contrast, medication gives better results for dysthymia. The subgroup of SSRIs may be slightly more efficacious than psychotherapy. On the other hand, significantly more patients drop off from the antidepressant treatment than from psychotherapy, likely because of the side effects of antidepressants. Successful psychotherapy appears to prevent the recurrence of depression even after it has been terminated or replaced by occasional booster sessions. The same degree of prevention can be achieved by continuing antidepressant treatment.
Electroconvulsive therapy
Main article: Electroconvulsive therapyElectroconvulsive therapy (ECT) is a procedure in which seizures are electrically induced in anesthetized patients. ECT is most often used as a last resort treatment by hospital psychiatrists for severe major depression which has not responded to trials of antidepressant or, less often, psychotherapy or supportive interventions. It has a quicker effect than antidepressant therapy, and thus may be the treatment of choice in emergencies such as catatonic depression where the patient has ceased oral intake of fluid or nutrients, or where there is severe suicidality. Some evidence suggests it is the most effective treatment for depression in the short-term and one study without a comparison group or assessment of additional treatments given, suggested remission is related to improved self-rated quality of life in both the short-term (correlated with the degree of amnesia) and after six months. However, ECT has been found to have much lower remission rates in real-world practice and on its own does not have a sustained benefit as nearly everyone relapses. The relapse rate in the first six months may be reduced by the use of psychiatric medications or further ECT (although some authorities, such as NICE, do not recommend the latter), but remains high. Common initial adverse effects include short-term memory loss, disorientation, headache; long-term memory and other cognitive deficits may persist. According to the American Psychiatric Association and the National Institute for Health and Clinical Excellence, available evidence suggests that the procedure, when administered according to their standards and without complications, does not cause brain damage in adults.
Other methods of treatment
Two products, St John's wort and S-Adenosyl methionine, are available as prescription antidepressants in several European countries, but in the US are classified as herbal supplements and sold over-the-counter. There is inconsistent evidence on the effect of St John's wort extract on major depression. The pharmaceutical quality of the extract has an effect on the safety and efficacy for the treatment of any type of depression. Clinical trials of S-Adenosyl methionine (SAM-e) have shown that it is equivalent to tricyclic antidepressants in effectiveness, although the safety and efficacy of over-the-counter versions is unknown. Other supplements such as omega-3 fatty acids, tryptophan, and 5-hydroxytryptophan (5-HTP), have shown no effect beyond those of placebo.

Repetitive transcranial magnetic stimulation (rTMS) utilizes powerful magnetic fields which applied to the brain from outside the head. Multiple controlled studies support the use of this method in treatment-resistant depression; it has been approved for this indication in Europe, Canada and Australia, but not in the US. It was inferior to ECT in a side-by-side randomized trial.
Other therapeutic approaches have been used to treat depression. Bright light therapy has been found to be an effective treatment for the winter depression produced by seasonal affective disorder. There has been some conflicting evidence as to its effectiveness for non-seasonal depression. Exercise has not been shown to reduce the symptoms of depression.
Prognosis
Major depressive episodes often resolve over time whether they are treated or not. Outpatients on a waiting list show a 10–15% reduction in symptoms over a few months, and around 20% will no longer meet full criteria. The median duration of an episode has been estimated at least 23 weeks, with the highest rate of recovery in the first three months.
General population studies indicate around half those who have a major depressive episode (whether treated or not) recover and remain well, while 35% will have at least one more, and around 15% experience chronic recurrence. Studies recruiting from selective inpatient sources suggest lower recovery and higher chronicity, while studies of mostly outpatients show that nearly all recover, with a median episode duration of 11 months. Around 90% of those with severe or psychotic depression, most of whom also meet criteria for other mental disorders, experience recurrence.
Recurrence is more likely if symptoms have not fully resolved with treatment. Current guidelines recommend continuing antidepressants for four to six months after remission to prevent relapse. Evidence from many randomized controlled trials indicates continuing antidepressant medications after recovery can reduce the chance of relapse by 70% (41% on placebo vs. 18% on antidepressant). The preventive effect probably lasts for at least the first 36 months of use. Thus, depression recurs despite the prolonged antidepressant treatment in a significant minority of patients; the reason for recurrence in these cases is poorly understood and could be a "true pharmacologic failure or a worsening of the disease, a relapse that overrides medication". Because of the difficulties of carrying out controlled clinical trials of longer duration, the approval of most antidepressants for the prevention of recurrence is based on trials that lasted up to a year.
Epidemiology
Depression is a major cause of morbidity worldwide. Lifetime prevalence varies widely, from 3% in Japan to 17% in the US. In most countries the number of people who would suffer from depression during their lives falls within an 8–12% range. In North America the probability of having a major depressive episode within a year-long period is 3–5% for males and 8–10% for females. Population studies have consistently shown major depression to be more common in women, although it is unclear why this is so, and whether factors unaccounted for are contributing to this. People are most likely to suffer their first depressive episode between the ages of 30 and 40, and there is a second, smaller peak of incidence between ages 50 and 60. The risk of major depression is increased in the first year after childbirth (postpartum depression), and after cardiovascular and neurological illnesses such as stroke, Parkinson's disease, and multiple sclerosis. Depressive episodes following a heart attack might even correspond with an increased risk of further cardiac complications, including death.

Depression is often associated with unemployment and poverty. A 2007 study that compared epidemiological factors in Canada and the US found the rate of major depression to be twice as high for Americans without medical insurance than either for Americans with insurance or for Canadians—for whom health care is publicly funded—in general. Major depression is currently the leading cause of disease burden in North America and other high-income countries, and the fourth leading cause worldwide. In the year 2030, it is predicted to be the second leading cause of disease burden worldwide after HIV, according to the World Health Organization.
Up to 60% of people who commit suicide have a mood disorder such as major depression, and the risk is especially high if a person has a marked sense of hopelessness or has both depression and borderline personality disorder. Depressed people also have a higher rate of dying from other causes. The suicide rate in major depression has often been quoted as 15% but this was taken from a review of studies of hospitalized patients, who were the most severely depressed. A broader reexamination has indicated an approximate figure of 3.4%, with differing rates of around 7% for men and 1% for women.
Comorbidity
Major depression frequently co-occurs with other psychiatric problems. The National Comorbidity Survey (US) reports that 58% of those with major depression also suffer from lifetime anxiety. Even mild anxiety symptoms can have a major impact on the course of a depressive illness, and the commingling of any anxiety symptoms with the primary depression is important to consider. Psychiatrist Ellen Frank found that depressed patients with lifetime panic symptoms experienced significant delays in their remission, and had higher levels of residual impairment. Robert Sapolsky similarly argues that the relationship between stress, anxiety, and depression could be measured and demonstrated biologically. There are increased rates of alcohol and drug abuse and particularly dependence, and around a third of individuals diagnosed with attention-deficit hyperactivity disorder develop comorbid depression. Post-traumatic stress disorder and depression often co-occur, and both can result from childhood trauma.
History
See also: History of mental disorders and Classification of mental disordersPrehistory to medieval periods

Notes in the Ancient Egyptian document known as the Ebers papyrus appear to refer to emotional distress of the heart or mind, which has been interpreted as sadness or depression. Passages of the Hebrew Bible (Old Testament), composed and compiled between the 12th and 2nd centuries BC, have been interpreted as describing mood disorders in figures such as Job, King Saul and in the psalms of David.
In Ancient Greece, disease was thought due to an imbalance in the four basic bodily fluids, or humors. Personality types were similarly thought to be determined by the dominant humor in a particular person. Derived from the Ancient Greek melas, "black", and kholé, "bile", melancholia was described as a distinct disease with particular mental and physical symptoms by Hippocrates in his Aphorisms, where he characterized all "fears and despondencies, if they last a long time" as being symptomatic of the ailment. Aretaeus of Cappadocia later noted that sufferers were "dull or stern; dejected or unreasonably torpid, without any manifest cause". The humoral theory fell out of favor but was revived in Rome by Galen. Melancholia was a far broader concept than today's depression; prominence was given to a clustering of the symptoms of sadness, dejection, and despondency, and often fear, anger, delusions and obsessions were included.
Influenced by Greek and Roman texts, physicians in the Persian and then the Muslim empire developed ideas about melancholia during the Islamic Golden Age. Ishaq ibn Imran (d. 908) combined the concepts of melancholia and phrenitis. Avicenna described melancholia as a depressive type of mood disorder in which the person may become suspicious and develop certain types of phobias. His work, the Canon of Medicine, became the standard of medical thinking in Europe alongside those of Hippocrates and Galen. Moral and spiritual theories also prevailed, and in Christian settings a malaise called acedia (sloth or absence of caring) was identified, involving low spirits and lethargy typically linked to isolation.
17th to 19th centuries
The seminal scholarly work of the 17th century was Robert Burton's The Anatomy of Melancholy, drawing on numerous theories and the author's own experiences. Burton suggested that melancholy could be combated with a healthy diet, sufficient sleep, music, and "meaningful work", along with talking about the problem with a friend. During the 18th century, the humoral theory of melancholia was increasingly challenged by mechanical and electrical explanations; references to dark and gloomy states gave way to ideas of slowed circulation and depleted energy. The German physician Johann Christian Heinroth, however, argued melancholia was a disturbance of the soul due to moral conflict within the patient. Eventually, various authors proposed up to 30 different subtypes of melancholia, and alternative terms were suggested and discarded. Hypochondria came to be seen as a separate disorder. Melancholia and Melancholy had been used interchangeably until the 19th century, but the former came to refer to a pathological condition and the latter to a temperament.
The term depression was derived from the Latin verb deprimere, "to press down". From the 14th century, "to depress" meant to subjugate or to bring down in spirits. It was used in 1665 in Richard Baker's Chronicle to refer to someone having "a great depression of spirit", and by Samuel Johnson in a similar sense in 1753. The term also came in to use in physiology and economics. An early usage referring to a psychiatric symptom was by Louis Delasiauve in 1856, and by the 1860s it was appearing in medical dictionaries to refer to a physiological and metaphorical lowering of emotional function. Since Aristotle, melancholia had been associated with men of learning and intellectual brilliance, a hazard of contemplation and creativity. The newer concept abandoned these associations and, through the 19th century, became more associated with women.
Although melancholia remained the dominant diagnostic term, depression gained increasing currency in medical treatises and was a synonym by the end of the century; the German psychiatrist Emil Kraepelin may have been the first to use it as the overarching term, referring to different kinds of melancholia as depressive states. English psychiatrist Henry Maudsley proposed an overarching category of affective disorder.
20th century to the present day
The influential system put forward by Kraepelin unified nearly all types of mood disorder into manic–depressive insanity, with a separate category of dementia praecox (now known as schizophrenia). Kraepelin worked from an assumption of underlying brain pathology, but also promoted a distinction between endogenous (internally caused) and exogenous (externally caused) types. Kurt Schneider coined the terms endogenous depression and reactive depression in 1920, the latter referring to reactivity in mood and not reaction to outside events, and therefore frequently misinterpreted. The division was challenged in 1926 by British psychiatrist Edward Mapother who found no clear distinction between the types. The unitarian view became more popular in the United Kingdom, while the binary view held sway in the US, influenced by the work of Adolf Meyer and before him Sigmund Freud.
Freud had emphasized early life experiences and conflicting psychological drives; he associated melancholia with psychological loss and self-criticism. Meyer put forward a mixed social and biological framework emphasizing reactions in the context of an individual's life, and argued that the term depression should be used instead of melancholia. The DSM-I (1952) contained depressive reaction and the DSM-II (1968) depressive neurosis, defined as an excessive reaction to internal conflict or an identifiable event, and also included a depressive type of manic-depressive psychosis within Major affective disorders.
The depressive reaction of the 1950s was distinguished from endogenous depression, purportedly a rare biological condition, which borrowed as a synonym the longstanding term, melancholic. Debate has persisted for most of the twentieth century over whether a unitary or binary model of depression is a truer reflection of the syndrome; in the former, there is a continuum of depression ranked only by severity and the result of a "psychobiological final common pathway", whereas the latter conceptualizes a distinction between biological and reactive depressive syndromes. The publishing of DSM-III saw the unitarian model gain a more universal acceptance.
In the mid-20th century, researchers theorized that depression was caused by a chemical imbalance in transmitters in the brain, a theory based on observations made in the 1950s of the effects of reserpine and isoniazid in altering monoamine neurotransmitter levels and affecting depressive symptoms. During the 1960s and 70s, manic-depression came to refer to just one type of mood disorder (now most commonly known as bipolar disorder) which was distinguished from (unipolar) depression. The terms unipolar and bipolar had been coined by Karl Kleist.
The term Major depressive disorder was introduced by a group of US psychiatrists in the mid-1970s as part of proposals for diagnostic criteria based on patterns of symptoms (called the "Research Diagnostic Criteria", building on earlier Feighner Criteria), and was incorporated in to the DSM-III in 1980. To maintain consistency the ICD-10 used the same criteria, with only minor alterations, but using the DSM diagnostic threshold to mark a mild depressive episode, adding higher threshold categories for moderate and severe episodes. The ancient idea of melancholia still survives in the notion of a melancholic subtype.
The new definitions of depression were widely accepted, albeit with some conflicting findings and views. There have been some continued empirical arguments for a return to the diagnosis of melancholia. There has been some criticism of the expansion of coverage of the diagnosis, related to the development and promotion of antidepressants and the biological model since the late 1950s.
Sociocultural aspects
See also: List of people with depression
Even today, people's conceptualizations of depression vary widely, both within and among cultures. "Because of the lack of scientific certainty," one commentator has observed, "the debate over depression turns on questions of language. What we call it—'disease,' 'disorder,' 'state of mind'—affects how we view, diagnose, and treat it." There are cultural differences in the extent to which serious depression is considered an illness requiring personal professional treatment, or is an indicator of something else, such as the need to address social or moral problems, the result of biological imbalances, or a reflection individual differences in the understanding of distress that may reinforce feelings of powerlessness, and emotional struggle. The diagnosis is less common in some countries, such as China. It has been argued that the Chinese traditionally deny or somatize emotional depression (although since the early 1980s the Chinese denial of depression may have modified drastically). Alternatively, it may be that Western cultures reframe and elevate some expressions of human distress to disorder status. Gordon Parker and others have argued that the Western concept of depression "medicalizes" sadness or misery.
Evolutionary theorists view depression as an adaptation to regulate relationships or resources, although it may be unwanted or disordered in modern environments. From this perspective, depression can be seen as "a species-wide evolved suite of emotional programmes that are mostly activated by a perception, almost always over-negative, of a major decline in personal usefulness, that can sometimes be linked to guilt, shame or perceived rejection". Like an ageing hunter in our foraging past, an alienated member of today's society may feel and act in ways that prompt support from friends and kin. Additionally, in a manner analogous to that in which physical pain has evolved to hinder actions that may cause further injury, "psychic misery" may have evolved to prevent hasty and maladaptive reactions to distressing situations. These insights may be helpful in counselling therapy.
There is discussion in Western countries that depression and mental illness in general may be linked to creativity in the arts. British literature gives many examples of reflections on depression. English philosopher John Stuart Mill experienced a several-months-long period of what he called "a dull state of nerves," when one is "unsusceptible to enjoyment or pleasurable excitement; one of those moods when what is pleasure at other times, becomes insipid or indifferent". He quoted Samuel Taylor Coleridge's "Dejection" as a perfect description of his case: "A grief without a pang, void, dark and drear, / A drowsy, stifled, unimpassioned grief, / Which finds no natural outlet or relief / In word, or sigh, or tear." English essayist and wit Samuel Johnson used the term "the black dog" in 1780s to describe his own depression. Subsequently popularized by depression sufferer former British Prime Minister Sir Winston Churchill, the term lives on in the Black Dog Institute, an Australian facility for research and education into mood disorders such as major depression and bipolar disorder.
Historical figures were often reluctant to discuss or seek treatment for depression due to social stigma about the condition, or due to ignorance of diagnosis or treatments. Nevertheless, analysis or interpretation of letters, journals, artwork, writings or statements of family and friends of some historical personalities has led to the presumption that they may have had some form of depression. People who may have had depression include the British writer Henry James and American president Abraham Lincoln. Some well-known contemporary people with possible depression include Canadian songwriter Leonard Cohen and American playwright and novelist Tennessee Williams. Even some pioneering psychologists, such as William James and John B. Watson, dealt with depression in their adulthoods.
Both William James and John Stuart Mill found relief from their depression in literature. For James, who was nearly driven to suicide during his depression, the choice to believe in free will was instrumental in overcoming this condition. This choice was inspired by an essay about free will by French philosopher Charles-Bernard Renouvier. Upon reading this essay, James no longer felt that "suicide the most manly form to put daring into," and declared, "now I will go a step further with my will, not only act with it, but believe as well; believe in my individual reality and creative power." Mill took solace in the work of English poet William Wordsworth. Mill wrote that, "What made Wordsworth's poems a medicine for my state of mind, was that they expressed, not mere outward beauty, but states of feeling, and of thought coloured by feeling, under the excitement of beauty."
References
- ^ Mayo Clinic Staff (2006-03-06). "Depression" (PDF). National Institute of Mental Health (NIMH). Retrieved 2008-09-07.
- Hays RD, Wells KB, Sherbourne CD; et al. (1995). "Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses". Archives of General Psychiatry. 52 (1): 11–19. PMID 7811158.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ American Psychiatric Association 2000, p. 349 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- ^ American Psychiatric Association 2000, p. 350 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Patel V, Abas M, Broadhead J; et al. (2001). (fulltext) "Depression in developing countries: Lessons from Zimbabwe". British Medical Journal. 322 (7284): 482–84. doi:10.1136/bmj.322.7284.482. Retrieved 2008-10-05.
{{cite journal}}: Check|url=value (help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Faculty of Psychiatry of Old Age, NSW Branch, RANZCP (2001). Consensus Guidelines for Assessment and Management of Depression in the Elderly (PDF). North Sydney, New South Wales: NSW Health Department. pp. p. 2. ISBN 0-7347-33410.
{{cite book}}:|pages=has extra text (help); Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: multiple names: authors list (link) - American Psychiatric Association 2000, p. 412 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Sadock 2002, p. 555
- American Psychiatric Association 2000, p. 354 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Wiener, Jerry M. (2004). Textbook of Child and Adolescent Psychiatry. Arlington, VA: American Psychiatric Publishing. pp. p. 413. ISBN 1585620572.
{{cite book}}:|pages=has extra text (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Kendler KS, Gatz M, Gardner CO, Pedersen NL (2006). "A Swedish national twin study of lifetime major depression". American Journal of Psychiatry. 163 (1): 109–14. doi:10.1176/appi.ajp.163.1.109. PMID 16390897.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Panksepp J, Moskal JR, Panksepp JB, Kroes RA (2002). "Comparative approaches in evolutionary psychology: Molecular neuroscience meets the mind" (PDF). Neuroendocrinology Letters. 23 (Supplement 4): 105–15. PMID 12496741.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sloman L, Gilbert P, Hasey G (2003). "Evolved mechanisms in depression: The role and interaction of attachment and social rank in depression". Journal of Affective Disorders. 74 (2): 107–21. doi:10.1016/S0165-0327(02)00116-7. PMID 12706512.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Nutt DJ (2008). "Relationship of neurotransmitters to the symptoms of major depressive disorder". Journal of Clinical Psychiatry. 69 Suppl E1: 4–7. PMID 18494537.
- Caspi A; et al. (2003). "Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene". Science. 301: 386–89. doi:10.1126/science.1083968. PMID 12869766.
{{cite journal}}: Explicit use of et al. in:|author=(help) - Mandell AJ, Knapp S (1979). "Asymmetry and mood, emergent properties of serotonin regulation: A proposed mechanism of action of lithium". Archives of General Psychiatry. 36 (8): 909–16. PMID 454111.
- Hirschfeld RM (2000). "History and evolution of the monoamine hypothesis of depression". Journal of Clinical Psychiatry. 61 Suppl 6: 4–6. PMID 10775017.
- Delgado PL, Moreno FA (2000). "Role of norepinephrine in depression". Journal of Clinical Psychiatry. 61 Suppl 1: 5–12. PMID 10703757.
- Delgado PL (2000). "Depression: The case for a monoamine deficiency". Journal of Clinical Psychiatry. 61 Suppl 6: 7–11. PMID 10775018.
- Lacasse J, Leo J (2005). "Serotonin and depression: A disconnect between the advertisements and the scientific literature". PLoS Med. 2 (12): e392. doi:10.1371/journal.pmed.0020392.g001. PMID 16268734. Retrieved 2008-10-30.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Videbech, P and Ravnkilde (2004). "Hippocampal Volume and Depression: A Meta-Analysis of MRI Studies," Am J Psychiatry, 161:1957–1966.
- Videbech, P(1997). "MRI findings in patients with affective disorder: a meta-analysis," Acta Psychiatrica Scandinavica, 96:157–168.
- Mayberg, Helen (July 6, 2007). "Brain pathway may underlie depression". Scientific American. 17 (4): 26–31. Retrieved 2008-09-13.
- Sheline YI, Gado MH, Kraemer HC (2003). "Untreated depression and hippocampal volume loss". American Journal of Psychiatry. 160: 1516–18. doi:10.1176/appi.ajp.160.8.1516. PMID 12900317.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Duman RS, Heninger GR, Nestler EJ (1997). "A molecular and cellular theory of depression". Archives of General Psychiatry. 54 (7): 597–606. PMID 9236543.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Drevets WC, Savitz J, Trimble M (2008). "The subgenual anterior cingulate cortex in mood disorders". CNS Spectrums. 13 (8): 663–81. PMID 18704022.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Sen S, Duman R, Sanacora G (2008). "Serum brain-derived neurotrophic factor, depression, and antidepressant medications: Meta-analyses and implications". Biological Psychiatry. 64 (6): 527–32. doi:10.1016/j.biopsych.2008.05.005. PMID 18571629.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Pariante Carmine M (2003). "Depression, stress and the adrenal axis". Journal of Neuroendocrinology. The British Society for Neuroendocrinology. PMID 12834443.
- Barlow 2005, pp. 227–28
- ^ Sadock 2002, p. 541
- Exline JJ, Yali AM, Sanderson WC (2000). "Guilt, discord, and alienation: the role of religious strain in depression and suicidality". Journal of clinical psychology. 56 (12): 1481–96. doi:10.1002/1097-4679(200012)56:12<1481::AID-1>3.0.CO;2-A. PMID 11132565.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Moreira-Almeida A, Neto FL, Koenig HG (2006). "Religiousness and mental health: A review". Revista brasileira de psiquiatria (Brazilian Journal of Psychiatry). 3: 242–250. PMID 16924349.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Warman DM, Beck AT (2003). "About treatment and supports: Cognitive behavioral therapy". National Alliance on Mental Illness (NAMI) website. Retrieved 2008-10-17.
{{cite web}}: Unknown parameter|month=ignored (help) - Seligman, Martin (1975). Helplessness: On depression, development and death. San Francisco, CA, USA: WH Freeman. ISBN 0716707519.
- Benassi V, Sweeney PD, Dufour C (1988). "Is there a relation between locus of control orientation and depression?". Journal of Abnormal Psychology. 97 (3): 357–67. doi:10.1037/0021-843X.97.3.357.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Barlow 2005, pp. 230–32
- Allen, Joseph P. (2003). "An Overview of Beck's Cognitive Theory of Depression in Contemporary Literature". Personality Papers. Retrieved 2008-10-30.
{{cite journal}}: Cite journal requires|journal=(help) - Pinto A, Francis G (1993). "Cognitive correlates of depressive symptoms in hospitalized adolescents". Adolescence. 28 (111): 661–72. PMID 8237551.
- Kanfer, R (1983). "Depression, Interpersonal Standard Setting". Journal of Abnormal Psychology. 92 (3): 319–29. doi:10.1037/0021-843X.92.3.319. PMID 6619407.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Bandura A (1998). "Self-Efficacy". In Friedman H (ed.). Encyclopedia of mental health. San Diego: Academic Press. Retrieved 2008-08-17.
- Taylor, Shelley E. (1991). Positive Illusions: Creative Self-deception and the Healthy Mind. New York, NY, USA: Basic Books. ISBN 0465060536.
- Alloy LB, Abramson LY (1979). "Judgment of contingency in depressed and nondepressed students: Sadder but wiser?". Journal of Experimental Psychology: General. 108: 441–85. doi:10.1037/0096-3445.108.4.441. PMID 528910.
- Brown GW, Harris TO (2001) . Social origins of Depression: A Study of psychiatric disorder in women. Routledge. ISBN 0-415-20268-X.
- Patten, SB (1991). "Are the Brown and Harris "vulnerability factors" risk factors for depression?". Journal of Psychiatry & Neuroscience. 16 (5): 267–71. PMID 1797101.
{{cite journal}}: Unknown parameter|month=ignored (help) - Hinrichsen GA, Emery EE (2006). "Interpersonal Factors and Late-Life Depression" (Subscription required). Clinical Psychology: Science and Practice. 12 (3): 264–75.
- Freud S (Strachey J, Trans.) (1953–74). The standard edition of the complete psychological works of Sigmund Freud. Vol. 22. London, UK. pp. p. 61.
{{cite book}}:|pages=has extra text (help)CS1 maint: location missing publisher (link) - Carhart-Harris RL, Mayberg HS, Malizia AL, Nutt D (2008). "Mourning and melancholia revisited: Correspondences between principles of Freudian metapsychology and empirical findings in neuropsychiatry". Annals of General Psychiatry. 7: 9. doi:10.1186/1744-859X-7-9. PMC 2515304. PMID 18652673.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Geppert, Cynthia A. (2006). "Biologic, Syndromic, Social, and Personal Damage". Psychiatric Times. 23 (6): 979–99.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ May R (1996). The meaning Of anxiety. New York: W. W. Norton and Company. ISBN 0-393-31456-1.
- Fromm Erich (1941). Escape from Freedom. New York: Holt, Rinehart, & Winston.
- ^ Heidegger Martin (1927). Being and time. Halle, Germany: Niemeyer. Cite error: The named reference "Being" was defined multiple times with different content (see the help page).
- Hergenhahn 2005, pp. 546–47
- Boeree, Dr. C. George (1998). "Abraham Maslow: Personality Theories" (PDF). Psychology Department, Shippensburg University. Retrieved 2008-10-27.
- Maslow A (1971). The farther reaches of human nature. New York, NY, USA. p. 318.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Mashman, RC (1997). "An evolutionary view of psychic misery". Journal of Social Behaviour & Personality. 12: 979–99.
- Nesse RM (2000). "Is depression an adaptation?". Archives of General Psychiatry. 57 (1): 14–20. doi:10.1001/archpsyc.57.1.14. PMID 10632228.
{{cite journal}}: Unknown parameter|month=ignored (help) - Gilbert P (2000). Overcoming Depression: A Self-Help Guide Using Cognitive Behavioral Techniques (2nd rev. ed.). London: Robinson Publishing. ISBN 1841191256.
- ^ Carey TJ (2005). "Evolution, depression and counselling". Counselling Psychology Quarterly. 18 (3): 215–22. doi:10.1080/09515070500304508.
- Gilman, Stephen E (2003). "Family disruption in childhood and risk of adult depression". American Journal of Psychiatry. 160: 939–46. doi:10.1176/appi.ajp.160.5.939. PMID 12727699.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - Gilman, Stephen E (2002). "Socioeconomic status in childhood and the lifetime risk of major depression". International Journal of Epidemiology. 31: 359–67. doi:10.1093/ije/31.2.359. PMID 11980797.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF (2004). "Adverse childhood experiences and the risk of depressive disorders in adulthood". Journal of Affective Disorders. 82: 217–25. doi:10.1016/j.jad.2003.12.013. PMID 15488250.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, Williamson DF (2002). "Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression". Psychiatric Services. 53: 1001–09. doi:10.1176/appi.ps.53.8.1001. PMID 12161676. Retrieved 2008-10-02.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hazel NA, Hammen C, Brennan PA, Najman J (2008). "Early childhood adversity and adolescent depression: The mediating role of continued stress". Psychological Medicine. 38: 581–89. doi:10.1017/S0033291708002857. PMID 18261247.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Nolan SA, Flynn C, Garber J (2003). "Prospective relations between rejection and depression in young adolescents". Journal of Personality and Social Psychology. 85: 745–55. doi:10.1037/0022-3514.85.4.745. PMID 14561127.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - van Hoof A, Quinten A, Raaijmakers AW, van Beek Y, Hale WW (III), Aleva L (2007). "A Multi-mediation Model on the Relations of Bullying, Victimization, Identity, and Family with Adolescent Depressive Symptoms". Journal of Youth and Adolescence. 37: 772–82. doi:10.1007/s10964-007-9261-8. Retrieved 2008-10-01.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA (2003). "Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety". Archives of General Psychiatry. 60: 789–96. doi:10.1001/archpsyc.60.8.789. PMID 12912762.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Stroud CB, Davila J, Moyer A (2008). "The relationship between stress and depression in first onsets versus recurrences: A meta-analytic review". Archives of General Psychiatry. 117: 206–13. PMID 18266498.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bruce ML, Hoff RA (1994). "Social and physical health risk factors for first-onset major depressive disorder in a community sample". Social Psychiatry and Psychiatric Epidemiology. 29: 165–71. PMID 7939965.
{{cite journal}}: Unknown parameter|month=ignored (help) - Bonde JP (2008). "Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence". Journal of Occupational and Environmental Medicine. 65: 438–45. doi:10.1136/oem.2007.038430. PMID 18417557.
{{cite journal}}: Unknown parameter|month=ignored (help) - Kim D (2008). "Blues from the Neighborhood? Neighborhood Characteristics and Depression". Epidemiologic Reviews. 30: 101. doi:10.1093/epirev/mxn009. PMID 18753674.
{{cite journal}}: Unknown parameter|month=ignored (help) - Dale J, Sorour E, Milner G (2008). "Do psychiatrists perform appropriate physical investigations for their patients? A review of current practices in a general psychiatric inpatient and outpatient setting". Journal of Mental Health. 17 (3): 293–98. doi:10.1080/09638230701498325.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Orengo C, Fullerton G, Tan R (2004). "Male depression: A review of gender concerns and testosterone therapy". Geriatrics. 59 (10): 24–30. PMID 15508552.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Reid LM, Maclullich AM (2006). "Subjective memory complaints and cognitive impairment in older people". Dementia and geriatric cognitive disorders. 22 (5–6): 471–85. doi:10.1159/000096295. PMID 17047326.
- ^ Katz IR (1998). "Diagnosis and treatment of depression in patients with Alzheimer's disease and other dementias". The Journal of clinical psychiatry. 59 Suppl 9: 38–44. PMID 9720486.
- Wright SL, Persad C (2007). "Distinguishing between depression and dementia in older persons: neuropsychological and neuropathological correlates". Journal of geriatric psychiatry and neurology. 20 (4): 189–98. doi:10.1177/0891988707308801. PMID 18004006.
{{cite journal}}: Unknown parameter|month=ignored (help) - Sadock 2002, p. 108
- Sadock 2002, p. 260
- Palmer B, Gates J, Lader M (2003). "Causes and Management of Hyponatremia". The Annals of Pharmacotherapy. 37 (11): 1694–702. doi:10.1345/aph.1D105. PMID 14565794.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kaufmann IM (1993). (link to fulltext) "Rural psychiatric services. A collaborative model". Canadian Family Physician. 39: 1957–61. PMID 8219844. Retrieved 2008-10-11.
{{cite journal}}: Check|url=value (help); Unknown parameter|day=ignored (help); Unknown parameter|month=ignored (help); Unknown parameter|pmcid=ignored (|pmc=suggested) (help) - "Call for action over Third World depression". BBC News (Health). British Broadcasting Corporation (BBC). November 1, 1999. Retrieved 2008-10-11.
- Gilbody S, House AO, Sheldon TA (2005). "Screening and case finding instruments for depression". Cochrane Database of Systematic Reviews (4). doi:10.1002/14651858.CD002792.pub2.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Gilbody S, Sheldon T, Wessely S (2006). "Should we screen for depression?". British Medical Journal. 332: 1027–30. doi:10.1136/bmj.332.7548.1027. PMID 16644833.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Beck Depression Inventory - 2nd Edition". Nova Southeastern University Center for Center for Psychological Studies. Retrieved 2008-10-17.
- Goodwin FK, Jamison KR (1990). Manic-Depressive Illness. New York: Oxford University Press. pp. pp. 361–62. ISBN 0-19-503934-3.
{{cite book}}:|pages=has extra text (help) - Beck AT (1972). Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press. pp. p. 333. ISBN 0-8122-1032-8.
{{cite book}}:|pages=has extra text (help) - Yesavage JA (1988). "Geriatric Depression Scale". Psychopharmacology Bulletin. 24 (4): 709–11.
- Hamilton M (1960). "A rating scale for depression". Journal of Neurology, Neurosurgery and Psychiatry. 23: 56–62. PMID 14399272.
- Bagby RM, Ryder AG, Schuller DR, Marshall MB (2004). "The Hamilton Depression Rating Scale: has the gold standard become a lead weight?". American Journal of Psychiatry. 161 (12): 2163–77. doi:10.1176/appi.ajp.161.12.2163. PMID 15569884.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Montgomery SA, Asberg M (1979). "A new depression scale designed to be sensitive to change". British Journal of Psychiatry. 134: 382–9. doi:10.1192/bjp.134.4.382. PMID 444788.
{{cite journal}}: Unknown parameter|month=ignored (help) - Demyttenaere K, De Fruyt J (2003). "Getting what you ask for: on the selectivity of depression rating scales". Psychotherapy and psychosomatics. 72: 61–70. doi:10.1159/000068690. PMID 12601223.
- Spitzer RL, Kroenke K, Williams JB (1999). "Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire". Journal of the American Medical Association. 282 (18): 1737–44. doi:10.1001/jama.282.18.1737. PMID 10568646.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Resources for clinicians: Patient health questionnaire". The MacArthur Initiative on Depression Primary Care. Dartmouth College & Duke University. 2006. Retrieved 2008-09-02.
- Sadock 2002, p. 288
- American Psychiatric Association 2000, p. 345 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- "Mood (affective) disorders". ICD-10, Chapter V, Mental and behavioural disorders. World Health Organization (WHO). 2004. Retrieved 2008-10-19.
- American Psychiatric Association 2000, p. 372 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Parker 1996, p. 173
- American Psychiatric Association 2000, p. 352 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Wakefield JC, Schmitz MF, First MB, Horwitz AV (2007). "Extending the bereavement exclusion for major depression to other losses: Evidence from the National Comorbidity Survey". Archives of General Psychiatry. 64 (4): 433–40. doi:10.1001/archpsyc.64.4.433. PMID 17404120.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Vedantam S (April 3, 2007). "Criteria for depression are too broad, researchers say: Guidelines may encompass many who are just sad". Washington Post (online) P.A02. Washington Post. Retrieved 2008-10-10.
- Kendler KS, Gardner CO (1998). "Boundaries of major depression: An evaluation of DSM-IV criteria". American Journal of Psychiatry. 155 (2): 172–77. PMID 9464194.
{{cite journal}}: Unknown parameter|day=ignored (help); Unknown parameter|month=ignored (help) - ^ Sadock 2002, p. 552
- American Psychiatric Association 2000, p. 778 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Carta MG, Altamura AC, Hardoy MC; et al. (2003). "Is recurrent brief depression an expression of mood spectrum disorders in young people?". European Archives of Psychiatry and Clinical Neuroscience. 253 (3): 149–53. doi:10.1007/s00406-003-0418-5.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Rapaport MH, Judd LL, Schettler PJ; et al. (2002). "A descriptive analysis of minor depression". American Journal of Psychiatry. 159 (4): 637–43. doi:10.1176/appi.ajp.159.4.637. PMID 11925303.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ American Psychiatric Association 2000, p. 355 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- American Psychiatric Association 2000, pp. 419–20 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- American Psychiatric Association 2000, p. 421–22 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- American Psychiatric Association 2000, pp. 417–18 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Nonacs, Ruta M (December 4, 2007). "Postpartum depression". eMedicine. Retrieved 2008-10-30.
- American Psychiatric Association 2000, p. 425 harvnb error: multiple targets (2×): CITEREFAmerican_Psychiatric_Association2000 (help)
- Akiskal HS, Benazzi F (2006). "The DSM-IV and ICD-10 categories of recurrent depressive and bipolar II disorders: Evidence that they lie on a dimensional spectrum". Journal of Affective Disorders. 92 (1): 45–54. doi:10.1016/j.jad.2005.12.035. PMID 16488021.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Loneliness as a Component of Psychiatric Disorders: The Relationship Between Loneliness and Depression" (subscription required). Medscape. Retrieved 2008-10-30.
- Patel V, Araya R, Bolton P; et al. (2004). (fulltext) "Editorial: Treating depression in the developing world". Tropical Medicine & International Health. 9 (5): 539–41. doi:10.1111/j.1365-3156.2004.01243.x. Retrieved 2008-10-05.
{{cite journal}}: Check|url=value (help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Thase, ME (1999). "When are psychotherapy and pharmacotherapy combinations the treatment of choice for major depressive disorder?". Psychiatric Quarterly. 70 (4): 333–46. doi:10.1023/A:1022042316895. PMID 10587988.
- NICE (2005). NICE guidelines: Depression in children and adolescents. London: NICE. pp. p. 5. ISBN 1-84629-074-0. Retrieved 2008-08-16.
{{cite book}}:|pages=has extra text (help) - Roth, Anthony (2005) . What Works for Whom? Second Edition: A Critical Review of Psychotherapy Research. Guilford Press. pp. p. 78. ISBN 159385272X.
{{cite book}}:|pages=has extra text (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Reinecke MA, Ryan NE, DuBois DL (1997). "Cognitive-behavioral therapy of depression and depressive symptoms during adolescence: A review and meta-analysis". Journal of the American Academy of Child and Adolescent Psychiatry. 37 (1): 26–34. PMID 9444896.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Harrington R, Whittaker J, Shoebridge P, Campbell F (1998). "Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder". British Medical Journal. 325 (7358): 229–30. doi:10.1136/bmj.325.7358.229. PMID 9596592.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Goodyer I, Dubicka B, Wilkinson P; et al. (2007). "Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: Randomised controlled trial". British Medical Journal. 335 (7611): 142. doi:10.1136/bmj.39224.494340.55. PMC 1925185. PMID 17556431.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Goodyer IM, Dubicka B, Wilkinson P; et al. (2008). "A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial". Health Technology Assessment. 12 (14): 1–80. PMID 18462573.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Domino ME, Burns BJ, Silva SG; et al. (2008). "Cost-effectiveness of treatments for adolescent depression: Results from TADS". American Journal of Psychiatry. 165 (5): 588–96. doi:10.1176/appi.ajp.2008.07101610. PMID 18413703.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Coelho HF, Canter PH, Ernst E (2007). "Mindfulness-based cognitive therapy: Evaluating current evidence and informing future research". Journal of Consulting and Clinical Psychology. 75 (6): 1000–05. doi:10.1037/0022-006X.75.6.1000. PMID 18085916.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Weissman MM, Markowitz JC, Klerman GL (2000). Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books. ISBN 0-465-09566-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Dworetzky J (1997). Psychology. Pacific Grove, CA, USA: Brooks/Cole Pub. Co. p. 602. ISBN 0-314-20412-1.
- Doidge N, Simon B, Lancee WJ; et al. (2002). "Psychoanalytic patients in the US, Canada, and Australia: II. A DSM-III-R validation study". Journal of the American Psychoanalytic Association. 50 (2): 615–27. doi:10.1177/00030651020500021101. PMID 12206545.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Durand VM, Barlow D (1999). Abnormal psychology: An integrative approach. Pacific Grove, CA, USA: Brooks/Cole Pub. Co. ISBN 0-534-34742-8.
- de Maat S, Dekker J, Schoevers R; et al. (2007). "Short Psychodynamic Supportive Psychotherapy, antidepressants, and their combination in the treatment of major depression: A mega-analysis based on three Randomized Clinical Trials". Depression and Anxiety. 25: 565. doi:10.1002/da.20305. PMID 17557313.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Sutherland JE, Sutherland SJ, Hoehns JD (2003). "Achieving the best outcome in treatment of depression". Journal of Family Practice. 52 (3): 201–09. PMID 12620174.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Zisook S, Rush AJ, Haight BR, Clines DC, Rockett CB (2006). "Use of bupropion in combination with serotonin reuptake inhibitors". Biological Psychiatry. 59 (3): 203–10. doi:10.1016/j.biopsych.2005.06.027. PMID 16165100.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Rush AJ, Trivedi MH, Wisniewski SR; et al. (2006). "Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression". New England Journal of Medicine. 354 (12): 1231–42. doi:10.1056/NEJMoa052963. PMID 16554525.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Trivedi MH, Fava M, Wisniewski SR, Thase ME, Quitkin F, Warden D, Ritz L, Nierenberg AA, Lebowitz BD, Biggs MM, Luther JF, Shores-Wilson K, Rush AJ (2006). "Medication augmentation after the failure of SSRIs for depression". New England Journal of Medicine. 354 (12): 1243–52. doi:10.1056/NEJMoa052964. PMID 16554526.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Mayers AG, Baldwin DS (2005). "Antidepressants and their effect on sleep". Human Psychopharmacology. 20 (8): 533–59. doi:10.1002/hup.726. PMID 16229049.
{{cite journal}}: Unknown parameter|month=ignored (help) - Winokur A, DeMartinis NA, McNally DP, Gary EM, Cormier JL, Gary KA (2003). "Comparative effects of mirtazapine and fluoxetine on sleep physiology measures in patients with major depression and insomnia". Journal of Clinical Psychiatry. 64 (10): 1224–29. PMID 14658972.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Lawrence RW (2004). "Effect of mirtazapine versus fluoxetine on "sleep quality"". Journal of Clinical Psychiatry. 65 (8): 1149–50. PMID 15323610.
{{cite journal}}: Unknown parameter|month=ignored (help) - Papakostas GI, Thase ME, Fava M, Nelson JC, Shelton RC (2007). "Are antidepressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agents". Biological Psychiatry. 62 (11): 1217–27. doi:10.1016/j.biopsych.2007.03.027. PMID 17588546.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Cipriani A, Geddes JR, Barbui C (2007). "Venlafaxine for major depression". British Medical Journal. 334: 215 (editorial). doi:10.1136/bmj.39098.457720.BE. PMID 17272528. Retrieved 2008-09-13.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Depression in children and young people: Identification and management in primary, community and secondary care". NHS National Institute for Health and Clinical Excellence. 2005. Retrieved 2008-08-17.
{{cite web}}: Unknown parameter|month=ignored (help) - Anderson IM (1998). "SSRIS versus tricyclic antidepressants in depressed inpatients: A meta-analysis of efficacy and tolerability". Depression and Anxiety. 7 Suppl 1: 11–17. doi:10.1002/(SICI)1520-6394(1998)7:1+<11::AID-DA4>3.0.CO;2-I. PMID 9597346.
- Anderson IM (2000). "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: A meta-analysis of efficacy and tolerability". Journal of Affective Disorders. 58 (1): 19–36. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555.
{{cite journal}}: Unknown parameter|month=ignored (help) - Krishnan KR (2007). "Revisiting monoamine oxidase inhibitors". Journal of Clinical Psychiatry. 68 Suppl 8: 35–41. PMID 17640156.
- Depression Guideline Panel. Depression in primary care. Vol. 2. Treatment of major depression. Clinical practice guideline. No. 5. Rockville, MD: Agency for Health Care Policy and Research, 1999.
- Wijeratne, Chanaka, Sachdev, Perminder (2008). "Treatment-resistant depression: Critique of current approaches". Australian and New Zealand Journal of Psychiatry. 42: 751–62. PMID 18696279.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Valenstein M, McCarthy JF, Austin KL, Greden JF, Young EA, Blow FC (2006). "What happened to lithium? Antidepressant augmentation in clinical settings". American Journal of Psychiatry. 163 (7): 1219–25. doi:10.1176/appi.ajp.163.7.1219. PMID 16816227.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bauer M, Dopfmer S (1999). "Lithium augmentation in treatment-resistant depression: Meta-analysis of placebo-controlled studies". Journal of Clinical Psychopharmacology. 19 (5): 427–34. doi:10.1097/00004714-199910000-00006. PMID 10505584.
- Guzzetta F, Tondo L, Centorrino F, Baldessarini RJ (2007). "Lithium treatment reduces suicide risk in recurrent major depressive disorder". Journal of Clinical Psychiatry. 68 (3): 380–83. PMID 17388706.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Nierenberg AA, Fava M, Trivedi MH, Wisniewski SR, Thase ME, McGrath PJ, Alpert JE, Warden D, Luther JF, Niederehe G, Lebowitz B, Shores-Wilson K, Rush AJ (2006). "A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: A STAR*D report". American Journal of Psychiatry. 163 (9): 1519–30. doi:10.1176/appi.ajp.163.9.1519. PMID 16946176.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bender KJ (2008-02-01). "Evidence Grows for Value of Antipsychotics as Antidepressant Adjuncts - Psychiatric Times". Psychiatric Times. Retrieved 2008-08-06.
- ^ Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT (2008). "Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration". PLoS Med. 5 (2): e45. doi:10.1371/journal.pmed.0050045. PMC 2253608. PMID 18303940.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R (2008). "Selective publication of antidepressant trials and its influence on apparent efficacy". N. Engl. J. Med. 358 (3): 252–60. doi:10.1056/NEJMsa065779. PMID 18199864.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, Glass DR, Pilkonis PA, Leber WR, Docherty JP (1989). "National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments". Archives of General Psychiatry. 46 (11): 971–82, discussion 983. PMID 2684085.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, Hedeker D (1995). "Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program". Journal of Consulting and Clinical Psychology. 63 (5): 841–47. doi:10.1037/0022-006X.63.5.841. PMID 7593878.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sotsky SM, Glass DR, Shea MT, Pilkonis PA, Collins JF, Elkin I, Watkins JT, Imber SD, Leber WR, Moyer J (1991). "Patient predictors of response to psychotherapy and pharmacotherapy: Findings in the NIMH Treatment of Depression Collaborative Research Program". American Journal of Psychiatry. 148 (8): 997–1008. PMID 1853989.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Turner EH, Rosenthal R (2008). "Efficacy of antidepressants". British Medical Journal. 336 (7643): 516–17. doi:10.1136/bmj.39510.531597.80. PMC 2265347. PMID 18319297.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cuijpers P, van Straten A, van Oppen P, Andersson G (2008). "Are Psychological and Pharmacologic Interventions Equally Effective in the Treatment of Adult Depressive Disorders? A Meta-Analysis of Comparative Studies". Journal of Clinical Psychiatry: e1 – e11.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Imel ZE, Malterer MB, McKay KM, Wampold BE (2008). "A meta-analysis of psychotherapy and medication in unipolar depression and dysthymia". Journal of Affective Disorders. 110 (3): 197–206. doi:10.1016/j.jad.2008.03.018. PMID 18456340.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ American Psychiatric Association (2000). "Practice guideline for the treatment of patients with major depressive disorder". American Journal of Psychiatry. 157 (Supp 4): 1–45. PMID 10767867.
{{cite journal}}: Unknown parameter|month=ignored (help) - The UK ECT Review Group (2003). "Efficacy and safety of electroconvulsive therapy in depressive disorders: A systematic review and meta-analysis". The Lancet. 361 (9360): 799–808. doi:10.1016/S0140-6736(03)12705-5.
- McCall WV, Prudic J, Olfson M, Sackeim H (2006). "Health-related quality of life following ECT in a large community sample". Journal of Affective Disorders. 90 (2–3): 69–74. doi:10.1016/j.jad.2005.12.002. PMID 16412519.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Prudic J, Olfson M, Marcus SC, Fuller RB, Sackeim HA (2004). "Effectiveness of electroconvulsive therapy in community settings". Biological Psychiatry. 55 (3): 301–12. doi:10.1016/j.biopsych.2003.09.015. PMID 14744473.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sackeim HA, Haskett RF, Mulsant BH; et al. (2001). "Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: A randomized controlled trial". JAMA: Journal of the American Medical Association. 285 (10): 1299–307. doi:10.1001/jama.285.10.1299. PMID 11255384.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Tew JD, Mulsant BH, Haskett RF, Joan P, Begley AE, Sackeim HA (2007). "Relapse during continuation pharmacotherapy after acute response to ECT: A comparison of usual care versus protocolized treatment". Annals of Clinical Psychiatry. 19 (1): 1–4. doi:10.1080/10401230601163360. PMID 17453654.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kellner CH, Knapp RG, Petrides G; et al. (2006). "Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: A multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE)". Archives of General Psychiatry. 63 (12): 1337–44. doi:10.1001/archpsyc.63.12.1337. PMID 17146008.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Barlow 2005, p. 239
- American Psychiatric Association. "Electroconvulsive Therapy (ECT)". Retrieved 2007-12-29.
- National Institute for Clinical Excellence (2003). Guidance on the use of electroconvulsive therapy (PDF). London: National Institute for Health and Clinical Excellence. ISBN 1-84257-282-2.
- Linde K, Mulrow CD, Berner M, Egger M (2005). "St John's wort for depression". Cochrane Database Systematic Reviews (2): CD000448. doi:10.1002/14651858.CD000448.pub2. PMID 15846605.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "St. John's Wort and Depression". NCCAM Health Information. Retrieved 2008-10-13.
- Mischoulon D, Fava M (2002). "Role of S-adenosyl-L-methionine in the treatment of depression: A review of the evidence". American Journal of Clinical Nutrition. 76 (5): 1158S – 61S. PMID 12420702.
{{cite journal}}: Unknown parameter|month=ignored (help) - Bressa GM (1994). "S-adenosyl-l-methionine (SAMe) as antidepressant: Meta-analysis of clinical studies". Acta Neurologica Scandinavica, Suppl. 154: 7–14. PMID 7941964.
- Appleton KM, Hayward RC, Gunnell D; et al. (2006). "Effects of n-3 long-chain polyunsaturated fatty acids on depressed mood: Systematic review of published trials". The American journal of clinical nutrition. 84 (6): 1308–16. PMID 17158410.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Shaw K, Turner J, Del Mar C (2002). "Tryptophan and 5-hydroxytryptophan for depression". Cochrane Database of Systematic Reviews (1): CD003198. doi:10.1002/14651858.CD003198. PMID 11869656.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Marangell LB, Martinez M, Jurdi RA, Zboyan H (2007). "Neurostimulation therapies in depression: A review of new modalities". Acta Psychiatrica Scandinavica. 116 (3): 174–81. doi:10.1111/j.1600-0447.2007.01033.x. PMID 17655558.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Schutter DJ (2008). "Antidepressant efficacy of high-frequency transcranial magnetic stimulation over the left dorsolateral prefrontal cortex in double-blind sham-controlled designs: A meta-analysis". Psychological Medicine: 1–11. doi:10.1017/S0033291708003462. PMID 18447962.
{{cite journal}}: Unknown parameter|month=ignored (help) - Eranti S, Mogg A, Pluck G; et al. (2007). "A randomized, controlled trial with 6-month follow-up of repetitive transcranial magnetic stimulation and electroconvulsive therapy for severe depression". American Journal of Psychiatry. 164 (1): 73–81. doi:10.1176/appi.ajp.164.1.73. PMID 17202547.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Golden RN, Gaynes BN, Ekstrom RD; et al. (2005). "The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence". American Journal of Psychiatry. 162 (4): 656–62. doi:10.1176/appi.ajp.162.4.656. PMID 15800134.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Tuunainen A, Kripke DF, Endo T (2004). "Light therapy for non-seasonal depression". Cochrane Database Syst Rev (2): CD004050. doi:10.1002/14651858.CD004050.pub2. PMID 15106233.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA (2008). "Exercise for depression". Cochrane database of systematic reviews (Online) (4): CD004366. doi:10.1002/14651858.CD004366.pub3. PMID 18843656.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Posternak MA, Miller I (2001). "Untreated short-term course of major depression: A meta-analysis of outcomes from studies using wait-list control groups". Journal of Affective Disorders. 66 (2–3): 139–46. doi:10.1016/S0165-0327(00)00304-9. PMID 11578666.
- Posternak MA, Solomon DA, Leon AC; et al. (2006). "The naturalistic course of unipolar major depression in the absence of somatic therapy". Journal of Nervous and Mental Disease. 194 (5): 324–29. doi:10.1097/01.nmd.0000217820.33841.53. PMID 16699380.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Eaton WW, Shao H, Nestadt G; et al. (2008). "Population-based study of first onset and chronicity in major depressive disorder". Archives of General Psychiatry. 65 (5): 513–20. doi:10.1001/archpsyc.65.5.513. PMID 18458203.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Holma KM, Holma IA, Melartin TK; et al. (2008). "Long-term outcome of major depressive disorder in psychiatric patients is variable". Journal of Clinical Psychiatry. 69 (2): 196–205. PMID 18251627.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Kanai T, Takeuchi H, Furukawa TA; et al. (2003). "Time to recurrence after recovery from major depressive episodes and its predictors". Psychological Medicine. 33 (5): 839–45. doi:10.1017/S0033291703007827. PMID 12877398.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Geddes JR, Carney SM, Davies C; et al. (2003). "Relapse prevention with antidepressant drug treatment in depressive disorders: A systematic review". Lancet. 361 (9358): 653–61. doi:10.1016/S0140-6736(03)12599-8. PMID 12606176.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Frank C (1999). "Skirmish or Siege? Is depression primarily a recurring disease? Can you ever really be cured?". Psychology Today Magazine. Retrieved 2008-10-30.
{{cite journal}}: Unknown parameter|month=ignored (help) - "The world health report 2001 - Mental Health: New Understanding, New Hope". WHO website. World Health Organization. 2001. Retrieved 2008-10-19.
- Andrade L, Caraveo-Anduaga JJ, Berglund P; et al. (2003). "The epidemiology of major depressive episodes: Results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys". Int J Methods Psychiatr Res. 12 (1): 3–21. doi:10.1002/mpr.138. PMID 12830306.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Kessler RC, Berglund P, Demler O; et al. (2003). "The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R)". JAMA. 289 (203): 3095–105. doi:10.1001/jama.289.23.3095. PMID 12813115.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005). "Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication". Archives of General Psychiatry. 62 (6): 617–27. doi:10.1001/archpsyc.62.6.593. PMID 15939837.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH (2000). "A 40-year perspective on the prevalence of depression: The Stirling County Study". Archives of General Psychiatry. 57 (3): 209–15. doi:10.1001/archpsyc.57.3.209. PMID 10711905.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kuehner, C (2003). "Gender differences in unipolar depression: An update of epidemiological findings and possible explanations". Acta Psychiatrica Scandinavica. 108 (3): 163–74. doi:10.1034/j.1600-0447.2003.00204.x. PMID 12890270.
- Eaton WW, Anthony JC, Gallo J; et al. (1997). "Natural history of diagnostic interview schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up". Archives of General Psychiatry. 54: 993–99. PMID 9366655.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Rickards H (2005). "Depression in neurological disorders: Parkinson's disease, multiple sclerosis, and stroke". Journal of Neurology Neurosurgery and Psychiatry. 76: i48 – i52. doi:10.1136/jnnp.2004.060426. PMID 15718222.
- Huffman JC, Smith FA, Blais MA; et al. (2008). "Pre-existing major depression predicts in-hospital cardiac complications after acute myocardial infarction". Psychosomatics. 49 (4): 309–16. doi:10.1176/appi.psy.49.4.309. PMID 18621936.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - "Country reports and charts available". WHO website - Mental health. World Health Organization. 2008. Retrieved 2008-09-16.
- Weich S, Lewis G (1998). (fulltext) "Poverty, unemployment, and common mental disorders: Population based cohort study". British Medical Journal. 317: 115–19. PMID 9657786. Retrieved 2008-09-16.
{{cite journal}}: Check|url=value (help) - Vasiliadis H-M, Lesage A, Adair C, Wang PS, Kessler RC (2007). "Do Canada and the United States differ in prevalence of depression and utilization of services?". Psychiatric Services. 58 (1): 63–71. doi:10.1176/appi.ps.58.1.63. PMID 17215414.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Mathers CD, Loncar D (2006). "Projections of global mortality and burden of disease from 2002 to 2030". PLoS Med. 3 (11): e442. doi:10.1371/journal.pmed.0030442. PMC 1664601. PMID 17132052.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - Barlow 2005, pp. 248–49
- Rush AJ (2007). "The varied clinical presentations of major depressive disorder". The Journal of clinical psychiatry. 68 (Supplement 8): 4–10. PMID 17640152.
- Bostwick, JM (2000). "Affective disorders and suicide risk: A reexamination". American Journal of Psychiatry. 157 (12): 1925–32. doi:10.1176/appi.ajp.157.12.1925. PMID 11097952.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Blair-West GW, Mellsop GW (2001). "Major depression: Does a gender-based down-rating of suicide risk challenge its diagnostic validity?". Australian and New Zealand Journal of Psychiatry. 35 (3): 322–28. doi:10.1046/j.1440-1614.2001.00895.x. PMID 11437805.
- Frank E, Prien RF, Jarrett RB; et al. (1991). "Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence". Archives of General Psychiatry. 48 (9): 851–55. PMID 1929776.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Sapolsky Robert M (2004). Why zebras don't get ulcers. Henry Holt and Company, LLC. pp. 291–98. ISBN 0-8050-7369-8.
- Grant BF (1995). "Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults". Journal of Substance Abuse. 7 (4): 481–87. doi:10.1016/0899-3289(95)90017-9. PMID 8838629.
- Hallowell EM, Ratey JJ (2005). Delivered from distraction: Getting the most out of life with Attention Deficit Disorder. New York: Ballantine Books. pp. pp. 253–55. ISBN 0-345-44231-8.
{{cite book}}:|pages=has extra text (help) - Vranceanu A-M, Hobfoll SE, Johnson RJ (2007). "Child multi-type maltreatment and associated depression and PTSD symptoms: The role of social support and stress". Child Abuse & Neglect. 31: 71–84. doi:10.1016/j.chiabu.2006.04.010. PMID 1839899.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Nasser, M. (1987) "Psychiatry in Ancient Egypt" (PDF). Bulletin Of The Royal College Of Psychiatrists, Vol 11 (December): 420–22
- ^ Davison, K (2006). "Historical aspects of mood disorders". Psychiatry. 5 (4): 115–18.
- Liddell, Henry George and Robert Scott (1980). A Greek-English Lexicon (Abridged Edition). United Kingdom: Oxford University Press. ISBN 0-19-910207-4.
- Hippocrates, Aphorisms, Section 6.23
- ^ Radden, J (2003). "Is this dame melancholy? Equating today's depression and past melancholia". Philosophy, Psychiatry, & Psychology. 10 (1): 37–52. doi:10.1353/ppp.2003.0081.
{{cite journal}}: Unknown parameter|month=ignored (help) - Jacquart D. "The Influence of Arabic Medicine in the Medieval West" in Morrison & Rashed 1996, pp. 980 harvnb error: no target: CITEREFMorrisonRashed1996 (help)
- Amber Haque (2004), Psychology from Islamic perspective: Contributions of early Muslim scholars and challenges to contemporary Muslim psychologists, Journal of Religion and Health 43 (4): 357–377 .
- S Safavi-Abbasi, LBC Brasiliense, RK Workman (2007), The fate of medical knowledge and the neurosciences during the time of Genghis Khan and the Mongolian Empire, Neurosurgical Focus 23 (1), E13, p. 3.
- Daly, RW (2007). "Before depression: The medieval vice of acedia". Psychiatry: Interpersonal & Biological Processes. 70 (1): 30–51. doi:10.1521/psyc.2007.70.1.30.
- Merkel, L. (2003) The History of Psychiatry PGY II Lecture Website of the University of Virginia Health System. Retrieved on 2008-08-04
- Kent 2003, p. 55
- "The Anatomy of Melancholy by Robert Burton". Project Gutenberg. Ist April 2004. Retrieved 2008-10-19.
{{cite web}}: Check date values in:|date=(help) - Jackson SW (1983). "Melancholia and mechanical explanation in eighteenth-century medicine". Journal of the History of Medical and Allied Sciences. 38 (3): 298–319. doi:10.1093/jhmas/38.3.298. PMID 6350428.
{{cite journal}}: Unknown parameter|month=ignored (help) - depress. (n.d.). Online Etymology Dictionary. Retrieved June 30, 2008, from Dictionary.com
- Wolpert, L. "Malignant Sadness: The Anatomy of Depression". The New York Times. Retrieved 2008-10-30.
- Berrios GE (1988). "Melancholia and depression during the 19th century: A conceptual history". British Journal of Psychiatry. 153: 298–304. doi:10.1192/bjp.153.3.298. PMID 3074848.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Lewis, AJ (1934). "Melancholia: A historical review". Journal of Mental Science. 80: 1–42. doi:10.1192/bjp.80.328.1.
- ^ Schneider, K (1920). "Zeitschrift für die gesante". Neurol Psychiatr. 59: 281–86.
- Mapother, E (1926). "Discussion of manic-depressive psychosis". British Medical Journal. 2: 872–79.
- Parker 1996, p. 11
- American Psychiatric Association (1968). "Schizophrenia". Diagnostic and statistical manual of mental disorders: DSM-II (PDF). Washington, DC: American Psychiatric Publishing, Inc. Retrieved 2008-08-03.
{{cite book}}: Cite has empty unknown parameter:|unused_data=(help); Text "pp. 36–37, 40" ignored (help) - ^ Parker, G (2007). "Is depression overdiagnosed? Yes". British Medical Journal. 335 (7615): 328. doi:10.1136/bmj.39268.475799.AD. PMID 17703040.
- ^ Parker G (2000). (abstract) "Classifying depression: Should paradigms lost be regained?". American Journal of Psychiatry. 157: 1195–1203. doi:10.1176/appi.ajp.157.8.1195. PMID 10910777.
{{cite journal}}: Check|url=value (help) - Akiskal HS, McKinney WT (1975). "Overview of recent research in depression: Integration of ten conceptual models into a comprehensive clnical frame". Archives of General Psychiatry. 32: 285–305. PMID 1092281.
- Schildkraut, JJ (1965). "The catecholamine hypothesis of affective disorders: A review of supporting evidence". American Journal of Psychiatry. 122 (5): 509–22.
- ^ Philipp M, Maier W, Delmo CD (1991). "The concept of major depression. I. Descriptive comparison of six competing operational definitions including ICD-10 and DSM-III-R". European Archives of Psychiatry and Clinical Neuroscience. 240 (4–5): 258–65. doi:10.1007/BF02189537. PMID 1829000.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Gruenberg, A.M., Goldstein, R.D., Pincus, H.A. (2005) Classification of Depression: Research and Diagnostic Criteria: DSM-IV and ICD-10 (PDF). Wiley.com. Retrieved on October 30, 2008.
- Bolwig, Tom G. (2007). "Melancholia: Beyond DSM, beyond neurotransmitters. Proceedings of a conference, May 2006, Copenhagen, Denmark". Acta Psychiatrica Scandinavica Suppl. 115 (433): 4–183. doi:10.1111/j.1600-0447.2007.00956.x. PMID 17280564.
- Fink M, Bolwig TG, Parker G, Shorter E (2007). "Melancholia: Restoration in psychiatric classification recommended". Acta Psychiatrica Scandinavica. 115 (2): 89–92. doi:10.1111/j.1600-0447.2006.00943.x.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Healy, David. (1999). The Antidepressant Era, Paperback Edition, Harvard University Press. ISBN 0-674-03958-0
- Maloney F (November 3, 2005). "The Depression Wars: Would Honest Abe Have Written the Gettysburg Address on Prozac?". Slate magazine. Retrieved 2008-10-03.
{{cite web}}: Unknown parameter|Publisher=ignored (|publisher=suggested) (help) - Karasz A (2005). "Cultural differences in conceptual models of depression". Social Science in Medicine. 60 (7): 1625–35. doi:10.1016/j.socscimed.2004.08.011. PMID 15652693.
{{cite journal}}: Unknown parameter|month=ignored (help) - Tilbury, F (2004). "There are orphans in Africa still looking for my hands': African women refugees and the sources of emotional distress". Health Sociology Review. 13 (1): 54–64. doi:10.5555/hesr.2004.13.1.54. Retrieved 2008-10-03.
{{cite journal}}: Check|doi=value (help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) - Parker, G (2001). "Depression in the planet's largest ethnic group: The Chinese". American Journal of Psychiatry. 158 (6): 857–64. PMID 11384889.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Pilgrim D, Bentall R (1999). "The medicalisation of misery: A critical realist analysis of the concept of depression". Journal of Mental Health. 8 (3): 261–74. doi:10.1080/09638239917580.
- Klein JM (2007-02-12). "The mind, as it evolves". Los Angeles Times (online). Los Angeles Times. Retrieved 2008-10-03.
- Geoghegan T (2008-02-28). "Is depression good for you?". BBC News Magazine. British Broadcasting Corporation (BBC). Retrieved 2008-10-19.
- Andreasen NC (2008). "The relationship between creativity and mood disorders". Dialogues in clinical neuroscience. 10 (2): 251–5. PMID 18689294. Retrieved 2008-10-31.
- Simonton, DK (2005). "Are genius and madness related? Contemporary answers to an ancient question". Psychiatric Times. 22 (7).
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Mill JS. "A crisis in my mental history: One stage onward". Autobiography (txt). Project Gutenberg EBook. pp. 1826–32. Retrieved 2008-08-09.
- ^ "Churchill's Black Dog?: The History of the 'Black Dog' as a Metaphor for Depression" (PDF). Black Dog Institute website. Black Dog Institute. 2005. Retrieved 2008-08-18.
{{cite web}}: Unknown parameter|month=ignored (help) - "Overview". Black Dog Institute website. Black Dog Institute. 2007. Retrieved 2008-08-18.
{{cite web}}: Unknown parameter|month=ignored (help) - "Henry James". pbs.org. Retrieved 2008-08-19.
- Burlingame, Michael (1997). The Inner World of Abraham Lincoln. Urbana: University of Illinois Press. ISBN 0-252-06667-7.
- Pita E (2001-09-26). "An Intimate Conversation with...Leonard Cohen". Retrieved 2008-10-03.
- Jeste ND, Palmer BW, Jeste DV (2004). "Tennessee Williams". American Journal of Geriatric Psychiatry. 12 (4): 370–75. doi:10.1176/appi.ajgp.12.4.370. PMID 15249274.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ James H (Ed.) (1920). Letters of William James (Vols. 1 and 2). Boston, MA, USA: Atlantic Monthly Press. pp. pp. 147–48.
{{cite book}}:|pages=has extra text (help) - ^ Hergenhahn 2005, p. 311
- Cohen D (1979). J. B. Watson: The Founder of Behaviourism. London, UK: Routledge & Kegan Paul. pp. p. 7. ISBN 0710000545.
{{cite book}}:|pages=has extra text (help)
Cited texts
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, Fourth Edition, Text Revision: DSM-IV-TR. Washington, DC: American Psychiatric Publishing, Inc. p. 943. ISBN 0890420254.
{{cite book}}: CS1 maint: ref duplicates default (link) - Barlow DH (2005). Abnormal psychology: An integrative approach (5th ed.). Belmont, CA, USA: Thomson Wadsworth. ISBN 0534633560.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Kent, Deborah (2003). Snake Pits, Talking Cures & Magic Bullets: A History of Mental Illness. Twenty-First Century Books. ISBN 0761327045.
{{cite book}}: CS1 maint: ref duplicates default (link) - Hergenhahn BR (2005). An Introduction to the History of Psychology (5th edition ed.). Belmont, CA, USA: Thomson Wadsworth. ISBN 0534554016.
{{cite book}}:|edition=has extra text (help) - Parker, Gordon (1996). Melancholia: A disorder of movement and mood: A phenomenological and neurobiological review. Cambridge: Cambridge University Press. ISBN 052147275X.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: ref duplicates default (link) - Sadock, Benjamin J. (2002). Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (9th ed.). Lippincott Williams & Wilkins. ISBN 0781731836.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: ref duplicates default (link)
External links
- DSM-IV Diagnostic Criteria for Major Depressive Disorder - DSM-IV-TR text from mindsite.com
- Template:Dmoz
- National Alliance on Mental Illness – Depression support, advocacy, and education
- National Depressive and Manic Depressive Association - National Depressive and Manic Depressive Association
- Black Dog Institute – Depression and Bipolar Disorder Information Australia
- Depression, out of the shadows - PBS TV program
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||