| Revision as of 00:47, 27 November 2012 editHarizotoh9 (talk | contribs)Extended confirmed users27,250 editsm →Treatment settings← Previous edit | Revision as of 01:23, 27 November 2012 edit undoParkSehJik (talk | contribs)992 edits freudian psychNext edit → | ||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
| {{construction}} | |||
| {{POV}} | |||
| {{pp-move-indef}} | {{pp-move-indef}} | ||
| ]'' comes from the ] for ] or ].<ref></ref> The fluttering insect appears in the ] of Britain's ]<ref>{{Cite journal|last=James|first=F.E.|year=1991|title=Psyche|journal=Psychiatric Bulletin|volume=15|pages=429–431|url=http://pb.rcpsych.org/cgi/reprint/15/7/429.pdf|accessdate=2008-08-04|doi=10.1192/pb.15.7.429|isbn=0-88163-257-0|publisher=Analytic Press|location=Hillsdale, NJ|issue=7}}</ref>]] | ]'' comes from the ] for ] or ].<ref></ref> The fluttering insect appears in the ] of Britain's ]<ref>{{Cite journal|last=James|first=F.E.|year=1991|title=Psyche|journal=Psychiatric Bulletin|volume=15|pages=429–431|url=http://pb.rcpsych.org/cgi/reprint/15/7/429.pdf|accessdate=2008-08-04|doi=10.1192/pb.15.7.429|isbn=0-88163-257-0|publisher=Analytic Press|location=Hillsdale, NJ|issue=7}}</ref>]] | ||
| '''Psychiatry''' is the ] ] devoted to the ] and ] of ]. These mental disorders include various ], ]al, ] and ] ]. The term was first coined by the German ] ] in 1808, and literally means the 'medical treatment of the soul' ('']'': soul; from ] ''psykhē'': soul; '']'': medical treatment; from Gk. ''iātrikos'': medical, ''iāsthai'': to heal). A medical doctor specializing in psychiatry is a ]. | '''Psychiatry''' is the ]{{dubious}} ] devoted to the ]{{dubious}} and ] of ]. These mental disorders include various ], ]al, ] and ] ]. The term was first coined by the German ] ] in 1808, and literally means the 'medical treatment of the soul' ('']'': soul; from ] ''psykhē'': soul; '']'': medical treatment; from Gk. ''iātrikos'': medical, ''iāsthai'': to heal). A medical doctor specializing in psychiatry is a ]. | ||
| <!--The following paragraph, while clearly "in the ballpark" topically, seems nonetheless to "come out of left field" contextually; the diathesis-stress concept obviously is integral to psychiatry, but in its current incarnation it makes for a rather "ambitious" transition between a basic definition of psychiatry (1st paragraph) and a first glance at psychiatry in action (3rd paragraph): "Mental disorders are currently conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience.<ref name=Insel>{{cite journal | author = Insel T.R., Wang P.S. | year = 2010 | title = Rethinking mental illness | url = | journal = JAMA | volume = 303 | issue = 19| pages = 1970–1971 | doi = 10.1001/jama.2010.555 | pmid = 20483974 }}</ref> In other words, the genetics of mental illness may really be the genetics of brain development, with different outcomes possible, depending on the biological and environmental context.<ref name="Insel"/>" | <!--The following paragraph, while clearly "in the ballpark" topically, seems nonetheless to "come out of left field" contextually; the diathesis-stress concept obviously is integral to psychiatry, but in its current incarnation it makes for a rather "ambitious" transition between a basic definition of psychiatry (1st paragraph) and a first glance at psychiatry in action (3rd paragraph): "Mental disorders are currently conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience.<ref name=Insel>{{cite journal | author = Insel T.R., Wang P.S. | year = 2010 | title = Rethinking mental illness | url = | journal = JAMA | volume = 303 | issue = 19| pages = 1970–1971 | doi = 10.1001/jama.2010.555 | pmid = 20483974 }}</ref> In other words, the genetics of mental illness may really be the genetics of brain development, with different outcomes possible, depending on the biological and environmental context.<ref name="Insel"/>" | ||
| Line 9: | Line 11: | ||
| Psychiatric treatment applies a variety of modalities, including ] ], ] and a wide range of other techniques such as ]. Treatment may be delivered on an ] or ] basis, depending on the severity of functional impairment or on other aspects of the disorder in question. Research and treatment within psychiatry as a whole are conducted on an interdisciplinary basis, sourcing an array of sub-specialties and theoretical approaches. | Psychiatric treatment applies a variety of modalities, including ] ], ] and a wide range of other techniques such as ]. Treatment may be delivered on an ] or ] basis, depending on the severity of functional impairment or on other aspects of the disorder in question. Research and treatment within psychiatry as a whole are conducted on an interdisciplinary basis, sourcing an array of sub-specialties and theoretical approaches. | ||
| There is controversy regarding the ] of pscyhiatric determination of presence of ] (mental "disorders"). Peer reviewed published criticism in medical journals goes so far as to state as a fact that "Politics and economics has replaced quality science" in psychiatry.<Ref name=TODDPP/> Unlike ] or even ], psychiatry may use the term “disease” or "disorder" without a systemic ] indicated, i.e. even without any ] and measurable abnormalities in anatomy, chemistry, and physiology hypothesized as causative for mental categories declared by psychiatrists to be diseases or disorders.<Ref name=TODDPP>''"While an operational definition for the term disease is lacking in traditional medicine, consensus indicates that it infers observable and measurable abnormalities in anatomy, chemistry, and physiology as causative for an observed cluster of symptoms. However, the term disease in psychiatry and psychology has a very different historical usage. It has been used when no systemic etiology has been indicated, it has been used politically for addictions, it has been used for the mere belief that a cluster of symptoms must be a disease because the symptoms are bizarre, and it has been used to justify crude medically based treatments, such as electroshock, lobotomies, involuntary commitments, and the sale of powerful drugs. With the advent of new medical machines, such as CAT scans, PET scans, and MRI's, a large volume of poorly conducted and questionable research has been pouring fourth to find diseases as a justification to promote psychotropic drugs. Politics and economics has replaced quality science."'', Toward an Operational Definition of Disease in Psychiatry and Psychology: Implications for Diagnosis and Treatment, David B. Stein, Steve Baldwin, Medicine, Pharmacy and Medical Law and Ethics, International Journal of Risk and Safety in Medicine, Volume 13, Number 1, 2000</ref> Psychiatry may apply the term “disease” politically, for the mere belief that a cluster of symptoms must be a disease because the symptoms are very uncommon, to justify crude its own specialty treatments such as ], to justify ]s, and for financial profit to justify the sale of ] drugs.<Ref name=TODDPP/> Philosopher of science ] cited examples from ] in explaining what counted as a "]".<ref>Popper, Karl (1963) Conjectures and Refutations</ref> ] have been called "]s" so frequently<ref name=IMN>''“The pejorative phrase ‘defendant’s whore’ or ‘prosecutor’s whore’ is '''frequently''' used describing experts who would ‘say anything wants him to say.’”'', 'They’re An Illusion to Me Now': Forensic Ethics, Sanism and Pretextuality, Michael L. Perlin, New York Law School Legal Studies Research Paper Series 07/08 # 27, </ref> that the expression appears in titles of academic publications on the subject.<ref name=CW>"Courtroom Whores" ?--or Why Do Attorneys Call Us? Findings from a Survey on Attorneys' Use of Mental Health Experts, Douglas Mossman & Marshall Kapp, 26 J. American Academy of Academic Psychiatry and the Law, 27 (1998)</ref><ref name=IMN/> | |||
| ==Theory and focus== | ==Theory and focus== | ||
| Line 40: | Line 44: | ||
| ===Approaches=== | ===Approaches=== | ||
| Psychiatric illnesses can be conceptualised in a number of different ways. The ] approach examines signs and symptoms and compares them with diagnostic criteria. Mental illness can be assessed, conversely, through a narrative which tries to incorporate symptoms into a meaningful life history and to frame them as responses to external conditions. Both approaches are important in the field of psychiatry,<ref>{{Cite journal|author=Verhulst J, Tucker G |title=Medical and narrative approaches in psychiatry |journal=Psychiatr Serv |volume=46 |issue=5 |pages=513–514 |year=1995 |month=May |pmid=7627683 |url=http://ps.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=7627683}}</ref> but have not sufficiently reconciled to settle ] over either the selection of a psychiatric ] or the specification of ]. The notion of a "]" is often used to underline the multifactorial nature of clinical impairment.<ref name="McLaren N 1998 86–92; discussion 93–6"/><ref name="McLaren_madness">{{Cite book|title = Humanizing Madness| last = McLaren |first = Niall |year = 2007 |isbn = 1-932690-39-5 |pages = |publisher = Loving Healing Press |location = Ann Arbor, MI}}{{Page needed|date=September 2010}}</ref><ref name="McLaren_psychiatry">{{Cite book|title = Humanizing Psychiatry |last = McLaren |first = Niall |year = 2009 |isbn = 1-61599-011-9|pages = |publisher = Loving Healing Press |location = Ann Arbor, MI}}{{Page needed|date=September 2010}}</ref> Alternatively, a ] acknowledges the physiological basis for the mind's existence, but identifies ] as an ] and independent realm in which disorder may occur.<ref name="McLaren N 1998 86–92; discussion 93–6"/><ref name = "McLaren_madness"/><ref name="McLaren_psychiatry"/> The biocognitive approach includes a ] ] and provides a ] revision of the biopsychosocial view, reflecting the efforts of psychiatrist ] to bring the discipline into scientific maturity in accordance with the paradigmatic standards of ] ].<ref name="McLaren N 1998 86–92; discussion 93–6">{{Cite journal|author=McLaren N |title=A critical review of the biopsychosocial model |journal=The Australian and New Zealand Journal of Psychiatry |volume=32 |issue=1 |pages=86–92; discussion 93–6|year=1998|month=February|pmid=9565189|doi=10.1046/j.1440-1614.1998.00343.x}}</ref><ref name = "McLaren_madness"/><ref name="McLaren_psychiatry"/> | Psychiatric illnesses can be conceptualised in a number of different ways. The ] approach examines signs and symptoms and compares them with diagnostic criteria. Mental illness can be assessed, conversely, through a narrative which tries to incorporate symptoms into a meaningful life history and to frame them as responses to external conditions. Both approaches are important in the field of psychiatry,<ref>{{Cite journal|author=Verhulst J, Tucker G |title=Medical and narrative approaches in psychiatry |journal=Psychiatr Serv |volume=46 |issue=5 |pages=513–514 |year=1995 |month=May |pmid=7627683 |url=http://ps.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=7627683}}</ref> but have not sufficiently reconciled to settle ] over either the selection of a psychiatric ] or the specification of ]. The notion of a "]" is often used to underline the multifactorial nature of clinical impairment.<ref name="McLaren N 1998 86–92; discussion 93–6"/><ref name="McLaren_madness">{{Cite book|title = Humanizing Madness| last = McLaren |first = Niall |year = 2007 |isbn = 1-932690-39-5 |pages = |publisher = Loving Healing Press |location = Ann Arbor, MI}}{{Page needed|date=September 2010}}</ref><ref name="McLaren_psychiatry">{{Cite book|title = Humanizing Psychiatry |last = McLaren |first = Niall |year = 2009 |isbn = 1-61599-011-9|pages = |publisher = Loving Healing Press |location = Ann Arbor, MI}}{{Page needed|date=September 2010}}</ref> Alternatively, a ] acknowledges the physiological basis for the mind's existence, but identifies ] as an ] and independent realm in which disorder may occur.<ref name="McLaren N 1998 86–92; discussion 93–6"/><ref name = "McLaren_madness"/><ref name="McLaren_psychiatry"/> The biocognitive approach includes a ] ] and provides a ] revision of the biopsychosocial view, reflecting the efforts of psychiatrist ] to bring the discipline into scientific maturity in accordance with the paradigmatic standards of ] ].<ref name="McLaren N 1998 86–92; discussion 93–6">{{Cite journal|author=McLaren N |title=A critical review of the biopsychosocial model |journal=The Australian and New Zealand Journal of Psychiatry |volume=32 |issue=1 |pages=86–92; discussion 93–6|year=1998|month=February|pmid=9565189|doi=10.1046/j.1440-1614.1998.00343.x}}</ref><ref name = "McLaren_madness"/><ref name="McLaren_psychiatry"/> | ||
| ⚫ | ===Subspecialties=== | ||
| ⚫ | Various subspecialties and/or theoretical approaches exist which are related to the field of psychiatry. They include the following: | ||
| ⚫ | *]; focuses on evaluation and treatment of individuals with alcohol, drug, or other substance-related disorders, and of individuals with dual diagnosis of substance-related and other psychiatric disorders. | ||
| ⚫ | *]; an approach to psychiatry that aims to understand mental disorders in terms of the biological function of the nervous system. | ||
| ⚫ | *]; the branch of psychiatry that specialises in work with children, teenagers, and their families. | ||
| ⚫ | *]; an approach that reflects an inclusive ] perspective and is practiced in ].<ref>American Association of Community Psychiatrists Retrieved on Aug-05-2008</ref> | ||
| ⚫ | *]; a branch of psychiatry concerned with the cultural and ethnic context of mental disorder and psychiatric services. | ||
| ⚫ | *]; the clinical application of psychiatry in emergency settings. | ||
| ⚫ | *]; the interface between law and psychiatry. | ||
| ⚫ | *]; a branch of psychiatry dealing with the study, prevention, and treatment of mental disorders in humans with old age. | ||
| ⚫ | <!--"Global mental health" sounds like the exact opposite of "psychiatric subspecialty". The content is sourced and seems perfectly suitable for inclusion in this article, but why here in this list?: *]; the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide.<ref name=Patel>{{cite journal | author = Patel V., Prince M. | year = 2010 | title = Global mental health - a new global health field comes of age | url = | journal = JAMA | volume = 303 | issue = 19| pages = 1976–1977 | doi = 10.1001/jama.2010.616 | pmid = 20483977 }}</ref>--> | ||
| ⚫ | *]; the branch of psychiatry that specializes in the interface between other medical specialties and psychiatry. | ||
| ⚫ | *]; covers special aspects of psychiatry and mental disorders within the military context. | ||
| ⚫ | *]; branch of medicine dealing with mental disorders attributable to diseases of the nervous system. | ||
| ⚫ | *]; a branch of psychiatry that focuses on the interpersonal and cultural context of mental disorder and mental wellbeing. | ||
| ⚫ | In the United States, psychiatry is one of the specialties which qualify for further education and board-certification in ], ], and ]. | ||
| ==Industry and academia== | ==Industry and academia== | ||
| Line 81: | Line 67: | ||
| The DSM has attracted praise for standardizing psychiatric diagnostic categories and criteria. It has also attracted controversy and criticism. Some critics argue that the DSM represents an ] system that enshrines the opinions of a few powerful psychiatrists. There are ongoing issues concerning the ] and ] of the diagnostic categories; the reliance on superficial ]; the use of artificial dividing lines between categories and from ']'; possible ] bias; ] of human distress and financial ], including with the practice of psychiatrists and with the ]; political controversies about the inclusion or exclusion of diagnoses from the manual, in general or in regard to specific issues; and the experience of those who are most directly affected by the manual by being diagnosed, including the ].<ref name="concept&evolution">Dalal PK, Sivakumar T. (2009) Indian Journal of Psychiatry, Volume 51, Issue 4, Page 310-319.</ref><ref>{{cite journal | url = http://ajp.psychiatryonline.org/cgi/content/full/160/1/4 | pmid = 12505793 | author-separator =, | author-name-separator= | doi=10.1176/appi.ajp.160.1.4 | volume=160 | issue=1 | year=2003 | month=January | pages=4–12 | title = Distinguishing Between the Validity and Utility of Psychiatric Diagnoses | last1 = Kendell | first1 = R. | journal = American Journal of Psychiatry | last2 = Jablensky | first2 = A}}</ref><ref>{{cite journal | pmid = 17329740 | author-separator =, | author-name-separator= | doi=10.1192/bjp.bp.106.024026 | volume=190 | year=2007 | month=March | pages=210–6 | title = Diagnostic stability of psychiatric disorders in clinical practice | last1 = Baca-Garcia | first1 = E. | last2 = Perez-Rodriguez | first2 = M. M. | last3 = Basurte-Villamor | first3 = I. | last4 = Del Moral | first4 = A. L. F. | last5 = Jimenez-Arriero | first5 = M. A. | last6 = De Rivera | first6 = J. L. G. | last7 = Saiz-Ruiz | first7 = J. | last8 = Oquendo | first8 = M. A. | journal = The British Journal of Psychiatry | issue = 3}}</ref><ref>{{cite journal | last1 = Pincus | first1 = H. A.| author-separator =, | author-name-separator= | year = 1998 | title = Clinical Significance" and DSM-IV | url = http://archpsyc.ama-assn.org/cgi/content/extract/55/12/1145 | journal = Arch Gen Psychiatry | volume = 55 | issue = 12| page = 1145 | pmid = 9862559 | doi = 10.1001/archpsyc.55.12.1145 | last2 = Zarin | first2 = DA | last3 = First | first3 = M | pages = 1145; author reply 1147–8 }}</ref> The publication of the DSM, with tightly guarded copyrights, now makes APA over $5 million a year, historically adding up to over $100 million.<ref>{{cite news| url=http://www.nytimes.com/2012/01/30/opinion/the-dsms-troubled-revision.html | work=The New York Times | first=Gary | last=Greenberg | title=The D.S.M.'s Troubled Revision | date=January 29, 2012}}</ref> | The DSM has attracted praise for standardizing psychiatric diagnostic categories and criteria. It has also attracted controversy and criticism. Some critics argue that the DSM represents an ] system that enshrines the opinions of a few powerful psychiatrists. There are ongoing issues concerning the ] and ] of the diagnostic categories; the reliance on superficial ]; the use of artificial dividing lines between categories and from ']'; possible ] bias; ] of human distress and financial ], including with the practice of psychiatrists and with the ]; political controversies about the inclusion or exclusion of diagnoses from the manual, in general or in regard to specific issues; and the experience of those who are most directly affected by the manual by being diagnosed, including the ].<ref name="concept&evolution">Dalal PK, Sivakumar T. (2009) Indian Journal of Psychiatry, Volume 51, Issue 4, Page 310-319.</ref><ref>{{cite journal | url = http://ajp.psychiatryonline.org/cgi/content/full/160/1/4 | pmid = 12505793 | author-separator =, | author-name-separator= | doi=10.1176/appi.ajp.160.1.4 | volume=160 | issue=1 | year=2003 | month=January | pages=4–12 | title = Distinguishing Between the Validity and Utility of Psychiatric Diagnoses | last1 = Kendell | first1 = R. | journal = American Journal of Psychiatry | last2 = Jablensky | first2 = A}}</ref><ref>{{cite journal | pmid = 17329740 | author-separator =, | author-name-separator= | doi=10.1192/bjp.bp.106.024026 | volume=190 | year=2007 | month=March | pages=210–6 | title = Diagnostic stability of psychiatric disorders in clinical practice | last1 = Baca-Garcia | first1 = E. | last2 = Perez-Rodriguez | first2 = M. M. | last3 = Basurte-Villamor | first3 = I. | last4 = Del Moral | first4 = A. L. F. | last5 = Jimenez-Arriero | first5 = M. A. | last6 = De Rivera | first6 = J. L. G. | last7 = Saiz-Ruiz | first7 = J. | last8 = Oquendo | first8 = M. A. | journal = The British Journal of Psychiatry | issue = 3}}</ref><ref>{{cite journal | last1 = Pincus | first1 = H. A.| author-separator =, | author-name-separator= | year = 1998 | title = Clinical Significance" and DSM-IV | url = http://archpsyc.ama-assn.org/cgi/content/extract/55/12/1145 | journal = Arch Gen Psychiatry | volume = 55 | issue = 12| page = 1145 | pmid = 9862559 | doi = 10.1001/archpsyc.55.12.1145 | last2 = Zarin | first2 = DA | last3 = First | first3 = M | pages = 1145; author reply 1147–8 }}</ref> The publication of the DSM, with tightly guarded copyrights, now makes APA over $5 million a year, historically adding up to over $100 million.<ref>{{cite news| url=http://www.nytimes.com/2012/01/30/opinion/the-dsms-troubled-revision.html | work=The New York Times | first=Gary | last=Greenberg | title=The D.S.M.'s Troubled Revision | date=January 29, 2012}}</ref> | ||
| ⚫ | ===Subspecialties=== | ||
| ⚫ | Various subspecialties and/or theoretical approaches exist which are related to the field of psychiatry. They include the following: | ||
| ⚫ | *]; focuses on evaluation and treatment of individuals with alcohol, drug, or other substance-related disorders, and of individuals with dual diagnosis of substance-related and other psychiatric disorders. | ||
| ⚫ | *]; an approach to psychiatry that aims to understand mental disorders in terms of the biological function of the nervous system. | ||
| ⚫ | *]; the branch of psychiatry that specialises in work with children, teenagers, and their families. | ||
| ⚫ | *]; an approach that reflects an inclusive ] perspective and is practiced in ].<ref>American Association of Community Psychiatrists Retrieved on Aug-05-2008</ref> | ||
| ⚫ | *]; a branch of psychiatry concerned with the cultural and ethnic context of mental disorder and psychiatric services. | ||
| ⚫ | *]; the clinical application of psychiatry in emergency settings. | ||
| ⚫ | *]; the interface between law and psychiatry. | ||
| ⚫ | *]; a branch of psychiatry dealing with the study, prevention, and treatment of mental disorders in humans with old age. | ||
| ⚫ | <!--"Global mental health" sounds like the exact opposite of "psychiatric subspecialty". The content is sourced and seems perfectly suitable for inclusion in this article, but why here in this list?: *]; the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide.<ref name=Patel>{{cite journal | author = Patel V., Prince M. | year = 2010 | title = Global mental health - a new global health field comes of age | url = | journal = JAMA | volume = 303 | issue = 19| pages = 1976–1977 | doi = 10.1001/jama.2010.616 | pmid = 20483977 }}</ref>--> | ||
| ⚫ | *]; the branch of psychiatry that specializes in the interface between other medical specialties and psychiatry. | ||
| ⚫ | *]; covers special aspects of psychiatry and mental disorders within the military context. | ||
| ⚫ | *]; branch of medicine dealing with mental disorders attributable to diseases of the nervous system. | ||
| ⚫ | *]; a branch of psychiatry that focuses on the interpersonal and cultural context of mental disorder and mental wellbeing. | ||
| ⚫ | In the United States, psychiatry is one of the specialties which qualify for further education and board-certification in ], ], and ]. | ||
| ====Treatment settings==== | ====Treatment settings==== | ||
| {{Cleanup-rewrite|2=section|date=May 2009}} | {{Cleanup-rewrite|2=section|date=May 2009}} | ||
| ==General considerations== | =====General considerations===== | ||
| Individuals with mental health conditions are commonly referred to as '']s'' but may also be called '']s'', '']s'', or ''service recipients''. They may come under the care of a psychiatric physician or other psychiatric practitioners by various paths, the two most common being self-] or referral by a primary-care physician. Alternatively, a person may be referred by hospital medical staff, by ], ], or, in the UK and Australia, by ] under a ]. | Individuals with mental health conditions are commonly referred to as '']s'' but may also be called '']s'', '']s'', or ''service recipients''. They may come under the care of a psychiatric physician or other psychiatric practitioners by various paths, the two most common being self-] or referral by a primary-care physician. Alternatively, a person may be referred by hospital medical staff, by ], ], or, in the UK and Australia, by ] under a ]. | ||
| ] | ] | ||
| Line 124: | Line 129: | ||
| ===Early modern period=== | ===Early modern period=== | ||
| In 1656, ] created a public system of hospitals for those suffering from mental disorders, but as in England, no real treatment was applied.<ref name= Shorter5/> In 1713 the Bethel Hospital Norwich was opened, the first purpose-built asylum in England, founded by Mary Chapman |
In 1656, ] created a public system of hospitals for those suffering from mental disorders, but as in England, no real treatment was applied.<ref name= Shorter5/> In 1713 the Bethel Hospital Norwich was opened, the first purpose-built asylum in England, founded by Mary Chapman . In 1758 English physician ] wrote his '']'' which called for treatments to be utilized in asylums.<ref name=Shorter9>Shorter, E. (1997), p. 9</ref> Thirty years later, then ruling monarch in England ] was known to be suffering from a mental disorder.<ref name= Elkes13/> Following the King's ] in 1789, mental illness came to be seen as something which could be treated and cured.<ref name=Elkes13/> The French doctor ] introduced ] approaches to those suffering from mental disorders.<ref name=Elkes13/> As a result of his work, the Governor of the Bicêtre ] in Paris released psychiatric patients from their chains in 1793, beginning what has been called the ''bright epoch of psychiatry''.<ref name="bukelic">{{cite book|last=Bukelic |first=Jovan|title=Neuropsihijatrija za III razred medicinske skole|editor=Mirjana Jovanovic|publisher=Zavod za udzbenike i nastavna sredstva|location=Belgrade |date=1995|edition=7th|pages=7|chapter=2|isbn=86-17-03418-1|accessdate=27 July 2011|language=Serbian}}</ref> At the York Retreat, a Quaker-run asylum in England which opened in 1796, a form of ] evolved independently from Pinel under the lay stewardship of the tea and coffee merchant ].<ref name="Cherry">{{citation|last=Cherry|first=Charles L.|title=A Quiet Haven: Quakers, Moral Treatment, and Asylum Reform|location=London & Toronto|publisher=Associated University Presses|year=1989}}</ref>{{rp|84-85|}} <ref name="Digby">{{citation|last=Digby|first=Anne|title=Madness, Morality and Medicine: A Study of the York Retreat|location=Cambridge|publisher=Cambridge University Press|date=1983}}</ref>{{rp|30}} <ref name="Glover">{{citation|last=Glover|first=Mary R.|title=The Retreat, York: An Early Experiment in the Treatment of Mental Illness|location=York|publisher=Ebor Press|date=1984}}</ref>{{rp|53}} Tuke's Retreat became a model throughout the world for humane and moral treatment of patients suffering from mental disorders.<ref name=Borthwick>{{cite journal | author = Borthwick A., Holman C., Kennard D., McFetridge M., Messruther K., Wilkes J. | year = 2001 | title = The relevance of moral treatment to contemporary mental health care | url = | journal = Journal of Mental Health | volume = 10 | issue = 4| pages = 427–439 | doi=10.1080/09638230124277}}</ref> The York Retreat inspired similar institutions in the United States, most notably the ] and the Hartford Retreat (now the ]). | ||
| ===19th century=== | ===19th century=== | ||
Revision as of 01:23, 27 November 2012
| This article or section is in a state of significant expansion or restructuring. You are welcome to assist in its construction by editing it as well. If this article or section has not been edited in several days, please remove this template. If you are the editor who added this template and you are actively editing, please be sure to replace this template with {{in use}} during the active editing session. Click on the link for template parameters to use.
This article was last edited by ParkSehJik (talk | contribs) 12 years ago. (Update timer) |
| The neutrality of this article is disputed. Relevant discussion may be found on the talk page. Please do not remove this message until conditions to do so are met. (Learn how and when to remove this message) |

Psychiatry is the medical specialty devoted to the Biomedical research and treatment of mental disorders. These mental disorders include various affective, behavioural, cognitive and perceptual abnormalities. The term was first coined by the German physician Johann Christian Reil in 1808, and literally means the 'medical treatment of the soul' (psych-: soul; from Ancient Greek psykhē: soul; -iatry: medical treatment; from Gk. iātrikos: medical, iāsthai: to heal). A medical doctor specializing in psychiatry is a psychiatrist.
Psychiatric assessment typically starts with a mental status examination and the compilation of a case history. Psychological tests and physical examinations may be conducted, including on occasion the use of neuroimaging or other neurophysiological techniques. Mental disorders are diagnosed in accordance with criteria listed in diagnostic manuals such as the widely used Diagnostic and Statistical Manual of Mental Disorders (DSM), published by the American Psychiatric Association, and the International Classification of Diseases (ICD), edited and used by the World Health Organization. The fifth edition of the DSM (DSM-5) is scheduled to be published in 2013, and its development is expected to be of significant interest to many medical fields.
Psychiatric treatment applies a variety of modalities, including psychoactive medication, psychotherapy and a wide range of other techniques such as transcranial magnetic stimulation. Treatment may be delivered on an inpatient or outpatient basis, depending on the severity of functional impairment or on other aspects of the disorder in question. Research and treatment within psychiatry as a whole are conducted on an interdisciplinary basis, sourcing an array of sub-specialties and theoretical approaches.
There is controversy regarding the scientific validity of pscyhiatric determination of presence of disease (mental "disorders"). Peer reviewed published criticism in medical journals goes so far as to state as a fact that "Politics and economics has replaced quality science" in psychiatry. Unlike evidence based medicine or even traditional medicine, psychiatry may use the term “disease” or "disorder" without a systemic etiology indicated, i.e. even without any observable and measurable abnormalities in anatomy, chemistry, and physiology hypothesized as causative for mental categories declared by psychiatrists to be diseases or disorders. Psychiatry may apply the term “disease” politically, for the mere belief that a cluster of symptoms must be a disease because the symptoms are very uncommon, to justify crude its own specialty treatments such as lobotomies, to justify involuntary commitments, and for financial profit to justify the sale of psychotropic drugs. Philosopher of science Karl Popper cited examples from Freudian psychiatry in explaining what counted as a "pseudoscience". Forensic psychiatrists have been called "whores" so frequently that the expression appears in titles of academic publications on the subject.
Theory and focus
"Psychiatry, more than any other branch of medicine, forces its practitioners to wrestle with the nature of evidence, the validity of introspection, problems in communication, and other long-standing philosophical issues" (Guze, 1992, p.4).
Psychiatry refers to a field of medicine focused specifically on the mind, aiming to study, prevent, and treat mental disorders in humans. It has been described as an intermediary between the world from a social context and the world from the perspective of those who are mentally ill.
Those who specialize in psychiatry are different than most other mental health professionals and physicians in that they must be familiar with both the social and biological sciences. The discipline is interested in the operations of different organs and body systems as classified by the patient's subjective experiences and the objective physiology of the patient. Psychiatry exists to treat mental disorders which are conventionally divided into three very general categories: mental illness, severe learning disability, and personality disorder. While the focus of psychiatry has changed little throughout time, the diagnostic and treatment processes have evolved dramatically and continue to do so. Since the late 20th century, the field of psychiatry has continued to become more biological and less conceptually isolated from the field of medicine.
Scope of practice

While the medical specialty of psychiatry utilizes research in the field of neuroscience, psychology, medicine, biology, biochemistry, and pharmacology, it has generally been considered a middle ground between neurology and psychology. Unlike other physicians and neurologists, psychiatrists specialize in the doctor-patient relationship and are trained to varying extents in the use of psychotherapy and other therapeutic communication techniques. Psychiatrists also differ from psychologists in that they are physicians and only their residency training (usually 3 to 4 years) is in psychiatry, and their graduate medical training is identical to all other physicians. Psychiatrists can therefore counsel patients, prescribe medication, order laboratory tests, order neuroimaging, and conduct physical examinations.
Ethics
Like other purveyors of professional ethics, the World Psychiatric Association issues an ethical code to govern the conduct of psychiatrists. The psychiatric code of ethics, first set forth through the Declaration of Hawaii in 1977, has been expanded through a 1983 Vienna update and, in 1996, the broader Madrid Declaration. The code was further revised in Hamburg, 1999. The World Psychiatric Association code covers such matters as patient assessment, up-to-date knowledge, the human dignity of incapacitated patients, confidentiality, research ethics, sex selection, euthanasia, organ transplantation, torture, the death penalty, media relations, genetics, and ethnic or cultural discrimination. In establishing such ethical codes, the profession has responded to a number of controversies about the practice of psychiatry.
Approaches
Psychiatric illnesses can be conceptualised in a number of different ways. The biomedical approach examines signs and symptoms and compares them with diagnostic criteria. Mental illness can be assessed, conversely, through a narrative which tries to incorporate symptoms into a meaningful life history and to frame them as responses to external conditions. Both approaches are important in the field of psychiatry, but have not sufficiently reconciled to settle controversy over either the selection of a psychiatric paradigm or the specification of psychopathology. The notion of a "biopsychosocial model" is often used to underline the multifactorial nature of clinical impairment. Alternatively, a "biocognitive model" acknowledges the physiological basis for the mind's existence, but identifies cognition as an irreducible and independent realm in which disorder may occur. The biocognitive approach includes a mentalist etiology and provides a dualist revision of the biopsychosocial view, reflecting the efforts of psychiatrist Niall McLaren to bring the discipline into scientific maturity in accordance with the paradigmatic standards of philosopher Thomas Kuhn.
Industry and academia
Practitioners
Main article: PsychiatristAll physicians can diagnose mental disorders and prescribe treatments utilizing principles of psychiatry. Psychiatrists are either: 1) clinicians who specialize in psychiatry and are certified in treating mental illness; or (2) scientists in the academic field of psychiatry who are qualified as research doctors in this field. Psychiatrists may also go through significant training to conduct psychotherapy, psychoanalysis and cognitive behavioral therapy, but it is their training as physicians that differentiates them from other mental health professionals.
Research

Psychiatric research is, by its very nature, interdisciplinary. It combines social, biological and psychological perspectives to understand the nature and treatment of mental disorders. Clinical and research psychiatrists study basic and clinical psychiatric topics at research institutions and publish articles in journals. Under the supervision of institutional review boards, psychiatric clinical researchers look at topics such as neuroimaging, genetics, and psychopharmacology in order to enhance diagnostic validity and reliability, to discover new treatment methods, and to classify new mental disorders.
Clinical application
Diagnostic systems
See also Diagnostic classification and rating scales used in psychiatry

Psychiatric diagnoses take place in a wide variety of settings and are performed by many different health professionals. Therefore, the diagnostic procedure may vary greatly based upon these factors. Typically, though, a psychiatric diagnosis utilizes a differential diagnosis procedure where a mental status examination and physical examination is conducted, pathological, psychopathological or psychosocial histories obtained, and sometimes neuroimages or other neurophysiological measurements are taken, or personality tests or cognitive tests administered. In some cases, a brain scan might be used to rule out other medical illnesses, but at this time relying on brain scans alone cannot accurately diagnose a mental illness or tell the risk of getting a mental illness in the future. A few psychiatrists are beginning to utilize genetics during the diagnostic process but on the whole this remains a research topic.
Diagnostic manuals
See also: Diagnostic and Statistical Manual of Mental DisordersThree main diagnostic manuals used to classify mental health conditions are in use today. The ICD-10 is produced and published by the World Health Organisation, includes a section on psychiatric conditions, and is used worldwide. The Diagnostic and Statistical Manual of Mental Disorders, produced and published by the American Psychiatric Association, is primarily focused on mental health conditions and is the main classification tool in the United States. It is currently in its fourth revised edition and is also used worldwide. The Chinese Society of Psychiatry has also produced a diagnostic manual, the Chinese Classification of Mental Disorders.
The stated intention of diagnostic manuals is typically to develop replicable and clinically useful categories and criteria, to facilitate consensus and agreed upon standards, whilst being atheoretical as regards etiology. However, the categories are nevertheless based on particular psychiatric theories and data; they are broad and often specified by numerous possible combinations of symptoms, and many of the categories overlap in symptomology or typically occur together. While originally intended only as a guide for experienced clinicians trained in its use, the nomenclature is now widely used by clinicians, administrators and insurance companies in many countries.
The DSM has attracted praise for standardizing psychiatric diagnostic categories and criteria. It has also attracted controversy and criticism. Some critics argue that the DSM represents an unscientific system that enshrines the opinions of a few powerful psychiatrists. There are ongoing issues concerning the validity and reliability of the diagnostic categories; the reliance on superficial symptoms; the use of artificial dividing lines between categories and from 'normality'; possible cultural bias; medicalization of human distress and financial conflicts of interest, including with the practice of psychiatrists and with the pharmaceutical industry; political controversies about the inclusion or exclusion of diagnoses from the manual, in general or in regard to specific issues; and the experience of those who are most directly affected by the manual by being diagnosed, including the consumer/survivor movement. The publication of the DSM, with tightly guarded copyrights, now makes APA over $5 million a year, historically adding up to over $100 million.
Subspecialties
Various subspecialties and/or theoretical approaches exist which are related to the field of psychiatry. They include the following:
- Addiction psychiatry; focuses on evaluation and treatment of individuals with alcohol, drug, or other substance-related disorders, and of individuals with dual diagnosis of substance-related and other psychiatric disorders.
- Biological psychiatry; an approach to psychiatry that aims to understand mental disorders in terms of the biological function of the nervous system.
- Child and adolescent psychiatry; the branch of psychiatry that specialises in work with children, teenagers, and their families.
- Community psychiatry; an approach that reflects an inclusive public health perspective and is practiced in community mental health services.
- Cross-cultural psychiatry; a branch of psychiatry concerned with the cultural and ethnic context of mental disorder and psychiatric services.
- Emergency psychiatry; the clinical application of psychiatry in emergency settings.
- Forensic psychiatry; the interface between law and psychiatry.
- Geriatric psychiatry; a branch of psychiatry dealing with the study, prevention, and treatment of mental disorders in humans with old age.
- Liaison psychiatry; the branch of psychiatry that specializes in the interface between other medical specialties and psychiatry.
- Military psychiatry; covers special aspects of psychiatry and mental disorders within the military context.
- Neuropsychiatry; branch of medicine dealing with mental disorders attributable to diseases of the nervous system.
- Social psychiatry; a branch of psychiatry that focuses on the interpersonal and cultural context of mental disorder and mental wellbeing.
In the United States, psychiatry is one of the specialties which qualify for further education and board-certification in pain medicine, palliative medicine, and sleep medicine.
Treatment settings
| This section may need to be rewritten to comply with Misplaced Pages's quality standards. You can help. The talk page may contain suggestions. (May 2009) |
General considerations
Individuals with mental health conditions are commonly referred to as patients but may also be called clients, consumers, or service recipients. They may come under the care of a psychiatric physician or other psychiatric practitioners by various paths, the two most common being self-referral or referral by a primary-care physician. Alternatively, a person may be referred by hospital medical staff, by court order, involuntary commitment, or, in the UK and Australia, by sectioning under a mental health law.

Persons who undergo a psychiatric assessment are evaluated by a psychiatrist for their mental and physical condition. This usually involves interviewing the person and often obtaining information from other sources such as other health and social care professionals, relatives, associates, law enforcement personnel, emergency medical personnel, and psychiatric rating scales. A mental status examination is carried out, and a physical examination is usually performed to establish or exclude other illnesses that may be contributing to the alleged psychiatric problems. A physical examination may also serve to identify any signs of self-harm; this examination is often performed by someone other than the psychiatrist, especially if blood tests and medical imaging are performed.
Like most medications, psychiatric medications can cause adverse effects in patients, and some require ongoing therapeutic drug monitoring, for instance full blood counts or, for patients taking lithium salts, serum levels of lithium, renal function, and thyroid function. Electroconvulsive therapy (ECT) is sometimes administered for serious and disabling conditions, such as those unresponsive to medication. The efficacy and adverse effects of psychiatric drugs may vary from patient to patient. Some groups that oppose psychiatry question the use of many of these drugs.
The close relationship between those prescribing psychiatric medication and pharmaceutical companies is a source of concern for some, particularly anti-psychiatry advocates. Also, such advocates are prone to questioning the influence which pharmaceutical companies are exerting on mental health policies.
For many years, controversy has surrounded the forced drugging and the "lack of insight" label of patients with severe psychiatric symptoms who resist treatment. Involuntary treatment is extremely rare outside the psychiatric system, allowable only in such cases as unconsciousness or the inability to communicate. People with psychiatric disabilities, on the other hand, may be forced to accept treatment even when vigorously protested against by the patient. Frequently those who resist treatment and are forced into it are labeled as having a "lack insight" into the seriousness of their problems and the treatment that their symptoms require. Thus, anti-psychiatry advocates conclude that "lack of insight" is often synonymous with being disagreeable toward the treating professional, and that people who disagree are labeled as noncompliant or uncooperative with necessary treatment.
Inpatient treatment
Psychiatric treatments have changed over the past several decades. In the past, psychiatric patients were often hospitalized for six months or more, with some cases involving hospitalization for many years. Today, people receiving psychiatric treatment are more likely to be seen as outpatients. If hospitalization is required, the average hospital stay is around one to two weeks, with only a small number receiving long-term hospitalization.
Psychiatric inpatients are people admitted to a hospital or clinic to receive psychiatric care. Some are admitted involuntarily, perhaps committed to a secure hospital, or in some jurisdictions to a facility within the prison system. In many countries including the USA and Canada, the criteria for involuntary admission vary with local jurisdiction. They may be as broad as having a mental health condition, or as narrow as being an immediate danger to themselves and/or others. Bed availability is often the real determinant of admission decisions to hard pressed public facilities. European Human Rights legislation restricts detention to medically certified cases of mental disorder, and adds a right to timely judicial review of detention.

Patients may be admitted voluntarily if the treating doctor considers that safety isn't compromised by this less restrictive option. Inpatient psychiatric wards may be secure (for those thought to have a particular risk of violence or self-harm) or unlocked/open. Some wards are mixed-sex whilst same-sex wards are increasingly favored to protect women inpatients. Once in the care of a hospital, people are assessed, monitored, and often given medication and care from a multidisciplinary team, which may include physicians, pharmacists, psychiatric nurse practitioners, psychiatric nurses, clinical psychologists, psychotherapists, psychiatric social workers, occupational therapists and social workers. If a person receiving treatment in a psychiatric hospital is assessed as at particular risk of harming themselves or others, they may be put on constant or intermittent one-to-one supervision, and may be physically restrained or medicated. People on inpatient wards may be allowed leave for periods of time, either accompanied or on their own.
In many developed countries there has been a massive reduction in psychiatric beds since the mid 20th century, with the growth of community care. Standards of inpatient care remain a challenge in some public and private facilities, due to levels of funding, and facilities in developing countries are typically grossly inadequate for the same reason.
Outpatient treatment
People may receive psychiatric care on an inpatient or outpatient basis. Outpatient treatment involves periodic visits to a clinician for consultation in his or her office, usually for an appointment lasting thirty to sixty minutes. These consultations normally involve the psychiatric practitioner interviewing the person to update their assessment of the person's condition, and to provide psychotherapy or review medication. The frequency with which a psychiatric practitioner sees people in treatment varies widely, from days to months, depending on the type, severity and stability of each person's condition, and depending on what the clinician and client decide would be best. Increasingly, psychiatrists are limiting their practices to psychopharmacology (prescribing medications) with little or no time devoted to psychotherapy or "talk" therapies, or behavior modification. Psychiatrists who serve the lower end of the market, which is dependent on insurance reimbursements, do not receive insurance payments for lengthy psychotherapy sessions which is competitive with that offered for the brief consultations needed for prescribing and monitoring medication. Psychotherapy in such situations is performed by a lower paid psychologist or social worker. The role of psychiatrists is changing in community psychiatry, with many assuming more leadership roles, coordinating and supervising teams of allied health professionals and junior doctors in delivery of health services.
History
Ancient
Although one may trace its germination to the late eighteenth century, the beginning of psychiatry as a medical specialty is dated to the middle of the nineteenth century. Starting in the 5th century BCE, mental disorders, especially those with psychotic traits, were considered supernatural in origin. This view existed throughout ancient Greece and Rome. Early manuals about mental disorders were created by the Greeks. In the 4th century BCE, Hippocrates theorized that physiological abnormalities may be the root of mental disorders. Religious leaders often turned to versions of exorcism to treat mental disorders often utilizing cruel and barbaric methods.
Middle Ages
Main article: Islamic psychologySpecialist hospitals were built in Baghdad in 705 AD, followed by Fes in the early 8th century, and Cairo in 800 AD.
Physicians who wrote on mental disorders and their treatment in the Medieval Islamic period included Muhammad ibn Zakarīya Rāzi (Rhazes), the Arab physician Najab ud-din Muhammad, and Abu Ali al-Hussain ibn Abdallah ibn Sina, known in the West as Avicenna.
Specialist hospitals were built in medieval Europe from the 13th century to treat mental disorders but were utilized only as custodial institutions and did not provide any type of treatment. Founded in the 13th century, Bethlem Royal Hospital in London is one of the oldest lunatic asylums. By 1547 the City of London acquired the hospital and continued its function until 1948. It is now part of the National Health Service and is an NHS Foundation Trust.

Early modern period
In 1656, Louis XIV of France created a public system of hospitals for those suffering from mental disorders, but as in England, no real treatment was applied. In 1713 the Bethel Hospital Norwich was opened, the first purpose-built asylum in England, founded by Mary Chapman . In 1758 English physician William Battie wrote his Treatise on Madness which called for treatments to be utilized in asylums. Thirty years later, then ruling monarch in England George III was known to be suffering from a mental disorder. Following the King's remission in 1789, mental illness came to be seen as something which could be treated and cured. The French doctor Philippe Pinel introduced humane treatment approaches to those suffering from mental disorders. As a result of his work, the Governor of the Bicêtre psychiatric hospital in Paris released psychiatric patients from their chains in 1793, beginning what has been called the bright epoch of psychiatry. At the York Retreat, a Quaker-run asylum in England which opened in 1796, a form of moral treatment evolved independently from Pinel under the lay stewardship of the tea and coffee merchant William Tuke. Tuke's Retreat became a model throughout the world for humane and moral treatment of patients suffering from mental disorders. The York Retreat inspired similar institutions in the United States, most notably the Brattleboro Retreat and the Hartford Retreat (now the Institute of Living).
19th century
In 1808, Johann Christian Reil coined the term psychiatry (Greek "ψυχιατρική", psychiatrikē) which comes from the Greek "ψυχή" (psychē: "soul or mind") and "ιατρός" (iatros: "healer"). At the turn of the century, England and France combined had only a few hundred individuals in asylums. By the late 1890s and early 1900s, this number had risen to the hundreds of thousands. The United States housed 150,000 patients in mental hospitals by 1904. German speaking countries housed more than 400 public and private sector asylums. These asylums were critical to the evolution of psychiatry as they provided places of practice throughout the world.
On continental Europe, universities often played a part in the administration of the asylums and, because of the relationship between the universities and asylums, scores of psychiatrists were being educated in Germany.. However, because of Germany's individual states and the lack of national regulation of asylums, the country had no organized centralization of asylums or psychiatry. The United Kingdom, unlike Germany, possessed a national body for asylum superintendents - the Medico-Psychological Association - established in 1866 under the Presidency of William A.F. Browne.
In the United States in 1834 Anna Marsh, a physician's widow, deeded the funds to build her country's first financially stable private asylum. The Brattleboro Retreat marked the beginning of America's private psychiatric hospitals challenging state institutions for patients, funding, and influence. Although based on England's York Retreat, it would be followed by specialty institutions of every treatment philosophy.
In 1838, France enacted a law to regulate both the admissions into asylums and asylum services across the country. This was the year in which William A.F. Browne achieved his appointment as Superintendent of the Crichton Royal at Dumfries in southern Scotland.

However, the new idea that mental illness could be ameliorated during the mid-nineteenth century were disappointed. Psychiatrists were pressured by an ever increasing patient population. The average number of patients in asylums in the United States jumped 927%. Numbers were similar in England and Germany. Overcrowding was rampant in France where asylums would commonly take in double their maximum capacity. Increases in asylum populations may have been a result of the transfer of care from families and poorhouses, but the specific reasons as to why the increase occurred is still debated today. No matter the cause, the pressure on asylums from the increase was taking its toll on the asylums and psychiatry as a specialty. Asylums were once again turning into custodial institutions and the reputation of psychiatry in the medical world had hit an extreme low.
20th century
Disease classification and rebirth of biological psychiatry
The 20th century introduced a new psychiatry into the world. Different perspectives of looking at mental disorders began to be introduced. The career of Emil Kraepelin reflects the convergence of different disciplines in psychiatry. Kraepelin initially was very attracted to psychology and ignored the ideas of anatomical psychiatry. Following his appointment to a professorship of psychiatry and his work in a university psychiatric clinic, Kraepelin's interest in pure psychology began to fade and he introduced a plan for a more comprehensive psychiatry. Kraepelin began to study and promote the ideas of disease classification for mental disorders, an idea introduced by Karl Ludwig Kahlbaum. The initial ideas behind biological psychiatry, stating that the different mental disorders were all biological in nature, evolved into a new concept of "nerves" and psychiatry became a rough approximation of neurology and neuropsychiatry. However, Kraepelin was criticized for considering schizophrenia as a biological illness in the absence of any detectable histologic or anatomic abnormalities. While Kraepelin tried to find organic causes of mental illness, he adopted many theses of positivist medicine, but he favoured the precision of nosological classification over the indefiniteness of etiological causation as his basic mode of psychiatric explanation.
Following Sigmund Freud's death, ideas stemming from psychoanalytic theory also began to take root. The psychoanalytic theory became popular among psychiatrists because it allowed the patients to be treated in private practices instead of warehoused in asylums. By the 1970s the psychoanalytic school of thought had become marginalized within the field.
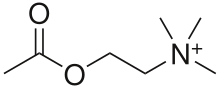
Biological psychiatry reemerged during this time. Psychopharmacology became an integral part of psychiatry starting with Otto Loewi's discovery of the neuromodulatory properties of acetylcholine; thus identifying it as the first-known neurotransmitter. Neuroimaging was first utilized as a tool for psychiatry in the 1980s. The discovery of chlorpromazine's effectiveness in treating schizophrenia in 1952 revolutionized treatment of the disease, as did lithium carbonate's ability to stabilize mood highs and lows in bipolar disorder in 1948. Psychotherapy was still utilized, but as a treatment for psychosocial issues. In the 1920s and 1930s, most asylum and academic psychiatrists in Europe believed that manic depressive disorder and schizophrenia were inherited, but in the decades after World War II, the conflation of genetics with Nazi racist ideology thoroughly discredited genetics. Now genetics were once again thought to play a role in mental illness. Molecular biology opened the door for specific genes contributing to mental disorders to be identified.
Transinstitutionalization and the aftermath
In 1963, US president John F. Kennedy introduced legislation delegating the National Institute of Mental Health to administer Community Mental Health Centers for those being discharged from state psychiatric hospitals. Later, though, the Community Mental Health Center's focus was diverted to provide psychotherapy sessions for those suffering from acute but mild mental disorders. Ultimately there were no arrangements made for actively and severely mentally ill patients who were being discharged from hospitals. Some of those suffering from mental disorders drifted into homelessness or ended up in prisons and jails. Studies found that 33% of the homeless population and 14% of inmates in prisons and jails were already diagnosed with a mental illness.
In 1973, psychologist David Rosenhan published the Rosenhan experiment, a study with results that led to questions about the validity of psychiatric diagnoses. Critics such as Robert Spitzer placed doubt on the validity and credibility of the study, but did concede that the consistency of psychiatric diagnoses needed improvement.
Psychiatry, like most medical specialties has a continuing, significant need for research into its diseases, classifications and treatments. Psychiatry adopts biology's fundamental belief that disease and health are different elements of an individual's adaptation to an environment. But psychiatry also recognizes that the environment of the human species is complex and includes physical, cultural, and interpersonal elements. In addition to external factors, the human brain must contain and organize an individual's hopes, fears, desires, fantasies and feelings. Psychiatry's difficult task is to bridge the understanding of these factors so that they can be studied both clinically and physiologically.
Ethical and legal issues
Anti-psychiatry and deinstitutionalization
Main article: Anti-psychiatryThe introduction of psychiatric medications and the use of laboratory tests altered the doctor-patient relationship between psychiatrists and their patients. Psychiatry's shift to the hard sciences had been interpreted as a lack of concern for patients. Anti-psychiatry had become more prevalent in the late twentieth century due to this and publications in the media which conceptualized mental disorders as myths. Others in the movement argued that psychiatry was a form of social control and demanded that institutionalized psychiatric care, stemming from Pinel's thereapeutic asylum, be abolished.
Electroconvulsive therapy (ECT) was one treatment that the anti-psychiatry movement wanted eliminated. They alleged that ECT damaged the brain and was used as a tool for discipline. While some believe there is no evidence that ECT damages the brain, there are some citations that ECT does cause damage. Sometimes ECT is used as punishment or as a threat and there have been isolated incidents where the use of ECT was threatened to keep the patients "in line". The prevalence of psychiatric medication helped initiate deinstitutionalization, the process of discharging patients from psychiatric hospitals to the community. The pressure from the anti-psychiatry movements and the ideology of community treatment from the medical arena helped sustain deinstitutionalization. Thirty-three years after deinstitutionalization started in the United States, only 19% of the patients in state hospitals remained. Mental health professionals envisioned a process wherein patients would be discharged into communities where they could participate in a normal life while living in a therapeutic atmosphere. Psychiatrists were criticized, however, for failing to develop community-based support and treatment. Community-based facilities were not available because of the political infighting between in-patient and community-based social services, and an unwillingness by social services to dispense funding to provide adequately for patients to be discharged into community-based facilities.
Political abuse of psychiatry
See also: Political abuse of psychiatry and Political abuse of psychiatry in the Soviet UnionIn some instances psychiatrists have been involved in the suppression of individual rights by states wherein the definitions of mental disease had been expanded to include political disobedience. Nowadays, in many countries, political prisoners are sometimes confined to mental institutions and abused therein. Psychiatry possesses a built-in capacity for abuse which is greater than in other areas of medicine. The diagnosis of mental disease can serve as proxy for the designation of social dissidents, allowing the state to hold persons against their will and to insist upon therapies that work in favour of ideological conformity and in the broader interests of society. In a monolithic state, psychiatry can be used to bypass standard legal procedures for establishing guilt or innocence and allow political incarceration without the ordinary odium attaching to such political trials. In Nazi Germany in the 1940s, the 'duty to care' was violated on an enormous scale: A reported 300,000 individuals were sterilized and 100,000 killed in Germany alone, as were many thousands further afield, mainly in eastern Europe. From the 1960s up to 1986, political abuse of psychiatry was reported to be systematic in the Soviet Union, and to surface on occasion in other Eastern European countries such as Romania, Hungary, Czechoslovakia, and Yugoslavia. A "mental health genocide" reminiscent of the Nazi aberrations has been located in the history of South African oppression during the apartheid era. A continued misappropriation of the discipline was subsequently attributed to the People's Republic of China.
Medicalization of deviance
See also: MedicalizationThe concept of medicalization is created by sociologists and used for explaining how medical knowledge is applied to a series of behaviors, over which medicine exerts control, although those behaviors are not self-evidently medical or biological. According to Kittrie, a number of phenomena considered "deviant", such as alcoholism, drug addiction and mental illness, were originally considered as moral, then legal, and now medical problems. As a result of these perceptions, peculiar deviants were subjected to moral, then legal, and now medical modes of social control. Similarly, Conrad and Schneider concluded their review of the medicalization of deviance by supposing that three major paradigms may be identified that have reigned over deviance designations in different historical periods: deviance as sin; deviance as crime; and deviance as sickness. According to Franco Basaglia and his followers, whose approach pointed out the role of psychiatric institutions in the control and medicalization of deviant behaviors and social problems, psychiatry is used as the provider of scientific support for social control to the existing establishment, and the ensuing standards of deviance and normality brought about repressive views of discrete social groups. As scholars have long argued, governmental and medical institutions code menaces to authority as mental diseases during political disturbances.
Prisoner Experimentation
Prisoners in psychiatric hospitals have been the subjects of experiments involving new medications. Vladimir Khailo of the USSR was an individual exposed to such treatment in the 1980's. However, the Involuntary treatment of prisoners by use of psychiatric drugs is not limited to Khailo. In July of 2012, reporters learned that "mind altering drugs" have also been injected into prisoners at Guantanamo Bay.
Psychiatric survivors movement
The psychiatric survivors movement arose out of the civil rights ferment of the late 1960s and early 1970s and the personal histories of psychiatric abuse experienced by some ex-patients rather than the intradisciplinary discourse of antipsychiatry. The key text in the intellectual development of the survivor movement, at least in the USA, was Judi Chamberlin's 1978 text, On Our Own: Patient Controlled Alternatives to the Mental Health System. Chamberlin was an ex-patient and co-founder of the Mental Patients' Liberation Front. Coalescing around the ex-patient newsletter Dendron, in late 1988 leaders from several of the main national and grassroots psychiatric survivor groups felt that an independent, human rights coalition focused on problems in the mental health system was needed. That year the Support Coalition International (SCI) was formed. SCI's first public action was to stage a counter-conference and protest in New York City, in May, 1990, at the same time as (and directly outside of) the American Psychiatric Association's annual meeting. In 2005 the SCI changed its name to Mind Freedom International with David W. Oaks as its director.
See also
- American Board of Psychiatry and Neurology
- American Osteopathic Board of Neurology and Psychiatry
- Psychology
- Psychologist
- Psychiatrist
- Biopsychiatry controversy
- Mental health
- Psychiatric assessment
- Telepsychiatry
- Anti-psychiatry
- Bullying in psychiatry
- Psychiatry organizations
- List of psychiatry journals
References
Notes
- Etymology of Butterfly
- James, F.E. (1991). "Psyche" (PDF). Psychiatric Bulletin. 15 (7). Hillsdale, NJ: Analytic Press: 429–431. doi:10.1192/pb.15.7.429. ISBN 0-88163-257-0. Retrieved 2008-08-04.
- Kupfer D.J., Regier D.A. (2010). "Why all of medicine should care about DSM-5". JAMA. 303 (19): 1974–1975. doi:10.1001/jama.2010.646. PMID 20483976.
- ^ "While an operational definition for the term disease is lacking in traditional medicine, consensus indicates that it infers observable and measurable abnormalities in anatomy, chemistry, and physiology as causative for an observed cluster of symptoms. However, the term disease in psychiatry and psychology has a very different historical usage. It has been used when no systemic etiology has been indicated, it has been used politically for addictions, it has been used for the mere belief that a cluster of symptoms must be a disease because the symptoms are bizarre, and it has been used to justify crude medically based treatments, such as electroshock, lobotomies, involuntary commitments, and the sale of powerful drugs. With the advent of new medical machines, such as CAT scans, PET scans, and MRI's, a large volume of poorly conducted and questionable research has been pouring fourth to find diseases as a justification to promote psychotropic drugs. Politics and economics has replaced quality science.", Toward an Operational Definition of Disease in Psychiatry and Psychology: Implications for Diagnosis and Treatment, David B. Stein, Steve Baldwin, Medicine, Pharmacy and Medical Law and Ethics, International Journal of Risk and Safety in Medicine, Volume 13, Number 1, 2000
- Popper, Karl (1963) Conjectures and Refutations
- ^ “The pejorative phrase ‘defendant’s whore’ or ‘prosecutor’s whore’ is frequently used describing experts who would ‘say anything wants him to say.’”, 'They’re An Illusion to Me Now': Forensic Ethics, Sanism and Pretextuality, Michael L. Perlin, New York Law School Legal Studies Research Paper Series 07/08 # 27,
- "Courtroom Whores" ?--or Why Do Attorneys Call Us? Findings from a Survey on Attorneys' Use of Mental Health Experts, Douglas Mossman & Marshall Kapp, 26 J. American Academy of Academic Psychiatry and the Law, 27 (1998)
- Guze, S.B. (1992), p. 4
- ^ Storrow, H.A. (1969). Outline of Clinical Psychiatry. New York:Appleton-Century-Crofts, p 1. ISBN 978-0-390-85075-1
- Lyness, J.M. (1997), p. 3
- Gask, L. (2004), p. 7
- Guze, S. B. (1992), p 131
- Gask, L. (2004), p. 113
- Gask, L. (2004), p. 128
- ^ Pietrini P (2003). "Toward a Biochemistry of Mind?". American Journal of Psychiatry. 160 (11): 1907–1908. doi:10.1176/appi.ajp.160.11.1907. PMID 14594732.
- ^ Shorter, E. (1997), p. 326
- Hauser, M.J. (Unknown last update). Student Information. Retrieved September 21, 2007, from http://www.psychiatry.com/student.php
- National Institute of Mental Health. (2006, January 31). Information about Mental Illness and the Brain. Retrieved April 19, 2007, from http://science-education.nih.gov/supplements/nih5/Mental/guide/info-mental-c.htm
- López-Muñoza, Francisco; Alamo, C; Dudley, M; Rubio, G; García-García, P; Molina, JD; Okasha, A (2006-12-07). "Progress in Neuro-Psychopharmacology and Biological Psychiatry: Psychiatry and political–institutional abuse from the historical perspective: The ethical lessons of the Nuremberg Trial on their 60th anniversary". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 31 (4). Cecilio Alamoa, Michael Dudleyb, Gabriel Rubioc, Pilar García-Garcíaa, Juan D. Molinad and Ahmed Okasha. Science Direct: 791. doi:10.1016/j.pnpbp.2006.12.007. PMID 17223241.
These practices, in which racial hygiene constituted one of the fundamental principles and euthanasia programmes were the most obvious consequence, violated the majority of known bioethical principles. Psychiatry played a central role in these programmes, and the mentally ill were the principal victims.
{{cite journal}}: More than one of|pages=and|page=specified (help) - Gluzman, S.F. (1991). "Abuse of psychiatry: analysis of the guilt of medical personnel". J Med Ethics. 17 (Suppl): 19–20. doi:10.1136/jme.17.Suppl.19. PMC 1378165. PMID 11651120.
Based on the generally accepted definition, we correctly term the utilisation of psychiatry for the punishment of political dissidents as torture.
- Debreu, Gerard (1988). "Part 1: Torture, Psychiatric Abuse, and the Ethics of Medicine". In Corillon, Carol (ed.). Science and Human Rights. National Academy of Sciences. Retrieved 2007-10-04.
Over the past two decades the systematic use of torture and psychiatric abuse have been sanctioned or condoned by more than one-third of the nations in the United Nations, about half of mankind.
- The WPA code of ethics.
- Verhulst J, Tucker G (1995). "Medical and narrative approaches in psychiatry". Psychiatr Serv. 46 (5): 513–514. PMID 7627683.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ McLaren N (1998). "A critical review of the biopsychosocial model". The Australian and New Zealand Journal of Psychiatry. 32 (1): 86–92, discussion 93–6. doi:10.1046/j.1440-1614.1998.00343.x. PMID 9565189.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ McLaren, Niall (2007). Humanizing Madness. Ann Arbor, MI: Loving Healing Press. ISBN 1-932690-39-5.
- ^ McLaren, Niall (2009). Humanizing Psychiatry. Ann Arbor, MI: Loving Healing Press. ISBN 1-61599-011-9.
- ^ About:Psychology. (Unknown last update) Difference Between Psychologists and Psychiatrists. Retrieved March 25, 2007, from http://psychology.about.com/od/psychotherapy/f/psychvspsych.htm
- Hedges, D.; Burchfield, C. (2006). Mind, Brain, and Drug: An Introduction to Psychopharmacology.. Boston: Pearson Education, p. 64,65. ISBN 978-0-205-35556-3
- University of Manchester. (Unknown last update). Research in Psychiatry. Retrieved October 13, 2007, from http://www.manchester.ac.uk/research/areas/subareas/?a=s&id=44694
- New York State Psychiatric Institute. (2007, March 15). Psychiatric Research Institute New York State. Retrieved October 13, 2007, from http://nyspi.org/
- Canadian Psychiatric Research Foundation. (2007, July 27). Canadian Psychiatric Research Foundation. Retrieved October 13, 2007, from http://www.cprf.ca/
- Elsevier. (2007, October 08). Journal of Psychiatric Research. Retrieved October 13, 2007, from http://www.elsevier.com/wps/find/journaldescription.cws_home/241/description
- Mitchell, J.E.; Crosby, R.D.; Wonderlich, S.A.; Adson, D.E. (2000). Elements of Clinical Research in Psychiatry. Washington D.C.: American Psychiatric Press. ISBN 978-0-88048-802-0.
- Meyendorf R (1980). "Diagnosis and differential diagnosis in psychiatry and the question of situation referred prognostic diagnosis". Schweizer Archiv Neurol Neurochir Psychiatry für Neurologie, Neurochirurgie et de psychiatrie. 126: 121–134.
- Leigh, H. (1983), p. 15
- Leigh, H. (1983), p. 67
- Leigh, H. (1983), p. 17
- Lyness, J.M. (1997), p. 10
- Hampel H.; Teipel S.J.; Kotter H.U.; et al. (1997). "Structural magnetic resonance imaging in diagnosis and research of Alzheimer's disease". Nervenarzt. 68 (5): 365–378. PMID 9280846.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Townsend B.A., Petrella J.R., Doraiswamy P.M. (2002). "The role of neuroimaging in geriatric psychiatry". Current Opinion in Psychiatry. 15 (4): 427–432. doi:10.1097/00001504-200207000-00014.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - NIMH publications (2009) Neuroimaging and Mental Illness
- Krebs M.O. (2005). "Future contributions on genetics". World Journal of Biological Psychiatry. 6: 49–55. doi:10.1080/15622970510030072. PMID 16166024.
- Benes F.M.; Herold, U; Brocke, B (2007). "An electrophysiological endophenotype of hypomanic and hyperthymic personality". Journal of Affective Disorders. 101 (1–3): 13–26. doi:10.1016/j.jad.2006.11.018. PMID 17207536.
- Vonk R.; der Schot A.C.; Kahn R.S.; et al. (2007). "Is autoimmune thyroiditis part of the genetic vulnerability (or an endophenotype) for bipolar disorder?". Biological Psychiatry. 62 (2): 135–140. doi:10.1016/j.biopsych.2006.08.041. PMID 17141745.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - World Health Organisation. (1992). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organisation. ISBN 978-92-4-154422-1
- ^ American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders (4th Edition). Washington D.C.: American Psychiatric Publishing, Inc. ISBN 978-0-89042-025-6
- Chen Y.F. (2002). "Chinese classification of mental disorders (CCMD-3) towards integration in international classification". Psychopathology. 35 (2–3): 171–175. doi:10.1159/000065140. PMID 12145505.
- Essen-Moller E (1971). "On classification of mental disorders". Acta Psychiatrica Scandinavica. 37: 119–126.
- Mezzich J.E. (1979). "Patterns and issues in multiaxial psychiatric diagnosis". Psychological Medicine. 9 (1): 125–137. doi:10.1017/S0033291700021632. PMID 370861.
- Guze S.B. (1970). "The need for toughmindedness in psychiatric thinking". Southern Medical Journal. 63 (6): 662–671. doi:10.1097/00007611-197006000-00012. PMID 5446229.
- Dalal PK, Sivakumar T. (2009) Moving towards ICD-11 and DSM-5: Concept and evolution of psychiatric classification. Indian Journal of Psychiatry, Volume 51, Issue 4, Page 310-319.
- Kendell, R.; Jablensky, A (2003). "Distinguishing Between the Validity and Utility of Psychiatric Diagnoses". American Journal of Psychiatry. 160 (1): 4–12. doi:10.1176/appi.ajp.160.1.4. PMID 12505793.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Baca-Garcia, E.; Perez-Rodriguez, M. M.; Basurte-Villamor, I.; Del Moral, A. L. F.; Jimenez-Arriero, M. A.; De Rivera, J. L. G.; Saiz-Ruiz, J.; Oquendo, M. A. (2007). "Diagnostic stability of psychiatric disorders in clinical practice". The British Journal of Psychiatry. 190 (3): 210–6. doi:10.1192/bjp.bp.106.024026. PMID 17329740.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Pincus, H. A.; Zarin, DA; First, M (1998). "Clinical Significance" and DSM-IV". Arch Gen Psychiatry. 55 (12): 1145. doi:10.1001/archpsyc.55.12.1145. PMID 9862559.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); More than one of|pages=and|page=specified (help); Unknown parameter|author-separator=ignored (help) - Greenberg, Gary (January 29, 2012). "The D.S.M.'s Troubled Revision". The New York Times.
- American Association of Community Psychiatrists About AACP Retrieved on Aug-05-2008
- Moncrieff et al. (2003). Active placebos versus antidepressants for depression. Cochrane databases.
- Hopper K, Wanderling J (2000). "Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia". Schizophrenia Bulletin. 26 (4): 835–46. doi:10.1093/oxfordjournals.schbul.a033498. PMID 11087016.
- Eds. Spiegel D, Lake J. (2006). Complementary And Alternative Treatments in Mental Health Care American Psychiatric Pub, Inc. Quote from p. xxi
- Loren R. Mosher, Richard Gosden and Sharon Beder, 'Drug companies and Schizophrenia: Unbridled Capitalism meets Madness', in Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia edited by John Read, Loren Mosher and Richard Bentall, Brunner-Routledge, New York, 2004, pp. 115-130.
- Richard Gosden and Sharon Beder, 'Pharmaceutical Industry Agenda Setting in Mental Health Policies', Ethical Human Sciences and Services 3(3) Fall/Winter 2001, pp. 147-159
- Thomas Ginsberg. "Donations tie drug firms and nonprofits". The Philadelphia Inquirer 28 May 2006.
- Rae E. Unzicker, Kate P. Wolters, Debra Robinson et al. From Privileges to Rights: People Labeled with Psychiatric Disabilities Speak for Themselves. National Council on Disability 20 January 2000.
- Treatment Protocol Project (2003). Acute inpatient psychiatric care: A source book. Darlinghurst, Australia: World Health Organisation. ISBN 0-9578073-1-7. OCLC 223935527.
{{cite book}}: More than one of|author=and|last=specified (help) - Harris, Gardiner (March 5, 2011). "Talk Doesn't Pay, So Psychiatry Turns to Drug Therapy". The New York Times. Retrieved March 6, 2011.
- ^ Shorter, E. (1997), p. 1
- ^ Elkes, A. & Thorpe, J.G. (1967). A Summary of Psychiatry. London: Faber & Faber, p. 13.
- Mohamed Reza Namazi (2001), "Avicenna, 980-1037", American Journal of Psychiatry 158 (11), p. 1796; Mohammadali M. Shoja, R. Shane Tubbs (2007), "The Disorder of Love in the Canon of Avicenna (A.D. 980–1037)", American Journal of Psychiatry 164 (2), pp 228-229;S Safavi-Abbasi, LBC Brasiliense, RK Workman (2007), "The fate of medical knowledge and the neurosciences during the time of Genghis Khan and the Mongolian Empire", Neurosurgical Focus 23 (1), E13, p. 3.
- ^ Shorter, E. (1997), p. 4
- ^ Shorter, E. (1997), p. 5
- Shorter, E. (1997), p. 9
- Bukelic, Jovan (1995). "2". In Mirjana Jovanovic (ed.). Neuropsihijatrija za III razred medicinske skole (in Serbian) (7th ed.). Belgrade: Zavod za udzbenike i nastavna sredstva. p. 7. ISBN 86-17-03418-1.
{{cite book}}:|access-date=requires|url=(help) - Cherry, Charles L. (1989), A Quiet Haven: Quakers, Moral Treatment, and Asylum Reform, London & Toronto: Associated University Presses
- Digby, Anne (1983), Madness, Morality and Medicine: A Study of the York Retreat, Cambridge: Cambridge University Press
- Glover, Mary R. (1984), The Retreat, York: An Early Experiment in the Treatment of Mental Illness, York: Ebor Press
- Borthwick A., Holman C., Kennard D., McFetridge M., Messruther K., Wilkes J. (2001). "The relevance of moral treatment to contemporary mental health care". Journal of Mental Health. 10 (4): 427–439. doi:10.1080/09638230124277.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Johann Christian Reil, Dictionary of Eighteenth Century German Philosophers
- British Journal of Psychiatry, Psychiatry’s 200th birthday
- Seminal contributions of Johann Christian Reil
- ^ Shorter, E. (1997), p. 34
- ^ Shorter, E. (1997), p. 35
- Shorter, E. (1997), p. 41
- ^ Shorter, E. (1997), p. 46
- Shorter, E. (1997), p. 47
- Shorter, E. (1997), p. 48
- Shorter, E. (1997), p. 49
- Rothman, D.J. (1990). The Discovery of the Asylum: Social Order and Disorder in the New Republic. Boston: Little Brown, p. 239. ISBN 978-0-316-75745-4
- Shorter, E. (1997), p. 65
- ^ Shorter, E. (1997), p. 101
- Shorter, E. (1997), p. 102
- ^ Shorter, E. (1997), p. 103
- Shorter, E. (1997), p. 114
- Cohen, Bruce (2003). Theory and practice of psychiatry. Oxford University Press. p. 221. ISBN 0-19-514937-8.
- Thiher, Allen (2005). Revels in Madness: Insanity in Medicine and Literature. University of Michigan Press. ISBN 0-472-08999-4.
- ^ Shorter, E. (1997), p. 145
- ^ Shorter, E. (1997), p. 246
- Shorter, E. (1997), p. 270
- Turner T. (2007). "Unlocking psychosis". Brit J Med. 334 (suppl): s7. doi:10.1136/bmj.39034.609074.94. PMID 17204765.
- Cade JFJ. "Lithium salts in the treatment of psychotic excitement". Med J Aust. 1949 (36): 349–352.
- Shorter, E. (1997), p. 239
- Eisenberg, Leon; Guttmacher, Laurence (2010). "Were we all asleep at the switch? A personal reminiscence of psychiatry from 1940 to 2010". Acta Psychiatrica Scandinavica. 122 (2): 89–102. doi:10.1111/j.1600-0447.2010.01544.x. PMID 20618173. Retrieved 15 March 2012.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Shorter, E. (1997), p. 280
- Slovenko R (2003). "The transinstitutionalization of the mentally ill". Ohio University Law Review. 29: 641.
- Torrey, E.F. (1988). Nowhere to Go: The Tragic Odyssey of the Homeless Mentally Ill. New York: Harper and Row, pp.25-29, 126-128. ISBN 978-0-06-015993-1
- Rosenhan D (1973). "On being sane in insane places". Science. 179 (4070): 250–258. doi:10.1126/science.179.4070.250. PMID 4683124.
- Spitzer R.L., Lilienfeld S.O., Miller M.B. (2005). "Rosenhan revisited: The scientific credibility of Lauren Slater's pseudopatient diagnosis study". Journal of Nervous and Mental Disease. 193 (11): 734–739. PMID 16260927.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lyness, J.M. (1997). Psychiatric Pearls. Philadelphia: F.A. Davis Company. ISBN 978-0-8036-0280-9
- ^ Guze, S. B. (1992), p. 130
- ^ Shorter, E. (1997), p. 273
- Shorter, E. (1997), p. 274
- Shorter, E. (1997), p. 277
- ^ Shorter, E. (1997), p. 282
- Weiner R.D. (1984). "Does ECT cause brain damage?". Behavioral and Brain Sciences. 7: 153.
- Meldrum B.S. (1986). "Neuropathological consequences of chemically and electrically induced seizures". Annals of the New York Academy of Sciences. 462: 18693.
- Dwork A.J., Arango V., Underwood M., Ilievski B., Rosoklija G., Sackeim H.A., Lisanby S.H. (2004). "Absence of histological lesions in primate models of ECT and magnetic seizure therapy". American Journal of Psychiatry. 161 (3): 576–578. doi:10.1176/appi.ajp.161.3.576. PMID 14992989.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Peter R. Breggin, M.D., Electroshock: It's Brain Disabling Effects.
- Dr. Sidney Sament Clinical Psychiatry News, March 1983, p. 4.
- Shorter, E. (1997), p. 279
- Semple, David; Smyth, Roger; Burns, Jonathan (2005). Oxford handbook of psychiatry. Oxford: Oxford University Press. p. 6. ISBN 0-19-852783-7.
- Noll, Richard (2007). The encyclopedia of schizophrenia and other psychotic disorders. Infobase Publishing. p. 3. ISBN 0-8160-6405-9.
- ^ Medicine betrayed: the participation of doctors in human rights abuses. Zed Books. 1992. ISBN 1-85649-104-8.
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1111/j.0902-4441.2000.007s0203.x, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1111/j.0902-4441.2000.007s0203.xinstead. - "Press conference exposes mental health genocide during apartheid, 14 June 1997". South African Government Information. Retrieved 3 April 2011.
- van Voren R. (2010). "Political Abuse of Psychiatry—An Historical Overview" (PDF). Schizophrenia Bulletin. 36 (1): 33–35. doi:10.1093/schbul/sbp119. PMC 2800147. PMID 19892821.
- White, Kevin (2002). An introduction to the sociology of health and illness. SAGE. p. 42. ISBN 0-7619-6400-2.
- ^ Manning, Nick (1989). The therapeutic community movement: charisma and routinization. London: Routledge. p. 1. ISBN 0-415-02913-9.
- Kittrie, Nicholas (1971). The right to be different: deviance and enforced therapy. Johns Hopkins Press. ISBN 0-8018-1319-0.
- Conrad, Peter; Schneider, Joseph (1992). Deviance and medicalization: from badness to sickness. Temple University Press. p. 36. ISBN 0-87722-999-6.
- Sapouna, Lydia; Herrmann, Peter (2006). Knowledge in Mental Health: Reclaiming the Social. Hauppauge: Nova Publishers. p. 70. ISBN 1-59454-812-9.
- Metzl, Jonathan (2010). The Protest Psychosis: How Schizophrenia Became a Black Disease. Beacon Press. p. 14. ISBN 0-8070-8592-8.
- http://books.google.com/books?id=jbv81IDXoREC&pg=PA194&dq=biological+experiments+psychiatric+prisons&hl=en&sa=X&ei=aoqgUJnOKYiv0AHh_IFY&ved=0CDMQ6AEwAA#v=onepage&q&f=false
- http://www.wired.com/dangerroom/2012/07/gitmo/
- ^ Corrigan, Patrick W. (2011-05-23). Challenging the Stigma of Mental Illness: Lessons for Therapists and Advocates. John Wiley and Sons. ISBN 978-1-119-99612-5.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Oaks, David (2006-08-01). "The evolution of the consumer movement". Psychiatric Services. 57 (8): 1212. doi:10.1176/appi.ps.57.8.1212. PMID 16870979. Retrieved 2011-08-05.
- Chamberlin, Judi (1978). On Our Own: Patient-Controlled Alternatives to the Mental Health System. New York: Hawthorne.
- Rissmiller, David J. (2006-06-01). "Evolution of the antipsychiatry movement into mental health consumerism". Psychiatric Services. 57 (6): 865. doi:10.1176/appi.ps.57.6.863. PMID 16754765. Retrieved 2011-08-05.
{{cite journal}}: More than one of|pages=and|page=specified (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Ludwig, Gregory (2006-08-01). "Letter". Psychiatric Services. 57 (8): 1213. doi:10.1176/appi.ps.57.8.1213. Retrieved 2011-08-05.
- About Us — MFI Portal
Cited texts
- Gask, L. (2004). A Short Introduction to Psychiatry. London: SAGE Publications Ltd., p. 113 ISBN 978-0-7619-7138-2
- Guze, S.B. (1992). Why Psychiatry Is a Branch of Medicine. New York: Oxford University Press, p. 4. ISBN 978-0-19-507420-8
- Leigh, H. (1983). Psychiatry in the practice of medicine. Menlo Park: Addison-Wesley Publishing Company. ISBN 978-0-201-05456-9
- Lyness, J.M. (1997). Psychiatric Pearls. Philadelphia: F.A. Davis Company, p. 3. ISBN 978-0-8036-0280-9
- Shorter, E. (1997). A History of Psychiatry: From the Era of the Asylum to the Age of Prozac. New York: John Wiley & Sons, Inc. ISBN 978-0-471-24531-5
Further reading
- Berrios G E, Porter R (1995) The History of Clinical Psychiatry. London, Athlone Press
- Berrios G E (1996) History of Mental symptoms. The History of Descriptive Psychopathology since the 19th century. Cambridge, Cambridge University Press
- Ford-Martin, Paula Anne Gale (2002), "Psychosis" Gale Encyclopedia of Medicine, Farmington Hills, Michigan
- Hirschfeld; et al. (2003). "Perceptions and impact of bipolar disorder: how far have we really come?". J. Clin. Psychiatry. 64 (2): 161–174. doi:10.4088/JCP.v64n0209. PMID 12633125.
- McGorry PD; Mihalopoulos C; Henry L; et al. (1995). "Spurious precision: procedural validity of diagnostic assessment in psychiatric disorders". American Journal of Psychiatry. 152 (2): 220–223. PMID 7840355.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - MedFriendly.com, Psychologist, Viewed 20 September 2006
- Moncrieff J, Cohen D (2005). "Rethinking models of psychotropic drug action". Psychotherapy & Psychosomatics. 74 (3): 145–153. doi:10.1159/000083999.
- C. Burke, Psychiatry: a "value-free" science? Linacre Quarterly, vol. 67/1 (February 2000), pp. 59–88.
- National Association of Cognitive-Behavioral Therapists, What is Cognitive-Behavioral Therapy?, Viewed 20 September 2006
- van Os J, Gilvarry C, Bale R et al. (1999) A comparison of the utility of dimensional and categorical representations of psychosis. Psychological Medicine 29 (3) 595-606
- Williams J.B.; Gibbon M.; First M.; Spitzer R.; Davies M.; Borus J.; Howes M.; Kane J.; Pope H. (1992). "The structured clinical interview for DSM-III-R (SCID) II: Multi-site test-retest reliability". Archives of General Psychiatry. 49 (8): 630–636. doi:10.1001/archpsyc.1992.01820080038006. PMID 1637253.
{{cite journal}}: Invalid|display-authors=9(help); Unknown parameter|author-separator=ignored (help) - Hiruta, Genshiro. (edited by Dr. Allan Beveridge) "Japanese psychiatry in the Edo period (1600-1868)." History of Psychiatry, Vol. 13, No. 50, 131-151 (2002).
External links
| Psychiatry | |
|---|---|
| Subspecialties |
|
| Organizations |
|
| Related topics |
|
| Lists | |
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| Neuroscience | ||
|---|---|---|
| Basic science |
|  |
| Clinical neuroscience |
| |
| Cognitive neuroscience | ||
| Interdisciplinary fields |
| |
| Concepts |
| |