| Revision as of 04:15, 30 January 2014 view sourceRoxy the dog (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers34,207 edits Reverted to revision 592832888 by Naniwako (talk): Revert POV edits. (TW)← Previous edit | Revision as of 01:37, 31 January 2014 view source QuackGuru (talk | contribs)Extended confirmed users79,978 edits →Legal and political status: Readability per User:Mallexikon.Next edit → | ||
| Line 339: | Line 339: | ||
| {{Main|Regulation of acupuncture}} | {{Main|Regulation of acupuncture}} | ||
| The ] were a series of nationwide acupuncture trials set up in 2001 and published in 2006 on behalf of several ] due to a dispute as to the usefulness of acupuncture.<ref name="spiegelacupuncture">{{cite news |first=Veronika |last=Hackenbroch |title=Die eingebildete Heilung |trans_title=The Imaginary Healing |url=http://www.spiegel.de/spiegel/print/d-32565481.html |work=] |language=German |date=2004-10-25}}</ref> As a result of the trials, acupuncture was paid for in Germany by the social insurance scheme for only low back pain and osteoarthritis of the knee.<ref name="Birch 2007"/> This decision was made in part on the results of the trials and in part for ] reasons.<ref name="Birch 2007">{{cite journal |url=http://www.paradigm-pubs.com/sites/www.paradigm-pubs.com/files/files/Birch-german-studies.pdf |journal=Journal of Chinese Medicine |title=Reflections on the German Acupuncture studies |author=Birch, S. |issue=83 |year=2007 |pages=12-17 }}</ref> In 2006, German researchers published the results of one of the first and largest randomized controlled clinical trials.<ref name="He-2013" /> However, as a result of the trial's conclusions, some ] corporations in Germany no longer reimburse acupuncture treatments.<ref name="He-2013" /> The trials also had a negative impact on acupuncture in the international community.<ref name="He-2013">{{cite journal |pmid= 24024341 |year= 2013 |last1= He |first1= W. |last2= Tong |first2= Y. |last3= Zhao |first3= Y. |last4= Zhang |first4= L. |last5= Ben |first5= H. |last6= Qin |first6= Q. |last7= Huang |first7= F. |last8= Rong |first8= P. |displayauthors= 4 |title= Review of controlled clinical trials on acupuncture versus sham acupuncture in Germany |volume= 33 |issue= 3 |pages= 403–7 |journal= Journal of traditional Chinese medicine}}</ref> | |||
| == See also == | == See also == | ||
Revision as of 01:37, 31 January 2014
For the recording, see Acupuncture (album).Medical intervention
| Acupuncture | |
|---|---|
 Needles being inserted into a patient's skin Needles being inserted into a patient's skin | |
| ICD-10-PCS | 8E0H30Z |
| ICD-9 | 99.91-99.92 |
| MeSH | D015670 |
| OPS-301 code | 8-975.2 |
| [edit on Wikidata] | |
| Acupuncture | |||||||
|---|---|---|---|---|---|---|---|
| Simplified Chinese | 针灸 | ||||||
| |||||||
Acupuncture is a collection of procedures involving penetration of the skin with needles to stimulate certain points on the body. In its classical form it is a characteristic component of traditional Chinese medicine (TCM). It has been categorized as a complementary health approach. According to traditional Chinese medicine, stimulating specific acupuncture points corrects imbalances in the flow of qi through channels known as meridians. Scientific investigation has not found any histological or physiological correlates for traditional Chinese concepts such as qi, meridians, and acupuncture points, and some contemporary practitioners use acupuncture without following the traditional Chinese approach.
Although minimally invasive, the puncturing of the skin with acupuncture needles poses problems when designing trials that adequately control for placebo effects. A number of studies comparing traditional acupuncture to sham procedures found that both sham and traditional acupuncture were superior to usual care but were themselves equivalent. These findings are apparently at odds with traditional Chinese theories regarding acupuncture point specificity. Existing evidence is consistent with acupuncture being no more effective than a placebo.
Acupuncture's use for certain minor conditions has been recognized by the United States National Institutes of Health, the National Health Service of the United Kingdom, the World Health Organization, and the National Center for Complementary and Alternative Medicine. However, skeptics have criticized various health governing bodies' endorsements of acupuncture as being unduly credulous and not including objections to or criticisms of the claims of acupuncture's effectiveness. Acupuncture is generally safe when administered using Clean Needle Technique (CNT) but there is a low risk of adverse effects, which can be serious.
History
Antiquity


The precise start date of acupuncture's invention in ancient China and how it evolved from early times are uncertain. Traditional Chinese religion attributes the introduction of acupuncture to the god Shennong. One explanation is that Han Chinese doctors observed that some soldiers wounded in battle by arrows were believed to have been cured of chronic afflictions that were otherwise untreated, and there are variations on this idea. Sharpened stones known as Bian shi have been found in China, suggesting the practice may date to the Neolithic or possibly even earlier in the Stone Age. Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) which suggests that acupuncture was practiced along with moxibustion. It has also been suggested that acupuncture has its origins in bloodletting or demonology.
Despite improvements in metallurgy over centuries, it was not until the 2nd century BCE during the Han Dynasty that stone and bone needles were replaced with metal. The earliest examples of metal needles were found in a tomb dated to c. 113 BCE, though their use might not necessarily have been acupuncture. The earliest example of the unseen meridians (经络, pinyin: jīng-luò) used for diagnosis and treatment are dated to the second century BCE but these records do not mention needling, while the earliest reference to therapeutic needling occurs in the historical Shiji text (史記, English: Records of the Grand Historian) but does not mention the meridians and may be a reference to lancing rather than acupuncture.
The earliest written record of acupuncture is found in the Huangdi Neijing (黄帝内经; translated as The Yellow Emperor's Inner Canon), dated approximately 200 BCE. It does not distinguish between acupuncture and moxibustion and gives the same indication for both treatments. The Mawangdui texts, which also date from the 2nd century BCE (though antedating both the Shiji and Huangdi Neijing), mention the use of pointed stones to open abscesses, and moxibustion, but not acupuncture. However, by the 2nd century BCE, acupuncture replaced moxibustion as the primary treatment of systemic conditions.
The practice of acupuncture expanded out of China into the areas now part of Japan, Korea, Vietnam and Taiwan, diverging from the narrower theory and practice of mainland TCM in the process. A large number of contemporary practitioners outside of China follow these non-TCM practices, particularly in Europe.
In Europe, examinations of the 5,000-year-old mummified body of Ötzi the Iceman have identified 15 groups of tattoos on his body, some of which are located on what are now seen as contemporary acupuncture points. This has been cited as evidence that practices similar to acupuncture may have been practiced elsewhere in Eurasia during the early Bronze Age.
Middle history
Korea is believed to be the second country that acupuncture spread to outside of China. Within Korea there is a legend that acupuncture was developed by the legendary emperor Dangun though it is more likely to have been brought into Korea from a Chinese colonial prefecture.
Around 90 works on acupuncture were written in China between the Han Dynasty and the Song Dynasty, and the Emperor Renzong of Song, in 1023, ordered the production of a bronze statuette depicting the meridians and acupuncture points then in use. However, after the end of the Song Dynasty, acupuncture lost status, and started to be seen as a technical profession, in comparison to the more scholarly profession of herbalism. It became rarer in the following centuries, and was associated with less prestigious practices like alchemy, shamanism, midwifery and moxibustion.
Portuguese missionaries in the 16th century were among the first to bring reports of acupuncture to the West. Jacob de Bondt, a Dutch surgeon traveling in Asia, described the practice in both Japan and Java. However, in China itself the practice was increasingly associated with the lower-classes and illiterate practitioners.
In 1674, Hermann Buschoff, a Dutch priest in Batavia, published the first book on moxibustion (from Japanese mogusa) for the cure of arthritis. The first elaborate Western treatise on acupuncture was published in 1683 by Willem ten Rhijne, a Dutch physician who had worked at the Dutch trading post Dejima in Nagasaki for two years. In 1757 the physician Xu Daqun described the further decline of acupuncture, saying it was a lost art, with few experts to instruct; its decline was attributed in part to the popularity of prescriptions and medications, as well as its association with the lower classes.
In 1822, an edict from the Emperor Daoguang banned the practice and teaching of acupuncture within the Imperial Academy of Medicine outright, as unfit for practice by gentlemen-scholars. At this point, acupuncture was still cited in Europe with both skepticism and praise, with little study and only a small amount of experimentation.
In the United States, the earliest reports of acupuncture date back to 1826, when Franklin Bache, a surgeon of the United States Navy, published a report in the North American Medical and Surgical Journal on his use of acupuncture to treat lower back pain. Since the beginning of the 19th century, acupuncture was practiced by Asian immigrants living in Chinatowns.
Modern era
In the early years after the Chinese Civil War, Chinese Communist Party leaders ridiculed traditional Chinese medicine, including acupuncture, as superstitious, irrational and backward, claiming that it conflicted with the Party's dedication to science as the way of progress. Communist Party Chairman Mao Zedong later reversed this position, saying that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level." Under Mao's leadership, in response to the lack of modern medical practitioners, acupuncture was revived and its theory rewritten to adhere to the political, economic and logistic necessities of providing for the medical needs of China's population. Despite Mao proclaiming the practice of Chinese medicine to be "scientific", the practice was based more on the materialist assumptions of Marxism in opposition to superstition rather than the Western practice of empirical investigation of nature. Later the 1950s TCM's theory was again rewritten at Mao's insistence as a political response to the lack of unity between scientific and traditional Chinese medicine, and to correct the supposed "bourgeois thought of Western doctors of medicine" (p. 109).
Acupuncture gained attention in the United States when President Richard Nixon visited China in 1972. During one part of the visit, the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia. Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients.
The greatest exposure in the West came after New York Times reporter James Reston received acupuncture in Beijing for post-operative pain in 1971 and wrote complaisantly about it in his newspaper. Also in 1972 the first legal acupuncture center in the U.S. was established in Washington DC; during 1973-1974, this center saw up to one thousand patients. In 1973 the American Internal Revenue Service allowed acupuncture to be deducted as a medical expense.
Acupuncture has been the subject of active scientific research both in regard to its basis and therapeutic effectiveness since the late 20th century, but it remains controversial among medical researchers and clinicians. In 2006, a BBC documentary Alternative Medicine filmed a patient undergoing open heart surgery allegedly under acupuncture-induced anesthesia. It was later revealed that the patient had been given a cocktail of weak anesthetics that in combination could have a much more powerful effect. The program was also criticized for its fanciful interpretation of the results of a brain scanning experiment.
On November 16, 2010, acupuncture was recognized by UNESCO as part of the world's intangible cultural heritage.
Theory
The general theory of acupuncture is based on the premise that bodily functions are regulated by an energy called qi (氣) which flows through the body; disruptions of this flow are believed to be responsible for disease. Acupuncture describes a family of procedures aiming to correct imbalances in the flow of qi by stimulation of anatomical locations on or under the skin (usually called acupuncture points or acupoints), by a variety of techniques. The most common mechanism of stimulation of acupuncture points employs penetration of the skin by thin metal needles, which are manipulated manually or by electrical stimulation.
Qi, meridians and acupuncture points
Main articles: Qi, Traditional Chinese medicine § TCM model of the body, Meridian (Chinese medicine), and Acupuncture pointTraditional Chinese medicine distinguishes not only one but several different kinds of qi. In a general sense, qi is something that is defined by five "cardinal functions":

- Actuation (推動, tuīdòng) – of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians.
- Warming (溫煦, pinyin: wēnxù) – the body, especially the limbs.
- Defense (防御, pinyin: fángyù) – against Exogenous Pathogenic Factors
- Containment (固攝, pinyin: gùshè) – of body fluids, i.e. keeping blood, sweat, urine, semen etc. from leakage or excessive emission.
- Transformation (氣化, pinyin: qìhuà) – of food, drink, and breath into qi, xue (blood), and jinye ("fluids"), and/or transformation of all of the latter into each other.
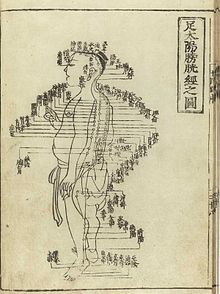
To fulfill its functions, qi has to steadily flow from the inside of the body (where the zang-fu organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints. It is assisted in its flow by "channels" referred to as meridians. TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài) respectively. There's also a number of less customary channels branching off from the "regular" meridians. Contemporary research has not supported the existence of qi or meridians. The meridians are believed to connect to the bodily organs, of which those considered hollow organs (such as the stomach and intestines) were also considered yang while those considered solid (such as the liver and lungs) were considered yin. They were also symbolically linked to the rivers found in ancient China, such as the Yangtze, Wei and Yellow Rivers.
Acupuncture points are mainly (but not always) found at specified locations along the meridians. There also is a number of acupuncture points with specified locations outside of the meridians; these are called "extraordinary" points and often credited with special therapeutic properties. A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes. The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in Han times, the number of bones thought to be in the body). The Huangdi Neijing mentioned only 160 and a further 135 could be deduced giving a total of 295. The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions. In addition, it is considered likely that some points used historically have since ceased being used.
TCM concept of disease
Main article: Traditional Chinese medicine § Concept of diseaseIn TCM, disease is generally perceived as a disharmony (or imbalance) in the functions or interactions of yin, yang, qi, xuĕ, zàng-fǔ, meridians etc. and/or of the interaction between the human body and the environment. Therapy is based on which "pattern of disharmony" can be identified. In the case of the meridians, typical disease patterns are invasions with wind, cold and damp Excesses.
In order to determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing or the sound of the voice.
TCM and its concept of disease do not strongly differentiate between cause and effect. In theory, however, endogenous, exogenous and miscellaneous causes of disease are recognized.
Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient to make a diagnosis according to the tradition which he or she uses. In TCM, there are four diagnostic methods: inspection, auscultation and olfaction, inquiring, and palpation.
- Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
- Auscultation and olfaction refer, respectively, to listening for particular sounds (such as wheezing) and attending to body odor.
- Inquiring focuses on the "seven inquiries", which are chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea.
- Palpation includes feeling the body for tender A-shi points, and palpation of the left and right radial pulses.
Tongue and pulse
Examination of the tongue and the pulse are among the principal diagnostic methods in TCM. Certain sectors of the tongue's surface are believed to correspond to the zàng-fŭ. For example, teeth marks on one part of the tongue might indicate a problem with the heart, while teeth marks on another part of the tongue might indicate a problem with the liver.
Pulse palpation involves measuring the pulse at a superficial and at a deep level at three locations on the radial artery (Cun, Guan, Chi, located two fingerbreadths from the wrist crease, one fingerbreadth from the wrist crease, and right at the wrist crease, respectively, usually palpated with the index, middle and ring finger) of each arm, for 12 pulses, all of which are thought to correspond with certain zàng-fŭ. The pulse is examined for several characteristics including rhythm, strength and volume, and described with qualities like "floating, slippery, bolstering-like, feeble, thready and quick". Each of these qualities indicate certain disease patterns. Learning TCM pulse diagnosis can take several years.
Scientific view on TCM theory

According to the 1997 NIH consensus statement on acupuncture:
Despite considerable efforts to understand the anatomy and physiology of the "acupuncture points", the definition and characterization of these points remains controversial. Even more elusive is the basis of some of the key traditional Eastern medical concepts such as the circulation of qi, the meridian system, and the five phases theory, which are difficult to reconcile with contemporary biomedical information but continue to play an important role in the evaluation of patients and the formulation of treatment in acupuncture.
Qi, yin, yang and meridians have no counterpart in modern studies of chemistry, biology, physics, or human physiology and to date scientists have been unable to find evidence that supports their existence.
Similarly, no research has established any consistent anatomical structure or function for either acupuncture points or meridians. Especially the nervous system has been evaluated for a relationship to acupuncture points, but no structures have been clearly linked to them. The electrical resistance of acupuncture points and meridians have also been studied, with conflicting results. In general, research on the electrical activity of acupuncture points lacks a standardized methodology and reporting protocols, and is of poor quality.
Acupuncturist Felix Mann, who is the author of the first comprehensive English language acupuncture textbook Acupuncture: The Ancient Chinese Art of Healing, has stated in lectures that "The traditional acupuncture points are no more real than the black spots a drunkard sees in front of his eyes" and "The meridians of acupuncture are no more real than the meridians of geography." In the same book, Mann also stated "Most of the ideas expressed in this book are based on clinical experience, careful observation and questions. These observations, rather than research, have cast a doubt in my mind about whether classical acupuncture points really exist."
Quackwatch has presented their view that:
TCM theory and practice are not based upon the body of knowledge related to health, disease, and health care that has been widely accepted by the scientific community. TCM practitioners disagree among themselves about how to diagnose patients and which treatments should go with which diagnoses. Even if they could agree, the TCM theories are so nebulous that no amount of scientific study will enable TCM to offer rational care.
Clinical practice
In a modern acupuncture session, an initial consultation is followed by taking the pulse on both arms, and an inspection of the tongue. Classically, in clinical practice, acupuncture is highly individualized and based on philosophy and intuition, and not on controlled scientific research. In the United States, acupuncture typically lasts from 10 to 60 minutes, with diagnosis and treatment for a single session ranging from $25 to $80 in 2011. Sometimes needles are left in the ear for up to 3 days.
Clinical practice varies depending on the country. A comparison of the average number of patients treated per hour found significant differences between China (10) and the United States (1.2).
Needles

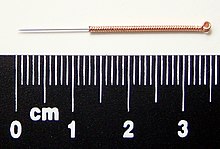
Acupuncture needles are typically made of stainless steel preventing them from rusting, breaking, and making them flexible. Once needles have been used they are thrown away to prevent contamination. Needles vary in length between 13 to 130 millimetres (0.51 to 5.12 in), with shorter needles used near the face and eyes, and longer needles in more fleshy areas; needle diameters vary from 0.16 mm (0.006 in) to 0.46 mm (0.018 in), with thicker needles used on more robust patients. Thinner needles may be flexible and require tubes for insertion. The tip of the needle should not be made too sharp to prevent breakage, although blunt needles cause more pain.
Apart from the usual filiform needle, there are also other needle types which can be utilized, such as three-edged needles and the Nine Ancient Needles. Japanese acupuncturists use extremely thin needles that are used superficially, sometimes without penetrating the skin, and surrounded by a guide tube (a technique adopted in China and the West). Korean acupuncture uses copper needles and has a greater focus on the hand.
Needling technique
Insertion
The skin is sterilized, e.g. with alcohol, and the needles are inserted, frequently with a plastic guide tube. Needles may be manipulated in various ways, e.g. spun, flicked, or moved up and down relative to the skin. Since most pain is felt in the superficial layers of the skin, a quick insertion of the needle is recommended.
Acupuncture can be painful. The skill level of the acupuncturist may influence how painful the needle insertion is, and a sufficiently skilled practitioner may be able to insert the needles without causing any pain.
De-qi sensation
De-qi (Chinese: 得气; pinyin: dé qì; "arrival of qi") refers to a sensation of numbness, distension, or electrical tingling at the needling site which might radiate along the corresponding meridian. If de-qi can not be generated, inaccurate location of the acupoint, improper depth of needle insertion, inadequate manual manipulation, or a very weak constitution of the patient have to be considered, all of which are thought to decrease the likelihood of successful treatment. If the de-qi sensation doesn't immediately occur upon needle insertion, various manual manipulation techniques can be applied to promote it (such as "plucking", "shaking" or "trembling").
Once de-qi is achieved, further techniques might be utilized which aim to "influence" the de-qi; for example, by certain manipulation the de-qi sensation allegedly can be conducted from the needling site towards more distant sites of the body. Other techniques aim at "tonifying" (Chinese: 补; pinyin: bǔ) or "sedating" (Chinese: 泄; pinyin: xiè) qi. The former techniques are used in deficiency patterns, the latter in excess patterns.
De qi is more important in Chinese acupuncture, while Western and Japanese patients may not consider it a necessary part of the treatment.
Related practices


- Acupressure (a blend of "acupuncture" and "pressure") uses physical pressure applied to acupressure points by the hand, elbow, or with various devices.
- Moxibustion – Acupuncture is often accompanied by moxibustion, the burning of cone-shaped preparations of mugwort on or near the skin, often but not always near or on an acupuncture point. Traditionally acupuncture was used to treat acute conditions while moxibustion was used for chronic diseases. Moxibustion could be direct (the cone was placed directly on the skin and allowed to burn the skin producing a blister and eventually a scar), or indirect (either a cone of mugwort was placed on a slice of garlic, ginger or other vegetable, or a cylinder of mugwort was held above the skin, close enough to either warm or burn it).
- Fire cupping
- Tuina is a TCM method of attempting to stimulate the flow of qi by various bare handed techniques that do not involve needles.
- Electroacupuncture is a form of acupuncture in which acupuncture needles are attached to a device that generates continuous electric pulses.
- Sonopuncture or acutonics is a stimulation of the body similar to acupuncture, but using sound instead of needles. This may be done using purpose-built transducers to direct a narrow ultrasound beam to a depth of 6–8 centimetres at acupuncture meridian points on the body. Alternatively, tuning forks or other sound emitting devices are used.
- Acupuncture point injection is the injection of various substances (such as drugs, vitamins or herbal extracts) into acupuncture point.
- Auriculotherapy - Ear acupuncture is a form of acupuncture developed in France which is based on the assumption of reflexological representation of the entire body in the outer ear.
- Scalp acupuncture is likewise based on reflexological considerations regarding the scalp area; it has been developed in Japan.
- Hand acupuncture similarly centers around assumed reflex zones of the hand; it has been developed in Korea.
- Medical acupuncture tries to integrate reflexological concepts, the trigger point model, and anatomical insights (such as dermatome distribution) into acupuncture practice, and emphasizes a more formulaic approach to acupuncture point location.
- Cosmetic acupuncture is the use of acupuncture in an attempt to reduce wrinkles on the face.
Effectiveness
The application of evidence-based medicine to researching acupuncture's effectiveness is a controversial activity, which has produced different results despite a growing evidence base. Some research results are encouraging but others suggest acupuncture's effects are mainly due to placebo.
Some scientists have opposed the very activity of investigating acupuncture's effectiveness. In the 1980s, writing of acupuncture's revival in the West, Petr Skrabanek argued that the principal issue that faced researchers was the demarcation between reason and absurdity, and that ideas should be rejected out-of-hand that lacked a testable hypothesis. More recently, Pete Greasley has expressed criticism of continued research into a practice based on a "magical, pseudoscientific rationale". Other scientists take a different view: Edzard Ernst has cautioned that prejudgement can lead to closed thinking, and that the aim of evidence-based research "is to establish whether a treatment works, not how it works or how plausible it is that it may work".
It is difficult to design research trials for acupuncture. Due to acupuncture's invasive nature, one of the major challenges in efficacy research is in the design of an appropriate placebo control group. The most commonly proposed placebo control has been "sham acupuncture" to control for different aspects of traditional acupuncture. This includes needling sites not traditionally indicated for treatment of a specific condition to control for the effectiveness of traditional acupuncture for specific conditions and/or needling performed superficially or using retracting needles or non-needles (including toothpicks) to control for needle penetration and stimulation.
A 2009 review concluded that the specific points chosen to needle do not matter, and no difference was found between needling according to "true" points chosen by traditional acupuncture theory and "sham" acupuncture points unrelated to any theory. The authors suggested four possible explanations for their observed superiority of both "true" and sham acupuncture over conventional treatment, but lack of difference in efficacy between "true" and sham acupuncture: Other authors have suggested randomized controlled trials may under-report the effectiveness of acupuncture as the "sham" treatment may still have active effects, though this position undercuts the traditional theory of acupuncture which associates specific acupuncture points with specific and distinct results.
Publication bias is also listed as a concern in the design of randomized trials of acupuncture. A 1998 review of studies on acupuncture found that trials originating in China, Japan, Hong Kong and Taiwan were uniformly favourable to acupuncture, as were ten out of 11 studies conducted in Russia. A 2011 assessment of the quality of randomized controlled trials on TCM, including acupuncture, concluded that the methodological quality of most such trials (including randomization, experimental control and blinding) was generally poor, particularly for trials published in Chinese journals (though the quality of acupuncture trials was better than the drug-related trials). The study also found that trials published in non-Chinese journals tended to be of higher quality.
Cancer
The American Cancer Society notes that in China acupuncture is promoted as a cure for physical illness and say that "available evidence does not suggest acupuncture is effective as a treatment for cancer", although clinical studies suggest it may be helpful in relieving some of the side effects of chemotherapy, such as nausea. Cancer Research UK say "there is no evidence to show that acupuncture helps in any way with treating or curing cancer, but research suggests that it is helpful in relieving some symptoms of cancer or the side effects of cancer treatment."
Fertility and childbirth
A 2013 systematic review and meta-analysis found no benefit of adjuvant acupuncture for in vitro fertilization on clinical pregnancy success rates. A 2010 Cochrane review found that there was no evidence acupuncture improved pregnancy rates irrespective of when it was performed and recommended against its use during in vitro fertilization either during egg retrieval or implantation.
Nausea and vomiting
Stimulation of a particular acupuncture point (PC6, located on the underside of the forearm, several finger-widths from the wrist) is traditionally thought to relieve nausea.
There is some evidence that acupuncture might help with post-operative nausea and vomiting (PONV), but the effects found are small and not likely to be clinically significant.
Stroke
There is no evidence acupuncture helps reduce the rates of death or disability after a stroke, but some suggestion it may help with dysphagia, which would need to be confirmed with future rigorous studies.
Pain
General
A 2012 meta-analysis conducted by the Acupuncture Trialists' Collaboration found "relatively modest" efficiency of acupuncture (in comparison to sham) for the treatment of four different types of chronic pain, and on that basis concluded it "is more than a placebo" and a reasonable referral option. Commenting on this meta-analysis both Edzard Ernst and David Colquhoun said the results were of negligible clinical significance.
Using the same dataset as the 2012 review, a 2013 meta-analysis found little evidence that the effectiveness of acupuncture (compared to sham) was modified by the technique or experience of the practitioner, or by the circumstances of the sessions. The researchers said these findings are unsurprising given the small differences between real and sham acupuncture. The same analysis also found that increased number of needles and more sessions appear to be associated with better outcomes when comparing acupuncture to non-acupuncture controls.
A 2011 overview of Cochrane reviews found high quality evidence that suggests acupuncture is effective for some but not all kinds of pain.
A 2010 systematic review suggested that acupuncture is more than a placebo for commonly occurring chronic pain conditions, but the authors acknowledged that it is still unknown if the overall benefit is clinically meaningful or cost-effective.
A 2007 review article noted that superficial needling, the primary form of traditional acupuncture in Japan, can stimulate endogenous production of opioids which could result in non-specific analgesia.
Peripheral osteoarthritis
A 2012 review found acupuncture to provide clinically significant relief from knee osteoarthritis pain and a larger improvement in function than sham acupuncture, standard care treatment, or waiting for treatment. A review from 2008 yielded similar positive results. The Osteoarthritis Research Society International released a set of consensus recommendations in 2008 that concluded acupuncture may be useful for treating the symptoms of osteoarthritis of the knee.
A 2010 Cochrance review found that acupuncture shows statistically significant benefit over sham acupuncture in the treatment of peripheral joint osteoarthritis; however, these benefits were found to be so small that their clinical significance was doubtful, and "probably due at least partially to placebo effects from incomplete blinding".
Headaches and migraines
A 2012 review found that acupuncture has demonstrated benefit for the treatment of headaches, but that safety needed to be more fully documented in order to make any strong recommendations in support of its use.
A 2009 Cochrane review of the use of acupuncture for migraine treatment concluded that "true" acupuncture wasn't more efficient than sham acupuncture, however, both "true" and sham acupuncture appear to be more effective than routine care in the treatment of migraines, with fewer adverse effects than prophylactic drug treatment.
Low back
A 2005 Cochrane review found there is insufficient evidence to recommend for or against either acupuncture or dry needling for acute low back pain. The same review found there is low quality evidence for pain relief and improvement compared to no treatment or sham therapy for chronic low back pain only in the short term immediately after treatment. The same review found acupuncture is not more effective than conventional therapy and CAM treatments. A 2005 review suggests there is insufficient evidence that acupuncture is more effective than other therapies. A review for the American Pain Society/American College of Physicians from 2007 found fair evidence that acupuncture is effective for chronic low back pain.
Post-operative
Reviews of acupuncture's effectiveness for management of post-operative pain have produced contradictory evidence. Overall, research findings are not convincing enough for acupuncture to be recommendable for use in a clinical setting, especially given the effectiveness of available conventional medicines.
Miscellaneous
A 2013 systematic review and meta-analysis found insufficient evidence for ankle sprain treatment with acupuncture, due to the limited number of high quality studies.
A 2012 review found there is evidence of benefit for acupuncture combined with exercise in treating shoulder pain after stroke. A 2011 review found inconclusive evidence regarding acupuncture efficacy in treating shoulder pain and lateral elbow pain.
A 2011 review stated that neck pain was one of only four types of pain for which a positive effect was suggested, but that the primary studies used carried a considerable risk of bias.
Other conditions
The Danish Knowledge and Research Center for Alternative Medicines has a fully updated list of all the Cochrane Collaboration regarding acupuncture and the overall conclusion is:
...the majority of the Cochrane reviews about acupuncture, acupressure, electroacupuncture and moxibustion there exists no solid evidence to determine the effectiveness of the treatments. The reviews point out that many of the studies suffer from methodological defects and shortcomings. Furthermore, the number of trial subjects has been limited. Thus most of the overall conclusions are uncertain.
For the following conditions, the Cochrane Collaboration or other review articles have concluded there is insufficient evidence to determine whether acupuncture is beneficial, often because of the paucity and poor quality of the research, and that further research is needed:
2There is mixed evidence for attention deficit hyperactivity disorder, with one review article concluding there was no evidence to support the use of acupuncture, and another concluding there was limited evidence but cautioned that firm conclusions could not be drawn because of the risk of bias.
Safety
Adverse events
A 2013 systematic review of English-language case reports found that serious adverse events associated with acupuncture are rare, but acupuncture is not without risk. Between 2000 and 2011, the incidence of English-language reported adverse events was 294 cases from 25 countries and regions. The most common adverse effect observed was infection, and the majority of infections were bacterial in nature, caused by skin contact at the needling site. Other adverse complications include bilateral hand edema, epithelioid granuloma, pseudolymphoma, argyria, pustules, pancytopenia, and scarring due to hot needle technique. When acupuncture needles are contaminated, risk of bacterial or other blood-borne infection increases, as with re-use of any type of needle.
When used on children, acupuncture carries a modest (11.8%) risk of adverse advents, thought to arise mostly from substandard practice. The harms are mostly mild in nature (e.g. bruising or bleeding) but on rare occasions very serious (e.g. cardiac rupture or hemoptysis). The same review found 279 adverse events, of which 25 were serious. There was limited research to draw definite conclusions about the overall safety of pediatric acupuncture. The incidence of serious adverse events was 5 per one million, which included children and adults.
A 2011 meta-review showed that serious adverse events are frequently due to practitioner error, rare, and diverse. The same review found 95 cases of severe adverse effects, including 5 deaths. The most reported adverse event was pneumothorax. The most common encountered adverse event was bacterial infection. Most such reports are from Asia, possibly reflecting the large number of treatments performed there or else a relatively higher number of poorly trained acupuncturists. Infectious diseases reported include both bacterial and viral infections. Though very rare in practice, traumatic injury to any site in the body is possible by needling too deeply, including the brain, any nerve, the kidneys, or heart. Many serious adverse events are not intrinsic to acupuncture but rather to bad practices (such as improper needling or unsterile needles), which may be why such complications have not been reported in surveys of adequately-trained acupuncturists.
A 2010 systematic review of the Chinese literature found numerous acupuncture related adverse events including pneumothorax, fainting, subarachnoid haemorrhage, and infection as the most frequent, and cardiovascular injuries, subarachnoid haemorrhage, pneumothorax, and recurrent cerebral haemorrhage as the most serious, most of which were due to improper technique. Between 1980 and 2009, the incidence of Chinese literature reported adverse events was 479 cases. The same review concluded that acupuncture can be considered inherently safe when practiced by properly trained practitioners, but the review also stated there is a need to find effective strategies to minimize the health risks.
Cost-effectiveness
A 2013 meta-analysis found that acupuncture for chronic low back pain was cost-effective as a complement to standard care, but not as a substitute for standard care. The same meta-analysis found there was no difference between sham and non-sham acupuncture. A 2011 systematic review found insufficient evidence for the cost-effectiveness of acupuncture in the treatment of chronic low back pain.
Risk of foregoing conventional medical care
Receiving alternative medicine as a replacement for standard modern medical care could result in inadequate diagnosis or treatment of conditions for which modern medicine has a better treatment record.
As with other alternative medicines, unethical or naïve practitioners may also induce patients to exhaust financial resources by pursuing ineffective treatment. Profession ethical codes set by accrediting organizations such as the National Certification Commission for Acupuncture and Oriental Medicine require practitioners to make "timely referrals to other health care professionals as may be appropriate."
Reception
General public
In recent years, several Western countries have seen a sharp increase in the number of people using acupuncture to treat common ailments:
- In Australia, a 2005 national survey revealed that nearly 1 in 10 adults have used acupuncture in the previous year.
- In the United States, less than one percent of the total population reported having used acupuncture in the early 1990s. In 2002, the National Center for Complementary and Alternative Medicine revealed that 2.1 million adults have used acupuncture in the previous 12 months. By the early 2010s, over 14 million Americans reported having used acupuncture as part of their health care. Each year, around 10 million acupuncture treatments are administered in the United States.
- In the United Kingdom, a total of 4 million acupuncture treatments were administered in 2009.
- According to several public health insurance organizations, women comprise over two-thirds of all acupuncture users in Germany. After the results of the German Acupuncture Trials were published in 2007, the number of regular users of acupuncture jumped by 20%, surpassing one million in 2011.
- In Switzerland, acupuncture has become the most frequently used complementary medicine since 2004.
Government agencies
In 2006, the NIH's National Center for Complementary and Alternative Medicine stated that it continued to abide by the pro-acupuncture recommendations of the 1997 NIH consensus statement, even if research is still unable to explain its mechanism.
In its 1997 statement, the NIH had concluded that despite research on acupuncture being difficult to conduct, there was sufficient evidence to encourage further study and expand its use. The consensus statement and conference that produced it were criticized by Wallace Sampson, founder of the Scientific Review of Alternative Medicine, writing for an affiliated publication of Quackwatch who stated the meeting was chaired by a strong proponent of acupuncture and failed to include speakers who had obtained negative results on studies of acupuncture. Sampson also stated he believed the report showed evidence of pseudoscientific reasoning.
The National Health Service of the United Kingdom states that at the present, no definite conclusions regarding acupuncture efficacy can be drawn, citing disagreement among scientists "over the way acupuncture trials should be carried out and over what their results mean".
International organizations
In 2003, the World Health Organization's Department of Essential Drugs and Medicine Policy produced a report on acupuncture. Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials was drafted, revised and updated by Zhu-Fan Xie, the Director for the Institute of Integrated Medicines of Beijing Medical University. It contained, based on research results available in early 1999, a list of diseases, symptoms or conditions for which it was believed acupuncture had been demonstrated as an effective treatment, as well as a second list of conditions that were possibly able to be treated with acupuncture. Noting the difficulties of conducting controlled research and the debate on how to best conduct research on acupuncture, the report described itself as "...intended to facilitate research on and the evaluation and application of acupuncture. It is hoped that it will provide a useful resource for researchers, health care providers, national health authorities and the general public." The coordinator for the team that produced the report, Xiaorui Zhang, stated that the report was designed to facilitate research on acupuncture, not recommend treatment for specific diseases.
Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials was controversial; critics assailed it as being problematic since, in spite of the disclaimer, supporters used it to claim that the WHO endorsed acupuncture and other alternative medicine practices that were either pseudoscientific or lacking sufficient evidence-basis. Medical scientists expressed concern that the evidence supporting acupuncture outlined in the report was weak, and Willem Betz of SKEPP (Studie Kring voor Kritische Evaluatie van Pseudowetenschap en het Paranormale, the Study Circle for the Critical Evaluation of Pseudoscience and the Paranormal) said that the report was evidence that the "WHO has been infiltrated by missionaries for alternative medicine." The WHO 2005 report was also criticized in the 2008 book Trick or Treatment for, in addition to being produced by a panel that included no critics of acupuncture, containing two major errors – including too many results from low-quality clinical trials, and including a large number of trials originating in China where, probably due to publication bias, no negative trials have ever been produced. In contrast, studies originating in the West include a mixture of positive, negative and neutral results. Ernst and Singh, the authors of the book, described the report as "highly misleading", a "shoddy piece of work that was never rigorously scrutinized" and stated that the results of high-quality clinical trials do not support the use of acupuncture to treat anything but pain and nausea. Ernst also described the statement in a 2006 peer reviewed article as "Perhaps the most obviously over-optimistic overview ", noting that of the 35 conditions that the WHO stated acupuncture was effective for, 27 of the systematic reviews that the WHO report was based on found that acupuncture was not effective for treating the specified condition.
On November 16, 2010, acupuncture and moxibustion were recognized by UNESCO as part of the world's intangible cultural heritage.
Public organizations
Brent Bauer comments on the Mayo Clinic website that it "it may be worth trying acupuncture" if other, more conventional treatments haven't helped in the treatment of low back pain, while noting that there was no difference in effectiveness between sham and real acupuncture.
In 1997, the American Medical Association Council on Scientific Affairs stated:
Critics contend that acupuncturists, including many traditionally trained physicians, merely stick needles in patients as a way to offer another form of treatment for which they can be reimbursed, since many insurance companies will do so. Critical reviews of acupuncture summarized by Hafner and others conclude that no evidence exists that acupuncture affects the course of any disease...Much of the information currently known about these therapies makes it clear that many have not been shown to be efficacious. Well-designed, stringently controlled research should be done to evaluate the efficacy of alternative therapies.
The National Council Against Health Fraud stated in 1990 that acupuncture’s "theory and practice are based on primitive and fanciful concepts of health and disease that bear no relationship to present scientific knowledge."
Skeptics
The 1993 book The Health Robbers, neurologist Arthur Taub called acupuncture "nonsense with needles." Quackwatch criticizes TCM as having unproven efficacy and an unsound scientific basis. Psychologist John Jackson stated that, "Acupuncture, both as a field of study and in practice, contains many of the hallmarks of pseudoscience. It is based on untenable principles and the small amount of evidence there is to support its use in pain relief can also be called into question." Steven Salzberg, director of the Center for Bioinformatics and Computational Biology and professor at the University of Maryland stated that, "acupuncture is pseudoscience. It’s based on magical thinking about a non-existent "life force" that has never had one whit of evidence to support it. The only benefits are placebo effects, as the sham acupuncture experiments demonstrate. The notion of "meridians" that can be somehow fixed by sticking needles into the skin is laughable". Steven Novella, Yale University professor of neurology, and founder and executive editor of the blog Science Based Medicine commenting on acupuncture, said "there has been recent controversy over the role of the placebo effect in ethical and evidence-based practice. This is, in my opinion, largely a back door attempt to justify CAM treatments that do not work. The claim is that placebo effects are real and useful".
Legal and political status
Main article: Regulation of acupunctureThe German acupuncture trials were a series of nationwide acupuncture trials set up in 2001 and published in 2006 on behalf of several German statutory health insurance companies due to a dispute as to the usefulness of acupuncture. As a result of the trials, acupuncture was paid for in Germany by the social insurance scheme for only low back pain and osteoarthritis of the knee. This decision was made in part on the results of the trials and in part for socio-political reasons. In 2006, German researchers published the results of one of the first and largest randomized controlled clinical trials. However, as a result of the trial's conclusions, some insurance corporations in Germany no longer reimburse acupuncture treatments. The trials also had a negative impact on acupuncture in the international community.
See also
- Chinese herbology
- Colorpuncture
- List of ineffective cancer treatments
- Perkinism
- Pressure point
- Susuk
Bibliography
- Aung, SKH; Chen WPD (2007). Clinical Introduction to Medical Acupuncture. Thieme Medical Publishers. ISBN 9781588902214.
- Barnes, LL (2005). Needles, Herbs, Gods, and Ghosts: China, Healing, and the West to 1848. Harvard University Press. ISBN 0674018729.
- Cheng, X (1987). Chinese Acupuncture and Moxibustion (1st ed.). Foreign Languages Press. ISBN 711900378X.
- Needham, J; Lu GD (2002). Celestial Lancets: A History and Rationale of Acupuncture and Moxa. Routledge. ISBN 0700714588.
- Singh, S; Ernst, E (2008). Trick or Treatment: Alternative Medicine on Trial. London: Bantam. ISBN 9780593061299.
- Stux, G (1988). Basics of Acupuncture. Berlin: Springer-Verlag. ISBN 354053072X.
{{cite book}}: Unknown parameter|coauthor=ignored (|author=suggested) (help) - Wiseman, N; Ellis, A (1996). Fundamentals of Chinese medicine. Paradigm Publications. ISBN 9780912111445.
Notes
- ^ Singh & Ernst (2008) stated, "Scientists are still unable to find a shred of evidence to support the existence of meridians or Ch'i", "The traditional principles of acupuncture are deeply flawed, as there is no evidence at all to demonstrate the existence of Ch'i or meridians" and "Acupuncture points and meridians are not a reality, but merely the product of an ancient Chinese philosophy"
References
- "What is CAM?". NCCAM. Retrieved 8 March 2013.
- ^ "Acupuncture". NIH Consensus Statement. 15 (5): 1–34. 1997. PMID 10228456. Archived from the original on 14 July 2007. Retrieved 17 July 2007.
- Singh & Ernst 2008, p. 72
- Singh & Ernst 2008, p. 107
- Singh & Ernst 2008, p. 387
- ^ Bauer, M (2006). "The Final Days of Traditional Beliefs? – Part One". Chinese Medicine Times. 1 (4): 31.
- ^ Ahn, Andrew C.; Colbert, Agatha P.; Anderson, Belinda J.; Martinsen, ØRjan G.; Hammerschlag, Richard; Cina, Steve; Wayne, Peter M.; Langevin, Helene M. (2008). "Electrical properties of acupuncture points and meridians: A systematic review" (PDF). Bioelectromagnetics. 29 (4): 245–56. doi:10.1002/bem.20403. PMID 18240287.
- ^ Mann, F (2000). Reinventing Acupuncture: A New Concept of Ancient Medicine. Elsevier. ISBN 0750648570.
{{cite book}}: CS1 maint: ref duplicates default (link) - de las Peñas, César Fernández; Arendt-Nielsen, Lars; Gerwin, Robert D (2010). Tension-type and cervicogenic headache: pathophysiology, diagnosis, and management. Jones & Bartlett Learning. pp. 251–4. ISBN 9780763752835.
- ^ Ernst, E.; Pittler, MH; Wider, B; Boddy, K (2007). "Acupuncture: its evidence-base is changing". The American Journal of Chinese Medicine. 35 (1): 21–5. doi:10.1142/S0192415X07004588. PMID 17265547.
- ^ White, A.R.; Filshie, J.; Cummings, T.M.; International Acupuncture Research Forum (2001). "Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding". Complementary Therapies in Medicine. 9 (4): 237–245. doi:10.1054/ctim.2001.0489. PMID 12184353.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16783282 , please use {{cite journal}} with
|pmid= 16783282instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20976074, please use {{cite journal}} with
|pmid= 20976074instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16420542 , please use {{cite journal}} with
|pmid= 16420542instead. - Madsen, M. V.; Gøtzsche, P. C; Hróbjartsson, A. (2009). "Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups". BMJ. 338: a3115. doi:10.1136/bmj.a3115. PMC 2769056. PMID 19174438.
- ^ Ernst, E; et al. (2011). "Acupuncture: Does it alleviate pain and are there serious risks? A review of reviews". Pain. 152 (4): 755–64. doi:10.1016/j.pain.2010.11.004. PMID 21440191.
- ^ "Acupuncture: Evidence for its effectiveness". National Health Service. 18 March 2010. Archived from the original on 14 August 2010. Retrieved 10 August 2010.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ World Health Organization (2003). Zhang X (ed.). "Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials". World Health Organization.
- ^ "Acupuncture". US National Center for Complementary and Alternative Medicine. 2006. Archived from the original on 8 February 2006. Retrieved 2 March 2006.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - "NHS to give back pain acupuncture". BBC. 26 May 2006. Archived from the original on 28 May 2009. Retrieved 26 May 2009.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - "NHS Acupuncture intro". NHS. 2009. Retrieved 25 February 2012.
- ^ Sampson, W (23 March 2005). "Critique of the NIH Consensus Conference on Acupuncture". Quackwatch. Archived from the original on 6 June 2009. Retrieved 5 June 2009.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ McCarthy, Michael (2005). "Critics slam draft WHO report on homoeopathy". The Lancet. 366 (9487): 705–6. doi:10.1016/S0140-6736(05)67159-0.
- ^ Singh & Ernst 2008, Chapter 2: The Truth About Acupuncture
- ^ Xu, Shifen; et al. (2013). "Adverse Events of Acupuncture: A Systematic Review of Case Reports". Evidence Based Complementary and Alternative Medicine. 2013: 581203. doi:10.1155/2013/581203. PMC 3616356. PMID 23573135.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: unflagged free DOI (link) - ^ Adams D, Cheng F, Jou H, Aung S, Yasui Y, Vohra S (2011). "The safety of pediatric acupuncture: a systematic review". Pediatrics (Systematic review). 128 (6): e1575–87. doi:10.1542/peds.2011-1091. PMID 22106073.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Classics of Traditional Medicine".
- Tiran, D; Mack S (2000). Complementary therapies for pregnancy and childbirth. Elsevier Health Sciences. pp. 79. ISBN 0702023280.
- e.g. White, A; Ernst E (1999). Acupuncture: a scientific appraisal. Elsevier Health Sciences. pp. 1. ISBN 0750641630.
- ^ Chiu, M (1993). Chinese acupuncture and moxibustion. Elsevier Health Sciences. p. 2. ISBN 0443042233.
- Ma, K.-W. (1992). "The roots and development of Chinese acupuncture: from prehistory to early 20th century" (PDF). Acupuncture in Medicine. 10: 92–9. doi:10.1136/aim.10.Suppl.92.
- Robson, T (2004). An Introduction to Complementary Medicine. Allen & Unwin. pp. 90. ISBN 1741140544.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6998524, please use {{cite journal}} with
|pmid= 6998524instead. - ^ Prioreschi, P (2004). A history of Medicine, Volume 2. Horatius Press. pp. 147–8. ISBN 1888456019.
- Ramey, D; Buell D (2004). "A true history of acupuncture". Focus on Complementary and Alternative Therapies. 9 (4): 269–73. doi:10.1211/fact.2004.00244.
- Fruehauf H (2010). "Chinese Medicine In Crisis: Science, Politics, And The Making Of "TCM"" (PDF). Retrieved 15 June 2011.
- Hicks, Angela; Hicks, John; Mole, Peter (2004). Five Element Constitutional Acupuncture (1st ed.). London: Churchill Livingstone. pp. ix. ISBN 0443071705.
- Dorfer, L; Moser, M; Bahr, F; Spindler, K; Egarter-Vigl, E; Giullén, S; Dohr, G; Kenner, T (1999). "A medical report from the stone age?" (PDF). The Lancet. 354 (9183): 1023–5. doi:10.1016/S0140-6736(98)12242-0. PMID 10501382.
- Needham & Lu, 2002, p. 262.
- Barnes, 2005, p. 25.
- Unschuld, P (1998). Chinese Medicine. Paradigm Publications. p. 94. ISBN 0912111550.
- Barnes, 2005, pp. 58–9.
- Barnes, 2005, p. 75.
- Barnes, 2005, p. 188.
- Barnes, 2005, pp. 308–9.
- ^ "Acupuncture (PDQ®)". National Cancer Institute. Retrieved 15 September 2013.
- Crozier RC (1968). Traditional medicine in modern China: science, nationalism, and the tensions of cultural change. Cambridge: Harvard University Press.
- Taylor, K (2005). Chinese Medicine in Early Communist China, 1945–63: a Medicine of Revolution. RoutledgeCurzon. ISBN 041534512X.
- Beyerstein, BL; Sampson W (1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 1)". Skeptical Inquirer. 20 (4). Committee for Skeptical Inquiry.
- Davidson JP (1999). The complete idiot's guide to managing stress. Indianapolis, Ind: Alpha Books. pp. 255. ISBN 0028629558.
- Fan, AY (2012). "The first acupuncture center in the United States: an interview with Dr. Yao Wu Lee, Washington Acupuncture Center". Journal of Chinese Integrative Medicine. 20 (5). Committee for Journal of Chinese Integrative Medicine.
- Frum, David (2000). How We Got Here: The '70s. New York, New York: Basic Books. p. 133. ISBN 0465041957.
- Simon Singh (26 March 2006). "A groundbreaking experiment ... or a sensationalized TV stunt?". The Guardian.
- Simon Singh (14 February 2006). "Did we really witness the 'amazing power' of acupuncture?". Daily Telegraph.
- ^ "Acupuncture and moxibustion of traditional Chinese medicine". UNESCO. Retrieved 25 May 2013.
- ^ Aung & Chen, 2007, pp 11–12.
- "氣的生理功能...(一)推動作用...(二)溫煦作用...(三)防御作用...(四)固攝作用...(五)氣化作用 as seen at 郭卜樂 (24t October 2009). "氣" (in Chinese). Archived from the original on 8 January 2009. Retrieved 2 December 2010.
{{cite web}}: Check date values in:|date=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - "(三)十二经脉 ...(四)奇经八脉 ..." as seen at "经络学" (in Chinese). Retrieved 22 February 2011.
{{cite web}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - Aung & Chen, 2007, pp 19–20.
- Needham & Lu, 2002, p. 23.
- Aung & Chen, 2007, p. 101.
- Needham & Lu, 2002, p. 15.
- Wiseman & Ellis 1996, p. 77
- Ergil, MC; Ergil, KV (2009). Pocket Atlas of Chinese Medicine. Stuttgart: Thieme. p. 19, 148. ISBN 9783131416117.
- Flaws, B; Finney D (2007). A handbook of TCM patterns & their treatments (6th ed.). Blue Poppy Press. pp. 1. ISBN 9780936185705.
- Flaws, B; Finney, D (1996). A handbook of TCM patterns & their treatments (6 (2007) ed.). Blue Poppy Press. pp. 169–173. ISBN 9780936185705.
- ^ Maciocia, G (1995). Tongue Diagnosis in Chinese Medicine. Eastland Press. ISBN 093961619X.
- Maciocia, G (2005). The Foundations of Chinese Medicine. Churchill Livingstone. ISBN 0443074895.
- Ross, J (1984). Zang Fu, the organ systems of traditional Chinese medicine. Elsevier. pp. 26. ISBN 9780443034824.
- anon (1980). Essentials of Chinese Acupuncture (1st ed.). Beijing: Foreign Languages Press. pp. 39–46.
- Cheng, 1987, chapter 12.
- Wright, Thomas; Eisenberg, David (1995). Encounters with Qi: exploring Chinese medicine. New York: Norton. pp. 53–4. ISBN 0393312135.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Colbert AP, Spaulding K, Larsen A, Ahn AC, Cutro JA (2011). "Electrodermal activity at acupoints: literature review and recommendations for reporting clinical trials". J Acupunct Meridian Stud (Literature review). 4 (1): 5–13. doi:10.1016/S2005-2901(11)60002-2. PMID 21440875.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Felix Mann (1972). Acupuncture: the ancient Chinese art of healing. Vintage Books. ISBN 9780394717272. Retrieved 13 September 2012.
- Mann 2000, p. 14.
- Mann 2000, p. 31.
- Mann 2000, p. 28.
- ^ Stephen Barrett, M.D. "Be Wary of Acupuncture, Qigong, and "Chinese Medicine"". Retrieved 31 December 2013. Cite error: The named reference "Quackwatch" was defined multiple times with different content (see the help page).
- Schwartz, L (2000). "Evidence-Based Medicine And Traditional Chinese Medicine: Not Mutually Exclusive". Medical Acupuncture. 12 (1): 38–41.
- ^ "What is involved in an Acupuncture & Traditional Chinese Medicine (TCM) Treatment?". acupuncture.com.
- ^ Young, J (2007). Complementary Medicine For Dummies. John Wiley & Sons. pp. 126–8. ISBN 0470519681.
- Napadow V, Kaptchuk TJ (2004). "Patient characteristics for outpatient acupuncture in Beijing, China". J Altern Complement Med (Research article). 10 (3): 565–72. doi:10.1089/1075553041323849. PMID 15253864.
{{cite journal}}: Unknown parameter|month=ignored (help) - Hicks, Angela. The acupuncture handbook: how acupuncture works and how it can help you.Piatkus Books,2005, p. 39.
- Hicks, Angela. The acupuncture handbook: how acupuncture works and how it can help you.Piatkus Books,2005, p. 41.
- ^ Aung & Chen, 2007, p. 116.
- Ellis, A; Wiseman N; Boss K (1991). Fundamentals of Chinese Acupuncture. Paradigm Publications. pp. 2–3. ISBN 091211133X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Aung & Chen, 2007, p. 113-4.
- ^ Steven Aung; William Chen (10 January 2007). Clinical Introduction to Medical Acupuncture. Thieme. p. 116. ISBN 9781588902214. Retrieved 20 September 2012.
- Needham & Lu, 2002, pp 170–173.
- "Sonopuncture". Educational Opportunities in Integrative Medicine. The Hunter Press. 2008. p. 34. ISBN 9780977655243.
- Bhagat (2004). Alternative Therapies. pp. 164–165. ISBN 9788180612206.
- "Sonopuncture". American Cancer Society's Guide to complementary and alternative cancer methods. American Cancer Society. 2000. p. 158. ISBN 9780944235249.
- "Cancer Dictionary – Acupuncture point injection". National Cancer Institute. Archived from the original on 27 March 2011. Retrieved 4 April 2011.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Braverman S (2004). "Medical Acupuncture Review: Safety, Efficacy, And Treatment Practices". Medical Acupuncture. 15 (3).
- Isaacs, Nora (13 December 2007). "Hold the Chemicals, Bring on the Needles". New York Times. Retrieved 23 November 2009.
- Skrabanek, Petr (1984). "Acupuncture and the Age of Unreason". The Lancet. 323 (8387): 1169. doi:10.1016/S0140-6736(84)91406-5.
- ^ Greasley, P (2010). "Is evaluating complementary and alternative medicine equivalent to evaluating the absurd?". Evaluation & the health professions. 33 (2): 127–39. doi:10.1177/0163278710361923. PMID 20457720.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19433697, please use {{cite journal}} with
|pmid= 19433697instead. - ^ Linde, K; Allais, G; Brinkhaus, B; Manheimer, E; Vickers, A; White, AR (2009). Linde, Klaus (ed.). "Acupuncture for migraine prophylaxis". Cochrane Database of Systematic Reviews (1): CD001218. doi:10.1002/14651858.CD001218.pub2. PMC 3099267. PMID 19160193.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15905259 , please use {{cite journal}} with
|pmid= 15905259instead. - ^ Vickers, A; Goyal, N; Harland, R; Rees, R (1998). "Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials". Controlled Clinical Trials. 19 (2): 159–66. doi:10.1016/S0197-2456(97)00150-5. PMID 9551280.
- Lee A, Copas JB, Henmi M, Gin T, Chung RC (2006). "Publication bias affected the estimate of postoperative nausea in an acupoint stimulation systematic review". J Clin Epidemiol. 59 (9): 980–3. doi:10.1016/j.jclinepi.2006.02.003. PMID 16895822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Tang, JL; Zhan, SY; Ernst, E (1999). "Review of randomised controlled trials of traditional Chinese medicine". BMJ (Clinical research ed.). 319 (7203): 160–1. doi:10.1136/bmj.319.7203.160. PMC 28166. PMID 10406751.
- He, J; Du, L; Liu, G; Fu, J; He, X; Yu, J; Shang, L (2011). "Quality assessment of reporting of randomization, allocation concealment, and blinding in traditional Chinese medicine RCTs: A review of 3159 RCTs identified from 260 systematic reviews". Trials. 12: 122. doi:10.1186/1745-6215-12-122. PMC 3114769. PMID 21569452.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - "Acupuncture". American Cancer Society. May 2010. Retrieved 22 September 2013.
- "Acupuncture". Cancer Research UK. Retrieved 22 September 2013.
- Manheimer, E; Van Der Windt, D; Cheng, K; Stafford, K; Liu, J; Tierney, J; Lao, L; Berman, BM; Langenberg, P; Bouter, LM (2013). "The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: A systematic review and meta-analysis". Human reproduction update. 19 (6): 696–713. doi:10.1093/humupd/dmt026. PMC 3796945. PMID 23814102.
- El-Toukhy, T; Khalaf, Y (2009). "The impact of acupuncture on assisted reproductive technology outcome". Current opinion in obstetrics & gynecology. 21 (3): 240–6. doi:10.1097/GCO.0b013e3283292491. PMID 19276803.
- ^ Lee MS, Ernst E (2014). "Acupuncture for surgical conditions: an overview of systematic reviews". Int. J. Clin. Pract. (Review). doi:10.1111/ijcp.12372. PMID 24447388.
{{cite journal}}: Unknown parameter|month=ignored (help) - Zhang JH, Wang D, Liu M (2014). "Overview of systematic reviews and meta-analyses of acupuncture for stroke". Neuroepidemiology (Systematic review). 42 (1): 50–8. doi:10.1159/000355435. PMID 24356063.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Vickers, AJ; Cronin, AM; Maschino, AC; Lewith, G; MacPherson, H; Foster, N; Sherman, N; Witt, K; Linde, C (2012). "Acupuncture for chronic pain: individual patient data meta-analysis". JAMA Internal Medicine. 12 (Suppl 1). for the Acupuncture Trialists' Collaboration: 1444–53. doi:10.1001/archinternmed.2012.3654. PMC 3373337. PMID 22965186.
- Jha, Alok (10 September 2012). "Acupuncture useful, but overall of little benefit, study shows". The Guardian. Retrieved 31 October 2013.
{{cite news}}: Italic or bold markup not allowed in:|newspaper=(help) - Colquhoun, David (17 September 2012). "Risks of acupuncture range from stray needles to pneumothorax, finds study". BMJ. Retrieved December 2013.
{{cite web}}: Check date values in:|accessdate=(help); Italic or bold markup not allowed in:|publisher=(help) - MacPherson, Hugh; Maschino, Alexandra C.; Lewith, George; Foster, Nadine E.; Witt, Claudia; Vickers, Andrew J.; Acupuncture Trialists' Collaboration (2013). Eldabe, Sam (ed.). "Characteristics of Acupuncture Treatment Associated with Outcome: An Individual Patient Meta-Analysis of 17,922 Patients with Chronic Pain in Randomised Controlled Trials". PLoS ONE. 8 (10): e77438. doi:10.1371/journal.pone.0077438. PMC 3795671. PMID 24146995.
When comparing acupuncture to sham controls, there was little evidence that the effects of acupuncture on pain were modified by any of the acupuncture characteristics evaluated, including style of acupuncture, the number or placement of needles, the number, frequency or duration of sessions, patient-practitioner interactions and the experience of the acupuncturist.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lee, MS; Ernst, E (2011). "Acupuncture for pain: An overview of Cochrane reviews". Chinese Journal of Integrative Medicine. 17 (3): 187–9. doi:10.1007/s11655-011-0665-7. PMID 21359919.
- Hopton A, MacPherson H (2010). "Acupuncture for chronic pain: is acupuncture more than an effective placebo? A systematic review of pooled data from meta-analyses". Pain Practice. 10 (2): 94–102. doi:10.1111/j.1533-2500.2009.00337.x. PMID 20070551.
- Manheimer, E; et al. (2007). "Meta-analysis: acupuncture for osteoarthritis of the knee". Annals of Internal Medicine. 146 (12): 868–77. doi:10.7326/0003-4819-146-12-200706190-00008. PMID 17577006.
- Cao, L; et al. (2012). "Needle acupuncture for osteoarthritis of the knee. A systematic review and updated meta-analysis". Saudi Medical Journal. 33 (5): 526–32. PMID 22588814.
- Selfe, TK; Taylor, AG (2008). "Acupuncture and osteoarthritis of the knee: a review of randomized, controlled trials". Family & Community Health. 31 (3): 247–54. doi:10.1097/01.FCH.0000324482.78577.0f. PMC 2810544. PMID 18552606.
- Zhang, W; et al. (2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (PDF). Osteoarthritis and Cartilage. 16 (2): 137–162. doi:10.1016/j.joca.2007.12.013. PMID 18279766.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help);|first12=missing|last12=(help);|first13=missing|last13=(help);|first14=missing|last14=(help);|first15=missing|last15=(help);|first16=missing|last16=(help) - Manheimer, E; et al. (2010). Manheimer, Eric (ed.). "Acupuncture for peripheral joint osteoarthritis (Review)" (PDF). Cochrane Database of Systematic Reviews (10). doi:10.1002/14651858.CD001977.pub2.
- Lee, Courtney; Crawford, Cindy; Wallerstedt, Dawn; York, Alexandra; Duncan, Alaine; Smith, Jennifer; Sprengel, Meredith; Welton, Richard; Jonas, Wayne (2012). "The effectiveness of acupuncture research across components of the trauma spectrum response (tsr): A systematic review of reviews". Systematic Reviews. 1: 46. doi:10.1186/2046-4053-1-46. PMC 3534620. PMID 23067573.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Furlan, AD; et al. (2005). Furlan, AD (ed.). "Acupuncture and dry-needling for low back pain" (PDF). Cochrane Database of Systematic Reviews (1): CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876.
- Manheimer, E; et al. (2005). "Meta-analysis: Acupuncture for low back pain" (PDF). Annals of Internal Medicine. 142 (8): 651–63. doi:10.7326/0003-4819-142-8-200504190-00014. PMID 15838072.
- Chou, R; Huffman, LH (2007). "Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline" (PDF). Annals of Internal Medicine. 147 (7): 492–504. doi:10.7326/0003-4819-147-7-200710020-00007. PMID 17909210.
{{cite journal}}:|first3=missing|last3=(help);|first4=missing|last4=(help) - Park, J; Hahn, S; Park, JY; Park, HJ; Lee, H (2013). "Acupuncture for ankle sprain: Systematic review and meta-analysis". BMC complementary and alternative medicine. 13: 55. doi:10.1186/1472-6882-13-55. PMC 3606608. PMID 23496981.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Lee, JA; et al. (Sept 2012). "Acupuncture for shoulder pain after stroke: A systematic review". Journal of Alternative and Complementary Medicine 18(9):818-23. 18 (9): 213–8. doi:10.1089/acm.2011.0457. PMC 3429280. PMID 2292441.
{{cite journal}}: Check date values in:|date=(help) - "Cochrane and Alternative Medicine – Acupuncture". Danish Knowledge and Research Center for Alternative Medicines. 28 September 2011. Retrieved 19 October 2011.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21901712, please use {{cite journal}} with
|pmid= 21901712instead. - Mccarney, RW; Brinkhaus, B; Lasserson, TJ; Linde, K (2003). McCarney, Robert W (ed.). "Acupuncture for chronic asthma". Cochrane Database of Systematic Reviews. 2003 (3): CD000008. doi:10.1002/14651858.CD000008.pub2. PMID 14973944. Archived from the original on 19 April 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - He, L; Zhou, MK; Zhou, D; Wu, B; Li, N; Kong, SY; Zhang, DP; Li, QF; Yang, J; et al. (2004). He, Li (ed.). "Acupuncture for Bell's palsy". Cochrane Database of Systematic Reviews. 2007 (4): CD002914. doi:10.1002/14651858.CD002914.pub3. PMID 17943775. Archived from the original on 6 April 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22161401, please use {{cite journal}} with
|pmid= 22161401instead. - Gates, S; Smith, LA; Foxcroft, DR; Gates, Simon (2006). Gates, Simon (ed.). "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews. 2006 (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523. Retrieved 2 May 2008.
- Smith, CA; Hay, PP; Smith, Caroline A (17 March 2004). Smith, Caroline A (ed.). "Acupuncture for depression". Cochrane Database of Systematic Reviews. 2004 (3): CD004046. doi:10.1002/14651858.CD004046.pub2. PMID 15846693. Archived from the original on 21 April 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Jordan, J (2006). "Acupuncture treatment for opiate addiction: A systematic review". Journal of Substance Abuse Treatment. 30 (4): 309–14. doi:10.1016/j.jsat.2006.02.005. PMID 16716845.
- Gates, Simon; Smith, Lesley A; Foxcroft, David (2006). Gates, Simon (ed.). "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523.
- Proctor, ML; Smith, CA; Farquhar, CM; Stones, RW; Zhu, Xiaoshu; Brown, Julie; Zhu, Xiaoshu (2002). Zhu, Xiaoshu (ed.). "Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea". Cochrane Database of Systematic Reviews. 2002 (1): CD002123. doi:10.1002/14651858.CD002123. PMID 11869624. Archived from the original on 5 June 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22161390, please use {{cite journal}} with
|pmid= 22161390instead. - Cheuk, DK; Wong, V; Cheuk, Daniel (2006). Cheuk, Daniel (ed.). "Acupuncture for epilepsy". Cochrane Database of Systematic Reviews. 2006 (2): CD005062. doi:10.1002/14651858.CD005062.pub2. PMID 16625622. Archived from the original on 30 May 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21782365, please use {{cite journal}} with
|pmid= 21782365instead. - Mayhew E; Ernst E (2007). "Acupuncture for fibromyalgia—a systematic review of randomized clinical trials" (PDF). Rheumatology (Oxford, England). 46 (5): 801–4. doi:10.1093/rheumatology/kel406. PMID 17189243.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Law, SK; Li, T; Law, Simon K (2007). Law, Simon K (ed.). "Acupuncture for glaucoma". Cochrane Database of Systematic Reviews. 2007 (4): CD006030. doi:10.1002/14651858.CD006030.pub2. PMC 3804313. PMID 17943876. Archived from the original on 14 May 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21376483, please use {{cite journal}} with
|pmid= 21376483instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19424092, please use {{cite journal}} with
|pmid= 19424092instead. - Cheuk, DK; Yeung, WF; Chung, KF; Wong, V; Cheuk, Daniel KL (2007). Cheuk, Daniel KL (ed.). "Acupuncture for insomnia". Cochrane Database of Systematic Reviews. 2007 (3): CD005472. doi:10.1002/14651858.CD005472.pub2. PMID 17636800. Archived from the original on 1 May 2008. Retrieved 2 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21463162, please use {{cite journal}} with
|pmid= 21463162instead. - Lim, B; Manheimer, E; Lao, L; Ziea, E; Wisniewski, J; Liu, J; Berman, B; Manheimer, Eric (2006). Manheimer, Eric (ed.). "Acupuncture for treatment of irritable bowel syndrome". Cochrane Database of Systematic Reviews. 2006 (4): CD005111. doi:10.1002/14651858.CD005111.pub2. PMID 17054239. Archived from the original on 14 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Smith, CA; Crowther, CA; Smith, Caroline A (2004). Smith, Caroline A (ed.). "Acupuncture for induction of labour". Cochrane Database of Systematic Reviews. 2004 (1): CD002962. doi:10.1002/14651858.CD002962.pub2. PMID 14973999. Archived from the original on 17 May 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21901710, please use {{cite journal}} with
|pmid= 21901710instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21833961, please use {{cite journal}} with
|pmid= 21833961instead. - Casimiro, L; Barnsley, L; Brosseau, L; Milne, S; Robinson, VA; Tugwell, P; Wells, G; Casimiro, Lynn (2005). Casimiro, Lynn (ed.). "Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis". Cochrane Database of Systematic Reviews. 2005 (4): CD003788. doi:10.1002/14651858.CD003788.pub2. PMID 16235342. Archived from the original on 13 April 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Green, S; Buchbinder, R; Hetrick, S; Green, Sally (2005). Green, Sally (ed.). "Acupuncture for shoulder pain". Cochrane Database of Systematic Reviews. 2005 (2): CD005319. doi:10.1002/14651858.CD005319. PMID 15846753. Archived from the original on 25 April 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Rathbone, J; Xia, J; Rathbone, John (2005). Rathbone, John (ed.). "Acupuncture for schizophrenia". Cochrane Database of Systematic Reviews. 2005 (4): CD005475. doi:10.1002/14651858.CD005475. PMID 16235404. Archived from the original on 18 April 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - White, AR; Rampes, H; Campbell, JL; White, Adrian R (2006). White, Adrian R (ed.). "Acupuncture and related interventions for smoking cessation". Cochrane Database of Systematic Reviews. 2006 (1): CD000009. doi:10.1002/14651858.CD000009.pub2. PMID 16437420. Archived from the original on 13 May 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Zhang, SH; Liu, M; Asplund, K; Li, L; Liu, Ming (2005). Liu, Ming (ed.). "Acupuncture for acute stroke". Cochrane Database of Systematic Reviews. 2005 (2): CD003317. doi:10.1002/14651858.CD003317.pub2. PMID 15846657. Archived from the original on 29 April 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Wu, HM; Tang, JL; Lin, XP; Lau, J; Leung, PC; Woo, J; Li, YP; Wu, Hong Mei (2006). Wu, Hong Mei (ed.). "Acupuncture for stroke rehabilitation". Cochrane Database of Systematic Reviews. 2006 (3): CD004131. doi:10.1002/14651858.CD004131.pub2. PMID 16856031. Retrieved 6 May 2008.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22326146, please use {{cite journal}} with
|pmid= 22326146instead. - Green, S; Buchbinder, R; Barnsley, L; Hall, S; White, M; Smidt, N; Assendelft, W; Green, Sally (2002). Green, Sally (ed.). "Acupuncture for lateral elbow pain". Cochrane Database of Systematic Reviews. 2002 (1): CD003527. doi:10.1002/14651858.CD003527. PMID 11869671. Retrieved 6 May 2008.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21796811, please use {{cite journal}} with
|pmid= 21796811instead. - Peng, WN; Zhao, H; Liu, ZS; Wang, S; Weina, Peng (2008). Weina, Peng (ed.). "Acupuncture for vascular dementia". Cochrane Database of Systematic Reviews. 2007 (2): CD004987. doi:10.1002/14651858.CD004987.pub2. PMID 17443563. Retrieved 6 May 2008.
- Li S, Yu B, Zhou D; et al. (2011). "Acupuncture for Attention Deficit Hyperactivity Disorder (ADHD) in children and adolescents". Cochrane Database Syst Rev (Systematic review) (4): CD007839. doi:10.1002/14651858.CD007839.pub2. PMID 21491402.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Lee MS, Choi TY, Kim JI, Kim L, Ernst E (2011). "Acupuncture for treating attention deficit hyperactivity disorder: a systematic review and meta-analysis". Chin J Integr Med (Systematic review). 17 (4): 257–60. doi:10.1007/s11655-011-0701-7. PMID 21509667.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Woo, P. C Y; Lin, A. W C; Lau, S. K P; Yuen, K.-Y. (2010). "Acupuncture transmitted infections". BMJ. 340: c1268. doi:10.1136/bmj.c1268. PMID 20299695.
- White, A. (2004). "A cumulative review of the range and incidence of significant adverse events associated with acupuncture". Acupuncture in medicine : journal of the British Medical Acupuncture Society. 22 (3): 122–133. PMID 15551936.
- ^ Zhang J, Shang H, Gao X, Ernst E (December 2010). "Acupuncture-related adverse events: a systematic review of the Chinese literature". Bull World Health Organ. 88 (12): 915–921C. doi:10.2471/BLT.10.076737. PMC 2995190. PMID 21124716.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Yekeler, E.; Tunaci, M; Tunaci, A; Dursun, M; Acunas, G (2006). "Frequency of Sternal Variations and Anomalies Evaluated by MDCT". American Journal of Roentgenology. 186 (4): 956–60. doi:10.2214/AJR.04.1779. PMID 16554563.
- ^ Taylor P, Pezzullo L, Grant SJ, Bensoussan A. (2013). "Cost-effectiveness of Acupuncture for Chronic Nonspecific Low Back Pain". Pain Practice: The Official Journal of World Institute of Pain. doi:10.1111/papr.12116.. PMID 24138020.
{{cite journal}}: Check|doi=value (help)CS1 maint: multiple names: authors list (link) - Standaert CJ, Friedly J, Erwin MW, Lee MJ, Rechtine G, Henrikson NB, Norvell DC (2011). "Comparative effectiveness of exercise, acupuncture, and spinal manipulation for low back pain". Spine. 1 (36): 21 Suppl):S120–30. doi:10.1097/BRS.0b013e31822ef878. PMID 21952184.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Barret, S (30 December 2007). "Be Wary of Acupuncture, Qigong, and "Chinese Medicine"". Quackwatch. Archived from the original on 29 September 2010. Retrieved 3 November 2010.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - "Final Report, Report into Traditional Chinese Medicine" (PDF). Parliament of New South Wales. 9 November 2005. Retrieved 3 November 2010.
- "NCCAOM Code of Ethics" (PDF). National Certification Commission for Acupuncture and Oriental Medicine. Archived from the original (PDF) on 27 November 2010. Retrieved 3 November 2010.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - Xue, CC; Zhang, AL; Lin, V; Myers, R; Polus, B; Story, DF (2008). "Acupuncture, chiropractic and osteopathy use in Australia: A national population survey". BMC Public Health. 88: 108. doi:10.1186/1471-2458-8-105. PMC 2322980. PMID 18377663. Retrieved 25 May 2013.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ "More Americans using acupuncture for common ailments". Fox News Channel. Retrieved 25 May 2013.
- Alderman, L (7 May 2010). "Acupuncture is popular, but you'll need to pay". The New York Times. Retrieved 25 May 2013.
- "Acupuncture". NYU Langone Medical Center. Retrieved 25 May 2013.
- Hopton, AK; Curnoe, S; Kanaan, M; MacPherson, H (2012). "Acupuncture in practice: Mapping the providers, the patients and the settings in a national cross-sectional survey". BMJ Open. 2 (1). bmj.com: e000456. doi:10.1136/bmjopen-2011-000456. PMC 3278493. PMID 22240649. Retrieved 25 May 2013.
- ^ "Frauen häufiger mit Akupunktur behandelt" (in German). Rheinische Post. Retrieved 25 May 2013.
{{cite web}}: Italic or bold markup not allowed in:|publisher=(help) - Carruzzo, P; Graz, B; Rodondi, PY; Michaud, PA (6 September 2013). "Offer and use of complementary and alternative medicine in hospitals of the French-speaking part of Switzerland". Swiss Medical Weekly. 143: w13756. doi:10.4414/smw.2013.13756. PMID 24018633.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Singh & Ernst, 2008, p. 277-8.
- Bauer, Brent A. "Acupuncture for back pain?". Mayo Clinic.
- "Report 12 of the Council on Scientific Affairs (A-97) – Alternative Medicine". American Medical Association. 1997. Retrieved 7 October 2009.
- "Position Paper on Acupuncture". National Council Against Health Fraud. 1990. Retrieved 27 January 2011.
- Arthur Taub (1993). Acupuncture: Nonsense with Needles.
- John Jackson. "What is acupuncture?".
- Steven Salzberg (2008). "Acupuncture infiltrates the University of Maryland and NEJM".
- Steven Novella. "Acupuncture Pseudoscience in the New England Journal of Medicine".
- Hackenbroch, Veronika (25 October 2004). "Die eingebildete Heilung". Der Spiegel (in German).
{{cite news}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ Birch, S. (2007). "Reflections on the German Acupuncture studies" (PDF). Journal of Chinese Medicine (83): 12–17.
- ^ He, W.; Tong, Y.; Zhao, Y.; Zhang, L.; Ben, H.; Qin, Q.; Huang, F.; Rong, P. (2013). "Review of controlled clinical trials on acupuncture versus sham acupuncture in Germany". Journal of traditional Chinese medicine. 33 (3): 403–7. PMID 24024341.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)
Further reading
- Deadman, P.; Baker, K; Al-Khafaji, M. (2007). A Manual of Acupuncture. Journal of Chinese Medicine Publications. ISBN 0951054651.
- Jin, G.; Jin, J.X.; Jin, L.L. (2006). Contemporary Medical Acupuncture – A Systems Approach. Springer. ISBN 7040192578.
- Ulett GA (2002). Shermer M (ed.). Acupuncture. ABC-CLIO. pp. 283–. ISBN 978-1-57607-653-8.
{{cite encyclopedia}}:|work=ignored (help) - William FW, ed. (2013). Acupuncture. Routledge. pp. 31–. ISBN 978-1-135-95522-9.
{{cite encyclopedia}}:|work=ignored (help)
External links
 Media related to Acupuncture at Wikimedia Commons
Media related to Acupuncture at Wikimedia Commons- Template:Dmoz
| Acupuncture | |
|---|---|
| Concepts | |
| Types | |
| Alternative medicine | |
|---|---|
| Systems | |
| People |
|
| Treatments | |
| Public-health issues | |
| Key terms | |
| Contrary viewpoints | |
| Traditional Chinese medicine (TCM) | |||||
|---|---|---|---|---|---|
| Practices | |||||
| Concepts |
| ||||
| Zangfu Organs |
| ||||
| Noted physicians |
| ||||
| Contemporary related topics | |||||
