| Revision as of 05:06, 19 February 2014 editBoboMeowCat (talk | contribs)4,152 edits →Asthma← Previous edit | Revision as of 06:23, 19 February 2014 edit undoRenamed user 51g7z61hz5af2azs6k6 (talk | contribs)6,460 edits →Asthma: added secondary references, language making clear that causative role of acetaminophen is still debated.Next edit → | ||
| Line 114: | Line 114: | ||
| ===Asthma=== | ===Asthma=== | ||
| An epidemiological association between paracetamol (acetaminophen) use and ]in children is well established. <ref>{{Cite pmid|22065272}}</ref> There is continuing debate over whether acetaminophen exposure increases the risk of asthma, or whether the association is due to "confounding by indication", in which the apparent association arises because illnesses commonly treated with acetaminophen predispose children to later development of asthma.<ref>{{cite journal |author=Heintze K, Petersen KU |title=The case of drug causation of childhood asthma: antibiotics and paracetamol |journal=Eur. J. Clin. Pharmacol. |volume=69 |issue=6 |pages=1197–209 |year=2013 |month=June |pmid=23292157 |pmc=3651816 |doi=10.1007/s00228-012-1463-7 |url=}}</ref><ref>{{cite journal |author=Henderson AJ, Shaheen SO |title=Acetaminophen and asthma |journal=Paediatr Respir Rev |volume=14 |issue=1 |pages=9–15; quiz 16 |year=2013 |month=March |pmid=23347656 |doi=10.1016/j.prrv.2012.04.004 |url=}}</ref> | |||
| An association between paracetamol (acetaminophen) use and ], in both children and adults, has been well established. <ref>{{Cite pmid|22065272}}</ref> | |||
| ===Other factors=== | ===Other factors=== | ||
Revision as of 06:23, 19 February 2014
Pharmaceutical compound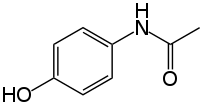 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tylenol (USA), Anacin Aspirin Free (USA), Apra (USA), Crocin (India), Feverall (USA), Genapap (USA), Panadol (UK), Panadol (Australia/New Zealand), Panodil (Denmark), Efferalgan (France), Doliprane (France) Dafalgan (France) Alvedon (Sweden) |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a681004 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral, rectal, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ~100% |
| Metabolism | 90 to 95% Hepatic |
| Elimination half-life | 1–4 h |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.002.870 |
| Chemical and physical data | |
| Formula | C8H9NO2 |
| Molar mass | 151.163 g/mol g·mol |
| 3D model (JSmol) | |
| Density | 1.263 g/cm |
| Melting point | 169 °C (336 °F) |
| Solubility in water | 12.78 mg/mL (20 °C) |
SMILES
| |
InChI
| |
| (verify) | |
Paracetamol (/ˌpærəˈsiːtəmɒl/ or /ˌpærəˈsɛtəmɒl/), acetaminophen /əˌsiːtəˈmɪnəfn/ , or APAP, chemically named N-acetyl-p-aminophenol, is a widely used over-the-counter analgesic (pain reliever) and antipyretic (fever reducer). Paracetamol is the International Nonproprietary Name (INN) and British Approved Name (BAN), while acetaminophen is the United States Adopted Name (USAN) and Japanese Adopted Name (JAN).
Paracetamol is classified as a mild analgesic. It is commonly used for the relief of headaches and other minor aches and pains and is a major ingredient in numerous cold and flu remedies. In combination with opioid analgesics, paracetamol can also be used in the management of more severe pain such as post-surgical pain and providing palliative care in advanced cancer patients. Though paracetamol is used to treat inflammatory pain, it is not generally classified as an NSAID because it exhibits only weak anti-inflammatory activity.
While generally safe for use at recommended doses (1,000 mg per single dose and up to 4,000 mg per day for adults), even small overdoses can be fatal. Compared to other over-the-counter pain relievers, paracetamol is significantly more toxic in overdose but may be less toxic when used chronically at recommended doses.
The onset of analgesia is approximately 11–29.5 minutes after oral administration of paracetamol, and its half-life is 1–4 hours.
Paracetamol is the active metabolite of phenacetin, once popular as an analgesic and antipyretic in its own right. However, unlike phenacetin and its combinations, paracetamol is not considered carcinogenic at therapeutic doses. The words acetaminophen (used in the United States, Canada, Japan, South Korea, Hong Kong, and Iran) and paracetamol (used elsewhere) both come from a chemical name for the compound: para-acetylaminophenol and para-acetylaminophenol. In some contexts, it is simply abbreviated as APAP, for acetyl-para-aminophenol.
Medical uses
Fever
Paracetamol is approved for reducing fever in people of all ages. The World Health Organization (WHO) recommends that paracetamol only be used to treat fever in children if their temperature is greater than 38.5 °C (101.3 °F). The efficacy of paracetamol by itself in children with fevers has been questioned and a meta-analysis showed that it is less effective than ibuprofen.
Pain
Paracetamol is used for the relief of pains associated with many parts of the body. It has analgesic properties comparable to those of aspirin, while its anti-inflammatory effects are weaker. It is better tolerated than aspirin in patients in whom excessive gastric acid secretion or prolongation of bleeding time may be a concern. Available without a prescription, it has in recent years increasingly become a common household drug.
Paracetamol has a relatively little anti-inflammatory activity, unlike other common analgesics such as the NSAIDs aspirin and ibuprofen, but ibuprofen and paracetamol have similar effects in the treatment of headache. Paracetamol can relieve pain in mild arthritis, but has no effect on the underlying inflammation, redness, and swelling of the joint.
Regarding comparative efficacy, studies show conflicting results when compared to NSAIDs. A randomised controlled trial of chronic pain from osteoarthritis in adults found similar benefit from paracetamol and ibuprofen.
The efficacy of paracetamol when used in a combination form with weak opioids (such as codeine) has been addressed by data studies in 1996 and 2009, which found that efficacy improves for approximately 50% of patients, but increases the number of patients experiencing adverse effects. Combination drugs of paracetamol and strong opioids like morphine reduce the amount of opioid used and improve analgesic effect.
A randomised controlled trial of acute musculoskeletal pain in children found that the standard over-the-counter dose of ibuprofen gives greater pain relief than the standard dose of paracetamol.
Adverse effects
In recommended doses and for a limited course of treatment, the side effects of paracetamol are mild to non-existent. However some risks and adverse correlations have been identified;
Liver damage
The ratio between fatal doses and therapeutic doses (the therapeutic index) is much smaller than for other over-the-counter painkillers. According to the US Food and Drug Administration as little as 25 percent above the maximum daily dose can cause liver damage when taken over several days.
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Paracetamol" – news · newspapers · books · scholar · JSTOR (January 2014) (Learn how and when to remove this message) |
Acute overdoses of paracetamol can cause potentially fatal liver damage. The risk may be heightened by chronic alcohol abuse. Paracetamol toxicity is the foremost cause of acute liver failure in the Western world, and accounts for most drug overdoses in the United States, the United Kingdom, Australia and New Zealand. In the United States, over 150 people die each year from overdoses, with up to 78,000 emergency room visits.
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Paracetamol" – news · newspapers · books · scholar · JSTOR (January 2014) (Learn how and when to remove this message) |
Paracetamol is metabolised by the liver and is hepatotoxic; side effects are multiplied when combined with alcoholic drinks, and very likely in chronic alcoholics or patients with liver damage. Some studies have suggested the possibility of a moderately increased risk of upper gastrointestinal complications such as stomach bleeding when high doses are taken chronically. Kidney damage is seen in rare cases, most commonly in overdose. The Food and Drug Administration has warned doctors against prescribing paracetamol/narcotic combinations whose dosages exceed 325 mg of paracetamol due to hepatoxicity risks of greater magnitude than the therapeutic benefits conferred.
Cancer
Chronic users of paracetamol may have a higher risk of developing blood cancer.
Skin reactions
On August 2, 2013, the U.S. Food and Drug Administration (FDA) issued a new warning about paracetamol. It stated that the drug could cause rare, and possibly fatal, skin reactions, such as Stevens–Johnson syndrome and toxic epidermal necrolysis. Prescription-strength products will be required to carry a warning label about skin reactions, and the FDA has urged manufacturers to do the same with over-the-counter products.
Hearing loss
Regular paracetamol use is correlated with increased hearing loss (ototoxicity).
Asthma
An epidemiological association between paracetamol (acetaminophen) use and asthmain children is well established. There is continuing debate over whether acetaminophen exposure increases the risk of asthma, or whether the association is due to "confounding by indication", in which the apparent association arises because illnesses commonly treated with acetaminophen predispose children to later development of asthma.
Other factors
In contrast to aspirin, paracetamol is not an antithrombotic, and thus may be used in patients where coagulation is a concern, and it does not cause gastric irritation. However, paracetamol does not help reduce inflammation, while aspirin does. Compared to ibuprofen—whose side effects may include diarrhea, vomiting and abdominal pain—paracetamol has fewer adverse gastrointestinal effects.
Paracetamol is generally believed to be safe for use in pregnancy as it does not affect the closure of the fetal ductus arteriosus as NSAIDs can. One prospective case control study examined the effects of paracetamol on fertility in male offspring in two cohorts, one in Finland and one in Denmark. A statistically significant increase in the incidence of undescended testicles was seen in the Danish cohort, but not in the Finnish group. Effects of paracetamol were seen mainly when used in combination with other analgesics.
Unlike aspirin, paracetamol is generally considered safe for children, as it is not associated with a risk of Reye's syndrome in children with viral illnesses. In one study, paracetamol use for fever in the first year of life was associated with a moderate increase in the incidence of asthmatic symptoms at 6–7 years, and that paracetamol use, both in the first year of life and in children aged 6–7 years, was associated with a moderate increased incidence of rhinoconjunctivitis and eczema.
Overdose
Main article: Paracetamol toxicityUntreated paracetamol overdose results in a lengthy, painful illness. Signs and symptoms of paracetamol toxicity may initially be absent or non-specific symptoms. The first symptoms of overdose usually begin several hours after ingestion, with nausea, vomiting, sweating, and pain as acute liver failure starts. People who take overdoses of paracetamol do not lose consciousness, although most people who use paracetamol wrongly believe that they will be rendered unconscious by the drug. The process of dying from an overdose usually takes three to five days.
Paracetamol hepatotoxicity is, by far, the most common cause of acute liver failure in both the United States and the United Kingdom. Toxicity of paracetamol arises often due to its quinone metabolite. Paracetamol overdose results in more calls to poison control centers in the US than overdose of any other pharmacological substance.
Untreated overdose can lead to liver failure and death within days. Treatment is aimed at removing the paracetamol from the body and replacing glutathione. Activated charcoal can be used to decrease absorption of paracetamol if the patient presents for treatment soon after the overdose. While the antidote, acetylcysteine, (also called N-acetylcysteine or NAC) acts as a precursor for glutathione, helping the body regenerate enough to prevent or at lease decrease the possible damage to the liver, a liver transplant is often required if damage to the liver becomes severe. NAC was usually given following a treatment nomogram (one for patients with risk factors, and one for those without) but the use of the nomogram is no longer recommended as the evidence base to support the use of risk factors was poor and inconsistent, and many of the risk factors are imprecise and difficult to determine with sufficient certainty in clinical practice. NAC also helps in neutralizing the imidoquinone metabolite of paracetamol. Renal failure is also a possible side effect.
There were tablets available until 2004 (brand-name in the UK Paradote) that combined paracetamol with an antidote (methionine), to protect the liver in case of an overdose. One theoretical, but rarely if ever used, option in the United States is to request a compounding pharmacy to make a similar drug mix for at-risk patients.
In June 2009, a U.S. Food and Drug Administration (FDA) advisory committee recommended that new restrictions should be placed on paracetamol usage in the United States to help protect people from the potential toxic effects. The maximum dosage at any given time would be decreased from 1000 mg to 650 mg, while combinations of paracetamol and narcotic analgesics would be prohibited. Committee members were particularly concerned by the fact that the present maximum dosages of paracetamol had been shown to produce alterations in hepatic function.
In January 2011, the FDA asked manufacturers of prescription combination products containing paracetamol to limit the amount of paracetamol to no more than 325 mg per tablet or capsule and began requiring manufacturers to update the labels of all prescription combination paracetamol products to warn of the potential risk for severe liver damage. Manufacturers will have three years to limit the amount of paracetamol in their prescription drug products to 325 mg per dosage unit. In November 2011, the Medicines and Healthcare products Regulatory Agency revised UK dosing of liquid paracetamol for children.
Mechanism of action


To date, the mechanism of action of paracetamol is not completely understood. The main mechanism proposed is the inhibition of cyclooxygenase (COX), and recent findings suggest that it is highly selective for COX-2. Because of its selectivity for COX-2 it does not significantly inhibit the production of the pro-clotting thromboxanes. While it has analgesic and antipyretic properties comparable to those of aspirin or other NSAIDs, its peripheral anti-inflammatory activity is usually limited by several factors, one of which is the high level of peroxides present in inflammatory lesions. However, in some circumstances, even peripheral anti-inflammatory activity comparable to NSAIDs can be observed.
An article in Nature Communications from researchers in London, UK and Lund, Sweden in November 2011 has found a hint to the analgesic mechanism of paracetamol, being that the metabolites of paracetamol e.g. NAPQI, act on TRPA1-receptors in the spinal cord to suppress the signal transduction from the superficial layers of the dorsal horn, to alleviate pain.
This conclusion has been contested in a new hypothesis paper on how paracetamol might act. The author concedes that NAPQI is the active metabolite but that this reactive compound should react not only with the thiol in TRPA1 but also with any other suitably available nucleophile that it happens to encounter. It is suggested that thiol groups in cysteine proteases, e.g. the proteases that take part in the processing of procytokines, such as those generating IL-1β and IL-6, might be the targets giving rise to overall analgesic effects.
The COX family of enzymes are responsible for the metabolism of arachidonic acid to prostaglandin H2, an unstable molecule that is, in turn, converted to numerous other pro-inflammatory compounds. Classical anti-inflammatories such as the NSAIDs block this step. Only when appropriately oxidised is the COX enzyme highly active. Paracetamol reduces the oxidised form of the COX enzyme, preventing it from forming pro-inflammatory chemicals. This leads to a reduced amount of prostaglandin E2 in the CNS, thus lowering the hypothalamic set-point in the thermoregulatory centre.
Aspirin is known to inhibit the cyclooxygenase (COX) family of enzymes and, because paracetamol's action is partially similar to aspirin's, much research has focused on whether paracetamol also inhibits COX. It is now clear that paracetamol acts via at least two pathways.
The exact mechanisms by which COX is inhibited in various circumstances are still a subject of discussion. Because of differences in the activity of paracetamol, aspirin, and other NSAIDs, it has been postulated that further COX variants may exist. One theory holds that paracetamol works by inhibiting the COX-3 isoform—a COX-1 splice variant—of the COX family of enzymes. When expressed in dogs, this enzyme shares a strong similarity to the other COX enzymes, produces pro-inflammatory chemicals, and is selectively inhibited by paracetamol. However, some research has suggested that, in humans and mice, the COX-3 enzyme is without inflammatory action and paracetamol's blockage of it is not significant in its functioning in humans.
Another possibility is that paracetamol blocks cyclooxygenase (as in aspirin), but that, in an inflammatory environment where the concentration of peroxides is high, the high oxidation state of paracetamol prevents its actions. This idea would mean that paracetamol has no direct effect at the site of inflammation, but instead acts in the CNS where the environment is not oxidative, to reduce temperature, etc.
Paracetamol also modulates the endogenous cannabinoid system. Paracetamol is metabolised to AM404, a compound with several actions; what is most important is that it inhibits the reuptake of the endogenous cannabinoid/vanilloid anandamide by neurons. Anandamide reuptake lowers synaptic levels of anandamide and results in more activation of the main pain receptor (nociceptor) of the body, the TRPV1 (older name: vanilloid receptor). By inhibiting anandamide reuptake, levels in the synapse remain high and are able to desensitise the TRPV1 receptor much like capsaicin. Furthermore, AM404 inhibits sodium channels, as do the anesthetics lidocaine and procaine. Either of these actions by themselves has been shown to reduce pain, and are a possible mechanism for paracetamol. However, it has been demonstrated that, after blocking cannabinoid receptors with synthetic antagonists, paracetamol's analgesic effects are prevented, suggesting its pain-relieving action involves the endogenous cannabinoid system. Spinal TRPA1 receptors have also been demonstrated to mediate antinociceptive effects of paracetamol and Δ9-tetrahydrocannabinol in mice.
Paracetamol's increase of social behavior in mice (which corresponds to its reduction of social rejection response in humans) does not appear to be due to cannabinoid receptor type 1 activity. It may result from serotonin receptor agonism.
Structure and reactivity

Paracetamol consists of a benzene ring core, substituted by one hydroxyl group and the nitrogen atom of an amide group in the para (1,4) pattern. The amide group is acetamide (ethanamide). It is an extensively conjugated system, as the lone pair on the hydroxyl oxygen, the benzene pi cloud, the nitrogen lone pair, the p orbital on the carbonyl carbon, and the lone pair on the carbonyl oxygen are all conjugated. The presence of two activating groups also make the benzene ring highly reactive toward electrophilic aromatic substitution. As the substituents are ortho, para-directing and para with respect to each other, all positions on the ring are more or less equally activated. The conjugation also greatly reduces the basicity of the oxygens and the nitrogen, while making the hydroxyl acidic through delocalisation of charge developed on the phenoxide anion.
Synthesis
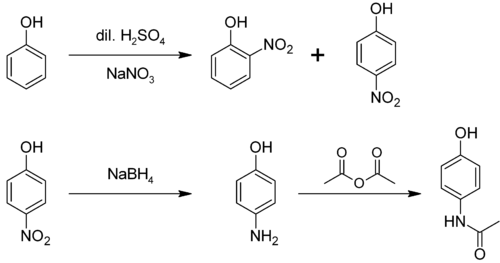
In the laboratory, paracetamol is prepared by nitrating phenol with sodium nitrate; steam-distillation of the result to collect the 4-nitrophenol (bp ~93 °C) from the other isomers; and reducing the nitro group with sodium borohydride. The resultant 4-aminophenol is then acetylated with acetic anhydride. In this reaction, phenol is strongly activating, thus the reaction requires only mild conditions (cf. the nitration of benzene). The industrial process is analogous, but hydrogenation is used instead of the sodium borohydride reduction.
A simpler synthesis by Hoechst-Celanese involves direct acylation of phenol with acetic anhydride catalyzed by HF, conversion of the ketone to a ketoxime with hydroxylamine, followed by the acid-catalyzed Beckmann rearrangement to give the amide.
Demand for paracetamol in the United States was estimated at 30–35 thousand tonnes per year in 1997, equal to the demand from the rest of the world.
Metabolism
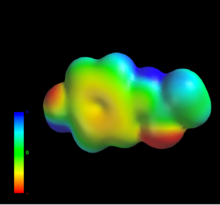
Paracetamol is metabolised primarily in the liver, into toxic and non-toxic products. Three metabolic pathways are notable:
- Glucuronidation is believed to account for 40% to two-thirds of the metabolism of paracetamol.
- Sulfation (sulfate conjugation) may account for 20–40%.
- N-hydroxylation and rearrangement, then GSH conjugation, accounts for less than 15%. The hepatic cytochrome P450 enzyme system metabolises paracetamol, forming a minor yet significant alkylating metabolite known as NAPQI (N-acetyl-p-benzo-quinone imine)(also known as N-acetylimidoquinone). NAPQI is then irreversibly conjugated with the sulfhydryl groups of glutathione.
All three pathways yield final products that are inactive, non-toxic, and eventually excreted by the kidneys. In the third pathway, however, the intermediate product NAPQI is toxic. NAPQI is primarily responsible for the toxic effects of paracetamol; this constitutes an example of toxication.
Production of NAPQI is due primarily to two isoenzymes of cytochrome P450: CYP2E1 and CYP1A2. The P450 gene is highly polymorphic, however, and individual differences in paracetamol toxicity are believed due to a third isoenzyme, CYP2D6. Genetic polymorphisms in CYP2D6 may contribute to significantly different rates of production of NAPQI. Furthermore, individuals can be classified as "extensive", "ultrarapid", "intermediate" and "poor" metabolisers (producers of NAPQI), depending on their levels of CYP2D6 expression. Although CYP2D6 metabolises paracetamol into NAPQI to a lesser extent than other P450 enzymes, its activity may contribute to paracetamol toxicity in extensive and ultrarapid metabolisers, and when paracetamol is taken at very large doses. At usual doses, NAPQI is quickly detoxified by conjugation with glutathione. Following overdose, and possibly also in extensive and ultrarapid metabolisers, this detoxification pathway becomes saturated, and, as a consequence, NAPQI accumulates causing liver and renal toxicity.
Reactions
4-Aminophenol may be obtained by the amide hydrolysis of paracetamol. 4-Aminophenol prepared this way, and related to the commercially available Metol, has been used as a developer in photography by hobbyists. This reaction is also used to determine paracetamol in urine samples: After hydrolysis with hydrochloric acid, 4-aminophenol reacts in ammonia solution with a phenol derivate, e.g. salicylic acid, to form an indophenol dye under oxidization by air.
History
Acetanilide was the first aniline derivative serendipitously found to possess analgesic as well as antipyretic properties, and was quickly introduced into medical practice under the name of Antifebrin by A. Cahn and P. Hepp in 1886. But its unacceptable toxic effects, the most alarming being cyanosis due to methemoglobinemia, prompted the search for less toxic aniline derivatives. Harmon Northrop Morse had already synthesised paracetamol at Johns Hopkins University via the reduction of p-nitrophenol with tin in glacial acetic acid in 1877, but it was not until 1887 that clinical pharmacologist Joseph von Mering tried paracetamol on patients. In 1893, von Mering published a paper reporting on the clinical results of paracetamol with phenacetin, another aniline derivative. Von Mering claimed that, unlike phenacetin, paracetamol had a slight tendency to produce methemoglobinemia. Paracetamol was then quickly discarded in favor of phenacetin. The sales of phenacetin established Bayer as a leading pharmaceutical company. Overshadowed in part by aspirin, introduced into medicine by Heinrich Dreser in 1899, phenacetin was popular for many decades, particularly in widely advertised over-the-counter "headache mixtures", usually containing phenacetin, an aminopyrine derivative of aspirin, caffeine, and sometimes a barbiturate.
Von Mering's claims remained essentially unchallenged for half a century, until two teams of researchers from the United States analyzed the metabolism of acetanilide and paracetamol. In 1947 David Lester and Leon Greenberg found strong evidence that paracetamol was a major metabolite of acetanilide in human blood, and in a subsequent study they reported that large doses of paracetamol given to albino rats did not cause methemoglobinemia. In three papers published in the September 1948 issue of the Journal of Pharmacology and Experimental Therapeutics, Bernard Brodie, Julius Axelrod and Frederick Flinn confirmed using more specific methods that paracetamol was the major metabolite of acetanilide in human blood, and established that it was just as efficacious an analgesic as its precursor. They also suggested that methemoglobinemia is produced in humans mainly by another metabolite, phenylhydroxylamine. A follow-up paper by Brodie and Axelrod in 1949 established that phenacetin was also metabolised to paracetamol. This led to a "rediscovery" of paracetamol. It has been suggested that contamination of paracetamol with 4-aminophenol, the substance von Mering synthesised it from, may be the cause for his spurious findings.
Paracetamol was first marketed in the United States in 1950 under the name Triagesic, a combination of paracetamol, aspirin, and caffeine. Reports in 1951 of three users stricken with the blood disease agranulocytosis led to its removal from the marketplace, and it took several years until it became clear that the disease was unconnected. Paracetamol was marketed in 1953 by Sterling-Winthrop Co. as Panadol, available only by prescription, and promoted as preferable to aspirin since it was safe for children and people with ulcers. In 1955, paracetamol was marketed as Children's Tylenol Elixir by McNeil Laboratories. In 1956, 500 mg tablets of paracetamol went on sale in the United Kingdom under the trade name Panadol, produced by Frederick Stearns & Co, a subsidiary of Sterling Drug Inc. Panadol was originally available only by prescription, for the relief of pain and fever, and was advertised as being "gentle to the stomach," since other analgesic agents of the time contained aspirin, a known stomach irritant. In 1963, paracetamol was added to the British Pharmacopoeia, and has gained popularity since then as an analgesic agent with few side-effects and little interaction with other pharmaceutical agents. Concerns about paracetamol's safety delayed its widespread acceptance until the 1970s, but in the 1980s paracetamol sales exceeded those of aspirin in many countries, including the United Kingdom. This was accompanied by the commercial demise of phenacetin, blamed as the cause of analgesic nephropathy and hematological toxicity.
The U.S. patent on paracetamol has long expired, and generic versions of the drug are widely available under the Drug Price Competition and Patent Term Restoration Act of 1984, although certain Tylenol preparations were protected until 2007. U.S. patent 6,126,967 filed September 3, 1998 was granted for "Extended release acetaminophen particles".
Available forms
See also: List of paracetamol brand names Tylenol 500 mg capsules
Tylenol 500 mg capsules Panadol 500 mg tablets
Panadol 500 mg tablets For comparison: The pure drug is a white crystalline powder.
For comparison: The pure drug is a white crystalline powder.
Paracetamol is available in a tablet, capsule, liquid suspension, suppository, intravenous, intramuscular and Effervescent form. The common adult dose is 500 mg to 1000 mg. The recommended maximum daily dose, for adults, is 4000 mg. In recommended doses, paracetamol is generally safe for children and infants, as well as for adults, although rare cases of acute liver injury have been linked to amounts lower than 2500 mg per day.
Panadol,which is marketed in Africa, Asia, Europe, Central America, and Australasia, is the most widely available brand of paracetamol, sold in over 80 countries. In North America, paracetamol is sold in generic form (usually labeled as acetaminophen) or under a number of trade names, for instance, Tylenol (McNeil-PPC, Inc.), Anacin-3, Tempra, Datril, and Ofirmev. In West Africa, paracetamol is sold in generic form (usually labeled as acetaminophen) or under a number of trade names, for instance, Apramol (Ajanta Pharma.). While there is brand named paracetamol available in the UK (e.g. Panadol), unbranded or generic paracetamol is more commonly sold. Acamol, a brand name for paracetamol produced by Teva Pharmaceutical Industries in Israel, is one of the most widely used drugs in that country. In the Philippines, the largest-selling paracetamol brand is Biogesic, manufactured by the drug giant United Laboratories. Biogesic tablet sales reach nearly a billion units each year in the country alone, not including liquid suspension formats. The brand is also available in most of the ASEAN countries where the drug giant has market presence. In Europe, the most common brands of paracetamol are Efferalgan and Doliprane. In India, the most common brand of paracetamol is Crocin manufactured by Glaxo SmithKline Asia. In Bangladesh the most popular two brand are Napa and Renova manufactured by Beximco Pharma and Opsonin Pharma respectively. In China paracetamol is sold over the counter as Duìyǐxiān'ānjīfēn Piàn (对乙酰氨基酚片). Likewise in Japan it is sold under the name Acetaminophen (アセトアミノフェン, Asetoaminofen). In North Korea the DPRK-Swiss joint venture PyongSu Pharma markets the drug as PyongSu Cetamol.
In some formulations, paracetamol is combined with the opioid codeine, sometimes referred to as co-codamol (BAN). In the United States and Canada, this is marketed under the name of Tylenol #1/2/3/4, which contain 8–10 mg, 15 mg, 30 mg, and 60 mg of codeine, respectively. In the U.S., this combination is available only by prescription, while the lowest-strength preparation is over-the-counter in Canada, and, in other countries, other strengths may be available over the counter. There are generic forms of these combinations as well. In the UK and in many other countries, this combination is marketed under the names of Tylex CD and Panadeine. Other names include Captin, Disprol, Dymadon, Fensum, Hedex, Mexalen, Nofedol, Panocod, Paralen, Pediapirin, Perfalgan, and Solpadeine. Paracetamol is also combined with other opioids such as dihydrocodeine, referred to as co-dydramol (BAN), oxycodone or hydrocodone, marketed in the U.S. as Percocet and Vicodin, respectively. Another very commonly used analgesic combination includes paracetamol in combination with propoxyphene napsylate, sold under the brand name Darvocet. A combination of paracetamol, codeine, and the calmative doxylamine succinate is marketed as Syndol or Mersyndol. The efficacy of paracetamol/codeine combinations have been questioned by recent research.
Paracetamol is commonly used in multi-ingredient preparations for migraine headache, typically including butalbital and paracetamol with or without caffeine, and sometimes containing codeine.
Veterinary use
Cats
Paracetamol is extremely toxic to cats, which lack the necessary glucuronyl transferase enzymes to safely break it down. Initial symptoms include vomiting, salivation, and discolouration of the tongue and gums.
Unlike an overdose in humans, liver damage is rarely the cause of death; instead, methemoglobin formation and the production of Heinz bodies in red blood cells inhibit oxygen transport by the blood, causing asphyxiation (methemoglobemia and hemolytic anemia).
Treatment with N-acetylcysteine, methylene blue or both is sometimes effective after the ingestion of small doses of paracetamol.
Dogs
Although paracetamol is believed to have no significant anti-inflammatory activity, it has been reported as effective as aspirin in the treatment of musculoskeletal pain in dogs.
A paracetamol-codeine product (trade name Pardale-V) licensed for use in dogs is available on veterinary prescription in the UK. It should be administered to dogs only on veterinary advice and with extreme caution.
The main effect of toxicity in dogs is liver damage, GI ulceration has been reported. N-acetylcysteine treatment is efficacious in dogs when administered within a 2 hours of paracetamol ingestion.
Snakes
Paracetamol is also lethal to snakes, and has been suggested as a chemical control program for the invasive brown tree snake (Boiga irregularis) in Guam. Doses of 80 mg are inserted into dead mice scattered by helicopter.
Controversy
In September 2013 an episode of This American Life entitled "Use Only as Directed" highlighted deaths from acetominophen overdose. This report was followed by two reports by ProPublica alleging that the "FDA has long been aware of studies showing the risks of acetaminophen. So has the maker of Tylenol, McNeil Consumer Healthcare, a division of Johnson & Johnson" and "McNeil, the maker of Tylenol, ... has repeatedly opposed safety warnings, dosage restrictions and other measures meant to safeguard users of the drug.".
A report prepared by an internal FDA working group describes a history of FDA initiatives designed to educate consumers about the risk of acetominophen overdose, and notes that one challenge to the Agency has been "identifying the appropriate message about the relative safety of acetaminophen, especially compared to other OTC pain relievers (e.g., aspirin and other NSAIDs)". The report notes that "Chronic use of NSAIDs is also associated with significant morbidity and mortality. NSAID gastrointestinal risk is substantial, with deaths and hospitalization estimated in one publication as 3200 and 32,000 per year respectively. Possible cardiovascular toxicity with chronic NSAID use has been a major discussion recently", finally noting that "The goal of the educational efforts is not to decrease appropriate acetaminophen use or encourage substitution of NSAID use, but rather to educate consumers so that they can avoid unnecessary health risks."
Classification
Paracetamol is part of the class of drugs known as "aniline analgesics"; it is the only such drug still in use today. It is not considered an NSAID because it does not exhibit significant anti-inflammatory activity (it is a weak COX inhibitor). This is despite the evidence that paracetamol and NSAIDs have some similar pharmacological activity.
References
- "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1021/ci0500132, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1021/ci0500132instead. - "melting point data for paracetamol". Lxsrv7.oru.edu. Retrieved 2011-03-19.
- Granberg RA, Rasmuson AC (1999). "Solubility of paracetamol in pure solvents". Journal of Chemical & Engineering Data. 44 (6): 1391–95. doi:10.1021/je990124v.
- Aghababian, Richard V. (22 October 2010). Essentials of Emergency Medicine. Jones & Bartlett Publishers. p. 814. ISBN 978-1-4496-1846-9.
- Ahmad, Jawad (17 October 2010). Hepatology and Transplant Hepatology: A Case Based Approach. Springer. p. 194. ISBN 978-1-4419-7085-5.
- ^ International Nonproprietary Names (INN) for Pharmaceutical Substances: Lists 1-96 of Proposed INN and lists 1-57 of Recommended INN, cumulative list N°12. World Health Organization. 2007. p. v. ISBN 9789240560253. Retrieved 20 January 2014.
- ^ Macintyre, Pamela; Rowbotham, David; Walker, Suellen (26 September 2008). Clinical Pain Management Second Edition: Acute Pain. CRC Press. p. 85. ISBN 978-0-340-94009-9.
- Scottish Intercollegiate Guidelines Network (SIGN) (2008). "6.1 and 7.1.1". Guideline 106: Control of pain in adults with cancer (PDF). Scotland: National Health Service (NHS). ISBN 9781905813384.
- Acetaminophen Drugs.com
- ^ "www.fda.gov" (PDF).
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1093/bja/aei109, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1093/bja/aei109instead. - Bergman K, Müller L, Teigen SW (1996). "The genotoxicity and carcinogenicity of paracetamol: a regulatory (re)view". Mutat Res. 349 (2): 263–88. doi:10.1016/0027-5107(95)00185-9. PMID 8600357.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Acetaminophen". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- "Baby paracetamol asthma concern". BBC News. September 19, 2008. Retrieved September 19, 2008.
- Meremikwu M, Oyo-Ita A (2002). "Paracetamol for treating fever in children". Cochrane Database Syst Rev (2): CD003676. doi:10.1002/14651858.CD003676. PMID 12076499.
- Perrott DA, Piira T, Goodenough B, Champion GD (2004). "Efficacy and safety of acetaminophen vs ibuprofen for treating children's pain or fever: a meta-analysis". Arch Pediatr Adolesc Med. 158 (6): 521–6. doi:10.1001/archpedi.158.6.521. PMID 15184213.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Medication and Drugs". MedicineNet. 1996–2010. Retrieved April 22, 2010.
{{cite news}}: CS1 maint: date format (link) - "Paracetamol". Arthritis Research UK. Retrieved October 16, 2013.
- Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI (1991). "Comparison of an anti-inflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee". N. Engl. J. Med. 325 (2): 87–91. doi:10.1056/NEJM199107113250203. PMID 2052056.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1111/j.1365-2710.2006.00754.x, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1111/j.1365-2710.2006.00754.xinstead. - Anton J M de Craen, Giuseppe Di Giulio, Angela J E M Lampe-Schoenmaeckers, Alphons G H Kessels, Jos Kleijnen (1996). "Analgesic efficacy and safety of paracetamol-codeine combinations versus paracetamol alone: a systematic review". BMJ. 313 (7053): 321–324. doi:10.1136/bmj.313.7053.321.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Laurence Toms, Sheena Derry, R Andrew Moore, Henry J McQuay (2009). "Single dose oral paracetamol (acetaminophen) with codeine for postoperative pain in adults". Cochrane Database of Systematic Reviews (1). doi:10.1002/14651858.CD001547.pub2.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Murnion B (2010). "Combination analgesics in adults". Australian Prescriber (33): 113–5.
- Clark E, Plint AC, Correll R, Gaboury I, Passi B (2007). "A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma". Pediatrics. 119 (3): 460–7. doi:10.1542/peds.2006-1347. PMID 17332198.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hughes, John (2008). Pain Management: From Basics to Clinical Practice. Elsevier Health Sciences. ISBN 9780443103360.
- ^ "Use Only as Directed". ProPublica. 2013-09-20. Retrieved 2013-09-21.
- ^ Daly FF, Fountain JS, Murray L, Graudins A, Buckley NA (2008). "Guidelines for the management of paracetamol poisoning in Australia and New Zealand—explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres". Med J Aust. 188 (5): 296–301. PMID 18312195.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Khashab M, Tector AJ, Kwo PY (2007). "Epidemiology of acute liver failure". Curr Gastroenterol Rep. 9 (1): 66–73. doi:10.1007/s11894-008-0023-x. PMID 17335680.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hawkins LC, Edwards JN, Dargan PI (2007). "Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature". Drug Saf. 30 (6): 465–79. doi:10.2165/00002018-200730060-00002. PMID 17536874.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Larson AM, Polson J, Fontana RJ, et al. (2005). "Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study". Hepatology. 42 (6): 1364–72. doi:10.1002/hep.20948. PMID 16317692.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Dukes, MNG (2000). Meyler's Side Effects of Drugs, Vol XIV. Elsevier. ISBN 9780444500939.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - García Rodríguez LA, Hernández-Díaz S (December 15, 2000). "The risk of upper gastrointestinal complications associated with nonsteroidal anti-inflammatory drugs, glucocorticoids, acetaminophen, and combinations of these agents". Arthritis Research & Therapy. 3 (2): 98–101. doi:10.1186/ar146. PMC 128885. PMID 11178116.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Sarg, Michael (2007). The Cancer Dictionary. Infobase Publishing. ISBN 9780816064113.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - "Painkillers 'cause kidney damage'". BBC News. November 23, 2003. Retrieved March 27, 2010.
- "FDA: Acetaminophen doses over 325 mg might lead to liver damage". Cnn.com. Retrieved 2014-02-18.
- Roland B. Walter, Filippo Milano, Theodore M. Brasky and Emily White (2011). "Long-Term Use of Acetaminophen, Aspirin, and Other Nonsteroidal Anti-Inflammatory Drugs and Risk of Hematologic Malignancies: Results From the Prospective Vitamins and Lifestyle (VITAL) Study". Journal of Clinical Oncology. 29 (17): 2424–31. doi:10.1200/JCO.2011.34.6346. PMC 3107756. PMID 21555699.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Acetaminophen linked to rare fatal skin reactions, FDA says". Washington Post. Retrieved 3 August 2013.
- "Analgesic Use and the Risk of Hearing Loss in Women". Aje.oxfordjournals.org. Retrieved 2014-02-18.
- USA (2014-01-24). "Acetaminophen ototoxicity after a... [Otolaryngol Head Neck Surg. 2010] - PubMed - NCBI". Ncbi.nlm.nih.gov. Retrieved 2014-02-18.
- "Hearing and common painkillers - Health news - NHS Choices". Nhs.uk. 2010-03-05. Retrieved 2014-02-18.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22065272, please use {{cite journal}} with
|pmid=22065272instead. - Heintze K, Petersen KU (2013). "The case of drug causation of childhood asthma: antibiotics and paracetamol". Eur. J. Clin. Pharmacol. 69 (6): 1197–209. doi:10.1007/s00228-012-1463-7. PMC 3651816. PMID 23292157.
{{cite journal}}: Unknown parameter|month=ignored (help) - Henderson AJ, Shaheen SO (2013). "Acetaminophen and asthma". Paediatr Respir Rev. 14 (1): 9–15, quiz 16. doi:10.1016/j.prrv.2012.04.004. PMID 23347656.
{{cite journal}}: Unknown parameter|month=ignored (help) - Neuss,G (2007). Chemistry: Course Companion. Oxford University Press. ISBN 978-0-19-915146-2.
- Ebrahimi, Sedigheh (2010). "Comparison of efficacy and safety of acetaminophen and ibuprofen administration as single dose to reduce fever in children". Iranian Journal of Pediatrics. 20 (4): 500–501.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - "Can I take paracetamol when I'm pregnant? - Health questions - NHS Choices". Nhs.uk. 2013-05-25. Retrieved 2014-02-18.
- Rudolph AM (1981). "Effects of aspirin and acetaminophen in pregnancy and in the newborn". Arch. Intern. Med. 141 (3 Spec No): 358–63. doi:10.1001/archinte.141.3.358. PMID 7469626.
- Lesko SM, Mitchell AA (1999). "The safety of acetaminophen and ibuprofen among children younger than two years old". Pediatrics. 104 (4): e39. doi:10.1542/peds.104.4.e39. PMID 10506264.
- Beasley, Richard; Clayton, Tadd; Crane, Julian; von Mutius, Erika; Lai, Christopher; Montefort, Stephen; Stewart, Alistair (2008). "Association between paracetamol use in infancy and childhood, and risk of asthma, rhino conjunctivitis, and eczema in children aged 6–7 years: analysis from Phase Three of the ISAAC programme". The Lancet. 372 (9643): 1039–1048. doi:10.1016/S0140-6736(08)61445-2.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Medicines and Healthcare products Regulatory Agency; Commission on Human Medicines (2008). "Paracetamol use in infancy: no strong evidence for asthma link". Drug Safety Update. 2 (4): 9. Retrieved May 1, 2009.
- Rumack B, Matthew H (1975). "Acetaminophen poisoning and toxicity". Pediatrics. 55 (6): 871–76. PMID 1134886.
- "Paracetamol". University of Oxford Centre for Suicide Research. 25 March 2013. Retrieved 20 April 2013.
- Ryder SD, Beckingham IJ (2001). "ABC of diseases of liver, pancreas, and biliary system. Other causes of parenchymal liver disease". BMJ. 322 (7281): 290–92. doi:10.1136/bmj.322.7281.290. PMC 1119531. PMID 11157536.
- ^ Mehta, Sweety (August 25, 2012) Metabolism of Paracetamol (Acetaminophen), Acetanilide and Phenacetin. pharmaxchange.info
- Lee WM (2004). "Acetaminophen and the U. S. Acute Liver Failure Study Group: lowering the risks of hepatic failure". Hepatology. 40 (1): 6–9. doi:10.1002/hep.20293. PMID 15239078.
- "Highlights of Prescribing Information" (PDF). Acetadote. Retrieved 2014-02-10.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - "Paracetamol overdose: new guidance on treatment with intravenous acetylcysteine". Drug Safety Update. 6 (2): A1. September 2012.
- "FDA May Restrict Acetaminophen". Webmd.com. 2009-07-01. Retrieved 2011-03-19.
- "FDA limits acetaminophen in prescription combination products; requires liver toxicity warnings" (Press release). U. S. Food and Drug Administration (FDA). January 13, 2011. Retrieved January 13, 2011.
- ^ "FDA Drug Safety Communication: Prescription Acetaminophen Products to be Limited to 325 mg Per Dosage Unit; Boxed Warning Will Highlight Potential for Severe Liver Failure". U. S. Food and Drug Administration (FDA). January 13, 2011. Retrieved January 13, 2011.
- Matthew Perrone (January 13, 2011). "FDA orders lowering pain reliever in Vicodin". The Boston Globe. Associated Press. Retrieved January 13, 2011.
- ^ Gardiner Harris (January 13, 2011). "F. D. A. Plans New Limits on Prescription Painkillers". The New York Times. Retrieved January 13, 2011.
- "Liquid paracetamol for children: Revised UK dosing instructions have been introduced". Mhra.gov.uk. Retrieved 2014-02-18.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17884974, please use {{cite journal}} with
|pmid=17884974instead. - Andersson DA, Gentry C, Alenmyr L, Killander D, Lewis SE, Andersson A, Bucher B, Galzi J-L, Sterner O, Bevan S, Högestätt ED, Zygmunt PM (2011). "TRPA1 mediates spinal antinociception induced by acetaminophen and the cannabinoid Δ(9)-tetrahydrocannabiorcol". Nat Commun. 2: 551. doi:10.1038/ncomms1559. PMID 22109525.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Claesson, A. "On the mechanism of paracetamol's analgesic activity and a note on related NSAID pharmacology". SlideShare. Retrieved 1 March 2013.
- Ohki S, Ogino N, Yamamoto S, Hayaishi O (1979). "Prostaglandin hydroperoxidase, an integral part of prostaglandin endoperoxide synthetase from bovine vesicular gland microsomes". J. Biol. Chem. 254 (3): 829–36. PMID 104998.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Harvison PJ, Egan RW, Gale PH, Nelson SD (1986). "Acetaminophen as a cosubstrate and inhibitor of prostaglandin H synthase". Adv. Exp. Med. Biol. Advances in Experimental Medicine and Biology. 197: 739–47. doi:10.1007/978-1-4684-5134-4_68. ISBN 978-1-4684-5136-8. PMID 3094341.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Aronoff DM, Oates JA, Boutaud O (2006). "New insights into the mechanism of action of acetaminophen: Its clinical pharmacologic characteristics reflect its inhibition of the two prostaglandin H2 synthases". Clin. Pharmacol. Ther. 79 (1): 9–19. doi:10.1016/j.clpt.2005.09.009. PMID 16413237.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Roberts, L.J. II. & Marrow, J.D. "Analgesic-antipyretic and Antiinflammatory Agents and Drugs Employed in the Treatment of Gout" in, "Goodman & Gilman's The Pharmacological Basis of Therapeutics 10th Edition" by Hardman, J.G. & Limbird, L.E. Published by McGraw Hill, 2001, pp.687–731 ISBN 0071354697
- ^ Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S (2006). "Paracetamol: new vistas of an old drug". CNS Drug Reviews. 12 (3–4): 250–75. doi:10.1111/j.1527-3458.2006.00250.x. PMID 17227290.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kis B, Snipes JA, Busija DW (2005). "Acetaminophen and the cyclooxygenase-3 puzzle: sorting out facts, fictions, and uncertainties". J. Pharmacol. Exp. Ther. 315 (1): 1–7. doi:10.1124/jpet.105.085431. PMID 15879007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Graham GG, Scott KF (2005). "Mechanism of action of paracetamol". American journal of therapeutics. 12 (1): 46–55. doi:10.1097/00045391-200501000-00008. PMID 15662292.
- ^ Chandrasekharan NV, Dai H, Roos KL; et al. (2002). "COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression". Proc. Natl. Acad. Sci. U.S.A. 99 (21): 13926–31. doi:10.1073/pnas.162468699. PMC 129799. PMID 12242329.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Högestätt ED, Jönsson BA, Ermund A; et al. (2005). "Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system". J. Biol. Chem. 280 (36): 31405–12. doi:10.1074/jbc.M501489200. PMID 15987694.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Köfalvi A (2008). "9. Alternative interacting sites and novel receptors for cannabinoid ligands". Cannabinoids and the Brain. Springer-Verlag. pp. 131–160. doi:10.1007/978-0-387-74349-3_9. ISBN 978-0-387-74348-6.
- Ottani A, Leone S, Sandrini M, Ferrari A, Bertolini A (2006). "The analgesic activity of paracetamol is prevented by the blockade of cannabinoid CB1 receptors". Eur. J. Pharmacol. 531 (1–3): 280–1. doi:10.1016/j.ejphar.2005.12.015. PMID 16438952.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Andersson, David; Gentry, Clive; Alenmyr, Lisa; Killander, Dan; Lewis, Simon E; Andersson, Anders; Bucher, Bernard; Galzi, Jean-Luc; Sterner, Olov (November 2011). "TRPA1 mediates spinal antinociception induced by acetaminophen and the cannabinoid Δ9-tetrahydrocannabiorcol". Nature Communications. 2 (2): 551. doi:10.1038/ncomms1559. PMID 22109525.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22542870, please use {{cite journal}} with
|pmid=22542870instead. - Bales, JR (1985). "Two-dimensional proton nuclear magnetic resonance "maps" of acetaminophen metabolites in human urine". Clinical Chemistry. 31 (5): 757–762. PMID 3987005.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Ellis, Frank (2002). Paracetamol: a curriculum resource. Cambridge: Royal Society of Chemistry. ISBN 0-85404-375-6.
- Anthony S. Travis (2007). "Manufacture and uses of the anilines: A vast array of processes and products". In Zvi Rappoport (ed.). The chemistry of Anilines Part 1. Wiley. p. 764. ISBN 978-0-470-87171-3.
- ^ Elmar Friderichs, Thomas Christoph, Helmut Buschmann. "Analgesics and Antipyretics". Ullmann's Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH. doi:10.1002/14356007.a02_269.pub2. ISBN 978-3527306732.
{{cite encyclopedia}}: CS1 maint: multiple names: authors list (link) - US patent 4524217, Kenneth G. Davenport & Charles B. Hilton, "Process for producing N-acyl-hydroxy aromatic amines", published 1985-06-18, assigned to Celanese Corporation
- "Paracetamol" (PDF). IARC Monographs. 73: 401.
- ^ Hendrickson, Robert G.; Kenneth E. Bizovi (2006). "Acetaminophen", in Nelson, Lewis H.; Flomenbaum, Neal; Goldfrank, Lewis R. et al. Goldfrank's toxicologic emergencies, p. 525, New York: McGraw-Hill. Retrieved on January 18, 2009 through Google Book Search.
- ^ Borne, Ronald F. "Nonsteroidal Anti-inflammatory Drugs" in Principles of Medicinal Chemistry, Fourth Edition. Eds. Foye, William O.; Lemke, Thomas L.; Williams, David A. Published by Williams & Wilkins, 1995. p. 544–545.
- Dong, H; Haining, RL; Thummel, KE; Rettie, AE; Nelson, SD (2000). "Involvement of human cytochrome P450 2D6 in the bioactivation of acetaminophen". Drug Metab Dispos. 28 (12): 1397–400. PMID 11095574.
- Henney, K (1939). Handbook of Photography. Whittlesey House. p. 324.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Novotny PE, Elser RC (1984). "Indophenol method for acetaminophen in serum examined" (PDF). Clin. Chem. 30 (6): 884–6. PMID 6723045.
- Cahn, A (1886). "Das Antifebrin, ein neues Fiebermittel". Centralbl. Klin. Med. 7: 561–64.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Morse HN (1878). "Ueber eine neue Darstellungsmethode der Acetylamidophenole". Berichte der deutschen chemischen Gesellschaft (in German). 11 (1): 232–3. doi:10.1002/cber.18780110151.
- ^ Milton Silverman, Mia Lydecker, Philip Randolph Lee (1992). Bad Medicine: The Prescription Drug Industry in the Third World. Stanford University Press. pp. 88–90. ISBN 0804716692.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Von Mering J. (1893) Beitrage zur Kenntniss der Antipyretica. Ther Monatsch 7: 577–587.
- ^ Sneader, Walter (2005). Drug Discovery: A History. Hoboken, N.J.: Wiley. p. 439. ISBN 0471899801.
- Lester D, Greenberg LA, Carroll RP (1947). "The metabolic fate of acetanilid and other aniline derivatives: II. Major metabolites of acetanilid appearing in the blood". J. Pharmacol. Exp. Ther. 90 (1): 68–75. PMID 20241897.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Brodie, BB (1948). "The estimation of acetanilide and its metabolic products, aniline, N-acetyl p-aminophenol and p-aminophenol (free and total conjugated) in biological fluids and tissues". J. Pharmacol. Exp. Ther. 94 (1): 22–28. PMID 18885610.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Brodie, BB (1948). "The fate of acetanilide in man" (PDF). J. Pharmacol. Exp. Ther. 94 (1): 29–38. PMID 18885611.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Flinn, Frederick B (1948). "The effect on the pain threshold of N-acetyl p-aminophenol, a product derived in the body from acetanilide". J. Pharmacol. Exp. Ther. 94 (1): 76–77. PMID 18885618.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Brodie BB, Axelrod J (1949). "The fate of acetophenetidin (phenacetin) in man and methods for the estimation of acetophenitidin and its metabolites in biological material". J Pharmacol Exp Ther. 94 (1): 58–67.
- Landau, Ralph; Achilladelis, Basil; Scriabine, Alexander (1999). Pharmaceutical Innovation: Revolutionizing Human Health. Chemical Heritage Foundation. pp. 248–249. ISBN 978-0-941901-21-5.
- Rapoport, Alan (15 December 1991). Headache Relief. Touchstone. p. 97. ISBN 978-0-671-74803-6.
- US patent 6126967, "Extended release acetaminophen particles", issued October 03, 2000
- "Acetaminophen." Physicians' Desk Reference, 63rd ed. Montvale, NJ: Thomson PDR; 2009: 1915–1916.
- "Acetaminophen Overdose and Liver Injury—Background and Options for Reducing Injury", Charles Ganley, MD, Gerald Dal Pan, MD, Bob Rappaport, MD, May 22, 2009, Retrieved July 8, 2010.
- "对乙酰氨基酚片说明书" (in Chinese). Beijing: Chinapharm. Retrieved 18 July 2010.
{{cite web}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - Allen AL (2003). "The diagnosis of acetaminophen toxicosis in a cat". Can Vet J. 44 (6): 509–10. PMC 340185. PMID 12839249.
- ^ Richardson, JA (2000). "Management of acetaminophen and ibuprofen toxicoses in dogs and cats" (PDF). J. Vet. Emerg. Crit. Care. 10 (4): 285–91. doi:10.1111/j.1476-4431.2000.tb00013.x.
- ^ Maddison, Jill E. (2002). Small Animal Clinical Pharmacology. Elsevier Health Sciences. pp. 260–1. ISBN 0702025739.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Pardale-V Oral Tablets". NOAH Compendium of Data Sheets for Animal Medicines. The National Office of Animal Health (NOAH). 11 November 2010. Retrieved 20 January 2011.
- Villar D, Buck WB, Gonzalez JM (1998). "Ibuprofen, aspirin and acetaminophen toxicosis and treatment in dogs and cats". Vet Hum Toxicol. 40 (3): 156–62. PMID 9610496.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Meadows, Irina; Gwaltney-Brant, Sharon (2006). "The 10 Most Common Toxicoses in Dogs". Veterinary Medicine: 142–8.
- Dunayer, E (2004). "Ibuprofen toxicosis in dogs, cats, and ferrets". Veterinary Medicine: 580–6.
- Johnston J, Savarie P, Primus T, Eisemann J, Hurley J, Kohler D (2002). "Risk assessment of an acetaminophen baiting program for chemical control of brown tree snakes on Guam: evaluation of baits, snake residues, and potential primary and secondary hazards". Environ Sci Technol. 36 (17): 3827–33. doi:10.1021/es015873n. PMID 12322757.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Brad Lendon (2010-09-07). "Tylenol-loaded mice dropped from air to control snakes". CNN. Retrieved 2010-09-07.
- Sabrina Richards (2012-05-01). "It's Raining Mice". The Scientist.
- "Use Only as Directed". This American Life. Episode 505. 20 September 2013. Public Radio International. WBEZ. Retrieved 24 September 2013.
{{cite episode}}: Unknown parameter|city=ignored (|location=suggested) (help); Unknown parameter|serieslink=ignored (|series-link=suggested) (help) - Gerth, Jeff (20 September 2013). "Use Only as Directed". ProPublica. Retrieved 24 September 2013.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Miller, T. Christian (20 September 2013). "Dose of Confusion". ProPublica. Retrieved 24 September 2013.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1158/0008-5472.CAN-07-6257, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1158/0008-5472.CAN-07-6257instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15254653, please use {{cite journal}} with
|pmid=15254653instead. - Byrant, Bronwen; Knights, Katleen; Salerno, Evelyn (2007). Pharmacology for health professionals. Elsevier. p. 270. ISBN 9780729537872.
{{cite book}}: CS1 maint: multiple names: authors list (link)
External links
- Paracetamol at Chemsynthesis
- Paracetamol International Chemical Safety Cards
- The Julius Axelrod Papers
- FDA: Safe Use of Over-the-Counter Pain Relievers/Fever Reducers
- FDA: Consumer Update "Acetaminophen and Liver Injury: Q and A for Consumers" (link)
- FDA: Consumer Update "Acetaminophen and Liver Injury: Q and A for Consumers" (PDF)
- U.S. National Library of Medicine: Drug Information Portal–Paracetamol
- Acetaminophen bound to proteins in the PDB
| Cannabinoids | |||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phytocannabinoids (comparison) |
| ||||||||||||||||||||||||||||||||||||||||
| Endocannabinoids |
| ||||||||||||||||||||||||||||||||||||||||
| Synthetic cannabinoid receptor agonists / neocannabinoids |
| ||||||||||||||||||||||||||||||||||||||||
| Allosteric CBRTooltip Cannabinoid receptor ligands | |||||||||||||||||||||||||||||||||||||||||
| Endocannabinoid enhancers (inactivation inhibitors) |
| ||||||||||||||||||||||||||||||||||||||||
| Anticannabinoids (antagonists/inverse agonists/antibodies) |
| ||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||
Template:Link FA Template:Link FA Template:Link FA Template:Link FA Template:Link FA Template:Link FA Template:Link FA Template:Link FA
Categories: