| Revision as of 20:18, 17 August 2014 editAwien (talk | contribs)Extended confirmed users8,947 editsm grammar tweaks← Previous edit | Revision as of 21:11, 22 August 2014 edit undoRjwilmsi (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers932,176 editsm Filling in journal cites, using AWB (10395)Next edit → | ||
| Line 62: | Line 62: | ||
| * Bladder and bowel control problems, including incontinence, ], and poor renal function<ref name="Mitchell" /> | * Bladder and bowel control problems, including incontinence, ], and poor renal function<ref name="Mitchell" /> | ||
| * ] and skin irritations<ref name="Mitchell" /> | * ] and skin irritations<ref name="Mitchell" /> | ||
| * Abnormal eye movement<ref name="Juranek & Salman">{{cite journal|last=Juranek|first=J|author2=Salman MS |title=Anomalous development of brain structure and function in spina bifida myelomeningocele|journal=Developmental Disabilities|year=2010|volume=16|series=1|pages=23–30|doi=10.1002/ddrr.88}}</ref> | * Abnormal eye movement<ref name="Juranek & Salman">{{cite journal|last=Juranek|first=J|author2=Salman MS |title=Anomalous development of brain structure and function in spina bifida myelomeningocele|journal=Developmental Disabilities|year=2010|volume=16|series=1|pages=23–30|doi=10.1002/ddrr.88|issue=1}}</ref> | ||
| 68% of children with spina bifida have an ] to ],<ref>{{cite news|url=http://www.sciencedaily.com/videos/2008/1206-protect_yourself_from_latex_allergies.htm|title=Protect Yourself From Latex Allergies: Plant Biologists And Immunochemists Develop Hypoallergenic Alternative To Latex|accessdate=12 October 2012|date=1 December 2008|work=]}}</ref> ranging from mild to life-threatening. The common use of latex in medical facilities makes this a particularly serious concern. The most common approach to avoid developing an allergy is to avoid contact with latex-containing products such as examination gloves and condoms and ] that do not specify they are latex free, and many other products, such as some commonly used by dentists.<ref name="emedicine"/> | 68% of children with spina bifida have an ] to ],<ref>{{cite news|url=http://www.sciencedaily.com/videos/2008/1206-protect_yourself_from_latex_allergies.htm|title=Protect Yourself From Latex Allergies: Plant Biologists And Immunochemists Develop Hypoallergenic Alternative To Latex|accessdate=12 October 2012|date=1 December 2008|work=]}}</ref> ranging from mild to life-threatening. The common use of latex in medical facilities makes this a particularly serious concern. The most common approach to avoid developing an allergy is to avoid contact with latex-containing products such as examination gloves and condoms and ] that do not specify they are latex free, and many other products, such as some commonly used by dentists.<ref name="emedicine"/> | ||
| Line 76: | Line 76: | ||
| ====Executive function==== | ====Executive function==== | ||
| Several studies have demonstrated difficulties with ] in youth with spina bifida,<ref name=Burmeister>{{cite journal|last=Burmeister|first=R|author2=Hannay HJ |author3=Copeland K |author4=Fletcher JM |author5=Boudousquie A |author6=Dennis M |title=Attention problems and executive functions in children with spina bifida and hydrocephalus|journal=Child Neuropsychology|year=2005|volume=11|pages=265–283|doi=10.1080/092970490911324|issue=3|pmid=16036451}}</ref><ref name="Tarazi 2008">{{cite journal|last=Tarazi|first=RA|author2=Zabel TA |author3=Mahone EM |title=Age-related changes in executive function among children with spina bifida/hydrocephalus based on parent behavior ratings|journal=The Clinical Neuropsychologist|year=2008|volume=22|issue=4|pages=585–602|doi=10.1080/13854040701425940|pmid=17853154|pmc=2575658}}</ref> with greater deficits observed in youth with shunted hydrocephalus.<ref name="Fletcher et al 1996">{{cite journal|last=Fletcher|first=JM|title=Attentional skills and executive functions in children with early hydrocephalus|journal=Developmental Neuropsychology|year=1996|volume=12|pages=53–76|author-separator=,|author2=Brookshire BL|author3=Landry SH|author4=Bohan TP|author5=Davidson KC|author6=Francis DJ|display-authors=5|doi=10.1080/87565649609540640|last7=Levin|first7=Harvey S.|last8=Brandt|first8=Michael E.|last9=Kramer|first9=Larry A.|last10=Morris|first10=Robin D.}}</ref> Unlike typically developing children, youths with spina bifida do not tend to improve in their executive functioning as they grow older.<ref name="Tarazi 2008" /> Specific areas of difficulty in some individuals include planning, organizing, initiating, and ]. Problem-solving, ], and visual planning may also be impaired.<ref name="Snow 1999">{{cite journal|last=Snow|first=JH|title=Executive processes for children with spina bifida|journal=Children's Health Care|year=1999|volume=28|issue=3|pages=241–253|doi=10.1207/s15326888chc2803_3}}</ref> Further, children with spina bifida may have poor ]. Although executive functions are often attributed to the ]s of the brain, individuals with spina bifida have intact frontal lobes; therefore, other areas of the brain may be implicated.<ref name="Fletcher et al 1996" /> | Several studies have demonstrated difficulties with ] in youth with spina bifida,<ref name=Burmeister>{{cite journal|last=Burmeister|first=R|author2=Hannay HJ |author3=Copeland K |author4=Fletcher JM |author5=Boudousquie A |author6=Dennis M |title=Attention problems and executive functions in children with spina bifida and hydrocephalus|journal=Child Neuropsychology|year=2005|volume=11|pages=265–283|doi=10.1080/092970490911324|issue=3|pmid=16036451}}</ref><ref name="Tarazi 2008">{{cite journal|last=Tarazi|first=RA|author2=Zabel TA |author3=Mahone EM |title=Age-related changes in executive function among children with spina bifida/hydrocephalus based on parent behavior ratings|journal=The Clinical Neuropsychologist|year=2008|volume=22|issue=4|pages=585–602|doi=10.1080/13854040701425940|pmid=17853154|pmc=2575658}}</ref> with greater deficits observed in youth with shunted hydrocephalus.<ref name="Fletcher et al 1996">{{cite journal|last=Fletcher|first=JM|title=Attentional skills and executive functions in children with early hydrocephalus|journal=Developmental Neuropsychology|year=1996|volume=12|pages=53–76|author-separator=,|author2=Brookshire BL|author3=Landry SH|author4=Bohan TP|author5=Davidson KC|author6=Francis DJ|display-authors=5|doi=10.1080/87565649609540640|last7=Levin|first7=Harvey S.|last8=Brandt|first8=Michael E.|last9=Kramer|first9=Larry A.|last10=Morris|first10=Robin D.|issue=1}}</ref> Unlike typically developing children, youths with spina bifida do not tend to improve in their executive functioning as they grow older.<ref name="Tarazi 2008" /> Specific areas of difficulty in some individuals include planning, organizing, initiating, and ]. Problem-solving, ], and visual planning may also be impaired.<ref name="Snow 1999">{{cite journal|last=Snow|first=JH|title=Executive processes for children with spina bifida|journal=Children's Health Care|year=1999|volume=28|issue=3|pages=241–253|doi=10.1207/s15326888chc2803_3}}</ref> Further, children with spina bifida may have poor ]. Although executive functions are often attributed to the ]s of the brain, individuals with spina bifida have intact frontal lobes; therefore, other areas of the brain may be implicated.<ref name="Fletcher et al 1996" /> | ||
| Individuals with spina bifida, especially those with shunted hydrocephalus, often have attention problems. Children with spina bifida and shunted hydrocephalus have higher rates of ] than typically developing children (31% vs. 17%).<ref name=Burmeister /> Deficits have been observed for selective attention and focused attention, although poor motor speed may contribute to poor scores on tests of attention.<ref name="Fletcher et al 1996" /><ref name="Rose Holmbeck">{{cite journal|last=Rose|first=BM|author2=Holmbeck GN |title=Attention and executive functions in adolescents with spina bifida|journal=Journal of Pediatric Psychology|year=2007|volume=32|issue=8|pages=983–994|doi=10.1093/jpepsy/jsm042|pmid=17556398}}</ref> Attention deficits may be evident at a very early age, as ]s with spina bifida lag behind their peers in orienting to faces.<ref name="Landry et al">{{cite journal|last=Landry|first=SH|author2=Robinson SS |author3=Copeland D |author4=Garner PW |title=Goal-directed behavior and perception of self-competence in children with spina bifida|journal=Journal of Pediatric Psychology|year=1993|volume=18|issue=3|pages=389–396|doi=10.1093/jpepsy/18.3.389|pmid=8340846}}</ref> | Individuals with spina bifida, especially those with shunted hydrocephalus, often have attention problems. Children with spina bifida and shunted hydrocephalus have higher rates of ] than typically developing children (31% vs. 17%).<ref name=Burmeister /> Deficits have been observed for selective attention and focused attention, although poor motor speed may contribute to poor scores on tests of attention.<ref name="Fletcher et al 1996" /><ref name="Rose Holmbeck">{{cite journal|last=Rose|first=BM|author2=Holmbeck GN |title=Attention and executive functions in adolescents with spina bifida|journal=Journal of Pediatric Psychology|year=2007|volume=32|issue=8|pages=983–994|doi=10.1093/jpepsy/jsm042|pmid=17556398}}</ref> Attention deficits may be evident at a very early age, as ]s with spina bifida lag behind their peers in orienting to faces.<ref name="Landry et al">{{cite journal|last=Landry|first=SH|author2=Robinson SS |author3=Copeland D |author4=Garner PW |title=Goal-directed behavior and perception of self-competence in children with spina bifida|journal=Journal of Pediatric Psychology|year=1993|volume=18|issue=3|pages=389–396|doi=10.1093/jpepsy/18.3.389|pmid=8340846}}</ref> | ||
| Line 207: | Line 207: | ||
| ===Endoscopic fetal surgery=== | ===Endoscopic fetal surgery=== | ||
| In contrast to the open fetal operative approach performed in the MOMS trial, a ] has been developed by the German pediatrician Thomas Kohl of the German Center for Fetal Surgery & Minimally-Invasive Therapy at the ], Germany.<ref>{{cite web|url=http://www.ukgm.de/ugm_2/deu/ugm_dzf/16799.html |title=Universitätsklinikum Giessen und Marburg - Offener Rücken/ Spina bifida aperta |publisher=Ukgm.de |accessdate=2011-10-23}}</ref> This approach has been heavily criticized by the independent authors of a controlled study about this cohort and deemed unethical by others.<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04148.x}}</ref><ref>{{cite journal|last1=SHURTLEFF|first1=DAVID|title=Fetal endoscopic myelomeningocele repair|journal=Developmental Medicine & Child Neurology|volume=54|issue=1|pages=4–5|doi=10.1111/j.1469-8749.2011.04141.x}}</ref> | In contrast to the open fetal operative approach performed in the MOMS trial, a ] has been developed by the German pediatrician Thomas Kohl of the German Center for Fetal Surgery & Minimally-Invasive Therapy at the ], Germany.<ref>{{cite web|url=http://www.ukgm.de/ugm_2/deu/ugm_dzf/16799.html |title=Universitätsklinikum Giessen und Marburg - Offener Rücken/ Spina bifida aperta |publisher=Ukgm.de |accessdate=2011-10-23}}</ref> This approach has been heavily criticized by the independent authors of a controlled study about this cohort and deemed unethical by others.<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04148.x | title=Fetal endoscopic myelomeningocele closure preserves segmental neurological function | journal=Developmental Medicine | date=2011 | volume=54 | issue=1 | pages=15–22 | first=RENATE J | last=VERBEEK}}</ref><ref>{{cite journal|last1=SHURTLEFF|first1=DAVID|title=Fetal endoscopic myelomeningocele repair|journal=Developmental Medicine & Child Neurology|volume=54|issue=1|pages=4–5|doi=10.1111/j.1469-8749.2011.04141.x|date=2011}}</ref> | ||
| This approach under general materno-fetal anesthesia uses three ] (small tubes) with an external diameter of 5 mm that are directly placed through the maternal abdominal wall into the uterine cavity under ultrasound guidance. Following intrauterine access, part of the amniotic fluid is removed and the uterus is insufflated with ] (this technique provides superior visualization of fetoscopic spina bifida closure, is called PACI (partial amniotic fluid insufflation), and has been safe for mothers and fetuses alike in over 70 procedures on human fetuses). After fetal posturing, the neural cord is freed from pathological adhesions and covered with patch material. Watertight closure is demonstrated by intraoperative bulging of the patch. Accordingly, reversal of hindbrain herniation can be documented within days after most procedures. | This approach under general materno-fetal anesthesia uses three ] (small tubes) with an external diameter of 5 mm that are directly placed through the maternal abdominal wall into the uterine cavity under ultrasound guidance. Following intrauterine access, part of the amniotic fluid is removed and the uterus is insufflated with ] (this technique provides superior visualization of fetoscopic spina bifida closure, is called PACI (partial amniotic fluid insufflation), and has been safe for mothers and fetuses alike in over 70 procedures on human fetuses). After fetal posturing, the neural cord is freed from pathological adhesions and covered with patch material. Watertight closure is demonstrated by intraoperative bulging of the patch. Accordingly, reversal of hindbrain herniation can be documented within days after most procedures. | ||
| Line 215: | Line 215: | ||
| In a cohort of 20 infants that underwent fetoscopic surgery on the lesion between July 2010 and December 2011 and were studied during the first six months of life, reversal of hindbrain herniation was observed in 18 (90%) and shunt insertion was required in only eight (40%). Normal to near normal leg function was observed in about two thirds of the infants. An abnormal foot position at birth was observed in only two. The fetuses that were operated at a mean of 24 weeks of gestation were born at a mean gestational age at delivery of about 33 weeks of gestation.<ref>T. Kohl, A. Kawecki u. a.: Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. In: Ultrasound Obstet Gynecol. Bnad 40:9, 2012</ref> | In a cohort of 20 infants that underwent fetoscopic surgery on the lesion between July 2010 and December 2011 and were studied during the first six months of life, reversal of hindbrain herniation was observed in 18 (90%) and shunt insertion was required in only eight (40%). Normal to near normal leg function was observed in about two thirds of the infants. An abnormal foot position at birth was observed in only two. The fetuses that were operated at a mean of 24 weeks of gestation were born at a mean gestational age at delivery of about 33 weeks of gestation.<ref>T. Kohl, A. Kawecki u. a.: Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. In: Ultrasound Obstet Gynecol. Bnad 40:9, 2012</ref> | ||
| In 2012, these results of the fetoscopic approach were presented at various national and international meetings, among them at the 1st European Symposium “Fetal Surgery for Spina bifida“ in April 2012 in ], at the 15th Congress of the ] in May 2012 in Bonn,<ref>{{cite web|url=http://www.dzft.de/?page_id=1420 |title=DZFT beim Kongress DGPGM | DZFT |publisher=Dzft.de |accessdate=2012-11-14}}</ref> at the World Congress of the Fetal Medicine Foundation in June 2012<ref>{{cite web|url=http://www.fetalmedicine.com/fmf/courses-congress/conferences/ |title=The Fetal Medicine Foundation / FMF World Congress |publisher=Fetalmedicine.com |accessdate=2012-11-14}}</ref> and at the World Congress of the ] (ISUOG) in ] in September 2012,<ref>{{cite web|url=http://www.isuog.org/WorldCongress/2012/ |title=World Congress 2012 | World Congress |publisher=ISUOG |date=2012-09-13 |accessdate=2012-11-14}}</ref> and published in abstract form.<ref>{{cite journal | author = Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Tchatcheva K, Axt-Fliedner R, Kohl T. et al. | year = 2012 | title = Mütterliches Outcome nach minimal-invasivem Verschluss einer Spina bifida | url = | journal = Ultraschall in Med | volume = 33 | issue = | page = S96 }}</ref><ref>Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Maternal outcome after minimally-invasive fetoscopic surgery for spina bifida. The Giessen experience 2010 – 2012. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 9</ref><ref>{{cite journal | author = Neubauer B, Degenhardt J, Axt-Fliedner R, Kohl T | year = 2012 | title = Frühe neurologische Befunde von Säuglingen nach minimal-invasivem fetoskopischen Verschluss ihrer Spina bifida aperta | url = | journal = Z Geburtsh Neonat | volume = 216 | issue = | page = 87 | doi=10.1055/s-0032-1309110}}</ref><ref>Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R, Neubauer B. "Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 9</ref><ref>Kohl T, Schürg R, Maxeiner H, Tchatcheva K, Degenhardt J, Stressig R, Axt-Fliedner R, Gembruch U. "Partial carbon dioxide insufflation (PACI) during fetoscopic surgery on 60 fetuses with spina bifida. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 73-74</ref><ref>Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R. "Preoperative sonoanatomic examination of fetal spina bifida permits prediction of surgical complexity during subsequent minimally-invasive fetoscopic closure. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 8</ref><ref>{{cite journal | author = Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T | year = 2012 | title = Rückverlagerung der Chiari-II Malformation innerhalb weniger Tage nach minimal-invasivem Patchverschluss ans Hinweis für einen effektiven Verschluss der Fehlbildung | url = | journal = Ultraschall in Med | volume = 33 | issue = | page = S95 }}</ref><ref>Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Reversal of hindbrain herniation within a few days after minimally-invasive fetoscopic surgery for spina bifida indicates the desired water-tight closure of the lesion. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 74</ref> | In 2012, these results of the fetoscopic approach were presented at various national and international meetings, among them at the 1st European Symposium “Fetal Surgery for Spina bifida“ in April 2012 in ], at the 15th Congress of the ] in May 2012 in Bonn,<ref>{{cite web|url=http://www.dzft.de/?page_id=1420 |title=DZFT beim Kongress DGPGM | DZFT |publisher=Dzft.de |accessdate=2012-11-14}}</ref> at the World Congress of the Fetal Medicine Foundation in June 2012<ref>{{cite web|url=http://www.fetalmedicine.com/fmf/courses-congress/conferences/ |title=The Fetal Medicine Foundation / FMF World Congress |publisher=Fetalmedicine.com |accessdate=2012-11-14}}</ref> and at the World Congress of the ] (ISUOG) in ] in September 2012,<ref>{{cite web|url=http://www.isuog.org/WorldCongress/2012/ |title=World Congress 2012 | World Congress |publisher=ISUOG |date=2012-09-13 |accessdate=2012-11-14}}</ref> and published in abstract form.<ref>{{cite journal | author = Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Tchatcheva K, Axt-Fliedner R, Kohl T. et al. | year = 2012 | title = Mütterliches Outcome nach minimal-invasivem Verschluss einer Spina bifida | url = | journal = Ultraschall in Med | volume = 33 | issue = | page = S96 }}</ref><ref>Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Maternal outcome after minimally-invasive fetoscopic surgery for spina bifida. The Giessen experience 2010 – 2012. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 9</ref><ref>{{cite journal | author = Neubauer B, Degenhardt J, Axt-Fliedner R, Kohl T | year = 2012 | title = Frühe neurologische Befunde von Säuglingen nach minimal-invasivem fetoskopischen Verschluss ihrer Spina bifida aperta | url = | journal = Z Geburtsh Neonat | volume = 216 | issue = 2| page = 87 | doi=10.1055/s-0032-1309110}}</ref><ref>Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R, Neubauer B. "Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 9</ref><ref>Kohl T, Schürg R, Maxeiner H, Tchatcheva K, Degenhardt J, Stressig R, Axt-Fliedner R, Gembruch U. "Partial carbon dioxide insufflation (PACI) during fetoscopic surgery on 60 fetuses with spina bifida. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 73-74</ref><ref>Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R. "Preoperative sonoanatomic examination of fetal spina bifida permits prediction of surgical complexity during subsequent minimally-invasive fetoscopic closure. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 8</ref><ref>{{cite journal | author = Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T | year = 2012 | title = Rückverlagerung der Chiari-II Malformation innerhalb weniger Tage nach minimal-invasivem Patchverschluss ans Hinweis für einen effektiven Verschluss der Fehlbildung | url = | journal = Ultraschall in Med | volume = 33 | issue = | page = S95 }}</ref><ref>Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Reversal of hindbrain herniation within a few days after minimally-invasive fetoscopic surgery for spina bifida indicates the desired water-tight closure of the lesion. ''Ultrasound Obstet Gynecol'' 2012;40(Suppl. 1) 74</ref> | ||
| In contrast to the low maternal and fetal complication rates that can be achieved by the current fetoscopic approach, its clinical introduction was affected by technical difficulties and a number of adverse fetal outcomes: Three of the first 19 procedures could not be completed, three fetuses died, and the mean gestational age at delivery was 29 weeks of gestation. As a result, the approach was heavily critizised by the independent authors of a controlled study about this cohort and deemed unethical by others.<ref>R. J. Verbeek, A. Heep (2012) Fetal endoscopic myelomeningocele closure preserves segmental neurological function. In: Developmental medicine and child neurology. 54(1) 15–22 {{doi|10.1111/j.1469-8749.2011.04148.x}} PMID 22126123</ref><ref>{{cite journal | author = Kohl T, Gembruch U, Thomas , Kohl Thomas, Gembruch Ulrich | year = 2008 | title = Current status and prospects of fetoscopic surgery for spina bifida in human fetuses | url = | journal = Fetal Diagnosis and Therapy | volume = 24 | issue = 3| pages = 318–320 | pmid = 18832851 | last2 = Gembruch | doi = 10.1159/000158549 }}</ref> Specifically, published in the January 2012 issue of Developmental Medicine & Child Neurology, David Shurtleff, Ph.D., stated that “the extremely high complication rates for mother and infant in this study and the principle of primum non nocere indicate that at this time it is unethical to pursue intrauterine endoscopic myelomeningocele repair in humans until the procedure has been perfected in animals.<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04141.x}}</ref> “ Additionally, VERBEEK, R. J.,et al, published in the same issue of Developmental Medicine & Child Neurology that “fetal endoscopic surgery is associated with spinal segmental neuroprotection, but it results in more complications. Before considering clinical implementation of fetal endoscopic myelomeningocele closure as standard care, the frequency of complications should be appropriately reduced and results assessed in larger groups over a longer period of time.”<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04148.x}}</ref> | In contrast to the low maternal and fetal complication rates that can be achieved by the current fetoscopic approach, its clinical introduction was affected by technical difficulties and a number of adverse fetal outcomes: Three of the first 19 procedures could not be completed, three fetuses died, and the mean gestational age at delivery was 29 weeks of gestation. As a result, the approach was heavily critizised by the independent authors of a controlled study about this cohort and deemed unethical by others.<ref>R. J. Verbeek, A. Heep (2012) Fetal endoscopic myelomeningocele closure preserves segmental neurological function. In: Developmental medicine and child neurology. 54(1) 15–22 {{doi|10.1111/j.1469-8749.2011.04148.x}} PMID 22126123</ref><ref>{{cite journal | author = Kohl T, Gembruch U, Thomas , Kohl Thomas, Gembruch Ulrich | year = 2008 | title = Current status and prospects of fetoscopic surgery for spina bifida in human fetuses | url = | journal = Fetal Diagnosis and Therapy | volume = 24 | issue = 3| pages = 318–320 | pmid = 18832851 | last2 = Gembruch | doi = 10.1159/000158549 }}</ref> Specifically, published in the January 2012 issue of Developmental Medicine & Child Neurology, David Shurtleff, Ph.D., stated that “the extremely high complication rates for mother and infant in this study and the principle of primum non nocere indicate that at this time it is unethical to pursue intrauterine endoscopic myelomeningocele repair in humans until the procedure has been perfected in animals.<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04141.x | title=Fetal endoscopic myelomeningocele repair | journal=Developmental Medicine | date=2011 | volume=54 | issue=1 | pages=4–5 | first=DAVID | last=SHURTLEFF}}</ref> “ Additionally, VERBEEK, R. J.,et al, published in the same issue of Developmental Medicine & Child Neurology that “fetal endoscopic surgery is associated with spinal segmental neuroprotection, but it results in more complications. Before considering clinical implementation of fetal endoscopic myelomeningocele closure as standard care, the frequency of complications should be appropriately reduced and results assessed in larger groups over a longer period of time.”<ref>{{cite journal|doi=10.1111/j.1469-8749.2011.04148.x | title=Fetal endoscopic myelomeningocele closure preserves segmental neurological function | journal=Developmental Medicine | date=2011 | volume=54 | issue=1 | pages=15–22 | first=RENATE J | last=VERBEEK}}</ref> | ||
| In contrast, with the completion of the MOMS trial, open fetal surgery for myelomeningocele is now one standard of care option, at highly experienced centers, for appropriate patients.<ref>{{cite journal|doi=10.1056/NEJMoa1014379}}</ref> | In contrast, with the completion of the MOMS trial, open fetal surgery for myelomeningocele is now one standard of care option, at highly experienced centers, for appropriate patients.<ref>{{cite journal|doi=10.1056/NEJMoa1014379 | title=A Randomized Trial of Prenatal versus Postnatal Repair of Myelomeningocele | journal=New England Journal of Medicine | date=2011 | volume=364 | issue=11 | pages=993–1004 | first=N. Scott | last=Adzick}}</ref> | ||
| ==Notable people== | ==Notable people== | ||
Revision as of 21:11, 22 August 2014
Medical condition| Spina bifida | |
|---|---|
| Specialty | Medical genetics, neurology |
Spina bifida (Latin: "split spine") is a developmental congenital disorder caused by the incomplete closing of the embryonic neural tube. Some vertebrae overlying the spinal cord are not fully formed and remain unfused and open. If the opening is large enough, this allows a portion of the spinal cord to protrude through the opening in the bones. There may or may not be a fluid-filled sac surrounding the spinal cord. Other neural tube defects include anencephaly, a condition in which the portion of the neural tube that will become the cerebrum does not close, and encephalocele, which results when other parts of the brain remain unfused.
Spina bifida malformations fall into three categories: spina bifida occulta, spina bifida cystica with meningocele, and spina bifida cystica with myelomeningocele. The most common location of the malformations is the lumbar and sacral areas. Myelomeningocele is the most significant and common form, and this leads to disability in most affected individuals. The terms spina bifida and myelomeningocele are usually used interchangeably.
Spina bifida can be surgically closed after birth, but this does not restore normal function to the affected part of the spinal cord. Intrauterine surgery for spina bifida has also been performed, and the safety and efficacy of this procedure are currently being investigated. A study conducted with mothers who had prior spina bifida births indicates the incidence of spina bifida can be decreased by up to 70% when the mother takes daily folic acid supplements prior to conception.
Spina bifida meningocele and myelomeningocele are among the most common birth defects, with a worldwide incidence of about 1 in every 1000 births. The occulta form is much more common, but only rarely causes neurological symptoms.
Classification

Spina bifida occulta
Occulta is Latin for "hidden". This is the mildest form of spina bifida. In occulta, the outer part of some of the vertebrae is not completely closed. The splits in the vertebrae are so small that the spinal cord does not protrude. The skin at the site of the lesion may be normal, or it may have some hair growing from it; there may be a dimple in the skin, or a birthmark.
Many people with this type of spina bifida do not even know they have it, as the condition is asymptomatic in most cases. The incidence of spina bifida occulta is approximately 10-20% of the population, and most people are diagnosed incidentally from spinal X-rays. A systematic review of radiographic research studies found no relationship between spina bifida occulta and back pain. More recent studies not included in the review support the negative findings.
However, other studies suggest spina bifida occulta is not always harmless. One study found, among patients with back pain, severity is worse if spina bifida occulta is present. To prevent confusion with true spina bifida and spina bifida occulta, incomplete posterior fusion is the correct terminology when discussing as incomplete posterior fusion is incidental finding that is very rarely of neurological significance and is not a true spina bifida.
Meningocele
A posterior meningocele (pronounced /məˈnɪŋɡəˌsil/) or meningeal cyst (pronounced /mɪˈnɪndʒiəl/ /sɪst/) is the least common form of spina bifida. In this form, the vertebrae develop normally, but the meninges are forced into the gaps between the vertebrae. As the nervous system remains undamaged, individuals with meningocele are unlikely to suffer long-term health problems, although cases of tethered cord have been reported. Causes of meningocele include teratoma and other tumors of the sacrococcyx and of the presacral space, and Currarino syndrome.
A meningocele may also form through dehiscences in the base of the skull. These may be classified by their localisation to occipital, frontoethmoidal, or nasal. Endonasal meningoceles lie at the roof of the nasal cavity and may be mistaken for a nasal polyp. They are treated surgically. Encephalomeningoceles are classified in the same way and also contain brain tissue.
Myelomeningocele
This type of spina bifida often results in the most severe complications. In individuals with myelomeningocele, the unfused portion of the spinal column allows the spinal cord to protrude through an opening. The meningeal membranes that cover the spinal cord form a sac enclosing the spinal elements.
Myeloschisis
Spina bifida with myeloschisis is the most severe form of myelomeningocele. In this type, the involved area is represented by a flattened, plate-like mass of nervous tissue with no overlying membrane. The exposure of these nerves and tissues make the baby more prone to life-threatening infections such as meningitis.
The protruding portion of the spinal cord and the nerves that originate at that level of the cord are damaged or not properly developed. As a result, there is usually some degree of paralysis and loss of sensation below the level of the spinal cord defect. Thus, the more cranial the level of the defect, the more severe the associated nerve dysfunction and resultant paralysis may be. People may have ambulatory problems, loss of sensation, deformities of the hips, knees or feet, and loss of muscle tone.
-
 X-ray image of spina bifida occulta in S-1
X-ray image of spina bifida occulta in S-1
-
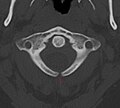 X-ray computed tomography scan of unfused arch at C1
X-ray computed tomography scan of unfused arch at C1
-
 Myelomeningocele in the lumbar area
Myelomeningocele in the lumbar area
(1) External sac with cerebrospinal fluid
(2) Spinal cord wedged between the vertebrae
Signs and symptoms
Physical complications
Physical signs of spina bifida may include:
- Leg weakness and paralysis
- Orthopedic abnormalities (i.e., club foot, hip dislocation, scoliosis)
- Bladder and bowel control problems, including incontinence, urinary tract infections, and poor renal function
- Pressure sores and skin irritations
- Abnormal eye movement
68% of children with spina bifida have an allergy to latex, ranging from mild to life-threatening. The common use of latex in medical facilities makes this a particularly serious concern. The most common approach to avoid developing an allergy is to avoid contact with latex-containing products such as examination gloves and condoms and catheters that do not specify they are latex free, and many other products, such as some commonly used by dentists.
The spinal cord lesion or the scarring due to surgery may result in a tethered spinal cord. In some individuals, this causes significant traction and stress on the spinal cord and can lead to a worsening of associated paralysis, scoliosis, back pain, and worsening bowel and/or bladder function.
Neurological complications
Many individuals with spina bifida have an associated abnormality of the cerebellum, called the Arnold Chiari II malformation. In affected individuals, the back portion of the brain is displaced from the back of the skull down into the upper neck. In about 90% of the people with myelomeningocele, hydrocephalus also occurs because the displaced cerebellum interferes with the normal flow of cerebrospinal fluid, causing an excess of the fluid to accumulate. In fact, the cerebellum also tends to be smaller in individuals with spina bifida, especially for those with higher lesion levels.
The corpus callosum is abnormally developed in 70-90% of individuals with spina bifida myelomeningocele; this impacts the communication processes between the left and right brain hemispheres. Further, white matter tracts connecting posterior brain regions with anterior regions appear less organized. White matter tracts between frontal regions have also been found to be impaired.
Cortex abnormalities may also be present. For example, frontal regions of the brain tend to be thicker than expected, while posterior and parietal regions are thinner. Thinner sections of the brain are also associated with increased cortical folding. Neurons within the cortex may also be displaced.
Executive function
Several studies have demonstrated difficulties with executive functions in youth with spina bifida, with greater deficits observed in youth with shunted hydrocephalus. Unlike typically developing children, youths with spina bifida do not tend to improve in their executive functioning as they grow older. Specific areas of difficulty in some individuals include planning, organizing, initiating, and working memory. Problem-solving, abstraction, and visual planning may also be impaired. Further, children with spina bifida may have poor cognitive flexibility. Although executive functions are often attributed to the frontal lobes of the brain, individuals with spina bifida have intact frontal lobes; therefore, other areas of the brain may be implicated.
Individuals with spina bifida, especially those with shunted hydrocephalus, often have attention problems. Children with spina bifida and shunted hydrocephalus have higher rates of ADHD than typically developing children (31% vs. 17%). Deficits have been observed for selective attention and focused attention, although poor motor speed may contribute to poor scores on tests of attention. Attention deficits may be evident at a very early age, as infants with spina bifida lag behind their peers in orienting to faces.
Academic skills
Individuals with spina bifida may struggle academically, especially in the subjects of mathematics and reading. In one study, 60% of children with spina bifida were diagnosed with a learning disability. In addition to brain abnormalities directly related to various academic skills, achievement is likely affected by impaired attentional control and executive functioning. Children with spina bifida may perform well in elementary school, but begin to struggle as academic demands increase.
Children with spina bifida are more likely than their typically developing peers to have dyscalculia. Individuals with spina bifida have demonstrated stable difficulties with arithmetic accuracy and speed, mathematical problem-solving, and general use and understanding of numbers in everyday life. Mathematics difficulties may be directly related to the thinning of the parietal lobes (regions implicated in mathematical functioning) and indirectly associated with deformities of the cerebellum and midbrain that affect other functions involved in mathematical skills. Further, higher numbers of shunt revisions are associated with poorer mathematics abilities. Working memory and inhibitory control deficiencies have been implicated for math difficulties, although visual-spatial difficulties are not likely involved. Early intervention to address mathematics difficulties and associated executive functions is crucial.
Individuals with spina bifida tend to have better reading skills than mathematics skills. Children and adults with spina bifida have stronger abilities in reading accuracy than in reading comprehension. Comprehension may be especially impaired for text that requires an abstract synthesis of information rather than a more literal understanding. Individuals with spina bifida may have difficulty with writing due to deficits in fine motor control and working memory.
Pathophysiology
Spina bifida is sometimes caused by the failure of the neural tube to close during the first month of embryonic development (often before the mother knows she is pregnant). Some forms are known to occur with primary conditions that cause raised central nervous system pressure, which raises the possibility of a dual pathogenesis
Under normal circumstances, the closure of the neural tube occurs around the 23rd (rostral closure) and 27th (caudal closure) day after fertilization. However, if something interferes and the tube fails to close properly, a neural tube defect will occur. Medications such as some anticonvulsants, diabetes, having a relative with spina bifida, obesity, and an increased body temperature from fever or external sources such as hot tubs and electric blankets may increase the chances of delivery of a baby with a spina bifida.
Extensive evidence from mouse strains with spina bifida indicates that there is sometimes a genetic basis for the condition. Human spina bifida, like other human diseases, such as cancer, hypertension and atherosclerosis (coronary artery disease), likely results from the interaction of multiple genes and environmental factors.
Research has shown the lack of folic acid (folate) is a contributing factor in the pathogenesis of neural tube defects, including spina bifida. Supplementation of the mother's diet with folate can reduce the incidence of neural tube defects by about 70%, and can also decrease the severity of these defects when they occur. It is unknown how or why folic acid has this effect.
Spina bifida does not follow direct patterns of heredity like muscular dystrophy or haemophilia. Studies show a woman having had one child with a neural tube defect such as spina bifida has about a 3% risk of having another child with a neural tube defect. This risk can be reduced to about 1% if the woman takes high doses (4 mg/day) of folic acid before and during pregnancy. For the general population, low-dose folic acid supplements are advised (0.4 mg/day).
Prevention

There is neither a single cause of spina bifida nor any known way to prevent it entirely. However, dietary supplementation with folic acid has been shown to be helpful in reducing the incidence of spina bifida. Sources of folic acid include whole grains, fortified breakfast cereals, dried beans, leaf vegetables and fruits.
Folate fortification of enriched grain products has been mandatory in the United States since 1998. The U.S. Food and Drug Administration, Public Health Agency of Canada and UK recommended amount of folic acid for women of childbearing age and women planning to become pregnant is at least 0.4 mg/day of folic acid from at least three months before conception, and continued for the first 12 weeks of pregnancy. Women who have already had a baby with spina bifida or other type of neural tube defect, or are taking anticonvulsant medication should take a higher dose of 4–5 mg/day.
Certain mutations in the gene VANGL1 are implicated as a risk factor for spina bifida: These mutations have been linked with spina bifida in some families with a history of spina bifida.
Pregnancy screening
Neural tube defects can usually be detected during pregnancy by testing the mother's blood (AFP screening) or a detailed fetal ultrasound. Increased levels of maternal serum alpha-fetoprotein (MSAFP) should be followed up by two tests - an ultrasound of the fetal spine and amniocentesis of the mother's amniotic fluid (to test for alpha-fetoprotein and acetylcholinesterase). AFP tests are now mandated by some state laws (including California). and failure to provide them can have legal ramifications. In one case a man born with spina bifida was awarded a $2 million settlement after court found his mother's OBGYN negligent for not performing these tests. Spina bifida may be associated with other malformations as in dysmorphic syndromes, often resulting in spontaneous miscarriage. In the majority of cases, though, spina bifida is an isolated malformation.
Genetic counseling and further genetic testing, such as amniocentesis, may be offered during the pregnancy, as some neural tube defects are associated with genetic disorders such as trisomy 18. Ultrasound screening for spina bifida is partly responsible for the decline in new cases, because many pregnancies are terminated out of fear that a newborn might have a poor future quality of life. With modern medical care, the quality of life of patients has greatly improved.
Treatment
There is no known cure for nerve damage caused by spina bifida. To prevent further damage of the nervous tissue and to prevent infection, pediatric neurosurgeons operate to close the opening on the back. The spinal cord and its nerve roots are put back inside the spine and covered with meninges. In addition, a shunt may be surgically installed to provide a continuous drain for the excess cerebrospinal fluid produced in the brain, as happens with hydrocephalus. Shunts most commonly drain into the abdomen or chest wall. However, if spina bifida is detected during pregnancy, then open or minimally-invasive fetal surgery can be performed.
In childhood
Most individuals with myelomeningocele will need periodic evaluations by a variety of specialists:
- Physiatrists coordinate the rehabilitation efforts of different therapists and prescribe specific therapies, adaptive equipment, or medications to encourage as high of a functional performance within the community as possible.
- Orthopedists monitor growth and development of bones, muscles, and joints.
- Neurosurgeons perform surgeries at birth and manage complications associated with tethered cord and hydrocephalus.
- Neurologists treat and evaluate nervous system issues, such as seizure disorders.
- Urologists to address kidney, bladder, and bowel dysfunction - many will need to manage their urinary systems with a program of catheterization. Bowel management programs aimed at improving elimination are also designed.
- Ophthalmologists evaluate and treat complications of the eyes.
- Orthotists design and customize various types of assistive technology, including braces, crutches, walkers, and wheelchairs to aid in mobility. As a general rule, the higher the level of the spina bifida defect, the more severe the paralysis, but paralysis does not always occur. Thus, those with low levels may need only short leg braces, whereas those with higher levels do best with a wheelchair, and some may be able to walk unaided.
- Physical therapists, occupational therapists, psychologists, and speech/language pathologists aid in rehabilitative therapies and increase independent living skills.
Transition to adulthood
Although many children's hospitals feature integrated multidisciplinary teams to coordinate healthcare of youth with spina bifida, the transition to adult healthcare can be difficult because the above healthcare professionals operate independently of each other, requiring separate appointments and communicate among each other much less frequently. Healthcare professionals working with adults may also be less knowledgeable about spina bifida because it is considered a childhood chronic health condition. Due to the potential difficulties of the transition, adolescents with spina bifida and their families are encouraged to begin to prepare for the transition around ages 14–16, although this may vary depending on the adolescent's cognitive and physical abilities and available family support. The transition itself should be gradual and flexible. The adolescent's multidisciplinary treatment team may aid in the process by preparing comprehensive, up-to-date documents detailing the adolescent's medical care, including information about medications, surgery, therapies, and recommendations. A transition plan and aid in identifying adult healthcare professionals are also helpful to include in the transition process.
Further complicating the transition process is the tendency for youths with spina bifida to be delayed in the development of autonomy, with boys particularly at risk for slower development of independence. An increased dependence on others (in particular family members) may interfere with the adolescent's self-management of health-related tasks, such as catheterization, bowel management, and taking medications. As part of the transition process, it is beneficial to begin discussions at an early age about educational and vocational goals, independent living, and community involvement.
Epidemiology
Spina bifida is one of the most common birth defects, with an average worldwide incidence of one to two cases per 1000 births, but certain populations have a significantly greater risk.
In the United States, the average incidence is 0.7 per 1000 live births. The incidence is higher on the East Coast than on the West Coast, and higher in white people (one case per 1000 live births) than in black people (0.1–0.4 case per 1000 live births). Immigrants from Ireland have a higher incidence of spina bifida than do natives. Highest rates of the defect in the USA can be found in Hispanic youth.
The highest incidence rates worldwide were found in Ireland and Wales, where three to four cases of myelomeningocele per 1000 population have been reported during the 1970s, along with more than six cases of anencephaly (both live births and stillbirths) per 1000 population. The reported overall incidence of myelomeningocele in the British Isles was 2.0–3.5 cases per 1000 births. Since then, the rate has fallen dramatically with 0.15 per 1000 live births reported in 1998, though this decline is partially accounted for because some fetuses are aborted when tests show signs of spina bifida (see Pregnancy screening above).
Parents of children with spina bifida have an increased risk of having a second child with a neural tube defect.
Fetal surgery research
- 1980 - Fetal surgical techniques using animal models were first developed at the University of California, San Francisco by Michael R. Harrison, N. Scott Adzick and research colleagues.
- 1994 - A surgical model that simulates the human disease is the fetal lamb model of myelomeningocele (MMC) introduced by Meuli and Adzick in 1994. The MMC-like defect was surgically created at 75 days of gestation (term 145 to 150 days) by a lumbo-sacral laminectomy. Approximately 3 weeks after creation of the defect a reversed latissimus dorsi flap was used to cover the exposed neural placode and the animals were delivered by cesarean section just prior term. Human MMC-like lesions with similar neurological deficit were found in the control newborn lambs. In contrast, animals that underwent closure had near-normal neurological function and well-preserved cytoarchitecture of the covered spinal cord on histopathological examination. Despite mild paraparesis, they were able to stand, walk, perform demanding motor test and demonstrated no signs of incontinence. Furthermore, sensory function of the hind limbs was present clinically and confirmed electrophysiologically. Further studies showed that this model, when combined with a lumbar spinal cord myelotomy leads to the hindbrain herniation characteristic of the Chiari II malformation and that in utero surgery restores normal hindbrain anatomy by stopping the leak of cerebrospinal fluid through the myelomeningocele lesion.
Surgeons at Vanderbilt University, led by Joseph Bruner, attempted to close spina bifida in 4 human fetuses using a skin graft from the mother using a laparoscope. Four cases were performed before stopping the procedure - two of the four fetuses died.
- 1998 - N. Scott Adzick and team at The Children's Hospital of Philadelphia performed open fetal surgery for spina bifida in an early gestation fetus (22 week gestation fetus) with a successful outcome. Open fetal surgery for myelomeningocele involves surgically opening the pregnant mother's abdomen and uterus to operate on the fetus. The exposed fetal spinal cord is covered in layers with surrounding fetal tissue at mid-gestation (19–25 weeks) to protect it from further damage caused by prolonged exposure to amniotic fluid. Between 1998 and 2003, Dr. Adzick, and his colleagues in the Center for Fetal Diagnosis and Treatment a The Children's Hospital Of Philadelphia, performed prenatal spina bifida repair in 58 mothers and observed significant benefit in the babies.
Surgeons at Vanderbilt University, led by Noel Tulipan, performed open fetal surgery at 28 to 30 weeks' gestation. All 4 fetuses were born premature but with evidence of reversal of their Chiari II malformation. Only 2 of the 4 required ventricular shunts after birth. Fetal surgery after 25 weeks has not shown benefit in subsequent studies.
Subsequently, 4 medical centers conducted 253 open spina bifida repairs prior to the Management of Myelomeningocele Study (MOMS) trial. The outcomes were mixed, and the only comparison groups were other children who had not undergone repair after birth in the past. To conclusively answer this question, the MOMS trial was launched in 2003 to determine the safety and efficacy of fetal surgery to close a myelomeningocele.
MOMS trial
Management of Myelomeningocele Study (MOMS) is a phase III clinical trial designed to compare two approaches to the treatment of spina bifida: surgery before birth (prenatal or fetal surgery) and surgery after birth (postnatal surgery).
Three fetal surgery centers participated in the trial—at The Children’s Hospital of Philadelphia, Vanderbilt University, and the University of California San Francisco. The biostatistics center at George Washington University (GWU) served as the coordinating center and oversaw data collection and analysis, while the Eunice Kennedy Shriver National Institute of Child Health and Human Development sponsored the trial.
The MOMS study was a prospective, randomized clinical trial. One sign of its prominence is that all U.S. fetal surgery centers not participating in the trial agreed to perform no fetal surgery for spina bifida during the 7-year duration of the trial.
Throughout the trial, women whose fetuses had been diagnosed with spina bifida contacted the trial’s coordinating center at GWU if they chose to volunteer for the study. That center randomly assigned half of the eligible women to receive prenatal surgery, the other half to receive postnatal surgery.
Postnatal surgery entailed delivery by planned cesarean section at 37 weeks gestation, after which the surgical team repaired the opening in the newborn’s spine, usually within 24 hours after birth. In prenatal surgery, done between 19 and 26 weeks’ gestation, the surgical team made incisions in the mother and her uterus, then repaired the spina bifida lesion while the fetus was in the womb. Mothers in this group stayed near the center for ongoing monitoring, then underwent delivery by planned cesarean section at 37 weeks, or earlier, because many of the babies in the prenatal surgery group arrived prematurely. In both study groups, surgeons used the same technique to cover the myelomeningocele with multiple layers of the fetus’s own tissue.
Clinicians who were independent of the surgical teams and blinded (not informed which of the two surgeries a given child received) evaluated the children from the study at one year of age and again at age 30 months.
The MOMS trial was closed for efficacy in December 2010 based on comparing outcomes after prenatal and postnatal repair in 183 patients - 77 patients were treated at The Children’s Hospital of Philadelphia, 54 at Vanderbilt University and 52 at The University of California San Francisco.
Unfortunately the study failed to address the possibility that some of the benefit of surgery to central nervous system function in the intervention group may have been caused by early delivery from the intrauterine environment. This issue casts some doubt on the studies findings. A case controlled comparison of intervention vs conservative management would have been unethical because of the exposure of infants within a control group to the adversity of premature delivery.
The trial concluded that the outcomes after prenatal spina bifida treatment are improved to the degree that the benefits of the surgery outweigh the maternal risks. This conclusion requires a value judgment on the relative value of fetal and maternal outcomes on which opinion is still divided. Results were reported in the New England Journal of Medicine by Adzick et al.
To be specific, the study found that prenatal repair resulted in:
- Reversal of the hindbrain herniation component of the Chiari II malformation
- Reduced need for ventricular shunting (a procedure in which a thin tube is introduced into the brain’s ventricles to drain fluid and relieve hydrocephalus)
- Reduced incidence or severity of potentially devastating neurologic effects caused by the spine’s exposure to amniotic fluid, such as impaired motor function
At one year of age, 40 percent of the children in the prenatal surgery group had received a shunt, compared to 83 percent of the children in the postnatal group. During pregnancy, all the fetuses in the trial had hindbrain herniation. However, at age 12 months, one-third (36 percent) of the infants in the prenatal surgery group no longer had any evidence of hindbrain herniation, compared to only 4 percent in the postnatal surgery group.
At age 30 months, children in the prenatal group had significantly better scores in measurements of motor function. While the ability to walk depends on the level of the spina bifida lesion, the study found a twofold increase in the proportion of children able to walk without crutches or other assistive devices—42 percent in the prenatal group compared to 21 percent in the postnatal group. With the completion of the MOMS trial, open fetal surgery for myelomeningocele is now one standard of care option, at a handful of highly experienced centers, for appropriate patients.
In Europe, open fetal surgery for spina bifida was introduced in 2003 by the Polish pediatric surgeon Janusz Bohosiewicz in Katowice. Through the end of 2011, more than 40 fetuses with spina bifida were operated at this center.
After the publication of the initial results of the MOMS trial, the NICHD agreed to fund phase two of the Management of Myelomeningocele Study (MOMS 2). MOMS2 is currently underway - the 183 patient families from the initial trial continue to be monitored by participating clinical sites. The continuation of the study will provide valuable insight into the lasting outcomes of prenatal repair of spina bifida versus standard postnatal repair in children 6 to 9 years of age. This opportunity to compare long-term results will help clinicians to learn more about all children with spina bifida and allow both clinical teams and patients to make informed choices about the treatment options available in the future.
Endoscopic fetal surgery
In contrast to the open fetal operative approach performed in the MOMS trial, a minimally-invasive fetoscopic approach has been developed by the German pediatrician Thomas Kohl of the German Center for Fetal Surgery & Minimally-Invasive Therapy at the University of Giessen, Germany. This approach has been heavily criticized by the independent authors of a controlled study about this cohort and deemed unethical by others.
This approach under general materno-fetal anesthesia uses three trocars (small tubes) with an external diameter of 5 mm that are directly placed through the maternal abdominal wall into the uterine cavity under ultrasound guidance. Following intrauterine access, part of the amniotic fluid is removed and the uterus is insufflated with carbon dioxide (this technique provides superior visualization of fetoscopic spina bifida closure, is called PACI (partial amniotic fluid insufflation), and has been safe for mothers and fetuses alike in over 70 procedures on human fetuses). After fetal posturing, the neural cord is freed from pathological adhesions and covered with patch material. Watertight closure is demonstrated by intraoperative bulging of the patch. Accordingly, reversal of hindbrain herniation can be documented within days after most procedures.
The observations in mothers and their fetuses that were operated over the past two and a half years by the matured minimally invasive approach showed the following results: Compared to the open fetal surgery technique, fetoscopic repair of myelomeningocele results in far less surgical trauma to the mother, as large incisions of her abdomen and uterus are not required. In contrast, the initial punctures have a diameter of 1.2 mm only. As a result, thinning of the uterine wall or dehisscence which have been among the most worriesome and critizised complications after the open operative approach do not occur following minimally invasive fetoscopic closure of spina bifida aperta. The risks of maternal chorioamniotis or fetal death as a result of the fetoscopic procedure run below 5%. Operated women are discharged home from hospital one week after the procedure. There is no need for chronic administration of tocolytic agents since postoperative uterine contractions are barely ever observed. The current cost of the entire fetoscopic procedure, including hospital stay, drugs, perioperative clinical, ECG, ultrasound and MRI-examinations, is approximately €16,000.
In a cohort of 20 infants that underwent fetoscopic surgery on the lesion between July 2010 and December 2011 and were studied during the first six months of life, reversal of hindbrain herniation was observed in 18 (90%) and shunt insertion was required in only eight (40%). Normal to near normal leg function was observed in about two thirds of the infants. An abnormal foot position at birth was observed in only two. The fetuses that were operated at a mean of 24 weeks of gestation were born at a mean gestational age at delivery of about 33 weeks of gestation.
In 2012, these results of the fetoscopic approach were presented at various national and international meetings, among them at the 1st European Symposium “Fetal Surgery for Spina bifida“ in April 2012 in Giessen, at the 15th Congress of the German Society for Prenatal Medicine and Obstetrics in May 2012 in Bonn, at the World Congress of the Fetal Medicine Foundation in June 2012 and at the World Congress of the International Society of Obstetrics and Gynecology (ISUOG) in Copenhagen in September 2012, and published in abstract form. In contrast to the low maternal and fetal complication rates that can be achieved by the current fetoscopic approach, its clinical introduction was affected by technical difficulties and a number of adverse fetal outcomes: Three of the first 19 procedures could not be completed, three fetuses died, and the mean gestational age at delivery was 29 weeks of gestation. As a result, the approach was heavily critizised by the independent authors of a controlled study about this cohort and deemed unethical by others. Specifically, published in the January 2012 issue of Developmental Medicine & Child Neurology, David Shurtleff, Ph.D., stated that “the extremely high complication rates for mother and infant in this study and the principle of primum non nocere indicate that at this time it is unethical to pursue intrauterine endoscopic myelomeningocele repair in humans until the procedure has been perfected in animals. “ Additionally, VERBEEK, R. J.,et al, published in the same issue of Developmental Medicine & Child Neurology that “fetal endoscopic surgery is associated with spinal segmental neuroprotection, but it results in more complications. Before considering clinical implementation of fetal endoscopic myelomeningocele closure as standard care, the frequency of complications should be appropriately reduced and results assessed in larger groups over a longer period of time.”
In contrast, with the completion of the MOMS trial, open fetal surgery for myelomeningocele is now one standard of care option, at highly experienced centers, for appropriate patients.
Notable people
Notable people with spina bifida include:
- Tanni Grey-Thompson - Welsh Paralympic athlete, member of British House of Lords
- Blaine Harrison - lead singer, keyboards, rhythm guitarist and former drummer of the British band Mystery Jets
- Rene Kirby - US actor in films such as Shallow Hal and Stuck on You
- John Mellencamp - US rock and roll musician
- Karin Muraszko - chair of Department of Neurosurgery at University of Michigan, first woman appointed to such a position in the US
- Jeffrey Tate - British conductor
- Hank Williams - US country music singer-songwriter
- Lucinda Williams - US country music singer-songwriter
- Miller Williams - US poet
- Chandre Oram - Man who has a tail due to spina bifida.
- George Schapell - US country music singer. Conjoined twin with Lori Schapell, Together they are the oldest confirmed conjoined twins.
- Justin Yoder, soapbox driver and protagonist of the Disney Channel movie Miracle in Lane 2
- Billy Bridges, Canadian Paralympic ice sledge hockey and wheelchair basketball player
- Aaron Fotheringham, an extreme wheelchair athlete.
Additional images
See also
References
- "Are There Different Types Of Spina Bifida?". SBA. Retrieved 22 February 2012.
- ^ Foster, Mark R. "Spina Bifida". Retrieved 2008-05-17.
- ^ "Spina Bifida Occulta". SBA. Retrieved 22 February 2012.
- "Spina Bifida Fact Sheet". National Institute of Neurological Disorders and Stroke. 2013.
- van Tulder MW, Assendelft WJ, Koes BW, Bouter LM (1997). "Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies". Spine. 22 (4): 427–34. doi:10.1097/00007632-199702150-00015. PMID 9055372.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Iwamoto J, Abe H, Tsukimura Y, Wakano K (2005). "Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school rugby players: a prospective study". Scandinavian journal of medicine & science in sports. 15 (3): 163–8. doi:10.1111/j.1600-0838.2004.00414.x. PMID 15885037.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Iwamoto J, Abe H, Tsukimura Y, Wakano K (2004). "Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school and college football players: a prospective study". The American journal of sports medicine. 32 (3): 781–6. doi:10.1177/0363546503261721. PMID 15090397.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Steinberg EL, Luger E, Arbel R, Menachem A, Dekel S (2003). "A comparative roentgenographic analysis of the lumbar spine in male army recruits with and without lower back pain". Clinical radiology. 58 (12): 985–9. doi:10.1016/S0009-9260(03)00296-4. PMID 14654032.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, Kalyon TA (2005). "Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain". Spine. 30 (8): E210–3. doi:10.1097/01.brs.0000158950.84470.2a. PMID 15834319.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Avrahami E, Frishman E, Fridman Z, Azor M (1994). "Spina bifida occulta of S1 is not an innocent finding". Spine. 19 (1): 12–5. doi:10.1097/00007632-199401000-00003. PMID 8153797.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Incomplete Fusion, Posterior Element". Retrieved 17 October 2013.
- "Myelomeningocele". NIH. Retrieved 2008-06-06.
- Mayo Clinic
- ^ Mitchell, L. E.; Adzick, N. S.; Melchionne, J.; Pasquariello, P. S.; Sutton, L. N.; Whitehead, A. S. (2004). "Spina bifida". Lancet. 364 (9448): 1885–1895. doi:10.1016/S0140-6736(04)17445-X. PMID 15555669.
- ^ Juranek, J; Salman MS (2010). "Anomalous development of brain structure and function in spina bifida myelomeningocele". Developmental Disabilities. 1. 16 (1): 23–30. doi:10.1002/ddrr.88.
- "Protect Yourself From Latex Allergies: Plant Biologists And Immunochemists Develop Hypoallergenic Alternative To Latex". Science Daily. 1 December 2008. Retrieved 12 October 2012.
- "Tethered Spinal Cord Syndrome". AANS. Retrieved 2011-10-23.
- ^ "Chiari Malformation Fact Sheet: National Institute of Neurological Disorders and Stroke (NINDS)". Ninds.nih.gov. 2011-09-16. Retrieved 2011-10-23.
- Barkovich, J (2005). Pediatric Neuroimaging. Philadelphia, PA: Lippincott, Williams & Wilkens.
- ^ Wills, KE (1993). "Neuropsychological functioning in children with spina bifida and/or hydrocephalus". Journal of Clinical Child Psychology. 22 (2): 247–265. doi:10.1207/s15374424jccp2202_11.
- ^ Burmeister, R; Hannay HJ; Copeland K; Fletcher JM; Boudousquie A; Dennis M (2005). "Attention problems and executive functions in children with spina bifida and hydrocephalus". Child Neuropsychology. 11 (3): 265–283. doi:10.1080/092970490911324. PMID 16036451.
- ^ Tarazi, RA; Zabel TA; Mahone EM (2008). "Age-related changes in executive function among children with spina bifida/hydrocephalus based on parent behavior ratings". The Clinical Neuropsychologist. 22 (4): 585–602. doi:10.1080/13854040701425940. PMC 2575658. PMID 17853154.
- ^ Fletcher, JM; Brookshire BL; Landry SH; Bohan TP; Davidson KC; et al. (1996). "Attentional skills and executive functions in children with early hydrocephalus". Developmental Neuropsychology. 12 (1): 53–76. doi:10.1080/87565649609540640.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Snow, JH (1999). "Executive processes for children with spina bifida". Children's Health Care. 28 (3): 241–253. doi:10.1207/s15326888chc2803_3.
- Rose, BM; Holmbeck GN (2007). "Attention and executive functions in adolescents with spina bifida". Journal of Pediatric Psychology. 32 (8): 983–994. doi:10.1093/jpepsy/jsm042. PMID 17556398.
- Landry, SH; Robinson SS; Copeland D; Garner PW (1993). "Goal-directed behavior and perception of self-competence in children with spina bifida". Journal of Pediatric Psychology. 18 (3): 389–396. doi:10.1093/jpepsy/18.3.389. PMID 8340846.
- Mayes, SD; Calhoun, SL (2006). "Frequency of reading, math, and writing disabilities in children with clinical disorders". Learning and Individual Differences. 16 (2): 145–157. doi:10.1016/j.lindif.2005.07.004.
- ^ Barnes, MA; Wilkinson, M; Khemani, E; Boudesquie, A; Dennis, M; Fletcher, JM (2006). "Arithmetic processing in children with spina bifida: Calculation accuracy, strategy use, and fact retrieval fluency". Journal of Learning Disabilities. 39 (2): 174–187. doi:10.1177/00222194060390020601. PMID 16583797.
- Dennis, M; Barnes, M (2002). "Math and numeracy in young adults with spina bifida and hydrocephalus". Developmental Neuropsychology. 21 (2): 141–155. doi:10.1207/S15326942DN2102_2. PMID 12139196.
- ^ Hetherington, R; Dennis M; Barnes M; Drake J; Gentili J (2006). "Functional outcome in young adults with spina bifida and hydrocephalus". Child's Nervous System. 22 (2): 117–124. doi:10.1007/s00381-005-1231-4.
- ^ English,, LH (2009). "Mathematical developmental development in spina bifida". Developmental Disabilities Research Reviews. 15 (1): 28–34. doi:10.1002/ddrr.48. PMC 3047453. PMID 19213013.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: extra punctuation (link) - ^ Barnes, M; Dennis M; Hetherington R (2004). "Reading and writing skills in young adults with spina bifida and hydrocephalus". Journal of the International Neuropsychological Society. 10 (5): 655–663. doi:10.1017/S1355617704105055. PMID 15327713.
- Fletcher, JM (2004). "Spina bifida: Genes, brain, and development". International Review of Research in Mental Retardation. International Review of Research in Mental Retardation. 29: 63–117. doi:10.1016/S0074-7750(04)29003-6. ISBN 9780123662293.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ T. Lissauer, G. Clayden. Illustrated Textbook of Paediatrics (Second Edition). Mosby, 2003. ISBN 0-7234-3178-7
- Holmes LB (1988). "Does taking vitamins at the time of conception prevent neural tube defects?". JAMA. 260 (21): 3181. doi:10.1001/jama.260.21.3181. PMID 3184398.
- Milunsky A; Jick H; Jick SS; et al. (1989). "Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects". JAMA. 262 (20): 2847–52. doi:10.1001/jama.262.20.2847. PMID 2478730.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Mulinare J, Cordero JF, Erickson JD, Berry RJ (1988). "Periconceptional use of multivitamins and the occurrence of neural tube defects". JAMA. 260 (21): 3141–5. doi:10.1001/jama.1988.03410210053035. PMID 3184392.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Folic Acid Fortification". FDA. February 1996.
- "Folic Acid - Public Health Agency of Canada".
- ^ "Why do I need folic acid?". NHS Direct. 2006-04-27. Archived from the original on April 13, 2006. Retrieved 2006-08-19.
- Kibar Z, Torban E, McDearmid JR, Reynolds A, Berghout J, Mathieu M, Kirillova I, De Marco P, Merello E, Hayes JM, Wallingford JB, Drapeau P, Capra V, Gros P (2007). "Mutations in VANGL1 associated with neural-tube defects" (–Scholar search). N. Engl. J. Med. 356 (14): 1432–7. doi:10.1056/NEJMoa060651. PMID 17409324.
{{cite journal}}: External link in|format= - "Medical malpractice: Childbirth, failed to perform AFP test" (PDF).
- "Center for Spina Bifida: Specialists and Services". Gillette Children's Hospital Center for Spina Bifida. Gillette Children's Hospital. Retrieved 15 November 2011.
- ^ Binks, JA; Barden WS; Burke TA; Young NL (2007). "What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida". Archives of Physical Medicine and Rehabilitation. 88 (8): 1064–1073. doi:10.1016/j.apmr.2007.04.018. PMID 17678671.
- Davis, BE; Shurtleff DB; Walker WO; Seidel KD; Duguay S (2006). "Acquisition of autonomy skills in adolescents with myelomeningocele". Developmental Medicine & Child Neurology. 48 (4): 253–258. doi:10.1017/S0012162206000569.
- Friedman, D; Holmbeck GN; DeLucia C; Jandasek B; Zebracki K (2009). "Trajectories of autonomy development across the adolescent transition in children with spina bifida". Rehabilitation Psychology. 54 (1): 16–27. doi:10.1037/a0014279. PMID 19618699.
- Monsen, RB (1992). "Autonomy, coping, and self-care agency in healthy adolescents and in adolescents with spina bifida". Journal of Pediatric Nursing. 7 (1): 9–13. PMID 1548569.
- Holmbeck, GN; Devine KA (2010). "Psychosocial and family functioning in spina bifida". Developmental Disabilities Research Reviews. 16 (1): 40–46. doi:10.1002/ddrr.90. PMC 2926127. PMID 20419770.
- ^ Lemire RJ (1988). "Neural tube defects". JAMA. 259 (4): 558–62. doi:10.1001/jama.259.4.558. PMID 3275817.
- ^ Cotton P (1993). "Finding neural tube 'zippers' may let geneticists tailor prevention of defects". JAMA. 270 (14): 1663–4. doi:10.1001/jama.270.14.1663. PMID 8411482.
- Boulet, SL (2008). "Trends in postfortification prevalence of spina bifida and ancephaly in the United States". Birth Defects Research (Part A). 82 (7): 527–532. doi:10.1002/bdra.20468.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Meuli, M; Meuli-Simmen, C; Hutchins, GM; Yingling, CD; Hoffman, KM; Harrison, MR; Adzick, NS (April 1995). "In utero surgery rescues neurological function at birth in sheep with spina bifida". Nature Medicine. 1 (4): 342–7. doi:10.1038/nm0495-342. PMID 7585064.
- Paek, BW; Farmer, DL; Wilkinson, CC; Albanese, CT; Peacock, W; Harrison, MR; Jennings, RW (2000). "Hindbrain herniation develops in surgically created myelomeningocele but is absent after repair in fetal lambs". American journal of obstetrics and gynecology. 183 (5): 1119–23. doi:10.1067/mob.2000.108867. PMID 11084552.
- Bouchard, S; Davey, MG; Rintoul, NE; Walsh, DS; Rorke, LB; Adzick, NS (March 2003). "Correction of hindbrain herniation and anatomy of the vermis after in utero repair of myelomeningocele in sheep". Journal of pediatric surgery. 38 (3): 451–8, discussion 451–8. doi:10.1053/jpsu.2003.50078. PMID 12632366.
- Meuli, M; Meuli-Simmen, C; Yingling, CD; Hutchins, GM; Timmel, GB; Harrison, MR; Adzick, NS (March 1996). "In utero repair of experimental myelomeningocele saves neurological function at birth". Journal of pediatric surgery. 31 (3): 397–402. doi:10.1016/S0022-3468(96)90746-0. PMID 8708911.
- Bruner, JP; Richards, WO; Tulipan, NB; Arney, TL (January 1999). "Endoscopic coverage of fetal myelomeningocele in utero". American journal of obstetrics and gynecology. 180 (1 Pt 1): 153–8. doi:10.1016/S0002-9378(99)70167-5. PMID 9914596.
- Adzick, N Scott; Sutton, Leslie N; Crombleholme, Timothy M; Flake, Alan W (1998). "Successful fetal surgery for spina bifida". The Lancet. 352 (9141): 1675–1676. doi:10.1016/S0140-6736(98)00070-1.
- Tubbs, RS; Chambers, MR; Smyth, MD; Bartolucci, AA; Bruner, JP; Tulipan, N; Oakes, WJ (March 2003). "Late gestational intrauterine myelomeningocele repair does not improve lower extremity function". Pediatric neurosurgery. 38 (3): 128–32. doi:10.1159/000068818. PMID 12601237.
- "Background of Management of Myelomeningocele Study (MOMS)". The GWU Biostatistics Center. Retrieved 2012-08-06.
- "Management of Myelomeningocele Study (MOMS) - Full Text View". ClinicalTrials.gov. Retrieved 2012-08-06.
- http://www.spinabifidamoms.com/english/index.html.
{{cite web}}: Missing or empty|title=(help) - http://www.spinabifidamoms.com/english/index.html.
{{cite web}}: Missing or empty|title=(help) - http://www.spinabifidamoms.com/english/index.html.
{{cite web}}: Missing or empty|title=(help) - http://www.spinabifidamoms.com/english/index.html.
{{cite web}}: Missing or empty|title=(help) - http://www.spinabifidamoms.com/english/index.html.
{{cite web}}: Missing or empty|title=(help) - Adzick, NS; Thom, Elizabeth A.; Spong, Catherine Y.; Brock, John W.; Burrows, Pamela K.; Johnson, Mark P.; Howell, Lori J.; Farrell, Jody A.; et al. (February 9, 2011). "A Randomized Trial of Prenatal versus Postnatal Repair of Myelomeningocele". New England Journal of Medicine. Online First. 364 (11): 993–1004. doi:10.1056/NEJMoa1014379. PMC 3770179. PMID 21306277.
- http://www.nejm.org/doi/full/10.1056/NEJMoa1014379.
{{cite web}}: Missing or empty|title=(help) - http://www.nejm.org/doi/full/10.1056/NEJMoa1014379.
{{cite web}}: Missing or empty|title=(help) - http://www.nejm.org/doi/full/10.1056/NEJMoa1014379.
{{cite web}}: Missing or empty|title=(help) - J. Bohosiewicz, T. Koszutski u. a.: Fetal repair of myelomeningocele in human fetuses. Experience related with 33 cases. In: Archives of Perinatal Medicine. Band 17, Nummer 2, 2011, S. 81–84.
- http://clinicaltrials.gov/show/NCT00060606.
{{cite web}}: Missing or empty|title=(help) - "Universitätsklinikum Giessen und Marburg - Offener Rücken/ Spina bifida aperta". Ukgm.de. Retrieved 2011-10-23.
- VERBEEK, RENATE J (2011). "Fetal endoscopic myelomeningocele closure preserves segmental neurological function". Developmental Medicine. 54 (1): 15–22. doi:10.1111/j.1469-8749.2011.04148.x.
- SHURTLEFF, DAVID (2011). "Fetal endoscopic myelomeningocele repair". Developmental Medicine & Child Neurology. 54 (1): 4–5. doi:10.1111/j.1469-8749.2011.04141.x.
- Verbeek, R; Heep A; et al. (15 December 2010). "Does fetal endoscopic closure of the myelomeningocele prevent loss of neurologic function in spina bifida aperta?". Cerebrospinal Fluid Research. 7 (1): S18 – S18. doi:10.1186/1743-8454-7-S1-S18.
{{cite journal}}: Unknown parameter|author-separator=ignored (help)CS1 maint: unflagged free DOI (link) - Farmer, DL (2003). "In utero repair of myelomeningocele: experimental pathophysiology, initial clinical experience, and outcomes". Arch Surg. 138 (8): 872–878. doi:10.1001/archsurg.138.8.872. PMID 12912746.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Kohl, Thomas (2008). "Current status and prospects of fetoscopic surgery for spina bifida in human fetuses". Fetal Diagn Ther. 24 (3): 318–320. doi:10.1159/000158549. PMID 18832851.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - T. Kohl, A. Kawecki u. a.: Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. In: Ultrasound Obstet Gynecol. Bnad 40:9, 2012
- "DZFT beim Kongress DGPGM | DZFT". Dzft.de. Retrieved 2012-11-14.
- "The Fetal Medicine Foundation / FMF World Congress". Fetalmedicine.com. Retrieved 2012-11-14.
- "World Congress 2012 | World Congress". ISUOG. 2012-09-13. Retrieved 2012-11-14.
- Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Tchatcheva K, Axt-Fliedner R, Kohl T.; et al. (2012). "Mütterliches Outcome nach minimal-invasivem Verschluss einer Spina bifida". Ultraschall in Med. 33: S96.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Maternal outcome after minimally-invasive fetoscopic surgery for spina bifida. The Giessen experience 2010 – 2012. Ultrasound Obstet Gynecol 2012;40(Suppl. 1) 9
- Neubauer B, Degenhardt J, Axt-Fliedner R, Kohl T (2012). "Frühe neurologische Befunde von Säuglingen nach minimal-invasivem fetoskopischen Verschluss ihrer Spina bifida aperta". Z Geburtsh Neonat. 216 (2): 87. doi:10.1055/s-0032-1309110.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R, Neubauer B. "Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 – 2011. Ultrasound Obstet Gynecol 2012;40(Suppl. 1) 9
- Kohl T, Schürg R, Maxeiner H, Tchatcheva K, Degenhardt J, Stressig R, Axt-Fliedner R, Gembruch U. "Partial carbon dioxide insufflation (PACI) during fetoscopic surgery on 60 fetuses with spina bifida. Ultrasound Obstet Gynecol 2012;40(Suppl. 1) 73-74
- Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R. "Preoperative sonoanatomic examination of fetal spina bifida permits prediction of surgical complexity during subsequent minimally-invasive fetoscopic closure. Ultrasound Obstet Gynecol 2012;40(Suppl. 1) 8
- Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T (2012). "Rückverlagerung der Chiari-II Malformation innerhalb weniger Tage nach minimal-invasivem Patchverschluss ans Hinweis für einen effektiven Verschluss der Fehlbildung". Ultraschall in Med. 33: S95.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Degenhardt J, Kawecki A, Enzensberger C, Stressig R, Axt-Fliedner R, Kohl T. "Reversal of hindbrain herniation within a few days after minimally-invasive fetoscopic surgery for spina bifida indicates the desired water-tight closure of the lesion. Ultrasound Obstet Gynecol 2012;40(Suppl. 1) 74
- R. J. Verbeek, A. Heep (2012) Fetal endoscopic myelomeningocele closure preserves segmental neurological function. In: Developmental medicine and child neurology. 54(1) 15–22 doi:10.1111/j.1469-8749.2011.04148.x PMID 22126123
- Kohl T, Gembruch U, Thomas , Kohl Thomas, Gembruch Ulrich; Gembruch (2008). "Current status and prospects of fetoscopic surgery for spina bifida in human fetuses". Fetal Diagnosis and Therapy. 24 (3): 318–320. doi:10.1159/000158549. PMID 18832851.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - SHURTLEFF, DAVID (2011). "Fetal endoscopic myelomeningocele repair". Developmental Medicine. 54 (1): 4–5. doi:10.1111/j.1469-8749.2011.04141.x.
- VERBEEK, RENATE J (2011). "Fetal endoscopic myelomeningocele closure preserves segmental neurological function". Developmental Medicine. 54 (1): 15–22. doi:10.1111/j.1469-8749.2011.04148.x.
- Adzick, N. Scott (2011). "A Randomized Trial of Prenatal versus Postnatal Repair of Myelomeningocele". New England Journal of Medicine. 364 (11): 993–1004. doi:10.1056/NEJMoa1014379.
- The Telegraph - World of Tanni Grey-Thompson, former Paralympic champion
- Martin, Dan (2008-06-14). "Dan Martin meets Blaine from the Mystery Jets". guardian.co.uk. Retrieved 2008-08-06.
- "Interview with actress Sascha Knopf from Shallow Hal". Movies.about.com. 2009-12-17. Retrieved 2011-10-23.
- "Mellencamp: Hoosier musician now Rock Hall of Famer". Indystar.com. Mar 11, 2008. Retrieved 2012-12-06.
- Gavin, Kara (2001). "U-M Neurosurgeon Urges Women to Protect their Children by Taking Folic Acid". Medicine at Michigan. 3 (2). Retrieved 2008-07-03.
- Service, Tom (13 October 2011). "Jeffrey Tate: 'I've had to fight all my life'". The Guardian. Retrieved 21 February 2012.
- Famous People and Spina Bifida
- ^ Lewine, Edward (March 1, 2009). "Domains: Country House". The New York Times. pp. MM17. Retrieved 2009-03-02.
External links
- CDC: Spina Bifida
- The International Federation for Spina Bifida and Hydrocephalus
- Spina Bifida Association of America
- UCSF Fetal Treatment Center: Myelomeningocele (Spina Bifida)
- National Institute of Neurological Disorders and Stroke: Spina Bifida Information Page
- Mayo Clinic: Spina bifida Symptoms
- The Children's Hospital of Philadelphia: Eligibility Guidelines for Prenatal Repair of Myelomeningocele
- Spina Bifida Information
- Information about Spina bifida and fetal treatment
- I'll Find A Way, Oscar®-winning documentary (1977) of a 9-year-old girl with spina bifida
| Congenital malformations and deformations of nervous system | |||||
|---|---|---|---|---|---|
| Brain |
| ||||
| Spinal cord |
| ||||
| Congenital malformations and deformations of musculoskeletal system / musculoskeletal abnormality | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Appendicular limb / dysmelia |
| ||||||||||||||||||||||
| Axial |
| ||||||||||||||||||||||
