| Revision as of 02:24, 7 March 2014 editEllenCT (talk | contribs)Extended confirmed users11,831 edits revert: on the contrary, this is an accurate summary of one of many of the source's arguments← Previous edit | Revision as of 21:09, 9 January 2015 edit undoRenamed user 51g7z61hz5af2azs6k6 (talk | contribs)6,460 edits →Development and marketing of antihypertensive drugs: expandNext edit → | ||
| (162 intermediate revisions by 50 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Use dmy dates|date=July 2014}} | |||
| ], a ] used in the treatment several ]s, is marketed by ], one of the world major ].]] | |||
| ], a ] used in the treatment of several ]s, is marketed by ], one of the world major ].]] | |||
| The '''pharmaceutical industry''' develops, produces, and markets ]s or ]s ]d for use as ]s.<ref>John L. McGuire, Horst Hasskarl, Gerd Bode, Ingrid Klingmann, Manuel Zahn "Pharmaceuticals, General Survey" Ullmann's Encyclopedia of Chemical Technology" Wiley-VCH, Weinheim, 2007. {{DOI|10.1002/14356007.a19_273.pub2}}</ref> Pharmaceutical companies are allowed to deal in ] or ] medications and medical devices. They are subject to a ] and regulations regarding the ]ing, testing and ensuring safety and efficacy and ]. | The '''pharmaceutical industry''' develops, produces, and markets ]s or ]s ]d for use as ]s.<ref>John L. McGuire, Horst Hasskarl, Gerd Bode, Ingrid Klingmann, Manuel Zahn "Pharmaceuticals, General Survey" Ullmann's Encyclopedia of Chemical Technology" Wiley-VCH, Weinheim, 2007. {{DOI|10.1002/14356007.a19_273.pub2}}</ref> Pharmaceutical companies are allowed to deal in ] or ] medications and medical devices. They are subject to a ] and regulations regarding the ]ing, testing and ensuring safety and efficacy and ]. | ||
| ==History== | ==History== | ||
| The earliest ] date to the ]. The first known drugstore was opened by ] in ] in 754,<ref>Information taken from the abstract of {{Cite journal| issn = 0350-199X | volume = 51 | issue = 1–2 | pages = 47–50 | last = Hadzović | first = S | title = Pharmacy and the great contribution of Arab-Islamic science to its development | language = Croatian | journal = Medicinski arhiv | year = 1997 | pmid = 9324574 | oclc = 32564530}}</ref> and many more soon began operating throughout the ] and eventually ] ]. By the 19th century, many of the drugstores in Europe and ] had eventually developed into larger pharmaceutical companies. | |||
| ===Mid-1800's - 1945: From botanicals to the first synthetic drugs=== | |||
| Most of today's major pharmaceutical companies were founded in the late 19th and early 20th centuries. Key discoveries of the 1920s and 1930s, such as ] and ], became mass-manufactured and distributed. ], Germany and Italy had particularly strong industries, with the United Kingdom, the United States, Belgium and the Netherlands following suit. | |||
| The modern pharmaceutical industry traces its roots to two sources. The first of these are local apothecaries that expanded from their traditional role distributing botanical drugs such as ] and ] to wholesale manufacture in the mid 1800s. Multinational corporations including ], ], Burroughs-Wellcome (now part of ]), ], ] and ] (now part of ]) began their histories as local apothecary shops in the mid-1800s. By the late 1880s, German dye manufacturers had perfected the purification of individual organic compounds from coal tar and other mineral sources and had also established rudimentary methods in ].<ref>{{cite web |url=http://pubs.acs.org/cen/coverstory/83/8325/8325emergence.html |title=Top Pharmaceuticals: Introduction: EMERGENCE OF PHARMACEUTICAL SCIENCE AND INDUSTRY: 1870-1930 |work= |accessdate=}}</ref> The development of synthetic chemical methods allowed scientists to systematically vary the structure of chemical substances, and growth in the emerging science of ] expanded their ability to evaluate the biological effects of these structural changes. | |||
| Legislation was enacted to test and approve drugs and to require appropriate labeling. Prescription and non-prescription drugs became legally distinguished from one another as the pharmaceutical industry matured. The industry got underway in earnest from the 1950s, due to the development of systematic scientific approaches, understanding of human biology (including ]) and sophisticated manufacturing techniques. | |||
| ====Epinephrine, norepinephrine, and amphetamine==== | |||
| By the 1890s the profound effect of adrenal extracts on many different tissue types had been discovered, setting off a search both for the mechanism of chemical signalling and efforts to exploit these observations for the development of new drugs. The blood pressure raising and vasoconstrictive effects of adrenal extracts were of particular interest to surgeons as ] agents and as treatment for shock, and a number of companies developed products based on adrenal extracts containing varying purities of the active substance. In 1897 John Abel of Johns Hopkins University identified the active principle as ], which he isolated in an impure state as the sulfate salt. Industrial chemist ] later developed a method for obtaining epinephrine in a pure state, and licensed the technology to ]. Parke Davis marketed epinephrine under the trade name ]. Injected epinephrine proved to be especially efficacious for the acute treatment of ] attacks, and an inhaled version was sold in the United States until 2011 (]).<ref name="Sneader2005">{{cite book|author=Walter Sneader|title=Drug Discovery: A History|url=http://books.google.com/books?id=jglFsz5EJR8C|date=31 October 2005|publisher=John Wiley & Sons|isbn=978-0-470-01552-0|pages= 155–156}}</ref><ref name="Rasmussen 2006 288–323">{{cite journal |title=Making the First Anti-Depressant: Amphetamine in American Medicine, 1929-1950 |journal=J Hist Med Allied Sci |year=2006 |last=Rasmussen |first=Nicolas |volume=61 |issue=3 |pages=288–323 |doi=10.1093/jhmas/jrj039 |accessdate=2014-11-08 }}</ref> By 1929 epinephrine had been formulated into an inhaler for use in the treatment of nasal congestion. | |||
| While highly effective, the requirement for injection limited the use of norepinephrine and orally active derivatives were sought. A structurally similar compound, ], was identified by Japanese chemists in the ''Ma Huang'' plant and marketed by Eli Lilly as an oral treatment for asthma. Following the work of Henry Dale and George Barger at Burroughs-Wellcome, academic chemist Gordon Alles synthesized amphetamine in and tested in asthma patients in 1929. The drug proved to have only modest anti-asthma effects, but produced sensations of exhilaration and palpitations. Amphetamine was developed by ] as a nasal decongestant under the trade name ] Amphetamine was eventually developed for the treatment of ], post-encepheletic parkinsonism, and mood elevation in depression and other psychiatric indications. It receive approval as a New and Nonofficial Remedy from the American Medical Association for these uses in 1937 and remained in common use for depression until the development of tricyclic antidepressants in the 1960s.<ref name="Rasmussen 2006 288–323"/> | |||
| ====Discovery and development of the barbiturates==== | |||
| ] | |||
| In 1903 ] and ] disclosed their discovery that diethylbarbituric acid, formed from the reaction of diethylmalonic acid, phosphorus oxychloride and urea, induces sleep in dogs. The discovery was patented and licensed to ], which marketed the compound under the trade name ] as a sleep aid beginning in 1904. Systematic investigations of the effect of structural changes on potency and duration of action led to the discovery of ] at Bayer in 1911 and the discovery of its potent anti-epileptic activity in 1912. Phenobarbital was among the most widely used drugs for the treatment of ] through the 1970s, and as of 2014, remains on the World Health Organizations list of essential medications.<ref>{{cite journal |author=Yasiry Z, Shorvon SD |title=How phenobarbital revolutionized epilepsy therapy: the story of phenobarbital therapy in epilepsy in the last 100 years |journal=Epilepsia |volume=53 Suppl 8 |issue= |pages=26–39 | date=December 2012 |pmid=23205960 |doi=10.1111/epi.12026 |url=}}</ref><ref>{{cite journal |author=López-Muñoz F, Ucha-Udabe R, Alamo C |title=The history of barbiturates a century after their clinical introduction |journal=Neuropsychiatr Dis Treat |volume=1 |issue=4 |pages=329–43 | date=December 2005 |pmid=18568113 |pmc=2424120 |doi= |url=}}</ref> The 1950s and 1960s saw increased awareness of the addictive properties and abuse potential of barbiturates and amphetamines and led to increasing restrictions on their use and growing government oversight of prescribers. The major use of these drugs today is restricted to the use of amphetamine for the treatment of ] and phenobarbital for ].<ref>{{cite journal |title=Drug Abuse Control Amendments of 1965 |journal=NEJM |date=1965-11-25 |volume=273 |pages=1222–1223 |doi=10.1056/NEJM196511252732213 |accessdate=2014-11-10 |quote="Officers of the Food and Drug Administration, aware of the seriousness of the problem, estimate that approximately half the 9,000,000,000 barbiturate and amphetamine capsules and tablets manufactured annually in this country are diverted to illegal use. The profits to be gained from the illegal sale of these drugs have proved an attraction to organized crime, for amphetamine can be purchased at wholesale for less than $1 per 1000 capsules, but when sold on the illegal market, it brings $30 to $50 per 1000 and when retailed to the individual buyer, a tablet may bring as much as 10 to 25 cents." }}</ref><ref>{{cite journal |title=Sedative-Hypnotic Drugs — The Barbiturates — I |journal=NEJM |year=1956 |volume=255 |pages=1150–1151 |doi=10.1056/NEJM195612132552409 |accessdate=2014-11-10 |quote=THE barbiturates, introduced into medicine by E. Fischer and J. von Mering1 in 1903, are certainly among the most widely used and abused drugs in medicine. Approximately 400 tons of these agents are manufactured each year; this is enough to put approximately 9,000,000 people to sleep each night for that period if each were given a 0.1-gm. dose }}</ref> | |||
| ====Insulin==== | |||
| A series of experiments performed from the late 1800s to the early 1900s revealed that ] is caused by the absence of a substance normally produced by the pancreas. In 1869, Oscar Minkowski and Joseph von Mering found that diabetes could be induced in dogs by surgical removal of the pancreas. In 1921, Canadian professors ] and his student Charles Best repeated this study, and found that injections of pancreatic extract reversed the symptoms produced by pancreas removal. The extract was demonstrated to work in people soon thereafter, but development of insulin therapy as a routine medical procedure was delayed by difficulties in producing the material in sufficient quantity and with reproducible purity. The researchers sought assistance from industrial collaborators at Eli Lilly and Co. based on the company's experience with large scale purification of biological materials. Chemist George Walden of Eli Lilly and Company found that careful adjustment of the pH of the extract allowed a relatively pure grade of insulin to be produced. Under pressure from Toronto University and a potential patent challenge by academic scientists who had independently developed a similar purification method, an agreement was reached for non-exclusive production of insulin by multiple companies. Prior to the discovery and widespread availability of insulin therapy the life expectancy of diabetics was only a few months.<ref>{{cite journal |author=Rosenfeld L |title=Insulin: discovery and controversy |journal=Clin. Chem. |volume=48 |issue=12 |pages=2270–88 | date=December 2002 |pmid=12446492 |doi= |url=}}</ref> | |||
| ====Early anti-infective research - Salvarsan, Prontosil, Penicillin and Vaccines==== | |||
| The development of drugs for the treatment of infectious diseases was a major focus of early research and development efforts; in 1900 pneumonia, tuberculosis, and diarrhea were the three leading causes of death in the United States and mortality in the first year of life exceeded 10%.<ref name="www.cdc.gov">{{cite web |url=http://www.cdc.gov/nchs/data/nvsr/nvsr47/nvs47_28.pdf |title=www.cdc.gov |format= |work= |accessdate=}}</ref><ref>{{cite web |url=http://www.cdc.gov/nchs/data/dvs/lead1900_98.pdf |title=www.cdc.gov |format= |work= |accessdate=}}</ref> | |||
| In 1911 ], the first synthetic anti-infective drug, was developed by ] and chemist Alfred Bertheim of the Institute of Experimental Therapy in Berlin. The drug was given the commercial name Salvarsan.<ref>{{cite journal |author=Sepkowitz KA |title=One hundred years of Salvarsan |journal=N. Engl. J. Med. |volume=365 |issue=4 |pages=291–3 | date=July 2011 |pmid=21793743 |doi=10.1056/NEJMp1105345 |url=}}</ref> Ehrlich, noting both the general toxicity of ] and the selective absorption of certain dyes by bacteria, hypothesized that an arsenic-containing dye with similar selective absorption properties could be used to treat bacterial infections. Arsphenamine was prepared as part of a campaign to synthesize a series of such compounds, and found to exhibit partially selective toxicity. Arsphenamine proved to be the first effective treatment for ], a disease which prior to that time was incurable and led inexorably to severe skin ulceration, neurological damage, and death. | |||
| Ehrlich’s approach of systematically varying the chemical structure of synthetic compounds and measuring the effects of these changes on biological activity was pursued broadly by industrial scientists, including ] scientists Josef Klarer, Fritz Mietzsch, and ]. This work, also based in the testing of compounds available from the German dye industry, led to the discover of ], the first representative of the ] class of ]. Compared to arsphenamine, the sulfonamides had a broader spectrum of activity and were far less toxic, rendering them useful for infections caused by pathogens such as ].<ref>{{cite journal |author=Aminov RI |title=A brief history of the antibiotic era: lessons learned and challenges for the future |journal=Front Microbiol |volume=1 |issue= |pages=134 |year=2010 |pmid=21687759 |pmc=3109405 |doi=10.3389/fmicb.2010.00134 |url=}}</ref> In 1939, Domagk received the ] for this discovery.<ref>], ''The Demon Under the Microscope'' (2006) ISBN 1-4000-8213-7 (cited in – ] '']'' 23 December 2006)</ref><ref></ref> Nonetheless, the dramatic decrease in deaths from infectious diseases that occurred prior to ] was primarily the result of improved public health measures such as clean water and less crowded housing, and that the impact of anti-infective drugs and vaccines was significant mainly after World War II.<ref name="www.nber.org">{{cite web |url=http://www.nber.org/papers/w8556.pdf |title=www.nber.org |format= |work= |accessdate=}}</ref><ref name="Klein 2012 167">{{cite book |last=Klein |first1=Herbert |title=A Population History of the United States |publisher=Cambridge University Press |year=2012 |page=167 |accessdate=2014-11-07 }}</ref> | |||
| In 1928, ] discovered the antibacterial effects of ], but its exploitation for the treatment of human disease awaited the development of methods for its large scale production and purification. These were developed by a U.S. and British government-led consortium of pharmaceutical companies during the Second World War.<ref name=ChemH> Manufacturing a Cure: Mass Producing Penicillin</ref><ref name=JParas>{{cite book | |||
| |author=John Parascandola |authorlink=John Parascandola |title=The History of antibiotics: a symposium | |||
| |publisher=American Institute of the History of Pharmacy No. 5 |year=1980 |isbn=0-931292-08-5 }}</ref> | |||
| Early progress toward the development of vaccines occurred throughout this period, primarily in the form of academic and government funded basic research directed toward the identification of the pathogens responsible for common communicable diseases. In 1885 ] and ] created the first ]. The first ]s were produced in 1914 from a mixture of ] and ] (produced from the serum of an inoculated animal), but the safety of the inoculation was marginal and it was not widely used. The United States recorded 206,000 cases of diphtheria in 1921 resulting in 15,520 deaths. In 1923 parallel efforts by ] at the Pasteur Institute and ] at the Wellcome Research Laboratories (later part of ]) led to the discovery that a safer vaccine could be produced by treating diphtheria toxin with ].<ref>{{cite web |url=http://www.historyofvaccines.org/content/timelines/diphtheria |title=Diphtheria — Timelines — History of Vaccines |format= |work= |accessdate=}}</ref> In 1944, ] of Squibb Pharmaceuticals developed the first ].<ref>{{cite web |url=http://articles.latimes.com/2005/apr/13/local/me-hilleman13++ |title=Maurice R. Hilleman, 85; Scientist Developed Many Vaccines That Saved Millions of Lives - Los Angeles Times |format= |work= |accessdate=}}</ref> Hilleman would later move to ] where he would play a key role in the development of vaccines against ], ], ], ], ], ], and ]. | |||
| ====Unsafe drugs and early industry regulation==== | |||
| ] | |||
| Prior to the beginning of the 20th century drugs were generally produced by small scale manufacturers with little regulatory control over manufacturing or claims of safety and efficacy. To the extent that such laws did exist, enforcement was lax. In the United States, increased regulation of vaccines and other biological drugs was spurred by tetanus outbreaks and deaths caused by the distribution of contaminated smallpox vaccine and diphtheria antitoxin.<ref>{{cite web |url=http://www.fda.gov/AboutFDA/WhatWeDo/History/Milestones/ucm128305.htm |title=Significant Dates in U.S. Food and Drug Law History |work= |accessdate=}}</ref> The Biologics Control Act of 1902 required that federal government grant premarket approval for every biological drug and for the process and facility producing such drugs. This was followed in 1906 by the ], which forbade the interstate distribution of adulterated or misbranded foods and drugs. A drug was considered misbranded if it contained alcohol, morphine, opium, cocaine, or any of several other potentially dangerous or addictive drugs, and if its label failed to indicate the quantity or proportion of such drugs. The government's attempts to use the law to prosecute manufacturers for making unsupported claims of efficacy were undercut by a Supreme Court ruling restricting the federal government's enforcement powers to cases of incorrect specification of the drug's ingredients.<ref>{{cite web |url=http://www.fdareview.org/history.shtml#first |title=FDAReview.org, a project of The Independent Institute |format= |work= |accessdate=}}</ref> | |||
| In 1937 over 100 people died after ingesting Elixir of Sulfanalimide manufactured by S.E. Massengill Company of Tennessee. The product was formulated in ], a highly toxic solvent that is now widely used as antifreeze.<ref>{{cite web |url=http://www.fda.gov/aboutfda/whatwedo/history/productregulation/sulfanilamidedisaster/default.htm |title=Sulfanilamide Disaster |work= |accessdate=}}</ref> Under the laws extant at that time, prosecution of the manufacturer was possible only under the technicality that the product had been called an "elixir", which literally implied a solution in ethanol. In response to this episode, the U.S. Congress passed ], which for the first time required pre-market demonstration of safety before a drug could be sold, and explicitly prohibited false therapeutic claims.<ref>{{cite web |url=http://www.fda.gov/aboutFDA/WhatWeDo/History/origin/ucm054826.htm |title=FDA History - Part II |work= |accessdate=}}</ref> | |||
| ===The Post-War Years, 1945-1970=== | |||
| ====Further advances in anti-infective research==== | |||
| The aftermath of the war saw an explosion in the discovery of new classes of antibacterial drugs<ref>{{cite journal |author=Zaffiri L, Gardner J, Toledo-Pereyra LH |title=History of antibiotics. From salvarsan to cephalosporins |journal=J Invest Surg |volume=25 |issue=2 |pages=67–77 | date=April 2012 |pmid=22439833 |doi=10.3109/08941939.2012.664099 |url=}}</ref> including the cephalosporins (developed by Eli Lilly based on the seminal work of ] and ]),<ref>{{cite journal |author=Hamilton-Miller JM |title=Development of the semi-synthetic penicillins and cephalosporins |journal=Int. J. Antimicrob. Agents |volume=31 |issue=3 |pages=189–92 | date=March 2008 |pmid=18248798 |doi=10.1016/j.ijantimicag.2007.11.010 |url=}}</ref><ref>{{cite journal |author=Abraham EP |title=Cephalosporins 1945-1986 |journal=Drugs |volume=34 Suppl 2 |issue= |pages=1–14 |year=1987 |pmid=3319494 |doi= |url=}}</ref> streptomycin (discovered during a Merck-funded research program in Selman Waksman's laboratory<ref>{{cite journal |author=Kingston W |title=Streptomycin, Schatz v. Waksman, and the balance of credit for discovery |journal=J Hist Med Allied Sci |volume=59 |issue=3 |pages=441–62 | date=July 2004 |pmid=15270337 |doi= |url=}}</ref>), the tetracyclines<ref>{{cite journal |author=Nelson ML, Levy SB |title=The history of the tetracyclines |journal=Ann. N. Y. Acad. Sci. |volume=1241 |issue= |pages=17–32 | date=December 2011 |pmid=22191524 |doi=10.1111/j.1749-6632.2011.06354.x |url=}}</ref> (discovered at Lederle Laboratories, now a part of ]), erythromycin (discovered at Eli Lilly and Co.)<ref>{{cite journal |author= |title=ERYTHROMYCIN |journal=Br Med J |volume=2 |issue=4793 |pages=1085–6 | date=November 1952 |pmid=12987755 |pmc=2022076 |doi= |url=}}</ref> and their extension to an increasingly wide range of bacterial pathogens. | |||
| ] before and after introduction of the vaccine.]] | |||
| ] | |||
| During the years 1940-1955, the rate of decline in the U.S. death rate accelerated from 2% per year to 8% per year, then returned to the historical rate of 2% per year. The dramatic decline in the immediate post-war years has been attributed to the rapid development of new treatments and vaccines for infectious disease that occurred during these years.<ref name="www.nber.org"/><ref name="Klein 2012 167"/> | |||
| Vaccine development continued to accelerate, with the most notable achievement of the period being Salk's 1954 development of the polio vaccine under the funding of the non-profit National Foundation for Infantile Paralysis.<ref>{{cite web |url=https://en.wikipedia.org/search/?title=Pharmaceutical_industry&action=edit§ion=8 |title=Editing Pharmaceutical industry (section) - Misplaced Pages, the 💕 |format= |work= |accessdate=}}</ref> The vaccine process was never patented, but was instead given to pharmaceutical companies to manufacture as a low cost generic. In 1960 Maurice Hilleman of Merck, Sharpe and Dohme identified the SV40 virus, which was later shown to cause tumors in many mammalian species. It was later determined that SV40 was present as a contaminant in polio vaccine lots that had been administered to 90% of the children in the United States.<ref>{{cite journal |author=SWEET BH, HILLEMAN MR |title=The vacuolating virus, S.V. 40 |journal=Proc. Soc. Exp. Biol. Med. |volume=105 |issue= |pages=420–7 | date=November 1960 |pmid=13774265 |doi= |url=}}</ref><ref>{{cite journal |author=Shah K, Nathanson N |title=Human exposure to SV40: review and comment |journal=Am. J. Epidemiol. |volume=103 |issue=1 |pages=1–12 | date=January 1976 |pmid=174424 |doi= |url=}}</ref> The contamination appears to have originated both in the original cell stock and in monkey tissue used for production. In 2004 the United States Cancer Institute announced that it had concluded that SV40 is not associated with cancer in people.<ref>{{cite web |url=http://www.cancer.gov/newscenter/newsfromnci/2004/sv40 |title=Studies:No Evidence That SV40 is Related to Cancer - National Cancer Institute |format= |work= |accessdate=}}</ref> | |||
| Other notable new vaccines of the period include those for measles (1962, John Franklin Enders of Children's Medical Center Boston, later refined by Maurice Hilleman at Merck), Rubella (1969, Hilleman, Merck) and mumps (1967, Hilleman, Merck)<ref>{{cite web |url=http://www.historyofvaccines.org/ |title=History of Vaccines — A Vaccine History Project of The College of Physicians of Philadelphia |format= |work= |accessdate=}}</ref> The United States incidences of rubella, congenitial rubella syndrome, measles, and mumps all fell by >95% in the immediate aftermath of widespread vaccination.<ref>{{cite web |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6204a1.htm |title=Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013 |work= |accessdate=}}</ref> The first 20 years of licensed measles vaccination in the U.S. prevented an estimated 52 million cases of the disease, 17,400 cases of ], and 5,200 deaths.<ref>{{cite journal |author=Bloch AB, Orenstein WA, Stetler HC et al. |title=Health impact of measles vaccination in the United States |journal=Pediatrics |volume=76 |issue=4 |pages=524–32 |year=1985 |pmid=3931045}}</ref> | |||
| ====Development and marketing of antihypertensive drugs==== | |||
| Hypertension is a risk factor for atherosclerosis,<ref name="pmid19110086">{{cite journal |author=Insull W |title=The pathology of atherosclerosis: plaque development and plaque responses to medical treatment |journal=] |volume=122 |issue=1 Suppl |pages=S3–S14 |date=January 2009 |pmid=19110086 |doi=10.1016/j.amjmed.2008.10.013 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(08)01017-6|accessdate=2009-06-20}}</ref> ],<ref name="pmid19427498">{{cite journal |author=Gaddam KK, Verma A, Thompson M, Amin R, Ventura H |title=Hypertension and cardiac failure in its various forms |journal=] |volume=93 |issue=3 |pages=665–80 |date=May 2009 |pmid=19427498 |doi=10.1016/j.mcna.2009.02.005 |url=http://journals.elsevierhealth.com/retrieve/pii/S0025-7125(09)00020-0|accessdate=2009-06-20}}</ref> ],<ref name="pmid18815511">{{cite journal |author=Agabiti-Rosei E |title=From macro- to microcirculation: benefits in hypertension and diabetes |journal=] |volume=26 Suppl 3 |issue= |pages=S15–21 |date=September 2008 |pmid=18815511 |doi=10.1097/01.hjh.0000334602.71005.52 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0263-6352&volume=26&issue=&spage=S15|accessdate=2009-06-20}}</ref><ref name="pmid19427499">{{cite journal |author=Murphy BP, Stanton T, Dunn FG |title=Hypertension and myocardial ischemia |journal=] |volume=93 |issue=3 |pages=681–95 |date=May 2009 |pmid=19427499 |doi=10.1016/j.mcna.2009.02.003 |url=http://journals.elsevierhealth.com/retrieve/pii/S0025-7125(09)00018-2|accessdate=2009-06-20}}</ref> ],<ref name="pmid19393824">{{cite journal |author=White WB |title=Defining the problem of treating the patient with hypertension and arthritis pain |journal=] |volume=122 |issue=5 Suppl |pages=S3–9 |date=May 2009 |pmid=19393824 |doi=10.1016/j.amjmed.2009.03.002 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(09)00206-X|accessdate=2009-06-20}}</ref> ],<ref name="pmid19195963">{{cite journal |author=Truong LD, Shen SS, Park MH, Krishnan B |title=Diagnosing nonneoplastic lesions in nephrectomy specimens |journal=] |volume=133 |issue=2 |pages=189–200 |date=February 2009 |pmid=19195963 |doi= 10.1043/1543-2165-133.2.189|url=http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=133&page=189|accessdate=2009-06-20}}</ref><ref name="pmid11842376">{{cite journal |author=Tracy RE, White S |title=A method for quantifying adrenocortical nodular hyperplasia at autopsy: some use of the method in illuminating hypertension and atherosclerosis |journal=] |volume=6 |issue=1 |pages=20–9 |date=February 2002 |pmid=11842376 |doi= 10.1053/adpa.2002.30606|url=http://linkinghub.elsevier.com/retrieve/pii/S1092913402249217|accessdate=2009-06-20}}</ref> and ],<ref name="pmid18672184">{{cite journal |author=Aronow WS |title=Hypertension and the older diabetic |journal=] |volume=24 |issue=3 |pages=489–501, vi–vii |date=August 2008 |pmid=18672184 |doi=10.1016/j.cger.2008.03.001 |url=http://journals.elsevierhealth.com/retrieve/pii/S0749-0690(08)00012-8|accessdate=2009-06-20}}</ref><ref name="pmid19008688">{{cite journal |author=Gardner AW, Afaq A |title=MANAGEMENT OF LOWER EXTREMITY PERIPHERAL ARTERIAL DISEASE |journal=] |volume=28 |issue=6 |pages=349–57 |year=2008 |pmid=19008688 |doi=10.1097/HCR.0b013e31818c3b96 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1932-7501&volume=28&issue=6&spage=349|accessdate=2009-06-20 |pmc=2743684}}</ref> and is the most important ] for ] ] and ], in ].<ref name="pmid19149532">{{cite journal |author=Novo S, Lunetta M, Evola S, Novo G |title=Role of ARBs in the blood hypertension therapy and prevention of cardiovascular events |journal=] |volume=10 |issue=1 |pages=20–5 |date=January 2009 |pmid=19149532 |doi= 10.2174/138945009787122897|url=http://www.bentham-direct.org/pages/content.php?CDT/2009/00000010/00000001/0003J.SGM|accessdate=2009-06-20}}</ref> Prior to 1940 approximately 23% of all deaths among persons over age 50 were attributed to hypetension. Severe cases of hypertension were treated by surgery.<ref>{{vcite2 journal |vauthors=Craig WM |title=Surgical Treatment of Hypertension |journal=Br Med J |volume=2 |issue=4120 |pages=1215–9 |year=1939 |pmid=20782854 |pmc=2178707 |doi= |url=}}</ref> | |||
| Early developments in the field of treating hypertension included quaternary ammonium ion sympathetic nervous system blocking agents, but these compounds were never widely used due to their severe side effects, because the long term health consequences of high blood pressure had not yet been established, and because they had to be administered by injection. | |||
| In 1952 researchers at Ciba discovered the first orally available vasodilator, hydrazaline. <ref>{{cite book |last=Sneader |first1=Walter |title=Drug Discovery. A History |location=New York |publisher=Wiley |year=2005 |page=371 |accessdate=2015-01-09 }}</ref> A major shortcoming of hydralazine monotherapy was that lost its effectiveness over time (]). In the mid-1950’s Karl H. Beyer, James M. Sprague, John E. Baer, and Frederick C. Novello of ] discovered and developed chlorothiazide, which remains the most widely used anthypertensive drug today.<ref> {{vcite2 journal |vauthors=Beyer KH |title=Chlorothiazide. How the thiazides evolved as antihypertensive therapy |journal=Hypertension |volume=22 |issue=3 |pages=388–91 |year=1993 |pmid=8349332 |doi= |url=}}</ref> This development was associated with a substantial decline in the mortality rate among people with hypertension.<ref> {{vcite2 journal |vauthors=BORHANI NO, HECHTER HH |title=RECENT CHANGES IN CVR DISEASE MORTALITY IN CALIFORNIA |journal=Public Health Rep |volume=79 |issue= |pages=147–60 |year=1964 |pmid=14119789 |pmc=1915335 |doi= |url=}}</ref> The inventors were recognized by a Public Health ] in 1975 for “the saving of untold thousands of lives and the alleviation of the suffering of millions of victims of hypertension”. <ref>{{cite web |url=http://www.laskerfoundation.org/awards/formaward.htm |title=The Lasker Foundation - Awards |format= |work= |accessdate=}}</ref> | |||
| A 2009 Cochrane review concluded that thiazide antihypertensive drugs reduce the risk of death (RR 0.89), stroke (RR 0.63), coronary heart disease (RR 0.84), and cardiovascular events (RR 0.70) in people with high blood pressure.<ref>{{cite journal |author=Wright JM, Musini VM |title=First-line drugs for hypertension |journal=Cochrane Database Syst Rev |volume= |issue=3 |pages=CD001841 |year=2009 |pmid=19588327 |doi=10.1002/14651858.CD001841.pub2 |url=}}</ref> In the ensuring years other classes of antihypertensive drug were developed and found wide acceptance in combination therapy, including loop diureteics (Lasix/furosemide, ], 1963),<ref>{{cite journal |author=Stason WB, Cannon PJ, Heinemann HO, Laragh JH |title=Furosemide. A clinical evaluation of its diuretic action |journal=Circulation |volume=34 |issue=5 |pages=910–20 |date=November 1966 |pmid=5332332 |doi= |url=}}</ref> ] (], 1964)<ref name="Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC 1964 1080–1081">{{cite journal|author=Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC |title=A new adrenergic betareceptor antagonist | journal=] |volume=283 |issue=7342 |pages=1080–1081 |year=1964 |pmid=14132613 |doi=10.1016/S0140-6736(64)91275-9}}</ref> ], and ]. ACE inhibitors reduce the risk of new onset kidney disease and death in diabetic patients, irrespective of whether they have hypertension.<ref>{{cite journal |author=Lv J, Perkovic V, Foote CV, Craig ME, Craig JC, Strippoli GF |title=Antihypertensive agents for preventing diabetic kidney disease |journal=Cochrane Database Syst Rev |volume=12 |issue= |pages=CD004136 |year=2012 |pmid=23235603 |doi=10.1002/14651858.CD004136.pub3 |url=}}</ref> | |||
| Numerous new drugs were developed during the 1950s and mass-produced and marketed through the 1960s. These included the first oral contraceptive, "The Pill", Cortisone, blood-pressure drugs and other heart medications. ]s, ] (Thorazine), ] (Haldol) and the tranquilizers ushered in the age of psychiatric medication. ] (Valium), discovered in 1960, was marketed from 1963 and rapidly became the most prescribed drug in history, prior to controversy over dependency and habituation. | Numerous new drugs were developed during the 1950s and mass-produced and marketed through the 1960s. These included the first oral contraceptive, "The Pill", Cortisone, blood-pressure drugs and other heart medications. ]s, ] (Thorazine), ] (Haldol) and the tranquilizers ushered in the age of psychiatric medication. ] (Valium), discovered in 1960, was marketed from 1963 and rapidly became the most prescribed drug in history, prior to controversy over dependency and habituation. | ||
| ====Thalidomide and the Kefauver-Harris Amendments==== | |||
| Attempts were made to increase regulation and to limit financial links between companies and prescribing physicians, including by the relatively new ] (FDA). Such calls increased in the 1960s after the ] tragedy came to light, in which the use of a new anti-emetic in pregnant women caused severe birth defects. In 1964, the World Medical Association issued its ], which set standards for clinical research and demanded that subjects give their informed consent before enrolling in an experiment. Pharmaceutical companies became required to prove ] in clinical trials before marketing drugs. | |||
| ] | |||
| In the U.S., a push for revisions of the FD&C Act emerged from Congressional hearings led by Senator ] of Tennessee in 1959. The hearings covered a wide range of policy issues, including advertising abuses, questionable efficacy of drugs, and the need for greater regulation of the industry. While momentum for new legislation temporarily flagged under extended debate, a new tragedy became apparent that underscored the need for more comprehensive regulation and provided the driving force for the passage of new laws. | |||
| On September 12, 1960, an American licensee, the William S. Merrell Company of Cincinnati, submitted to FDA a new drug application for Kevadon (]), the brand name of a sedative that had been marketed in Europe since 1956: thalidomide. The FDA medical officer in charge of this review, ], believed the data were incomplete to support the safety of this drug. | |||
| The firm continued to pressure Kelsey and the agency to approve the application—until November 1961, when the drug was pulled off the German market because of its association with grave congenital abnormalities. Several thousand newborns in Europe and elsewhere suffered the teratogenic effects of thalidomide. Though the drug was never approved in this country, the firm distributed Kevadon to over 1,000 physicians under the guise of investigational use. Over 20,000 Americans received thalidomide in this "study," including 624 pregnant patients, and about 17 known newborns suffered the effects of the drug. | |||
| The thalidomide tragedy resurrected Kefauver's bill to enhance drug regulation that had stalled in Congress, and the ] became law on October 10, 1962. Manufacturers henceforth had to prove to FDA that their drugs were effective as well as safe before they could go on the market. FDA received authority to regulate advertising of prescription drugs and to establish ]. Finally, the law required that all drugs introduced between 1938 and 1962 had to be effective. An FDA - National Academy of Sciences collaborative study showed that nearly 40 percent of these products were not effective. A similarly comprehensive study of over-the-counter products began ten years later.<ref>{{cite web |url=http://www.fda.gov/AboutFDA/WhatWeDo/History/FOrgsHistory/CDER/CenterforDrugEvaluationandResearchBrochureandChronology/ucm114470.htm#1951 |title=Brochure: The History of Drug Regulation in the United States |format= |work= |accessdate=}}</ref> | |||
| ===1970-1980=== | |||
| Cancer drugs were a feature of the 1970s. From 1978, India took over as the primary center of pharmaceutical production without patent protection.<ref>{{cite book | url = http://www.dklevine.com/papers/ip.ch.9.m1004.pdf | author = Boldrin & Levine | title = Against Intellectual Monopoly | chapter = 9}}</ref> | Cancer drugs were a feature of the 1970s. From 1978, India took over as the primary center of pharmaceutical production without patent protection.<ref>{{cite book | url = http://www.dklevine.com/papers/ip.ch.9.m1004.pdf | author = Boldrin & Levine | title = Against Intellectual Monopoly | chapter = 9}}</ref> | ||
| Line 20: | Line 82: | ||
| The pharmaceutical industry entered the 1980s pressured by economics and a host of new regulations, both safety and environmental, but also transformed by new DNA chemistries and new technologies for analysis and computation.{{Citation needed|date=September 2007}} Drugs for heart disease and for AIDS were a feature of the 1980s, involving challenges to regulatory bodies and a faster approval process. | The pharmaceutical industry entered the 1980s pressured by economics and a host of new regulations, both safety and environmental, but also transformed by new DNA chemistries and new technologies for analysis and computation.{{Citation needed|date=September 2007}} Drugs for heart disease and for AIDS were a feature of the 1980s, involving challenges to regulatory bodies and a faster approval process. | ||
| ===1980-Today=== | |||
| ] and ]s (HMOs) spread during the 1980s as part of an effort to contain rising medical costs, and the development of preventative and maintenance medications became more important. A new business atmosphere became institutionalized in the 1990s, characterized by mergers and takeovers, and by a dramatic increase in the use of contract research organizations for clinical development and even for basic R&D. The pharmaceutical industry confronted a new business climate and new regulations, born in part from dealing with world market forces and protests by activists in developing countries. ] activism was also a challenge. | |||
| Controversies emerged around adverse effects, notably regarding ] in the US, and marketing tactics. Pharmaceutical companies became increasingly accused of ] or over-medicalizing personal or social problems.<ref name="Moynihan">Ray Moynihan and Alan Cassels (2005). ''Selling Sickness: How Drug Companies are Turning Us All Into Patients''. Allen & Unwin. New York. ISBN 1-74114-579-1</ref> | |||
| Marketing changed dramatically in the 1990s. The Internet made possible the direct purchase of medicines by drug consumers and of raw materials by drug producers, transforming the nature of business. In the US, Direct-to-consumer advertising proliferated on radio and TV because of new FDA regulations in 1997 that liberalized requirements for the presentation of risks. The new antidepressants, the SSRIs, notably ] (Prozac), rapidly became bestsellers and marketed for additional disorders. | |||
| Since 2008, pharmaceutical companies have been increasing the cost of name-brand prescriptions to offset declining revenues as out-of-patent drugs become available as generics.<ref> ''The Incidental Economist'' November 29, 2012</ref> Simultaneously, pharmaceutical manufacturers are taking increasing advantage of ]s to avoid taxation.<ref> ''Wall Street Journal'', February 6, 2013</ref> | |||
| Drug development progressed from a hit-and-miss approach to rational drug discovery in both laboratory design and natural-product surveys. Demand for nutritional supplements and so-called alternative medicines created new opportunities and increased competition in the industry. Controversies emerged around adverse effects, notably regarding ] in the US, and marketing tactics. Pharmaceutical companies became increasingly accused of ] or over-medicalizing personal or social problems.<ref name="Moynihan">Ray Moynihan and Alan Cassels (2005). ''Selling Sickness: How Drug Companies are Turning Us All Into Patients''. Allen & Unwin. New York. ISBN 1-74114-579-1</ref> | |||
| ==Research and development== | ==Research and development== | ||
| Line 32: | Line 94: | ||
| '''Drug development''' refers to activities undertaken after a compound is identified as a potential drug in order to establish its suitability as a medication. Objectives of drug development are to determine appropriate ] and ], as well as to establish ]. Research in these areas generally includes a combination of '']'' studies, '']'' studies, and ]. The amount of capital required for late stage development has made it a historical strength of the larger pharmaceutical companies.<ref>{{cite journal | publisher = Tufts Center for the Study of Drug Development | title = Annual Impact Report | url = http://csdd.tufts.edu}}</ref> | '''Drug development''' refers to activities undertaken after a compound is identified as a potential drug in order to establish its suitability as a medication. Objectives of drug development are to determine appropriate ] and ], as well as to establish ]. Research in these areas generally includes a combination of '']'' studies, '']'' studies, and ]. The amount of capital required for late stage development has made it a historical strength of the larger pharmaceutical companies.<ref>{{cite journal | publisher = Tufts Center for the Study of Drug Development | title = Annual Impact Report | url = http://csdd.tufts.edu}}</ref> | ||
| Often, large multinational corporations exhibit ], participating in a broad range of drug discovery and development, manufacturing and quality control, marketing, sales, and distribution. Smaller organizations, on the other hand, often focus on a specific aspect such as discovering drug candidates or developing formulations. Often, collaborative agreements between research organizations and large pharmaceutical companies are formed to explore the potential of new drug substances. More recently, multi-nationals are increasingly relying on contract research organizations to manage drug development.<ref>http://www.outsourcing-pharma.com/Clinical-Development/Pfizer-teams-with-Parexel-and-Icon-in-CRO-sector-s-latest-strategic-deals |
Often, large multinational corporations exhibit ], participating in a broad range of drug discovery and development, manufacturing and quality control, marketing, sales, and distribution. Smaller organizations, on the other hand, often focus on a specific aspect such as discovering drug candidates or developing formulations. Often, collaborative agreements between research organizations and large pharmaceutical companies are formed to explore the potential of new drug substances. More recently, multi-nationals are increasingly relying on contract research organizations to manage drug development.<ref>http://www.outsourcing-pharma.com/Clinical-Development/Pfizer-teams-with-Parexel-and-Icon-in-CRO-sector-s-latest-strategic-deals</ref> | ||
| ===The cost of innovation=== | ===The cost of innovation=== | ||
| Drug companies are like other companies in that they manufacture products that must be sold for a profit in order for the company to survive and grow. They are different from some companies because the ] business is very risky. For instance, only one out of every ten thousand discovered compounds actually becomes an approved drug for sale. Much expense is incurred in the early phases of development of compounds that will not become approved ].<ref name="Why Drugs Cost So Much">{{cite web |url=http://www.medicinenet.com/script/main/art.asp?articlekey=18892 |title=Why Drugs Cost So Much|publisher=Medicine.net}}</ref> | |||
| In addition, it takes about 7 to 10 years and only 3 out of every 20 approved ] bring in sufficient revenue to cover their developmental costs, and only 1 out of every 3 approved drugs generates enough money to cover the development costs of previous failures. This means that for a drug company to survive, it needs to discover a blockbuster (billion-dollar drug) every few years.<ref name="Why Drugs Cost So Much"/> | |||
| ] discovery and development is very expensive; of all compounds investigated for use in humans only a small fraction are eventually ] in most nations by government appointed medical institutions or boards, who have to approve new ] before they can be marketed in those countries. In 2010 18 NMEs (New Molecular Entities) were approved and three biologics by the FDA, or 21 in total, which is down from 26 in 2009 and 24 in 2008. On the other hand, there were only 18 approvals in total in 2007 and 22 back in 2006. Since 2001, the Center for Drug Evaluation and Research has averaged 22.9 approvals a year.<ref>{{cite web |url=http://www.pharmalot.com/2011/02/how-many-new-drugs-did-fda-approve-last-year/ |title=How Many New Drugs Did FDA Approve Last Year?|publisher=pharmalot.com}}</ref> | ] discovery and development is very expensive; of all compounds investigated for use in humans only a small fraction are eventually ] in most nations by government appointed medical institutions or boards, who have to approve new ] before they can be marketed in those countries. In 2010 18 NMEs (New Molecular Entities) were approved and three biologics by the FDA, or 21 in total, which is down from 26 in 2009 and 24 in 2008. On the other hand, there were only 18 approvals in total in 2007 and 22 back in 2006. Since 2001, the Center for Drug Evaluation and Research has averaged 22.9 approvals a year.<ref>{{cite web |url=http://www.pharmalot.com/2011/02/how-many-new-drugs-did-fda-approve-last-year/ |title=How Many New Drugs Did FDA Approve Last Year?|publisher=pharmalot.com}}</ref> | ||
| This approval comes only after heavy investment in ] and ]s, as well as a commitment to ongoing ]. Drugs which fail part-way through this process often incur large costs, while generating no revenue in return. If the cost of these failed drugs is taken into account, the cost of developing a successful new drug (] or NCE), has been estimated at about 1.3 billion USD<ref></ref>(not including ]). Professors Light and Lexchin reported in 2012, however, that the rate of approval for new drugs has been a relatively stable average rate of 15 to 25 for decades.<ref name=Perry>{{cite news|author=Perry, Susan|title=Donald Light and Joel Lexchin in BMJ 2012;345:e4348, quoted in: Big Pharma's claim of an 'innovation crisis' is a myth, BMJ authors say|url=http://www.minnpost.com/second-opinion/2012/08/big-pharmas-claim-innovation-crisis-myth-bmj-authors-say|date=August 8, 2012|publisher=MinnPost|accessdate=August 8, 2012}}</ref> | This approval comes only after heavy investment in ] and ]s, as well as a commitment to ongoing ]. Drugs which fail part-way through this process often incur large costs, while generating no revenue in return. If the cost of these failed drugs is taken into account, the cost of developing a successful new drug (], or NCE), has been estimated at about 1.3 billion USD<ref></ref>(not including ]). Professors Light and Lexchin reported in 2012, however, that the rate of approval for new drugs has been a relatively stable average rate of 15 to 25 for decades.<ref name=Perry>{{cite news|author=Perry, Susan|title=Donald Light and Joel Lexchin in BMJ 2012;345:e4348, quoted in: Big Pharma's claim of an 'innovation crisis' is a myth, BMJ authors say|url=http://www.minnpost.com/second-opinion/2012/08/big-pharmas-claim-innovation-crisis-myth-bmj-authors-say|date=August 8, 2012|publisher=MinnPost|accessdate=August 8, 2012}}</ref> | ||
| Industry-wide research and investment reached a record $65.3 billion in 2009.<ref name="Press release"></ref> While the cost of research in the U.S. was about {{dollarsign|$}}34.2 billion between 1995 and 2010, revenues rose faster (revenues rose by {{dollarsign|$}}200.4 billion in that time).<ref name=Perry /> | Industry-wide research and investment reached a record $65.3 billion in 2009.<ref name="Press release"></ref> While the cost of research in the U.S. was about {{dollarsign|$}}34.2 billion between 1995 and 2010, revenues rose faster (revenues rose by {{dollarsign|$}}200.4 billion in that time).<ref name=Perry /> | ||
| A study by the consulting firm ] reported that the cost for discovering, developing and launching (which factored in marketing and other business expenses) a new drug (along with the prospective drugs that fail) rose over a five-year period to nearly $1.7 billion in 2003.<ref name=autogenerated1>''Has the Pharmaceutical Blockbuster Model Gone Bust?'', ] press release, December 8, 2003. </ref> According to Forbes, development costs between $4 billion to $11 billion per drug.<ref>{{cite |
A study by the consulting firm ] reported that the cost for discovering, developing and launching (which factored in marketing and other business expenses) a new drug (along with the prospective drugs that fail) rose over a five-year period to nearly $1.7 billion in 2003.<ref name=autogenerated1>''Has the Pharmaceutical Blockbuster Model Gone Bust?'', ] press release, December 8, 2003. </ref> According to Forbes, development costs between $4 billion to $11 billion per drug.<ref>{{cite news | url = http://www.forbes.com/sites/matthewherper/2012/02/10/the-truly-staggering-cost-of-inventing-new-drugs/ | title = The Truly Staggering Cost Of Inventing New Drugs | date = 2012-02-10 | author = Matthew Harper | work=Forbes}}</ref> | ||
| Some of these estimates also take into account the ] of investing capital many years before revenues are realized (see ]). Because of the very long time needed for discovery, development, and approval of pharmaceuticals, these costs can accumulate to nearly half the total expense. Some approved drugs, such as those based on re-formulation of an existing ] (also referred to as Line-extensions) are much less expensive to develop. | |||
| Calculations and claims in this area are controversial because of the implications for regulation and ] of the industry through tax credits and federally funded research grants.<ref name="cbo">{{cite web |url=http://www.cbo.gov/doc.cfm?index=8221&type=0 |title=Federal Support for Research and Development |publisher=] |date=June 2007 |author=Sheila Campbell, et al}}</ref> | |||
| ==="Me-too" drugs=== | |||
| Competition between pharmaceutical companies has resulted in "me-too" drugs, which are defined as chemically-similar compounds or compounds with the same ] as an existing, approved chemical entity.<ref>{{Cite journal | last1 = Garattini | first1 = S. | author1-link = | title = Are me-too drugs justificed? | journal = Journal of Nephrology | volume = 10 | issue = 6 | pages = 283–294 | publisher = | location = | date = | year = 1997 | pmid = 9442441 | issn = | doi = | postscript = <!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}} }}</ref> Much of the “me-too” drug phenomenon is actually a result of independent parallel research at rival companies.<ref>{{cite web |url=http://www.economist.com/blogs/freeexchange/2007/04/me_too_me_too|title=Me too! Me too! |publisher=The Economist |date=17 April 2007}}</ref><ref>{{Cite journal | last1 = DiMasi | first1 = JA | last2 = Faden | first2= LD | title = Competitiveness in follow-on drug R&D: a race or imitation? | journal = Nature Reviews Drug Discovery | volume = 10 | issue = 1 | pages = 23–27 | publisher = | location = | date = January 2011 | url = http://www.nature.com/nrd/journal/v10/n1/full/nrd3296.html | issn = | doi =10.1038/nrd3296 | pmid = 21151030 | postscript = <!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}} }}</ref> It may take 10 or more years for a drug to go from discovery to FDA approval, and if a new ] is discovered, multiple companies often will simultaneously develop a drug treatment within this pathway, leading to several similar drugs arriving on the market within a short period of time.<ref>{{cite web |url=http://www.nejm.org/doi/full/10.1056/NEJM200405133502019#t=article| title=Correspondence: "Me-Too" Products – Friend or Foe? |publisher=The New England Journal of Medicine |date=13 May 2004}}</ref> | |||
| Critics of the pharmaceutical industry suggest that "me-too" drugs are only brought to market because their development is cheaper and less risky than drugs with a novel mechanism of action.<ref>{{Cite journal | last1 = Angel | first1 = Marcia | author1-link = Marcia Angel | title = Excess in the pharmaceutical industry | journal = Canadian Medical Association Journal | volume = 171 | issue = 12 | pages = 1451–3| publisher = | location = | date = 7 December 2004 | url = http://www.cmaj.ca/cgi/content/full/171/12/1451#R5-12 | issn = | doi = 10.1503/cmaj.1041594 | pmid = 15583183 | pmc = 534578 | postscript = <!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}} }}</ref> However, proponents point to the cost benefits of market competition between similar drugs. When a second drug arrives on the market, the manufacturer of the first drug no longer has a monopoly, and the resulting competition puts a downward pressure on pricing.<ref name="Lee2004">{{cite journal | doi = 10.1056/NEJMp038215 | title = "Me-Too" Products — Friend or Foe? | year = 2004 | last1 = Lee | first1 = Thomas H. | journal = New England Journal of Medicine | volume = 350 | issue = 3 | pages = 211–2 | pmid = 14724297}}</ref> To be approved by the FDA, second and third entrants also need to offer advantages over the existing therapy, such as fewer side effects or more convenient dose schedules.<ref name="Lee2004" /> | |||
| ===Controversies=== | ===Controversies=== | ||
| Due to repeated accusations and findings that some clinical trials conducted or funded by pharmaceutical companies may report only positive results for the preferred medication, the industry has been looked at much more closely by independent groups and government agencies.<ref>{{Cite web|url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=retrieve&db=pubmed&list_uids=14970094&dopt=Abstract|title=Association between industry funding and statistically significant pro-industry findings in medical and surgical randomized trials|publisher=|author=Bhandari M, Busse JW, Jackowski D, Montori VM, Schunemann H, Sprague S, Mears D, Schemitsch EH, Heels-Ansdell D, Devereaux PJ|date=2004-02-17|accessdate=2007-05-24}}</ref><ref>Ben Goldacre: The Guardian, 2012.</ref> | Due to repeated accusations and findings that some clinical trials conducted or funded by pharmaceutical companies may report only positive results for the preferred medication, the industry has been looked at much more closely by independent groups and government agencies.<ref>{{Cite web|url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=retrieve&db=pubmed&list_uids=14970094&dopt=Abstract|title=Association between industry funding and statistically significant pro-industry findings in medical and surgical randomized trials|publisher=|author=Bhandari M, Busse JW, Jackowski D, Montori VM, Schunemann H, Sprague S, Mears D, Schemitsch EH, Heels-Ansdell D, Devereaux PJ|date=2004-02-17|accessdate=2007-05-24}}</ref><ref>Ben Goldacre: The Guardian, 2012.</ref> | ||
| In response to specific cases in which unfavorable data from pharmaceutical company-sponsored research was not published, the ] have published new guidelines urging companies to report all findings and limit the financial involvement in drug companies of researchers.<ref name="moynihanbmj"/> US congress signed into law a bill which requires phase II and phase III clinical trials to be ] by the sponsor on the website run by the NIH.<ref>{{Cite web|url=http://www.hhlaw.com/files/Publication/edbf3429-125c-41c9-9442-b552e69b756c/Presentation/PublicationAttachment/972a9053-8c8d-46e4-ac96-ecf4892a8643/Pharma.pdf |format=PDF|title=Hogan & Hartson Update on Pharmaceutical Trial Registration |accessdate=2008-06-02 |publisher= |date=2008-03-03}}</ref> | In response to specific cases in which unfavorable data from pharmaceutical company-sponsored research was not published, the ] have published new guidelines urging companies to report all findings and limit the financial involvement in drug companies of researchers.<ref name="moynihanbmj">Moynihan R (]). . ''BMJ: British Medical Journal''. Volume 326, Issue 7400, Pages 1193–1196. Retrieved on 2007-10-06.</ref> US congress signed into law a bill which requires phase II and phase III clinical trials to be ] by the sponsor on the website run by the NIH.<ref>{{Cite web|url=http://www.hhlaw.com/files/Publication/edbf3429-125c-41c9-9442-b552e69b756c/Presentation/PublicationAttachment/972a9053-8c8d-46e4-ac96-ecf4892a8643/Pharma.pdf |format=PDF|title=Hogan & Hartson Update on Pharmaceutical Trial Registration |accessdate=2008-06-02 |publisher= |date=2008-03-03}}</ref> | ||
| Drug researchers not directly employed by pharmaceutical companies often look to companies for grants, and companies often look to researchers for studies that will make their products look favorable. Sponsored researchers are rewarded by drug companies, for example with support for their conference/symposium costs. Lecture scripts and even journal articles presented by academic researchers may actually be |
Drug researchers not directly employed by pharmaceutical companies often look to companies for grants, and companies often look to researchers for studies that will make their products look favorable. Sponsored researchers are rewarded by drug companies, for example with support for their conference/symposium costs. Lecture scripts and even journal articles presented by academic researchers may actually be "ghost-written" by pharmaceutical companies.<ref>{{Cite news|url=http://observer.guardian.co.uk/uk_news/story/0,6903,1101680,00.html|title=Revealed: how drug firms 'hoodwink' medical journals|publisher=]|author=Barnett, Antony|date=2003-12-07|accessdate=2007-05-24 | location=London}}</ref> | ||
| Researchers who have tried to reveal ethical issues with clinical trials, or publish papers showing harmful effects of drugs – and who saw themselves as ]s – have faced or been threatened with lawsuits from drug companies, or have lost their jobs.<ref>]. '']''. Fourth Estate, 2012, p. 345: "In the UK, whistleblowers are sacked and silenced." | |||
| * For a notable example in the United States, see Petersen, Melody. , ''The New York Times'', March 12, 2003, p. 2: | |||
| :*He (])<!--note:square brackets not working because of link--> said he felt threatened when at least one executive told him that if he talked publicly about the company's marketing he would be made a scapegoat and be described as a rogue employee in a company that played by the rules." | |||
| * For other examples, see {{cite journal|title=What Can We Learn from Medical Whistleblowers?|author= Lenzer, Jeanne|date=2005-05-27|volume=2|issue=7|pages=e209|doi=10.1371/journal.pmed.0020209|journal=PLoS medicine|pmid=15913416|pmc=1140678}}: | |||
| :*"Whistleblowers have been compared to bees—they have just one sting to use and using it may lead to career suicide . Many of the whistleblowers at the roundtable said they had experienced retaliation from their employers for raising concerns, but all had felt obligated to speak out about practices in medicine and medical research that they believe are risking the public's health or safety." | |||
| :*" Jones ... wouldn't back down from his investigation, he said, and was demoted. On November 22, 2002, he filed a civil rights lawsuit 'to preserve my job and my right to speak out.' His employer, he said, took him off investigative duties altogether." | |||
| :*"Stefan Kruszewski, who has filed a law suit in a federal court in Pennsylvania, raised concerns to his seniors in the Pennsylvania Department of Public Welfare about prescribing practices in the state that he did not feel were evidence based, and said he lost his job for raising his concerns."</ref> For example, Dutch medical researcher Dr. Koos Stiekema was sued by the pharmaceutical company ] for violating his confidentiality agreement, after he discussed his concerns about a clinical trial design with three ethics committees in 1999. Organon's other experts agreed that the trial design was safe, and a court in Amsterdam awarded Organon ₤550,000 for the trial-delay costs that resulted from Stiekema's disclosures.<ref>{{cite journal|title=How whistleblowing cost one doctor £550000|publisher=|date=2002-05-25|pmc=1123215|volume=324|issue=7348|pmid=12028975|last1=Sheldon|first1=T|pages=1240|journal=BMJ (Clinical research ed.)|doi=10.1136/bmj.324.7348.1240}}</ref> The award was overturned on appeal; the court ruled that Stiekema's breach of confidentiality was "justified by a higher interest."<ref>Faunce, Thomas Alured. ''Pilgrims in Medicine: Conscience, Legalism and Human Rights''. Martinus Nijhoff Publishers, 2005, .</ref> In the United States, corporate whistleblowers are given a percentage of any fines levied.<ref>Goldacre 2012, p. 344.</ref> | |||
| Since 2008, pharmaceutical companies have been increasing the cost of name-brand prescriptions to offset declining revenues as out-of-patent drugs become available as generics.<ref> ''The Incidental Economist'' November 29, 2012</ref> Simultaneously, pharmaceutical manufacturers are taking increasing advantage of ]s to avoid taxation.<ref> ''Wall Street Journal'', February 6, 2013</ref> | |||
| An investigation by ] found that at least 21 doctors have been paid more than $500,000 for speeches and consulting by drugs manufacturers since 2009, with half of the top earners working in ], and about $2 billion in total paid to doctors for such services. ], ] and ] have paid billions of dollars in federal settlements over allegations that they paid doctors to promote drugs for unapproved uses. Some prominent medical schools have since tightened rules on faculty acceptance of such payments by drug companies.<ref>Tracy Weber and Charles Ornstein (March 11, 2013) ''ProPublica''</ref> | An investigation by ] found that at least 21 doctors have been paid more than $500,000 for speeches and consulting by drugs manufacturers since 2009, with half of the top earners working in ], and about $2 billion in total paid to doctors for such services. ], ] and ] have paid billions of dollars in federal settlements over allegations that they paid doctors to promote drugs for unapproved uses. Some prominent medical schools have since tightened rules on faculty acceptance of such payments by drug companies.<ref>Tracy Weber and Charles Ornstein (March 11, 2013) ''ProPublica''</ref> | ||
| Line 76: | Line 119: | ||
| {{Main|Food and Drug Administration}} | {{Main|Food and Drug Administration}} | ||
| In the ], new pharmaceutical products must be approved by the ] (FDA) as being both safe and effective. This process generally involves submission of an ] filing with sufficient pre-clinical data to support proceeding with human trials. Following IND approval, three phases of progressively larger human clinical trials may be conducted. Phase I generally studies ] using healthy volunteers. Phase II can include ] and ] in patients, and Phase III is a very large study of efficacy in the intended patient population. Following the successful completion of phase III testing, a ] is submitted to the FDA. The FDA review the data and if the product is seen as having a positive benefit-risk assessment, approval to market the product in the US is granted.<ref name="standard2011">{{cite journal |author=Liberti L, McAuslane JN, Walker S |title=Standardizing the Benefit-Risk Assessment of New Medicines: Practical Applications of Frameworks for the Pharmaceutical Healthcare Professional | In the ], new pharmaceutical products must be approved by the ] (FDA) as being both safe and effective. This process generally involves submission of an ] filing with sufficient pre-clinical data to support proceeding with human trials. Following IND approval, three phases of progressively larger human clinical trials may be conducted. Phase I generally studies ] using healthy volunteers. Phase II can include ] and ] in patients, and Phase III is a very large study of efficacy in the intended patient population. Following the successful completion of phase III testing, a ] is submitted to the FDA. The FDA review the data and if the product is seen as having a positive benefit-risk assessment, approval to market the product in the US is granted.<ref name="standard2011">{{cite journal |author=Liberti L, McAuslane JN, Walker S |title=Standardizing the Benefit-Risk Assessment of New Medicines: Practical Applications of Frameworks for the Pharmaceutical Healthcare Professional | ||
| |url=http://adisonline.com/pharmaceuticalmedicine/Abstract/2011/25030/Standardizing_the_Benefit_Risk_Assessment_of_New.1.aspx |journal=Pharm Med |volume=25 |issue=3 |pages=139–46 |year=2011 |doi=10.1007/BF03256855}}</ref> | |url=http://adisonline.com/pharmaceuticalmedicine/Abstract/2011/25030/Standardizing_the_Benefit_Risk_Assessment_of_New.1.aspx |journal=Pharm Med |volume=25 |issue=3 |pages=139–46 |year=2011 |doi=10.1007/BF03256855}}</ref> | ||
| A fourth phase of post-approval surveillance is also often required due to the fact that even the largest clinical trials cannot effectively predict the prevalence of rare side-effects. ] ensures that after marketing the safety of a drug is monitored closely. In certain instances, its indication may need to be limited to particular patient groups, and in others the substance is withdrawn from the market completely. |
A fourth phase of post-approval surveillance is also often required due to the fact that even the largest clinical trials cannot effectively predict the prevalence of rare side-effects. ] ensures that after marketing the safety of a drug is monitored closely. In certain instances, its indication may need to be limited to particular patient groups, and in others the substance is withdrawn from the market completely. | ||
| The FDA provides information about approved drugs at the Orange Book site.<ref>{{Cite web|url=http://www.fda.gov/cder/ob/default.htm|title=Electronic Orange Book|publisher=U.S. Food and Drug Administration|accessdate=2007-05-31}}</ref> | The FDA provides information about approved drugs at the Orange Book site.<ref>{{Cite web|url=http://www.fda.gov/cder/ob/default.htm|title=Electronic Orange Book|publisher=U.S. Food and Drug Administration|accessdate=2007-05-31}}</ref> | ||
| Line 97: | Line 140: | ||
| ==Industry revenues== | ==Industry revenues== | ||
| <ref>http://www.imshealth.com/deployedfiles/ims/Global/Content/Corporate/Press%20Room/Top-Line%20Market%20Data%20&%20Trends/2011%20Top-line%20Market%20Data/Regional_Pharma_Market_by_Spending_2011-2016.pdf</ref> | <ref>http://www.imshealth.com/deployedfiles/ims/Global/Content/Corporate/Press%20Room/Top-Line%20Market%20Data%20&%20Trends/2011%20Top-line%20Market%20Data/Regional_Pharma_Market_by_Spending_2011-2016.pdf</ref> | ||
| For the first time ever, in 2011, global spending on prescription drugs topped $954 billion, even as growth slowed somewhat in Europe and North America. The United States accounts for more than a third of the global pharmaceutical market, with $340 billion in annual sales followed by the EU and Japan. Emerging markets such as China, Russia, South Korea and Mexico outpaced that market, growing a huge 81 percent.<ref name='forbes-10'/> According to IMS the global pharmaceutical industry can reach to US$1.1 trillion by 2014.<ref>http://www.imshealth.com/portal/site/ims/menuitem.d248e29c86589c9c30e81c033208c22a/?vgnextoid=4b8c410b6c718210VgnVCM100000ed152ca2RCRD</ref> | For the first time ever, in 2011, global spending on prescription drugs topped $954 billion, even as growth slowed somewhat in Europe and North America. The United States accounts for more than a third of the global pharmaceutical market, with $340 billion in annual sales followed by the EU and Japan. Emerging markets such as China, Russia, South Korea and Mexico outpaced that market, growing a huge 81 percent.<ref name='forbes-10'>{{Cite news|url=http://www.forbes.com/home/sciencesandmedicine/2006/03/21/pfizer-merck-amgen-cx_mh_pk_0321topdrugs.html|title=The World's Ten Best-Selling Drugs|author=Herper, Matthew and Kang, Peter|publisher=]|date=2006-03-22|accessdate=2007-05-31}}</ref> According to IMS the global pharmaceutical industry can reach to US$1.1 trillion by 2014.<ref>http://www.imshealth.com/portal/site/ims/menuitem.d248e29c86589c9c30e81c033208c22a/?vgnextoid=4b8c410b6c718210VgnVCM100000ed152ca2RCRD</ref> | ||
| The top ten best-selling drugs of 2013 totaled $75.6 billion in sales, with the anti-inflammatory drug ] being the best-selling drug world wide at $10.7 billion in sales. The second and third best selling were Enbrel and Remicade, respectively.<ref>http://www.theguardian.com/business/2014/mar/27/bestselling-prescription-drugs</ref> The top three best-selling drugs in the United States in 2013 were Abilify ($6.3 billion,) Nexium ($6 billion) and Humira ($5.4 billion).<ref>http://www.drugs.com/stats/top100/2013/sales</ref> The best-selling drug ever, Lipitor, averaged $13 billion annually and netted $141 billion total over its lifetime before Pfizer's patent expired in November 2011. | |||
| Pfizer's cholesterol pill ] remains a best-selling drug world wide.{{dubious|date=August 2013}}{{Update inline|date=August 2013}} Its ] were $12.9 billion, more than twice as much as its closest competitors: ], the blood thinner from Bristol-Myers Squibb and Sanofi-Aventis; ], the heartburn pill from AstraZeneca; and ], the asthma inhaler from GlaxoSmithKline.<ref name='forbes-10'>{{Cite web|url=http://www.forbes.com/home/sciencesandmedicine/2006/03/21/pfizer-merck-amgen-cx_mh_pk_0321topdrugs.html|title=The World's Ten Best-Selling Drugs|author=Herper, Matthew and Kang, Peter|publisher=]|date=2006-03-22|accessdate=2007-05-31}}</ref> | |||
| ] publishes an analysis of trends expected in the pharmaceutical industry in 2007, including increasing profits in most sectors despite loss of some patents, and new 'blockbuster' drugs on the horizon.<ref>{{Cite web|url=http://www.imshealth.com/ims/portal/front/articleC/0,2777,6025_3665_79210022,00.html|title=IMS Health Forecasts 5 to 6 Percent Growth for Global Pharmaceutical Market in 2007|publisher=IMS Health|date=2006-10-24|accessdate=2007-06-19}}</ref> | ] publishes an analysis of trends expected in the pharmaceutical industry in 2007, including increasing profits in most sectors despite loss of some patents, and new 'blockbuster' drugs on the horizon.<ref>{{Cite web|url=http://www.imshealth.com/ims/portal/front/articleC/0,2777,6025_3665_79210022,00.html|title=IMS Health Forecasts 5 to 6 Percent Growth for Global Pharmaceutical Market in 2007|publisher=IMS Health|date=2006-10-24|accessdate=2007-06-19}}</ref> | ||
| ''Teradata Magazine'' predicted that by 2007, $40 billion in U.S. sales could be lost at the top 10 pharmaceutical companies as a result of slowdown in R&D innovation and the expiry of patents on major products, with 19 blockbuster drugs losing patent.<ref>{{Cite web|url=http://www.teradata.com/t/page/131951/|title=Prescription for change|publisher=Teradata Magazine online|date=March 2005|accessdate=2007-06-19 |archiveurl = http://web.archive.org/web/20070928024747/http://www.teradata.com/t/page/131951/ |archivedate = 2007-09-28}}</ref> As the number of patents that expire accumulates faster than the number of marketed drugs, this amount is expected to increase even more in the near future.<ref>{{Cite |
''Teradata Magazine'' predicted that by 2007, $40 billion in U.S. sales could be lost at the top 10 pharmaceutical companies as a result of slowdown in R&D innovation and the expiry of patents on major products, with 19 blockbuster drugs losing patent.<ref>{{Cite web|url=http://www.teradata.com/t/page/131951/|title=Prescription for change|publisher=Teradata Magazine online|date=March 2005|accessdate=2007-06-19 |archiveurl = http://web.archive.org/web/20070928024747/http://www.teradata.com/t/page/131951/ |archivedate = 2007-09-28}}</ref> As the number of patents that expire accumulates faster than the number of marketed drugs, this amount is expected to increase even more in the near future.<ref>{{Cite news|url=http://www.nytimes.com/2011/03/07/business/07drug.html?pagewanted=all&_r=0|title= Drug Firms Face Billions in Losses in '11 as Patents End|publisher=NY Times | first=Duff|last=Wilson|date=2011-03-06}}</ref><ref>{{Cite web|url=http://www.uspharmacist.com/content/s/216/c/35249/|title=Drug Patent Expirations and the "Patent Cliff"|publisher=US Pharmacist}}</ref> | ||
| Drug Firms Face Billions in Losses in ’11 as Patents End|publisher=NY Times}}</ref><ref>{{Cite web|url=http://www.uspharmacist.com/content/s/216/c/35249/|title=Drug Patent Expirations and the "Patent Cliff"|publisher=US Pharmacist}}</ref> | |||
| ===Market leaders in terms of healthcare revenue=== | |||
| {{update|date=May 2013}} | |||
| {{Main|List of pharmaceutical companies}} | |||
| The following is a list of the 20 largest ] and ] companies ranked by healthcare revenue. Some companies (e.g., ], ] and ]) have additional revenue not included here. The phrase '''Big pharma''' is often used to refer to companies with revenue in excess of $3 billion, and/or ] expenditure in excess of $500 million. | |||
| {{Clear}} | |||
| {|class="sortable wikitable" | |||
| !Revenue <br /> | |||
| Rank <br /> | |||
| 2008<ref>''Top 50 Pharmaceutical Companies Charts & Lists'', </ref> | |||
| !Company | |||
| !Country | |||
| !width=100|Total Revenues <small>(USD millions)</small> | |||
| !width=100|Healthcare R&D 2006 <small>(USD millions)</small> | |||
| !width=100|Net income/ (loss) 2006 <small>(USD millions)</small> | |||
| !width=100|Employees 2006 | |||
| |- | |||
| |align=center|1||]||USA||align=right|67,809||align=right|7,599||align=right|19,337||align=right|122,200 | |||
| |- | |||
| |align=center|2||]||]||align=right|53,324||align=right|7,125||align=right|11,053||align=right|138,000 | |||
| |- | |||
| |align=center|3||]||USA||align=right|45,987||align=right|4,783||align=right|4,434||align=right|74,372 | |||
| |- | |||
| |align=center|4||]||]||align=right|44,200||align=right|1,791||align=right|6,450||align=right|106,200 | |||
| |- | |||
| |align=center|5||]||]||align=right|42,813||align=right|6,373||align=right|10,135||align=right|106,000 | |||
| |- | |||
| |align=center|6||]||]||align=right|37,020||align=right|5,349||align=right|7,202||align=right|102,695 | |||
| |- | |||
| |align=center|7||]||]||align=right|35,645||align=right|5,565||align=right|5,033||align=right|100,735 | |||
| |- | |||
| |align=center|8||]||]||align=right|33,547||align=right|5,258||align=right|7,318||align=right|100,289 | |||
| |- | |||
| |align=center|9||]||United Kingdom||align=right|26,475||align=right|3,902||align=right|6,063||align=right|50,000+ | |||
| |- | |||
| |align=center|10||]||USA||align=right|22,476||align=right|2,255||align=right|1,717||align=right|66,800 | |||
| |- | |||
| |align=center|11||]||USA||align=right|17,914||align=right|3,067||align=right|1,585||align=right|60,000 | |||
| |- | |||
| |align=center|12||]||USA||align=right|15,691||align=right|3,129||align=right|2,663||align=right|50,060 | |||
| |- | |||
| |align=center|13||]||USA||align=right|14,268||align=right|3,366||align=right|2,950||align=right|48,000 | |||
| |- | |||
| |align=center|14||]||Germany ||align=right|13,284||align=right|1,977||align=right|2,163||align=right|43,000 | |||
| |- | |||
| |align=center|15||]||USA||align=right|10,594||align=right|2,188||align=right|1,057||align=right|41,500 | |||
| |- | |||
| |align=center|16||]||USA||align=right|10,378||align=right|614||align=right|1,397||align=right|38,428 | |||
| |- | |||
| |align=center|17||]||]||align=right|10,284||align=right|1,620||align=right|2,870||align=right|15,000 | |||
| |- | |||
| |align=center|18||]||USA||align=right|9,284||align=right|1,773||align=right|2,113||align=right|33,500 | |||
| |- | |||
| |align=center|19||]||USA||align=right|8,964||align=right|n/a||align=right|10,340||align=right|29,258 | |||
| |- | |||
| |align=center| ||SUM|| ||align=right|497,519||align=right|70,843||align=right|110,077||align=right|1,342,700 | |||
| |- | |||
| |align=center| ||AVERAGE|| ||align=right|24,876||align=right|3,542||align=right|5504||align=right|67,135 | |||
| |} | |||
| ===Market leaders in terms of sales=== | |||
| The top 15 pharmaceutical companies by ] are:<ref name="Press release"/><ref>''IMS Health 2008'', </ref> | |||
| {|class="sortable wikitable" | |||
| ! Rank !! Company !! Sales ($M) !! Based/Headquartered in | |||
| |- | |||
| | 1 || ] || 43,363 ||] | |||
| |- | |||
| | 2 || ]||36,506 || ] | |||
| |- | |||
| | 3 || ] || 36,506 || ] | |||
| |- | |||
| | 4 || ] ||35,642 || ] | |||
| |- | |||
| | 5 || ] || 32,516 ||] | |||
| |- | |||
| | 6 || ] || 30,336 || ] | |||
| |- | |||
| | 7 || ] || 29,425 ||] | |||
| |- | |||
| | 8 || ] || 26,191 ||] | |||
| |- | |||
| | 9 || ] || 19,466 ||] | |||
| |- | |||
| | 10 || ] || 19,140 || ] | |||
| |- | |||
| | 11 || ] || 15,794 || ] | |||
| |- | |||
| | 12 || ] || 15,682 || ] | |||
| |- | |||
| | 13 || ] || 15,660 || ] | |||
| |- | |||
| | 14 || ] || 15,274 || ] | |||
| |- | |||
| | 15 || ] || 13,819 || ] | |||
| |- | |||
| |} | |||
| ===Patents and generics=== | ===Patents and generics=== | ||
| Depending on a number of considerations, a company may apply for and be granted a ] for the drug, or the process of producing the drug, granting exclusivity rights typically for about 20 years.<ref></ref> However, only after rigorous study and testing, which takes 10 to 15 years on average, will governmental authorities grant permission for the company to market and sell the drug.<ref>{{Cite web|url=http://www.phrma.org/files/NDA2006.pdf|format=PDF|title=New Drug Approvals in 2006|date=March 2007|accessdate=2008-02-23 |archiveurl = http://web.archive.org/web/20080228023631/http://www.phrma.org/files/NDA2006.pdf <!-- Bot retrieved archive --> |archivedate = 2008-02-28}}</ref> Patent protection enables the owner of the patent to recover the costs of research and development through high profit margins for the ]ed drug. When the patent protection for the drug expires, a ] is usually developed and sold by a competing company. The development and approval of generics is less expensive, allowing them to be sold at a lower price. Often the owner of the branded drug will introduce a generic version before the patent expires in order to get a head start in the generic market.<ref>{{Cite web|url=http://www.phrma.org/files/IMS%20Authorized%20Generics%20Report_6-22-06.pdf|format=PDF|title=Assessment of Authorized Generics in the U.S|publisher=IMS Consulting|date=June 2006|accessdate=2008-02-23 |archiveurl = http://web.archive.org/web/20080228023633/http://www.phrma.org/files/IMS+Authorized+Generics+Report_6-22-06.pdf <!-- Bot retrieved archive --> |archivedate = 2008-02-28}}</ref> Restructuring has therefore become routine, driven by the patent expiration of products launched during the industry's 'golden era' in the 1990s and companies' failure to develop sufficient new blockbuster products to replace lost revenues.<ref></ref> | Depending on a number of considerations, a company may apply for and be granted a ] for the drug, or the process of producing the drug, granting exclusivity rights typically for about 20 years.<ref></ref> However, only after rigorous study and testing, which takes 10 to 15 years on average, will governmental authorities grant permission for the company to market and sell the drug.<ref>{{Cite web|url=http://www.phrma.org/files/NDA2006.pdf|format=PDF|title=New Drug Approvals in 2006|date=March 2007|accessdate=2008-02-23 |archiveurl = http://web.archive.org/web/20080228023631/http://www.phrma.org/files/NDA2006.pdf <!-- Bot retrieved archive --> |archivedate = 2008-02-28}}</ref> Patent protection enables the owner of the patent to recover the costs of research and development through high profit margins for the ]ed drug. When the patent protection for the drug expires, a ] is usually developed and sold by a competing company. The development and approval of generics is less expensive, allowing them to be sold at a lower price. Often the owner of the branded drug will introduce a generic version before the patent expires in order to get a head start in the generic market.<ref>{{Cite web|url=http://www.phrma.org/files/IMS%20Authorized%20Generics%20Report_6-22-06.pdf|format=PDF|title=Assessment of Authorized Generics in the U.S|publisher=IMS Consulting|date=June 2006|accessdate=2008-02-23 |archiveurl = http://web.archive.org/web/20080228023633/http://www.phrma.org/files/IMS+Authorized+Generics+Report_6-22-06.pdf <!-- Bot retrieved archive --> |archivedate = 2008-02-28}}</ref> Restructuring has therefore become routine, driven by the patent expiration of products launched during the industry's 'golden era' in the 1990s and companies' failure to develop sufficient new blockbuster products to replace lost revenues.<ref></ref> | ||
| . | |||
| ===Medicare Part D=== | |||
| In 2003 the United States enacted the ] (MMA), a program to provide prescription drug benefits to the ] and ]. This program is a component of ] and is known as ]. This program, set to begin in January 2006, will significantly alter the revenue models for pharmaceutical companies. Revenues from the program are expected to be $724 billion between 2006 and 2015.<ref>{{Cite web|url=http://www.kff.org/medicare/upload/7044-02.pdf |format=PDF|title=The medicare Prescriptions Drug Benefit|publisher=]|date=September 2005|accessdate=2007-06-12 |archiveurl = http://web.archive.org/web/20060217051127/http://www.kff.org/medicare/upload/7044-02.pdf |archivedate = 2006-02-17}}</ref> | |||
| Pharmaceuticals developed by biotechnological processes often must be injected in a physician's office rather than be delivered in the form of a capsule taken orally. Medicare payments for these drugs are usually made through Medicare Part B (physician office) rather than Part D (prescription drug plan). | |||
| ===Mergers, acquisitions, and co-marketing of drugs=== | |||
| A ], or ] deal between pharmaceutical companies may occur as a result of complementary capabilities between them. A small ] company might have a new drug but no sales or marketing capability. Conversely, a large pharmaceutical company might have unused capacity in a large sales force due to a gap in the company pipeline of new products. It may be in both companies' interest to enter into a deal to capitalize on the synergy between the companies. | |||
| ===Prescriptions=== | ===Prescriptions=== | ||
| In the U.S., prescriptions have increased over the past decade to 3.4 billion annually, a 61 percent increase. ] jumped 250 percent from $72 billion to $250 billion, while the average price of prescriptions has more than doubled from $30 to $68.<ref></ref> | In the U.S., prescriptions have increased over the past decade to 3.4 billion annually, a 61 percent increase. ] jumped 250 percent from $72 billion to $250 billion, while the average price of prescriptions has more than doubled from $30 to $68.<ref></ref> | ||
| ===Publications=== | |||
| The drug company ] publishes the ], the world's best-selling medical textbook, and the ], a collection of information about chemical compounds. | |||
| ==Marketing== | ==Marketing== | ||
| ] | |||
| {{Main|Pharmaceutical marketing}} | |||
| Advertising is common in healthcare journals as well as through more mainstream media routes. In some countries, notably the US, they are allowed to advertise directly to the general public. Pharmaceutical companies generally employ sales people (often called 'drug reps' or, an older term, 'detail men') to market directly and personally to physicians and other healthcare providers. In some countries, notably the US, pharmaceutical companies also employ ] to influence politicians. Marketing of prescription drugs in the US is regulated by the federal ]. | |||
| ===To healthcare professionals=== | ===To healthcare professionals=== | ||
| In 2008, Senator ] began an investigation about unreported payments to physicians by pharmaceutical companies. Grassley led a Congressional Investigation which found that well-known university ]s, who had promoted ]s, had violated federal and university regulations by failing to report $1.6 million in consulting income from the pharmaceutical companies which made the drugs.<ref>{{cite web |url=http://www.nytimes.com/2008/06/08/us/08conflict.html?pagewanted=all&_r=0 |title=Researchers Fail to Reveal Full Drug Pay - NYTimes.com |format= |work= |accessdate=}}</ref> Weeks later, Business Week reported that Grassley alleged that ], chair of psychiatry at ], had underreported his investments in Corcept Therapeutics, a company he founded.<ref>{{cite news | url = http://www.businessweek.com/technology/content/jun2008/tc20080626_630542.htm | title = Drug Makers and College Labs: Too Cozy? | work = Business Week | first = Arlene | last = Weintraub | date = June 26, 2008}}</ref> Dr. Schatzberg had reported only $100,000 investments in Corcept, but Grassley stated that his investments actually totalled over $6 million. Dr. Schaztberg later stepped down from his grant which is funded by the ] (NIH).<ref>{{cite news | url = http://chronicle.com/news/article/4922/stanford-researcher-accused-of-conflicts-steps-down-as-nih-principal-investigator | title = Stanford Researcher, Accused of Conflicts, Steps Down as NIH Principal Investigator | work = The Chronicle of Higher Education | date = August 1, 2008}}</ref> Similarly, Dr. ] resigned as chair of the psychiatry department at ] after failing to report a third of the $2.8 million in consulting fees he received from ]. At the time he received these fees, Dr. Nemeroff had been principal investigator of a $3.9 million NIH grant evaluating five medications for depression manufactured by GlaxoSmithKline.<ref>{{cite news | url = http://articles.latimes.com/2008/oct/04/science/sci-doctors4 | title = Doctor Accused in Congress' Probe | work = The Los Angeles Times | date= October 4, 2008 | first1=Denise | last1=Gellene | first2=Thomas H. | last2=Maugh II}}</ref> | |||
| Currently, there are approximately 81,000 ]s in the United States<ref name="ZS Associates; Pharmaceutical">{{cite web |url=http://www.zsassociates.com/news_events/news_media/the_doctor_wont_see_you_mr_pharma_rep_now/ |title=ZS Associates; Pharmaceutical |work= |accessdate=}}</ref> pursuing some 830,000 pharmaceutical prescribers. A pharmaceutical representative will often try to see a given physician every few weeks. Representatives often have a call list of about 200–300 physicians with 120–180 targets that should be visited in 1–2 or 3 week cycle. The number of pharmaceutical sales reps has been shrinking between 2008 and 2010, an estimated 30% industry wide reduction has occurred and current estimates are there may only be 60,000 pharmaceutical sales reps in the United States.<ref name="ZS Associates; Pharmaceutical"/> | |||
| In 2008, Senator ] began an investigation about unreported payments to physicians by pharmaceutical companies. Grassley led a Congressional Investigation which found that well-known university ]s, who had promoted ]s, had violated federal and university regulations by secretly receiving large sums of money from the pharmaceutical companies which made the drugs.<ref>{{cite book |last=Kirk |first=Stuart A. |title=Mad Science: Psychiatric Coercion, Diagnosis, and Drugs |year=2013 |publisher=Transaction Publishers |page= 21}}</ref> The ] reported that Dr. ] of Harvard University had failed to report over a million dollars of income that he had received from pharmaceutical companies.<ref>{{cite news | url = http://www.nytimes.com/2008/06/08/us/08conflict.html | title = Researchers Fail to Reveal Full Drug Pay | work = The New York Times | first1 = Gardiner | last1 = Harris | first2 = Benedict | last2 = Carey | date = June 8, 2008}}</ref> Weeks later, Business Week reported that Grassley alleged that ], chair of psychiatry at ], had underreported his investments in Corcept Therapeutics, a company he founded.<ref>{{cite news | url = http://www.businessweek.com/technology/content/jun2008/tc20080626_630542.htm | title = Drug Makers and College Labs: Too Cozy? | work = Business Week | first = Arlene | last = Weintraub | date = June 26, 2008}}</ref> Dr. Schatzberg had reported only $100,000 investments in Corcept, but Grassley stated that his investments actually totalled over $6 million. Dr. Schaztberg later stepped down from his grant which is funded by the ] (NIH).<ref>{{cite news | url = http://chronicle.com/news/article/4922/stanford-researcher-accused-of-conflicts-steps-down-as-nih-principal-investigator | title = Stanford Researcher, Accused of Conflicts, Steps Down as NIH Principal Investigator | work = The Chronicle of Higher Education | date = August 1, 2008}}</ref> Similarly, Dr. ] resigned as chair of the psychiatry department at ] after failing to report a third of the $2.8 million in consulting fees he received from ]. At the time he received these fees, Dr. Nemeroff had been principal investigator of a $3.9 million NIH grant evaluating five medications for depression manufactured by GlaxoSmithKline.<ref>{{cite news | url = http://articles.latimes.com/2008/oct/04/science/sci-doctors4 | title = Doctor Accused in Congress' Probe | work = The Los Angeles Times | date= October 4, 2008 | first1=Denise | last1=Gellene | first2=Thomas H. | last2=Maugh II}}</ref> | |||
| The book '']'' also discusses the influence of drug representatives, how ghostwriters are employed by the drug companies to write papers for academics to publish, how independent the academic journals really are, how the drug companies finance doctors' continuing education, and how patients' groups are often funded by industry.<ref>'']'', pp. 274, 287, 303, 311.</ref> | The book '']'' also discusses the influence of drug representatives, how ghostwriters are employed by the drug companies to write papers for academics to publish, how independent the academic journals really are, how the drug companies finance doctors' continuing education, and how patients' groups are often funded by industry.<ref>'']'', pp. 274, 287, 303, 311.</ref> | ||
| ===To insurance and public health bodies=== | |||
| Private insurance or public health bodies (e.g. the NHS in the UK) decide which drugs to pay for, and restrict the drugs that can be prescribed through the use of formularies. Public and private insurers restrict the brands, types and number of drugs that they will cover. Not only can the insurer affect drug sales by including or excluding a particular drug from a formulary, they can affect sales by tiering or placing bureaucratic hurdles to prescribing certain drugs as well. In January 2006, the U.S. instituted a new public prescription drug plan through its Medicare program known as ]. This program engages private insurers to negotiate with pharmaceutical companies for the placement of drugs on tiered formularies. | |||
| In 2008, for the first time, Charles Grassley asked the ] to disclose how much of its annual budget came from drug industry funds. The APA said that industry contributed 28% of its budget ($14 million at that time), mainly through paid advertising in APA journals and funds for continuing medical education.<ref name=stuarta>{{cite book |last=Kirk |first=Stuart A. |title=Mad Science: Psychiatric Coercion, Diagnosis, and Drugs |year=2013 |publisher=Transaction Publishers |page= 217}}</ref> | |||
| ===To retail pharmacies and stores=== | |||
| Commercial stores and pharmacies are a major target of non-prescription sales and marketing for pharmaceutical companies. | |||
| ===Direct to consumer advertising=== | ===Direct to consumer advertising=== | ||
| Line 251: | Line 174: | ||
| ===Controversy about drug marketing and lobbying=== | ===Controversy about drug marketing and lobbying=== | ||
| There has been increasing controversy surrounding pharmaceutical marketing and influence. There have been accusations and findings of influence on doctors and other health professionals through drug reps, including the constant provision of marketing 'gifts' and biased information to health professionals;<ref>{{Cite web|url=http://www.nofreelunch.org/|title=No Free Lunch|accessdate=2007-05-23}}</ref><ref>{{Cite news|url=http://www.washingtonpost.com/wp-dyn/content/article/2005/05/05/AR2005050501115_pf.html|title= Merck CEO Resigns as Drug Probe Continues|publisher=]|date=2005-05-06|accessdate=2007-05-23 | first=Marc | last=Kaufman}}</ref> highly prevalent advertising in journals and conferences; funding independent healthcare organizations and health promotion campaigns; lobbying physicians and politicians (more than any other industry in the US<ref>{{Cite web|url=http://www.publicintegrity.org/rx/report.aspx?aid=723|title=Drug Lobby Second to None: How the pharmaceutical industry gets its way in Washington|publisher=publicintegrity.org|date=2005-07-07|accessdate=2007-05-23}}</ref>); sponsorship of ]s or nurse training; sponsorship of continuing educational events, with influence on the curriculum;<ref>Ray Moynihan (2003-05-31). . ''BMJ: British Medical Journal'', Volume 326, Issue 7400, Page 1163. Retrieved on 2007-10-07.</ref> and hiring physicians as paid consultants on medical advisory boards. | There has been increasing controversy surrounding pharmaceutical marketing and influence. There have been accusations and findings of influence on doctors and other health professionals through drug reps, including the constant provision of marketing 'gifts' and biased information to health professionals;<ref>{{Cite web|url=http://www.nofreelunch.org/|title=No Free Lunch|accessdate=2007-05-23}}</ref><ref>{{Cite news|url=http://www.washingtonpost.com/wp-dyn/content/article/2005/05/05/AR2005050501115_pf.html|title= Merck CEO Resigns as Drug Probe Continues|publisher=]|date=2005-05-06|accessdate=2007-05-23 | first=Marc | last=Kaufman}}</ref> highly prevalent advertising in journals and conferences; funding independent healthcare organizations and health promotion campaigns; lobbying physicians and politicians (more than any other industry in the US<ref>{{Cite web|url=http://www.publicintegrity.org/rx/report.aspx?aid=723|title=Drug Lobby Second to None: How the pharmaceutical industry gets its way in Washington|publisher=publicintegrity.org|date=2005-07-07|accessdate=2007-05-23}}</ref>); sponsorship of ]s or nurse training; sponsorship of continuing educational events, with influence on the curriculum;<ref>Ray Moynihan (2003-05-31). . ''BMJ: British Medical Journal'', Volume 326, Issue 7400, Page 1163. Retrieved on 2007-10-07.</ref> and hiring physicians as paid consultants on medical advisory boards. | ||
| To help ensure the status quo on U.S. drug regulation and pricing, the pharmaceutical industry has thousands of lobbyists in Washington, DC that lobby Congress and protect their interests. The pharmaceutical industry spent $855 million, more than any other industry, on lobbying activities from 1998 to 2006, according to the non-partisan Center for Public Integrity.<ref></ref> | |||
| Some advocacy groups, such as ], have criticized the effect of drug marketing to physicians because they say it biases physicians to prescribe the marketed drugs even when others might be cheaper or better for the patient.<ref name="Koerner">Koerner BI (March/April, 2003), . ''Mother Jones'', Retrieved on 2007-10-06.</ref> | Some advocacy groups, such as ], have criticized the effect of drug marketing to physicians because they say it biases physicians to prescribe the marketed drugs even when others might be cheaper or better for the patient.<ref name="Koerner">Koerner BI (March/April, 2003), . ''Mother Jones'', Retrieved on 2007-10-06.</ref> | ||
| Line 260: | Line 181: | ||
| A 2005 review by a special committee of the ] government came to all the above conclusions in a European Union context<ref>{{Cite web|url=http://www.epha.org/a/1773|title=UK parliamentarians put the pharma industry under the spotlight|publisher=European Public Health Alliance|accessdate=2007-05-23}}</ref> whilst also highlighting the contributions and needs of the industry. | A 2005 review by a special committee of the ] government came to all the above conclusions in a European Union context<ref>{{Cite web|url=http://www.epha.org/a/1773|title=UK parliamentarians put the pharma industry under the spotlight|publisher=European Public Health Alliance|accessdate=2007-05-23}}</ref> whilst also highlighting the contributions and needs of the industry. | ||
| Meta-analyses have shown that psychiatric studies sponsored by pharmaceutical companies are several times more likely to report positive results, and if a drug company employee is involved the effect is even larger.<ref>Buchkowsky SS, Jewesson PJ. (2004) Industry sponsorship and authorship of clinical trials over 20 years. Ann Pharmacother. 2004 Apr;38(4):579-85. PMID 14982982</ref><ref>{{cite journal |author=Perlis RH, Perlis CS, Wu Y, Hwang C, Joseph M, Nierenberg AA |title=Industry sponsorship and financial conflict of interest in the reporting of clinical trials in psychiatry |journal=Am J Psychiatry |volume=162 |issue=10 |pages=1957–60 |date=October 2005 |pmid=16199844 |doi=10.1176/appi.ajp.162.10.1957 |url=}}</ref><ref>Tungaraza T, Poole R. (2007) Influence of drug company authorship and sponsorship on drug trial outcomes. Br J Psychiatry. 2007 Jul;191:82-3. PMID 17602130</ref> Influence has also extended to the training of doctors and nurses in medical schools, which is being fought.<ref></ref> | |||
| It has been argued that the design of the ] and the expansion of the criteria represents an increasing medicalization of human nature, or "]", driven by drug company influence on psychiatry.<ref>Healy D (2006) PLoS Med 3(4): e185.</ref> The potential for direct ] has been raised, partly because roughly half the authors who selected and defined the DSM-IV psychiatric disorders had or previously had financial relationships with the pharmaceutical industry.<ref>Cosgrove, Lisa, Krimsky, Sheldon,Vijayaraghavan, Manisha, Schneider, Lisa,</ref> The president of the organization that designs and publishes the DSM, the ], stated in 2005 that in general American psychiatry has "allowed the biopsychosocial model to become the bio-bio-bio model" and that the gifts from drug reps are little more than "kickbacks and bribes".<ref>Sharfstein, SS. (2005) ''Psychiatric News'' August 19, 2005 Volume 40 Number 16</ref> | |||
| In the US, starting in 2013, under the Physician Financial Transparency Reports (part of the Sunshine Act), the Centers for Medicare & Medicaid Services has to collect information from applicable manufacturers and group purchasing organizations in order to report information about their financial relationships with physicians and hospitals. Data are made public in the Centers for Medicare & Medicaid Services website. The expectation is that relationship between doctors and Pharmaceutical industry will become fully transparent.<ref></ref> | |||
| ===Regulatory issues === | |||
| It has been argued that the design of the ] and the expansion of the criteria represents an increasing medicalization of human nature, or "]", driven by drug company influence on psychiatry.<ref>Healy D (2006) PLoS Med 3(4): e185.</ref> The potential for direct ] has been raised, partly because roughly half the authors who selected and defined the DSM-IV psychiatric disorders had or previously had financial relationships with the pharmaceutical industry.<ref>Cosgrove, Lisa, Krimsky, Sheldon,Vijayaraghavan, Manisha, Schneider, Lisa,</ref> The president of the organization that designs and publishes the DSM, the ], recently acknowledged that in general American psychiatry has "allowed the biopsychosocial model to become the bio-bio-bio model" and that the gifts from drug reps are little more than "kickbacks and bribes".<ref>Sharfstein, SS. (2005) ''Psychiatric News'' August 19, 2005 Volume 40 Number 16</ref> | |||
| Ben Goldacre has argued that regulators – such as the ] (MHRA) in the UK, or the ] (FDA) in the United States – advance the interests of the drug companies rather than the interests of the public due to revolving door exchange of employees between the regulator and the companies and friendships develop between regulator and company employees.<ref>'']'', p. 123ff.</ref> He argues that regulators do not require that new drugs offer an improvement over what is already available, or even that they be particularly effective.<ref>''Bad Pharma'', p. 143ff.</ref> | |||
| Others have argued that excessive regulation suppresses therapeutic innovation, and that the current cost of regulator-required clinical trials prevents the full exploitation of new genetic and biological knowledge for the treatment of human disease. A 2012 report by the President's Council of Advisors on Science and Technology made several key recommendations to reduce regulatory burdens to new drug development, including 1) expanding the FDA's use of accelerated approval processes, 2) creating an expedited approval pathway for drugs intended for use in narrowly defined populations, and 3) undertaking pilot projects designed to evaluate the feasibility of a new, adaptive drug approval process.<ref>{{cite web |url=http://www.whitehouse.gov/sites/default/files/microsites/ostp/pcast-fda-final.pdf |title=www.whitehouse.gov |format= |work= |accessdate=}}</ref> | |||
| ===Regulatory capture=== | |||
| Chapter three of the book '']'' describes the concept of "]," whereby a regulator – such as the ] (MHRA) in the UK, or the ] (FDA) in the United States – ends up advancing the interests of the drug companies rather than the interests of the public. The author, ], writes that this happens for a number of reasons, including the ] of employees between the regulator and the companies, and the fact that friendships develop between regulator and company employees simply because they have knowledge and interests in common. The chapter also discusses ] and ], and the difficulty of having ineffective drugs removed from the market once they have been approved.<ref>'']'', p. 123ff.</ref> He argues that regulators do not require that new drugs offer an improvement over what is already available, or even that they be particularly effective.<ref>''Bad Pharma'', p. 143ff.</ref> | |||
| ===Pharmaceutical fraud=== | ===Pharmaceutical fraud=== | ||
| {{See also|List of largest pharmaceutical settlements in the United States}} | {{See also|List of largest pharmaceutical settlements in the United States}} | ||
| ] involves activities that result in false claims to insurers or programs such as ] in the United States or equivalent state programs for financial gain to a pharmaceutical company. There are several different schemes<ref name="FBIFraudTypes">{{cite web|url=http://www.fbi.gov/stats-services/publications/fcs_report2006/financial-crimes-report-to-the-public-fiscal-year-2006#Health|publisher=FBI|year=2006|title=Financial Crimes to the Public Report 2006}}</ref> used to defraud the ] which are particular to the pharmaceutical industry. These include: Good Manufacturing Practice (GMP) Violations, Off Label Marketing, Best Price Fraud, CME Fraud, Medicaid Price Reporting, and Manufactured Compound Drugs |
] involves activities that result in false claims to insurers or programs such as ] in the United States or equivalent state programs for financial gain to a pharmaceutical company. There are several different schemes<ref name="FBIFraudTypes">{{cite web|url=http://www.fbi.gov/stats-services/publications/fcs_report2006/financial-crimes-report-to-the-public-fiscal-year-2006#Health|publisher=FBI|year=2006|title=Financial Crimes to the Public Report 2006}}</ref> used to defraud the ] which are particular to the pharmaceutical industry. These include: Good Manufacturing Practice (GMP) Violations, Off Label Marketing, Best Price Fraud, CME Fraud, Medicaid Price Reporting, and Manufactured Compound Drugs.<ref name="FBIHealthCareGeneral">{{cite web|url=http://www.fbi.gov/about-us/investigate/white_collar/health-care-fraud|title=FBI-Health Care Fraud|publisher=FBI}}</ref> Of this amount $2.5 billion was recovered through ''False Claims Act'' cases in FY 2010. Examples of fraud cases include the ] $3 billion settlement, ] $2.3 billion settlement and ] $650 million settlement. Damages from fraud can be recovered by use of the ], most commonly under the '']'' provisions which rewards an individual for being a "]", or ].<ref name="DOJHealthCareFraudReport">{{cite web|url=http://www.justice.gov/usao/tne/health_care.html|title=Department of Justice|publisher=Department of Justice}}</ref> | ||
| Every major company selling the antipsychotics — ], ], ], ] and ] — has either settled recent government cases, under the False Claims Act, for hundreds of millions of dollars or is currently under investigation for possible health care fraud. Following charges of illegal marketing, two of the settlements set records last year for the largest criminal fines ever imposed on corporations. One involved Eli Lilly's antipsychotic ], and the other involved ]. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, ]; Pfizer settled that part of the claim for $301 million, without admitting any wrongdoing.<ref name=bied2010>{{cite news |url=http://www.nytimes.com/2010/10/03/business/03psych.html?_r=3&hp=&pagewanted=all |title=Side Effects May Include Lawsuits |author=Duff Wilson |date=October 2, 2010 |work=New York Times }}</ref> | |||
| On 2 July 2012, ] pleaded guilty to criminal charges and agreed to a $3 billion settlement of the largest health-care fraud case in the U.S. and the largest payment by a drug company.<ref>{{cite news| url=http://www.bbc.co.uk/news/world-us-canada-18673220| title=GlaxoSmithKline | date= 4 July 2012}}</ref> The settlement is related to the company's illegal promotion of prescription drugs, its failure to report safety data,<ref>{{cite |
On 2 July 2012, ] pleaded guilty to criminal charges and agreed to a $3 billion settlement of the largest health-care fraud case in the U.S. and the largest payment by a drug company.<ref>{{cite news| url=http://www.bbc.co.uk/news/world-us-canada-18673220| title=GlaxoSmithKline | date= 4 July 2012 | work=BBC News}}</ref> The settlement is related to the company's illegal promotion of prescription drugs, its failure to report safety data,<ref>{{cite news |url=http://www.bloomberg.com/news/2012-07-02/glaxosmithkline-agrees-to-pay-3-billion-in-u-s-drug-settlement.html |title=GlaxoSmithKline Agrees to Pay $3 Billion in U.S. Drug Settlement |date=2 July 2012 | work=Bloomberg}}</ref> ] doctors, and promoting medicines for uses for which they were not licensed. The drugs involved were ], ], ], ], and ] for off-label, non-covered uses. Those and the drugs ], ], ], and ] were involved in the ].<ref>{{cite web|url=http://www.wnyc.org/articles/wnyc-news/2012/jul/02/drug-giant-pays-record-setting-fine/|title=NY to Get Millions in GlaxoSmithKlein Settlement|author=Fred Mogul|publisher=]|date=2 July 2012|accessdate=2 July 2012}}</ref><ref>{{cite news|url=http://www.bbc.co.uk/news/world-us-canada-18673220|title=BBC News -GlaxoSmithKline to pay $3bn in US drug fraud scandal|work=]|accessdate=2 July 2012|date=2012-07-02}}</ref><ref>{{cite news|url=http://www.nytimes.com/2012/07/03/business/glaxosmithkline-agrees-to-pay-3-billion-in-fraud-settlement.html|title=Glaxo Agrees to Pay $3 Billion in Fraud Settlement|date=July 2, 2012|author=Thomas, Katie and Schmidt, Michael S.|work=The New York Times|accessdate=July 3, 2012}}</ref> | ||
| The following is a list of the four largest settlements reached with pharmaceutical companies from 1991 to 2012, rank ordered by the size of the total settlement. Legal claims against the pharmaceutical industry have varied widely over the past two decades, including ], ] promotion, and inadequate manufacturing practices.<ref>Sammy Almashat, M.D., M.P.H., Charles Preston, M.D., M.P.H., Timothy Waterman, B.S., Sidney Wolfe, M.D., Rapidly Increasing Criminal and Civil Monetary Penalties Against the Pharmaceutical Industry: 1991 – 2010, Public |
The following is a list of the four largest settlements reached with pharmaceutical companies from 1991 to 2012, rank ordered by the size of the total settlement. Legal claims against the pharmaceutical industry have varied widely over the past two decades, including ], ] promotion, and inadequate manufacturing practices.<ref>Sammy Almashat, M.D., M.P.H., Charles Preston, M.D., M.P.H., Timothy Waterman, B.S., Sidney Wolfe, M.D., Rapidly Increasing Criminal and Civil Monetary Penalties Against the Pharmaceutical Industry: 1991 – 2010, Public Citizen's Health Research Group, December 16, 2010</ref><ref>{{cite news| url=http://www.nytimes.com/2012/07/03/business/glaxosmithkline-agrees-to-pay-3-billion-in-fraud-settlement.html?pagewanted=all | work=The New York Times | first1=Katie | last1=Thomas | first2=Michael S. | last2=Schmidt | title=GlaxoSmithKline Agrees to Pay $3 Billion in Fraud Settlement | date=2012-07-02}}</ref> | ||
| {| class="wikitable" | {| class="wikitable" | ||
| Line 291: | Line 216: | ||
| ==Developing world== | ==Developing world== | ||
| The role of pharmaceutical companies in the developing world is a matter of some debate, ranging from those highlighting the aid provided to the developing world, to those critical of the use of the poorest in human clinical trials, often without adequate protections, particularly in ] lacking a strong ]. Other criticisms include an alleged reluctance of the industry to invest in treatments of diseases in less economically advanced countries, such as ]; Criticism for the price of ]ed ] medication, which could limit therapeutic options for patients in the ], where most of the AIDS infected people are living. However, a better policy of ] would benefit to both patients and companies. | |||
| In September 2008 the was launched in India to combat infectious diseases common to developing countries. | |||
| ===Patents=== | ===Patents=== | ||
| Patents have been criticized in the developing world, as they are thought to reduce access to existing medicines.<ref>See for example: 't Hoen, Ellen. "TRIPS, Pharmaceutical Patents, and Access to Essential Medicines: A Long Way from Seattle to Doha". Chicago Journal of International Law, 27(43), 2002; Musungu, Sisule F., and Cecilia Oh. "The Use of Flexibilities in TRIPS by Developing Countries: Can They Provide Access to Medicines?" Commission on Intellectual Property Rights, Innovation and Public Health, The World Health Organization, 2005.</ref> Reconciling patents and universal access to medicine would require an efficient international policy of ]. Moreover, under the ] agreement of the ], countries must allow pharmaceutical products to be patented. In 2001, the WTO adopted the ], which indicates that the TRIPS agreement should be read with the goals of public health in mind, and allows some methods for circumventing pharmaceutical monopolies: via ] or ], even before patent expiration.<ref>WTO. "The Doha Declaration on TRIPS and public health", 2001. Available online at http://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm.</ref> | |||
| {{See also|Criticism of patents}} | |||
| Patents have been criticized in the developing world, as they are thought to reduce access to existing medicines.<ref>See for example: 't Hoen, Ellen. "TRIPS, Pharmaceutical Patents, and Access to Essential Medicines: A Long Way from Seattle to Doha". Chicago Journal of International Law, 27(43), 2002; Musungu, Sisule F., and Cecilia Oh. "The Use of Flexibilities in TRIPS by Developing Countries: Can They Provide Access to Medicines?" Commission on Intellectual Property Rights, Innovation and Public Health, The World Health Organization, 2005.</ref> There is mixed evidence on the efficacy of patents to stimulate pharmaceutical innovation, with recent evidence suggesting that patent grants slow down innovation.<ref>{{cite journal|author1=Murray, F.|author2=Stern, S.|title=Do Formal Intellectual Property Rights Hinder the Free Flow of Scientific Knowledge? An Empirical Test of the Anti-Commons Hypothesis|journal=Journal of Economic Behavior and Organization|year=2007|doi=10.1016|url=http://fmurray.scripts.mit.edu/docs/murraysternJEBO.pdf|accessdate=21 April 2013}}</ref> Reconciling patents and universal access to medicine would require an efficient international policy of ]. Moreover, under the ] agreement of the ], countries must allow pharmaceutical products to be patented. In 2001, the WTO adopted the ], which indicates that the TRIPS agreement should be read with the goals of public health in mind, and allows some methods for circumventing pharmaceutical monopolies: via ] or ], even before patent expiration.<ref>WTO. "The Doha Declaration on TRIPS and public health", 2001. Available online at http://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm.</ref> | |||
| In March 2001, 40 multi-national pharmaceutical companies brought litigation against ] for its ], which allowed the generic production of antiretroviral drugs (ARVs) for treating HIV, despite the fact that these drugs were on-patent.<ref>"Pharmaceutical Manufacturer's Association v. The President of South Africa (PMA)", 2002 (2) SA 674 (CC) (S. Africa).</ref> HIV was and is an epidemic in South Africa, and ARVs at the time cost between 10,000 and 15,000 USD per patient per year. This was unaffordable for most South African citizens, and so the South African government committed to providing ARVs at prices closer to what people could afford. To do so, they would need to ignore the patents on drugs and produce generics within the country (using a compulsory license), or import them from abroad. The Indian pharmaceutical company ] audaciously offered to make the drugs at 350 USD per patient per year, roughly 1/40th of the lowest price available from a patent holder, which stunned the world community. After massive international protest in favour of public health rights (including the collection of 250,000 signatures by ]), the governments of several developed countries (including The Netherlands, Germany, France, and later the US) backed the South African government, and the case was dropped in April of that year.<ref>Helfer, Laurence R. and Graeme W. Austin. "Human Rights and Intellectual Property: Mapping the Global Interface". Cambridge University Press: 2011, pp. 145–48.</ref> | |||
| In March 2001, 40 multi-national pharmaceutical companies brought litigation against ] for its ], which allowed the generic production of antiretroviral drugs (ARVs) for treating HIV, despite the fact that these drugs were on-patent.<ref>"Pharmaceutical Manufacturer's Association v. The President of South Africa (PMA)", 2002 (2) SA 674 (CC) (S. Africa).</ref> HIV was and is an epidemic in South Africa, and ARVs at the time cost between 10,000 and 15,000 USD per patient per year. This was unaffordable for most South African citizens, and so the South African government committed to providing ARVs at prices closer to what people could afford. To do so, they would need to ignore the patents on drugs and produce generics within the country (using a compulsory license), or import them from abroad. After international protest in favour of public health rights (including the collection of 250,000 signatures by ]), the governments of several developed countries (including The Netherlands, Germany, France, and later the US) backed the South African government, and the case was dropped in April of that year.<ref>Helfer, Laurence R. and Graeme W. Austin. "Human Rights and Intellectual Property: Mapping the Global Interface". Cambridge University Press: 2011, pp. 145–48.</ref> | |||
| ===Nigerian clinical trial=== | |||
| {{See also|Kano trovafloxacin trial litigation}} | |||
| In 1996, a pediatric clinical trial conducted on behalf of ] tested the antibiotic ] allegedly without first obtaining the informed consent of participants or their parents.<ref>{{Cite news|url=http://www.washingtonpost.com/ac2/wp-dyn/A11939-2000Dec15|title=As Drug Testing Spreads, Profits and Lives Hang in Balance|author=Stephens, Joe|publisher=Washington Post|date=2000-12-17|accessdate=2007-06-25}}</ref><ref>{{Cite web|url=http://bmj.bmjjournals.com/cgi/content/full/323/7313/592/b|title=Nigerians to sue US drug company over meningitis treatment|Kovac, Carl|publisher=BMJ|date=2001-09-15|accessdate=2007-06-25}}</ref><ref>{{Cite web|url=http://www.bmj.com/cgi/content/full/322/7280/194|title=Pfizer accused of testing new drug without ethical approval|author=Wise, Jacqui|publisher=BMJ|date=2001-01-27|accessdate=2007-06-25}}</ref><ref>{{Cite web|url=http://www.channel4.com/health/microsites/D/dying_for_drugs/resources4.html|title=Dying For Drugs|publisher=channel4.com|accessdate=2007-06-25}}</ref> | |||
| ===Charitable programs=== | ===Charitable programs=== | ||
| Line 311: | Line 228: | ||
| * ]'s commitment to give free albendazole tablets to the WHO for, and until, the elimination of ] worldwide.</sup> | * ]'s commitment to give free albendazole tablets to the WHO for, and until, the elimination of ] worldwide.</sup> | ||
| * In 2006, ] committed USD 755 million in corporate citizenship initiatives around the world, particularly focusing on improved access to medicines in the developing world through its Access to Medicine projects, including donations of medicines to patients affected by ], ], and ]; ] patient assistance programs; and relief to support major humanitarian organisations with emergency medical needs.<ref>http://www.corporatecitizenship.novartis.com Novartis corporate citizenship</ref> | * In 2006, ] committed USD 755 million in corporate citizenship initiatives around the world, particularly focusing on improved access to medicines in the developing world through its Access to Medicine projects, including donations of medicines to patients affected by ], ], and ]; ] patient assistance programs; and relief to support major humanitarian organisations with emergency medical needs.<ref>http://www.corporatecitizenship.novartis.com Novartis corporate citizenship</ref> | ||
| However, some NGOs such as ] do not routinely accept corporate donations of medicines. More precisely, they do not become reliant on such supplies of medicines because the supply is dependent upon the fluid, profit-driven charities of said pharmaceutical companies, and thus may dry up during a critical or otherwise important time. The book '']'' by ex-MSF president ] describes this in detail. | |||
| ==Pharmaceutical industry in popular culture== | |||
| As for many other major industries since the middle of the twentieth century, the pharmaceutical industry has been stereotyped as a global shadowy force in numerous western fiction works. Notorious films such as '']'' (1993) and '']'' and novels/films such as '']'' characterize this trend. | |||
| ==Industry associations== | |||
| * ] (EUCOPE) | |||
| * ] (DIA) | |||
| * ] | |||
| * ] (EFPIA) | |||
| * ] (EphMRA) | |||
| * ] (IFPMA) | |||
| * ] (JPMA) | |||
| * ] (NYHPC) | |||
| * ] (PhRMA) | |||
| * ] (IPHA) | |||
| ==Regulatory authorities== | |||
| {{Main|Regulation of therapeutic goods}} | |||
| * ] (ICH) | |||
| * ] (EMEA) | |||
| * ] (TGA) | |||
| * ] (FDA) | |||
| * ] | |||
| * ] (MHRA) | |||
| * ] (CDSCO) | |||
| * ] | |||
| * ] | |||
| * ] | |||
| == See also == | == See also == | ||
| * ] | |||
| {{Columns-list|2| | |||
| * '']'' (2012) by ] | |||
| * '']'' (2006) by Jacky Law | |||
| * ] | * ] | ||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| * ] | * ] | ||
| * ] | * ] | ||
| * '']'' (2008) by ] | |||
| }} | |||
| ==References== | ==References== | ||
| {{Reflist |
{{Reflist}} | ||
| ==Bibliography== | |||
| <!-- further reading items are candidates for becoming references upon addition of information to the main article --> | |||
| * Angell, Marcia. ''The truth about the drug companies''. Random House, New York, 2004, 305 S. ISBN 0-375-50846-5. | |||
| * Coyne, J. Lessons in conflict of interest: "The construction of the martyrdom of David Healy and the dilemma of bioethics." American Journal of Bioethics 5 (1): W3-W14, 2005. | |||
| * Greene, Jeremy A., and Scott H. Podolsky, "Keeping Modern in Medicine: Pharmaceutical Promotion and Physician Education in Postwar America," ''Bulletin of the History of Medicine,'' 83 (Summer 2009), 331–77 | |||
| * {{cite encyclopedia |last1=Henninger |first1=Daniel |authorlink= Daniel Henninger |editor= ] (ed.) |encyclopedia=] |title=Drug Lag |url=http://www.econlib.org/library/Enc1/DrugLag.html |year=2002 |edition= 1st |publisher=] }} {{OCLC|317650570|50016270|163149563}} | |||
| * Ajai R. Singh, Shakuntala A. Singh: , ], 2007, 5(1). Retrieved 2011-03-27. ISBN 978-81-89753-14-6 | |||
| ===Economics of the industry=== | |||
| * Merrill Goozner: ''''. University of California Press, Berkeley, 2004, 297 S. ISBN 0-520-23945-8. | |||
| ===Relationship between pharma and the medical profession=== | |||
| * Joanna Moncrieff, "", '']'', 27 June 2006. | |||
| * Jaconelli T, ", '']'', 2008. | |||
| * Jerome P Kassirer, ", '']'', 2007, 5(1), pp. 1–6. Retrieved 2011-03-27. | |||
| * Joel Lexchin, ", '']'', 2007, 5(1), pp. 7–10. Retrieved 2011-03-27. | |||
| ===Relationship between pharma and the nursing profession=== | |||
| * Lakeman, R. (2010). Mental health nursing is not for sale: rethinking nursing's relationship with the pharmaceutical industry. Journal of Psychiatric and Mental Health Nursing, 17(2), 172–177. | |||
| * Lakeman, R., & Cutcliffe, J. (2009). Misplaced epistemological certainty and pharmaco-centrism in mental health nursing. Journal of Psychiatric and Mental Health Nursing, 16(2), 199–205. | |||
| ===Relationship between pharma and consumers (general public)=== | |||
| * Ray Moynihan, Alan Cassels: ''Selling sickness: How the world's biggest pharmaceutical companies are turning us all into patients''. Nation Books, New York, 2005. | |||
| * Kornfield R, Donohue J, Berndt ER, Alexander GC. Changing promotion of prescription drugs to consumers and providers, 2001–2010. PLOS One. 2013;8:1-7. | |||
| ===Industry trends=== | |||
| * {{Cite news| last =Carlson | first =Bruce | date =2008-08-01 | title =Pharma Outsourcing on Upward Trajectory | periodical =Genetic Engineering & Biotechnology News | series =BioMarket Trends | publisher =Mary Ann Liebert | volume =28 | issue =14 | pages =14 | url =http://www.genengnews.com/articles/chitem.aspx?aid=2547 | issn =1937-8661 | accessdate =2008-09-26 | postscript =<!-- Bot retrieved archive -->}} | |||
| == External links == | |||
| * {{commonscat-inline}} | |||
| {{Pharmaceutical industry by country}} | {{Pharmaceutical industry by country}} | ||
| {{Pharmaceutical industry in the United Kingdom}} | {{Pharmaceutical industry in the United Kingdom}} | ||
| Line 406: | Line 252: | ||
| ] | ] | ||
| ] | ] | ||
| {{Link GA|ca}} | |||
Revision as of 21:09, 9 January 2015

The pharmaceutical industry develops, produces, and markets drugs or pharmaceuticals licensed for use as medications. Pharmaceutical companies are allowed to deal in generic or brand medications and medical devices. They are subject to a variety of laws and regulations regarding the patenting, testing and ensuring safety and efficacy and marketing of drugs.
History
Mid-1800's - 1945: From botanicals to the first synthetic drugs
The modern pharmaceutical industry traces its roots to two sources. The first of these are local apothecaries that expanded from their traditional role distributing botanical drugs such as morphine and quinine to wholesale manufacture in the mid 1800s. Multinational corporations including Merck, Hoffman-La Roche, Burroughs-Wellcome (now part of GlaxoSmithKline), Abbott Laboratories, Eli Lilly and Upjohn (now part of Pfizer) began their histories as local apothecary shops in the mid-1800s. By the late 1880s, German dye manufacturers had perfected the purification of individual organic compounds from coal tar and other mineral sources and had also established rudimentary methods in organic chemical synthesis. The development of synthetic chemical methods allowed scientists to systematically vary the structure of chemical substances, and growth in the emerging science of pharmacology expanded their ability to evaluate the biological effects of these structural changes.
Epinephrine, norepinephrine, and amphetamine
By the 1890s the profound effect of adrenal extracts on many different tissue types had been discovered, setting off a search both for the mechanism of chemical signalling and efforts to exploit these observations for the development of new drugs. The blood pressure raising and vasoconstrictive effects of adrenal extracts were of particular interest to surgeons as hemostatic agents and as treatment for shock, and a number of companies developed products based on adrenal extracts containing varying purities of the active substance. In 1897 John Abel of Johns Hopkins University identified the active principle as epinephrine, which he isolated in an impure state as the sulfate salt. Industrial chemist Jokichi Takamine later developed a method for obtaining epinephrine in a pure state, and licensed the technology to Parke Davis. Parke Davis marketed epinephrine under the trade name Adrenalin. Injected epinephrine proved to be especially efficacious for the acute treatment of asthma attacks, and an inhaled version was sold in the United States until 2011 (Primatene Mist). By 1929 epinephrine had been formulated into an inhaler for use in the treatment of nasal congestion.
While highly effective, the requirement for injection limited the use of norepinephrine and orally active derivatives were sought. A structurally similar compound, ephedrine, was identified by Japanese chemists in the Ma Huang plant and marketed by Eli Lilly as an oral treatment for asthma. Following the work of Henry Dale and George Barger at Burroughs-Wellcome, academic chemist Gordon Alles synthesized amphetamine in and tested in asthma patients in 1929. The drug proved to have only modest anti-asthma effects, but produced sensations of exhilaration and palpitations. Amphetamine was developed by Smith, Kline and French as a nasal decongestant under the trade name Benzedrine Inhaler. Amphetamine was eventually developed for the treatment of narcolepsy, post-encepheletic parkinsonism, and mood elevation in depression and other psychiatric indications. It receive approval as a New and Nonofficial Remedy from the American Medical Association for these uses in 1937 and remained in common use for depression until the development of tricyclic antidepressants in the 1960s.
Discovery and development of the barbiturates

In 1903 Hermann Emil Fischer and Joseph von Mering disclosed their discovery that diethylbarbituric acid, formed from the reaction of diethylmalonic acid, phosphorus oxychloride and urea, induces sleep in dogs. The discovery was patented and licensed to Bayer pharmaceuticals, which marketed the compound under the trade name Veronal as a sleep aid beginning in 1904. Systematic investigations of the effect of structural changes on potency and duration of action led to the discovery of phenobarbital at Bayer in 1911 and the discovery of its potent anti-epileptic activity in 1912. Phenobarbital was among the most widely used drugs for the treatment of epilepsy through the 1970s, and as of 2014, remains on the World Health Organizations list of essential medications. The 1950s and 1960s saw increased awareness of the addictive properties and abuse potential of barbiturates and amphetamines and led to increasing restrictions on their use and growing government oversight of prescribers. The major use of these drugs today is restricted to the use of amphetamine for the treatment of attention deficit disorder and phenobarbital for epilepsy.
Insulin
A series of experiments performed from the late 1800s to the early 1900s revealed that diabetes is caused by the absence of a substance normally produced by the pancreas. In 1869, Oscar Minkowski and Joseph von Mering found that diabetes could be induced in dogs by surgical removal of the pancreas. In 1921, Canadian professors Frederick Banting and his student Charles Best repeated this study, and found that injections of pancreatic extract reversed the symptoms produced by pancreas removal. The extract was demonstrated to work in people soon thereafter, but development of insulin therapy as a routine medical procedure was delayed by difficulties in producing the material in sufficient quantity and with reproducible purity. The researchers sought assistance from industrial collaborators at Eli Lilly and Co. based on the company's experience with large scale purification of biological materials. Chemist George Walden of Eli Lilly and Company found that careful adjustment of the pH of the extract allowed a relatively pure grade of insulin to be produced. Under pressure from Toronto University and a potential patent challenge by academic scientists who had independently developed a similar purification method, an agreement was reached for non-exclusive production of insulin by multiple companies. Prior to the discovery and widespread availability of insulin therapy the life expectancy of diabetics was only a few months.
Early anti-infective research - Salvarsan, Prontosil, Penicillin and Vaccines
The development of drugs for the treatment of infectious diseases was a major focus of early research and development efforts; in 1900 pneumonia, tuberculosis, and diarrhea were the three leading causes of death in the United States and mortality in the first year of life exceeded 10%.
In 1911 arsphenamine, the first synthetic anti-infective drug, was developed by Paul Ehrlich and chemist Alfred Bertheim of the Institute of Experimental Therapy in Berlin. The drug was given the commercial name Salvarsan. Ehrlich, noting both the general toxicity of arsenic and the selective absorption of certain dyes by bacteria, hypothesized that an arsenic-containing dye with similar selective absorption properties could be used to treat bacterial infections. Arsphenamine was prepared as part of a campaign to synthesize a series of such compounds, and found to exhibit partially selective toxicity. Arsphenamine proved to be the first effective treatment for syphilis, a disease which prior to that time was incurable and led inexorably to severe skin ulceration, neurological damage, and death.
Ehrlich’s approach of systematically varying the chemical structure of synthetic compounds and measuring the effects of these changes on biological activity was pursued broadly by industrial scientists, including Bayer scientists Josef Klarer, Fritz Mietzsch, and Gerhard Domagk. This work, also based in the testing of compounds available from the German dye industry, led to the discover of Prontosil, the first representative of the sulfonamide class of antibiotics. Compared to arsphenamine, the sulfonamides had a broader spectrum of activity and were far less toxic, rendering them useful for infections caused by pathogens such as streptococci. In 1939, Domagk received the Nobel Prize in Medicine for this discovery. Nonetheless, the dramatic decrease in deaths from infectious diseases that occurred prior to World War II was primarily the result of improved public health measures such as clean water and less crowded housing, and that the impact of anti-infective drugs and vaccines was significant mainly after World War II.
In 1928, Alexander Fleming discovered the antibacterial effects of penicillin, but its exploitation for the treatment of human disease awaited the development of methods for its large scale production and purification. These were developed by a U.S. and British government-led consortium of pharmaceutical companies during the Second World War.
Early progress toward the development of vaccines occurred throughout this period, primarily in the form of academic and government funded basic research directed toward the identification of the pathogens responsible for common communicable diseases. In 1885 Louis Pasteur and Pierre Paul Émile Roux created the first rabies vaccine. The first diphtheria vaccines were produced in 1914 from a mixture of diphtheria toxin and antitoxin (produced from the serum of an inoculated animal), but the safety of the inoculation was marginal and it was not widely used. The United States recorded 206,000 cases of diphtheria in 1921 resulting in 15,520 deaths. In 1923 parallel efforts by Gaston Ramon at the Pasteur Institute and Alexander Glenny at the Wellcome Research Laboratories (later part of GlaxoSmithKline) led to the discovery that a safer vaccine could be produced by treating diphtheria toxin with formaldehyde. In 1944, Maurice Hilleman of Squibb Pharmaceuticals developed the first vaccine against Japanese encephelitis. Hilleman would later move to Merck where he would play a key role in the development of vaccines against measles, mumps, chickenpox, rubella, hepatitis A, hepatitis B, and meningitis.
Unsafe drugs and early industry regulation

Prior to the beginning of the 20th century drugs were generally produced by small scale manufacturers with little regulatory control over manufacturing or claims of safety and efficacy. To the extent that such laws did exist, enforcement was lax. In the United States, increased regulation of vaccines and other biological drugs was spurred by tetanus outbreaks and deaths caused by the distribution of contaminated smallpox vaccine and diphtheria antitoxin. The Biologics Control Act of 1902 required that federal government grant premarket approval for every biological drug and for the process and facility producing such drugs. This was followed in 1906 by the Pure Food and Drugs Act, which forbade the interstate distribution of adulterated or misbranded foods and drugs. A drug was considered misbranded if it contained alcohol, morphine, opium, cocaine, or any of several other potentially dangerous or addictive drugs, and if its label failed to indicate the quantity or proportion of such drugs. The government's attempts to use the law to prosecute manufacturers for making unsupported claims of efficacy were undercut by a Supreme Court ruling restricting the federal government's enforcement powers to cases of incorrect specification of the drug's ingredients.
In 1937 over 100 people died after ingesting Elixir of Sulfanalimide manufactured by S.E. Massengill Company of Tennessee. The product was formulated in diethylene glycol, a highly toxic solvent that is now widely used as antifreeze. Under the laws extant at that time, prosecution of the manufacturer was possible only under the technicality that the product had been called an "elixir", which literally implied a solution in ethanol. In response to this episode, the U.S. Congress passed the Federal Food, Drug, and Cosmetic Act of 1938, which for the first time required pre-market demonstration of safety before a drug could be sold, and explicitly prohibited false therapeutic claims.
The Post-War Years, 1945-1970
Further advances in anti-infective research
The aftermath of the war saw an explosion in the discovery of new classes of antibacterial drugs including the cephalosporins (developed by Eli Lilly based on the seminal work of Giuseppe Brotzu and Edward Abraham), streptomycin (discovered during a Merck-funded research program in Selman Waksman's laboratory), the tetracyclines (discovered at Lederle Laboratories, now a part of Pfizer), erythromycin (discovered at Eli Lilly and Co.) and their extension to an increasingly wide range of bacterial pathogens.
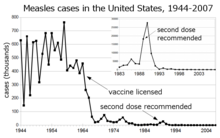
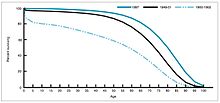
During the years 1940-1955, the rate of decline in the U.S. death rate accelerated from 2% per year to 8% per year, then returned to the historical rate of 2% per year. The dramatic decline in the immediate post-war years has been attributed to the rapid development of new treatments and vaccines for infectious disease that occurred during these years. Vaccine development continued to accelerate, with the most notable achievement of the period being Salk's 1954 development of the polio vaccine under the funding of the non-profit National Foundation for Infantile Paralysis. The vaccine process was never patented, but was instead given to pharmaceutical companies to manufacture as a low cost generic. In 1960 Maurice Hilleman of Merck, Sharpe and Dohme identified the SV40 virus, which was later shown to cause tumors in many mammalian species. It was later determined that SV40 was present as a contaminant in polio vaccine lots that had been administered to 90% of the children in the United States. The contamination appears to have originated both in the original cell stock and in monkey tissue used for production. In 2004 the United States Cancer Institute announced that it had concluded that SV40 is not associated with cancer in people.
Other notable new vaccines of the period include those for measles (1962, John Franklin Enders of Children's Medical Center Boston, later refined by Maurice Hilleman at Merck), Rubella (1969, Hilleman, Merck) and mumps (1967, Hilleman, Merck) The United States incidences of rubella, congenitial rubella syndrome, measles, and mumps all fell by >95% in the immediate aftermath of widespread vaccination. The first 20 years of licensed measles vaccination in the U.S. prevented an estimated 52 million cases of the disease, 17,400 cases of mental retardation, and 5,200 deaths.
Development and marketing of antihypertensive drugs
Hypertension is a risk factor for atherosclerosis, heart failure, coronary artery disease, stroke, renal disease, and peripheral arterial disease, and is the most important risk factor for cardiovascular morbidity and mortality, in industrialized countries. Prior to 1940 approximately 23% of all deaths among persons over age 50 were attributed to hypetension. Severe cases of hypertension were treated by surgery.
Early developments in the field of treating hypertension included quaternary ammonium ion sympathetic nervous system blocking agents, but these compounds were never widely used due to their severe side effects, because the long term health consequences of high blood pressure had not yet been established, and because they had to be administered by injection.
In 1952 researchers at Ciba discovered the first orally available vasodilator, hydrazaline. A major shortcoming of hydralazine monotherapy was that lost its effectiveness over time (tachyphylaxis). In the mid-1950’s Karl H. Beyer, James M. Sprague, John E. Baer, and Frederick C. Novello of Merck and Co. discovered and developed chlorothiazide, which remains the most widely used anthypertensive drug today. This development was associated with a substantial decline in the mortality rate among people with hypertension. The inventors were recognized by a Public Health Lasker Award in 1975 for “the saving of untold thousands of lives and the alleviation of the suffering of millions of victims of hypertension”.
A 2009 Cochrane review concluded that thiazide antihypertensive drugs reduce the risk of death (RR 0.89), stroke (RR 0.63), coronary heart disease (RR 0.84), and cardiovascular events (RR 0.70) in people with high blood pressure. In the ensuring years other classes of antihypertensive drug were developed and found wide acceptance in combination therapy, including loop diureteics (Lasix/furosemide, Hoechst Pharmaceuticals, 1963), beta blockers (ICI Pharmaceuticals, 1964) ACE inhibitors, and angiotensin receptor blockers. ACE inhibitors reduce the risk of new onset kidney disease and death in diabetic patients, irrespective of whether they have hypertension.
Numerous new drugs were developed during the 1950s and mass-produced and marketed through the 1960s. These included the first oral contraceptive, "The Pill", Cortisone, blood-pressure drugs and other heart medications. MAO inhibitors, chlorpromazine (Thorazine), haloperidol (Haldol) and the tranquilizers ushered in the age of psychiatric medication. Diazepam (Valium), discovered in 1960, was marketed from 1963 and rapidly became the most prescribed drug in history, prior to controversy over dependency and habituation.
Thalidomide and the Kefauver-Harris Amendments

In the U.S., a push for revisions of the FD&C Act emerged from Congressional hearings led by Senator Estes Kefauver of Tennessee in 1959. The hearings covered a wide range of policy issues, including advertising abuses, questionable efficacy of drugs, and the need for greater regulation of the industry. While momentum for new legislation temporarily flagged under extended debate, a new tragedy became apparent that underscored the need for more comprehensive regulation and provided the driving force for the passage of new laws.
On September 12, 1960, an American licensee, the William S. Merrell Company of Cincinnati, submitted to FDA a new drug application for Kevadon (thalidomide), the brand name of a sedative that had been marketed in Europe since 1956: thalidomide. The FDA medical officer in charge of this review, Frances Kelsey, believed the data were incomplete to support the safety of this drug.
The firm continued to pressure Kelsey and the agency to approve the application—until November 1961, when the drug was pulled off the German market because of its association with grave congenital abnormalities. Several thousand newborns in Europe and elsewhere suffered the teratogenic effects of thalidomide. Though the drug was never approved in this country, the firm distributed Kevadon to over 1,000 physicians under the guise of investigational use. Over 20,000 Americans received thalidomide in this "study," including 624 pregnant patients, and about 17 known newborns suffered the effects of the drug.
The thalidomide tragedy resurrected Kefauver's bill to enhance drug regulation that had stalled in Congress, and the Kefauver-Harris Amendment became law on October 10, 1962. Manufacturers henceforth had to prove to FDA that their drugs were effective as well as safe before they could go on the market. FDA received authority to regulate advertising of prescription drugs and to establish good manufacturing practices. Finally, the law required that all drugs introduced between 1938 and 1962 had to be effective. An FDA - National Academy of Sciences collaborative study showed that nearly 40 percent of these products were not effective. A similarly comprehensive study of over-the-counter products began ten years later.
1970-1980
Cancer drugs were a feature of the 1970s. From 1978, India took over as the primary center of pharmaceutical production without patent protection.
The industry remained relatively small scale until the 1970s when it began to expand at a greater rate. Legislation allowing for strong patents, to cover both the process of manufacture and the specific products, came into force in most countries. By the mid-1980s, small biotechnology firms were struggling for survival, which led to the formation of mutually beneficial partnerships with large pharmaceutical companies and a host of corporate buyouts of the smaller firms. Pharmaceutical manufacturing became concentrated, with a few large companies holding a dominant position throughout the world and with a few companies producing medicines within each country.
The pharmaceutical industry entered the 1980s pressured by economics and a host of new regulations, both safety and environmental, but also transformed by new DNA chemistries and new technologies for analysis and computation. Drugs for heart disease and for AIDS were a feature of the 1980s, involving challenges to regulatory bodies and a faster approval process.
1980-Today
Controversies emerged around adverse effects, notably regarding Vioxx in the US, and marketing tactics. Pharmaceutical companies became increasingly accused of disease mongering or over-medicalizing personal or social problems.
Since 2008, pharmaceutical companies have been increasing the cost of name-brand prescriptions to offset declining revenues as out-of-patent drugs become available as generics. Simultaneously, pharmaceutical manufacturers are taking increasing advantage of tax havens to avoid taxation.
Research and development
Main articles: Drug discovery and Drug developmentDrug discovery is the process by which potential drugs are discovered or designed. In the past most drugs have been discovered either by isolating the active ingredient from traditional remedies or by serendipitous discovery. Modern biotechnology often focuses on understanding the metabolic pathways related to a disease state or pathogen, and manipulating these pathways using molecular biology or biochemistry. A great deal of early-stage drug discovery has traditionally been carried out by universities and research institutions.
Drug development refers to activities undertaken after a compound is identified as a potential drug in order to establish its suitability as a medication. Objectives of drug development are to determine appropriate formulation and dosing, as well as to establish safety. Research in these areas generally includes a combination of in vitro studies, in vivo studies, and clinical trials. The amount of capital required for late stage development has made it a historical strength of the larger pharmaceutical companies.
Often, large multinational corporations exhibit vertical integration, participating in a broad range of drug discovery and development, manufacturing and quality control, marketing, sales, and distribution. Smaller organizations, on the other hand, often focus on a specific aspect such as discovering drug candidates or developing formulations. Often, collaborative agreements between research organizations and large pharmaceutical companies are formed to explore the potential of new drug substances. More recently, multi-nationals are increasingly relying on contract research organizations to manage drug development.
The cost of innovation
Drug discovery and development is very expensive; of all compounds investigated for use in humans only a small fraction are eventually approved in most nations by government appointed medical institutions or boards, who have to approve new drugs before they can be marketed in those countries. In 2010 18 NMEs (New Molecular Entities) were approved and three biologics by the FDA, or 21 in total, which is down from 26 in 2009 and 24 in 2008. On the other hand, there were only 18 approvals in total in 2007 and 22 back in 2006. Since 2001, the Center for Drug Evaluation and Research has averaged 22.9 approvals a year. This approval comes only after heavy investment in pre-clinical development and clinical trials, as well as a commitment to ongoing safety monitoring. Drugs which fail part-way through this process often incur large costs, while generating no revenue in return. If the cost of these failed drugs is taken into account, the cost of developing a successful new drug (new chemical entity, or NCE), has been estimated at about 1.3 billion USD(not including marketing expenses). Professors Light and Lexchin reported in 2012, however, that the rate of approval for new drugs has been a relatively stable average rate of 15 to 25 for decades.
Industry-wide research and investment reached a record $65.3 billion in 2009. While the cost of research in the U.S. was about $34.2 billion between 1995 and 2010, revenues rose faster (revenues rose by $200.4 billion in that time).
A study by the consulting firm Bain & Company reported that the cost for discovering, developing and launching (which factored in marketing and other business expenses) a new drug (along with the prospective drugs that fail) rose over a five-year period to nearly $1.7 billion in 2003. According to Forbes, development costs between $4 billion to $11 billion per drug.
Some of these estimates also take into account the opportunity cost of investing capital many years before revenues are realized (see Time-value of money). Because of the very long time needed for discovery, development, and approval of pharmaceuticals, these costs can accumulate to nearly half the total expense. Some approved drugs, such as those based on re-formulation of an existing active ingredient (also referred to as Line-extensions) are much less expensive to develop.
Controversies
Due to repeated accusations and findings that some clinical trials conducted or funded by pharmaceutical companies may report only positive results for the preferred medication, the industry has been looked at much more closely by independent groups and government agencies.
In response to specific cases in which unfavorable data from pharmaceutical company-sponsored research was not published, the Pharmaceutical Research and Manufacturers of America have published new guidelines urging companies to report all findings and limit the financial involvement in drug companies of researchers. US congress signed into law a bill which requires phase II and phase III clinical trials to be registered by the sponsor on the clinicaltrials.gov website run by the NIH.
Drug researchers not directly employed by pharmaceutical companies often look to companies for grants, and companies often look to researchers for studies that will make their products look favorable. Sponsored researchers are rewarded by drug companies, for example with support for their conference/symposium costs. Lecture scripts and even journal articles presented by academic researchers may actually be "ghost-written" by pharmaceutical companies.
An investigation by ProPublica found that at least 21 doctors have been paid more than $500,000 for speeches and consulting by drugs manufacturers since 2009, with half of the top earners working in psychiatry, and about $2 billion in total paid to doctors for such services. AstraZeneca, Johnson & Johnson and Eli Lilly have paid billions of dollars in federal settlements over allegations that they paid doctors to promote drugs for unapproved uses. Some prominent medical schools have since tightened rules on faculty acceptance of such payments by drug companies.
Product approval
Main article: Food and Drug AdministrationIn the United States, new pharmaceutical products must be approved by the Food and Drug Administration (FDA) as being both safe and effective. This process generally involves submission of an Investigational New Drug filing with sufficient pre-clinical data to support proceeding with human trials. Following IND approval, three phases of progressively larger human clinical trials may be conducted. Phase I generally studies toxicity using healthy volunteers. Phase II can include Pharmacokinetics and Dosing in patients, and Phase III is a very large study of efficacy in the intended patient population. Following the successful completion of phase III testing, a New Drug Application is submitted to the FDA. The FDA review the data and if the product is seen as having a positive benefit-risk assessment, approval to market the product in the US is granted.
A fourth phase of post-approval surveillance is also often required due to the fact that even the largest clinical trials cannot effectively predict the prevalence of rare side-effects. Postmarketing surveillance ensures that after marketing the safety of a drug is monitored closely. In certain instances, its indication may need to be limited to particular patient groups, and in others the substance is withdrawn from the market completely.
The FDA provides information about approved drugs at the Orange Book site.
In many non-US western countries a 'fourth hurdle' of cost effectiveness analysis has developed before new technologies can be provided. This focuses on the efficiency (in terms of the cost per QALY) of the technologies in question rather than their efficacy. In England NICE approval requires technologies be made available by the NHS, whilst similar arrangements exist with the Scottish Medicines Consortium in Scotland and the Pharmaceutical Benefits Advisory Committee in Australia. A product must pass the threshold for cost-effectiveness if it is to be approved. Treatments must represent 'value for money' and a net benefit to society. There is much speculation that a NICE style framework may be implemented in the USA in an attempt to decrease Medicare and Medicaid spending by balancing benefits to patients versus profits for the medical industry.
In the UK, the British National Formulary is the core guide for pharmacists and clinicians.
Orphan drugs
Main article: Orphan drugThere are special rules for certain rare diseases ("orphan diseases") involving fewer than 200,000 patients in the United States, or larger populations in certain circumstances. Because medical research and development of drugs to treat such diseases is financially disadvantageous, companies that do so are rewarded with tax reductions, fee waivers, and market exclusivity on that drug for a limited time (seven years), regardless of whether the drug is protected by patents.
Legal issues
Where pharmaceutics have been shown to cause side-effects, civil action has occurred, especially in countries where tort payouts are likely to be large. The top 20 pharmaceutical cases account for over $16 billion in recoveries. Due to high-profile cases leading to large compensations, most pharmaceutical companies endorse tort reform. Recent controversies have involved Vioxx and SSRI antidepressants.
Industry revenues
For the first time ever, in 2011, global spending on prescription drugs topped $954 billion, even as growth slowed somewhat in Europe and North America. The United States accounts for more than a third of the global pharmaceutical market, with $340 billion in annual sales followed by the EU and Japan.(pdf) Emerging markets such as China, Russia, South Korea and Mexico outpaced that market, growing a huge 81 percent. According to IMS the global pharmaceutical industry can reach to US$1.1 trillion by 2014.
The top ten best-selling drugs of 2013 totaled $75.6 billion in sales, with the anti-inflammatory drug Humira being the best-selling drug world wide at $10.7 billion in sales. The second and third best selling were Enbrel and Remicade, respectively. The top three best-selling drugs in the United States in 2013 were Abilify ($6.3 billion,) Nexium ($6 billion) and Humira ($5.4 billion). The best-selling drug ever, Lipitor, averaged $13 billion annually and netted $141 billion total over its lifetime before Pfizer's patent expired in November 2011.
IMS Health publishes an analysis of trends expected in the pharmaceutical industry in 2007, including increasing profits in most sectors despite loss of some patents, and new 'blockbuster' drugs on the horizon.
Teradata Magazine predicted that by 2007, $40 billion in U.S. sales could be lost at the top 10 pharmaceutical companies as a result of slowdown in R&D innovation and the expiry of patents on major products, with 19 blockbuster drugs losing patent. As the number of patents that expire accumulates faster than the number of marketed drugs, this amount is expected to increase even more in the near future.
Patents and generics
Depending on a number of considerations, a company may apply for and be granted a patent for the drug, or the process of producing the drug, granting exclusivity rights typically for about 20 years. However, only after rigorous study and testing, which takes 10 to 15 years on average, will governmental authorities grant permission for the company to market and sell the drug. Patent protection enables the owner of the patent to recover the costs of research and development through high profit margins for the branded drug. When the patent protection for the drug expires, a generic drug is usually developed and sold by a competing company. The development and approval of generics is less expensive, allowing them to be sold at a lower price. Often the owner of the branded drug will introduce a generic version before the patent expires in order to get a head start in the generic market. Restructuring has therefore become routine, driven by the patent expiration of products launched during the industry's 'golden era' in the 1990s and companies' failure to develop sufficient new blockbuster products to replace lost revenues.
.
Prescriptions
In the U.S., prescriptions have increased over the past decade to 3.4 billion annually, a 61 percent increase. Retail sales of prescription drugs jumped 250 percent from $72 billion to $250 billion, while the average price of prescriptions has more than doubled from $30 to $68.
Marketing
Advertising is common in healthcare journals as well as through more mainstream media routes. In some countries, notably the US, they are allowed to advertise directly to the general public. Pharmaceutical companies generally employ sales people (often called 'drug reps' or, an older term, 'detail men') to market directly and personally to physicians and other healthcare providers. In some countries, notably the US, pharmaceutical companies also employ lobbyists to influence politicians. Marketing of prescription drugs in the US is regulated by the federal Prescription Drug Marketing Act of 1987.
To healthcare professionals
In 2008, Senator Charles Grassley began an investigation about unreported payments to physicians by pharmaceutical companies. Grassley led a Congressional Investigation which found that well-known university psychiatrists, who had promoted psychoactive drugs, had violated federal and university regulations by failing to report $1.6 million in consulting income from the pharmaceutical companies which made the drugs. Weeks later, Business Week reported that Grassley alleged that Alan Schatzberg, chair of psychiatry at Stanford University, had underreported his investments in Corcept Therapeutics, a company he founded. Dr. Schatzberg had reported only $100,000 investments in Corcept, but Grassley stated that his investments actually totalled over $6 million. Dr. Schaztberg later stepped down from his grant which is funded by the National Institutes of Health (NIH). Similarly, Dr. Charles Nemeroff resigned as chair of the psychiatry department at Emory University after failing to report a third of the $2.8 million in consulting fees he received from GlaxoSmithKline. At the time he received these fees, Dr. Nemeroff had been principal investigator of a $3.9 million NIH grant evaluating five medications for depression manufactured by GlaxoSmithKline.
The book Bad Pharma also discusses the influence of drug representatives, how ghostwriters are employed by the drug companies to write papers for academics to publish, how independent the academic journals really are, how the drug companies finance doctors' continuing education, and how patients' groups are often funded by industry.
Direct to consumer advertising
Main article: Direct-to-consumer advertisingSince the 1980s new methods of marketing for prescription drugs to consumers have become important. Direct-to-consumer media advertising was legalised in the FDA Guidance for Industry on Consumer-Directed Broadcast Advertisements.
Internationally, many pharmaceutical companies market directly to the consumer rather than going through a conventional retail sales channel.
Controversy about drug marketing and lobbying
There has been increasing controversy surrounding pharmaceutical marketing and influence. There have been accusations and findings of influence on doctors and other health professionals through drug reps, including the constant provision of marketing 'gifts' and biased information to health professionals; highly prevalent advertising in journals and conferences; funding independent healthcare organizations and health promotion campaigns; lobbying physicians and politicians (more than any other industry in the US); sponsorship of medical schools or nurse training; sponsorship of continuing educational events, with influence on the curriculum; and hiring physicians as paid consultants on medical advisory boards.
Some advocacy groups, such as No Free Lunch, have criticized the effect of drug marketing to physicians because they say it biases physicians to prescribe the marketed drugs even when others might be cheaper or better for the patient.
There have been related accusations of disease mongering (over-medicalising) to expand the market for medications. An inaugural conference on that subject took place in Australia in 2006. In 2009, the Government-funded National Prescribing Service launched the "Finding Evidence – Recognising Hype" program, aimed at educating GPs on methods for independent drug analysis.
A 2005 review by a special committee of the UK government came to all the above conclusions in a European Union context whilst also highlighting the contributions and needs of the industry.
Meta-analyses have shown that psychiatric studies sponsored by pharmaceutical companies are several times more likely to report positive results, and if a drug company employee is involved the effect is even larger. Influence has also extended to the training of doctors and nurses in medical schools, which is being fought.
It has been argued that the design of the Diagnostic and Statistical Manual of Mental Disorders and the expansion of the criteria represents an increasing medicalization of human nature, or "disease mongering", driven by drug company influence on psychiatry. The potential for direct conflict of interest has been raised, partly because roughly half the authors who selected and defined the DSM-IV psychiatric disorders had or previously had financial relationships with the pharmaceutical industry. The president of the organization that designs and publishes the DSM, the American Psychiatric Association, stated in 2005 that in general American psychiatry has "allowed the biopsychosocial model to become the bio-bio-bio model" and that the gifts from drug reps are little more than "kickbacks and bribes".
In the US, starting in 2013, under the Physician Financial Transparency Reports (part of the Sunshine Act), the Centers for Medicare & Medicaid Services has to collect information from applicable manufacturers and group purchasing organizations in order to report information about their financial relationships with physicians and hospitals. Data are made public in the Centers for Medicare & Medicaid Services website. The expectation is that relationship between doctors and Pharmaceutical industry will become fully transparent.
Regulatory issues
Ben Goldacre has argued that regulators – such as the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK, or the Food and Drug Administration (FDA) in the United States – advance the interests of the drug companies rather than the interests of the public due to revolving door exchange of employees between the regulator and the companies and friendships develop between regulator and company employees. He argues that regulators do not require that new drugs offer an improvement over what is already available, or even that they be particularly effective.
Others have argued that excessive regulation suppresses therapeutic innovation, and that the current cost of regulator-required clinical trials prevents the full exploitation of new genetic and biological knowledge for the treatment of human disease. A 2012 report by the President's Council of Advisors on Science and Technology made several key recommendations to reduce regulatory burdens to new drug development, including 1) expanding the FDA's use of accelerated approval processes, 2) creating an expedited approval pathway for drugs intended for use in narrowly defined populations, and 3) undertaking pilot projects designed to evaluate the feasibility of a new, adaptive drug approval process.
Pharmaceutical fraud
See also: List of largest pharmaceutical settlements in the United StatesPharmaceutical fraud involves activities that result in false claims to insurers or programs such as Medicare in the United States or equivalent state programs for financial gain to a pharmaceutical company. There are several different schemes used to defraud the health care system which are particular to the pharmaceutical industry. These include: Good Manufacturing Practice (GMP) Violations, Off Label Marketing, Best Price Fraud, CME Fraud, Medicaid Price Reporting, and Manufactured Compound Drugs. Of this amount $2.5 billion was recovered through False Claims Act cases in FY 2010. Examples of fraud cases include the GlaxoSmithKline $3 billion settlement, Pfizer $2.3 billion settlement and Merck & Co. $650 million settlement. Damages from fraud can be recovered by use of the False Claims Act, most commonly under the qui tam provisions which rewards an individual for being a "whistleblower", or relator (law).
Every major company selling the antipsychotics — Bristol-Myers Squibb, Eli Lilly, Pfizer, AstraZeneca and Johnson & Johnson — has either settled recent government cases, under the False Claims Act, for hundreds of millions of dollars or is currently under investigation for possible health care fraud. Following charges of illegal marketing, two of the settlements set records last year for the largest criminal fines ever imposed on corporations. One involved Eli Lilly's antipsychotic Zyprexa, and the other involved Bextra. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, Geodon; Pfizer settled that part of the claim for $301 million, without admitting any wrongdoing.
On 2 July 2012, GlaxoSmithKline pleaded guilty to criminal charges and agreed to a $3 billion settlement of the largest health-care fraud case in the U.S. and the largest payment by a drug company. The settlement is related to the company's illegal promotion of prescription drugs, its failure to report safety data, bribing doctors, and promoting medicines for uses for which they were not licensed. The drugs involved were Paxil, Wellbutrin, Advair, Lamictal, and Zofran for off-label, non-covered uses. Those and the drugs Imitrex, Lotronex, Flovent, and Valtrex were involved in the kickback scheme.
The following is a list of the four largest settlements reached with pharmaceutical companies from 1991 to 2012, rank ordered by the size of the total settlement. Legal claims against the pharmaceutical industry have varied widely over the past two decades, including Medicare and Medicaid fraud, off-label promotion, and inadequate manufacturing practices.
| Company | Settlement | Violation(s) | Year | Product(s) | Laws allegedly violated (if applicable) |
|---|---|---|---|---|---|
| GlaxoSmithKline | $3 billion | Off-label promotion/ failure to disclose safety data |
2012 | Avandia/Wellbutrin/Paxil | False Claims Act/FDCA |
| Pfizer | $2.3 billion | Off-label promotion/kickbacks | 2009 | Bextra/Geodon/ Zyvox/Lyrica |
False Claims Act/FDCA |
| Abbott Laboratories | $1.5 billion | Off-label promotion | 2012 | Depakote | False Claims Act/FDCA |
| Eli Lilly | $1.4 billion | Off-label promotion | 2009 | Zyprexa | False Claims Act/FDCA |
Developing world
Patents
Patents have been criticized in the developing world, as they are thought to reduce access to existing medicines. Reconciling patents and universal access to medicine would require an efficient international policy of price discrimination. Moreover, under the TRIPS agreement of the World Trade Organization, countries must allow pharmaceutical products to be patented. In 2001, the WTO adopted the Doha Declaration, which indicates that the TRIPS agreement should be read with the goals of public health in mind, and allows some methods for circumventing pharmaceutical monopolies: via compulsory licensing or parallel imports, even before patent expiration.
In March 2001, 40 multi-national pharmaceutical companies brought litigation against South Africa for its Medicines Act, which allowed the generic production of antiretroviral drugs (ARVs) for treating HIV, despite the fact that these drugs were on-patent. HIV was and is an epidemic in South Africa, and ARVs at the time cost between 10,000 and 15,000 USD per patient per year. This was unaffordable for most South African citizens, and so the South African government committed to providing ARVs at prices closer to what people could afford. To do so, they would need to ignore the patents on drugs and produce generics within the country (using a compulsory license), or import them from abroad. After international protest in favour of public health rights (including the collection of 250,000 signatures by MSF), the governments of several developed countries (including The Netherlands, Germany, France, and later the US) backed the South African government, and the case was dropped in April of that year.
Charitable programs
Charitable programs and drug discovery & development efforts are routinely undertaken by pharmaceutical companies. Some examples include:
- "Merck's Gift," wherein billions of river blindness drugs were donated in Africa
- Pfizer's gift of free/discounted fluconazole and other drugs for AIDS in South Africa
- GSK's commitment to give free albendazole tablets to the WHO for, and until, the elimination of lymphatic filariasis worldwide.
- In 2006, Novartis committed USD 755 million in corporate citizenship initiatives around the world, particularly focusing on improved access to medicines in the developing world through its Access to Medicine projects, including donations of medicines to patients affected by leprosy, tuberculosis, and malaria; Glivec patient assistance programs; and relief to support major humanitarian organisations with emergency medical needs.
See also
- Big Pharma conspiracy theory
- Clinical trial
- Drug development
- Drug discovery
- List of pharmaceutical companies
- Pharmaceutical marketing
- Pharmacy
References
- John L. McGuire, Horst Hasskarl, Gerd Bode, Ingrid Klingmann, Manuel Zahn "Pharmaceuticals, General Survey" Ullmann's Encyclopedia of Chemical Technology" Wiley-VCH, Weinheim, 2007. doi:10.1002/14356007.a19_273.pub2
- "Top Pharmaceuticals: Introduction: EMERGENCE OF PHARMACEUTICAL SCIENCE AND INDUSTRY: 1870-1930".
- Walter Sneader (31 October 2005). Drug Discovery: A History. John Wiley & Sons. pp. 155–156. ISBN 978-0-470-01552-0.
- ^ Rasmussen, Nicolas (2006). "Making the First Anti-Depressant: Amphetamine in American Medicine, 1929-1950". J Hist Med Allied Sci. 61 (3): 288–323. doi:10.1093/jhmas/jrj039.
{{cite journal}}:|access-date=requires|url=(help) - Yasiry Z, Shorvon SD (December 2012). "How phenobarbital revolutionized epilepsy therapy: the story of phenobarbital therapy in epilepsy in the last 100 years". Epilepsia. 53 Suppl 8: 26–39. doi:10.1111/epi.12026. PMID 23205960.
- López-Muñoz F, Ucha-Udabe R, Alamo C (December 2005). "The history of barbiturates a century after their clinical introduction". Neuropsychiatr Dis Treat. 1 (4): 329–43. PMC 2424120. PMID 18568113.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Drug Abuse Control Amendments of 1965". NEJM. 273: 1222–1223. 25 November 1965. doi:10.1056/NEJM196511252732213.
Officers of the Food and Drug Administration, aware of the seriousness of the problem, estimate that approximately half the 9,000,000,000 barbiturate and amphetamine capsules and tablets manufactured annually in this country are diverted to illegal use. The profits to be gained from the illegal sale of these drugs have proved an attraction to organized crime, for amphetamine can be purchased at wholesale for less than $1 per 1000 capsules, but when sold on the illegal market, it brings $30 to $50 per 1000 and when retailed to the individual buyer, a tablet may bring as much as 10 to 25 cents.
{{cite journal}}:|access-date=requires|url=(help) - "Sedative-Hypnotic Drugs — The Barbiturates — I". NEJM. 255: 1150–1151. 1956. doi:10.1056/NEJM195612132552409.
THE barbiturates, introduced into medicine by E. Fischer and J. von Mering1 in 1903, are certainly among the most widely used and abused drugs in medicine. Approximately 400 tons of these agents are manufactured each year; this is enough to put approximately 9,000,000 people to sleep each night for that period if each were given a 0.1-gm. dose
{{cite journal}}:|access-date=requires|url=(help) - Rosenfeld L (December 2002). "Insulin: discovery and controversy". Clin. Chem. 48 (12): 2270–88. PMID 12446492.
- ^ "www.cdc.gov" (PDF).
- "www.cdc.gov" (PDF).
- Sepkowitz KA (July 2011). "One hundred years of Salvarsan". N. Engl. J. Med. 365 (4): 291–3. doi:10.1056/NEJMp1105345. PMID 21793743.
- Aminov RI (2010). "A brief history of the antibiotic era: lessons learned and challenges for the future". Front Microbiol. 1: 134. doi:10.3389/fmicb.2010.00134. PMC 3109405. PMID 21687759.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Thomas Hager, The Demon Under the Microscope (2006) ISBN 1-4000-8213-7 (cited in "The Saga of a Sulfa Drug Pioneer" – NPR Weekend Edition 23 December 2006)
- NobelPrize.org
- ^ "www.nber.org" (PDF).
- ^ Klein, Herbert (2012). A Population History of the United States. Cambridge University Press. p. 167.
{{cite book}}:|access-date=requires|url=(help) - Chemical Heritage Manufacturing a Cure: Mass Producing Penicillin
- John Parascandola (1980). The History of antibiotics: a symposium. American Institute of the History of Pharmacy No. 5. ISBN 0-931292-08-5.
- "Diphtheria — Timelines — History of Vaccines".
- "Maurice R. Hilleman, 85; Scientist Developed Many Vaccines That Saved Millions of Lives - Los Angeles Times".
- "Significant Dates in U.S. Food and Drug Law History".
- "FDAReview.org, a project of The Independent Institute".
- "Sulfanilamide Disaster".
- "FDA History - Part II".
- Zaffiri L, Gardner J, Toledo-Pereyra LH (April 2012). "History of antibiotics. From salvarsan to cephalosporins". J Invest Surg. 25 (2): 67–77. doi:10.3109/08941939.2012.664099. PMID 22439833.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hamilton-Miller JM (March 2008). "Development of the semi-synthetic penicillins and cephalosporins". Int. J. Antimicrob. Agents. 31 (3): 189–92. doi:10.1016/j.ijantimicag.2007.11.010. PMID 18248798.
- Abraham EP (1987). "Cephalosporins 1945-1986". Drugs. 34 Suppl 2: 1–14. PMID 3319494.
- Kingston W (July 2004). "Streptomycin, Schatz v. Waksman, and the balance of credit for discovery". J Hist Med Allied Sci. 59 (3): 441–62. PMID 15270337.
- Nelson ML, Levy SB (December 2011). "The history of the tetracyclines". Ann. N. Y. Acad. Sci. 1241: 17–32. doi:10.1111/j.1749-6632.2011.06354.x. PMID 22191524.
- "ERYTHROMYCIN". Br Med J. 2 (4793): 1085–6. November 1952. PMC 2022076. PMID 12987755.
- "Editing Pharmaceutical industry (section) - Misplaced Pages, the 💕".
- SWEET BH, HILLEMAN MR (November 1960). "The vacuolating virus, S.V. 40". Proc. Soc. Exp. Biol. Med. 105: 420–7. PMID 13774265.
- Shah K, Nathanson N (January 1976). "Human exposure to SV40: review and comment". Am. J. Epidemiol. 103 (1): 1–12. PMID 174424.
- "Studies:No Evidence That SV40 is Related to Cancer - National Cancer Institute".
- "History of Vaccines — A Vaccine History Project of The College of Physicians of Philadelphia".
- "Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013".
- Bloch AB, Orenstein WA, Stetler HC; et al. (1985). "Health impact of measles vaccination in the United States". Pediatrics. 76 (4): 524–32. PMID 3931045.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Insull W (January 2009). "The pathology of atherosclerosis: plaque development and plaque responses to medical treatment". The American Journal of Medicine. 122 (1 Suppl): S3 – S14. doi:10.1016/j.amjmed.2008.10.013. PMID 19110086. Retrieved 20 June 2009.
- Gaddam KK, Verma A, Thompson M, Amin R, Ventura H (May 2009). "Hypertension and cardiac failure in its various forms". The Medical Clinics of North America. 93 (3): 665–80. doi:10.1016/j.mcna.2009.02.005. PMID 19427498. Retrieved 20 June 2009.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Agabiti-Rosei E (September 2008). "From macro- to microcirculation: benefits in hypertension and diabetes". Journal of Hypertension. 26 Suppl 3: S15–21. doi:10.1097/01.hjh.0000334602.71005.52. PMID 18815511. Retrieved 20 June 2009.
- Murphy BP, Stanton T, Dunn FG (May 2009). "Hypertension and myocardial ischemia". The Medical Clinics of North America. 93 (3): 681–95. doi:10.1016/j.mcna.2009.02.003. PMID 19427499. Retrieved 20 June 2009.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - White WB (May 2009). "Defining the problem of treating the patient with hypertension and arthritis pain". The American Journal of Medicine. 122 (5 Suppl): S3–9. doi:10.1016/j.amjmed.2009.03.002. PMID 19393824. Retrieved 20 June 2009.
- Truong LD, Shen SS, Park MH, Krishnan B (February 2009). "Diagnosing nonneoplastic lesions in nephrectomy specimens". Archives of Pathology & Laboratory Medicine. 133 (2): 189–200. doi:10.1043/1543-2165-133.2.189. PMID 19195963. Retrieved 20 June 2009.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Tracy RE, White S (February 2002). "A method for quantifying adrenocortical nodular hyperplasia at autopsy: some use of the method in illuminating hypertension and atherosclerosis". Annals of Diagnostic Pathology. 6 (1): 20–9. doi:10.1053/adpa.2002.30606. PMID 11842376. Retrieved 20 June 2009.
- Aronow WS (August 2008). "Hypertension and the older diabetic". Clinics in Geriatric Medicine. 24 (3): 489–501, vi–vii. doi:10.1016/j.cger.2008.03.001. PMID 18672184. Retrieved 20 June 2009.
- Gardner AW, Afaq A (2008). "MANAGEMENT OF LOWER EXTREMITY PERIPHERAL ARTERIAL DISEASE". Journal of Cardiopulmonary Rehabilitation and Prevention. 28 (6): 349–57. doi:10.1097/HCR.0b013e31818c3b96. PMC 2743684. PMID 19008688. Retrieved 20 June 2009.
- Novo S, Lunetta M, Evola S, Novo G (January 2009). "Role of ARBs in the blood hypertension therapy and prevention of cardiovascular events". Current Drug Targets. 10 (1): 20–5. doi:10.2174/138945009787122897. PMID 19149532. Retrieved 20 June 2009.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Craig WM (1939). "Surgical Treatment of Hypertension". Br Med J. 2 (4120): 1215–9. PMC 2178707. PMID 20782854.
- Sneader, Walter (2005). Drug Discovery. A History. New York: Wiley. p. 371.
{{cite book}}:|access-date=requires|url=(help) - Beyer KH (1993). "Chlorothiazide. How the thiazides evolved as antihypertensive therapy". Hypertension. 22 (3): 388–91. PMID 8349332.
- BORHANI NO, HECHTER HH (1964). "RECENT CHANGES IN CVR DISEASE MORTALITY IN CALIFORNIA". Public Health Rep. 79: 147–60. PMC 1915335. PMID 14119789.
- "The Lasker Foundation - Awards".
- Wright JM, Musini VM (2009). "First-line drugs for hypertension". Cochrane Database Syst Rev (3): CD001841. doi:10.1002/14651858.CD001841.pub2. PMID 19588327.
- Stason WB, Cannon PJ, Heinemann HO, Laragh JH (November 1966). "Furosemide. A clinical evaluation of its diuretic action". Circulation. 34 (5): 910–20. PMID 5332332.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC (1964). "A new adrenergic betareceptor antagonist". The Lancet. 283 (7342): 1080–1081. doi:10.1016/S0140-6736(64)91275-9. PMID 14132613.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lv J, Perkovic V, Foote CV, Craig ME, Craig JC, Strippoli GF (2012). "Antihypertensive agents for preventing diabetic kidney disease". Cochrane Database Syst Rev. 12: CD004136. doi:10.1002/14651858.CD004136.pub3. PMID 23235603.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Brochure: The History of Drug Regulation in the United States".
- Boldrin & Levine. "9". Against Intellectual Monopoly (PDF).
- ^ Ray Moynihan and Alan Cassels (2005). Selling Sickness: How Drug Companies are Turning Us All Into Patients. Allen & Unwin. New York. ISBN 1-74114-579-1
- "Chart of the day: brand vs. generic drug price growth" The Incidental Economist November 29, 2012
- "A New Rx for Tax Bills: Shuffling Sales Abroad, Rates for Big Drug Firms Are Dropping" Wall Street Journal, February 6, 2013
- "Annual Impact Report". Tufts Center for the Study of Drug Development.
{{cite journal}}: Cite journal requires|journal=(help) - http://www.outsourcing-pharma.com/Clinical-Development/Pfizer-teams-with-Parexel-and-Icon-in-CRO-sector-s-latest-strategic-deals
- "How Many New Drugs Did FDA Approve Last Year?". pharmalot.com.
- Tufts Center for the Study of Drug Development
- ^ Perry, Susan (8 August 2012). "Donald Light and Joel Lexchin in BMJ 2012;345:e4348, quoted in: Big Pharma's claim of an 'innovation crisis' is a myth, BMJ authors say". MinnPost. Retrieved 8 August 2012.
- The Pharmaceutical Research and Manufacturers of America (PhRMA)
- Has the Pharmaceutical Blockbuster Model Gone Bust?, Bain & Company press release, December 8, 2003. Press release
- Matthew Harper (10 February 2012). "The Truly Staggering Cost Of Inventing New Drugs". Forbes.
- Bhandari M, Busse JW, Jackowski D, Montori VM, Schunemann H, Sprague S, Mears D, Schemitsch EH, Heels-Ansdell D, Devereaux PJ (17 February 2004). "Association between industry funding and statistically significant pro-industry findings in medical and surgical randomized trials". Retrieved 24 May 2007.
{{cite web}}: CS1 maint: multiple names: authors list (link) - Ben Goldacre: The drugs don't work: a modern medical scandal The Guardian, 2012.
- Moynihan R (2003-05- cvc31). Who pays for the pizza? Redefining the relationships between doctors and drug companies. 2: Disentanglement. BMJ: British Medical Journal. Volume 326, Issue 7400, Pages 1193–1196. Retrieved on 2007-10-06.
- "Hogan & Hartson Update on Pharmaceutical Trial Registration" (PDF). 3 March 2008. Retrieved 2 June 2008.
- Barnett, Antony (7 December 2003). "Revealed: how drug firms 'hoodwink' medical journals". London: The Observer. Retrieved 24 May 2007.
- Tracy Weber and Charles Ornstein (March 11, 2013) "Dollars for Docs Mints a Millionaire" ProPublica
- Liberti L, McAuslane JN, Walker S (2011). "Standardizing the Benefit-Risk Assessment of New Medicines: Practical Applications of Frameworks for the Pharmaceutical Healthcare Professional". Pharm Med. 25 (3): 139–46. doi:10.1007/BF03256855.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Electronic Orange Book". U.S. Food and Drug Administration. Retrieved 31 May 2007.
- Harris, Gardiner (3 December 2008). "British Balance Benefit vs. Cost of Latest Drugs". The New York Times. Retrieved 22 May 2010.
- "The Orphan Drug Act (as amended)". U.S. Food and Drug Administration. Retrieved 24 September 2007.
- http://www.imshealth.com/deployedfiles/ims/Global/Content/Corporate/Press%20Room/Top-Line%20Market%20Data%20&%20Trends/2011%20Top-line%20Market%20Data/Regional_Pharma_Market_by_Spending_2011-2016.pdf
- Herper, Matthew and Kang, Peter (22 March 2006). "The World's Ten Best-Selling Drugs". Forbes. Retrieved 31 May 2007.
{{cite news}}: CS1 maint: multiple names: authors list (link) - http://www.imshealth.com/portal/site/ims/menuitem.d248e29c86589c9c30e81c033208c22a/?vgnextoid=4b8c410b6c718210VgnVCM100000ed152ca2RCRD
- http://www.theguardian.com/business/2014/mar/27/bestselling-prescription-drugs
- http://www.drugs.com/stats/top100/2013/sales
- "IMS Health Forecasts 5 to 6 Percent Growth for Global Pharmaceutical Market in 2007". IMS Health. 24 October 2006. Retrieved 19 June 2007.
- "Prescription for change". Teradata Magazine online. March 2005. Archived from the original on 28 September 2007. Retrieved 19 June 2007.
- Wilson, Duff (6 March 2011). "Drug Firms Face Billions in Losses in '11 as Patents End". NY Times.
- "Drug Patent Expirations and the "Patent Cliff"". US Pharmacist.
- Frequently Asked Questions (FAQs)
- "New Drug Approvals in 2006" (PDF). March 2007. Archived from the original (PDF) on 28 February 2008. Retrieved 23 February 2008.
- "Assessment of Authorized Generics in the U.S" (PDF). IMS Consulting. June 2006. Archived from the original (PDF) on 28 February 2008. Retrieved 23 February 2008.
- Sanofi Laying Off 1,700 in US
- Retail prescription drug sales 1995 to 2006 PDF from www.census.gov
- "Researchers Fail to Reveal Full Drug Pay - NYTimes.com".
- Weintraub, Arlene (26 June 2008). "Drug Makers and College Labs: Too Cozy?". Business Week.
- "Stanford Researcher, Accused of Conflicts, Steps Down as NIH Principal Investigator". The Chronicle of Higher Education. 1 August 2008.
- Gellene, Denise; Maugh II, Thomas H. (4 October 2008). "Doctor Accused in Congress' Probe". The Los Angeles Times.
- Bad Pharma, pp. 274, 287, 303, 311.
- "No Free Lunch". Retrieved 23 May 2007.
- Kaufman, Marc (6 May 2005). "Merck CEO Resigns as Drug Probe Continues". Washington Post. Retrieved 23 May 2007.
- "Drug Lobby Second to None: How the pharmaceutical industry gets its way in Washington". publicintegrity.org. 7 July 2005. Retrieved 23 May 2007.
- Ray Moynihan (2003-05-31). Drug company sponsorship of education could be replaced at a fraction of its cost. BMJ: British Medical Journal, Volume 326, Issue 7400, Page 1163. Retrieved on 2007-10-07.
- Koerner BI (March/April, 2003), Dr. No Free Lunch. Mother Jones, Retrieved on 2007-10-06.
- "A Collection of Articles on Disease Mongering". Public Library of Science. Retrieved 23 May 2007.
- "UK parliamentarians put the pharma industry under the spotlight". European Public Health Alliance. Retrieved 23 May 2007.
- Buchkowsky SS, Jewesson PJ. (2004) Industry sponsorship and authorship of clinical trials over 20 years. Ann Pharmacother. 2004 Apr;38(4):579-85. PMID 14982982
- Perlis RH, Perlis CS, Wu Y, Hwang C, Joseph M, Nierenberg AA (October 2005). "Industry sponsorship and financial conflict of interest in the reporting of clinical trials in psychiatry". Am J Psychiatry. 162 (10): 1957–60. doi:10.1176/appi.ajp.162.10.1957. PMID 16199844.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Tungaraza T, Poole R. (2007) Influence of drug company authorship and sponsorship on drug trial outcomes. Br J Psychiatry. 2007 Jul;191:82-3. PMID 17602130
- Medical schools and journals fight drug industry influence
- Healy D (2006) The Latest Mania: Selling Bipolar Disorder PLoS Med 3(4): e185.
- Cosgrove, Lisa, Krimsky, Sheldon,Vijayaraghavan, Manisha, Schneider, Lisa,Financial Ties between DSM-IV Panel Members and the Pharmaceutical Industry
- Sharfstein, SS. (2005) Big Pharma and American Psychiatry: The Good, the Bad, and the Ugly Psychiatric News August 19, 2005 Volume 40 Number 16
- Open Payments page in the Centers for Medicare & Medicaid Services website
- Bad Pharma, p. 123ff.
- Bad Pharma, p. 143ff.
- "www.whitehouse.gov" (PDF).
- "Financial Crimes to the Public Report 2006". FBI. 2006.
- "FBI-Health Care Fraud". FBI.
- "Department of Justice". Department of Justice.
- Duff Wilson (2 October 2010). "Side Effects May Include Lawsuits". New York Times.
- "GlaxoSmithKline". BBC News. 4 July 2012.
- "GlaxoSmithKline Agrees to Pay $3 Billion in U.S. Drug Settlement". Bloomberg. 2 July 2012.
- Fred Mogul (2 July 2012). "NY to Get Millions in GlaxoSmithKlein Settlement". WNYC. Retrieved 2 July 2012.
- "BBC News -GlaxoSmithKline to pay $3bn in US drug fraud scandal". BBC Online. 2 July 2012. Retrieved 2 July 2012.
- Thomas, Katie and Schmidt, Michael S. (2 July 2012). "Glaxo Agrees to Pay $3 Billion in Fraud Settlement". The New York Times. Retrieved 3 July 2012.
{{cite news}}: CS1 maint: multiple names: authors list (link) - Sammy Almashat, M.D., M.P.H., Charles Preston, M.D., M.P.H., Timothy Waterman, B.S., Sidney Wolfe, M.D., Rapidly Increasing Criminal and Civil Monetary Penalties Against the Pharmaceutical Industry: 1991 – 2010, Public Citizen's Health Research Group, December 16, 2010
- Thomas, Katie; Schmidt, Michael S. (2 July 2012). "GlaxoSmithKline Agrees to Pay $3 Billion in Fraud Settlement". The New York Times.
- USDOJ: GlaxoSmithKline to Plead Guilty and Pay $3 Billion to Resolve Fraud Allegations and Failure to Report Safety Data
- http://www.justice.gov/usao/ma/news/Pfizer/Pfizer%20-%20PR%20(Final).pdf
- USDOJ: Abbott Labs to Pay $1.5 Billion to Resolve Criminal & Civil Investigations of Off-label Promotion of Depakote
- #09-038: Eli Lilly and Company Agrees to Pay $1.415 Billion to Resolve Allegations of Off-label Promotion of Zyprexa (2009-01-15)
- See for example: 't Hoen, Ellen. "TRIPS, Pharmaceutical Patents, and Access to Essential Medicines: A Long Way from Seattle to Doha". Chicago Journal of International Law, 27(43), 2002; Musungu, Sisule F., and Cecilia Oh. "The Use of Flexibilities in TRIPS by Developing Countries: Can They Provide Access to Medicines?" Commission on Intellectual Property Rights, Innovation and Public Health, The World Health Organization, 2005.
- WTO. "The Doha Declaration on TRIPS and public health", 2001. Available online at http://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm.
- "Pharmaceutical Manufacturer's Association v. The President of South Africa (PMA)", 2002 (2) SA 674 (CC) (S. Africa).
- Helfer, Laurence R. and Graeme W. Austin. "Human Rights and Intellectual Property: Mapping the Global Interface". Cambridge University Press: 2011, pp. 145–48.
- http://www.cartercenter.org/healthprograms/showdoc.asp?programID=2&submenu=healthprograms
- Pfizer Will Donate Fluconazole to South Africa
- http://www.corporatecitizenship.novartis.com Novartis corporate citizenship
| Pharmaceutical industry by country | |
|---|---|
| List of pharmaceutical companies |
| Companies | |
|---|---|
| Regulatory bodies | |
| Professional bodies | |
| Miscellaneous | |
| Books |
|
| Lists | |
| Related templates | |
| Related categories |
|
| Major industries | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| Public health | |||||||
|---|---|---|---|---|---|---|---|
| General |
| ||||||
| Preventive healthcare | |||||||
| Population health | |||||||
| Biological and epidemiological statistics | |||||||
| Infectious and epidemic disease prevention | |||||||
| Food hygiene and safety management | |||||||
| Health behavioral sciences | |||||||
| Organizations, education and history |
| ||||||
| Medicine | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Specialties and subspecialties |
| ||||||||||
| Medical education | |||||||||||
| Related topics | |||||||||||