| Revision as of 19:06, 3 May 2015 view sourceKww (talk | contribs)Extended confirmed users, Rollbackers82,486 edits undue weight to fringe views. If you want to make this change, get a consensus to include it that does *not* include editors that practice acupuncture for a living← Previous edit | Revision as of 19:07, 3 May 2015 view source A1candidate (talk | contribs)15,335 edits formatNext edit → | ||
| Line 13: | Line 13: | ||
| }} | }} | ||
| '''Acupuncture''' (from ], 'acus' (needle) + 'punctura' (to puncture)<ref>{{cite journal|last1=Pyne|first1=D.|last2=Shenker|first2=N. G.|title=Demystifying acupuncture|journal=Rheumatology|volume=47|issue=8|year=2008|pages=1132–1136|issn=1462-0324|doi=10.1093/rheumatology/ken161|pmid=18460551}}</ref>) is the stimulation of ]s along the skin of the body using thin needles.<ref name="Adams 2011"/> It can be associated with the application of heat, pressure, or laser to these same points.<ref name="Adams 2011"/> Clinical practice varies in different countries.<ref name="Ernst2006"/> Traditional acupuncture involves needle insertion, ], and ].<ref name="Xu S"/> It is a form of ]<ref name=Berman2010/> and a key component of ] (TCM).<ref name=Liu-2013/> According to the theories of TCM, stimulating acupuncture points corrects imbalances in the flow of '']'' through channels known as ].<ref name=Barrett2007/> TCM |
'''Acupuncture''' (from ], 'acus' (needle) + 'punctura' (to puncture)<ref>{{cite journal|last1=Pyne|first1=D.|last2=Shenker|first2=N. G.|title=Demystifying acupuncture|journal=Rheumatology|volume=47|issue=8|year=2008|pages=1132–1136|issn=1462-0324|doi=10.1093/rheumatology/ken161|pmid=18460551}}</ref>) is the stimulation of ]s along the skin of the body using thin needles.<ref name="Adams 2011"/> It can be associated with the application of heat, pressure, or laser to these same points.<ref name="Adams 2011"/> Clinical practice varies in different countries.<ref name="Ernst2006"/> Traditional acupuncture involves needle insertion, ], and ].<ref name="Xu S"/> It is a form of ]<ref name=Berman2010/> and a key component of ] (TCM).<ref name=Liu-2013/> According to the theories of TCM, stimulating acupuncture points corrects imbalances in the flow of '']'' through channels known as ].<ref name=Barrett2007/> Some believe that TCM has a strong scientific basis, <ref>{{cite book |last=Adams |first=David James |date= 2013|title=Traditional Chinese Medicine: Scientific Basis for its Use|url=https://books.google.com/books?id=vh9PkMT2b0wC |location= |publisher=]|page=2 |isbn=1849736618 |access-date= }}</ref> but according to ], it is not based upon ],<ref name=Barrett2007/> and others describe acupuncture as a type of ].<ref name=Baran2014/><ref name=khine/> At least two national health bodies recognise it can be effective in some circumstances.<ref name="NHS" /><ref name="Australia">{{cite book|title=Alcohol and Other Drugs: A Handbook for Health Professionals|url=http://www.health.gov.au/internet/main/publishing.nsf/Content/E5203E6D5CBAA696CA257BF0001E02ED/$File/part2-2.pdf|title=Chapter 8: Cocaine|pages=105-118|accessdate=May 2, 2015}}</ref> ]s issued by medical societies including the ],<ref name="APS">{{cite journal|last1=Chou|first1=R|last2=Huffman|first2=LH|last3=American Pain Society|last4=American College of Physicians|title=Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline.|journal=Annals of internal medicine|date=2 October 2007|volume=147|issue=7|pages=492-504|doi=10.7326/0003-4819-147-7-200710020-00006|pmid=17909210|url=http://annals.org/article.aspx?articleid=736814}}</ref> ],<ref name="chest">{{cite journal|last1=Deng|first1=Gary E.|last2=Rausch|first2=Sarah M.|last3=Jones|first3=Lee W.|last4=Gulati|first4=Amitabh|last5=Kumar|first5=Nagi B.|last6=Greenlee|first6=Heather|last7=Pietanza|first7=M. Catherine|last8=Cassileth|first8=Barrie R.|title=Complementary Therapies and Integrative Medicine in Lung Cancer|journal=]|quote=In patients having nausea and vomiting from either chemotherapy or radiation therapy, acupuncture or related techniques is suggested as an adjunct treatment option|date=1 May 2013|volume=143|issue=5_suppl|pages=e420S|doi=10.1378/chest.12-2364|url=http://journal.publications.chestnet.org/article.aspx?articleid=1685298}}</ref> ],<ref>{{cite journal|last1=Camilleri|first1=M|last2=Parkman|first2=HP|last3=Shafi|first3=MA|last4=Abell|first4=TL|last5=Gerson|first5=L|last6=American College of Gastroenterology|title=Clinical guideline: management of gastroparesis.|journal=]|date=January 2013|volume=108|issue=1|pages=18-37|pmid=23147521|url=http://www.ncbi.nlm.nih.gov/pubmed/23147521|quote=Acupuncture can be considered as an alternative therapy. This has been associated with improved rates of gastric emptying and reduction of symptoms.}}</ref> ],<ref>{{cite journal|last1=Seidman|first1=M. D.|last2=Gurgel|first2=R. K.|last3=Lin|first3=S. Y.|last4=Schwartz|first4=S. R.|last5=Baroody|first5=F. M.|last6=Bonner|first6=J. R.|last7=Dawson|first7=D. E.|last8=Dykewicz|first8=M. S.|last9=Hackell|first9=J. M.|last10=Han|first10=J. K.|last11=Ishman|first11=S. L.|last12=Krouse|first12=H. J.|last13=Malekzadeh|first13=S.|last14=Mims|first14=J. W.|last15=Omole|first15=F. S.|last16=Reddy|first16=W. D.|last17=Wallace|first17=D. V.|last18=Walsh|first18=S. A.|last19=Warren|first19=B. E.|last20=Wilson|first20=M. N.|last21=Nnacheta|first21=L. C.|title=Clinical Practice Guideline: Allergic Rhinitis Executive Summary|journal=]|date=2 February 2015|volume=152|issue=2|pages=197–206|doi=10.1177/0194599814562166|url=http://oto.sagepub.com/content/152/2/197.full|quote=Clinicians may offer acupuncture, or refer to a clinician who can offer acupuncture, for patients with allergic rhinitis who are interested in nonpharmacologic therapy.}}</ref> and ]<ref>{{cite journal|last1=Abdulla|first1=A|last2=Adams|first2=N|last3=Bone|first3=M|last4=Elliott|first4=AM|last5=Gaffin|first5=J|last6=Jones|first6=D|last7=Knaggs|first7=R|last8=Martin|first8=D|last9=Sampson|first9=L|last10=Schofield|first10=P|last11=British Geriatric Society|title=Guidance on the management of pain in older people.|journal=]|date=March 2013|volume=42 Suppl 1|pages=i1-57|doi=10.1093/ageing/afs200|pmid=23420266|url=http://www.ncbi.nlm.nih.gov/pubmed/23420266|quote=Consider the use of non-pharmacological strategies such as physiotherapy, cognitive behavioural approaches and acupuncture, in combination with medication}}</ref> have suggested the use of acupuncture for some groups of patients. The claim that acupuncture is medically effective has in the past been declared a pseudoscientific claim, but we now have plausible scientific evidence for acupuncture's effectiveness.<ref>{{cite book |last=Curd |first=Martin |date=2013 |title=The Routledge Companion to Philosophy of Science|url=https://books.google.com/books?id=GfopAAAAQBAJ&q=pseudoscience#v=snippet&q=acupuncture&f=false|location= |publisher=Routledge |page=470|isbn= 1135011087|access-date= }}</ref> However, ] and ] describe it as a "borderlands science" lying between normal science and pseudoscience.<ref name=Massimo2013/> Most medical textbooks in the field of ] assert that acupuncture treatment has proven efficacy for relieving pain when compared to placebo treatment.<ref name="miller"/> | ||
| <!-- Efficacy --> | <!-- Efficacy --> | ||
| Line 86: | Line 86: | ||
| A 2010 systematic review suggested that acupuncture is more than a placebo for commonly occurring chronic pain conditions, but the authors acknowledged that it is still unknown if the overall benefit is clinically meaningful or cost-effective.<ref name=Hopton2010>{{cite journal|last1=Hopton|first1=Ann|last2=MacPherson|first2=Hugh|title=Acupuncture for Chronic Pain: Is Acupuncture More than an Effective Placebo? A Systematic Review of Pooled Data from Meta-analyses|journal=Pain Practice|volume=10|issue=2|year=2010|pages=94–102|issn=15307085|doi=10.1111/j.1533-2500.2009.00337.x|pmid=20070551}}</ref> A 2010 review found real acupuncture and sham acupuncture produce similar improvements, which can only be accepted as evidence against the efficacy of acupuncture.<ref name=Enck2010/> The same review found limited evidence that real acupuncture and sham acupuncture appear to produce biological differences despite similar effects.<ref name=Enck2010>{{cite journal|last1=Enck|first1=Paul|last2=Klosterhalfen|first2=Sibylle|last3=Zipfel|first3=Stephan|title=Acupuncture, psyche and the placebo response|journal=Autonomic Neuroscience|volume=157|issue=1-2|year=2010|pages=68–73|issn=15660702|doi=10.1016/j.autneu.2010.03.005|pmid=20359961}}</ref> A 2009 systematic review and meta-analysis found that acupuncture had a small analgesic effect, which appeared to lack any clinical importance and could not be discerned from bias.<ref name=Madsen2009/> The same review found that it remains unclear whether acupuncture reduces pain independent of a psychological impact of the needling ritual.<ref name=Madsen2009>{{cite journal |last1=Madsen |first1=M. V. |last2=Gøtzsche |first2=P. C |last3=Hróbjartsson |first3=A. |title=Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups |journal=BMJ |volume=338 |pages=a3115 |year=2009 |pmid=19174438 |pmc=2769056 |doi=10.1136/bmj.a3115}}</ref> | A 2010 systematic review suggested that acupuncture is more than a placebo for commonly occurring chronic pain conditions, but the authors acknowledged that it is still unknown if the overall benefit is clinically meaningful or cost-effective.<ref name=Hopton2010>{{cite journal|last1=Hopton|first1=Ann|last2=MacPherson|first2=Hugh|title=Acupuncture for Chronic Pain: Is Acupuncture More than an Effective Placebo? A Systematic Review of Pooled Data from Meta-analyses|journal=Pain Practice|volume=10|issue=2|year=2010|pages=94–102|issn=15307085|doi=10.1111/j.1533-2500.2009.00337.x|pmid=20070551}}</ref> A 2010 review found real acupuncture and sham acupuncture produce similar improvements, which can only be accepted as evidence against the efficacy of acupuncture.<ref name=Enck2010/> The same review found limited evidence that real acupuncture and sham acupuncture appear to produce biological differences despite similar effects.<ref name=Enck2010>{{cite journal|last1=Enck|first1=Paul|last2=Klosterhalfen|first2=Sibylle|last3=Zipfel|first3=Stephan|title=Acupuncture, psyche and the placebo response|journal=Autonomic Neuroscience|volume=157|issue=1-2|year=2010|pages=68–73|issn=15660702|doi=10.1016/j.autneu.2010.03.005|pmid=20359961}}</ref> A 2009 systematic review and meta-analysis found that acupuncture had a small analgesic effect, which appeared to lack any clinical importance and could not be discerned from bias.<ref name=Madsen2009/> The same review found that it remains unclear whether acupuncture reduces pain independent of a psychological impact of the needling ritual.<ref name=Madsen2009>{{cite journal |last1=Madsen |first1=M. V. |last2=Gøtzsche |first2=P. C |last3=Hróbjartsson |first3=A. |title=Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups |journal=BMJ |volume=338 |pages=a3115 |year=2009 |pmid=19174438 |pmc=2769056 |doi=10.1136/bmj.a3115}}</ref> | ||
| According to '']'' |
According to '']'' acupuncture treatment has proven efficacy for relieving pain when compared to placebo treatment.<ref name="miller">{{cite book|title=].|date=2014|publisher=Elsevier|isbn=0702052833|page=1235|quote=When compared with placebo, acupuncture treatment has proven efficacy for relieving pain}}</ref> | ||
| === Low back === | === Low back === | ||
| Line 200: | Line 200: | ||
| To fulfill its functions, qi has to steadily flow from the inside of the body (where the ] organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints.<ref name=meridian-theory/> It is assisted in its flow by "channels" referred to as meridians.<ref name=meridian-theory/> TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 ({{zh|p=shí-èr jīngmài}}, lit. "the Twelve Vessels") and 奇经八脉 ({{zh|p=qí jīng bā mài}}).<ref name=meridian-theory>"(三)十二经脉 ...(四)奇经八脉 ..." as seen at {{cite web |url= http://www.pharmnet.com.cn/tcm/knowledge/detail/100044.html |script-title=zh:经络学 |accessdate=22 February 2011 |language=Chinese |trans_title=meridian theory}}</ref> There's also a number of less customary channels branching off from the "regular" meridians.<ref name=Aung19>], 2007, pp .</ref> Contemporary research has not supported the existence of ''qi'' or meridians.<ref name=Bauer>{{cite journal |first=M |last=Bauer |url=http://www.chinesemedicinetimes.com/section.php?xSec=122 |journal=Chinese Medicine Times |volume=1 |issue=4 |page=31 |year=2006 |title=The Final Days of Traditional Beliefs? – Part One}}</ref><ref name="Ahn2008">{{cite journal |last1=Ahn |first1=Andrew C. |last2=Colbert |first2=Agatha P. |last3=Anderson |first3=Belinda J. |last4=Martinsen |first4=ØRjan G. |last5=Hammerschlag |first5=Richard |last6=Cina |first6=Steve |last7=Wayne |first7=Peter M. |last8=Langevin |first8=Helene M. |title=Electrical properties of acupuncture points and meridians: A systematic review |journal=Bioelectromagnetics |volume=29 |issue=4 |pages=245–256 |year=2008 |pmid=18240287 |doi=10.1002/bem.20403 |url=https://mn.uio.no/fysikk/english/research/projects/bioimpedance/publications/papers/meridian_rev.pdf}}</ref><ref name=Mann2000>{{cite book | last = Mann | first = F | authorlink = Felix Mann | isbn = 0750648570 | publisher = ] | year = 2000 | title = Reinventing Acupuncture: A New Concept of Ancient Medicine}}</ref><ref name="SinghErnst2008Ch2">{{harvnb|Singh & Ernst|2008|loc= Chapter 2: The Truth About Acupuncture}}</ref> The meridians are believed to connect to the bodily ], of which those considered hollow organs (such as the stomach and intestines) were also considered ''yang'' while those considered solid (such as the liver and lungs) were considered ''yin''. They were also symbolically linked to the rivers found in ancient China, such as the ], ] and ]s.<ref>], 2002, p. .</ref> | To fulfill its functions, qi has to steadily flow from the inside of the body (where the ] organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints.<ref name=meridian-theory/> It is assisted in its flow by "channels" referred to as meridians.<ref name=meridian-theory/> TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 ({{zh|p=shí-èr jīngmài}}, lit. "the Twelve Vessels") and 奇经八脉 ({{zh|p=qí jīng bā mài}}).<ref name=meridian-theory>"(三)十二经脉 ...(四)奇经八脉 ..." as seen at {{cite web |url= http://www.pharmnet.com.cn/tcm/knowledge/detail/100044.html |script-title=zh:经络学 |accessdate=22 February 2011 |language=Chinese |trans_title=meridian theory}}</ref> There's also a number of less customary channels branching off from the "regular" meridians.<ref name=Aung19>], 2007, pp .</ref> Contemporary research has not supported the existence of ''qi'' or meridians.<ref name=Bauer>{{cite journal |first=M |last=Bauer |url=http://www.chinesemedicinetimes.com/section.php?xSec=122 |journal=Chinese Medicine Times |volume=1 |issue=4 |page=31 |year=2006 |title=The Final Days of Traditional Beliefs? – Part One}}</ref><ref name="Ahn2008">{{cite journal |last1=Ahn |first1=Andrew C. |last2=Colbert |first2=Agatha P. |last3=Anderson |first3=Belinda J. |last4=Martinsen |first4=ØRjan G. |last5=Hammerschlag |first5=Richard |last6=Cina |first6=Steve |last7=Wayne |first7=Peter M. |last8=Langevin |first8=Helene M. |title=Electrical properties of acupuncture points and meridians: A systematic review |journal=Bioelectromagnetics |volume=29 |issue=4 |pages=245–256 |year=2008 |pmid=18240287 |doi=10.1002/bem.20403 |url=https://mn.uio.no/fysikk/english/research/projects/bioimpedance/publications/papers/meridian_rev.pdf}}</ref><ref name=Mann2000>{{cite book | last = Mann | first = F | authorlink = Felix Mann | isbn = 0750648570 | publisher = ] | year = 2000 | title = Reinventing Acupuncture: A New Concept of Ancient Medicine}}</ref><ref name="SinghErnst2008Ch2">{{harvnb|Singh & Ernst|2008|loc= Chapter 2: The Truth About Acupuncture}}</ref> The meridians are believed to connect to the bodily ], of which those considered hollow organs (such as the stomach and intestines) were also considered ''yang'' while those considered solid (such as the liver and lungs) were considered ''yin''. They were also symbolically linked to the rivers found in ancient China, such as the ], ] and ]s.<ref>], 2002, p. .</ref> | ||
| Acupuncture points are mainly (but not always) found at specified locations along the meridians.<ref name=Aung101/> There also is a number of acupuncture points with specified locations outside of the meridians; these are called extraordinary points and are credited to treat certain diseases.<ref name=Aung101/> A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes.<ref name=Aung101>], 2007, p. .</ref> The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in ] times, the number of bones thought to be in the body).<ref name=Needham15/> The '']'' mentioned only 160 and a further 135 could be deduced giving a total of 295.<ref name=Needham15/> The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions.<ref name=Needham15/> In addition, it is considered likely that some points used historically have since ceased being used.<ref name=Needham15>], 2002, p. .</ref> | Acupuncture points are mainly (but not always) found at specified locations along the meridians.<ref name=Aung101/> There also is a number of acupuncture points with specified locations outside of the meridians; these are called extraordinary points and are credited to treat certain diseases.<ref name=Aung101/> A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes.<ref name=Aung101>], 2007, p. .</ref> The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in ] times, the number of bones thought to be in the body).<ref name=Needham15/> The '']'' mentioned only 160 and a further 135 could be deduced giving a total of 295.<ref name=Needham15/> The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions.<ref name=Needham15/> In addition, it is considered likely that some points used historically have since ceased being used.<ref name=Needham15>], 2002, p. .</ref> | ||
| <!---=== Blood === | <!---=== Blood === | ||
| TCM asserts that blood is propelled by qi, that the 100 blood "vessels are the pathways of the blood’, that the vessels gather at a specific acupuncture point (Taiyuan LU-9) associated with the lung (or lungs), and that when qi flow is not in balance, blood pools and stagnates.<ref>Classic of Difficulties (45th Difficulty)</ref><ref>The Classic of Categories</ref><ref name=APDB>{{cite web |title=Some Acupuncture Points Which Treat Disorders of Blood |author=Peter Deadman and Mazin Al-Khafaji |url= http://www.acupuncture.com/education/theory/ptsforblood.htm |publisher=acupuncture.com}}</ref> Modern science-based medicine has shown that blood is propelled by pumping action of the heart, and that there are many more than 100 blood vessels, that the vessels do not gather at that or any specific point, and that blood doesn't fail to circulate except by failure of pumping by the heart, and does not pool or stagnate except when a vessel is physically blocked or the heart pumping is disrupted.---> | TCM asserts that blood is propelled by qi, that the 100 blood "vessels are the pathways of the blood’, that the vessels gather at a specific acupuncture point (Taiyuan LU-9) associated with the lung (or lungs), and that when qi flow is not in balance, blood pools and stagnates.<ref>Classic of Difficulties (45th Difficulty)</ref><ref>The Classic of Categories</ref><ref name=APDB>{{cite web |title=Some Acupuncture Points Which Treat Disorders of Blood |author=Peter Deadman and Mazin Al-Khafaji |url= http://www.acupuncture.com/education/theory/ptsforblood.htm |publisher=acupuncture.com}}</ref> Modern science-based medicine has shown that blood is propelled by pumping action of the heart, and that there are many more than 100 blood vessels, that the vessels do not gather at that or any specific point, and that blood doesn't fail to circulate except by failure of pumping by the heart, and does not pool or stagnate except when a vessel is physically blocked or the heart pumping is disrupted.---> | ||
Revision as of 19:07, 3 May 2015
For the recording, see Acupuncture (album).Medical intervention
| Acupuncture | |
|---|---|
 Needles being inserted into a person's skin Needles being inserted into a person's skin | |
| ICD-10-PCS | 8E0H30Z |
| ICD-9 | 99.91-99.92 |
| MeSH | D015670 |
| OPS-301 code | 8-975.2 |
| [edit on Wikidata] | |
Acupuncture (from Latin, 'acus' (needle) + 'punctura' (to puncture)) is the stimulation of acupuncture points along the skin of the body using thin needles. It can be associated with the application of heat, pressure, or laser to these same points. Clinical practice varies in different countries. Traditional acupuncture involves needle insertion, moxibustion, and cupping therapy. It is a form of alternative medicine and a key component of traditional Chinese medicine (TCM). According to the theories of TCM, stimulating acupuncture points corrects imbalances in the flow of qi through channels known as meridians. Some believe that TCM has a strong scientific basis, but according to Quackwatch, it is not based upon scientific knowledge, and others describe acupuncture as a type of pseudoscience. At least two national health bodies recognise it can be effective in some circumstances. Clinical practice guidelines issued by medical societies including the American College of Physicians, American College of Chest Physicians, American College of Gastroenterology, American Academy of Otolaryngology – Head and Neck Surgery, and British Geriatrics Society have suggested the use of acupuncture for some groups of patients. The claim that acupuncture is medically effective has in the past been declared a pseudoscientific claim, but we now have plausible scientific evidence for acupuncture's effectiveness. However, Massimo Pigliucci and Maarten Boudry describe it as a "borderlands science" lying between normal science and pseudoscience. Most medical textbooks in the field of anesthesiology assert that acupuncture treatment has proven efficacy for relieving pain when compared to placebo treatment.
Evidence on the effectiveness of acupuncture is variable and inconsistent, even for single conditions. An overview of high-quality Cochrane reviews stated that acupuncture may alleviate certain kinds of pain. A systematic review of systematic reviews found that for reducing pain, real acupuncture was no better than sham acupuncture and concluded that there is little evidence that acupuncture is an effective treatment for reducing pain. Although minimally invasive, the puncturing of the skin with acupuncture needles poses problems when designing trials that adequately control for placebo effects. Some research results suggest acupuncture can alleviate pain, though other research consistently suggests that acupuncture's effects are mainly due to placebo. The evidence suggests that short-term treatment with acupuncture does not produce long-term benefits. A systematic review concluded that the analgesic effect of acupuncture seemed to lack clinical relevance and could not be clearly distinguished from bias.
Acupuncture is generally safe when done by an appropriately trained practitioner using clean technique and single-use needles. When properly delivered, it has a low rate of mostly minor adverse effects. Between 2000 and 2009, at least ninety-five cases of serious adverse events, including five deaths, were reported to have resulted from acupuncture. Many of these cases occurred in developed countries and many were due to malpractice. The most frequently reported adverse events were pneumothorax and infections. Since serious adverse events continue to be reported, it is recommended that acupuncturists be trained sufficiently to reduce the risk. A meta-analysis found that acupuncture for chronic low back pain was cost-effective as an adjunct to standard care, but not as a substitute for standard care except in cases where comorbid depression presented, while a systematic review found insufficient evidence for the cost-effectiveness of acupuncture in the treatment of chronic low back pain.
Acupuncture has been the subject of active scientific research, both in regard to its basis and therapeutic effectiveness, since the late 20th century. Scientific investigation has not found any histological or physiological evidence for traditional Chinese concepts such as qi, meridians, and acupuncture points. In response, some contemporary practitioners use acupuncture without following the traditional Chinese approach and have abandoned the concepts of qi and meridians as pseudoscientific. Acupuncture is currently used widely throughout China and many other countries, including the United States. It is uncertain exactly when acupuncture originated or how it evolved, but it is generally thought to derive from ancient China. In Chinese history the introduction of acupuncture is attributed to the emperor Shennong. Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) that suggest acupuncture along with moxibustion was in practice.
Clinical practice
Acupuncture is the stimulation of specific acupuncture points along the skin of the body using thin needles. It can be associated with the application of heat, pressure, or laser light to these points. Classically, acupuncture is individualized and based on philosophy and intuition, and not on scientific research. In modern acupuncture, a consultation is followed by taking the pulse on both arms and inspecting the tongue. This initial evaluation may last up to 60 minutes. Subsequent visits typically last about a half an hour. The number and frequency of acupuncture sessions vary, but most practitioners do not think one session is sufficient. A common treatment plan for a single complaint usually involves six to twelve treatments, to be carried out over a few months. A typical session entails lying still while approximately five to twenty needles are inserted; for the majority of cases, the needles will be left in place for ten to twenty minutes.
Clinical practice varies depending on the country. A comparison of the average number of patients treated per hour found significant differences between China (10) and the United States (1.2). Traditional acupuncture involves needle insertion, moxibustion, and cupping therapy. Traditional acupuncture may be accompanied by various ancillary procedures, such as palpation of the radial artery and other parts of the body and examining the tongue. Acupuncturists generally practice acupuncture as an overall system of care, which includes using traditional diagnostic techniques, acupuncture needling, and other adjunctive treatments. Chinese herbs are also often used. Although various different techniques of acupuncture practice have emerged, the method used in traditional Chinese medicine (TCM) seems to be the most widely adopted in the US. The main methods practiced in the UK are TCM and Western medical acupuncture.
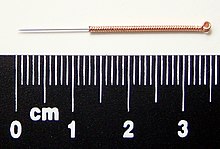
Needles
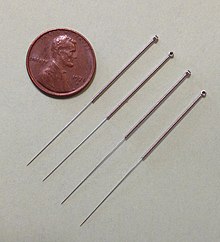
Acupuncture needles are typically made of stainless steel, making them flexible and preventing them from rusting or breaking. Needles are usually disposed of after each use to prevent contamination. Reusable needles when used should be sterilized between applications. Needles vary in length between 13 to 130 millimetres (0.51 to 5.12 in), with shorter needles used near the face and eyes, and longer needles in more fleshy areas; needle diameters vary from 0.16 mm (0.006 in) to 0.46 mm (0.018 in), with thicker needles used on more robust patients. Thinner needles may be flexible and require tubes for insertion. The tip of the needle should not be made too sharp to prevent breakage, although blunt needles cause more pain.
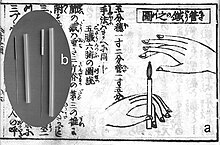
Apart from the usual filiform needle, other needle types include three-edged needles and the Nine Ancient Needles. Japanese acupuncturists use extremely thin needles that are used superficially, sometimes without penetrating the skin, and surrounded by a guide tube (a 17th-century invention adopted in China and the West). Korean acupuncture uses copper needles and has a greater focus on the hand.
Needling technique
Insertion
The skin is sterilized and the needles are inserted, frequently with a plastic guide tube. Needles may be manipulated in various ways, including spinning, flicking, or moving up and down relative to the skin. Since most pain is felt in the superficial layers of the skin, a quick insertion of the needle is recommended. Often, the needles are stimulated by hand in order to cause a dull, localized, aching sensation that is called de qi, as well as "needle grasp," a tugging feeling felt by the acupuncturist and generated by a mechanical interaction between the needle and skin. Acupuncture can be painful. The skill level of the acupuncturist may influence how painful the needle insertion is, and a sufficiently skilled practitioner may be able to insert the needles without causing any pain.
De-qi sensation
De-qi (Chinese: 得气; pinyin: dé qì; "arrival of qi") refers to a sensation of numbness, distension, or electrical tingling at the needling site which might radiate along the corresponding meridian. If de-qi can not be generated, then inaccurate location of the acupoint, improper depth of needle insertion, inadequate manual manipulation, or a very weak constitution of the patient can be considered, all of which are thought to decrease the likelihood of successful treatment. If the de-qi sensation doesn't immediately occur upon needle insertion, various manual manipulation techniques can be applied to promote it (such as "plucking", "shaking" or "trembling").
Once de-qi is achieved, further techniques might be utilized which aim to "influence" the de-qi; for example, by certain manipulation the de-qi sensation allegedly can be conducted from the needling site towards more distant sites of the body. Other techniques aim at "tonifying" (Chinese: 补; pinyin: bǔ) or "sedating" (Chinese: 泄; pinyin: xiè) qi. The former techniques are used in deficiency patterns, the latter in excess patterns.De qi is more important in Chinese acupuncture, while Western and Japanese patients may not consider it a necessary part of the treatment.
Non-invasive needling
There is also a non-invasive therapy developed in early 20th century Japan using an elaborate set of "needles" for the treatment of children (shōnishin or shōnihari).
Related practices


- Acupressure, a non-invasive form of acupuncture, uses physical pressure applied to acupressure points by the hand, elbow, or with various devices.
- Acupuncture is often accompanied by moxibustion, the burning of cone-shaped preparations of moxa (made from dried mugwort) on or near the skin, often but not always near or on an acupuncture point. Traditionally, acupuncture was used to treat acute conditions while moxibustion was used for chronic diseases. Moxibustion could be direct (the cone was placed directly on the skin and allowed to burn the skin producing a blister and eventually a scar), or indirect (either a cone of moxa was placed on a slice of garlic, ginger or other vegetable, or a cylinder of moxa was held above the skin, close enough to either warm or burn it).
- Cupping therapy is an ancient Chinese form of alternative medicine in which a local suction is created on the skin; practitioners believe this mobilizes blood flow in order to promote healing.
- Tui na is a TCM method of attempting to stimulate the flow of qi by various bare-handed techniques that do not involve needles.
- Electroacupuncture is a form of acupuncture in which acupuncture needles are attached to a device that generates continuous electric pulses (this has been described as "essentially transdermal electrical nerve stimulation masquerading as acupuncture").
- Sonopuncture is a stimulation of the body similar to acupuncture using sound instead of needles. This may be done using purpose-built transducers to direct a narrow ultrasound beam to a depth of 6–8 centimetres at acupuncture meridian points on the body. Alternatively, tuning forks or other sound emitting devices are used.
- Acupuncture point injection is the injection of various substances (such as drugs, vitamins or herbal extracts) into acupoints.
- Auriculotherapy, commonly known as ear acupuncture, auricular acupuncture, or auriculoacupuncture, is considered to date back to ancient China which involves inserting needles to stimulate points on the outer ear. The modern approach was developed in France during the early 1950s. There is no scientific evidence that it can cure disease; the evidence of effectiveness is negligible.
- Scalp acupuncture, developed in Japan, is based on reflexological considerations regarding the scalp area. Hand acupuncture, developed in Korea, centers around assumed reflex zones of the hand. Medical acupuncture attempts to integrate reflexological concepts, the trigger point model, and anatomical insights (such as dermatome distribution) into acupuncture practice, and emphasizes a more formulaic approach to acupuncture point location.
- Cosmetic acupuncture is the use of acupuncture in an attempt to reduce wrinkles on the face.
Effectiveness
Using the principles of evidence-based medicine to research acupuncture is controversial, and has produced different results in a growing evidence base. Some research results suggest acupuncture can alleviate pain but others consistently suggest that acupuncture's effects are mainly due to placebo. It is difficult but not impossible to design rigorous research trials for acupuncture. Due to acupuncture's invasive nature, one of the major challenges in efficacy research is in the design of an appropriate placebo control group. For efficacy studies to determine whether acupuncture has specific effects, "sham" forms of acupuncture where the patient, practitioner, and analyst are blinded seem the most acceptable approach. The under-performance of acupuncture in such trials may indicate that therapeutic effects are due entirely to non-specific effects, or that the sham treatments are not inert or systematic protocols yield less than optimal treatment. A 2012 review found "A common control procedure has been the use of sham acupuncture where needles are inserted on either meridians not specific for the condition under study, or in areas outside meridians; often this is coupled with a more superficial needle insertion than what is performed in the true acupuncture group." The research seems to suggest that needles do not need to stimulate the traditionally specified acupuncture points or penetrate the skin to attain an anticipated effect (e.g. psychosocial factors). A 2012 review found "acupuncture was not better than sham interventions or conventional therapy in the longer term." The evidence suggests that any benefits of acupuncture are short-lasting.
Any evidence on the effectiveness of acupuncture is "variable and inconsistent, even for single conditions", and publication bias is cited as a concern in the reviews of randomized controlled trials (RCTs) of acupuncture. A 1998 review of studies on acupuncture found that trials originating in China, Japan, Hong Kong and Taiwan were uniformly favourable to acupuncture, as were ten out of 11 studies conducted in Russia. A 2011 assessment of the quality of RCTs on TCM, including acupuncture, concluded that the methodological quality of most such trials (including randomization, experimental control and blinding) was generally poor, particularly for trials published in Chinese journals (though the quality of acupuncture trials was better than the drug-related trials). The study also found that trials published in non-Chinese journals tended to be of higher quality.
A 2014 Nature Reviews Cancer article found that "contrary to the claimed mechanism of redirecting the flow of qi through meridians, researchers usually find that it generally does not matter where the needles are inserted, how often (that is, no dose-response effect is observed), or even if needles are actually inserted. In other words, ‘sham’ or ‘placebo’ acupuncture generally produces the same effects as ‘real’ acupuncture and, in some cases, does better." A 2013 meta-analysis found little evidence that the effectiveness of acupuncture on pain (compared to sham) was modified by the location of the needles, the number of needles used, the experience or technique of the practitioner, or by the circumstances of the sessions. The same analysis also suggested that the number of needles and sessions is important, as greater numbers improved the outcomes of acupuncture compared to non-acupuncture controls. A 2013 editorial found that the inconsistency of results of acupuncture studies (that acupuncture relieved pain in some conditions but had no effect in other very similar conditions) suggests false positive results, which may be caused by factors like biased study designs, poor blinding, and the classification of electrified needles (a type of TENS) as acupuncture. The same editorial suggested that given the inability to find consistent results despite more than 3,000 studies of acupuncture, the treatment seems to be a placebo effect and the existing equivocal positive results are noise one expects to see after a large number of studies are performed on an inert therapy. It concluded that the best controlled studies showed a clear pattern, in which the outcome does not rely upon needle location or even needle insertion, and since "these variables are those that define acupuncture, the only sensible conclusion is that acupuncture does not work."
Pain
A 2014 systematic review suggests that the nocebo effect of acupuncture is clinically relevant and that the rate of adverse events may be a gauge of the nocebo effect. A 2012 meta-analysis conducted by the Acupuncture Trialists' Collaboration found "relatively modest" efficiency of acupuncture (in comparison to sham) for the treatment of four different types of chronic pain, and on that basis concluded that it "is more than a placebo" and a reasonable referral option. Commenting on this meta-analysis, both Edzard Ernst and David Colquhoun said the results were of negligible clinical significance. Edzard Ernst later stated that "I fear that, once we manage to eliminate this bias … we might find that the effects of acupuncture exclusively are a placebo response." Andrew Vickers, lead author of the original 2012 paper and chair of the Acupuncture Trialists' Collaboration, rejects that analysis, stating that the differences between acupuncture and sham acupuncture are statistically significant.
A 2011 overview of high-quality Cochrane reviews suggested that acupuncture is effective for some but not all kinds of pain. A 2011 systematic review of systematic reviews which highlighted recent high-quality RCTs found that for reducing pain, real acupuncture was no better than sham acupuncture, and concluded that numerous reviews have shown little convincing evidence that acupuncture is an effective treatment for reducing pain. The same review found that neck pain was one of only four types of pain for which a positive effect was suggested, but cautioned that the primary studies used carried a considerable risk of bias.
A 2010 systematic review suggested that acupuncture is more than a placebo for commonly occurring chronic pain conditions, but the authors acknowledged that it is still unknown if the overall benefit is clinically meaningful or cost-effective. A 2010 review found real acupuncture and sham acupuncture produce similar improvements, which can only be accepted as evidence against the efficacy of acupuncture. The same review found limited evidence that real acupuncture and sham acupuncture appear to produce biological differences despite similar effects. A 2009 systematic review and meta-analysis found that acupuncture had a small analgesic effect, which appeared to lack any clinical importance and could not be discerned from bias. The same review found that it remains unclear whether acupuncture reduces pain independent of a psychological impact of the needling ritual.
According to Miller's Anesthesia acupuncture treatment has proven efficacy for relieving pain when compared to placebo treatment.
Low back
A 2013 systematic review found supportive evidence that real acupuncture may be more effective than sham acupuncture with respect to relieving lower back pain, but there were methodological limitations with the studies. A 2013 systematic review found that acupuncture may be effective for nonspecific lower back pain, but the authors noted there were limitations in the studies examined, such as heterogeneity in study characteristics and low methodological quality in many studies. A 2012 systematic review found some supporting evidence that acupuncture was more effective than no treatment for chronic non-specific low back pain; the evidence was conflicting comparing the effectiveness over other treatment approaches. A 2011 overview of Cochrane reviews found inconclusive evidence regarding acupuncture efficacy in treating low back pain. A 2011 systematic review of systematic reviews found that "for chronic low back pain, individualized acupuncture is not better in reducing symptoms than formula acupuncture or sham acupuncture with a toothpick that does not penetrate the skin." A 2013 meta-analysis found that acupuncture was better than no treatment for reducing lower back pain, but not better than sham acupuncture, and concluded that the effect of acupuncture "is likely to be produced by the nonspecific effects of manipulation". A 2010 review found that sham acupuncture was as effective as real acupuncture for chronic low back pain. The specific therapeutic effects of acupuncture were small, whereas its clinically relevant benefits were mostly due to contextual and psychosocial circumstances. Brain imaging studies have shown that traditional acupuncture and sham acupuncture differ in their effect on limbic structures, while at the same time showed equivalent analgesic effects. A 2005 Cochrane review found insufficient evidence to recommend for or against either acupuncture or dry needling for acute low back pain. The same review found low quality evidence for pain relief and improvement compared to no treatment or sham therapy for chronic low back pain only in the short term immediately after treatment. The same review also found that acupuncture is not more effective than conventional therapy and other alternative medicine treatments.
Headaches and migraines
A 2012 review found that acupuncture has demonstrated benefit for the treatment of headaches, but that safety needed to be more fully documented in order to make any strong recommendations in support of its use. A 2009 Cochrane review of the use of acupuncture for migraine prophylaxis treatment concluded that "true" acupuncture was no more efficient than sham acupuncture, but "true" acupuncture appeared to be as effective as, or possibly more effective than routine care in the treatment of migraines, with fewer adverse effects than prophylactic drug treatment. The same review stated that the specific points chosen to needle may be of limited importance. A 2009 Cochrane review found insufficient evidence to support acupuncture for tension-type headaches. The same review found evidence that suggested that acupuncture might be considered a helpful non-pharmacological approach for frequent episodic or chronic tension-type headache. A separate 2009 Cochrane review found that acupuncture could be useful in the prophylaxis of tension-type headaches.
Osteoarthritis
As of 2014 a meta-analysis showed that acupuncture may help osteoarthritis pain but it was noted that the effects were insignificant in comparison to sham needles. A 2013 systematic review and network meta-analysis found that the evidence suggests that acupuncture may be considered one of the more effective physical treatments for alleviating pain due to knee osteoarthritis in the short-term compared to other relevant physical treatments, though much of the evidence in the topic is of poor quality and there is uncertainty about the efficacy of many of the treatments. A 2012 review found "the potential beneficial action of acupuncture on osteoarthritis pain does not appear to be clinically relevant." A 2014 review concluded that "current evidence supports the use of acupuncture as an alternative to traditional analgesics in osteoarthritis patients." A 2010 Cochrane review found that acupuncture shows statistically significant benefit over sham acupuncture in the treatment of peripheral joint osteoarthritis; however, these benefits were found to be so small that their clinical significance was doubtful, and "probably due at least partially to placebo effects from incomplete blinding". A guideline issued by the National Clinical Guideline Centre stated that acupuncture should not be used in osteoarthritis management.
Extremity conditions
A 2007 review found that acupuncture was significantly better than sham acupuncture at treating chronic knee pain; the evidence was not conclusive due to the lack of large, high-quality trials. A 2014 systematic review found moderate quality evidence that acupuncture was more effective than sham acupuncture in the treatment of lateral elbow pain. A 2014 systematic review found that although manual acupuncture was effective at relieving short-term pain when used to treat tennis elbow, its long-term effect in relieving pain was "unremarkable".
A 2011 overview of Cochrane reviews found inconclusive evidence regarding acupuncture efficacy in treating shoulder pain and lateral elbow pain.
Nausea and vomiting and post-operative pain
A 2014 overview of systematic reviews found insufficient evidence to suggest that acupuncture is an effective treatment for postoperative nausea and vomiting (PONV) in a clinical setting. A 2013 systematic review concluded that acupuncture might be beneficial in prevention and treatment of PONV. A 2009 Cochrane review found that stimulation of the P6 acupoint on the wrist was as effective (or ineffective) as antiemetic drugs and was associated with minimal side effects. The same review found "no reliable evidence for differences in risks of postoperative nausea or vomiting after P6 acupoint stimulation compared to antiemetic drugs."
A 2014 overview of systematic reviews found insufficient evidence to suggest that acupuncture is effective for surgical or post-operative pain. For the use of acupuncture for post-operative pain, there was contradictory evidence. A 2014 systematic review found supportive but limited evidence for use of acupuncture for acute post-operative pain after back surgery. A 2014 systematic review found that while the evidence suggested acupuncture could be an effective treatment for postoperative gastroparesis, a firm conclusion could not be reached because the trials examined were of low quality.
Clinical practice guidelines issued recently by the American College of Chest Physicians have stated that "in patients having nausea and vomiting from either chemotherapy or radiation therapy, acupuncture or related techniques is suggested as an adjunct treatment option". The Society of Obstetricians and Gynaecologists of Canada recommended that "acupoint electrical stimulation may be used as an alternative or adjuvant therapy for prevention of PONV."
Allergies
A 2015 meta-analysis suggests that acupuncture might be a good option for people with allergic rhinitis (AR). Several randomized clinical trials (RCTs) support the use of acupuncture for AR and itch. Experimental studies refer to a specific effect of acupuncture in atopic eczema and asthma, but large RCTs are lacking. Using acupuncture to treat other allergic conditions such as contact eczema, drug rashes, or anaphylaxis is not recommended. Additional research is required to clearly determine any effects of allergic disease therapy above placebo. There is insufficient evidence that acupuncture has specific effects on seasonal allergic rhinitis (SAR). There is some evidence that acupuncture might have specific effects on perennial allergic rhinitis (PAR), though all of the efficacy studies were small and conclusions should be made with caution. There is mixed evidence for the symptomatic treatment or prevention of AR. For seasonal AR, the evidence failed to demonstrate specific effects for acupuncture. For perennial AR, there was suggestive evidence for the effectiveness of acupuncture. Acupuncture is an unproven treatment for allergic-immunologic conditions. A 2015 clinical practice guideline released by the American Academy of Otolaryngology – Head and Neck Surgery stated that clinicians may offer acupuncture as a treatment for allergic rhinitis to patients interested in non-pharmacologic treatments. The confidence in the evidence of effectiveness of acupuncture for this condition was low.
Cancer-related conditions
A 2012 systematic review of randomised clinical trials (RCTs) using acupuncture in the treatment of cancer pain found that the number and quality of RCTs was too low to draw definite conclusions. A 2011 Cochrane review found that there is insufficient evidence to determine whether acupuncture is an effective treatment for cancer pain in adults. A 2014 systematic review found that acupuncture may be effective as an adjunctive treatment to palliative care for cancer patients. A 2013 overview of reviews found evidence that acupuncture could be beneficial for people with cancer-related symptoms, but also identified few rigorous trials and high heterogeneity between trials.
A 2013 systematic review found that acupuncture is an acceptable adjunctive treatment for chemotherapy-induced nausea and vomiting, but that further research with a low risk of bias is needed. A 2013 systematic review found that the quantity and quality of available RCTs for analysis were too low to draw valid conclusions for the effectiveness of acupuncture for cancer-related fatigue. A 2014 systematic review reached inconclusive results with regard to the effectiveness of acupuncture for treating cancer-related fatigue. A 2012 systematic review and meta-analysis found very limited evidence regarding the effectiveness of acupuncture compared with conventional intramuscular injections for the treatment of hiccups in cancer patients. The methodological quality and amount of RCTs in the review was low. In 2013, the American College of Chest Physicians stated that "in patients with cancer related pain and peripheral neuropathy, acupuncture is suggested as an adjunct treatment in patients with inadequate control of symptoms".
Fertility and childbirth
A 2014 systematic review and meta-analysis found poor quality evidence for use of acupuncture in infertile men to improve sperm motility, sperm concentration, and the pregnancy rate; the evidence was rated as insufficient to draw any conclusion regarding efficacy. A 2013 Cochrane review found no evidence of acupuncture for improving the success of in vitro fertilization (IVF). A 2013 systematic review found no benefit of adjuvant acupuncture for IVF on pregnancy success rates. A 2012 systematic review found that acupuncture may be a useful adjunct to IVF, but its conclusions were rebutted after reevaluation using more rigorous, high quality meta-analysis standards. A 2011 overview of systematic reviews found that the evidence that acupuncture was effective was not compelling for most gynecologic conditions. The exceptions to this conclusion included the use of acupuncture during embryo transfer as an adjunct to in vitro fertilization. A 2012 systematic review and meta-analysis found that acupuncture did not significantly improve the outcomes of in vitro fertilization.
Rheumatological conditions
A 2013 Cochrane review found low to moderate evidence that acupuncture improves pain and stiffness in treating people with fibromyalgia compared with no treatment and standard care. A 2012 review found "there is insufficient evidence to recommend acupuncture for the treatment of fibromyalgia." A 2010 systematic review found a small pain relief effect that was not apparently discernible from bias; acupuncture is not a recommendable treatment for the management of fibromyalgia on the basis of this review.
A 2012 review found that the effectiveness of acupuncture to treat rheumatoid arthritis is "sparse and inconclusive." A 2005 Cochrane review concluded that acupuncture use to treat rheumatoid arthritis "has no effect on ESR, CRP, pain, patient's global assessment, number of swollen joints, number of tender joints, general health, disease activity and reduction of analgesics." A 2010 overview of systematic reviews found insufficient evidence to recommend acupuncture in the treatment of most rheumatic conditions, with the exceptions of osteoarthritis, low back pain, and lateral elbow pain.
Stroke
A 2014 overview of systematic reviews and meta-analyses found that the evidence does not demonstrate acupuncture helps reduce the rates of death or disability after a stroke or improve other aspects of stroke recovery, such as poststroke motor dysfunction, but the evidence suggests it may help with poststroke neurological impairment and dysfunction such as dysphagia, which would need to be confirmed with future rigorous studies. A 2012 review found evidence of benefit for acupuncture combined with exercise in treating shoulder pain after stroke. A 2010 systematic review found that acupuncture was not effective as a treatment for functional recovery after a stroke. A 2008 Cochrane review found that evidence was insufficient to draw any conclusion about the effect of acupuncture on dysphagia after acute stroke. A 2006 Cochrane review found no clear evidence for acupuncture on subacute or chronic stroke. A 2005 Cochrane review found no clear evidence of benefit for acupuncture on acute stroke. A 2014 meta-analysis found tentative evidence for acupuncture in cerebral infarction, a type of ischemic stroke, but the authors noted the trials reviewed were often of poor quality. Another 2014 meta-analysis found that the effectiveness of acupuncture for treating spasticity after a stroke was uncertain as the studies available were of poor quality. A 2015 systematic review and meta-analysis found that acupuncture could be effective to treat spasticity after stroke, but called for more studies to be conducted to determine how long its effects lasted.
Other conditions
For the following conditions, the Cochrane Collaboration or other reviews have concluded there is no strong evidence of benefit: alcohol dependence, angina pectoris, ankle sprain, attention deficit hyperactivity disorder, autism, asthma, bell's palsy, traumatic brain injury, carpal tunnel syndrome, chronic obstructive pulmonary disease, cardiac arrhythmias, cerebral hemorrhage, cocaine dependence, constipation, depression, diabetic peripheral neuropathy, drug detoxification, dry eye, primary dysmenorrhoea, dyspepsia, enuresis, endometriosis, epilepsy, erectile dysfunction, essential hypertension, glaucoma, gynaecological conditions (except possibly fertility and nausea/vomiting), hot flashes, hypoxic ischemic encephalopathy in neonates, insomnia, induction of childbirth, irritable bowel syndrome, labor induction, labor pain, lumbar spinal stenosis, major depressive disorders in pregnant women, myopia, obesity, obstetrical conditions, Parkinson's disease, polycystic ovary syndrome, premenstrual syndrome, preoperative anxiety, psychological symptoms associated with opioid addiction, restless legs syndrome, schizophrenia, sensorineural hearing loss, smoking cessation, stress urinary incontinence, acute stroke, stroke rehabilitation, temporomandibular joint dysfunction, tennis elbow, tinnitus, uremic itching, uterine fibroids, vascular dementia, and whiplash.
Moxibustion and cupping
A 2010 overview of systematic reviews found that moxibustion was effective for several conditions but the primary studies were of poor quality, so there persists ample uncertainty, which limits the conclusiveness of their findings. A 2012 systematic review suggested that cupping therapy seems to be effective for herpes zoster and various other conditions but due to the high risk of publication bias, larger studies are needed to draw definitive conclusions.
Safety
Adverse events
Acupuncture is generally safe when administered by an experienced, appropriately trained practitioner using clean technique and sterile single-use needles. When not delivered properly by a qualified practitioner it can cause potentially serious adverse effects. To reduce the risk of serious adverse events after acupuncture, acupuncturists should be trained sufficiently. People with serious spinal disease, such as cancer or infection, are not good candidates for acupuncture. Contraindications to acupuncture are conditions that should not be treated with acupuncture; these contraindications include coagulopathy disorders (e.g. haemophilia and advanced liver disease), warfarin use, severe psychiatric disorders (e.g. psychosis), and skin infections or skin trauma (e.g. burns). Further, electroacupuncture should be avoided at the spot of implanted electrical devices (e.g. pacemakers).
A 2011 systematic review of systematic reviews (internationally and without language restrictions) found that serious complications following acupuncture continue to be reported. Between 2000 and 2009, ninety-five cases of serious adverse events, including five deaths, were reported. Many such events are not inherent to acupuncture but are due to malpractice of acupuncturists. This might be why such complications have not been reported in surveys of adequately-trained acupuncturists. Most such reports are from Asia, which may reflect the large number of treatments performed there or it might be because there are a relatively higher number of poorly trained Asian acupuncturists. Many serious adverse events were reported from developed countries. This included Australia, Austria, Canada, Croatia, France, Germany, Holland, Ireland, New Zealand, Spain, Sweden, Switzerland, the UK, and the US. The number of adverse effects reported from the UK appears particularly unusual, which may indicate less under-reporting in the UK than other countries. 38 cases of infections were reported and 42 cases of organ trauma were reported. The most frequent adverse events included pneumothorax, and bacterial and viral infections.
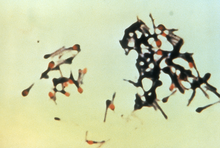
A 2013 review found (without restrictions regarding publication date, study type or language) 295 cases of infections; mycobacterium was the pathogen in at least 96%. Likely sources of infection include towels, hot packs or boiling tank water, and reusing reprocessed needles. Possible sources of infection include contaminated needles, reusing personal needles, a person's skin contained mycobacterium and reusing needles at various sites in the same person. Although acupuncture is generally considered a safe procedure, in the last decade reports of infection transmission have increased significantly, including those of mycobacterium. Although it is recommended that practitioners of acupuncture use disposable needles, the reuse of sterilized needles is still permitted. It is also recommended that thorough control practices for preventing infection be implemented and adapted.
English-language
A 2013 systematic review of the English-language case reports found that serious adverse events associated with acupuncture are rare, but acupuncture is not without risk. Between 2000 and 2011, there were 294 adverse events reported in the English-language literature from 25 countries and regions. The majority of the reported adverse events were relatively minor, and the incidences were low. For example, a prospective survey of 34,000 acupuncture treatments found no serious adverse events and 43 minor ones, a rate of 1.3 per 1000 interventions. Another survey found there were 7.1% minor adverse events, of which 5 were serious, amid 97,733 acupuncture patients. The most common adverse effect observed was infection (e.g. mycobacterium), and the majority of infections were bacterial in nature, caused by skin contact at the needling site. Infection has also resulted from skin contact with unsterilized equipment or dirty towels, in an unhygienic clinical setting. Other adverse complications included five reported cases of spinal cord injuries (e.g. migrating broken needles or needling too deeply), four brain injuries, four peripheral nerve injuries, five heart injuries, seven other organ and tissue injuries, bilateral hand edema, epithelioid granuloma, pseudolymphoma, argyria, pustules, pancytopenia, and scarring due to hot needle technique. Adverse reactions from acupuncture, which are unusual and uncommon in typical acupuncture practice, were syncope, galactorrhoea, bilateral nystagmus, pyoderma gangrenosum, hepatotoxicity, eruptive lichen planus, and spontaneous needle migration.
A 2013 systematic review found 31 cases of vascular injuries were caused by acupuncture, 3 resulting in death. Two died from pericardial tamponade and one was from an aortoduodenal fistula. The same review found vascular injuries were rare, bleeding and pseudoaneurysm were most prevalent. A 2011 systematic review (without restriction in time or language), aiming to summarize all reported case of cardiac tamponade after acupuncture, found 26 cases resulting in 14 deaths, with little doubt about causality in most fatal instances. The same review concluded cardiac tamponade was a serious, usually fatal, though theoretically avoidable complication following acupuncture, and urged training to minimize risk.
A 2012 review found a number of adverse events were reported after acupuncture in the UK's National Health Service (NHS) but most (95%) were not severe. Though, miscategorization and under-reporting may alter the total figures. From January 2009 to December 2011, there were 468 safety incidents recognized within the NHS organizations. The adverse events recorded included retained needles (31%), dizziness (30%), loss of consciousness/unresponsive (19%), falls (4%), bruising or soreness at needle site (2%), pneumothorax (1%) and other adverse side effects (12%). Acupuncture practitioners should know, and be prepared to be responsible for, any substantial harm from treatments. Some acupuncture proponents argue that because of its long history this suggests it is safe. However, there is an increasing literature on adverse events (e.g. spinal cord injury).
Acupuncture seems to be safe in people getting anticoagulants, assuming needles are used at the correct location and depth. Studies are required to verify these findings. The evidence suggests that acupuncture might be a safe option for people with allergic rhinitis.
Chinese, South Korean, and Japanese-language
A 2010 systematic review of the Chinese-language literature found numerous acupuncture-related adverse events including pneumothorax, fainting, subarachnoid hemorrhage, and infection as the most frequent, and cardiovascular injuries, subarachnoid hemorrhage, pneumothorax, and recurrent cerebral hemorrhage as the most serious, most of which were due to improper technique. Between 1980 and 2009, the Chinese-language literature reported 479 adverse events. Prospective surveys shown that mild, transient acupuncture-associated adverse events ranged from 6.71% to 15%. A study with 190,924 patients, the prevalence of serious adverse events was roughly 0.024%. Another study shown a rate of adverse events requiring specific treatment was 2.2%, 4,963 incidences were among 229,230 patients. Infections, mainly hepatitis, after acupuncture are reported often in the English-language research, though it is rarely reported in the Chinese-language research, making it plausible that in China acupuncture-associated infections have been underreported. Infections were mostly caused by poor sterilization of acupuncture needles. Other adverse events included spinal epidural haematoma (in the cervical, thoracic and lumbar spine), chylothorax, injuries of abdominal organs and tissues, injuries in the neck region, injuries to the eyes, including orbital hemorrhage, traumatic cataract, injury of the oculomotor nerve and retinal puncture, hemorrhage to the cheeks and the hypoglottis, peripheral motor nerve injuries and subsequent motor dysfunction, local allergic reactions to metal needles, stroke, and cerebral hemorrhage after acupuncture.
A causal link between acupuncture and the adverse events cardiac arrest, pyknolepsy, shock, fever, cough, thirst, aphonia, leg numbness, and sexual dysfunction remains uncertain. The same review concluded that acupuncture can be considered inherently safe when practiced by properly trained practitioners, but the review also stated there is a need to find effective strategies to minimize the health risks. Between 1999 and 2010, the Republic of Korean-literature contained reports of 1104 adverse events. Between the 1980s and 2002, the Japanese-language literature contained reports of 150 adverse events.
Children and pregnancy
When used on children, acupuncture is safe when administered by well-trained, licensed practitioners using sterile needles; however, a 2011 review found there was limited research to draw definite conclusions about the overall safety of pediatric acupuncture. The same review found 279 adverse events, of which 25 were serious. The adverse events were mostly mild in nature (e.g. bruising or bleeding). The prevalence of mild adverse events ranged from 10.1% to 13.5%, an estimated 168 incidences were among 1,422 patients. On rare occasions adverse events were serious (e.g. cardiac rupture or hemoptysis), many might have been a result of substandard practice. The incidence of serious adverse events was 5 per one million, which included children and adults. When used during pregnancy, the majority of adverse events caused by acupuncture were mild and transient, with few serious adverse events. The most frequent mild adverse event was needling or unspecified pain, followed by bleeding. Although two deaths (one stillbirth and one neonatal death) were reported, there was a lack of acupuncture associated maternal mortality. Limiting the evidence as certain, probable or possible in the causality evaluation, the estimated incidence of adverse events following acupuncture in pregnant women was 131 per 10,000. Although acupuncture is not contraindicated in pregnant women, some specific acupuncture points that are particularly sensitive to needle insertion; these spots, as well as the abdominal region, should be avoided during pregnancy.
Moxibustion and cupping
Four adverse events associated with moxibustion were bruising, burns and cellulitis, spinal epidural abscess, and large superficial basal cell carcinoma. Ten adverse events were associated with cupping. The minor ones were keloid scarring, burns, and bullae; the serious ones were acquired hemophilia A, stroke following cupping on the back and neck, factitious panniculitis, reversible cardiac hypertrophy, and iron deficiency anemia.
Cost-effectiveness
A 2013 meta-analysis found that acupuncture for chronic low back pain was cost-effective as a complement to standard care, but not as a substitute for standard care except in cases where comorbid depression presented. The same meta-analysis found there was no difference between sham and non-sham acupuncture. A 2011 systematic review found insufficient evidence for the cost-effectiveness of acupuncture in the treatment of chronic low back pain. A 2010 systematic review found that the cost-effectiveness of acupuncture could not be concluded. A 2012 review found that acupuncture was cost-effective for some pain conditions.
Risk of forgoing conventional medical care
As with other alternative medicines, unethical or naïve practitioners may induce patients to exhaust financial resources by pursuing ineffective treatment. Profession ethical codes set by accrediting organizations such as the National Certification Commission for Acupuncture and Oriental Medicine require practitioners to make "timely referrals to other health care professionals as may be appropriate."
Conceptual basis
| Acupuncture | |||||||
|---|---|---|---|---|---|---|---|
| Simplified Chinese | 针刺 | ||||||
| |||||||
Acupuncture, a type of pseudoscience that enjoys some popularity in contemporary society, is a key component of traditional Chinese medicine (TCM), a medical system which a Nature editorial described as "fraught with pseudoscience", with the majority of its treatments having no logical mechanism of action. Many within the scientific community consider it to be quackery and pseudoscience. Massimo Pigliucci and Maarten Boudry describe it as a "borderlands science" lying between normal science and pseudoscience. Acupuncture has notions of a superstitious pre-scientific culture, similar to European humoral theory. According to TCM, the general theory of acupuncture is based on the premise that bodily functions are regulated by an energy called qi (氣) that flows through the body; disruptions of this flow are believed to be responsible for disease. Health is viewed by traditional acupuncturists as a balance of yin and yang, sometimes equated to the sympathetic and parasympathetic nervous systems. Acupuncture describes a family of procedures aiming to correct imbalances in the flow of qi by stimulation of anatomical locations on or under the skin (usually called acupuncture points or acupoints), by a variety of techniques. The most common mechanism of stimulation of acupuncture points employs penetration of the skin by thin metal needles, which are manipulated manually or the needle may be further stimulated by electrical stimulation (electroacupuncture).
Qi, meridians and acupuncture points
Main articles: Qi, Traditional Chinese medicine § Model of the body, Meridian (Chinese medicine), and Acupuncture pointTraditional Chinese medicine (TCM) distinguishes several different kinds of qi. In a general sense, qi is something that is defined by five "cardinal functions":

Actuation (推動, tuīdòng) is of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians. Warming (溫煦, pinyin: wēnxù) the body, especially the limbs. Defense (防御, pinyin: fángyù) against Exogenous Pathogenic Factors Containment (固攝, pinyin: gùshè) of body fluids, i.e. keeping blood, sweat, urine, semen etc. from leakage or excessive emission. Transformation (氣化, pinyin: qìhuà) of food, drink, and breath into qi, xue (blood), and jinye ("fluids"), and/or transformation of all of the latter into each other.
To fulfill its functions, qi has to steadily flow from the inside of the body (where the zang-fu organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints. It is assisted in its flow by "channels" referred to as meridians. TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài). There's also a number of less customary channels branching off from the "regular" meridians. Contemporary research has not supported the existence of qi or meridians. The meridians are believed to connect to the bodily organs, of which those considered hollow organs (such as the stomach and intestines) were also considered yang while those considered solid (such as the liver and lungs) were considered yin. They were also symbolically linked to the rivers found in ancient China, such as the Yangtze, Wei and Yellow Rivers.
Acupuncture points are mainly (but not always) found at specified locations along the meridians. There also is a number of acupuncture points with specified locations outside of the meridians; these are called extraordinary points and are credited to treat certain diseases. A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes. The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in Han times, the number of bones thought to be in the body). The Neijing mentioned only 160 and a further 135 could be deduced giving a total of 295. The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions. In addition, it is considered likely that some points used historically have since ceased being used.
TCM concept of disease
See also: Traditional Chinese medicine § Concept of diseaseIn TCM, disease is generally perceived as a disharmony or imbalance in the functions or interactions of such concepts as yin, yang, qi, xuĕ, zàng-fǔ, meridians, and of the interaction between the body and the environment. Therapy is based on which "pattern of disharmony" can be identified. In the case of the meridians, typical disease patterns are invasions with wind, cold, and damp Excesses. In order to determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing, or the sound of the voice. TCM and its concept of disease do not strongly differentiate between cause and effect. In theory, however, endogenous, exogenous and miscellaneous causes of disease are recognized.
Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient to make a diagnosis according to the tradition used. In TCM, the four diagnostic methods are: inspection, ausculation and olfaction, inquiring, and palpation. Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge. Auscultation and olfaction is listening for particular sounds (such as wheezing) and attending to body odor. Inquiring is focusing on the "seven inquiries": chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea. Palpation is focusing on feeling the body for tender A-shi points and feeling the left and right radial pulses. There is significant heterogeneity among acupuncturists considering appropriate treatment protocols.
Tongue and pulse
Examination of the tongue and the pulse are among the principal diagnostic methods in TCM. Certain sectors of the tongue's surface are believed to correspond to the zàng-fŭ. For example, teeth marks on one part of the tongue might indicate a problem with the heart, while teeth marks on another part of the tongue might indicate a problem with the liver.
Pulse palpation involves measuring the pulse at a superficial and at a deep level at three locations on the radial artery (Cun, Guan, Chi, located two fingerbreadths from the wrist crease, one fingerbreadth from the wrist crease, and right at the wrist crease, respectively, usually palpated with the index, middle and ring finger) of each arm, for 12 pulses, all of which are thought to correspond with certain zàng-fŭ. The pulse is examined for several characteristics including rhythm, strength, and volume, and is described with qualities like "floating, slippery, bolstering-like, feeble, thready and quick". Each of these qualities indicate certain disease patterns. Training on the use of TCM pulse diagnosis can take several years.
Scientific view on TCM theory

Some modern practitioners have embraced the use of acupuncture to treat pain, but have abandoned the use of qi, meridians, yin and yang as explanatory frameworks. Some practitioners no longer consider the idea of an energy flow to apply. They, along with acupuncture researchers, explain the analgesic effects of acupuncture as caused by the release of endorphins, and recognize the lack of evidence that it can affect the course of any disease. A 2014 review stated that despite ample controversy encircling the validity of acupuncture as a modality, developing literature on its physiological effects in animals and humans is giving new views into the basic mechanisms for acupuncture needling. The same review proposed a model combining both connective tissue plasticity and peripheral sensory modulation as a needle response for acupuncture's physiological effects.
It is a generally held belief within the acupuncture community that acupuncture points and meridians structures are special conduits for electrical signals but no research has established any consistent anatomical structure or function for either acupuncture points or meridians. The electrical resistance of acupuncture points and meridians have also been studied, with conflicting results. There has been little systematic investigation of which components of an acupuncture session may be important for any therapeutic effect, including needle placement and depth, type and intensity of stimulation, and number of needles used.
Quackwatch states that:
TCM theory and practice are not based upon the body of knowledge related to health, disease, and health care that has been widely accepted by the scientific community. TCM practitioners disagree among themselves about how to diagnose patients and which treatments should go with which diagnoses. Even if they could agree, the TCM theories are so nebulous that no amount of scientific study will enable TCM to offer rational care.
Acupuncture analgesia
The evidence indicates that acupuncture-induced pain relief effect, known as acupuncture analgesia, has physiological, anatomical and neurochemical origins. The mechanism of action for acupuncture is still unclear. Evidence suggests that acupuncture generates a sequence of events that include the release of endogenous opioid-like substances that modulate pain signals within the central nervous system, and that it is possible to inhibit acupuncture's analgesic effects with the opioid antagonist naloxone. Mechanical deformation of the skin by acupuncture needles appears to result in the release of adenosine. A 2014 Nature Reviews Cancer review journal found that the key mouse studies that suggested acupuncture relieves pain via the local release of adenosine, which then triggered close-by A1 receptors "caused more tissue damage and inflammation relative to the size of the animal in mice than in humans, such studies unnecessarily muddled a finding that local inflammation can result in the local release of adenosine with analgesic effect." The anti-nociceptive effect of acupuncture may be mediated by the adenosine A1 receptor. Electroacupuncture may inhibit pain by the activation of a variety of bioactive chemicals through peripheral, spinal, and supraspinal mechanisms of the nervous system.
Mechanisms in other conditions
It has been proposed that acupuncture's effects in gastrointestinal disorders may relate to its effects on the parasympathetic and sympathetic nervous system, which have been said to be the "Western medicine" equivalent of "yin and yang". Acupuncture has also been found to exert anti-inflammatory effects, which may be mediated by the activation of the vagus nerve and deactivation of inflammatory macrophages.
History
Antiquity

The precise start date that acupuncture was generally held to have originated in ancient China and how it evolved from early times is uncertain. Chinese history attributes the introduction of acupuncture to the emperor Shennong. One explanation is that Han Chinese doctors observed that some soldiers wounded in battle by arrows were believed to have been cured of chronic afflictions that were otherwise untreated, and there are variations on this idea. Sharpened stones known as Bian shi have been found in China, suggesting the practice may date to the Neolithic or possibly even earlier in the Stone Age. Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) which suggests that acupuncture was practiced along with moxibustion. It has also been suggested that acupuncture has its origins in bloodletting or demonology.
Despite improvements in metallurgy over centuries, it was not until the 2nd century BCE during the Han Dynasty that stone and bone needles were replaced with metal. The earliest examples of metal needles were found in a tomb dated to c. 113 BCE, though their use might not necessarily have been acupuncture. The earliest example of the unseen meridians (经络, pinyin: jīng-luò) used for diagnosis and treatment are dated to the second century BCE but these records do not mention needling, while the earliest reference to therapeutic needling occurs in the historical Shiji text (史記, English: Records of the Grand Historian) but does not mention the meridians and may be a reference to lancing rather than acupuncture.
The earliest written record of acupuncture is found in the Huangdi Neijing (黄帝内经; translated as The Yellow Emperor's Inner Canon), dated approximately 200 BCE. It does not distinguish between acupuncture and moxibustion and gives the same indication for both treatments. The Mawangdui texts, which also date from the 2nd century BCE (though antedating both the Shiji and Huangdi Neijing), mention the use of pointed stones to open abscesses, and moxibustion, but not acupuncture. However, by the 2nd century BCE, acupuncture replaced moxibustion as the primary treatment of systemic conditions.
The practice of acupuncture expanded out of China into the areas now part of Japan, Korea, Vietnam and Taiwan, diverging from the narrower theory and practice of mainland TCM in the process. A large number of contemporary practitioners outside of China follow these non-TCM practices, particularly in Europe.
In Europe, examinations of the 5,000-year-old mummified body of Ötzi the Iceman have identified 15 groups of tattoos on his body, some of which are located on what are now seen as contemporary acupuncture points. This has been cited as evidence that practices similar to acupuncture may have been practiced elsewhere in Eurasia during the early Bronze Age.
Middle history
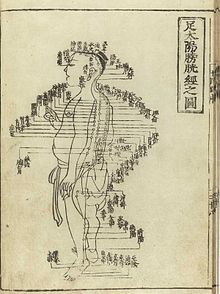
Korea is believed to be the second country that acupuncture spread to outside of China. Within Korea there is a legend that acupuncture was developed by the legendary emperor Dangun though it is more likely to have been brought into Korea from a Chinese colonial prefecture.
Around 90 works on acupuncture were written in China between the Han Dynasty and the Song Dynasty, and the Emperor Renzong of Song, in 1023, ordered the production of a bronze statuette (Dongren) depicting the meridians and acupuncture points then in use. However, after the end of the Song Dynasty, acupuncture lost status, and started to be seen as a technical profession, in comparison to the more scholarly profession of herbalism. It became rarer in the following centuries, and was associated with less prestigious practices like alchemy, shamanism, midwifery and moxibustion.
Portuguese missionaries in the 16th century were among the first to bring reports of acupuncture to the West. Jacob de Bondt, a Dutch surgeon traveling in Asia, described the practice in both Japan and Java. However, in China itself the practice was increasingly associated with the lower-classes and illiterate practitioners.
In 1674, Hermann Buschoff, a Dutch priest in Batavia, published the first book on moxibustion (from Japanese mogusa). The first elaborate Western treatise on acupuncture was published in 1683 by Willem ten Rhijne, a Dutch physician who had worked at the Dutch trading post Dejima in Nagasaki for two years. In 1712 a detailed description of the treatment of "Colics" in Japan was published by the German physician Engelbert Kaempfer. But while moxibustion was widely discussed among central European physicians, ten Rhijne's and especially Kaempfer's explanations about piercing the abdomen had caused some misunderstandings that eventually led to the refutal of acupuncture by influential scholars such as Lorenz Heister and Georg Stahl.
In 1757 the Chinese physician Xu Daqun described the further decline of acupuncture, saying it was a lost art, with few experts to instruct; its decline was attributed in part to the popularity of prescriptions and medications, as well as its association with the lower classes. In 1822, an edict from the Emperor Daoguang banned the practice and teaching of acupuncture within the Imperial Academy of Medicine outright, as unfit for practice by gentlemen-scholars. At this point, acupuncture was still cited in Europe with both skepticism and praise, with little study and only a small amount of experimentation.
While the details of how acupuncture came to Europe are debated, the French doctor Louis Berlioz (the father of the composer Hector Berlioz) is usually credited with first experimenting the procedure in 1810, before publishing his findings in 1816. In the United States, the earliest reports of acupuncture date back to 1826, when Franklin Bache, a surgeon of the United States Navy, published a report in the North American Medical and Surgical Journal on his use of acupuncture to treat lower back pain. Since the beginning of the 19th century, acupuncture was practiced by Asian immigrants living in Chinatowns.
Modern era
In the early years after the Chinese Civil War, Chinese Communist Party leaders ridiculed traditional Chinese medicine, including acupuncture, as superstitious, irrational and backward, claiming that it conflicted with the Party's dedication to science as the way of progress. Communist Party Chairman Mao Zedong later reversed this position, saying that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level." Under Mao's leadership, in response to the lack of modern medical practitioners, acupuncture was revived and its theory rewritten to adhere to the political, economic and logistic necessities of providing for the medical needs of China's population. Despite Mao proclaiming the practice of Chinese medicine to be "scientific", the practice was based more on the materialist assumptions of Marxism in opposition to superstition rather than the Western practice of empirical investigation of nature. Later the 1950s TCM's theory was again rewritten at Mao's insistence as a political response to the lack of unity between scientific and traditional Chinese medicine, and to correct the supposed "bourgeois thought of Western doctors of medicine". Despite publicly promoting the practice, Mao himself did not believe in or use traditional Chinese medicine.
Acupuncture gained attention in the United States when the U.S. President Richard Nixon visited China in 1972. During one part of the visit, the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia. Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients. One patient receiving open heart surgery while awake was ultimately found to have received a combination of three powerful sedatives as well as large injections of a local anesthetic into the wound.
The greatest exposure in the West came after New York Times reporter James Reston received acupuncture in Beijing for post-operative pain in 1971 and wrote complaisantly about it in his newspaper. In 1972 the first legal acupuncture center in the U.S. was established in Washington DC; during 1973-1974, this center saw up to one thousand patients. In 1973 the American Internal Revenue Service allowed acupuncture to be deducted as a medical expense.
Acupuncture has been the subject of active scientific research both in regard to its basis and therapeutic effectiveness since the late 20th century. Even though acupuncture is currently widely used in clinical practice, it remains a controversial topic. In 2006, a BBC documentary Alternative Medicine filmed a patient undergoing open heart surgery allegedly under acupuncture-induced anesthesia. It was later revealed that the patient had been given a cocktail of weak anesthetics that in combination could have a much more powerful effect. The program was also criticized for its fanciful interpretation of the results of a brain scanning experiment. In 2010, acupuncture was recognized by UNESCO as part of the world's intangible cultural heritage.
Ethics
The National Institutes of Health (NIH) consensus statement and conference that produced it in 1997 were criticized by Wallace Sampson, founder of the Scientific Review of Alternative Medicine, writing for an affiliated publication of Quackwatch who stated the meeting was chaired by a strong proponent of acupuncture and failed to include speakers who had obtained negative results on studies of acupuncture. Sampson also stated he believed the report showed evidence of pseudoscientific reasoning.
The 2003 World Health Organization's (WHO) report was controversial; critics assailed it as being problematic since, in spite of the disclaimer, supporters used it to claim that the WHO endorsed acupuncture that were lacking sufficient evidence-basis. Medical scientists expressed concern that the evidence supporting acupuncture outlined in the report was weak, and Willem Betz of SKEPP (Studie Kring voor Kritische Evaluatie van Pseudowetenschap en het Paranormale, the Study Circle for the Critical Evaluation of Pseudoscience and the Paranormal) said that the report was evidence that the "WHO has been infiltrated by missionaries for alternative medicine". The WHO 2003 report was also criticized in the 2008 book Trick or Treatment for, in addition to being produced by a panel that included no critics of acupuncture, containing two major errors – including too many results from low-quality clinical trials, and including a large number of trials originating in China where, probably due to publication bias, no negative trials have ever been produced. Ernst and Singh, the authors of the book, described the report as "highly misleading" and a "shoddy piece of work that was never rigorously scrutinized" and stated that the results of high-quality clinical trials do not support the use of acupuncture to treat anything but pain and nausea. Ernst also described the statement in a 2006 peer reviewed article as "erhaps the most obviously over-optimistic overview ", noting that of the 35 conditions that the WHO stated acupuncture was effective for, 27 of the systematic reviews that the WHO report was based on found that acupuncture was not effective for treating the specified condition.
Placebos have been used in medical care to treat the elderly. For example, a response to "sham" acupuncture in osteoarthritis may be used in the elderly. Placebos have usually been regarded as deception and thus unethical. However, some physicians and ethicists have suggested circumstances for applicable uses for placebos such as it might present a theoretical advantage of an inexpensive treatment without adverse reactions or interactions with drugs or other medications.
Acupuncture is a commonly used alternative medicine modality. Many physicians in the UK appear to recommend alternative medicine, which raises ethical issues. Physicians have a duty of care requiring that each patient be treated with the best treatment for a given condition and situation. As the evidence for most types of alternative medicine is far from strong, the use of alternative medicine in regular healthcare can present an ethical question. A large proportion of physicians in the UK appear to employ some type of alternative medicine, but many have not received the relevant training, which raises issues associated with medical ethics and professional competence.
In 2010, Brian Berman published a paper in the New England Journal of Medicine which recommended the use of acupuncture for lower back pain. According to David Gorski, "What Berman is doing in this article in the NEJM is the same thing that CAM advocates in general and acupuncture apologists in particular have a maddening tendency to do. They either cherry pick studies that appear to indicate that their favored woo works. When, as Berman et al were, they are forced to admit that well-designed studies with lots of patients show that their woo is no better than a valid placebo control, they then shift to embracing the placebo, to owning it, so to speak, all without actually calling it placebo".
Acupuncture is perceptibly used at academic medical centers despite little or no convincing scientific evidence for explicit effects for any condition that is discernible from placebo. The evidence that the majority of CAM modalities, such as acupuncture, are little more than 'theatrical placebos' is so compelling that some proponents of acupuncture have essentially conceded this position by advocating the 'harnessing of placebo effects' or developing 'meaningful placebos'.
Reception
Acupuncture has become popular in the US, China, and other parts of the world. It is viewed as a form of alternative medicine that aims to treat a range of conditions. Acupuncture is most commonly used for pain relief. There is limited evidence that acupuncture is rarely used alone but rather as an adjunct to other treatment modalities.
Australia
In Australia, a 2005 national survey revealed that nearly 1 in 10 adults have used acupuncture in the previous year.
China
Acupuncture is most popular in China.
Finland
Acupuncture is among popular CAM treatments in all five Nordic countries but it is used less in Finland.
Germany
According to several public health insurance organizations, women comprise over two-thirds of all acupuncture users in Germany. After the results of the German Acupuncture Trials were published in 2007, the number of regular users of acupuncture jumped by 20%, surpassing one million in 2011.
Japan
Utilization of acupuncture in Japan is estimated at around 6% annually, with around 25% of the population experiencing acupuncture at some point in life. The majority of patients who seek out acupuncture do so for musculoskeletal problems, including lower back pain, shoulder stiffness, and knee pain. Practice is governed by a national licensing program and protected by law. Use is generally not covered by public health insurance, and skews towards the elderly and people with a lower education level. Approximately half of users surveyed indicated a likelihood to seek such remedies in the future, while 37% did not.
Switzerland
In Switzerland, acupuncture has become the most frequently used alternative medicine since 2004.
United Kingdom
In the UK, the National Health Service (NHS) advises that acupuncture is only recommended as a treatment option for chronic lower back pain, chronic tension-type headaches and migraines.
In the United Kingdom, a total of 4 million acupuncture treatments were administered in 2009.
United States
In the U.S., less than one percent of the total population reported having used acupuncture in the early 1990s. In 2002, the National Center for Complementary and Alternative Medicine revealed that 2.1 million adults have used acupuncture in the previous 12 months. By the early 2010s, over 14 million Americans reported having used acupuncture as part of their health care. Each year, around 10 million acupuncture treatments are administered in the US. Acupuncture is used at many academic medical centers, including Duke Center for Integrative Medicine, the Johns Hopkins School of Medicine, Mayo Clinic, Stanford University School of Medicine, David Geffen School of Medicine at UCLA, Harvard Medical School, and Yale School of Medicine. "Probably the most common form of pseudoscience to wend its way into what should be bastions of scientific medicine is acupuncture," David Gorski explained in 2010. "Acupuncture and reiki remain widely practised and even embraced at academic institutions, and even homeopathy continued to be practised despite clinical trials that demonstrate effects indistinguishable from placebo effects," David Gorski and Steven Novella wrote in the 2014 journal Trends in Molecular Medicine.
Legal and political status
Main article: Regulation of acupunctureAustralia
In 2000, the Chinese Medicine Registration Board of Victoria, Australia (CMBV) established an independent government agency to oversee the practice of Chinese Herbal Medicine and Acupuncture in the state. Acupuncturists in New South Wales are bound by the guidelines in the Public Health (Skin Penetration) Regulation 2000.
Canada
Acupuncture is regulated in five provinces in Canada: Alberta, British Columbia, Ontario, Quebec, and Newfoundland.
Finland
Since acupuncture is deregulated in Finland many people without education in healthcare are able to give acupuncture treatment.
France
Since 1955, the French advisory body Académie Nationale de Médecine (National Academy of Medicine) has accepted acupuncture as a treatment.
Germany
The German acupuncture trials were a series of nationwide acupuncture trials set up in 2001 and published in 2006 on behalf of several German statutory health insurance companies due to a dispute as to the usefulness of acupuncture. The trials were considered to be one of the largest clinical studies in the field of acupuncture. As a result of the trials, acupuncture was paid for in Germany by the social insurance scheme for low back pain and osteoarthritis of the knee. but coverage was not offered for headache or migraine. However, because of the outcome of these trials, in the case of the other conditions, insurance corporations in Germany were not convinced that acupuncture had adequate benefits over usual care or sham treatments. Highlighting the results of the placebo group, researchers refused to accept a placebo therapy as efficient.
New Zealand
Traditional/lay acupuncture is not a regulated health profession. Osteopaths have a scope of practice for Western Medical Acupuncture and Related Needling Techniques.
United Kingdom
Acupuncturists are not a nationally regulated profession in the United Kingdom. Acupuncture practice is regulated by law in England and Wales for health and safety criteria under The Local Government (Miscellaneous Provisions).
United States
In 1996, the Food and Drug Administration reclassified acupuncture needles as a Class II medical device, allowing their use by qualified practitioners. All states permit acupuncture to be administered; some by physicians only and some by acupuncturists under medical supervision, and some with no supervision.
Veterinary acupuncture
| This section may lend undue weight to certain ideas, incidents, or controversies. Please help to create a more balanced presentation. Discuss and resolve this issue before removing this message. (April 2015) |
A 2006 review concluded "There is no compelling evidence to recommend or reject acupuncture for any condition in domestic animals" (although some species were discluded from the review). It went on further to conclude that some encouraging data do exist. More recently (2014), it has been stated that acupuncture offers a compelling and safe method for pain management analgesia which is growing rapidly in popularity with both veterinarians and pet owners. While acupuncture has become well accepted in veterinary medicine because it is minimally invasive, research results for pain and other conditions have varied, and there continue to challenges with establishing experimental controls. Rigorous evidence for complementary and alternative techniques lacking is lacking in veterninary medicine; although evidence, particularly for acupuncture, is increasing and is likely to continue to expand. Acupuncture for chronic pain in horses is "occasionally superior to standard interventions, is similar to sham acupuncture treatments, and varies in differences from placebo groups."
Recent (i.e. post-2011) reviews in both veterinary text books and scientific journals indicate that acupuncture can be used for therapeutic or homeostatic effects in animals, especially in the three areas of pain management, geriatric medicine and sports medicine.
In 2015, the American Animal Hospital Association (AAHA) and American Association of Feline Practitioners (AAFP) issued joint guidelines for the management of pain in cats and dogs. The guidelines stated "There is a solid and still growing body of evidence for the use of acupuncture for the treatment of pain in veterinary medicine to the extent that it is now an accepted treatment modality for painful animals."
See also
- Chinese herbology
- Colorpuncture
- List of ineffective cancer treatments
- Perkinism
- Pressure point
- Susuk
Bibliography
- Aung, SKH; Chen WPD (2007). Clinical Introduction to Medical Acupuncture. Thieme Medical Publishers. ISBN 9781588902214.
- Barnes, LL (2005). Needles, Herbs, Gods, and Ghosts: China, Healing, and the West to 1848. Harvard University Press. ISBN 0674018729.
- Cheng, X (1987). Chinese Acupuncture and Moxibustion (1st ed.). Foreign Languages Press. ISBN 711900378X.
- Cheng, X (2010). Chinese Acupuncture and Moxibustion (3rd ed.). Foreign Languages Press. ISBN 9787119059945. OCLC 624373192.
- Needham, J; Lu GD (2002). Celestial Lancets: A History and Rationale of Acupuncture and Moxa. Routledge. ISBN 0700714588.
- Singh, S; Ernst, E (2008). Trick or Treatment: Alternative Medicine on Trial. London: Bantam. ISBN 9780593061299.
- Stux, G; Pomeranz B (1988). Basics of Acupuncture. Berlin: Springer-Verlag. ISBN 354053072X.
- Stux, G; Pomeranz B (2012). Basics of Acupuncture. Springer-Verlag. ISBN 9783642491139. OCLC 878966679.
- Wiseman, N; Ellis, A (1996). Fundamentals of Chinese medicine. Paradigm Publications. ISBN 9780912111445.
- Madsen, M. V.; Gøtzsche, P. C; Hróbjartsson, A. (2009). "Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups". BMJ. 338: a3115. doi:10.1136/bmj.a3115. PMC 2769056. PMID 19174438.
Notes
- Placebo or sham acupuncture is a form of acupuncture that uses non-penetrating needles or needling at non-acupuncture points.
- ^ Singh & Ernst (2008) stated, "Scientists are still unable to find a shred of evidence to support the existence of meridians or Ch'i", "The traditional principles of acupuncture are deeply flawed, as there is no evidence at all to demonstrate the existence of Ch'i or meridians" and "Acupuncture points and meridians are not a reality, but merely the product of an ancient Chinese philosophy"
References
- Pyne, D.; Shenker, N. G. (2008). "Demystifying acupuncture". Rheumatology. 47 (8): 1132–1136. doi:10.1093/rheumatology/ken161. ISSN 1462-0324. PMID 18460551.
- ^ Adams, D; Cheng, F; Jou, H; Aung, S; Yasui, Y; Vohra, S (December 2011). "The safety of pediatric acupuncture: a systematic review". Pediatrics. 128 (6): e1575–e1587. doi:10.1542/peds.2011-1091. PMID 22106073.
- ^ Ernst, E. (2006). "Acupuncture--a critical analysis". Journal of Internal Medicine. 259 (2): 125–137. doi:10.1111/j.1365-2796.2005.01584.x. ISSN 0954-6820. PMID 16420542.
- ^ Xu, Shifen; et al. (2013). "Adverse Events of Acupuncture: A Systematic Review of Case Reports". Evidence Based Complementary and Alternative Medicine. 2013: 581203. doi:10.1155/2013/581203. PMC 3616356. PMID 23573135.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Berman, Brian; Langevin, Helene; Witt, Claudia; Dubner, Ronald (29 July 2010). "Acupuncture for Chronic Low Back Pain". New England Journal of Medicine. 363 (5): 454–461. doi:10.1056/NEJMct0806114. PMID 20818865.
- ^ Liu, Gang; Ma, Hui-juan; Hu, Pan-pan; Tian, Yang-hua; Hu, Shen; Fan, Jin; Wang, Kai (2013). "Effects of painful stimulation and acupuncture on attention networks in healthy subjects". Behavioral and Brain Functions. 9 (1): 23. doi:10.1186/1744-9081-9-23. ISSN 1744-9081. PMC 3680197. PMID 23758880.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Barrett, S (30 December 2007). "Be Wary of Acupuncture, Qigong, and "Chinese Medicine"". Quackwatch. Archived from the original on 29 September 2010. Retrieved 3 November 2010.
- Adams, David James (2013). Traditional Chinese Medicine: Scientific Basis for its Use. Royal Society of Chemistry. p. 2. ISBN 1849736618.
- ^ Baran GR, Kiana MF, Samuel SP (2014). Chapter 2: Science, Pseudoscience, and Not Science: How Do They Differ?. Springer. pp. 19–57. doi:10.1007/978-1-4614-8541-4_2. ISBN 978-1-4614-8540-7.
various pseudosciences maintain their popularity in our society: acupuncture, astrology, homeopathy, etc.
{{cite book}}:|work=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Good R (2012). Khine MS (ed.). Chapter 5: Why the Study of Pseudoscience Should Be Included in Nature of Science Studies. Springer. p. 103. ISBN 978-94-007-2457-0.
Believing in something like chiropractic or acupuncture really can help relieve pain to a small degree but many related claims of medical cures by these pseudosciences are bogus.
{{cite book}}:|work=ignored (help) - ^ "Acupuncture". NHSChoices. Retrieved 2 May 2015.
- Chapter 8: Cocaine (PDF). pp. 105–118. Retrieved 2 May 2015.
- Chou, R; Huffman, LH; American Pain Society; American College of Physicians (2 October 2007). "Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline". Annals of internal medicine. 147 (7): 492–504. doi:10.7326/0003-4819-147-7-200710020-00006. PMID 17909210.
- ^ Deng, Gary E.; Rausch, Sarah M.; Jones, Lee W.; Gulati, Amitabh; Kumar, Nagi B.; Greenlee, Heather; Pietanza, M. Catherine; Cassileth, Barrie R. (1 May 2013). "Complementary Therapies and Integrative Medicine in Lung Cancer". Chest (journal). 143 (5_suppl): e420S. doi:10.1378/chest.12-2364.
In patients having nausea and vomiting from either chemotherapy or radiation therapy, acupuncture or related techniques is suggested as an adjunct treatment option
- Camilleri, M; Parkman, HP; Shafi, MA; Abell, TL; Gerson, L; American College of Gastroenterology (January 2013). "Clinical guideline: management of gastroparesis". The American Journal of Gastroenterology. 108 (1): 18–37. PMID 23147521.
Acupuncture can be considered as an alternative therapy. This has been associated with improved rates of gastric emptying and reduction of symptoms.
- Seidman, M. D.; Gurgel, R. K.; Lin, S. Y.; Schwartz, S. R.; Baroody, F. M.; Bonner, J. R.; Dawson, D. E.; Dykewicz, M. S.; Hackell, J. M.; Han, J. K.; Ishman, S. L.; Krouse, H. J.; Malekzadeh, S.; Mims, J. W.; Omole, F. S.; Reddy, W. D.; Wallace, D. V.; Walsh, S. A.; Warren, B. E.; Wilson, M. N.; Nnacheta, L. C. (2 February 2015). "Clinical Practice Guideline: Allergic Rhinitis Executive Summary". Otolaryngology-Head and Neck Surgery. 152 (2): 197–206. doi:10.1177/0194599814562166.
Clinicians may offer acupuncture, or refer to a clinician who can offer acupuncture, for patients with allergic rhinitis who are interested in nonpharmacologic therapy.
- Abdulla, A; Adams, N; Bone, M; Elliott, AM; Gaffin, J; Jones, D; Knaggs, R; Martin, D; Sampson, L; Schofield, P; British Geriatric Society (March 2013). "Guidance on the management of pain in older people". Age and Ageing. 42 Suppl 1: i1-57. doi:10.1093/ageing/afs200. PMID 23420266.
Consider the use of non-pharmacological strategies such as physiotherapy, cognitive behavioural approaches and acupuncture, in combination with medication
- Curd, Martin (2013). The Routledge Companion to Philosophy of Science. Routledge. p. 470. ISBN 1135011087.
- ^ Pigliucci, Massimo (2013). Philosophy of Pseudoscience: Reconsidering the Demarcation Problem. University of Chicago Press. p. 206.
- ^ Miller's Anesthesia. Elsevier. 2014. p. 1235. ISBN 0702052833.
When compared with placebo, acupuncture treatment has proven efficacy for relieving pain
- ^ Colquhoun, D; Novella S (2013). "Acupuncture is a theatrical placebo: the end of a myth" (PDF). Anesthesia & Analgesia. 116 (6): 1360–1363. doi:10.1213/ANE.0b013e31828f2d5e. PMID 23709076.
- ^ Lee, MS; Ernst, E (2011). "Acupuncture for pain: An overview of Cochrane reviews". Chinese Journal of Integrative Medicine. 17 (3): 187–189. doi:10.1007/s11655-011-0665-7. PMID 21359919.
- Madsen 2009, p. a3115
- ^ Ernst, E.; Lee, Myeong Soo; Choi, Tae-Young (2011). "Acupuncture: Does it alleviate pain and are there serious risks? A review of reviews" (PDF). Pain. 152 (4): 755–764. doi:10.1016/j.pain.2010.11.004. ISSN 0304-3959. PMID 21440191.
- ^ Ernst, E.; Pittler, MH; Wider, B; Boddy, K (2007). "Acupuncture: its evidence-base is changing". The American Journal of Chinese Medicine. 35 (1): 21–25. doi:10.1142/S0192415X07004588. PMID 17265547.
- ^ Johnson, M. I. (2006). "The clinical effectiveness of acupuncture for pain relief--you can be certain of uncertainty". Acupuncture in medicine : journal of the British Medical Acupuncture Society. 24 (2): 71–79. doi:10.1136/aim.24.2.71. PMID 16783282.
- ^ Wang, Shu-Ming; Kain, Zeev N.; White, Paul F. (2008). "Acupuncture Analgesia: II. Clinical Considerations". Anesthesia & Analgesia. 106 (2): 611–621. doi:10.1213/ane.0b013e318160644d. ISSN 0003-2999. PMID 18227323.
- ^ Madsen, M. V.; Gøtzsche, P. C; Hróbjartsson, A. (2009). "Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups". BMJ. 338: a3115. doi:10.1136/bmj.a3115. PMC 2769056. PMID 19174438.
- ^ "Acupuncture (PDQ®)". National Cancer Institute. Retrieved 15 September 2013.
- ^ Taylor P, Pezzullo L, Grant SJ, Bensoussan A. (2013). "Cost-effectiveness of Acupuncture for Chronic Nonspecific Low Back Pain". Pain Practice: The Official Journal of World Institute of Pain. 14 (7): 599–606. doi:10.1111/papr.12116. PMID 24138020.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Standaert CJ, Friedly J, Erwin MW, Lee MJ, Rechtine G, Henrikson NB, Norvell DC (2011). "Comparative effectiveness of exercise, acupuncture, and spinal manipulation for low back pain". Spine. 1 (36): 21 (Suppl):S120–30. doi:10.1097/BRS.0b013e31822ef878. PMID 21952184.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Singh & Ernst 2008, p. 72
- Singh & Ernst 2008, p. 107
- Singh & Ernst 2008, p. 387
- ^ Bauer, M (2006). "The Final Days of Traditional Beliefs? – Part One". Chinese Medicine Times. 1 (4): 31.
- ^ Ahn, Andrew C.; Colbert, Agatha P.; Anderson, Belinda J.; Martinsen, ØRjan G.; Hammerschlag, Richard; Cina, Steve; Wayne, Peter M.; Langevin, Helene M. (2008). "Electrical properties of acupuncture points and meridians: A systematic review" (PDF). Bioelectromagnetics. 29 (4): 245–256. doi:10.1002/bem.20403. PMID 18240287.
- ^ Mann, F (2000). Reinventing Acupuncture: A New Concept of Ancient Medicine. Elsevier. ISBN 0750648570.
- ^ de las Peñas, César Fernández; Arendt-Nielsen, Lars; Gerwin, Robert D (2010). Tension-type and cervicogenic headache: pathophysiology, diagnosis, and management. Jones & Bartlett Learning. pp. 251–254. ISBN 9780763752835.
- ^ Williams, WF (2013). Encyclopedia of Pseudoscience: From Alien Abductions to Zone Therapy. Routledge. pp. 3–4. ISBN 1135955220.
{{cite book}}:|work=ignored (help) - ^ Ulett, GA (2002). "Acupuncture". In Shermer, M (ed.). The Skeptic: Encyclopedia of Pseudoscience. ABC-CLIO. p. 283291. ISBN 1576076539.
- ^ Zhang J, Shang H, Gao X, Ernst E (December 2010). "Acupuncture-related adverse events: a systematic review of the Chinese literature". Bull World Health Organ. 88 (12): 915–921C. doi:10.2471/BLT.10.076737. PMC 2995190. PMID 21124716.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ White, A.; Ernst, E. (2004). "A brief history of acupuncture". Rheumatology (Oxford, England). 43 (5): 662–663. doi:10.1093/rheumatology/keg005. PMID 15103027.
- ^ "Classics of Traditional Medicine". United States National Library of Medicine. 2012.
- ^ Robson, T (2004). An Introduction to Complementary Medicine. Allen & Unwin. pp. 90. ISBN 1741140544.
- Schwartz, L (2000). "Evidence-Based Medicine And Traditional Chinese Medicine: Not Mutually Exclusive". Medical Acupuncture. 12 (1): 38–41.
- ^ "What you can expect". Mayo Clinic Staff. Mayo Foundation for Medical Education and Research. January 2012.
- ^ Young, J (2007). Complementary Medicine For Dummies. John Wiley & Sons. pp. 126–128. ISBN 0470519681.
- Napadow, Vitaly; Kaptchuk, Ted J. (June 2004). "Patient Characteristics for Outpatient Acupuncture in Beijing, China". The Journal of Alternative and Complementary Medicine. 10 (3): 565–572. doi:10.1089/1075553041323849. ISSN 1075-5535. PMID 15253864.
- ^ Sherman KJ, Cherkin DC, Eisenberg DM, Erro J, Hrbek A, Deyo RA (2005). "The practice of acupuncture: who are the providers and what do they do?". Ann Fam Med. 3 (2): 151–158. doi:10.1370/afm.248. PMC 1466855. PMID 15798042.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wheway, Jayne; Agbabiaka, Taofikat B.; Ernst, Edzard (2012). "Patient safety incidents from acupuncture treatments: a review of reports to the National Patient Safety Agency". International Journal of Risk & Safety In Medicine. 24 (3): 163–169. doi:10.3233/JRS-2012-0569. PMID 22936058.
- ^ Angela Hicks (2005). The Acupuncture Handbook: How Acupuncture Works and How It Can Help You (1 ed.). Piatkus Books. p. 41. ISBN 978-0749924720.
- Collinge, William J. (1996). The American Holistic Health Association Complete guide to alternative medicine. New York: Warner Books. ISBN 0-446-67258-0.
- ^ Aung & Chen, 2007, p. 116.
- Ellis, A; Wiseman N; Boss K (1991). Fundamentals of Chinese Acupuncture. Paradigm Publications. pp. 2–3. ISBN 091211133X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Aung & Chen, 2007, p. 113–114.
- Loyeung, B. Y.; Cobbin, D. M. (2013). "Investigating the effects of three needling parameters (manipulation, retention time, and insertion site) on needling sensation and pain profiles: A study of eight deep needling interventions". Evidence-Based Complementary and Alternative Medicine. 2013: 136763. doi:10.1155/2013/136763. PMC 3789497. PMID 24159337.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Steven Aung; William Chen (10 January 2007). Clinical Introduction to Medical Acupuncture. Thieme. p. 116. ISBN 9781588902214. Retrieved 20 September 2012.
- Stephen Birch (2011). Japanese Pediatric Acupuncture. Thieme. ISBN 978-3131500618.
- Thomas Wernicke (2014). The Art of Non-Invasive Paediatric Acupuncture. Jessica Kingsley Publishers. ISBN 978-1848191600.
- Webster's New World Medical Dictionary. Houghton Mifflin Harcourt. 29 January 2009. p. 6. ISBN 0544188977.
- Lee, Eun Jin; Frazier, Susan K (2011). "The Efficacy of Acupressure for Symptom Management: A Systematic Review". Journal of Pain and Symptom Management. 42 (4): 589–603. doi:10.1016/j.jpainsymman.2011.01.007. PMC 3154967. PMID 21531533.
- Needham & Lu, 2002, pp 170–173.
- "British Cupping Society".
- Farlex (2012). "Tui na". Farlex.
- "Sonopuncture". Educational Opportunities in Integrative Medicine. The Hunter Press. 2008. p. 34. ISBN 9780977655243.
- Bhagat (2004). Alternative Therapies. pp. 164–165. ISBN 9788180612206.
- "Sonopuncture". American Cancer Society's Guide to complementary and alternative cancer methods. American Cancer Society. 2000. p. 158. ISBN 9780944235249.
- "Cancer Dictionary – Acupuncture point injection". National Cancer Institute. Archived from the original on 27 March 2011. Retrieved 4 April 2011.
- ^ Barrett, M.D., Stephen. "Auriculotherapy: A Skeptical Look". Acupuncture Watch.
- Braverman S (2004). "Medical Acupuncture Review: Safety, Efficacy, And Treatment Practices". Medical Acupuncture. 15 (3).
- Isaacs, Nora (13 December 2007). "Hold the Chemicals, Bring on the Needles". New York Times. Retrieved 23 November 2009.
- ^ White, A.R.; Filshie, J.; Cummings, T.M.; International Acupuncture Research Forum (2001). "Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding". Complementary Therapies in Medicine. 9 (4): 237–245. doi:10.1054/ctim.2001.0489. ISSN 0965-2299. PMID 12184353.
- Witt, Claudia M; Aickin, Mikel; Baca, Trini; Cherkin, Dan; Haan, Mary N; Hammerschlag, Richard; Hao, Jason; Kaplan, George A; Lao, Lixing; McKay, Terri; Pierce, Beverly; Riley, David; Ritenbaugh, Cheryl; Thorpe, Kevin; Tunis, Sean; Weissberg, Jed; Berman, Brian M (2012). "Effectiveness guidance document (EGD) for acupuncture research - a consensus document for conducting trials". BMC Complementary and Alternative Medicine. 12 (1): 148. doi:10.1186/1472-6882-12-148. ISSN 1472-6882. PMID 22953730.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Langevin, Helene M.; Wayne, Peter M.; MacPherson, Hugh; Schnyer, Rosa; Milley, Ryan M.; Napadow, Vitaly; Lao, Lixing; Park, Jongbae; Harris, Richard E.; Cohen, Misha; Sherman, Karen J.; Haramati, Aviad; Hammerschlag, Richard (2011). "Paradoxes in Acupuncture Research: Strategies for Moving Forward". Evidence-Based Complementary and Alternative Medicine. 2011: 1–11. doi:10.1155/2011/180805. ISSN 1741-427X. PMC 2957136. PMID 20976074.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Paterson, C.; Dieppe, P. (2005). "Characteristic and incidental (placebo) effects in complex interventions such as acupuncture". BMJ. 330 (7501): 1202–1205. doi:10.1136/bmj.330.7501.1202. PMC 558023. PMID 15905259.
- ^ Amezaga Urruela, Matxalen; Suarez-Almazor, Maria E. (2012). "Acupuncture in the Treatment of Rheumatic Diseases". Current Rheumatology Reports. 14 (6): 589–597. doi:10.1007/s11926-012-0295-x. ISSN 1523-3774. PMC 3691014. PMID 23055010.
- Lee A, Copas JB, Henmi M, Gin T, Chung RC (2006). "Publication bias affected the estimate of postoperative nausea in an acupoint stimulation systematic review". J Clin Epidemiol. 59 (9): 980–983. doi:10.1016/j.jclinepi.2006.02.003. PMID 16895822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Tang, JL; Zhan, SY; Ernst, E (1999). "Review of randomised controlled trials of traditional Chinese medicine". BMJ (Clinical research ed.). 319 (7203): 160–161. doi:10.1136/bmj.319.7203.160. PMC 28166. PMID 10406751.
- Vickers, A; Goyal, N; Harland, R; Rees, R (1998). "Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials". Controlled Clinical Trials. 19 (2): 159–166. doi:10.1016/S0197-2456(97)00150-5. PMID 9551280.
- ^ He, J; Du, L; Liu, G; Fu, J; He, X; Yu, J; Shang, L (2011). "Quality assessment of reporting of randomization, allocation concealment, and blinding in traditional Chinese medicine RCTs: A review of 3159 RCTs identified from 260 systematic reviews". Trials. 12 (1): 122. doi:10.1186/1745-6215-12-122. PMC 3114769. PMID 21569452.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Gorski, David H. (2014). "Integrative oncology: really the best of both worlds?". Nature Reviews Cancer. doi:10.1038/nrc3822. ISSN 1474-175X. PMID 25230880.
- ^ MacPherson, Hugh; Maschino, Alexandra C; Lewith, George; Foster, Nadine E; Witt, Claudia; Vickers, Andrew J; Acupuncture Trialists' Collaboration (2013). Eldabe, Sam (ed.). "Characteristics of Acupuncture Treatment Associated with Outcome: An Individual Patient Meta-Analysis of 17,922 Patients with Chronic Pain in Randomised Controlled Trials". PLoS ONE. 8 (10): e77438. doi:10.1371/journal.pone.0077438. PMC 3795671. PMID 24146995.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Koog, Yun Hyung; Lee, Jin Su; Wi, Hyungsun (2014). "Clinically meaningful nocebo effect occurs in acupuncture treatment: a systematic review". Journal of Clinical Epidemiology. 67 (8): 858–869. doi:10.1016/j.jclinepi.2014.02.021. ISSN 0895-4356. PMID 24780405.
- Vickers, AJ; Cronin, AM; Maschino, AC; Lewith, G; MacPherson, H; Foster, N; Sherman, N; Witt, K; Linde, C (2012). "Acupuncture for chronic pain: individual patient data meta-analysis". JAMA Internal Medicine. 12 (Suppl 1). for the Acupuncture Trialists' Collaboration: 1444–1453. doi:10.1001/archinternmed.2012.3654. PMC 3658605. PMID 22965186.
- Jha, Alok (10 September 2012). "Acupuncture useful, but overall of little benefit, study shows". The Guardian.
{{cite news}}: Italic or bold markup not allowed in:|newspaper=(help) - Colquhoun, David (17 September 2012). "Re: Risks of acupuncture range from stray needles to pneumothorax, finds study". BMJ.
- ^ Vickers, A. J.; Maschino, A. C.; Lewith, G.; MacPherson, H.; Sherman, K. J.; Witt, C. M. (2013). "Responses to the Acupuncture Trialists' Collaboration individual patient data meta-analysis". Acupuncture in Medicine. 31 (1): 98–100. doi:10.1136/acupmed-2013-010312. ISSN 0964-5284. PMID 23449559.
- ^ Hopton, Ann; MacPherson, Hugh (2010). "Acupuncture for Chronic Pain: Is Acupuncture More than an Effective Placebo? A Systematic Review of Pooled Data from Meta-analyses". Pain Practice. 10 (2): 94–102. doi:10.1111/j.1533-2500.2009.00337.x. ISSN 1530-7085. PMID 20070551.
- ^ Enck, Paul; Klosterhalfen, Sibylle; Zipfel, Stephan (2010). "Acupuncture, psyche and the placebo response". Autonomic Neuroscience. 157 (1–2): 68–73. doi:10.1016/j.autneu.2010.03.005. ISSN 1566-0702. PMID 20359961.
- Lee, Jun-Hwan; Choi, Tae-Young; Lee, Myeong Soo; Lee, Hyejung; Shin, Byung-Cheul; Lee, Hyangsook (February 2013). "Acupuncture for Acute Low Back Pain". The Clinical Journal of Pain. 29 (2): 172–185. doi:10.1097/AJP.0b013e31824909f9. PMID 23269281.
- Lam, Megan; Curry, Philip (November 2013). "Effectiveness of Acupuncture for Nonspecific Chronic Low Back Pain". Spine. 38 (24): 2124–2138. doi:10.1097/01.brs.0000435025.65564.b7. PMID 24026151.
- ^ Hutchinson, Amanda J P; Ball, Simon; Andrews, Jeremy C H; Jones, Gareth G (2012). "The effectiveness of acupuncture in treating chronic non-specific low back pain: a systematic review of the literature". Journal of Orthopaedic Surgery and Research. 7 (1): 36. doi:10.1186/1749-799X-7-36. ISSN 1749-799X. PMID 23111099.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Xu, Mai; Yan, Shi; Yin, Xu; Li, Xiuyang; Gao, Shuguang; Han, Rui; Wei, Licheng; Luo, Wei; Lei, Guanghua (January 2013). "Acupuncture for Chronic Low Back Pain in Long-Term Follow-Up: A Meta-Analysis of 13 Randomized Controlled Trials". The American Journal of Chinese Medicine. 41 (01): 1–19. doi:10.1142/S0192415X13500018. PMID 23336503.
- ^ Furlan, AD; et al. (2005). Furlan, AD (ed.). "Acupuncture and dry-needling for low back pain" (PDF). Cochrane Database of Systematic Reviews (1): CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876.
- Lee, Courtney; Crawford, Cindy; Wallerstedt, Dawn; York, Alexandra; Duncan, Alaine; Smith, Jennifer; Sprengel, Meredith; Welton, Richard; Jonas, Wayne (2012). "The effectiveness of acupuncture research across components of the trauma spectrum response (tsr): A systematic review of reviews". Systematic Reviews. 1 (1): 46. doi:10.1186/2046-4053-1-46. PMC 3534620. PMID 23067573.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Linde, K; Allais, G; Brinkhaus, B; Manheimer, E; Vickers, A; White, AR (2009). Linde, Klaus (ed.). "Acupuncture for migraine prophylaxis". Cochrane Database of Systematic Reviews (1): CD001218. doi:10.1002/14651858.CD001218.pub2. PMC 3099267. PMID 19160193. Cite error: The named reference "Linde2009" was defined multiple times with different content (see the help page).
- Linde, K; Allais, G; Brinkhaus, B; Manheimer, E; Vickers, A; White, AR (21 January 2009). "Acupuncture for tension-type headache". The Cochrane database of systematic reviews (1): CD007587. doi:10.1002/14651858.CD007587. PMC 3099266. PMID 19160338.
- Kmietowicz, Z. (2014). "Acupuncture does not improve chronic knee pain, study finds". BMJ. 349 (sep30 27): g5899. doi:10.1136/bmj.g5899. ISSN 1756-1833. PMID 25273362.
- Corbett, M.S.; Rice, S.J.C.; Madurasinghe, V.; Slack, R.; Fayter, D.A.; Harden, M.; Sutton, A.J.; MacPherson, H.; Woolacott, N.F. (2013). "Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis". Osteoarthritis and Cartilage. 21 (9): 1290–1298. doi:10.1016/j.joca.2013.05.007. ISSN 1063-4584. PMID 23973143.
- Manyanga, Taru; Froese, Maria; Zarychanski, Ryan; Abou-Setta, Ahmed; Friesen, Carol; Tennenhouse, Michael; Shay, Barbara L (2014). "Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis". BMC Complementary and Alternative Medicine. 14 (1): 312. doi:10.1186/1472-6882-14-312. PMID 25151529.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Manheimer, E; Cheng, K; Linde, K; Lao, L; Yoo, J; Wieland, S; Van Der Windt, DAWM; Berman, BM; Bouter, LM (2010). Manheimer, Eric (ed.). "Acupuncture for peripheral joint osteoarthritis (Review)" (PDF). Cochrane Database of Systematic Reviews (10): CD001977. doi:10.1002/14651858.CD001977.pub2. PMC 3169099. PMID 20091527.
- "Osteoarthritis. Care and management in adults". National Guideline Clearinghouse. Retrieved 6 February 2015.
- White, A.; Foster, N. E.; Cummings, M.; Barlas, P. (25 January 2007). "Acupuncture treatment for chronic knee pain: a systematic review". Rheumatology. 46 (3): 384–390. doi:10.1093/rheumatology/kel413. PMID 17215263.
- Gadau, Marcus; Yeung, Wing-Fai; Liu, Hua; Zaslawski, Chris; Tan, Yuan-Sheng; Wang, Fu-Chun; Bangrazi, Sergio; Chung, Ka-Fai; Bian, Zhao-Xiang; Zhang, Shi-Ping (2014). "Acupuncture and moxibustion for lateral elbow pain: a systematic review of randomized controlled trials". BMC Complementary and Alternative Medicine. 14 (1): 136. doi:10.1186/1472-6882-14-136. PMID 24726029.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Chang, WD; Lai, PT; Tsou, YA (2014). "Analgesic effect of manual acupuncture and laser acupuncture for lateral epicondylalgia: a systematic review and meta-analysis". The American journal of Chinese medicine. 42 (6): 1301–1314. doi:10.1142/S0192415X14500815. PMID 25384448.
- ^ Lee, M. S.; Ernst, E. (2014). "Acupuncture for surgical conditions: an overview of systematic reviews". International Journal of Clinical Practice. 68 (6): 783–789. doi:10.1111/ijcp.12372. ISSN 1368-5031. PMID 24447388.
- Cheong, Kah Bik; Zhang, Ji-ping; Huang, Yong; Zhang, Zhang-jin; Baradaran, Hamid Reza (13 December 2013). "The Effectiveness of Acupuncture in Prevention and Treatment of Postoperative Nausea and Vomiting - A Systematic Review and Meta-Analysis". PLoS ONE. 8 (12): e82474. doi:10.1371/journal.pone.0082474. PMID 24349293.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lee A, Fan, LTY (2009). Lee, Anna (ed.). "Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting". Cochrane Database Syst Rev (2): CD003281. doi:10.1002/14651858.CD003281.pub3. PMC 3113464. PMID 19370583.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cho, Young-Hun; Kim, Chang-Kyu; Heo, Kwang-Ho; Lee, Myeong Soo; Ha, In-Hyuk; Son, Dong Wuk; Choi, Byung Kwan; Song, Geun-Sung; Shin, Byung-Cheul (2014). "Acupuncture for Acute Postoperative Pain after Back Surgery: A Systematic Review and Meta-analysis of Randomized Controlled Trials". Pain Practice. 15 (3). doi:10.1111/papr.12208. ISSN 1530-7085. PMID 24766648.
- Cheong, Kah Bik; Zhang, Ji-ping; Huang, Yong (August 2014). "The effectiveness of acupuncture in postoperative gastroparesis syndrome – A systematic review and meta-analysis". Complementary Therapies in Medicine. 22 (4): 767–786. doi:10.1016/j.ctim.2014.05.002. PMID 25146082.
- McCracken, G; Houston, P; Lefebvre, G; Society of Obstetricians and Gynecologists of Canada (July 2008). "Guideline for the management of postoperative nausea and vomiting" (PDF). Journal of Obstetrics and Gynaecology Canada. 30 (7): 600–7, 608–16. PMID 18644183.
- ^ Feng, S; Han, M; Fan, Y; Liao, Z. "Acupuncture for the treatment of allergic rhinitis: A systematic review and meta-analysis". American Journal of Rhinologic Society. 29 (1): 57–62. doi:10.2500/ajra.2015.29.4116. PMID 25590322.
- ^ Pfab, Florian; Schalock, Peter C; Napadow, Vitaly; Athanasiadis, Georgios I; Huss-Marp, Johannes; Ring, Johannes (2014). "Acupuncture for allergic disease therapy – the current state of evidence". Expert Review of Clinical Immunology. 10 (7): 1–11. doi:10.1586/1744666X.2014.924855. ISSN 1744-666X. PMID 24881629.
- ^ Witt, C.M.; Brinkhaus, B. (2010). "Efficacy, effectiveness and cost-effectiveness of acupuncture for allergic rhinitis — An overview about previous and ongoing studies". Autonomic Neuroscience. 157 (1–2): 42–45. doi:10.1016/j.autneu.2010.06.006. ISSN 1566-0702. PMID 20609633.
- ^ Lee, Myeong Soo; Pittler, Max H.; Shin, Byung-Cheul; Kim, Jong-In; Ernst, Edzard (2009). "Acupuncture for allergic rhinitis: a systematic review". Annals of Allergy, Asthma & Immunology. 102 (4): 269–279. doi:10.1016/S1081-1206(10)60330-4. ISSN 1081-1206. PMID 19441597.
- Shah, Rachna; Greenberger, Paul A. (2012). "Chapter 29: Unproved and controversial methods and theories in allergy-immunology". Allergy and Asthma Proceedings. 33 (3): 100–102. doi:10.2500/aap.2012.33.3562. ISSN 1088-5412. PMID 22794702.
- Seidman, M. D.; Gurgel, R. K.; Lin, S. Y.; Schwartz, S. R.; Baroody, F. M.; Bonner, J. R.; Dawson, D. E.; Dykewicz, M. S.; Hackell, J. M.; Han, J. K.; Ishman, S. L.; Krouse, H. J.; Malekzadeh, S.; Mims, J. W.; Omole, F. S.; Reddy, W. D.; Wallace, D. V.; Walsh, S. A.; Warren, B. E.; Wilson, M. N.; Nnacheta, L. C. (2 February 2015). "Clinical Practice Guideline: Allergic Rhinitis Executive Summary". Otolaryngology -- Head and Neck Surgery. 152 (2): 197–206. doi:10.1177/0194599814562166. PMID 25645524.
- Seidman, M. D.; Gurgel, R. K.; Lin, S. Y.; Schwartz, S. R.; Baroody, F. M.; Bonner, J. R.; Dawson, D. E.; Dykewicz, M. S.; Hackell, J. M.; Han, J. K.; Ishman, S. L.; Krouse, H. J.; Malekzadeh, S.; Mims, J. W.; Omole, F. S.; Reddy, W. D.; Wallace, D. V.; Walsh, S. A.; Warren, B. E.; Wilson, M. N.; Nnacheta, L. C. (2 February 2015). "Clinical Practice Guideline: Allergic Rhinitis". Otolaryngology -- Head and Neck Surgery. 152 (1 Suppl): S1–S43. doi:10.1177/0194599814561600. PMID 25644617.
- Choi, T. Y.; Lee, M. S.; Kim, T. H.; Zaslawski, C; Ernst, E (2012). "Acupuncture for the treatment of cancer pain: A systematic review of randomised clinical trials". Supportive Care in Cancer. 20 (6): 1147–1158. doi:10.1007/s00520-012-1432-9. PMID 22447366.
- Paley, C. A.; Johnson, M. I.; Tashani, O. A.; Bagnall, A. M. (2011). "Acupuncture for cancer pain in adults". The Cochrane database of systematic reviews (1): CD007753. doi:10.1002/14651858.CD007753.pub2. PMID 21249694.
- Lian, WL; Pan, MQ; Zhou, DH; Zhang, ZJ (February 2014). "Effectiveness of acupuncture for palliative care in cancer patients: a systematic review". Chinese journal of integrative medicine. 20 (2): 136–147. doi:10.1007/s11655-013-1439-1. PMID 24338183.
- Towler, P; Molassiotis, A; Brearley, SG (October 2013). "What is the evidence for the use of acupuncture as an intervention for symptom management in cancer supportive and palliative care: an integrative overview of reviews". Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 21 (10): 2913–2923. doi:10.1007/s00520-013-1882-8. PMID 23868190.
- Garcia, M. K.; McQuade, J; Haddad, R; Patel, S; Lee, R; Yang, P; Palmer, J. L.; Cohen, L (2013). "Systematic review of acupuncture in cancer care: A synthesis of the evidence". Journal of Clinical Oncology. 31 (7): 952–960. doi:10.1200/JCO.2012.43.5818. PMC 3577953. PMID 23341529.
- Posadzki, P; Moon, T. W.; Choi, T. Y.; Park, T. Y.; Lee, M. S.; Ernst, E (2013). "Acupuncture for cancer-related fatigue: A systematic review of randomized clinical trials". Supportive Care in Cancer. 21 (7): 2067–2073. doi:10.1007/s00520-013-1765-z. PMID 23435597.
- Ling, Wai-man; Lui, Liza Y. Y.; So, Winnie K. W.; Chan, Kuen (1 November 2014). "Effects of Acupuncture and Acupressure on Cancer-Related Fatigue: A Systematic Review". Oncology Nursing Forum. 41 (6): 581–592. doi:10.1188/14.ONF.581-592. PMID 25355016.
- ^ Choi, T. Y.; Lee, M. S.; Ernst, E (2012). "Acupuncture for cancer patients suffering from hiccups: A systematic review and meta-analysis". Complementary Therapies in Medicine. 20 (6): 447–455. doi:10.1016/j.ctim.2012.07.007. PMID 23131378.
- Deng, Gary E.; Rausch, Sarah M.; Jones, Lee W.; Gulati, Amitabh; Kumar, Nagi B.; Greenlee, Heather; Pietanza, M. Catherine; Cassileth, Barrie R. (1 May 2013). "Complementary Therapies and Integrative Medicine in Lung Cancer". Chest (journal). 143 (5_suppl): e420S. doi:10.1378/chest.12-2364.
- Jerng, UiMin; Jo, Jun-Young; Lee, Seunghoon; Lee, Jin-Moo; Kwon, Ohmin (2014). "The effectiveness and safety of acupuncture for poor semen quality in infertile males: a systematic review and meta-analysis". Asian Journal of Andrology. 0 (5). doi:10.4103/1008-682X.129130. ISSN 1008-682X. PMID 25038176.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Cheong, YC; Dix, S; Hung Yu Ng, E; Ledger, WL; Farquhar, C (26 July 2013). "Acupuncture and assisted reproductive technology". The Cochrane database of systematic reviews. 7: CD006920. doi:10.1002/14651858.CD006920.pub3. PMID 23888428.
- Manheimer, E; Van Der Windt, D; Cheng, K; Stafford, K; Liu, J; Tierney, J; Lao, L; Berman, BM; Langenberg, P; Bouter, LM (2013). "The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: A systematic review and meta-analysis". Human reproduction update. 19 (6): 696–713. doi:10.1093/humupd/dmt026. PMC 3796945. PMID 23814102.
- Zheng, CH; Huang, GY; Zhang, MM; Wang, W (March 2012). "Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization: a systematic review and meta-analysis". Fertility and Sterility. 97 (3): 599–611. doi:10.1016/j.fertnstert.2011.12.007. PMID 22243605.
- Meldrum, David R.; Fisher, Andrew R.; Butts, Samantha F.; Su, H. Irene; Sammel, Mary D. (2013). "Acupuncture—help, harm, or placebo?". Fertility and Sterility. 99 (7): 1821–1824. doi:10.1016/j.fertnstert.2012.12.046. ISSN 0015-0282. PMID 23357452.
- Kang, Hyun-Sun; Jeong, Daun; Kim, Dong-Il; Lee, Myeong Soo (April 2011). "The use of acupuncture for managing gynaecologic conditions: An overview of systematic reviews". Maturitas. 68 (4): 346–354. doi:10.1016/j.maturitas.2011.02.001. PMID 21376483.
- Qu, F; Zhou, J; Ren, RX (May 2012). "Effects of acupuncture on the outcomes of in vitro fertilization: a systematic review and meta-analysis". Journal of alternative and complementary medicine (New York, N.Y.). 18 (5): 429–439. doi:10.1089/acm.2011.0158. PMID 22540969.
- Deare JC, Zheng Z, Xue CC, Liu JP, Shang J, Scott SW, Littlejohn G (2013). "Acupuncture for treating fibromyalgia". Cochrane Database Syst Rev. 31 (5): CD007070. doi:10.1002/14651858.CD007070.pub2. PMC 4105202. PMID 23728665.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Langhorst, J.; Klose, P.; Musial, F.; Irnich, D.; Hauser, W. (2010). "Efficacy of acupuncture in fibromyalgia syndrome--a systematic review with a meta-analysis of controlled clinical trials". Rheumatology. 49 (4): 778–788. doi:10.1093/rheumatology/kep439. ISSN 1462-0324. PMID 20100789.
- Casimiro, L; Barnsley, L; Brosseau, L; Milne, S; Robinson, VA; Tugwell, P; Wells, G; Casimiro, Lynn (2005). Casimiro, Lynn (ed.). "Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis". Cochrane Database of Systematic Reviews. 2005 (4): CD003788. doi:10.1002/14651858.CD003788.pub2. PMID 16235342. Archived from the original on 13 April 2008. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - Ernst, E.; Lee, M. S. (29 June 2010). "Acupuncture for rheumatic conditions: an overview of systematic reviews". Rheumatology. 49 (10): 1957–1961. doi:10.1093/rheumatology/keq180. PMID 20591833.
- Zhang JH, Wang D, Liu M (2014). "Overview of systematic reviews and meta-analyses of acupuncture for stroke". Neuroepidemiology (Systematic review). 42 (1): 50–58. doi:10.1159/000355435. PMID 24356063.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lee, JA; et al. (September 2012). "Acupuncture for shoulder pain after stroke: A systematic review". Journal of Alternative and Complementary Medicine 18(9):818-23. 18 (9): 213–218. doi:10.1089/acm.2011.0457. PMC 3429280. PMID 22924414.
- Kong, J. C.; Lee, M. S.; Shin, B.-C.; Song, Y.-S.; Ernst, E. (27 September 2010). "Acupuncture for functional recovery after stroke: a systematic review of sham-controlled randomized clinical trials". Canadian Medical Association Journal. 182 (16): 1723–1729. doi:10.1503/cmaj.091113. PMID 20876268.
- Xie, Yue; Wang, Liping; He, Jinghua; Wu, Taixiang; Xie, Yue (2008). "Acupuncture for dysphagia in acute stroke". Cochrane Database Syst Rev (3): CD006076. doi:10.1002/14651858.CD006076.pub2. PMID 18646136.
- Wu, Hong Mei; Tang, Jin-Ling; Lin, Xiao Ping; Lau, Joseph TF; Leung, Ping Chung; Woo, Jean; Li, Youping; Wu, Hong Mei (2006). "Acupuncture for stroke rehabilitation". Protocols (3): CD004131. doi:10.1002/14651858.CD004131.pub2. PMID 16856031.
- Zhang, Shihong; Liu, Ming; Asplund, Kjell; Li, Lin; Liu, Ming (2005). "Acupuncture for acute stroke". Protocols (2): CD003317. doi:10.1002/14651858.CD003317.pub2. PMID 15846657.
- Li, L; Zhang, H; Meng, SQ; Qian, HZ (2014). "An updated meta-analysis of the efficacy and safety of acupuncture treatment for cerebral infarction". PLOS ONE. 9 (12): e114057. doi:10.1371/journal.pone.0114057. PMID 25438041.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Park, SW; Yi, SH; Lee, JA; Hwang, PW; Yoo, HC; Kang, KS (September 2014). "Acupuncture for the treatment of spasticity after stroke: a meta-analysis of randomized controlled trials". Journal of alternative and complementary medicine (New York, N.Y.). 20 (9): 672–682. doi:10.1089/acm.2014.0097. PMID 25192034.
- Lim, Sung Min; Yoo, Junghee; Lee, Euiju; Kim, Hyun Jung; Shin, Seungwon; Han, Gajin; Ahn, Hyeong Sik (2015). "Acupuncture for Spasticity after Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Evidence-Based Complementary and Alternative Medicine. 2015: 1–12. doi:10.1155/2015/870398. PMID 25628750.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Cho, Seung-Hun; Whang, Wei-Wan (2009). "Acupuncture for Alcohol Dependence: A Systematic Review". Alcoholism: Clinical and Experimental Research. 33 (8): 1305–1313. doi:10.1111/j.1530-0277.2009.00959.x. ISSN 0145-6008. PMID 19413653.
- Yu, C; Ji, K; Cao, H; Wang, Y; Jin, HH; Zhang, Z; Yang, G (28 March 2015). "Effectiveness of acupuncture for angina pectoris: a systematic review of randomized controlled trials". BMC complementary and alternative medicine. 15 (1): 90. doi:10.1186/s12906-015-0586-7. PMID 25888363.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Kim, T.H.; Lee, M.S.; Kim, K.H.; Kang, J.W.; Choi, T.Y.; Ernst, E. (23 June 2014). "Acupuncture for treating acute ankle sprains in adults". Bone, Joint and Muscle Trauma Group. Cochrane Database of Systematic Reviews. 6 (6). John Wiley & Sons: Art. no. CD009065. doi:10.1002/14651858.CD009065.pub2. PMID 24953665.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help); Unknown parameter|nopp=ignored (|no-pp=suggested) (help); Unknown parameter|subscription=ignored (|url-access=suggested) (help) - Park, J; Hahn, S; Park, JY; Park, HJ; Lee, H (2013). "Acupuncture for ankle sprain: Systematic review and meta-analysis". BMC Complementary and Alternative Medicine. 13 (1): 55. doi:10.1186/1472-6882-13-55. PMC 3606608. PMID 23496981.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Li S, Yu B, Zhou D; et al. (2011). "Acupuncture for Attention Deficit Hyperactivity Disorder (ADHD) in children and adolescents". Cochrane Database Syst Rev (Systematic review) (4): CD007839. doi:10.1002/14651858.CD007839.pub2. PMID 21491402.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lee MS, Choi TY, Kim JI, Kim L, Ernst E (April 2011). "Acupuncture for treating attention deficit hyperactivity disorder: a systematic review and meta-analysis". Chin J Integr Med (Systematic review). 17 (4): 257–260. doi:10.1007/s11655-011-0701-7. PMID 21509667.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cheuk, D. K.; Wong, V.; Chen, W. X. (2011). Cheuk, Daniel KL (ed.). "Acupuncture for autism spectrum disorders (ASD)". Cochrane database of systematic reviews (Online). 9 (9): CD007849. doi:10.1002/14651858.CD007849.pub2. PMID 21901712.
- Lee, Myeong Soo; Choi, Tae-Young; Shin, Byung-Cheul; Ernst, Edzard (29 November 2011). "Acupuncture for Children with Autism Spectrum Disorders: A Systematic Review of Randomized Clinical Trials". Journal of Autism and Developmental Disorders. 42 (8): 1671–1683. doi:10.1007/s10803-011-1409-4. PMID 22124580.
- Mccarney, RW; Brinkhaus, B; Lasserson, TJ; Linde, K (2003). McCarney, Robert W (ed.). "Acupuncture for chronic asthma". Cochrane Database of Systematic Reviews. 2003 (3): CD000008. doi:10.1002/14651858.CD000008.pub2. PMID 14973944. Archived from the original on 19 April 2008. Retrieved 2 May 2008.
- Zhang, J; Li, X; Xu, J; Ernst, E (September 2012). "Laser acupuncture for the treatment of asthma in children: a systematic review of randomized controlled trials". The Journal of asthma : official journal of the Association for the Care of Asthma. 49 (7): 773–777. doi:10.3109/02770903.2012.691194. PMID 22873427.
- Chen, N; Zhou, M; He, L; Zhou, D; Li, N (2010). "Acupuncture for Bell's palsy". The Cochrane database of systematic reviews (8): CD002914. doi:10.1002/14651858.CD002914.pub5. PMID 20687071.
- Wong, Virginia; Cheuk, Daniel KL; Lee, Simon; Chu, Vanessa; Wong, Virginia (2013). "Acupuncture for acute management and rehabilitation of traumatic brain injury". Cochrane Database Syst Rev. 3: CD007700. doi:10.1002/14651858.CD007700.pub3. PMID 23543554.
- Sim, H.; Shin, B. C.; Lee, M. S.; Jung, A; Lee, H; Ernst, E (2011). "Acupuncture for carpal tunnel syndrome: A systematic review of randomized controlled trials". The Journal of Pain. 12 (3): 307–314. doi:10.1016/j.jpain.2010.08.006. PMID 21093382.
- Choi, T.-Y.; Jun, J. H.; Choi, J.-Y.; Kim, J.-I.; Lee, M. S.; Ernst, E. (2014). "Acupuncture for the treatment of chronic obstructive pulmonary disease: a protocol of a systematic review". BMJ Open. 4 (4): e004590. doi:10.1136/bmjopen-2013-004590. ISSN 2044-6055. PMID 24776710.
- Kim, Tae-Hun; Choi, Tae Yong; Lee, Myeong Soo; Ernst, Edzard (2011). "Acupuncture treatment for cardiac arrhythmias: A systematic review of randomized controlled trials". International Journal of Cardiology. 149 (2): 263–265. doi:10.1016/j.ijcard.2011.02.049. ISSN 0167-5273. PMID 21421272.
- Zheng, Guo-qing; Zhao, Zhi-Ming; Wang, Yan; Gu, Yong; Li, Yue; Chen, Xing-miao; Fu, Shu-Ping; Shen, Jiangang (April 2011). "Meta-Analysis of Scalp Acupuncture for Acute Hypertensive Intracerebral Hemorrhage". The Journal of Alternative and Complementary Medicine. 17 (4): 293–299. doi:10.1089/acm.2010.0156. PMID 21438797.
- Gates, S; Smith, LA; Foxcroft, DR; Gates, Simon (2006). Gates, Simon (ed.). "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews. 2006 (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523. Retrieved 2 May 2008.
- Zhang, T; Chon, TY; Liu, B; Do, A; Li, G; Bauer, B; Wang, L; Liu, Z (2013). "Efficacy of acupuncture for chronic constipation: a systematic review". The American journal of Chinese medicine. 41 (4): 717–742. doi:10.1142/S0192415X13500493. PMID 23895148.
- Smith, Caroline A; Hay, Phillipa PJ; MacPherson, Hugh; Smith, Caroline A (2010). "Acupuncture for depression". Cochrane Database Syst Rev (1): CD004046. doi:10.1002/14651858.CD004046.pub3. PMID 20091556.
- Ernst, E.; Lee, M. S.; Choi, T.-Y. (2010). "Acupuncture for Depression?: A Systematic Review of Systematic Reviews". Evaluation & the Health Professions. 34 (4): 403–412. doi:10.1177/0163278710386109. ISSN 0163-2787. PMID 21138913.
- Chen, W; Yang, GY; Liu, B; Manheimer, E; Liu, JP (2013). "Manual acupuncture for treatment of diabetic peripheral neuropathy: a systematic review of randomized controlled trials". PLOS ONE. 8 (9): e73764. doi:10.1371/journal.pone.0073764. PMID 24069229.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Jordan, J (2006). "Acupuncture treatment for opiate addiction: A systematic review". Journal of Substance Abuse Treatment. 30 (4): 309–314. doi:10.1016/j.jsat.2006.02.005. PMID 16716845.
- Gates, Simon; Smith, Lesley A; Foxcroft, David (2006). Gates, Simon (ed.). "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523.
- Lee, MS; Shin, BC; Choi, TY; Ernst, E (March 2011). "Acupuncture for treating dry eye: a systematic review". Acta ophthalmologica. 89 (2): 101–106. doi:10.1111/j.1755-3768.2009.01855.x. PMID 20337604.
- Smith, C. A.; Zhu, X; He, L; Song, J (2011). "Acupuncture for dysmenorrhoea". The Cochrane database of systematic reviews (1): CD007854. doi:10.1002/14651858.CD007854.pub2. PMID 21249697.
- Lan, L; Zeng, F; Liu, GJ; Ying, L; Wu, X; Liu, M; Liang, FR (13 October 2014). "Acupuncture for functional dyspepsia". The Cochrane database of systematic reviews. 10: CD008487. doi:10.1002/14651858.CD008487.pub2. PMID 25306866.
- Huang, T.; Shu, X.; Huang, Y. S.; Cheuk, D. K. (2011). Huang, Tao (ed.). "Complementary and miscellaneous interventions for nocturnal enuresis in children". Cochrane database of systematic reviews (Online). 12 (12): CD005230. doi:10.1002/14651858.CD005230.pub2. PMID 22161390.
- Zhu, Xiaoshu; Hamilton, Kindreth D; McNicol, Ewan D; Zhu, Xiaoshu (2011). "Acupuncture for pain in endometriosis". Cochrane Database Syst Rev (9): CD007864. doi:10.1002/14651858.CD007864.pub2. PMID 21901713.
- Cheuk, Daniel KL; Wong, Virginia; Cheuk, Daniel KL (2014). "Acupuncture for epilepsy". Cochrane Database Syst Rev. 5: CD005062. doi:10.1002/14651858.CD005062.pub4. PMID 24801225.
- Ernst, E.; Posadzki, P.; Lee, M. S. (2011). "Complementary and alternative medicine (CAM) for sexual dysfunction and erectile dysfunction in older men and women: An overview of systematic reviews". Maturitas. 70 (1): 37–41. doi:10.1016/j.maturitas.2011.06.011. PMID 21782365.
- Wang, Jie; Xiong, Xingjiang; Liu, Wei (2013). "Acupuncture for essential hypertension". International Journal of Cardiology. 169 (5): 317–326. doi:10.1016/j.ijcard.2013.09.001. ISSN 0167-5273. PMID 24060112.
- Law, Simon K; Li, Tianjing; Law, Simon K (2013). "Acupuncture for glaucoma". Cochrane Database Syst Rev. 5: CD006030. doi:10.1002/14651858.CD006030.pub3. PMID 23728656.
- Kang, H. S.; Jeong, D.; Kim, D. I.; Lee, M. S. (2011). "The use of acupuncture for managing gynaecologic conditions: An overview of systematic reviews". Maturitas. 68 (4): 346–354. doi:10.1016/j.maturitas.2011.02.001. PMID 21376483.
- Cho, S. H.; Whang, W. W. (2009). "Acupuncture for vasomotor menopausal symptoms". Menopause. 16 (5): 1065–1073. doi:10.1097/gme.0b013e3181a48abd. PMID 19424092.
- Dodin, Sylvie; Blanchet, Claudine; Marc, Isabelle; Ernst, Edzard; Wu, Taixiang; Vaillancourt, Caroline; Paquette, Joalee; Maunsell, Elizabeth; Dodin, Sylvie (2013). "Acupuncture for menopausal hot flushes". Cochrane Database Syst Rev. 7: CD007410. doi:10.1002/14651858.CD007410.pub2. PMID 23897589.
- Lee, Myeong Soo; Kim, Kun-Hyung; Shin, Byung-Cheul; Choi, Sun-Mi; Ernst, Edzard (2009). "Acupuncture for treating hot flushes in men with prostate cancer: a systematic review". Supportive Care in Cancer. 17 (7): 763–770. doi:10.1007/s00520-009-0589-3. ISSN 0941-4355. PMID 19224253.
- Wong, Virginia; Cheuk, Daniel KL; Chu, Vanessa; Wong, Virginia (2013). "Acupuncture for hypoxic ischemic encephalopathy in neonates". doi:10.1002/14651858.CD007968.pub2.
{{cite journal}}: Cite journal requires|journal=(help) - Cheuk, DK; Yeung, WF; Chung, KF; Wong, V; Cheuk, Daniel KL (2012). Cheuk, Daniel KL (ed.). "Acupuncture for insomnia". Cochrane Database of Systematic Reviews. 12 (9): CD005472. doi:10.1002/14651858.CD005472.pub3. PMID 22972087.
- Ernst, E.; Lee, M. S.; Choi, T. Y. (2011). "Acupuncture for insomnia? An overview of systematic reviews". European Journal of General Practice. 17 (2): 116–123. doi:10.3109/13814788.2011.568475. PMID 21463162.
- Smith, Caroline A; Crowther, Caroline A; Grant, Suzanne J; Smith, Caroline A (2013). "Acupuncture for induction of labour". Cochrane Database Syst Rev. 8: CD002962. doi:10.1002/14651858.CD002962.pub3. PMID 23945980.
- Manheimer, E; Cheng, K; Wieland, L. S.; Min, L. S.; Shen, X; Berman, B. M.; Lao, L (2012). "Acupuncture for treatment of irritable bowel syndrome". The Cochrane database of systematic reviews. 5: CD005111. doi:10.1002/14651858.CD005111.pub3. PMC 3718572. PMID 22592702.
- Manheimer, Eric; Wieland, L Susan; Cheng, Ke; Li, Shih Min; Shen, Xueyong; Berman, Brian M; Lao, Lixing (10 April 2012). "Acupuncture for Irritable Bowel Syndrome: Systematic Review and Meta-Analysis". The American Journal of Gastroenterology. 107 (6): 835–847. doi:10.1038/ajg.2012.66. PMID 22488079.
- Chao, GQ; Zhang, S (21 February 2014). "Effectiveness of acupuncture to treat irritable bowel syndrome: a meta-analysis". World journal of gastroenterology : WJG. 20 (7): 1871–1877. doi:10.3748/wjg.v20.i7.1871. PMID 24587665.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Santesso, Nancy (2014). "A Summary of a Cochrane Review: Acupuncture for Induction of Labor". Global Advances in Health and Medicine. 3 (4): 64–65. doi:10.7453/gahmj.2014.027. ISSN 2164-957X. PMID 25105081.
- Smith, C. A.; Collins, C. T.; Crowther, C. A.; Levett, K. M. (2011). "Acupuncture or acupressure for pain management in labour". The Cochrane database of systematic reviews (7): CD009232. doi:10.1002/14651858.CD009232. PMID 21735441.
- Cho, S-H; Lee, H; Ernst, E (July 2010). "Acupuncture for pain relief in labour: a systematic review and meta-analysis". BJOG: An International Journal of Obstetrics & Gynaecology. 117 (8): 907–920. doi:10.1111/j.1471-0528.2010.02570.x. PMID 20438555.
- Kim, KH; Kim, TH; Lee, BR; Kim, JK; Son, DW; Lee, SW; Yang, GY (October 2013). "Acupuncture for lumbar spinal stenosis: a systematic review and meta-analysis". Complementary therapies in medicine. 21 (5): 535–56. doi:10.1016/j.ctim.2013.08.007. PMID 24050593.
- Dennis, CL; Dowswell, T (31 July 2013). "Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression". The Cochrane database of systematic reviews. 7: CD006795. doi:10.1002/14651858.CD006795.pub3. PMID 23904069.
- Wei, M. L.; Liu, J. P.; Li, N.; Liu, M. (2011). Wei, Mao Ling (ed.). "Acupuncture for slowing the progression of myopia in children and adolescents". Cochrane database of systematic reviews (Online). 9 (9): CD007842. doi:10.1002/14651858.CD007842.pub2. PMID 21901710.
- Cho, SH; Lee, JS; Thabane, L; Lee, J (February 2009). "Acupuncture for obesity: a systematic review and meta-analysis". International journal of obesity (2005). 33 (2): 183–196. doi:10.1038/ijo.2008.269. PMID 19139756.
- Sui, Y.; Zhao, H. L.; Wong, V. C. W.; Brown, N.; Li, X. L.; Kwan, A. K. L.; Hui, H. L. W.; Ziea, E. T. C.; Chan, J. C. N. (May 2012). "A systematic review on use of Chinese medicine and acupuncture for treatment of obesity". Obesity Reviews. 13 (5): 409–430. doi:10.1111/j.1467-789X.2011.00979.x. PMID 22292480.
- Ernst, E; Lee, M. S.; Choi, T. Y. (2011). "Acupuncture in obstetrics and gynecology: An overview of systematic reviews". The American Journal of Chinese Medicine. 39 (3): 423–431. doi:10.1142/S0192415X11008920. PMID 21598411.
- Kim, Hee Jin; Jeon, Beom S. (2014). "Is acupuncture efficacious therapy in Parkinson's disease?". Journal of the Neurological Sciences. 341 (1–2): 1–7. doi:10.1016/j.jns.2014.04.016. ISSN 0022-510X. PMID 24798223.
- Lee, HS; Park, HL; Lee, SJ; Shin, BC; Choi, JY; Lee, MS (April 2013). "Scalp acupuncture for Parkinson's disease: a systematic review of randomized controlled trials". Chinese journal of integrative medicine. 19 (4): 297–306. doi:10.1007/s11655-013-1431-9. PMID 23546633.
- Lim, D.C.; Chen, W.; Cheng, L.N.; Xue, C.C.; Wong, F.W.; O'Sullivan, A.J.; Liu, J.P. (2011). Lim, Danforn CE (ed.). "Acupuncture for polycystic ovarian syndrome". Cochrane database of systematic reviews (Online) (8): CD007689. doi:10.1002/14651858.CD007689.pub2. PMID 21833961.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - Kim, SY; Park, HJ; Lee, H; Lee, H (July 2011). "Acupuncture for premenstrual syndrome: a systematic review and meta-analysis of randomised controlled trials". BJOG : an international journal of obstetrics and gynaecology. 118 (8): 899–915. doi:10.1111/j.1471-0528.2011.02994.x. PMID 21609380.
- Bae, H; Bae, H; Min, BI; Cho, S (2014). "Efficacy of acupuncture in reducing preoperative anxiety: a meta-analysis". Evidence-based complementary and alternative medicine: eCAM. 2014: 850367. doi:10.1155/2014/850367. PMID 25254059.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Boyuan, Zhang; Yang, Chen; Ke, Cheng; Xueyong, Shen; Sheng, Liu (2014). "Efficacy of Acupuncture for Psychological Symptoms Associated with Opioid Addiction: A Systematic Review and Meta-Analysis". Evidence-Based Complementary and Alternative Medicine. 2014: 1–13. doi:10.1155/2014/313549.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Cui, Ye; Wang, Yin; Liu, Zhishun; Cui, Ye (2008). "Acupuncture for restless legs syndrome". Cochrane Database Syst Rev (4): CD006457. doi:10.1002/14651858.CD006457.pub2. PMID 18843716.
- Shen, Xiaohong; Xia, Jun; Adams, Clive E; Shen, Xiaohong (2014). "Acupuncture for schizophrenia". Cochrane Database Syst Rev. 10: CD005475. doi:10.1002/14651858.CD005475.pub2. PMID 25330045.
- Zhang, XC; Xu, XP; Xu, WT; Hou, WZ; Cheng, YY; Li, CX; Ni, GX (2015). "Acupuncture Therapy for Sudden Sensorineural Hearing Loss: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". PloS one. 10 (4): e0125240. doi:10.1371/journal.pone.0125240. PMID 25919000.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - White AR, Rampes H, Liu JP, Stead LF, Campbell J (2014). "Acupuncture and related interventions for smoking cessation". Cochrane Database Syst Rev (Systematic review). 1: CD000009. doi:10.1002/14651858.CD000009.pub4. PMID 24459016.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wang, Yang; Zhishun, Liu; Peng, Weina; Zhao, Jie; Liu, Baoyan; Wang, Yang (2013). "Acupuncture for stress urinary incontinence in adults". Cochrane Database Syst Rev. 7: CD009408. doi:10.1002/14651858.CD009408.pub2. PMID 23818069.
- Zhang, SH; Liu, M; Asplund, K; Li, L; Liu, Ming (2005). Liu, Ming (ed.). "Acupuncture for acute stroke". Cochrane Database of Systematic Reviews. 2005 (2): CD003317. doi:10.1002/14651858.CD003317.pub2. PMID 15846657. Archived from the original on 29 April 2008. Retrieved 6 May 2008.
- Wu, HM; Tang, JL; Lin, XP; Lau, J; Leung, PC; Woo, J; Li, YP; Wu, Hong Mei (2006). Wu, Hong Mei (ed.). "Acupuncture for stroke rehabilitation". Cochrane Database of Systematic Reviews. 2006 (3): CD004131. doi:10.1002/14651858.CD004131.pub2. PMID 16856031. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - Laurence, B. (2012). "Acupuncture may be no more Effective than Sham Acupuncture in Treating Temporomandibular Joint Disorders". Journal of Evidence Based Dental Practice. 12 (1): 2–4. doi:10.1016/j.jebdp.2011.12.001. PMID 22326146.
- La Touche, Roy; Goddard, Greg; De-la-Hoz, José Luis; Wang, Kelun; Paris-Alemany, Alba; Angulo-Díaz-Parreño, Santiago; Mesa, Juan; Hernández, Mar (2010). "Acupuncture in the Treatment of Pain in Temporomandibular Disorders: A Systematic Review and Meta-analysis of Randomized Controlled Trials". The Clinical Journal of Pain. 26 (6): 541–550. doi:10.1097/AJP.0b013e3181e2697e. ISSN 0749-8047. PMID 20551730.
- Green, S; Buchbinder, R; Barnsley, L; Hall, S; White, M; Smidt, N; Assendelft, W; Green, Sally (2002). Green, Sally (ed.). "Acupuncture for lateral elbow pain". Cochrane Database of Systematic Reviews. 2002 (1): CD003527. doi:10.1002/14651858.CD003527. PMID 11869671. Retrieved 6 May 2008.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - Kim, J. I.; Choi, J. Y.; Lee, D. H.; Choi, T. Y.; Lee, M. S.; Ernst, E (2012). "Acupuncture for the treatment of tinnitus: A systematic review of randomized clinical trials". BMC Complementary and Alternative Medicine. 12 (1): 97. doi:10.1186/1472-6882-12-97. PMC 3493359. PMID 22805113.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - Liu, F; Han, X; Li, Y; Yu, S (25 October 2014). "Acupuncture in the treatment of tinnitus: a systematic review and meta-analysis". European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. doi:10.1007/s00405-014-3341-7. PMID 25344063.
- Kim, K. H.; Lee, M. S.; Choi, S. M. (2010). "Acupuncture for treating uremic pruritus in patients with end-stage renal disease: A systematic review". Journal of pain and symptom management. 40 (1): 117–125. doi:10.1016/j.jpainsymman.2009.11.325. PMID 21796811.
- Zhang, Yan; Peng, Weina; Clarke, Jane; Zhishun, Liu; Zhang, Yan (2010). "Acupuncture for uterine fibroids". Cochrane Database Syst Rev (1): CD007221. doi:10.1002/14651858.CD007221.pub2. PMID 20091625.
- Peng, WN; Zhao, H; Liu, ZS; Wang, S; Weina, Peng (2008). Weina, Peng (ed.). "Acupuncture for vascular dementia". Cochrane Database of Systematic Reviews. 2007 (2): CD004987. doi:10.1002/14651858.CD004987.pub2. PMID 17443563. Retrieved 6 May 2008.
- Moon, TW; Posadzki, P; Choi, TY; Park, TY; Kim, HJ; Lee, MS; Ernst, E (2014). "Acupuncture for treating whiplash associated disorder: a systematic review of randomised clinical trials". Evidence-based complementary and alternative medicine : eCAM. 2014: 870271. doi:10.1155/2014/870271. PMC 4034516. PMID 24899912.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Lee, MS; Kang, JW; Ernst, E (2010). "Does moxibustion work? An overview of systematic reviews". BMC research notes. 3 (1): 284. doi:10.1186/1756-0500-3-284. PMC 2987875. PMID 21054851.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Cao, H.; Li, X.; Liu, J. (2012). Malaga, German (ed.). "An Updated Review of the Efficacy of Cupping Therapy". PLoS ONE. 7 (2): e31793. doi:10.1371/journal.pone.0031793. PMC 3289625. PMID 22389674.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Gnatta JR, Kurebayashi LF, Paes da Silva MJ (2013). "Atypical mycobacterias associated to acupuncuture: an integrative review". Rev Lat Am Enfermagem. 21 (1): 450–458. doi:10.1590/s0104-11692013000100022. PMID 23546331.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bergqvist D (2013). "Vascular injuries caused by acupuncture. A systematic review". International Angiology. 32 (1): 1–8. PMID 23435388.
- ^ Ernst E, Zhang J (2011). "Cardiac tamponade caused by acupuncture: a review of the literature". Int J Cardiol. 16 (3): 287–289. doi:10.1016/j.ijcard.2010.10.016. PMID 21093944.
- ^ "Acupuncture Safety in Patients Receiving Anticoagulants: A Systematic Review". The Permanente Journal. 19 (1): 68–73. 2014. doi:10.7812/TPP/14-057. ISSN 1552-5767. PMID 25432001.
- Shin, H. K.; Jeong, S. J.; Lee, M. S.; Ernst, E (2013). "Adverse events attributed to traditional Korean medical practices: 1999-2010". Bulletin of the World Health Organization. 91 (8): 569–575. doi:10.2471/BLT.12.111609. PMC 3738306. PMID 23940404.
- Yamashita H, Tsukayama H (2008). "Safety of acupuncture practice in Japan: patient reactions, therapist negligence and error reduction strategies". Evid Based Complement Alternat Med. 5 (4): 391–398. doi:10.1093/ecam/nem086. PMC 2586322. PMID 18955234.
- ^ Park J1, Sohn Y, White AR, Lee H (February 2014). "The safety of acupuncture during pregnancy: a systematic review". Acupunct Med (Systematic review). 32 (3): 257–266. doi:10.1136/acupmed-2013-010480. PMC 4112450. PMID 24554789.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - Ambrósio, E.M.M.; Bloor, K.; MacPherson, H. (October 2012). "Costs and consequences of acupuncture as a treatment for chronic pain: A systematic review of economic evaluations conducted alongside randomised controlled trials". Complementary Therapies in Medicine. 20 (5): 364–374. doi:10.1016/j.ctim.2012.05.002. PMID 22863652.
- "Final Report, Report into Traditional Chinese Medicine" (PDF). Parliament of New South Wales. 9 November 2005. Retrieved 3 November 2010.
- "NCCAOM Code of Ethics" (PDF). National Certification Commission for Acupuncture and Oriental Medicine. Archived from the original (PDF) on 27 November 2010. Retrieved 3 November 2010.
- "Hard to swallow". Nature (journal). 448 (7150): 105–106. 2007. doi:10.1038/448106a. PMID 17625521.
- Wang, Shu-Ming (2013). "Acupuncture in 21st Century Anesthesia: Is There a Needle in the Haystack?" (PDF). Anesthesia & Analgesia. 116 (6): 1356–1359. doi:10.1213/ANE.0b013e31828f5efa. PMID 23709075.
- Steven Novella (25 January 2012). "What Is Traditional Chinese Medicine?". Science-based Medicine.
- Takahashi, Toku (2011). "Mechanism of Acupuncture on Neuromodulation in the Gut-A Review". Neuromodulation: Technology at the Neural Interface. 14 (1): 8–12. doi:10.1111/j.1525-1403.2010.00295.x. ISSN 1094-7159. PMID 21992155.
- ^ Aung & ChenSteven K. H. Aung; William Pai-Dei Chen (2007). Clinical Introduction to Medical Acupuncture. Thieme. pp. 11–12. ISBN 978-1-58890-221-4.
- ^ "氣的生理功能...(一)推動作用...(二)溫煦作用...(三)防御作用...(四)固攝作用...(五)氣化作用 as seen at 郭卜樂 (24 October 2009). 氣 (in Chinese). Archived from the original on 8 January 2009. Retrieved 2 December 2010.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ "(三)十二经脉 ...(四)奇经八脉 ..." as seen at 经络学 (in Chinese). Retrieved 22 February 2011.
{{cite web}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - Aung & Chen, 2007, pp 19–20.
- Singh & Ernst 2008, Chapter 2: The Truth About Acupuncture
- Needham & Lu, 2002, p. 23.
- ^ Aung & Chen, 2007, p. 101.
- ^ Needham & Lu, 2002, p. 15.
- Wiseman & Ellis 1996, p. 77
- Ergil, MC; Ergil, KV (2009). Pocket Atlas of Chinese Medicine. Stuttgart: Thieme. p. 19, 148. ISBN 9783131416117.
- Flaws, B; Finney D (2007). A handbook of TCM patterns & their treatments (6th ed.). Blue Poppy Press. pp. 1. ISBN 9780936185705.
- Flaws, B; Finney, D (1996). A handbook of TCM patterns & their treatments (6 (2007) ed.). Blue Poppy Press. pp. 169–173. ISBN 9780936185705.
- ^ Maciocia, G (1995). Tongue Diagnosis in Chinese Medicine. Eastland Press. ISBN 093961619X.
- Maciocia, G (2005). The Foundations of Chinese Medicine. Churchill Livingstone. ISBN 0443074895.
- Ross, J (1984). Zang Fu, the organ systems of traditional Chinese medicine. Elsevier. pp. 26. ISBN 9780443034824.
- anon (1980). Essentials of Chinese Acupuncture (1st ed.). Beijing: Foreign Languages Press. pp. 39–46.
- ^ Cheng, 1987, chapter 12.
- Eisenberg, David (1995). Encounters with Qi: exploring Chinese medicine. New York: Norton. p. 260. ISBN 0393312135.
- ^ Langevin, Helene M. (2014). "Acupuncture, Connective Tissue, and Peripheral Sensory Modulation". Critical Reviews in Eukaryotic Gene Expression. 24 (3): 249–253. doi:10.1615/CritRevEukaryotGeneExpr.2014008284. ISSN 1045-4403. PMID 25072149.
- Zhao, Zhi-Qi (2008). "Neural mechanism underlying acupuncture analgesia". Progress in Neurobiology. 85 (4): 355–375. doi:10.1016/j.pneurobio.2008.05.004. ISSN 0301-0082. PMID 18582529.
- ^ Wang, Shu-Ming; Kain, Zeev N.; White, Paul (2008). "Acupuncture Analgesia: I. The Scientific Basis". Anesthesia & Analgesia. 106 (2): 602–610. doi:10.1213/01.ane.0000277493.42335.7b. ISSN 0003-2999. PMID 18227322.
- Staud, R; Price, DD (May 2006). "Mechanisms of acupuncture analgesia for clinical and experimental pain". Expert Review of Neurotherapeutics. 6 (5): 661–667. doi:10.1586/14737175.6.5.661. PMID 16734514.
- Berman, Brian M.; Langevin, Helene M.; Witt, Claudia M.; Dubner, Ronald (29 July 2010). "Acupuncture for Chronic Low Back Pain". New England Journal of Medicine. 363 (5): 454–461. doi:10.1056/NEJMct0806114. PMID 20818865.
Acupuncture also has effects on local tissues, including mechanical stimulation of connective tissue, release of adenosine at the site of needle stimulation, and increases in local blood flow
- Sawynok J. Masino S, Boison D (ed.). Chapter 17: Adenosine and Pain. New York, NY: Springer. p. 352. doi:10.1007/978-1-4614-3903-5_17. ISBN 978-1-4614-3903-5.
in an elegant series of experiments, adenosine has been implicated as a mediator of acupuncture analgesia
{{cite book}}:|work=ignored (help) - Gorski, David H. (2014). "Integrative oncology: really the best of both worlds?". Nature Reviews Cancer. doi:10.1038/nrc3822. ISSN 1474-175X. PMID 25230880.
- Yang, Edward S.; Li, Pei-Wen; Nilius, Bernd; Li, Geng (26 August 2011). "Ancient Chinese medicine and mechanistic evidence of acupuncture physiology". European Journal of Physiology. 462 (5): 645–653. doi:10.1007/s00424-011-1017-3.
Anti-nociceptive effect of acupuncture requires A1 receptors
- Zylka, Mark J. (April 2011). "Pain-relieving prospects for adenosine receptors and ectonucleotidases". Trends in Molecular Medicine. 17 (4): 188–196. doi:10.1016/j.molmed.2010.12.006.
Antinociceptive effects of acupuncture require A1R activation
- Langevin, Helene (2014). "Acupuncture, Connective Tissue, and Peripheral Sensory Modulation". Critical Reviews in Eukaryotic Gene Expression. 24 (3): 249–53. doi:10.1615/CritRevEukaryotGeneExpr.2014008284. PMID 25072149.
- Zhang, Ruixin; Lao, Lixing; Ren, Ke; Berman, Brian M. (February 2014). "Mechanisms of Acupuncture–Electroacupuncture on Persistent Pain". Anesthesiology (journal). 120 (2): 482–503. doi:10.1097/ALN.0000000000000101. PMID 24322588.
- Takahashi, T (January 2011). "Mechanism of acupuncture on neuromodulation in the gut--a review". Neuromodulation : journal of the International Neuromodulation Society. 14 (1): 8–12, discussion 12. doi:10.1111/j.1525-1403.2010.00295.x. PMID 21992155.
- Kavoussi, B; Ross, BE (September 2007). "The neuroimmune basis of anti-inflammatory acupuncture". Integrative cancer therapies. 6 (3): 251–257. doi:10.1177/1534735407305892. PMID 17761638.
- Tiran, D; Mack S (2000). Complementary therapies for pregnancy and childbirth. Elsevier Health Sciences. pp. 79. ISBN 0702023280.
- e.g. White, A; Ernst E (1999). Acupuncture: a scientific appraisal. Elsevier Health Sciences. pp. 1. ISBN 0750641630.
- ^ Chiu, M (1993). Chinese acupuncture and moxibustion. Elsevier Health Sciences. p. 2. ISBN 0443042233.
- Ma, K.-W. (1992). "The roots and development of Chinese acupuncture: from prehistory to early 20th century" (PDF). Acupuncture in Medicine. 10: 92–99. doi:10.1136/aim.10.Suppl.92.
- Epler Jr, D. C. (1980). "Bloodletting in early Chinese medicine and its relation to the origin of acupuncture". Bulletin of the history of medicine. 54 (3): 337–367. PMID 6998524.
- Barnes, L. L. (1998). "The psychologizing of Chinese healing practices in the United States". Culture, medicine and psychiatry. 22 (4): 413–443. PMID 10063466.
- ^ Ramey, D; Buell D (2004). "A true history of acupuncture". Focus on Alternative and Complementary Therapies. 9 (4): 269–273. doi:10.1211/fact.2004.00244.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) - ^ Prioreschi, P (2004). A history of Medicine, Volume 2. Horatius Press. pp. 147–148. ISBN 1888456019.
- Fruehauf H (2010). "Chinese Medicine In Crisis: Science, Politics, And The Making Of "TCM"" (PDF). Retrieved 15 June 2011.
- Hicks, Angela; Hicks, John; Mole, Peter (2004). Five Element Constitutional Acupuncture (1st ed.). London: Churchill Livingstone. pp. ix. ISBN 0443071705.
- ^ Dorfer, L; Moser, M; Bahr, F; Spindler, K; Egarter-Vigl, E; Giullén, S; Dohr, G; Kenner, T (1999). "A medical report from the stone age?" (PDF). The Lancet. 354 (9183): 1023–1025. doi:10.1016/S0140-6736(98)12242-0. PMID 10501382.
- ^ Needham & Lu, 2002, p. 262.
- ^ Barnes, 2005, p. 25.
- Unschuld, P (1998). Chinese Medicine. Paradigm Publications. p. 94. ISBN 0912111550.based on Michel, Wolfgang (1993). "Frühe westliche Beobachtungen zur Akupunktur und Moxibustion ". Sudhoffs Archiv. Zeitschrift für Wissenschaftsgeschichte. 354: 194–222. doi:10.2307/20777697. ISSN 0039-4564.
- ^ Barnes, 2005, pp. 58–9.
- Michel, Wolfgang, Michel-Zaitsu, Wolfgang. "Collections | Kyushu University Library". Hdl.handle.net. Retrieved 16 June 2014.
{{cite web}}: CS1 maint: multiple names: authors list (link) - Barnes, 2005, p. 75.
- Michel, Wolfgang (2004). "Far Eastern Medicine in Seventeenth and Early Eighteenth Century Germany". Studies in Languages and Cultures. 20: 67–82. doi:10.2307/20777697. ISSN 0039-4564.
- Barnes, 2005, p. 188.
- ^ Barnes, 2005, pp. 308–9.
- ^ "Acupuncture (PDQ®)". National Cancer Institute. Retrieved 15 September 2013.
- ^ Crozier RC (1968). Traditional medicine in modern China: science, nationalism, and the tensions of cultural change (1 ed.). Cambridge: Harvard University Press. ISBN 978-0674901056.
- ^ Taylor, K (2005). Chinese Medicine in Early Communist China, 1945–63: a Medicine of Revolution. RoutledgeCurzon. p. 109. ISBN 041534512X.
- Li, Zhi-Sui (2011). The Private Life of Chairman Mao. Random House. pp. 84. ISBN 0307791394.
- ^ Beyerstein, BL; Sampson W (1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 1)". Skeptical Inquirer. 20 (4). Committee for Skeptical Inquiry.
- Davidson JP (1999). The complete idiot's guide to managing stress. Indianapolis, Ind: Alpha Books. pp. 255. ISBN 0028629558.
- Fan, AY (2012). "The first acupuncture center in the United States: an interview with Dr. Yao Wu Lee, Washington Acupuncture Center". Journal of Integrative Medicine. 20 (5). Committee for Journal of Chinese Integrative Medicine.
- Frum, David (2000). How We Got Here: The '70s. New York City: Basic Books. p. 133. ISBN 0465041957.
- Simon Singh (26 March 2006). "A groundbreaking experiment ... or a sensationalized TV stunt?". The Guardian.
- Simon Singh (14 February 2006). "Did we really witness the 'amazing power' of acupuncture?". Daily Telegraph.
- "Acupuncture and moxibustion of traditional Chinese medicine". UNESCO. Retrieved 25 May 2013.
- Sampson, W (23 March 2005). "Critique of the NIH Consensus Conference on Acupuncture". Quackwatch. Archived from the original on 6 June 2009. Retrieved 5 June 2009.
- ^ McCarthy, Michael (2005). "Critics slam draft WHO report on homoeopathy". The Lancet. 366 (9487): 705–706. doi:10.1016/S0140-6736(05)67159-0. PMID 16130229.
- ^ Singh & Ernst, 2008, p. 277-8.
- ^ Cherniack, E Paul (2010). "Would the elderly be better off if they were given more placebos?". Geriatrics & Gerontology International. 10 (2): 131–137. doi:10.1111/j.1447-0594.2009.00580.x. ISSN 1444-1586. PMID 20100289.
- Posadzki, P.; Alotaibi, A.; Ernst, E. (2012). "Prevalence of use of complementary and alternative medicine (CAM) by physicians in the UK: a systematic review of surveys". Clinical Medicine. 12 (6): 505–512. doi:10.7861/clinmedicine.12-6-505. ISSN 1470-2118. PMID 23342401.
- Berman, Brian M.; Langevin, Helene M.; Witt, Claudia M.; Dubner, Ronald (29 July 2010). "Acupuncture for Chronic Low Back Pain". New England Journal of Medicine. 363 (5): 454–461. doi:10.1056/NEJMct0806114.
- ^ David Gorski (3 August 2010). "Credulity about acupuncture infiltrates the New England Journal of Medicine". Science-based Medicine.
- "Acupuncture for Pain". NCCAM. Retrieved 9 May 2014.
- Xue, CC; Zhang, AL; Lin, V; Myers, R; Polus, B; Story, DF (2008). "Acupuncture, chiropractic and osteopathy use in Australia: A national population survey". BMC Public Health. 88 (1): 108. doi:10.1186/1471-2458-8-105. PMC 2322980. PMID 18377663. Retrieved 25 May 2013.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - Skovgaard, L.; Nicolajsen, P. H.; Pedersen, E.; Kant, M.; Fredrikson, S.; Verhoef, M.; Meyrowitsch, D. W. (2012). "Use of Complementary and Alternative Medicine among People with Multiple Sclerosis in the Nordic Countries". Autoimmune Diseases. 2012: 1–13. doi:10.1155/2012/841085. ISSN 2090-0422. PMID 23304461.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Frauen häufiger mit Akupunktur behandelt" (in German). Rheinische Post. Retrieved 25 May 2013.
{{cite web}}: Italic or bold markup not allowed in:|publisher=(help) - ^ Ishizaki, Naoto; Yano, Tadashi; Kawakita, Kenji (2010). "Public Status and Prevalence of Acupuncture in Japan". Evidence-Based Complementary and Alternative Medicine. 7 (4): 493–500. doi:10.1093/ecam/nen037. ISSN 1741-427X. PMID 18955345.
- Carruzzo, P; Graz, B; Rodondi, PY; Michaud, PA (6 September 2013). "Offer and use of complementary and alternative medicine in hospitals of the French-speaking part of Switzerland". Swiss Medical Weekly. 143: w13756. doi:10.4414/smw.2013.13756. PMID 24018633.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hopton, AK; Curnoe, S; Kanaan, M; MacPherson, H (2012). "Acupuncture in practice: Mapping the providers, the patients and the settings in a national cross-sectional survey". BMJ Open. 2 (1). bmj.com: e000456. doi:10.1136/bmjopen-2011-000456. PMC 3278493. PMID 22240649. Retrieved 25 May 2013.
- ^ David B. Samadi. "More Americans using acupuncture for common ailments". Fox News Channel. Retrieved 25 May 2013.
- Alderman, L (7 May 2010). "Acupuncture is popular, but you'll need to pay". The New York Times. Retrieved 25 May 2013.
- "Acupuncture". The Skeptic's Dictionary.
- Swingle, Anne Bennett (2005). "Acupuncture, Actually". Dome. Vol. 56, no. 8. The Johns Hopkins University. Retrieved 5 September 2014.
- Mudur, GS (20 August 2014). "US doctors spark homeopathy row". The Telegraph.
- "Welcome to the Chinese Medicine Registration Board of Victoria".
- "Public health (skin penetration) regulation" (PDF). Health board of New South Wales. 2000. Retrieved 25 May 2013.
- "CTCMA". College of Traditional Chinese Medicine Practitioners and Acupuncturists of British Columbia. Retrieved 25 May 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - "Traditional Chinese Medicine Act, 2006". S.O. 2006, c. 27.
- Birgitta Ojala. "Acupuncture in Finland". Åland Medical Acupuncture Association.
- Bossy, Jean (1988). "Acupuncture in France". Acupunct Med. 5: 6–8. doi:10.1136/aim.5.1.6.
- ^ Hackenbroch, Veronika (25 October 2004). "Die eingebildete Heilung". Der Spiegel (in German).
{{cite news}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - Birch, S. (2007). "Reflections on the German Acupuncture studies" (PDF). Journal of Chinese Medicine (83): 12–17.
- ^ TJ Hinrichs, Linda L. Barnes (2013). TJ Hinrichs, Linda L. Barnes (ed.). Chinese Medicine and Healing: An Illustrated History (1 ed.). Belknap Press. p. 314. ISBN 0674047370.
- Stuart B. Porter (2013). Stuart B. Porter (ed.). Tidy's Physiotherapy (15 ed.). Churchill Livingstone. p. 408. ISBN 0702043443.
- "Scopes of Practice". osteopathiccouncil.org.nz.
- "The Statutory Regulation of the Acupuncture Profession" (PDF). Acupuncture Regulatory Working Group. September 2003.
{{cite journal}}: Cite journal requires|journal=(help) - Archived 2007-12-19 at the Wayback Machine
- Barrett, Stephen; Taub, Arthur (21 February 2005). "Chapter 18: Acupuncture: Nonsense with Needles". The Health Robbers: A Close Look at Quackery in America (1st ed.). Amherst, New York: Prometheus Books (published 30 September 1993). pp. 259–268.
{{cite book}}:|work=ignored (help) - Habacher, Gabriele; Pittler, Max H.; Ernst, Edzard (2006). "Effectiveness of Acupuncture in Veterinary Medicine: Systematic Review". Journal of Veterinary Internal Medicine. 20 (3): 480–488. doi:10.1111/j.1939-1676.2006.tb02885.x. ISSN 0891-6640. PMID 16734078.
- ^ Fry, L.M., Neary, S.M., Sharrock, J. and Rychel, J.K. (2014). "Acupuncture for analgesia in veterinary medicine". Topics in Companion Animal Medicine. 29 (2): 35–42. PMID 25454374.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Alvarez, L. (2015). "Chapter 18: Acupuncture". Handbook of Veterinary Pain Management (3rd edition). Elsevier. ISBN 978-0323089357.
Rigorous evidence-based medicine continues to be insufficient and often inadequate in the veterinary field of complementary and alternative medicine; however, evidence is mounting, especially in the area of acupuncture, and should continue to expand.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - von Schweinitz, D.G. (2015). "Chapter 17: Acupuncture for pain control". In Sprayberry, K.A. Robinson, N.E. (ed.). Robinson's Current Therapy In Equine Medicine (7 ed.). Elsevier. pp. 69–75. ISBN 978-1455745555.
{{cite book}}: CS1 maint: multiple names: editors list (link) - Karen M. Tobias and Spencer A. Johnston., ed. (2012). Veterinary Surgery: Small Animal. Elsevier.
- William W. Muir III, John A.E. Hubbell, Richard Bednarski and Philip Lerche., ed. (2013). "Chapter 19: Integrative medicine: Acupuncture analgesia". Handbook of Veterinary Anesthesia (5 ed.). Elsevier.
{{cite book}}: CS1 maint: multiple names: editors list (link) - Ortel, S., Goldberg, M.E., Conarton, L., Koudhttps://en.wikipedia.org/search/?title=Acupuncture&action=edit§ion=8#elka, K. and Downing. R. (2015). "Chapter 17: The veterinary technician in althernative therapies". In Mary Ellen Goldberg (ed.). Pain Management for Veterinary Technicians and Nurses. John Wiley and Sons: Ames, Iowa. p. 317.
{{cite book}}: External link in|author= - Skarda R.T. and Glowaski, M. "Chapter 24: Acupuncture". In Tranquilli, W.J., Thurmon, J.C and Grimm, K.A. (ed.). Lumb and Jones' Veterinary Anesthesia and Analgesia (4 ed.). Blackwell Publishing.
{{cite book}}: CS1 maint: multiple names: editors list (link) - Xie H. and Wedemeyer, L. (2012). "Reviews: The validity of acupuncture in veterinary medicine". American Journal of Traditional Chinese Veterinary Medicine. 7 (1): 35–44.
- Hulea, C.I. and Cristina, R.T. (2012). "Acupuncture as a therapeutic tool in health disorders in animals: A review". Scientific Papers: Animal Science and Biotechnologies. 45 (2): 166–177.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Araújo, A.M.S. (2014). "Acupuncture in equine reproductive disorders (Review)". PUBVET. 8 (18). ISSN 1982-1263.
- Parrah, J.D., Moulvi, B.A., Dedmari, F.H., Athar, H. and Kalim, M.O. (2012). "Acupuncture in veterinary medicine - a review". Veterinary Practitioner. 13 (2): 370–373. ISSN 0972-4036.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Corti, L. (2014). "Nonpharmaceutical approaches to pain management". Topics in Companion Animal Medicine. 29 (1): 24–28.
- AAHA/AAFP (2015). "2015 AAHA/AAFP pain management guidelines for dogs and cats". Journal of Feline Medicine and Surgery. 17: 251–272.
Further reading
- Deadman, P.; Baker, K; Al-Khafaji, M. (2007). A Manual of Acupuncture. Journal of Chinese Medicine Publications. ISBN 0951054651.
- Jin, G.; Jin, J.X.; Jin, L.L. (2006). Contemporary Medical Acupuncture – A Systems Approach. Springer. ISBN 7040192578.
- Ulett GA (2002). Shermer M (ed.). Acupuncture. ABC-CLIO. pp. 283 ff. ISBN 978-1-57607-653-8.
{{cite encyclopedia}}:|work=ignored (help) - William FW, ed. (2013). Acupuncture. Routledge. pp. 3–4. ISBN 978-1-135-95522-9.
{{cite encyclopedia}}:|work=ignored (help)
External links
 Media related to Acupuncture at Wikimedia Commons
Media related to Acupuncture at Wikimedia Commons- Template:Dmoz
| Acupuncture | |
|---|---|
| Concepts | |
| Types | |
| Alternative medicine | |
|---|---|
| Systems | |
| People |
|
| Treatments | |
| Public-health issues | |
| Key terms | |
| Contrary viewpoints | |
| Traditional Chinese medicine (TCM) | |||||
|---|---|---|---|---|---|
| Practices | |||||
| Concepts |
| ||||
| Zangfu Organs |
| ||||
| Noted physicians |
| ||||
| Contemporary related topics | |||||
