| Revision as of 17:20, 18 May 2007 edit192.246.233.55 (talk) →Medical opinions← Previous edit | Latest revision as of 11:52, 12 December 2024 edit undo2604:2000:2fc0:f:e123:5ff5:2949:5def (talk)No edit summary | ||
| (443 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Study of the different types of sensory perception of fetuses during pregnancy}} | |||
| {{Abortion}} | |||
| {{expert needed|biology|date=August 2009|reason=discrepancy between abortion subsection and rest of the article, and lacking scientific consensus in article overall}} | |||
| '''Fetal pain''', its existence, and its implications are debated politically and academically, particularly in regards to the ]. | |||
| '''Prenatal perception''' is the study of the extent of ] and other types of ] during ]. In practical terms, this means the study of ]es; none of the accepted indicators of perception are present in ]s. Studies of this type inform the ], along with certain related pieces of legislation in countries affected by that debate. As of 2022, there is not any ] on whether a fetus can feel pain.<ref>{{Cite news |last=Belluck |first=Pam |date=2013-09-17 |title=Complex Science at Issue in Politics of Fetal Pain |language=en-US |work=The New York Times |url=https://www.nytimes.com/2013/09/17/health/complex-science-at-issue-in-politics-of-fetal-pain.html |access-date=2022-09-20 |issn=0362-4331}}</ref><ref>{{Cite web |last=Levitan |first=Dave |date=2015-05-18 |title=Does a Fetus Feel Pain at 20 Weeks? |url=https://www.factcheck.org/2015/05/does-a-fetus-feel-pain-at-20-weeks/ |access-date=2022-09-20 |website=FactCheck.org |language=en-US}}</ref><ref>{{Cite news |last=Karni |first=Annie |date=2022-09-13 |title=Graham Proposes 15-Week Abortion Ban, Splitting Republicans |language=en-US |work=The New York Times |url=https://www.nytimes.com/2022/09/13/us/politics/lindsey-graham-abortion.html |access-date=2022-09-20 |issn=0362-4331}}</ref> | |||
| ==Prenatal hearing== | |||
| ==Overview== | |||
| Numerous studies have found evidence indicating a fetus's ability to respond to auditory stimuli. The earliest fetal response to a sound stimulus has been observed at 16 weeks' gestational age, while the auditory system is fully functional at 25–29 weeks' gestation.<ref>{{cite journal |last1=Graven |first1=Stanley N. |last2=Browne |first2=Joy V. |title=Auditory Development in the Fetus and Infant |journal=Newborn and Infant Nursing Reviews |date=December 2008 |volume=8 |issue=4 |pages=187–193 |doi=10.1053/j.nainr.2008.10.010 |s2cid=6361226 |url=https://www.sciencedirect.com/science/article/pii/S1527336908001347 |access-date=31 May 2022 |language=en |issn=1527-3369}}</ref> At 33–41 weeks' gestation, the fetus is able to distinguish its mother's voice from others.<ref>{{cite journal |doi=10.1016/j.infbeh.2008.10.002 |pmid=19058856 |title=Fetal sensitivity to properties of maternal speech and language |journal=Infant Behavior and Development |volume=32 |issue=1 |pages=59–71 |year=2009 |last1=Kisilevsky |first1=B.S. |last2=Hains |first2=S.M.J. |last3=Brown |first3=C.A. |last4=Lee |first4=C.T. |last5=Cowperthwaite |first5=B. |last6=Stutzman |first6=S.S. |last7=Swansburg |first7=M.L. |last8=Lee |first8=K. |last9=Xie |first9=X. |last10=Huang |first10=H. |last11=Ye |first11=H.-H. |last12=Zhang |first12=K. |last13=Wang |first13=Z. }}</ref><ref>{{cite journal |doi=10.1002/dev.20229 |pmid=17577240 |title=Estimated cardiac vagal tone predicts fetal responses to mother's and stranger's voices |journal=Developmental Psychobiology |volume=49 |issue=5 |pages=543–7 |year=2007 |last1=Smith |first1=Laura S. |last2=Dmochowski |first2=Pawel A. |last3=Muir |first3=Darwin W. |last4=Kisilevsky |first4=Barbara S. }}</ref> | |||
| Whether a ] has the ability to feel ] and to ] is part of the ] debate.<ref>White, R. Frank. "", ''American Society of Anesthesiologists Newsletter'' (October 2001). Retrieved ].</ref> <ref>David, Barry & and Goldberg, Barth. "", ''Illinois Bar Journal'' (December 2002). Retrieved ].</ref> Determining the stage of pregnancy at which a fetus is able to feel pain or suffering could have a significant effect on the abortion debate as well as ]s and practices. For example, legislation has been proposed requiring abortion providers to tell a woman that the fetus may feel pain during the abortion procedure, and requiring her to accept or decline anesthesia for the fetus.<ref>Weisman, Jonathan. "", ''Washington Post'' ]. Retrieved ].</ref> | |||
| ==Prenatal pain== | |||
| A lack of fetal pain does not necessarily "resolve the question of whether abortion is morally acceptable or should be legal".<ref name="Derby"/> Still unresolved would be whether "the obligation not to harm other human subjects extends considerably beyond that of not causing pain."<ref name="McCullagh">McCullagh Peter. ". London: All-Party Parliamentary Pro-Life Group (1996). Dr. McCullagh is a Senior fellow in developmental physiology at the John Curtin School of Medical Research, Australian National University. This report was reprinted in the Catholic Medical Quarterly, XLV11 no 2, November 1996, p6. Retrieved ].</ref> | |||
| ] | |||
| The hypothesis that human fetuses are capable of perceiving ] during the first trimester has little evidence, although fetuses at 14 weeks may respond to touch.<ref>{{Cite journal|last1=Marx|first1=Viola|last2=Nagy|first2=Emese|date=2015-06-08|title=Fetal Behavioural Responses to Maternal Voice and Touch|journal=PLOS ONE|volume=10|issue=6|pages=e0129118|doi=10.1371/journal.pone.0129118|issn=1932-6203|pmc=4460088|pmid=26053388|bibcode=2015PLoSO..1029118M|doi-access=free}}</ref>{{Additional citation needed|date=May 2022|reason=Source is just a single article and not a review; The 8-week figure was only mentioned in passing as a figure from a popular book instead of being an experimental result.}} A multidisciplinary ] from 2005 found limited evidence that thalamocortical pathways begin to function "around 29 to 30 weeks' gestational age", only after which a fetus is capable of feeling pain.<ref name="Lee">{{cite journal|last1=Lee|first1=Susan J.|last2=Ralston|first2=Henry J. Peter|last3=Drey|first3=Eleanor A.|last4=Partridge|first4=John Colin|last5=Rosen|first5=Mark A.|year=2005|title=Fetal Pain|journal=JAMA|volume=294|issue=8|pages=947–54|doi=10.1001/jama.294.8.947|pmid=16118385|doi-access=free}}</ref><ref>{{cite journal |doi=10.1136/bmj.332.7546.909 |pmid=16613970 |pmc=1440624 |title=Can fetuses feel pain? |journal=BMJ |volume=332 |issue=7546 |pages=909–12 |year=2006 |last1=Derbyshire |first1=S. W G }}</ref> | |||
| In March 2010, the Royal College of Obstetricians and Gynecologists submitted a report,<ref name="royalcollege">{{Cite web|date=March 2010|title=Fetal Awareness – Review of Research and Recommendations for Practice|url=http://www.rcog.org.uk/files/rcog-corp/RCOGFetalAwarenessWPR0610.pdf|url-status=dead|archive-url=https://web.archive.org/web/20111002222748/http://www.rcog.org.uk/files/rcog-corp/RCOGFetalAwarenessWPR0610.pdf|archive-date=2011-10-02|publisher=]|via=Internet Archive|access-date=2019-03-27}}</ref> concluding that "Current research shows that the sensory structures are not developed or specialized enough to respond to pain in a fetus of less than 24 weeks",<ref name="royalcollege" />{{rp|22}} | |||
| Most scientists believe that a fetus is able to feel pain sometime during the pregnancy, often beginning less than 24 weeks after conception, although the question of exactly when pain might be possible is disputed.<ref>Derbyshire, David, , Telegraph (UK) ]: "a Daily Telegraph straw poll found many neurologists were concerned that foetuses could feel pain in the womb before 24 weeks after conception."</ref> Some academics argue that it appears as early as seven weeks after conception. Others claim that pain cannot be felt until the ] of pregnancy or until after birth.<ref name="AboPain">Robinson, B.A. (2006). . ''Ontario Consultants for Religious Tolerance.'' Retrieved December 14, 2005.</ref> | |||
| {{blockquote|The neural regions and pathways that are responsible for pain experience remain under debate but it is generally accepted that pain from physical trauma requires an intact pathway from the periphery, through the spinal cord, into the thalamus and on to regions of the cerebral cortex including the primary sensory cortex (S1), the insular cortex and the anterior cingulated cortex. Fetal pain is not possible before these necessary neural pathways and structures have developed.<ref name="royalcollege" />{{rp|3}}}} | |||
| There may be an "emerging consensus among developmental ] that the establishment of ] connections" (at about 26 weeks) is a critical event with regard to fetal perception of pain.<ref name="Johnson"/> Nevertheless, because pain can involve sensory, emotional and cognitive factors, it is "impossible to know" when painful experiences may become possible, even if it is known when thalamocortical connections are established.<ref name="Johnson">Johnson, Martin and Everitt, Barry. '''' (Blackwell 2000): "The multidimensionality of pain perception, involving sensory, emotional, and cognitive factors may in itself be the basis of conscious, painful experience, but it will remain difficult to attribute this to a fetus at any particular developmental age." Retrieved ].</ref> According to ], "there is no consensus among the medical and scientific experts about precisely when a fetus becomes pain-capable. Some put the point at 28 weeks. Others say 26 or 24 and still others younger still."<ref>Caplan, Arthur. Testimony to U.S. Congress, Subcommittee on the Constitution, Civil Rights, and Civil Liberties. "." (]). Retrieved ].</ref> | |||
| The report specifically identified the ] as the area of the ] responsible for processing of pain. The anterior cingulate is part of the cerebral cortex, which begins to develop in the fetus at week 26. A co-author of that report reviewed the evidence in 2020, specifically the functionality of the thalamic projections into the cortical ], and posited "an immediate and unreflective pain experience...from as early as 12 weeks."<ref>{{Cite journal|last1=Derbyshire|first1=Stuart WG|last2=Bockmann|first2=John C.|date=2020-01-01|title=Reconsidering fetal pain|url=https://jme.bmj.com/content/46/1/3|journal=Journal of Medical Ethics|language=en|volume=46|issue=1|pages=3–6|doi=10.1136/medethics-2019-105701|issn=0306-6800|pmid=31937669|doi-access=free}}</ref> | |||
| Multiple nerve systems are involved in the sensation of ]. When the ] and ] are fully developed, the sensation is triggered by ]s reacting to some stimulus. The resulting signal travels via the ] to nociceptors associated with the ]. It then travels up the spinal column to the ], and onward to the ], where it is finally interpreted as a painful sensation. Pain "may exist even in the absence of physical stimuli," and conversely "nociception without pain" exists as well.<ref name="Lee" /> Some scientists believe "the cortex is not required for conscious sensory perception."<ref name="Anand"/> | |||
| There is a consensus among ] that the establishment of ] connections (at weeks 22–34, reliably at 29) is a critical event with regard to fetal perception of pain, as they allow peripheral sensory information to arrive at the cortex.<ref>Johnson, Martin and Everitt, Barry. '''' (Blackwell 2000), p. 235. Retrieved 2007-02-21.</ref> | |||
| Early in development, from about 12-18 weeks gestation, there is a complete link from the periphery to the thalamus in the brain, and the fetus shows clear evidence of defensive reactions against tissue damage including hormonal and hemodynamic responses. After about 26 weeks gestation there is a complete link from the thalamus to the cortex of the brain. Cortical responses in premature babies of about 25 weeks gestation have been recorded during the usual heel lance procedure performed shortly after birth (for blood sampling). In summary, there is good evidence that from about 26 weeks gestation the fetal brain can be considered a functional unit capable of processing noxious sensory input, and pain before that point may also be possible. | |||
| Electroencephalography indicates that the capacity for functional pain perception in premature infants does not exist before 29 or 30 weeks; a 2005 meta-analysis states that withdrawal reflexes and changes of heart rates and hormone levels in response to invasive procedures are reflexes that do not indicate fetal pain.<ref name="Lee"/> | |||
| == Medical opinions == | |||
| Several types of evidence suggest that a fetus does not awaken during its time in the womb. Much of the literature concerning fetal pain simply extrapolates from findings and research of premature babies. The presence of such chemicals as ], ], and ]-D<sub>2</sub> in both human and animal fetuses, indicate that the fetus is both ] and ] when in the womb. These chemicals are oxidized with the newborn's first few breaths and washed out of the tissues, increasing consciousness.<ref>{{Cite journal|last1=Lagercrantz|first1=Hugo|last2=Changeux|first2=Jean-Pierre|date=March 2009|title=The Emergence of Human Consciousness: From Fetal to Neonatal Life|journal=Pediatric Research|volume=65|issue=3|pages=255–260|doi=10.1203/PDR.0b013e3181973b0d|pmid=19092726|s2cid=39391626|issn=0031-3998|quote=The delivery from the mother's womb thus causes arousal from a "resting," sleeping, state in utero. After birth, electrophysiological signs on EEG scalp recordings indicate an intense flow of novel sensory stimuli after birth… In addition, arousal is enhanced by the release from endogenous analgesia possibly caused by removal of the mentioned placental "suppressors" which in utero selectively inhibit neural activity of the fetus…. The catecholamine surge triggered by vaginal delivery may also be critical for the arousal at birth.|doi-access=free}}</ref> If the fetus is asleep throughout gestation then the possibility of fetal pain is greatly minimized,<ref name="Diesch">{{cite journal |doi=10.1016/j.brainresrev.2005.01.006 |pmid=16269314 |title=The importance of 'awareness' for understanding fetal pain |journal=Brain Research Reviews |volume=49 |issue=3 |pages=455–71 |year=2005 |last1=Mellor |first1=David J. |last2=Diesch |first2=Tamara J. |last3=Gunn |first3=Alistair J. |last4=Bennet |first4=Laura |s2cid=9833426 }}</ref><ref>{{cite news|last=Paul|first=AM|title=The First Ache|url=https://www.nytimes.com/2008/02/10/magazine/10Fetal-t.html|newspaper=The New York Times|date=2008-02-10}}</ref> although some studies found that the adenosine levels in third-trimester fetuses are only slightly greater than those in adults' blood.<ref>{{cite journal |doi=10.3109/14767058.2011.632040 |title=Is fetal pain a real evidence? |journal=] |volume=25 |issue=8 |pages=1203–8 |year=2012 |last1=Bellieni |first1=Carlo Valerio |last2=Buonocore |first2=Giuseppe |pmid=22023261 |s2cid=20578842 }}</ref> | |||
| ⚫ | {{ |
||
| ===Fetal anesthesia=== | |||
| In ], Stanislav Reinis and Jerome Goldman wrote that, "The first detectable brain activity in response to noxious stimuli occurs in the thalamus between the ninth and tenth weeks."<ref>Reinis, Stanislav and Goldman, Jerome. '''' (Thomas 1980).</ref> | |||
| Direct fetal ] is used for only a minority of prenatal surgeries.<ref>{{cite journal |doi=10.3109/14767058.2012.718392 |title=Use of fetal analgesia during prenatal surgery |journal=The Journal of Maternal-Fetal & Neonatal Medicine |volume=26 |pages=90–5 |year=2012 |last1=Bellieni |first1=Carlo V. |last2=Tei |first2=M. |last3=Stazzoni |first3=G. |last4=Bertrando |first4=S. |last5=Cornacchione |first5=S. |last6=Buonocore |first6=G. |issue=1 |pmid=22881840 |s2cid=46355976 }}</ref> | |||
| Some caution that unnecessary use of fetal anesthetic may pose potential health risks to the mother. "In the context of abortion, fetal analgesia would be used solely for beneficence toward the fetus, assuming fetal pain exists. This interest must be considered in concert with maternal safety and fetal effectiveness of any proposed anesthetic or analgesic technique. For instance, general anesthesia increases abortion morbidity and mortality for women and substantially increases the cost of abortion. Although placental transfer of many opioids and sedative-hypnotics has been determined, the maternal dose required for fetal analgesia is unknown, as is the safety for women at such doses.<ref name="Lee"/> Given the maternal risk involved and the lack of evidence of any potential benefit to the fetus, administering fetal anesthesia for abortion is not recommended.<ref>{{Cite journal|last1=Society for Maternal-Fetal Medicine|last2=Society of Family Planning|last3=Norton|first3=Mary E.|last4=Cassidy|first4=Arianna|last5=Ralston|first5=Steven J.|last6=Chatterjee|first6=Debnath|last7=Farmer|first7=Diana|last8=Beasley|first8=Anitra D.|last9=Dragoman|first9=Monica|date=2022-02-01|title=Society for Maternal-Fetal Medicine Consult Series #59: The use of analgesia and anesthesia for maternal-fetal procedures|url=https://www.contraceptionjournal.org/article/S0010-7824(21)00441-8/abstract|journal=Contraception|language=English|volume=106|pages=10–15|doi=10.1016/j.contraception.2021.10.003|issn=0010-7824|pmid=34740602|s2cid=243477250|doi-access=free}}</ref> | |||
| In ], anesthesiologist Vincent J. Collins wrote: "because the requisite neurological structures are present at that time and because they are functioning, as evidenced by the aversive response of the human fetus, it may be concluded with reasonable medical certainty that the fetus can sense pain at least by 13 ½ weeks."<ref>Collins, Vincent et al. | |||
| "Fetal Pain and Abortion: the Medical Evidence", ''Studies in Law and Medicine'', No 18 (1984).</ref> Dr. Collins was one of several scientists who wrote an open letter to President Reagan, asserting that, "The ability to feel pain and respond to it is clearly not a phenomenon that develops de novo at birth....by the close of the first trimester the fetus is a sentient, moving being."<ref>Schmidt, Richard et al., "" (]). Retrieved ].</ref> | |||
| Fetal pain legislation may make abortions more difficult to obtain, because abortion clinics lack the equipment and expertise to supply fetal anesthesia. Currently, anesthesia is administered directly to fetuses only while they are undergoing surgery.<ref name="paul">{{cite news |last=Paul |first=Annie Murphy |url=https://www.nytimes.com/2008/02/10/magazine/10Fetal-t.html |title=The First Ache |work=New York Times |date=February 10, 2008}}</ref> | |||
| A ] study observed changes in heart rates and ] of newborn ] after ], ], and surgery — effects which were alleviated with the administration of ].<ref>Anand, K., Phil, D., & Hickey, P.R. (1987). Pain and its effects on the human neonate and fetus. ''New England Journal of Medicine, 316 (21),'' 1321-9. Retrieved ] from .</ref> | |||
| Doctors for a Woman's Choice on Abortion state that the majority of surgical abortions in Britain are already performed with general anesthesia, which also affects the fetus. In a letter to the ''British Medical Journal'' in April 1997, they deemed the discussion "unhelpful to women and to the scientific debate"<ref>{{cite journal |doi=10.1136/bmj.314.7088.1201 |title=Do fetuses feel pain? |journal=BMJ |volume=314 |issue=7088 |pages=1201 |year=1997 |last1=Savage |first1=W. |last2=Wall |first2=P. D |last3=Derbyshire |first3=S. W. |pmc=2126513 |pmid=9146414 }}</ref> despite a report in the ''British Medical Journal'' that "the theoretical possibility that the fetus may feel pain (albeit much earlier than most embryologists and physiologists consider likely) with the procedure of legal abortion".<ref>{{cite journal |doi=10.1136/bmj.314.7076.302a |title=Do fetuses feel pain? |journal=BMJ |volume=314 |issue=7076 |pages=302–3 |year=1997 |last1=McCullagh |first1=P. |last2=Saunders |first2=P J |pmc=2125716 |pmid=9022510 }}</ref> Yet if mothers' general anesthesia were enough to anesthetise the fetus, all fetuses would be born sleepy after a cesarean section performed in general anesthesia, which is not the case.<ref>{{cite journal |doi=10.1097/ACO.0000000000000185 |title=General anesthesia for caesarean section |journal=Curr Opin Anesthesiol |volume=28 |issue=3 |pages=240–246 |year=2015 |last1=Devroe |first1=S.|pmid=25827280 |s2cid=38558311 }}</ref> Dr. Carlo V. Bellieni also agrees that the anesthesia that women receive for fetal surgery is not sufficient to anesthetize the fetus.<ref>Bellieni, Carlo V. (2021-05). . ''Pediatric Research'' '''89''' (7): 1612-1618. {{ISSN|1530-0447}}. {{doi|10.1038/s41390-020-01170-2}}.</ref> | |||
| In ], Dr. Robert J. White, director of the Division of Neurosurgery and Brain Research Laboratory at ] and a member of the ]'s ], gave testimony before the House Constitution Subcommittee of the ]. He stated that, at 20 weeks' gestation, the fetus "is fully capable of experiencing pain...Without question, all of this is a dreadfully painful experience for any infant subjected to such a surgical procedure."<ref>White, Robert. Testimony to U.S. House Judiciary Committee, Subcommittee on the Constitution (]). Quoted in . Retrieved ].</ref> | |||
| ==United States legislation== | |||
| In ], developmental physiologist Peter McCullagh wrote: "At what stage of human prenatal development are those anatomical structures subserving the appreciation of pain present and functional? The balance of evidence at the present time indicates that these structures are present and functional before the tenth week of intrauterine life."<ref name="McCullagh"/> | |||
| ===Federal legislation=== | |||
| In ], Dr. Paul Ranalli, a ] at the ], cited several observations to support the belief that a fetus can experience pain, including observing a fetus "withdraw from painful stimulation", and the fact that ]s detected in pain-stricken adults have also been found in the blood samples of aborted fetuses.<ref>Ranalli, Paul. "" (]).</ref> Dr. Ranalli is a member on the Advisory Board of the deVeber Institute for Bioethics and Social Research, a ] organization.<ref>The deVeber Institute for Bioethics and Social Research. (2004). . Retrieved ].</ref> The group Canadian Physicians for Life cites Ranalli for the proposition that, "enough development has occurred by 12-14 weeks that some pain perception is likely."<ref>. Retrieved ].</ref> | |||
| In 1985, questions about fetal pain were raised during congressional hearings concerning the movie '']''.<ref>Hearing Before the Subcommittee on the Constitution of the Committee on the Judiciary, United States Senate, Ninety-Ninth Congress. (May 21, 1985). S. Hrg. 99–429; Serial No. J-99-28, pages 10 and following</ref> | |||
| In 2013 during the ], ] introduced a bill named the "]" (H.R. 1797). It passed in the House on June 18, 2013, and was received in the U.S. Senate, read twice, and referred to the Judiciary Committee.<ref>''{{Dead link|date=August 2021 |bot=InternetArchiveBot |fix-attempted=yes }}'' H.R.1797, 113th Cong., 1st Sess. (2013)</ref> | |||
| Also in ], a "Working Party" appointed by the ] in the ] stated that "very early in pregnancy fetuses will react to stimuli, but that reaction does not in itself provide any evidence that the fetus experiences those stimuli."<ref> RCOG Press. October 1997.</ref> The Working Party further stated that, "Little sensory input" reaches the brain of the developing foetus before 26 weeks, and "therefore reactions to noxious stimuli cannot be interpreted as feeling or perceiving pain."<ref> BBC.co.uk. 29 August, 2000. Accessed ]. A British government report said in 2007 (shortly before the RCOG report) that signals from the thalamus begin to reach the cortex between "22-34 weeks" after conception. See Parliamentary Office of Science and Technology,'''' (February 1997). Retrieved ].</ref> | |||
| In 2004 during the ], ] introduced a bill named the "]" for the stated purpose of "ensur that women seeking an abortion are fully informed regarding the pain experienced by their unborn child", which was read twice and referred to committee.<ref>'' {{Webarchive|url=https://web.archive.org/web/20081014160455/http://thomas.loc.gov/cgi-bin/query/z?c108:S.2466: |date=2008-10-14 }},'' S.2466, 108t Cong., 2nd Sess. (2004)</ref><ref>Weisman, Jonathan. "", ''Washington Post'' 2006-12-05. Retrieved 2007-02-06.</ref> | |||
| In ], it was noted in the ''British Journal of Obstetrics and Gynaecology'' that, "The first neurones to link the cortex with the rest of the brain are monoamine pathways, and reach the cortex from about 16 weeks of gestation. Their activation could be associated with unpleasant conscious experience, even if not pain."<ref>Glover, Vivette and Fisk, Nicholas. "", ''British Journal of Obstetrics and Gynaecology'' (]) Retrieved ]. Also see "", ''BBC News'', (]): "Professor Vivette Glover from Queen Charlotte's and Chelsea Hospital in London, says she believes that foetuses over 17 weeks old may feel pain." Retrieved ].</ref> | |||
| ===State legislation=== | |||
| In ], a working group of the ] in the United Kingdom suggested that doctors should consider the use of analgesia and sedation for fetuses over 24 weeks of age undergoing surgery.<ref>Medical Research Council, '''' (]). Retrieved ].</ref> Dr. Eve Johnstone, the chair of that working group, told '']'' that a fetus was aware of pain by 24 weeks, maybe as early as 20 weeks,<ref>Highfield, Roger. "," The Telegraph (]). Retrieved ].</ref> because "onnections from the thalamus to the cortex begin to form at about 20 weeks gestation."<ref>Medical Research Council, '''' (]). Retrieved ].</ref> Dr. Susan Dudley of the National Abortion Federation in the U.S. responded: "The obvious and most important thing to say is most abortions take place before 20 weeks."<ref>Beaucar, Kelley. , ''Fox News'' (]). Retrieved ].</ref> | |||
| Subsequently, 25 states have examined similar legislation related to fetal pain and/or fetal anesthesia,<ref name="paul"/> and in 2010 ] banned abortions after 20 weeks on the basis of fetal pain.<ref>Kliff, Sarah '''' The Daily Beast Apr 13, 2010</ref> Eight states – Arkansas, Georgia, Louisiana, Minnesota, Oklahoma, Alaska, South Dakota, and Texas – have passed laws which introduced information on fetal pain in their state-issued abortion-counseling literature, which one opponent of these laws, the ] founded by Planned Parenthood, has termed "generally irrelevant" and not in line "with the current medical literature".<ref>{{cite journal |author1=Gold Rachel Benson |author2=Nash Elizabeth | year = 2007 | title = State Abortion Counseling Policies and the Fundamental Principles of Informed Consent | url = http://www.guttmacher.org/pubs/gpr/10/4/gpr100406.html | journal = Guttmacher Policy Review | volume = 10 | issue = 4 }}</ref> ], director of the Center for Bioethics at the University of Pennsylvania, said laws such as these "reduce ... the process of informed consent to the reading of a fixed script created and mandated by politicians not doctors."<ref>]. "" ''MSNBC.com'', November 30, 2005</ref> | |||
| ==See also== | |||
| In ], Mellor and colleagues reviewed several lines of evidence that suggested a fetus does not awake during it's time in the womb. If the fetus is asleep throughout gestation then the possibility of fetal pain is greatly minimised. <ref>Mellor D.J., Diesch T.J., Gunn A.J., & Bennet L. (2005). . ''Brain Research Reviews, 49(3)'', 455-71. Retrieved December 23, 2006.</ref> | |||
| * ] | |||
| * ] | |||
| * ] | |||
| ⚫ | ==References== | ||
| Later in ], a ] of existing experiments published in the ] (JAMA) concluded that the limited available evidence indicates fetal perception of pain is unlikely before the third trimester, and that electroencephalography suggests the capacity for functional pain perception in premature infants probably does not exist before 29 or 30 weeks; this study asserted that withdrawal reflexes and changes in heart rates and hormone levels in response to invasive procedures are reflexes that do not indicate fetal pain.<ref name="Lee">Lee, Susan J., Ralston, Henry J. Peter, Drey, Eleanor A., Partridge, John Colin, & Rosen, Mark A. (2005). . ''Journal of the American Medical Association, 294 (8)'', 947-954. Retrieved ]. "Evidence regarding the capacity for fetal pain is limited but indicates that fetal perception of pain is unlikely before the third trimester....electroecephalography suggests the capacity for functional pain perception in preterm neonates does not exist before 29 or 30 weeks." A news report about this JAMA study can be found here: "," ''BBC News'' (]). Retrieved ].</ref> This meta-study was criticised by pro-life groups who were skeptical because of the prior involvement of several authors of the report. One directs an abortion clinic at ], while the lead author undertook legal work with ] for six months.<ref>Bazar, Emily. , ''USA Today'' (]). Retrieved ].</ref> | |||
| {{Reflist|30em}} | |||
| ⚫ | ==External links== | ||
| Also in ], the meta-study published in JAMA was criticized by K. J. S. Anand: | |||
| * from U.S. Congress, House Judiciary Committee, Subcommittee on the Constitution, Civil Rights, and Civil Liberties (2005). This includes testimony both for and against proposed legislation dealing with fetal pain. | |||
| {{quote|"The conclusions of Lee and colleagues regarding fetal pain are flawed, because they ignore a large body of research related to pain processing in the brain, present a faulty scientific rationale and use inconsistent methodology for their systematic review. Based on the available scientific evidence, we cannot dismiss the high likelihood of fetal pain perception before the third trimester of human gestation….Fetal development of the thalamus occurs much earlier than the sensory cortex, providing the substrate and mechanisms for conscious pain perception during the second trimester, but not in the first trimester...." | |||
| * from Ontario Consultants on Religious Tolerance. This site : "We feel that all women considering an abortion should be fully informed and as free as possible from outside pressure." | |||
| <ref name="Anand">Anand, K. ", written testimony to Congress (]). Retrieved ].</ref>}} | |||
| ⚫ | * ] site presenting case for fetal pain from second month of pregnancy: . | ||
| * Statement of National Abortion Federation Opposing H.R. 3442, the "Unborn Child Pain Awareness Act" (2008) and . | |||
| ⚫ | * National Right to Life Committee's webpage of testimonies regarding fetal pain: | ||
| * by Eric Schulzke in ''Deseret News'' | |||
| ⚫ | {{Pain}} | ||
| In November of ], Dr. Jean Wright testified to Congress that data "shows 16 weeks and even earlier, many of these infants feel pain and have negative outcomes from it."<ref>Wright, Jean. Testimony to U.S. Congress, Subcommittee on the Constitution, Civil Rights, and Civil Liberties. "." (]). Dr. Wright is Professor and Chair of Pediatrics, Mercer School of Medicine. Retrieved ].</ref> | |||
| {{Neuroscience}} | |||
| {{Mental processes}} | |||
| In ], a clinical review published in the ''British Medical Journal'' concluded that pain is dependent upon cognitive and emotional developments that occur after birth: | |||
| {{quote|"Theories of development assume that the early human mind begins with minimal content and gradually evolves into the rich experience of older children and adults. Although the view of a neonate as a blank slate, or tabula rasa, is generally rejected, it is broadly accepted that psychological processes have content concerning people, objects, and symbols, which lay in the first instance outside the brain. If pain also depends on content derived from outside the brain, then fetal pain cannot be possible, regardless of neural development." <ref name="Derby">Derbyshire, S.W.G. (2006). . ''British Medical Journal'', 332 (7546), 909-12. Retrieved ]. Derbyshire has served as an unpaid consultant to Planned Parenthood of Virginia and Planned Parenthood of Wisconsin, as well as the UK-based Pro-Choice Forum. See | |||
| "", Forbes (]). Retrieved ]. A news report about the Derbyshire article can be found here: "", ''BBC News'' (]). Retrieved ].</ref>}} | |||
| Also in ], a study in the ''Journal of Neuroscience'' stated: "We conclude that noxious information is transmitted to the preterm infant cortex from 25 weeks, highlighting the potential for both higher-level pain processing and pain-induced plasticity in the human brain from a very early age." <ref>Slater, Rebecca et al. "", ''Journal of Neuroscience'', (]). Retrieved ].</ref> | |||
| ⚫ | ==References== | ||
| <references /> | |||
| {{abortion}} | |||
| ⚫ | == |
||
| {{Pregnancy}} | |||
| ⚫ | * |
||
| {{Humandevelopment}} | |||
| * 109th Congress, U.S.A. "<u>Unborn Child Pain Awareness Act of 2005.</u>" 1st Session, S.51. (January, 2005). , | |||
| ⚫ | * National Right to Life Committee's webpage of testimonies regarding fetal pain |
||
| ] | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
Latest revision as of 11:52, 12 December 2024
Study of the different types of sensory perception of fetuses during pregnancy| This article needs attention from an expert in biology. The specific problem is: discrepancy between abortion subsection and rest of the article, and lacking scientific consensus in article overall. WikiProject Biology may be able to help recruit an expert. (August 2009) |
Prenatal perception is the study of the extent of somatosensory and other types of perception during pregnancy. In practical terms, this means the study of fetuses; none of the accepted indicators of perception are present in embryos. Studies of this type inform the abortion controversy, along with certain related pieces of legislation in countries affected by that debate. As of 2022, there is not any scientific consensus on whether a fetus can feel pain.
Prenatal hearing
Numerous studies have found evidence indicating a fetus's ability to respond to auditory stimuli. The earliest fetal response to a sound stimulus has been observed at 16 weeks' gestational age, while the auditory system is fully functional at 25–29 weeks' gestation. At 33–41 weeks' gestation, the fetus is able to distinguish its mother's voice from others.
Prenatal pain
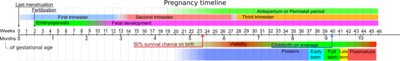
The hypothesis that human fetuses are capable of perceiving pain during the first trimester has little evidence, although fetuses at 14 weeks may respond to touch. A multidisciplinary systematic review from 2005 found limited evidence that thalamocortical pathways begin to function "around 29 to 30 weeks' gestational age", only after which a fetus is capable of feeling pain.
In March 2010, the Royal College of Obstetricians and Gynecologists submitted a report, concluding that "Current research shows that the sensory structures are not developed or specialized enough to respond to pain in a fetus of less than 24 weeks",
The neural regions and pathways that are responsible for pain experience remain under debate but it is generally accepted that pain from physical trauma requires an intact pathway from the periphery, through the spinal cord, into the thalamus and on to regions of the cerebral cortex including the primary sensory cortex (S1), the insular cortex and the anterior cingulated cortex. Fetal pain is not possible before these necessary neural pathways and structures have developed.
The report specifically identified the anterior cingulate as the area of the cerebral cortex responsible for processing of pain. The anterior cingulate is part of the cerebral cortex, which begins to develop in the fetus at week 26. A co-author of that report reviewed the evidence in 2020, specifically the functionality of the thalamic projections into the cortical subplate, and posited "an immediate and unreflective pain experience...from as early as 12 weeks."
There is a consensus among developmental neurobiologists that the establishment of thalamocortical connections (at weeks 22–34, reliably at 29) is a critical event with regard to fetal perception of pain, as they allow peripheral sensory information to arrive at the cortex.
Electroencephalography indicates that the capacity for functional pain perception in premature infants does not exist before 29 or 30 weeks; a 2005 meta-analysis states that withdrawal reflexes and changes of heart rates and hormone levels in response to invasive procedures are reflexes that do not indicate fetal pain.
Several types of evidence suggest that a fetus does not awaken during its time in the womb. Much of the literature concerning fetal pain simply extrapolates from findings and research of premature babies. The presence of such chemicals as adenosine, pregnanolone, and prostaglandin-D2 in both human and animal fetuses, indicate that the fetus is both sedated and anesthetized when in the womb. These chemicals are oxidized with the newborn's first few breaths and washed out of the tissues, increasing consciousness. If the fetus is asleep throughout gestation then the possibility of fetal pain is greatly minimized, although some studies found that the adenosine levels in third-trimester fetuses are only slightly greater than those in adults' blood.
Fetal anesthesia
Direct fetal analgesia is used for only a minority of prenatal surgeries.
Some caution that unnecessary use of fetal anesthetic may pose potential health risks to the mother. "In the context of abortion, fetal analgesia would be used solely for beneficence toward the fetus, assuming fetal pain exists. This interest must be considered in concert with maternal safety and fetal effectiveness of any proposed anesthetic or analgesic technique. For instance, general anesthesia increases abortion morbidity and mortality for women and substantially increases the cost of abortion. Although placental transfer of many opioids and sedative-hypnotics has been determined, the maternal dose required for fetal analgesia is unknown, as is the safety for women at such doses. Given the maternal risk involved and the lack of evidence of any potential benefit to the fetus, administering fetal anesthesia for abortion is not recommended.
Fetal pain legislation may make abortions more difficult to obtain, because abortion clinics lack the equipment and expertise to supply fetal anesthesia. Currently, anesthesia is administered directly to fetuses only while they are undergoing surgery.
Doctors for a Woman's Choice on Abortion state that the majority of surgical abortions in Britain are already performed with general anesthesia, which also affects the fetus. In a letter to the British Medical Journal in April 1997, they deemed the discussion "unhelpful to women and to the scientific debate" despite a report in the British Medical Journal that "the theoretical possibility that the fetus may feel pain (albeit much earlier than most embryologists and physiologists consider likely) with the procedure of legal abortion". Yet if mothers' general anesthesia were enough to anesthetise the fetus, all fetuses would be born sleepy after a cesarean section performed in general anesthesia, which is not the case. Dr. Carlo V. Bellieni also agrees that the anesthesia that women receive for fetal surgery is not sufficient to anesthetize the fetus.
United States legislation
Federal legislation
In 1985, questions about fetal pain were raised during congressional hearings concerning the movie The Silent Scream.
In 2013 during the 113th Congress, Representative Trent Franks introduced a bill named the "Pain-Capable Unborn Child Protection Act" (H.R. 1797). It passed in the House on June 18, 2013, and was received in the U.S. Senate, read twice, and referred to the Judiciary Committee.
In 2004 during the 108th Congress, Senator Sam Brownback introduced a bill named the "Unborn Child Pain Awareness Act" for the stated purpose of "ensur that women seeking an abortion are fully informed regarding the pain experienced by their unborn child", which was read twice and referred to committee.
State legislation
Subsequently, 25 states have examined similar legislation related to fetal pain and/or fetal anesthesia, and in 2010 Nebraska banned abortions after 20 weeks on the basis of fetal pain. Eight states – Arkansas, Georgia, Louisiana, Minnesota, Oklahoma, Alaska, South Dakota, and Texas – have passed laws which introduced information on fetal pain in their state-issued abortion-counseling literature, which one opponent of these laws, the Guttmacher Institute founded by Planned Parenthood, has termed "generally irrelevant" and not in line "with the current medical literature". Arthur Caplan, director of the Center for Bioethics at the University of Pennsylvania, said laws such as these "reduce ... the process of informed consent to the reading of a fixed script created and mandated by politicians not doctors."
See also
References
- Belluck, Pam (2013-09-17). "Complex Science at Issue in Politics of Fetal Pain". The New York Times. ISSN 0362-4331. Retrieved 2022-09-20.
- Levitan, Dave (2015-05-18). "Does a Fetus Feel Pain at 20 Weeks?". FactCheck.org. Retrieved 2022-09-20.
- Karni, Annie (2022-09-13). "Graham Proposes 15-Week Abortion Ban, Splitting Republicans". The New York Times. ISSN 0362-4331. Retrieved 2022-09-20.
- Graven, Stanley N.; Browne, Joy V. (December 2008). "Auditory Development in the Fetus and Infant". Newborn and Infant Nursing Reviews. 8 (4): 187–193. doi:10.1053/j.nainr.2008.10.010. ISSN 1527-3369. S2CID 6361226. Retrieved 31 May 2022.
- Kisilevsky, B.S.; Hains, S.M.J.; Brown, C.A.; Lee, C.T.; Cowperthwaite, B.; Stutzman, S.S.; Swansburg, M.L.; Lee, K.; Xie, X.; Huang, H.; Ye, H.-H.; Zhang, K.; Wang, Z. (2009). "Fetal sensitivity to properties of maternal speech and language". Infant Behavior and Development. 32 (1): 59–71. doi:10.1016/j.infbeh.2008.10.002. PMID 19058856.
- Smith, Laura S.; Dmochowski, Pawel A.; Muir, Darwin W.; Kisilevsky, Barbara S. (2007). "Estimated cardiac vagal tone predicts fetal responses to mother's and stranger's voices". Developmental Psychobiology. 49 (5): 543–7. doi:10.1002/dev.20229. PMID 17577240.
- Marx, Viola; Nagy, Emese (2015-06-08). "Fetal Behavioural Responses to Maternal Voice and Touch". PLOS ONE. 10 (6): e0129118. Bibcode:2015PLoSO..1029118M. doi:10.1371/journal.pone.0129118. ISSN 1932-6203. PMC 4460088. PMID 26053388.
- ^ Lee, Susan J.; Ralston, Henry J. Peter; Drey, Eleanor A.; Partridge, John Colin; Rosen, Mark A. (2005). "Fetal Pain". JAMA. 294 (8): 947–54. doi:10.1001/jama.294.8.947. PMID 16118385.
- Derbyshire, S. W G (2006). "Can fetuses feel pain?". BMJ. 332 (7546): 909–12. doi:10.1136/bmj.332.7546.909. PMC 1440624. PMID 16613970.
- ^ "Fetal Awareness – Review of Research and Recommendations for Practice" (PDF). Royal College of Obstetricians and Gynaecologists. March 2010. Archived from the original (PDF) on 2011-10-02. Retrieved 2019-03-27 – via Internet Archive.
- Derbyshire, Stuart WG; Bockmann, John C. (2020-01-01). "Reconsidering fetal pain". Journal of Medical Ethics. 46 (1): 3–6. doi:10.1136/medethics-2019-105701. ISSN 0306-6800. PMID 31937669.
- Johnson, Martin and Everitt, Barry. Essential reproduction (Blackwell 2000), p. 235. Retrieved 2007-02-21.
- Lagercrantz, Hugo; Changeux, Jean-Pierre (March 2009). "The Emergence of Human Consciousness: From Fetal to Neonatal Life". Pediatric Research. 65 (3): 255–260. doi:10.1203/PDR.0b013e3181973b0d. ISSN 0031-3998. PMID 19092726. S2CID 39391626.
The delivery from the mother's womb thus causes arousal from a "resting," sleeping, state in utero. After birth, electrophysiological signs on EEG scalp recordings indicate an intense flow of novel sensory stimuli after birth… In addition, arousal is enhanced by the release from endogenous analgesia possibly caused by removal of the mentioned placental "suppressors" which in utero selectively inhibit neural activity of the fetus…. The catecholamine surge triggered by vaginal delivery may also be critical for the arousal at birth.
- Mellor, David J.; Diesch, Tamara J.; Gunn, Alistair J.; Bennet, Laura (2005). "The importance of 'awareness' for understanding fetal pain". Brain Research Reviews. 49 (3): 455–71. doi:10.1016/j.brainresrev.2005.01.006. PMID 16269314. S2CID 9833426.
- Paul, AM (2008-02-10). "The First Ache". The New York Times.
- Bellieni, Carlo Valerio; Buonocore, Giuseppe (2012). "Is fetal pain a real evidence?". The Journal of Maternal-Fetal & Neonatal Medicine. 25 (8): 1203–8. doi:10.3109/14767058.2011.632040. PMID 22023261. S2CID 20578842.
- Bellieni, Carlo V.; Tei, M.; Stazzoni, G.; Bertrando, S.; Cornacchione, S.; Buonocore, G. (2012). "Use of fetal analgesia during prenatal surgery". The Journal of Maternal-Fetal & Neonatal Medicine. 26 (1): 90–5. doi:10.3109/14767058.2012.718392. PMID 22881840. S2CID 46355976.
- Society for Maternal-Fetal Medicine; Society of Family Planning; Norton, Mary E.; Cassidy, Arianna; Ralston, Steven J.; Chatterjee, Debnath; Farmer, Diana; Beasley, Anitra D.; Dragoman, Monica (2022-02-01). "Society for Maternal-Fetal Medicine Consult Series #59: The use of analgesia and anesthesia for maternal-fetal procedures". Contraception. 106: 10–15. doi:10.1016/j.contraception.2021.10.003. ISSN 0010-7824. PMID 34740602. S2CID 243477250.
- ^ Paul, Annie Murphy (February 10, 2008). "The First Ache". New York Times.
- Savage, W.; Wall, P. D; Derbyshire, S. W. (1997). "Do fetuses feel pain?". BMJ. 314 (7088): 1201. doi:10.1136/bmj.314.7088.1201. PMC 2126513. PMID 9146414.
- McCullagh, P.; Saunders, P J (1997). "Do fetuses feel pain?". BMJ. 314 (7076): 302–3. doi:10.1136/bmj.314.7076.302a. PMC 2125716. PMID 9022510.
- Devroe, S. (2015). "General anesthesia for caesarean section". Curr Opin Anesthesiol. 28 (3): 240–246. doi:10.1097/ACO.0000000000000185. PMID 25827280. S2CID 38558311.
- Bellieni, Carlo V. (2021-05). "Analgesia for fetal pain during prenatal surgery: 10 years of progress". Pediatric Research 89 (7): 1612-1618. ISSN 1530-0447. doi:10.1038/s41390-020-01170-2.
- Hearing Before the Subcommittee on the Constitution of the Committee on the Judiciary, United States Senate, Ninety-Ninth Congress. (May 21, 1985). First session on: The medical evidence concerning fetal pain. S. Hrg. 99–429; Serial No. J-99-28, pages 10 and following
- Pain-Capable Unborn Child Protection Act of 2013 H.R.1797, 113th Cong., 1st Sess. (2013)
- Unborn Child Pain Awareness Act of 2005 Archived 2008-10-14 at the Wayback Machine, S.2466, 108t Cong., 2nd Sess. (2004)
- Weisman, Jonathan. "House to Consider Abortion Anesthesia Bill", Washington Post 2006-12-05. Retrieved 2007-02-06.
- Kliff, Sarah Newly Passed 'Fetal Pain' Bill in Nebraska Is a Big Deal The Daily Beast Apr 13, 2010
- Gold Rachel Benson; Nash Elizabeth (2007). "State Abortion Counseling Policies and the Fundamental Principles of Informed Consent". Guttmacher Policy Review. 10 (4).
- Caplan, Arthur. "Abortion politics twist facts in fetal pain laws" MSNBC.com, November 30, 2005
External links
- "Oversight Hearing on Pain of the Unborn" from U.S. Congress, House Judiciary Committee, Subcommittee on the Constitution, Civil Rights, and Civil Liberties (2005). This includes testimony both for and against proposed legislation dealing with fetal pain.
- "Can a embryo or fetus feel pain? Various opinions and studies" from Ontario Consultants on Religious Tolerance. This site states: "We feel that all women considering an abortion should be fully informed and as free as possible from outside pressure."
- Anti-abortion site presenting case for fetal pain from second month of pregnancy: HTML version.
- Statement of National Abortion Federation Opposing H.R. 3442, the "Unborn Child Pain Awareness Act" (2008) PDF version and HTML version.
- National Right to Life Committee's webpage of testimonies regarding fetal pain: HTML version
- Small survivors: How the disputed science of fetal pain is reshaping abortion law by Eric Schulzke in Deseret News
| Pain | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| By region/system |
| ||||||||||
| Measurement and testing | |||||||||||
| Pathophysiology | |||||||||||
| Management | |||||||||||
| Related concepts | |||||||||||
| Mental processes | |
|---|---|
| Cognition | |
| Perception | |
| Memory | |
| Other | |
| Pregnancy and childbirth | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Planning | |||||||||
| Conception | |||||||||
| Testing | |||||||||
| Types | |||||||||
| Childbirth |
| ||||||||
| Prenatal |
| ||||||||
| Postpartum |
| ||||||||
| Obstetric history | |||||||||
| Development of the human body | |
|---|---|
| Before birth | |
| Birth and after | |
| Phases | |
| Social and legal | |