| Revision as of 10:20, 2 September 2008 view sourceFranamax (talk | contribs)18,113 edits →Nomenclature: add wikilinked term← Previous edit | Latest revision as of 07:25, 30 December 2024 view source OAbot (talk | contribs)Bots440,440 editsm Open access bot: doi updated in citation with #oabot. | ||
| Line 1: | Line 1: | ||
| {{Short description|Group of diseases involving cell growth}} | |||
| {{sprotected2}} | |||
| {{About|the group of diseases}} | |||
| {{otheruses}} | |||
| {{Pp-semi-indef}} | |||
| {{Infobox_Disease | |||
| {{pp-move}} | |||
| | Name = Cancer | |||
| {{Use dmy dates|date=February 2024}} | |||
| | Image = Normal cancer cell division from NIH-2.svg | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| | Caption = When normal cells are damaged beyond repair, they are eliminated by ] (A). Cancer cells avoid apoptosis and continue to multiply in an unregulated manner (B). | |||
| {{Infobox medical condition (new) | |||
| | DiseasesDB = 28843 | |||
| | name = Cancer | |||
| | ICD10 = | |||
| | image = Tumor Mesothelioma2 legend.jpg | |||
| | ICD9 = | |||
| | caption = A coronal ] showing a malignant ]<br />Legend: → ] ←, ✱ central ], 1 & 3 ]s, 2 ], 4 ]s, 5 ], 6 ], 7 & 8 ]s, 9 ] | |||
| | ICDO = | |||
| | field = ] | |||
| | OMIM = | |||
| | synonyms = ] ], malignant ] | |||
| | MedlinePlus = 001289 | |||
| | pronounce = {{IPAc-en|audio=en-us-cancer.ogg|ˈ|k|æ|n|s|ər}} | |||
| | eMedicineSubj = | |||
| | symptoms = Lump, abnormal bleeding, prolonged cough, unexplained ], change in ]s<ref name=NHS2012/> | |||
| | eMedicineTopic = | |||
| | complications = | |||
| | MeshID = D009369 | |||
| | onset = | |||
| | duration = | |||
| | causes = | |||
| | risks = Exposure to ]s, tobacco, ], poor ], ], excessive ], certain infections<ref name=WHO2018/><ref name=Enviro2008/> | |||
| | diagnosis = | |||
| | differential = | |||
| | prevention = | |||
| | treatment = ], surgery, ], ]<ref name=WHO2018/><ref name=TCT2018/> | |||
| | medication = | |||
| | prognosis = Average ] 66% (USA)<ref name=Seer2014/> | |||
| | frequency = 24 million annually (2019)<ref name="kocarnik">{{cite journal | vauthors = Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD, etal | title = Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019 | journal = JAMA Oncology | volume = 8 | issue = 3 | pages = 420–444 | date = March 2022 | pmid = 34967848 | pmc = 8719276 | doi = 10.1001/jamaoncol.2021.6987 |issn = 2374-2437}}</ref> | |||
| | deaths = 10 million annually (2019)<ref name=kocarnik/> | |||
| }} | }} | ||
| '''Cancer''' is a group of ]s involving ] with the potential to ] or ] to other parts of the body.<ref name=WHO2018/><ref name=WhatIsCancerNCI/> These contrast with ]s, which do not spread.<ref name=WhatIsCancerNCI/> Possible ] include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in ].<ref name=NHS2012>{{cite web |title=Cancer – Signs and symptoms |url=http://www.nhs.uk/Conditions/Cancer/Pages/Symptoms.aspx |website=NHS Choices |access-date=10 June 2014 |url-status=live |archive-url=https://web.archive.org/web/20140608104550/http://www.nhs.uk/Conditions/cancer/Pages/symptoms.aspx |archive-date=8 June 2014}}</ref> While these symptoms may indicate cancer, they can also have other causes.<ref name=NHS2012/> Over ] of cancers affect humans.<ref name=WhatIsCancerNCI/> | |||
| ] specimen containing a large cancer of the breast (in this case, an invasive ]).]] | |||
| ] is the cause of about 22% of cancer deaths.<ref name=WHO2018>{{cite web |title=Cancer |url=https://www.who.int/en/news-room/fact-sheets/detail/cancer |website=World Health Organization |access-date=19 December 2018 |date=12 September 2018}}</ref> Another 10% are due to ], poor ], ] or ].<ref name=WHO2018/><ref>{{cite web |title=Obesity and Cancer Risk |url=http://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet#q3 |publisher=National Cancer Institute |access-date=4 July 2015 |date=3 January 2012 |url-status=live |archive-url=https://web.archive.org/web/20150704154440/http://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet#q3 |archive-date=4 July 2015}}</ref><ref>{{cite journal | vauthors = Jayasekara H, MacInnis RJ, Room R, English DR | title = Long-Term Alcohol Consumption and Breast, Upper Aero-Digestive Tract and Colorectal Cancer Risk: A Systematic Review and Meta-Analysis | journal = Alcohol and Alcoholism | volume = 51 | issue = 3 | pages = 315–30 | date = May 2016 | pmid = 26400678 | doi = 10.1093/alcalc/agv110 | doi-access = free }}</ref> Other factors include certain infections, exposure to ], and environmental pollutants.<ref name="Enviro2008">{{cite journal |vauthors=Anand P, Kunnumakkara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB |date=September 2008 |title=Cancer is a preventable disease that requires major lifestyle changes |journal=Pharmaceutical Research |volume=25 |issue=9 |pages=2097–116 |doi=10.1007/s11095-008-9661-9 |pmc=2515569 |pmid=18626751}}{{Erratum|doi=10.1007/s11095-008-9690-4|pmid=18626751|checked=yes}}</ref> ] with specific viruses, bacteria and parasites is an environmental factor causing approximately 16–18% of cancers worldwide.<ref>{{Cite journal|url=https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(19)30488-7/fulltext|title=Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis|first1=Catherine|last1=de Martel|first2=Damien|last2=Georges|first3=Freddie|last3=Bray|first4=Jacques|last4=Ferlay|first5=Gary M|last5=Clifford|date=15 February 2020|journal=The Lancet Global Health|volume=8|issue=2|pages=e180–e190|doi=10.1016/S2214-109X(19)30488-7|pmid=31862245 |doi-access=free}}</ref> These infectious agents include '']'', ], ], ], ], ], ] and ]. ] (HIV) does not directly cause cancer but it causes immune deficiency that can magnify the risk due to other infections, sometimes up to several thousand fold (in the case of ]). Importantly, vaccination against ] and ] have been shown to nearly eliminate risk of cancers caused by these viruses in persons successfully vaccinated prior to infection. | |||
| ] specimen containing an invasive ] (the crater-like, reddish, irregularly-shaped tumor).]] | |||
| These environmental factors act, at least partly, by changing the ]s of a cell.<ref name=WCR2014Scr/> Typically, many genetic changes are required before cancer develops.<ref name=WCR2014Scr/> Approximately 5–10% of cancers are due to inherited genetic defects.<ref name=ACS-heredity>{{cite web |publisher=] |title=Heredity and Cancer |access-date=22 July 2013 |url=http://www.cancer.org/cancer/cancercauses/geneticsandcancer/heredity-and-cancer |url-status=live |archive-url=https://web.archive.org/web/20130802043732/http://www.cancer.org/cancer/cancercauses/geneticsandcancer/heredity-and-cancer |archive-date=2 August 2013}}</ref> Cancer can be detected by certain signs and symptoms or screening tests.<ref name=WHO2018/> It is then typically further investigated by ] and confirmed by ].<ref>{{cite web |title=How is cancer diagnosed? |url=http://www.cancer.org/treatment/understandingyourdiagnosis/examsandtestdescriptions/testingbiopsyandcytologyspecimensforcancer/testing-biopsy-and-cytology-specimens-for-cancer-how-is-cancer-diagnosed |website=American Cancer Society |date=29 January 2013 |access-date=10 June 2014 |url-status=live |archive-url=https://web.archive.org/web/20140714120018/http://www.cancer.org/treatment/understandingyourdiagnosis/examsandtestdescriptions/testingbiopsyandcytologyspecimensforcancer/testing-biopsy-and-cytology-specimens-for-cancer-how-is-cancer-diagnosed |archive-date=14 July 2014}}</ref> | |||
| ] specimen containing a ], here a ] (the whitish tumor near the bronchi).]] | |||
| The risk of developing certain cancers can be reduced by not smoking, maintaining a healthy weight, limiting alcohol intake, eating plenty of vegetables, fruits, and ]s, ] against certain infectious diseases, limiting consumption of ] and ], and limiting exposure to direct sunlight.<ref name=Kushi2012>{{cite journal |vauthors=Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, Gansler T |s2cid=2067308 |title=American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity |journal= CA: A Cancer Journal for Clinicians |volume=62 |issue=1 |pages=30–67 |year=2012 |pmid=22237782 |doi=10.3322/caac.20140|doi-access=free }}</ref><ref>{{cite journal |vauthors=Parkin DM, Boyd L, Walker LC |title=16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010 |journal=British Journal of Cancer |volume=105 | issue = Suppl 2 |pages=S77–81 |date=December 2011 |pmid=22158327 |pmc=3252065 |doi=10.1038/bjc.2011.489}}</ref> Early detection through screening is useful for ] and ].<ref name=WCR2014Scr>{{cite book |title=World Cancer Report 2014 |date=2014 |publisher=World Health Organization |isbn=978-92-832-0429-9 |url=http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |pages=Chapter 4.7 |archive-url=https://web.archive.org/web/20170712114430/http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |archive-date=12 July 2017 }}</ref> The benefits of ] are controversial.<ref name=WCR2014Scr/><ref name=Got2013>{{cite journal |vauthors=Gøtzsche PC, Jørgensen KJ |title=Screening for breast cancer with mammography |journal=The Cochrane Database of Systematic Reviews |volume=2013 |issue=6 |pages=CD001877 |date=June 2013 |pmid=23737396 |pmc=6464778 |doi=10.1002/14651858.CD001877.pub5}}</ref> Cancer is often treated with some combination of ], surgery, ] and ].<ref name=WHO2018/><ref name=TCT2018>{{cite web |url=https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies/targeted-therapies-fact-sheet |title=Targeted Cancer Therapies |website=cancer.gov |publisher=National Cancer Institute |date=26 February 2018 |access-date=28 March 2018 }}</ref> Pain and symptom management are an important part of care.<ref name=WHO2018/> ] is particularly important in people with advanced disease.<ref name=WHO2018/> The chance of survival depends on the type of cancer and ] at the start of treatment.<ref name=WCR2014Scr/> In children under 15 at diagnosis, the ] in the ] is on average 80%.<ref name=WCR2014Peads>{{cite book |title=World Cancer Report 2014 |date=2014 |publisher=World Health Organization |isbn=978-92-832-0429-9 |url=http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |pages=Chapter 1.3 |archive-url=https://web.archive.org/web/20170712114430/http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |archive-date=12 July 2017 }}</ref> For cancer in the United States, the average five-year survival rate is 66% for all ages.<ref name=Seer2014>{{cite web |title=SEER Stat Fact Sheets: All Cancer Sites |publisher=National Cancer Institute |url=http://seer.cancer.gov/statfacts/html/all.html |access-date=18 June 2014 |url-status=live |archive-url=https://web.archive.org/web/20100926191037/http://seer.cancer.gov/statfacts/html/all.html |archive-date=26 September 2010}}</ref> | |||
| ] specimen containing a ] (the yellowish, spongy-looking tumor in the lower left).]] | |||
| In 2015, about 90.5 million people worldwide had cancer.<ref name=GBD2015Pre>{{cite journal |author=GBD |author-link=Global Burden of Disease Study |collaboration=Disease and Injury Incidence and Prevalence Collaborators |title=Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015 |journal= The Lancet |date=8 October 2016 |volume=388 |issue=10053 |pages=1545–1602 |pmid=27733282 |doi=10.1016/S0140-6736(16)31678-6 |pmc=5055577}}</ref> In 2019, annual cancer cases grew by 23.6 million people, and there were 10 million deaths worldwide, representing over the previous decade increases of 26% and 21%, respectively.<ref name=kocarnik /><ref>{{cite journal|doi=10.1146/annurev-cancerbio-030419-033612|doi-access=free|title=Metabolic Drivers in Hereditary Cancer Syndromes|year=2020| vauthors = Sciacovelli M, Schmidt C, Maher ER, Frezza C |journal=Annual Review of Cancer Biology|volume=4|pages=77–97}}</ref> | |||
| '''Cancer''' (medical term: ] ]) is a class of ]s in which a group of ] display ''uncontrolled growth'' (] beyond the normal limits), ''invasion'' (intrusion on and destruction of adjacent tissues), and sometimes '']'' (spread to other locations in the body via lymph or blood). These three ] properties of cancers differentiate them from ]s, which are self-limited, do not invade or metastasize. Most cancers form a ] but some, like ], do not. The branch of medicine concerned with the study, diagnosis, treatment, and prevention of cancer is ]. | |||
| The most common types of cancer in males are ], ], ], and ].<ref name=WCR2014>{{cite book |title=World Cancer Report 2014 |date=2014 |publisher=World Health Organization |isbn=978-92-832-0429-9 |pages=Chapter 1.1}}</ref><ref name="auto">{{cite journal | vauthors = Siegel RL, Miller KD, Wagle NS, Jemal A | title = Cancer statistics, 2023 | journal = CA | volume = 73 | issue = 1 | pages = 17–48 | date = January 2023 | pmid = 36633525 | doi = 10.3322/caac.21763 | doi-access = free }}</ref> In females, the most common types are ], colorectal cancer, lung cancer, and ].<ref name=WCR2014Scr/><ref name=auto/> If ] other than ] were included in total new cancer cases each year, it would account for around 40% of cases.<ref>{{cite journal | vauthors = Dubas LE, Ingraffea A | title = Nonmelanoma skin cancer | journal = Facial Plastic Surgery Clinics of North America | volume = 21 | issue = 1 | pages = 43–53 | date = February 2013 | pmid = 23369588 | doi = 10.1016/j.fsc.2012.10.003 }}</ref><ref name=Cak2012>{{cite journal | vauthors = Cakir BÖ, Adamson P, Cingi C | title = Epidemiology and economic burden of nonmelanoma skin cancer | journal = Facial Plastic Surgery Clinics of North America | volume = 20 | issue = 4 | pages = 419–422 | date = November 2012 | pmid = 23084294 | doi = 10.1016/j.fsc.2012.07.004 }}</ref> In children, ] and ] are most common, except in Africa, where ] occurs more often.<ref name=WCR2014Peads/> In 2012, about 165,000 children under 15 years of age were diagnosed with cancer.<ref name=WCR2014/> The risk of cancer increases significantly with age, and many cancers occur more commonly in developed countries.<ref name=WCR2014Scr/> Rates are increasing as ] and as lifestyle changes occur in the developing world.<ref name=Epi11>{{cite journal | vauthors = Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D | title = Global cancer statistics | journal = CA | volume = 61 | issue = 2 | pages = 69–90 | date = February 2011 | pmid = 21296855 | doi = 10.3322/caac.20107 | s2cid = 30500384 | doi-access = free }}</ref> The global total economic costs of cancer were estimated at ]1.16 trillion (equivalent to ${{Inflation|US|1.16|2010|r=2}} trillion in {{Inflation/year|US}}) per year {{as of|2010|lc=y}}.<ref name=WCR2014Eco>{{cite book |title=World Report 2014 |date=2014 |publisher=World Health Organization |isbn=978-92-832-0429-9 |url=http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |pages=Chapter 6.7 |archive-url=https://web.archive.org/web/20170712114430/http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |archive-date=12 July 2017 }}</ref> | |||
| Cancer may affect people at all ages, even ]es, but the risk for most varieties increases with age.<ref name="Cancer Research UK">{{cite web | last =Cancer Research UK | title =UK cancer incidence statistics by age | month=January | year=2007 | url =http://info.cancerresearchuk.org/cancerstats/incidence/age/ | accessdate =2007-06-25 }}</ref> Cancer causes about 13% of ].<ref name="WHO">{{cite web | last =WHO | authorlink =World Health Organization | title =Cancer | publisher =World Health Organization |month=February | year=2006 | url =http://www.who.int/mediacentre/factsheets/fs297/en/ | accessdate =2007-06-25 }}</ref> According to the ], 7.6 million people died from cancer in the world during 2007.<ref name="American Cancer Society">{{cite web | last =American Cancer Society | authorlink =Reuters | title =Report sees 7.6 million global 2007 cancer deaths | publisher =Reuters |month=December | year=2007 | url =http://today.reuters.com/news/articlenews.aspx?type=healthNews&storyid=2007-12-17T052342Z_01_N16330649_RTRUKOC_0_US-CANCER-WORLD.xml | accessdate =2007-12-17 }}</ref> Cancers can affect all animals. | |||
| ])]] | |||
| Nearly all cancers are caused by abnormalities in the ] of the ] cells. These abnormalities may be due to the effects of ], such as ], ], ], or ]. Other cancer-promoting genetic abnormalities may be randomly acquired through errors in ], or are ], and thus present in all cells from birth. The ] of cancers are usually affected by complex interactions between carcinogens and the host's ]. New aspects of the genetics of cancer pathogenesis, such as ], and ] are increasingly recognized as important. | |||
| {{TOC limit}} | |||
| Genetic abnormalities found in cancer typically affect two general classes of genes. Cancer-promoting '']s'' are typically activated in cancer cells, giving those cells new properties, such as hyperactive growth and division, protection against ], loss of respect for normal tissue boundaries, and the ability to become established in diverse tissue environments. '']s'' are then inactivated in cancer cells, resulting in the loss of normal functions in those cells, such as accurate DNA replication, control over the ], orientation and adhesion within tissues, and interaction with protective cells of the ]. | |||
| == Etymology and definitions == | |||
| The word comes from the ancient Greek καρκίνος, meaning 'crab' and 'tumor'. Greek physicians ] and ], among others, noted the similarity of crabs to some tumors with swollen veins. The word was introduced in English in the modern medical sense around 1600.<ref>{{Cite web |title=cancer |url=https://www.etymonline.com/word/cancer |url-status=live |archive-url=https://web.archive.org/web/20221107103233/https://www.etymonline.com/word/cancer |archive-date=7 November 2022 |website=www.etymonline.com}}</ref> | |||
| Diagnosis usually requires the ] examination of a tissue ] specimen by a ], although the initial indication of malignancy can be symptoms or ] imaging abnormalities. Most cancers can be treated and some cured, depending on the specific type, location, and ]. Once diagnosed, cancer is usually treated with a combination of ], ] and ]. As research develops, treatments are becoming more specific for different varieties of cancer. There has been significant progress in the development of ] drugs that act specifically on detectable molecular abnormalities in certain tumors, and which minimize damage to normal cells. The prognosis of cancer patients is most influenced by the type of cancer, as well as the ], or extent of the disease. In addition, ] ] and the presence of specific molecular markers can also be useful in establishing prognosis, as well as in determining individual treatments. | |||
| Cancers comprise a large family of diseases that involve abnormal ] with the potential to invade or spread to other parts of the body.<ref name=WHO2018/><ref name=WhatIsCancerNCI/> They form a subset of ]s. A neoplasm or tumor is a group of cells that have undergone unregulated growth and will often form a mass or lump, but may be distributed diffusely.<ref name=ACSglossary>{{cite web |title=Cancer Glossary |website=cancer.org |publisher=American Cancer Society |url=http://www.cancer.org/cancer/cancerglossary/index |access-date=11 September 2013 |url-status=live |archive-url=https://web.archive.org/web/20130901160014/http://www.cancer.org/cancer/cancerglossary/index |archive-date=1 September 2013}}</ref><ref name=NCIdefinition>{{cite web |title=What is cancer? |website=cancer.gov |publisher=National Cancer Institute |access-date=28 March 2018 |url=https://www.cancer.gov/about-cancer/understanding/what-is-cancer|date=17 September 2007}}</ref> | |||
| ==Classification== | |||
| Cancer is generally classified according to the tissue from which the cancerous cells originate, the primary tumor, as well as the normal cell type they most resemble. These are location and histology, respectively. | |||
| All tumor cells show the ]. These characteristics are required to produce a malignant tumor. They include:<ref name=Han2000/> | |||
| * ] and division absent the proper signals | |||
| ===Nomenclature=== | |||
| * Continuous growth and division even given contrary signals | |||
| The following closely related terms may be used to designate abnormal growths: | |||
| * Avoidance of ] | |||
| * ''']:''' originally, it meant any abnormal swelling, lump or mass. In current English, however, the word tumor has become synonymous with neoplasm, specifically solid neoplasm. Note that some neoplasms, such as ], do not form tumors. | |||
| * ] | |||
| * ''']:''' the scientific term to describe an abnormal proliferation of genetically altered cells. Neoplasms can be benign or malignant: | |||
| * Promoting ] | |||
| ** '''Malignant neoplasm''' or '''malignant tumor''': synonymous with '''cancer'''. | |||
| * ] of tissue and formation of ]<ref name=Han2000/> | |||
| ** '''Benign neoplasm''' or ''']''': a tumor (solid neoplasm) that stops growing by itself, does not invade other tissues and does not form metastases. | |||
| * '''Invasive''' tumor is another synonym of '''cancer'''. The name refers to invasion of surrounding tissues. | |||
| The progression from normal cells to cells that can form a detectable mass to cancer involves multiple steps known as malignant progression.<ref name=Han2000>{{cite journal |vauthors=Hanahan D, Weinberg RA |s2cid=1478778 |title=The hallmarks of cancer |journal=Cell |volume=100 |issue=1 |pages=57–70 |date=January 2000 |pmid=10647931 |doi=10.1016/S0092-8674(00)81683-9 |author-link1=Douglas Hanahan |author-link2=Robert Weinberg (biologist)|doi-access=free }}</ref><ref name=Han2011>{{cite journal |vauthors=Hanahan D, Weinberg RA |title=Hallmarks of cancer: the next generation |journal=Cell |volume=144 |issue=5 |pages=646–74 |date=March 2011 |pmid=21376230 |doi=10.1016/j.cell.2011.02.013|doi-access=free }}</ref> | |||
| * '''Pre-malignancy''', '''pre-cancer''' or '''non-invasive''' tumor: A neoplasm that is not invasive but has the potential to progress to cancer (become invasive) if left untreated. These lesions are, in order of increasing potential for cancer, ], ] and ]. | |||
| The following terms can be used to describe a cancer: | |||
| * '''Screening''': a test done on healthy people to detect tumors before they become apparent. A ] is a screening test. | |||
| * '''Diagnosis''': the confirmation of the cancerous nature of a lump. This usually requires a ] or removal of the tumor by ], followed by examination by a ]. | |||
| * '''Surgical excision''': the removal of a tumor by a ]. | |||
| ** '''Surgical margins''': the evaluation by a ] of the edges of the tissue removed by the surgeon to determine if the tumor was removed completely ("negative margins") or if tumor was left behind ("positive margins"). | |||
| * '''Grade''': a number (usually on a scale of 3) established by a ] to describe the degree of resemblance of the tumor to the surrounding benign tissue. | |||
| * '''Stage''': a number (usually on a scale of 4) established by the ] to describe the degree of invasion of the body by the tumor. | |||
| * '''Recurrence''': new tumors that appear at the site of the original tumor after surgery. | |||
| * '''Metastasis''': new tumors that appear far from the original tumor. | |||
| * '''Transformation:''' the concept that a low-grade tumor transforms to a high-grade tumor over time. Example: ]. | |||
| * '''Chemotherapy''': treatment with drugs. | |||
| * '''Radiation therapy''': treatment with radiations. | |||
| * '''Adjuvant''' therapy: treatment, either chemotherapy or radiation therapy, given after surgery to kill the remaining cancer cells. | |||
| * '''Prognosis''': the probability of cure after the therapy. It is usually expressed as a probability of survival five years after diagnosis. Alternatively, it can be expressed as the number of years when 50% of the patients are still alive. Both numbers are derived from statistics accumulated with hundreds of similar patients to give a ]. | |||
| Cancers are classified by the type of cell that resembles the tumor and, therefore, the tissue presumed to be the origin of the tumor. Examples of general categories include: | |||
| * ''']:''' Malignant tumors derived from ] cells. This group represents the most common cancers, including the common forms of ], ], ] and ]. | |||
| * ''']:''' Malignant tumors derived from ], or ] cells. | |||
| * ''']''' and ''']:''' Malignancies derived from hematopoietic (]-forming) cells | |||
| * ''']:''' Tumors derived from ] cells. In adults most often found in the ] and ]; in fetuses, babies, and young children most often found on the body midline, particularly at the tip of the tailbone; in horses most often found at the poll (base of the skull). | |||
| * '''Blastic tumor or ]:''' A tumor (usually malignant) which resembles an immature or embryonic tissue. Many of these tumors are most common in children. | |||
| Malignant tumors (cancers) are usually named using '''-carcinoma''', '''-sarcoma''' or '''-blastoma''' as a suffix, with the Latin or Greek word for the organ of origin as the root. For instance, a cancer of the liver is called '']''; a cancer of the fat cells is called ''liposarcoma''. For common cancers, the English organ name is used. For instance, the most common type of ] is called ''ductal carcinoma of the breast'' or ''mammary ductal carcinoma''. Here, the adjective ''ductal'' refers to the appearance of the cancer under the microscope, resembling normal breast ducts. | |||
| ]s (which are not cancers) are named using '''-oma''' as a suffix with the organ name as the root. For instance, a benign tumor of the smooth muscle of the uterus is called ''leiomyoma'' (the common name of this frequent tumor is ''fibroid''). Unfortunately, some cancers also use the '''-oma''' suffix, examples being ] and ]. | |||
| ===Adult cancers=== | |||
| In the U.S. and other developed countries, cancer is presently responsible for about 25% of all deaths.<ref name="CACancerJClin2005-Jemal"> | |||
| {{cite journal | author=Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, Feuer EJ, Thun MJ | title=Cancer statistics, 2005 | journal=CA Cancer J Clin | year=2005 | pages=10–30 | volume=55 | issue=1 | url=http://caonline.amcancersoc.org/cgi/content/full/55/1/10 | pmid=15661684 | doi=10.3322/canjclin.55.1.10 | doi_brokendate=2008-06-26}}</ref> On a yearly basis, 0.5% of the population is diagnosed with cancer. The statistics below are for adults in the United States, and may vary substantially in other countries: | |||
| {| class="wikitable" | |||
| ! colspan="2" | <big>Male</big> | |||
| | rowspan="7" | | |||
| ! colspan="2" | <big>Female</big> | |||
| |- | |||
| ! width="170px" | most common (by occurrence) !! width="170px" | most common (by mortality)<ref name="CACancerJClin2005-Jemal" /> | |||
| ! width="170px" | most common (by occurrence)!! width="170px" | most common (by mortality)<ref name="CACancerJClin2005-Jemal" /> | |||
| |- | |||
| |] (33%) || lung cancer (31%) || ] (32%) || lung cancer (27%) | |||
| |- | |||
| | ] (13%) || prostate cancer (10%) || lung cancer (12%) || breast cancer (15%) | |||
| |- | |||
| | ] (10%) || colorectal cancer (10%) || colorectal cancer (11%) || colorectal cancer (10%) | |||
| |- | |||
| | ] (7%) || ] (5%) || ] (6%) || ] (6%) | |||
| |- | |||
| | cutaneous ] (5%) || ] (4%) || ] (4%) || pancreatic cancer (6%) | |||
| |} | |||
| ===Child cancers=== | |||
| Cancer can also occur in young children and adolescents, but it is rare (about 150 cases per million yearly in the US). Statistics from the SEER program of the US ] demonstrate that childhood cancers increased 19% between 1975 and 1990, mainly due to an increased incidence in ]. Since 1990, incidence rates have decreased.<ref name="SEER1999">James G. Gurney, Malcolm A. Smith, Julie A. Ross (1999) ''Cancer Incidence and Survival among Children and Adolescents, United States SEER program 1975-1995'', Cancer Statistics Branch, National Cancer Institute, available online from the </ref> | |||
| There is a reasonable doubt that children living near ] face an increased risk of cancer.<ref>http://www.globalresearch.ca/index.php?context=va%26aid=8785</ref> | |||
| ===Infant cancers=== | |||
| The age of peak incidence of cancer in children occurs during the first year of life, in ]s. The average annual incidence in the United States, 1975-1995, was 233 per million infants.<ref name="SEER1999"/> Several estimates of incidence exist. According to SEER,<ref name="SEER1999"/> in the United States: | |||
| *] comprised 28% of infant cancer cases and was the most common malignancy among these young children (65 per million infants). | |||
| *The ] as a group (41 per million infants) represented the next most common type of cancer, comprising 17% of all cases. | |||
| *] comprised 13% of infant cancer, with an average annual incidence rate of nearly 30 per million infants. | |||
| *The average annual incidence rates for malignant germ cell and malignant soft tissue tumors were essentially the same at 15 per million infants. Each comprised about 6% of infant cancer. | |||
| According to another study:<ref name="CACancerJClin2005-Jemal" /> | |||
| *] (usually ]) is the most common infant malignancy (30%), followed by the ] and ]. The remainder consists of ], ]s, ] (arising from muscle), ], ] and ]. | |||
| ] (a ]) often is cited as the most common tumor in this age group, but most teratomas are surgically removed while still benign, hence not necessarily cancer. Prior to the widespread routine use of prenatal ultrasound examinations, the incidence of ]s diagnosed at birth was 25 to 29 per million births<!-- 1:40,000 to 1:35,000 -->. | |||
| Female and male infants have essentially the same overall cancer incidence rates, a notable difference compared to older children. | |||
| White infants have higher cancer rates than black infants. Leukemias accounted for a substantial proportion of this difference: the average annual rate for white infants (48.7 per million) was 66% higher than for | |||
| black infants (29.4 per million).<ref name="SEER1999"/> | |||
| Relative survival for infants is very good for neuroblastoma, ] and ], and fairly good (80%) for leukemia, but not for most other types of cancer. | |||
| == Signs and symptoms == | == Signs and symptoms == | ||
| {{Main|Signs and symptoms of cancer}} | |||
| Roughly, cancer symptoms can be divided into three groups: | |||
| ] depend on the location of the tumor.]] | |||
| * ''Local symptoms'': unusual lumps or swelling ('']''), ] (bleeding), ] and/or ]ation. Compression of surrounding tissues may cause symptoms such as ] (yellowing the eyes and skin). | |||
| * ''Symptoms of ] (spreading)'': enlarged ]s, ] and ], ] (enlarged ]), bone pain, ] of affected bones and ] symptoms. Although advanced cancer may cause ], it is often not the first symptom. | |||
| When cancer begins, it produces no symptoms. Signs and symptoms appear as the mass grows or ]. The findings that result depend on cancer's type and location. Few symptoms are ]. Many frequently occur in individuals who have other conditions. Cancer can be difficult to diagnose and can be considered a "]".<ref name=Card10/> | |||
| * ''Systemic symptoms'': ], ], ] and ] (]), excessive ] (]), ] and specific ], i.e. specific conditions that are due to an active cancer, such as ] or hormonal changes. | |||
| People may become anxious or depressed post-diagnosis. The risk of suicide in people with cancer is approximately double.<ref>{{cite journal |vauthors=Anguiano L, Mayer DK, Piven ML, Rosenstein D |s2cid=45874503 |title=A literature review of suicide in cancer patients |journal=Cancer Nursing |volume=35 |issue=4 |pages=E14–26 |date=July–August 2012 |pmid=21946906 |doi=10.1097/NCC.0b013e31822fc76c|doi-access=free }}</ref> | |||
| Every symptom in the above list can be caused by a variety of conditions (a list of which is referred to as the ]). Cancer may be a common or uncommon cause of each item. | |||
| == |
=== Local symptoms === | ||
| Local symptoms may occur due to the mass of the tumor or its ulceration. For example, mass effects from lung cancer can block the ] resulting in cough or ]; ] can cause narrowing of the ], making it difficult or painful to swallow; and ] may lead to narrowing or blockages in the ], affecting bowel habits. Masses in breasts or testicles may produce observable lumps. ] can cause bleeding that can lead to symptoms such as ] (lung cancer), ] or ] (colon cancer), ] (bladder cancer), or ] (endometrial or cervical cancer). Although localized pain may occur in advanced cancer, the initial tumor is usually painless. Some cancers can cause a buildup of fluid within the chest or ].<ref name="Card10">Holland Chp. 1</ref> | |||
| Most cancers are initially recognized either because signs or symptoms appear or through screening. Neither of these lead to a definitive diagnosis, which usually requires the opinion of a ], a type of physician (medical doctor) who specializes in the diagnosis of cancer and other diseases. | |||
| === |
=== Systemic symptoms === | ||
| Systemic symptoms may occur due to the body's response to the cancer. This may include fatigue, unintentional weight loss, or skin changes.<ref>{{cite book | vauthors = O'Dell M, Stubblefield M |title=Cancer rehabilitation principles and practice |year=2009 |publisher=Demos Medical |location=New York |isbn=978-1-933864-33-4 |page=983 |url={{google books |plainurl=y |id=_JaPlNYgXkEC |page=983}}}}</ref> Some cancers can cause a systemic inflammatory state that leads to ongoing muscle loss and weakness, known as ].<ref>{{cite journal | vauthors = Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE | title = Definition and classification of cancer cachexia: an international consensus | journal = The Lancet. Oncology | volume = 12 | issue = 5 | pages = 489–95 | date = May 2011 | pmid = 21296615 | doi = 10.1016/S1470-2045(10)70218-7 }}</ref> | |||
| ] | |||
| Some cancers, such as ], ]s, and ] or ]s, can cause a persistent ].<ref name=Card10/> | |||
| People with suspected cancer are investigated with ]s. These commonly include ]s, ]s, ]s and ]. | |||
| Shortness of breath, called ], is a common symptom of cancer and its treatment. The causes of cancer-related dyspnea can include tumors in or around the lung, blocked airways, fluid in the lungs, pneumonia, or treatment reactions including an ].<ref>{{Cite web |title=Shortness of Breath {{!}} Cancer-related Side Effects |url=https://www.cancer.org/cancer/managing-cancer/side-effects/shortness-of-breath.html |access-date=10 October 2023 |website=www.cancer.org |language=en}}</ref> Treatment for dyspnea in patients with advanced cancer can include ], bilevel ventilation, ]/] and multicomponent ].<ref>{{Cite book | vauthors = Dy SM, Gupta A, Waldfogel JM, Sharma R, Zhang A, Feliciano JL, Sedhom R, Day J, Gersten RA, Davidson PM, Bass EB |url=http://www.ncbi.nlm.nih.gov/books/NBK565137/ |title=Interventions for Breathlessness in Patients With Advanced Cancer |date=2020 |publisher=Agency for Healthcare Research and Quality (US) |series=AHRQ Comparative Effectiveness Reviews |location=Rockville (MD) |pmid=33289989}}</ref> | |||
| === Biopsy === | |||
| A cancer may be suspected for a variety of reasons, but the definitive diagnosis of most malignancies must be confirmed by ] examination of the cancerous cells by a ]. Tissue can be obtained from a ] or ]. Many biopsies (such as those of the skin, breast or liver) can be done in a doctor's office. Biopsies of other organs are performed under ] and require ] in an ]. | |||
| Some systemic symptoms of cancer are caused by hormones or other molecules produced by the tumor, known as ]. Common paraneoplastic syndromes include ], which can cause ], constipation and dehydration, or ], which can also cause altered mental status, vomiting, headaches, or seizures.<ref>{{cite journal | vauthors = Dimitriadis GK, Angelousi A, Weickert MO, Randeva HS, Kaltsas G, Grossman A | title = Paraneoplastic endocrine syndromes | journal = Endocrine-Related Cancer | volume = 24 | issue = 6 | pages = R173–R190 | date = June 2017 | pmid = 28341725 | doi = 10.1530/ERC-17-0036 | doi-access = free }}</ref> | |||
| The tissue ] given by the pathologist indicates the type of cell that is proliferating, its ] and other features of the tumor. Together, this information is useful to evaluate the ] of this patient and to choose the best treatment. ] and ] are other types of testing that the pathologist may perform on the tissue specimen. These tests may provide information about future behavior of the cancer (prognosis) and best treatment. | |||
| === Metastasis === | |||
| {{Main|Metastasis}} | |||
| == Treatment == | |||
| ] is the spread of cancer to other locations in the body. The dispersed tumors are called metastatic tumors, while the original is called the primary tumor. Almost all cancers can metastasize.<ref name=metastasis/> Most cancer deaths are due to cancer that has metastasized.<ref name="What is Metastasized Cancer">{{cite web |title=What is Metastasized Cancer? |url=http://www.nccn.com/component/content/article/54-cancer-basics/925-what-is-metastasized-cancer.html |website=National Comprehensive Cancer Network |access-date=18 July 2013 |archive-url=https://web.archive.org/web/20130707200430/http://www.nccn.com/component/content/article/54-cancer-basics/925-what-is-metastasized-cancer.html |archive-date=7 July 2013}}</ref> | |||
| Cancer can be treated by ], ], ], ], ] or other methods. The choice of therapy depends upon the location and grade of the tumor and the ] of the disease, as well as the general state of the patient (]). A number of ]s are also under development. | |||
| Metastasis is common in the late stages of cancer and it can occur via the blood or the ] or both. The typical steps in metastasis are: | |||
| Complete removal of the cancer without damage to the rest of the body is the goal of treatment. Sometimes this can be accomplished by surgery, but the propensity of cancers to invade adjacent tissue or to spread to distant sites by microscopic metastasis often limits its effectiveness. The effectiveness of chemotherapy is often limited by toxicity to other tissues in the body. Radiation can also cause damage to normal tissue. | |||
| # Local ] | |||
| Because "cancer" refers to a class of diseases, it is unlikely that there will ever be a single "]" any more than there will be a single treatment for all ]s. | |||
| # ] into the blood or lymph. | |||
| # Circulation through the body. | |||
| === Surgery === | |||
| # ] into the new tissue. | |||
| In theory, non-] cancers can be cured if entirely removed by ], but this is not always possible. When the cancer has ] to other sites in the body prior to surgery, complete surgical excision is usually impossible. In the ]ian model of cancer progression, tumors grow locally, then spread to the lymph nodes, then to the rest of the body. This has given rise to the popularity of local-only treatments such as surgery for small cancers. Even small localized tumors are increasingly recognized as possessing metastatic potential. | |||
| # Proliferation | |||
| # ] | |||
| Examples of surgical procedures for cancer include ] for breast cancer and ] for prostate cancer. The goal of the surgery can be either the removal of only the tumor, or the entire organ. A single cancer cell is invisible to the naked eye but can regrow into a new tumor, a process called recurrence. For this reason, the ] will examine the surgical specimen to determine if a margin of healthy tissue is present, thus decreasing the chance that microscopic cancer cells are left in the patient. | |||
| Different types of cancers tend to metastasize to particular organs. Overall, the most common places for metastases to occur are the ]s, ], brain, and the ]s.<ref name="metastasis">{{cite web |url=https://www.cancer.gov/types/metastatic-cancer |title=Metastatic Cancer: Questions and Answers |access-date=28 March 2018|publisher=National Cancer Institute |date=12 May 2015}}</ref> | |||
| In addition to removal of the primary tumor, surgery is often necessary for ], e.g. determining the extent of the disease and whether it has ] to regional ]s. Staging is a major determinant of ] and of the need for ]. | |||
| While some cancers can be cured if detected early, metastatic cancer is more difficult to treat and control. Nevertheless, some recent treatments are demonstrating encouraging results.<ref>{{cite web |title=Why is cancer so hard to cure? |url=https://www.theage.com.au/national/why-is-cancer-so-hard-to-cure-20230626-p5djiw.html |access-date=17 July 2023 |website=The Age|date=15 July 2023 }}</ref> | |||
| Occasionally, surgery is necessary to control symptoms, such as ] or ]. This is referred to as ]. | |||
| === Radiation therapy === | |||
| {{main|Radiation therapy}} | |||
| ] (also called radiotherapy, X-ray therapy, or irradiation) is the use of ionizing radiation to kill cancer cells and shrink tumors. Radiation therapy can be administered externally via ] (EBRT) or internally via ]. The effects of radiation therapy are localised and confined to the region being treated. Radiation therapy injures or destroys cells in the area being treated (the "target tissue") by damaging their genetic material, making it impossible for these cells to continue to grow and divide. Although radiation damages both cancer cells and normal cells, most normal cells can recover from the effects of radiation and function properly. The goal of radiation therapy is to damage as many cancer cells as possible, while limiting harm to nearby healthy tissue. Hence, it is given in many fractions, allowing healthy tissue to recover between fractions. | |||
| Radiation therapy may be used to treat almost every type of solid tumor, including cancers of the brain, breast, cervix, larynx, lung, pancreas, prostate, skin, stomach, uterus, or soft tissue sarcomas. Radiation is also used to treat leukemia and lymphoma. Radiation dose to each site depends on a number of factors, including the radiosensitivity of each cancer type and whether there are tissues and organs nearby that may be damaged by radiation. Thus, as with every form of treatment, radiation therapy is not without its side effects. | |||
| === Chemotherapy === | |||
| {{main|Chemotherapy}} | |||
| ] is the treatment of cancer with ] ("anticancer drugs") that can destroy cancer cells. In current usage, the term "chemotherapy" usually refers to ''cytotoxic'' drugs which affect rapidly dividing cells in general, in contrast with ''targeted therapy'' (see below). Chemotherapy drugs interfere with cell division in various possible ways, e.g. with the duplication of ] or the separation of newly formed ]s. Most forms of chemotherapy target all rapidly dividing cells and are not specific for cancer cells, although some degree of specificity may come from the inability of many cancer cells to repair ], while normal cells generally can. Hence, chemotherapy has the potential to harm healthy tissue, especially those tissues that have a high replacement rate (e.g. intestinal lining). These cells usually repair themselves after chemotherapy. | |||
| Because some drugs work better together than alone, two or more drugs are often given at the same time. This is called "combination chemotherapy"; most chemotherapy regimens are given in a combination. | |||
| The treatment of some ]s and ]s requires the use of high-dose chemotherapy, and ] (TBI). This treatment ablates the bone marrow, and hence the body's ability to recover and repopulate the blood. For this reason, bone marrow, or peripheral blood stem cell harvesting is carried out before the ablative part of the therapy, to enable "rescue" after the treatment has been given. This is known as autologous ]. Alternatively, ] may be transplanted from a matched unrelated donor (MUD). | |||
| === Targeted therapies === | |||
| {{main|Targeted therapy}} | |||
| Targeted therapy, which first became available in the late 1990s, has had a significant impact in the treatment of some types of cancer, and is currently a very active research area. This constitutes the use of agents specific for the deregulated proteins of cancer cells. Small molecule targeted therapy drugs are generally inhibitors of ] domains on mutated, overexpressed, or otherwise critical proteins within the cancer cell. Prominent examples are the tyrosine kinase inhibitors ] and ]. | |||
| ] is another strategy in which the therapeutic agent is an ] which specifically binds to a protein on the surface of the cancer cells. Examples include the anti-] antibody ] (Herceptin) used in breast cancer, and the anti-CD20 antibody ], used in a variety of ] malignancies. | |||
| ] can also involve small ]s as "homing devices" which can bind to cell surface receptors or affected ] surrounding the tumor. Radionuclides which are attached to this peptides (e.g. RGDs) eventually kill the cancer cell if the nuclide decays in the vicinity of the cell. Especially oligo- or multimers of these binding motifs are of great interest, since this can lead to enhanced tumor specificity and avidity. | |||
| ] (PDT) is a ternary treatment for cancer involving a photosensitizer, tissue oxygen, and light (often using ]). PDT can be used as treatment for ] (BCC) or ]; PDT can also be useful in removing traces of malignant tissue after surgical removal of large tumors.<ref>{{cite journal |last=Dolmans |first=DE |coauthors=Fukumura D, Jain RK |year=2003 |month=May |title=Photodynamic therapy for cancer |journal=Nat Rev Cancer |volume=3 |issue=5 |pages=380–7 |pmid=12724736 |url=http://www.nature.com/nrc/journal/v3/n5/abs/nrc1071_fs.html |doi=10.1038/nrc1071}}</ref> | |||
| === Immunotherapy === | |||
| {{main|Cancer immunotherapy}} | |||
| Cancer immunotherapy refers to a diverse set of therapeutic strategies designed to induce the patient's own ] to fight the tumor. Contemporary methods for generating an immune response against tumours include intravesical ] immunotherapy for superficial bladder cancer, and use of ]s and other ]s to induce an immune response in ] and ] patients. ]s to generate specific ]s are the subject of intensive research for a number of tumours, notably ] and ]. ] is a vaccine-like strategy in late clinical trials for ] in which ]s from the patient are loaded with ] peptides to induce a specific immune response against prostate-derived cells. | |||
| Allogeneic ] ("bone marrow transplantation" from a genetically non-identical donor) can be considered a form of immunotherapy, since the donor's immune cells will often attack the tumor in a phenomenon known as ]. For this reason, allogeneic HSCT leads to a higher cure rate than autologous transplantation for several cancer types, although the side effects are also more severe. | |||
| === Hormonal therapy === | |||
| {{main|Hormonal therapy (oncology)}} | |||
| The growth of some cancers can be inhibited by providing or blocking certain hormones. Common examples of hormone-sensitive tumors include certain types of breast and prostate cancers. Removing or blocking ] or ] is often an important additional treatment. In certain cancers, administration of hormone agonists, such as ]s may be therapeutically beneficial. | |||
| ===Angiogenesis inhibitors=== | |||
| {{Main|Angiogenesis inhibitor}} | |||
| Angiogenesis inhibitors prevent the extensive growth of blood vessels (]) that tumors require to survive. Some, such as ], have been approved and are in clinical use. One of the main problems with anti-angiogenesis drugs is that many factors stimulate blood vessel growth, in normal cells and cancer. Anti-angiogenesis drugs only target one factor, so the other factors continue to stimulate blood vessel growth. Other problems include ], maintenance of stability and activity and targeting at the tumor vasculature.<ref>{{cite journal |author=Kleinman HK, Liau G |title=Gene therapy for antiangiogenesis |journal=J. Natl. Cancer Inst. |volume=93 |issue=13 |pages=965–7 |year=2001 |month=July |pmid=11438554 |doi=10.1093/jnci/93.13.965 |url=http://jnci.oxfordjournals.org/cgi/content/full/93/13/965}}</ref> | |||
| === Symptom control === | |||
| Although the control of the symptoms of cancer is not typically thought of as a treatment directed at the cancer, it is an important determinant of the ] of cancer patients, and plays an important role in the decision whether the patient is able to undergo other treatments. Although doctors generally have the therapeutic skills to reduce pain, nausea, vomiting, diarrhea, hemorrhage and other common problems in cancer patients, the multidisciplinary specialty of ] has arisen specifically in response to the symptom control needs of this group of patients. | |||
| ], such as ] and ], and ]s, drugs to suppress nausea and vomiting, are very commonly used in patients with cancer-related symptoms. Improved ] such as ] and analogues, as well as ] have made aggressive treatments much more feasible in cancer patients. | |||
| ] due to cancer is almost always associated with continuing tissue damage due to the disease process or the treatment (i.e. surgery, radiation, chemotherapy). Although there is always a role for environmental factors and affective disturbances in the genesis of pain behaviors, these are not usually the predominant etiologic factors in patients with cancer pain. Furthermore, many patients with severe pain associated with cancer are nearing the end of their lives and ] therapies are required. Issues such as social stigma of using ], work and functional status, and health care consumption are not likely to be important in the overall case management. Hence, the typical strategy for cancer pain management is to get the patient as comfortable as possible using opioids and other medications, surgery, and physical measures. Doctors have been reluctant to prescribe narcotics for pain in terminal cancer patients, for fear of contributing to addiction or suppressing respiratory function. The ] movement, a more recent offshoot of the ] movement, has engendered more widespread support for preemptive pain treatment for cancer patients. | |||
| ] is a very common problem for cancer patients, and has only recently become important enough for oncologists to suggest treatment, even though it plays a significant role in many patients' quality of life. | |||
| === Treatment trials === | |||
| {{Main|Experimental cancer treatment}} | |||
| ]s, also called research studies, test new treatments in people with cancer. The goal of this research is to find better ways to treat cancer and help cancer patients. Clinical trials test many types of treatment such as new drugs, new approaches to surgery or radiation therapy, new combinations of treatments, or new methods such as ]. | |||
| A clinical trial is one of the final stages of a long and careful cancer research process. The search for new treatments begins in the laboratory, where scientists first develop and test new ideas. If an approach seems promising, the next step may be testing a treatment in animals to see how it affects cancer in a living being and whether it has harmful effects. Of course, treatments that work well in the lab or in animals do not always work well in people. Studies are done with cancer patients to find out whether promising treatments are safe and effective. | |||
| Patients who take part may be helped personally by the treatment they receive. They get up-to-date care from cancer experts, and they receive either a new treatment being tested or the best available standard treatment for their cancer. At the same time, new treatments also may have unknown risks, but if a new treatment proves effective or more effective than standard treatment, study patients who receive it may be among the first to benefit. There is no guarantee that a new treatment being tested or a standard treatment will produce good results. In children with cancer, a survey of trials found that those enrolled in trials were on average not more likely to do better or worse than those on standard treatment; this confirms that success or failure of an experimental treatment cannot be predicted.<ref>{{cite journal |author=Kumar A, Soares H, Wells R, ''et al'' |title=Are experimental treatments for cancer in children superior to established treatments? Observational study of randomised controlled trials by the Children's Oncology Group |journal=BMJ |volume=331 |issue=7528 |pages=1295 |year=2005 |month=December |pmid=16299015 |pmc=1298846 |doi=10.1136/bmj.38628.561123.7C |url=http://bmj.bmjjournals.com/cgi/content/full/331/7528/1295}}</ref> | |||
| === Complementary and alternative === | |||
| {{Main|Unproven cancer therapy}} | |||
| ] (CAM) treatments are the diverse group of medical and health care systems, practices, and products that are not part of conventional medicine.<ref name="mnalt">{{cite journal |author=Cassileth BR, Deng G |title=Complementary and alternative therapies for cancer |journal=Oncologist |volume=9 |issue=1 |pages=80–9 |year=2004 |pmid=14755017 |url=http://theoncologist.alphamedpress.org/cgi/content/full/9/1/80 |doi=10.1634/theoncologist.9-1-80}}</ref> "Complementary medicine" refers to methods and substances used along with conventional medicine, while "alternative medicine" refers to compounds used instead of conventional medicine.<ref> ]. retrieved ] ].</ref> CAM use is common among people with cancer; a 2000 study found that 69% cancer patients had used at least one CAM therapy as part of their cancer treatment.<ref name=Richardson2000>{{cite journal |author=Richardson MA, Sanders T, Palmer JL, Greisinger A, Singletary SE |title=Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology |journal=J. Clin. Oncol. |volume=18 |issue=13 |pages=2505–14 |year=2000 |month=July |pmid=10893280 |url=http://jco.ascopubs.org/cgi/content/full/18/13/2505}}</ref> Most complementary and alternative medicines for cancer have not been rigorously studied or tested. Some alternative treatments which have been investigated and shown to be ineffective continue to be marketed and promoted.<ref name="pmid15061600">{{cite journal |author=Vickers A |title=Alternative cancer cures: "unproven" or "disproven"? |journal=CA Cancer J Clin |volume=54 |issue=2 |pages=110–8 |year=2004 |pmid=15061600 |doi= |url=http://caonline.amcancersoc.org/cgi/content/full/54/2/110}}</ref> | |||
| == Prognosis == | |||
| Cancer has a reputation for being a deadly disease. While this certainly applies to certain particular types, the truths behind the historical connotations of cancer are increasingly being overturned by advances in medical care. Some types of cancer have a prognosis that is substantially better than nonmalignant diseases such as ] and ]. | |||
| Progressive and disseminated malignant disease has a substantial impact on a cancer patient's quality of life, and many cancer treatments (such as ]) may have severe side-effects. In the advanced stages of cancer, many patients need extensive care, affecting family members and friends. ] solutions may include permanent or "respite" hospice nursing. | |||
| === Emotional impact === | |||
| Many local organizations offer a variety of practical and support services to people with cancer. Support can take the form of ], ], advice, financial assistance, transportation to and from treatment, films or information about cancer. Neighborhood organizations, local health care providers, or area hospitals may have resources or services available. | |||
| Counseling can provide emotional support to cancer patients and help them better understand their illness. Different types of counseling include individual, group, family, peer counseling, bereavement, patient-to-patient, and sexuality. | |||
| Many governmental and charitable organizations have been established to help patients cope with cancer. These organizations often are involved in cancer prevention, cancer treatment, and cancer research. | |||
| == Causes == | == Causes == | ||
| {{Main|Causes of cancer}} | |||
| {{main|Carcinogenesis}} | |||
| ] for carcinogenic substances]] | |||
| ] | |||
| Cancer is a diverse class of diseases which differ widely in their causes and biology. The common thread in all known cancers is the acquisition of abnormalities in the genetic material of the cancer cell and its progeny. Research into the pathogenesis of cancer can be divided into three broad areas of focus. The first area of research focuses on the agents and events which cause or facilitate genetic changes in cells destined to become cancer. Second, it is important to uncover the precise nature of the genetic damage, and the genes which are affected by it. The third focus is on the consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell, and in facilitating additional genetic events, leading to further progression of the cancer. | |||
| The majority of cancers, some 90–95% of cases, are due to genetic mutations from environmental and lifestyle factors.<ref name=Enviro2008/> The remaining 5–10% are due to ].<ref name=Enviro2008/> '']'' refers to any cause that is not ], such as lifestyle, economic, and behavioral factors and not merely pollution.<ref name="isbn0-387-78192-7">{{cite book | vauthors = Manton K, Akushevich I, Kravchenko J |title=Cancer Mortality and Morbidity Patterns in the U.S. Population: An Interdisciplinary Approach |url={{google books |plainurl=y |id=fDIbuwtYPlAC}}|date=28 December 2008|publisher=Springer Science & Business Media|isbn=978-0-387-78193-8|quote = The term ''environment'' refers not only to air, water, and soil but also to substances and conditions at home and at the workplace, including diet, smoking, alcohol, drugs, exposure to chemicals, sunlight, ionizing radiation, electromagnetic fields, infectious agents, etc. Lifestyle, economic and behavioral factors are all aspects of our environment. }}</ref> Common environmental factors that contribute to cancer death include tobacco use (25–30%), diet and ] (30–35%), infections (15–20%), ] (both ionizing and non-ionizing, up to 10%), lack of ], and pollution.<ref name=Enviro2008/><ref>{{cite journal | vauthors = Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, McCullough ML, Patel AV, Ma J, Soerjomataram I, Flanders WD, Brawley OW, Gapstur SM, Jemal A | title = Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States | journal = CA: A Cancer Journal for Clinicians | volume = 68 | issue = 1 | pages = 31–54 | date = January 2018 | pmid = 29160902 | doi = 10.3322/caac.21440 | doi-access = free }}</ref> Psychological stress does not appear to be a risk factor for the onset of cancer,<ref name=Cohen2019>{{cite journal | vauthors = Cohen S, Murphy ML, Prather AA | title = Ten Surprising Facts About Stressful Life Events and Disease Risk | journal = Annual Review of Psychology | volume = 70 | pages = 577–597 | date = January 2019 | pmid = 29949726 | pmc = 6996482 | doi = 10.1146/annurev-psych-010418-102857 | quote = the strongest conclusion derived from decades of research on stressors and cancer is that stressful events may be associated with decreased cancer survival but are probably not associated with disease incidence (Chida et al. 2008). }}</ref><ref name="pmid23393080">{{cite journal | vauthors = Heikkilä K, Nyberg ST, Theorell T, Fransson EI, Alfredsson L, Bjorner JB, Bonenfant S, Borritz M, Bouillon K, Burr H, Dragano N, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Madsen IE, Magnusson Hanson LL, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Salo P, Rugulies R, Steptoe A, Suominen S, Vahtera J, Virtanen M, Väänänen A, Westerholm P, Westerlund H, Zins M, Ferrie JE, Singh-Manoux A, Batty GD, Kivimäki M | title = Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women | journal = BMJ | volume = 346 | pages = f165 | date = February 2013 | pmid = 23393080 | pmc = 3567204 | doi = 10.1136/bmj.f165 }}</ref> though it may worsen outcomes in those who already have cancer.<ref name=Cohen2019/> | |||
| === Chemical carcinogens === | |||
| Environmental or lifestyle factors that caused cancer to develop in an individual can be identified by analyzing mutational signatures from genomic sequencing of tumor DNA. For example, this can reveal if lung cancer was caused by tobacco smoke, if skin cancer was caused by UV radiation, or if ] were caused by previous chemotherapy treatment.<ref name=cds>{{cite journal | vauthors = Steele CD, Pillay N, Alexandrov LB | title = An overview of mutational and copy number signatures in human cancer | journal = The Journal of Pathology | volume = 257 | issue = 4 | pages = 454–465 | date = July 2022 | pmid = 35420163 | pmc = 9324981 | doi = 10.1002/path.5912 }}</ref> | |||
| Cancer pathogenesis is traceable back to ] that impact cell growth and metastasis. Substances that cause ] are known as mutagens, and mutagens that cause cancers are known as carcinogens. Particular substances have been linked to specific types of cancer. ] is associated with ] and ]. Prolonged exposure to ] fibers is associated with ]. | |||
| Cancer is generally not a ].<ref name=Tolar>{{cite journal |vauthors=Tolar J, Neglia JP |s2cid=34197973 |title=Transplacental and other routes of cancer transmission between individuals |journal=Journal of Pediatric Hematology/Oncology |volume=25 |issue=6 |pages=430–4 |date=June 2003 |pmid=12794519 |doi=10.1097/00043426-200306000-00002}}</ref> Exceptions include rare transmissions that occur with pregnancies and occasional ]. However, transmissible infectious diseases such as ], ], ] and ], can contribute to the development of cancer.{{citation needed|date=March 2024}} | |||
| Many ]s are also ]s, but some carcinogens are not mutagens. ] is an example of a chemical carcinogen that is not a mutagen. Such chemicals are thought to promote cancers through their stimulating effect on the rate of cell ]. Faster rates of mitosis leaves less time for repair enzymes to repair damaged DNA during ], increasing the likelihood of a genetic mistake. A mistake made during mitosis can lead to the daughter cells receiving the wrong number of ] (''see ] above''). | |||
| === Chemicals === | |||
| ] | |||
| {{Further|Alcohol and cancer|Smoking and cancer}} | |||
| Decades of research have demonstrated the strong association between ] use and cancers of many sites, making it perhaps the most important human carcinogen. Hundreds of epidemiological studies have confirmed this association. Further support comes from the fact that ] death rates in the United States have mirrored ] patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking followed by decreases in lung cancer death rates in men. | |||
| ] | |||
| Exposure to particular substances have been linked to specific types of cancer. These substances are called '']s''. | |||
| === Ionizing radiation === | |||
| Sources of ], such as ] gas, can cause cancer. Prolonged exposure to ] from the ] can lead to ] and other skin malignancies. | |||
| ], for example, causes 90% of lung cancer.<ref name="pmid9594919">{{cite journal |vauthors=Biesalski HK, Bueno de Mesquita B, Chesson A, Chytil F, Grimble R, Hermus RJ, Köhrle J, Lotan R, Norpoth K, Pastorino U, Thurnham D |title=European Consensus Statement on Lung Cancer: risk factors and prevention. Lung Cancer Panel |journal=CA: A Cancer Journal for Clinicians |volume=48 |issue=3 |pages=167–76; discussion 164–66 |year=1998 |pmid=9594919 |doi=10.3322/canjclin.48.3.167|s2cid=20891885 |doi-access=free }}</ref> Tobacco use can cause cancer throughout the body including in the mouth and throat, ], ], stomach, bladder, kidney, cervix, colon/rectum, liver and ].<ref name="pmid12270001">{{cite journal |vauthors=Kuper H, Boffetta P, Adami HO |s2cid=6132726 |title=Tobacco use and cancer causation: association by tumour type |journal=Journal of Internal Medicine |volume=252 |issue=3 |pages=206–24 |date=September 2002 |pmid=12270001 |doi=10.1046/j.1365-2796.2002.01022.x|doi-access=free }}</ref><ref>{{Cite web |date=27 August 2019 |title=Cancer and Tobacco Use |url=https://www.cdc.gov/vitalsigns/cancerandtobacco/index.html |access-date=25 October 2023 |website=Centers for Disease Control and Prevention |language=en-us}}</ref> Tobacco smoke contains over fifty known carcinogens, including ]s and ]s.<ref name=Kuper/> | |||
| Radiation from ]s has been conjectured for some time as a cause but this theory has not gained mainstream support. Nevertheless some experts caution against prolonged exposure.<ref>'''', , 23 July 2008</ref> | |||
| Tobacco is responsible for about one in five cancer deaths worldwide<ref name="Kuper">{{cite journal |vauthors=Kuper H, Adami HO, Boffetta P |s2cid=9172672 |title=Tobacco use, cancer causation and public health impact |journal=Journal of Internal Medicine |volume=251 |issue=6 |pages=455–66 |date=June 2002 |pmid=12028500 |doi=10.1046/j.1365-2796.2002.00993.x|doi-access=free }}</ref> and about one in three in the developed world.<ref name="Sasco">{{cite journal |vauthors=Sasco AJ, Secretan MB, Straif K |title=Tobacco smoking and cancer: a brief review of recent epidemiological evidence |journal=Lung Cancer |volume=45 | issue = Suppl 2 |pages=S3–9 |date=August 2004 |pmid=15552776 |doi=10.1016/j.lungcan.2004.07.998}}</ref> Lung cancer death rates in the United States have mirrored ] patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking rates since the 1950s followed by decreases in lung cancer death rates in men since 1990.<ref name="pmid16998161">{{cite journal |vauthors=Thun MJ, Jemal A |title=How much of the decrease in cancer death rates in the United States is attributable to reductions in tobacco smoking? |journal=Tobacco Control |volume=15 |issue=5 |pages=345–47 |date=October 2006 |pmid=16998161 |pmc=2563648 |doi=10.1136/tc.2006.017749}}</ref><ref name="pmid18434333">{{cite journal |vauthors=Dubey S, Powell CA |title=Update in lung cancer 2007 |journal=American Journal of Respiratory and Critical Care Medicine |volume=177 |issue=9 |pages=941–46 |date=May 2008 |pmid=18434333 |pmc=2720127 |doi=10.1164/rccm.200801-107UP}}</ref> | |||
| === Infectious diseases === | |||
| In Western Europe, 10% of cancers in males and 3% of cancers in females are attributed to alcohol exposure, especially liver and digestive tract cancers.<ref name="pmid21474525">{{cite journal |vauthors=Schütze M, Boeing H, Pischon T, Rehm J, Kehoe T, Gmel G, Olsen A, Tjønneland AM, Dahm CC, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC, Trichopoulou A, Benetou V, Zylis D, Kaaks R, Rohrmann S, Palli D, Berrino F, Tumino R, Vineis P, Rodríguez L, Agudo A, Sánchez MJ, Dorronsoro M, Chirlaque MD, Barricarte A, Peeters PH, van Gils CH, Khaw KT, Wareham N, Allen NE, Key TJ, Boffetta P, Slimani N, Jenab M, Romaguera D, Wark PA, Riboli E, Bergmann MM |title=Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study |journal=BMJ |volume=342 |pages=d1584 |date=April 2011 |pmid=21474525 |pmc=3072472 |doi=10.1136/bmj.d1584}}</ref> Cancer from work-related substance exposures may cause between 2 and 20% of cases,<ref name="pmid18055160">{{cite journal |vauthors=Irigaray P, Newby JA, Clapp R, Hardell L, Howard V, Montagnier L, Epstein S, Belpomme D |title=Lifestyle-related factors and environmental agents causing cancer: an overview |journal=Biomedicine & Pharmacotherapy |volume=61 |issue=10 |pages=640–58 |date=December 2007 |pmid=18055160 |doi=10.1016/j.biopha.2007.10.006}}</ref> causing at least 200,000 deaths.<ref name="WHO_occup">{{cite press release |title=WHO calls for prevention of cancer through healthy workplaces |publisher=World Health Organization |date=27 April 2007 |url=https://www.who.int/mediacentre/news/notes/2007/np19/en/index.html |access-date=13 October 2007 |archive-url=https://web.archive.org/web/20071012202014/http://www.who.int/mediacentre/news/notes/2007/np19/en/index.html |archive-date=12 October 2007}}</ref> Cancers such as lung cancer and ] can come from inhaling tobacco smoke or ] fibers, or ] from exposure to ].<ref name=WHO_occup/> | |||
| Some cancers can be caused by ] with ]s.<ref>{{cite journal |author=Pagano JS, Blaser M, Buendia MA, ''et al'' |title=Infectious agents and cancer: criteria for a causal relation |journal=Semin. Cancer Biol. |volume=14 |issue=6 |pages=453–71 |year=2004 |month=December |pmid=15489139 |doi=10.1016/j.semcancer.2004.06.009}}</ref> Many cancers originate from a ] infection; this is especially true in animals such as ]s, but also in ]s, as viruses are responsible for 15% of human cancers worldwide. The main viruses associated with human cancers are ], ] and ] virus, ], and ]. Experimental and epidemiological data imply a causative role for viruses and they appear to be the second most important risk factor for cancer development in humans, exceeded only by tobacco usage.<ref name="zur Hausen-viruses">{{cite journal | author = zur Hausen H | title = Viruses in human cancers | journal = Science | volume = 254 | issue = 5035 | pages = 1167| year = 1991 | pmid = 1659743| doi = 10.1126/science.1659743 }}</ref> The mode of virally-induced tumors can be divided into two, ''acutely-transforming'' or ''slowly-transforming''. In acutely transforming viruses, the virus carries an overactive oncogene called viral-oncogene (v-onc), and the infected cell is transformed as soon as v-onc is expressed. In contrast, in slowly-transforming viruses, the virus genome is inserts near a proto-oncogene in the host genome. The viral ] or other transcription regulation elements then cause overexpression of that proto-oncogene. This induces uncontrolled cell division. Because the site of insertion is not specific to proto-oncogenes and the chance of insertion near any proto-oncogene is low, slowly-transforming viruses will cause tumors much longer after infection than the acutely-transforming viruses. | |||
| Exposure to ] (PFOA), which is predominantly used in the production of ], is known to cause two kinds of cancer.<ref>{{cite web |url= https://www.scientificamerican.com/article/erin-brockovich-blasts-u-s-regulation-of-toxic-chemicals/ |title= Erin Brockovich Blasts U.S. Regulation of Toxic Chemicals |website= scientificamerican.com | publisher= Scientific American |date= 28 December 2020}}</ref><ref>{{cite news |title=Environmental Pollutant, PFOA, Associated with Increased Risk of Kidney Cancer |url=https://dceg.cancer.gov/news-events/news/2020/pfoa-kidney |work=] |date=24 September 2020}}</ref> | |||
| Hepatitis viruses, including ] and ], can induce a chronic viral infection that leads to ] in 0.47% of ] patients per year (especially in Asia, less so in North America), and in 1.4% of ] carriers per year. Liver cirrhosis, whether from chronic viral hepatitis infection or alcoholism, is associated with the development of ], and the combination of cirrhosis and viral hepatitis presents the highest risk of ] development. Worldwide, ] is one of the most common, and most deadly, cancers due to a huge burden of ] transmission and disease. | |||
| Chemotherapy drugs such as ] compounds are ] that increase the risk of ]<ref name=cds/> | |||
| Advances in cancer research have made a vaccine designed to prevent cancer available. In 2006, the US ] approved a ] vaccine, called ]. The vaccine protects against four HPV types, which together cause 70% of cervical cancers and 90% of genital warts. In March 2007, the US ] ] (ACIP) officially recommended that females aged 11-12 receive the vaccine, and indicated that females as young as age 9 and as old as age 26 are also candidates for immunization. | |||
| ], an ], is a ] that can cause ] to develop.<ref name=cds/> | |||
| In addition to viruses, researchers have noted a connection between ]. The most prominent example is the link between chronic infection of the wall of the stomach with '']'' and ].<ref>{{cite journal |author=Peter S, Beglinger C |title=Helicobacter pylori and gastric cancer: the causal relationship |journal=Digestion |volume=75 |issue=1 |pages=25–35 |year=2007 |pmid=17429205 |doi=10.1159/000101564}}</ref><ref>{{cite journal |author=Wang C, Yuan Y, Hunt RH |title=The association between Helicobacter pylori infection and early gastric cancer: a meta-analysis |journal=Am. J. Gastroenterol. |volume=102 |issue=8 |pages=1789–98 |year=2007 |month=August |pmid=17521398 |doi=10.1111/j.1572-0241.2007.01335.x}}</ref> Although only a minority of those infected with ''Helicobacter'' go on to develop cancer, since this pathogen is quite common it is probably responsible for the majority of these cancers.<ref>{{cite journal |author=Cheung TK, Xia HH, Wong BC |title=Helicobacter pylori eradication for gastric cancer prevention |journal=J. Gastroenterol. |volume=42 Suppl 17 |issue= |pages=10–5 |year=2007 |month=January |pmid=17238019 |doi=10.1007/s00535-006-1939-2}}</ref> | |||
| === |
=== Diet and exercise === | ||
| {{Main|Diet and cancer}} | |||
| Some hormones can act in a similar manner to non-mutagenic carcinogens in that they may stimulate excessive cell growth. A well-established example is the role of ] states in promoting ]. | |||
| {{anchor|Diet}}Diet, ], and ] are related to up to 30–35% of cancer deaths.<ref name=Enviro2008/><ref name="Nutri06">{{cite journal |vauthors=Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, Gansler T, Andrews KS, Thun MJ |s2cid=19823935 |title=American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity |journal=CA: A Cancer Journal for Clinicians |volume=56 |issue=5 |pages=254–81; quiz 313–14 |year=2006 |pmid=17005596 |doi=10.3322/canjclin.56.5.254|doi-access=free /></ref> In the United States, excess body weight is associated with the development of many types of cancer and is a factor in 14–20% of cancer deaths.<ref name="Nutri06"/> A UK study including data on over 5 million people showed higher ] to be related to at least 10 types of cancer and responsible for around 12,000 cases each year in that country.<ref name="BhaskaranLancet">{{cite journal |vauthors=Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L |title=Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults |journal=Lancet |volume=384 |issue=9945 |pages=755–65 |date=August 2014 |pmid=25129328 |doi=10.1016/S0140-6736(14)60892-8 |pmc=4151483/></ref> Physical inactivity is believed to contribute to cancer risk, not only through its effect on body weight but also through negative effects on the ] and ].<ref name="Nutri06"/> More than half of the effect from the diet is due to ] (eating too much), rather than from eating too few vegetables or other healthful foods.{{citation needed|date=March 2024}} | |||
| === Immune system dysfunction === | |||
| Some specific foods are linked to specific cancers. A high-salt diet is linked to ].<ref name=pmid18990005/> ], a frequent food contaminant, causes liver cancer.<ref name=pmid18990005/> ] chewing can cause oral cancer.<ref name="pmid18990005">{{cite journal |vauthors=Park S, Bae J, Nam BH, Yoo KY |title=Aetiology of cancer in Asia |journal=Asian Pacific Journal of Cancer Prevention |volume=9 |issue=3 |pages=371–80 |year=2008 |pmid=18990005 |url=http://www.apocpcontrol.org/page/popup_paper_file_view.php?pno=MzcxIFBhcmsucCZrY29kZT04MjI=&pgubun=i|archive-url=https://web.archive.org/web/20110904052252/http://www.apocpcontrol.org/page/popup_paper_file_view.php?pno=MzcxIFBhcmsucCZrY29kZT04MjI=&pgubun=i |archive-date=4 September 2011}}</ref> National differences in dietary practices may partly explain differences in cancer incidence. For example, ] is more common in Japan due to its high-salt diet<ref name="pmid19107449">{{Cite book |vauthors=Brenner H, Rothenbacher D, Arndt V |chapter=Epidemiology of Stomach Cancer |title=Cancer Epidemiology |volume=472 |chapter-url={{google books |plainurl=y |id=5v1JAQAAIAAJ |page=467}}|pages = 467–77 | year = 2009 | pmid = 19107449 | doi = 10.1007/978-1-60327-492-0_23 | isbn = 978-1-60327-491-3 | series = Methods in Molecular Biology |issue=5450 |pmc=2166976 }}</ref> while ] is more common in the United States. Immigrant cancer profiles mirror those of their new country, often within one generation.<ref name="pmid14278899">{{cite journal |vauthors=Buell P, Dunn JE |title=Cancer Mortality Among Japanese Issei and Nisei of California |journal=Cancer |volume=18 |issue=5 |pages=656–64 |date=May 1965 |pmid=14278899 |doi=10.1002/1097-0142(196505)18:5<656::AID-CNCR2820180515>3.0.CO;2-3|doi-access=free }}</ref> | |||
| ] is associated with a number of malignancies, including ], ], and ]-associated malignancies such as ] and ]. ]-defining illnesses have long included these diagnoses. The increased incidence of malignancies in HIV patients points to the breakdown of immune surveillance as a possible etiology of cancer.<ref>{{cite journal |author=Wood C, Harrington W |title=AIDS and associated malignancies |journal=Cell Res. |volume=15 |issue=11-12 |pages=947–52 |year=2005 |pmid=16354573 |doi=10.1038/sj.cr.7290372}}</ref> Certain other immune deficiency states (e.g. ] and ]) are also associated with increased risk of malignancy.<ref>{{cite journal |author=Mellemkjaer L, Hammarstrom L, Andersen V, ''et al'' |title=Cancer risk among patients with IgA deficiency or common variable immunodeficiency and their relatives: a combined Danish and Swedish study |journal=Clin. Exp. Immunol. |volume=130 |issue=3 |pages=495–500 |year=2002 |pmid=12452841|doi=10.1046/j.1365-2249.2002.02004.x}}</ref> | |||
| === Infection === | |||
| {{Main|Infectious causes of cancer}} | |||
| Worldwide, approximately 18% of cancer deaths are related to ]s.<ref name=Enviro2008/> This proportion ranges from a high of 25% in Africa to less than 10% in the developed world.<ref name=Enviro2008/> Viruses<ref>{{cite journal | vauthors = Moore PS, Chang Y | title = Why do viruses cause cancer? Highlights of the first century of human tumour virology | journal = Nature Reviews. Cancer | volume = 10 | issue = 12 | pages = 878–889 | date = December 2010 | pmid = 21102637 | pmc = 3718018 | doi = 10.1038/nrc2961 | publisher = Springer Science and Business Media LLC }}</ref> are the usual infectious agents that cause cancer but ] and ] may also play a role. ]es (viruses that can cause human cancer) include: | |||
| * ] (]), | |||
| * ] (] and ]), | |||
| * ] (] and primary effusion lymphomas), | |||
| * ] and ] viruses (]) | |||
| * ] (T-cell leukemias). | |||
| * ] (]) | |||
| Bacterial infection may also increase the risk of cancer, as seen in | |||
| * '']''-induced ].<ref name="Viral04">{{cite journal |vauthors=Pagano JS, Blaser M, Buendia MA, Damania B, Khalili K, Raab-Traub N, Roizman B |title=Infectious agents and cancer: criteria for a causal relation |journal=Seminars in Cancer Biology |volume=14 |issue=6 |pages=453–71 |date=December 2004 |pmid=15489139 |doi=10.1016/j.semcancer.2004.06.009 }}</ref><ref name="LjubojevicSkerlev2014">{{cite journal |vauthors=Ljubojevic S, Skerlev M |title=HPV-associated diseases |journal=Clinics in Dermatology |volume=32 |issue=2 |pages=227–34 |year=2014 |pmid=24559558 |doi=10.1016/j.clindermatol.2013.08.007}}</ref> | |||
| * ], a ] associated with '']'' infection (])<ref name=cds/> | |||
| Parasitic infections associated with cancer include: | |||
| * '']'' (]) | |||
| * The ]s, '']'' and '']'' (]).<ref name="pmid20539059">{{cite journal |vauthors=Samaras V, Rafailidis PI, Mourtzoukou EG, Peppas G, Falagas ME |title=Chronic bacterial and parasitic infections and cancer: a review |journal=Journal of Infection in Developing Countries |volume=4 |issue=5 |pages=267–81 |date=June 2010 |pmid=20539059 |doi=10.3855/jidc.819 |url=http://www.jidc.org/index.php/journal/article/download/20539059/387|url-status=live |archive-url=https://web.archive.org/web/20111004123357/http://www.jidc.org/index.php/journal/article/download/20539059/387 |archive-date=4 October 2011|doi-access=free }}</ref> | |||
| === Radiation === | |||
| {{Main|Radiation-induced cancer}} | |||
| Radiation exposure such as ] and radioactive material is a risk factor for cancer.<ref name=NCI2019Rad>{{cite web |title=Radiation |url=https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation |publisher=National Cancer Institute |access-date=8 June 2019 |language=en |date=29 April 2015}}</ref><ref name=WHO2019>{{cite web |title=Sunlight |url=https://www.cancer.gov/about-cancer/causes-prevention/risk/sunlight |publisher=National Cancer Institute |access-date=8 June 2019 |language=en |date=29 April 2015}}</ref><ref>{{cite web |title=Cancer prevention |url=https://www.who.int/cancer/prevention/en/ |website=WHO |access-date=8 June 2019}}</ref> Many ]s are due to ultraviolet radiation, mostly from sunlight.<ref name=WHO2019/> Sources of ionizing radiation include ] and ] gas.<ref name=WHO2019/> | |||
| Ionizing radiation is not a particularly strong ].<ref name=Little>{{cite book |veditors=Kufe DW, Pollock RE, Weichselbaum RR, Bast RC, Gansler TS, Holland JF, Frei E |title=Cancer medicine | vauthors = Little JB |chapter=Chapter 14: Ionizing Radiation |edition=6th |publisher=B.C. Decker |location=Hamilton, Ont |year=2000 |isbn=978-1-55009-113-7 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK20793/ |url-status=live |archive-url=https://web.archive.org/web/20160102193148/http://www.ncbi.nlm.nih.gov/books/NBK20793/ |archive-date=2 January 2016}}</ref> Residential exposure to ] gas, for example, has similar cancer risks as ]. Radiation is a more potent source of cancer when combined with other cancer-causing agents, such as radon plus tobacco smoke. Radiation can cause cancer in most parts of the body, in all animals and at any age. Children are twice as likely to develop radiation-induced leukemia as adults; radiation exposure before birth has ten times the effect.<ref name=Little/> | |||
| Medical use of ionizing radiation is a small but growing source of radiation-induced cancers. Ionizing radiation may be used to treat other cancers, but this may, in some cases, induce a second form of cancer.<ref name=Little/> It is also used in some kinds of ].<ref name="pmid18046031">{{cite journal |vauthors=Brenner DJ, Hall EJ |s2cid=2760372 |title=Computed tomography—an increasing source of radiation exposure |journal=The New England Journal of Medicine |volume=357 |issue=22 |pages=2277–84 |date=November 2007 |pmid=18046031 |doi=10.1056/NEJMra072149|url=https://repositorio.unal.edu.co/handle/unal/79492 }}</ref> | |||
| Prolonged exposure to ] from the ] can lead to ] and other skin malignancies.<ref name=Cleaver>{{cite book |vauthors=Cleaver JE, Mitchell DL |veditors=Bast RC, Kufe DW, Pollock RE |title=Holland-Frei Cancer Medicine |edition=5th |publisher=B.C. Decker |location=Hamilton, Ontario |year=2000 |chapter=15. Ultraviolet Radiation Carcinogenesis |isbn=978-1-55009-113-7 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK20854/ |access-date=31 January 2011 | display-editors = etal |url-status=live |archive-url=https://web.archive.org/web/20150904102726/http://www.ncbi.nlm.nih.gov/books/NBK20854/ |archive-date=4 September 2015}}</ref> Clear evidence establishes ultraviolet radiation, especially the non-ionizing medium wave ], as the cause of most non-melanoma ]s, which are the most common forms of cancer in the world.<ref name=Cleaver/> | |||
| Non-ionizing ] radiation from mobile phones, ] and other similar sources has been described as a ] by the ]'s ].<ref>{{cite web |title=IARC classifies radiofrequency electromagnetic fields as possibly carcinogenic to humans |url=http://www.iarc.fr/en/media-centre/pr/2011/pdfs/pr208_E.pdf |website=World Health Organization |url-status=live |archive-url=https://web.archive.org/web/20110601063650/http://www.iarc.fr/en/media-centre/pr/2011/pdfs/pr208_E.pdf |archive-date=1 June 2011}}</ref> Evidence, however, has not supported a concern.<ref name=NCI2019EF>{{cite web |title=Electromagnetic Fields and Cancer |url=https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/electromagnetic-fields-fact-sheet |publisher=National Cancer Institute |access-date=8 June 2019 |language=en |date=7 January 2019}}</ref><ref name=NCI2019Rad/> This includes that studies have not found a consistent link between mobile phone radiation and cancer risk.<ref>{{cite web |url=https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/cell-phones-fact-sheet |title=Cell Phones and Cancer Risk – National Cancer Institute |publisher=Cancer.gov |date=8 May 2013 |access-date=28 March 2018}}</ref> | |||
| === Heredity === | === Heredity === | ||
| {{Main|Cancer syndrome}} | |||
| Most forms of cancer are "sporadic", and have no basis in heredity. There are, however, a number of recognised ]s of cancer with a hereditary component, often a defective tumor suppressor ]. Famous examples are: | |||
| The vast majority of cancers are non-hereditary (sporadic). ]s are primarily caused by an inherited genetic defect. Less than 0.3% of the population are carriers of a genetic mutation that has a large effect on cancer risk and these cause less than 3–10% of cancer.<ref name=Expert09>{{cite journal |vauthors=Roukos DH |s2cid=24746283 |title=Genome-wide association studies: how predictable is a person's cancer risk? |journal=Expert Review of Anticancer Therapy |volume=9 |issue=4 |pages=389–92 |date=April 2009 |pmid=19374592 |doi=10.1586/era.09.12|doi-access=free }}</ref> Some of these ]s include: certain inherited mutations in the genes '']'' and '']'' with a more than 75% risk of breast cancer and ],<ref name=Expert09/> and ] (HNPCC or Lynch syndrome), which is present in about 3% of people with ],<ref name=Lancet10>{{cite journal |vauthors=Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, Starling N |s2cid=25299272 |title=Colorectal cancer |journal=Lancet |volume=375 |issue=9719 |pages=1030–47 |date=March 2010 |pmid=20304247 |doi=10.1016/S0140-6736(10)60353-4}}</ref> among others. | |||
| * certain inherited mutations in the genes '']'' and '']'' are associated with an elevated risk of ] and ] | |||
| * tumors of various endocrine organs in ] (MEN types 1, 2a, 2b) | |||
| Statistically for cancers causing most mortality, the ] of developing ] when a ] (parent, sibling or child) has been diagnosed with it is about 2.<ref name="Kampman2007">{{cite journal | vauthors = Kampman E | title = A first-degree relative with colorectal cancer: what are we missing? | journal = Cancer Epidemiology, Biomarkers & Prevention | volume = 16 | issue = 1 | pages = 1–3 | date = January 2007 | pmid = 17220324 | doi = 10.1158/1055-9965.EPI-06-0984 | doi-access = free }}</ref> The corresponding relative risk is 1.5 for lung cancer,<ref name="CotéLiu2012">{{cite journal | vauthors = Coté ML, Liu M, Bonassi S, Neri M, Schwartz AG, Christiani DC, Spitz MR, Muscat JE, Rennert G, Aben KK, Andrew AS, Bencko V, Bickeböller H, Boffetta P, Brennan P, Brenner H, Duell EJ, Fabianova E, Field JK, Foretova L, Friis S, Harris CC, Holcatova I, Hong YC, Isla D, Janout V, Kiemeney LA, Kiyohara C, Lan Q, Lazarus P, Lissowska J, Le Marchand L, Mates D, Matsuo K, Mayordomo JI, McLaughlin JR, Morgenstern H, Müeller H, Orlow I, Park BJ, Pinchev M, Raji OY, Rennert HS, Rudnai P, Seow A, Stucker I, Szeszenia-Dabrowska N, Dawn Teare M, Tjønnelan A, Ugolini D, van der Heijden HF, Wichmann E, Wiencke JK, Woll PJ, Yang P, Zaridze D, Zhang ZF, Etzel CJ, Hung RJ | title = Increased risk of lung cancer in individuals with a family history of the disease: a pooled analysis from the International Lung Cancer Consortium | journal = European Journal of Cancer | volume = 48 | issue = 13 | pages = 1957–68 | date = September 2012 | pmid = 22436981 | doi = 10.1016/j.ejca.2012.01.038 | pmc = 3445438 }}</ref> and 1.9 for ].<ref name="Watkins BrunerMoore2003">{{cite journal | vauthors = Bruner DW, Moore D, Parlanti A, Dorgan J, Engstrom P | title = Relative risk of prostate cancer for men with affected relatives: systematic review and meta-analysis | journal = International Journal of Cancer | volume = 107 | issue = 5 | pages = 797–803 | date = December 2003 | pmid = 14566830 | doi = 10.1002/ijc.11466 | s2cid = 25591527 }}</ref> For breast cancer, the relative risk is 1.8 with a first-degree relative having developed it at 50 years of age or older, and 3.3 when the relative developed it when being younger than 50 years of age.<ref name="Singletary2003">{{cite journal | vauthors = Singletary SE | title = Rating the risk factors for breast cancer | journal = Annals of Surgery | volume = 237 | issue = 4 | pages = 474–482 | date = April 2003 | pmid = 12677142 | pmc = 1514477 | doi = 10.1097/01.SLA.0000059969.64262.87 }}</ref> | |||
| * ] (various tumors such as ], breast cancer, ], ]s) due to mutations of ] | |||
| * ] (]s and colonic polyposis) | |||
| Taller people have an increased risk of cancer because they have more cells than shorter people. Since height is genetically determined to a large extent, taller people have a heritable increase of cancer risk.<ref>{{cite journal | vauthors = Green J, Cairns BJ, Casabonne D, Wright FL, Reeves G, Beral V | title = Height and cancer incidence in the Million Women Study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk | journal = The Lancet. Oncology | volume = 12 | issue = 8 | pages = 785–94 | date = August 2011 | pmid = 21782509 | pmc = 3148429 | doi = 10.1016/S1470-2045(11)70154-1 }}</ref> | |||
| * ] an inherited mutation of the ''APC'' gene that leads to early onset of ]. | |||
| * ] (HNPCC, also known as Lynch syndrome) can include familial cases of ], uterine cancer, ], and ], without a preponderance of ]. | |||
| === Physical agents === | |||
| * ], when occurring in young children, is due to a hereditary mutation in the retinoblastoma gene. | |||
| Some substances cause cancer primarily through their physical, rather than chemical, effects.<ref name=Maltoni>{{cite book |vauthors=Maltoni CF, Holland JF |veditors=Bast RC, Kufe DW, Pollock RE |title=Holland-Frei Cancer Medicine |edition=5th |publisher=B.C. Decker |location=Hamilton, Ontario |year=2000 |chapter=Chapter 16: Physical Carcinogens |isbn=978-1-55009-113-7 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK20770/ |access-date=31 January 2011 | display-editors = etal |url-status=live |archive-url=https://web.archive.org/web/20150904102726/http://www.ncbi.nlm.nih.gov/books/NBK20770/ |archive-date=4 September 2015}}</ref> A prominent example of this is prolonged exposure to ], naturally occurring mineral fibers that are a major cause of ] (cancer of the ]) usually the serous membrane surrounding the lungs.<ref name=Maltoni/> Other substances in this category, including both naturally occurring and synthetic asbestos-like fibers, such as ], ], ] and ], are believed to have similar effects.<ref name=Maltoni/> Non-fibrous particulate materials that cause cancer include powdered metallic ] and ] and ] (], ] and ]).<ref name=Maltoni/> Usually, physical carcinogens must get inside the body (such as through inhalation) and require years of exposure to produce cancer.<ref name=Maltoni/> | |||
| * ] patients, who have an extra ], are known to develop malignancies such as ] and ], though the reasons for this difference are not well understood. | |||
| Physical trauma resulting in cancer is relatively rare.<ref name=Gaeta>{{cite book | vauthors = Gaeta JF | veditors = Bast RC, Kufe DW, Pollock RE |title=Holland-Frei Cancer Medicine |edition=5th |publisher=B.C. Decker |location=Hamilton, Ontario |year=2000 |chapter=Chapter 17: Trauma and Inflammation |isbn=978-1-55009-113-7 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK20784/ |access-date=27 January 2011|display-editors=etal |url-status=live |archive-url=https://web.archive.org/web/20150904102726/http://www.ncbi.nlm.nih.gov/books/NBK20784/ |archive-date=4 September 2015}}</ref> Claims that breaking bones resulted in bone cancer, for example, have not been proven.<ref name=Gaeta/> Similarly, physical trauma is not accepted as a cause for cervical cancer, breast cancer or brain cancer.<ref name=Gaeta/> One accepted source is frequent, long-term application of hot objects to the body. It is possible that repeated burns on the same part of the body, such as those produced by ] and kairo heaters (charcoal ]s), may produce skin cancer, especially if carcinogenic chemicals are also present.<ref name=Gaeta/> Frequent consumption of scalding hot tea may produce esophageal cancer.<ref name=Gaeta/> Generally, it is believed that cancer arises, or a pre-existing cancer is encouraged, during the process of healing, rather than directly by the trauma.<ref name=Gaeta/> However, repeated injuries to the same tissues might promote excessive cell proliferation, which could then increase the odds of a cancerous mutation.{{citation needed|date=March 2024}} | |||
| === Other causes === | |||
| A few types of cancer in non-humans have been found to be caused by the tumor cells themselves. This phenomenon is seen in dogs with ], also known as canine transmissible venereal tumor<ref>{{cite journal |author=Murgia C, Pritchard JK, Kim SY, Fassati A, Weiss RA |title=Clonal origin and evolution of a transmissible cancer |journal=Cell |volume=126 |issue=3 |pages=477–87 |year=2006 |pmid=16901782 |doi=10.1016/j.cell.2006.05.051}}</ref>, as well as ] in ]. The closest known analogue to this in humans is individuals who have developed cancer from tumors hiding inside organ transplants. | |||
| Chronic ] has been hypothesized to directly cause mutation.<ref name=Gaeta/><ref name="ColottaAllavena2009">{{cite journal |vauthors=Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A |title=Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability |journal=Carcinogenesis |volume=30 |issue=7 |pages=1073–81 |date=July 2009 |pmid=19468060 |doi=10.1093/carcin/bgp127 |type=review|doi-access=free }}</ref> Inflammation can contribute to proliferation, survival, angiogenesis and migration of cancer cells by influencing the ].<ref>{{cite journal |vauthors=Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R |title=Interaction of tumor cells with the microenvironment |journal=Cell Communication and Signaling |volume=9 |page=18 |date=September 2011 |pmid=21914164 |doi=10.1186/1478-811X-9-18 |number=18 |pmc=3180438 |doi-access=free }}</ref><ref>{{cite journal |vauthors=Mantovani A |title=Molecular pathways linking inflammation and cancer |journal=Current Molecular Medicine |volume=10 |issue=4 |pages=369–73 |date=June 2010 |pmid=20455855 |doi=10.2174/156652410791316968 |type=review}}</ref> ]s build up an inflammatory pro-tumorigenic microenvironment.<ref>{{cite journal |vauthors=Borrello MG, Degl'Innocenti D, Pierotti MA |title=Inflammation and cancer: the oncogene-driven connection |journal=Cancer Letters |volume=267 |issue=2 |pages=262–70 |date=August 2008 |pmid=18502035 |doi=10.1016/j.canlet.2008.03.060 |type=review}}</ref> | |||
| === Hormones === | |||
| ]s also play a role in the development of cancer by promoting ].<ref name=Henderson>{{cite book |vauthors=Henderson BE, Bernstein L, Ross RK |veditors=Bast RC, Kufe DW, Pollock RE |title=Holland-Frei Cancer Medicine |edition=5th |publisher=B.C. Decker |location=Hamilton, Ontario |year=2000 |chapter=Chapter 13: Hormones and the Etiology of Cancer |isbn=978-1-55009-113-7 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK20759/ |access-date=27 January 2011 | display-editors = etal |url-status=live |archive-url=https://web.archive.org/web/20170910174411/https://www.ncbi.nlm.nih.gov/books/NBK20759/ |archive-date=10 September 2017}}</ref> ]s and their binding proteins play a key role in cancer cell proliferation, differentiation and ], suggesting possible involvement in carcinogenesis.<ref>{{cite journal |vauthors=Rowlands MA, Gunnell D, Harris R, Vatten LJ, Holly JM, Martin RM |title=Circulating insulin-like growth factor peptides and prostate cancer risk: a systematic review and meta-analysis |journal=International Journal of Cancer |volume=124 |issue=10 |pages=2416–29 |date=May 2009 |pmid=19142965 |pmc=2743036 |doi=10.1002/ijc.24202}}</ref> | |||
| Hormones are important agents in sex-related cancers, such as cancer of the breast, ], prostate, ovary and ] and also of ] and ].<ref name=Henderson/> For example, the daughters of women who have breast cancer have significantly higher levels of ] and ] than the daughters of women without breast cancer. These higher hormone levels may explain their higher risk of breast cancer, even in the absence of a breast-cancer gene.<ref name=Henderson/> Similarly, men of African ancestry have significantly higher levels of ] than men of European ancestry and have a correspondingly higher level of prostate cancer.<ref name=Henderson/> Men of Asian ancestry, with the lowest levels of testosterone-activating ], have the lowest levels of prostate cancer.<ref name=Henderson/> | |||
| Other factors are relevant: obese people have higher levels of some hormones associated with cancer and a higher rate of those cancers.<ref name=Henderson/> Women who take ] have a higher risk of developing cancers associated with those hormones.<ref name=Henderson/> On the other hand, people who exercise far more than average have lower levels of these hormones and lower risk of cancer.<ref name=Henderson/> ] may be promoted by ]s.<ref name=Henderson/> Some treatments and prevention approaches leverage this cause by artificially reducing hormone levels and thus discouraging hormone-sensitive cancers.<ref name=Henderson/> | |||
| === Autoimmune diseases === | |||
| There is an association between ] and an increased risk of all cancers. People with untreated celiac disease have a higher risk, but this risk decreases with time after diagnosis and strict treatment. This may be due to the adoption of a ], which seems to have a protective role against development of malignancy in people with celiac disease. However, the delay in diagnosis and initiation of a gluten-free diet seems to increase the risk of malignancies.<ref name="pmid26402826">{{cite journal |vauthors=Han Y, Chen W, Li P, Ye J |title=Association Between Coeliac Disease and Risk of Any Malignancy and Gastrointestinal Malignancy: A Meta-Analysis |journal=Medicine |volume=94 |issue=38 |pages=e1612 |date=September 2015 |pmid=26402826 |pmc=4635766 |doi=10.1097/MD.0000000000001612}}</ref> Rates of gastrointestinal cancers are increased in people with ] and ], due to chronic inflammation. ] and ] used to treat these diseases may promote developing extra-intestinal malignancies.<ref>{{cite journal |vauthors=Axelrad JE, Lichtiger S, Yajnik V |title=Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment |journal=World Journal of Gastroenterology |volume=22 |issue=20 |pages=4794–801 |date=May 2016 |pmid=27239106 |pmc=4873872 |doi=10.3748/wjg.v22.i20.4794 |doi-access=free }}</ref> | |||
| == Pathophysiology == | == Pathophysiology == | ||
| {{Main|Carcinogenesis}} | |||
| ] | |||
| === Genetics === | |||
| Cancer is fundamentally a disease of regulation of tissue growth. In order for a normal cell to ] into a cancer cell, ] which regulate cell growth and differentiation must be altered. Genetic changes can occur at many levels, from gain or loss of entire chromosomes to a mutation affecting a ]. There are two broad categories of genes which are affected by these changes. ]s may be normal genes which are expressed at inappropriately high levels, or altered genes which have novel properties. In either case, expression of these genes promotes the malignant phenotype of cancer cells. ]s are genes which inhibit cell division, survival, or other properties of cancer cells. Tumor suppressor genes are often disabled by cancer-promoting genetic changes. Typically, changes in many genes are required to transform a normal cell into a cancer cell. | |||
| {{Main|Oncogenomics}} | |||
| ] | |||
| There is a diverse classification scheme for the various genomic changes which may contribute to the generation of cancer cells. Most of these changes are ]s, or changes in the ] sequence of genomic DNA. ], the presence of an abnormal number of chromosomes, is one genomic change which is not a mutation, and may involve either gain or loss of one or more ] through errors in ]. | |||
| Cancer is fundamentally a disease of tissue growth regulation. For a normal cell to ] into a cancer cell, the ]s that regulate cell growth and differentiation must be altered.<ref name="pmid18234754">{{cite journal |vauthors=Croce CM |s2cid=8813076 |title=Oncogenes and cancer |journal=The New England Journal of Medicine |volume=358 |issue=5 |pages=502–11 |date=January 2008 |pmid=18234754 |doi=10.1056/NEJMra072367}}</ref> | |||
| Large-scale mutations involve the deletion or gain of a portion of a chromosome. ] occurs when a cell gains many copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material. ] occurs when two separate chromosomal regions become abnormally fused, often at a characteristic location. A well-known example of this is the ], or translocation of chromosomes 9 and 22, which occurs in ], and results in production of the ]-] ], an oncogenic ]. | |||
| The affected genes are divided into two broad categories. ]s are genes that promote cell growth and reproduction. ]s are genes that inhibit cell division and survival. Malignant transformation can occur through the formation of novel oncogenes, the inappropriate over-expression of normal oncogenes, or by the under-expression or disabling of tumor suppressor genes. Typically, changes in multiple genes are required to transform a normal cell into a cancer cell.<ref name="pmid11905807">{{cite journal |vauthors=Knudson AG |s2cid=20201610 |title=Two genetic hits (more or less) to cancer |journal=Nature Reviews. Cancer |volume=1 |issue=2 |pages=157–62 |date=November 2001 |pmid=11905807 |doi=10.1038/35101031}}</ref> | |||
| Small-scale mutations include point mutations, deletions, and insertions, which may occur in the ] of a gene and affect its ], or may occur in the gene's ] and alter the function or stability of its ] product. Disruption of a single gene may also result from ] from a ] or ], and such an event may also result in the expression of viral oncogenes in the affected cell and its descendants. | |||
| Genetic changes can occur at different levels and by different mechanisms. The gain or loss of an entire ] can occur through errors in ]. More common are ]s, which are changes in the ] sequence of genomic DNA. | |||
| ===Epigenetics=== | |||
| Large-scale mutations involve the deletion or gain of a portion of a chromosome. ] occurs when a cell gains copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material. ] occurs when two separate chromosomal regions become abnormally fused, often at a characteristic location. A well-known example of this is the ], or translocation of chromosomes 9 and 22, which occurs in ] and results in production of the ]-] ], an oncogenic ]. | |||
| ]s is the study of the regulation of gene expression through chemical, non-mutational changes in DNA structure. The theory of ] in cancer pathogenesis is that non-mutational changes to DNA can lead to alterations in gene expression. Normally, ] are silent, for example, because of ]. Loss of that methylation can induce the aberrant expression of ], leading to cancer pathogenesis. Known mechanisms of epigenetic change include ], and methylation or acetylation of ] proteins bound to chromosomal DNA at specific locations. Classes of medications, known as ] and ] inhibitors, can re-regulate the epigenetic signaling in the cancer cell. | |||
| Small-scale mutations include point mutations, deletions, and insertions, which may occur in the ] region of a gene and affect its ], or may occur in the gene's ] and alter the function or stability of its ] product. Disruption of a single gene may also result from ] from a ] or ], leading to the expression of ''viral'' oncogenes in the affected cell and its descendants. | |||
| === Oncogenes === | |||
| ]s promote cell growth through a variety of ways. Many can produce ]s, a "chemical messenger" between cells which encourage ], the effect of which depends on the ] of the receiving tissue or cells. In other words, when a hormone receptor on a recipient cell is stimulated, the signal is conducted from the surface of the cell to the ] to effect some change in gene transcription regulation at the nuclear level. Some oncogenes are part of the signal transduction system itself, or the signal ] in cells and tissues themselves, thus controlling the sensitivity to such hormones. Oncogenes often produce ]s, or are involved in ] of DNA in ], which creates the ]s and ]s responsible for producing the products and ] cells use and interact with. | |||
| Replication of the data contained within the DNA of living cells will ] result in some errors (mutations). Complex error correction and prevention are built into the process and safeguard the cell against cancer. If a significant error occurs, the damaged cell can self-destruct through programmed cell death, termed ]. If the error control processes fail, then the mutations will survive and be passed along to ]. | |||
| Mutations in proto-oncogenes, which are the normally quiescent counterparts of ], can modify their ] and function, increasing the amount or activity of the product protein. When this happens, the proto-oncogenes become ]s, and this transition upsets the normal balance of ] regulation in the cell, making uncontrolled growth possible. The chance of cancer cannot be reduced by removing proto-oncogenes from the ], even if this were possible, as they are critical for growth, repair and ] of the organism. It is only when they become mutated that the signals for growth become excessive. | |||
| Some environments make errors more likely to arise and propagate. Such environments can include the presence of disruptive substances called ]s, repeated physical injury, heat, ionising radiation, or ].<ref>{{cite journal |vauthors=Nelson DA, Tan TT, Rabson AB, Anderson D, Degenhardt K, White E |title=Hypoxia and defective apoptosis drive genomic instability and tumorigenesis |journal=Genes & Development |volume=18 |issue=17 |pages=2095–107 |date=September 2004 |pmid=15314031 |pmc=515288 |doi=10.1101/gad.1204904}}</ref> | |||
| One of the first ] to be defined in cancer research is the ]. Mutations in the Ras family of ]s (comprising H-Ras, N-Ras and K-Ras) are very common, being found in 20% to 30% of all human tumours.<ref>{{cite journal | author=Bos J | title=ras oncogenes in human cancer: a review | journal=Cancer Res | volume=49 | issue=17 | pages=4682–9 | year=1989 | pmid=2547513}}</ref> Ras was originally identified in the Harvey sarcoma virus genome, and researchers were surprised that not only was this gene present in the human genome but that, when ligated to a stimulating control element, could induce cancers in cell line cultures.<ref name="pmid6283358">{{cite journal |author=Chang EH, Furth ME, Scolnick EM, Lowy DR |title=Tumorigenic transformation of mammalian cells induced by a normal human gene homologous to the oncogene of Harvey murine sarcoma virus |journal=Nature |volume=297 |issue=5866 |pages=479–83 |year=1982 |pmid=6283358|doi=10.1038/297479a0}}</ref> | |||
| The errors that cause cancer are self-amplifying and compounding, for example: | |||
| * A mutation in the error-correcting machinery of a cell might cause that cell and its children to accumulate errors more rapidly. | |||
| === Tumor suppressor genes === | |||
| * A further mutation in an oncogene might cause the cell to reproduce more rapidly and more frequently than its normal counterparts. | |||
| ]s code for anti-proliferation signals and proteins that suppress mitosis and cell growth. Generally, tumor suppressors are ]s that are activated by cellular ] or DNA damage. Often DNA damage will cause the presence of free-floating genetic material as well as other signs, and will trigger enzymes and pathways which lead to the activation of ]. The functions of such genes is to arrest the progression of the cell cycle in order to carry out DNA repair, preventing mutations from being passed on to daughter cells. The ] protein, one of the most important studied tumor suppressor genes, is a transcription factor activated by many cellular stressors including ] and ] damage. | |||
| * A further mutation may cause loss of a tumor suppressor gene, disrupting the apoptosis signaling pathway and immortalizing the cell. | |||
| * A further mutation in the signaling machinery of the cell might send error-causing signals to nearby cells. | |||
| Despite nearly half of all cancers possibly involving alterations in p53, its tumor suppressor function is poorly understood. p53 clearly has two functions: one a nuclear role as a transcription factor, and the other a cytoplasmic role in regulating the cell cycle, cell division, and apoptosis. | |||
| The transformation of a normal cell into cancer is akin to a ] caused by initial errors, which compound into more severe errors, each progressively allowing the cell to escape more controls that limit normal tissue growth. This rebellion-like scenario is an undesirable ], where the driving forces of ] work against the body's design and enforcement of order. Once cancer has begun to develop, this ongoing process, termed '']'', drives progression towards more invasive ].<ref name="pmid17109012">{{cite journal |vauthors=Merlo LM, Pepper JW, Reid BJ, Maley CC |s2cid=8040576 |title=Cancer as an evolutionary and ecological process |journal=Nature Reviews. Cancer |volume=6 |issue=12 |pages=924–35 |date=December 2006 |pmid=17109012 |doi=10.1038/nrc2013}}</ref> Clonal evolution leads to intra-] (cancer cells with heterogeneous mutations) that complicates designing effective treatment strategies and requires an ]. | |||
| The ] is the preferential use of glycolysis for energy to sustain cancer growth. p53 has been shown to regulate the shift from the respiratory to the glycolytic pathway.<ref name="Mantoba-Warburg">{{cite journal | author = Matoba S, Kang J, Patino W, Wragg A, Boehm M, Gavrilova O, Hurley P, Bunz F, Hwang P | title = p53 regulates mitochondrial respiration | journal = Science | volume = 312 | issue = 5780 | pages = 1650–3 | year = 2006 | pmid = 16728594 | doi = 10.1126/science.1126863}}</ref> | |||
| Characteristic abilities developed by cancers are divided into categories, specifically evasion of apoptosis, self-sufficiency in growth signals, insensitivity to anti-growth signals, sustained angiogenesis, limitless replicative potential, metastasis, reprogramming of energy metabolism and evasion of immune destruction.<ref name=Han2000/><ref name=Han2011/> | |||
| However, a mutation can damage the tumor suppressor gene itself, or the signal pathway which activates it, "switching it off". The invariable consequence of this is that DNA repair is hindered or inhibited: DNA damage accumulates without repair, inevitably leading to cancer. | |||
| === Epigenetics === | |||
| Mutations of tumor suppressor genes that occur in ] cells are passed along to ], and increase the likelihood for cancer diagnoses in subsequent generations. Members of these families have increased incidence and decreased latency of multiple tumors. The tumor types are typical for each type of tumor suppressor gene mutation, with some mutations causing particular cancers, and other mutations causing others. The mode of inheritance of mutant tumor suppressors is that an affected member inherits a defective copy from one parent, and a normal copy from the other. For instance, individuals who inherit one mutant '']'' allele (and are therefore ] for mutated ''p53'') can develop ] and ], known as ]. Other inherited tumor suppressor gene syndromes include '']'' mutations, linked to ], and '']'' gene mutations, linked to ]. Adenopolyposis colon cancer is associated with thousands of polyps in colon while young, leading to ] at a relatively early age. Finally, inherited mutations in '']'' and '']'' lead to early onset of ]. | |||
| {{Main|Cancer epigenetics}} | |||
| ] | |||
| Development of cancer was proposed in 1971 to depend on at least two mutational events. In what became known as the ] ], an inherited, germ-line mutation in a ] would only cause cancer if another mutation event occurred later in the organism's life, inactivating the other ] of that ].<ref>{{cite journal |author=Knudson A |title=Mutation and cancer: statistical study of retinoblastoma |journal=] |volume=68 |issue=4 |pages=820–3 |year=1971 |pmid=5279523 |doi=10.1073/pnas.68.4.820}}</ref> | |||
| The classical view of cancer is a set of diseases driven by progressive ] ] that include mutations in tumor-suppressor genes and ]s, and in ] abnormalities. A role for ] was identified in the early 21st century.<ref>{{cite journal |vauthors=Baylin SB, Ohm JE |s2cid=2514545 |title=Epigenetic gene silencing in cancer – a mechanism for early oncogenic pathway addiction? |journal=Nature Reviews. Cancer |volume=6 |issue=2 |pages=107–16 |date=February 2006 |pmid=16491070 |doi=10.1038/nrc1799}}</ref> | |||
| Usually, oncogenes are ], as they contain ]s, while mutated tumor suppressors are ], as they contain ]s. Each cell has two copies of the same gene, one from each parent, and under most cases gain of function mutations in just one copy of a particular proto-oncogene is enough to make that gene a true oncogene. On the other hand, loss of function mutations need to happen in both copies of a tumor suppressor gene to render that gene completely non-functional. However, cases exist in which one mutated copy of a ] can render the other, ] copy non-functional. This phenomenon is called the ''dominant negative effect'' and is observed in many p53 mutations. | |||
| ] alterations are functionally relevant modifications to the genome that do not change the nucleotide sequence. Examples of such modifications are changes in ] (hypermethylation and hypomethylation), ]<ref>{{cite journal |vauthors=Kanwal R, Gupta S |title=Epigenetic modifications in cancer |journal=Clinical Genetics |volume=81 |issue=4 |pages=303–11 |date=April 2012 |pmid=22082348 |pmc=3590802 |doi=10.1111/j.1399-0004.2011.01809.x}}</ref> and changes in chromosomal architecture (caused by inappropriate expression of proteins such as ] or ]).<ref>{{cite journal |vauthors=Baldassarre G, Battista S, Belletti B, Thakur S, Pentimalli F, Trapasso F, Fedele M, Pierantoni G, Croce CM, Fusco A |title=Negative regulation of BRCA1 gene expression by HMGA1 proteins accounts for the reduced BRCA1 protein levels in sporadic breast carcinoma |journal=Molecular and Cellular Biology |volume=23 |issue=7 |pages=2225–38 |date=April 2003 |pmid=12640109 |pmc=150734 |doi=10.1128/MCB.23.7.2225-2238.2003}}/</ref> Each of these alterations regulates gene expression without altering the underlying ]. These changes may remain through ]s, endure for multiple generations, and can be considered as equivalent to mutations. | |||
| Knudson’s two hit model has recently been challenged by several investigators. Inactivation of one allele of some tumor suppressor genes is sufficient to cause tumors. This phenomenon is called ] and has been demonstrated by a number of experimental approaches. Tumors caused by ] usually have a later age of onset when compared with those by a two hit process.<ref name="Fodde-Haploinsufficiency">{{cite journal | author = Fodde R, Smits R | title = Cancer biology. A matter of dosage | journal = Science | volume = 298 | issue = 5594 | pages = 761–3 | year = 2002 | pmid = 12399571 | doi = 10.1126/science.1077707}}</ref> | |||
| Epigenetic alterations occur frequently in cancers. As an example, one study listed protein coding genes that were frequently altered in their ] in association with colon cancer. These included 147 hypermethylated and 27 hypomethylated genes. Of the hypermethylated genes, 10 were hypermethylated in 100% of colon cancers and many others were hypermethylated in more than 50% of colon cancers.<ref name="Sch">{{cite journal |vauthors=Schnekenburger M, Diederich M |title=Epigenetics Offer New Horizons for Colorectal Cancer Prevention |journal=Current Colorectal Cancer Reports |volume=8 |issue=1 |pages=66–81 |date=March 2012 |pmid=22389639 |pmc=3277709 |doi=10.1007/s11888-011-0116-z}}</ref> | |||
| === Cancer cell biology === | |||
| ] | |||
| While epigenetic alterations are found in cancers, the epigenetic alterations in DNA repair genes, causing reduced expression of DNA repair proteins, may be of particular importance. Such alterations may occur early in progression to cancer and are a possible cause of the ] instability characteristic of cancers.<ref>{{cite journal |vauthors=Jacinto FV, Esteller M |title=Mutator pathways unleashed by epigenetic silencing in human cancer |journal=Mutagenesis |volume=22 |issue=4 |pages=247–53 |date=July 2007 |pmid=17412712 |doi=10.1093/mutage/gem009|doi-access=free }}</ref><ref>{{cite journal |vauthors=Lahtz C, Pfeifer GP |title=Epigenetic changes of DNA repair genes in cancer |journal=Journal of Molecular Cell Biology |volume=3 |issue=1 |pages=51–8 |date=February 2011 |pmid=21278452 |pmc=3030973 |doi=10.1093/jmcb/mjq053}}</ref><ref>{{cite journal |vauthors=Bernstein C, Nfonsam V, Prasad AR, Bernstein H |title=Epigenetic field defects in progression to cancer |journal=World Journal of Gastrointestinal Oncology |volume=5 |issue=3 |pages=43–49 |date=March 2013 |pmid=23671730 |pmc=3648662 |doi=10.4251/wjgo.v5.i3.43 |doi-access=free }}</ref> | |||
| Often, the multiple genetic changes which result in cancer may take many years to accumulate. During this time, the biological behavior of the pre-malignant cells slowly change from the properties of normal cells to cancer-like properties. Pre-malignant tissue can have a distinctive appearance under the ]. Among the distinguishing traits are an increased number of dividing cells, variation in ] size and shape, variation in cell size and shape, loss of specialized cell features, and loss of normal tissue organization. ] is an abnormal type of excessive cell proliferation characterized by loss of normal tissue arrangement and cell structure in pre-malignant cells. These early neoplastic changes must be distinguished from hyperplasia, a reversible increase in cell division caused by an external stimulus, such as a hormonal imbalance or chronic irritation. | |||
| Reduced expression of DNA repair genes disrupts DNA repair. This is shown in the figure at the 4th level from the top. (In the figure, red wording indicates the central role of DNA damage and defects in DNA repair in progression to cancer.) When DNA repair is deficient DNA damage remains in cells at a higher than usual level (5th level) and causes increased frequencies of mutation and/or epimutation (6th level). Mutation rates increase substantially in cells defective in ]<ref>{{cite journal |vauthors=Narayanan L, Fritzell JA, Baker SM, Liskay RM, Glazer PM |title=Elevated levels of mutation in multiple tissues of mice deficient in the DNA mismatch repair gene Pms2 |journal=Proceedings of the National Academy of Sciences of the United States of America |volume=94 |issue=7 |pages=3122–27 |date=April 1997 |pmid=9096356 |pmc=20332 |doi=10.1073/pnas.94.7.3122|bibcode=1997PNAS...94.3122N |doi-access=free }}</ref><ref>{{cite journal |vauthors=Hegan DC, Narayanan L, Jirik FR, Edelmann W, Liskay RM, Glazer PM |title=Differing patterns of genetic instability in mice deficient in the mismatch repair genes Pms2, Mlh1, Msh2, Msh3 and Msh6 |journal=Carcinogenesis |volume=27 |issue=12 |pages=2402–08 |date=December 2006 |pmid=16728433 |pmc=2612936 |doi=10.1093/carcin/bgl079}}</ref> or in ]al repair (HRR).<ref>{{cite journal |vauthors=Tutt AN, van Oostrom CT, Ross GM, van Steeg H, Ashworth A |title=Disruption of Brca2 increases the spontaneous mutation rate in vivo: synergism with ionizing radiation |journal=EMBO Reports |volume=3 |issue=3 |pages=255–60 |date=March 2002 |pmid=11850397 |pmc=1084010 |doi=10.1093/embo-reports/kvf037}}</ref> Chromosomal rearrangements and aneuploidy also increase in HRR defective cells.<ref>{{cite journal |vauthors=German J |title=Bloom's syndrome. I. Genetical and clinical observations in the first twenty-seven patients |journal=American Journal of Human Genetics |volume=21 |issue=2 |pages=196–227 |date=March 1969 |pmid=5770175 |pmc=1706430}}</ref> | |||
| The most severe cases of dysplasia are referred to as "]." In Latin, the term "in situ" means "in place", so carcinoma in situ refers to an uncontrolled growth of cells that remains in the original location and has not shown invasion into other tissues. Nevertheless, carcinoma in situ may develop into an invasive malignancy and is usually removed surgically, if possible. | |||
| Higher levels of DNA damage cause increased mutation (right side of figure) and increased epimutation. During repair of DNA double strand breaks, or repair of other DNA damage, incompletely cleared repair sites can cause epigenetic gene silencing.<ref>{{cite journal |vauthors=O'Hagan HM, Mohammad HP, Baylin SB |title=Double strand breaks can initiate gene silencing and SIRT1-dependent onset of DNA methylation in an exogenous promoter CpG island |journal=PLOS Genetics |volume=4 |issue=8 |pages=e1000155 |date=August 2008 |pmid=18704159 |pmc=2491723 |doi=10.1371/journal.pgen.1000155 | veditors = Lee JT |doi-access=free }}</ref><ref>{{cite journal |vauthors=Cuozzo C, Porcellini A, Angrisano T, Morano A, Lee B, Di Pardo A, Messina S, Iuliano R, Fusco A, Santillo MR, Muller MT, Chiariotti L, Gottesman ME, Avvedimento EV |title=DNA damage, homology-directed repair, and DNA methylation |journal=PLOS Genetics |volume=3 |issue=7 |pages=e110 |date=July 2007 |pmid=17616978 |pmc=1913100 |doi=10.1371/journal.pgen.0030110 |doi-access=free }}</ref> | |||
| ==== Clonal evolution ==== | |||
| Deficient expression of DNA repair proteins due to an inherited mutation can increase cancer risks. Individuals with an inherited impairment in any of 34 DNA repair genes (see article ]) have increased cancer risk, with some defects ensuring a 100% lifetime chance of cancer (e.g. p53 mutations).<ref>{{cite journal |vauthors=Malkin D |title=Li-fraumeni syndrome |journal=Genes & Cancer |volume=2 |issue=4 |pages=475–84 |date=April 2011 |pmid=21779515 |pmc=3135649 |doi=10.1177/1947601911413466}}</ref> Germ line DNA repair mutations are noted on the figure's left side. However, such ] mutations (which cause highly penetrant cancer syndromes) are the cause of only about 1 percent of cancers.<ref>{{cite journal |vauthors=Fearon ER |title=Human cancer syndromes: clues to the origin and nature of cancer |journal=Science |volume=278 |issue=5340 |pages=1043–50 |date=November 1997 |pmid=9353177 |doi=10.1126/science.278.5340.1043|bibcode=1997Sci...278.1043F }}</ref> | |||
| {{main | Somatic evolution in cancer}} | |||
| The process by which normal tissue becomes malignant is a process of ] within the body<ref>Nowell PC: The clonal evolution of tumor cell populations. Science 1976, 194(4260):23-28.</ref>. Millions of years of biological ] insure that the cellular metabolic changes that enable cancer to grow occur only very rarely. Most changes in cellular metabolism that allow cells to grow in a disorderly fashion lead to cell death. Cancer cells undergo a process of ], in that the few cells with new genetic changes that enhance their survival or reproduction continue to multiply, and soon come to dominate the growing tumor, as cells with less favorable genetic change are out-competed<ref>Merlo LM, Pepper JW, Reid BJ, Maley CC: Cancer as an evolutionary and ecological process. Nat Rev Cancer 2006, 6(12):924-935.</ref>. This process is called ]. Tumors often continue to evolve in response to chemotherapy treatments, and on occasion aberrant cells may ] to particular anti-cancer pharmaceuticals. | |||
| In sporadic cancers, deficiencies in DNA repair are occasionally caused by a mutation in a DNA repair gene but are much more frequently caused by epigenetic alterations that reduce or silence expression of DNA repair genes. This is indicated in the figure at the 3rd level. Many studies of heavy metal-induced carcinogenesis show that such heavy metals cause a reduction in expression of DNA repair enzymes, some through epigenetic mechanisms. DNA repair inhibition is proposed to be a predominant mechanism in heavy metal-induced carcinogenicity. In addition, frequent epigenetic alterations of the DNA sequences code for small RNAs called ]s (or miRNAs). miRNAs do not code for proteins, but can "target" protein-coding genes and reduce their expression. | |||
| ==== Biological properties of cancer cells ==== | |||
| Cancers usually arise from an assemblage of mutations and epimutations that confer a selective advantage leading to clonal expansion (see ]). Mutations, however, may not be as frequent in cancers as epigenetic alterations. An average cancer of the breast or colon can have about 60 to 70 protein-altering mutations, of which about three or four may be "driver" mutations and the remaining ones may be "passenger" mutations.<ref>{{cite journal |vauthors=Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW |title=Cancer genome landscapes |journal=Science |volume=339 |issue=6127 |pages=1546–58 |date=March 2013 |pmid=23539594 |pmc=3749880 |doi=10.1126/science.1235122|bibcode=2013Sci...339.1546V }}</ref> | |||
| In a 2000 article by Hanahan and ], the biological properties of malignant tumor cells were summarized as follows:<ref name="pmid10647931">{{cite journal |author=Hanahan D, Weinberg RA |title=The hallmarks of cancer |journal=Cell |volume=100 |issue=1 |pages=57–70 |year=2000 |pmid=10647931|doi=10.1016/S0092-8674(00)81683-9}}</ref> | |||
| * Acquisition of self-sufficiency in ], leading to unchecked growth. | |||
| === Metastasis === | |||
| * Loss of sensitivity to anti-growth signals, also leading to unchecked growth. | |||
| {{Main|Metastasis}} | |||
| * Loss of capacity for ], in order to allow growth despite genetic errors and external anti-growth signals. | |||
| ] is the spread of cancer to other locations in the body. The dispersed tumors are called metastatic tumors, while the original is called the primary tumor. Almost all cancers can metastasize.<ref name=metastasis/> Most cancer deaths are due to cancer that has metastasized.<ref name="What is Metastasized Cancer"/> | |||
| * Loss of capacity for ], leading to limitless replicative potential (immortality) | |||
| * Acquisition of sustained ], allowing the tumor to grow beyond the limitations of passive nutrient diffusion. | |||
| Metastasis is common in the late stages of cancer and it can occur via the blood or the ] or both. The typical steps in metastasis are local ], ] into the blood or lymph, circulation through the body, ] into the new tissue, proliferation and ]. Different types of cancers tend to metastasize to particular organs, but overall the most common places for metastases to occur are the ]s, ], brain and the ]s.<ref name=metastasis/> | |||
| * Acquisition of ability to invade neighbouring ], the defining property of invasive carcinoma. | |||
| * Acquisition of ability to build ] at distant sites, the classical property of malignant tumors (carcinomas or others). | |||
| === Metabolism === | |||
| {{Main|Tumor metabolome}} | |||
| The completion of these multiple steps would be a very rare event without : | |||
| * Loss of capacity to repair genetic errors, leading to an increased ] rate (genomic instability), thus accelerating all the other changes. | |||
| Normal cells typically generate only about 30% of energy from ],<ref name="pmid23226794">{{cite journal | vauthors = Zheng J | title=Energy metabolism of cancer: Glycolysis versus oxidative phosphorylation (Review) | journal=] | volume=4 | issue=6 | pages=1151–1157 | year=2012 | doi = 10.3892/ol.2012.928 | pmc= 3506713 | pmid=23226794}}</ref> whereas most cancers rely on glycolysis for energy production (]).<ref name="pmid20181022">{{cite journal | vauthors = Seyfried TN, Shelton LM | title=Cancer as a metabolic disease | journal=Nutrition & Metabolism | volume=7 | page=7 | year=2010 | doi = 10.1186/1743-7075-7-7 | pmc= 2845135 | pmid=20181022 | doi-access=free }}</ref><ref name="pmid31781842">{{cite journal | vauthors = Weiss JM | title=The promise and peril of targeting cell metabolism for cancer therapy | journal=] | volume=69 | issue=2 | pages=255–261 | year=2020 | doi = 10.1007/s00262-019-02432-7 | pmc= 7004869 | pmid=31781842}}</ref> But a minority of cancer types rely on ] as the primary energy source, including ], ], and ].<ref name="pmid33028168">{{cite journal | vauthors = Farhadi P, Yarani R, Dokaneheifard S, Mansouri K | title = The emerging role of targeting cancer metabolism for cancer therapy | journal = ] | volume = 42 | issue = 10 | page = 1010428320965284 | year = 2020 | doi = 10.1177/1010428320965284 | pmid = 33028168 | s2cid = 222214285 | doi-access = free }}</ref> Even in these cases, however, the use of glycolysis as an energy source rarely exceeds 60%.<ref name=pmid23226794/> A few cancers use ] as the major energy source, partly because it provides nitrogen required for ] (DNA, RNA) synthesis.<ref name="pmid26771115">{{cite journal | vauthors=Pavlova NN, Thompson CB | title=The Emerging Hallmarks of Cancer Metabolism | journal=] | volume=23 | issue=1 | pages=27–47 | year=2016 | doi = 10.1016/j.cmet.2015.12.006 | pmc= 4715268 | pmid=26771115}}</ref> ]s often use oxidative phosphorylation or glutamine as a primary energy source.<ref name="pmid32670883">{{cite journal | vauthors=Yadav UP, Singh T, Kumar P, Mehta K | title=Metabolic Adaptations in Cancer Stem Cells | journal=] | volume=10 | page=1010 | year=2020 | doi = 10.3389/fonc.2020.01010 | pmc= 7330710 | pmid=32670883| doi-access=free }}</ref> | |||
| These biological changes are classical in ]s; other malignant tumor may not need all to achieve them all. For example, tissue invasion and displacement to distant sites are normal properties of ]; these steps are not needed in the development of ]. The different steps do not necessarily represent individual mutations. For example, inactivation of a single gene, coding for the ] protein, will cause genomic instability, evasion of apoptosis and increased angiogenesis. Not all the cancer cells are dividing. Rather, a subset of the cells in a tumor, called ]s, replicate themselves and generate differentiated cells.<ref>{{cite journal |author=Cho RW, Clarke MF |title=Recent advances in cancer stem cells |journal=Curr. Opin. Genet. Dev. |volume=18 |issue=1 |pages=48–53 |year=2008 |month=February |pmid=18356041 |doi=10.1016/j.gde.2008.01.017}}</ref> | |||
| == Diagnosis == | |||
| ] showing lung cancer in the left lung]] | |||
| Most cancers are initially recognized either because of the appearance of signs or symptoms or through ].<ref>{{Cite web |title=Cancer Screening Guidelines {{!}} Detecting Cancer Early |url=https://www.cancer.org/healthy/find-cancer-early/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html |access-date=24 May 2022 |publisher=American Cancer Society|date=14 March 2022 |language=en}}</ref> Neither of these leads to a definitive diagnosis, which requires the examination of a tissue sample by a ].<ref name="HollandFrei6">{{cite book | chapter=Role of the Surgical Pathologist in the Diagnosis and Management of the Cancer Patient | vauthors = Connolly JL, Schnitt SJ, Wang HH, Longtine JA, Dvorak A, Dvorak HF |author6-link=Harold F. Dvorak | veditors = Holland JF, Frei E, Kufe DW |editor1-link=James F. Holland |editor2-link=Emil Frei |title=Holland-Frei Cancer Medicine |edition=6 |location=Hamilton (ON) |publisher=BC Decker |year=2003 |isbn=978-1-55009-213-4 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK13237/ |url=https://www.ncbi.nlm.nih.gov/books/NBK12354/}}</ref> People with suspected cancer are investigated with ]s. These commonly include ]s, ], (]) ]s and ]. | |||
| The tissue ] from the biopsy indicates the type of cell that is proliferating, its ], genetic abnormalities and other features. Together, this information is useful to evaluate the ] and to choose the best treatment. | |||
| ] and ] are other types of tissue tests. These tests provide information about molecular changes (such as ]s, ]s and numerical ] changes) and may thus also indicate the prognosis and best treatment. | |||
| Cancer diagnosis can cause psychological distress and psychosocial interventions, such as talking therapy, may help people with this.<ref>{{cite journal | vauthors = Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M | title = Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients | journal = The Cochrane Database of Systematic Reviews | volume = 11 | pages = CD007064 | date = November 2012 | issue = 11 | pmid = 23152241 | pmc = 6457819 | doi = 10.1002/14651858.cd007064.pub2 }}</ref> Some people choose to disclose the diagnosis widely; others prefer to keep the information private, especially shortly after the diagnosis, or to disclose it only partially or to selected people.<ref>{{Cite journal | vauthors = Pearson C |date=10 January 2024 |title=Why Some People Keep Serious Illnesses Private |url=https://www.nytimes.com/2024/01/10/well/family/hidden-cancer-lloyd-austin.html |journal=The New York Times}}</ref> | |||
| == Classification == | |||
| {{further|List of cancer types|List of oncology-related terms}} | |||
| ]s, with typical ] features shown, although they vary substantially from case to case.]] | |||
| Cancers are classified by the ] that the tumor cells resemble and is therefore presumed to be the origin of the tumor. These types include: | |||
| * ]: Cancers derived from ] cells. This group includes many of the most common cancers and include nearly all those in the ], ], ], ] and ]. Most of these are of the ] type, which means that the cancer has ]-like differentiation. | |||
| * ]: Cancers arising from ] (i.e. ], ], fat, ]), each of which develops from cells originating in ] cells outside the ]. | |||
| * ] and ]: These two classes arise from hematopoietic (blood-forming) cells that leave the marrow and tend to mature in the ]s and blood, respectively.<ref>{{cite book | vauthors = Varricchio C | title = A cancer source book for nurses |publisher=Jones and Bartlett Publishers |location=Boston |year=2004 |page=229 |isbn=978-0-7637-3276-9 |url={{google books |plainurl=y |id=jkqdgZcF9qcC |page=229}}}}</ref> | |||
| * ]: Cancers derived from ] cells, most often presenting in the ] or the ] (] and ], respectively). | |||
| * ]: Cancers derived from immature "precursor" cells or embryonic tissue. | |||
| Cancers are usually named using ''-carcinoma'', ''-sarcoma'' or ''-blastoma'' as a suffix, with the Latin or Greek word for the ] or tissue of origin as the root. For example, cancers of the liver ] arising from malignant epithelial cells is called '']'', while a malignancy arising from primitive liver precursor cells is called a ] and a cancer arising from fat cells is called a '']''. For some common cancers, the English organ name is used. For example, the most common type of breast cancer is called '']''. Here, the adjective ''ductal'' refers to the appearance of cancer under the microscope, which suggests that it has originated in the milk ducts. | |||
| ]s (which are not cancers) are named using ''-oma'' as a suffix with the organ name as the root. For example, a benign tumor of smooth muscle cells is called a '']'' (the common name of this frequently occurring benign tumor in the uterus is '']''). Confusingly, some types of cancer use the ''-noma'' suffix, examples including ] and ]. | |||
| Some types of cancer are named for the size and shape of the cells under a microscope, such as giant cell carcinoma, ] and ]. | |||
| <gallery> | |||
| File:Breast cancer gross appearance.jpg|An invasive ] of the breast (pale area at the center) surrounded by spikes of whitish scar tissue and yellow fatty tissue | |||
| File:Colon cancer 2.jpg|An invasive ] (top center) in a ] specimen | |||
| File:Lung cancer.jpg|A ] (the whitish tumor) near the ] in a lung specimen | |||
| File:BreastCancer.jpg|A large invasive ] in a ] specimen | |||
| File:Histopathology of squamous-cell carcinoma.png|] with typical histopathology features. | |||
| File:Histopathology of small cell carcinoma, annotated.png|Histopathology of ], with typical findings.<ref>Image by Mikael Häggström, MD. Source for findings: {{cite web|url=https://www.pathologyoutlines.com/topic/lungtumorsmallcell.html|title=Lung – Small cell carcinoma|website=Pathology Outlines| vauthors = Underwood CI, Glass C }} Last author update: 20 September 2022</ref> | |||
| </gallery> | |||
| == Prevention == | == Prevention == | ||
| {{Main|Cancer prevention}} | |||
| Cancer prevention is defined as active measures to decrease the incidence of cancer. This can be accomplished by avoiding ]s or altering their ], pursuing a lifestyle or diet that modifies cancer-causing factors and/or medical intervention (], treatment of pre-malignant lesions). The ] concept of "prevention" is usually defined as either ], for people who have not been diagnosed with a particular disease, or ], aimed at reducing recurrence or complications of a previously diagnosed illness. | |||
| ] | |||
| ]s attributable to 11 Level 2 risk factors globally in 2019.<ref name="10.1016/S0140-6736(22)01438-6"/>]] | |||
| ] that show associations between risk factors and specific cancers mostly serve to generate hypotheses about potential interventions that could reduce cancer incidence or ]. ]s then test whether hypotheses generated by epidemiological trials and laboratory research actually result in reduced cancer incidence and mortality. In many cases, findings from observational ] studies are not confirmed by randomized controlled trials. | |||
| Cancer prevention is defined as active measures to decrease cancer risk.<ref>{{cite web |title=Cancer prevention: 7 steps to reduce your risk |publisher=] |url=http://www.mayoclinic.com/health/cancer-prevention/CA00024 |date=27 September 2008 |access-date=30 January 2010 |url-status=live |archive-url=https://web.archive.org/web/20100208082208/http://www.mayoclinic.com/health/cancer-prevention/CA00024 |archive-date=8 February 2010}}</ref> The vast majority of cancer cases are due to environmental risk factors. Many of these environmental factors are controllable lifestyle choices. Thus, cancer is generally preventable.<ref name=Danaei>{{cite journal |vauthors=Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M |s2cid=17354479 |title=Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors |journal=Lancet |volume=366 |issue=9499 |pages=1784–93 |date=November 2005 |pmid=16298215 |doi=10.1016/S0140-6736(05)67725-2|doi-access=free }}</ref> Between 70% and 90% of common cancers are due to environmental factors and therefore potentially preventable.<ref>{{cite journal |vauthors=Wu S, Powers S, Zhu W, Hannun YA |title=Substantial contribution of extrinsic risk factors to cancer development |journal=Nature |volume=529 |issue=7584 |pages=43–7 |date=January 2016 |pmid=26675728 |pmc=4836858 |doi=10.1038/nature16166 |bibcode=2016Natur.529...43W}}</ref> | |||
| About a third of the twelve most common cancers worldwide are due to nine potentially modifiable risk factors. Men with cancer are twice as likely as women to have a modifiable risk factor for their disease. The nine risk factors are ], excessive ] use, diet low in ] and ], limited ], ] infection (unsafe sex), urban ], domestic use of solid fuels, and contaminated injections (hepatitis B and C).<ref>{{cite journal |author=Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M |title=Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors |journal=Lancet |volume=366 |issue=9499 |pages=1784–93 |year=2005 |pmid=16298215 |doi=10.1016/S0140-6736(05)67725-2| url=http://www.thelancet.com/journals/lancet/article/PIIS0140673605677252/fulltext}}</ref> | |||
| Greater than 30% of cancer deaths could be prevented by avoiding risk factors including: tobacco, ]/], poor diet, ], ], ]s and air pollution.<ref name="Cancer Cancer">{{cite web |url=https://www.who.int/mediacentre/factsheets/fs297/en/ |title=Cancer |website=World Health Organization |access-date=9 January 2011 |url-status=live |archive-url=https://web.archive.org/web/20101229092321/http://www.who.int/mediacentre/factsheets/fs297/en/ |archive-date=29 December 2010}}</ref> Further, poverty could be considered as an indirect risk factor in human cancers.<ref>{{cite journal | vauthors = Heidary F, Rahimi A, Gharebaghi R | title = Poverty as a risk factor in human cancers | journal = Iranian Journal of Public Health | volume = 42 | issue = 3 | pages = 341–343 | date = 2013 | pmid = 23641414 | pmc = 3633807 }}</ref> Not all environmental causes are controllable, such as naturally occurring ] and cancers caused through hereditary ] and thus are not preventable via personal behavior. | |||
| ===Modifiable ("lifestyle") risk factors=== | |||
| In 2019, ~44% of all cancer deaths – or ~4.5 M deaths or ~105 million lost ]s – were ]<!--(causal-contributing factors)-->, led by ], ] and ], according to a ] ].<ref name="10.1016/S0140-6736(22)01438-6">{{cite journal | vauthors = Tran KB, Lang JJ, Compton K, Xu R, Acheson AR, Henrikson HJ, etal | title = The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019 | language = English | journal = Lancet | volume = 400 | issue = 10352 | pages = 563–591 | date = August 2022 | pmid = 35988567 | pmc = 9395583 | doi = 10.1016/S0140-6736(22)01438-6 | doi-access = free }}</ref> | |||
| Examples of modifiable cancer risk factors include ] consumption (associated with increased risk of oral, esophageal, breast, and other cancers), smoking (although 20% of women with lung cancer have never smoked, versus 10% of men<ref>{{cite web | title= Lung Cancer in American Women: Facts | url=http://www.nationallungcancerpartnership.org/page.cfm?l=factsWomen | accessdate=2007-01-19 }}</ref>), physical inactivity (associated with increased risk of colon, breast, and possibly other cancers), and being ] (associated with colon, breast, endometrial, and possibly other cancers). Based on epidemiologic evidence, it is now thought that avoiding excessive alcohol consumption may contribute to reductions in risk of certain cancers; however, compared with tobacco exposure, the magnitude of effect is modest or small and the strength of evidence is often weaker. Other lifestyle and environmental factors known to affect cancer risk (either beneficially or detrimentally) include certain sexually transmitted diseases, the use of exogenous hormones, exposure to ] and ] radiation, and certain occupational and chemical exposures. | |||
| === Dietary === | |||
| Every year, at least 200,000 people die worldwide from cancer related to their workplace.<ref name=WHO_occup>{{cite press release |title=WHO calls for prevention of cancer through healthy workplaces |publisher=World Health Organization |date=2007-04-27 |url=http://www.who.int/mediacentre/news/notes/2007/np19/en/index.html |accessdate=2007-10-13}} </ref> Millions of workers run the risk of developing cancers such as ] and ] from inhaling asbestos fibers and tobacco smoke, or ] from exposure to ] at their workplaces.<ref name=WHO_occup/> Currently, most cancer deaths caused by occupational risk factors occur in the developed world.<ref name=WHO_occup/> It is estimated that approximately 20,000 cancer deaths and 40,000 new cases of cancer each year in the U.S. are attributable to occupation.<ref>{{cite web|url=http://www.cdc.gov/niosh/topics/cancer/|title=National Institute for Occupational Safety and Health- Occupational Cancer |accessdate=2007-10-13|publisher=United States National Institute for Occupational Safety and Health}}</ref> | |||
| {{Main|Diet and cancer}} | |||
| While many dietary recommendations have been proposed to reduce cancer risks, the evidence to support them is not definitive.<ref name=Kushi2012/><ref name=Diet11>{{cite journal |vauthors=Wicki A, Hagmann J |title=Diet and cancer |journal=] |volume=141 |pages=w13250 |date=September 2011 |pmid=21904992 |doi=10.4414/smw.2011.13250|doi-access=free }}</ref> The primary dietary factors that increase risk are ] and alcohol consumption. Diets low in fruits and vegetables and high in red meat have been implicated but reviews and meta-analyses do not come to a consistent conclusion.<ref name="pmid22202045">{{cite journal |vauthors=Cappellani A, Di Vita M, Zanghi A, Cavallaro A, Piccolo G, Veroux M, Berretta M, Malaguarnera M, Canzonieri V, Lo Menzo E |title=Diet, obesity and breast cancer: an update |journal=Frontiers in Bioscience |volume=4 |pages=90–108 |date=January 2012 |issue=1 |pmid=22202045 |doi=10.2741/253}}</ref><ref name="pmid21119663">{{cite journal |vauthors=Key TJ |title=Fruit and vegetables and cancer risk |journal=British Journal of Cancer |volume=104 |issue=1 |pages=6–11 |date=January 2011 |pmid=21119663 |pmc=3039795 |doi=10.1038/sj.bjc.6606032}}</ref> A 2014 meta-analysis found no relationship between fruits and vegetables and cancer.<ref>{{cite journal |vauthors=Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB |title=Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies |journal=BMJ |volume=349 |pages=g4490 |date=July 2014 |pmid=25073782 |pmc=4115152 |doi=10.1136/bmj.g4490}}</ref> Coffee is associated with a reduced risk of ].<ref name="pmid17484871">{{cite journal |vauthors=Larsson SC, Wolk A |title=Coffee consumption and risk of liver cancer: a meta-analysis |journal=Gastroenterology |volume=132 |issue=5 |pages=1740–5 |date=May 2007 |pmid=17484871 |doi=10.1053/j.gastro.2007.03.044|url=http://www.gastrojournal.org/article/S0016508507005689/pdf |doi-access=free }}</ref> Studies have linked excessive consumption of ] or ] to an increased risk of breast cancer, ] and ], a phenomenon that could be due to the presence of ] in meats cooked at high temperatures.<ref name="pmid19838915">{{cite journal |vauthors=Zheng W, Lee SA |title=Well-done meat intake, heterocyclic amine exposure, and cancer risk |journal=Nutrition and Cancer |volume=61 |issue=4 |pages=437–46 |year=2009 |pmid=19838915 |pmc=2769029 |doi=10.1080/01635580802710741}}</ref><ref name="pmid20374790">{{cite journal |vauthors=Ferguson LR |title=Meat and cancer |journal=Meat Science |volume=84 |issue=2 |pages=308–13 |date=February 2010 |pmid=20374790 |doi=10.1016/j.meatsci.2009.06.032}}</ref> In 2015 the ] reported that eating ] (e.g., ], ], ], ]) and, to a lesser degree, ] was linked to some cancers.<ref name="WHO-20151026">{{cite news |author=Staff |title=World Health Organization – IARC Monographs evaluate consumption of red meat and processed meat |url=http://www.iarc.fr/en/media-centre/pr/2015/pdfs/pr240_E.pdf |date=26 October 2015 |work=] |access-date=26 October 2015 |url-status=live |archive-url=https://web.archive.org/web/20151026144543/http://www.iarc.fr/en/media-centre/pr/2015/pdfs/pr240_E.pdf |archive-date=26 October 2015}}</ref><ref name="NYT-20151026">{{cite news | vauthors = Hauser C |title=W.H.O. Report Links Some Cancers With Processed or Red Meat |url=https://www.nytimes.com/2015/10/27/health/report-links-some-types-of-cancer-with-processed-or-red-meat.html |date=26 October 2015 |work=] |access-date=26 October 2015 |url-status=live |archive-url=https://web.archive.org/web/20151026173834/http://www.nytimes.com/2015/10/27/health/report-links-some-types-of-cancer-with-processed-or-red-meat.html |archive-date=26 October 2015}}</ref> | |||
| See ] for more on that topic. | |||
| ] for cancer prevention typically include an emphasis on vegetables, fruit, ] and fish and an avoidance of processed and red meat (beef, pork, lamb), ], ] and ].<ref name=Kushi2012/><ref name=Diet11/> | |||
| ===Diet=== | |||
| === Medication === | |||
| {{main|Diet and cancer}} | |||
| Medications can be used to prevent cancer in a few circumstances.<ref>Holland Chp.33</ref> In the general population, ] reduce the risk of ]; however, due to cardiovascular and gastrointestinal side effects, they cause overall harm when used for prevention.<ref name="pmid17339623">{{cite journal |vauthors=Rostom A, Dubé C, Lewin G, Tsertsvadze A, Barrowman N, Code C, Sampson M, Moher D |title=Nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force |journal=Annals of Internal Medicine |volume=146 |issue=5 |pages=376–89 |date=March 2007 |pmid=17339623 |doi=10.7326/0003-4819-146-5-200703060-00010|doi-access=free }}</ref> ] has been found to reduce the risk of death from cancer by about 7%.<ref name="pmid21144578">{{cite journal |vauthors=Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW |s2cid=22950940 |title=Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials |journal=Lancet |volume=377 |issue=9759 |pages=31–41 |date=January 2011 |pmid=21144578 |doi=10.1016/S0140-6736(10)62110-1}}</ref> ]s may decrease the rate of ] formation in people with ]; however, it is associated with the same adverse effects as NSAIDs.<ref name="pmid20594533">{{cite journal |vauthors=Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, Maguire C, Hind D, Tappenden P |title=Chemoprevention of colorectal cancer: systematic review and economic evaluation |journal=Health Technology Assessment |volume=14 |issue=32 |pages=1–206 |date=June 2010 |pmid=20594533 |doi=10.3310/hta14320|doi-access=free }}</ref> Daily use of ] or ] reduce the risk of breast cancer in high-risk women.<ref name="pmid19020189">{{cite journal |vauthors=Thomsen A, Kolesar JM |title=Chemoprevention of breast cancer |journal=American Journal of Health-System Pharmacy |volume=65 |issue=23 |pages=2221–28 |date=December 2008 |pmid=19020189 |doi=10.2146/ajhp070663}}</ref> The benefit versus harm for ] such as ] is not clear.<ref name="pmid18425978">{{cite journal |vauthors=Wilt TJ, MacDonald R, Hagerty K, Schellhammer P, Kramer BS |title=Five-alpha-reductase Inhibitors for prostate cancer prevention |veditors=Wilt TJ |journal=The Cochrane Database of Systematic Reviews |issue=2 |pages=CD007091 |date=April 2008 |pmid=18425978 |doi=10.1002/14651858.CD007091|pmc=11270836 }}</ref> | |||
| The consensus on diet and cancer is that ] increases the risk of developing cancer. Particular dietary practices often explain differences in cancer incidence in different countries (e.g. ] is more common in ], while ] is more common in the United States). Studies have shown that immigrants develop the risk of their new country, often within one generation, suggesting a substantial link between diet and cancer.<ref>{{cite journal |author=Buell P, Dunn JE |title=Cancer mortality among Japanese Issei and Nisei of California |journal=Cancer |volume=18 |issue= |pages=656–64 |year=1965 |pmid=14278899|doi=10.1002/1097-0142(196505)18:5<656::AID-CNCR2820180515>3.0.CO;2-3}}</ref> Whether reducing obesity in a population also reduces cancer incidence is unknown. | |||
| ] supplementation does not appear to be effective at preventing cancer.<ref name="pmid20939459">{{cite journal |title=Vitamins and minerals: not for cancer or cardiovascular prevention |journal=Prescrire International |volume=19 |issue=108 |page=182 |date=August 2010 |pmid=20939459 |url=http://english.prescrire.org/en/81/168/46461/0/2010/ArchiveNewsDetails.aspx?page=2 |url-status=live |archive-url=https://web.archive.org/web/20120525134048/http://english.prescrire.org/en/81/168/46461/0/2010/ArchiveNewsDetails.aspx?page=2 |archive-date=25 May 2012}}</ref> While low blood levels of ] are correlated with increased cancer risk,<ref name="pmid16595781">{{cite journal |vauthors=Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ, Willett WC |title=Prospective study of predictors of vitamin D status and cancer incidence and mortality in men |journal=Journal of the National Cancer Institute |volume=98 |issue=7 |pages=451–59 |date=April 2006 |pmid=16595781 |doi=10.1093/jnci/djj101 |citeseerx=10.1.1.594.1654}}</ref><ref>{{cite web |title=Vitamin D Has Role in Colon Cancer Prevention |url=http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Vitamin_D_Has_Role_in_Colon_Cancer_Prevention.asp |access-date=27 July 2007 |archive-url=https://web.archive.org/web/20061204052746/http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Vitamin_D_Has_Role_in_Colon_Cancer_Prevention.asp |archive-date=4 December 2006 }}</ref><ref>{{cite journal |vauthors=Holick MF |title=Vitamin D, sunlight and cancer connection |journal=Anti-Cancer Agents in Medicinal Chemistry |volume=13 |issue=1 |pages=70–82 |date=January 2013 |pmid=23094923 |doi=10.2174/187152013804487308}}</ref> whether this relationship is causal and vitamin D supplementation is protective is not determined.<ref name="pmid16595770">{{cite journal |vauthors=Schwartz GG, Blot WJ |title=Vitamin D status and cancer incidence and mortality: something new under the sun |journal=Journal of the National Cancer Institute |volume=98 |issue=7 |pages=428–30 |date=April 2006 |pmid=16595770 |doi=10.1093/jnci/djj127|doi-access=free }}</ref><ref name=Futil2014>{{cite journal |vauthors=Bolland MJ, Grey A, Gamble GD, Reid IR |title=The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis |journal=The Lancet. Diabetes & Endocrinology |volume=2 |issue=4 |pages=307–320 |date=April 2014 |pmid=24703049 |doi=10.1016/S2213-8587(13)70212-2}}</ref> One 2014 review found that supplements had no significant effect on cancer risk.<ref name=Futil2014/> Another 2014 review concluded that vitamin D<sub>3</sub> may decrease the risk of death from cancer (one fewer death in 150 people treated over 5 years), but concerns with the quality of the data were noted.<ref>{{cite journal |vauthors=Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Wetterslev J, Simonetti RG, Bjelakovic M, Gluud C |s2cid=205189615 |title=Vitamin D supplementation for prevention of mortality in adults |journal=The Cochrane Database of Systematic Reviews |volume=1 |issue=1 |pages=CD007470 |date=January 2014 |pmid=24414552 |doi=10.1002/14651858.cd007470.pub3|pmc=11285307 }}</ref> | |||
| Despite frequent reports of particular substances (including foods) having a beneficial or detrimental effect on cancer risk, few of these have an established link to cancer. These reports are often based on studies in cultured cell media or animals. Public health recommendations cannot be made on the basis of these studies until they have been validated in an observational (or occasionally a prospective interventional) trial in humans. | |||
| ] supplementation increases lung cancer rates in those who are high risk.<ref name="pmid21738614">{{cite journal | vauthors = Fritz H, Kennedy D, Fergusson D, Fernandes R, Doucette S, Cooley K, Seely A, Sagar S, Wong R, Seely D | title = Vitamin A and retinoid derivatives for lung cancer: a systematic review and meta analysis | journal = PLOS ONE | volume = 6 | issue = 6 | pages = e21107 | year = 2011 | pmid = 21738614 | pmc = 3124481 | doi = 10.1371/journal.pone.0021107 | bibcode = 2011PLoSO...621107F | veditors = Minna JD | doi-access = free }}</ref> ] supplementation is not effective in preventing colon cancer and may increase colon polyps.<ref name="pmid17551129">{{cite journal | vauthors = Cole BF, Baron JA, Sandler RS, Haile RW, Ahnen DJ, Bresalier RS, McKeown-Eyssen G, Summers RW, Rothstein RI, Burke CA, Snover DC, Church TR, Allen JI, Robertson DJ, Beck GJ, Bond JH, Byers T, Mandel JS, Mott LA, Pearson LH, Barry EL, Rees JR, Marcon N, Saibil F, Ueland PM, Greenberg ER | title = Folic acid for the prevention of colorectal adenomas: a randomized clinical trial | journal = JAMA | volume = 297 | issue = 21 | pages = 2351–2359 | date = June 2007 | pmid = 17551129 | doi = 10.1001/jama.297.21.2351 | doi-access = free }}</ref> Selenium supplementation has not been shown to reduce the risk of cancer.<ref>{{cite journal | vauthors = Vinceti M, Filippini T, Del Giovane C, Dennert G, Zwahlen M, Brinkman M, Zeegers MP, Horneber M, D'Amico R, Crespi CM | title = Selenium for preventing cancer | journal = The Cochrane Database of Systematic Reviews | volume = 1 | issue = 1 | pages = CD005195 | date = January 2018 | pmid = 29376219 | pmc = 6491296 | doi = 10.1002/14651858.CD005195.pub4 }}</ref> | |||
| Proposed dietary interventions for primary cancer risk reduction generally gain support from epidemiological association studies. Examples of such studies include reports that reduced meat consumption is associated with decreased risk of colon cancer,<ref name="pmid9663397">{{cite journal |author=Slattery ML, Boucher KM, Caan BJ, Potter JD, Ma KN |title=Eating patterns and risk of colon cancer |journal=Am. J. Epidemiol. |volume=148 |issue=1 |pages=4–16 |year=1998 |pmid=9663397 |doi=}}</ref> | |||
| === Vaccination === | |||
| and reports that consumption of coffee is associated with a reduced risk of liver cancer.<ref name="pmid17484871">{{cite journal |author=Larsson SC, Wolk A |title=Coffee consumption and risk of liver cancer: a meta-analysis |journal=Gastroenterology |volume=132 |issue=5 |pages=1740–5 |year=2007 |pmid=17484871 |doi=10.1053/j.gastro.2007.03.044}}</ref> Studies have linked consumption of grilled meat to an increased risk of ],<ref name="pmid9096659">{{cite journal |author=Ward MH, Sinha R, Heineman EF, ''et al'' |title=Risk of adenocarcinoma of the stomach and esophagus with meat cooking method and doneness preference |journal=Int. J. Cancer |volume=71 |issue=1 |pages=14–9 |year=1997 |pmid=9096659|doi=10.1002/(SICI)1097-0215(19970328)71:1<14::AID-IJC4>3.0.CO;2-6}}</ref> ],<ref name="pmid16140978">{{cite journal |author=Sinha R, Peters U, Cross AJ, ''et al'' |title=Meat, meat cooking methods and preservation, and risk for colorectal adenoma |journal=Cancer Res. |volume=65 |issue=17 |pages=8034–41 |year=2005 |pmid=16140978 |doi=10.1158/0008-5472.CAN-04-3429 |doi_brokendate=2008-06-26}}</ref> ],<ref name="pmid17435448">{{cite journal |author=Steck SE, Gaudet MM, Eng SM, ''et al'' |title=Cooked meat and risk of breast cancer--lifetime versus recent dietary intake |journal=Epidemiology (Cambridge, Mass.) |volume=18 |issue=3 |pages=373–82 |year=2007 |pmid=17435448 |doi=10.1097/01.ede.0000259968.11151.06}}</ref> and ],<ref name="pmid16172241">{{cite journal |author=Anderson KE, Kadlubar FF, Kulldorff M, ''et al'' |title=Dietary intake of heterocyclic amines and benzo(a)pyrene: associations with pancreatic cancer |journal=Cancer Epidemiol. Biomarkers Prev. |volume=14 |issue=9 |pages=2261–5 |year=2005 |pmid=16172241 |doi=10.1158/1055-9965.EPI-04-0514}}</ref> a phenomenon which could be due to the presence of carcinogens such as ] in foods cooked at high temperatures. | |||
| ]s have been developed that prevent infection by some ]ic viruses.<ref name=vacc_facts_nci>{{cite web |url=https://www.cancer.gov/about-cancer/causes-prevention/vaccines-fact-sheet |title=Cancer Vaccine Fact Sheet |publisher=] |date=8 June 2006 |access-date=28 March 2018 }}</ref> ] (] and ]) decrease the risk of developing ].<ref name=vacc_facts_nci/> The ] prevents infection with hepatitis B virus and thus decreases the risk of liver cancer.<ref name=vacc_facts_nci/> The administration of human papillomavirus and hepatitis B vaccinations is recommended where resources allow.<ref name="pmid24176569">{{cite journal |author4-link=Ding-Shinn Chen |vauthors=Lertkhachonsuk AA, Yip CH, Khuhaprema T, Chen DS, Plummer M, Jee SH, Toi M, Wilailak S |title=Cancer prevention in Asia: resource-stratified guidelines from the Asian Oncology Summit 2013 |journal=The Lancet. Oncology |volume=14 |issue=12 |pages=e497–507 |date=November 2013 |pmid=24176569 |doi=10.1016/S1470-2045(13)70350-4|arxiv=cond-mat/0606434 }}</ref> | |||
| A 2005 ] study showed that consumption of a plant-based diet and lifestyle changes resulted in a reduction in cancer markers in a group of men with prostate cancer who were using no conventional treatments at the time.<ref name="Ornish">{{cite journal | author = Ornish D et al. | title = Intensive lifestyle changes may affect the progression of prostate cancer | journal = The Journal of Urology | volume = 174 | issue = 3 | pages = 1065–9; discussion 1069–70 | year = 2005 | pmid = 16094059 | doi = 10.1097/01.ju.0000169487.49018.73}}</ref> | |||
| == Screening == | |||
| These results were amplified by a 2006 study in which over 2,400 women were studied, half randomly assigned to a normal diet, the other half assigned to a diet containing less than 20% calories from fat. The women on the low fat diet were found to have a markedly lower risk of breast cancer recurrence, in the interim report of December, 2006.<ref>{{cite journal |author=Chlebowski RT, Blackburn GL, Thomson CA, ''et al'' |title=Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study |journal=J. Natl. Cancer Inst. |volume=98 |issue=24 |pages=1767–76 |year=2006 |pmid=17179478 |doi=10.1093/jnci/djj494}}</ref> | |||
| {{Main|Cancer screening}} | |||
| Unlike diagnostic efforts prompted by ]s and ]s, cancer screening involves efforts to detect cancer after it has formed, but before any noticeable symptoms appear.<ref name=NIH>{{cite web |url=https://www.cancer.gov/about-cancer/screening/patient-screening-overview-pdq |title=Cancer Screening Overview (PDQ®)–Patient Version |publisher=National Cancer Institute |access-date=28 March 2018 |date=13 January 2010}}</ref> This may involve ], ] or ] or ].<ref name=NIH/> | |||
| Recent studies have also demonstrated potential links between some forms of cancer and high consumption of refined sugars and other simple carbohydrates.<ref>{{cite journal |author=Romieu I, Lazcano-Ponce E, Sanchez-Zamorano LM, Willett W, Hernandez-Avila M |title=Carbohydrates and the risk of breast cancer among Mexican women |journal=Cancer Epidemiol. Biomarkers Prev. |volume=13 |issue=8 |pages=1283–9 |year=2004 |month=August |pmid=15298947 |url=http://cebp.aacrjournals.org/cgi/content/full/13/8/1283}}</ref><ref>{{cite journal | author= Francesca Bravi, Cristina Bosetti, Lorenza Scotti, Renato Talamini, Maurizio Montella, Valerio Ramazzotti, Eva Negri, Silvia Franceschi, and Carlo La Vecchia | title=Food Groups and Renal Cell Carcinoma: A Case-Control Study from Italy | journal=International Journal of Cancer | year=2006 | month=October | volume=355:1991-2002 | url=http://www3.interscience.wiley.com/cgi-bin/abstract/113412400/ABSTRACT | doi=10.1002/ijc.22225). | doi_brokendate=2008-06-26}}</ref><ref>{{cite journal | author= Sun Ha Jee, PhD, MHS; Heechoul Ohrr, MD, PhD; Jae Woong Sull, PhD, MHS; Ji Eun Yun, MPH; Min Ji, MPH; Jonathan M. Samet, MD, MS | title= Fasting Serum Glucose Level and Cancer Risk in Korean Men and Women | journal= Journal of the American Medical Association | volume = 293 No. 2 | doi= 10.1001/jama.293.2.194 | year= 2005 | pages= 194 | pmid= 15644546}}</ref><ref>{{cite journal | author= Dominique S. Michaud, Simin Liu, Edward Giovannucci, Walter C. Willett, Graham A. Colditz, Charles S. Fuchs | title= Dietary Sugar, Glycemic Load, and Pancreatic Cancer Risk in a Prospective Study | journal= Journal of the National Cancer Institute | volume= 94, Num 17| url=http://jnci.oxfordjournals.org/cgi/content/abstract/94/17/1293 | pmid= 12208894 | doi= 10.1093/jnci/94.17.1293 | year= 2002 | pages= 1293}}</ref><ref>{{cite journal | author= Vasundara Venkateswaran, Ahmed Q. Haddad, Neil E. Fleshner, Rong Fan, Linda M. Sugar, Rob Nam, Laurence H. Klotz, Michael Pollak| title=Association of Diet-Induced Hyperinsulinemia With Accelerated Growth of Prostate Cancer (LNCaP) Xenografts | volume= 99, Num 23 |url=http://jnci.oxfordjournals.org/cgi/content/short/99/23/1793| pmid=18042933| doi=10.1093/jnci/djm231| year=2007| journal=JNCI Journal of the National Cancer Institute| pages=1793}}</ref> Although the degree of correlation and the degree of causality is still debated,<ref>Friebe, Richard: '''', Time Magazine, Sep. 17, 2007</ref><ref>Hitti, Miranda: '''', , February 22, 2008</ref><ref>Moynihan, Timothy:'''', MayoClinic.com, retrieved 22 Feb 2008</ref> some organizations have in fact begun to recommend reducing intake of refined sugars and starches as part of their cancer prevention regimens.<ref>'''', American Institute for Cancer Research, retrieved 20 Feb 2008</ref><ref>'''', The Nation's Health: The Official Newspaper of the American Public Health Association, February 2005</ref><ref>{{cite journal |author=Kushi LH, Byers T, Doyle C, ''et al'' |title=American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity |journal=CA Cancer J Clin |volume=56 |issue=5 |pages=254–81; quiz 313–4 |year=2006 |pmid=17005596 |doi=10.3322/canjclin.56.5.254 |url=http://caonline.amcancersoc.org/cgi/content/full/56/5/254 |doi_brokendate=2008-06-26}}</ref><ref>Dummert, Erin RD, CD: '''', The Diet Channel, October 25, 2006</ref> | |||
| ] is not available for many types of cancers. Even when tests are available, they may not be recommended for everyone. '']'' or ''mass screening'' involves screening everyone.<ref name=Wilson>Wilson JMG, Jungner G. (1968) Geneva: ]. Public Health Papers, No. 34.</ref> ''Selective screening'' identifies people who are at higher risk, such as people with a family history.<ref name=Wilson/> Several factors are considered to determine whether the benefits of screening outweigh the risks and the costs of screening.<ref name=NIH/> These factors include: | |||
| In November 2007, the ] (AICR), in conjunction with the ] (WCRF), published ''Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective''', "the most current and comprehensive analysis of the literature on diet, physical activity and cancer".<ref>"" ''dietandcancerreport.org''. Retrieved on August 27, 2008.</ref> The WCRF/AICR Expert Report lists 10 recommendations that people can follow to help reduce their risk of developing cancer, including the following dietary guidelines: (1) reducing intake of foods and drinks that promote weight gain, namely energy-dense foods and sugary drinks, (2) eating mostly foods of plant origin, (3) limiting intake of red meat and avoiding processed meat, (4) limiting consumption of alcoholic beverages, and (5) reducing intake of salt and avoiding mouldy cereals (grains) or pulses (legumes).<ref>"". ''dietandcancerreport.org''. Retrieved on August 27, 2008.</ref><ref>Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. World Cancer Research Fund (2007). ISBN 978-0-9722522-2-5.</ref> | |||
| * Possible harms from the screening test: for example, X-ray images involve exposure to potentially harmful ] | |||
| * The likelihood of the test correctly identifying cancer | |||
| ===Vitamins=== | |||
| * The likelihood that cancer is present: Screening is not normally useful for rare cancers. | |||
| The idea that cancer can be prevented through vitamin supplementation stems from early observations correlating human disease with vitamin deficiency, such as ] with ] deficiency, and ] with ] deficiency. This has largely not been proven to be the case with cancer, and vitamin supplementation is largely not proving effective in preventing cancer. The cancer-fighting components of food are also proving to be more numerous and varied than previously understood, so patients are increasingly being advised to consume fresh, unprocessed fruits and vegetables for maximal health benefits.<ref>The Omnivore's Dilemma, Andrew Pollan</ref> | |||
| * Possible harms from follow-up procedures | |||
| * Whether suitable treatment is available | |||
| ] have shown that low ] status is correlated to increased cancer risk.<ref>{{cite journal |author=Giovannucci E, Liu Y, Rimm EB, ''et al'' |title=Prospective study of predictors of vitamin D status and cancer incidence and mortality in men |journal=J. Natl. Cancer Inst. |volume=98 |issue=7 |pages=451–9 |year=2006 |month=April |pmid=16595781 |doi=10.1093/jnci/djj101}}</ref><ref>{{cite web|url=http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Vitamin_D_Has_Role_in_Colon_Cancer_Prevention.asp|title=Vitamin D Has Role in Colon Cancer Prevention|accessdate=2007-07-27}}</ref> However, the results of such studies need to be treated with caution, as they cannot show whether a correlation between two factors means that one causes the other (''i.e.'' ]).<ref>{{cite journal |author=Schwartz GG, Blot WJ |title=Vitamin D status and cancer incidence and mortality: something new under the sun |journal=J. Natl. Cancer Inst. |volume=98 |issue=7 |pages=428–30 |year=2006 |month=April |pmid=16595770 |doi=10.1093/jnci/djj127 |url=http://jnci.oxfordjournals.org/cgi/content/full/98/7/428}}</ref> The possibility that Vitamin D might protect against cancer has been contrasted with the risk of malignancy from sun exposure. Since exposure to the sun enhances natural human production of vitamin D, some cancer researchers have argued that the potential deleterious malignant effects of sun exposure are far outweighed by the cancer-preventing effects of extra vitamin D synthesis in sun-exposed skin. In 2002, Dr. William B. Grant claimed that 23,800 premature cancer deaths occur in the US annually due to insufficient UVB exposure (apparently via vitamin D deficiency).<ref>{{cite web|url=http://www3.interscience.wiley.com/cgi-bin/abstract/91016211/ABSTRACT?CRETRY=1&SRETRY=0|title=www3.interscience.wiley.com/cgi-bin/abstract/91016211/ABSTRACT?CRETRY=1&SRETRY=0<!--INSERT TITLE-->|accessdate=2007-07-27}}</ref> This is higher than 8,800 deaths occurred from melanoma or squamous cell carcinoma, so the overall effect of sun exposure might be beneficial. Another research group<ref>{{cite web|url=http://cat.inist.fr/?aModele=afficheN&cpsidt=17357586|title=cat.inist.fr/?aModele=afficheN&cpsidt=17357586<!--INSERT TITLE-->|accessdate=2007-07-27}}</ref><ref> | |||
| * Whether early detection improves treatment outcomes | |||
| Grant WB, Garland CF, Holick MF. Comparisons of estimated economic burdens due to insufficient solar ultraviolet irradiance and vitamin D and excess solar UV irradiance for the United States. Photochem Photobiol. 2005 Nov-Dec;81(6):1276-86.</ref> estimates that 50,000–63,000 individuals in the United States and 19,000 - 25,000 in the UK die prematurely from cancer annually due to insufficient vitamin D. | |||
| * Whether cancer will ever need treatment | |||
| * Whether the test is acceptable to the people: If a screening test is too burdensome (for example, extremely painful), then people will refuse to participate.<ref name=Wilson/> | |||
| The case of ] provides an example of the importance of ]. ] studying both diet and serum levels observed that high levels of ], a precursor to ], were associated with a protective effect, reducing the risk of cancer. This effect was particularly strong in ]. This ] led to a series of large randomized ] conducted in both ] and the ] (CARET study) during the 1980s and 1990s. This study provided about 80,000 smokers or former smokers with daily supplements of beta-carotene or ]s. Contrary to expectation, these tests found no benefit of ] supplementation in reducing lung cancer incidence and mortality. In fact, the risk of lung cancer was slightly, but not significantly, ''increased'' by beta-carotene, leading to an early termination of the study.<ref name="CancerTopics-Bcarotene">National Cancer Institute U.S. National Institutes of Health</ref> | |||
| * Cost | |||
| Results reported in the ] (JAMA) in 2007 indicate that folic acid supplementation is not effective in preventing colon cancer, and folate consumers may be more likely to form colon polyps.<ref>{{cite journal |author=Cole BF, Baron JA, Sandler RS, ''et al'' |title=Folic acid for the prevention of colorectal adenomas: a randomized clinical trial |journal=JAMA |volume=297 |issue=21 |pages=2351–9 |year=2007 |pmid=17551129 |doi=10.1001/jama.297.21.2351}}</ref> | |||
| === Recommendations === | |||
| ===Chemoprevention=== | |||
| ==== U.S. Preventive Services Task Force ==== | |||
| {{POV-section|date=June 2008}} | |||
| The ] (USPSTF) issues recommendations for various cancers: | |||
| The concept that medications could be used to prevent cancer is an attractive one, and many high-quality clinical trials support the use of such chemoprevention in defined circumstances. | |||
| * Strongly recommends ] screening in women who are ] and have a ] at least until the age of 65.<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm |title=Screening for Cervical Cancer |year=2003 |website=] |archive-url=https://web.archive.org/web/20101223103447/http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm |archive-date=23 December 2010|access-date=21 December 2010 }}</ref> | |||
| * Recommend that Americans be screened for ] via ] testing, ], or ] starting at age 50 until age 75.<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspscolo.htm |title=Screening for Colorectal Cancer |year=2008 |website=] |archive-url=https://web.archive.org/web/20150207110937/http://www.uspreventiveservicestaskforce.org/uspstf/uspscolo.htm |archive-date=7 February 2015|access-date=21 December 2010 }}</ref> | |||
| Daily use of ], a ] (SERM), typically for 5 years, has been demonstrated to reduce the risk of developing ] in high-risk women by about 50%. A recent study reported that the ] ] has similar benefits to ] in preventing breast cancer in high-risk women, with a more favorable side effect profile.<ref name=STAR-P2>{{cite journal |author=Vogel V, Costantino J, Wickerham D, Cronin W, Cecchini R, Atkins J, Bevers T, Fehrenbacher L, Pajon E, Wade J, Robidoux A, Margolese R, James J, Lippman S, Runowicz C, Ganz P, Reis S, McCaskill-Stevens W, Ford L, Jordan V, Wolmark N |title=Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial |journal=JAMA |volume=295 |issue=23 |pages=2727–41 |year=2006 |pmid=16754727 |doi=10.1001/jama.295.23.joc60074}}</ref> | |||
| * Evidence is insufficient to recommend for or against screening for ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsskca.htm |title=Screening for Skin Cancer |year=2009 |website=] |archive-url=https://web.archive.org/web/20110108054103/http://www.uspreventiveservicestaskforce.org/uspstf/uspsskca.htm |archive-date=8 January 2011|access-date=21 December 2010 }}</ref> ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsoral.htm |title=Screening for Oral Cancer |year=2004 |website=] |archive-url=https://web.archive.org/web/20101024144627/http://www.uspreventiveservicestaskforce.org/uspstf/uspsoral.htm |archive-date=24 October 2010|access-date=21 December 2010 }}</ref> lung cancer,<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspslung.htm |title=Lung Cancer Screening |year=2004 |website=] |archive-url=https://web.archive.org/web/20101104055403/http://www.uspreventiveservicestaskforce.org/uspstf/uspslung.htm |archive-date=4 November 2010|access-date=21 December 2010 }}</ref> or ] in men under 75.<ref name="USPSTFPr08">{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsprca.htm |title=Screening for Prostate Cancer |year=2008 |website=] |archive-url=https://web.archive.org/web/20101231105229/http://www.uspreventiveservicestaskforce.org/uspstf/uspsprca.htm |archive-date=31 December 2010|access-date=21 December 2010 }}</ref> | |||
| * Routine screening is not recommended for ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm |title=Screening for Bladder Cancer |year=2004 |website=] |archive-url=https://web.archive.org/web/20100823053849/http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm |archive-date=23 August 2010|access-date=21 December 2010 }}</ref> ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm |title=Screening for Testicular Cancer |year=2004 |website=] |archive-url=http://arquivo.pt/wayback/20160515181437/http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm |archive-date=15 May 2016|access-date=21 December 2010 }}</ref> ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsovar.htm |title=Screening for Ovarian Cancer |year=2004 |website=] |archive-url=https://web.archive.org/web/20101023221553/http://www.uspreventiveservicestaskforce.org/uspstf/uspsovar.htm |archive-date=23 October 2010|access-date=21 December 2010 }}</ref> ],<ref>{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspspanc.htm |title=Screening for Pancreatic Cancer |year=2004 |website=] |archive-url=https://web.archive.org/web/20101121030321/http://www.uspreventiveservicestaskforce.org/uspstf/uspspanc.htm |archive-date=21 November 2010|access-date=21 December 2010 }}</ref> or ].<ref name="USPSTF-20111007">{{cite journal | vauthors = Chou R, Croswell JM, Dana T, Bougatsos C, Blazina I, Fu R, Gleitsmann K, Koenig HC, Lam C, Maltz A, Rugge JB, Lin K | title = Screening for prostate cancer: a review of the evidence for the U.S. Preventive Services Task Force | journal = Annals of Internal Medicine | volume = 155 | issue = 11 | pages = 762–71 | date = December 2011 | pmid = 21984740 | doi = 10.7326/0003-4819-155-11-201112060-00375 | publisher = ]| doi-access = free}}</ref> | |||
| ] is a SERM like ]; it has been shown (in the STAR trial) to reduce the risk of breast cancer in high-risk women equally as well as tamoxifen. In this trial, which studied almost 20,000 women, ] had fewer side effects than ], though it did permit more ] to form.<ref name=STAR-P2/> | |||
| * Recommends ] for breast cancer screening every two years from ages 50–74, but does not recommend either ] or ].<ref name="USPSTFBr09">{{cite web |url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm |title=Screening for Breast Cancer |year=2009 |website=] |archive-url=https://web.archive.org/web/20130102015424/http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm |archive-date=2 January 2013|access-date=21 December 2010 }}</ref> A 2013 ] concluded that breast cancer screening by mammography had no effect in reducing mortality because of overdiagnosis and overtreatment.<ref>{{cite journal | vauthors = Gøtzsche PC, Jørgensen KJ | title = Screening for breast cancer with mammography | journal = The Cochrane Database of Systematic Reviews | issue = 6 | pages = CD001877 | date = June 2013 | volume = 2013 | pmid = 23737396 | doi = 10.1002/14651858.CD001877.pub5 | pmc = 6464778 }}</ref> | |||
| ], a ], has been shown to lower the risk of prostate cancer, though it seems to mostly prevent low-grade tumors.<ref>{{cite journal |author=Thompson I, Goodman P, Tangen C, Lucia M, Miller G, Ford L, Lieber M, Cespedes R, Atkins J, Lippman S, Carlin S, Ryan A, Szczepanek C, Crowley J, Coltman C |title=The influence of finasteride on the development of prostate cancer |journal=N Engl J Med |volume=349 |issue=3 |pages=215–24 |year=2003 |pmid=12824459 |doi=10.1056/NEJMoa030660}}</ref> | |||
| ==== Japan ==== | |||
| The effect of ] such as ] and ] upon the risk of colon polyps have been studied in ] patients<ref>{{cite journal |author=Hallak A, Alon-Baron L, Shamir R, Moshkowitz M, Bulvik B, Brazowski E, Halpern Z, Arber N |title=Rofecoxib reduces polyp recurrence in familial polyposis |journal=Dig Dis Sci |volume=48 |issue=10 |pages=1998–2002 |year=2003 |pmid=14627347 |doi=10.1023/A:1026130623186}}</ref> | |||
| Screens for ] using ] due to the high incidence there.<ref name=Epi11/> | |||
| and in the general population.<ref>{{cite journal |author=Baron J, Sandler R, Bresalier R, Quan H, Riddell R, Lanas A, Bolognese J, Oxenius B, Horgan K, Loftus S, Morton D |title=A randomized trial of rofecoxib for the chemoprevention of colorectal adenomas |journal=Gastroenterology |volume=131 |issue=6 |pages=1674–82 |year=2006 |pmid=17087947 |doi=10.1053/j.gastro.2006.08.079}}</ref><ref>{{cite journal |author=Bertagnolli M, Eagle C, Zauber A, Redston M, Solomon S, Kim K, Tang J, Rosenstein R, Wittes J, Corle D, Hess T, Woloj G, Boisserie F, Anderson W, Viner J, Bagheri D, Burn J, Chung D, Dewar T, Foley T, Hoffman N, Macrae F, Pruitt R, Saltzman J, Salzberg B, Sylwestrowicz T, Gordon G, Hawk E |title=Celecoxib for the prevention of sporadic colorectal adenomas |journal=N Engl J Med |volume=355 |issue=9 |pages=873–84 |year=2006 |pmid=16943400 |doi=10.1056/NEJMoa061355}}</ref> | |||
| In both groups, there were significant reductions in ] ], but this came at the price of increased cardiovascular toxicity. | |||
| === Genetic testing === | |||
| {{See also|Cancer syndrome}} | |||
| ===Genetic testing=== | |||
| {| class="wikitable floatright" style="text-align:center" width="50%" | |||
| ] for high-risk individuals is already available for certain cancer-related genetic mutations. Carriers of genetic mutations that increase risk for cancer incidence can undergo enhanced surveillance, chemoprevention, or risk-reducing surgery. Early identification of inherited genetic risk for cancer, along with cancer-preventing interventions such as surgery or enhanced surveillance, can be lifesaving for high-risk individuals. | |||
| {| class="wikitable" | |||
| |- | |- | ||
| ! Gene | ! Gene | ||
| ! Cancer types | ! Cancer types | ||
| ! Availability | |||
| |- | |- | ||
| | ], ] | | ], ] | ||
| | Breast, ovarian, pancreatic | | Breast, ovarian, pancreatic | ||
| | Commercially available for clinical specimens | |||
| |- | |- | ||
| | ], ], ], ], ] | | ], ], ], ], ], ] | ||
| | Colon, uterine, small bowel, stomach, urinary tract | | Colon, uterine, small bowel, stomach, urinary tract | ||
| | Commercially available for clinical specimens | |||
| |} | |} | ||
| ] for individuals at high risk of certain cancers is recommended by unofficial groups.<ref name=pmid24176569/><ref name=BRCA08>{{cite journal |vauthors=Gulati AP, ] |s2cid=29630942 |title=The clinical management of BRCA1 and BRCA2 mutation carriers |journal=Current Oncology Reports |volume=10 |issue=1 |pages=47–53 |date=January 2008 |pmid=18366960 |doi=10.1007/s11912-008-0008-9}}</ref> Carriers of these mutations may then undergo enhanced surveillance, chemoprevention, or preventative surgery to reduce their subsequent risk.<ref name=BRCA08/> | |||
| ===Vaccination=== | |||
| == Management == | |||
| Considerable {{ww}} research effort is now devoted to the development of ]s to prevent infection by oncogenic infectious agents, as well as to mount an immune response against cancer-specific ]s) and to potential venues for ] for individuals with genetic mutations or polymorphisms that put them at high risk of cancer. | |||
| {{Main|Treatment of cancer|Oncology|}} | |||
| As reported above, a preventive ] exists that targets certain sexually transmitted strains of ] that are associated with the development of ] and ]. The only two HPV vaccines on the market as of October 2007 are ] and ]. | |||
| Many treatment options for cancer exist. The primary ones include surgery, ], ], ], ] and ]. Which treatments are used depends on the type, location and grade of the cancer as well as the patient's health and preferences. The ] may or may not be curative.{{citation needed|date=March 2024}} | |||
| ===Screening=== | |||
| === Chemotherapy === | |||
| Cancer ] is an attempt to detect unsuspected cancers in an asymptomatic population. Screening tests suitable for large numbers of healthy people must be relatively affordable, safe, noninvasive procedures with acceptably low rates of ] results. If signs of cancer are detected, more definitive and invasive follow up tests are performed to confirm the diagnosis. | |||
| ] is the treatment of cancer with one or more ] anti-] drugs (]) as part of a ]. The term encompasses a variety of drugs, which are divided into broad categories such as ] and ]s.<ref name="Lind2008">{{cite journal | vauthors = Lind MJ |title=Principles of cytotoxic chemotherapy |journal=Medicine |year=2008 |volume=36 |issue=1 |pages=19–23 |doi=10.1016/j.mpmed.2007.10.003 }}</ref> Traditional chemotherapeutic agents act by killing cells that divide rapidly, a critical property of most cancer cells. | |||
| Screening for cancer can lead to earlier diagnosis in specific cases. Early diagnosis may lead to extended life, but may also falsely prolong the lead time to death through ] or ]. | |||
| It was found that providing combined cytotoxic drugs is better than a single drug, a process called the ], which has an advantage in the statistics of survival and response to the tumor and in the progress of the disease.<ref>{{cite book | vauthors = Frei III E, Eder JP |title=Combination Chemotherapy |date=2003 |url=https://www.ncbi.nlm.nih.gov/books/NBK13955/ |access-date=4 April 2020 |language=en}}</ref> A Cochrane review concluded that combined therapy was more effective to treat metastasized breast cancer. However, generally it is not certain whether combination chemotherapy leads to better health outcomes, when both survival and toxicity are considered.<ref>{{cite journal | vauthors = Dear RF, McGeechan K, Jenkins MC, Barratt A, Tattersall MH, Wilcken N | title = Combination versus sequential single agent chemotherapy for metastatic breast cancer | journal = The Cochrane Database of Systematic Reviews | issue = 12 | pages = CD008792 | date = December 2013 | volume = 2021 | pmid = 24347031 | doi = 10.1002/14651858.CD008792.pub2 | pmc = 8094913 }}</ref> | |||
| A number of different screening tests have been developed for different malignancies. Breast cancer screening can be done by ], though this approach was discredited by a 2005 study in over 300,000 Chinese women. Screening for breast cancer with ]s has been shown to reduce the average stage of diagnosis of breast cancer in a population. Stage of diagnosis in a country has been shown to decrease within ten years of introduction of mammographic screening programs. Colorectal cancer can be detected through ]ing and ], which reduces both colon cancer incidence and mortality, presumably through the detection and removal of pre-malignant polyps. Similarly, cervical cytology testing (using the ]) leads to the identification and excision of precancerous lesions. Over time, such testing has been followed by a dramatic reduction of ] incidence and mortality. ] is recommended for men beginning at the age of 15 years to detect ]. Prostate cancer can be screened using a ] along with ] (PSA) blood testing, though some authorities (such as the ]) recommend against routinely screening all men. | |||
| ] is a form of chemotherapy that targets specific molecular differences between cancer and normal cells. The first targeted therapies blocked the ] molecule, inhibiting the growth of breast cancer. Another common example is the class of ], which are used to treat ] (CML).<ref name=TCT2018/> Currently, targeted therapies exist for many of the most common cancer types, including ], breast cancer, ], ], ], ], lung cancer, ], ], ], ], and ] as well as other cancer types.<ref name=TCT2018/> | |||
| Screening for cancer is controversial in cases when it is not yet known if the test actually saves lives. The controversy arises when it is not clear if the benefits of screening outweigh the risks of follow-up diagnostic tests and cancer treatments. For example: when screening for ], the ] test may detect small cancers that would never become life threatening, but once detected will lead to treatment. This situation, called overdiagnosis, puts men at risk for complications from unnecessary treatment such as surgery or radiation. Follow up procedures used to diagnose prostate cancer (]) may cause side effects, including bleeding and infection. Prostate cancer treatment may cause ] (inability to control urine flow) and ] (erections inadequate for intercourse). Similarly, for ], there have recently been criticisms that breast screening programs in some countries cause more problems than they solve. This is because screening of women in the general population will result in a large number of women with false positive results which require extensive follow-up investigations to exclude cancer, leading to having a high number-to-treat (or number-to-screen) to prevent or catch a single case of breast cancer early. | |||
| The efficacy of chemotherapy depends on the type of cancer and the stage. In combination with surgery, chemotherapy has proven useful in cancer types including breast cancer, colorectal cancer, ], ], ], ovarian cancer and certain lung cancers.<ref name=HollandTx40/> Chemotherapy is curative for some cancers, such as some ],<ref>{{cite journal |vauthors=Nastoupil LJ, Rose AC, Flowers CR |title=Diffuse large B-cell lymphoma: current treatment approaches |journal=Oncology |volume=26 |issue=5 |pages=488–95 |date=May 2012 |pmid=22730604}}</ref><ref>{{cite journal |vauthors=Freedman A |title=Follicular lymphoma: 2012 update on diagnosis and management |journal=American Journal of Hematology |volume=87 |issue=10 |pages=988–95 |date=October 2012 |pmid=23001911 |doi=10.1002/ajh.23313|s2cid=35447562 |doi-access=free }}</ref> ineffective in some ],<ref>{{cite journal |vauthors=Rampling R, James A, Papanastassiou V |title=The present and future management of malignant brain tumours: surgery, radiotherapy, chemotherapy |journal=Journal of Neurology, Neurosurgery, and Psychiatry |volume=75 |issue=Suppl 2 |pages=ii24–30 |date=June 2004 |pmid=15146036 |pmc=1765659 |doi=10.1136/jnnp.2004.040535}}</ref> and needless in others, such as most ]s.<ref>{{cite journal |vauthors=Madan V, Lear JT, Szeimies RM |title=Non-melanoma skin cancer |journal=Lancet |volume=375 |issue=9715 |pages=673–85 |date=February 2010 |pmid=20171403 |doi=10.1016/S0140-6736(09)61196-X|pmc=3339125 }}</ref> The effectiveness of chemotherapy is often limited by its toxicity to other tissues in the body. Even when chemotherapy does not provide a permanent cure, it may be useful to reduce symptoms such as pain or to reduce the size of an inoperable tumor in the hope that surgery will become possible in the future. | |||
| Cervical cancer screening via the ] has the best cost-benefit profile of all the forms of cancer screening from a public health perspective as, being largely caused by a virus, it has clear risk factors (sexual contact), and the natural progression of cervical cancer is that it normally spreads slowly over a number of years therefore giving more time for the screening program to catch it early. Moreover, the test itself is easy to perform and relatively cheap. | |||
| === Radiation === | |||
| ] involves the use of ] in an attempt to either cure or improve symptoms.<!--<ref name=H41/> --> It works by damaging the DNA of cancerous tissue, causing ] resulting in the death of the cancer cells.<ref>{{cite journal | vauthors = Vitale I, Galluzzi L, Castedo M, Kroemer G | title = Mitotic catastrophe: a mechanism for avoiding genomic instability | journal = Nature Reviews. Molecular Cell Biology | volume = 12 | issue = 6 | pages = 385–392 | date = June 2011 | pmid = 21527953 | doi = 10.1038/nrm3115 | s2cid = 22483746 }}</ref> To spare normal tissues (such as skin or organs, which radiation must pass through to treat the tumor), shaped radiation beams are aimed from multiple exposure angles to intersect at the tumor, providing a much larger dose there than in the surrounding, healthy tissue. As with chemotherapy, cancers vary in their response to radiation therapy.<ref>{{cite book | vauthors = Bomford CK, Kunkler IH, Walter J | title = Walter and Miller's Textbook of Radiation therapy | edition = 6th | page = 311 }}</ref><ref>{{cite web |url=http://www.gpnotebook.co.uk/simplepage.cfm?ID=2060451853 |title=tumour radiosensitivity – General Practice Notebook | vauthors = McMorran J, Crowther D, McMorran S, Youngmin S, Wacogne I, Pleat J, Clive P |url-status=live |archive-url=https://web.archive.org/web/20150924023421/http://www.gpnotebook.co.uk/simplepage.cfm?ID=2060451853 |archive-date=24 September 2015}}</ref><ref>{{cite web |url=https://patient.info/doctor/radiotherapy-pro |title=Radiotherapy |publisher=] | vauthors = Tidy C |date=23 December 2015 | url-status = live |archive-url=https://web.archive.org/web/20170709084620/https://patient.info/doctor/radiotherapy-pro |archive-date=9 July 2017}} Last Checked: 23 December 2015</ref> | |||
| For these reasons, it is important that the benefits and risks of diagnostic procedures and treatment be taken into account when considering whether to undertake cancer screening. | |||
| Radiation therapy is used in about half of cases. The radiation can be either from internal sources (]) or external sources. The radiation is most commonly low energy X-rays for treating skin cancers, while higher energy X-rays are used for cancers within the body.<ref>{{cite journal |vauthors=Hill R, Healy B, Holloway L, Kuncic Z, Thwaites D, Baldock C |s2cid=18082594 |title=Advances in kilovoltage x-ray beam dosimetry |journal=Physics in Medicine and Biology |volume=59 |issue=6 |pages=R183–231 |date=March 2014 |pmid=24584183 |doi=10.1088/0031-9155/59/6/r183|bibcode=2014PMB....59R.183H }}</ref> Radiation is typically used in addition to surgery and or chemotherapy. For certain types of cancer, such as early ], it may be used alone.<ref name=H41/> Radiation therapy after surgery for brain metastases has been shown to not improve overall survival in patients compared to surgery alone.<ref>{{Cite web |date=13 August 2019 |title=Radiation Therapy for Brain Metastases: A Systematic Review |url=https://www.pcori.org/research-results/2019/radiation-therapy-brain-metastases-systematic-review |access-date=10 October 2023 |website=PCORI |language=en}}</ref> For painful ], radiation therapy has been found to be effective in about 70% of patients.<ref name="H41">Holland Chp. 41</ref> | |||
| Use of ] to search for cancer in people without clear symptoms is similarly marred with problems. There is a significant risk of detection of what has been recently called an '']'' - a benign lesion that may be interpreted as a malignancy and be subjected to potentially dangerous investigations. Recent studies of ]-based screening for ] in smokers have had equivocal results, and systematic screening is not recommended as of July 2007. ] of plain-film ] to screen for lung cancer in smokers have shown no benefit for this approach. | |||
| === Surgery === | |||
| ] has shown promise, but is still in the early stages of research. | |||
| Surgery is the primary method of treatment for most isolated, solid cancers and may play a role in palliation and prolongation of survival. It is typically an important part of definitive diagnosis and staging of tumors, as biopsies are usually required. In localized cancer, surgery typically attempts to remove the entire mass along with, in certain cases, the ]s in the area. For some types of cancer this is sufficient to eliminate the cancer.<ref name=HollandTx40>Holland Chp. 40</ref> | |||
| === Palliative care === | |||
| ] is treatment that attempts to help the patient feel better and may be combined with an attempt to treat the cancer. Palliative care includes action to reduce physical, emotional, spiritual and psycho-social distress. Unlike treatment that is aimed at directly killing cancer cells, the primary goal of palliative care is to improve ]. | |||
| People at all stages of cancer treatment typically receive some kind of palliative care. In some cases, ] ] recommend that patients and physicians respond to cancer only with palliative care. This applies to patients who:<ref name="ASCOfive">{{Cite journal |author1=American Society of Clinical Oncology |author1-link=American Society of Clinical Oncology |title=Five Things Physicians and Patients Should Question |journal=Choosing Wisely: An Initiative of the ABIM Foundation |url=http://choosingwisely.org/wp-content/uploads/2012/04/5things_12_factsheet_Amer_Soc_Clin_Onc.pdf |access-date=14 August 2012 |archive-url=https://web.archive.org/web/20120731073425/http://choosingwisely.org/wp-content/uploads/2012/04/5things_12_factsheet_Amer_Soc_Clin_Onc.pdf |archive-date=31 July 2012}}<br/>* The American Society of Clinical Oncology made this recommendation based on various cancers.</ref> | |||
| * for lung cancer, see {{cite journal |vauthors=Azzoli CG, Temin S, Aliff T, Baker S, Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D, Nordquist L, Pao W, Pfister DG, Piantadosi S, Schiller JH, Smith R, Smith TJ, Strawn JR, Trent D, Giaccone G |title=2011 Focused Update of 2009 American Society of Clinical Oncology Clinical Practice Guideline Update on Chemotherapy for Stage IV Non-Small-Cell Lung Cancer |journal=Journal of Clinical Oncology |volume=29 |issue=28 |pages=3825–31 |date=October 2011 |pmid=21900105 |pmc=3675703 |doi=10.1200/JCO.2010.34.2774 | author20 = American Society of Clinical Oncology}} and {{cite journal |vauthors=Ettinger DS, Akerley W, Bepler G, Blum MG, Chang A, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Ganti AK, Govindan R, Grannis FW, Jahan T, Jahanzeb M, Johnson DH, Kessinger A, Komaki R, Kong FM, Kris MG, Krug LM, Le QT, Lennes IT, Martins R, O'Malley J, Osarogiagbon RU, Otterson GA, Patel JD, Pisters KM, Reckamp K, Riely GJ, Rohren E, Simon GR, Swanson SJ, Wood DE, Yang SC |title=Non-small cell lung cancer |journal=Journal of the National Comprehensive Cancer Network |volume=8 |issue=7 |pages=740–801 |date=July 2010 |pmid=20679538| doi = 10.6004/jnccn.2010.0056 |doi-access=free }} | |||
| * for breast cancer, see {{cite journal |vauthors=Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, Erban JK, Farrar WB, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Jahanzeb M, Kiel K, Ljung BM, Marcom PK, Mayer IA, McCormick B, Nabell LM, Pierce LJ, Reed EC, Smith ML, Somlo G, Theriault RL, Topham NS, Ward JH, Winer EP, Wolff AC |title=Breast cancer. Clinical practice guidelines in oncology |journal=Journal of the National Comprehensive Cancer Network |volume=7 |issue=2 |pages=122–92 |date=February 2009 |pmid=19200416 |author29=NCCN Breast Cancer Clinical Practice Guidelines Panel| doi = 10.6004/jnccn.2009.0012 |doi-access=free }} | |||
| * for colon cancer, see {{cite journal |vauthors=Engstrom PF, Arnoletti JP, Benson AB, Chen YJ, Choti MA, Cooper HS, Covey A, Dilawari RA, Early DS, Enzinger PC, Fakih MG, Fleshman J, Fuchs C, Grem JL, Kiel K, Knol JA, Leong LA, Lin E, Mulcahy MF, Rao S, Ryan DP, Saltz L, Shibata D, Skibber JM, Sofocleous C, Thomas J, Venook AP, Willett C |title=NCCN Clinical Practice Guidelines in Oncology: colon cancer |journal=Journal of the National Comprehensive Cancer Network |volume=7 |issue=8 |pages=778–831 |date=September 2009 |pmid=19755046 |author29=National Comprehensive Cancer Network|doi=10.6004/jnccn.2009.0056 |doi-access=free }} | |||
| * for other general statements see {{cite journal |vauthors=Smith TJ, Hillner BE |title=Bending the cost curve in cancer care |journal=The New England Journal of Medicine |volume=364 |issue=21 |pages=2060–5 |date=May 2011 |pmid=21612477 |doi=10.1056/NEJMsb1013826|pmc=4042405 }} and {{cite journal |vauthors=Peppercorn JM, Smith TJ, Helft PR, Debono DJ, Berry SR, Wollins DS, Hayes DM, Von Roenn JH, Schnipper LE |title=American society of clinical oncology statement: toward individualized care for patients with advanced cancer |journal=Journal of Clinical Oncology |volume=29 |issue=6 |pages=755–60 |date=February 2011 |pmid=21263086 |doi=10.1200/JCO.2010.33.1744 | author10 = American Society of Clinical Oncology|s2cid=40873748 }} | |||
| * Display low ], implying limited ability to care for themselves | |||
| * Received no benefit from prior ] | |||
| * Are not eligible to participate in any appropriate ] | |||
| * No strong evidence implies that treatment would be effective | |||
| Palliative care may be confused with ] and therefore only indicated when people approach ]. Like hospice care, palliative care attempts to help the patient cope with their immediate needs and to increase comfort. Unlike hospice care, palliative care does not require people to stop treatment aimed at the cancer. | |||
| Multiple national ]s recommend early palliative care for patients whose cancer has produced distressing symptoms or who need help coping with their illness. In patients first diagnosed with metastatic disease, palliative care may be immediately indicated. Palliative care is indicated for patients with a prognosis of less than 12 months of life even given aggressive treatment.<ref>{{cite web |url=http://www.nccn.org/professionals/physician_gls/default.asp |title=NCCN Guidelines |url-status=live |archive-url=https://web.archive.org/web/20080514153600/http://www.nccn.org/professionals/physician_gls/default.asp |archive-date=14 May 2008}}</ref><ref>{{cite web |url=http://www.nationalconsensusproject.org/guideline.pdf |title=Clinical Practice Guidelines for Quality Palliative Care |publisher=The National Consensus Project for Quality Palliative Care (NCP) |archive-url=https://web.archive.org/web/20110516082645/http://www.nationalconsensusproject.org/Guideline.pdf |archive-date=16 May 2011}}</ref><ref>{{cite journal |vauthors=Levy MH, Back A, Bazargan S, Benedetti C, Billings JA, Block S, Bruera E, Carducci MA, Dy S, Eberle C, Foley KM, Harris JD, Knight SJ, Milch R, Rhiner M, Slatkin NE, Spiegel D, Sutton L, Urba S, Von Roenn JH, Weinstein SM |s2cid=44343423 |title=Palliative care. Clinical practice guidelines in oncology |journal=Journal of the National Comprehensive Cancer Network |volume=4 |issue=8 |pages=776–818 |date=September 2006 |pmid=16948956 |doi= 10.6004/jnccn.2006.0068}}</ref> | |||
| === Immunotherapy === | |||
| {{Main|Cancer immunotherapy}} | |||
| A variety of therapies using ], stimulating or helping the ] to fight cancer, have come into use since 1997. Approaches include:<ref>{{cite journal |vauthors=Waldmann TA |date=March 2003 |title=Immunotherapy: past, present and future |url=https://zenodo.org/record/1233435 |journal=Nature Medicine |volume=9 |issue=3 |pages=269–77 |doi=10.1038/nm0303-269 |pmid=12612576 |s2cid=9745527 |doi-access=free}}</ref> | |||
| * ] | |||
| * ] (therapy that targets the ]s or regulators of the ]) | |||
| * ] | |||
| === Laser therapy === | |||
| {{Main|Lasers in cancer treatment}} | |||
| ] therapy uses high-intensity light to treat cancer by shrinking or destroying tumors or precancerous growths. Lasers are most commonly used to treat superficial cancers that are on the surface of the body or the lining of internal organs. It is used to treat basal cell skin cancer and the very early stages of others like cervical, penile, vaginal, vulvar, and non-small cell lung cancer. It is often combined with other treatments, such as surgery, chemotherapy, or radiation therapy. ] (LITT), or interstitial laser ], uses lasers to treat some cancers using hyperthermia, which uses heat to shrink tumors by damaging or killing cancer cells. Laser are more precise than surgery and cause less damage, pain, bleeding, swelling, and scarring. A disadvantage is surgeons must have specialized training. It may be more expensive than other treatments.<ref name="NIHlaser">{{cite web|url=https://www.cancer.gov/about-cancer/treatment/types/surgery/lasers-fact-sheet|title=Lasers in Cancer Treatment|date=13 September 2011|publisher=National Institutes of Health, National Cancer Institute|access-date=15 December 2017}}{{PD-notice}}</ref> | |||
| === Alternative medicine === | |||
| ] are a diverse group of therapies, practices and products that are not part of conventional medicine.<ref name="mnalt">{{cite journal |vauthors=Cassileth BR, Deng G |title=Complementary and alternative therapies for cancer |journal=The Oncologist |volume=9 |issue=1 |pages=80–89 |year=2004 |pmid=14755017 |doi=10.1634/theoncologist.9-1-80|s2cid=6453919 |url=http://theoncologist.alphamedpress.org/content/9/1/80.full.pdf }}</ref> "Complementary medicine" refers to methods and substances used along with conventional medicine, while "alternative medicine" refers to compounds used instead of conventional medicine.<ref> {{webarchive|url=https://web.archive.org/web/20051208040402/http://nccam.nih.gov/health/whatiscam/ |date=8 December 2005 }} ]. Retrieved 3 February 2008.</ref> Most complementary and alternative medicines for cancer have not been studied or tested using conventional techniques such as clinical trials. Some alternative treatments have been investigated and shown to be ineffective but still continue to be marketed and promoted. Cancer researcher Andrew J. Vickers stated, "The label 'unproven' is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been 'disproven'."<ref name="pmid15061600">{{cite journal |vauthors=Vickers A |title=Alternative cancer cures: "unproven" or "disproven"? |journal=CA: A Cancer Journal for Clinicians |volume=54 |issue=2 |pages=110–18 |year=2004 |pmid=15061600 |doi=10.3322/canjclin.54.2.110|citeseerx=10.1.1.521.2180 |s2cid=35124492 }}</ref> | |||
| == Prognosis == | |||
| {{See also|Cancer survival rates|List of cancer mortality rates in the United States|Cancer survivor}} | |||
| ] | |||
| Survival rates vary by cancer type and by the stage at which it is diagnosed, ranging from majority survival to complete mortality five years after diagnosis. Once a cancer has metastasized, prognosis normally becomes much worse. About half of patients receiving treatment for invasive cancer (excluding ] and non-melanoma skin cancers) die from that cancer or its treatment.<ref name=Epi11/> A majority of cancer deaths are due to metastases of the primary tumor.<ref>{{cite journal | vauthors = Tammela T, Sage J | title = Investigating Tumor Heterogeneity in Mouse Models | journal = Annual Review of Cancer Biology | volume = 4 | issue = 1 | pages = 99–119 | date = March 2020 | pmid = 34164589 | pmc = 8218894 | doi = 10.1146/annurev-cancerbio-030419-033413 | doi-access = free }}</ref> | |||
| Survival is worse in the ],<ref name=Epi11/> partly because the types of cancer that are most common there are harder to treat than those associated with ].<ref>{{cite book |title=World Cancer Report 2014 |date=2014 |publisher=World Health Organization |isbn=978-92-832-0429-9 |url=http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |page=22 |archive-url=https://web.archive.org/web/20170712114430/http://www.searo.who.int/publications/bookstore/documents/9283204298/en/ |archive-date=12 July 2017}}</ref> | |||
| Those who survive cancer develop a second primary cancer at about twice the rate of those never diagnosed.<ref name=isbn1-55009-213-8/> The increased risk is believed to be due to the random chance of developing any cancer, the likelihood of surviving the first cancer, the same risk factors that produced the first cancer, unwanted side effects of treating the first cancer (particularly radiation therapy), and better compliance with screening.<ref name="isbn1-55009-213-8">{{cite book | veditors = Frei E, Kufe DW, Holland JF | vauthors = Rheingold S, Neugut A, Meadows A | title = Holland-Frei Cancer Medicine | edition = 6th | publisher = BC Decker | location = Hamilton, Ont | year = 2003 | page = | isbn = 978-1-55009-213-4 | chapter-url = https://www.ncbi.nlm.nih.gov/books/NBK20948/#A41087 | chapter = 156: Secondary Cancers: Incidence, Risk Factors, and Management | url = https://archive.org/details/cancermedicine60002unse/page/2399 }}</ref> | |||
| Predicting short- or long-term survival depends on many factors. The most important are the cancer type and the patient's age and overall health. Those who are ] with other health problems have lower survival rates than otherwise healthy people. ]s are unlikely to survive for five years even if treatment is successful. People who report a higher quality of life tend to survive longer.<ref>{{cite journal |vauthors=Montazeri A |title=Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008 |journal=Health and Quality of Life Outcomes |volume=7 |page=102 |date=December 2009 |pmid=20030832 |pmc=2805623 |doi=10.1186/1477-7525-7-102 |author-link=Ali Montazeri |doi-access=free }}</ref> People with lower quality of life may be affected by ] and other complications and/or disease progression that both impairs quality and quantity of life. Additionally, patients with worse prognoses may be depressed or report poorer quality of life because they perceive that their condition is likely to be fatal. | |||
| People with cancer have an increased risk of ] which can be life-threatening.<ref name=":1">{{cite journal | vauthors = Akl EA, Kahale LA, Hakoum MB, Matar CF, Sperati F, Barba M, Yosuico VE, Terrenato I, Synnot A, Schünemann H | title = Parenteral anticoagulation in ambulatory patients with cancer | journal = The Cochrane Database of Systematic Reviews | volume = 2021 | pages = CD006652 | date = September 2017 | issue = 9 | pmid = 28892556 | pmc = 6419241 | doi = 10.1002/14651858.CD006652.pub5 }}</ref> The use of ] such as ] decrease the risk of blood clots but have not been shown to increase survival in people with cancer.<ref name=:1/> People who take blood thinners also have an increased risk of bleeding.<ref name=:1/> | |||
| Although extremely rare, some forms of cancer, even from an advanced stage, can heal spontaneously. This phenomenon is known as ].<ref>{{cite journal | vauthors = Radha G, Lopus M | title = The spontaneous remission of cancer: Current insights and therapeutic significance | journal = Translational Oncology | volume = 14 | issue = 9 | page = 101166 | date = September 2021 | pmid = 34242964 | pmc = 8271173 | doi = 10.1016/j.tranon.2021.101166 }}</ref> | |||
| == Epidemiology == | == Epidemiology == | ||
| {{Main|Epidemiology of cancer}} | |||
| ] | |||
| {{See also|List of countries by cancer rate}} | |||
| {{Image frame | |||
| Cancer ] is the study of the incidence of cancer as a way to infer possible trends and causes. The first such cause of cancer was identified by British surgeon ], who discovered in 1775 that cancer of the ] was a common disease among ]s. The work of other individual physicians led to various insights, but when physicians started working together they could make firmer conclusions. | |||
| |width=520<!-- Must be kept at this size at this point (December 2017) --> | |||
| |content ={{Global Heat Maps by Year| title=| table=Cancer death rate.tab| column=deaths| columnName=Deaths per 10,000| year=2017|%=}} | |||
| A founding paper of this discipline was the work of ], who published a comparative study in 1926 of 500 breast cancer cases and 500 control patients of the same background and lifestyle for the British Ministry of Health. Her ground-breaking work on cancer epidemiology was carried on by ] and ], who published "] and Other Causes of Death In Relation to ]. A Second Report on the Mortality of British Doctors" followed in 1956 (otherwise known as the ]). Richard Doll left the ] Medical Research Center (MRC), to start the ] unit for Cancer epidemiology in 1968. With the use of ]s, the unit was the first to compile large amounts of cancer data. Modern epidemiological methods are closely linked to current concepts of disease and ] policy. Over the past 50 years, great efforts have been spent on gathering data across medical practise, hospital, provincial, state, and even country boundaries, as a way to study the interdependence of environmental and cultural factors on cancer incidence. | |||
| |caption=Age-standardized death rate from cancer per 10,000 people.<ref>{{cite web |title=Cancer death rates |url=https://ourworldindata.org/grapher/cancer-death-rates |website=Our World in Data |access-date=4 October 2019}}</ref> | |||
| |align=right | |||
| Cancer epidemiology must contend with problems of ] and ]. Lead time bias is the concept that early diagnosis may artificially inflate the survival statistics of a cancer, without really improving the natural history of the disease. Length bias is the concept that slower growing, more indolent tumors are more likely to be diagnosed by screening tests, but improvements in diagnosing more cases of indolent cancer may not translate into better patient outcomes after the implementation of screening programs. A similar epidemiological concern is ], the tendency of screening tests to diagnose diseases that may not actually impact the patient's longevity. This problem especially applies to ] and ].<ref name="pmid15283896">{{cite journal |author=Brawley OW |title=Prostate cancer screening: clinical applications and challenges |journal=Urol. Oncol. |volume=22 |issue=4 |pages=353–7 |year=2004 |pmid=15283896 |doi=10.1016/j.urolonc.2004.04.014}}</ref> | |||
| }} | |||
| Some cancer researchers have argued that negative cancer clinical trials lack sufficient ] to discover a benefit to treatment. This may be due to fewer patients enrolled in the study than originally planned.<ref name="pmid17687153">{{cite journal |author=Bedard PL, Krzyzanowska MK, Pintilie M, Tannock IF |title=Statistical power of negative randomized controlled trials presented at American Society for Clinical Oncology annual meetings |journal=J. Clin. Oncol. |volume=25 |issue=23 |pages=3482–7 |year=2007 |pmid=17687153 |doi=10.1200/JCO.2007.11.3670}}</ref> | |||
| Estimates are that in 2018, 18.1 million new cases of cancer and 9.6 million deaths occur globally.<ref name=IARC2018/> About 20% of males and 17% of females will get cancer at some point in time while 13% of males and 9% of females will die from it.<ref name=IARC2018>{{cite web |title=Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018 |url=https://www.iarc.fr/wp-content/uploads/2018/09/pr263_E.pdf |website=iarc.fr |access-date=5 December 2018}}</ref> | |||
| State and regional ] are organizations that abstract clinical data about cancer from patient medical records. These institutions provide information to state and national public health groups to help track trends in cancer diagnosis and treatment. One of the largest and most important ] is ], administered by the ].<ref>{{cite web |url=http://seer.cancer.gov/ |title=SEER Surveillance Epidemiology and End Results |accessdate=2007-11-02 |work=}}</ref> Health information privacy concerns have led to the restricted use of ] data in the ]<ref name="lancetva">Furlow, B, ''Lancet Oncology'' 2007; 8:762-763. Retrieved ].</ref><ref name= "mpva"> (] ]). ''Medpage Today''. Retrieved ]. </ref><ref name="nytva"> (] ]). ''New York Times''. Retrieved ].</ref> and other institutions.<ref name="iomhip"> (] ]). ''IOM Presentation''. Retrieved ].</ref> | |||
| In 2008, approximately 12.7 million cancers were ] (excluding ]s and other non-invasive cancers)<ref name=Epi11/> and in 2010 nearly 7.98 million people died.<ref name=Loz2012>{{cite journal |vauthors=Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA | s2cid = 1541253 |title=Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010 |journal=Lancet |volume=380 |issue=9859 |pages=2095–128 |date=December 2012 |pmid=23245604 |doi=10.1016/S0140-6736(12)61728-0 | pmc = 10790329 |hdl=10536/DRO/DU:30050819| url = https://zenodo.org/record/2557786 |hdl-access=free }}</ref> Cancers account for approximately 16% of deaths. The most common {{as of|2018|lc=yes}} are lung cancer (1.76 million deaths), ] (860,000) ] (780,000), ] (780,000), and breast cancer (620,000).<ref name=WHO2018/> This makes invasive cancer the leading cause of death in the ] and the second leading in the ].<ref name=Epi11/> Over half of cases occur in the developing world.<ref name=Epi11/> | |||
| In some Western countries, such as the USA,<ref name="CACancerJClin2005-Jemal" /> and the UK<ref name="BBC2000-news"> | |||
| Deaths from cancer were 5.8 million in 1990.<ref name=Loz2012/> Deaths have been increasing primarily due to longer lifespans and lifestyle changes in the developing world.<ref name=Epi11/> The most significant ] for developing cancer is age.<ref name=Coleman>{{cite book | vauthors = Coleman WB, Rubinas TC | veditors = Tsongalis GJ, Coleman WL | title = Molecular Pathology: The Molecular Basis of Human Disease | publisher = Elsevier Academic Press | location = Amsterdam | year = 2009 | page = 66 | chapter = 4 | chapter-url = {{google books |plainurl=y |id=7MaclAEA}} | isbn = 978-0-12-374419-7 }}{{dead link|date=July 2023 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> Although it is possible for cancer to strike at any age, most patients with invasive cancer are over 65.<ref name=Coleman/> According to cancer researcher ], "If we lived long enough, sooner or later we all would get cancer."<ref name=Weinberg>{{cite news |url=https://www.nytimes.com/2010/12/28/health/28cancer.html |title=Unearthing Prehistoric Tumors, and Debate |newspaper=] |date=28 December 2010 | vauthors = Johnson G |url-status=live |archive-url=https://web.archive.org/web/20170624233156/http://www.nytimes.com/2010/12/28/health/28cancer.html |archive-date=24 June 2017}}</ref> Some of the association between aging and cancer is attributed to ],<ref>{{cite journal | vauthors = Pawelec G, Derhovanessian E, Larbi A | title = Immunosenescence and cancer | journal = Critical Reviews in Oncology/Hematology | volume = 75 | issue = 2 | pages = 165–72 | date = August 2010 | pmid = 20656212 | doi = 10.1016/j.critrevonc.2010.06.012 }}</ref> errors accumulated in ] over a lifetime<ref>{{cite book |vauthors=Alberts B, Johnson A, Lewis J |title=Molecular biology of the cell |publisher=Garland Science |location=New York |year=2002 |edition=4th |chapter=The Preventable Causes of Cancer |isbn=978-0-8153-4072-0 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK26897/ |quote=A certain irreducible background incidence of cancer is to be expected regardless of circumstances: mutations can never be absolutely avoided, because they are an inescapable consequence of fundamental limitations on the accuracy of DNA replication, as discussed in Chapter 5. If a human could live long enough, it is inevitable that at least one of his or her cells would eventually accumulate a set of mutations sufficient for cancer to develop. | display-authors = etal |url-status=live |archive-url=https://web.archive.org/web/20160102193148/http://www.ncbi.nlm.nih.gov/books/NBK26897/ |archive-date=2 January 2016}}</ref> and age-related changes in the ].<ref>{{cite journal | vauthors = Anisimov VN, Sikora E, Pawelec G | s2cid = 17412298 | title = Relationships between cancer and aging: a multilevel approach | journal = Biogerontology | volume = 10 | issue = 4 | pages = 323–38 | date = August 2009 | pmid = 19156531 | doi = 10.1007/s10522-008-9209-8 }}</ref> Aging's effect on cancer is complicated by factors such as DNA damage and inflammation promoting it and factors such as vascular aging and endocrine changes inhibiting it.<ref>{{cite journal | vauthors = de Magalhães JP | s2cid = 5726826 | title = How ageing processes influence cancer | journal = Nature Reviews. Cancer | volume = 13 | issue = 5 | pages = 357–65 | date = May 2013 | pmid = 23612461 | doi = 10.1038/nrc3497 }}</ref> | |||
| (] ]). ''BBC News online''. Retrieved ].</ref> cancer is overtaking ] as the leading cause of death. In many ] countries cancer incidence (insofar as this can be measured) appears much lower, most likely because of the higher death rates due to infectious disease or injury. With the increased control over ] and ] in some Third World countries, incidence of cancer is expected to rise; this is termed the epidemiologic transition in ] terminology. | |||
| Some slow-growing cancers are particularly common, but often are not fatal. ] studies in Europe and Asia showed that up to 36% of people have undiagnosed and apparently harmless ] at the time of their deaths and that 80% of men develop ] by age 80.<ref>{{cite book | vauthors = David S, Fraumeni JF |title=Cancer Epidemiology and Prevention |url={{google books |plainurl=y |id=qfN8Y1_lbDYC |page=977}}|date=24 August 2006|publisher=Oxford University Press|isbn=978-0-19-974797-9|page=977}}</ref><ref>{{cite book | vauthors = Bostwick DG, Eble JN |title=Urological Surgical Pathology |publisher=Mosby |location=St. Louis |year=2007 |page=468 |isbn=978-0-323-01970-5 |url={{google books |plainurl=y |id=z7AA-DS0VegC |page=335}}}}</ref> As these cancers do not cause the patient's death, identifying them would have represented ] rather than useful medical care. | |||
| Cancer epidemiology closely mirrors risk factor spread in various countries. ] (] cancer) is rare in the West but is the main cancer in ] and neighbouring countries, most likely due to the ] presence of ] and ] in that population. Similarly, with ] becoming more common in various Third World countries, ] cancer incidence has increased in a parallel fashion. | |||
| The three most common ]s are ] (34%), ]s (23%) and ]s (12%).<ref name=Euro10>{{cite journal | vauthors = Kaatsch P | title = Epidemiology of childhood cancer | journal = Cancer Treatment Reviews | volume = 36 | issue = 4 | pages = 277–285 | date = June 2010 | pmid = 20231056 | doi = 10.1016/j.ctrv.2010.02.003 }}</ref> In the United States cancer affects about 1 in 285 children.<ref name=Eli2014>{{cite journal | vauthors = Ward E, DeSantis C, Robbins A, Kohler B, Jemal A | title = Childhood and adolescent cancer statistics, 2014 | journal = CA | volume = 64 | issue = 2 | pages = 83–103 | date = January 2014 | pmid = 24488779 | doi = 10.3322/caac.21219 | s2cid = 34364885 | doi-access = free }}</ref> Rates of childhood cancer increased by 0.6% per year between 1975 and 2002 in the United States<ref>{{cite journal | vauthors = Ward EM, Thun MJ, Hannan LM, Jemal A | title = Interpreting cancer trends | journal = Annals of the New York Academy of Sciences | volume = 1076 | issue = 1 | pages = 29–53 | date = September 2006 | pmid = 17119192 | doi = 10.1196/annals.1371.048 | s2cid = 1579801 | bibcode = 2006NYASA1076...29W }}</ref> and by 1.1% per year between 1978 and 1997 in Europe.<ref name=Euro10/> Death from childhood cancer decreased by half between 1975 and 2010 in the United States.<ref name=Eli2014/> | |||
| == History == | == History == | ||
| {{Main|History of cancer}} | |||
| ] of the breast (pale area at the center) shows an oval tumor surrounded by spikes of whitish scar tissue in the surrounding yellow fatty tissue. The silhouette vaguely resembles a crab.]] | |||
| ] with two views of a Dutch woman who had a tumor removed from her neck in 1689]] | |||
| Today, the Greek term ] is the medical term for a malignant tumor derived from ] cells. It is ] who translated ''carcinos'' into the ] ''cancer'', also meaning crab. | |||
| Cancer has existed for all of human history.<ref name=Hist1/> The earliest written record regarding cancer is from {{circa|1600 BC}} in the Egyptian ] and describes breast cancer.<ref name=Hist1>{{cite journal |vauthors=Hajdu SI |s2cid=39667103 |title=A note from history: landmarks in history of cancer, part 1 |journal=Cancer |volume=117 |issue=5 |pages=1097–102 |date=March 2011 |pmid=20960499 |doi=10.1002/cncr.25553|doi-access=free }}</ref> ] ({{circa|460 BC|370 BC}}) described several kinds of cancer, referring to them with the ] word ] ''karkinos'' (crab or ]).<ref name=Hist1/> This name comes from the appearance of the cut surface of a solid malignant tumor, with "the veins stretched on all sides as the animal the crab has its feet, whence it derives its name".<ref>Paul of Aegina, 7th century AD, quoted in {{cite web | vauthors = Moss RW |title=Galen on Cancer |url=http://www.cancerdecisions.com/speeches/galen1989.html |archive-url=https://web.archive.org/web/20110716111312/http://www.cancerdecisions.com/speeches/galen1989.html |archive-date=16 July 2011 |publisher=CancerDecisions |year=2004 }} Referenced from Michael Shimkin, Contrary to Nature, Washington, DC: Superintendent of Document, DHEW Publication No. (NIH) 79–720, p. 35.</ref> ] stated that "cancer of the breast is so called because of the fancied resemblance to a crab given by the lateral prolongations of the tumor and the adjacent distended veins".<ref name="Majno2004">{{cite book | vauthors = Majno G, Joris I |title=Cells, Tissues, and Disease: Principles of General Pathology: Principles of General Pathology |url={{google books |plainurl=y |id=8yAf6U7njlcC |page=738}}|access-date=11 September 2013|date=12 August 2004|publisher=Oxford University Press|isbn=978-0-19-974892-1}}</ref>{{rp|738}} ] ({{circa|25 BC}} – 50 AD) translated ''karkinos'' into the ] ''cancer'', also meaning crab and recommended surgery as treatment.<ref name=Hist1/> ] (2nd century AD) disagreed with the use of surgery and recommended ] instead.<ref name=Hist1/> These recommendations largely stood for 1000 years.<ref name=Hist1/> | |||
| ] used "''oncos''" to describe ''all'' tumours, the root for the modern word ].<ref name="Galen">{{cite journal |author=Karpozilos A, Pavlidis N |title=The treatment of cancer in Greek antiquity |journal=Eur. J. Cancer |volume=40 |issue=14 |pages=2033–40 |year=2004 |pmid=15341975 |doi=10.1016/j.ejca.2004.04.036}}</ref> | |||
| In the 15th, 16th and 17th centuries, it became acceptable for doctors to ] to discover the cause of death.<ref name=Hist2>{{cite journal |vauthors=Hajdu SI |s2cid=28148111 |title=A note from history: landmarks in history of cancer, part 2 |journal=Cancer |volume=117 |issue=12 |pages=2811–20 |date=June 2011 |pmid=21656759 |doi=10.1002/cncr.25825|doi-access=free }}</ref> The German professor ] believed that breast cancer was caused by a milk clot in a mammary duct. The Dutch professor ], a follower of ], believed that all disease was the outcome of chemical processes and that acidic ] fluid was the cause of cancer. His contemporary ] believed that cancer was a poison that slowly spreads and concluded that it was ].<ref>{{cite book | vauthors = Yalom M |title=A history of the breast |year=1998 |publisher=Ballantine Books |location=New York |isbn=978-0-679-43459-7 |url={{google books |plainurl=y |id=FFX1U3KUjPsC}}|edition=1}}</ref> | |||
| ] described several kinds of cancers. He called benign tumours ''oncos'', ] for swelling, and malignant tumours ''carcinos'', Greek for ] or ]. This name comes from the appearance of the cut surface of a solid malignant tumour, with ''the veins stretched on all sides as the animal the crab has its feet, whence it derives its name''<ref>Paul of Aegina, 7th Century AD, quoted in Shimkin, op.cit., p. 35., </ref> (see picture). He later added the suffix ''-oma'', Greek for swelling, giving the name ''carcinoma''. Since it was against Greek tradition to open the body, Hippocrates only described and made drawings of outwardly visible tumors on the skin, nose, and breasts. Treatment was based on the ] of four bodily fluids (black and yellow bile, blood, and phlegm). According to the patient's humor, treatment consisted of diet, blood-letting, and/or laxatives. Through the centuries it was discovered that cancer could occur anywhere in the body, but humor-theory based treatment remained popular until the 19th century with the discovery of ]. | |||
| The physician John Hill described ] as the cause of nose cancer in 1761.<ref name=Hist2/> This was followed by the report in 1775 by British surgeon ] that ], a cancer of the ], was a common disease among ]s.<ref>{{cite journal |vauthors=Hajdu SI |title=A note from history: landmarks in history of cancer, part 3 |journal=Cancer |volume=118 |issue=4 |pages=1155–68 |date=February 2012 |pmid=21751192 |doi=10.1002/cncr.26320|s2cid=38892895 |doi-access=free }}</ref> With the widespread use of the microscope in the 18th century, it was discovered that the 'cancer poison' spread from the primary tumor through the lymph nodes to other sites ("]"). This view of the disease was first formulated by the English surgeon ] between 1871 and 1874.<ref>{{cite journal | vauthors = Grange JM, Stanford JL, Stanford CA | title = Campbell De Morgan's 'Observations on cancer', and their relevance today | journal = Journal of the Royal Society of Medicine | volume = 95 | issue = 6 | pages = 296–299 | date = June 2002 | pmid = 12042378 | pmc = 1279913 | doi = 10.1177/014107680209500609 }}</ref> | |||
| Our oldest description and ] treatment of cancer was discovered in Egypt and dates back to approximately 1600 B.C. The ] describes 8 cases of ulcers of the breast that were treated by cauterization, with a tool called "the fire drill." The writing says about the disease, "There is no treatment."<ref name=CancerOrgHistory>American Cancer Society, , ''History of Cancer''</ref> | |||
| == Society and culture == | |||
| Another very early ] treatment for cancer was described in the 1020s by ] (Ibn Sina) in '']''. He stated that the ] should be radical and that all diseased ] should be removed, which included the use of ] or the removal of ]s running in the direction of the ]. He also recommended the use of ] for the area being treated if necessary.<ref name=Patricia>Patricia Skinner (2001), , ''Encyclopedia of Alternative Medicine''</ref> | |||
| Although many diseases (such as heart failure) may have a worse prognosis than most cases of cancer, cancer is the subject of widespread fear and taboos. The ] of "a long illness" to describe cancers leading to death is still commonly used in obituaries, rather than naming the disease explicitly, reflecting an apparent ].<ref>{{Cite news | vauthors = Barbara E |author-link=Barbara Ehrenreich |title=Welcome to Cancerland |newspaper=] |date=November 2001 |issn=0017-789X |url=http://www.barbaraehrenreich.com/cancerland.htm |archive-url=https://web.archive.org/web/20131108181820/http://www.barbaraehrenreich.com/cancerland.htm |archive-date=8 November 2013}}</ref> Cancer is also euphemised as "the C-word";<ref>{{cite journal | vauthors = Pozorski A |s2cid=160969212 |title=Confronting the "C" Word: Cancer and Death in Philip Roth's Fiction |journal=Philip Roth Studies |date=20 March 2015 |volume=11 |issue=1 |pages=105–123 |doi=10.5703/philrothstud.11.1.105 |url=https://muse.jhu.edu/article/577333/pdf |access-date=13 April 2020 |language=en |issn=1940-5278}}</ref><ref>{{cite news | vauthors = Wollaston S |title=The C-Word review – a wonderful testament to a woman who faced cancer with honesty, verve and wit |url=https://www.theguardian.com/tv-and-radio/2015/may/04/the-c-word-review-sheridan-smith-cancer-wonderful-testament |access-date=13 April 2020 |work=The Guardian |date=4 May 2015}}</ref><ref>{{cite news |title=Avoiding the 'C' Word for Low-Risk Thyroid Cancer |url=https://www.medscape.com/viewarticle/901265 |access-date=13 April 2020 |work=Medscape}}</ref> ] uses the term to try to lessen the fear around the disease.<ref>{{cite news |title=The C word: how we react to cancer today |url=https://www.networks.nhs.uk/news/the-c-word-how-we-react-to-cancer-today |website=NHS Networks |access-date=13 April 2020 |language=en-gb |archive-date=22 October 2020 |archive-url=https://web.archive.org/web/20201022210915/https://www.networks.nhs.uk/news/the-c-word-how-we-react-to-cancer-today }}</ref> In Nigeria, one local name for cancer translates into English as "the disease that cannot be cured".<ref name=":0">{{Cite book|url=https://books.google.com/books?id=Tmrp7dkvJk4C&pg=PA196|title=Handbook of Psychiatry in Palliative Medicine| vauthors = Chochinov HM, Breitbart W |date=2009|publisher=Oxford University Press|isbn=978-0-19-530107-6|page=196|language=en}}</ref> This deep belief that cancer is necessarily a difficult and usually deadly disease is reflected in the systems chosen by society to compile cancer statistics: the most common form of cancer—non-melanoma ]s, accounting for about one-third of cancer cases worldwide, but very few deaths<ref name="Bolognia">{{cite book | vauthors = Rapini RP, Bolognia JL, Jorizzo JL |title=Dermatology: 2-Volume Set |publisher=Mosby |location=St. Louis |year=2007 |isbn=978-1-4160-2999-1 }}</ref><ref>{{cite web |title=Skin cancers |url=https://www.who.int/uv/faq/skincancer/en/index1.html |publisher=World Health Organization |access-date=19 January 2011 |url-status=live |archive-url=https://web.archive.org/web/20100927065836/http://www.who.int/uv/faq/skincancer/en/index1.html |archive-date=27 September 2010}}</ref>—are excluded from cancer statistics specifically because they are easily treated and almost always cured, often in a single, short, outpatient procedure.<ref>{{cite book | vauthors = McCulley M, Greenwell P |title=Molecular therapeutics: 21st-century medicine |publisher=J. Wiley |location=London |year=2007 |page=207 |url={{google books |plainurl=y |id=aG3SNAEACAAJ0470019166}} |isbn=978-0-470-01916-0 }}{{dead link|date=July 2023 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> | |||
| In the 16th and 17th centuries, it became more acceptable for doctors to ] to discover the cause of death. The German professor ] believed that breast cancer was caused by a milk clot in a mammary duct. The Dutch professor ], a follower of ], believed that all disease was the outcome of chemical processes, and that acidic ] fluid was the cause of cancer. His contemporary ] believed that cancer was a poison that slowly spreads, and concluded that it was ].<ref name="Marilyn Yalom"> | |||
| Western conceptions of ] for people with cancer include a duty to fully disclose the medical situation to the person, and the right to engage in ] in a way that respects the person's own values. In other cultures, other rights and values are preferred. For example, most African cultures value whole families rather than ]. In parts of Africa, a diagnosis is commonly made so late that cure is not possible, and treatment, if available at all, would quickly bankrupt the family. As a result of these factors, African healthcare providers tend to let family members decide whether, when and how to disclose the diagnosis, and they tend to do so slowly and circuitously, as the person shows interest and an ability to cope with the grim news.<ref name=:0/> People from Asian and South American countries also tend to prefer a slower, less candid approach to disclosure than is idealized in the United States and Western Europe, and they believe that sometimes it would be preferable not to be told about a cancer diagnosis.<ref name=:0/> In general, disclosure of the diagnosis is more common than it was in the 20th century, but full disclosure of the prognosis is not offered to many patients around the world.<ref name=:0/> | |||
| Marilyn Yalom "A history of the breast" 1997. New York: Alfred A. Knopf. ISBN 0-679-43459-3</ref> | |||
| In the United States and some other cultures, cancer is regarded as a disease that must be "fought" to end the "civil insurrection"; a ] was declared in the US. Military metaphors are particularly common in descriptions of cancer's human effects, and they emphasize both the state of the patient's health and the need to take immediate, decisive actions himself rather than to delay, to ignore or to rely entirely on others. The military metaphors also help rationalize radical, destructive treatments.<ref name="Gwyn">{{cite book | vauthors = Low G, Cameron L |title=Researching and Applying Metaphor |chapter-url={{google books |plainurl=y |id=8aOxMvo_ag8C}}|year=1999|publisher=Cambridge University Press|isbn=978-0-521-64964-3| chapter=10}}</ref><ref>{{cite book | vauthors = Sulik GA |title=Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health |url={{google books |plainurl=y |id=_it2CwAAQBAJ |page=78}}|year=2010|publisher=Oxford University Press|isbn=978-0-19-974993-5|pages=78–89}}</ref> | |||
| With the widespread use of the microscope in the 18th century, it was discovered that the 'cancer poison' spread from the primary tumor through the lymph nodes to other sites ("]"). This view of the disease was first formulated by the English surgeon ] between 1871 and 1874.<ref>{{cite journal |author=Grange JM, Stanford JL, Stanford CA |title=Campbell De Morgan's 'Observations on cancer', and their relevance today |journal=Journal of the Royal Society of Medicine |volume=95 |issue=6 |pages=296–9 |year=2002 |url=http://www.jrsm.org/cgi/content/full/95/6/296|pmid=12042378|doi=10.1258/jrsm.95.6.296}}</ref> The use of ] to treat cancer had poor results due to problems with hygiene. The renowned Scottish surgeon ] saw only 2 breast tumor patients out of 60 surviving surgery for two years. In the 19th century, ] improved surgical hygiene and as the survival statistics went up, surgical removal of the tumor became the primary treatment for cancer. With the exception of ] who in the late 1800s felt that the rate of cure after surgery had been higher ''before'' asepsis (and who injected bacteria into tumors with mixed results), cancer treatment became dependent on the individual art of the surgeon at removing a tumor. During the same period, the idea that the body was made up of various ], that in turn were made up of millions of cells, laid rest the humor-theories about chemical imbalances in the body. The age of ] was born. | |||
| In the 1970s, a relatively popular ] in the US was a specialized form of ], based on the idea that cancer was caused by a bad attitude.<ref name=Olson/> People with a "cancer personality"—depressed, repressed, self-loathing and afraid to express their emotions—were believed to have manifested cancer through subconscious desire. Some psychotherapists claimed that treatment to change the patient's outlook on life would cure the cancer.<ref name=Olson/> Among other effects, this belief allowed society to ] for having caused the cancer (by "wanting" it) or having prevented its cure (by not becoming a sufficiently happy, fearless and loving person).<ref name=Ehrenreich/> It also increased patients' anxiety, as they incorrectly believed that natural emotions of sadness, anger or fear shorten their lives.<ref name=Ehrenreich/> The idea was ridiculed by ], who published '']'' while recovering from treatment for breast cancer in 1978.<ref name=Olson>{{cite book | vauthors = Olson JS |title=Bathsheba's Breast: Women, Cancer, and History |url={{google books |plainurl=y |id=gp9aMBieClMC |page=145}}|year=2005|publisher=JHU Press|isbn=978-0-8018-8064-3| pages = 145–70 | oclc = 186453370 }}</ref> Although the original idea is now generally regarded as nonsense, the idea partly persists in a reduced form with a widespread, but incorrect, belief that deliberately cultivating a habit of ] will increase survival.<ref name=Ehrenreich>{{cite book | vauthors = Ehrenreich B |author-link=Barbara Ehrenreich |title=Bright-sided: How the Relentless Promotion of Positive Thinking Has Undermined America |url={{google books |plainurl=y |id=wxJlvB7bCO4C |page=15}}|year=2009|publisher=Henry Holt and Company|isbn=978-0-8050-8749-9| pages = 15–44 }}</ref> This notion is particularly strong in ].<ref name=Ehrenreich /> | |||
| When ] and ] discovered ] at the end of the 19th century, they stumbled upon the first effective non-surgical cancer treatment. With radiation came also the first signs of multi-disciplinary approaches to cancer treatment. The surgeon was no longer operating in isolation, but worked together with hospital radiologists to help patients. The complications in communication this brought, along with the necessity of the patient's treatment in a hospital facility rather than at home, also created a parallel process of compiling patient data into hospital files, which in turn led to the first statistical patient studies. | |||
| One idea about why people with cancer are blamed or stigmatized, called the ], is that blaming cancer on the patient's actions or attitudes allows the blamers to regain a sense of control. This is based upon the blamers' belief that the world is fundamentally just and so any dangerous illness, like cancer, must be a type of punishment for bad choices, because in a just world, bad things would not happen to good people.<ref>{{Cite news |title=A Sick Stigma: Why are cancer patients blamed for their illness? |date=24 September 2013 |url=http://www.slate.com/articles/health_and_science/medical_examiner/2013/09/cancer_stigma_don_t_blame_patients_for_their_disease_no_matter_what_the.html |newspaper=Slate | vauthors = Huff C |url-status=live |archive-url=https://web.archive.org/web/20131011120507/http://www.slate.com/articles/health_and_science/medical_examiner/2013/09/cancer_stigma_don_t_blame_patients_for_their_disease_no_matter_what_the.html |archive-date=11 October 2013}}</ref> | |||
| Cancer patient treatment and studies were restricted to individual physicians' practices until ], when medical research centers discovered that there were large international differences in disease incidence. This insight drove national public health bodies to make it possible to compile health data across practises and hospitals, a process that many countries do today. The Japanese medical community observed that the bone marrow of bomb victims in ] and ] was completely destroyed. They concluded that diseased ] could also be destroyed with radiation, and this led to the discovery of bone marrow transplants for ]. Since WWII, trends in ] are to improve on a micro-level the existing treatment methods, standardize them, and globalize them as a way to find cures through ] and international partnerships. | |||
| === Economic effect === | |||
| The total health care expenditure on cancer in the US was estimated to be $80.2 billion in 2015.<ref>{{cite web |title=Economic Impact of Cancer |url=https://www.cancer.org/cancer/cancer-basics/economic-impact-of-cancer.html |website=American Cancer Society |date=3 January 2018 |access-date=5 July 2018}}</ref> Even though cancer-related health care expenditure have increased in absolute terms during recent decades, the share of health expenditure devoted to cancer treatment has remained close to 5% between the 1960s and 2004.<ref>{{cite journal |vauthors=Bosanquet N, Sikora K |title=The economics of cancer care in the UK |journal=Lancet Oncology |volume=5 |issue=9 |pages=568–74 |year=2004 |pmid=15337487 |doi=10.1016/S1470-2045(04)01569-4}}</ref><ref>{{cite journal |vauthors=Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML |title=Projections of the cost of cancer care in the United States: 2010–2020 |journal=Journal of the National Cancer Institute |volume=103 |issue=2 |pages=117–28 |year=2011 |pmid=21228314 |pmc=3107566 |doi=10.1093/jnci/djq495}}</ref> A similar pattern has been observed in Europe where about 6% of all health care expenditure are spent on cancer treatment.<ref>{{cite journal |vauthors=Jönsson B, Hofmarcher T, Lindgren P, Wilking N |title=The cost and burden of cancer in the European Union 1995–2014 |journal=European Journal of Cancer |volume=66 |issue=Oct |pages=162–70 |year=2016 |pmid=27589247 |doi=10.1016/j.ejca.2016.06.022}}</ref><ref name=EJC2018>{{cite journal |vauthors=Hofmarcher T, Lindgren P, Wilking N, Jönsson B |title=The cost of cancer in Europe 2018 |journal=European Journal of Cancer |volume=129 |issue=Apr |pages=41–49 |year=2020 |pmid=32120274 |doi=10.1016/j.ejca.2020.01.011|doi-access=free }}</ref> In addition to health care expenditure and ], cancer causes indirect costs in the form of productivity losses due to sick days, permanent incapacity and disability as well as premature death during working age. Cancer causes also costs for informal care. Indirect costs and informal care costs are typically estimated to exceed or equal the health care costs of cancer.<ref>{{cite journal |vauthors=Luengo-Fernandez R, Leal J, Gray A, Sullivan R |title=Economic burden of cancer across the European Union: a population-based cost analysis |journal=Lancet Oncology |volume=14 |issue=12 |pages=1165–74 |year=2013 |pmid=24131614 |doi=10.1016/S1470-2045(13)70442-X}}</ref><ref name=EJC2018 /> | |||
| ==Research== | |||
| {{main|Cancer research}} | |||
| === Workplace === | |||
| In the United States, cancer is included as a protected condition by the ] (EEOC), mainly due to the potential for cancer having discriminating effects on workers.<ref name="EEOC">U.S. Equal Employment Opportunity Commission. "Questions & Answers about Cancer in the Workplace and the Americans with Disabilities Act (ADA)." https://www.eeoc.gov/laws/types/cancer.cfm</ref> Discrimination in the workplace could occur if an employer holds a false belief that a person with cancer is not capable of doing a job properly, and may ask for more ] than other employees. Employers may also make hiring or firing decisions based on misconceptions about cancer disabilities, if present. The EEOC provides interview guidelines for employers, as well as lists of possible solutions for assessing and accommodating employees with cancer.<ref name="EEOC" /> | |||
| Cancer research is the intense scientific effort to understand disease processes and discover possible therapies. The improved understanding of ] and ] due to cancer research has led to a number of new, effective treatments for cancer since President Nixon declared "War on Cancer" in 1971. | |||
| === Effect on divorce === | |||
| ==See also== | |||
| * ] | |||
| A study found women were around six times more likely to be ] soon after a diagnosis of cancer compared to men.<ref>{{cite journal | vauthors = Glantz MJ, Chamberlain MC, Liu Q, Hsieh CC, Edwards KR, Van Horn A, Recht L | title = Gender disparity in the rate of partner abandonment in patients with serious medical illness | journal = Cancer | volume = 115 | issue = 22 | pages = 5237–5242 | date = November 2009 | pmid = 19645027 | doi = 10.1002/cncr.24577 }}</ref> Rate of separation for cancer-survivors showed correlations with race, age, income, and ] in a study.<ref>{{cite journal | vauthors = Stephens C, Westmaas JL, Kim J, Cannady R, Stein K | title = Gender differences in associations between cancer-related problems and relationship dissolution among cancer survivors | journal = Journal of Cancer Survivorship | volume = 10 | issue = 5 | pages = 865–873 | date = October 2016 | pmid = 26995006 | doi = 10.1007/s11764-016-0532-9 }}</ref> A review found a somewhat decreased divorce rate for most cancer types, and noted ] and ] weaknesses for many studies on effects of cancer on divorce.<ref>{{cite journal | vauthors = Fugmann D, Boeker M, Holsteg S, Steiner N, Prins J, Karger A | title = A Systematic Review: The Effect of Cancer on the Divorce Rate | journal = Frontiers in Psychology | volume = 13 | page = 828656 | date = 9 March 2022 | pmid = 35356338 | pmc = 8959852 | doi = 10.3389/fpsyg.2022.828656 | doi-access = free }}</ref> | |||
| * ] | |||
| * ] (AACR) | |||
| == Research == | |||
| * ] (ACS) | |||
| {{Main|Cancer research}} | |||
| * ] (ASCO) | |||
| ]]] | |||
| * ] (EORTC) | |||
| Because cancer is a class of diseases,<ref name=WhatIsCancerNCI>{{cite web |url=https://www.cancer.gov/about-cancer/understanding/what-is-cancer |title=What Is Cancer? |publisher=] |access-date=28 March 2018|date=17 September 2007}}</ref><ref>{{cite web |url=http://www.atsdr.cdc.gov/COM/cancer-fs.html |title=Cancer Fact Sheet |publisher=Agency for Toxic Substances & Disease Registry |date=30 August 2002 |access-date=17 August 2009 |archive-url=https://web.archive.org/web/20090813142933/http://www.atsdr.cdc.gov/COM/cancer-fs.html |archive-date=13 August 2009}}</ref> it is unlikely that there will ever be a single "]" any more than there will be a single treatment for all ]s.<ref>{{cite web |url=http://www.livescience.com/health/060919_bad_cancer.html |title=Exciting New Cancer Treatments Emerge Amid Persistent Myths | vauthors = Wanjek C |website=] |date=16 September 2006 |access-date=17 August 2009 |url-status=live |archive-url=https://web.archive.org/web/20080516080512/http://www.livescience.com/health/060919_bad_cancer.html |archive-date=16 May 2008}}</ref> ]s were once incorrectly thought to have potential as a "]" treatment applicable to many types of cancer.<ref>{{cite journal |vauthors=Hayden EC |title=Cutting off cancer's supply lines |journal=Nature |volume=458 |issue=7239 |pages=686–87 |date=April 2009 |pmid=19360048 |doi=10.1038/458686b|doi-access=free }}</ref> Angiogenesis inhibitors and other cancer therapeutics are used in combination to reduce cancer morbidity and mortality.<ref>{{cite journal |vauthors=Bagri A, Kouros-Mehr H, Leong KG, Plowman GD |title=Use of anti-VEGF adjuvant therapy in cancer: challenges and rationale |journal=Trends in Molecular Medicine |volume=16 |issue=3 |pages=122–32 |date=March 2010 |pmid=20189876 |doi=10.1016/j.molmed.2010.01.004}}</ref> | |||
| * ] (NCI) | |||
| * ] (NCCN) | |||
| ]s are studied in ]s to compare the proposed treatment to the best existing treatment. Treatments that succeeded in one cancer type can be tested against other types.<ref>{{cite journal |vauthors=Sleigh SH, Barton CL |s2cid=25267555 |title=Repurposing Strategies for Therapeutics |journal=Pharmaceutical Medicine|volume=24 |issue=3 |pages=151–59 |year=2010 |doi=10.1007/BF03256811 }}</ref> Diagnostic tests are under development to better target the right therapies to the right patients, based on their individual biology.<ref>{{cite journal |vauthors=Winther H, Jorgensen JT |s2cid=43505621 |title=Drug-Diagnostic Co-Development in Cancer |journal=Pharmaceutical Medicine |volume=24 |issue=6 |pages=363–75 |year=2010 |doi=10.1007/BF03256837 }}</ref> | |||
| Cancer research focuses on the following issues: | |||
| * Agents (e.g. viruses) and events (e.g. mutations) that cause or facilitate genetic changes in cells destined to become cancer. | |||
| * The precise nature of the genetic damage and the genes that are affected by it. | |||
| * The consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell and in facilitating additional genetic events that lead to further progression of the cancer. | |||
| The improved understanding of ] and ] due to cancer research has led to new treatments for cancer since US President ] declared the "]" in 1971. Since then, the country has spent over $200 billion on cancer research, including resources from public and private sectors.<ref>{{cite web | vauthors = Begley S |url=http://www.newsweek.com/id/157548/page/2 |title=Rethinking the War on Cancer |date=16 September 2008 |website=Newsweek |access-date=8 September 2008 |archive-url=https://web.archive.org/web/20080910012446/http://www.newsweek.com/id/157548/page/2 |archive-date=10 September 2008}}</ref> The cancer death rate (adjusting for size and age of the population) declined by five percent between 1950 and 2005.<ref name="24cancer">{{cite news |url=https://www.nytimes.com/2009/04/24/health/policy/24cancer.html |url-access=subscription |title=Advances Elusive in the Drive to Cure Cancer | vauthors = Kolata G |date=23 April 2009 |work=] |access-date=5 May 2009 |url-status=live |archive-url=https://web.archive.org/web/20120114120509/http://www.nytimes.com/2009/04/24/health/policy/24cancer.html |archive-date=14 January 2012}}</ref> | |||
| Competition for financial resources appears to have suppressed the creativity, cooperation, risk-taking and original thinking required to make fundamental discoveries, unduly favoring low-risk research into small incremental advancements over riskier, more innovative research. Other consequences of competition appear to be many studies with dramatic claims whose results cannot be replicated and perverse incentives that encourage grantee institutions to grow without making sufficient investments in their own faculty and facilities.<ref>{{cite journal | vauthors = Alberts B, Kirschner MW, Tilghman S | author-link1 = Bruce Alberts | author-link4 = Harold Varmus |year=2014 |title=Rescuing US biomedical research from its systemic flaws |bibcode-access=free |journal=Proceedings of the National Academy of Sciences of the United States of America |volume=111 |issue=16 |pages=5773–77 |doi=10.1073/pnas.1404402111 |pmid=24733905 |pmc=4000813|bibcode=2014PNAS..111.5773A |doi-access=free }}</ref><ref name=24cancer/><ref>{{cite news |url=https://www.nytimes.com/2009/06/28/health/research/28cancer.html |url-access=subscription |title=Grant System Leads Cancer Researchers to Play It Safe | vauthors = Kolata G |date=27 June 2009 |work=The New York Times |access-date=29 December 2009 |url-status=live |archive-url=https://web.archive.org/web/20110608133344/http://www.nytimes.com/2009/06/28/health/research/28cancer.html |archive-date=8 June 2011}}</ref><ref>{{cite journal | vauthors = Powell K |s2cid=4465686 |year=2016 |title=Young, talented and fed-up: scientists tell their stories |journal=Nature |volume=538 |issue= 7626|pages=446–49 |doi=10.1038/538446a |pmid=27786221|bibcode=2016Natur.538..446P |doi-access=free }}</ref> | |||
| ], which uses convert viruses, is being studied. | |||
| In the wake of the ] pandemic, there has been a worry that cancer research and treatment are slowing down.<ref>{{Cite web|url=https://www.nbcnews.com/think/opinion/covid-s-impact-cancer-care-turning-oncologists-worst-fears-reality-ncna1257743|title = Opinion | I'm an oncologist. My worst fears about Covid and cancer are coming true|website = ]| date=12 February 2021 }}</ref><ref>{{Cite web|url=https://www.nydailynews.com/opinion/ny-oped-dont-sacrifice-cancer-care-to-covid-20210113-nesit6kuunfenpjcl2lpo2ftny-story.html|title=Don't sacrifice cancer care to COVID|website=]|date=13 January 2021 }}</ref> | |||
| On 2 December 2023, ] published a groundbreaking discovery involving "NK cell-engaging nanodrones" for targeted cancer treatment. The development of "NK cell-engaging nanodrones" represents a significant leap forward in cancer treatment, showcasing how cutting-edge nanotechnology and immunotherapy can be combined to target and eliminate cancer cells with unprecedented precision. These nanodrones are designed to harness the power of natural killer (NK) cells, which play a crucial role in the body's immune response against tumors. By directing these NK cells specifically to the sites of tumors, the nanodrones can effectively concentrate the immune system's attack on the cancer cells, potentially leading to better outcomes for patients.<ref name=:2/> | |||
| The key innovation here lies in the use of protein cage nanoparticle-based systems. These systems are engineered to carry signals that attract NK cells directly to the tumor, overcoming one of the major challenges in cancer immunotherapy: ensuring that the immune cells find and attack only the cancer cells without harming healthy tissue. This targeted approach not only increases the efficacy of the treatment but also minimizes side effects, a common concern with broader-acting cancer therapies.<ref name=":2">{{Cite web |title=Revolutionary nanodrones enable targeted cancer treatment |url=https://www.sciencedaily.com/releases/2023/12/231229164725.htm |access-date=2024-03-24 |website=ScienceDaily |language=en}}</ref> | |||
| == Pregnancy == | |||
| Cancer affects approximately 1 in 1,000 pregnant women. The most common cancers found during pregnancy are the same as the most common cancers found in non-pregnant women during childbearing ages: breast cancer, cervical cancer, leukemia, lymphoma, melanoma, ovarian cancer and colorectal cancer.<ref name=yarbro/> | |||
| Diagnosing a new cancer in a pregnant woman is difficult, in part because any symptoms are commonly assumed to be a normal discomfort associated with pregnancy. As a result, cancer is typically discovered at a somewhat later stage than average. Some imaging procedures, such as ] (magnetic resonance imaging), ]s, ultrasounds and ] with fetal shielding are considered safe during pregnancy; some others, such as ], are not.<ref name=yarbro/> | |||
| Treatment is generally the same as for non-pregnant women. However, radiation and radioactive drugs are normally avoided during pregnancy, especially if the fetal dose might exceed 100 cGy. In some cases, some or all treatments are postponed until after birth if the cancer is diagnosed late in the pregnancy. Early deliveries are often used to advance the start of treatment. Surgery is generally safe, but pelvic surgeries during the first trimester may cause miscarriage. Some treatments, especially certain chemotherapy drugs given during the ], increase the risk of ]s and pregnancy loss (spontaneous abortions and stillbirths).<ref name=yarbro/> | |||
| Elective abortions are not required and, for the most common forms and stages of cancer, do not improve the mother's survival. In a few instances, such as advanced uterine cancer, the pregnancy cannot be continued and in others, the patient may end the pregnancy so that she can begin aggressive chemotherapy.<ref name=yarbro/> | |||
| Some treatments can interfere with the mother's ability to give birth vaginally or to breastfeed.<ref name=yarbro/> Cervical cancer may require birth by ]. Radiation to the breast reduces the ability of that breast to produce milk and increases the risk of ]. Also, when chemotherapy is given after birth, many of the drugs appear in breast milk, which could harm the baby.<ref name=yarbro>{{cite book | vauthors = Yarbro CH, Wujcik D, Gobel BH |title=Cancer Nursing: Principles and Practice |url={{google books |plainurl=y |id=LJVTQs4QjJ0C |page=901}}|year=2010|publisher=Jones & Bartlett Learning|isbn=978-0-7637-6357-2|pages = 901–905}}</ref> | |||
| == Other animals == | |||
| ], concentrating mainly on cats and dogs, is a growing specialty in wealthy countries and the major forms of human treatment such as surgery and radiotherapy may be offered. The most common types of cancer differ, but the cancer burden seems at least as high in pets as in humans. Animals, typically rodents, are often used in cancer research and studies of natural cancers in larger animals may benefit research into human cancer.<ref>{{cite journal | vauthors = Thamm D |title=How companion animals contribute to the fight against cancer in humans |journal=Veterinaria Italiana |date=March 2009 |volume=54 |issue=1 |pages=111–20 |pmid=20391394 |url=http://www.izs.it/vet_italiana/2009/45_1/111.pdf |access-date=18 July 2014 |url-status=live |archive-url=https://web.archive.org/web/20140723044907/http://www.izs.it/vet_italiana/2009/45_1/111.pdf |archive-date=23 July 2014}}</ref> | |||
| Across wild animals, there is still limited data on cancer. Nonetheless, a study published in 2022, explored cancer risk in (non-domesticated) zoo mammals, belonging to 191 species, 110,148 individual, demonstrated that cancer is a ubiquitous disease of mammals and it can emerge anywhere along the mammalian phylogeny.<ref>{{cite journal | vauthors = Vincze O, Colchero F, Lemaître JF, Conde DA, Pavard S, Bieuville M, Urrutia AO, Ujvari B, Boddy AM, Maley CC, Thomas F, Giraudeau M | title = Cancer risk across mammals | journal = Nature | volume = 601 | issue = 7892 | pages = 263–267 | date = January 2022 | pmid = 34937938 | pmc = 8755536 | doi = 10.1038/s41586-021-04224-5 | s2cid = 245425871 | bibcode = 2022Natur.601..263V }}</ref> This research also highlighted that cancer risk is not uniformly distributed along mammals. For instance, species in the order ] are particularly prone to be affected by cancer (e.g. over 25% of ]s, ]es and ] die of cancer), while ]s (especially ]s) appear to face consistently low cancer risks. | |||
| In non-humans, a few types of ] have also been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with ] (also known as canine transmissible venereal tumor), and in ] with ] (DFTD).<ref name="pmid16901782">{{cite journal |vauthors=Murgia C, Pritchard JK, Kim SY, Fassati A, Weiss RA |title=Clonal origin and evolution of a transmissible cancer |journal=Cell |volume=126 |issue=3 |pages=477–87 |date=August 2006 |pmid=16901782 |pmc=2593932 |doi=10.1016/j.cell.2006.05.051}}</ref> | |||
| == See also == | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| ==References== | |||
| == References == | |||
| {{reflist|2}} | |||
| {{reflist}} | |||
| ===General references=== | |||
| == Further reading == | |||
| * ''The Basic Science of Oncology.'' Tannock IF, Hill RP ''et al'' (eds) 4th ed.2005 McGraw-Hill. ISBN 0-07138-774-9. | |||
| {{refbegin}} | |||
| * ''Principles of Cancer Biology.'' Kleinsmith, LJ (2006). Pearson Benjamin Cummings. ISBN 0-80534-003-3. | |||
| * {{cite book | vauthors = Bast RC, Croe CM, Hait WN, Hong WK, Kufe DW, Piccart-Gebhart M, Pollock RE, Weichselbaum RR, Yang H, Holland JF |title=Holland-Frei Cancer Medicine |url={{google books |plainurl=y |id=onCBjwEACAAJ}} |year=2016 |publisher=Wiley |isbn=978-1-118-93469-2}} | |||
| * {{cite journal | author = Parkin D, Bray F, Ferlay J, Pisani P | title = Global cancer statistics, 2002 | journal = CA Cancer J Clin | volume = 55 | issue = 2 | pages = 74–108 | year = | doi = 10.3322/canjclin.55.2.74 | doi_brokendate = 2008-06-26 }}'''' | |||
| * {{cite book | vauthors = Kleinsmith LJ |title=Principles of cancer biology |url={{google books |plainurl=y |id=LKVrAAAAMAAJ}}|year=2006|publisher=Pearson Benjamin Cummings|isbn=978-0-8053-4003-7}} | |||
| * ''Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective''. World Cancer Research Fund (2007). ISBN 978-0-9722522-2-5. '''' | |||
| * {{cite book |last=Mukherjee |first=Siddhartha |author-link=Siddhartha Mukherjee |title=The Emperor of All Maladies: A Biography of Cancer |year=2010 |publisher=Simon & Schuster |isbn=978-1-4391-0795-9 |url=https://archive.org/details/emperorofallmala00mukh |access-date=7 August 2013 }} | |||
| * Textbook | |||
| * {{cite book | vauthors = Pazdur R, Camphausen KA, Wagman LD, Hoskins WJ |title=Cancer Management: A Multidisciplinary Approach | year=2009 | publisher = Cmp United Business Media | isbn = 978-1-891483-62-2 | url = http://www.cancernetwork.com/cancer-management-11 | archive-url = https://web.archive.org/web/20090515031918/http://www.cancernetwork.com/cancer-management-11 | archive-date = 15 May 2009 | id = {{google books |id=wbLnPAAACAAJ}} }} | |||
| * {{cite journal | author=Robert A. Weinberg | title=How Cancer Arises; An explosion of research is uncovering the long-hidden molecular underpinnings of cancer—and suggesting new therapies | url=http://www.bme.utexas.edu/research/orly/teaching/BME303/Weinberg.pdf | publication=Scientific American | month=September | year=1996 | pages=62–70 | quote=Introductary explanation of cancer biology in layman's language | format=PDF }} | |||
| * {{cite book | vauthors = Schwab M |title=Encyclopedia of Cancer |url={{google books |plainurl=y |id=mLUEf1kbbDgC}}|year= 2008|publisher=Springer Science & Business Media|isbn=978-3-540-36847-2}} | |||
| * {{cite book | vauthors = Tannock I |title=The basic science of oncology |url={{google books |plainurl=y |id=Bb4F4pj2BdYC}}|year=2005|publisher=McGraw-Hill Professional|isbn=978-0-07-138774-3}} | |||
| ==External links== | |||
| {{ |
{{refend}} | ||
| {{Commons|Cancer (illness)}} | |||
| == External links == | |||
| * {{dmoz|Health/Conditions_and_Diseases/Cancer/}} | |||
| {{wikiversity|Cell biology/Cancer}} | |||
| * {{Yahoo directory|Health/Diseases_and_Conditions/Cancers/|Cancer}} | |||
| {{EB1911 poster|Cancer}} | |||
| {{Commons category|Cancers}} | |||
| ===Professional and research=== | |||
| ;Global | |||
| * (WHO) | | |||
| * A review of worldwide strategies for the prevention and treatment of cancer. | |||
| * at '']'' | |||
| * | |||
| * | |||
| * (including cancer) by a Joint ]/] Expert consultation (2003) | |||
| * National Firefighter Registry (NFR) for Cancer, ], USA | |||
| * leads a global network of cancer charities. Its carries detailed analysis on the global origins and prevention of cancer. | |||
| * , EU OSHA. The site shares information to help prevent workers from being exposed to carcinogens in the workplace. | |||
| * An ] Program to establish cancer care capacity and comprehensive cancer control in developing world | |||
| * , NIOSH. | |||
| * NIOSH Pocket guide to chemical hazards, . | |||
| ;North America | |||
| {{Medical condition classification and resources | |||
| * | |||
| | DiseasesDB = 28843 | |||
| * | |||
| | ICD10 ={{ICD10|C00-C97}} | |||
| * – Trusted tools for helping patients make informed decisions | |||
| | ICD9 = {{ICD9|140}}—{{ICD9|239}} | |||
| * | |||
| | ICDO = | |||
| * | |||
| | MedlinePlus = 001289 | |||
| * – Oncologist-approved cancer information | |||
| | eMedicineSubj = | |||
| * | |||
| | eMedicineTopic = | |||
| * Information for patients diagnosed with cancer, provided by the College of American Pathologists. | |||
| | MeshID = D009369 | |||
| * - 2005 United States Cancer Statistics | |||
| }} | |||
| * | |||
| {{Tumors|state=uncollapsed}} | |||
| * US Government agency responsible for conducting and supporting research, training, health information dissemination, and other programs with respect to the cause, diagnosis, prevention, and treatment of cancer, rehabilitation from cancer, and the continuing care of cancer patients and the families of cancer patients. | |||
| {{Disease groups}} | |||
| * - This publication reports cancer incidence and mortality in Canada, analyzed by gender, age and province/territory. | |||
| {{Authority control}} | |||
| * Textbook | |||
| ] | |||
| ;South America | |||
| * | |||
| ;Europe | |||
| * European Organization for Research and Treatment of Cancer. A European non-profit organization that sets up and executes clinical trials. | |||
| * UK cancer information charity. | |||
| * One of the world's foremost independent cancer research organisations, based in the United Kingdom. | |||
| ===Support and advocacy=== | |||
| * Patient advocate group | |||
| * | |||
| * : An ] Program to establish cancer care capacity and comprehensive cancer control in developing world | |||
| * from ] - provides links to news, general sites, diagnosis, treatment and alternative therapies, clinical trials, research, related issues, organizations, other MedlinePlus and . | |||
| * - In-depth, up-to-date information for people with a professional or general interest in cancer and health. | |||
| * - Australia's national non-government cancer control organisation, involved in research, information, prevention, patient treatment and support. | |||
| * ACOR is a unique collection of online communities designed to provide timely and accurate information in a supportive environment. ACOR offers access to mailing lists that provide support, information, and community to everyone affected by cancer and related disorders. | |||
| * Multimedia guide to cancer biology from Cold Spring Harbor Laboratory | |||
| * | |||
| {{Tumors}} | |||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| {{Link FA|hu}} | |||
| {{Link FA|vi}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 07:25, 30 December 2024
Group of diseases involving cell growth This article is about the group of diseases. For other uses, see Cancer (disambiguation).Medical condition
| Cancer | |
|---|---|
| Other names | Malignant tumor, malignant neoplasm |
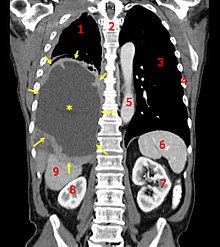 | |
| A coronal CT scan showing a malignant mesothelioma Legend: → tumor ←, ✱ central pleural effusion, 1 & 3 lungs, 2 spine, 4 ribs, 5 aorta, 6 spleen, 7 & 8 kidneys, 9 liver | |
| Pronunciation | |
| Specialty | Oncology |
| Symptoms | Lump, abnormal bleeding, prolonged cough, unexplained weight loss, change in bowel movements |
| Risk factors | Exposure to carcinogens, tobacco, obesity, poor diet, lack of physical activity, excessive alcohol, certain infections |
| Treatment | Radiation therapy, surgery, chemotherapy, targeted therapy |
| Prognosis | Average five-year survival 66% (USA) |
| Frequency | 24 million annually (2019) |
| Deaths | 10 million annually (2019) |
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in bowel movements. While these symptoms may indicate cancer, they can also have other causes. Over 100 types of cancers affect humans.
Tobacco use is the cause of about 22% of cancer deaths. Another 10% are due to obesity, poor diet, lack of physical activity or excessive alcohol consumption. Other factors include certain infections, exposure to ionizing radiation, and environmental pollutants. Infection with specific viruses, bacteria and parasites is an environmental factor causing approximately 16–18% of cancers worldwide. These infectious agents include Helicobacter pylori, hepatitis B, hepatitis C, human papillomavirus infection, Epstein–Barr virus, Human T-lymphotropic virus 1, Kaposi's sarcoma-associated herpesvirus and Merkel cell polyomavirus. Human immunodeficiency virus (HIV) does not directly cause cancer but it causes immune deficiency that can magnify the risk due to other infections, sometimes up to several thousand fold (in the case of Kaposi's sarcoma). Importantly, vaccination against hepatitis B and human papillomavirus have been shown to nearly eliminate risk of cancers caused by these viruses in persons successfully vaccinated prior to infection.
These environmental factors act, at least partly, by changing the genes of a cell. Typically, many genetic changes are required before cancer develops. Approximately 5–10% of cancers are due to inherited genetic defects. Cancer can be detected by certain signs and symptoms or screening tests. It is then typically further investigated by medical imaging and confirmed by biopsy.
The risk of developing certain cancers can be reduced by not smoking, maintaining a healthy weight, limiting alcohol intake, eating plenty of vegetables, fruits, and whole grains, vaccination against certain infectious diseases, limiting consumption of processed meat and red meat, and limiting exposure to direct sunlight. Early detection through screening is useful for cervical and colorectal cancer. The benefits of screening for breast cancer are controversial. Cancer is often treated with some combination of radiation therapy, surgery, chemotherapy and targeted therapy. Pain and symptom management are an important part of care. Palliative care is particularly important in people with advanced disease. The chance of survival depends on the type of cancer and extent of disease at the start of treatment. In children under 15 at diagnosis, the five-year survival rate in the developed world is on average 80%. For cancer in the United States, the average five-year survival rate is 66% for all ages.
In 2015, about 90.5 million people worldwide had cancer. In 2019, annual cancer cases grew by 23.6 million people, and there were 10 million deaths worldwide, representing over the previous decade increases of 26% and 21%, respectively.
The most common types of cancer in males are lung cancer, prostate cancer, colorectal cancer, and stomach cancer. In females, the most common types are breast cancer, colorectal cancer, lung cancer, and cervical cancer. If skin cancer other than melanoma were included in total new cancer cases each year, it would account for around 40% of cases. In children, acute lymphoblastic leukemia and brain tumors are most common, except in Africa, where non-Hodgkin lymphoma occurs more often. In 2012, about 165,000 children under 15 years of age were diagnosed with cancer. The risk of cancer increases significantly with age, and many cancers occur more commonly in developed countries. Rates are increasing as more people live to an old age and as lifestyle changes occur in the developing world. The global total economic costs of cancer were estimated at US$1.16 trillion (equivalent to $1.62 trillion in 2023) per year as of 2010.
Etymology and definitions
The word comes from the ancient Greek καρκίνος, meaning 'crab' and 'tumor'. Greek physicians Hippocrates and Galen, among others, noted the similarity of crabs to some tumors with swollen veins. The word was introduced in English in the modern medical sense around 1600.
Cancers comprise a large family of diseases that involve abnormal cell growth with the potential to invade or spread to other parts of the body. They form a subset of neoplasms. A neoplasm or tumor is a group of cells that have undergone unregulated growth and will often form a mass or lump, but may be distributed diffusely.
All tumor cells show the six hallmarks of cancer. These characteristics are required to produce a malignant tumor. They include:
- Cell growth and division absent the proper signals
- Continuous growth and division even given contrary signals
- Avoidance of programmed cell death
- Limitless number of cell divisions
- Promoting blood vessel construction
- Invasion of tissue and formation of metastases
The progression from normal cells to cells that can form a detectable mass to cancer involves multiple steps known as malignant progression.
Signs and symptoms
Main article: Signs and symptoms of cancer
When cancer begins, it produces no symptoms. Signs and symptoms appear as the mass grows or ulcerates. The findings that result depend on cancer's type and location. Few symptoms are specific. Many frequently occur in individuals who have other conditions. Cancer can be difficult to diagnose and can be considered a "great imitator".
People may become anxious or depressed post-diagnosis. The risk of suicide in people with cancer is approximately double.
Local symptoms
Local symptoms may occur due to the mass of the tumor or its ulceration. For example, mass effects from lung cancer can block the bronchus resulting in cough or pneumonia; esophageal cancer can cause narrowing of the esophagus, making it difficult or painful to swallow; and colorectal cancer may lead to narrowing or blockages in the bowel, affecting bowel habits. Masses in breasts or testicles may produce observable lumps. Ulceration can cause bleeding that can lead to symptoms such as coughing up blood (lung cancer), anemia or rectal bleeding (colon cancer), blood in the urine (bladder cancer), or abnormal vaginal bleeding (endometrial or cervical cancer). Although localized pain may occur in advanced cancer, the initial tumor is usually painless. Some cancers can cause a buildup of fluid within the chest or abdomen.
Systemic symptoms
Systemic symptoms may occur due to the body's response to the cancer. This may include fatigue, unintentional weight loss, or skin changes. Some cancers can cause a systemic inflammatory state that leads to ongoing muscle loss and weakness, known as cachexia.
Some cancers, such as Hodgkin's disease, leukemias, and liver or kidney cancers, can cause a persistent fever.
Shortness of breath, called dyspnea, is a common symptom of cancer and its treatment. The causes of cancer-related dyspnea can include tumors in or around the lung, blocked airways, fluid in the lungs, pneumonia, or treatment reactions including an allergic response. Treatment for dyspnea in patients with advanced cancer can include fans, bilevel ventilation, acupressure/reflexology and multicomponent nonpharmacological interventions.
Some systemic symptoms of cancer are caused by hormones or other molecules produced by the tumor, known as paraneoplastic syndromes. Common paraneoplastic syndromes include hypercalcemia, which can cause altered mental state, constipation and dehydration, or hyponatremia, which can also cause altered mental status, vomiting, headaches, or seizures.
Metastasis
Main article: MetastasisMetastasis is the spread of cancer to other locations in the body. The dispersed tumors are called metastatic tumors, while the original is called the primary tumor. Almost all cancers can metastasize. Most cancer deaths are due to cancer that has metastasized.
Metastasis is common in the late stages of cancer and it can occur via the blood or the lymphatic system or both. The typical steps in metastasis are:
- Local invasion
- Intravasation into the blood or lymph.
- Circulation through the body.
- Extravasation into the new tissue.
- Proliferation
- Angiogenesis
Different types of cancers tend to metastasize to particular organs. Overall, the most common places for metastases to occur are the lungs, liver, brain, and the bones.
While some cancers can be cured if detected early, metastatic cancer is more difficult to treat and control. Nevertheless, some recent treatments are demonstrating encouraging results.
Causes
Main article: Causes of cancer

The majority of cancers, some 90–95% of cases, are due to genetic mutations from environmental and lifestyle factors. The remaining 5–10% are due to inherited genetics. Environmental refers to any cause that is not inherited, such as lifestyle, economic, and behavioral factors and not merely pollution. Common environmental factors that contribute to cancer death include tobacco use (25–30%), diet and obesity (30–35%), infections (15–20%), radiation (both ionizing and non-ionizing, up to 10%), lack of physical activity, and pollution. Psychological stress does not appear to be a risk factor for the onset of cancer, though it may worsen outcomes in those who already have cancer.
Environmental or lifestyle factors that caused cancer to develop in an individual can be identified by analyzing mutational signatures from genomic sequencing of tumor DNA. For example, this can reveal if lung cancer was caused by tobacco smoke, if skin cancer was caused by UV radiation, or if secondary cancers were caused by previous chemotherapy treatment.
Cancer is generally not a transmissible disease. Exceptions include rare transmissions that occur with pregnancies and occasional organ donors. However, transmissible infectious diseases such as hepatitis B, Epstein-Barr virus, Human Papilloma Virus and HIV, can contribute to the development of cancer.
Chemicals
Further information: Alcohol and cancer and Smoking and cancer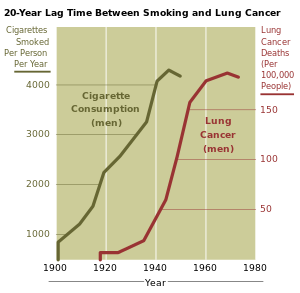
Exposure to particular substances have been linked to specific types of cancer. These substances are called carcinogens.
Tobacco smoke, for example, causes 90% of lung cancer. Tobacco use can cause cancer throughout the body including in the mouth and throat, larynx, esophagus, stomach, bladder, kidney, cervix, colon/rectum, liver and pancreas. Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.
Tobacco is responsible for about one in five cancer deaths worldwide and about one in three in the developed world. Lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking rates since the 1950s followed by decreases in lung cancer death rates in men since 1990.
In Western Europe, 10% of cancers in males and 3% of cancers in females are attributed to alcohol exposure, especially liver and digestive tract cancers. Cancer from work-related substance exposures may cause between 2 and 20% of cases, causing at least 200,000 deaths. Cancers such as lung cancer and mesothelioma can come from inhaling tobacco smoke or asbestos fibers, or leukemia from exposure to benzene.
Exposure to perfluorooctanoic acid (PFOA), which is predominantly used in the production of Teflon, is known to cause two kinds of cancer.
Chemotherapy drugs such as platinum-based compounds are carcinogens that increase the risk of secondary cancers
Azathioprine, an immunosuppressive medication, is a carcinogen that can cause primary tumors to develop.
Diet and exercise
Main article: Diet and cancerDiet, physical inactivity, and obesity are related to up to 30–35% of cancer deaths. In the United States, excess body weight is associated with the development of many types of cancer and is a factor in 14–20% of cancer deaths. A UK study including data on over 5 million people showed higher body mass index to be related to at least 10 types of cancer and responsible for around 12,000 cases each year in that country. Physical inactivity is believed to contribute to cancer risk, not only through its effect on body weight but also through negative effects on the immune system and endocrine system. More than half of the effect from the diet is due to overnutrition (eating too much), rather than from eating too few vegetables or other healthful foods.
Some specific foods are linked to specific cancers. A high-salt diet is linked to gastric cancer. Aflatoxin B1, a frequent food contaminant, causes liver cancer. Betel nut chewing can cause oral cancer. National differences in dietary practices may partly explain differences in cancer incidence. For example, gastric cancer is more common in Japan due to its high-salt diet while colon cancer is more common in the United States. Immigrant cancer profiles mirror those of their new country, often within one generation.
Infection
Main article: Infectious causes of cancerWorldwide, approximately 18% of cancer deaths are related to infectious diseases. This proportion ranges from a high of 25% in Africa to less than 10% in the developed world. Viruses are the usual infectious agents that cause cancer but bacteria and parasites may also play a role. Oncoviruses (viruses that can cause human cancer) include:
- Human papillomavirus (cervical cancer),
- Epstein–Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma),
- Kaposi's sarcoma herpesvirus (Kaposi's sarcoma and primary effusion lymphomas),
- Hepatitis B and hepatitis C viruses (hepatocellular carcinoma)
- Human T-cell leukemia virus-1 (T-cell leukemias).
- Merkel cell polyomavirus (Merkel cell carcinoma)
Bacterial infection may also increase the risk of cancer, as seen in
- Helicobacter pylori-induced gastric carcinoma.
- Colibactin, a genotoxin associated with Escherichia coli infection (colorectal cancer)
Parasitic infections associated with cancer include:
- Schistosoma haematobium (squamous cell carcinoma of the bladder)
- The liver flukes, Opisthorchis viverrini and Clonorchis sinensis (cholangiocarcinoma).
Radiation
Main article: Radiation-induced cancerRadiation exposure such as ultraviolet radiation and radioactive material is a risk factor for cancer. Many non-melanoma skin cancers are due to ultraviolet radiation, mostly from sunlight. Sources of ionizing radiation include medical imaging and radon gas.
Ionizing radiation is not a particularly strong mutagen. Residential exposure to radon gas, for example, has similar cancer risks as passive smoking. Radiation is a more potent source of cancer when combined with other cancer-causing agents, such as radon plus tobacco smoke. Radiation can cause cancer in most parts of the body, in all animals and at any age. Children are twice as likely to develop radiation-induced leukemia as adults; radiation exposure before birth has ten times the effect.
Medical use of ionizing radiation is a small but growing source of radiation-induced cancers. Ionizing radiation may be used to treat other cancers, but this may, in some cases, induce a second form of cancer. It is also used in some kinds of medical imaging.
Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies. Clear evidence establishes ultraviolet radiation, especially the non-ionizing medium wave UVB, as the cause of most non-melanoma skin cancers, which are the most common forms of cancer in the world.
Non-ionizing radio frequency radiation from mobile phones, electric power transmission and other similar sources has been described as a possible carcinogen by the World Health Organization's International Agency for Research on Cancer. Evidence, however, has not supported a concern. This includes that studies have not found a consistent link between mobile phone radiation and cancer risk.
Heredity
Main article: Cancer syndromeThe vast majority of cancers are non-hereditary (sporadic). Hereditary cancers are primarily caused by an inherited genetic defect. Less than 0.3% of the population are carriers of a genetic mutation that has a large effect on cancer risk and these cause less than 3–10% of cancer. Some of these syndromes include: certain inherited mutations in the genes BRCA1 and BRCA2 with a more than 75% risk of breast cancer and ovarian cancer, and hereditary nonpolyposis colorectal cancer (HNPCC or Lynch syndrome), which is present in about 3% of people with colorectal cancer, among others.
Statistically for cancers causing most mortality, the relative risk of developing colorectal cancer when a first-degree relative (parent, sibling or child) has been diagnosed with it is about 2. The corresponding relative risk is 1.5 for lung cancer, and 1.9 for prostate cancer. For breast cancer, the relative risk is 1.8 with a first-degree relative having developed it at 50 years of age or older, and 3.3 when the relative developed it when being younger than 50 years of age.
Taller people have an increased risk of cancer because they have more cells than shorter people. Since height is genetically determined to a large extent, taller people have a heritable increase of cancer risk.
Physical agents
Some substances cause cancer primarily through their physical, rather than chemical, effects. A prominent example of this is prolonged exposure to asbestos, naturally occurring mineral fibers that are a major cause of mesothelioma (cancer of the serous membrane) usually the serous membrane surrounding the lungs. Other substances in this category, including both naturally occurring and synthetic asbestos-like fibers, such as wollastonite, attapulgite, glass wool and rock wool, are believed to have similar effects. Non-fibrous particulate materials that cause cancer include powdered metallic cobalt and nickel and crystalline silica (quartz, cristobalite and tridymite). Usually, physical carcinogens must get inside the body (such as through inhalation) and require years of exposure to produce cancer.
Physical trauma resulting in cancer is relatively rare. Claims that breaking bones resulted in bone cancer, for example, have not been proven. Similarly, physical trauma is not accepted as a cause for cervical cancer, breast cancer or brain cancer. One accepted source is frequent, long-term application of hot objects to the body. It is possible that repeated burns on the same part of the body, such as those produced by kanger and kairo heaters (charcoal hand warmers), may produce skin cancer, especially if carcinogenic chemicals are also present. Frequent consumption of scalding hot tea may produce esophageal cancer. Generally, it is believed that cancer arises, or a pre-existing cancer is encouraged, during the process of healing, rather than directly by the trauma. However, repeated injuries to the same tissues might promote excessive cell proliferation, which could then increase the odds of a cancerous mutation.
Chronic inflammation has been hypothesized to directly cause mutation. Inflammation can contribute to proliferation, survival, angiogenesis and migration of cancer cells by influencing the tumor microenvironment. Oncogenes build up an inflammatory pro-tumorigenic microenvironment.
Hormones
Hormones also play a role in the development of cancer by promoting cell proliferation. Insulin-like growth factors and their binding proteins play a key role in cancer cell proliferation, differentiation and apoptosis, suggesting possible involvement in carcinogenesis.
Hormones are important agents in sex-related cancers, such as cancer of the breast, endometrium, prostate, ovary and testis and also of thyroid cancer and bone cancer. For example, the daughters of women who have breast cancer have significantly higher levels of estrogen and progesterone than the daughters of women without breast cancer. These higher hormone levels may explain their higher risk of breast cancer, even in the absence of a breast-cancer gene. Similarly, men of African ancestry have significantly higher levels of testosterone than men of European ancestry and have a correspondingly higher level of prostate cancer. Men of Asian ancestry, with the lowest levels of testosterone-activating androstanediol glucuronide, have the lowest levels of prostate cancer.
Other factors are relevant: obese people have higher levels of some hormones associated with cancer and a higher rate of those cancers. Women who take hormone replacement therapy have a higher risk of developing cancers associated with those hormones. On the other hand, people who exercise far more than average have lower levels of these hormones and lower risk of cancer. Osteosarcoma may be promoted by growth hormones. Some treatments and prevention approaches leverage this cause by artificially reducing hormone levels and thus discouraging hormone-sensitive cancers.
Autoimmune diseases
There is an association between celiac disease and an increased risk of all cancers. People with untreated celiac disease have a higher risk, but this risk decreases with time after diagnosis and strict treatment. This may be due to the adoption of a gluten-free diet, which seems to have a protective role against development of malignancy in people with celiac disease. However, the delay in diagnosis and initiation of a gluten-free diet seems to increase the risk of malignancies. Rates of gastrointestinal cancers are increased in people with Crohn's disease and ulcerative colitis, due to chronic inflammation. Immunomodulators and biologic agents used to treat these diseases may promote developing extra-intestinal malignancies.
Pathophysiology
Main article: CarcinogenesisGenetics
Main article: Oncogenomics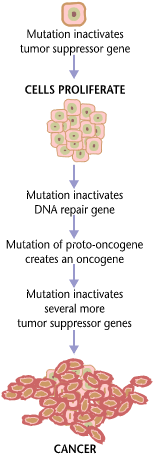
Cancer is fundamentally a disease of tissue growth regulation. For a normal cell to transform into a cancer cell, the genes that regulate cell growth and differentiation must be altered.
The affected genes are divided into two broad categories. Oncogenes are genes that promote cell growth and reproduction. Tumor suppressor genes are genes that inhibit cell division and survival. Malignant transformation can occur through the formation of novel oncogenes, the inappropriate over-expression of normal oncogenes, or by the under-expression or disabling of tumor suppressor genes. Typically, changes in multiple genes are required to transform a normal cell into a cancer cell.
Genetic changes can occur at different levels and by different mechanisms. The gain or loss of an entire chromosome can occur through errors in mitosis. More common are mutations, which are changes in the nucleotide sequence of genomic DNA.
Large-scale mutations involve the deletion or gain of a portion of a chromosome. Genomic amplification occurs when a cell gains copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material. Translocation occurs when two separate chromosomal regions become abnormally fused, often at a characteristic location. A well-known example of this is the Philadelphia chromosome, or translocation of chromosomes 9 and 22, which occurs in chronic myelogenous leukemia and results in production of the BCR-abl fusion protein, an oncogenic tyrosine kinase.
Small-scale mutations include point mutations, deletions, and insertions, which may occur in the promoter region of a gene and affect its expression, or may occur in the gene's coding sequence and alter the function or stability of its protein product. Disruption of a single gene may also result from integration of genomic material from a DNA virus or retrovirus, leading to the expression of viral oncogenes in the affected cell and its descendants.
Replication of the data contained within the DNA of living cells will probabilistically result in some errors (mutations). Complex error correction and prevention are built into the process and safeguard the cell against cancer. If a significant error occurs, the damaged cell can self-destruct through programmed cell death, termed apoptosis. If the error control processes fail, then the mutations will survive and be passed along to daughter cells.
Some environments make errors more likely to arise and propagate. Such environments can include the presence of disruptive substances called carcinogens, repeated physical injury, heat, ionising radiation, or hypoxia.
The errors that cause cancer are self-amplifying and compounding, for example:
- A mutation in the error-correcting machinery of a cell might cause that cell and its children to accumulate errors more rapidly.
- A further mutation in an oncogene might cause the cell to reproduce more rapidly and more frequently than its normal counterparts.
- A further mutation may cause loss of a tumor suppressor gene, disrupting the apoptosis signaling pathway and immortalizing the cell.
- A further mutation in the signaling machinery of the cell might send error-causing signals to nearby cells.
The transformation of a normal cell into cancer is akin to a chain reaction caused by initial errors, which compound into more severe errors, each progressively allowing the cell to escape more controls that limit normal tissue growth. This rebellion-like scenario is an undesirable survival of the fittest, where the driving forces of evolution work against the body's design and enforcement of order. Once cancer has begun to develop, this ongoing process, termed clonal evolution, drives progression towards more invasive stages. Clonal evolution leads to intra-tumour heterogeneity (cancer cells with heterogeneous mutations) that complicates designing effective treatment strategies and requires an evolutionary approach to designing treatment.
Characteristic abilities developed by cancers are divided into categories, specifically evasion of apoptosis, self-sufficiency in growth signals, insensitivity to anti-growth signals, sustained angiogenesis, limitless replicative potential, metastasis, reprogramming of energy metabolism and evasion of immune destruction.
Epigenetics
Main article: Cancer epigenetics
The classical view of cancer is a set of diseases driven by progressive genetic abnormalities that include mutations in tumor-suppressor genes and oncogenes, and in chromosomal abnormalities. A role for epigenetic alterations was identified in the early 21st century.
Epigenetic alterations are functionally relevant modifications to the genome that do not change the nucleotide sequence. Examples of such modifications are changes in DNA methylation (hypermethylation and hypomethylation), histone modification and changes in chromosomal architecture (caused by inappropriate expression of proteins such as HMGA2 or HMGA1). Each of these alterations regulates gene expression without altering the underlying DNA sequence. These changes may remain through cell divisions, endure for multiple generations, and can be considered as equivalent to mutations.
Epigenetic alterations occur frequently in cancers. As an example, one study listed protein coding genes that were frequently altered in their methylation in association with colon cancer. These included 147 hypermethylated and 27 hypomethylated genes. Of the hypermethylated genes, 10 were hypermethylated in 100% of colon cancers and many others were hypermethylated in more than 50% of colon cancers.
While epigenetic alterations are found in cancers, the epigenetic alterations in DNA repair genes, causing reduced expression of DNA repair proteins, may be of particular importance. Such alterations may occur early in progression to cancer and are a possible cause of the genetic instability characteristic of cancers.
Reduced expression of DNA repair genes disrupts DNA repair. This is shown in the figure at the 4th level from the top. (In the figure, red wording indicates the central role of DNA damage and defects in DNA repair in progression to cancer.) When DNA repair is deficient DNA damage remains in cells at a higher than usual level (5th level) and causes increased frequencies of mutation and/or epimutation (6th level). Mutation rates increase substantially in cells defective in DNA mismatch repair or in homologous recombinational repair (HRR). Chromosomal rearrangements and aneuploidy also increase in HRR defective cells.
Higher levels of DNA damage cause increased mutation (right side of figure) and increased epimutation. During repair of DNA double strand breaks, or repair of other DNA damage, incompletely cleared repair sites can cause epigenetic gene silencing.
Deficient expression of DNA repair proteins due to an inherited mutation can increase cancer risks. Individuals with an inherited impairment in any of 34 DNA repair genes (see article DNA repair-deficiency disorder) have increased cancer risk, with some defects ensuring a 100% lifetime chance of cancer (e.g. p53 mutations). Germ line DNA repair mutations are noted on the figure's left side. However, such germline mutations (which cause highly penetrant cancer syndromes) are the cause of only about 1 percent of cancers.
In sporadic cancers, deficiencies in DNA repair are occasionally caused by a mutation in a DNA repair gene but are much more frequently caused by epigenetic alterations that reduce or silence expression of DNA repair genes. This is indicated in the figure at the 3rd level. Many studies of heavy metal-induced carcinogenesis show that such heavy metals cause a reduction in expression of DNA repair enzymes, some through epigenetic mechanisms. DNA repair inhibition is proposed to be a predominant mechanism in heavy metal-induced carcinogenicity. In addition, frequent epigenetic alterations of the DNA sequences code for small RNAs called microRNAs (or miRNAs). miRNAs do not code for proteins, but can "target" protein-coding genes and reduce their expression.
Cancers usually arise from an assemblage of mutations and epimutations that confer a selective advantage leading to clonal expansion (see Field defects in progression to cancer). Mutations, however, may not be as frequent in cancers as epigenetic alterations. An average cancer of the breast or colon can have about 60 to 70 protein-altering mutations, of which about three or four may be "driver" mutations and the remaining ones may be "passenger" mutations.
Metastasis
Main article: MetastasisMetastasis is the spread of cancer to other locations in the body. The dispersed tumors are called metastatic tumors, while the original is called the primary tumor. Almost all cancers can metastasize. Most cancer deaths are due to cancer that has metastasized.
Metastasis is common in the late stages of cancer and it can occur via the blood or the lymphatic system or both. The typical steps in metastasis are local invasion, intravasation into the blood or lymph, circulation through the body, extravasation into the new tissue, proliferation and angiogenesis. Different types of cancers tend to metastasize to particular organs, but overall the most common places for metastases to occur are the lungs, liver, brain and the bones.
Metabolism
Main article: Tumor metabolomeNormal cells typically generate only about 30% of energy from glycolysis, whereas most cancers rely on glycolysis for energy production (Warburg effect). But a minority of cancer types rely on oxidative phosphorylation as the primary energy source, including lymphoma, leukemia, and endometrial cancer. Even in these cases, however, the use of glycolysis as an energy source rarely exceeds 60%. A few cancers use glutamine as the major energy source, partly because it provides nitrogen required for nucleotide (DNA, RNA) synthesis. Cancer stem cells often use oxidative phosphorylation or glutamine as a primary energy source.
Diagnosis
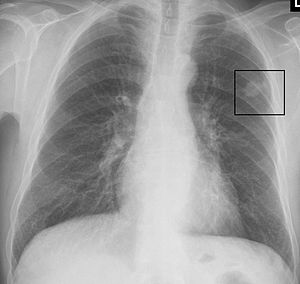
Most cancers are initially recognized either because of the appearance of signs or symptoms or through screening. Neither of these leads to a definitive diagnosis, which requires the examination of a tissue sample by a pathologist. People with suspected cancer are investigated with medical tests. These commonly include blood tests, X-rays, (contrast) CT scans and endoscopy.
The tissue diagnosis from the biopsy indicates the type of cell that is proliferating, its histological grade, genetic abnormalities and other features. Together, this information is useful to evaluate the prognosis and to choose the best treatment.
Cytogenetics and immunohistochemistry are other types of tissue tests. These tests provide information about molecular changes (such as mutations, fusion genes and numerical chromosome changes) and may thus also indicate the prognosis and best treatment.
Cancer diagnosis can cause psychological distress and psychosocial interventions, such as talking therapy, may help people with this. Some people choose to disclose the diagnosis widely; others prefer to keep the information private, especially shortly after the diagnosis, or to disclose it only partially or to selected people.
Classification
Further information: List of cancer types and List of oncology-related terms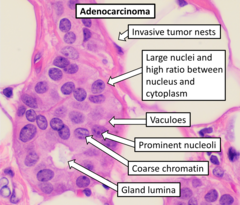
Cancers are classified by the type of cell that the tumor cells resemble and is therefore presumed to be the origin of the tumor. These types include:
- Carcinoma: Cancers derived from epithelial cells. This group includes many of the most common cancers and include nearly all those in the breast, prostate, lung, pancreas and colon. Most of these are of the adenocarcinoma type, which means that the cancer has gland-like differentiation.
- Sarcoma: Cancers arising from connective tissue (i.e. bone, cartilage, fat, nerve), each of which develops from cells originating in mesenchymal cells outside the bone marrow.
- Lymphoma and leukemia: These two classes arise from hematopoietic (blood-forming) cells that leave the marrow and tend to mature in the lymph nodes and blood, respectively.
- Germ cell tumor: Cancers derived from pluripotent cells, most often presenting in the testicle or the ovary (seminoma and dysgerminoma, respectively).
- Blastoma: Cancers derived from immature "precursor" cells or embryonic tissue.
Cancers are usually named using -carcinoma, -sarcoma or -blastoma as a suffix, with the Latin or Greek word for the organ or tissue of origin as the root. For example, cancers of the liver parenchyma arising from malignant epithelial cells is called hepatocarcinoma, while a malignancy arising from primitive liver precursor cells is called a hepatoblastoma and a cancer arising from fat cells is called a liposarcoma. For some common cancers, the English organ name is used. For example, the most common type of breast cancer is called ductal carcinoma of the breast. Here, the adjective ductal refers to the appearance of cancer under the microscope, which suggests that it has originated in the milk ducts.
Benign tumors (which are not cancers) are named using -oma as a suffix with the organ name as the root. For example, a benign tumor of smooth muscle cells is called a leiomyoma (the common name of this frequently occurring benign tumor in the uterus is fibroid). Confusingly, some types of cancer use the -noma suffix, examples including melanoma and seminoma.
Some types of cancer are named for the size and shape of the cells under a microscope, such as giant cell carcinoma, spindle cell carcinoma and small-cell carcinoma.
-
 An invasive ductal carcinoma of the breast (pale area at the center) surrounded by spikes of whitish scar tissue and yellow fatty tissue
An invasive ductal carcinoma of the breast (pale area at the center) surrounded by spikes of whitish scar tissue and yellow fatty tissue
-
 An invasive colorectal carcinoma (top center) in a colectomy specimen
An invasive colorectal carcinoma (top center) in a colectomy specimen
-
 A squamous-cell carcinoma (the whitish tumor) near the bronchi in a lung specimen
A squamous-cell carcinoma (the whitish tumor) near the bronchi in a lung specimen
-
 A large invasive ductal carcinoma in a mastectomy specimen
A large invasive ductal carcinoma in a mastectomy specimen
-
 Squamous cell carcinoma with typical histopathology features.
Squamous cell carcinoma with typical histopathology features.
-
 Histopathology of small-cell carcinoma, with typical findings.
Histopathology of small-cell carcinoma, with typical findings.
Prevention
Main article: Cancer prevention

Cancer prevention is defined as active measures to decrease cancer risk. The vast majority of cancer cases are due to environmental risk factors. Many of these environmental factors are controllable lifestyle choices. Thus, cancer is generally preventable. Between 70% and 90% of common cancers are due to environmental factors and therefore potentially preventable.
Greater than 30% of cancer deaths could be prevented by avoiding risk factors including: tobacco, excess weight/obesity, poor diet, physical inactivity, alcohol, sexually transmitted infections and air pollution. Further, poverty could be considered as an indirect risk factor in human cancers. Not all environmental causes are controllable, such as naturally occurring background radiation and cancers caused through hereditary genetic disorders and thus are not preventable via personal behavior.
In 2019, ~44% of all cancer deaths – or ~4.5 M deaths or ~105 million lost disability-adjusted life years – were due to known clearly preventable risk factors, led by smoking, alcohol use and high BMI, according to a GBD systematic analysis.
Dietary
Main article: Diet and cancerWhile many dietary recommendations have been proposed to reduce cancer risks, the evidence to support them is not definitive. The primary dietary factors that increase risk are obesity and alcohol consumption. Diets low in fruits and vegetables and high in red meat have been implicated but reviews and meta-analyses do not come to a consistent conclusion. A 2014 meta-analysis found no relationship between fruits and vegetables and cancer. Coffee is associated with a reduced risk of liver cancer. Studies have linked excessive consumption of red or processed meat to an increased risk of breast cancer, colon cancer and pancreatic cancer, a phenomenon that could be due to the presence of carcinogens in meats cooked at high temperatures. In 2015 the IARC reported that eating processed meat (e.g., bacon, ham, hot dogs, sausages) and, to a lesser degree, red meat was linked to some cancers.
Dietary recommendations for cancer prevention typically include an emphasis on vegetables, fruit, whole grains and fish and an avoidance of processed and red meat (beef, pork, lamb), animal fats, pickled foods and refined carbohydrates.
Medication
Medications can be used to prevent cancer in a few circumstances. In the general population, NSAIDs reduce the risk of colorectal cancer; however, due to cardiovascular and gastrointestinal side effects, they cause overall harm when used for prevention. Aspirin has been found to reduce the risk of death from cancer by about 7%. COX-2 inhibitors may decrease the rate of polyp formation in people with familial adenomatous polyposis; however, it is associated with the same adverse effects as NSAIDs. Daily use of tamoxifen or raloxifene reduce the risk of breast cancer in high-risk women. The benefit versus harm for 5-alpha-reductase inhibitor such as finasteride is not clear.
Vitamin supplementation does not appear to be effective at preventing cancer. While low blood levels of vitamin D are correlated with increased cancer risk, whether this relationship is causal and vitamin D supplementation is protective is not determined. One 2014 review found that supplements had no significant effect on cancer risk. Another 2014 review concluded that vitamin D3 may decrease the risk of death from cancer (one fewer death in 150 people treated over 5 years), but concerns with the quality of the data were noted.
Beta-Carotene supplementation increases lung cancer rates in those who are high risk. Folic acid supplementation is not effective in preventing colon cancer and may increase colon polyps. Selenium supplementation has not been shown to reduce the risk of cancer.
Vaccination
Vaccines have been developed that prevent infection by some carcinogenic viruses. Human papillomavirus vaccine (Gardasil and Cervarix) decrease the risk of developing cervical cancer. The hepatitis B vaccine prevents infection with hepatitis B virus and thus decreases the risk of liver cancer. The administration of human papillomavirus and hepatitis B vaccinations is recommended where resources allow.
Screening
Main article: Cancer screeningUnlike diagnostic efforts prompted by symptoms and medical signs, cancer screening involves efforts to detect cancer after it has formed, but before any noticeable symptoms appear. This may involve physical examination, blood or urine tests or medical imaging.
Cancer screening is not available for many types of cancers. Even when tests are available, they may not be recommended for everyone. Universal screening or mass screening involves screening everyone. Selective screening identifies people who are at higher risk, such as people with a family history. Several factors are considered to determine whether the benefits of screening outweigh the risks and the costs of screening. These factors include:
- Possible harms from the screening test: for example, X-ray images involve exposure to potentially harmful ionizing radiation
- The likelihood of the test correctly identifying cancer
- The likelihood that cancer is present: Screening is not normally useful for rare cancers.
- Possible harms from follow-up procedures
- Whether suitable treatment is available
- Whether early detection improves treatment outcomes
- Whether cancer will ever need treatment
- Whether the test is acceptable to the people: If a screening test is too burdensome (for example, extremely painful), then people will refuse to participate.
- Cost
Recommendations
U.S. Preventive Services Task Force
The U.S. Preventive Services Task Force (USPSTF) issues recommendations for various cancers:
- Strongly recommends cervical cancer screening in women who are sexually active and have a cervix at least until the age of 65.
- Recommend that Americans be screened for colorectal cancer via fecal occult blood testing, sigmoidoscopy, or colonoscopy starting at age 50 until age 75.
- Evidence is insufficient to recommend for or against screening for skin cancer, oral cancer, lung cancer, or prostate cancer in men under 75.
- Routine screening is not recommended for bladder cancer, testicular cancer, ovarian cancer, pancreatic cancer, or prostate cancer.
- Recommends mammography for breast cancer screening every two years from ages 50–74, but does not recommend either breast self-examination or clinical breast examination. A 2013 Cochrane review concluded that breast cancer screening by mammography had no effect in reducing mortality because of overdiagnosis and overtreatment.
Japan
Screens for gastric cancer using photofluorography due to the high incidence there.
Genetic testing
See also: Cancer syndrome| Gene | Cancer types |
|---|---|
| BRCA1, BRCA2 | Breast, ovarian, pancreatic |
| HNPCC, MLH1, MSH2, MSH6, PMS1, PMS2 | Colon, uterine, small bowel, stomach, urinary tract |
Genetic testing for individuals at high risk of certain cancers is recommended by unofficial groups. Carriers of these mutations may then undergo enhanced surveillance, chemoprevention, or preventative surgery to reduce their subsequent risk.
Management
Main articles: Treatment of cancer and OncologyMany treatment options for cancer exist. The primary ones include surgery, chemotherapy, radiation therapy, hormonal therapy, targeted therapy and palliative care. Which treatments are used depends on the type, location and grade of the cancer as well as the patient's health and preferences. The treatment intent may or may not be curative.
Chemotherapy
Chemotherapy is the treatment of cancer with one or more cytotoxic anti-neoplastic drugs (chemotherapeutic agents) as part of a standardized regimen. The term encompasses a variety of drugs, which are divided into broad categories such as alkylating agents and antimetabolites. Traditional chemotherapeutic agents act by killing cells that divide rapidly, a critical property of most cancer cells.
It was found that providing combined cytotoxic drugs is better than a single drug, a process called the combination therapy, which has an advantage in the statistics of survival and response to the tumor and in the progress of the disease. A Cochrane review concluded that combined therapy was more effective to treat metastasized breast cancer. However, generally it is not certain whether combination chemotherapy leads to better health outcomes, when both survival and toxicity are considered.
Targeted therapy is a form of chemotherapy that targets specific molecular differences between cancer and normal cells. The first targeted therapies blocked the estrogen receptor molecule, inhibiting the growth of breast cancer. Another common example is the class of Bcr-Abl inhibitors, which are used to treat chronic myelogenous leukemia (CML). Currently, targeted therapies exist for many of the most common cancer types, including bladder cancer, breast cancer, colorectal cancer, kidney cancer, leukemia, liver cancer, lung cancer, lymphoma, pancreatic cancer, prostate cancer, skin cancer, and thyroid cancer as well as other cancer types.
The efficacy of chemotherapy depends on the type of cancer and the stage. In combination with surgery, chemotherapy has proven useful in cancer types including breast cancer, colorectal cancer, pancreatic cancer, osteogenic sarcoma, testicular cancer, ovarian cancer and certain lung cancers. Chemotherapy is curative for some cancers, such as some leukemias, ineffective in some brain tumors, and needless in others, such as most non-melanoma skin cancers. The effectiveness of chemotherapy is often limited by its toxicity to other tissues in the body. Even when chemotherapy does not provide a permanent cure, it may be useful to reduce symptoms such as pain or to reduce the size of an inoperable tumor in the hope that surgery will become possible in the future.
Radiation
Radiation therapy involves the use of ionizing radiation in an attempt to either cure or improve symptoms. It works by damaging the DNA of cancerous tissue, causing mitotic catastrophe resulting in the death of the cancer cells. To spare normal tissues (such as skin or organs, which radiation must pass through to treat the tumor), shaped radiation beams are aimed from multiple exposure angles to intersect at the tumor, providing a much larger dose there than in the surrounding, healthy tissue. As with chemotherapy, cancers vary in their response to radiation therapy.
Radiation therapy is used in about half of cases. The radiation can be either from internal sources (brachytherapy) or external sources. The radiation is most commonly low energy X-rays for treating skin cancers, while higher energy X-rays are used for cancers within the body. Radiation is typically used in addition to surgery and or chemotherapy. For certain types of cancer, such as early head and neck cancer, it may be used alone. Radiation therapy after surgery for brain metastases has been shown to not improve overall survival in patients compared to surgery alone. For painful bone metastasis, radiation therapy has been found to be effective in about 70% of patients.
Surgery
Surgery is the primary method of treatment for most isolated, solid cancers and may play a role in palliation and prolongation of survival. It is typically an important part of definitive diagnosis and staging of tumors, as biopsies are usually required. In localized cancer, surgery typically attempts to remove the entire mass along with, in certain cases, the lymph nodes in the area. For some types of cancer this is sufficient to eliminate the cancer.
Palliative care
Palliative care is treatment that attempts to help the patient feel better and may be combined with an attempt to treat the cancer. Palliative care includes action to reduce physical, emotional, spiritual and psycho-social distress. Unlike treatment that is aimed at directly killing cancer cells, the primary goal of palliative care is to improve quality of life.
People at all stages of cancer treatment typically receive some kind of palliative care. In some cases, medical specialty professional organizations recommend that patients and physicians respond to cancer only with palliative care. This applies to patients who:
- for lung cancer, see Azzoli CG, Temin S, Aliff T, Baker S, Brahmer J, Johnson DH, et al. (October 2011). "2011 Focused Update of 2009 American Society of Clinical Oncology Clinical Practice Guideline Update on Chemotherapy for Stage IV Non-Small-Cell Lung Cancer". Journal of Clinical Oncology. 29 (28): 3825–31. doi:10.1200/JCO.2010.34.2774. PMC 3675703. PMID 21900105. and Ettinger DS, Akerley W, Bepler G, Blum MG, Chang A, Cheney RT, et al. (July 2010). "Non-small cell lung cancer". Journal of the National Comprehensive Cancer Network. 8 (7): 740–801. doi:10.6004/jnccn.2010.0056. PMID 20679538.
- for breast cancer, see Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, et al. (February 2009). "Breast cancer. Clinical practice guidelines in oncology". Journal of the National Comprehensive Cancer Network. 7 (2): 122–92. doi:10.6004/jnccn.2009.0012. PMID 19200416.
- for colon cancer, see Engstrom PF, Arnoletti JP, Benson AB, Chen YJ, Choti MA, Cooper HS, et al. (September 2009). "NCCN Clinical Practice Guidelines in Oncology: colon cancer". Journal of the National Comprehensive Cancer Network. 7 (8): 778–831. doi:10.6004/jnccn.2009.0056. PMID 19755046.
- for other general statements see Smith TJ, Hillner BE (May 2011). "Bending the cost curve in cancer care". The New England Journal of Medicine. 364 (21): 2060–5. doi:10.1056/NEJMsb1013826. PMC 4042405. PMID 21612477. and Peppercorn JM, Smith TJ, Helft PR, Debono DJ, Berry SR, Wollins DS, et al. (February 2011). "American society of clinical oncology statement: toward individualized care for patients with advanced cancer". Journal of Clinical Oncology. 29 (6): 755–60. doi:10.1200/JCO.2010.33.1744. PMID 21263086. S2CID 40873748.
- Display low performance status, implying limited ability to care for themselves
- Received no benefit from prior evidence-based treatments
- Are not eligible to participate in any appropriate clinical trial
- No strong evidence implies that treatment would be effective
Palliative care may be confused with hospice and therefore only indicated when people approach end of life. Like hospice care, palliative care attempts to help the patient cope with their immediate needs and to increase comfort. Unlike hospice care, palliative care does not require people to stop treatment aimed at the cancer.
Multiple national medical guidelines recommend early palliative care for patients whose cancer has produced distressing symptoms or who need help coping with their illness. In patients first diagnosed with metastatic disease, palliative care may be immediately indicated. Palliative care is indicated for patients with a prognosis of less than 12 months of life even given aggressive treatment.
Immunotherapy
Main article: Cancer immunotherapyA variety of therapies using immunotherapy, stimulating or helping the immune system to fight cancer, have come into use since 1997. Approaches include:
- Monoclonal antibody therapy
- Checkpoint therapy (therapy that targets the immune checkpoints or regulators of the immune system)
- Adoptive cell transfer
Laser therapy
Main article: Lasers in cancer treatmentLaser therapy uses high-intensity light to treat cancer by shrinking or destroying tumors or precancerous growths. Lasers are most commonly used to treat superficial cancers that are on the surface of the body or the lining of internal organs. It is used to treat basal cell skin cancer and the very early stages of others like cervical, penile, vaginal, vulvar, and non-small cell lung cancer. It is often combined with other treatments, such as surgery, chemotherapy, or radiation therapy. Laser-induced interstitial thermotherapy (LITT), or interstitial laser photocoagulation, uses lasers to treat some cancers using hyperthermia, which uses heat to shrink tumors by damaging or killing cancer cells. Laser are more precise than surgery and cause less damage, pain, bleeding, swelling, and scarring. A disadvantage is surgeons must have specialized training. It may be more expensive than other treatments.
Alternative medicine
Complementary and alternative cancer treatments are a diverse group of therapies, practices and products that are not part of conventional medicine. "Complementary medicine" refers to methods and substances used along with conventional medicine, while "alternative medicine" refers to compounds used instead of conventional medicine. Most complementary and alternative medicines for cancer have not been studied or tested using conventional techniques such as clinical trials. Some alternative treatments have been investigated and shown to be ineffective but still continue to be marketed and promoted. Cancer researcher Andrew J. Vickers stated, "The label 'unproven' is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been 'disproven'."
Prognosis
See also: Cancer survival rates, List of cancer mortality rates in the United States, and Cancer survivor
Survival rates vary by cancer type and by the stage at which it is diagnosed, ranging from majority survival to complete mortality five years after diagnosis. Once a cancer has metastasized, prognosis normally becomes much worse. About half of patients receiving treatment for invasive cancer (excluding carcinoma in situ and non-melanoma skin cancers) die from that cancer or its treatment. A majority of cancer deaths are due to metastases of the primary tumor.
Survival is worse in the developing world, partly because the types of cancer that are most common there are harder to treat than those associated with developed countries.
Those who survive cancer develop a second primary cancer at about twice the rate of those never diagnosed. The increased risk is believed to be due to the random chance of developing any cancer, the likelihood of surviving the first cancer, the same risk factors that produced the first cancer, unwanted side effects of treating the first cancer (particularly radiation therapy), and better compliance with screening.
Predicting short- or long-term survival depends on many factors. The most important are the cancer type and the patient's age and overall health. Those who are frail with other health problems have lower survival rates than otherwise healthy people. Centenarians are unlikely to survive for five years even if treatment is successful. People who report a higher quality of life tend to survive longer. People with lower quality of life may be affected by depression and other complications and/or disease progression that both impairs quality and quantity of life. Additionally, patients with worse prognoses may be depressed or report poorer quality of life because they perceive that their condition is likely to be fatal.
People with cancer have an increased risk of blood clots in their veins which can be life-threatening. The use of blood thinners such as heparin decrease the risk of blood clots but have not been shown to increase survival in people with cancer. People who take blood thinners also have an increased risk of bleeding.
Although extremely rare, some forms of cancer, even from an advanced stage, can heal spontaneously. This phenomenon is known as spontaneous remission.
Epidemiology
Main article: Epidemiology of cancer See also: List of countries by cancer rate| Graphs are unavailable due to technical issues. Updates on reimplementing the Graph extension, which will be known as the Chart extension, can be found on Phabricator and on MediaWiki.org. |
Estimates are that in 2018, 18.1 million new cases of cancer and 9.6 million deaths occur globally. About 20% of males and 17% of females will get cancer at some point in time while 13% of males and 9% of females will die from it.
In 2008, approximately 12.7 million cancers were diagnosed (excluding non-melanoma skin cancers and other non-invasive cancers) and in 2010 nearly 7.98 million people died. Cancers account for approximately 16% of deaths. The most common as of 2018 are lung cancer (1.76 million deaths), colorectal cancer (860,000) stomach cancer (780,000), liver cancer (780,000), and breast cancer (620,000). This makes invasive cancer the leading cause of death in the developed world and the second leading in the developing world. Over half of cases occur in the developing world.
Deaths from cancer were 5.8 million in 1990. Deaths have been increasing primarily due to longer lifespans and lifestyle changes in the developing world. The most significant risk factor for developing cancer is age. Although it is possible for cancer to strike at any age, most patients with invasive cancer are over 65. According to cancer researcher Robert A. Weinberg, "If we lived long enough, sooner or later we all would get cancer." Some of the association between aging and cancer is attributed to immunosenescence, errors accumulated in DNA over a lifetime and age-related changes in the endocrine system. Aging's effect on cancer is complicated by factors such as DNA damage and inflammation promoting it and factors such as vascular aging and endocrine changes inhibiting it.
Some slow-growing cancers are particularly common, but often are not fatal. Autopsy studies in Europe and Asia showed that up to 36% of people have undiagnosed and apparently harmless thyroid cancer at the time of their deaths and that 80% of men develop prostate cancer by age 80. As these cancers do not cause the patient's death, identifying them would have represented overdiagnosis rather than useful medical care.
The three most common childhood cancers are leukemia (34%), brain tumors (23%) and lymphomas (12%). In the United States cancer affects about 1 in 285 children. Rates of childhood cancer increased by 0.6% per year between 1975 and 2002 in the United States and by 1.1% per year between 1978 and 1997 in Europe. Death from childhood cancer decreased by half between 1975 and 2010 in the United States.
History
Main article: History of cancer
Cancer has existed for all of human history. The earliest written record regarding cancer is from c. 1600 BC in the Egyptian Edwin Smith Papyrus and describes breast cancer. Hippocrates (c. 460 BC – c. 370 BC) described several kinds of cancer, referring to them with the Greek word καρκίνος karkinos (crab or crayfish). This name comes from the appearance of the cut surface of a solid malignant tumor, with "the veins stretched on all sides as the animal the crab has its feet, whence it derives its name". Galen stated that "cancer of the breast is so called because of the fancied resemblance to a crab given by the lateral prolongations of the tumor and the adjacent distended veins". Celsus (c. 25 BC – 50 AD) translated karkinos into the Latin cancer, also meaning crab and recommended surgery as treatment. Galen (2nd century AD) disagreed with the use of surgery and recommended purgatives instead. These recommendations largely stood for 1000 years.
In the 15th, 16th and 17th centuries, it became acceptable for doctors to dissect bodies to discover the cause of death. The German professor Wilhelm Fabry believed that breast cancer was caused by a milk clot in a mammary duct. The Dutch professor Francois de la Boe Sylvius, a follower of Descartes, believed that all disease was the outcome of chemical processes and that acidic lymph fluid was the cause of cancer. His contemporary Nicolaes Tulp believed that cancer was a poison that slowly spreads and concluded that it was contagious.
The physician John Hill described tobacco sniffing as the cause of nose cancer in 1761. This was followed by the report in 1775 by British surgeon Percivall Pott that chimney sweeps' carcinoma, a cancer of the scrotum, was a common disease among chimney sweeps. With the widespread use of the microscope in the 18th century, it was discovered that the 'cancer poison' spread from the primary tumor through the lymph nodes to other sites ("metastasis"). This view of the disease was first formulated by the English surgeon Campbell De Morgan between 1871 and 1874.
Society and culture
Although many diseases (such as heart failure) may have a worse prognosis than most cases of cancer, cancer is the subject of widespread fear and taboos. The euphemism of "a long illness" to describe cancers leading to death is still commonly used in obituaries, rather than naming the disease explicitly, reflecting an apparent stigma. Cancer is also euphemised as "the C-word"; Macmillan Cancer Support uses the term to try to lessen the fear around the disease. In Nigeria, one local name for cancer translates into English as "the disease that cannot be cured". This deep belief that cancer is necessarily a difficult and usually deadly disease is reflected in the systems chosen by society to compile cancer statistics: the most common form of cancer—non-melanoma skin cancers, accounting for about one-third of cancer cases worldwide, but very few deaths—are excluded from cancer statistics specifically because they are easily treated and almost always cured, often in a single, short, outpatient procedure.
Western conceptions of patients' rights for people with cancer include a duty to fully disclose the medical situation to the person, and the right to engage in shared decision-making in a way that respects the person's own values. In other cultures, other rights and values are preferred. For example, most African cultures value whole families rather than individualism. In parts of Africa, a diagnosis is commonly made so late that cure is not possible, and treatment, if available at all, would quickly bankrupt the family. As a result of these factors, African healthcare providers tend to let family members decide whether, when and how to disclose the diagnosis, and they tend to do so slowly and circuitously, as the person shows interest and an ability to cope with the grim news. People from Asian and South American countries also tend to prefer a slower, less candid approach to disclosure than is idealized in the United States and Western Europe, and they believe that sometimes it would be preferable not to be told about a cancer diagnosis. In general, disclosure of the diagnosis is more common than it was in the 20th century, but full disclosure of the prognosis is not offered to many patients around the world.
In the United States and some other cultures, cancer is regarded as a disease that must be "fought" to end the "civil insurrection"; a War on Cancer was declared in the US. Military metaphors are particularly common in descriptions of cancer's human effects, and they emphasize both the state of the patient's health and the need to take immediate, decisive actions himself rather than to delay, to ignore or to rely entirely on others. The military metaphors also help rationalize radical, destructive treatments. In the 1970s, a relatively popular alternative cancer treatment in the US was a specialized form of talk therapy, based on the idea that cancer was caused by a bad attitude. People with a "cancer personality"—depressed, repressed, self-loathing and afraid to express their emotions—were believed to have manifested cancer through subconscious desire. Some psychotherapists claimed that treatment to change the patient's outlook on life would cure the cancer. Among other effects, this belief allowed society to blame the victim for having caused the cancer (by "wanting" it) or having prevented its cure (by not becoming a sufficiently happy, fearless and loving person). It also increased patients' anxiety, as they incorrectly believed that natural emotions of sadness, anger or fear shorten their lives. The idea was ridiculed by Susan Sontag, who published Illness as Metaphor while recovering from treatment for breast cancer in 1978. Although the original idea is now generally regarded as nonsense, the idea partly persists in a reduced form with a widespread, but incorrect, belief that deliberately cultivating a habit of positive thinking will increase survival. This notion is particularly strong in breast cancer culture.
One idea about why people with cancer are blamed or stigmatized, called the just-world fallacy, is that blaming cancer on the patient's actions or attitudes allows the blamers to regain a sense of control. This is based upon the blamers' belief that the world is fundamentally just and so any dangerous illness, like cancer, must be a type of punishment for bad choices, because in a just world, bad things would not happen to good people.
Economic effect
The total health care expenditure on cancer in the US was estimated to be $80.2 billion in 2015. Even though cancer-related health care expenditure have increased in absolute terms during recent decades, the share of health expenditure devoted to cancer treatment has remained close to 5% between the 1960s and 2004. A similar pattern has been observed in Europe where about 6% of all health care expenditure are spent on cancer treatment. In addition to health care expenditure and financial toxicity, cancer causes indirect costs in the form of productivity losses due to sick days, permanent incapacity and disability as well as premature death during working age. Cancer causes also costs for informal care. Indirect costs and informal care costs are typically estimated to exceed or equal the health care costs of cancer.
Workplace
In the United States, cancer is included as a protected condition by the Equal Employment Opportunity Commission (EEOC), mainly due to the potential for cancer having discriminating effects on workers. Discrimination in the workplace could occur if an employer holds a false belief that a person with cancer is not capable of doing a job properly, and may ask for more sick leave than other employees. Employers may also make hiring or firing decisions based on misconceptions about cancer disabilities, if present. The EEOC provides interview guidelines for employers, as well as lists of possible solutions for assessing and accommodating employees with cancer.
Effect on divorce
A study found women were around six times more likely to be divorced soon after a diagnosis of cancer compared to men. Rate of separation for cancer-survivors showed correlations with race, age, income, and comorbidities in a study. A review found a somewhat decreased divorce rate for most cancer types, and noted study heterogeneity and methodological weaknesses for many studies on effects of cancer on divorce.
Research
Main article: Cancer research
Because cancer is a class of diseases, it is unlikely that there will ever be a single "cure for cancer" any more than there will be a single treatment for all infectious diseases. Angiogenesis inhibitors were once incorrectly thought to have potential as a "silver bullet" treatment applicable to many types of cancer. Angiogenesis inhibitors and other cancer therapeutics are used in combination to reduce cancer morbidity and mortality.
Experimental cancer treatments are studied in clinical trials to compare the proposed treatment to the best existing treatment. Treatments that succeeded in one cancer type can be tested against other types. Diagnostic tests are under development to better target the right therapies to the right patients, based on their individual biology.
Cancer research focuses on the following issues:
- Agents (e.g. viruses) and events (e.g. mutations) that cause or facilitate genetic changes in cells destined to become cancer.
- The precise nature of the genetic damage and the genes that are affected by it.
- The consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell and in facilitating additional genetic events that lead to further progression of the cancer.
The improved understanding of molecular biology and cellular biology due to cancer research has led to new treatments for cancer since US President Richard Nixon declared the "War on Cancer" in 1971. Since then, the country has spent over $200 billion on cancer research, including resources from public and private sectors. The cancer death rate (adjusting for size and age of the population) declined by five percent between 1950 and 2005.
Competition for financial resources appears to have suppressed the creativity, cooperation, risk-taking and original thinking required to make fundamental discoveries, unduly favoring low-risk research into small incremental advancements over riskier, more innovative research. Other consequences of competition appear to be many studies with dramatic claims whose results cannot be replicated and perverse incentives that encourage grantee institutions to grow without making sufficient investments in their own faculty and facilities.
Virotherapy, which uses convert viruses, is being studied.
In the wake of the COVID-19 pandemic, there has been a worry that cancer research and treatment are slowing down.
On 2 December 2023, Nano Today published a groundbreaking discovery involving "NK cell-engaging nanodrones" for targeted cancer treatment. The development of "NK cell-engaging nanodrones" represents a significant leap forward in cancer treatment, showcasing how cutting-edge nanotechnology and immunotherapy can be combined to target and eliminate cancer cells with unprecedented precision. These nanodrones are designed to harness the power of natural killer (NK) cells, which play a crucial role in the body's immune response against tumors. By directing these NK cells specifically to the sites of tumors, the nanodrones can effectively concentrate the immune system's attack on the cancer cells, potentially leading to better outcomes for patients.
The key innovation here lies in the use of protein cage nanoparticle-based systems. These systems are engineered to carry signals that attract NK cells directly to the tumor, overcoming one of the major challenges in cancer immunotherapy: ensuring that the immune cells find and attack only the cancer cells without harming healthy tissue. This targeted approach not only increases the efficacy of the treatment but also minimizes side effects, a common concern with broader-acting cancer therapies.
Pregnancy
Cancer affects approximately 1 in 1,000 pregnant women. The most common cancers found during pregnancy are the same as the most common cancers found in non-pregnant women during childbearing ages: breast cancer, cervical cancer, leukemia, lymphoma, melanoma, ovarian cancer and colorectal cancer.
Diagnosing a new cancer in a pregnant woman is difficult, in part because any symptoms are commonly assumed to be a normal discomfort associated with pregnancy. As a result, cancer is typically discovered at a somewhat later stage than average. Some imaging procedures, such as MRIs (magnetic resonance imaging), CT scans, ultrasounds and mammograms with fetal shielding are considered safe during pregnancy; some others, such as PET scans, are not.
Treatment is generally the same as for non-pregnant women. However, radiation and radioactive drugs are normally avoided during pregnancy, especially if the fetal dose might exceed 100 cGy. In some cases, some or all treatments are postponed until after birth if the cancer is diagnosed late in the pregnancy. Early deliveries are often used to advance the start of treatment. Surgery is generally safe, but pelvic surgeries during the first trimester may cause miscarriage. Some treatments, especially certain chemotherapy drugs given during the first trimester, increase the risk of birth defects and pregnancy loss (spontaneous abortions and stillbirths).
Elective abortions are not required and, for the most common forms and stages of cancer, do not improve the mother's survival. In a few instances, such as advanced uterine cancer, the pregnancy cannot be continued and in others, the patient may end the pregnancy so that she can begin aggressive chemotherapy.
Some treatments can interfere with the mother's ability to give birth vaginally or to breastfeed. Cervical cancer may require birth by Caesarean section. Radiation to the breast reduces the ability of that breast to produce milk and increases the risk of mastitis. Also, when chemotherapy is given after birth, many of the drugs appear in breast milk, which could harm the baby.
Other animals
Veterinary oncology, concentrating mainly on cats and dogs, is a growing specialty in wealthy countries and the major forms of human treatment such as surgery and radiotherapy may be offered. The most common types of cancer differ, but the cancer burden seems at least as high in pets as in humans. Animals, typically rodents, are often used in cancer research and studies of natural cancers in larger animals may benefit research into human cancer.
Across wild animals, there is still limited data on cancer. Nonetheless, a study published in 2022, explored cancer risk in (non-domesticated) zoo mammals, belonging to 191 species, 110,148 individual, demonstrated that cancer is a ubiquitous disease of mammals and it can emerge anywhere along the mammalian phylogeny. This research also highlighted that cancer risk is not uniformly distributed along mammals. For instance, species in the order Carnivora are particularly prone to be affected by cancer (e.g. over 25% of clouded leopards, bat-eared foxes and red wolves die of cancer), while ungulates (especially even-toed ungulates) appear to face consistently low cancer risks.
In non-humans, a few types of transmissible cancer have also been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with Sticker's sarcoma (also known as canine transmissible venereal tumor), and in Tasmanian devils with devil facial tumour disease (DFTD).
See also
- Cancer screening
- Cancer treatment
- Causes of cancer
- Epidemiology of cancer
- Occupational cancer
- Oncology
- Metabolic theory of cancer
References
- ^ "Cancer – Signs and symptoms". NHS Choices. Archived from the original on 8 June 2014. Retrieved 10 June 2014.
- ^ "Cancer". World Health Organization. 12 September 2018. Retrieved 19 December 2018.
- ^ Anand P, Kunnumakkara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, et al. (September 2008). "Cancer is a preventable disease that requires major lifestyle changes". Pharmaceutical Research. 25 (9): 2097–116. doi:10.1007/s11095-008-9661-9. PMC 2515569. PMID 18626751. (Erratum: doi:10.1007/s11095-008-9690-4, PMID 18626751)
- ^ "Targeted Cancer Therapies". cancer.gov. National Cancer Institute. 26 February 2018. Retrieved 28 March 2018.
- ^ "SEER Stat Fact Sheets: All Cancer Sites". National Cancer Institute. Archived from the original on 26 September 2010. Retrieved 18 June 2014.
- ^ Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD, et al. (March 2022). "Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019". JAMA Oncology. 8 (3): 420–444. doi:10.1001/jamaoncol.2021.6987. ISSN 2374-2437. PMC 8719276. PMID 34967848.
- ^ "What Is Cancer?". National Cancer Institute. 17 September 2007. Retrieved 28 March 2018.
- "Obesity and Cancer Risk". National Cancer Institute. 3 January 2012. Archived from the original on 4 July 2015. Retrieved 4 July 2015.
- Jayasekara H, MacInnis RJ, Room R, English DR (May 2016). "Long-Term Alcohol Consumption and Breast, Upper Aero-Digestive Tract and Colorectal Cancer Risk: A Systematic Review and Meta-Analysis". Alcohol and Alcoholism. 51 (3): 315–30. doi:10.1093/alcalc/agv110. PMID 26400678.
- de Martel C, Georges D, Bray F, Ferlay J, Clifford GM (15 February 2020). "Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis". The Lancet Global Health. 8 (2): e180 – e190. doi:10.1016/S2214-109X(19)30488-7. PMID 31862245.
- ^ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 4.7. ISBN 978-92-832-0429-9. Archived from the original on 12 July 2017.
- "Heredity and Cancer". American Cancer Society. Archived from the original on 2 August 2013. Retrieved 22 July 2013.
- "How is cancer diagnosed?". American Cancer Society. 29 January 2013. Archived from the original on 14 July 2014. Retrieved 10 June 2014.
- ^ Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. (2012). "American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity". CA: A Cancer Journal for Clinicians. 62 (1): 30–67. doi:10.3322/caac.20140. PMID 22237782. S2CID 2067308.
- Parkin DM, Boyd L, Walker LC (December 2011). "16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010". British Journal of Cancer. 105 (Suppl 2): S77–81. doi:10.1038/bjc.2011.489. PMC 3252065. PMID 22158327.
- Gøtzsche PC, Jørgensen KJ (June 2013). "Screening for breast cancer with mammography". The Cochrane Database of Systematic Reviews. 2013 (6): CD001877. doi:10.1002/14651858.CD001877.pub5. PMC 6464778. PMID 23737396.
- ^ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.3. ISBN 978-92-832-0429-9. Archived from the original on 12 July 2017.
- GBD, et al. (Disease and Injury Incidence and Prevalence Collaborators) (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". The Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Sciacovelli M, Schmidt C, Maher ER, Frezza C (2020). "Metabolic Drivers in Hereditary Cancer Syndromes". Annual Review of Cancer Biology. 4: 77–97. doi:10.1146/annurev-cancerbio-030419-033612.
- ^ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-92-832-0429-9.
- ^ Siegel RL, Miller KD, Wagle NS, Jemal A (January 2023). "Cancer statistics, 2023". CA. 73 (1): 17–48. doi:10.3322/caac.21763. PMID 36633525.
- Dubas LE, Ingraffea A (February 2013). "Nonmelanoma skin cancer". Facial Plastic Surgery Clinics of North America. 21 (1): 43–53. doi:10.1016/j.fsc.2012.10.003. PMID 23369588.
- Cakir BÖ, Adamson P, Cingi C (November 2012). "Epidemiology and economic burden of nonmelanoma skin cancer". Facial Plastic Surgery Clinics of North America. 20 (4): 419–422. doi:10.1016/j.fsc.2012.07.004. PMID 23084294.
- ^ Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (February 2011). "Global cancer statistics". CA. 61 (2): 69–90. doi:10.3322/caac.20107. PMID 21296855. S2CID 30500384.
- World Report 2014. World Health Organization. 2014. pp. Chapter 6.7. ISBN 978-92-832-0429-9. Archived from the original on 12 July 2017.
- "cancer". www.etymonline.com. Archived from the original on 7 November 2022.
- "Cancer Glossary". cancer.org. American Cancer Society. Archived from the original on 1 September 2013. Retrieved 11 September 2013.
- "What is cancer?". cancer.gov. National Cancer Institute. 17 September 2007. Retrieved 28 March 2018.
- ^ Hanahan D, Weinberg RA (January 2000). "The hallmarks of cancer". Cell. 100 (1): 57–70. doi:10.1016/S0092-8674(00)81683-9. PMID 10647931. S2CID 1478778.
- ^ Hanahan D, Weinberg RA (March 2011). "Hallmarks of cancer: the next generation". Cell. 144 (5): 646–74. doi:10.1016/j.cell.2011.02.013. PMID 21376230.
- ^ Holland Chp. 1
- Anguiano L, Mayer DK, Piven ML, Rosenstein D (July–August 2012). "A literature review of suicide in cancer patients". Cancer Nursing. 35 (4): E14–26. doi:10.1097/NCC.0b013e31822fc76c. PMID 21946906. S2CID 45874503.
- O'Dell M, Stubblefield M (2009). Cancer rehabilitation principles and practice. New York: Demos Medical. p. 983. ISBN 978-1-933864-33-4.
- Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. (May 2011). "Definition and classification of cancer cachexia: an international consensus". The Lancet. Oncology. 12 (5): 489–95. doi:10.1016/S1470-2045(10)70218-7. PMID 21296615.
- "Shortness of Breath | Cancer-related Side Effects". www.cancer.org. Retrieved 10 October 2023.
- Dy SM, Gupta A, Waldfogel JM, Sharma R, Zhang A, Feliciano JL, et al. (2020). Interventions for Breathlessness in Patients With Advanced Cancer. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 33289989.
- Dimitriadis GK, Angelousi A, Weickert MO, Randeva HS, Kaltsas G, Grossman A (June 2017). "Paraneoplastic endocrine syndromes". Endocrine-Related Cancer. 24 (6): R173 – R190. doi:10.1530/ERC-17-0036. PMID 28341725.
- ^ "Metastatic Cancer: Questions and Answers". National Cancer Institute. 12 May 2015. Retrieved 28 March 2018.
- ^ "What is Metastasized Cancer?". National Comprehensive Cancer Network. Archived from the original on 7 July 2013. Retrieved 18 July 2013.
- "Why is cancer so hard to cure?". The Age. 15 July 2023. Retrieved 17 July 2023.
- "Share of cancer deaths attributed to tobacco". Our World in Data. Retrieved 5 March 2020.
- Manton K, Akushevich I, Kravchenko J (28 December 2008). Cancer Mortality and Morbidity Patterns in the U.S. Population: An Interdisciplinary Approach. Springer Science & Business Media. ISBN 978-0-387-78193-8.
The term environment refers not only to air, water, and soil but also to substances and conditions at home and at the workplace, including diet, smoking, alcohol, drugs, exposure to chemicals, sunlight, ionizing radiation, electromagnetic fields, infectious agents, etc. Lifestyle, economic and behavioral factors are all aspects of our environment.
- Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. (January 2018). "Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States". CA: A Cancer Journal for Clinicians. 68 (1): 31–54. doi:10.3322/caac.21440. PMID 29160902.
- ^ Cohen S, Murphy ML, Prather AA (January 2019). "Ten Surprising Facts About Stressful Life Events and Disease Risk". Annual Review of Psychology. 70: 577–597. doi:10.1146/annurev-psych-010418-102857. PMC 6996482. PMID 29949726.
the strongest conclusion derived from decades of research on stressors and cancer is that stressful events may be associated with decreased cancer survival but are probably not associated with disease incidence (Chida et al. 2008).
- Heikkilä K, Nyberg ST, Theorell T, Fransson EI, Alfredsson L, Bjorner JB, et al. (February 2013). "Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women". BMJ. 346: f165. doi:10.1136/bmj.f165. PMC 3567204. PMID 23393080.
- ^ Steele CD, Pillay N, Alexandrov LB (July 2022). "An overview of mutational and copy number signatures in human cancer". The Journal of Pathology. 257 (4): 454–465. doi:10.1002/path.5912. PMC 9324981. PMID 35420163.
- Tolar J, Neglia JP (June 2003). "Transplacental and other routes of cancer transmission between individuals". Journal of Pediatric Hematology/Oncology. 25 (6): 430–4. doi:10.1097/00043426-200306000-00002. PMID 12794519. S2CID 34197973.
- Biesalski HK, Bueno de Mesquita B, Chesson A, Chytil F, Grimble R, Hermus RJ, et al. (1998). "European Consensus Statement on Lung Cancer: risk factors and prevention. Lung Cancer Panel". CA: A Cancer Journal for Clinicians. 48 (3): 167–76, discussion 164–66. doi:10.3322/canjclin.48.3.167. PMID 9594919. S2CID 20891885.
- Kuper H, Boffetta P, Adami HO (September 2002). "Tobacco use and cancer causation: association by tumour type". Journal of Internal Medicine. 252 (3): 206–24. doi:10.1046/j.1365-2796.2002.01022.x. PMID 12270001. S2CID 6132726.
- "Cancer and Tobacco Use". Centers for Disease Control and Prevention. 27 August 2019. Retrieved 25 October 2023.
- ^ Kuper H, Adami HO, Boffetta P (June 2002). "Tobacco use, cancer causation and public health impact". Journal of Internal Medicine. 251 (6): 455–66. doi:10.1046/j.1365-2796.2002.00993.x. PMID 12028500. S2CID 9172672.
- Sasco AJ, Secretan MB, Straif K (August 2004). "Tobacco smoking and cancer: a brief review of recent epidemiological evidence". Lung Cancer. 45 (Suppl 2): S3–9. doi:10.1016/j.lungcan.2004.07.998. PMID 15552776.
- Thun MJ, Jemal A (October 2006). "How much of the decrease in cancer death rates in the United States is attributable to reductions in tobacco smoking?". Tobacco Control. 15 (5): 345–47. doi:10.1136/tc.2006.017749. PMC 2563648. PMID 16998161.
- Dubey S, Powell CA (May 2008). "Update in lung cancer 2007". American Journal of Respiratory and Critical Care Medicine. 177 (9): 941–46. doi:10.1164/rccm.200801-107UP. PMC 2720127. PMID 18434333.
- Schütze M, Boeing H, Pischon T, Rehm J, Kehoe T, Gmel G, et al. (April 2011). "Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study". BMJ. 342: d1584. doi:10.1136/bmj.d1584. PMC 3072472. PMID 21474525.
- Irigaray P, Newby JA, Clapp R, Hardell L, Howard V, Montagnier L, et al. (December 2007). "Lifestyle-related factors and environmental agents causing cancer: an overview". Biomedicine & Pharmacotherapy. 61 (10): 640–58. doi:10.1016/j.biopha.2007.10.006. PMID 18055160.
- ^ "WHO calls for prevention of cancer through healthy workplaces" (Press release). World Health Organization. 27 April 2007. Archived from the original on 12 October 2007. Retrieved 13 October 2007.
- "Erin Brockovich Blasts U.S. Regulation of Toxic Chemicals". scientificamerican.com. Scientific American. 28 December 2020.
- "Environmental Pollutant, PFOA, Associated with Increased Risk of Kidney Cancer". National Cancer Institute. 24 September 2020.
- ^ {{cite journal |vauthors=Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, Gansler T, Andrews KS, Thun MJ |s2cid=19823935 |title=American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity |journal=CA: A Cancer Journal for Clinicians |volume=56 |issue=5 |pages=254–81; quiz 313–14 |year=2006 |pmid=17005596 |doi=10.3322/canjclin.56.5.254|doi-access=free />
- {{cite journal |vauthors=Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L |title=Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults |journal=Lancet |volume=384 |issue=9945 |pages=755–65 |date=August 2014 |pmid=25129328 |doi=10.1016/S0140-6736(14)60892-8 |pmc=4151483/>
- ^ Park S, Bae J, Nam BH, Yoo KY (2008). "Aetiology of cancer in Asia". Asian Pacific Journal of Cancer Prevention. 9 (3): 371–80. PMID 18990005. Archived from the original on 4 September 2011.
- Brenner H, Rothenbacher D, Arndt V (2009). "Epidemiology of Stomach Cancer". Cancer Epidemiology. Methods in Molecular Biology. Vol. 472. pp. 467–77. doi:10.1007/978-1-60327-492-0_23. ISBN 978-1-60327-491-3. PMC 2166976. PMID 19107449.
- Buell P, Dunn JE (May 1965). "Cancer Mortality Among Japanese Issei and Nisei of California". Cancer. 18 (5): 656–64. doi:10.1002/1097-0142(196505)18:5<656::AID-CNCR2820180515>3.0.CO;2-3. PMID 14278899.
- Moore PS, Chang Y (December 2010). "Why do viruses cause cancer? Highlights of the first century of human tumour virology". Nature Reviews. Cancer. 10 (12). Springer Science and Business Media LLC: 878–889. doi:10.1038/nrc2961. PMC 3718018. PMID 21102637.
- Pagano JS, Blaser M, Buendia MA, Damania B, Khalili K, Raab-Traub N, et al. (December 2004). "Infectious agents and cancer: criteria for a causal relation". Seminars in Cancer Biology. 14 (6): 453–71. doi:10.1016/j.semcancer.2004.06.009. PMID 15489139.
- Ljubojevic S, Skerlev M (2014). "HPV-associated diseases". Clinics in Dermatology. 32 (2): 227–34. doi:10.1016/j.clindermatol.2013.08.007. PMID 24559558.
- Samaras V, Rafailidis PI, Mourtzoukou EG, Peppas G, Falagas ME (June 2010). "Chronic bacterial and parasitic infections and cancer: a review". Journal of Infection in Developing Countries. 4 (5): 267–81. doi:10.3855/jidc.819. PMID 20539059. Archived from the original on 4 October 2011.
- ^ "Radiation". National Cancer Institute. 29 April 2015. Retrieved 8 June 2019.
- ^ "Sunlight". National Cancer Institute. 29 April 2015. Retrieved 8 June 2019.
- "Cancer prevention". WHO. Retrieved 8 June 2019.
- ^ Little JB (2000). "Chapter 14: Ionizing Radiation". In Kufe DW, Pollock RE, Weichselbaum RR, Bast RC, Gansler TS, Holland JF, Frei E (eds.). Cancer medicine (6th ed.). Hamilton, Ont: B.C. Decker. ISBN 978-1-55009-113-7. Archived from the original on 2 January 2016.
- Brenner DJ, Hall EJ (November 2007). "Computed tomography—an increasing source of radiation exposure". The New England Journal of Medicine. 357 (22): 2277–84. doi:10.1056/NEJMra072149. PMID 18046031. S2CID 2760372.
- ^ Cleaver JE, Mitchell DL (2000). "15. Ultraviolet Radiation Carcinogenesis". In Bast RC, Kufe DW, Pollock RE, et al. (eds.). Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 978-1-55009-113-7. Archived from the original on 4 September 2015. Retrieved 31 January 2011.
- "IARC classifies radiofrequency electromagnetic fields as possibly carcinogenic to humans" (PDF). World Health Organization. Archived (PDF) from the original on 1 June 2011.
- "Electromagnetic Fields and Cancer". National Cancer Institute. 7 January 2019. Retrieved 8 June 2019.
- "Cell Phones and Cancer Risk – National Cancer Institute". Cancer.gov. 8 May 2013. Retrieved 28 March 2018.
- ^ Roukos DH (April 2009). "Genome-wide association studies: how predictable is a person's cancer risk?". Expert Review of Anticancer Therapy. 9 (4): 389–92. doi:10.1586/era.09.12. PMID 19374592. S2CID 24746283.
- Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, et al. (March 2010). "Colorectal cancer". Lancet. 375 (9719): 1030–47. doi:10.1016/S0140-6736(10)60353-4. PMID 20304247. S2CID 25299272.
- Kampman E (January 2007). "A first-degree relative with colorectal cancer: what are we missing?". Cancer Epidemiology, Biomarkers & Prevention. 16 (1): 1–3. doi:10.1158/1055-9965.EPI-06-0984. PMID 17220324.
- Coté ML, Liu M, Bonassi S, Neri M, Schwartz AG, Christiani DC, et al. (September 2012). "Increased risk of lung cancer in individuals with a family history of the disease: a pooled analysis from the International Lung Cancer Consortium". European Journal of Cancer. 48 (13): 1957–68. doi:10.1016/j.ejca.2012.01.038. PMC 3445438. PMID 22436981.
- Bruner DW, Moore D, Parlanti A, Dorgan J, Engstrom P (December 2003). "Relative risk of prostate cancer for men with affected relatives: systematic review and meta-analysis". International Journal of Cancer. 107 (5): 797–803. doi:10.1002/ijc.11466. PMID 14566830. S2CID 25591527.
- Singletary SE (April 2003). "Rating the risk factors for breast cancer". Annals of Surgery. 237 (4): 474–482. doi:10.1097/01.SLA.0000059969.64262.87. PMC 1514477. PMID 12677142.
- Green J, Cairns BJ, Casabonne D, Wright FL, Reeves G, Beral V (August 2011). "Height and cancer incidence in the Million Women Study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk". The Lancet. Oncology. 12 (8): 785–94. doi:10.1016/S1470-2045(11)70154-1. PMC 3148429. PMID 21782509.
- ^ Maltoni CF, Holland JF (2000). "Chapter 16: Physical Carcinogens". In Bast RC, Kufe DW, Pollock RE, et al. (eds.). Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 978-1-55009-113-7. Archived from the original on 4 September 2015. Retrieved 31 January 2011.
- ^ Gaeta JF (2000). "Chapter 17: Trauma and Inflammation". In Bast RC, Kufe DW, Pollock RE, et al. (eds.). Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 978-1-55009-113-7. Archived from the original on 4 September 2015. Retrieved 27 January 2011.
- Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (July 2009). "Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability". Carcinogenesis (review). 30 (7): 1073–81. doi:10.1093/carcin/bgp127. PMID 19468060.
- Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R (September 2011). "Interaction of tumor cells with the microenvironment". Cell Communication and Signaling. 9 (18): 18. doi:10.1186/1478-811X-9-18. PMC 3180438. PMID 21914164.
- Mantovani A (June 2010). "Molecular pathways linking inflammation and cancer". Current Molecular Medicine (review). 10 (4): 369–73. doi:10.2174/156652410791316968. PMID 20455855.
- Borrello MG, Degl'Innocenti D, Pierotti MA (August 2008). "Inflammation and cancer: the oncogene-driven connection". Cancer Letters (review). 267 (2): 262–70. doi:10.1016/j.canlet.2008.03.060. PMID 18502035.
- ^ Henderson BE, Bernstein L, Ross RK (2000). "Chapter 13: Hormones and the Etiology of Cancer". In Bast RC, Kufe DW, Pollock RE, et al. (eds.). Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 978-1-55009-113-7. Archived from the original on 10 September 2017. Retrieved 27 January 2011.
- Rowlands MA, Gunnell D, Harris R, Vatten LJ, Holly JM, Martin RM (May 2009). "Circulating insulin-like growth factor peptides and prostate cancer risk: a systematic review and meta-analysis". International Journal of Cancer. 124 (10): 2416–29. doi:10.1002/ijc.24202. PMC 2743036. PMID 19142965.
- Han Y, Chen W, Li P, Ye J (September 2015). "Association Between Coeliac Disease and Risk of Any Malignancy and Gastrointestinal Malignancy: A Meta-Analysis". Medicine. 94 (38): e1612. doi:10.1097/MD.0000000000001612. PMC 4635766. PMID 26402826.
- Axelrad JE, Lichtiger S, Yajnik V (May 2016). "Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment". World Journal of Gastroenterology. 22 (20): 4794–801. doi:10.3748/wjg.v22.i20.4794. PMC 4873872. PMID 27239106.
- Croce CM (January 2008). "Oncogenes and cancer". The New England Journal of Medicine. 358 (5): 502–11. doi:10.1056/NEJMra072367. PMID 18234754. S2CID 8813076.
- Knudson AG (November 2001). "Two genetic hits (more or less) to cancer". Nature Reviews. Cancer. 1 (2): 157–62. doi:10.1038/35101031. PMID 11905807. S2CID 20201610.
- Nelson DA, Tan TT, Rabson AB, Anderson D, Degenhardt K, White E (September 2004). "Hypoxia and defective apoptosis drive genomic instability and tumorigenesis". Genes & Development. 18 (17): 2095–107. doi:10.1101/gad.1204904. PMC 515288. PMID 15314031.
- Merlo LM, Pepper JW, Reid BJ, Maley CC (December 2006). "Cancer as an evolutionary and ecological process". Nature Reviews. Cancer. 6 (12): 924–35. doi:10.1038/nrc2013. PMID 17109012. S2CID 8040576.
- Baylin SB, Ohm JE (February 2006). "Epigenetic gene silencing in cancer – a mechanism for early oncogenic pathway addiction?". Nature Reviews. Cancer. 6 (2): 107–16. doi:10.1038/nrc1799. PMID 16491070. S2CID 2514545.
- Kanwal R, Gupta S (April 2012). "Epigenetic modifications in cancer". Clinical Genetics. 81 (4): 303–11. doi:10.1111/j.1399-0004.2011.01809.x. PMC 3590802. PMID 22082348.
- Baldassarre G, Battista S, Belletti B, Thakur S, Pentimalli F, Trapasso F, et al. (April 2003). "Negative regulation of BRCA1 gene expression by HMGA1 proteins accounts for the reduced BRCA1 protein levels in sporadic breast carcinoma". Molecular and Cellular Biology. 23 (7): 2225–38. doi:10.1128/MCB.23.7.2225-2238.2003. PMC 150734. PMID 12640109./
- Schnekenburger M, Diederich M (March 2012). "Epigenetics Offer New Horizons for Colorectal Cancer Prevention". Current Colorectal Cancer Reports. 8 (1): 66–81. doi:10.1007/s11888-011-0116-z. PMC 3277709. PMID 22389639.
- Jacinto FV, Esteller M (July 2007). "Mutator pathways unleashed by epigenetic silencing in human cancer". Mutagenesis. 22 (4): 247–53. doi:10.1093/mutage/gem009. PMID 17412712.
- Lahtz C, Pfeifer GP (February 2011). "Epigenetic changes of DNA repair genes in cancer". Journal of Molecular Cell Biology. 3 (1): 51–8. doi:10.1093/jmcb/mjq053. PMC 3030973. PMID 21278452.
- Bernstein C, Nfonsam V, Prasad AR, Bernstein H (March 2013). "Epigenetic field defects in progression to cancer". World Journal of Gastrointestinal Oncology. 5 (3): 43–49. doi:10.4251/wjgo.v5.i3.43. PMC 3648662. PMID 23671730.
- Narayanan L, Fritzell JA, Baker SM, Liskay RM, Glazer PM (April 1997). "Elevated levels of mutation in multiple tissues of mice deficient in the DNA mismatch repair gene Pms2". Proceedings of the National Academy of Sciences of the United States of America. 94 (7): 3122–27. Bibcode:1997PNAS...94.3122N. doi:10.1073/pnas.94.7.3122. PMC 20332. PMID 9096356.
- Hegan DC, Narayanan L, Jirik FR, Edelmann W, Liskay RM, Glazer PM (December 2006). "Differing patterns of genetic instability in mice deficient in the mismatch repair genes Pms2, Mlh1, Msh2, Msh3 and Msh6". Carcinogenesis. 27 (12): 2402–08. doi:10.1093/carcin/bgl079. PMC 2612936. PMID 16728433.
- Tutt AN, van Oostrom CT, Ross GM, van Steeg H, Ashworth A (March 2002). "Disruption of Brca2 increases the spontaneous mutation rate in vivo: synergism with ionizing radiation". EMBO Reports. 3 (3): 255–60. doi:10.1093/embo-reports/kvf037. PMC 1084010. PMID 11850397.
- German J (March 1969). "Bloom's syndrome. I. Genetical and clinical observations in the first twenty-seven patients". American Journal of Human Genetics. 21 (2): 196–227. PMC 1706430. PMID 5770175.
- O'Hagan HM, Mohammad HP, Baylin SB (August 2008). Lee JT (ed.). "Double strand breaks can initiate gene silencing and SIRT1-dependent onset of DNA methylation in an exogenous promoter CpG island". PLOS Genetics. 4 (8): e1000155. doi:10.1371/journal.pgen.1000155. PMC 2491723. PMID 18704159.
- Cuozzo C, Porcellini A, Angrisano T, Morano A, Lee B, Di Pardo A, et al. (July 2007). "DNA damage, homology-directed repair, and DNA methylation". PLOS Genetics. 3 (7): e110. doi:10.1371/journal.pgen.0030110. PMC 1913100. PMID 17616978.
- Malkin D (April 2011). "Li-fraumeni syndrome". Genes & Cancer. 2 (4): 475–84. doi:10.1177/1947601911413466. PMC 3135649. PMID 21779515.
- Fearon ER (November 1997). "Human cancer syndromes: clues to the origin and nature of cancer". Science. 278 (5340): 1043–50. Bibcode:1997Sci...278.1043F. doi:10.1126/science.278.5340.1043. PMID 9353177.
- Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW (March 2013). "Cancer genome landscapes". Science. 339 (6127): 1546–58. Bibcode:2013Sci...339.1546V. doi:10.1126/science.1235122. PMC 3749880. PMID 23539594.
- ^ Zheng J (2012). "Energy metabolism of cancer: Glycolysis versus oxidative phosphorylation (Review)". Oncology Letters. 4 (6): 1151–1157. doi:10.3892/ol.2012.928. PMC 3506713. PMID 23226794.
- Seyfried TN, Shelton LM (2010). "Cancer as a metabolic disease". Nutrition & Metabolism. 7: 7. doi:10.1186/1743-7075-7-7. PMC 2845135. PMID 20181022.
- Weiss JM (2020). "The promise and peril of targeting cell metabolism for cancer therapy". Cancer Immunology, Immunotherapy. 69 (2): 255–261. doi:10.1007/s00262-019-02432-7. PMC 7004869. PMID 31781842.
- Farhadi P, Yarani R, Dokaneheifard S, Mansouri K (2020). "The emerging role of targeting cancer metabolism for cancer therapy". Tumor Biology. 42 (10): 1010428320965284. doi:10.1177/1010428320965284. PMID 33028168. S2CID 222214285.
- Pavlova NN, Thompson CB (2016). "The Emerging Hallmarks of Cancer Metabolism". Cell Metabolism. 23 (1): 27–47. doi:10.1016/j.cmet.2015.12.006. PMC 4715268. PMID 26771115.
- Yadav UP, Singh T, Kumar P, Mehta K (2020). "Metabolic Adaptations in Cancer Stem Cells". Frontiers in Oncology. 10: 1010. doi:10.3389/fonc.2020.01010. PMC 7330710. PMID 32670883.
- "Cancer Screening Guidelines | Detecting Cancer Early". American Cancer Society. 14 March 2022. Retrieved 24 May 2022.
- Connolly JL, Schnitt SJ, Wang HH, Longtine JA, Dvorak A, Dvorak HF (2003). "Role of the Surgical Pathologist in the Diagnosis and Management of the Cancer Patient". In Holland JF, Frei E, Kufe DW (eds.). Holland-Frei Cancer Medicine (6 ed.). Hamilton (ON): BC Decker. ISBN 978-1-55009-213-4.
- Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M (November 2012). "Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients". The Cochrane Database of Systematic Reviews. 11 (11): CD007064. doi:10.1002/14651858.cd007064.pub2. PMC 6457819. PMID 23152241.
- Pearson C (10 January 2024). "Why Some People Keep Serious Illnesses Private". The New York Times.
- Varricchio C (2004). A cancer source book for nurses. Boston: Jones and Bartlett Publishers. p. 229. ISBN 978-0-7637-3276-9.
- Image by Mikael Häggström, MD. Source for findings: Underwood CI, Glass C. "Lung – Small cell carcinoma". Pathology Outlines. Last author update: 20 September 2022
- ^ Tran KB, Lang JJ, Compton K, Xu R, Acheson AR, Henrikson HJ, et al. (August 2022). "The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019". Lancet. 400 (10352): 563–591. doi:10.1016/S0140-6736(22)01438-6. PMC 9395583. PMID 35988567.
- "Cancer prevention: 7 steps to reduce your risk". Mayo Clinic. 27 September 2008. Archived from the original on 8 February 2010. Retrieved 30 January 2010.
- Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M (November 2005). "Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors". Lancet. 366 (9499): 1784–93. doi:10.1016/S0140-6736(05)67725-2. PMID 16298215. S2CID 17354479.
- Wu S, Powers S, Zhu W, Hannun YA (January 2016). "Substantial contribution of extrinsic risk factors to cancer development". Nature. 529 (7584): 43–7. Bibcode:2016Natur.529...43W. doi:10.1038/nature16166. PMC 4836858. PMID 26675728.
- "Cancer". World Health Organization. Archived from the original on 29 December 2010. Retrieved 9 January 2011.
- Heidary F, Rahimi A, Gharebaghi R (2013). "Poverty as a risk factor in human cancers". Iranian Journal of Public Health. 42 (3): 341–343. PMC 3633807. PMID 23641414.
- ^ Wicki A, Hagmann J (September 2011). "Diet and cancer". Swiss Medical Weekly. 141: w13250. doi:10.4414/smw.2011.13250. PMID 21904992.
- Cappellani A, Di Vita M, Zanghi A, Cavallaro A, Piccolo G, Veroux M, et al. (January 2012). "Diet, obesity and breast cancer: an update". Frontiers in Bioscience. 4 (1): 90–108. doi:10.2741/253. PMID 22202045.
- Key TJ (January 2011). "Fruit and vegetables and cancer risk". British Journal of Cancer. 104 (1): 6–11. doi:10.1038/sj.bjc.6606032. PMC 3039795. PMID 21119663.
- Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. (July 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
- Larsson SC, Wolk A (May 2007). "Coffee consumption and risk of liver cancer: a meta-analysis". Gastroenterology. 132 (5): 1740–5. doi:10.1053/j.gastro.2007.03.044. PMID 17484871.
- Zheng W, Lee SA (2009). "Well-done meat intake, heterocyclic amine exposure, and cancer risk". Nutrition and Cancer. 61 (4): 437–46. doi:10.1080/01635580802710741. PMC 2769029. PMID 19838915.
- Ferguson LR (February 2010). "Meat and cancer". Meat Science. 84 (2): 308–13. doi:10.1016/j.meatsci.2009.06.032. PMID 20374790.
- Staff (26 October 2015). "World Health Organization – IARC Monographs evaluate consumption of red meat and processed meat" (PDF). International Agency for Research on Cancer. Archived (PDF) from the original on 26 October 2015. Retrieved 26 October 2015.
- Hauser C (26 October 2015). "W.H.O. Report Links Some Cancers With Processed or Red Meat". The New York Times. Archived from the original on 26 October 2015. Retrieved 26 October 2015.
- Holland Chp.33
- Rostom A, Dubé C, Lewin G, Tsertsvadze A, Barrowman N, Code C, et al. (March 2007). "Nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 146 (5): 376–89. doi:10.7326/0003-4819-146-5-200703060-00010. PMID 17339623.
- Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW (January 2011). "Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials". Lancet. 377 (9759): 31–41. doi:10.1016/S0140-6736(10)62110-1. PMID 21144578. S2CID 22950940.
- Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, et al. (June 2010). "Chemoprevention of colorectal cancer: systematic review and economic evaluation". Health Technology Assessment. 14 (32): 1–206. doi:10.3310/hta14320. PMID 20594533.
- Thomsen A, Kolesar JM (December 2008). "Chemoprevention of breast cancer". American Journal of Health-System Pharmacy. 65 (23): 2221–28. doi:10.2146/ajhp070663. PMID 19020189.
- Wilt TJ, MacDonald R, Hagerty K, Schellhammer P, Kramer BS (April 2008). Wilt TJ (ed.). "Five-alpha-reductase Inhibitors for prostate cancer prevention". The Cochrane Database of Systematic Reviews (2): CD007091. doi:10.1002/14651858.CD007091. PMC 11270836. PMID 18425978.
- "Vitamins and minerals: not for cancer or cardiovascular prevention". Prescrire International. 19 (108): 182. August 2010. PMID 20939459. Archived from the original on 25 May 2012.
- Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ, et al. (April 2006). "Prospective study of predictors of vitamin D status and cancer incidence and mortality in men". Journal of the National Cancer Institute. 98 (7): 451–59. CiteSeerX 10.1.1.594.1654. doi:10.1093/jnci/djj101. PMID 16595781.
- "Vitamin D Has Role in Colon Cancer Prevention". Archived from the original on 4 December 2006. Retrieved 27 July 2007.
- Holick MF (January 2013). "Vitamin D, sunlight and cancer connection". Anti-Cancer Agents in Medicinal Chemistry. 13 (1): 70–82. doi:10.2174/187152013804487308. PMID 23094923.
- Schwartz GG, Blot WJ (April 2006). "Vitamin D status and cancer incidence and mortality: something new under the sun". Journal of the National Cancer Institute. 98 (7): 428–30. doi:10.1093/jnci/djj127. PMID 16595770.
- ^ Bolland MJ, Grey A, Gamble GD, Reid IR (April 2014). "The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis". The Lancet. Diabetes & Endocrinology. 2 (4): 307–320. doi:10.1016/S2213-8587(13)70212-2. PMID 24703049.
- Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Wetterslev J, Simonetti RG, et al. (January 2014). "Vitamin D supplementation for prevention of mortality in adults". The Cochrane Database of Systematic Reviews. 1 (1): CD007470. doi:10.1002/14651858.cd007470.pub3. PMC 11285307. PMID 24414552. S2CID 205189615.
- Fritz H, Kennedy D, Fergusson D, Fernandes R, Doucette S, Cooley K, et al. (2011). Minna JD (ed.). "Vitamin A and retinoid derivatives for lung cancer: a systematic review and meta analysis". PLOS ONE. 6 (6): e21107. Bibcode:2011PLoSO...621107F. doi:10.1371/journal.pone.0021107. PMC 3124481. PMID 21738614.
- Cole BF, Baron JA, Sandler RS, Haile RW, Ahnen DJ, Bresalier RS, et al. (June 2007). "Folic acid for the prevention of colorectal adenomas: a randomized clinical trial". JAMA. 297 (21): 2351–2359. doi:10.1001/jama.297.21.2351. PMID 17551129.
- Vinceti M, Filippini T, Del Giovane C, Dennert G, Zwahlen M, Brinkman M, et al. (January 2018). "Selenium for preventing cancer". The Cochrane Database of Systematic Reviews. 1 (1): CD005195. doi:10.1002/14651858.CD005195.pub4. PMC 6491296. PMID 29376219.
- ^ "Cancer Vaccine Fact Sheet". NCI. 8 June 2006. Retrieved 28 March 2018.
- ^ Lertkhachonsuk AA, Yip CH, Khuhaprema T, Chen DS, Plummer M, Jee SH, et al. (November 2013). "Cancer prevention in Asia: resource-stratified guidelines from the Asian Oncology Summit 2013". The Lancet. Oncology. 14 (12): e497–507. arXiv:cond-mat/0606434. doi:10.1016/S1470-2045(13)70350-4. PMID 24176569.
- ^ "Cancer Screening Overview (PDQ®)–Patient Version". National Cancer Institute. 13 January 2010. Retrieved 28 March 2018.
- ^ Wilson JMG, Jungner G. (1968) Principles and practice of screening for disease. Geneva: World Health Organization. Public Health Papers, No. 34.
- "Screening for Cervical Cancer". U.S. Preventive Services Task Force. 2003. Archived from the original on 23 December 2010. Retrieved 21 December 2010.
- "Screening for Colorectal Cancer". U.S. Preventive Services Task Force. 2008. Archived from the original on 7 February 2015. Retrieved 21 December 2010.
- "Screening for Skin Cancer". U.S. Preventive Services Task Force. 2009. Archived from the original on 8 January 2011. Retrieved 21 December 2010.
- "Screening for Oral Cancer". U.S. Preventive Services Task Force. 2004. Archived from the original on 24 October 2010. Retrieved 21 December 2010.
- "Lung Cancer Screening". U.S. Preventive Services Task Force. 2004. Archived from the original on 4 November 2010. Retrieved 21 December 2010.
- "Screening for Prostate Cancer". U.S. Preventive Services Task Force. 2008. Archived from the original on 31 December 2010. Retrieved 21 December 2010.
- "Screening for Bladder Cancer". U.S. Preventive Services Task Force. 2004. Archived from the original on 23 August 2010. Retrieved 21 December 2010.
- "Screening for Testicular Cancer". U.S. Preventive Services Task Force. 2004. Archived from the original on 15 May 2016. Retrieved 21 December 2010.
- "Screening for Ovarian Cancer". U.S. Preventive Services Task Force. 2004. Archived from the original on 23 October 2010. Retrieved 21 December 2010.
- "Screening for Pancreatic Cancer". U.S. Preventive Services Task Force. 2004. Archived from the original on 21 November 2010. Retrieved 21 December 2010.
- Chou R, Croswell JM, Dana T, Bougatsos C, Blazina I, Fu R, et al. (December 2011). "Screening for prostate cancer: a review of the evidence for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 155 (11). United States Preventive Services Task Force: 762–71. doi:10.7326/0003-4819-155-11-201112060-00375. PMID 21984740.
- "Screening for Breast Cancer". U.S. Preventive Services Task Force. 2009. Archived from the original on 2 January 2013. Retrieved 21 December 2010.
- Gøtzsche PC, Jørgensen KJ (June 2013). "Screening for breast cancer with mammography". The Cochrane Database of Systematic Reviews. 2013 (6): CD001877. doi:10.1002/14651858.CD001877.pub5. PMC 6464778. PMID 23737396.
- ^ Gulati AP, Domchek SM (January 2008). "The clinical management of BRCA1 and BRCA2 mutation carriers". Current Oncology Reports. 10 (1): 47–53. doi:10.1007/s11912-008-0008-9. PMID 18366960. S2CID 29630942.
- Lind MJ (2008). "Principles of cytotoxic chemotherapy". Medicine. 36 (1): 19–23. doi:10.1016/j.mpmed.2007.10.003.
- Frei III E, Eder JP (2003). Combination Chemotherapy. Retrieved 4 April 2020.
- Dear RF, McGeechan K, Jenkins MC, Barratt A, Tattersall MH, Wilcken N (December 2013). "Combination versus sequential single agent chemotherapy for metastatic breast cancer". The Cochrane Database of Systematic Reviews. 2021 (12): CD008792. doi:10.1002/14651858.CD008792.pub2. PMC 8094913. PMID 24347031.
- ^ Holland Chp. 40
- Nastoupil LJ, Rose AC, Flowers CR (May 2012). "Diffuse large B-cell lymphoma: current treatment approaches". Oncology. 26 (5): 488–95. PMID 22730604.
- Freedman A (October 2012). "Follicular lymphoma: 2012 update on diagnosis and management". American Journal of Hematology. 87 (10): 988–95. doi:10.1002/ajh.23313. PMID 23001911. S2CID 35447562.
- Rampling R, James A, Papanastassiou V (June 2004). "The present and future management of malignant brain tumours: surgery, radiotherapy, chemotherapy". Journal of Neurology, Neurosurgery, and Psychiatry. 75 (Suppl 2): ii24–30. doi:10.1136/jnnp.2004.040535. PMC 1765659. PMID 15146036.
- Madan V, Lear JT, Szeimies RM (February 2010). "Non-melanoma skin cancer". Lancet. 375 (9715): 673–85. doi:10.1016/S0140-6736(09)61196-X. PMC 3339125. PMID 20171403.
- Vitale I, Galluzzi L, Castedo M, Kroemer G (June 2011). "Mitotic catastrophe: a mechanism for avoiding genomic instability". Nature Reviews. Molecular Cell Biology. 12 (6): 385–392. doi:10.1038/nrm3115. PMID 21527953. S2CID 22483746.
- Bomford CK, Kunkler IH, Walter J. Walter and Miller's Textbook of Radiation therapy (6th ed.). p. 311.
- McMorran J, Crowther D, McMorran S, Youngmin S, Wacogne I, Pleat J, et al. "tumour radiosensitivity – General Practice Notebook". Archived from the original on 24 September 2015.
- Tidy C (23 December 2015). "Radiotherapy". Patient UK. Archived from the original on 9 July 2017. Last Checked: 23 December 2015
- Hill R, Healy B, Holloway L, Kuncic Z, Thwaites D, Baldock C (March 2014). "Advances in kilovoltage x-ray beam dosimetry". Physics in Medicine and Biology. 59 (6): R183–231. Bibcode:2014PMB....59R.183H. doi:10.1088/0031-9155/59/6/r183. PMID 24584183. S2CID 18082594.
- ^ Holland Chp. 41
- "Radiation Therapy for Brain Metastases: A Systematic Review". PCORI. 13 August 2019. Retrieved 10 October 2023.
- American Society of Clinical Oncology. "Five Things Physicians and Patients Should Question" (PDF). Choosing Wisely: An Initiative of the ABIM Foundation. Archived from the original (PDF) on 31 July 2012. Retrieved 14 August 2012.
* The American Society of Clinical Oncology made this recommendation based on various cancers. - "NCCN Guidelines". Archived from the original on 14 May 2008.
- "Clinical Practice Guidelines for Quality Palliative Care" (PDF). The National Consensus Project for Quality Palliative Care (NCP). Archived from the original (PDF) on 16 May 2011.
- Levy MH, Back A, Bazargan S, Benedetti C, Billings JA, Block S, et al. (September 2006). "Palliative care. Clinical practice guidelines in oncology". Journal of the National Comprehensive Cancer Network. 4 (8): 776–818. doi:10.6004/jnccn.2006.0068. PMID 16948956. S2CID 44343423.
- Waldmann TA (March 2003). "Immunotherapy: past, present and future". Nature Medicine. 9 (3): 269–77. doi:10.1038/nm0303-269. PMID 12612576. S2CID 9745527.
- "Lasers in Cancer Treatment". National Institutes of Health, National Cancer Institute. 13 September 2011. Retrieved 15 December 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- Cassileth BR, Deng G (2004). "Complementary and alternative therapies for cancer" (PDF). The Oncologist. 9 (1): 80–89. doi:10.1634/theoncologist.9-1-80. PMID 14755017. S2CID 6453919.
- What Is CAM? Archived 8 December 2005 at the Wayback Machine National Center for Complementary and Alternative Medicine. Retrieved 3 February 2008.
- Vickers A (2004). "Alternative cancer cures: "unproven" or "disproven"?". CA: A Cancer Journal for Clinicians. 54 (2): 110–18. CiteSeerX 10.1.1.521.2180. doi:10.3322/canjclin.54.2.110. PMID 15061600. S2CID 35124492.
- "Three measures of cancer mortality". Our World in Data. Retrieved 7 March 2020.
- Tammela T, Sage J (March 2020). "Investigating Tumor Heterogeneity in Mouse Models". Annual Review of Cancer Biology. 4 (1): 99–119. doi:10.1146/annurev-cancerbio-030419-033413. PMC 8218894. PMID 34164589.
- World Cancer Report 2014. World Health Organization. 2014. p. 22. ISBN 978-92-832-0429-9. Archived from the original on 12 July 2017.
- ^ Rheingold S, Neugut A, Meadows A (2003). "156: Secondary Cancers: Incidence, Risk Factors, and Management". In Frei E, Kufe DW, Holland JF (eds.). Holland-Frei Cancer Medicine (6th ed.). Hamilton, Ont: BC Decker. p. 2399. ISBN 978-1-55009-213-4.
- Montazeri A (December 2009). "Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008". Health and Quality of Life Outcomes. 7: 102. doi:10.1186/1477-7525-7-102. PMC 2805623. PMID 20030832.
- ^ Akl EA, Kahale LA, Hakoum MB, Matar CF, Sperati F, Barba M, et al. (September 2017). "Parenteral anticoagulation in ambulatory patients with cancer". The Cochrane Database of Systematic Reviews. 2021 (9): CD006652. doi:10.1002/14651858.CD006652.pub5. PMC 6419241. PMID 28892556.
- Radha G, Lopus M (September 2021). "The spontaneous remission of cancer: Current insights and therapeutic significance". Translational Oncology. 14 (9): 101166. doi:10.1016/j.tranon.2021.101166. PMC 8271173. PMID 34242964.
- "Cancer death rates". Our World in Data. Retrieved 4 October 2019.
- ^ "Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018" (PDF). iarc.fr. Retrieved 5 December 2018.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ Coleman WB, Rubinas TC (2009). "4". In Tsongalis GJ, Coleman WL (eds.). Molecular Pathology: The Molecular Basis of Human Disease. Amsterdam: Elsevier Academic Press. p. 66. ISBN 978-0-12-374419-7.
- Johnson G (28 December 2010). "Unearthing Prehistoric Tumors, and Debate". The New York Times. Archived from the original on 24 June 2017.
- Pawelec G, Derhovanessian E, Larbi A (August 2010). "Immunosenescence and cancer". Critical Reviews in Oncology/Hematology. 75 (2): 165–72. doi:10.1016/j.critrevonc.2010.06.012. PMID 20656212.
- Alberts B, Johnson A, Lewis J, et al. (2002). "The Preventable Causes of Cancer". Molecular biology of the cell (4th ed.). New York: Garland Science. ISBN 978-0-8153-4072-0. Archived from the original on 2 January 2016.
A certain irreducible background incidence of cancer is to be expected regardless of circumstances: mutations can never be absolutely avoided, because they are an inescapable consequence of fundamental limitations on the accuracy of DNA replication, as discussed in Chapter 5. If a human could live long enough, it is inevitable that at least one of his or her cells would eventually accumulate a set of mutations sufficient for cancer to develop.
- Anisimov VN, Sikora E, Pawelec G (August 2009). "Relationships between cancer and aging: a multilevel approach". Biogerontology. 10 (4): 323–38. doi:10.1007/s10522-008-9209-8. PMID 19156531. S2CID 17412298.
- de Magalhães JP (May 2013). "How ageing processes influence cancer". Nature Reviews. Cancer. 13 (5): 357–65. doi:10.1038/nrc3497. PMID 23612461. S2CID 5726826.
- David S, Fraumeni JF (24 August 2006). Cancer Epidemiology and Prevention. Oxford University Press. p. 977. ISBN 978-0-19-974797-9.
- Bostwick DG, Eble JN (2007). Urological Surgical Pathology. St. Louis: Mosby. p. 468. ISBN 978-0-323-01970-5.
- ^ Kaatsch P (June 2010). "Epidemiology of childhood cancer". Cancer Treatment Reviews. 36 (4): 277–285. doi:10.1016/j.ctrv.2010.02.003. PMID 20231056.
- ^ Ward E, DeSantis C, Robbins A, Kohler B, Jemal A (January 2014). "Childhood and adolescent cancer statistics, 2014". CA. 64 (2): 83–103. doi:10.3322/caac.21219. PMID 24488779. S2CID 34364885.
- Ward EM, Thun MJ, Hannan LM, Jemal A (September 2006). "Interpreting cancer trends". Annals of the New York Academy of Sciences. 1076 (1): 29–53. Bibcode:2006NYASA1076...29W. doi:10.1196/annals.1371.048. PMID 17119192. S2CID 1579801.
- ^ Hajdu SI (March 2011). "A note from history: landmarks in history of cancer, part 1". Cancer. 117 (5): 1097–102. doi:10.1002/cncr.25553. PMID 20960499. S2CID 39667103.
- Paul of Aegina, 7th century AD, quoted in Moss RW (2004). "Galen on Cancer". CancerDecisions. Archived from the original on 16 July 2011. Referenced from Michael Shimkin, Contrary to Nature, Washington, DC: Superintendent of Document, DHEW Publication No. (NIH) 79–720, p. 35.
- Majno G, Joris I (12 August 2004). Cells, Tissues, and Disease: Principles of General Pathology: Principles of General Pathology. Oxford University Press. ISBN 978-0-19-974892-1. Retrieved 11 September 2013.
- ^ Hajdu SI (June 2011). "A note from history: landmarks in history of cancer, part 2". Cancer. 117 (12): 2811–20. doi:10.1002/cncr.25825. PMID 21656759. S2CID 28148111.
- Yalom M (1998). A history of the breast (1 ed.). New York: Ballantine Books. ISBN 978-0-679-43459-7.
- Hajdu SI (February 2012). "A note from history: landmarks in history of cancer, part 3". Cancer. 118 (4): 1155–68. doi:10.1002/cncr.26320. PMID 21751192. S2CID 38892895.
- Grange JM, Stanford JL, Stanford CA (June 2002). "Campbell De Morgan's 'Observations on cancer', and their relevance today". Journal of the Royal Society of Medicine. 95 (6): 296–299. doi:10.1177/014107680209500609. PMC 1279913. PMID 12042378.
- Barbara E (November 2001). "Welcome to Cancerland". Harper's Magazine. ISSN 0017-789X. Archived from the original on 8 November 2013.
- Pozorski A (20 March 2015). "Confronting the "C" Word: Cancer and Death in Philip Roth's Fiction". Philip Roth Studies. 11 (1): 105–123. doi:10.5703/philrothstud.11.1.105. ISSN 1940-5278. S2CID 160969212. Retrieved 13 April 2020.
- Wollaston S (4 May 2015). "The C-Word review – a wonderful testament to a woman who faced cancer with honesty, verve and wit". The Guardian. Retrieved 13 April 2020.
- "Avoiding the 'C' Word for Low-Risk Thyroid Cancer". Medscape. Retrieved 13 April 2020.
- "The C word: how we react to cancer today". NHS Networks. Archived from the original on 22 October 2020. Retrieved 13 April 2020.
- ^ Chochinov HM, Breitbart W (2009). Handbook of Psychiatry in Palliative Medicine. Oxford University Press. p. 196. ISBN 978-0-19-530107-6.
- Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- "Skin cancers". World Health Organization. Archived from the original on 27 September 2010. Retrieved 19 January 2011.
- McCulley M, Greenwell P (2007). Molecular therapeutics: 21st-century medicine. London: J. Wiley. p. 207. ISBN 978-0-470-01916-0.
- Low G, Cameron L (1999). "10". Researching and Applying Metaphor. Cambridge University Press. ISBN 978-0-521-64964-3.
- Sulik GA (2010). Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. Oxford University Press. pp. 78–89. ISBN 978-0-19-974993-5.
- ^ Olson JS (2005). Bathsheba's Breast: Women, Cancer, and History. JHU Press. pp. 145–70. ISBN 978-0-8018-8064-3. OCLC 186453370.
- ^ Ehrenreich B (2009). Bright-sided: How the Relentless Promotion of Positive Thinking Has Undermined America. Henry Holt and Company. pp. 15–44. ISBN 978-0-8050-8749-9.
- Huff C (24 September 2013). "A Sick Stigma: Why are cancer patients blamed for their illness?". Slate. Archived from the original on 11 October 2013.
- "Economic Impact of Cancer". American Cancer Society. 3 January 2018. Retrieved 5 July 2018.
- Bosanquet N, Sikora K (2004). "The economics of cancer care in the UK". Lancet Oncology. 5 (9): 568–74. doi:10.1016/S1470-2045(04)01569-4. PMID 15337487.
- Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011). "Projections of the cost of cancer care in the United States: 2010–2020". Journal of the National Cancer Institute. 103 (2): 117–28. doi:10.1093/jnci/djq495. PMC 3107566. PMID 21228314.
- Jönsson B, Hofmarcher T, Lindgren P, Wilking N (2016). "The cost and burden of cancer in the European Union 1995–2014". European Journal of Cancer. 66 (Oct): 162–70. doi:10.1016/j.ejca.2016.06.022. PMID 27589247.
- ^ Hofmarcher T, Lindgren P, Wilking N, Jönsson B (2020). "The cost of cancer in Europe 2018". European Journal of Cancer. 129 (Apr): 41–49. doi:10.1016/j.ejca.2020.01.011. PMID 32120274.
- Luengo-Fernandez R, Leal J, Gray A, Sullivan R (2013). "Economic burden of cancer across the European Union: a population-based cost analysis". Lancet Oncology. 14 (12): 1165–74. doi:10.1016/S1470-2045(13)70442-X. PMID 24131614.
- ^ U.S. Equal Employment Opportunity Commission. "Questions & Answers about Cancer in the Workplace and the Americans with Disabilities Act (ADA)." https://www.eeoc.gov/laws/types/cancer.cfm
- Glantz MJ, Chamberlain MC, Liu Q, Hsieh CC, Edwards KR, Van Horn A, et al. (November 2009). "Gender disparity in the rate of partner abandonment in patients with serious medical illness". Cancer. 115 (22): 5237–5242. doi:10.1002/cncr.24577. PMID 19645027.
- Stephens C, Westmaas JL, Kim J, Cannady R, Stein K (October 2016). "Gender differences in associations between cancer-related problems and relationship dissolution among cancer survivors". Journal of Cancer Survivorship. 10 (5): 865–873. doi:10.1007/s11764-016-0532-9. PMID 26995006.
- Fugmann D, Boeker M, Holsteg S, Steiner N, Prins J, Karger A (9 March 2022). "A Systematic Review: The Effect of Cancer on the Divorce Rate". Frontiers in Psychology. 13: 828656. doi:10.3389/fpsyg.2022.828656. PMC 8959852. PMID 35356338.
- "Cancer Fact Sheet". Agency for Toxic Substances & Disease Registry. 30 August 2002. Archived from the original on 13 August 2009. Retrieved 17 August 2009.
- Wanjek C (16 September 2006). "Exciting New Cancer Treatments Emerge Amid Persistent Myths". Live Science. Archived from the original on 16 May 2008. Retrieved 17 August 2009.
- Hayden EC (April 2009). "Cutting off cancer's supply lines". Nature. 458 (7239): 686–87. doi:10.1038/458686b. PMID 19360048.
- Bagri A, Kouros-Mehr H, Leong KG, Plowman GD (March 2010). "Use of anti-VEGF adjuvant therapy in cancer: challenges and rationale". Trends in Molecular Medicine. 16 (3): 122–32. doi:10.1016/j.molmed.2010.01.004. PMID 20189876.
- Sleigh SH, Barton CL (2010). "Repurposing Strategies for Therapeutics". Pharmaceutical Medicine. 24 (3): 151–59. doi:10.1007/BF03256811. S2CID 25267555.
- Winther H, Jorgensen JT (2010). "Drug-Diagnostic Co-Development in Cancer". Pharmaceutical Medicine. 24 (6): 363–75. doi:10.1007/BF03256837. S2CID 43505621.
- Begley S (16 September 2008). "Rethinking the War on Cancer". Newsweek. Archived from the original on 10 September 2008. Retrieved 8 September 2008.
- ^ Kolata G (23 April 2009). "Advances Elusive in the Drive to Cure Cancer". The New York Times. Archived from the original on 14 January 2012. Retrieved 5 May 2009.
- Alberts B, Kirschner MW, Tilghman S (2014). "Rescuing US biomedical research from its systemic flaws". Proceedings of the National Academy of Sciences of the United States of America. 111 (16): 5773–77. Bibcode:2014PNAS..111.5773A. doi:10.1073/pnas.1404402111. PMC 4000813. PMID 24733905.
- Kolata G (27 June 2009). "Grant System Leads Cancer Researchers to Play It Safe". The New York Times. Archived from the original on 8 June 2011. Retrieved 29 December 2009.
- Powell K (2016). "Young, talented and fed-up: scientists tell their stories". Nature. 538 (7626): 446–49. Bibcode:2016Natur.538..446P. doi:10.1038/538446a. PMID 27786221. S2CID 4465686.
- "Opinion | I'm an oncologist. My worst fears about Covid and cancer are coming true". NBC News. 12 February 2021.
- "Don't sacrifice cancer care to COVID". New York Daily News. 13 January 2021.
- ^ "Revolutionary nanodrones enable targeted cancer treatment". ScienceDaily. Retrieved 24 March 2024.
- ^ Yarbro CH, Wujcik D, Gobel BH (2010). Cancer Nursing: Principles and Practice. Jones & Bartlett Learning. pp. 901–905. ISBN 978-0-7637-6357-2.
- Thamm D (March 2009). "How companion animals contribute to the fight against cancer in humans" (PDF). Veterinaria Italiana. 54 (1): 111–20. PMID 20391394. Archived (PDF) from the original on 23 July 2014. Retrieved 18 July 2014.
- Vincze O, Colchero F, Lemaître JF, Conde DA, Pavard S, Bieuville M, et al. (January 2022). "Cancer risk across mammals". Nature. 601 (7892): 263–267. Bibcode:2022Natur.601..263V. doi:10.1038/s41586-021-04224-5. PMC 8755536. PMID 34937938. S2CID 245425871.
- Murgia C, Pritchard JK, Kim SY, Fassati A, Weiss RA (August 2006). "Clonal origin and evolution of a transmissible cancer". Cell. 126 (3): 477–87. doi:10.1016/j.cell.2006.05.051. PMC 2593932. PMID 16901782.
Further reading
- Bast RC, Croe CM, Hait WN, Hong WK, Kufe DW, Piccart-Gebhart M, et al. (2016). Holland-Frei Cancer Medicine. Wiley. ISBN 978-1-118-93469-2.
- Kleinsmith LJ (2006). Principles of cancer biology. Pearson Benjamin Cummings. ISBN 978-0-8053-4003-7.
- Mukherjee S (2010). The Emperor of All Maladies: A Biography of Cancer. Simon & Schuster. ISBN 978-1-4391-0795-9. Retrieved 7 August 2013.
- Pazdur R, Camphausen KA, Wagman LD, Hoskins WJ (2009). Cancer Management: A Multidisciplinary Approach. Cmp United Business Media. ISBN 978-1-891483-62-2. Cancer at Google Books. Archived from the original on 15 May 2009.
- Schwab M (2008). Encyclopedia of Cancer. Springer Science & Business Media. ISBN 978-3-540-36847-2.
- Tannock I (2005). The basic science of oncology. McGraw-Hill Professional. ISBN 978-0-07-138774-3.
External links
- IARC Publications (WHO) | Publications.iarc.fr
- "On telling cancer patients to have a positive attitude" at The Atlantic
- WHO fact sheet on cancer
- National Firefighter Registry (NFR) for Cancer, National Institute for Occupational Safety and Health (NIOSH), USA
- Stop carcinogens at work, EU OSHA. The site shares information to help prevent workers from being exposed to carcinogens in the workplace.
- Occupational Cancer, NIOSH.
- NIOSH Pocket guide to chemical hazards, Appendix A- NIOSH Potential Occupational Carcinogens.
| Classification | D |
|---|---|
| External resources |
| Overview of tumors, cancer and oncology | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Conditions |
| ||||||||||
| Staging/grading | |||||||||||
| Carcinogenesis | |||||||||||
| Misc. | |||||||||||
| Major Disease groups | |
|---|---|