| Revision as of 22:12, 3 September 2008 view sourceRamdrake (talk | contribs)8,680 edits You are misconstruing what the reference says. As per W¨P:BRD, please take it to the talk page.← Previous edit | Latest revision as of 19:46, 21 December 2024 view source GreenC bot (talk | contribs)Bots2,547,818 edits Rescued 1 archive link; reformat 1 link. Wayback Medic 2.5 per WP:USURPURL and JUDI batch #20 | ||
| Line 1: | Line 1: | ||
| {{short description|Inhalation of tobacco smoke by persons other than the intended active smoker}} | |||
| {{redirect|Second hand smoke|the ] album|Second-hand Smoke}} | |||
| {{Redirect|Second hand smoke|the Sublime album|Second-hand Smoke{{!}}''Second-hand Smoke''}} | |||
| ] before a ] came into effect on March 29, 2004]] | |||
| {{pp-semi-indef}} | |||
| ] before a ] came into effect on March 29, 2004]] | |||
| '''Passive smoking''' is the |
'''Passive smoking''' is the inhalation of ], called '''passive smoke''', '''secondhand smoke''' ('''SHS''') or '''environmental tobacco smoke''' ('''ETS'''), by individuals other than the active ]. It occurs when tobacco smoke ]s into the surrounding atmosphere as an ] ], which leads to its inhalation by nearby bystanders within the same environment. Exposure to secondhand tobacco smoke causes many of the same ],<ref name="sg-report">{{cite web |url = http://www.surgeongeneral.gov/library/reports/secondhandsmoke/fullreport.pdf |title = The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General |publisher = ] |date = 2006-06-27 |access-date = 2012-07-24 |quote = Secondhand smoke causes premature death and disease in children and in adults who do not smoke |archive-url = https://web.archive.org/web/20190226003026/https://www.surgeongeneral.gov/library/reports/secondhandsmoke/fullreport.pdf |archive-date = 2019-02-26 |url-status = dead }}</ref><ref name=IARC2004>{{harvnb|IARC|2004}} </ref> although at a lower prevalence due to the reduced concentration of smoke that enters the ]. | ||
| According to a WHO report published in 2023, more than 1.3 million deaths are attributed to passive smoking worldwide every year.<ref>{{Cite web |title=Tobacco |url=https://www.who.int/news-room/fact-sheets/detail/tobacco |access-date=2024-02-24 |website=www.who.int |language=en}}</ref> The health risks of secondhand smoke are a matter of ],<ref name="kessler" /><ref name="Samet008">{{cite journal |author=Samet JM |title=Secondhand smoke: facts and lies |journal=Salud Pública de México |volume=50 |issue=5 |pages=428–34 |year=2008 |pmid=18852940 |doi= 10.1590/S0036-36342008000500016|doi-access=free }}</ref><ref name="Circ07" /> and have been a major motivation for ]s in ]s and indoor venues, including ]s, ] and ]s, as well as some open ]s.<ref>{{Cite web|title = CDC - Fact Sheet - Smoke-Free Policies Reduce Smoking - Smoking & Tobacco Use|url = https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/protection/reduce_smoking/|website = Smoking and Tobacco Use|access-date = 2015-04-24}}</ref> | |||
| The risks associated with passive smoking are one of the main reasons for ]s in workplaces and indoor public places, including ], bars and night clubs. | |||
| Concerns around secondhand smoke have played a central role in the debate over the harms and regulation of tobacco products. Since the early 1970s, the ] has viewed public concern over secondhand smoke as a serious threat to its business interests.<ref name="smoke-screen">{{cite book |last1=Diethelm |first1=Pascal |last2=McKee |first2=Martin |title=Lifting the smokescreen: tobacco industry strategy to defeat smoke free policies and legislation |date=2006 |isbn=978-1-904097-57-0 |oclc=891398524 |url=https://www.oxysuisse.ch/files/public/publications/20060200-diethelm-mckee-lifting-the-smokescreen.pdf |page=5 |quote=The industry quickly realised that, if it wanted to continue to prosper, it became vital that research did not demonstrate that tobacco smoke was a dangerous community air pollutant. This requirement has been the central pillar of its passive smoking policy from the early 1970s to the present day }}</ref> Despite the industry's awareness of the harms of secondhand smoke as early as the 1980s, the tobacco industry coordinated a scientific controversy with the purpose of stopping regulation of their products.<ref name="kessler"/>{{rp|1242}}<ref name=Circ07>{{cite journal |last1=Tong |first1=Elisa K. |last2=Glantz |first2=Stanton A. |title=Tobacco Industry Efforts Undermining Evidence Linking Secondhand Smoke With Cardiovascular Disease |journal=Circulation |date=16 October 2007 |volume=116 |issue=16 |pages=1845–1854 |doi=10.1161/CIRCULATIONAHA.107.715888 |pmid=17938301 |s2cid=4021497|doi-access=free }}</ref> | |||
| ==Long-term effects== | |||
| Research has generated scientific evidence that secondhand smoke (that is, in the case of cigarettes, a mixture of smoke released from the smoldering end of the cigarette and smoke exhaled by the smoker) causes the same problems as direct smoking, including ],<ref>"An individual male never-smoker living with a current or former smoker is estimated to have an approximately 9.6% chance of dying of ischemic heart disease by the age of 74 years, compared with a 7.4% chance for a male never-smoker living with a nonsmoker. The corresponding lifetime risks for women are 6.1% and 4.9%." , ''The Journal of the American Medical Association'', Vol. 267 No. 1, January 1, 1992</ref> ], ], and ] such as ], ] and ].<ref>{{cite journal | author=Boyle P, Autier P, Bartelink H ''et al.'' | title=European Code Against Cancer and scientific justification: third version (2003). | journal=Ann Oncol. | volume=14 | issue=7 | year=2003 | pmid=12853336 | pages=973 | doi=10.1093/annonc/mdg305}}</ref> Specifically, ] have shown lifelong non-smokers with partners who smoke in the home have a 20–30% greater risk of lung cancer, and those exposed to cigarette smoke in the workplace have an increased risk of 16–19%.<ref>{{cite journal | author=Sasco AJ, Secretan MB, Straif K. | title=Tobacco smoking and cancer: a brief review of recent epidemiological evidence. | journal=Lung Cancer | volume=45 | issue=Suppl 2 | pages=S3–9 | year=2004 | pmid=15552776 | doi=10.1016/j.lungcan.2004.07.998}}</ref> | |||
| {{TOC limit|3}} | |||
| A wide array of negative effects are attributed, in whole or in part, to frequent, long term exposure to second hand smoke.<ref>{{cite journal | author=Taylor R et al | title=Passive smoking and lung cancer: a cumulative meta-analysis. | journal=Aust N Z J Public Health | volume=25 | issue=3 | pages=203–11 | year=2001 | pmid=11494987 | doi=10.1111/j.1467-842X.2001.tb00564.x}}</ref><ref>{{cite journal | author=He J et al | title=Passive smoking and the risk of coronary heart disease—a meta-analysis of epidemiologic studies. | journal=N Engl J Med | volume=340 | issue= | pages=920–6 | year=1999 | pmid=10089185 | doi=10.1056/NEJM199903253401204}}</ref><ref>{{cite journal | author=Svendsen KH, Kuller LH, Martin MJ, Ockene JK. | title=Effects of passive smoking in the Multiple Risk Factor Intervention Trial. | journal=Am J Epidemiol | volume=126 | issue= | pages=783–95 | year=1987 | pmid=3661526}}</ref> Some of these effects include: | |||
| ==Terminology== | |||
| ] created the term "passive smoking" ("''Passivrauchen''") in a publication in the ] during the 1930s. <ref>{{cite journal |url=https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(14)70064-5/fulltext |title=Fritz Lickint |last=Gourd |first=Katherine |date=2014 |journal=The Lancet. Respiratory Medicine |volume=2 |issue=5 |pages=358–359 |publisher=] |doi=10.1016/S2213-2600(14)70064-5 |pmid=24726404 |access-date=7 December 2023 |quote=}}</ref><ref>{{cite web |url=https://www.afro.who.int/sites/default/files/2017-09/Chapter%2032.%20The%20history%20of%20tobacco.pdf |title=Chapter 32 History of Tobacco |author=<!--Not stated--> |date=2017 |website=www.afro.who.int |publisher=] |access-date=7 December 2023 |quote=}}</ref><ref>{{cite journal |last1= Brawley |first1=Otis W. |last2=Glynn |first2=Thomas J.|last3=Khuri|first3=Fadlo R.|last4= Wender|first4=Richard C. |date=18 November 2013 |title=The first surgeon general's report on smoking and health: The 50th anniversary |journal=CA |volume=64 |issue=1 |pages=5–8 |doi= 10.3322/caac.21210 |pmid=24249254 |doi-access=free }}</ref> Terms used include "environmental tobacco smoke" to refer to the airborne matter, while "involuntary smoking" and "passive smoking" refer to exposure to secondhand smoke.<ref>{{cite web |title=Health Effects of Exposure to Secondhand Smoke |url=http://www.epa.gov/smokefree/healtheffects.html |url-status=dead |archive-url=https://web.archive.org/web/20150905193507/http://www.epa.gov/smokefree/healtheffects.html |archive-date=5 September 2015 |access-date=6 September 2015 |publisher=United States Environmental Protection Agency}}</ref><ref name=chapman>{{cite journal|last1=Chapman|first1=S.|title=Other people's smoke: what's in a name?|journal=Tobacco Control|date=1 June 2003|volume=12|issue=2|pages=113–4|doi=10.1136/tc.12.2.113 |pmid=12773710 |pmc=1747703}}</ref> The term "environmental tobacco smoke" can be traced back to a 1974 industry-sponsored meeting held in ], while the term "passive smoking" was first used in the title of a scientific paper in 1970.<ref name=chapman/> The ] prefers to use the phrase "secondhand smoke" rather than "environmental tobacco smoke", stating that "The descriptor 'secondhand' captures the involuntary nature of the exposure, while 'environmental' does not."<ref name="sg-report"/>{{rp|9}} Most researchers consider the term "passive smoking" to be synonymous with "secondhand smoke".<ref name=protano/> In contrast, a 2011 commentary in '']'' argued that research into "thirdhand smoke" renders it inappropriate to refer to passive smoking with the term "secondhand smoke", which the authors stated constitutes a ].<ref name=protano>{{cite journal|last1=Protano|first1=Carmela|last2=Vitali|first2=Matteo|title=The New Danger of Thirdhand Smoke: Why Passive Smoking Does Not Stop at Secondhand Smoke|journal=Environmental Health Perspectives|date=1 October 2011|volume=119|issue=10|pages=a422|doi=10.1289/ehp.1103956 |pmid=21968336 |pmc=3230455 }}</ref> | |||
| The term "]" is sometimes used to refer to smoke that goes into the air directly from a burning ], ], or ],<ref name="Sidestream Smoke">{{harvnb|IARC|2004|p=1191}}: "During smoking of cigarettes, cigars, pipes and other tobacco productions, in addition to the mainstream smoke drawn and inhaled by the smokers, a stream of smoke is released between puffs into the air from the burning cone. Once released, this stream (also known as the sidestream smoke) is mixed with exhaled mainstream smoke as well as the air in an indoor environment to form the secondhand smoke to which ..."</ref> while "mainstream smoke" refers to smoke that a smoker exhales. | |||
| == Health effects == | |||
| Secondhand smoke causes many of the same diseases as ], including ]s, ], and ]s.<ref name="sg-report"/><ref name=IARC2004/><ref name="calepa2005">{{cite report |author1=California Environmental Protection Agency: Air Resources Board |title=Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant |date=24 June 2005 |url=https://escholarship.org/uc/item/8hk6960q }}</ref> These include: | |||
| * ]: | * ]: | ||
| ** General: overall increased risk;<ref> |
** General: overall increased risk;<ref>{{harvnb|Surgeon General|2006|pp=30–46}}</ref> reviewing the evidence accumulated on a worldwide basis, the ] concluded in 2004 that "Involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) is carcinogenic to humans."<ref name=IARC2004/> The ] reports that about 70 chemicals present in secondhand smoke are carcinogenic.<ref>{{cite web |title=Secondhand Smoke (SHS) Facts |url=https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/general_facts/index.htm |website=CDC |date=5 January 2021 |access-date=August 5, 2021}}</ref> | ||
| ** ]: Passive smoking is a risk factor for lung cancer.<ref>{{cite journal|last1=Alberg|first1=Anthony J.|last2=Brock|first2=Malcolm V.|last3=Ford|first3=Jean G.|last4=Samet|first4=Jonathan M.|last5=Spivack|first5=Simon D.|title=Epidemiology of Lung Cancer|journal=Chest|date=1 May 2013|volume=143|issue=5_suppl|pages=e1S–e29S |pmid=23649439 |pmc=4694610 |doi=10.1378/chest.12-2345 }}</ref><ref>{{cite journal |last1=Bhatnagar|first1=A |last2=Whitsel|first2=LP |last3=Ribisl|first3=KM| last4=Bullen|first4=C |last5=Chaloupka|first5=F |last6=Piano|first6=MR |last7=Robertson|first7=RM |last8=McAuley|first8=T |last9=Goff|first9=D |last10=Benowitz|first10=N |last11=((American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes))|first11=Research|title=Electronic cigarettes: a policy statement from the American Heart Association |journal=Circulation|date=14 October 2014|volume=130|issue=16|pages=1418–36|doi=10.1161/CIR.0000000000000107|pmid=25156991|pmc=7643636 |s2cid=16075813 |url=https://escholarship.org/uc/item/52p2317d }}</ref> In the United States, secondhand smoke is estimated to cause more than 7,000 deaths from lung cancer a year among non-smokers.<ref>{{cite web|title=Health Effects of Secondhand Smoke|url=https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/|access-date=30 May 2015|date=November 24, 2014}}</ref> A quarter of all cases occur in people who have never smoked.<ref>{{Cite journal |last1=Pallis |first1=Athanasios G. |last2=Syrigos |first2=Konstantinos N. |date=December 2013 |title=Lung cancer in never smokers: Disease characteristics and risk factors |url=http://dx.doi.org/10.1016/j.critrevonc.2013.06.011 |journal=Critical Reviews in Oncology/Hematology |volume=88 |issue=3 |pages=494–503 |doi=10.1016/j.critrevonc.2013.06.011 |pmid=23921082 |issn=1040-8428}}</ref> | |||
| ** ]: the effect of passive smoking on lung cancer has been extensively studied. A series of studies from the USA from 1986–2003,<ref>{{cite journal |author= |title=1986 Surgeon General's report: the health consequences of involuntary smoking |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=35 |issue=50 |pages=769–70 |year=1986 |pmid=3097495 |doi=}}</ref><ref>National Research Council. Environmental tobacco smoke: measuring exposures and assessing health effects, NRC, Washington, DC (1986).</ref><ref name="EPA report">US Environmental Protection Agency. {{PDF|1=}}</ref><ref>{{cite journal |author= |title=Health effects of exposure to environmental tobacco smoke. California Environmental Protection Agency |journal=Tob Control |volume=6 |issue=4 |pages=346–53 |year=1997 |pmid=9583639 |doi=}}</ref><ref>{{cite journal |author= |title=State-specific prevalence of current cigarette smoking among adults, and policies and attitudes about secondhand smoke--United States, 2000 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=50 |issue=49 |pages=1101–6 |year=2001 |pmid=11794619 |doi=}}</ref><ref>{{cite journal |author=Alberg AJ, Samet JM |title=Epidemiology of lung cancer |journal=Chest |volume=123 |issue=1 Suppl |pages=21S–49S |year=2003 |pmid=12527563|doi=10.1378/chest.123.1_suppl.21S}}</ref> the UK in 1998,<ref>{{cite web | title=Report of the Scientific Committee on Tobacco and Health to the Chief Medical Officer, Part II | url=http://www.archive.official-documents.co.uk/document/doh/tobacco/part-2.htm | accessdate=2006-07-26}}</ref><ref>{{cite journal |author=Hackshaw AK |title=Lung cancer and passive smoking |journal=Stat Methods Med Res |volume=7 |issue=2 |pages=119–36 |year=1998 |pmid=9654638|doi=10.1191/096228098675091404}}</ref> Australia in 1997<ref>National Health and Medical Research Council. The health effects of passive smoking, Australian Government Publishing Service, Canberra (1997).</ref> and internationally in 2004<ref>{{cite journal |author=Brennan P, Buffler P, Reynolds P, Wu A, Wichmann H, Agudo A, Pershagen G, Jöckel K, Benhamou S, Greenberg R, Merletti F, Winck C, Fontham E, Kreuzer M, Darby S, Forastiere F, Simonato L, Boffetta P |title=Secondhand smoke exposure in adulthood and risk of lung cancer among never smokers: a pooled analysis of two large studies |journal=Int. J. Cancer |volume=109 |issue=1 |pages=125–31 |year=2004 |pmid=14735478 | doi=10.1002/ijc.11682}}</ref> have consistently shown a significant increase in ] among those exposed to passive smoke. | |||
| ** ]: The ] concluded in 2005 that passive smoking increases the risk of breast cancer in younger, primarily premenopausal females by 70%<ref name="calepa2005" /> and the US ] has concluded that the evidence is "suggestive", but still insufficient to assert such a causal relationship.<ref name="sg-report"/> In contrast, the ] concluded in 2004 that there was "no support for a causal relation between involuntary exposure to tobacco smoke and breast cancer in never-smokers."<ref name=IARC2004/> A 2015 meta-analysis found that the evidence that passive smoking moderately increased the risk of breast cancer had become "more substantial than a few years ago".<ref>{{cite journal |last1=Macacu |first1=Alina |last2=Autier |first2=Philippe |last3=Boniol |first3=Mathieu |last4=Boyle |first4=Peter |title=Active and passive smoking and risk of breast cancer: a meta-analysis |journal=Breast Cancer Research and Treatment |date=November 2015 |volume=154 |issue=2 |pages=213–224 |doi=10.1007/s10549-015-3628-4 |pmid=26546245 |s2cid=4680641 |url=https://strathprints.strath.ac.uk/55324/1/Macacu_etal_BCRT_2015_Active_and_passive_smoking_and_risk_of_breast_cancer.pdf }}</ref> | |||
| **] risk is increased by 70% in younger, primarily premenopausal women. The ] has concluded that passive smoking causes breast cancer<ref name="calepa2005" /> and the US ]<ref></ref> has concluded that the evidence is "suggestive," one step below causal. | |||
| ** ]: A 2015 overview of systematic reviews found that exposure to secondhand smoke increased the risk of cervical cancer.<ref name=cao/> | |||
| **Passive smoking does not appear to be associated with ]<ref>{{cite journal |author=Hassan MM, Abbruzzese JL, Bondy ML, ''et al'' |title=Passive smoking and the use of noncigarette tobacco products in association with risk for pancreatic cancer: a case-control study |journal=Cancer |volume=109 |issue=12 |pages=2547–56 |year=2007 |pmid=17492688 |doi=10.1002/cncr.22724}}</ref> | |||
| ** ]: A 2016 systematic review and meta-analysis found that secondhand smoke exposure was associated with a significant increase in the risk of bladder cancer.<ref>{{cite journal|last1=Cumberbatch|first1=Marcus G.|last2=Rota|first2=Matteo|last3=Catto|first3=James W.F.|last4=La Vecchia|first4=Carlo|title=The Role of Tobacco Smoke in Bladder and Kidney Carcinogenesis: A Comparison of Exposures and Meta-analysis of Incidence and Mortality Risks|journal=European Urology|date=September 2016|volume=70|issue=3|pages=458–466 |pmid=26149669 |doi=10.1016/j.eururo.2015.06.042 |url=http://eprints.whiterose.ac.uk/88607/8/WRRO_88607.pdf}}</ref> | |||
| * ]: risk of ear infections<ref>{{cite book | last = Bull | first = P.D. | title = Diseases of the Ear, Nose and Throat | publisher = Blackwell Science | date = 1996 | location = | url = | doi = | id = ISBN 0-86542-634-1 }}</ref> | |||
| * ]: risk of ] |
* ]: risk of ]<ref>{{harvnb|Surgeon General|2006|loc=Ch. 8}}</ref><ref>{{cite journal|last1=Lv|first1=X|last2=Sun|first2=J|last3=Bi|first3=Y|last4=Xu|first4=M|last5=Lu|first5=J|last6=Zhao|first6=L|last7=Xu|first7=Y|title=Risk of all-cause mortality and cardiovascular disease associated with secondhand smoke exposure: a systematic review and meta-analysis|journal=International Journal of Cardiology|date=15 November 2015|volume=199|pages=106–15|doi=10.1016/j.ijcard.2015.07.011|pmid=26188829}}</ref> and reduced heart rate variability.<ref>{{cite journal|last1=Dinas|first1=PC|last2=Koutedakis|first2=Y|last3=Flouris|first3=AD|title=Effects of active and passive tobacco cigarette smoking on heart rate variability |journal=International Journal of Cardiology|date=20 February 2013|volume=163|issue=2|pages=109–15|doi=10.1016/j.ijcard.2011.10.140|pmid=22100604}}</ref> | ||
| ** Epidemiological studies have shown that both active and passive cigarette smoking increase the risk of atherosclerosis.<ref>{{cite journal |last1=Zou |first1=N |last2=Hong |first2=J |last3=Dai |first3=QY |title=Passive cigarette smoking induces inflammatory injury in human arterial walls |journal=Chinese Medical Journal |date=20 February 2009 |volume=122 |issue=4 |pages=444–448 |doi=10.3760/cma.j.issn.0366-6999.2009.04.0016 |pmid=19302752 |url=https://journals.lww.com/cmj/Fulltext/2009/02020/Passive_cigarette_smoking_induces_inflammatory.18.aspx |doi-access=free }}</ref> | |||
| ** Passive smoking is strongly associated with an increased risk of stroke, and this increased risk is disproportionately high at low levels of exposure.<ref>{{cite journal |last1=Oono |first1=I.P. |last2=Mackay |first2=D.F. |last3=Pell |first3=J.P. |title=Meta-analysis of the association between secondhand smoke exposure and stroke |journal=Journal of Public Health |date=December 2011 |volume=33 |issue=4 |pages=496–502 |doi=10.1093/pubmed/fdr025 |pmid=21422014 |doi-access=free }}</ref> | |||
| * ]: | * ]: | ||
| ** Risk of ]<ref>{{harvnb|Surgeon General|2006|pp=555–8}}</ref> | |||
| **Risk of ]<ref>U.S. Surgeon General's Report on Secondhand Smoke (; pages 555 - 558)</ref><ref></ref> | |||
| ** Risk of ] (COPD)<ref>{{cite journal |last1=Bentayeb |first1=Malek |last2=Simoni |first2=Marzia |last3=Norback |first3=Dan |last4=Baldacci |first4=Sandra |last5=Maio |first5=Sara |last6=Viegi |first6=Giovanni |last7=Annesi-Maesano |first7=Isabella |title=Indoor air pollution and respiratory health in the elderly |journal=Journal of Environmental Science and Health, Part A |date=6 December 2013 |volume=48 |issue=14 |pages=1783–1789 |doi=10.1080/10934529.2013.826052 |pmid=24007433 |s2cid=41862447 }}</ref> | |||
| * ]: | |||
| ** According to a 2015 review, passive smoking may increase the risk of ] infection and accelerate the progression of the disease, but the evidence remains weak.<ref>{{cite journal |last1=Dogar |first1=O. F. |last2=Pillai |first2=N. |last3=Safdar |first3=N. |last4=Shah |first4=S. K. |last5=Zahid |first5=R. |last6=Siddiqi |first6=K. |title=Second-hand smoke and the risk of tuberculosis: a systematic review and a meta-analysis |journal=Epidemiology and Infection |date=November 2015 |volume=143 |issue=15 |pages=3158–3172 |doi=10.1017/S0950268815001235 |pmid=26118887 |pmc=9150979 |s2cid=206285892 }}</ref> | |||
| **Risk of ]<ref>{{cite journal |author=Fantuzzi G, Aggazzotti G, Righi E, ''et al'' |title=Preterm delivery and exposure to active and passive smoking during pregnancy: a case-control study from Italy |journal=Paediatr Perinat Epidemiol |volume=21 |issue=3 |pages=194–200 |year=2007 |pmid=17439527 |doi=10.1111/j.1365-3016.2007.00815.x}}</ref> | |||
| ** The majority of studies on the association between secondhand smoke exposure and ] have found a significant association between the two.<ref>{{cite journal |last1=Hur |first1=Kevin |last2=Liang |first2=Jonathan |last3=Lin |first3=Sandra Y. |title=The role of secondhand smoke in sinusitis: a systematic review: Sinusitis and secondhand smoke |journal=] |date=January 2014 |volume=4 |issue=1 |pages=22–28 |doi=10.1002/alr.21232 |pmid=24574074 |s2cid=9537143|doi-access=free }}</ref> | |||
| * ] and ]: Exposure to secondhand smoke may increase the risk of cognitive impairment and dementia in adults 50 and over.<ref>{{cite journal|last1=Chen|first1=R|last2=Hu|first2=Z|last3=Orton|first3=S|last4=Chen|first4=RL|last5=Wei|first5=L|title=Association of passive smoking with cognitive impairment in nonsmoking older adults: a systematic literature review and a new study of Chinese cohort |journal=Journal of Geriatric Psychiatry and Neurology|date=December 2013|volume=26|issue=4|pages=199–208|doi=10.1177/0891988713496165|pmid=23877565|hdl=2436/621630|s2cid=43097513|hdl-access=free}}</ref> Children exposed to secondhand smoke show reduced vocabulary and reasoning skills when compared with non-exposed children as well as more general cognitive and intellectual deficits.<ref name=LingHeffernan2016>{{cite journal |last1=Ling |first1=Jonathan |last2=Heffernan |first2=Thomas |title=The Cognitive Deficits Associated with Second-Hand Smoking |journal=Frontiers in Psychiatry |date=24 March 2016 |volume=7 |page=46 |doi=10.3389/fpsyt.2016.00046 |pmid=27047401 |pmc=4805605 |doi-access=free }}</ref> | |||
| * ]: Exposure to secondhand smoke is associated with an increased risk of depressive symptoms.<ref>{{cite journal|last1=Zeng|first1=Yan-Ni|last2=Li|first2=Ya-Min|title=Secondhand smoke exposure and mental health in adults: a meta-analysis of cross-sectional studies|journal=Social Psychiatry and Psychiatric Epidemiology|date=10 December 2015|volume=51|issue=9|pages=1339–48|doi=10.1007/s00127-015-1164-5 |pmid=26661619|s2cid=7772929}}</ref> | |||
| * During ]: | |||
| ** ]: a 2014 meta-analysis found that maternal secondhand smoke exposure increased the risk of miscarriage by 11%.<ref>{{cite journal|last1=Pineles|first1=B. L.|last2=Park|first2=E.|last3=Samet|first3=J. M.|title=Systematic Review and Meta-Analysis of Miscarriage and Maternal Exposure to Tobacco Smoke During Pregnancy|journal=American Journal of Epidemiology|date=10 February 2014|volume=179|issue=7|pages=807–823|doi=10.1093/aje/kwt334|pmid=24518810|pmc=3969532}}</ref> | |||
| ** ]<ref name="calepa2005"/><sup>, part B, ch. 3</sup>.<ref>{{harvnb|Surgeon General|2006|pp=198–205}}</ref> | |||
| ** ]<ref name="calepa2005"/><sup>, part B, ch. 3</sup><ref>{{cite journal|last1=Cui|first1=H|last2=Gong|first2=TT|last3=Liu|first3=CX|last4=Wu|first4=QJ|title=Associations between Passive Maternal Smoking during Pregnancy and Preterm Birth: Evidence from a Meta-Analysis of Observational Studies|journal=PLOS ONE|date=25 January 2016|volume=11|issue=1|pages=e0147848|doi=10.1371/journal.pone.0147848|pmid=26808045|pmc=4726502|bibcode=2016PLoSO..1147848C|doi-access=free}}</ref> (Evidence of the causal link is described only as "suggestive" by the US Surgeon General in his 2006 report.<ref>{{harvnb|Surgeon General|2006|pp=194–7}}</ref>) Laws limiting smoking decrease premature births.<ref>{{cite journal|last1=Been|first1=Jasper|title=Effect of smoke-free legislation on perinatal and child health: a systematic review and meta-analysis|journal=Lancet|date=28 March 2014|doi=10.1016/S0140-6736(14)60082-9|pmid=24680633|volume=383|issue=9928|pages=1549–60|last2=Nurmatov|first2=U. B.|last3=Cox|first3=B|last4=Nawrot|first4=T. S.|last5=Van Schayck|first5=C. P.|last6=Sheikh|first6=A|s2cid=8532979}}</ref> | |||
| ** ] and ]s in children<ref>{{cite journal|last1=Leonardi-Bee|first1=J|last2=Britton|first2=J|last3=Venn|first3=A|title=Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis |journal=Pediatrics|date=April 2011|volume=127|issue=4|pages=734–41|doi=10.1542/peds.2010-3041|pmid=21382949|s2cid=19866471}}</ref> | |||
| ** Recent studies comparing females exposed to secondhand smoke and non-exposed females, demonstrate that females exposed while pregnant have higher risks of delivering a child with congenital abnormalities, longer lengths, smaller head circumferences, and ].<ref>{{cite journal |vauthors=Salmasi G, Grady R, Jones J, McDonald SD |title=Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses |journal=Acta Obstet Gynecol Scand |volume=89 |issue=4 |pages=423–41 |year=2010 |pmid=20085532 |doi=10.3109/00016340903505748 |s2cid=9206564 |doi-access=free }}</ref><ref>{{cite journal|last1=Wang|first1=Meng|last2=Wang|first2=Zhi-Ping|last3=Zhang|first3=Meng|last4=Zhao|first4=Zhong-Tang|title=Maternal passive smoking during pregnancy and neural tube defects in offspring: a meta-analysis|journal=Archives of Gynecology and Obstetrics|date=13 August 2013|volume=289|issue=3|pages=513–521 |pmid=23942772 |doi=10.1007/s00404-013-2997-3 |s2cid=6526042}}</ref> | |||
| * General: | * General: | ||
| ** Worsening of asthma, allergies, and other conditions<ref>{{cite journal | |
** Worsening of asthma, allergies, and other conditions.<ref>{{cite journal |author=Janson C |title=The effect of passive smoking on respiratory health in children and adults |journal=Int J Tuberc Lung Dis |volume=8 |issue=5 |pages=510–6 |year=2004 |pmid=15137524 }}</ref> A 2014 systematic review and meta-analysis found that passive smoking was associated with a slightly increased risk of allergic diseases among children and adolescents; the evidence for an association was weaker for adults.<ref>{{cite journal|last1=Saulyte|first1=Jurgita|last2=Regueira|first2=Carlos|last3=Montes-Martínez|first3=Agustín|last4=Khudyakov|first4=Polyna|last5=Takkouche|first5=Bahi|last6=Novotny|first6=Thomas E.|title=Active or Passive Exposure to Tobacco Smoking and Allergic Rhinitis, Allergic Dermatitis, and Food Allergy in Adults and Children: A Systematic Review and Meta-Analysis|journal=PLOS Medicine|date=11 March 2014|volume=11|issue=3|pages=e1001611 |pmid=24618794 |pmc=3949681 |doi=10.1371/journal.pmed.1001611 |doi-access=free }}</ref> | ||
| ** ].<ref>{{cite journal|last1=Wei|first1=X|last2=E|first2=M|last3=Yu|first3=S|title=A meta-analysis of passive smoking and risk of developing Type 2 Diabetes Mellitus |journal=Diabetes Research and Clinical Practice|date=January 2015|volume=107|issue=1|pages=9–14|doi=10.1016/j.diabres.2014.09.019|pmid=25488377}}</ref><ref>{{cite journal|last1=Wang|first1=Y|last2=Ji|first2=J|last3=Liu|first3=YJ|last4=Deng|first4=X|last5=He|first5=QQ|title=Passive smoking and risk of type 2 diabetes: a meta-analysis of prospective cohort studies|journal=PLOS ONE|date=2013|volume=8|issue=7|pages=e69915|doi=10.1371/journal.pone.0069915|pmid=23922856|pmc=3724674|bibcode=2013PLoSO...869915W|doi-access=free}}</ref><ref>{{cite journal|last1=Sun|first1=K|last2=Liu|first2=D|last3=Wang|first3=C|last4=Ren|first4=M|last5=Yang|first5=C|last6=Yan|first6=L|title=Passive smoke exposure and risk of diabetes: a meta-analysis of prospective studies |journal=Endocrine|date=November 2014|volume=47|issue=2|pages=421–7|doi=10.1007/s12020-014-0194-1|pmid=24532101|s2cid=3276501}}</ref> It remains unclear whether the association between passive smoking and diabetes is causal.<ref>{{cite journal|last1=Pan|first1=An|last2=Wang|first2=Yeli|last3=Talaei|first3=Mohammad|last4=Hu|first4=Frank B|last5=Wu|first5=Tangchun|title=Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis|journal=The Lancet Diabetes & Endocrinology|date=December 2015|volume=3|issue=12|pages=958–967|doi=10.1016/S2213-8587(15)00316-2|pmid=26388413|pmc=4656094}}</ref> | |||
| * ]<ref>{{cite web | title=Parents warned not to smoke at home | url=http://observer.guardian.co.uk/uk_news/story/0,,2110076,00.html | publisher = The Guardian | accessdate = 2007-06-24}}</ref> | |||
| * Risk of carrying '']'' or '']''.<ref name=cao/> | |||
| **Risk of ] (SIDS)<ref>The on Secondhand Smoke (; pages 180–194)</ref> | |||
| * A possible increased risk of ].<ref>{{cite journal|last1=Akinkugbe|first1=Aderonke A.|last2=Slade|first2=Gary D.|last3=Divaris|first3=Kimon|last4=Poole|first4=Charles|title=Systematic Review and Meta-analysis of the Association Between Exposure to Environmental Tobacco Smoke and Periodontitis Endpoints Among Nonsmokers|journal=Nicotine & Tobacco Research|date=November 2016|volume=18|issue=11|pages=2047–56 |pmid=27083214 |pmc=5055738 |doi=10.1093/ntr/ntw105 }}</ref> | |||
| **Risk of developing ]<ref>U.S. Surgeon General's Report on Secondhand Smoke (; pages 311–319)</ref><ref>{{cite journal |author=Vork KL, Broadwin RL, Blaisdell RJ |title=Developing asthma in childhood from exposure to secondhand tobacco smoke: insights from a meta-regression |journal=Environ. Health Perspect. |volume=115 |issue=10 |pages=1394–400 |year=2007 |pmid=17938726 |doi=10.1289/ehp.10155}}</ref> | |||
| * Overall increased risk of death in both adults, where it was estimated to kill 53,000 nonsmokers per year in the U.S in 1991,<ref>{{cite journal |vauthors=Glantz SA, Parmley WW |title=Passive smoking and heart disease. Epidemiology, physiology, and biochemistry |journal=Circulation |volume=83 |issue=1 |pages=1–12 |year=1991 |pmid=1984876 |doi=10.1161/01.cir.83.1.1|doi-access=free }}</ref><ref>{{cite journal |vauthors=Taylor AE, Johnson DC, Kazemi H |title=Environmental tobacco smoke and cardiovascular disease. A position paper from the Council on Cardiopulmonary and Critical Care, American Heart Association |journal=Circulation |volume=86 |issue=2 |pages=699–702 |year=1992 |pmid=1638735 |doi=10.1161/01.cir.86.2.699|doi-access=free }}</ref> and in children.<ref>{{harvnb|Surgeon General|2006|pp=376–380}}</ref> The World Health Organization states that passive smoking causes about 600,000 deaths a year, and about 1% of the global burden of disease.<ref>{{cite web | url=https://www.who.int/gho/phe/secondhand_smoke/en/ | title=Second-hand smoke | website=WHO website | access-date=24 April 2015}}</ref> As of 2017, passive smoking causes about 900,000 deaths a year, which is about 1/8 of all deaths caused by smoking.<ref>{{cite news|title=The last gasp|url=https://www.economist.com/blogs/graphicdetail/2017/07/daily-chart-11|access-date=20 July 2017|newspaper=]|date=19 July 2017}}</ref> | |||
| **Risk of lung infections<ref>{{cite journal |author=Spencer N, Coe C |title=Parent reported longstanding health problems in early childhood: a cohort study |journal=Arch. Dis. Child. |volume=88 |issue=7 |pages=570–3 |year=2003 |pmid=12818898|doi=10.1136/adc.88.7.570}}</ref><ref>{{cite journal |author=de Jongste JC, Shields MD |title=Cough . 2: Chronic cough in children |journal=Thorax |volume=58 |issue=11 |pages=998–1003 |year=2003 |pmid=14586058 |doi=}}</ref><ref>{{cite journal |author=Dybing E, Sanner T |title=Passive smoking, sudden infant death syndrome (SIDS) and childhood infections |journal=Hum Exp Toxicol |volume=18 |issue=4 |pages=202–5 |year=1999 |pmid=10333302|doi=10.1191/096032799678839914}}</ref><ref name="Difranza 2004">{{cite journal |author=DiFranza JR, Aligne CA, Weitzman M |title=Prenatal and postnatal environmental tobacco smoke exposure and children's health |journal=Pediatrics |volume=113 |issue=4 Suppl |pages=1007–15 |year=2004 |pmid=15060193 |doi= |url=http://pediatrics.aappublications.org/cgi/content/full/113/4/S1/1007}}</ref> | |||
| * Skin conditions: A 2016 systematic review and meta-analysis found that passive smoking was associated with a higher rate of ].<ref>{{cite journal|last1=Kantor|first1=R|last2=Kim|first2=A|last3=Thyssen|first3=JP|last4=Silverberg|first4=JI|title=Association of atopic dermatitis with smoking: A systematic review and meta-analysis|journal=Journal of the American Academy of Dermatology|date=December 2016|volume=75|issue=6|pages=1119–1125.e1|pmid=27542586|doi=10.1016/j.jaad.2016.07.017|pmc=5216172}}</ref> | |||
| **More severe illness with ], and worse outcome<ref>{{cite journal |author=Chatzimichael A, Tsalkidis A, Cassimos D, ''et al'' |title=The role of breastfeeding and passive smoking on the development of severe bronchiolitis in infants |journal=Minerva Pediatr. |volume=59 |issue=3 |pages=199–206 |year=2007 |pmid=17519864 |doi=}}</ref> | |||
| **Increased risk of developing ] if exposed to a carrier<ref>{{cite journal |author=den Boon S, Verver S, Marais BJ, ''et al'' |title=Association between passive smoking and infection with Mycobacterium tuberculosis in children |journal=Pediatrics |volume=119 |issue=4 |pages=734–9 |year=2007 |pmid=17403844 |doi=10.1542/peds.2006-1796}}</ref> | |||
| **Risk of allergies | |||
| **Risk of ]<ref>{{cite journal |author=Mahid SS, Minor KS, Stromberg AJ, Galandiuk S |title=Active and passive smoking in childhood is related to the development of inflammatory bowel disease |journal=Inflamm. Bowel Dis. |volume=13 |issue=4 |pages=431–8 |year=2007 |pmid=17206676 |doi=10.1002/ibd.20070}}</ref> | |||
| **Risk of learning difficulties, developmental delays, and neurobehavioral effects.<ref>{{cite journal |author=Richards GA, Terblanche AP, Theron AJ, ''et al'' |title=Health effects of passive smoking in adolescent children |journal=S. Afr. Med. J. |volume=86 |issue=2 |pages=143–7 |year=1996 |pmid=8619139 |doi=}}</ref><ref>, The Collaborative on Health and the Environment’s | |||
| Learning and Developmental Disabilities Initiative, November 7, 2007</ref> Animal models suggest a role for nicotine and ] in neurocognitive problems<ref name="Difranza 2004"/> | |||
| *Overall increased risk of death in both adults, where it is estimated to kill 53,000 nonsmokers per year, making it the 3<sup>rd</sup> leading cause of ] in the U.S.<ref>{{cite journal |author=Glantz SA, Parmley WW |title=Passive smoking and heart disease. Epidemiology, physiology, and biochemistry |journal=Circulation |volume=83 |issue=1 |pages=1–12 |year=1991 |pmid=1984876 |doi= |url=http://circ.ahajournals.org/cgi/content/abstract/83/1/1?ijkey=4a5be6d1e9e3a9b7d6b3b9ab29a0f748d8b955ed&keytype2=tf_ipsecsha}}</ref><ref> {{cite journal |author=Taylor AE, Johnson DC, Kazemi H |title=Environmental tobacco smoke and cardiovascular disease. A position paper from the Council on Cardiopulmonary and Critical Care, American Heart Association |journal=Circulation |volume=86 |issue=2 |pages=699–702 |year=1992 |pmid=1638735 |doi= |url=http://circ.ahajournals.org/cgi/content/abstract/86/2/699}}</ref> and in children<ref>U.S. Surgeon General's Report on Secondhand Smoke (; pages 376–380)</ref> | |||
| ===Risk to children=== | |||
| ==Short-term effects== | |||
| * ] (SIDS).<ref>{{cite journal|last1=Anderson|first1=HR|last2=Cook|first2=DG|title=Passive smoking and sudden infant death syndrome: review of the epidemiological evidence |journal=Thorax|date=November 1997|volume=52|issue=11|pages=1003–9|pmid=9487351|doi=10.1136/thx.52.11.1003|pmc=1758452}}</ref> In his 2006 report, the US Surgeon General concludes: "The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke and sudden infant death syndrome."<ref>{{harvnb|Surgeon General|2006|p=194}}</ref> Secondhand smoking has been estimated to be associated with 430 SIDS deaths in the United States annually.<ref name=ala> August 2006.</ref> | |||
| * ].<ref>{{harvnb|Surgeon General|2006|pp=311–9}}</ref><ref>{{cite journal |vauthors=Vork KL, Broadwin RL, Blaisdell RJ |title=Developing Asthma in Childhood from Exposure to Secondhand Tobacco Smoke: Insights from a Meta-Regression |journal=] |volume=115 |issue=10 |pages=1394–400 |year=2007 |pmid=17938726 |pmc=2022647 |doi=10.1289/ehp.10155 }}</ref><ref>{{cite journal|last1=Tinuoye|first1=O.|last2=Pell|first2=J. P.|last3=Mackay|first3=D. F.|title=Meta-Analysis of the Association Between Secondhand Smoke Exposure and Physician-Diagnosed Childhood Asthma|journal=Nicotine & Tobacco Research|date=28 March 2013|volume=15|issue=9|pages=1475–1483|doi=10.1093/ntr/ntt033|pmid=23539174}}</ref> Secondhand smoke exposure is also associated with an almost doubled risk of hospitalization for asthma exacerbation among children with asthma.<ref>{{cite journal|last1=Wang|first1=Zhen|last2=May|first2=Sara M.|last3=Charoenlap|first3=Suvanee|last4=Pyle|first4=Regan|last5=Ott|first5=Nancy L.|last6=Mohammed|first6=Khaled|last7=Joshi|first7=Avni Y.|title=Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis|journal=Annals of Allergy, Asthma & Immunology|date=November 2015|volume=115|issue=5|pages=396–401.e2|doi=10.1016/j.anai.2015.08.005|pmid=26411971|doi-access=free}}</ref> | |||
| * Lung infections,<ref>{{cite journal |vauthors=de Jongste JC, Shields MD |title=Cough • 2: Chronic cough in children |journal=Thorax |volume=58 |issue=11 |pages=998–1003 |year=2003 |pmid=14586058 |pmc=1746521 |doi=10.1136/thorax.58.11.998 }}</ref><ref>{{cite journal |vauthors=Dybing E, Sanner T |title=Passive smoking, sudden infant death syndrome (SIDS) and childhood infections |journal=Hum Exp Toxicol |volume=18 |issue=4 |pages=202–5 |year=1999 |pmid=10333302|doi=10.1191/096032799678839914 |s2cid=21365217 }}</ref><ref name="Difranza 2004">{{cite journal |vauthors=DiFranza JR, Aligne CA, Weitzman M |title=Prenatal and postnatal environmental tobacco smoke exposure and children's health |journal=] |volume=113 |issue=4 Suppl |pages=1007–15 |year=2004 |pmid=15060193 |doi=10.1542/peds.113.S3.1007 |s2cid=248349 |url=http://pediatrics.aappublications.org/content/113/Supplement_3/1007.long }}</ref> also including more severe illness with ]<ref name=Chatzimichael/> and ],<ref name="CDC2007"> {{webarchive|url=https://web.archive.org/web/20110911020755/http://www.cdc.gov/nccdphp/publications/factsheets/Prevention/pdf/smoking.pdf |date=2011-09-11 }}. Centers for Disease Control and Prevention. July 2007.</ref> and worse outcome,<ref name=Chatzimichael>{{cite journal |last1=Chatzimichael |first1=A |last2=Tsalkidis |first2=A |last3=Cassimos |first3=D |last4=Gardikis |first4=S |last5=Tripsianis |first5=G |last6=Deftereos |first6=S |last7=Ktenidou-Kartali |first7=S |last8=Tsanakas |first8=I |title=The role of breastfeeding and passive smoking on the development of severe bronchiolitis in infants |journal=Minerva Pediatrica |date=June 2007 |volume=59 |issue=3 |pages=199–206 |pmid=17519864 |url=https://www.minervamedica.it/en/journals/minerva-pediatrica/article.php?cod=R15Y2007N03A0199 }}</ref> as well as increased risk of developing tuberculosis if exposed to a carrier.<ref>{{cite journal|last1=Jafta|first1=N|last2=Jeena|first2=PM|last3=Barregard|first3=L|last4=Naidoo|first4=RN|title=Childhood tuberculosis and exposure to indoor air pollution: a systematic review and meta-analysis |journal=The International Journal of Tuberculosis and Lung Disease|date=May 2015|volume=19|issue=5|pages=596–602|doi=10.5588/ijtld.14.0686|pmid=25868030}}</ref> In the United States, it is estimated that secondhand smoke has been associated with between 150,000 and 300,000 lower respiratory tract infections in infants and children under 18 months of age, resulting in between 7,500 and 15,000 hospitalizations each year.<ref name=ala/> | |||
| * Impaired respiratory function and slowed lung growth<ref name="CDC2007"/> | |||
| * Allergies<ref>{{cite journal|last1=Feleszko|first1=W|last2=Ruszczyński|first2=M|last3=Jaworska|first3=J|last4=Strzelak|first4=A|last5=Zalewski|first5=BM|last6=Kulus|first6=M|title=Environmental tobacco smoke exposure and risk of allergic sensitisation in children: a systematic review and meta-analysis |journal=Archives of Disease in Childhood|date=November 2014|volume=99|issue=11|pages=985–92|doi=10.1136/archdischild-2013-305444|pmid=24958794|s2cid=206856566}}</ref> | |||
| * Maternal passive smoking increases the risk of non-syndromic ]s by 50% among their children.<ref>{{cite journal|last1=Sabbagh|first1=HJ|last2=Hassan|first2=MH|last3=Innes|first3=NP|last4=Elkodary|first4=HM|last5=Little|first5=J|last6=Mossey|first6=PA|title=Passive smoking in the etiology of non-syndromic orofacial clefts: a systematic review and meta-analysis|journal=PLOS ONE|date=2015|volume=10|issue=3|pages=e0116963|doi=10.1371/journal.pone.0116963|pmid=25760440|pmc=4356514|bibcode=2015PLoSO..1016963S|doi-access=free}}</ref> | |||
| * Learning difficulties, developmental delays, ] problems,<ref>{{cite journal|last1=Pagani|first1=Linda S.|title=Environmental tobacco smoke exposure and brain development: The case of attention deficit/hyperactivity disorder|journal=]|date=July 2014|volume=44|pages=195–205|doi=10.1016/j.neubiorev.2013.03.008|pmid=23545330|s2cid=20470659}}</ref> and neurobehavioral effects.<ref>{{cite web|url=http://www.iceh.org/pdfs/LDDI/LDDIStatement.pdf |title=Scientific Consensus Statement on Environmental Agents Associated with Neurodevelopmental Disorders |publisher=The Collaborative on Health and the Environment's Learning and Developmental Disabilities Initiative |date=July 1, 2008 |archive-url=https://web.archive.org/web/20090327101820/http://www.iceh.org/pdfs/LDDI/LDDIStatement.pdf |url-status=dead |archive-date=2009-03-27 }}</ref><ref>{{cite journal |last1=Chen |first1=Ruoling |last2=Clifford |first2=Angela |last3=Lang |first3=Linda |last4=Anstey |first4=Kaarin J. |title=Is exposure to secondhand smoke associated with cognitive parameters of children and adolescents?—a systematic literature review |journal=Annals of Epidemiology |date=October 2013 |volume=23 |issue=10 |pages=652–661 |doi=10.1016/j.annepidem.2013.07.001 |pmid=23969303 |doi-access=free |hdl=1885/10932 |hdl-access=free }}</ref> Animal models suggest a role for nicotine and ] in neurocognitive problems.<ref name="Difranza 2004"/> | |||
| * Increased risk of ]s.<ref name="Difranza 2004"/><ref>{{harvnb|Surgeon General|2006|pp=293–309}}</ref><ref>{{cite journal |last1=Jones |first1=Laura L. |last2=Hassanien |first2=A |last3=Cook |first3=DG |last4=Britton |first4=J |last5=Leonardi-Bee |first5=J |title=Parental Smoking and the Risk of Middle Ear Disease in Children: A Systematic Review and Meta-analysis |journal=Archives of Pediatrics & Adolescent Medicine |date=1 January 2012 |volume=166 |issue=1 |pages=18–27 |doi=10.1001/archpediatrics.2011.158 |pmid=21893640 |doi-access=free }}</ref> | |||
| * Invasive ].<ref name=cao>{{cite journal |last1=Lee |first1=Chien-Chang |last2=Middaugh |first2=Nicole A. |last3=Howie |first3=Stephen R. C. |last4=Ezzati |first4=Majid |title=Association of Secondhand Smoke Exposure with Pediatric Invasive Bacterial Disease and Bacterial Carriage: A Systematic Review and Meta-analysis |journal=PLOS Medicine |date=7 December 2010 |volume=7 |issue=12 |pages=e1000374 |doi=10.1371/journal.pmed.1000374 |pmid=21151890 |pmc=4595077 |bibcode=2015PLoSO..1039907C |doi-access=free }}</ref><ref>{{cite journal|last1=Lee|first1=Chien-Chang|last2=Middaugh|first2=Nicole A.|last3=Howie|first3=Stephen R. C.|last4=Ezzati|first4=Majid|last5=Lanphear|first5=Bruce P.|title=Association of Secondhand Smoke Exposure with Pediatric Invasive Bacterial Disease and Bacterial Carriage: A Systematic Review and Meta-analysis|journal=PLOS Medicine|date=7 December 2010|volume=7|issue=12|pages=e1000374|doi=10.1371/journal.pmed.1000374|pmid=21151890|pmc=2998445 |doi-access=free }}</ref> | |||
| * ] complications and some negative surgical outcomes.<ref>{{cite journal|last1=Chiswell|first1=C|last2=Akram|first2=Y|title=Impact of environmental tobacco smoke exposure on anaesthetic and surgical outcomes in children: a systematic review and meta-analysis|journal=Archives of Disease in Childhood|date=February 2017|volume=102|issue=2|pages=123–130|doi=10.1136/archdischild-2016-310687|pmid=27417307|pmc=5284464}}</ref> | |||
| * ]: Most studies have found a significant association between passive smoking and sleep disordered breathing in children, but further studies are needed to determine whether this association is causal.<ref>{{cite journal|last1=Jara|first1=SM|last2=Benke|first2=JR|last3=Lin|first3=SY|last4=Ishman|first4=SL|title=The association between secondhand smoke and sleep-disordered breathing in children: a systematic review|journal=The Laryngoscope|date=January 2015|volume=125|issue=1|pages=241–7|doi=10.1002/lary.24833|pmid=25130300|s2cid=23401780}}</ref> | |||
| * Adverse effects on the cardiovascular system of children.<ref>{{cite journal|last1=Raghuveer|first1=Geetha|last2=White|first2=David A.|last3=Hayman|first3=Laura L.|last4=Woo|first4=Jessica G.|last5=Villafane|first5=Juan|last6=Celermajer|first6=David|last7=Ward|first7=Kenneth D.|last8=de Ferranti|first8=Sarah D.|last9=Zachariah|first9=Justin|title=Cardiovascular Consequences of Childhood Secondhand Tobacco Smoke Exposure: Prevailing Evidence, Burden, and Racial and Socioeconomic Disparities: A Scientific Statement From the American Heart Association|journal=Circulation|date=18 October 2016|volume=134|issue=16|pages=e336–59 |pmid=27619923 |pmc=5207215 |doi=10.1161/CIR.0000000000000443 }}</ref> | |||
| == Evidence == | |||
| There is some evidence that reducing exposure to tobacco smoke cuts the risk of ]. When ] implemented a 100% smokefree law, heart attack admissions in the local hospital dropped by 40%, and rebounded when a court suspended the law.<ref>{{cite journal |author=Sargent RP, Shepard RM, Glantz SA |title=Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study |journal=BMJ |volume=328 |issue=7446 |pages=977–80 |year=2004 |pmid=15066887 |doi=10.1136/bmj.38055.715683.55}}</ref> Heart attack admissions have been shown by meta-analysis to drop by an average 27%<ref>{{cite journal |author=Dinno A, Glantz S |title=Clean indoor air laws immediately reduce heart attacks |journal=Prev Med |volume=45 |issue=1 |pages=9–11 |year=2007 |pmid=17499350 |doi=10.1016/j.ypmed.2007.03.013}}</ref> after the implementation of smoke-free laws. | |||
| ] | |||
| ] studies show that non-smokers exposed to secondhand smoke are at risk for many of the health problems associated with direct smoking.{{cn|date=December 2024}} | |||
| In 1992, a review estimated that secondhand smoke exposure was responsible for 35,000 to 40,000 deaths per year in the ] in the early 1980s.<ref name="steenland">{{cite journal |last1=Steenland |first1=K. |title=Passive smoking and the risk of heart disease |journal=JAMA |date=1 January 1992 |volume=267 |issue=1 |pages=94–99 |doi=10.1001/jama.267.1.94 |pmid=1727204 }}</ref> The ] of heart disease due to ETS was 2.2%, while the ] was 23%. A 1997 meta-analysis found that secondhand smoke exposure increased the risk of heart disease by a quarter,<ref>{{cite journal |last1=Law |first1=M R |last2=Morris |first2=J K |last3=Wald |first3=N J |title=Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence |journal=BMJ |date=18 October 1997 |volume=315 |issue=7114 |pages=973–980 |doi=10.1136/bmj.315.7114.973 |pmid=9365294 |pmc=2127675 }}</ref> and two 1999 meta-analyses reached similar conclusions.<ref>{{cite journal |last1=Thun |first1=M |last2=Henley |first2=J |last3=Apicella |first3=L |title=Epidemiologic studies of fatal and nonfatal cardiovascular disease and ETS exposure from spousal smoking |journal=Environmental Health Perspectives |date=December 1999 |volume=107 |issue=suppl 6 |pages=841–846 |doi=10.1289/ehp.99107s6841 |pmid=10592140 |pmc=1566204 |jstor=3434563 }}</ref><ref>{{cite journal |last1=He |first1=Jiang |last2=Vupputuri |first2=Suma |last3=Allen |first3=Krista |last4=Prerost |first4=Monica R. |last5=Hughes |first5=Janet |last6=Whelton |first6=Paul K. |title=Passive Smoking and the Risk of Coronary Heart Disease — A Meta-Analysis of Epidemiologic Studies |journal=New England Journal of Medicine |date=25 March 1999 |volume=340 |issue=12 |pages=920–926 |doi=10.1056/NEJM199903253401204 |pmid=10089185 |doi-access=free }}</ref> | |||
| Adults or children with ] can experience attacks brought on by passive smoking<ref>{{cite journal | author=Jang AS et al | title=The effect of passive smoking on asthma symptoms, atopy, and airway hyperresponsiveness in schoolchildren. | journal=J Korean Med Sci. | volume=19 | issue=2 | pages=214–7 | year=2004 | pmid=15082893}}</ref><ref>{{cite journal | author=Skorge TD, Eagan TM, Eide GE, Gulsvik A, Bakke PS. | title=The adult incidence of asthma and respiratory symptoms by passive smoking in uterus or in childhood. | journal=Am J Respir Crit Care Med. | volume=172 | issue=1 | pages=61–6 | year=2005 | pmid=15805186 | doi=10.1164/rccm.200409-1158OC}}</ref><ref>{{cite journal | author=Wafula EM, Limbe MS, Onyango FE, Nduati R. | title=Effects of passive smoking and breastfeeding on childhood bronchial asthma. | journal=East Afr Med J | volume=76 | issue=11 | pages=606–9 | year=1999 | pmid=10734518}}</ref><ref>{{cite journal | author=Cantani A, Micera M. | title=Epidemiology of passive smoke: a prospective study in 589 children. | journal=Eur Rev Med Pharmacol Sci. | volume=9 | issue=1 | pages=23–30 | year=2005 | pmid=15850141}}</ref><ref>{{cite journal | author=Eisner MD, Klein J, Hammond SK, ''et al.'' | title=Directly measured second hand smoke exposure and asthma health outcomes. | journal=Thorax | volume=2005 | issue=60 | pages=814–821 | year=2005 | pmid=16192366 | doi=10.1136/thx.2004.037283}}</ref>, and there has been one case study report of a death due to an asthma attack associated with passive smoking<ref>Stanbury M, Chester D, Hanna EA, Rosenman KD. . Am J Ind Med. 2008 Feb;51(2):111-6. PMID 18067177</ref>. | |||
| Since the 1980's there has been substantial evidence that there is a relationship between parents smoking in the house and children developing asthma and other related illnesses. <ref>Cook and Strachan 1997, 1998; | |||
| Jaakkola 2000; J.J.K. Jaakkola and Jaakkola</ref> | |||
| 2002). There have also been studies that investigated the exposure to tobacco smoke with the age of the child. Research has shown that the younger the child-as young as a fetus even-- the more susceptible and harmful the effects of second hand smoking can be. (<ref>How Exposure to Environmental Tobacco Smoke, Outdoor Air Pollutants,and Increased Pollen Burdens Influences the Incidence of AsthmaM. Ian Gilmour,1 Maritta S. Jaakkola,2 Stephanie J. London,3 Andre E. Nel,4 and Christine A. Rogers5 | |||
| </ref> These children of smokers tend to have a lung capacity that is less than children of the same height,weight, age, and sex of those children who are not exposed to constant second hand smoke.<ref>Growing Up in Smoke. Lynn Michell. Pluto Press 1990, Page 16</ref>Children who are exposed to cigarette smoke in their home day after day are more likely to cough, wheeze,get sore throats, and respiratory problems than children who live in homes with non-smokers.<ref>Growing Up in Smoke. Lynn Michell. Pluto Press 1990, Page 16</ref>Although it is not indefinite that the increased amount of asthma amongst children is primarily due to environmental tobacco smoke, there is substantial evidence that leads to the conclusion that it has a tremendous impact on it. | |||
| Evidence shows that inhaled sidestream smoke, the main component of secondhand smoke, is about four times more toxic than mainstream smoke. This fact has been known to the tobacco industry since the 1980s, though it kept its findings secret.<ref name="diethem2005">{{cite journal |vauthors=Diethelm PA, Rielle JC, McKee M |title=The whole truth and nothing but the truth? The research that Philip Morris did not want you to see |journal=Lancet |volume=366 |issue=9479 |pages=86–92 |year=2005 |pmid=15993237 |doi=10.1016/S0140-6736(05)66474-4 |s2cid=10442244 }}</ref><ref name="glantz2005">{{cite journal |vauthors=Schick S, Glantz S |title=Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke |journal=Tobacco Control |volume=14 |issue=6 |pages=396–404 |year=2005 |pmid=16319363 |doi=10.1136/tc.2005.011288 |pmc=1748121 }}</ref><ref name="schick2006">{{cite journal |vauthors=Schick S, Glantz SA |title=Sidestream cigarette smoke toxicity increases with aging and exposure duration |journal=Tobacco Control |volume=15 |issue=6 |pages=424–9 |year=2006 |pmid=17130369 |doi=10.1136/tc.2006.016162 |pmc=2563675 }}</ref><ref name="schick2007">{{cite journal |last1=Schick |first1=S. F. |last2=Glantz |first2=S. |title=Concentrations of the Carcinogen 4-(Methylnitrosamino)-1-(3-Pyridyl)-1-Butanone in Sidestream Cigarette Smoke Increase after Release into Indoor Air: Results from Unpublished Tobacco Industry Research |journal=Cancer Epidemiology, Biomarkers & Prevention|date=1 August 2007 |volume=16 |issue=8 |pages=1547–1553 |doi=10.1158/1055-9965.EPI-07-0210 |pmid=17684127 |s2cid=690030 |doi-access=free }}</ref> Some scientists believe that the risk of passive smoking, in particular the risk of developing ], may have been substantially underestimated.<ref>{{cite journal |last1=Whincup |first1=Peter H |last2=Gilg |first2=Julie A |last3=Emberson |first3=Jonathan R |last4=Jarvis |first4=Martin J |last5=Feyerabend |first5=Colin |last6=Bryant |first6=Andrew |last7=Walker |first7=Mary |last8=Cook |first8=Derek G |title=Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement |journal=BMJ |date=24 July 2004 |volume=329 |issue=7459 |pages=200–205 |doi=10.1136/bmj.38146.427188.55 |pmid=15229131 |pmc=487731 }}</ref> | |||
| Tobacco smoke is an ], and allergy sufferers can experience stuffy or runny noses, watery or burning eyes, sneezing, coughing, wheezing, a feeling of suffocation, and other typical allergy symptoms within minutes of exposure. | |||
| In 1997, a meta-analysis on the relationship between secondhand smoke exposure and lung cancer concluded that such exposure caused lung cancer. The increase in risk was estimated to be 24% among non-smokers who lived with a smoker.<ref>{{cite journal |last1=Hackshaw |first1=A K |last2=Law |first2=M R |last3=Wald |first3=N J |title=The accumulated evidence on lung cancer and environmental tobacco smoke |journal=BMJ |date=18 October 1997 |volume=315 |issue=7114 |pages=980–988 |doi=10.1136/bmj.315.7114.980 |pmid=9365295 |pmc=2127653 }}</ref> In 2000, Copas and Shi reported that there was clear evidence of publication bias in the studies included in this meta-analysis. They further concluded that after correcting for publication bias, and assuming that 40% of all studies are unpublished, this increased risk decreased from 24% to 15%.<ref>{{cite journal |last1=Copas |first1=J B |last2=Shi |first2=JQ |title=Reanalysis of epidemiological evidence on lung cancer and passive smoking |journal=BMJ |date=12 February 2000 |volume=320 |issue=7232 |pages=417–418 |doi=10.1136/bmj.320.7232.417 |pmid=10669446 |pmc=27286 }}</ref> This conclusion has been challenged on the basis that the assumption that 40% of all studies are unpublished was "extreme".<ref name=IARC2004/>{{rp|1269}} In 2006, Takagi et al. reanalyzed the data from this meta-analysis to account for publication bias and estimated that the relative risk of lung cancer among those exposed to secondhand smoke was 1.19, slightly lower than the original estimate.<ref>{{cite journal |last1=Takagi |first1=Hisato |last2=Sekino |first2=Seishiro |last3=Kato |first3=Takayoshi |last4=Matsuno |first4=Yukihiro |last5=Umemoto |first5=Takuya |title=Revisiting evidence on lung cancer and passive smoking: Adjustment for publication bias by means of "trim and fill" algorithm |journal=Lung Cancer |date=February 2006 |volume=51 |issue=2 |pages=245–246 |doi=10.1016/j.lungcan.2005.11.004 |pmid=16386820 }}</ref> A 2000 meta-analysis found a ] of 1.48 for lung cancer among men exposed to secondhand smoke, and a relative risk of 1.16 among those exposed to it at work.<ref>{{cite journal |last1=Zhong |first1=Lijie |last2=Goldberg |first2=Mark S |last3=Parent |first3=Marie-Élise |last4=Hanley |first4=James A |title=Exposure to environmental tobacco smoke and the risk of lung cancer: a meta-analysis |journal=Lung Cancer |date=January 2000 |volume=27 |issue=1 |pages=3–18 |doi=10.1016/s0169-5002(99)00093-8 |pmid=10672779 }}</ref> Another meta-analysis confirmed the finding of an increased risk of lung cancer among women with spousal exposure to secondhand smoke the following year. It found a relative risk of lung cancer of 1.29 for women exposed to secondhand smoke from their spouses.<ref>{{cite journal |last1=Taylor |first1=Richard |last2=Gumming |first2=Robert |last3=Woodward |first3=Alistair |last4=Black |first4=Megan |title=Passive smoking and lung cancer: a cumulative meta-analysis |journal=Australian and New Zealand Journal of Public Health |date=June 2001 |volume=25 |issue=3 |pages=203–211 |doi=10.1111/j.1467-842x.2001.tb00564.x |pmid=11494987 |s2cid=25724906 |doi-access=free }}</ref> A 2014 meta-analysis noted that "the association between exposure to secondhand smoke and lung cancer risk is well established."<ref>{{cite journal |last1=Kim |first1=Claire H. |last2=Lee |first2=Yuan-Chin Amy |last3=Hung |first3=Rayjean J. |last4=McNallan |first4=Sheila R. |last5=Cote |first5=Michele L. |last6=Lim |first6=Wei-Yen |last7=Chang |first7=Shen-Chih |last8=Kim |first8=Jin Hee |last9=Ugolini |first9=Donatella |last10=Chen |first10=Ying |last11=Liloglou |first11=Triantafillos |last12=Andrew |first12=Angeline S. |last13=Onega |first13=Tracy |last14=Duell |first14=Eric J. |last15=Field |first15=John K. |last16=Lazarus |first16=Philip |last17=Le Marchand |first17=Loic |last18=Neri |first18=Monica |last19=Vineis |first19=Paolo |last20=Kiyohara |first20=Chikako |last21=Hong |first21=Yun-Chul |last22=Morgenstern |first22=Hal |last23=Matsuo |first23=Keitaro |last24=Tajima |first24=Kazuo |last25=Christiani |first25=David C. |last26=McLaughlin |first26=John R. |last27=Bencko |first27=Vladimir |last28=Holcatova |first28=Ivana |last29=Boffetta |first29=Paolo |last30=Brennan |first30=Paul |last31=Fabianova |first31=Eleonora |last32=Foretova |first32=Lenka |last33=Janout |first33=Vladimir |last34=Lissowska |first34=Jolanta |last35=Mates |first35=Dana |last36=Rudnai |first36=Peter |last37=Szeszenia-Dabrowska |first37=Neonila |last38=Mukeria |first38=Anush |last39=Zaridze |first39=David |last40=Seow |first40=Adeline |last41=Schwartz |first41=Ann G. |last42=Yang |first42=Ping |last43=Zhang |first43=Zuo-Feng |title=Exposure to secondhand tobacco smoke and lung cancer by histological type: A pooled analysis of the International Lung Cancer Consortium (ILCCO): Secondhand tobacco smoke and lung cancer |journal=International Journal of Cancer |date=15 October 2014 |volume=135 |issue=8 |pages=1918–1930 |doi=10.1002/ijc.28835 |pmid=24615328 |pmc=4126868 }}</ref> | |||
| Many former smokers, and those who are trying to quit prefer to not be around smoke as it can cause them to have cravings. | |||
| A minority of epidemiologists have found it hard to understand how secondhand smoke, which is more diluted than actively inhaled smoke, could have an effect that is such a large fraction of the added risk of coronary heart disease among active smokers.<ref name="nature">{{cite journal |author=Novak K |title=Passive smoking: out from the haze |journal=Nature |volume=447 |issue=7148 |pages=1049–51 |year=2007 |pmid=17597735 |doi=10.1038/4471049a |bibcode=2007Natur.447.1049N |s2cid=9627500 |doi-access=free }}</ref><ref>{{cite journal |last1=Bailar |first1=John C. |title=Passive Smoking, Coronary Heart Disease, and Meta-Analysis |journal=New England Journal of Medicine |date=25 March 1999 |volume=340 |issue=12 |pages=958–959 |doi=10.1056/NEJM199903253401211 |pmid=10089192 }}</ref> One proposed explanation is that secondhand smoke is not simply a diluted version of "mainstream" smoke, but has a different composition with more toxic substances per gram of total particulate matter.<ref name="nature"/> Passive smoking appears to be capable of precipitating the acute manifestations of cardio-vascular diseases (atherothrombosis) and may also have a negative impact on the outcome of patients who have acute coronary syndromes.<ref>{{cite journal |last1=Raupach |first1=Tobias |last2=Schäfer |first2=Katrin |last3=Konstantinides |first3=Stavros |last4=Andreas |first4=Stefan |title=Secondhand smoke as an acute threat for the cardiovascular system: a change in paradigm |journal=European Heart Journal |date=1 February 2006 |volume=27 |issue=4 |pages=386–392 |doi=10.1093/eurheartj/ehi601 |pmid=16230308 |doi-access=free }}</ref> | |||
| ==Causal mechanisms== | |||
| In 2004, the ] (IARC) of the ] (WHO) reviewed all significant published evidence related to tobacco smoking and cancer. It concluded: | |||
| A study issued in 2002 by the International Agency for Research on Cancer of the ] concluded that nonsmokers are exposed to the same carcinogens as active smokers.<ref>{{cite web | title= Disparity in Protecting Food Service Staff from Secondhand Smoke Shows Need for Comprehensive Smoke-Free Policies, Say Groups | url=http://releases.usnewswire.com/GetRelease.asp?id=28683 }}</ref> ] contains more than 4000 chemicals, including 69 known carcinogens such as formaldehyde, lead, arsenic, benzene, and radioactive polonium 210,<ref>; the overall evaluation of the Monograph is: "Involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) is carcinogenic to humans (Group 1)."</ref> and several well-established ]s have been shown by the tobacco companies' own research to be present at higher concentrations in sidestream smoke than in mainstream smoke.<ref>{{cite journal | author=Schick S, Glantz S. | title=Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke. | journal=Tob Control. | volume=14 | issue=6 | pages=396–404 | year=2005 | pmid=16319363 | doi=10.1136/tc.2005.011288}}</ref> | |||
| {{blockquote|These meta-analyses show that there is a statistically significant and consistent association between lung cancer risk in spouses of smokers and exposure to second-hand tobacco smoke from the spouse who smokes. The excess risk is of the order of 20% for women and 30% for men and remains after controlling for some potential sources of bias and confounding.<ref name=IARC2004/>}} | |||
| Environmental tobacco smoke (ETS) has been shown to be a much higher source of pollution than an idling ] engine in regard to ] matter (PM) emission. In an experiment conducted by the Tobacco Control Unit of the National Cancer Institute, three cigarettes were left ]ing, one after the other, in a 60 m³ garage with a limited air exchange. The cigarettes produced PM indoor pollution exceeding outdoor limits, as well as PM concentrations up to 10-fold that of the idling engine.<ref>{{cite journal |author=Invernizzi G, Ruprecht A, Mazza R, ''et al'' |title=Particulate matter from tobacco versus diesel car exhaust: an educational perspective |journal=Tob Control |volume=13 |issue=3 |pages=219–21 |year=2004 |pmid=15333875 |doi=10.1136/tc.2003.005975}}</ref> | |||
| Subsequent meta-analyses have confirmed these findings.<ref name="pmid17690135">{{cite journal |last1=Taylor |first1=R. |last2=Najafi |first2=F. |last3=Dobson |first3=A. |title=Meta-analysis of studies of passive smoking and lung cancer: effects of study type and continent |journal=International Journal of Epidemiology |date=1 October 2007 |volume=36 |issue=5 |pages=1048–1059 |doi=10.1093/ije/dym158 |pmid=17690135 |doi-access=free }}</ref><ref name="pmid17267733">{{cite journal |last1=Stayner |first1=Leslie |last2=Bena |first2=James |last3=Sasco |first3=Annie J. |last4=Smith |first4=Randall |last5=Steenland |first5=Kyle |last6=Kreuzer |first6=Michaela |last7=Straif |first7=Kurt |title=Lung Cancer Risk and Workplace Exposure to Environmental Tobacco Smoke |journal=American Journal of Public Health |date=March 2007 |volume=97 |issue=3 |pages=545–551 |doi=10.2105/AJPH.2004.061275 |pmid=17267733 |pmc=1805004 }}</ref> | |||
| Tobacco smoke exposure has immediate and substantial effects on blood and blood vessels in a way that increases the risk of a heart attack, particularly in people already at risk.<ref>{{cite journal |author=Barnoya J, Glantz SA |title=Cardiovascular effects of secondhand smoke: nearly as large as smoking |journal=Circulation |volume=111 |issue=20 |pages=2684–98 |year=2005 |pmid=15911719 |doi=10.1161/CIRCULATIONAHA.104.492215}}</ref> Exposure to tobacco smoke for 30 minutes significantly reduces coronary flow velocity reserve in healthy nonsmokers.<ref name="pmid11466122">{{cite journal |author=Otsuka R, Watanabe H, Hirata K, ''et al'' |title=Acute effects of passive smoking on the coronary circulation in healthy young adults |journal=JAMA |volume=286 |issue=4 |pages=436–41 |year=2001 |pmid=11466122|doi=10.1001/jama.286.4.436}}</ref> | |||
| ==Epidemiological studies of passive smoking== | |||
| Epidemiological studies show that non-smokers exposed to secondhand smoke are at risk for many of the health problems associated with direct smoking. | |||
| In 1992, the '']'' published a review of the available evidence regarding the relationship between secondhand smoke and heart disease, and estimated that passive smoking was responsible for 35,000 to 40,000 deaths per year in the ] in the early 1980s.<ref>{{cite journal |author=Steenland K |title=Passive smoking and the risk of heart disease |journal=JAMA |volume=267 |issue=1 |pages=94–9 |year=1992 |pmid=1727204| doi= 10.1001/jama.267.1.94}}</ref> Some studies find that non-smokers living with smokers have about a 25% increase in risk of death from heart attack, are more likely to suffer a stroke, and can sometimes contract genital cancer. | |||
| Some research, with better measures of secondhand smoke exposure suggests that risks to nonsmokers may be even greater than this estimate. A British study reported that exposure to secondhand smoke increases the risk of heart disease among non-smokers by as much as 60%, similar to light smoking.<ref name="pmid15229131">{{cite journal |author=Whincup PH, Gilg JA, Emberson JR, ''et al'' |title=Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement |journal=BMJ |volume=329 |issue=7459 |pages=200–5 |year=2004 |pmid=15229131 |doi=10.1136/bmj.38146.427188.55}}</ref> | |||
| Parental smoking can affect children and babies, and is associated with low birth weight, sudden infant death syndrome (SIDS), bronchitis and pneumonia, and ].<ref>{{cite web | title=Fact sheet published by the Victorian government (Australia) | url=http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Smoking_and_heart_disease_the_facts?OpenDocument | accessdate=2006-07-26}}</ref> | |||
| In 2002, a group of 29 experts from 12 countries convened by the Monographs Programme of the ] (IARC) of the ] (WHO) reviewed all significant published evidence related to tobacco smoking and cancer. It concluded: | |||
| <blockquote>These meta-analyses show that there is a statistically significant and consistent association between lung cancer risk in spouses of smokers and exposure to secondhand tobacco smoke from the spouse who smokes. The excess risk is of the order of 20% for women and 30% for men and remains after controlling for some potential sources of bias and confounding.<ref>{{cite web | title=Monographs Programme report on SHS | url=http://monographs.iarc.fr/htdocs/monographs/vol83/02-involuntary.html | accessdate=2006-07-26}}</ref></blockquote> | |||
| Subsequent meta-analyses have confirmed these findings,<ref name="pmid17690135">{{cite journal |author=Taylor R, Najafi F, Dobson A |title=Meta-analysis of studies of passive smoking and lung cancer: effects of study type and continent |journal= International Journal of Epidemiology|volume= 36|issue= |pages=1048|year=2007 |pmid=17690135 |doi=10.1093/ije/dym158}}</ref><ref name="pmid17267733">{{cite journal |author=Stayner L, Bena J, Sasco AJ, ''et al'' |title=Lung cancer risk and workplace exposure to environmental tobacco smoke |journal=American journal of public health |volume=97 |issue=3 |pages=545–51 |year=2007 |pmid=17267733 |doi=10.2105/AJPH.2004.061275}}</ref> and additional studies have found that high overall exposure to passive smoke even among people with non-smoking partners is associated with greater risks than partner smoking and is widespread in non-smokers.<ref name="pmid15229131"/> | |||
| The National Asthma Council of Australia cites studies showing that environmental tobacco smoke (ETS) is probably the most important indoor pollutant, especially around young children:<ref>{{cite web | title=Health effects of indoor air pollution | url=http://www.nationalasthma.org.au/html/management/infopapers/health_professionals/4005.asp | accessdate=2006-07-26 }}</ref> | |||
| The National Asthma Council of Australia cites studies showing that secondhand smoke is probably the most important ], especially around young children:<ref>{{cite web |title=Health effects of indoor air pollution |url=http://www.nationalasthma.org.au/html/management/infopapers/health_professionals/4005.asp |access-date=2006-07-26 |url-status=dead |archive-url=https://web.archive.org/web/20060805200559/http://www.nationalasthma.org.au/HTML/management/infopapers/health_professionals/4005.asp |archive-date=2006-08-05 }}</ref> | |||
| * Smoking by either parent, particularly by the mother, increases the risk of asthma in children. | * Smoking by either parent, particularly by the mother, increases the risk of asthma in children. | ||
| * The outlook for early childhood asthma is less favourable in smoking households. | * The outlook for early childhood asthma is less favourable in smoking households. | ||
| Line 80: | Line 88: | ||
| * Doctor-diagnosed asthma is more common among non-smoking adults exposed to ETS than those not exposed. Among people with asthma, higher ETS exposure is associated with a greater risk of severe attacks. | * Doctor-diagnosed asthma is more common among non-smoking adults exposed to ETS than those not exposed. Among people with asthma, higher ETS exposure is associated with a greater risk of severe attacks. | ||
| In ] |
In ], exposure to secondhand smoke has been estimated to cause between 3,000<ref>{{cite journal |last1=Wirth |first1=N. |last2=Abou-Hamdan |first2=K. |last3=Spinosa |first3=A. |last4=Bohadana |first4=A. |last5=Martinet |first5=Y. |title=Le tabagisme passif |trans-title=Passive smoking |language=fr |journal=Revue de Pneumologie Clinique |date=March 2005 |volume=61 |issue=1 |pages=7–15 |doi=10.1016/s0761-8417(05)84776-5 |pmid=15772574 }}</ref> and 5,000 premature deaths per year, with the larger figure cited by Prime Minister ] during his announcement of a nationwide smoke-free law: "That makes more than 13 deaths a day. It is an unacceptable reality in our country in terms of public health."<ref name="France to ban smoking">{{cite news |title=France to ban smoking in public |url=http://news.bbc.co.uk/1/hi/world/europe/6032125.stm |access-date=2006-10-09 |publisher = ] |date = 2006-10-08}}</ref> | ||
| There is good observational evidence that smoke-free legislation reduces the number of hospital admissions for heart disease.<ref>{{cite journal |last1=Meyers |first1=David G. |last2=Neuberger |first2=John S. |last3=He |first3=Jianghua |title=Cardiovascular Effect of Bans on Smoking in Public Places |journal=Journal of the American College of Cardiology |date=September 2009 |volume=54 |issue=14 |pages=1249–1255 |doi=10.1016/j.jacc.2009.07.022 |pmid=19778665 |doi-access=free }}</ref><ref>{{cite journal |last1=Lin |first1=Hualiang |last2=Wang |first2=Hongchun |last3=Wu |first3=Wei |last4=Lang |first4=Lingling |last5=Wang |first5=Qinzhou |last6=Tian |first6=Linwei |title=The effects of smoke-free legislation on acute myocardial infarction: a systematic review and meta-analysis |journal=BMC Public Health |date=December 2013 |volume=13 |issue=1 |pages=529 |doi=10.1186/1471-2458-13-529 |pmid=23721370 |pmc=3671962 |doi-access=free }}</ref> | |||
| ===Studies of passive smoking in animals=== | |||
| Experimental studies in which animals are exposed to tobacco smoke have produced results supporting the ]icity of passive smoking. The International Agency for Research on Cancer expert group concluded that: | |||
| === Exposure and risk levels === | |||
| <blockquote>There is ''limited evidence'' in experimental animals for the carcinogenicity of mixtures of mainstream and sidestream tobacco smoke. | |||
| The ] of the ] concluded in 2004 that there was sufficient evidence that secondhand smoke caused cancer in humans.<ref name=IARC2004/> Those who work in environments where smoke is not regulated are at higher risk.<ref>{{cite journal |last1=Wells |first1=A J |title=Lung cancer from passive smoking at work |journal=American Journal of Public Health |date=July 1998 |volume=88 |issue=7 |pages=1025–1029 |doi=10.2105/ajph.88.7.1025 |pmid=9663148 |pmc=1508269 }}</ref><ref name="pmid17267733"/> Workers particularly at risk of exposure include those in installation repair and maintenance, construction and extraction, and transportation.<ref name=Fitzsimmons/> | |||
| Much research has come from studies of nonsmokers who are married to a smoker. The ], in his 2006 report, estimated that living or working in a place where smoking is permitted increases the non-smokers' risk of developing heart disease by 25–30% and lung cancer by 20–30%.<ref>{{Cite book|title = The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General|url = https://www.ncbi.nlm.nih.gov/books/NBK44324/|publisher = Centers for Disease Control and Prevention (US)|date = 2006|access-date = 2015-04-24|pmid = 20669524|series = Publications and Reports of the Surgeon General|author1 = Office on Smoking Health (US)}}</ref> | |||
| There is ''sufficient evidence'' in experimental animals for the carcinogenicity of sidestream smoke condensates.<ref>{{cite web | title=International Agency for Research on Cancer (IARC) - Involuntary Smoking | url=http://www.inchem.org/documents/iarc/vol83/02-involuntary.html | accessdate=2006-07-17 }}</ref></blockquote> | |||
| Similarly, children who are exposed to environmental tobacco smoke are shown to experience a range of adverse effects<ref name="PugmireSweeting2017">{{cite journal |last1=Pugmire |first1=Juliana |last2=Sweeting |first2=Helen |last3=Moore |first3=Laurence |title=Environmental tobacco smoke exposure among infants, children and young people: now is no time to relax |journal=Archives of Disease in Childhood |date=February 2017 |volume=102 |issue=2 |pages=117–118 |doi=10.1136/archdischild-2016-311652 |pmid=28100555 |s2cid=41806496 |doi-access=free }}</ref><ref name="StrachanCook1997">{{cite journal |last1=Strachan |first1=D P |last2=Cook |first2=D G |title=Health effects of passive smoking. 1. Parental smoking and lower respiratory illness in infancy and early childhood |journal=Thorax |date=October 1997 |volume=52 |issue=10 |pages=905–914 |doi=10.1136/thx.52.10.905 |pmid=9404380 |pmc=1758431 }}</ref><ref name="StrachanCook1998">{{cite journal |last1=Strachan |first1=D. P. |last2=Cook |first2=D. G. |title=Health effects of passive smoking. 4. Parental smoking, middle ear disease and adenotonsillectomy in children |journal=Thorax |date=1 January 1998 |volume=53 |issue=1 |pages=50–56 |doi=10.1136/thx.53.1.50 |pmid=9577522 |pmc=1758689 }}</ref> and a higher risk of becoming smokers later in life.<ref>{{cite journal |last1=Song |first1=Anna V. |last2=Glantz |first2=Stanton A. |last3=Halpern-Felsher |first3=Bonnie L. |title=Perceptions of Second-hand Smoke Risks Predict Future Adolescent Smoking Initiation |journal=Journal of Adolescent Health |date=December 2009 |volume=45 |issue=6 |pages=618–625 |doi=10.1016/j.jadohealth.2009.04.022 |pmid=19931835 |pmc=2814413 }}</ref> The ] has identified reduction of exposure to environmental tobacco smoke as key element for actions to encourage healthy child development.<ref>{{cite web|access-date=2024-06-12|title=WHO Framework Convention on Tobacco Control (WHO FCTC)|url=https://www.who.int/europe/teams/tobacco/who-framework-convention-on-tobacco-control-(who-fctc)|website=www.who.int}}</ref> | |||
| Secondhand smoke is generally recognized as a risk factor for cancer in pets.<ref>, by Andrea Thompson. Posted at LiveScience on ] ]; accessed ] ].</ref> A study conducted by the ] and the ] concluded that cats living with a smoker were more likely to get ]; the risk increased with the duration of exposure to secondhand smoke and the number of smokers in the household.<ref>{{cite journal | author=Snyder LA, Bertone ER, Jakowski RM, Dooner MS, Jennings-Ritchie J, Moore AS. | title=p53 expression and environmental tobacco smoke exposure in feline oral squamous cell carcinoma. | journal=Vet Pathol | volume=41 | issue=3 | pages=209–14 | year=2004 | pmid=15133168 | doi=10.1354/vp.41-3-209}}</ref> A study by ] researchers, looking at cases of canine lung cancer, was generally inconclusive, though the authors reported a weak relation for lung cancer in dogs exposed to environmental tobacco smoke.<ref>{{cite journal | author=Reif JS, Dunn K, Ogilvie GK, Harris CK. | title=Passive smoking and canine lung cancer risk. | journal=Am J Epidemiol. | volume=135 | issue=3 | pages=234–9 | year=1992 | pmid=1546698}}</ref> | |||
| The US ] monitors the extent of and trends in exposure to environmental tobacco smoke by measuring serum ] in national health ].<ref>{{cite journal |last1=Tsai |first1=James |last2=Homa |first2=David M. |last3=Gentzke |first3=Andrea S. |last4=Mahoney |first4=Margaret |last5=Sharapova |first5=Saida R. |last6=Sosnoff |first6=Connie S. |last7=Caron |first7=Kevin T. |last8=Wang |first8=Lanqing |last9=Melstrom |first9=Paul C. |last10=Trivers |first10=Katrina F. |title=Exposure to Secondhand Smoke Among Nonsmokers — United States, 1988–2014 |journal=MMWR. Morbidity and Mortality Weekly Report |date=7 December 2018 |volume=67 |issue=48 |pages=1342–1346 |doi=10.15585/mmwr.mm6748a3|pmid=30521502 |pmc=6329485 }}</ref> The ] of secondhand smoke exposure among U.S. nonsmokers declined from 87.5% in 1988 to 25.2% in 2014. However, nearly half of ] and the poor were exposed in 2014. | |||
| In 1990, a tobacco-industry researcher in ] proposed a study of the effects on animals of lifetime exposure to secondhand smoke. The proposed study was blocked by ],<ref>{{cite journal |author=Drope J, Chapman S |title=Tobacco industry efforts at discrediting scientific knowledge of environmental tobacco smoke: a review of internal industry documents |journal=Journal of epidemiology and community health |volume=55 |issue=8 |pages=588–94 |year=2001 |pmid=11449018|doi=10.1136/jech.55.8.588}}</ref> as described in an internal company report: | |||
| === Interventions to reduce environmental tobacco smoke === | |||
| <blockquote>PM recently succeeded in blocking Adlkofer's plan to conduct lifetime animal inhalation study of sidestream smoke. ( . . .an INBIFO study has shown that in 90-day inhalation test, no non-reversible changes has been detected. In a lifetime study, the results were almost certain to be less favorable. Based on the analysis, the other members of the German industry agreed that the proposed study should not proceed.)<ref>, from the . Accessed ] ].</ref></blockquote> | |||
| A systematic review compared smoking control programmes and their effects on smoke exposure in children. The review distinguishes between community-based, ill-child and healthy-child settings and the most common types of interventions were counselling or brief advice during clinical visits. The review did not find superior outcomes for any intervention, and the authors caution that evidence from adult settings may not generalise well to children.<ref name="BehbodSharma2018">{{cite journal |last1=Behbod |first1=Behrooz |last2=Sharma |first2=Mohit |last3=Baxi |first3=Ruchi |last4=Roseby |first4=Robert |last5=Webster |first5=Premila |title=Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke |journal=Cochrane Database of Systematic Reviews |date=31 January 2018 |volume=1 |issue=1 |pages=CD001746 |doi=10.1002/14651858.CD001746.pub4 |pmid=29383710 |pmc=6491082 }}</ref> | |||
| ===Biomarkers=== | |||
| ===Risk level of passive smoking=== | |||
| ] | |||
| The ] of the ] concluded in 2002 that: | |||
| Environmental tobacco smoke can be evaluated either by directly measuring tobacco smoke pollutants found in the air or by using biomarkers, an indirect measure of exposure. ] monitored through breath, ], ], ], and proteins are the most specific biological markers of tobacco smoke exposure.<ref name=Metz05>{{cite journal |vauthors=Metz-Favre C, Donnay C, de Blay F |title= |language=fr |journal=Rev Mal Respir |volume=22 |issue=1 Pt 1 |pages=81–92 |date=February 2005 |pmid=15968761 |doi=10.1016/S0761-8425(05)85439-7 }}</ref><ref>{{cite journal |author=McClure JB |title=Are biomarkers useful treatment aids for promoting health behavior change? An empirical review |journal=Am J Prev Med |volume=22 |issue=3 |pages=200–7 |date=April 2002 |pmid=11897465 |doi=10.1016/S0749-3797(01)00425-1 }}</ref> Biochemical tests are a much more reliable biomarker of secondhand smoke exposure than surveys. Certain groups of people are reluctant to disclose their smoking status and exposure to tobacco smoke, especially pregnant women and parents of young children. This is due to their smoking being socially unacceptable. Also, it may be difficult for individuals to recall their exposure to tobacco smoke.<ref>{{cite journal |vauthors=Klesges RC, Debon M, Ray JW |title=Are self-reports of smoking rate biased? Evidence from the Second National Health and Nutrition Examination Survey |journal=J Clin Epidemiol |volume=48 |issue=10 |pages=1225–33 |date=October 1995 |pmid=7561984 |doi=10.1016/0895-4356(95)00020-5 }}</ref> | |||
| A 2007 study in the '']'' journal found a positive correlation between secondhand tobacco smoke exposure and concentrations of nicotine and/or biomarkers of nicotine in the body. Significant biological levels of nicotine from secondhand smoke exposure were equivalent to nicotine levels from active smoking and levels that are associated with behaviour changes due to nicotine consumption.<ref>{{cite journal |vauthors=Okoli CT, Kelly T, Hahn EJ |title=Secondhand smoke and nicotine exposure: a brief review |journal=Addict Behav |volume=32 |issue=10 |pages=1977–88 |date=October 2007 |pmid=17270359 |doi=10.1016/j.addbeh.2006.12.024 }}</ref> | |||
| <blockquote>There is ''sufficient evidence'' that involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) causes lung cancer in humans. | |||
| ====Cotinine==== | |||
| ... | |||
| ], the metabolite of nicotine, is a biomarker of secondhand smoke exposure. Typically, cotinine is measured in the blood, saliva, and urine. Hair analysis has recently become a new, noninvasive measurement technique. Cotinine accumulates in hair during hair growth, which results in a measure of long-term, cumulative exposure to tobacco smoke.<ref name=Florescu09>{{cite journal |vauthors=Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, Koren G |title=Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology |journal=Ther Drug Monit |volume=31 |issue=1 |pages=14–30 |date=February 2009 |pmid=19125149 |pmc=3644554 |doi=10.1097/FTD.0b013e3181957a3b }}</ref> Urinary cotinine levels have been a reliable biomarker of tobacco exposure and have been used as a reference in many epidemiological studies.<ref name="BehbodSharma2018"/> However, cotinine levels found in the urine reflect exposure only over the preceding 48 hours. Cotinine levels of the skin, such as the hair and nails, reflect tobacco exposure over the previous three months and are a more reliable biomarker.<ref name=Metz05/> | |||
| ====Carbon monoxide (CO)==== | |||
| Involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) is ''carcinogenic to humans (Group 1)''.<ref>{{cite web | title=International Agency for Research on Cancer (IARC) - Involuntary Smoking | url=http://www.inchem.org/documents/iarc/vol83/02-involuntary.html | accessdate=2006-07-17 }}</ref></blockquote> | |||
| ] is also a reliable biomarker of secondhand smoke exposure as well as tobacco use. With high sensitivity and specificity, it not only provides an accurate measure, but the test is also non-invasive, highly reproducible, and low in cost. Breath CO monitoring measures the concentration of CO in an exhalation in ], and this can be directly correlated to the blood CO concentration (]).<ref>{{cite journal |vauthors=Irving JM, Clark EC, Crombie IK, Smith WC |title=Evaluation of a portable measure of expired-air carbon monoxide |journal=Prev Med |volume=17 |issue=1 |pages=109–15 |date=January 1988 |pmid=3362796 |doi=10.1016/0091-7435(88)90076-X }}</ref> Breath CO monitors can also be used by emergency services to identify patients who are suspected of having CO poisoning. | |||
| == Pathophysiology == | |||
| Most experts believe that moderate, occasional exposure to secondhand smoke presents a small but measurable cancer risk to nonsmokers. The overall risk depends on the effective dose received over time. The risk is more significant if non-smokers spend many hours in an environment where cigarette smoke is prevalent, such as a business where many employees or patrons are smoking throughout the day, or a residential care facility where residents smoke freely.<ref>{{cite journal |author=Boffetta P, Agudo A, Ahrens W, ''et al'' |title=Multicenter case-control study of exposure to environmental tobacco smoke and lung cancer in Europe |journal=J. Natl. Cancer Inst. |volume=90 |issue=19 |pages=1440–50 |year=1998 |pmid=9776409|doi=10.1093/jnci/90.19.1440}}</ref> | |||
| A 2004 study by the ] of the ] concluded that non-smokers are exposed to the same carcinogens as active smokers. ] contains more than 4,000 chemicals, including 69 known carcinogens. Of special concern are ], tobacco-specific N-], and ], such as ], all known to be highly carcinogenic. Mainstream smoke, sidestream smoke, and secondhand smoke contain largely the same components, however the concentration varies depending on type of smoke.<ref name=IARC2004/> Several well-established ]s have been shown by the tobacco companies' own research to be present at higher concentrations in sidestream smoke than in mainstream smoke.<ref>{{cite journal |vauthors=Schick S, Glantz S |title=Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke |journal=Tob. Control |volume=14 |issue=6 |pages=396–404 |year=2005 |pmid=16319363 |pmc=1748121 |doi=10.1136/tc.2005.011288 }}</ref> | |||
| Secondhand smoke has been shown to produce more particulate-matter (PM) pollution than an idling low-emission ]. In an experiment conducted by the Italian National Cancer Institute, three cigarettes were left ]ing, one after the other, in a 60 m<sup>3</sup> garage with a limited air exchange. The cigarettes produced PM pollution exceeding outdoor limits, as well as PM concentrations up to 10-fold that of the idling engine.<ref>{{cite journal |vauthors=Invernizzi G, Ruprecht A, Mazza R, etal |title=Particulate matter from tobacco versus diesel car exhaust: an educational perspective |journal=Tob Control |volume=13 |issue=3 |pages=219–21 |year=2004 |pmid=15333875 |pmc=1747905 |doi=10.1136/tc.2003.005975 }}</ref> | |||
| In May 2006, the United States ] issued its first new study on secondhand smoke in 20 years. ] ] summarized: | |||
| Secondhand tobacco smoke exposure has immediate and substantial effects on blood and blood vessels in a way that increases the risk of a heart attack, particularly in people already at risk.<ref>{{cite journal |vauthors=Barnoya J, Glantz SA |title=Cardiovascular effects of secondhand smoke: nearly as large as smoking |journal=Circulation |volume=111 |issue=20 |pages=2684–98 |year=2005 |pmid=15911719 |doi=10.1161/CIRCULATIONAHA.104.492215 |s2cid=2291566 |doi-access=free }}</ref> Exposure to tobacco smoke for 30 minutes significantly reduces coronary flow velocity reserve in healthy nonsmokers.<ref name="pmid11466122">{{cite journal |vauthors=Otsuka R, Watanabe H, Hirata K, etal |title=Acute effects of passive smoking on the coronary circulation in healthy young adults |journal=JAMA |volume=286 |issue=4 |pages=436–41 |year=2001 |pmid=11466122|doi=10.1001/jama.286.4.436 |doi-access=free }}</ref> Secondhand smoke is also associated with impaired ] among adult nonsmokers.<ref>{{cite journal|last1=Celermajer|first1=David S.|last2=Adams|first2=Mark R.|last3=Clarkson|first3=Peter|last4=Robinson|first4=Jacqui|last5=McCredie|first5=Robyn|last6=Donald|first6=Ann|last7=Deanfield|first7=John E.|title=Passive Smoking and Impaired Endothelium-Dependent Arterial Dilatation in Healthy Young Adults|journal=New England Journal of Medicine|date=18 January 1996|volume=334|issue=3|pages=150–155|doi=10.1056/NEJM199601183340303|pmid=8531969|doi-access=free}}</ref> Secondhand smoke exposure also affects ] function, vascular ], and myocardial exercise tolerance at levels commonly found in the workplace.<ref>{{cite journal|last1=Howard|first1=G|last2=Thun|first2=MJ|title=Why is environmental tobacco smoke more strongly associated with coronary heart disease than expected? A review of potential biases and experimental data|journal=Environmental Health Perspectives|date=December 1999|volume=107|issue=Suppl 6|pages=853–8|pmid=10592142|pmc=1566209|doi=10.2307/3434565|jstor=3434565}}</ref> | |||
| <blockquote>The health effects of secondhand smoke exposure are more pervasive than we previously thought. The scientific evidence is now indisputable: secondhand smoke is not a mere annoyance. It is a serious health hazard that can lead to disease and premature death in children and nonsmoking adults.</blockquote> | |||
| Pulmonary emphysema can be induced in rats through acute exposure to sidestream tobacco smoke (30 cigarettes per day) over a period of 45 days.<ref>{{cite journal |last1=Cendon |first1=S.P. |last2=Battlehner |first2=C. |last3=Lorenzi-Filho |first3=G. |last4=Dohlnikoff |first4=M. |last5=Pereira |first5=P.M. |last6=Conceição |first6=G.M.S. |last7=Beppu |first7=O.S. |last8=Saldiva |first8=P.H.N. |title=Pulmonary emphysema induced by passive smoking: an experimental study in rats |journal=Brazilian Journal of Medical and Biological Research |date=October 1997 |volume=30 |issue=10 |pages=1241–1247 |doi=10.1590/s0100-879x1997001000017 |pmid=9496445 |doi-access=free }}</ref> Degranulation of ]s contributing to lung damage has also been observed.<ref>{{cite journal |author1=Eren, U. |author2=Kum, S. |author3=Sandikci, M. |author4=Kara, E. |title=Effects of long-term passive smoking on the mast cells in rat lungs |journal=Revue de Médecine Vétérinaire |volume=6 |pages=319–322 |year=2006 |url=http://revmedvet.com/artdes-us.php?id=1434|archive-url=https://web.archive.org/web/20090113060853/http://revmedvet.com/artdes-us.php?id=1434|url-status=usurped|archive-date=January 13, 2009}}</ref> | |||
| The study estimated that living or working in a place where smoking is permitted increases the non-smokers' risk of developing heart disease by 25–30% and lung cancer by 20–30%. The report also found that passive smoke causes ] (SIDS), respiratory problems, ear infections, and ] attacks in children.<ref>{{cite news|title=Study: Secondhand Smoke Effects Pervasive|author=Marc Kaufman|url=http://www.washingtonpost.com/wp-dyn/content/article/2006/06/27/AR2006062700710.html|date=Tuesday, June 27, 2006|work=]}}</ref> | |||
| The term "]" was recently coined to identify the residual tobacco smoke contamination that remains after the cigarette is extinguished and secondhand smoke has cleared from the air.<ref>{{cite journal |vauthors=Matt GE, Quintana PJ, Hovell MF, etal |title=Households contaminated by environmental tobacco smoke: sources of infant exposures |journal=Tob Control |volume=13 |issue=1 |pages=29–37 |date=March 2004 |pmid=14985592 |pmc=1747815 |doi= 10.1136/tc.2003.003889}}</ref><ref>{{cite journal |vauthors=Winickoff JP, Friebely J, Tanski SE, etal |title=Beliefs about the health effects of "thirdhand" smoke and home smoking bans |journal=Pediatrics |volume=123 |issue=1 |pages=e74–9 |date=January 2009 |pmid=19117850 |doi=10.1542/peds.2008-2184 |pmc=3784302 }}</ref><ref>{{cite news |url = https://www.nytimes.com/2009/01/03/health/research/03smoke.html |work = ] |title = A New Cigarette Hazard: 'Third-Hand Smoke' |first = Roni Caryn |last = Rabin |date = 2009-01-02 |access-date = 2009-01-12}}</ref> Preliminary research suggests that by-products of third-hand smoke may pose a health risk,<ref>{{cite journal |last1=Sleiman |first1=M. |last2=Gundel |first2=L. A. |last3=Pankow |first3=J. F. |last4=Jacob |first4=P. |last5=Singer |first5=B. C. |last6=Destaillats |first6=H. |title=Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards |journal=Proceedings of the National Academy of Sciences |date=13 April 2010 |volume=107 |issue=15 |pages=6576–6581 |doi=10.1073/pnas.0912820107 |pmid=20142504 |pmc=2872399 |doi-access=free }}</ref> | |||
| ==Current state of scientific opinion== | |||
| though the magnitude of risk, if any, remains unknown. In October 2011, it was reported that Christus St. Frances Cabrini Hospital in ], would seek to eliminate third-hand smoke beginning in July 2012, and that employees whose clothing smelled of smoke would not be allowed to work. This prohibition was enacted because third-hand smoke poses a special danger for the developing brains of infants and small children.<ref>, Fox News, October 3, 2011</ref> | |||
| Currently, there is widespread ] that exposure to secondhand smoke is harmful.<ref name="kessler"/> The link between passive smoking and health risks is accepted by every major medical and scientific organization, including: | |||
| * The ]<ref>, a monograph of the ] and ]. Accessed ] ].</ref> | |||
| * The U.S. ]<ref>{{PDFlink||219 ]<!-- application/pdf, 225034 bytes -->}}. From the 11th Report on Carcinogens of the U.S. ]. Accessed ] ].</ref> | |||
| * The ]<ref> from the U.S. ]. Accessed ] ].</ref> | |||
| * The ]<ref>, from the ]. Accessed ] ].</ref> | |||
| * The U.S. ]<ref>, from the U.S. ]. Accessed ] ].</ref> | |||
| * The ]<ref>, from the ]. Accessed ] ].</ref> | |||
| * The ]<ref name="calepa2005" /> | |||
| * The ],<ref>, from the ]. Accessed ] ].</ref> ],<ref>, from the ]. Accessed ] ].</ref> and ]<ref>, from the ]. Accessed ] ].</ref> | |||
| * The ]<ref>. A press release from the ]. Accessed ] ].</ref> | |||
| * The ]<ref>. From the ] policy website. Accessed ] ].</ref> | |||
| *The Australian ]<ref name="nphp">, from the Australian National Public Health Partnership; see p. 6. Released November 2000; accessed ] ].</ref> | |||
| *The ] Scientific Committee on Tobacco and Health<ref>Two relevant reports have been published by the Scientific Committee: | |||
| *A concluded that passive smoking was a cause of lung cancer, heart disease, and other health problems. | |||
| *A , reviewing new evidence published since the 1998 report, found that recent research had confirmed the initially reported link between passive smoking and health risks.</ref> | |||
| *The governments of 151 nations have signed and ] the ], which states that "Parties recognize that scientific evidence has unequivocally established that exposure to tobacco smoke causes death, disease and disability."<ref> Part III, Article 8. Accessed ] ].</ref> | |||
| In 2008, there were more than 161,000 deaths attributed to lung cancer in the United States. Of these deaths, an estimated 10% to 15% were caused by factors other than first-hand smoking; equivalent to 16,000 to 24,000 deaths annually. Slightly more than half of the lung cancer deaths caused by factors other than first-hand smoking were found in nonsmokers. Lung cancer in non-smokers may well be considered one of the most common cancer mortalities in the United States. Clinical epidemiology of lung cancer has linked the primary factors closely tied to lung cancer in non-smokers as exposure to secondhand tobacco smoke, carcinogens including radon, and other indoor air pollutants.<ref>{{cite journal |last1=Samet |first1=J. M. |last2=Avila-Tang |first2=E. |last3=Boffetta |first3=P. |last4=Hannan |first4=L. M. |last5=Olivo-Marston |first5=S. |last6=Thun |first6=M. J. |last7=Rudin |first7=C. M. |title=Lung Cancer in Never Smokers: Clinical Epidemiology and Environmental Risk Factors |journal=Clinical Cancer Research |date=15 September 2009 |volume=15 |issue=18 |pages=5626–5645 |doi=10.1158/1078-0432.CCR-09-0376 |pmid=19755391 |pmc=3170525 }}</ref> | |||
| While there is scientific agreement regarding the existence of a link between passive smoking and heart disease, the magnitude of the increased risk remains debated by a minority of epidemiologists.<ref name="nature">{{cite journal |author=Novak K |title=Passive smoking: out from the haze |journal=Nature |volume=447 |issue=7148 |pages=1049–51 |year=2007 |pmid=17597735 |doi=10.1038/4471049a}}</ref> For example, John Bailar of the ] questioned the proportionality of the passive smoking risk, stating: | |||
| == Opinion of public health authorities == | |||
| <blockquote>Regular smoking only increases the risk of cardiovascular disease by 75%, so how could second-hand smoke, which is much more dilute, have an effect one-third that size?</blockquote> | |||
| There is widespread ] that exposure to secondhand smoke is harmful.<ref name="kessler">{{harvnb|Kessler|2006}}</ref> The link between passive smoking and health risks is accepted by every major medical and scientific organisation, including: | |||
| * ]<ref name=IARC2004/> | |||
| * U.S. ]<ref>{{cite web |url = https://ntp.niehs.nih.gov/ntp/roc/content/profiles/tobaccorelatedexposures.pdf |title = Environmental Tobacco Smoke |website = 11th Report on Carcinogens |publisher = U.S. ] |access-date = 2007-08-27 |url-status = live |archive-url = https://web.archive.org/web/20080716173310/http://ntp.niehs.nih.gov/ntp/roc/eleventh/profiles/s176toba.pdf |archive-date = 2008-07-16 }}</ref> | |||
| * ]<ref>{{cite web |url =https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/general_facts/index.htm |title = Secondhand Smoke Fact Sheet |publisher = U.S. ] |date = 2017-02-21 }}</ref> | |||
| * ]<ref name="sg-report"/> | |||
| * U.S. ]<ref>{{cite web |url = http://cancercontrol.cancer.gov/tcrb/monographs/10/index.html |title = Health Effects of Exposure to Environmental Tobacco Smoke |publisher = U.S. ] |access-date = 2007-08-22 |url-status = dead |archive-url = https://web.archive.org/web/20070905172350/http://cancercontrol.cancer.gov/tcrb/monographs/10/index.html |archive-date = 2007-09-05 }}</ref> | |||
| * ]<ref>{{cite web |url = http://www.epa.gov/smokefree/healtheffects.html |title = Health Effects of Exposure to Secondhand Smoke |publisher = ] |access-date = 2007-09-24}}</ref> | |||
| * ]<ref name="calepa2005"/> | |||
| * ],<ref>{{cite web |url = http://www.americanheart.org/presenter.jhtml?identifier=3039906 |title = The Truth about Secondhand Smoke |publisher = ] |access-date = 2007-08-27}}</ref> ],<ref>{{cite web |url = http://www.lungusa.org/site/pp.asp?c=dvLUK9O0E&b=35422 |title = Secondhand Smoke Fact Sheet |publisher = ] |access-date = 2007-09-24 |archive-url = https://web.archive.org/web/20070918063752/http://www.lungusa.org/site/pp.asp?c=dvLUK9O0E&b=35422 |archive-date = 2007-09-18}}</ref> and ]<ref>{{cite web |url = http://www.cancer.org/docroot/PED/content/PED_10_2X_Secondhand_Smoke-Clean_Indoor_Air.asp |title = Secondhand Smoke |publisher = ] |access-date = 2007-08-27 |url-status = dead |archive-url = https://web.archive.org/web/20070914162226/http://www.cancer.org/docroot/PED/content/PED_10_2X_Secondhand_Smoke-Clean_Indoor_Air.asp |archive-date = 2007-09-14 }}</ref> | |||
| * ]<ref>{{cite press release |url = http://www.ama-assn.org/ama/pub/category/16496.html |title = AMA: Surgeon General's secondhand smoke report a wake-up call to lawmakers |publisher = ] |access-date = 2007-08-27}}</ref> | |||
| * ]<ref>{{cite web |url = http://aappolicy.aappublications.org/cgi/content/full/pediatrics%3b107/4/794 |title = Tobacco's Toll: Implications for the Pediatrician |publisher = ] |access-date = 2007-10-02 |url-status = dead |archive-url = https://web.archive.org/web/20071015203456/http://aappolicy.aappublications.org/cgi/content/full/pediatrics;107/4/794 |archive-date = 2007-10-15 }}</ref> | |||
| * Australian ]<ref name="nphp">{{cite web |url = http://www.nphp.gov.au/publications/legislation/smoke_passive.pdf |title = National Response to Passive Smoking in Enclosed Public Places and Workplaces |publisher = Australian National Public Health Partnership |date = November 2000 |access-date = 2007-09-11 |url-status = dead |archive-url = https://web.archive.org/web/20140212191352/http://www.nphp.gov.au/publications/legislation/smoke_passive.pdf |archive-date = 2014-02-12 }}</ref> | |||
| * ] Scientific Committee on Tobacco and Health<ref>Two relevant reports have been published by the Scientific Committee: | |||
| * A concluded that passive smoking was a cause of lung cancer, heart disease, and other health problems. | |||
| * A {{webarchive|url=https://web.archive.org/web/20120206182922/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4101474 |date=2012-02-06 }}, reviewing new evidence published since the 1998 report, found that recent research had confirmed the initially reported link between passive smoking and health risks.</ref> | |||
| == Public opinion == | |||
| One proposed explanation is that secondhand smoke is not simply a diluted version of "mainstream" smoke, but has a different composition with more toxic substances per gram of total particulate matter.<ref name="nature"/> The more toxic makeup of secondhand smoke was first recognized in the tobacco industry's own research, though it never published its findings.<ref>Several medical journal articles have described both the more toxic composition of secondhand smoke and the tobacco industry's unpublished research confirming this. For example, see: | |||
| Recent major surveys conducted by the U.S. ] and ] have found widespread public awareness that secondhand smoke is harmful. In both 1992 and 2000 surveys, more than 80% of respondents agreed with the statement that secondhand smoke was harmful. A 2001 study found that 95% of adults agreed that secondhand smoke was harmful to children, and 96% considered tobacco-industry claims that secondhand smoke was not harmful to be untruthful.<ref>{{harvnb|Surgeon General|2006|p=588 Ch. 10}}</ref> | |||
| *{{cite journal |author=Diethelm PA, Rielle JC, McKee M |title=The whole truth and nothing but the truth? The research that Philip Morris did not want you to see |journal=Lancet |volume=366 |issue=9479 |pages=86–92 |year=2005 |pmid=15993237 |doi=10.1016/S0140-6736(05)66474-4}} | |||
| *{{cite journal |author=Schick S, Glantz S |title=Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke |journal=Tobacco control |volume=14 |issue=6 |pages=396–404 |year=2005 |pmid=16319363 |doi=10.1136/tc.2005.011288}} | |||
| *{{cite journal |author=Schick S, Glantz SA |title=Sidestream cigarette smoke toxicity increases with aging and exposure duration |journal=Tobacco control |volume=15 |issue=6 |pages=424–9 |year=2006 |pmid=17130369 |doi=10.1136/tc.2006.016162}} | |||
| *{{cite journal |author=Schick SF, Glantz S |title=Concentrations of the carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in sidestream cigarette smoke increase after release into indoor air: results from unpublished tobacco industry research |journal=Cancer Epidemiol. Biomarkers Prev. |volume=16 |issue=8 |pages=1547–53 |year=2007 |pmid=17684127 |doi=10.1158/1055-9965.EPI-07-0210}}</ref> Some scientists believe that the risk of passive smoking, in particular the risk of developing coronary heart diseases, may have been substantially underestimated.<ref>{{cite web |url=http://www.newscientist.com/article.ns?id=dn6091 |title=Passive smoking danger was underestimated, by Gaia Vince ''New Scientist'' 2004 June 30|accessdate=2007-07-24 |format= |work=}}</ref> | |||
| A 2007 ] found that 56% of respondents felt that secondhand smoke was "very harmful", a number that has held relatively steady since 1997. Another 29% believe that secondhand smoke is "somewhat harmful"; 10% answered "not too harmful", while 5% said "not at all harmful".<ref>{{cite web | url=http://www.gallup.com/poll/28216/more-smokers-feeling-harassed-smoking-bans.aspx | title=More Smokers Feeling Harassed by Smoking Bans | website=Gallup | date=25 July 2007 | access-date=20 February 2015 | author=Saad, Lydia}}</ref> | |||
| The health benefit to non-smokers of ]s has also been disputed by a small number of epidemiologists, who call for a prospective trial to more accurately determine the benefit. These epidemiologists advocate indoor smoking bans, but express a concern that widespread outdoor smoking bans, as implemented by some towns in the U.S., may be unsupported by the evidence available thus far.<ref name="nature"/> | |||
| == Controversy over harm == | |||
| ===Public opinion=== | |||
| As part of its attempt to prevent or delay tighter regulation of smoking, the tobacco industry funded a number of scientific studies and, where the results cast doubt on the risks associated with secondhand smoke, sought wide publicity for those results. The industry also funded libertarian and conservative think tanks, such as the ] in the United States and the ] in Australia which criticised both scientific research on passive smoking and policy proposals to restrict smoking.<ref>"". Accessed 8 April 2011.</ref><ref>Nahan, Mike. ''The Australian'', 10 April 2000, "The IPA sings its own song".</ref> ''New Scientist'' and the '']'' have identified these industry-wide coordinated activities as one of the earliest expressions of ]. Further, they state that the disinformation spread by the tobacco industry has created a ''tobacco denialism'' movement, sharing many characteristics of other forms of ], such as ].<ref>{{cite journal |last1=Shermer |first1=Michael |title=I am a sceptic, but I'm not a denier |journal=New Scientist |date=May 2010 |volume=206 |issue=2760 |pages=36–37 |doi=10.1016/S0262-4079(10)61210-9 |bibcode=2010NewSc.206R..36S }}</ref><ref>{{cite journal |last1=Diethelm |first1=P. |last2=McKee |first2=M. |title=Denialism: what is it and how should scientists respond? |journal=The European Journal of Public Health |date=16 October 2008 |volume=19 |issue=1 |pages=2–4 |doi=10.1093/eurpub/ckn139 |pmid=19158101 |s2cid=8098426 |doi-access=free }}</ref> | |||
| Recent major surveys conducted by the U.S. ] and ] have found widespread public belief that secondhand smoke is harmful. In both 1992 and 2000 surveys, more than 80% of respondents agreed with the statement that secondhand smoke was harmful. A 2001 study found that 95% of adults agreed that secondhand smoke was harmful to children, and 96% considered tobacco-industry claims that secondhand smoke was not harmful to be untruthful. <ref name="chapter10">. Accessed ] ].</ref><sup>, p. 588</sup> | |||
| ===Industry-funded studies and critiques=== | |||
| A 2007 ] found that 56% of respondents felt that secondhand smoke was "very harmful", a number that has held relatively steady since 1997. Another 29% believe that secondhand smoke is "somewhat harmful"; 10% answered "not too harmful", while 5% said "not at all harmful". | |||
| Regarding ]s, the poll found a majority (54%) in favor of complete smoking bans in restaurants; however, most respondents favored designated smoking areas in hotels, motels and workplaces. In bars, the survey found that 45% prefer smoking areas, 29% support a smoking ban, and 23% want no restrictions on smoking.<ref>{{cite web | title=Gallup Poll | url=http://www.gallup.com/poll/28216/.aspx}}</ref> | |||
| ====Enstrom and Kabat==== | |||
| ==Controversy over harms of passive smoking== | |||
| A 2003 study by ] and ], published in the '']'', argued that the harms of passive smoking had been overstated.<ref>{{cite journal |vauthors=Enstrom JE, Kabat GC |title=Environmental tobacco smoke and tobacco related mortality in a prospective study of Californians, 1960-98 |journal=BMJ |volume=326 |issue=7398 |page=1057 |year=2003 |pmid=12750205 |doi=10.1136/bmj.326.7398.1057 |pmc=155687 }}</ref> Their analysis reported no statistically significant relationship between passive smoking and lung cancer, coronary heart disease (CHD), or ], though the accompanying editorial noted that "they may overemphasise the negative nature of their findings."<ref>{{cite journal |author=Davey Smith G |title=Effect of passive smoking on health: More information is available, but the controversy still persists |journal=BMJ |volume=326 |issue=7398 |pages=1048–9 |year=2003 |pmid=12750182 |doi=10.1136/bmj.326.7398.1048 |pmc=1125974 }}</ref> This paper was widely promoted by the tobacco industry as evidence that the harms of passive smoking were unproven.<ref>{{harvnb|Kessler|2006|p=1383}}</ref><ref name="tong2007">{{cite journal |vauthors=Tong EK, Glantz SA |title=Tobacco industry efforts undermining evidence linking secondhand smoke with cardiovascular disease |journal=Circulation |volume=116 |issue=16 |pages=1845–54 |year=2007 |pmid=17938301 |doi=10.1161/CIRCULATIONAHA.107.715888 |s2cid=4021497 |doi-access=free }}</ref> The ] (ACS), whose database Enstrom and Kabat used to compile their data, criticized the paper as "neither reliable nor independent", stating that scientists at the ACS had repeatedly pointed out serious flaws in Enstrom and Kabat's methodology prior to publication.<ref name="acsresponse">{{cite press release |url = http://www.no-smoke.org/pdf/BMJrelease.pdf |title = American Cancer Society Condemns Tobacco Industry Study for Inaccurate Use of Data |publisher = ] |date = 2003-05-13 |access-date = 2007-08-29}}</ref> Notably, the study had failed to identify a comparison group of "unexposed" persons.<ref>{{cite journal |last1=Thun |first1=Michael J |title=More misleading science from the tobacco industry |journal=BMJ |date=4 October 2003 |volume=327 |issue=7418 |pages=E237–E238 |doi=10.1136/bmjusa.03070002 |s2cid=74351979 }}</ref> | |||
| Enstrom's ties to the tobacco industry also drew scrutiny; in a 1997 letter to ], Enstrom requested a "substantial research commitment... in order for me to effectively compete against the large mountain of epidemiologic data and opinions that already exist regarding the health effects of ETS and active smoking."<ref>{{cite web |url = http://legacy.library.ucsf.edu/tid/dfk37d00 |title = Proposed Research on the relationship of Low Levels of Active Smoking to Mortality: Letter from James Enstrom to Philip Morris Scientific Affairs office |date = 1997-01-01 |access-date = 2007-08-29}}</ref> In a ], the Enstrom and Kabat paper was cited by the US District Court as "a prime example of how nine tobacco companies engaged in criminal racketeering and fraud to hide the dangers of tobacco smoke."<ref name="nature-2007-review">{{cite journal |author=Dalton R |title=Passive-smoking study faces review |journal=Nature |volume=446 |issue=7133 |pages=242 |date=March 2007 |pmid=17361147 |doi=10.1038/446242a |bibcode=2007Natur.446..242D |s2cid=27691890 |doi-access=free }}</ref> The Court found that the study had been funded and managed by the ],<ref>{{harvnb|Kessler|2006|p=1380}}</ref> a tobacco industry ] tasked with "offsetting" damaging studies on passive smoking, as well as by Philip Morris who stated that Enstrom's work was "clearly litigation-oriented".<ref>{{harvnb|Kessler|2006|pp=1380–3}}</ref> A 2005 paper in ''Tobacco Control'' argued that the disclosure section in the Enstrom and Kabat BMJ paper, although it met the journal's requirements, "does not reveal the full extent of the relationship the authors had with the tobacco industry."<ref>{{cite journal|last1=Bero|first1=LA|last2=Glantz|first2=S|last3=Hong|first3=MK|title=The limits of competing interest disclosures |journal=Tobacco Control|date=April 2005|volume=14|issue=2|pages=118–26|pmid=15791022|pmc=1748015}}</ref> | |||
| In 1986, the ] issued a report concluding that secondhand smoke was a cause of disease. In the same year, the ] and the ] also released reports concluding that secondhand smoke was a cause of lung cancer.<ref>From , a report of the U.S. Surgeon General. See Executive Summary, p. 4. Accessed ] ].</ref> Over the subsequent 20 years, the accumulation of scientific evidence has led to a ] that passive smoking is indeed harmful to non-smokers.<ref>Currently the health risks of passive smoking are accepted by every major medical and scientific organization, as detailed elsewhere in this article. Specific descriptions of the development of scientific consensus on the topic can be found here: | |||
| *, on the release of the 2006 report on the harms of involuntary smoking. Delivered ] ]; accessed ] ]. | |||
| *, delivered by Judge Gladys Kessler. See p. 1406 & 1525 in particular. Accessed ] ]. | |||
| *. From a 2006 report by the U.S. Surgeon General. Page 577: "By 2000, there was little debate within the scientific community as to whether secondhand smoke causes diseases and other adverse health effects in children and adults."</ref> A ] found, in a ] case against the tobacco industry, that the industry had internally acknowledged the harmfulness of passive smoking even earlier.<ref name="kessler">, Final Opinion of Judge Gladys Kessler, United States District Court for the District of Columbia. Accessed ] ].</ref><sup>, pp. 1523–1525</sup> Nonetheless, the tobacco industry has played a central role in generating and sustaining controversy over the effects of passive smoking.<ref>According to the ]'s 2006 report on passive smoking, "The industry has funded or carried out research that has been judged to be biased, supported scientists to generate letters to editors that criticized research publications, attempted to undermine the findings of key studies... and attempted to sustain controversy even as the scientific community reached consensus." As quoted in the '']'': , by Marc Kaufman. Published ] ]; accessed ] ].</ref><ref name="whitecoat">. Accessed ] ].</ref><ref name="tong2007">{{cite journal |author=Tong EK, Glantz SA |title=Tobacco industry efforts undermining evidence linking secondhand smoke with cardiovascular disease |journal=Circulation |volume=116 |issue=16 |pages=1845–54 |year=2007 |pmid=17938301 |doi=10.1161/CIRCULATIONAHA.107.715888}}</ref> | |||
| In 2006, Enstrom and Kabat published a ] of studies regarding passive smoking and coronary heart disease in which they reported a very weak association between passive smoking and heart disease mortality.<ref>{{cite journal|last1=Enstrom|first1=JE|last2=Kabat|first2=GC|title=Environmental tobacco smoke and coronary heart disease mortality in the United States--a meta-analysis and critique |journal=Inhalation Toxicology|date=March 2006|volume=18|issue=3|pages=199–210|doi=10.1080/08958370500434255|pmid=16399662|citeseerx=10.1.1.495.2191|s2cid=7457133}}</ref> They concluded that exposure to secondhand smoke increased the risk of death from CHD by only 5%, although this analysis has been criticized for including two previous industry-funded studies that suffered from widespread exposure misclassification.<ref name=Circ07/> | |||
| === Critique of individual studies and epidemiology === | |||
| ====Gori==== | |||
| A number of studies funded by the tobacco industry have yielded results inconsistent with the scientific consensus, or have criticised the epidemiological approach associated with that consensus. | |||
| ], a tobacco industry spokesman and consultant<ref>{{harvnb|Kessler|2006|p=162}}</ref><ref>, United States Factual Memorandum Pursuant to Order No. 470, Section V, United States District Court for the District of Columbia. p. 44</ref><ref>, from the Legacy Tobacco Documents Archive. Retrieved July 19, 2007.</ref> and an expert on risk utility and scientific research, wrote in the ] ]'s magazine '']'' that "...of the 75 published studies of ETS and lung cancer, some 70% did not report statistically significant differences of risk and are moot. Roughly 17% claim an increased risk and 13% imply a reduction of risk."<ref>{{cite journal |author=Gori, Gio Batta |title=Stoking the Rigged Terror of Secondhand Smoke |journal=Regulation |volume=30 |issue=1 |pages=14–7 |date=Spring 2007 |url=http://www.cato.org/pubs/regulation/regv30n1/v30n1-5.pdf |url-status=dead |archive-url=https://web.archive.org/web/20090116012647/http://www.cato.org/pubs/regulation/regv30n1/v30n1-5.pdf |archive-date=2009-01-16 }}</ref> | |||
| ====Milloy==== | |||
| A 2003 study by Enstrom and Kabat, published in the '']'', argued that the harms of passive smoking had been overstated.<ref>{{cite journal |author=Enstrom JE, Kabat GC |title=Environmental tobacco smoke and tobacco related mortality in a prospective study of Californians, 1960-98 |journal=BMJ |volume=326 |issue=7398 |pages=1057 |year=2003 |pmid=12750205 |doi=10.1136/bmj.326.7398.1057}}</ref> Their analysis reported no statistically significant relationship between passive smoking and lung cancer, though the accompanying editorial noted that "they may overemphasise the negative nature of their findings."<ref>{{cite journal |author=Davey Smith G |title=Effect of passive smoking on health |journal=BMJ |volume=326 |issue=7398 |pages=1048–9 |year=2003 |pmid=12750182 |doi=10.1136/bmj.326.7398.1048}}</ref> This paper was widely promoted by the tobacco industry as evidence that the harms of passive smoking were unproven.<ref name="tong2007"/><ref name="kessler"/><sup>, p. 1383</sup> The ] (ACS), whose database Enstrom and Kabat used to compile their data, criticized the paper as "neither reliable nor independent", stating that scientists at the ACS had repeatedly pointed out serious flaws in Enstrom and Kabat' s methodology prior to publication.<ref name="acsresponse">: A press release from the ]. Dated ] ]; accessed ] ].</ref> Enstrom's ties to the tobacco industry also drew scrutiny; in a 1997 letter to ], Enstrom requested a "substantial research commitment... in order for me to effectively compete against the large mountain of epidemiologic data and opinions that already exist regarding the health effects of ETS and active smoking."<ref>: Letter from James Enstrom to Philip Morris Scientific Affairs office, dated ] ]. Accessed ] ].</ref> The study was funded and managed by the Center for Indoor Air Research, a tobacco industry ] described in confidential Philip Morris documents as "responsible for producing studies to offset the IARC study" on passive smoking,<ref> Legacy Tobacco Documents Library</ref> and Enstrom's work was viewed by Philip Morris as "clearly litigation-oriented."<ref name="kessler"/><sup>, pp. 1380–1383</sup> Enstrom himself has defended the accuracy of his study against what he terms "illegitimate criticism by those who have attempted to suppress and discredit it."<ref>{{cite journal |author=Enstrom JE |title=Defending legitimate epidemiologic research: combating Lysenko pseudoscience |journal=Epidemiol Perspect Innov|volume=4 |issue=1 |pages=11 |year=2007 |pmid=17927827 |doi=10.1186/1742-5573-4-11}}</ref> | |||
| ], the "]" commentator for ] and a former ] consultant,<ref>, by Paul D. Thacker. Published in '']'' on January 26, 2006. Retrieved August 22, 2007.</ref><ref>, listing Milloy as a paid consultant. Retrieved August 22, 2007.</ref> claimed that "of the 19 studies" on passive smoking "only 8— slightly more than 42%— reported statistically significant increases in heart disease incidence."<ref>, by ]. Retrieved May 31, 2013.</ref> | |||
| Another component of criticism cited by Milloy focused on ] and epidemiological practices in studies of passive smoking. Milloy, who has a master's degree from the Johns Hopkins School of Hygiene and Public Health, argued that studies yielding relative risks of less than 2 were meaningless junk science. This approach to epidemiological analysis was criticized in the '']'': | |||
| ], a tobacco industry consultant and spokeperson,<ref>, from the Legacy Tobacco Documents Archive. Accessed ] ].</ref> wrote in the ] ]'s journal ''Regulation'' that "...of the 75 published studies of ETS and lung cancer, some 70 percent did not report statistically significant differences of risk and are moot. Roughly 17 percent claim an increased risk and 13 percent imply a reduction of risk."<ref> www.cato.org/pubs/regulation/regv30n1/v30n1-5.pdf </ref> ], the "]" commentator for ] and a former ] consultant,<ref>, by Paul D. Thacker. Published in '']'' on ] ]; accessed ] ].</ref><ref>, listing Milloy as a paid consultant. Accessed ] ].</ref> claimed that "...of the 37 studies , only 7 – less than 19 percent – reported statistically significant increases in lung cancer incidence."<ref>, by ]. Accessed ] ].</ref> | |||
| {{blockquote|A major component of the industry attack was the mounting of a campaign to establish a "bar" for "sound science" that could not be fully met by most individual investigations, leaving studies that did not meet the criteria to be dismissed as "junk science."<ref>{{cite journal |vauthors=Samet JM, Burke TA |title=Turning Science Into Junk: The Tobacco Industry and Passive Smoking |journal=Am J Public Health |volume=91 |issue=11 |pages=1742–4 |year=2001 |pmid=11684591 |doi=10.2105/AJPH.91.11.1742 |pmc=1446866 }}</ref>}} | |||
| Another component of criticism promoted by Milloy focused on ] and epidemiological practices in studies of passive smoking. Milloy argued that studies yielding relative risks of less than 2 were meaningless ]. This approach to epidemiological analysis was criticized in the '']'': | |||
| <blockquote>A major component of the industry attack was the mounting of a campaign to establish a "bar" for "sound science" that could not be fully met by most individual investigations, leaving studies that did not meet the criteria to be dismissed as "junk science."<ref>{{cite journal |author=Samet JM, Burke TA |title=Turning science into junk: the tobacco industry and passive smoking |journal=American journal of public health |volume=91 |issue=11 |pages=1742–4 |year=2001 |pmid=11684591 |doi=}}</ref></blockquote> | |||
| The tobacco industry and affiliated scientists also put forward a set of "Good Epidemiology Practices" which would have the practical effect of obscuring the link between secondhand smoke and lung cancer; the privately |
The tobacco industry and affiliated scientists also put forward a set of "Good Epidemiology Practices" which would have the practical effect of obscuring the link between secondhand smoke and lung cancer; the privately stated goal of these standards was to "impede adverse legislation".<ref>{{dead link|date=March 2018 |bot=InternetArchiveBot |fix-attempted=yes }}, from the Philip Morris document archive. Retrieved October 3, 2007. Also cited in {{cite journal |last1=Ong |first1=Elisa K. |last2=Glantz |first2=Stanton A. |title=Constructing 'Sound Science' and 'Good Epidemiology': Tobacco, Lawyers, and Public Relations Firms |journal=American Journal of Public Health |date=November 2001 |volume=91 |issue=11 |pages=1749–1757 |doi=10.2105/ajph.91.11.1749 |pmid=11684593 |pmc=1446868 }}</ref> However, this effort was largely abandoned when it became clear that no independent epidemiological organization would agree to the standards proposed by Philip Morris et al.<ref name="pmid11684593">{{cite journal |vauthors=Ong EK, Glantz SA |title=Constructing "Sound Science" and "Good Epidemiology": Tobacco, Lawyers, and Public Relations Firms |journal=Am J Public Health |volume=91 |issue=11 |pages=1749–57 |year=2001 |pmid=11684593 |doi=10.2105/AJPH.91.11.1749 |pmc=1446868 }}</ref> | ||
| === |
==== Levois and Layard ==== | ||
| In 1995, Levois and Layard, both tobacco industry consultants, published two analyses in the journal '']'' regarding the association between spousal exposure to secondhand smoke and heart disease. Both of these papers reported no association between secondhand smoke and heart disease.<ref>{{cite journal |last1=Layard |first1=M.W. |title=Ischemic Heart Disease and Spousal Smoking in the National Mortality Followback Survey |journal=Regulatory Toxicology and Pharmacology |date=February 1995 |volume=21 |issue=1 |pages=180–183 |doi=10.1006/rtph.1995.1022 |pmid=7784629 }}</ref><ref>{{cite journal |last1=Levois |first1=M.E. |last2=Layard |first2=M.W. |title=Publication Bias in the Environmental Tobacco Smoke/Coronary Heart Disease Epidemiologic Literature |journal=Regulatory Toxicology and Pharmacology |date=February 1995 |volume=21 |issue=1 |pages=184–191 |doi=10.1006/rtph.1995.1023 |pmid=7784630 }}</ref> These analyses have been criticized for failing to distinguish between current and former smokers, despite the fact that former smokers, unlike current ones, are not at a significantly increased risk of heart disease.<ref name=Circ07/><ref>{{cite journal |last1=Law |first1=Malcolm R |last2=Wald |first2=Nicholas J |title=Environmental tobacco smoke and ischemic heart disease |journal=Progress in Cardiovascular Diseases |date=July 2003 |volume=46 |issue=1 |pages=31–38 |doi=10.1016/s0033-0620(03)00078-1 |pmid=12920699 }}</ref> | |||
| ==== World Health Organization controversy ==== | |||
| A 1998 report by the ] (IARC) on environmental tobacco smoke (ETS) found "weak evidence of a dose-response relationship between risk of lung cancer and exposure to spousal and workplace ETS."<ref>{{cite journal |author=Boffetta P, Agudo A, Ahrens W, ''et al'' |title=Multicenter case-control study of exposure to environmental tobacco smoke and lung cancer in Europe |journal=J. Natl. Cancer Inst. |volume=90 |issue=19 |pages=1440–50 |year=1998 |pmid=9776409|doi=10.1093/jnci/90.19.1440}}</ref> | |||
| A 1998 study by the ] (IARC) on environmental tobacco smoke (ETS) found "weak evidence of a ] between risk of lung cancer and exposure to spousal and workplace ETS."<ref name="environmental1440">{{cite journal |last1=Boffetta |first1=Paolo |last2=Agudo |first2=Antonio |last3=Ahrens |first3=Wolfgang |last4=Benhamou |first4=Ellen |last5=Benhamou |first5=Simone |last6=Darby |first6=Sarah C. |last7=Ferro |first7=Gilles |last8=Fortes |first8=Cristina |last9=Gonzalez |first9=Carlos A. |last10=Jöckel |first10=Karl-Heinz |last11=Krauss |first11=Martin |last12=Kreienbrock |first12=Lothar |last13=Kreuzer |first13=Michaela |last14=Mendes |first14=Anabela |last15=Merletti |first15=Franco |last16=Nyberg |first16=Fredrik |last17=Pershagen |first17=Göran |last18=Pohlabeln |first18=Hermann |last19=Riboli |first19=Elio |last20=Schmid |first20=Giovanni |last21=Simonato |first21=Lorenzo |last22=Tre'daniel |first22=Jean |last23=Whitley |first23=Elise |last24=Wichmann |first24=Heinz-Erich |last25=Winck |first25=Carlos |last26=Zambon |first26=Paola |last27=Saracci |first27=Rodolfo |title=Multicenter Case-Control Study of Exposure to Environmental Tobacco Smoke and Lung Cancer in Europe |journal=JNCI: Journal of the National Cancer Institute |date=7 October 1998 |volume=90 |issue=19 |pages=1440–1450 |doi=10.1093/jnci/90.19.1440 |pmid=9776409 |doi-access=free }}</ref> | |||
| In March of 1998, before the study was published, reports appeared in the media alleging that the IARC and the ] (WHO) were suppressing information. The reports, appearing in the British '']''<ref>{{cite web | title=Passive Smoking Doesn't Cause Cancer —Official | url=http://tobaccodocuments.org/pm/2063594041-4042.html}}</ref> and '']'',<ref>{{cite web |title=Smokescreens - The World Health Organization is showing signs of allowing politics to get in the way of truth. The Economist March 14th, 1998 | url=http://ltdlimages.library.ucsf.edu/imagesv/v/d/m/vdm97d00/Svdm97d00.pdf}}</ref> among other sources,<ref>Le Grand C. Anti-smokers blown away by study. Australian 1998, March 10.</ref><ref>WHO Rejects smoking link with lung cancer. Zimbabwe Independent 1998, Oct 23.</ref><ref>No Link Between Passive Smoking and Lung Cancer. ] 1998, March 9.</ref> alleged that the WHO withheld from publication its own report that supposedly failed to prove an association between passive smoking and a number of other diseases (lung cancer in particular). | |||
| In March 1998, before the study was published, reports appeared in the media alleging that the IARC and the ] (WHO) were suppressing information. The reports, appearing in the British '']''<ref>{{cite web |title=Passive Smoking Doesn't Cause Cancer —Official |url=http://tobaccodocuments.org/pm/2063594041-4042.html |url-status=dead |archive-url=https://web.archive.org/web/20071013185243/http://tobaccodocuments.org/pm/2063594041-4042.html |archive-date=2007-10-13 }}</ref> and '']'',<ref>{{cite web|title=Smokescreens – The World Health Organization is showing signs of allowing politics to get in the way of truth. The Economist March 14th, 1998|url=http://ltdlimages.library.ucsf.edu/imagesv/v/d/m/vdm97d00/Svdm97d00.pdf|url-status=dead|archive-url=https://web.archive.org/web/20071129085456/http://ltdlimages.library.ucsf.edu/imagesv/v/d/m/vdm97d00/Svdm97d00.pdf|archive-date=2007-11-29}}</ref> among other sources,<ref>Le Grand C. Anti-smokers blown away by study. Australian 1998, March 10.</ref><ref>WHO Rejects smoking link with lung cancer. Zimbabwe Independent 1998, Oct 23.</ref><ref>No Link Between Passive Smoking and Lung Cancer. ] 1998, March 9.</ref> alleged that the WHO withheld from publication of its own report that supposedly failed to prove an association between passive smoking and a number of other diseases (lung cancer in particular). | |||
| In response, the WHO issued a press release stating that the results of the study had been "completely misrepresented" in the popular press and were in fact very much in line with similar studies demonstrating the harms of passive smoking.<ref>{{cite web | title=Passive Smoking Does Cause Lung Cancer, Do Not Let Them Fool You | url=http://www.who.int/inf-pr-1998/en/pr98-29.html}}</ref> The study was published in the ''Journal of the National Cancer Institute'' in October of the same year. An accompanying editorial summarized: | |||
| In response, the WHO issued a press release stating that the results of the study had been "completely misrepresented" in the popular press and were in fact very much in line with similar studies demonstrating the harms of passive smoking.<ref>{{cite journal |title=Passive smoking does cause lung cancer, do not let them fool you |journal=The Ceylon Medical Journal |date=June 1998 |volume=43 |issue=2 |pages=98 |pmid=9704550 }}</ref> The study was published in the ''Journal of the National Cancer Institute'' in October of the same year, and concluded the authors found "no association between childhood exposure to ETS and lung cancer risk" but "did find weak evidence of a dose–response relationship between risk of lung cancer and exposure to spousal and workplace ETS."<ref name="environmental1440"/> An accompanying editorial summarized: | |||
| <blockquote>When all the evidence, including the important new data reported in this issue of the Journal, is assessed, the inescapable scientific conclusion is that ETS is a low-level lung carcinogen.<ref>{{cite journal |author=Blot WJ, McLaughlin JK |title=Passive smoking and lung cancer risk: what is the story now? |journal=J. Natl. Cancer Inst. |volume=90 |issue=19 |pages=1416–7 |year=1998 |pmid=9776401|doi=10.1093/jnci/90.19.1416}}</ref></blockquote> | |||
| {{blockquote|When all the evidence, including the important new data reported in this issue of the Journal, is assessed, the inescapable scientific conclusion is that ETS is a low-level lung carcinogen.<ref>{{cite journal |last1=Blot |first1=William J. |last2=McLaughlin |first2=Joseph K. |title=Passive Smoking and Lung Cancer Risk: What Is the Story Now? |journal=JNCI: Journal of the National Cancer Institute |date=7 October 1998 |volume=90 |issue=19 |pages=1416–1417 |doi=10.1093/jnci/90.19.1416 |pmid=9776401 |doi-access=free }}</ref>}} | |||
| With the release of formerly classified tobacco industry documents through the ], it was found that the controversy over the WHO's alleged suppression of data had been engineered by ], ], and other tobacco companies in an effort to discredit scientific findings which would harm their business interests.<ref>{{cite journal |author=Ong EK, Glantz SA |title=Tobacco industry efforts subverting International Agency for Research on Cancer's second-hand smoke study |journal=Lancet |volume=355 |issue=9211 |pages=1253–9 |year=2000 |pmid=10770318 |doi=10.1016/S0140-6736(00)02098-5}}</ref> A WHO inquiry, conducted after the release of the tobacco-industry documents, found that this controversy was generated by the tobacco industry as part of its larger campaign to cut the WHO's budget, distort the results of scientific studies on passive smoking, and discredit the WHO as an institution. This campaign was carried out using a network of ostensibly independent ] and international and scientific experts with hidden financial ties to the industry.<ref>{{cite web | title=Tobacco Companies Strategies to Undermine Tobacco Control Activities at the World Health Organization | url=http://www.who.int/tobacco/media/en/who_inquiry.pdf}}</ref> | |||
| With the release of formerly classified tobacco industry documents through the ], it was found (by Elisa Ong and ]) that the controversy over the WHO's alleged suppression of data had been engineered by ], ], and other tobacco companies in an effort to discredit scientific findings which would harm their business interests.<ref name="ong-glantz-2000">{{cite journal |vauthors=Ong EK, Glantz SA |title=Tobacco industry efforts subverting International Agency for Research on Cancer's second-hand smoke study |journal=Lancet |volume=355 |issue=9211 |pages=1253–9 |year=2000 |pmid=10770318 |doi=10.1016/S0140-6736(00)02098-5 |s2cid=25145666 }}</ref> A WHO inquiry, conducted after the release of the tobacco-industry documents, found that this controversy was generated by the tobacco industry as part of its larger campaign to cut the WHO's budget, distort the results of scientific studies on passive smoking, and discredit the WHO as an institution. This campaign was carried out using a network of ostensibly independent ] and international and scientific experts with hidden financial ties to the industry.<ref>{{cite web|title=Tobacco Companies Strategies to Undermine Tobacco Control Activities at the World Health Organization|url=https://www.who.int/tobacco/media/en/who_inquiry.pdf|archive-url=http://webarchive.loc.gov/all/20040821060747/http://www.who.int/tobacco/media/en/who_inquiry.pdf|url-status=dead|archive-date=2004-08-21|access-date=2008-12-30}}</ref> | |||
| ===EPA lawsuit=== | |||
| In 1993, the ] (EPA) issued a report estimating that 3,000 lung cancer related deaths in the ] were caused by passive smoking annually.<ref name="EPA report"/> | |||
| ], ], and groups representing growers, distributors and marketers of tobacco took legal action, claiming that the EPA had manipulated this study and ignored accepted scientific and statistical practices. | |||
| ==== EPA lawsuit ==== | |||
| The ] ruled in favor of the tobacco industry in 1998, finding that the EPA had failed to follow proper scientific and epidemiologic practices and had "cherry picked" evidence to support conclusions which they had committed to in advance.<ref>{{cite web | title=The Osteen Decision | url=http://www.tobacco.org/Documents/980717osteen.html}}</ref> The court stated in part, "“EPA publicly committed to a conclusion before research had begun…adjusted established procedure and scientific norms to validate the Agency's public conclusion... In conducting the ETS Risk Assessment, disregarded information and made findings on selective information; did not disseminate significant epidemiologic information; deviated from its Risk Assessment Guidelines; failed to disclose important findings and reasoning…" | |||
| In 1993, the ] (EPA) issued a report estimating that 3,000 lung cancer related deaths in the ] were caused by passive smoking annually.<ref name="EPA report">US Environmental Protection Agency. {{cite web|url= http://oaspub.epa.gov/eims/eimscomm.getfile?p_download_id=36793 |title=Respiratory health effects of passive smoking: Lung cancer and other disorders }}</ref> | |||
| ], ], and groups representing growers, distributors and marketers of tobacco took legal action, claiming that the EPA had manipulated this study and ignored accepted scientific and statistical practices. | |||
| In 2002, the EPA successfully appealed this decision to the ]. The EPA's appeal was upheld on the preliminary grounds that their report had no regulatory weight, and the earlier finding was vacated.<ref>{{cite web | title=Flue-Cured Tobacco Cooperative vs. EPA | url=http://pacer.ca4.uscourts.gov/opinion.pdf/982407.P.pdf}}</ref> | |||
| In 1998 the U.S. Department of Health and Human Services, through the publication by its National Toxicology Program of the 9th Report on Carcinogens, listed environmental tobacco smoke among the known carcinogens, observing of the EPA assessment that "The individual studies were carefully summarized and evaluated."<ref> {{Citation| first= | last=| coauthors=| contribution=Final Report on Carcinogens - Background Document for Environmental Tobacco Smoke| title=Meeting of the NTP Board of Scientific Counselors - Report on Carcinogens Subcommittee| editor-first=U.S. Department of Health and Human Services, National Toxicology Program| editor-last=| coeditors=| publisher=| place=Research Triangle Park, North Carolina| pages=| date=December 2-3, 1998| year=1998| id= | contribution-url=http://ntp.niehs.nih.gov/files/EnvironmentalTS.pdf| format=| accessdate= }}</ref><sup>p. 24</sup> | |||
| The ] ruled in favor of the tobacco industry in 1998, finding that the EPA had failed to follow proper scientific and epidemiologic practices and had "cherry picked" evidence to support conclusions which they had committed to in advance.<ref>{{cite web |title=The Osteen Decision |url=http://www.tobacco.org/Documents/980717osteen.html |archive-url=https://web.archive.org/web/20000815224937/http://www.tobacco.org/Documents/980717osteen.html |url-status=dead |archive-date=2000-08-15 }}</ref> The court stated in part, "EPA publicly committed to a conclusion before research had begun...adjusted established procedure and scientific norms to validate the Agency's public conclusion... In conducting the ETS Risk Assessment, disregarded information and made findings on selective information; did not disseminate significant epidemiologic information; deviated from its Risk Assessment Guidelines; failed to disclose important findings and reasoning..." | |||
| ===Tobacco-industry funding of research=== | |||
| The tobacco industry's role in funding scientific research on passive smoking has been controversial.<ref>{{cite journal |author=Thun MJ |title=Passive smoking: tobacco industry publishes disinformation |journal=BMJ |volume=327 |issue=7413 |pages=502–3; author reply 504–5 |year=2003 |pmid=12946979 |doi=10.1136/bmj.327.7413.502-c}}</ref> A review of published studies found that tobacco-industry affilation was strongly correlated with findings exonerating passive smoking; researchers affiliated with the tobacco industry were 88 times more likely than independent researchers to conclude that passive smoking was not harmful.<ref name="pmid9605902">{{cite journal |author=Barnes DE, Bero LA |title=Why review articles on the health effects of passive smoking reach different conclusions |journal=JAMA |volume=279 |issue=19 |pages=1566–70 |year=1998 |pmid=9605902|doi=10.1001/jama.279.19.1566}}</ref> In a specific example which came to light with the release of tobacco-industry documents, Philip Morris executives successfully encouraged an author to revise his industry-funded review article to downplay the role of secondhand smoke in ].<ref>{{cite journal |author=Tong EK, England L, Glantz SA |title=Changing conclusions on secondhand smoke in a sudden infant death syndrome review funded by the tobacco industry |journal=Pediatrics |volume=115 |issue=3 |pages=e356–66 |year=2005 |pmid=15741361 |doi=10.1542/peds.2004-1922}}</ref> The 2006 U.S. Surgeon General's report criticized the tobacco industry's role in the scientific debate: | |||
| In 2002, the EPA successfully appealed this decision to the ]. The EPA's appeal was upheld on the preliminary grounds that their report had no regulatory weight, and the earlier finding was vacated.<ref>{{cite web|title=Flue-Cured Tobacco Cooperative vs. EPA|url=http://pacer.ca4.uscourts.gov/opinion.pdf/982407.P.pdf|access-date=2008-12-30|url-status=dead|archive-url=https://web.archive.org/web/20081009020709/http://pacer.ca4.uscourts.gov/opinion.pdf/982407.P.pdf|archive-date=2008-10-09}}</ref> | |||
| <blockquote>The industry has funded or carried out research that has been judged to be biased, supported scientists to generate letters to editors that criticized research publications, attempted to undermine the findings of key studies, assisted in establishing a scientific society with a journal, and attempted to sustain controversy even as the scientific community reached consensus.<ref>; see p. 21.</ref></blockquote> | |||
| In 1998, the U.S. Department of Health and Human Services, through the publication by its National Toxicology Program of the 9th Report on Carcinogens, listed environmental tobacco smoke among the known carcinogens, observing of the EPA assessment that "The individual studies were carefully summarized and evaluated."<ref>{{cite book |contribution=Final Report on Carcinogens – Background Document for Environmental Tobacco Smoke |title=Meeting of the NTP Board of Scientific Counselors – Report on Carcinogens Subcommittee |editor1=U.S. Department of Health |editor2=Human Services |editor3=National Toxicology Program |location=Research Triangle Park, North Carolina |date=December 2–3, 1998 |url=https://ntp.niehs.nih.gov/ntp/newhomeroc/other_background/tobacco_smoking1_2apps_508.pdf |page=24 |archive-url=https://web.archive.org/web/20071129085500/http://ntp.niehs.nih.gov/files/EnvironmentalTS.pdf |archive-date=2007-11-29 }}</ref> | |||
| This strategy was outlined at an international meeting of tobacco companies in 1988, at which Philip Morris proposed to set up a team of scientists, organized by company lawyers, to "carry out work on ETS to keep the controversy alive."<ref name="whitecoat"/> All scientific research was subject to oversight and "filtering" by tobacco-industry lawyers: | |||
| ==== Tobacco-industry funding of research ==== | |||
| <blockquote>Philip Morris then expect the group of scientists to operate within the confines of decisions taken by PM scientists to determine the general direction of research, which apparently would then be 'filtered' by lawyers to eliminate areas of sensitivity.<ref name="whitecoat"/></blockquote> | |||
| The tobacco industry's role in funding scientific research on secondhand smoke has been controversial.<ref>{{cite journal |author=Thun MJ |title=Passive smoking: Tobacco industry publishes disinformation |journal=BMJ |volume=327 |issue=7413 |pages=502–3; author reply 504–5 |year=2003 |pmid=12946979 |doi=10.1136/bmj.327.7413.502-c |pmc=188400 }}</ref> A review of published studies found that tobacco-industry affiliation was strongly correlated with findings exonerating secondhand smoke; researchers affiliated with the tobacco industry were 88 times more likely than independent researchers to conclude that secondhand smoke was not harmful.<ref name="pmid9605902">{{cite journal |vauthors=Barnes DE, Bero LA |title=Why review articles on the health effects of passive smoking reach different conclusions |journal=JAMA |volume=279 |issue=19 |pages=1566–70 |year=1998 |pmid=9605902|doi=10.1001/jama.279.19.1566 }}</ref> In a specific example which came to light with the release of tobacco-industry documents, Philip Morris executives successfully encouraged an author to revise his industry-funded review article to downplay the role of secondhand smoke in ].<ref>{{cite journal |vauthors=Tong EK, England L, Glantz SA |title=Changing conclusions on secondhand smoke in a sudden infant death syndrome review funded by the tobacco industry |journal=Pediatrics |volume=115 |issue=3 |pages=e356–66 |year=2005 |pmid=15741361 |doi=10.1542/peds.2004-1922 |s2cid=33226933 |doi-access=free }}</ref> The 2006 U.S. Surgeon General's report criticized the tobacco industry's role in the scientific debate: | |||
| {{blockquote|The industry has funded or carried out research that has been judged to be biased, supported scientists to generate letters to editors that criticized research publications, attempted to undermine the findings of key studies, assisted in establishing a scientific society with a journal, and attempted to sustain controversy even as the scientific community reached consensus.<ref>{{cite web |title = The Health Consequences of Involuntary Exposure to Tobacco Smoke |publisher = ] |website = Executive Summary |year = 2006 |access-date =2009-01-28 |url = http://www.surgeongeneral.gov/library/secondhandsmoke/report/executivesummary.pdf |page=21}}</ref>}} | |||
| This strategy was outlined at an international meeting of tobacco companies in 1988, at which Philip Morris proposed to set up a team of scientists, organized by company lawyers, to "carry out work on ETS to keep the controversy alive."<ref name="whitecoat">{{cite web |url = http://tobaccodocuments.org/landman/2063791182-1187.html |title = Minutes of a meeting of Philip Morris with British tobacco companies to discuss tobacco-industry strategy on passive smoking |access-date = 2007-08-27 |url-status = dead |archive-url = https://web.archive.org/web/20071013185238/http://tobaccodocuments.org/landman/2063791182-1187.html |archive-date = 2007-10-13 }}</ref> All scientific research was subject to oversight and "filtering" by tobacco-industry lawyers: | |||
| {{blockquote | |||
| |Philip Morris then expect the group of scientists to operate within the confines of decisions taken by PM scientists to determine the general direction of research, which apparently would then be 'filtered' by lawyers to eliminate areas of sensitivity.<ref name="whitecoat"/> | |||
| }} | |||
| Philip Morris reported that it was putting "...vast amounts of funding into these projects... in attempting to coordinate and pay so many scientists on an international basis to keep the ETS controversy alive."<ref name="whitecoat"/> | Philip Morris reported that it was putting "...vast amounts of funding into these projects... in attempting to coordinate and pay so many scientists on an international basis to keep the ETS controversy alive."<ref name="whitecoat"/> | ||
| ==Tobacco industry response== | ===Tobacco industry response=== | ||
| Measures to tackle secondhand smoke pose a serious economic threat to the tobacco industry, having broadened the definition of smoking beyond a personal habit to something with a social impact. In a confidential 1978 report, the tobacco industry described increasing public concerns about secondhand smoke as "the most dangerous development to the viability of the tobacco industry that has yet occurred."<ref>, produced for the Tobacco Institute and released under the terms of the ].</ref> In ''United States of America v. Philip Morris et al.'', the District Court for the District of Columbia found that the tobacco industry "... recognized from the mid-1970s forward that the health effects of passive smoking posed a profound threat to industry viability and cigarette profits," and that the industry responded with "efforts to undermine and discredit the scientific consensus that ETS causes disease."<ref name="kessler"/> | |||
| Accordingly, the tobacco industry have developed several strategies to |
Accordingly, the tobacco industry have developed several strategies to minimise the impact on their business: | ||
| * The industry has sought to position the secondhand smoke debate as essentially concerned with civil liberties and ] rather than with health, by funding groups such as ].<ref name="voice-smoker">{{cite journal |last1=Smith |first1=E. A. |last2=Malone |first2=R. E. |title='We will speak as the smoker': the tobacco industry's smokers' rights groups |journal=The European Journal of Public Health |date=5 January 2007 |volume=17 |issue=3 |pages=306–313 |doi=10.1093/eurpub/ckl244 |pmid=17065174 |pmc=2794244 }}</ref> | |||
| * ] in research;<ref name="smoke-screen"/> in all reviews of the effects of secondhand smoke on health published between 1980 and 1995, the only factor associated with concluding that secondhand smoke is not harmful was whether an author was affiliated with the tobacco industry.<ref name="pmid9605902"/> However, not all studies that failed to find evidence of harm were by industry-affiliated authors. | |||
| * Delaying and discrediting legitimate research (see<ref name="smoke-screen"/> for an example of how the industry attempted to discredit ]'s landmark study, and<ref>{{cite journal |vauthors=Trotter L, Chapman S |title="Conclusions about exposure to ETS and health that will be unhelpful to us"*: How the tobacco industry attempted to delay and discredit the 1997 Australian National Health and Medical Research Council report on passive smoking |journal=Tob Control |volume=12 |issue=Suppl 3:iii |pages=102–6 |year=2003 |pmid=14645955 |doi=10.1136/tc.12.suppl_3.iii102 |pmc=1766130 }}</ref> for an example of how it attempted to delay and discredit a major Australian report on passive smoking) | |||
| * Promoting "good epidemiology" and attacking so-called ] (a term popularised by industry lobbyist ]): attacking the methodology behind research showing health risks as flawed and attempting to promote ]. Ong & Glantz (2001) cite an internal Phillip Morris memo giving evidence of this as company policy.<ref name="pmid11684593"/> | |||
| * Creation of outlets for favourable research. In 1989, the tobacco industry established the International Society of the Built Environment, which published the ] journal ''Indoor and Built Environment''. This journal did not require conflict-of-interest disclosures from its authors. With documents made available through the ], it was found that the executive board of the society and the editorial board of the journal were dominated by paid tobacco-industry consultants. The journal published a large amount of material on passive smoking, much of which was "industry-positive".<ref>{{cite journal |vauthors=Garne D, Watson M, Chapman S, Byrne F |title=Environmental tobacco smoke research published in the journal Indoor and Built Environment and associations with the tobacco industry |journal=Lancet |volume=365 |issue=9461 |pages=804–9 |year=2005 |pmid=15733724 |doi=10.1016/S0140-6736(05)17990-2 |s2cid=23160158 }}</ref> | |||
| Citing the tobacco industry's production of biased research and efforts to undermine scientific findings, the 2006 U.S. Surgeon General's report concluded that the industry had "attempted to sustain controversy even as the scientific community reached consensus... industry documents indicate that the tobacco industry has engaged in widespread activities... that have gone beyond the bounds of accepted scientific practice."<ref name="sg-exec-summary"/> The U.S. District Court, in ''U.S.A. v. Philip Morris et al.'', found that "...despite their internal acknowledgment of the hazards of secondhand smoke, Defendants have fraudulently denied that ETS causes disease."<ref>{{harvnb|Kessler|2006|p=1523}}</ref> | |||
| * ]: the industry has sought to position the passive smoking debate as essentially concerned with civil liberties and smokers' ] rather than with health.{{Fact|date=August 2007}} | |||
| * Funding bias in research; in all reviews of the effects of passive smoking on health published between 1980 and 1995, the only factor associated with concluding that passive smoking is not harmful was whether an author was affiliated with the tobacco industry.<ref name="pmid9605902"/> | |||
| * Delaying and discrediting legitimate research: Australia<ref>{{cite journal | author=Trotter L, Chapman S | title="Conclusions about exposure to ETS and health that will be unhelpful to us": how the tobacco industry attempted to delay and discredit the 1997 Australian National Health and Medical Research Council report on passive smoking. | journal=Tob Control | volume=12 | issue=Suppl 3:iii | pages=102–6 | year=2003 | pmid=14645955 | doi=10.1136/tc.12.suppl_3.iii102}}</ref> | |||
| * Promoting "good epidemiology" and attacking so-called ] (a term popularised by industry lobbyist ]): attacking the methodology behind research showing health risks as flawed and attempting to promote ] . Ong & Glantz (2001) cite an internal Phillip Morris memo giving evidence of this as company policy<ref name="pmid11684593"/> | |||
| *Creation of outlets for favorable research. In 1989, the tobacco industry established the International Society of the Built Environment, which published the ] journal ''Indoor and Built Environment''. This journal did not require conflict-of-interest disclosures from its authors. With documents made available through the ], it was found that the executive board of the society and the editorial board of the journal were dominated by paid tobacco-industry consultants. The journal published a large amount of material on passive smoking, much of which was "industry-positive".<ref>{{cite journal |author=Garne D, Watson M, Chapman S, Byrne F |title=Environmental tobacco smoke research published in the journal Indoor and Built Environment and associations with the tobacco industry |journal=Lancet |volume=365 |issue=9461 |pages=804–9 |year=2005 |pmid=15733724 |doi=10.1016/S0140-6736(05)17990-2}}</ref> | |||
| ==== Position of major tobacco companies ==== | |||
| Citing the tobacco industry's production of biased research and efforts to undermine scientific findings, the 2006 U.S. Surgeon General's report concluded that the industry had "attempted to sustain controversy even as the scientific community reached consensus... industry documents indicate that the tobacco industry has engaged in widespread activities... that have gone beyond the bounds of accepted scientific practice."<ref>, 2006.</ref> The U.S. District Court, in ''U.S.A. v. Philip Morris et al.'', found that "...despite their internal acknowledgment of the hazards of secondhand smoke, Defendants have fraudulently denied that ETS causes disease."<ref name="kessler"/><sup>, p. 1523</sup> | |||
| The positions of major tobacco companies on the issue of secondhand smoke is somewhat varied. In general, tobacco companies have continued to focus on questioning the methodology of studies showing that secondhand smoke is harmful. Some (such as ] and ]) acknowledge the medical consensus that secondhand smoke carries health risks, while others continue to assert that the evidence is inconclusive. Several tobacco companies advocate the creation of smoke-free areas within public buildings as an alternative to comprehensive ].<ref>The most current positions of major tobacco companies on the issue of passive smoking can be found on their websites. As of 13 January 2009, the following websites contain tobacco-industry positions on the topic: | |||
| * ]: | |||
| * ]: {{cite web |title=Imperial Tobacco Group PLC - Media - Our view - Smoking and health - Environmental tobacco smoke |url=http://www.imperial-tobacco.com/index.asp?page=82 |url-status=dead |archive-url=https://web.archive.org/web/20090116015146/http://www.imperial-tobacco.com/index.asp?page=82 |archive-date=2009-01-16 |access-date=2008-10-25}} | |||
| * ]: {{Webarchive|url=https://web.archive.org/web/20101006025905/http://www.philipmorrisusa.com/en/cms/Products/Cigarettes/Health_Issues/Secondhand_Smoke/default.aspx|date=2010-10-06}} and | |||
| * ]: {{cite web |title=R.J. Reynolds Tobacco Company - Smoking & Health - Summary of Opinions |url=http://www.rjrt.com/smoking/summaryCover.asp |url-status=dead |archive-url=https://web.archive.org/web/20061118145334/http://www.rjrt.com/smoking/summaryCover.asp |archive-date=2006-11-18 |access-date=2006-11-19}}</ref> | |||
| === |
=== US racketeering lawsuit against tobacco companies === | ||
| On September 22, 1999, the ] filed a ] lawsuit against Philip Morris and other major cigarette manufacturers.<ref> U.S. Department of Justice</ref> Almost 7 years later, on August 17, 2006, U.S. District Court Judge ] found that the Government had proven its case and that the tobacco company defendants had violated the ].<ref name="kessler" /> In particular, Judge Kessler found that PM and other tobacco companies had: | |||
| '''''' (site accessed on November 19, 2006)<br /> | |||
| * conspired to minimize, distort and confuse the public about the health hazards of smoking; | |||
| <blockquote> | |||
| * publicly denied, while internally acknowledging, that secondhand tobacco smoke is harmful to nonsmokers, and | |||
| Non-smokers who breathe air containing ambient smoke are often referred to as | |||
| * destroyed documents relevant to litigation. | |||
| passive smokers and many studies have been conducted to assess their risks. Some | |||
| studies on exposure to ambient smoke conclude that it represents a risk for health. | |||
| </blockquote> | |||
| '''''' (site accessed on July 27, 2007)<br /> | |||
| <blockquote> | |||
| '''The World Health Organisation, the United States Surgeon General and other public health bodies have concluded that exposure to environmental tobacco smoke (ETS), sometimes called ‘second-hand smoke’, is a cause of various serious diseases, including lung cancer, heart disease and respiratory illnesses in children.'''<br /> | |||
| They conclude that there is no known safe level of ETS exposure and hence advise that public health policy would be best served by bans on public smoking.<br /> | |||
| '''Our view of the science'''<br /> | |||
| The risks associated with ETS have been measured in epidemiological studies. These mainly use questionnaires to compare the incidence of diseases such as lung cancer in non-smoking women whose husbands were smokers, with non-smoking women whose husbands were non-smokers.<br /> | |||
| For lung cancer, the major studies report that relative risk associated with prolonged non-smoker exposure to ETS is 1.3. A relative risk of 1 means no risk, and prolonged active smoking is typically associated with a relative risk of lung cancer of the order of 20 or higher.<br /> | |||
| For heart disease, the major studies also report a relative risk for ETS exposure of around 1.3. The relative risk for active smoking and heart disease is typically of the order of 3 to 5.<br /> | |||
| Many epidemiologists say that relative risks below 2 are weak associations and are more difficult to quantify than stronger associations. Perhaps because the relative risks reported in individual studies tend to be below 2, many studies do not reach statistical significance.<br /> | |||
| Studies of respiratory illnesses in children whose parents smoke, and research into whether ETS exposure exacerbates symptoms for people with conditions such as asthma, suggest that ETS can increase risks of respiratory illnesses in children and can affect people with pre-existing conditions such as asthma. | |||
| The ruling found that tobacco companies undertook joint efforts to undermine and discredit the scientific consensus that secondhand smoke causes disease, notably by controlling research findings via paid consultants. The ruling also concluded that tobacco companies were fraudulently continuing to deny the health effects of ETS exposure.<ref name="kessler" /> | |||
| '''Our approach to regulation'''<br /> | |||
| We support regulation that accommodates the interests of both non-smokers and smokers and limits non-smokers’ involuntary exposure to ETS. | |||
| On May 22, 2009, a three-judge panel of the U.S. Court of Appeals for the District of Columbia Circuit unanimously upheld the lower court's 2006 ruling.<ref name="rico-appeal">, U.S. Court of Appeals for the District of Columbia Circuit, 22 May 2009</ref><ref> Bloomberg news, 22 May 2009</ref><ref> Reuters, 22 May 2009</ref> | |||
| We favour restrictions on smoking in enclosed public places and we accept that there needs to be regulation.<br /> | |||
| We support practical initiatives such as the creation of smoke-free areas, combined with adequate provision for smokers. | |||
| == Smoke-free laws == | |||
| </blockquote> | |||
| {{See also|Smoking ban|List of smoking bans|Smoking bans in private vehicles}} | |||
| '''''' (site accessed on November 19, 2006)<br /> | |||
| <blockquote> | |||
| Imperial Tobacco recognises that other people’s tobacco smoke can be unpleasant or annoying, and can raise concerns leading to calls to ban smoking . However, it is our view that the scientific evidence, taken as a whole, is insufficient to establish that other people’s tobacco smoke is a cause of any disease.<br /> | |||
| The statistical population studies (epidemiology) which have led to claims that other people’s tobacco smoke is a risk to health are subject to some methodological flaws. Most individual studies show no statistical effects. When study results are combined (a process called ‘meta analysis’), at most they indicate a very small increase in relative risk. | |||
| </blockquote> | |||
| '''''' (site accessed on November 19, 2006)<br /> | |||
| <blockquote> | |||
| We agree that ETS can be annoying to non-smokers and that in poorly ventilated areas ETS can cause substantial irritation of the eyes, nose and throat. We therefore ask all smokers to be aware of and show consideration for people with whom they come into contact. However, we do not believe that the claim that ETS is a cause of lung cancer, heart disease and chronic pulmonary diseases in non-smokers has been convincingly demonstrated or that a reliable causal link between ETS exposure and chronic diseases has been established. | |||
| </blockquote> | |||
| '''''' (site accessed on November 19, 2006)<br /> | |||
| <blockquote> | |||
| Public health officials have concluded that secondhand smoke from cigarettes causes disease, including lung cancer and heart disease, in non-smoking adults, as well as causes conditions in children such as asthma, respiratory infections, cough, wheeze, otitis media (middle ear infection) and Sudden Infant Death Syndrome. In addition, public health officials have concluded that secondhand smoke can exacerbate adult asthma and cause eye, throat and nasal irritation.<br /> | |||
| Philip Morris USA believes that the public should be guided by the conclusions of public health officials regarding the health effects of secondhand smoke in deciding whether to be in places where secondhand smoke is present, or if they are smokers, when and where to smoke around others. Particular care should be exercised where children are concerned, and adults should avoid smoking around them.<br /> | |||
| We also believe that the conclusions of public health officials concerning environmental tobacco smoke are sufficient to warrant measures that regulate smoking in public places. We also believe that where smoking is permitted, the government should require the posting of warning notices that communicate public health officials' conclusions that secondhand smoke causes disease in non-smokers. | |||
| </blockquote> | |||
| '''''' (site accessed on November 19, 2006)<br /> | |||
| <blockquote> | |||
| RJRT believes that individuals should rely on the conclusions of the U.S. Surgeon General, the Centers for Disease Control and other public health and medical officials when making decisions regarding smoking. | |||
| </blockquote> | |||
| As a consequence of the health risks associated with secondhand smoke, many national and local governments have outlawed smoking in indoor public places, including ]s, ]s, and ]s, as well as some outdoor open areas.<ref> {{webarchive|url=https://web.archive.org/web/20131126094031/http://gothamist.com/2011/05/18/smokers_just_daring_bloomberg_to_ti.php |date=2013-11-26 }}</ref> ] was the first country in the world to institute a comprehensive national ban on smoking in all indoor workplaces on 29 March 2004. Since then, many others have followed suit. The countries which have ratified the ] (FCTC) have a legal obligation to implement ''effective'' legislation "for protection from exposure to tobacco smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places." (Article 8 of the FCTC<ref name="framework-treaty">{{cite web |url = http://whqlibdoc.who.int/publications/2003/9241591013.pdf |title = WHO Framework Convention on Tobacco Control |publisher = ] |quote = Parties recognize that scientific evidence has unequivocally established that exposure to tobacco causes death, disease and disability |date = 2005-02-27 |access-date = 2009-01-12 }}</ref>) The parties to the FCTC have further adopted ''Guidelines on the Protection from Exposure to secondhand Smoke'' which state that "effective measures to provide protection from exposure to tobacco smoke ... require the total elimination of smoking and tobacco smoke in a particular space or environment in order to create a 100% smoke-free environment."<ref name="fctc-guidelines">{{cite web |title = Guidelines on the Protection from Exposure to Secondhand Smoke |website = ] |publisher = ] |year = 2007 |access-date =2009-01-29 |url =https://www.who.int/fctc/cop/art%208%20guidelines_english.pdf }}</ref> | |||
| ==Smoking bans== | |||
| :''See also: ]s, ]'' | |||
| As a consequence of the health risks associated with passive smoking, a general ] in all establishments serving food and drink, including ]s, ]s, and ]s, was introduced in ] on ] ], in ] on 10 January 2005 and in ] on ] ]. Other places, including ] on 1 June 2007, throughout the ] between ] ] and ] ], and ] have similar legislation in place. | |||
| Opinion polls have shown considerable support for smoke-free laws. In June 2007, a survey of 15 countries found 80% approval for such laws.<ref></ref> A survey in France, reputedly a nation of smokers, showed 70% support.<ref name="France to ban smoking"/> | |||
| These initial bans have grown in scope, with countries (such as ], the ], ]), jurisdictions (like ], ], ], ], and ] in the U.S.) now prohibiting smoking in public buildings as well as establishments such as restaurants and clubs. Many office buildings contain specially ventilated smoking areas; some are required by ] to provide them. | |||
| === Effects === | |||
| The state of Hawaii recently passed a bill making it illegal to smoke in any public place or within 20 feet of an entrance or ventilation shaft intake of a building. | |||
| Smoking bans by governments result in decreased harm from secondhand smoke, including less admissions for ].<ref>{{cite journal |last1=Frazer |first1=Kate |last2=Callinan |first2=Joanne E |last3=McHugh |first3=Jack |last4=van Baarsel |first4=Susan |last5=Clarke |first5=Anna |last6=Doherty |first6=Kirsten |last7=Kelleher |first7=Cecily |title=Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption |journal=Cochrane Database of Systematic Reviews |date=4 February 2016 |volume=2016 |issue=2 |pages=CD005992 |doi=10.1002/14651858.CD005992.pub3 |pmid=26842828 |pmc=6486282 }}</ref> In the first 18 months after the town of ], enacted a smoke-free law in 2003, hospital admissions for heart attacks dropped 27%. Admissions in neighbouring towns without smoke-free laws showed no change, and the decline in heart attacks in Pueblo was attributed to the resulting reduction in secondhand smoke exposure.<ref>{{cite journal |title=Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance—City of Pueblo, Colorado, 2002–2006 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=57 |issue=51 |pages=1373–7 |date=January 2009 |pmid=19116606 |url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5751a1.htm |author1= Centers for Disease Control and Prevention (CDC) }}</ref> A 2004 smoking ban instituted in ] workplaces decreased workers' secondhand smoke exposure from 8% of workers in 2003 to 5.4% of workers in 2010.<ref name=Fitzsimmons>{{cite web |url = http://blogs.cdc.gov/niosh-science-blog/2013/11/21/ets/ |title = Reducing Worker Exposure to ETS |publisher = National Institute for Occupational Safety and Health (NIOSH) |date = 21 November 2013 |last = Fitzsimmons |first = Kathleen |access-date = 14 January 2015}}</ref> A 2016 review also found that bans and policy changes in specific locations such as hospitals or universities can lead to reduced smoking rates. In prison settings bans might lead to reduced mortality and to lower exposure to secondhand smoke.<ref>{{cite journal |last1=Frazer |first1=Kate |last2=McHugh |first2=Jack |last3=Callinan |first3=Joanne E |last4=Kelleher |first4=Cecily |title=Impact of institutional smoking bans on reducing harms and secondhand smoke exposure |journal=Cochrane Database of Systematic Reviews |date=27 May 2016 |volume=2016 |issue=5 |pages=CD011856 |doi=10.1002/14651858.CD011856.pub2 |pmid=27230795 |pmc=10164285 }}</ref> | |||
| In 2001, a systematic review for the Guide to Community Preventive Services acknowledged strong evidence of the effectiveness of smoke-free policies and restrictions in reducing expose to secondhand smoke. A follow-up to this review, identified the evidence on which the effectiveness of smoking bans reduced the prevalence of tobacco use. Articles published until 2005, were examined to further support this evidence. The examined studies provided sufficient evidence that smoke-free policies reduce tobacco use among workers when implemented in worksites or by communities.<ref>{{cite journal | vauthors = Hopkins DP, Razi S, Leeks KD, Priya Kalra G, Chattopadhyay SK, Soler RE | year = 2010 | title = Smokefree policies to reduce tobacco use. A systematic review | journal = Am J Prev Med | volume = 38 | issue = 2 Suppl | pages = S275–89 | doi = 10.1016/j.amepre.2009.10.029 | pmid = 20117612| author7 = Task Force on Community Preventive Services }}</ref> | |||
| Some regions and local governments have banned smoking in all workplaces, in taxicabs, and in ventilated smoking rooms or enclosed smoking shelters such as those found in front of hospitals. | |||
| While a number of studies funded by the tobacco industry have claimed a negative economic impact from smoke-free laws, no independently funded research has shown any such impact. A 2003 review reported that independently funded, methodologically sound research consistently found either no economic impact or a positive impact from smoke-free laws.<ref>{{cite journal |vauthors=Scollo M, Lal A, Hyland A, Glantz S |title=Review of the quality of studies on the economic effects of smoke-free policies on the hospitality industry |journal=Tobacco Control |date=Mar 2003 |pmid=12612356 |pmc=1759095 |volume=12 |issue=1 |pages=13–20 |doi=10.1136/tc.12.1.13}}</ref> | |||
| Even in countries traditionally seen as nations of smokers {{Who|date=October 2007}}, opinion polls have shown support for bans, with 70% of those in France supporting a ban.<ref name="France to ban smoking"/> | |||
| Air nicotine levels were measured in Guatemalan bars and restaurants before and after an implemented smoke-free law in 2009. Nicotine concentrations significantly decreased in both the bars and restaurants measured. Also, the employees' support for a smoke-free workplace substantially increased in the post-implementation survey compared to pre-implementation survey.<ref>{{cite journal |vauthors=Barnoya J, Arvizu M, Jones MR, Hernandez JC, Breysse PN, Navas-Acien A |title=Secondhand smoke exposure in bars and restaurants in Guatemala City: before and after smoking ban evaluation |journal=Cancer Causes Control |volume=22 |issue=1 |pages=151–6 |date=November 2010 |pmid=21046446 |doi=10.1007/s10552-010-9673-8 |s2cid=673901 }}</ref> | |||
| In the first 18 months after the town of ], ] enacted a smoking ban in 2003, hospital admissions for heart attacks dropped 27%. Admissions in neighboring towns without smoking bans showed no change. Raymond Gibbons, M.D., ] president said, "The decline in the number of heart attack hospitalizations within the first year and a half after the non-smoking ban that was observed in this study is most likely due to a decrease in the effect of secondhand smoke as a triggering factor for heart attacks."<ref>{{cite web | |||
| | last = | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Reduction in the Incidence of Acute Myocardial Infarction Associated with a Citywide Smoking Ordinance | |||
| | work = | |||
| | publisher = ] | |||
| | date = 2006-10-3 | |||
| | url = http://www.heart.org/presenter.jhtml?identifier=3043008 | |||
| | format = | |||
| | doi = | |||
| | accessdate = 2007-01-18 }}</ref> | |||
| == |
=== Public opinion === | ||
| Recent surveys taken by the ] demonstrate supportive attitudes of the public towards smoke-free policies in outdoor areas. A vast majority of the public supports restricting smoking in various outdoor settings. The respondents' support for the policies were for varying reasons such as litter control, establishing positive smoke-free role models for youth, reducing youth opportunities to smoke, and avoiding exposure to secondhand smoke.<ref>{{cite journal |last1=Thomson |first1=George |last2=Wilson |first2=Nick |last3=Edwards |first3=Richard |title=At the frontier of tobacco control: A brief review of public attitudes toward smoke-free outdoor places |journal=Nicotine & Tobacco Research |date=June 2009 |volume=11 |issue=6 |pages=584–590 |doi=10.1093/ntr/ntp046 |pmid=19359392 |doi-access=free }}</ref> | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| === Alternative forms === | |||
| ==External links== | |||
| Alternatives to smoke-free laws have also been proposed as a means of ], particularly in bars and restaurants. For example, critics of smoke-free laws cite studies suggesting ventilation as a means of reducing tobacco smoke pollutants and improving air quality.<ref>{{cite news |title=No ifs or butts |url=https://www.building.co.uk/no-ifs-or-butts/3047478.article |work=Building |date=7 March 2005 }}</ref> Ventilation has also been heavily promoted by the tobacco industry as an alternative to outright bans, via a network of ostensibly independent experts with often undisclosed ties to the industry.<ref>{{cite journal |vauthors=Drope J, Bialous SA, Glantz SA |title=Tobacco industry efforts to present ventilation as an alternative to smoke-free environments in North America |journal=Tob Control |volume=13 |issue=Suppl 1 |pages=i41–7 |date=March 2004 |pmid=14985616 |pmc=1766145 |doi= 10.1136/tc.2003.004101|quote = The industry developed a network of ventilation 'experts' to promote its position that smoke-free environments were not necessary, often without disclosing the financial relationship between these experts and the industry. }}</ref> However, not all critics have connections to the industry. | |||
| ===Scientific bodies=== | |||
| * , from the U.S. ] | |||
| The ] (ASHRAE) officially concluded in 2005 that while completely isolated smoking rooms do eliminate the risk to nearby non-smoking areas, smoking bans are the only means of eliminating health risks associated with indoor exposure. They further concluded that no system of dilution or cleaning was effective at eliminating risk.<ref name="ASHRAE">{{cite web |title=ASHRAE Position Document on Environmental Tobacco Smoke |url=https://www.ashrae.org/file%20library/about/position%20documents/pd_environmental-tobacco-smoke-2020-07-1.pdf |publisher=] |date=July 2020 }}</ref> The ] and the ] have reached similar conclusions.<ref name="sg-exec-summary">{{cite web |title = The Health Consequences of Involuntary Exposure to Tobacco Smoke |publisher = ] |website = Executive Summary |year = 2006 |access-date =2009-01-28 |url = http://www.surgeongeneral.gov/library/secondhandsmoke/report/executivesummary.pdf }}</ref><ref name="ecjrc">{{cite web|publisher=] ] |title=Institute for Health and Consumer Protection Activity Report 2003 |year=2003 |url=http://ihcp.jrc.ec.europa.eu/docs/IHCP_annual_report/ihcp03.pdf |access-date=2009-01-28 |url-status=dead |archive-url=https://web.archive.org/web/20090327101821/http://ihcp.jrc.ec.europa.eu/docs/IHCP_annual_report/ihcp03.pdf |archive-date=March 27, 2009 }}</ref> The implementation guidelines for the ] states that engineering approaches, such as ventilation, are ineffective and do not protect against secondhand smoke exposure.<ref name="fctc-guidelines" /> However, this does not necessarily mean that such measures are useless in reducing harm, only that they fall short of the goal of reducing exposure completely to zero. | |||
| * {{PDFlink||219 ]<!-- application/pdf, 225034 bytes -->}}. From the 11th Report on Carcinogens of the U.S. ] | |||
| * , from the ] | |||
| Others have suggested a system of tradable smoking pollution permits, similar to the ] pollution permits systems used by the ] in recent decades to curb other types of pollution.<ref>{{cite news |title = Let Bars Buy, Sell Smoking Permits |url = http://www.madison.com/archives/read.php?ref=/madison.com/html/archive_files/wsj/2005/09/25/0509240280.php |first = Robert |last = Haveman |author2 = John Mullahy |work = ] |date = September 25, 2005 |access-date = 2009-01-28 |page = B2 |url-status = dead |archive-url = https://web.archive.org/web/20090104145317/http://www.madison.com/archives/read.php?ref=%2Fmadison.com%2Fhtml%2Farchive_files%2Fwsj%2F2005%2F09%2F25%2F0509240280.php |archive-date = January 4, 2009 }}</ref> This would guarantee that a portion of bars/restaurants in a jurisdiction will be smoke-free, while leaving the decision to the market. | |||
| * , a monograph of the ] and ] | |||
| * from the U.S. ] | |||
| ==In animals== | |||
| {{main|Animals and tobacco smoke}} | |||
| Multiple studies have been conducted to determine the carcinogenicity of environmental tobacco smoke to animals. These studies typically fall under the categories of simulated environmental tobacco smoke, administering condensates of ], or observational studies of cancer among pets. | |||
| To simulate environmental tobacco smoke, scientists expose animals to sidestream smoke, that which emanates from the cigarette's burning cone and through its paper, or a combination of mainstream and sidestream smoke.<ref name=IARC2004/> The IARC monographs conclude that mice with prolonged exposure to simulated environmental tobacco smoke, that is six hours a day, five days a week, for five months with a subsequent four-month interval before dissection, will have significantly higher incidence and multiplicity of lung tumors than with control groups. | |||
| The IARC monographs concluded that sidestream smoke condensates had a significantly higher carcinogenic effect on mice than did mainstream smoke condensates.<ref name=IARC2004/> | |||
| ===Observational studies=== | |||
| Secondhand smoke is popularly recognised as a risk factor for cancer in pets.<ref>{{cite web |url = http://www.livescience.com/animals/070831_pets_smoking.html |title = Secondhand Smoke Causes Cancer in Pets |first = Andrea |last = Thompson |publisher = LiveScience |date = 2007-08-31 |access-date = 2007-08-31}}</ref> A study conducted by the ] and the ] linked the occurrence of feline oral cancer to exposure to environmental tobacco smoke through an ] of the ] gene.<ref>{{cite journal |vauthors=Snyder LA, Bertone ER, Jakowski RM, Dooner MS, Jennings-Ritchie J, Moore AS |title=p53 expression and environmental tobacco smoke exposure in feline oral squamous cell carcinoma |journal=Vet Pathol |volume=41 |issue=3 |pages=209–14 |year=2004 |pmid=15133168 |doi=10.1354/vp.41-3-209 |s2cid=24749614 |doi-access=free }}</ref> Another study conducted at the same universities concluded that cats living with a smoker were more likely to get ]; the risk increased with the duration of exposure to secondhand smoke and the number of smokers in the household.<ref>{{cite journal |vauthors= Bertone ER, Snyder LA, Moore AS |title= Environmental Tobacco Smoke and Risk of Malignant Lymphoma in Pet Cats |journal=American Journal of Epidemiology |volume=156 |issue=3 |pages=268–273 |year=2002 |pmid=12142262 |doi= 10.1093/aje/kwf044 |doi-access=free }}</ref> A study by ] researchers, looking at cases of canine lung cancer, was generally inconclusive, though the authors reported a weak relation for lung cancer in dogs exposed to environmental tobacco smoke. The number of smokers within the home, the number of packs smoked in the home per day, and the amount of time that the dog spent within the home had no effect on the dog's risk for lung cancer.<ref>{{cite journal |vauthors=Reif JS, Dunn K, Ogilvie GK, Harris CK |title=Passive smoking and canine lung cancer risk |journal=Am J Epidemiol |volume=135 |issue=3 |pages=234–9 |year=1992 |pmid=1546698 |doi=10.1093/oxfordjournals.aje.a116276}}</ref> | |||
| == See also == | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * '']'' | |||
| == References == | |||
| {{Reflist|colwidth=30em}} | |||
| == External links == | |||
| ;Scientific bodies | |||
| {{Refbegin}} | |||
| * , from the U.S. ] | |||
| * {{cite web |url= https://ntp.niehs.nih.gov/ntp/roc/content/profiles/tobaccorelatedexposures.pdf |title= Environmental Tobacco Smoke |url-status= live |archive-url= https://web.archive.org/web/20080716173310/http://ntp.niehs.nih.gov/ntp/roc/eleventh/profiles/s176toba.pdf |archive-date= 2008-07-16 }} {{small|(219 KB)}}. From the 11th Report on Carcinogens of the U.S. ] | |||
| * {{cite journal |author1=U.S. Dept. of Health and Human Services |author2=Centers for Disease Control and Prevention |author3=Coordinating Center for Health Promotion |author4=National Center for Chronic Disease Prevention and Health Promotion |author5=Office on Smoking and Health |url=https://www.ncbi.nlm.nih.gov/books/NBK44324/ |title=The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General |series=Publications and Reports of the Surgeon General |publisher=] |date=2006-06-27 |location=Atlanta, Ga. |pmid=20669524 |id=O2NLM: WA 754 H4325 2006|ref=CITEREFSurgeon_General2006 |quote=Secondhand smoke exposure causes disease and premature death in children and adults who do not smoke}} | |||
| * {{cite book |author1=World Health Organization |author2=International Agency for Research on Cancer |title=Tobacco Smoke and Involuntary Smoking |publisher=IARC Working Group on the Evaluation of Carcinogenic Risks to Humans | |||
| |location=Lyon, France |year=2004 |isbn=978-92-832-1283-6 |url=http://monographs.iarc.fr/ENG/Monographs/vol83/mono83.pdf |volume=83 |series=IARC monographs on the evaluation of carcinogenic risks to humans |ref=CITEREFIARC2004|author-link1=World Health Organization |author-link2=International Agency for Research on Cancer }} | |||
| * from the U.S. ] | |||
| * from the U.S. ] | |||
| * , from the ] | * , from the ] | ||
| * ] | |||
| * {{cite journal |last1=Öberg |first1=Mattias |last2=Jaakkola |first2=Maritta S |last3=Woodward |first3=Alistair |last4=Peruga |first4=Armando |last5=Prüss-Ustün |first5=Annette |title=Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries |journal=The Lancet |date=January 2011 |volume=377 |issue=9760 |pages=139–146 |doi=10.1016/S0140-6736(10)61388-8 |pmid=21112082 |s2cid=7179156 }} | |||
| {{Refend}} | |||
| ;Tobacco industry | |||
| {{Refbegin}} | |||
| * {{PDFlink||1.55 ]<!-- application/pdf, 1629184 bytes -->}}: Report of the Committee of Experts on Tobacco Industry Documents from the ] | |||
| * {{cite web |url=https://www.who.int/tobacco/media/en/who_inquiry.pdf |archive-url=http://webarchive.loc.gov/all/20040821060747/http://www.who.int/tobacco/media/en/who_inquiry.pdf |url-status=dead |archive-date=August 21, 2004 |title=Tobacco Company Strategies to Undermine Tobacco Control Activities |access-date=October 5, 2020 }} {{small|(1.55 MB)}}: Report of the Committee of Experts on Tobacco Industry Documents from the ] | |||
| * and from the ] | * and from the ] | ||
| * , made public as a result of the ] | * , made public as a result of the ] | ||
| {{Refend}} | |||
| ;Other links | |||
| {{Refbegin}} | |||
| * Article from ], a healthcare organisation. | |||
| * , by WHO Framework Convention on Tobacco Control | |||
| * | |||
| * | |||
| * | |||
| * {{cite journal |last1=Small |first1=Elysia |last2=Shah |first2=Hina P. |last3=Davenport |first3=Jake J. |last4=Geier |first4=Jacqueline E. |last5=Yavarovich |first5=Kate R. |last6=Yamada |first6=Hidetaka |last7=Sabarinath |first7=Sreedharan N. |last8=Derendorf |first8=Hartmut |last9=Pauly |first9=James R. |last10=Gold |first10=Mark S. |last11=Bruijnzeel |first11=Adrie W. |title=Tobacco smoke exposure induces nicotine dependence in rats |journal=Psychopharmacology |date=January 2010 |volume=208 |issue=1 |pages=143–158 |doi=10.1007/s00213-009-1716-z |pmid=19936715 |pmc=3586198 }} | |||
| * information on health and economic issues related to debates over smokefree restaurants and bars maintained by the ] | |||
| * {{cite web |url=http://publichealthlawcenter.org/sites/default/files/resources/doj-final-opinion.pdf |title=United States of America v. Philip Morris et al.: Final Opinion of Judge Gladys Kessler |publisher=] |last=Kessler |first=Gladys |date=August 17, 2006 }} | |||
| * | |||
| * | |||
| {{Refend}} | |||
| ==References== | |||
| <div class="references-small"> | |||
| <!--See http://en.wikipedia.org/Wikipedia:Footnotes for an explanation of how to generate footnotes using the <ref(erences/)> tags--> | |||
| {{reflist|2}} | |||
| </div> | |||
| {{Smoking nav}} | |||
| ] | |||
| {{Cigarettes}} | |||
| ] | |||
| {{HVAC}} | |||
| ] | |||
| {{Recreational drug use}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Passive Smoking}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 19:46, 21 December 2024
Inhalation of tobacco smoke by persons other than the intended active smoker "Second hand smoke" redirects here. For the Sublime album, see Second-hand Smoke.

Passive smoking is the inhalation of tobacco smoke, called passive smoke, secondhand smoke (SHS) or environmental tobacco smoke (ETS), by individuals other than the active smoker. It occurs when tobacco smoke diffuses into the surrounding atmosphere as an aerosol pollutant, which leads to its inhalation by nearby bystanders within the same environment. Exposure to secondhand tobacco smoke causes many of the same health effects caused by active smoking, although at a lower prevalence due to the reduced concentration of smoke that enters the airway.
According to a WHO report published in 2023, more than 1.3 million deaths are attributed to passive smoking worldwide every year. The health risks of secondhand smoke are a matter of scientific consensus, and have been a major motivation for smoking bans in workplaces and indoor venues, including restaurants, bars and night clubs, as well as some open public spaces.
Concerns around secondhand smoke have played a central role in the debate over the harms and regulation of tobacco products. Since the early 1970s, the tobacco industry has viewed public concern over secondhand smoke as a serious threat to its business interests. Despite the industry's awareness of the harms of secondhand smoke as early as the 1980s, the tobacco industry coordinated a scientific controversy with the purpose of stopping regulation of their products.
Terminology
Fritz Lickint created the term "passive smoking" ("Passivrauchen") in a publication in the German language during the 1930s. Terms used include "environmental tobacco smoke" to refer to the airborne matter, while "involuntary smoking" and "passive smoking" refer to exposure to secondhand smoke. The term "environmental tobacco smoke" can be traced back to a 1974 industry-sponsored meeting held in Bermuda, while the term "passive smoking" was first used in the title of a scientific paper in 1970. The Surgeon General of the United States prefers to use the phrase "secondhand smoke" rather than "environmental tobacco smoke", stating that "The descriptor 'secondhand' captures the involuntary nature of the exposure, while 'environmental' does not." Most researchers consider the term "passive smoking" to be synonymous with "secondhand smoke". In contrast, a 2011 commentary in Environmental Health Perspectives argued that research into "thirdhand smoke" renders it inappropriate to refer to passive smoking with the term "secondhand smoke", which the authors stated constitutes a pars pro toto.
The term "sidestream smoke" is sometimes used to refer to smoke that goes into the air directly from a burning cigarette, cigar, or pipe, while "mainstream smoke" refers to smoke that a smoker exhales.
Health effects
Secondhand smoke causes many of the same diseases as direct smoking, including cardiovascular diseases, lung cancer, and respiratory diseases. These include:
- Cancer:
- General: overall increased risk; reviewing the evidence accumulated on a worldwide basis, the International Agency for Research on Cancer concluded in 2004 that "Involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) is carcinogenic to humans." The Centers for Disease Control and Prevention reports that about 70 chemicals present in secondhand smoke are carcinogenic.
- Lung cancer: Passive smoking is a risk factor for lung cancer. In the United States, secondhand smoke is estimated to cause more than 7,000 deaths from lung cancer a year among non-smokers. A quarter of all cases occur in people who have never smoked.
- Breast cancer: The California Environmental Protection Agency concluded in 2005 that passive smoking increases the risk of breast cancer in younger, primarily premenopausal females by 70% and the US Surgeon General has concluded that the evidence is "suggestive", but still insufficient to assert such a causal relationship. In contrast, the International Agency for Research on Cancer concluded in 2004 that there was "no support for a causal relation between involuntary exposure to tobacco smoke and breast cancer in never-smokers." A 2015 meta-analysis found that the evidence that passive smoking moderately increased the risk of breast cancer had become "more substantial than a few years ago".
- Cervical cancer: A 2015 overview of systematic reviews found that exposure to secondhand smoke increased the risk of cervical cancer.
- Bladder cancer: A 2016 systematic review and meta-analysis found that secondhand smoke exposure was associated with a significant increase in the risk of bladder cancer.
- Circulatory system: risk of heart disease and reduced heart rate variability.
- Epidemiological studies have shown that both active and passive cigarette smoking increase the risk of atherosclerosis.
- Passive smoking is strongly associated with an increased risk of stroke, and this increased risk is disproportionately high at low levels of exposure.
- Lung problems:
- Risk of asthma
- Risk of chronic obstructive pulmonary disease (COPD)
- According to a 2015 review, passive smoking may increase the risk of tuberculosis infection and accelerate the progression of the disease, but the evidence remains weak.
- The majority of studies on the association between secondhand smoke exposure and sinusitis have found a significant association between the two.
- Cognitive impairment and dementia: Exposure to secondhand smoke may increase the risk of cognitive impairment and dementia in adults 50 and over. Children exposed to secondhand smoke show reduced vocabulary and reasoning skills when compared with non-exposed children as well as more general cognitive and intellectual deficits.
- Mental health: Exposure to secondhand smoke is associated with an increased risk of depressive symptoms.
- During pregnancy:
- Miscarriage: a 2014 meta-analysis found that maternal secondhand smoke exposure increased the risk of miscarriage by 11%.
- Low birth weight.
- Premature birth (Evidence of the causal link is described only as "suggestive" by the US Surgeon General in his 2006 report.) Laws limiting smoking decrease premature births.
- Stillbirth and congenital malformations in children
- Recent studies comparing females exposed to secondhand smoke and non-exposed females, demonstrate that females exposed while pregnant have higher risks of delivering a child with congenital abnormalities, longer lengths, smaller head circumferences, and neural tube defects.
- General:
- Worsening of asthma, allergies, and other conditions. A 2014 systematic review and meta-analysis found that passive smoking was associated with a slightly increased risk of allergic diseases among children and adolescents; the evidence for an association was weaker for adults.
- Type 2 diabetes. It remains unclear whether the association between passive smoking and diabetes is causal.
- Risk of carrying Neisseria meningitidis or Streptococcus pneumoniae.
- A possible increased risk of periodontitis.
- Overall increased risk of death in both adults, where it was estimated to kill 53,000 nonsmokers per year in the U.S in 1991, and in children. The World Health Organization states that passive smoking causes about 600,000 deaths a year, and about 1% of the global burden of disease. As of 2017, passive smoking causes about 900,000 deaths a year, which is about 1/8 of all deaths caused by smoking.
- Skin conditions: A 2016 systematic review and meta-analysis found that passive smoking was associated with a higher rate of atopic dermatitis.
Risk to children
- Sudden infant death syndrome (SIDS). In his 2006 report, the US Surgeon General concludes: "The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke and sudden infant death syndrome." Secondhand smoking has been estimated to be associated with 430 SIDS deaths in the United States annually.
- Asthma. Secondhand smoke exposure is also associated with an almost doubled risk of hospitalization for asthma exacerbation among children with asthma.
- Lung infections, also including more severe illness with bronchiolitis and bronchitis, and worse outcome, as well as increased risk of developing tuberculosis if exposed to a carrier. In the United States, it is estimated that secondhand smoke has been associated with between 150,000 and 300,000 lower respiratory tract infections in infants and children under 18 months of age, resulting in between 7,500 and 15,000 hospitalizations each year.
- Impaired respiratory function and slowed lung growth
- Allergies
- Maternal passive smoking increases the risk of non-syndromic orofacial clefts by 50% among their children.
- Learning difficulties, developmental delays, executive function problems, and neurobehavioral effects. Animal models suggest a role for nicotine and carbon monoxide in neurocognitive problems.
- Increased risk of middle ear infections.
- Invasive meningococcal disease.
- Anesthesia complications and some negative surgical outcomes.
- Sleep disordered breathing: Most studies have found a significant association between passive smoking and sleep disordered breathing in children, but further studies are needed to determine whether this association is causal.
- Adverse effects on the cardiovascular system of children.
Evidence
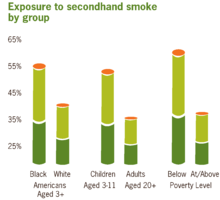
Epidemiological studies show that non-smokers exposed to secondhand smoke are at risk for many of the health problems associated with direct smoking.
In 1992, a review estimated that secondhand smoke exposure was responsible for 35,000 to 40,000 deaths per year in the United States in the early 1980s. The absolute risk increase of heart disease due to ETS was 2.2%, while the attributable risk percent was 23%. A 1997 meta-analysis found that secondhand smoke exposure increased the risk of heart disease by a quarter, and two 1999 meta-analyses reached similar conclusions.
Evidence shows that inhaled sidestream smoke, the main component of secondhand smoke, is about four times more toxic than mainstream smoke. This fact has been known to the tobacco industry since the 1980s, though it kept its findings secret. Some scientists believe that the risk of passive smoking, in particular the risk of developing coronary heart diseases, may have been substantially underestimated.
In 1997, a meta-analysis on the relationship between secondhand smoke exposure and lung cancer concluded that such exposure caused lung cancer. The increase in risk was estimated to be 24% among non-smokers who lived with a smoker. In 2000, Copas and Shi reported that there was clear evidence of publication bias in the studies included in this meta-analysis. They further concluded that after correcting for publication bias, and assuming that 40% of all studies are unpublished, this increased risk decreased from 24% to 15%. This conclusion has been challenged on the basis that the assumption that 40% of all studies are unpublished was "extreme". In 2006, Takagi et al. reanalyzed the data from this meta-analysis to account for publication bias and estimated that the relative risk of lung cancer among those exposed to secondhand smoke was 1.19, slightly lower than the original estimate. A 2000 meta-analysis found a relative risk of 1.48 for lung cancer among men exposed to secondhand smoke, and a relative risk of 1.16 among those exposed to it at work. Another meta-analysis confirmed the finding of an increased risk of lung cancer among women with spousal exposure to secondhand smoke the following year. It found a relative risk of lung cancer of 1.29 for women exposed to secondhand smoke from their spouses. A 2014 meta-analysis noted that "the association between exposure to secondhand smoke and lung cancer risk is well established."
A minority of epidemiologists have found it hard to understand how secondhand smoke, which is more diluted than actively inhaled smoke, could have an effect that is such a large fraction of the added risk of coronary heart disease among active smokers. One proposed explanation is that secondhand smoke is not simply a diluted version of "mainstream" smoke, but has a different composition with more toxic substances per gram of total particulate matter. Passive smoking appears to be capable of precipitating the acute manifestations of cardio-vascular diseases (atherothrombosis) and may also have a negative impact on the outcome of patients who have acute coronary syndromes.
In 2004, the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO) reviewed all significant published evidence related to tobacco smoking and cancer. It concluded:
These meta-analyses show that there is a statistically significant and consistent association between lung cancer risk in spouses of smokers and exposure to second-hand tobacco smoke from the spouse who smokes. The excess risk is of the order of 20% for women and 30% for men and remains after controlling for some potential sources of bias and confounding.
Subsequent meta-analyses have confirmed these findings.
The National Asthma Council of Australia cites studies showing that secondhand smoke is probably the most important indoor pollutant, especially around young children:
- Smoking by either parent, particularly by the mother, increases the risk of asthma in children.
- The outlook for early childhood asthma is less favourable in smoking households.
- Children with asthma who are exposed to smoking in the home generally have more severe disease.
- Many adults with asthma identify ETS as a trigger for their symptoms.
- Doctor-diagnosed asthma is more common among non-smoking adults exposed to ETS than those not exposed. Among people with asthma, higher ETS exposure is associated with a greater risk of severe attacks.
In France, exposure to secondhand smoke has been estimated to cause between 3,000 and 5,000 premature deaths per year, with the larger figure cited by Prime Minister Dominique de Villepin during his announcement of a nationwide smoke-free law: "That makes more than 13 deaths a day. It is an unacceptable reality in our country in terms of public health."
There is good observational evidence that smoke-free legislation reduces the number of hospital admissions for heart disease.
Exposure and risk levels
The International Agency for Research on Cancer of the World Health Organization concluded in 2004 that there was sufficient evidence that secondhand smoke caused cancer in humans. Those who work in environments where smoke is not regulated are at higher risk. Workers particularly at risk of exposure include those in installation repair and maintenance, construction and extraction, and transportation.
Much research has come from studies of nonsmokers who are married to a smoker. The US Surgeon General, in his 2006 report, estimated that living or working in a place where smoking is permitted increases the non-smokers' risk of developing heart disease by 25–30% and lung cancer by 20–30%.
Similarly, children who are exposed to environmental tobacco smoke are shown to experience a range of adverse effects and a higher risk of becoming smokers later in life. The WHO has identified reduction of exposure to environmental tobacco smoke as key element for actions to encourage healthy child development.
The US Centers for Disease Control and Prevention monitors the extent of and trends in exposure to environmental tobacco smoke by measuring serum cotinine in national health surveys. The prevalence of secondhand smoke exposure among U.S. nonsmokers declined from 87.5% in 1988 to 25.2% in 2014. However, nearly half of blacks and the poor were exposed in 2014.
Interventions to reduce environmental tobacco smoke
A systematic review compared smoking control programmes and their effects on smoke exposure in children. The review distinguishes between community-based, ill-child and healthy-child settings and the most common types of interventions were counselling or brief advice during clinical visits. The review did not find superior outcomes for any intervention, and the authors caution that evidence from adult settings may not generalise well to children.
Biomarkers

Environmental tobacco smoke can be evaluated either by directly measuring tobacco smoke pollutants found in the air or by using biomarkers, an indirect measure of exposure. Carbon monoxide monitored through breath, nicotine, cotinine, thiocyanates, and proteins are the most specific biological markers of tobacco smoke exposure. Biochemical tests are a much more reliable biomarker of secondhand smoke exposure than surveys. Certain groups of people are reluctant to disclose their smoking status and exposure to tobacco smoke, especially pregnant women and parents of young children. This is due to their smoking being socially unacceptable. Also, it may be difficult for individuals to recall their exposure to tobacco smoke.
A 2007 study in the Addictive Behaviors journal found a positive correlation between secondhand tobacco smoke exposure and concentrations of nicotine and/or biomarkers of nicotine in the body. Significant biological levels of nicotine from secondhand smoke exposure were equivalent to nicotine levels from active smoking and levels that are associated with behaviour changes due to nicotine consumption.
Cotinine
Cotinine, the metabolite of nicotine, is a biomarker of secondhand smoke exposure. Typically, cotinine is measured in the blood, saliva, and urine. Hair analysis has recently become a new, noninvasive measurement technique. Cotinine accumulates in hair during hair growth, which results in a measure of long-term, cumulative exposure to tobacco smoke. Urinary cotinine levels have been a reliable biomarker of tobacco exposure and have been used as a reference in many epidemiological studies. However, cotinine levels found in the urine reflect exposure only over the preceding 48 hours. Cotinine levels of the skin, such as the hair and nails, reflect tobacco exposure over the previous three months and are a more reliable biomarker.
Carbon monoxide (CO)
Carbon monoxide monitored via breath is also a reliable biomarker of secondhand smoke exposure as well as tobacco use. With high sensitivity and specificity, it not only provides an accurate measure, but the test is also non-invasive, highly reproducible, and low in cost. Breath CO monitoring measures the concentration of CO in an exhalation in parts per million, and this can be directly correlated to the blood CO concentration (carboxyhemoglobin). Breath CO monitors can also be used by emergency services to identify patients who are suspected of having CO poisoning.
Pathophysiology
A 2004 study by the International Agency for Research on Cancer of the World Health Organization concluded that non-smokers are exposed to the same carcinogens as active smokers. Sidestream smoke contains more than 4,000 chemicals, including 69 known carcinogens. Of special concern are polynuclear aromatic hydrocarbons, tobacco-specific N-nitrosamines, and aromatic amines, such as 4-aminobiphenyl, all known to be highly carcinogenic. Mainstream smoke, sidestream smoke, and secondhand smoke contain largely the same components, however the concentration varies depending on type of smoke. Several well-established carcinogens have been shown by the tobacco companies' own research to be present at higher concentrations in sidestream smoke than in mainstream smoke.
Secondhand smoke has been shown to produce more particulate-matter (PM) pollution than an idling low-emission diesel engine. In an experiment conducted by the Italian National Cancer Institute, three cigarettes were left smoldering, one after the other, in a 60 m garage with a limited air exchange. The cigarettes produced PM pollution exceeding outdoor limits, as well as PM concentrations up to 10-fold that of the idling engine.
Secondhand tobacco smoke exposure has immediate and substantial effects on blood and blood vessels in a way that increases the risk of a heart attack, particularly in people already at risk. Exposure to tobacco smoke for 30 minutes significantly reduces coronary flow velocity reserve in healthy nonsmokers. Secondhand smoke is also associated with impaired vasodilation among adult nonsmokers. Secondhand smoke exposure also affects platelet function, vascular endothelium, and myocardial exercise tolerance at levels commonly found in the workplace.
Pulmonary emphysema can be induced in rats through acute exposure to sidestream tobacco smoke (30 cigarettes per day) over a period of 45 days. Degranulation of mast cells contributing to lung damage has also been observed.
The term "third-hand smoke" was recently coined to identify the residual tobacco smoke contamination that remains after the cigarette is extinguished and secondhand smoke has cleared from the air. Preliminary research suggests that by-products of third-hand smoke may pose a health risk, though the magnitude of risk, if any, remains unknown. In October 2011, it was reported that Christus St. Frances Cabrini Hospital in Alexandria, Louisiana, would seek to eliminate third-hand smoke beginning in July 2012, and that employees whose clothing smelled of smoke would not be allowed to work. This prohibition was enacted because third-hand smoke poses a special danger for the developing brains of infants and small children.
In 2008, there were more than 161,000 deaths attributed to lung cancer in the United States. Of these deaths, an estimated 10% to 15% were caused by factors other than first-hand smoking; equivalent to 16,000 to 24,000 deaths annually. Slightly more than half of the lung cancer deaths caused by factors other than first-hand smoking were found in nonsmokers. Lung cancer in non-smokers may well be considered one of the most common cancer mortalities in the United States. Clinical epidemiology of lung cancer has linked the primary factors closely tied to lung cancer in non-smokers as exposure to secondhand tobacco smoke, carcinogens including radon, and other indoor air pollutants.
Opinion of public health authorities
There is widespread scientific consensus that exposure to secondhand smoke is harmful. The link between passive smoking and health risks is accepted by every major medical and scientific organisation, including:
- World Health Organization
- U.S. National Institutes of Health
- Centers for Disease Control
- United States Surgeon General
- U.S. National Cancer Institute
- United States Environmental Protection Agency
- California Environmental Protection Agency
- American Heart Association, American Lung Association, and American Cancer Society
- American Medical Association
- American Academy of Pediatrics
- Australian National Health and Medical Research Council
- United Kingdom Scientific Committee on Tobacco and Health
Public opinion
Recent major surveys conducted by the U.S. National Cancer Institute and Centers for Disease Control have found widespread public awareness that secondhand smoke is harmful. In both 1992 and 2000 surveys, more than 80% of respondents agreed with the statement that secondhand smoke was harmful. A 2001 study found that 95% of adults agreed that secondhand smoke was harmful to children, and 96% considered tobacco-industry claims that secondhand smoke was not harmful to be untruthful.
A 2007 Gallup poll found that 56% of respondents felt that secondhand smoke was "very harmful", a number that has held relatively steady since 1997. Another 29% believe that secondhand smoke is "somewhat harmful"; 10% answered "not too harmful", while 5% said "not at all harmful".
Controversy over harm
As part of its attempt to prevent or delay tighter regulation of smoking, the tobacco industry funded a number of scientific studies and, where the results cast doubt on the risks associated with secondhand smoke, sought wide publicity for those results. The industry also funded libertarian and conservative think tanks, such as the Cato Institute in the United States and the Institute of Public Affairs in Australia which criticised both scientific research on passive smoking and policy proposals to restrict smoking. New Scientist and the European Journal of Public Health have identified these industry-wide coordinated activities as one of the earliest expressions of corporate denialism. Further, they state that the disinformation spread by the tobacco industry has created a tobacco denialism movement, sharing many characteristics of other forms of denialism, such as HIV-AIDS denialism.
Industry-funded studies and critiques
Enstrom and Kabat
A 2003 study by James Enstrom and Geoffrey Kabat, published in the British Medical Journal, argued that the harms of passive smoking had been overstated. Their analysis reported no statistically significant relationship between passive smoking and lung cancer, coronary heart disease (CHD), or chronic obstructive pulmonary disease, though the accompanying editorial noted that "they may overemphasise the negative nature of their findings." This paper was widely promoted by the tobacco industry as evidence that the harms of passive smoking were unproven. The American Cancer Society (ACS), whose database Enstrom and Kabat used to compile their data, criticized the paper as "neither reliable nor independent", stating that scientists at the ACS had repeatedly pointed out serious flaws in Enstrom and Kabat's methodology prior to publication. Notably, the study had failed to identify a comparison group of "unexposed" persons.
Enstrom's ties to the tobacco industry also drew scrutiny; in a 1997 letter to Philip Morris, Enstrom requested a "substantial research commitment... in order for me to effectively compete against the large mountain of epidemiologic data and opinions that already exist regarding the health effects of ETS and active smoking." In a US racketeering lawsuit against tobacco companies, the Enstrom and Kabat paper was cited by the US District Court as "a prime example of how nine tobacco companies engaged in criminal racketeering and fraud to hide the dangers of tobacco smoke." The Court found that the study had been funded and managed by the Center for Indoor Air Research, a tobacco industry front group tasked with "offsetting" damaging studies on passive smoking, as well as by Philip Morris who stated that Enstrom's work was "clearly litigation-oriented". A 2005 paper in Tobacco Control argued that the disclosure section in the Enstrom and Kabat BMJ paper, although it met the journal's requirements, "does not reveal the full extent of the relationship the authors had with the tobacco industry."
In 2006, Enstrom and Kabat published a meta-analysis of studies regarding passive smoking and coronary heart disease in which they reported a very weak association between passive smoking and heart disease mortality. They concluded that exposure to secondhand smoke increased the risk of death from CHD by only 5%, although this analysis has been criticized for including two previous industry-funded studies that suffered from widespread exposure misclassification.
Gori
Gio Batta Gori, a tobacco industry spokesman and consultant and an expert on risk utility and scientific research, wrote in the libertarian Cato Institute's magazine Regulation that "...of the 75 published studies of ETS and lung cancer, some 70% did not report statistically significant differences of risk and are moot. Roughly 17% claim an increased risk and 13% imply a reduction of risk."
Milloy
Steven Milloy, the "junk science" commentator for Fox News and a former Philip Morris consultant, claimed that "of the 19 studies" on passive smoking "only 8— slightly more than 42%— reported statistically significant increases in heart disease incidence."
Another component of criticism cited by Milloy focused on relative risk and epidemiological practices in studies of passive smoking. Milloy, who has a master's degree from the Johns Hopkins School of Hygiene and Public Health, argued that studies yielding relative risks of less than 2 were meaningless junk science. This approach to epidemiological analysis was criticized in the American Journal of Public Health:
A major component of the industry attack was the mounting of a campaign to establish a "bar" for "sound science" that could not be fully met by most individual investigations, leaving studies that did not meet the criteria to be dismissed as "junk science."
The tobacco industry and affiliated scientists also put forward a set of "Good Epidemiology Practices" which would have the practical effect of obscuring the link between secondhand smoke and lung cancer; the privately stated goal of these standards was to "impede adverse legislation". However, this effort was largely abandoned when it became clear that no independent epidemiological organization would agree to the standards proposed by Philip Morris et al.
Levois and Layard
In 1995, Levois and Layard, both tobacco industry consultants, published two analyses in the journal Regulatory Toxicology and Pharmacology regarding the association between spousal exposure to secondhand smoke and heart disease. Both of these papers reported no association between secondhand smoke and heart disease. These analyses have been criticized for failing to distinguish between current and former smokers, despite the fact that former smokers, unlike current ones, are not at a significantly increased risk of heart disease.
World Health Organization controversy
A 1998 study by the International Agency for Research on Cancer (IARC) on environmental tobacco smoke (ETS) found "weak evidence of a dose–response relationship between risk of lung cancer and exposure to spousal and workplace ETS."
In March 1998, before the study was published, reports appeared in the media alleging that the IARC and the World Health Organization (WHO) were suppressing information. The reports, appearing in the British Sunday Telegraph and The Economist, among other sources, alleged that the WHO withheld from publication of its own report that supposedly failed to prove an association between passive smoking and a number of other diseases (lung cancer in particular).
In response, the WHO issued a press release stating that the results of the study had been "completely misrepresented" in the popular press and were in fact very much in line with similar studies demonstrating the harms of passive smoking. The study was published in the Journal of the National Cancer Institute in October of the same year, and concluded the authors found "no association between childhood exposure to ETS and lung cancer risk" but "did find weak evidence of a dose–response relationship between risk of lung cancer and exposure to spousal and workplace ETS." An accompanying editorial summarized:
When all the evidence, including the important new data reported in this issue of the Journal, is assessed, the inescapable scientific conclusion is that ETS is a low-level lung carcinogen.
With the release of formerly classified tobacco industry documents through the Tobacco Master Settlement Agreement, it was found (by Elisa Ong and Stanton Glantz) that the controversy over the WHO's alleged suppression of data had been engineered by Philip Morris, British American Tobacco, and other tobacco companies in an effort to discredit scientific findings which would harm their business interests. A WHO inquiry, conducted after the release of the tobacco-industry documents, found that this controversy was generated by the tobacco industry as part of its larger campaign to cut the WHO's budget, distort the results of scientific studies on passive smoking, and discredit the WHO as an institution. This campaign was carried out using a network of ostensibly independent front organizations and international and scientific experts with hidden financial ties to the industry.
EPA lawsuit
In 1993, the United States Environmental Protection Agency (EPA) issued a report estimating that 3,000 lung cancer related deaths in the United States were caused by passive smoking annually.
Philip Morris, R.J. Reynolds Tobacco Company, and groups representing growers, distributors and marketers of tobacco took legal action, claiming that the EPA had manipulated this study and ignored accepted scientific and statistical practices.
The United States District Court for the Middle District of North Carolina ruled in favor of the tobacco industry in 1998, finding that the EPA had failed to follow proper scientific and epidemiologic practices and had "cherry picked" evidence to support conclusions which they had committed to in advance. The court stated in part, "EPA publicly committed to a conclusion before research had begun...adjusted established procedure and scientific norms to validate the Agency's public conclusion... In conducting the ETS Risk Assessment, disregarded information and made findings on selective information; did not disseminate significant epidemiologic information; deviated from its Risk Assessment Guidelines; failed to disclose important findings and reasoning..."
In 2002, the EPA successfully appealed this decision to the United States Court of Appeals for the Fourth Circuit. The EPA's appeal was upheld on the preliminary grounds that their report had no regulatory weight, and the earlier finding was vacated.
In 1998, the U.S. Department of Health and Human Services, through the publication by its National Toxicology Program of the 9th Report on Carcinogens, listed environmental tobacco smoke among the known carcinogens, observing of the EPA assessment that "The individual studies were carefully summarized and evaluated."
Tobacco-industry funding of research
The tobacco industry's role in funding scientific research on secondhand smoke has been controversial. A review of published studies found that tobacco-industry affiliation was strongly correlated with findings exonerating secondhand smoke; researchers affiliated with the tobacco industry were 88 times more likely than independent researchers to conclude that secondhand smoke was not harmful. In a specific example which came to light with the release of tobacco-industry documents, Philip Morris executives successfully encouraged an author to revise his industry-funded review article to downplay the role of secondhand smoke in sudden infant death syndrome. The 2006 U.S. Surgeon General's report criticized the tobacco industry's role in the scientific debate:
The industry has funded or carried out research that has been judged to be biased, supported scientists to generate letters to editors that criticized research publications, attempted to undermine the findings of key studies, assisted in establishing a scientific society with a journal, and attempted to sustain controversy even as the scientific community reached consensus.
This strategy was outlined at an international meeting of tobacco companies in 1988, at which Philip Morris proposed to set up a team of scientists, organized by company lawyers, to "carry out work on ETS to keep the controversy alive." All scientific research was subject to oversight and "filtering" by tobacco-industry lawyers:
Philip Morris then expect the group of scientists to operate within the confines of decisions taken by PM scientists to determine the general direction of research, which apparently would then be 'filtered' by lawyers to eliminate areas of sensitivity.
Philip Morris reported that it was putting "...vast amounts of funding into these projects... in attempting to coordinate and pay so many scientists on an international basis to keep the ETS controversy alive."
Tobacco industry response
Measures to tackle secondhand smoke pose a serious economic threat to the tobacco industry, having broadened the definition of smoking beyond a personal habit to something with a social impact. In a confidential 1978 report, the tobacco industry described increasing public concerns about secondhand smoke as "the most dangerous development to the viability of the tobacco industry that has yet occurred." In United States of America v. Philip Morris et al., the District Court for the District of Columbia found that the tobacco industry "... recognized from the mid-1970s forward that the health effects of passive smoking posed a profound threat to industry viability and cigarette profits," and that the industry responded with "efforts to undermine and discredit the scientific consensus that ETS causes disease."
Accordingly, the tobacco industry have developed several strategies to minimise the impact on their business:
- The industry has sought to position the secondhand smoke debate as essentially concerned with civil liberties and smokers' rights rather than with health, by funding groups such as FOREST.
- Funding bias in research; in all reviews of the effects of secondhand smoke on health published between 1980 and 1995, the only factor associated with concluding that secondhand smoke is not harmful was whether an author was affiliated with the tobacco industry. However, not all studies that failed to find evidence of harm were by industry-affiliated authors.
- Delaying and discrediting legitimate research (see for an example of how the industry attempted to discredit Takeshi Hirayama's landmark study, and for an example of how it attempted to delay and discredit a major Australian report on passive smoking)
- Promoting "good epidemiology" and attacking so-called junk science (a term popularised by industry lobbyist Steven Milloy): attacking the methodology behind research showing health risks as flawed and attempting to promote sound science. Ong & Glantz (2001) cite an internal Phillip Morris memo giving evidence of this as company policy.
- Creation of outlets for favourable research. In 1989, the tobacco industry established the International Society of the Built Environment, which published the peer-reviewed journal Indoor and Built Environment. This journal did not require conflict-of-interest disclosures from its authors. With documents made available through the Master Settlement, it was found that the executive board of the society and the editorial board of the journal were dominated by paid tobacco-industry consultants. The journal published a large amount of material on passive smoking, much of which was "industry-positive".
Citing the tobacco industry's production of biased research and efforts to undermine scientific findings, the 2006 U.S. Surgeon General's report concluded that the industry had "attempted to sustain controversy even as the scientific community reached consensus... industry documents indicate that the tobacco industry has engaged in widespread activities... that have gone beyond the bounds of accepted scientific practice." The U.S. District Court, in U.S.A. v. Philip Morris et al., found that "...despite their internal acknowledgment of the hazards of secondhand smoke, Defendants have fraudulently denied that ETS causes disease."
Position of major tobacco companies
The positions of major tobacco companies on the issue of secondhand smoke is somewhat varied. In general, tobacco companies have continued to focus on questioning the methodology of studies showing that secondhand smoke is harmful. Some (such as British American Tobacco and Philip Morris) acknowledge the medical consensus that secondhand smoke carries health risks, while others continue to assert that the evidence is inconclusive. Several tobacco companies advocate the creation of smoke-free areas within public buildings as an alternative to comprehensive smoke-free laws.
US racketeering lawsuit against tobacco companies
On September 22, 1999, the U.S. Department of Justice filed a racketeering lawsuit against Philip Morris and other major cigarette manufacturers. Almost 7 years later, on August 17, 2006, U.S. District Court Judge Gladys Kessler found that the Government had proven its case and that the tobacco company defendants had violated the Racketeer Influenced Corrupt Organizations Act (RICO). In particular, Judge Kessler found that PM and other tobacco companies had:
- conspired to minimize, distort and confuse the public about the health hazards of smoking;
- publicly denied, while internally acknowledging, that secondhand tobacco smoke is harmful to nonsmokers, and
- destroyed documents relevant to litigation.
The ruling found that tobacco companies undertook joint efforts to undermine and discredit the scientific consensus that secondhand smoke causes disease, notably by controlling research findings via paid consultants. The ruling also concluded that tobacco companies were fraudulently continuing to deny the health effects of ETS exposure.
On May 22, 2009, a three-judge panel of the U.S. Court of Appeals for the District of Columbia Circuit unanimously upheld the lower court's 2006 ruling.
Smoke-free laws
See also: Smoking ban, List of smoking bans, and Smoking bans in private vehiclesAs a consequence of the health risks associated with secondhand smoke, many national and local governments have outlawed smoking in indoor public places, including restaurants, cafés, and nightclubs, as well as some outdoor open areas. Ireland was the first country in the world to institute a comprehensive national ban on smoking in all indoor workplaces on 29 March 2004. Since then, many others have followed suit. The countries which have ratified the WHO Framework Convention on Tobacco Control (FCTC) have a legal obligation to implement effective legislation "for protection from exposure to tobacco smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places." (Article 8 of the FCTC) The parties to the FCTC have further adopted Guidelines on the Protection from Exposure to secondhand Smoke which state that "effective measures to provide protection from exposure to tobacco smoke ... require the total elimination of smoking and tobacco smoke in a particular space or environment in order to create a 100% smoke-free environment."
Opinion polls have shown considerable support for smoke-free laws. In June 2007, a survey of 15 countries found 80% approval for such laws. A survey in France, reputedly a nation of smokers, showed 70% support.
Effects
Smoking bans by governments result in decreased harm from secondhand smoke, including less admissions for acute coronary syndrome. In the first 18 months after the town of Pueblo, Colorado, enacted a smoke-free law in 2003, hospital admissions for heart attacks dropped 27%. Admissions in neighbouring towns without smoke-free laws showed no change, and the decline in heart attacks in Pueblo was attributed to the resulting reduction in secondhand smoke exposure. A 2004 smoking ban instituted in Massachusetts workplaces decreased workers' secondhand smoke exposure from 8% of workers in 2003 to 5.4% of workers in 2010. A 2016 review also found that bans and policy changes in specific locations such as hospitals or universities can lead to reduced smoking rates. In prison settings bans might lead to reduced mortality and to lower exposure to secondhand smoke.
In 2001, a systematic review for the Guide to Community Preventive Services acknowledged strong evidence of the effectiveness of smoke-free policies and restrictions in reducing expose to secondhand smoke. A follow-up to this review, identified the evidence on which the effectiveness of smoking bans reduced the prevalence of tobacco use. Articles published until 2005, were examined to further support this evidence. The examined studies provided sufficient evidence that smoke-free policies reduce tobacco use among workers when implemented in worksites or by communities.
While a number of studies funded by the tobacco industry have claimed a negative economic impact from smoke-free laws, no independently funded research has shown any such impact. A 2003 review reported that independently funded, methodologically sound research consistently found either no economic impact or a positive impact from smoke-free laws.
Air nicotine levels were measured in Guatemalan bars and restaurants before and after an implemented smoke-free law in 2009. Nicotine concentrations significantly decreased in both the bars and restaurants measured. Also, the employees' support for a smoke-free workplace substantially increased in the post-implementation survey compared to pre-implementation survey.
Public opinion
Recent surveys taken by the Society for Research on Nicotine and Tobacco demonstrate supportive attitudes of the public towards smoke-free policies in outdoor areas. A vast majority of the public supports restricting smoking in various outdoor settings. The respondents' support for the policies were for varying reasons such as litter control, establishing positive smoke-free role models for youth, reducing youth opportunities to smoke, and avoiding exposure to secondhand smoke.
Alternative forms
Alternatives to smoke-free laws have also been proposed as a means of harm reduction, particularly in bars and restaurants. For example, critics of smoke-free laws cite studies suggesting ventilation as a means of reducing tobacco smoke pollutants and improving air quality. Ventilation has also been heavily promoted by the tobacco industry as an alternative to outright bans, via a network of ostensibly independent experts with often undisclosed ties to the industry. However, not all critics have connections to the industry.
The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) officially concluded in 2005 that while completely isolated smoking rooms do eliminate the risk to nearby non-smoking areas, smoking bans are the only means of eliminating health risks associated with indoor exposure. They further concluded that no system of dilution or cleaning was effective at eliminating risk. The U.S. Surgeon General and the European Commission Joint Research Centre have reached similar conclusions. The implementation guidelines for the WHO Framework Convention on Tobacco Control states that engineering approaches, such as ventilation, are ineffective and do not protect against secondhand smoke exposure. However, this does not necessarily mean that such measures are useless in reducing harm, only that they fall short of the goal of reducing exposure completely to zero.
Others have suggested a system of tradable smoking pollution permits, similar to the cap-and-trade pollution permits systems used by the United States Environmental Protection Agency in recent decades to curb other types of pollution. This would guarantee that a portion of bars/restaurants in a jurisdiction will be smoke-free, while leaving the decision to the market.
In animals
Main article: Animals and tobacco smokeMultiple studies have been conducted to determine the carcinogenicity of environmental tobacco smoke to animals. These studies typically fall under the categories of simulated environmental tobacco smoke, administering condensates of sidestream smoke, or observational studies of cancer among pets.
To simulate environmental tobacco smoke, scientists expose animals to sidestream smoke, that which emanates from the cigarette's burning cone and through its paper, or a combination of mainstream and sidestream smoke. The IARC monographs conclude that mice with prolonged exposure to simulated environmental tobacco smoke, that is six hours a day, five days a week, for five months with a subsequent four-month interval before dissection, will have significantly higher incidence and multiplicity of lung tumors than with control groups.
The IARC monographs concluded that sidestream smoke condensates had a significantly higher carcinogenic effect on mice than did mainstream smoke condensates.
Observational studies
Secondhand smoke is popularly recognised as a risk factor for cancer in pets. A study conducted by the Tufts University School of Veterinary Medicine and the University of Massachusetts Amherst linked the occurrence of feline oral cancer to exposure to environmental tobacco smoke through an overexpression of the p53 gene. Another study conducted at the same universities concluded that cats living with a smoker were more likely to get feline lymphoma; the risk increased with the duration of exposure to secondhand smoke and the number of smokers in the household. A study by Colorado State University researchers, looking at cases of canine lung cancer, was generally inconclusive, though the authors reported a weak relation for lung cancer in dogs exposed to environmental tobacco smoke. The number of smokers within the home, the number of packs smoked in the home per day, and the amount of time that the dog spent within the home had no effect on the dog's risk for lung cancer.
See also
References
- ^ "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General" (PDF). Surgeon General of the United States. 2006-06-27. Archived from the original (PDF) on 2019-02-26. Retrieved 2012-07-24.
Secondhand smoke causes premature death and disease in children and in adults who do not smoke
- ^ IARC 2004 "There is sufficient evidence that involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) causes lung cancer in humans"
- "Tobacco". www.who.int. Retrieved 2024-02-24.
- ^ Kessler 2006
- Samet JM (2008). "Secondhand smoke: facts and lies". Salud Pública de México. 50 (5): 428–34. doi:10.1590/S0036-36342008000500016. PMID 18852940.
- ^ Tong, Elisa K.; Glantz, Stanton A. (16 October 2007). "Tobacco Industry Efforts Undermining Evidence Linking Secondhand Smoke With Cardiovascular Disease". Circulation. 116 (16): 1845–1854. doi:10.1161/CIRCULATIONAHA.107.715888. PMID 17938301. S2CID 4021497.
- "CDC - Fact Sheet - Smoke-Free Policies Reduce Smoking - Smoking & Tobacco Use". Smoking and Tobacco Use. Retrieved 2015-04-24.
- ^ Diethelm, Pascal; McKee, Martin (2006). Lifting the smokescreen: tobacco industry strategy to defeat smoke free policies and legislation (PDF). p. 5. ISBN 978-1-904097-57-0. OCLC 891398524.
The industry quickly realised that, if it wanted to continue to prosper, it became vital that research did not demonstrate that tobacco smoke was a dangerous community air pollutant. This requirement has been the central pillar of its passive smoking policy from the early 1970s to the present day
- Gourd, Katherine (2014). "Fritz Lickint". The Lancet. Respiratory Medicine. 2 (5). The Lancet: 358–359. doi:10.1016/S2213-2600(14)70064-5. PMID 24726404. Retrieved 7 December 2023.
- "Chapter 32 History of Tobacco" (PDF). www.afro.who.int. World Health Organization. 2017. Retrieved 7 December 2023.
- Brawley, Otis W.; Glynn, Thomas J.; Khuri, Fadlo R.; Wender, Richard C. (18 November 2013). "The first surgeon general's report on smoking and health: The 50th anniversary". CA. 64 (1): 5–8. doi:10.3322/caac.21210. PMID 24249254.
- "Health Effects of Exposure to Secondhand Smoke". United States Environmental Protection Agency. Archived from the original on 5 September 2015. Retrieved 6 September 2015.
- ^ Chapman, S. (1 June 2003). "Other people's smoke: what's in a name?". Tobacco Control. 12 (2): 113–4. doi:10.1136/tc.12.2.113. PMC 1747703. PMID 12773710.
- ^ Protano, Carmela; Vitali, Matteo (1 October 2011). "The New Danger of Thirdhand Smoke: Why Passive Smoking Does Not Stop at Secondhand Smoke". Environmental Health Perspectives. 119 (10): a422. doi:10.1289/ehp.1103956. PMC 3230455. PMID 21968336.
- IARC 2004, p. 1191: "During smoking of cigarettes, cigars, pipes and other tobacco productions, in addition to the mainstream smoke drawn and inhaled by the smokers, a stream of smoke is released between puffs into the air from the burning cone. Once released, this stream (also known as the sidestream smoke) is mixed with exhaled mainstream smoke as well as the air in an indoor environment to form the secondhand smoke to which ..."
- ^ California Environmental Protection Agency: Air Resources Board (24 June 2005). Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant (Report).
- Surgeon General 2006, pp. 30–46
- "Secondhand Smoke (SHS) Facts". CDC. 5 January 2021. Retrieved August 5, 2021.
- Alberg, Anthony J.; Brock, Malcolm V.; Ford, Jean G.; Samet, Jonathan M.; Spivack, Simon D. (1 May 2013). "Epidemiology of Lung Cancer". Chest. 143 (5_suppl): e1S–e29S. doi:10.1378/chest.12-2345. PMC 4694610. PMID 23649439.
- Bhatnagar, A; Whitsel, LP; Ribisl, KM; Bullen, C; Chaloupka, F; Piano, MR; Robertson, RM; McAuley, T; Goff, D; Benowitz, N; American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes, Research (14 October 2014). "Electronic cigarettes: a policy statement from the American Heart Association". Circulation. 130 (16): 1418–36. doi:10.1161/CIR.0000000000000107. PMC 7643636. PMID 25156991. S2CID 16075813.
- "Health Effects of Secondhand Smoke". November 24, 2014. Retrieved 30 May 2015.
- Pallis, Athanasios G.; Syrigos, Konstantinos N. (December 2013). "Lung cancer in never smokers: Disease characteristics and risk factors". Critical Reviews in Oncology/Hematology. 88 (3): 494–503. doi:10.1016/j.critrevonc.2013.06.011. ISSN 1040-8428. PMID 23921082.
- Macacu, Alina; Autier, Philippe; Boniol, Mathieu; Boyle, Peter (November 2015). "Active and passive smoking and risk of breast cancer: a meta-analysis" (PDF). Breast Cancer Research and Treatment. 154 (2): 213–224. doi:10.1007/s10549-015-3628-4. PMID 26546245. S2CID 4680641.
- ^ Lee, Chien-Chang; Middaugh, Nicole A.; Howie, Stephen R. C.; Ezzati, Majid (7 December 2010). "Association of Secondhand Smoke Exposure with Pediatric Invasive Bacterial Disease and Bacterial Carriage: A Systematic Review and Meta-analysis". PLOS Medicine. 7 (12): e1000374. Bibcode:2015PLoSO..1039907C. doi:10.1371/journal.pmed.1000374. PMC 4595077. PMID 21151890.
- Cumberbatch, Marcus G.; Rota, Matteo; Catto, James W.F.; La Vecchia, Carlo (September 2016). "The Role of Tobacco Smoke in Bladder and Kidney Carcinogenesis: A Comparison of Exposures and Meta-analysis of Incidence and Mortality Risks" (PDF). European Urology. 70 (3): 458–466. doi:10.1016/j.eururo.2015.06.042. PMID 26149669.
- Surgeon General 2006, Ch. 8
- Lv, X; Sun, J; Bi, Y; Xu, M; Lu, J; Zhao, L; Xu, Y (15 November 2015). "Risk of all-cause mortality and cardiovascular disease associated with secondhand smoke exposure: a systematic review and meta-analysis". International Journal of Cardiology. 199: 106–15. doi:10.1016/j.ijcard.2015.07.011. PMID 26188829.
- Dinas, PC; Koutedakis, Y; Flouris, AD (20 February 2013). "Effects of active and passive tobacco cigarette smoking on heart rate variability". International Journal of Cardiology. 163 (2): 109–15. doi:10.1016/j.ijcard.2011.10.140. PMID 22100604.
- Zou, N; Hong, J; Dai, QY (20 February 2009). "Passive cigarette smoking induces inflammatory injury in human arterial walls". Chinese Medical Journal. 122 (4): 444–448. doi:10.3760/cma.j.issn.0366-6999.2009.04.0016. PMID 19302752.
- Oono, I.P.; Mackay, D.F.; Pell, J.P. (December 2011). "Meta-analysis of the association between secondhand smoke exposure and stroke". Journal of Public Health. 33 (4): 496–502. doi:10.1093/pubmed/fdr025. PMID 21422014.
- Surgeon General 2006, pp. 555–8
- Bentayeb, Malek; Simoni, Marzia; Norback, Dan; Baldacci, Sandra; Maio, Sara; Viegi, Giovanni; Annesi-Maesano, Isabella (6 December 2013). "Indoor air pollution and respiratory health in the elderly". Journal of Environmental Science and Health, Part A. 48 (14): 1783–1789. doi:10.1080/10934529.2013.826052. PMID 24007433. S2CID 41862447.
- Dogar, O. F.; Pillai, N.; Safdar, N.; Shah, S. K.; Zahid, R.; Siddiqi, K. (November 2015). "Second-hand smoke and the risk of tuberculosis: a systematic review and a meta-analysis". Epidemiology and Infection. 143 (15): 3158–3172. doi:10.1017/S0950268815001235. PMC 9150979. PMID 26118887. S2CID 206285892.
- Hur, Kevin; Liang, Jonathan; Lin, Sandra Y. (January 2014). "The role of secondhand smoke in sinusitis: a systematic review: Sinusitis and secondhand smoke". International Forum of Allergy & Rhinology. 4 (1): 22–28. doi:10.1002/alr.21232. PMID 24574074. S2CID 9537143.
- Chen, R; Hu, Z; Orton, S; Chen, RL; Wei, L (December 2013). "Association of passive smoking with cognitive impairment in nonsmoking older adults: a systematic literature review and a new study of Chinese cohort". Journal of Geriatric Psychiatry and Neurology. 26 (4): 199–208. doi:10.1177/0891988713496165. hdl:2436/621630. PMID 23877565. S2CID 43097513.
- Ling, Jonathan; Heffernan, Thomas (24 March 2016). "The Cognitive Deficits Associated with Second-Hand Smoking". Frontiers in Psychiatry. 7: 46. doi:10.3389/fpsyt.2016.00046. PMC 4805605. PMID 27047401.
- Zeng, Yan-Ni; Li, Ya-Min (10 December 2015). "Secondhand smoke exposure and mental health in adults: a meta-analysis of cross-sectional studies". Social Psychiatry and Psychiatric Epidemiology. 51 (9): 1339–48. doi:10.1007/s00127-015-1164-5. PMID 26661619. S2CID 7772929.
- Pineles, B. L.; Park, E.; Samet, J. M. (10 February 2014). "Systematic Review and Meta-Analysis of Miscarriage and Maternal Exposure to Tobacco Smoke During Pregnancy". American Journal of Epidemiology. 179 (7): 807–823. doi:10.1093/aje/kwt334. PMC 3969532. PMID 24518810.
- Surgeon General 2006, pp. 198–205
- Cui, H; Gong, TT; Liu, CX; Wu, QJ (25 January 2016). "Associations between Passive Maternal Smoking during Pregnancy and Preterm Birth: Evidence from a Meta-Analysis of Observational Studies". PLOS ONE. 11 (1): e0147848. Bibcode:2016PLoSO..1147848C. doi:10.1371/journal.pone.0147848. PMC 4726502. PMID 26808045.
- Surgeon General 2006, pp. 194–7
- Been, Jasper; Nurmatov, U. B.; Cox, B; Nawrot, T. S.; Van Schayck, C. P.; Sheikh, A (28 March 2014). "Effect of smoke-free legislation on perinatal and child health: a systematic review and meta-analysis". Lancet. 383 (9928): 1549–60. doi:10.1016/S0140-6736(14)60082-9. PMID 24680633. S2CID 8532979.
- Leonardi-Bee, J; Britton, J; Venn, A (April 2011). "Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis". Pediatrics. 127 (4): 734–41. doi:10.1542/peds.2010-3041. PMID 21382949. S2CID 19866471.
- Salmasi G, Grady R, Jones J, McDonald SD (2010). "Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses". Acta Obstet Gynecol Scand. 89 (4): 423–41. doi:10.3109/00016340903505748. PMID 20085532. S2CID 9206564.
- Wang, Meng; Wang, Zhi-Ping; Zhang, Meng; Zhao, Zhong-Tang (13 August 2013). "Maternal passive smoking during pregnancy and neural tube defects in offspring: a meta-analysis". Archives of Gynecology and Obstetrics. 289 (3): 513–521. doi:10.1007/s00404-013-2997-3. PMID 23942772. S2CID 6526042.
- Janson C (2004). "The effect of passive smoking on respiratory health in children and adults". Int J Tuberc Lung Dis. 8 (5): 510–6. PMID 15137524.
- Saulyte, Jurgita; Regueira, Carlos; Montes-Martínez, Agustín; Khudyakov, Polyna; Takkouche, Bahi; Novotny, Thomas E. (11 March 2014). "Active or Passive Exposure to Tobacco Smoking and Allergic Rhinitis, Allergic Dermatitis, and Food Allergy in Adults and Children: A Systematic Review and Meta-Analysis". PLOS Medicine. 11 (3): e1001611. doi:10.1371/journal.pmed.1001611. PMC 3949681. PMID 24618794.
- Wei, X; E, M; Yu, S (January 2015). "A meta-analysis of passive smoking and risk of developing Type 2 Diabetes Mellitus". Diabetes Research and Clinical Practice. 107 (1): 9–14. doi:10.1016/j.diabres.2014.09.019. PMID 25488377.
- Wang, Y; Ji, J; Liu, YJ; Deng, X; He, QQ (2013). "Passive smoking and risk of type 2 diabetes: a meta-analysis of prospective cohort studies". PLOS ONE. 8 (7): e69915. Bibcode:2013PLoSO...869915W. doi:10.1371/journal.pone.0069915. PMC 3724674. PMID 23922856.
- Sun, K; Liu, D; Wang, C; Ren, M; Yang, C; Yan, L (November 2014). "Passive smoke exposure and risk of diabetes: a meta-analysis of prospective studies". Endocrine. 47 (2): 421–7. doi:10.1007/s12020-014-0194-1. PMID 24532101. S2CID 3276501.
- Pan, An; Wang, Yeli; Talaei, Mohammad; Hu, Frank B; Wu, Tangchun (December 2015). "Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis". The Lancet Diabetes & Endocrinology. 3 (12): 958–967. doi:10.1016/S2213-8587(15)00316-2. PMC 4656094. PMID 26388413.
- Akinkugbe, Aderonke A.; Slade, Gary D.; Divaris, Kimon; Poole, Charles (November 2016). "Systematic Review and Meta-analysis of the Association Between Exposure to Environmental Tobacco Smoke and Periodontitis Endpoints Among Nonsmokers". Nicotine & Tobacco Research. 18 (11): 2047–56. doi:10.1093/ntr/ntw105. PMC 5055738. PMID 27083214.
- Glantz SA, Parmley WW (1991). "Passive smoking and heart disease. Epidemiology, physiology, and biochemistry". Circulation. 83 (1): 1–12. doi:10.1161/01.cir.83.1.1. PMID 1984876.
- Taylor AE, Johnson DC, Kazemi H (1992). "Environmental tobacco smoke and cardiovascular disease. A position paper from the Council on Cardiopulmonary and Critical Care, American Heart Association". Circulation. 86 (2): 699–702. doi:10.1161/01.cir.86.2.699. PMID 1638735.
- Surgeon General 2006, pp. 376–380
- "Second-hand smoke". WHO website. Retrieved 24 April 2015.
- "The last gasp". The Economist. 19 July 2017. Retrieved 20 July 2017.
- Kantor, R; Kim, A; Thyssen, JP; Silverberg, JI (December 2016). "Association of atopic dermatitis with smoking: A systematic review and meta-analysis". Journal of the American Academy of Dermatology. 75 (6): 1119–1125.e1. doi:10.1016/j.jaad.2016.07.017. PMC 5216172. PMID 27542586.
- Anderson, HR; Cook, DG (November 1997). "Passive smoking and sudden infant death syndrome: review of the epidemiological evidence". Thorax. 52 (11): 1003–9. doi:10.1136/thx.52.11.1003. PMC 1758452. PMID 9487351.
- Surgeon General 2006, p. 194
- ^ "Secondhand Smoke and Children Fact Sheet", American Lung Association August 2006.
- Surgeon General 2006, pp. 311–9
- Vork KL, Broadwin RL, Blaisdell RJ (2007). "Developing Asthma in Childhood from Exposure to Secondhand Tobacco Smoke: Insights from a Meta-Regression". Environ. Health Perspect. 115 (10): 1394–400. doi:10.1289/ehp.10155. PMC 2022647. PMID 17938726.
- Tinuoye, O.; Pell, J. P.; Mackay, D. F. (28 March 2013). "Meta-Analysis of the Association Between Secondhand Smoke Exposure and Physician-Diagnosed Childhood Asthma". Nicotine & Tobacco Research. 15 (9): 1475–1483. doi:10.1093/ntr/ntt033. PMID 23539174.
- Wang, Zhen; May, Sara M.; Charoenlap, Suvanee; Pyle, Regan; Ott, Nancy L.; Mohammed, Khaled; Joshi, Avni Y. (November 2015). "Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis". Annals of Allergy, Asthma & Immunology. 115 (5): 396–401.e2. doi:10.1016/j.anai.2015.08.005. PMID 26411971.
- de Jongste JC, Shields MD (2003). "Cough • 2: Chronic cough in children". Thorax. 58 (11): 998–1003. doi:10.1136/thorax.58.11.998. PMC 1746521. PMID 14586058.
- Dybing E, Sanner T (1999). "Passive smoking, sudden infant death syndrome (SIDS) and childhood infections". Hum Exp Toxicol. 18 (4): 202–5. doi:10.1191/096032799678839914. PMID 10333302. S2CID 21365217.
- ^ DiFranza JR, Aligne CA, Weitzman M (2004). "Prenatal and postnatal environmental tobacco smoke exposure and children's health". Pediatrics. 113 (4 Suppl): 1007–15. doi:10.1542/peds.113.S3.1007. PMID 15060193. S2CID 248349.
- ^ Chatzimichael, A; Tsalkidis, A; Cassimos, D; Gardikis, S; Tripsianis, G; Deftereos, S; Ktenidou-Kartali, S; Tsanakas, I (June 2007). "The role of breastfeeding and passive smoking on the development of severe bronchiolitis in infants". Minerva Pediatrica. 59 (3): 199–206. PMID 17519864.
- ^ Preventing Smoking and Exposure to Secondhand Smoke Before, During, and After Pregnancy Archived 2011-09-11 at the Wayback Machine. Centers for Disease Control and Prevention. July 2007.
- Jafta, N; Jeena, PM; Barregard, L; Naidoo, RN (May 2015). "Childhood tuberculosis and exposure to indoor air pollution: a systematic review and meta-analysis". The International Journal of Tuberculosis and Lung Disease. 19 (5): 596–602. doi:10.5588/ijtld.14.0686. PMID 25868030.
- Feleszko, W; Ruszczyński, M; Jaworska, J; Strzelak, A; Zalewski, BM; Kulus, M (November 2014). "Environmental tobacco smoke exposure and risk of allergic sensitisation in children: a systematic review and meta-analysis". Archives of Disease in Childhood. 99 (11): 985–92. doi:10.1136/archdischild-2013-305444. PMID 24958794. S2CID 206856566.
- Sabbagh, HJ; Hassan, MH; Innes, NP; Elkodary, HM; Little, J; Mossey, PA (2015). "Passive smoking in the etiology of non-syndromic orofacial clefts: a systematic review and meta-analysis". PLOS ONE. 10 (3): e0116963. Bibcode:2015PLoSO..1016963S. doi:10.1371/journal.pone.0116963. PMC 4356514. PMID 25760440.
- Pagani, Linda S. (July 2014). "Environmental tobacco smoke exposure and brain development: The case of attention deficit/hyperactivity disorder". Neuroscience & Biobehavioral Reviews. 44: 195–205. doi:10.1016/j.neubiorev.2013.03.008. PMID 23545330. S2CID 20470659.
- "Scientific Consensus Statement on Environmental Agents Associated with Neurodevelopmental Disorders" (PDF). The Collaborative on Health and the Environment's Learning and Developmental Disabilities Initiative. July 1, 2008. Archived from the original (PDF) on 2009-03-27.
- Chen, Ruoling; Clifford, Angela; Lang, Linda; Anstey, Kaarin J. (October 2013). "Is exposure to secondhand smoke associated with cognitive parameters of children and adolescents?—a systematic literature review". Annals of Epidemiology. 23 (10): 652–661. doi:10.1016/j.annepidem.2013.07.001. hdl:1885/10932. PMID 23969303.
- Surgeon General 2006, pp. 293–309
- Jones, Laura L.; Hassanien, A; Cook, DG; Britton, J; Leonardi-Bee, J (1 January 2012). "Parental Smoking and the Risk of Middle Ear Disease in Children: A Systematic Review and Meta-analysis". Archives of Pediatrics & Adolescent Medicine. 166 (1): 18–27. doi:10.1001/archpediatrics.2011.158. PMID 21893640.
- Lee, Chien-Chang; Middaugh, Nicole A.; Howie, Stephen R. C.; Ezzati, Majid; Lanphear, Bruce P. (7 December 2010). "Association of Secondhand Smoke Exposure with Pediatric Invasive Bacterial Disease and Bacterial Carriage: A Systematic Review and Meta-analysis". PLOS Medicine. 7 (12): e1000374. doi:10.1371/journal.pmed.1000374. PMC 2998445. PMID 21151890.
- Chiswell, C; Akram, Y (February 2017). "Impact of environmental tobacco smoke exposure on anaesthetic and surgical outcomes in children: a systematic review and meta-analysis". Archives of Disease in Childhood. 102 (2): 123–130. doi:10.1136/archdischild-2016-310687. PMC 5284464. PMID 27417307.
- Jara, SM; Benke, JR; Lin, SY; Ishman, SL (January 2015). "The association between secondhand smoke and sleep-disordered breathing in children: a systematic review". The Laryngoscope. 125 (1): 241–7. doi:10.1002/lary.24833. PMID 25130300. S2CID 23401780.
- Raghuveer, Geetha; White, David A.; Hayman, Laura L.; Woo, Jessica G.; Villafane, Juan; Celermajer, David; Ward, Kenneth D.; de Ferranti, Sarah D.; Zachariah, Justin (18 October 2016). "Cardiovascular Consequences of Childhood Secondhand Tobacco Smoke Exposure: Prevailing Evidence, Burden, and Racial and Socioeconomic Disparities: A Scientific Statement From the American Heart Association". Circulation. 134 (16): e336–59. doi:10.1161/CIR.0000000000000443. PMC 5207215. PMID 27619923.
- Steenland, K. (1 January 1992). "Passive smoking and the risk of heart disease". JAMA. 267 (1): 94–99. doi:10.1001/jama.267.1.94. PMID 1727204.
- Law, M R; Morris, J K; Wald, N J (18 October 1997). "Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence". BMJ. 315 (7114): 973–980. doi:10.1136/bmj.315.7114.973. PMC 2127675. PMID 9365294.
- Thun, M; Henley, J; Apicella, L (December 1999). "Epidemiologic studies of fatal and nonfatal cardiovascular disease and ETS exposure from spousal smoking". Environmental Health Perspectives. 107 (suppl 6): 841–846. doi:10.1289/ehp.99107s6841. JSTOR 3434563. PMC 1566204. PMID 10592140.
- He, Jiang; Vupputuri, Suma; Allen, Krista; Prerost, Monica R.; Hughes, Janet; Whelton, Paul K. (25 March 1999). "Passive Smoking and the Risk of Coronary Heart Disease — A Meta-Analysis of Epidemiologic Studies". New England Journal of Medicine. 340 (12): 920–926. doi:10.1056/NEJM199903253401204. PMID 10089185.
- Diethelm PA, Rielle JC, McKee M (2005). "The whole truth and nothing but the truth? The research that Philip Morris did not want you to see". Lancet. 366 (9479): 86–92. doi:10.1016/S0140-6736(05)66474-4. PMID 15993237. S2CID 10442244.
- Schick S, Glantz S (2005). "Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke". Tobacco Control. 14 (6): 396–404. doi:10.1136/tc.2005.011288. PMC 1748121. PMID 16319363.
- Schick S, Glantz SA (2006). "Sidestream cigarette smoke toxicity increases with aging and exposure duration". Tobacco Control. 15 (6): 424–9. doi:10.1136/tc.2006.016162. PMC 2563675. PMID 17130369.
- Schick, S. F.; Glantz, S. (1 August 2007). "Concentrations of the Carcinogen 4-(Methylnitrosamino)-1-(3-Pyridyl)-1-Butanone in Sidestream Cigarette Smoke Increase after Release into Indoor Air: Results from Unpublished Tobacco Industry Research". Cancer Epidemiology, Biomarkers & Prevention. 16 (8): 1547–1553. doi:10.1158/1055-9965.EPI-07-0210. PMID 17684127. S2CID 690030.
- Whincup, Peter H; Gilg, Julie A; Emberson, Jonathan R; Jarvis, Martin J; Feyerabend, Colin; Bryant, Andrew; Walker, Mary; Cook, Derek G (24 July 2004). "Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement". BMJ. 329 (7459): 200–205. doi:10.1136/bmj.38146.427188.55. PMC 487731. PMID 15229131.
- Hackshaw, A K; Law, M R; Wald, N J (18 October 1997). "The accumulated evidence on lung cancer and environmental tobacco smoke". BMJ. 315 (7114): 980–988. doi:10.1136/bmj.315.7114.980. PMC 2127653. PMID 9365295.
- Copas, J B; Shi, JQ (12 February 2000). "Reanalysis of epidemiological evidence on lung cancer and passive smoking". BMJ. 320 (7232): 417–418. doi:10.1136/bmj.320.7232.417. PMC 27286. PMID 10669446.
- Takagi, Hisato; Sekino, Seishiro; Kato, Takayoshi; Matsuno, Yukihiro; Umemoto, Takuya (February 2006). "Revisiting evidence on lung cancer and passive smoking: Adjustment for publication bias by means of "trim and fill" algorithm". Lung Cancer. 51 (2): 245–246. doi:10.1016/j.lungcan.2005.11.004. PMID 16386820.
- Zhong, Lijie; Goldberg, Mark S; Parent, Marie-Élise; Hanley, James A (January 2000). "Exposure to environmental tobacco smoke and the risk of lung cancer: a meta-analysis". Lung Cancer. 27 (1): 3–18. doi:10.1016/s0169-5002(99)00093-8. PMID 10672779.
- Taylor, Richard; Gumming, Robert; Woodward, Alistair; Black, Megan (June 2001). "Passive smoking and lung cancer: a cumulative meta-analysis". Australian and New Zealand Journal of Public Health. 25 (3): 203–211. doi:10.1111/j.1467-842x.2001.tb00564.x. PMID 11494987. S2CID 25724906.
- Kim, Claire H.; Lee, Yuan-Chin Amy; Hung, Rayjean J.; McNallan, Sheila R.; Cote, Michele L.; Lim, Wei-Yen; Chang, Shen-Chih; Kim, Jin Hee; Ugolini, Donatella; Chen, Ying; Liloglou, Triantafillos; Andrew, Angeline S.; Onega, Tracy; Duell, Eric J.; Field, John K.; Lazarus, Philip; Le Marchand, Loic; Neri, Monica; Vineis, Paolo; Kiyohara, Chikako; Hong, Yun-Chul; Morgenstern, Hal; Matsuo, Keitaro; Tajima, Kazuo; Christiani, David C.; McLaughlin, John R.; Bencko, Vladimir; Holcatova, Ivana; Boffetta, Paolo; Brennan, Paul; Fabianova, Eleonora; Foretova, Lenka; Janout, Vladimir; Lissowska, Jolanta; Mates, Dana; Rudnai, Peter; Szeszenia-Dabrowska, Neonila; Mukeria, Anush; Zaridze, David; Seow, Adeline; Schwartz, Ann G.; Yang, Ping; Zhang, Zuo-Feng (15 October 2014). "Exposure to secondhand tobacco smoke and lung cancer by histological type: A pooled analysis of the International Lung Cancer Consortium (ILCCO): Secondhand tobacco smoke and lung cancer". International Journal of Cancer. 135 (8): 1918–1930. doi:10.1002/ijc.28835. PMC 4126868. PMID 24615328.
- ^ Novak K (2007). "Passive smoking: out from the haze". Nature. 447 (7148): 1049–51. Bibcode:2007Natur.447.1049N. doi:10.1038/4471049a. PMID 17597735. S2CID 9627500.
- Bailar, John C. (25 March 1999). "Passive Smoking, Coronary Heart Disease, and Meta-Analysis". New England Journal of Medicine. 340 (12): 958–959. doi:10.1056/NEJM199903253401211. PMID 10089192.
- Raupach, Tobias; Schäfer, Katrin; Konstantinides, Stavros; Andreas, Stefan (1 February 2006). "Secondhand smoke as an acute threat for the cardiovascular system: a change in paradigm". European Heart Journal. 27 (4): 386–392. doi:10.1093/eurheartj/ehi601. PMID 16230308.
- Taylor, R.; Najafi, F.; Dobson, A. (1 October 2007). "Meta-analysis of studies of passive smoking and lung cancer: effects of study type and continent". International Journal of Epidemiology. 36 (5): 1048–1059. doi:10.1093/ije/dym158. PMID 17690135.
- ^ Stayner, Leslie; Bena, James; Sasco, Annie J.; Smith, Randall; Steenland, Kyle; Kreuzer, Michaela; Straif, Kurt (March 2007). "Lung Cancer Risk and Workplace Exposure to Environmental Tobacco Smoke". American Journal of Public Health. 97 (3): 545–551. doi:10.2105/AJPH.2004.061275. PMC 1805004. PMID 17267733.
- "Health effects of indoor air pollution". Archived from the original on 2006-08-05. Retrieved 2006-07-26.
- Wirth, N.; Abou-Hamdan, K.; Spinosa, A.; Bohadana, A.; Martinet, Y. (March 2005). "Le tabagisme passif" [Passive smoking]. Revue de Pneumologie Clinique (in French). 61 (1): 7–15. doi:10.1016/s0761-8417(05)84776-5. PMID 15772574.
- ^ "France to ban smoking in public". BBC. 2006-10-08. Retrieved 2006-10-09.
- Meyers, David G.; Neuberger, John S.; He, Jianghua (September 2009). "Cardiovascular Effect of Bans on Smoking in Public Places". Journal of the American College of Cardiology. 54 (14): 1249–1255. doi:10.1016/j.jacc.2009.07.022. PMID 19778665.
- Lin, Hualiang; Wang, Hongchun; Wu, Wei; Lang, Lingling; Wang, Qinzhou; Tian, Linwei (December 2013). "The effects of smoke-free legislation on acute myocardial infarction: a systematic review and meta-analysis". BMC Public Health. 13 (1): 529. doi:10.1186/1471-2458-13-529. PMC 3671962. PMID 23721370.
- Wells, A J (July 1998). "Lung cancer from passive smoking at work". American Journal of Public Health. 88 (7): 1025–1029. doi:10.2105/ajph.88.7.1025. PMC 1508269. PMID 9663148.
- ^ Fitzsimmons, Kathleen (21 November 2013). "Reducing Worker Exposure to ETS". National Institute for Occupational Safety and Health (NIOSH). Retrieved 14 January 2015.
- Office on Smoking Health (US) (2006). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Publications and Reports of the Surgeon General. Centers for Disease Control and Prevention (US). PMID 20669524. Retrieved 2015-04-24.
- Pugmire, Juliana; Sweeting, Helen; Moore, Laurence (February 2017). "Environmental tobacco smoke exposure among infants, children and young people: now is no time to relax". Archives of Disease in Childhood. 102 (2): 117–118. doi:10.1136/archdischild-2016-311652. PMID 28100555. S2CID 41806496.
- Strachan, D P; Cook, D G (October 1997). "Health effects of passive smoking. 1. Parental smoking and lower respiratory illness in infancy and early childhood". Thorax. 52 (10): 905–914. doi:10.1136/thx.52.10.905. PMC 1758431. PMID 9404380.
- Strachan, D. P.; Cook, D. G. (1 January 1998). "Health effects of passive smoking. 4. Parental smoking, middle ear disease and adenotonsillectomy in children". Thorax. 53 (1): 50–56. doi:10.1136/thx.53.1.50. PMC 1758689. PMID 9577522.
- Song, Anna V.; Glantz, Stanton A.; Halpern-Felsher, Bonnie L. (December 2009). "Perceptions of Second-hand Smoke Risks Predict Future Adolescent Smoking Initiation". Journal of Adolescent Health. 45 (6): 618–625. doi:10.1016/j.jadohealth.2009.04.022. PMC 2814413. PMID 19931835.
- "WHO Framework Convention on Tobacco Control (WHO FCTC)". www.who.int. Retrieved 2024-06-12.
- Tsai, James; Homa, David M.; Gentzke, Andrea S.; Mahoney, Margaret; Sharapova, Saida R.; Sosnoff, Connie S.; Caron, Kevin T.; Wang, Lanqing; Melstrom, Paul C.; Trivers, Katrina F. (7 December 2018). "Exposure to Secondhand Smoke Among Nonsmokers — United States, 1988–2014". MMWR. Morbidity and Mortality Weekly Report. 67 (48): 1342–1346. doi:10.15585/mmwr.mm6748a3. PMC 6329485. PMID 30521502.
- ^ Behbod, Behrooz; Sharma, Mohit; Baxi, Ruchi; Roseby, Robert; Webster, Premila (31 January 2018). "Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke". Cochrane Database of Systematic Reviews. 1 (1): CD001746. doi:10.1002/14651858.CD001746.pub4. PMC 6491082. PMID 29383710.
- ^ Metz-Favre C, Donnay C, de Blay F (February 2005). "". Rev Mal Respir (in French). 22 (1 Pt 1): 81–92. doi:10.1016/S0761-8425(05)85439-7. PMID 15968761.
- McClure JB (April 2002). "Are biomarkers useful treatment aids for promoting health behavior change? An empirical review". Am J Prev Med. 22 (3): 200–7. doi:10.1016/S0749-3797(01)00425-1. PMID 11897465.
- Klesges RC, Debon M, Ray JW (October 1995). "Are self-reports of smoking rate biased? Evidence from the Second National Health and Nutrition Examination Survey". J Clin Epidemiol. 48 (10): 1225–33. doi:10.1016/0895-4356(95)00020-5. PMID 7561984.
- Okoli CT, Kelly T, Hahn EJ (October 2007). "Secondhand smoke and nicotine exposure: a brief review". Addict Behav. 32 (10): 1977–88. doi:10.1016/j.addbeh.2006.12.024. PMID 17270359.
- Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, Koren G (February 2009). "Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology". Ther Drug Monit. 31 (1): 14–30. doi:10.1097/FTD.0b013e3181957a3b. PMC 3644554. PMID 19125149.
- Irving JM, Clark EC, Crombie IK, Smith WC (January 1988). "Evaluation of a portable measure of expired-air carbon monoxide". Prev Med. 17 (1): 109–15. doi:10.1016/0091-7435(88)90076-X. PMID 3362796.
- Schick S, Glantz S (2005). "Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke". Tob. Control. 14 (6): 396–404. doi:10.1136/tc.2005.011288. PMC 1748121. PMID 16319363.
- Invernizzi G, Ruprecht A, Mazza R, et al. (2004). "Particulate matter from tobacco versus diesel car exhaust: an educational perspective". Tob Control. 13 (3): 219–21. doi:10.1136/tc.2003.005975. PMC 1747905. PMID 15333875.
- Barnoya J, Glantz SA (2005). "Cardiovascular effects of secondhand smoke: nearly as large as smoking". Circulation. 111 (20): 2684–98. doi:10.1161/CIRCULATIONAHA.104.492215. PMID 15911719. S2CID 2291566.
- Otsuka R, Watanabe H, Hirata K, et al. (2001). "Acute effects of passive smoking on the coronary circulation in healthy young adults". JAMA. 286 (4): 436–41. doi:10.1001/jama.286.4.436. PMID 11466122.
- Celermajer, David S.; Adams, Mark R.; Clarkson, Peter; Robinson, Jacqui; McCredie, Robyn; Donald, Ann; Deanfield, John E. (18 January 1996). "Passive Smoking and Impaired Endothelium-Dependent Arterial Dilatation in Healthy Young Adults". New England Journal of Medicine. 334 (3): 150–155. doi:10.1056/NEJM199601183340303. PMID 8531969.
- Howard, G; Thun, MJ (December 1999). "Why is environmental tobacco smoke more strongly associated with coronary heart disease than expected? A review of potential biases and experimental data". Environmental Health Perspectives. 107 (Suppl 6): 853–8. doi:10.2307/3434565. JSTOR 3434565. PMC 1566209. PMID 10592142.
- Cendon, S.P.; Battlehner, C.; Lorenzi-Filho, G.; Dohlnikoff, M.; Pereira, P.M.; Conceição, G.M.S.; Beppu, O.S.; Saldiva, P.H.N. (October 1997). "Pulmonary emphysema induced by passive smoking: an experimental study in rats". Brazilian Journal of Medical and Biological Research. 30 (10): 1241–1247. doi:10.1590/s0100-879x1997001000017. PMID 9496445.
- Eren, U.; Kum, S.; Sandikci, M.; Kara, E. (2006). "Effects of long-term passive smoking on the mast cells in rat lungs". Revue de Médecine Vétérinaire. 6: 319–322. Archived from the original on January 13, 2009.
- Matt GE, Quintana PJ, Hovell MF, et al. (March 2004). "Households contaminated by environmental tobacco smoke: sources of infant exposures". Tob Control. 13 (1): 29–37. doi:10.1136/tc.2003.003889. PMC 1747815. PMID 14985592.
- Winickoff JP, Friebely J, Tanski SE, et al. (January 2009). "Beliefs about the health effects of "thirdhand" smoke and home smoking bans". Pediatrics. 123 (1): e74–9. doi:10.1542/peds.2008-2184. PMC 3784302. PMID 19117850.
- Rabin, Roni Caryn (2009-01-02). "A New Cigarette Hazard: 'Third-Hand Smoke'". New York Times. Retrieved 2009-01-12.
- Sleiman, M.; Gundel, L. A.; Pankow, J. F.; Jacob, P.; Singer, B. C.; Destaillats, H. (13 April 2010). "Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards". Proceedings of the National Academy of Sciences. 107 (15): 6576–6581. doi:10.1073/pnas.0912820107. PMC 2872399. PMID 20142504.
- Louisiana Hospital to Ban Odor of Smoke on Workers' Clothes, Fox News, October 3, 2011
- Samet, J. M.; Avila-Tang, E.; Boffetta, P.; Hannan, L. M.; Olivo-Marston, S.; Thun, M. J.; Rudin, C. M. (15 September 2009). "Lung Cancer in Never Smokers: Clinical Epidemiology and Environmental Risk Factors". Clinical Cancer Research. 15 (18): 5626–5645. doi:10.1158/1078-0432.CCR-09-0376. PMC 3170525. PMID 19755391.
- "Environmental Tobacco Smoke" (PDF). 11th Report on Carcinogens. U.S. National Institutes of Health. Archived (PDF) from the original on 2008-07-16. Retrieved 2007-08-27.
- "Secondhand Smoke Fact Sheet". U.S. Centers for Disease Control and Prevention. 2017-02-21.
- "Health Effects of Exposure to Environmental Tobacco Smoke". U.S. National Cancer Institute. Archived from the original on 2007-09-05. Retrieved 2007-08-22.
- "Health Effects of Exposure to Secondhand Smoke". United States Environmental Protection Agency. Retrieved 2007-09-24.
- "The Truth about Secondhand Smoke". American Heart Association. Retrieved 2007-08-27.
- "Secondhand Smoke Fact Sheet". American Lung Association. Archived from the original on 2007-09-18. Retrieved 2007-09-24.
- "Secondhand Smoke". American Cancer Society. Archived from the original on 2007-09-14. Retrieved 2007-08-27.
- "AMA: Surgeon General's secondhand smoke report a wake-up call to lawmakers" (Press release). American Medical Association. Retrieved 2007-08-27.
- "Tobacco's Toll: Implications for the Pediatrician". American Academy of Pediatrics. Archived from the original on 2007-10-15. Retrieved 2007-10-02.
- "National Response to Passive Smoking in Enclosed Public Places and Workplaces" (PDF). Australian National Public Health Partnership. November 2000. Archived from the original (PDF) on 2014-02-12. Retrieved 2007-09-11.
- Two relevant reports have been published by the Scientific Committee:
- A 1998 report of the SCOTH concluded that passive smoking was a cause of lung cancer, heart disease, and other health problems.
- A 2004 update by the SCOTH Archived 2012-02-06 at the Wayback Machine, reviewing new evidence published since the 1998 report, found that recent research had confirmed the initially reported link between passive smoking and health risks.
- Surgeon General 2006, p. 588 Ch. 10
- Saad, Lydia (25 July 2007). "More Smokers Feeling Harassed by Smoking Bans". Gallup. Retrieved 20 February 2015.
- "Cato and the tobacco industry". Accessed 8 April 2011.
- Nahan, Mike. The Australian, 10 April 2000, "The IPA sings its own song".
- Shermer, Michael (May 2010). "I am a sceptic, but I'm not a denier". New Scientist. 206 (2760): 36–37. Bibcode:2010NewSc.206R..36S. doi:10.1016/S0262-4079(10)61210-9.
- Diethelm, P.; McKee, M. (16 October 2008). "Denialism: what is it and how should scientists respond?". The European Journal of Public Health. 19 (1): 2–4. doi:10.1093/eurpub/ckn139. PMID 19158101. S2CID 8098426.
- Enstrom JE, Kabat GC (2003). "Environmental tobacco smoke and tobacco related mortality in a prospective study of Californians, 1960-98". BMJ. 326 (7398): 1057. doi:10.1136/bmj.326.7398.1057. PMC 155687. PMID 12750205.
- Davey Smith G (2003). "Effect of passive smoking on health: More information is available, but the controversy still persists". BMJ. 326 (7398): 1048–9. doi:10.1136/bmj.326.7398.1048. PMC 1125974. PMID 12750182.
- Kessler 2006, p. 1383
- Tong EK, Glantz SA (2007). "Tobacco industry efforts undermining evidence linking secondhand smoke with cardiovascular disease". Circulation. 116 (16): 1845–54. doi:10.1161/CIRCULATIONAHA.107.715888. PMID 17938301. S2CID 4021497.
- "American Cancer Society Condemns Tobacco Industry Study for Inaccurate Use of Data" (PDF) (Press release). American Cancer Society. 2003-05-13. Retrieved 2007-08-29.
- Thun, Michael J (4 October 2003). "More misleading science from the tobacco industry". BMJ. 327 (7418): E237 – E238. doi:10.1136/bmjusa.03070002. S2CID 74351979.
- "Proposed Research on the relationship of Low Levels of Active Smoking to Mortality: Letter from James Enstrom to Philip Morris Scientific Affairs office". 1997-01-01. Retrieved 2007-08-29.
- Dalton R (March 2007). "Passive-smoking study faces review". Nature. 446 (7133): 242. Bibcode:2007Natur.446..242D. doi:10.1038/446242a. PMID 17361147. S2CID 27691890.
- Kessler 2006, p. 1380
- Kessler 2006, pp. 1380–3
- Bero, LA; Glantz, S; Hong, MK (April 2005). "The limits of competing interest disclosures". Tobacco Control. 14 (2): 118–26. PMC 1748015. PMID 15791022.
- Enstrom, JE; Kabat, GC (March 2006). "Environmental tobacco smoke and coronary heart disease mortality in the United States--a meta-analysis and critique". Inhalation Toxicology. 18 (3): 199–210. CiteSeerX 10.1.1.495.2191. doi:10.1080/08958370500434255. PMID 16399662. S2CID 7457133.
- Kessler 2006, p. 162
- United States of America v. Philip Morris et al., United States Factual Memorandum Pursuant to Order No. 470, Section V, United States District Court for the District of Columbia. p. 44
- ETS / IAQ SCIENTIFIC CONSULTANTS, from the Legacy Tobacco Documents Archive. Retrieved July 19, 2007.
- Gori, Gio Batta (Spring 2007). "Stoking the Rigged Terror of Secondhand Smoke" (PDF). Regulation. 30 (1): 14–7. Archived from the original (PDF) on 2009-01-16.
- Smoked Out: Pundit for Hire, by Paul D. Thacker. Published in The New Republic on January 26, 2006. Retrieved August 22, 2007.
- Philip Morris budget for "Strategy and Social Responsibility", listing Milloy as a paid consultant. Retrieved August 22, 2007.
- "Secondhand Joking", by Steven Milloy. Retrieved May 31, 2013.
- Samet JM, Burke TA (2001). "Turning Science Into Junk: The Tobacco Industry and Passive Smoking". Am J Public Health. 91 (11): 1742–4. doi:10.2105/AJPH.91.11.1742. PMC 1446866. PMID 11684591.
- Scientific Communications Through the Media, from the Philip Morris document archive. Retrieved October 3, 2007. Also cited in Ong, Elisa K.; Glantz, Stanton A. (November 2001). "Constructing 'Sound Science' and 'Good Epidemiology': Tobacco, Lawyers, and Public Relations Firms". American Journal of Public Health. 91 (11): 1749–1757. doi:10.2105/ajph.91.11.1749. PMC 1446868. PMID 11684593.
- ^ Ong EK, Glantz SA (2001). "Constructing "Sound Science" and "Good Epidemiology": Tobacco, Lawyers, and Public Relations Firms". Am J Public Health. 91 (11): 1749–57. doi:10.2105/AJPH.91.11.1749. PMC 1446868. PMID 11684593.
- Layard, M.W. (February 1995). "Ischemic Heart Disease and Spousal Smoking in the National Mortality Followback Survey". Regulatory Toxicology and Pharmacology. 21 (1): 180–183. doi:10.1006/rtph.1995.1022. PMID 7784629.
- Levois, M.E.; Layard, M.W. (February 1995). "Publication Bias in the Environmental Tobacco Smoke/Coronary Heart Disease Epidemiologic Literature". Regulatory Toxicology and Pharmacology. 21 (1): 184–191. doi:10.1006/rtph.1995.1023. PMID 7784630.
- Law, Malcolm R; Wald, Nicholas J (July 2003). "Environmental tobacco smoke and ischemic heart disease". Progress in Cardiovascular Diseases. 46 (1): 31–38. doi:10.1016/s0033-0620(03)00078-1. PMID 12920699.
- ^ Boffetta, Paolo; Agudo, Antonio; Ahrens, Wolfgang; Benhamou, Ellen; Benhamou, Simone; Darby, Sarah C.; Ferro, Gilles; Fortes, Cristina; Gonzalez, Carlos A.; Jöckel, Karl-Heinz; Krauss, Martin; Kreienbrock, Lothar; Kreuzer, Michaela; Mendes, Anabela; Merletti, Franco; Nyberg, Fredrik; Pershagen, Göran; Pohlabeln, Hermann; Riboli, Elio; Schmid, Giovanni; Simonato, Lorenzo; Tre'daniel, Jean; Whitley, Elise; Wichmann, Heinz-Erich; Winck, Carlos; Zambon, Paola; Saracci, Rodolfo (7 October 1998). "Multicenter Case-Control Study of Exposure to Environmental Tobacco Smoke and Lung Cancer in Europe". JNCI: Journal of the National Cancer Institute. 90 (19): 1440–1450. doi:10.1093/jnci/90.19.1440. PMID 9776409.
- "Passive Smoking Doesn't Cause Cancer —Official". Archived from the original on 2007-10-13.
- "Smokescreens – The World Health Organization is showing signs of allowing politics to get in the way of truth. The Economist March 14th, 1998" (PDF). Archived from the original (PDF) on 2007-11-29.
- Le Grand C. Anti-smokers blown away by study. Australian 1998, March 10.
- WHO Rejects smoking link with lung cancer. Zimbabwe Independent 1998, Oct 23.
- No Link Between Passive Smoking and Lung Cancer. The Times 1998, March 9.
- "Passive smoking does cause lung cancer, do not let them fool you". The Ceylon Medical Journal. 43 (2): 98. June 1998. PMID 9704550.
- Blot, William J.; McLaughlin, Joseph K. (7 October 1998). "Passive Smoking and Lung Cancer Risk: What Is the Story Now?". JNCI: Journal of the National Cancer Institute. 90 (19): 1416–1417. doi:10.1093/jnci/90.19.1416. PMID 9776401.
- Ong EK, Glantz SA (2000). "Tobacco industry efforts subverting International Agency for Research on Cancer's second-hand smoke study". Lancet. 355 (9211): 1253–9. doi:10.1016/S0140-6736(00)02098-5. PMID 10770318. S2CID 25145666.
- "Tobacco Companies Strategies to Undermine Tobacco Control Activities at the World Health Organization" (PDF). Archived from the original (PDF) on 2004-08-21. Retrieved 2008-12-30.
- US Environmental Protection Agency. "Respiratory health effects of passive smoking: Lung cancer and other disorders".
- "The Osteen Decision". Archived from the original on 2000-08-15.
- "Flue-Cured Tobacco Cooperative vs. EPA" (PDF). Archived from the original (PDF) on 2008-10-09. Retrieved 2008-12-30.
- U.S. Department of Health; Human Services; National Toxicology Program, eds. (December 2–3, 1998). "Final Report on Carcinogens – Background Document for Environmental Tobacco Smoke". Meeting of the NTP Board of Scientific Counselors – Report on Carcinogens Subcommittee (PDF). Research Triangle Park, North Carolina. p. 24. Archived from the original (PDF) on 2007-11-29.
{{cite book}}: CS1 maint: location missing publisher (link) - Thun MJ (2003). "Passive smoking: Tobacco industry publishes disinformation". BMJ. 327 (7413): 502–3, author reply 504–5. doi:10.1136/bmj.327.7413.502-c. PMC 188400. PMID 12946979.
- ^ Barnes DE, Bero LA (1998). "Why review articles on the health effects of passive smoking reach different conclusions". JAMA. 279 (19): 1566–70. doi:10.1001/jama.279.19.1566. PMID 9605902.
- Tong EK, England L, Glantz SA (2005). "Changing conclusions on secondhand smoke in a sudden infant death syndrome review funded by the tobacco industry". Pediatrics. 115 (3): e356–66. doi:10.1542/peds.2004-1922. PMID 15741361. S2CID 33226933.
- "The Health Consequences of Involuntary Exposure to Tobacco Smoke" (PDF). Executive Summary. Surgeon General of the United States. 2006. p. 21. Retrieved 2009-01-28.
- ^ "Minutes of a meeting of Philip Morris with British tobacco companies to discuss tobacco-industry strategy on passive smoking". Archived from the original on 2007-10-13. Retrieved 2007-08-27.
- A Study of Public Attitudes toward Cigarette Smoking and the Tobacco Industry in 1978, produced for the Tobacco Institute and released under the terms of the Tobacco Master Settlement Agreement.
- Smith, E. A.; Malone, R. E. (5 January 2007). "'We will speak as the smoker': the tobacco industry's smokers' rights groups". The European Journal of Public Health. 17 (3): 306–313. doi:10.1093/eurpub/ckl244. PMC 2794244. PMID 17065174.
- Trotter L, Chapman S (2003). ""Conclusions about exposure to ETS and health that will be unhelpful to us"*: How the tobacco industry attempted to delay and discredit the 1997 Australian National Health and Medical Research Council report on passive smoking". Tob Control. 12 (Suppl 3:iii): 102–6. doi:10.1136/tc.12.suppl_3.iii102. PMC 1766130. PMID 14645955.
- Garne D, Watson M, Chapman S, Byrne F (2005). "Environmental tobacco smoke research published in the journal Indoor and Built Environment and associations with the tobacco industry". Lancet. 365 (9461): 804–9. doi:10.1016/S0140-6736(05)17990-2. PMID 15733724. S2CID 23160158.
- ^ "The Health Consequences of Involuntary Exposure to Tobacco Smoke" (PDF). Executive Summary. Surgeon General of the United States. 2006. Retrieved 2009-01-28.
- Kessler 2006, p. 1523
- The most current positions of major tobacco companies on the issue of passive smoking can be found on their websites. As of 13 January 2009, the following websites contain tobacco-industry positions on the topic:
- British American Tobacco:
- Imperial Tobacco: "Imperial Tobacco Group PLC - Media - Our view - Smoking and health - Environmental tobacco smoke". Archived from the original on 2009-01-16. Retrieved 2008-10-25.
- Philip Morris: USA Archived 2010-10-06 at the Wayback Machine and International
- R. J. Reynolds Tobacco Company: "R.J. Reynolds Tobacco Company - Smoking & Health - Summary of Opinions". Archived from the original on 2006-11-18. Retrieved 2006-11-19.
- Litigation Against Tobacco Companies U.S. Department of Justice
- Appeal Ruling, U.S. Court of Appeals for the District of Columbia Circuit, 22 May 2009
- Altria, Cigarette Makers Lose 'Lights' Ruling Appeal Bloomberg news, 22 May 2009
- U.S. appeals court agrees tobacco companies lied Reuters, 22 May 2009
- Smokers Daring Bloomberg To Ticket Them Under Park Ban Archived 2013-11-26 at the Wayback Machine
- "WHO Framework Convention on Tobacco Control" (PDF). World Health Organization. 2005-02-27. Retrieved 2009-01-12.
Parties recognize that scientific evidence has unequivocally established that exposure to tobacco causes death, disease and disability
- ^ "Guidelines on the Protection from Exposure to Secondhand Smoke" (PDF). Framework Convention on Tobacco Control. World Health Organization. 2007. Retrieved 2009-01-29.
- Market Research World
- Frazer, Kate; Callinan, Joanne E; McHugh, Jack; van Baarsel, Susan; Clarke, Anna; Doherty, Kirsten; Kelleher, Cecily (4 February 2016). "Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption". Cochrane Database of Systematic Reviews. 2016 (2): CD005992. doi:10.1002/14651858.CD005992.pub3. PMC 6486282. PMID 26842828.
- Centers for Disease Control and Prevention (CDC) (January 2009). "Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance—City of Pueblo, Colorado, 2002–2006". MMWR Morb. Mortal. Wkly. Rep. 57 (51): 1373–7. PMID 19116606.
- Frazer, Kate; McHugh, Jack; Callinan, Joanne E; Kelleher, Cecily (27 May 2016). "Impact of institutional smoking bans on reducing harms and secondhand smoke exposure". Cochrane Database of Systematic Reviews. 2016 (5): CD011856. doi:10.1002/14651858.CD011856.pub2. PMC 10164285. PMID 27230795.
- Hopkins DP, Razi S, Leeks KD, Priya Kalra G, Chattopadhyay SK, Soler RE (2010). "Smokefree policies to reduce tobacco use. A systematic review". Am J Prev Med. 38 (2 Suppl): S275–89. doi:10.1016/j.amepre.2009.10.029. PMID 20117612.
- Scollo M, Lal A, Hyland A, Glantz S (Mar 2003). "Review of the quality of studies on the economic effects of smoke-free policies on the hospitality industry". Tobacco Control. 12 (1): 13–20. doi:10.1136/tc.12.1.13. PMC 1759095. PMID 12612356.
- Barnoya J, Arvizu M, Jones MR, Hernandez JC, Breysse PN, Navas-Acien A (November 2010). "Secondhand smoke exposure in bars and restaurants in Guatemala City: before and after smoking ban evaluation". Cancer Causes Control. 22 (1): 151–6. doi:10.1007/s10552-010-9673-8. PMID 21046446. S2CID 673901.
- Thomson, George; Wilson, Nick; Edwards, Richard (June 2009). "At the frontier of tobacco control: A brief review of public attitudes toward smoke-free outdoor places". Nicotine & Tobacco Research. 11 (6): 584–590. doi:10.1093/ntr/ntp046. PMID 19359392.
- "No ifs or butts". Building. 7 March 2005.
- Drope J, Bialous SA, Glantz SA (March 2004). "Tobacco industry efforts to present ventilation as an alternative to smoke-free environments in North America". Tob Control. 13 (Suppl 1): i41–7. doi:10.1136/tc.2003.004101. PMC 1766145. PMID 14985616.
The industry developed a network of ventilation 'experts' to promote its position that smoke-free environments were not necessary, often without disclosing the financial relationship between these experts and the industry.
- "ASHRAE Position Document on Environmental Tobacco Smoke" (PDF). American Society of Heating, Refrigerating and Air-Conditioning Engineers. July 2020.
- "Institute for Health and Consumer Protection Activity Report 2003" (PDF). European Commission Joint Research Centre. 2003. Archived from the original (PDF) on March 27, 2009. Retrieved 2009-01-28.
- Haveman, Robert; John Mullahy (September 25, 2005). "Let Bars Buy, Sell Smoking Permits". Wisconsin State Journal. p. B2. Archived from the original on January 4, 2009. Retrieved 2009-01-28.
- Thompson, Andrea (2007-08-31). "Secondhand Smoke Causes Cancer in Pets". LiveScience. Retrieved 2007-08-31.
- Snyder LA, Bertone ER, Jakowski RM, Dooner MS, Jennings-Ritchie J, Moore AS (2004). "p53 expression and environmental tobacco smoke exposure in feline oral squamous cell carcinoma". Vet Pathol. 41 (3): 209–14. doi:10.1354/vp.41-3-209. PMID 15133168. S2CID 24749614.
- Bertone ER, Snyder LA, Moore AS (2002). "Environmental Tobacco Smoke and Risk of Malignant Lymphoma in Pet Cats". American Journal of Epidemiology. 156 (3): 268–273. doi:10.1093/aje/kwf044. PMID 12142262.
- Reif JS, Dunn K, Ogilvie GK, Harris CK (1992). "Passive smoking and canine lung cancer risk". Am J Epidemiol. 135 (3): 234–9. doi:10.1093/oxfordjournals.aje.a116276. PMID 1546698.
External links
- Scientific bodies
- Health Effects of Exposure to Environmental Tobacco Smoke, from the U.S. National Cancer Institute
- "Environmental Tobacco Smoke" (PDF). Archived (PDF) from the original on 2008-07-16. (219 KB). From the 11th Report on Carcinogens of the U.S. National Institutes of Health
- U.S. Dept. of Health and Human Services; Centers for Disease Control and Prevention; Coordinating Center for Health Promotion; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health (2006-06-27). "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General". Publications and Reports of the Surgeon General. Atlanta, Ga.: Surgeon General of the United States. PMID 20669524. O2NLM: WA 754 H4325 2006.
Secondhand smoke exposure causes disease and premature death in children and adults who do not smoke
{{cite journal}}: Cite journal requires|journal=(help) - World Health Organization; International Agency for Research on Cancer (2004). Tobacco Smoke and Involuntary Smoking (PDF). IARC monographs on the evaluation of carcinogenic risks to humans. Vol. 83. Lyon, France: IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. ISBN 978-92-832-1283-6.
- Secondhand Smoke Fact Sheet from the U.S. Centers for Disease Control and Prevention
- Tobacco Smoke in the Workplace from the U.S. Centers for Disease Control and Prevention
- Health Effects of Exposure to Environmental Tobacco Smoke, from the California Environmental Protection Agency
- Environmental Tobacco Smoke Exposure in Children Aged 3-19 Years with and Without Asthma in the United States, 1999-2010 National Center for Health Statistics
- Öberg, Mattias; Jaakkola, Maritta S; Woodward, Alistair; Peruga, Armando; Prüss-Ustün, Annette (January 2011). "Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries". The Lancet. 377 (9760): 139–146. doi:10.1016/S0140-6736(10)61388-8. PMID 21112082. S2CID 7179156.
- Tobacco industry
- "Tobacco Company Strategies to Undermine Tobacco Control Activities" (PDF). Archived from the original (PDF) on August 21, 2004. Retrieved October 5, 2020. (1.55 MB): Report of the Committee of Experts on Tobacco Industry Documents from the World Health Organization
- The Legacy Tobacco Documents Library and British American Tobacco Documents Archive from the University of California, San Francisco
- Philip Morris USA Document Archive, made public as a result of the Tobacco Master Settlement Agreement
- Other links
- Guidelines Protection from Exposure to Secondhand Smoke, by WHO Framework Convention on Tobacco Control
- WHO Policy recommendations on protection from exposure to second-hand tobacco smoke
- Small, Elysia; Shah, Hina P.; Davenport, Jake J.; Geier, Jacqueline E.; Yavarovich, Kate R.; Yamada, Hidetaka; Sabarinath, Sreedharan N.; Derendorf, Hartmut; Pauly, James R.; Gold, Mark S.; Bruijnzeel, Adrie W. (January 2010). "Tobacco smoke exposure induces nicotine dependence in rats". Psychopharmacology. 208 (1): 143–158. doi:10.1007/s00213-009-1716-z. PMC 3586198. PMID 19936715.
- Kessler, Gladys (August 17, 2006). "United States of America v. Philip Morris et al.: Final Opinion of Judge Gladys Kessler" (PDF). United States District Court for the District of Columbia.
- "How Secondhand Cigarette Smoke Changes Your Genes"
| Cigarettes | |||
|---|---|---|---|
| Types | |||
| Components | |||
| Peripherals | |||
| Culture | |||
| Health issues | |||
| Related products | |||
| Tobacco industry |
| ||
| Government and the law | |||
| Lists | |||
| Heating, ventilation, and air conditioning | |
|---|---|
| Fundamental concepts |
|
| Technology |
|
| Components |
|
| Measurement and control |
|
| Professions, trades, and services |
|
| Industry organizations | |
| Health and safety |
|
| See also | |
| Recreational drug use | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||