| Revision as of 23:52, 8 November 2008 editFritzpoll (talk | contribs)Extended confirmed users12,706 editsm Reverted edits by 68.198.88.43 to last version by Fritzpoll (HG)← Previous edit | Latest revision as of 18:33, 29 October 2024 edit undoAadirulez8 (talk | contribs)Extended confirmed users43,495 editsm v2.05 - Fix errors for CW project (Reference before punctuation)Tag: WPCleaner | ||
| Line 1: | Line 1: | ||
| {{Short description|Illness from eating spoiled food}} | |||
| {{Use mdy dates|date=February 2015}} | |||
| {{Food safety}} | {{Food safety}} | ||
| {{For|the disease most commonly referred to as food poisoning|Salmonellosis}} | |||
| '''Foodborne illness''' (also known as '''foodborne disease''' and '''food poisoning''')<ref> | |||
| {{DorlandsDict|nine/000952820|food poisoning}} | |||
| </ref> is any ] resulting from the ] by pathogenic ], ]es, or ]s,<ref name=CDC>{{cite web | |||
| |url=https://www.cdc.gov/ncidod/dbmd/diseaseinfo/foodborneinfections_g.htm | |||
| |access-date=3 July 2016 | |||
| |title=Foodborne Illness - Frequently Asked Questions | |||
| |publisher=US Centers for Disease Control and Prevention | |||
| |url-status=dead | |||
| |archive-url=https://web.archive.org/web/20110303025929/http://www.cdc.gov/ncidod/dbmd/diseaseinfo/foodborneinfections_g.htm | |||
| |archive-date=March 3, 2011 | |||
| }} | |||
| </ref> as well as ] (the agents of ]), and ]s such as ]s in peanuts, ], and various species of ] that have not been boiled for at least 10 minutes. | |||
| Symptoms vary depending on the cause. They often include ], ], and aches, and may include ]. Bouts of vomiting can be repeated with an extended delay in between. This is because even if infected food was eliminated from the stomach in the first bout, ]s, like bacteria (if applicable), can pass through the ] into the ] and begin to multiply. Some types of microbes stay in the intestine. | |||
| There are two types of food poisoning: food infection and food intoxication. Food infection refers to the presence of bacteria or other microbes whose ] affect the body. Food intoxication only requires the presence of the bacteria's ] to affect the body, while the microbe that produced the toxin is no longer present or able to cause infection. In spite of the common term food poisoning, most cases are caused by a variety of ]ic ], ]es, ]s or ]s that contaminate food,<ref></ref> rather than chemical or natural ]s. | |||
| For contaminants requiring an ], symptoms may not manifest for hours to days, depending on the cause and on the quantity of consumption. Longer incubation periods tend to cause those affected to not associate the symptoms with the item consumed, so they may misattribute the symptoms to ], for example. | |||
| ==Causes== | ==Causes== | ||
| {{see also|Pathogen}} | |||
| Foodborne illness usually arises from improper handling, preparation, or ]. Good ] practices before, during, and after food preparation can reduce the chances of contracting an illness. The action of monitoring food to ensure that it will not cause foodborne illness is known as ''']'''. Foodborne disease can also be caused by a large variety of toxins that affect the environment. For foodborne illness caused by chemicals, see ]. | |||
| ] | |||
| Foodborne illness usually arises from improper handling, preparation, or ]. Good ] practices before, during, and after food preparation can reduce the chances of contracting an illness. There is a consensus in the public health community that regular hand-washing is one of the most effective defenses against the spread of foodborne illness. The action of monitoring food to ensure that it will not cause foodborne illness is known as ]. Foodborne disease can also be caused by a large variety of toxins that affect the environment.<ref>For foodborne illness caused by chemicals, see ].</ref> | |||
| Furthermore, foodborne illness can be caused by a number of chemicals, such as ]s, ]s, and natural toxic substances such as ], ] or ].<ref>{{cite web|url=https://www.fda.gov/food/chemicals-metals-pesticides-food | title = Chemicals, Metals & Pesticides in Food |website = ] | date= 2021 }}</ref> | |||
| ==Symptoms and mortality== | |||
| ]s typically begin several hours to several days after consumption and depending on the agent involved, can include one or more of the following: ], ], ], ], ], ], ] or ]. | |||
| In most cases the body is able to permanently recover after a short period of ] discomfort and illness. However, foodborne illness can result in permanent health problems or even death, especially for people at high risk, including ], young children, ] women (and their ]es), ] people, ] people and others with weak ]s. | |||
| Foodborne illness is a major cause of ], which typically occurs 1–3 weeks afterward. Similarly, people with ] disease are especially susceptible to infections from ], which can be found in ]s or crabs. | |||
| ] poisoning from reef fish and other animals manifests rapidly as ] and ], and is often fatal. | |||
| ==Incubation period== | |||
| The delay between consumption of a contaminated food and appearance of the first ]s of illness is called the ]. This ranges from hours to days (and rarely months or even years, such as in the case of ] or ]), depending on the agent, and on how much was consumed. If symptoms occur within 1–6 hours after eating the food, it suggests that it is caused by a bacterial toxin or a chemical rather than live bacteria. | |||
| The long incubation period of many foodborne illnesses tends to cause sufferers to attribute their symptoms to "]." | |||
| During the incubation period, ]s pass through the ] into the ], attach to the ]s lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a ] that is absorbed into the ]stream, and some can directly invade the deeper body tissues. The symptoms produced depend on the type of microbe.<ref>{{cite web|url=http://www.cdc.gov/ncidod/diseases/food/index.htm |title=Food-Related Diseases}}</ref> | |||
| ==Infectious dose== | |||
| The infectious dose is the amount of agent that must be consumed to give rise to symptoms of foodborne illness, and varies according to the agent and the consumer's age and overall health. In the case of ] a relatively large inoculum of 1 million to 1 billion organisms is necessary to produce symptoms in healthy human volunteers, as Salmonellae are very sensitive to acid. An unusually high stomach pH level (low acidity) greatly reduces the number of bacteria required to cause symptoms by a factor of between 10 and 100. | |||
| ==Pathogenic agents== | |||
| {{see also|Pathogen}} | |||
| ===Bacteria=== | ===Bacteria=== | ||
| ] are a common cause of foodborne illness. In the ] |
] are a common cause of foodborne illness. In 2000, the ] reported the individual bacteria involved as the following: '']'' 77.3%, '']'' 20.9%, ] 1.4%, and all others less than 0.56%.<ref>{{cite web | ||
| |url=http://food.gov.uk/enforcement/regulation/betregs/ria/ria2011/controllingecoliia2011 | |||
| |access-date=14 August 2016 | |||
| |title=Reducing the risk from ''E. coli'' 0157 – controlling cross-contamination | |||
| |publisher=Food Standards Agency, United Kingdom | |||
| |date=February 2011 | |||
| |url-status=bot: unknown | |||
| |archive-url=https://web.archive.org/web/20140416193433/http://food.gov.uk/enforcement/regulation/betregs/ria/ria2011/controllingecoliia2011 | |||
| |archive-date=April 16, 2014 | |||
| |df=mdy | |||
| }} | |||
| </ref> | |||
| In the past, bacterial infections were thought to be more prevalent because few places had the capability to test for ] and no active surveillance was being done for this particular agent. Toxins from bacterial infections are delayed because the bacteria need time to multiply. As a result, symptoms associated with intoxication are usually not seen until 12–72 hours or more after eating contaminated food. However, in some cases, such as Staphylococcal food poisoning, the onset of illness can be as soon as 30 minutes after ingesting contaminated food.<ref>{{cite web|url=https://www.cdc.gov/foodsafety/diseases/staphylococcal.html |title=Staphylococcal Food Poisoning |access-date=3 July 2016 |publisher=U.S. Centers for Disease Control and Prevention}}</ref> | |||
| '''Most common''' bacterial foodborne pathogens are: | |||
| *'']'' which can lead to secondary ] and ]<ref name=cazp>{{cite journal | |||
| | last = Humphrey | |||
| | first = Tom ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Campylobacters as zoonotic pathogens: A food production perspective <internet> | |||
| | journal = International Journal of Food Microbiology | |||
| | volume = 117 | |||
| | issue = 3 | |||
| | publisher = | |||
| | doi = 10.1016 | |||
| |date=2007 | |||
| | url = http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T7K-4N0PPRG-1&_user=10&_coverDate=07%2F15%2F2007&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=74b7c07635a1873ca815b3139b56d2e0 | |||
| | doi_brokendate = 2008-06-21}}</ref> | |||
| *'']'', the "cafeteria germ"<ref name=USDA> {{cite web | |||
| | title = Foodborne Illness: What Consumers | |||
| Need to Know | |||
| | last = USDA | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | accessyear = 2008 | |||
| | url = http://www.fsis.usda.gov/Fact_Sheets/Foodborne_Illness_What_Consumers_Need_to_Know/index.asp | |||
| | publisher = }}</ref> | |||
| *'']'' spp. - its ''S. Typhimurium'' infection is caused by consumption of eggs that are not adequately cooked or by other interactive human-animal pathogens<ref name=aoostpt>{{cite web | |||
| | last = Tribe | |||
| | first = Ingrid G. ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = An outbreak of Salmonella Typhimurium phage type 135 infection linked to the consumption of raw shell eggs in an aged care facility <internet> | |||
| | publisher = | |||
| | accessdaymonth = 29 August | |||
| | accessyear = 2008 | |||
| | url = http://www.health.gov.au/internet/main/Publishing.nsf/Content/cda-pubs-cdi-2002-cdi2601-cdi2601h.htm}}</ref><ref name=sisaa>{{cite web | |||
| | last = Centers for Disease Control and Prevention | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Salmonella Infection (salmonellosis) and Animals <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.cdc.gov/healthypets/diseases/salmonellosis.htm}}</ref><ref name=rcfp>{{cite web | |||
| | last = Doyle | |||
| | first = M. P. | |||
| | authorlink = | |||
| | coauthors = M. C. Erickson | |||
| | title = Reducing the carriage of foodborne pathogens in livestock and poultry <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.poultryscience.org/ps/paperpdfs/06/p0660960.pdf}}</ref> | |||
| *'']'' enterohemorrhagic (EHEC) which causes ] | |||
| ] | |||
| Other '''common''' bacterial foodborne pathogens are: | |||
| A 2022 study concluded that washing uncooked chicken could increase the risk of ] transfer, and that specific washing conditions can decrease the risk of transfer.<ref>{{Cite web |last1=Chemistry |first1=University of |last2=Prague |first2=Technology |title=Chickensplash! Exploring the health concerns of washing raw chicken |url=https://phys.org/news/2022-09-chickensplash-exploring-health-raw-chicken.html |access-date=2022-10-03 |website=phys.org |language=en}}</ref><ref>{{cite journal | vauthors = Carmody CD, Mueller RC, Grodner BM, Chlumsky O, Wilking JN, McCalla SG | title = Chickensplash! Exploring the health concerns of washing raw chicken | journal = Physics of Fluids | volume = 34 | issue = 3 | pages = 031910 | date = March 2022 | pmid = 35392485 | pmc = 8958727 | doi = 10.1063/5.0083979 | bibcode = 2022PhFl...34c1910C }}</ref> | |||
| *'']'' | |||
| *'']'', other ], such as enteroinvasive (EIEC), enteropathogenic (EPEC), enterotoxigenic (ETEC), enteroaggregative (EAEC or EAgEC) | |||
| ] | |||
| *'']'' | |||
| *'']'' spp. | |||
| *'']'' | |||
| *'']'' | |||
| *'']'', including O1 and non-O1 | |||
| *'']'' | |||
| *'']'' | |||
| *'']'' and '']'' | |||
| Most common bacterial foodborne pathogens are: | |||
| * '']'' which can lead to secondary ] and ]<ref name=cazp>{{cite journal | vauthors = Humphrey T, O'Brien S, Madsen M | title = Campylobacters as zoonotic pathogens: a food production perspective | journal = International Journal of Food Microbiology | volume = 117 | issue = 3 | pages = 237–257 | date = July 2007 | pmid = 17368847 | doi = 10.1016/j.ijfoodmicro.2007.01.006 }}</ref> | |||
| *'']'' spp. | |||
| * '']'', the "cafeteria germ"<ref name=USDA> | |||
| *'']'' | |||
| {{cite web| title = Foodborne Illness: What Consumers Need to Know| work = USDA.gov| access-date = 14 August 2016| url = http://www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/get-answers/food-safety-fact-sheets/foodborne-illness-and-disease/foodborne-illness-what-consumers-need-to-know/CT_Index}} | |||
| *'']'' or Q fever | |||
| </ref><ref>{{cite journal | vauthors = Kiu R, Caim S, Painset A, Pickard D, Swift C, Dougan G, Mather AE, Amar C, Hall LJ | display-authors = 6 | title = Phylogenomic analysis of gastroenteritis-associated ''Clostridium perfringens'' in England and Wales over a 7-year period indicates distribution of clonal toxigenic strains in multiple outbreaks and extensive involvement of enterotoxin-encoding (CPE) plasmids | journal = Microbial Genomics | volume = 5 | issue = 10 | pages = e000297 | date = October 2019 | pmid = 31553300 | pmc = 6861862 | doi = 10.1099/mgen.0.000297 | doi-access = free }}</ref> | |||
| *'']'' | |||
| * '']'' ] – its ''S. typhimurium'' infection is caused by consumption of eggs or poultry that are not adequately cooked or by other interactive human-animal pathogens<ref name=aoostpt> | |||
| {{cite journal | vauthors = Tribe IG, Cowell D, Cameron P, Cameron S | title = An outbreak of Salmonella typhimurium phage type 135 infection linked to the consumption of raw shell eggs in an aged care facility | journal = Communicable Diseases Intelligence Quarterly Report | volume = 26 | issue = 1 | pages = 38–39 | year = 2002 | pmid = 11950200 | url = https://www.health.gov.au/internet/main/publishing.nsf/Content/cda-pubs-cdi-2002-cdi2601-cdi2601h.htm | url-status = dead | archive-url = https://web.archive.org/web/20140217035354/https://www.health.gov.au/internet/main/publishing.nsf/Content/cda-pubs-cdi-2002-cdi2601-cdi2601h.htm | archive-date = February 17, 2014 }} | |||
| </ref><ref name=sisaa>{{cite web| work = Centers for Disease Control and Prevention| title = Salmonella Infection (salmonellosis) and Animals| access-date = August 12, 2007| url = https://www.cdc.gov/healthypets/diseases/salmonellosis.htm| archive-url = https://web.archive.org/web/20070704172311/http://www.cdc.gov/healthypets/diseases/salmonellosis.htm| archive-date = July 4, 2007| url-status = dead}}</ref><ref name=rcfp>{{cite journal | vauthors = Doyle MP, Erickson MC | title = Reducing the carriage of foodborne pathogens in livestock and poultry | journal = Poultry Science | volume = 85 | issue = 6 | pages = 960–973 | date = June 2006 | pmid = 16776463 | doi = 10.1093/ps/85.6.960 | doi-access = free }}</ref> | |||
| * '']'' enterohemorrhagic (EHEC) which can cause ] | |||
| Other common bacterial foodborne pathogens are:<ref>{{cite web|url=https://www.cdc.gov/foodsafety/foodborne-germs.html | author = CDC | title = Foodborne Germs and Illnesses| date = March 18, 2020}}</ref> | |||
| ====Exotoxins==== | |||
| * '']'' | |||
| In addition to disease caused by direct bacterial infection, some foodborne illnesses are caused by ]s which are ] by the cell as the bacterium grows. Exotoxins can produce illness even when the microbes that produced them have been killed. Symptoms typically appear after 1–6 hours depending on the amount of toxin ingested. | |||
| * '']'', other ], such as enteroinvasive (EIEC), enteropathogenic (EPEC), enterotoxigenic (ETEC), enteroaggregative (EAEC or EAgEC) | |||
| * '']'' | |||
| * '']'' spp. | |||
| * '']'' | |||
| * '']'' | |||
| * '']'', including O1 and non-O1 | |||
| * '']'' | |||
| * '']'' | |||
| * '']'' and '']'' | |||
| Less common bacterial agents:{{citation needed|date=January 2021}} | |||
| *'']'' | |||
| *'']'' | * '']'' spp. | ||
| *'']'' | * '']'' | ||
| * '']'' or Q fever | |||
| *'']'' | |||
| * '']'' | |||
| ==== Enterotoxins ==== | |||
| For example '']'' produces a toxin that causes intense ]. The rare but potentially deadly disease ] occurs when the ] bacterium '']'' grows in improperly canned low-acid foods and produces ], a powerful paralytic toxin. The disease of MMS was recently diagnosed for the first time in the United States in Tucson, Arizona. Symptoms include nausea, fatigue and excessive vomiting. This disease is caused from eating meat sticks that are past an acceptable shelf life. | |||
| {{see also|Botulism}} | |||
| In addition to disease caused by direct bacterial infection, some foodborne illnesses are caused by ]s (]s targeting the intestines). Enterotoxins can produce illness even when the microbes that produced them have been killed. Symptom onset varies with the toxin but may be rapid in onset, as in the case of enterotoxins of '']'' in which symptoms appear in one to six hours.<ref>. Mayo Clinic.</ref> This causes intense ] including or not including diarrhea (resulting in ]), and staphylococcal enterotoxins (most commonly ] but also including ]) are the most commonly reported enterotoxins although cases of poisoning are likely underestimated.<ref name=Staph>{{cite journal | vauthors = Argudín MÁ, Mendoza MC, Rodicio MR | title = Food poisoning and Staphylococcus aureus enterotoxins | journal = Toxins | volume = 2 | issue = 7 | pages = 1751–1773 | date = July 2010 | pmid = 22069659 | pmc = 3153270 | doi = 10.3390/toxins2071751 | doi-access = free }}</ref> It occurs mainly in cooked and processed foods due to competition with other biota in raw foods, and humans are the main cause of contamination as a substantial percentage of humans are persistent carriers of ''S. aureus''.<ref name=Staph/> The CDC has estimated about 240,000 cases per year in the United States.<ref>. Ohio State University Extension HYG-5564-11].</ref> | |||
| Pseudoalteromonas tetraodonis, certain species of ] and ], and some other bacteria, produce the lethal ], which is present in the ]s of some living animal species rather than being a product of ]. | |||
| * '']'' | |||
| * '']'' | |||
| * '']'' | |||
| The rare but potentially deadly disease ] occurs when the ] bacterium '']'' grows in improperly canned low-acid foods and produces ], a powerful paralytic toxin.{{cn|date=August 2023}} | |||
| === Mycotoxins and alimentary mycotoxicoses === | |||
| The term '''alimentary mycotoxicoses''' refers to the effect of poisoning by ] through food consumption. ] have prominently affected on human and animal health such as an outbreak which occurred in the UK in 1960 that caused the death of 100,000 turkeys which had consumed ]-contaminated peanut meal and the death of 5000 human lives by Alimentary toxic aleukia (ALA) in the ] in ]<ref name=fam>{{cite web | |||
| | last = E. Mount | |||
| | first = Michael | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Fungi and Mycotoxins <internet> | |||
| | publisher = | |||
| | accessdaymonth = 11 August | |||
| | accessyear = 2007 | |||
| | url = http://www.vetmed.ucdavis.edu/PHR/PHR250/2007/25007Myc.pdf}}</ref>. The common foodborne ] include | |||
| ''Pseudoalteromonas tetraodonis'', certain species of '']'' and '']'', and some other bacteria, produce the lethal ], which is present in the ] of some living animal species rather than being a product of ].{{citation needed|date=January 2021}} | |||
| * ] - originated from ] and ]. They are frequently found in tree nuts, peanuts, maize, sorghum and other oilseeds, including corn and cottonseeds. The pronounced forms of ] are those of B1, B2, G1, and G2, amongst which Aflatoxin B1 predominantly targets the liver, which will result in ], ], and ] <ref name=afltx>{{cite web | |||
| | last = Center for Food Safety & Applied Nutrition | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Aflatoxins <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.cfsan.fda.gov/~mow/chap41.html}}</ref><sup>,</sup> <ref name=gtlmg>{{cite web | |||
| | last = Food and Agriculture Organization of the United Nations | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = GASGA Technical Leaflet - 3 Mycotoxins in Grain <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fao.org/Wairdocs/X5008E/X5008e01.htm}}</ref>. In the US, the acceptable level of total aflatoxins in foods is less than 20 μg/kg, except for Aflatoxin M1 in milk, which should be less than 0.5 μg/kg <ref name=cfh>{{cite web | |||
| | last = World Health Organization | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Chapter 2 Foodborne Hazards in ''Basic Food Safety for Health Workers'' <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.who.int/entity/foodsafety/publications/capacity/en/2.pdf}}</ref>. The official document can be found at ]'s website <ref name=sec683100>{{cite web | |||
| | last = Food and Drug Administration | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Sec. 683.100 Action Levels for Aflatoxins in Animal Feeds (CPG 7126.33) <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fda.gov/ora/compliance_ref/cpg/cpgvet/cpg683-100.html}}</ref><sup>,</sup> <ref name=mfcvmp>{{cite web | |||
| | last = Henry | |||
| | first = Michael H. | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Mycotoxins in Feeds: CVM’s Perspective <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fda.gov/cvm/fdaaustintx823.htm}}</ref>. | |||
| * Altertoxins - are those of ] (AOH), Alternariol methyl ether (AME), Altenuene (ALT), Altertoxin-1 (ATX-1), Tenuazonic acid (TeA) and Radicinin (RAD), originated from ] spp. Some of the toxins can be present in sorghum, ], wheat and tomatoes <ref name=atwdw>{{cite web | |||
| | last = Webley | |||
| | first = D. J. ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Alternaria toxins in weather-damaged wheat and sorghum in the 1995-1996 Australian harvest <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.publish.csiro.au/paper/A97005.htm}}</ref><sup>,</sup> <ref name=amwwc>{{cite web | |||
| | last = Li | |||
| | first = Feng-qin | |||
| | authorlink = | |||
| | coauthors = Takumi Yoshizawa | |||
| | title = Alternaria Mycotoxins in Weathered Wheat from China <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://pubs.acs.org/cgi-bin/abstract.cgi/jafcau/2000/48/i07/abs/jf0000171.html}}</ref><sup>,</sup> <ref name=sbtp>{{cite web | |||
| | last = da Motta | |||
| | first = Silvana | |||
| | authorlink = | |||
| | coauthors = Lucia M. Valente Soares | |||
| | title = Survey of Brazilian tomato products for alternariol, alternariol monomethyl ether, tenuazonic acid and cyclopiazonic acid <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.informaworld.com/smpp/content~content=a713810863~db=all}}</ref>. Some research has shown that the toxins can be easily cross-contaminated between grain commodities, suggesting that manufacturing and storage of grain commodities is a critical practice <ref name=pamaa>{{cite web | |||
| | last = Li | |||
| | first = F. Q. ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Production of Alternaria Mycotoxins by Alternaria alternata Isolated from Weather-Damaged Wheat <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.ingentaconnect.com/content/iafp/jfp/2001/00000064/00000004/art00025}}</ref>. | |||
| * Citrinin - | |||
| * Citreoviridin - | |||
| * ] - | |||
| * ] | |||
| * ] / ] ] - ] | |||
| * ] - Crop corn can be easily contaminated by the fungi ], and its ] will cause Leukoencephalomalacia (LEM) in horses, Pulmonary edema syndrome (PES) in pigs, liver cancer in rats and ] in humans <ref name=ftihah>{{cite web | |||
| | last = Marasas | |||
| | first = Walter F. O. | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Fumonisins: Their implications for human and animal health <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www3.interscience.wiley.com/cgi-bin/abstract/112640083/ABSTRACT?CRETRY=1&SRETRY=0}}</ref><sup>,</sup> <ref name=off>{{cite web | |||
| | last = Soriano | |||
| | first = J.M. | |||
| | authorlink = | |||
| | coauthors = S. Dragacci | |||
| | title = Occurrence of fumonisins in foods <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T6V-4D636PW-1&_user=10&_coverDate=01%2F01%2F2004&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=4a033a232e75e4ebf3ee269c06744491}}</ref>. For human and animal health, both the ] and the ] have regulated the content levels of toxins in food and animal feed <ref name=CVMF>{{cite web | |||
| | last = Food and Drug Administration | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = CVM and Fumonisins <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fda.gov/cvm/fumonisin.htm}}</ref><sup>,</sup> <ref name=mcmmp>{{cite web | |||
| | last = Food Standards Agency | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = More contaminated maize meal products withdrawn from sale <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.food.gov.uk/news/newsarchive/2003/sep/moremaize}}</ref>. | |||
| * Fusaric acid - | |||
| * Fusarochromanone - | |||
| * ] - | |||
| * Lolitrem alkaloids - | |||
| * Moniliformin - | |||
| * 3-Nitropropionic acid - | |||
| * Nivalenol - | |||
| * ] - In Australia, The Limit of Reporting (LOR) level for ] (OTA) analyses in 20th Australian Total Diet Survey was 1 µg/kg <ref name=2atds>{{cite web | |||
| | last = Food Standards Australia New Zealand | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = 20th Australian Total Diet Survey - Part B <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.foodstandards.gov.au/newsroom/publications/20thaustraliantotaldietsurveyjanuary2003/20thaustraliantotaldietsurveyfullreport/partb20thatds/partbmetals.cfm}}</ref>, whereas the ] restricts the content of OTA to 5 µg/kg in cereal commodities, 3 µg/kg in processed products and 10 µg/kg in dried vine fruits <ref name=wrmff>{{cite web | |||
| | last = FAO FOOD AND NUTRITION PAPER 81 | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Worldwide regulations for mycotoxins in food and feed in 2003 <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fao.org/docrep/007/y5499e/y5499e0f.htm}}</ref>. | |||
| * Oosporeine - | |||
| * ] - Currently, this toxin has been advisably regulated on fruit products. The ] and the ] have limited it to under 50 µg/kg for fruit juice and fruit nectar, while limits of 25 µg/kg for solid-contained fruit products and 10 µg/kg for baby foods were specified by the ] <ref name=wrmff>{{cite web | |||
| | last = FAO FOOD AND NUTRITION PAPER 81 | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Worldwide regulations for mycotoxins in food and feed in 2003 <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.fao.org/docrep/007/y5499e/y5499e0f.htm}}</ref><sup>,</sup> <ref name=pajajc>{{cite web | |||
| | last = Food and Drug Administration | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Patulin in Apple Juice, Apple Juice Concentrates and Apple Juice Products <internet> | |||
| | publisher = | |||
| | accessdaymonth = 16 August | |||
| | accessyear = 2007 | |||
| | url = http://vm.cfsan.fda.gov/~dms/patubckg.html}}</ref> | |||
| * Phomopsins - | |||
| * Sporidesmin A - | |||
| * ] - | |||
| * Tremorgenic ] - Five of them have been reported to be associated with molds found in fermented meats. These are Fumitremorgen B, Paxilline, ], Verrucosidin, and Verruculogen <ref name=gaftm>{{cite web | |||
| | last = Sabater-Vilar | |||
| | first = M. | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Genotoxicity Assessment of Five Tremorgenic Mycotoxins (Fumitremorgen B, Paxilline, Penitrem A, Verruculogen, and Verrucosidin) Produced by Molds Isolated from Fermented Meats <internet> | |||
| | publisher = | |||
| | accessdaymonth = 16 August | |||
| | accessyear = 2007 | |||
| | url = http://www.ingentaconnect.com/content/iafp/jfp/2003/00000066/00000011/art00023}}</ref>. | |||
| * ] - sourced from Cephalosporium, ], Myrothecium, ] and ]. The toxins are usually found in molded maize, wheat, corn, peanuts and rice, or animal feed of hay and straw <ref name=ofst>{{cite web | |||
| | last = Adejumo | |||
| | first = Timothy O. | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Occurrence of Fusarium species and trichothecenes in Nigerian maize <internet> | |||
| | publisher = Elsevier | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T7K-4N5CX4H-3&_user=10&_coverDate=05%2F30%2F2007&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=d02d1b28456dfbef669d57692ac28244}}</ref><sup>,</sup> <ref name=snhe>{{cite web | |||
| | last = Mazur | |||
| | first = Lynnette J. | |||
| | authorlink = | |||
| | coauthors = Janice Kim | |||
| | title = Spectrum of Noninfectious Health Effects From Molds <internet> | |||
| | publisher = American Academy of Pediatrics | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://pediatrics.aappublications.org/cgi/content/full/118/6/e1909}}</ref>. Four trichothecenes, T-2 toxin, HT-2 toxin, diacetoxyscirpenol (DAS) and ] (DON) have been most commonly encountered by humans and animals. The consequences of oral intake of, or dermal exposure to, the toxins will result in Alimentary toxic aleukia, ], ], ] and/or skin irritaion <ref name=tthm>{{cite web | |||
| | last = Froquet | |||
| | first = R. ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Trichothecene toxicity on human megakaryocyte progenitors (CFU-MK) <internet> | |||
| | publisher = SAGE Publications | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://het.sagepub.com/cgi/content/abstract/20/2/84}}</ref><sup>,</sup> <ref name=csytt>{{cite web | |||
| | last = Joffe | |||
| | first = A. Z. | |||
| | authorlink = | |||
| | coauthors = B. Yagen | |||
| | title = Comparative study of the yield of T-2 toxic produced by Fusarium poae, F. sporotrichioides and F. sporotrichioides var. tricinctum strains from different sources <internet> | |||
| | publisher = SAGE Publications | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://het.sagepub.com/cgi/content/abstract/20/2/84}}</ref><sup>,</sup> <ref name=fis>{{cite web | |||
| | last = Hay | |||
| | first = Rod J. | |||
| | authorlink = | |||
| | coauthors = B. Yagen | |||
| | title = Fusarium infections of the skin <internet> | |||
| | publisher = | |||
| | accessdaymonth = 12 August | |||
| | accessyear = 2007 | |||
| | url = http://www.co-infectiousdiseases.com/pt/re/coinfdis/abstract.00001432-200704000-00002.htm;jsessionid=G2JGL27MSRdb4TS82LyckCgxLH2zJLX3ynBfjz5kjMyfh4WpVkLg!1152499061!181195629!8091!-1}}</ref>. In 1993, the ] issued a document for the content limits of DON in food and animal feed at an advisory level <ref name=gifda>{{cite web | |||
| | last = Food and Drug Administration | |||
| | first = | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Guidance for Industry and FDA - Letter to State Agricultural Directors, State Feed Control Officials, and Food, Feed, and Grain Trade Organizations <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.cfsan.fda.gov/~dms/graingui.html}}</ref>. In 2003, US published a patent that is very promising for farmers to produce a trichothecene-resistant crop <ref name=trtp>{{cite web | |||
| | last = Hohn | |||
| | first = Thomas M. | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Trichothecene-resistant transgenic plants <internet> | |||
| | publisher = | |||
| | accessdaymonth = 13 August | |||
| | accessyear = 2007 | |||
| | url = http://www.patentstorm.us/patents/6646184.html}}</ref>. | |||
| * ] - | |||
| * Zearalenols - | |||
| ====Emerging foodborne pathogens==== | ====Emerging foodborne pathogens==== | ||
| * '']'', ''Aeromonas caviae'', ''Aeromonas sobria'' | |||
| Much is still not known about foodborne illness. Approximately sixty percent of outbreaks are still caused by unknown sources. | |||
| Scandinavian outbreaks of '']'' have recently increased to an annual basis, connected to the non-canonical contamination of pre-washed salad.<ref>{{cite journal | vauthors = Karlsson PA, Tano E, Jernberg C, Hickman RA, Guy L, Järhult JD, Wang H | title = Molecular Characterization of Multidrug-Resistant ''Yersinia enterocolitica'' From Foodborne Outbreaks in Sweden | journal = Frontiers in Microbiology | volume = 12 | pages = 664665 | date = 2021-05-13 | pmid = 34054769 | pmc = 8155512 | doi = 10.3389/fmicb.2021.664665 | doi-access = free }}</ref> | |||
| *'']'', ''Aeromonas caviae'', ''Aeromonas sobria'' | |||
| ====Preventing bacterial food poisoning==== | ====Preventing bacterial food poisoning==== | ||
| ] of ] help in the prevention of food poisoning.]]Governments have the primary mandate of ensuring safe food for all, however all actors in the food chain are responsible to ensure only safe food reaches the consumer, thus preventing foodborne illnesses. This is achieved through the implementation of strict hygiene rules and a public veterinary and phytosanitary service that monitors animal products throughout the ], from farming to delivery in shops and restaurants. This regulation includes: | |||
| * ]: |
* ]: the origin of the ingredients (farm of origin, identification of the crop or animal) and where and when it has been processed must be known in the final product; in this way, the origin of the disease can be traced and resolved (and possibly penalized), and the final products can be removed from sale if a problem is detected; | ||
| * enforcement of hygiene procedures |
* enforcement of hygiene procedures such as ] and the "]"; | ||
| * power of control and of law enforcement of ]s. | * power of control and of law enforcement of ]s. | ||
| In August 2006, the United States ] approved ] which involves spraying meat with viruses that infect bacteria, and thus preventing infection. This has raised concerns |
In August 2006, the United States ] approved ] which involves spraying meat with viruses that infect bacteria, and thus preventing infection. This has raised concerns because without ], consumers would not know that meat and poultry products have been treated with the spray.<ref>{{cite news| url=https://www.forbes.com/business/healthcare/feeds/ap/2006/08/18/ap2959720.html |title=FDA Says Viruses Safe for Treating Meat |archive-url=https://web.archive.org/web/20060825040502/http://www.forbes.com/business/healthcare/feeds/ap/2006/08/18/ap2959720.html|archive-date=August 25, 2006|access-date=September 2, 2014}}</ref> | ||
| At home, prevention mainly consists of good ] practices. Many forms of bacterial poisoning can be prevented |
At home, prevention mainly consists of good ] practices. Many forms of bacterial poisoning can be prevented by cooking food sufficiently, and either eating it quickly or refrigerating it effectively.<ref name=CDC/> Many toxins, however, are not destroyed by heat treatment. | ||
| Techniques that help prevent food borne illness in the kitchen are hand washing, rinsing ],<ref>{{Cite web|url=http://minnesota.cbslocal.com/2010/11/09/good-question-does-washing-fruit-do-anything/|title=Good Question: Does Washing Fruit Do Anything? |last=DeRusha |first=Jason | name-list-style = vanc |access-date=2016-09-18|date=2010-11-09}}</ref> preventing cross-contamination, proper storage, and maintaining cooking temperatures. In general, freezing or refrigerating prevents virtually all bacteria from growing, and heating food sufficiently kills parasites, viruses, and most bacteria. Bacteria grow most rapidly at the range of temperatures between {{convert|40|and|140|°F|°C}}, called the "danger zone". Storing food below or above the "danger zone" can effectively limit the production of toxins. For storing leftovers, the food must be put in shallow containers | |||
| for quick cooling and must be refrigerated within two hours. When food is reheated, it must reach an internal temperature of {{convert|165|F|C}} or until hot or steaming to kill bacteria.<ref>. U.D. Department of Agriculture</ref> | |||
| === Mycotoxins and alimentary mycotoxicoses === | |||
| The term ] refers to the effect of poisoning by ]s through food consumption. The term mycotoxin is usually reserved for the toxic chemical compounds naturally produced by fungi that readily colonize crops under given temperature and moisture conditions. Mycotoxins can have important effects on human and animal health. For example, an outbreak which occurred in the UK during 1960 caused the death of 100,000 turkeys which had consumed ]-contaminated peanut meal. In the ] in ], 5,000 people died due to ] (ALA).<ref name=fam>{{cite web| last = Mount| first = Michael | name-list-style = vanc | title = Fungi and Mycotoxins| publisher = vetmed.ucdavis.edu| access-date = August 11, 2007| url = http://www.vetmed.ucdavis.edu/PHR/PHR250/2007/25007Myc.pdf| archive-url = https://web.archive.org/web/20070927001355/http://www.vetmed.ucdavis.edu/PHR/PHR250/2007/25007Myc.pdf| archive-date = September 27, 2007| url-status = dead}}</ref> In Kenya, mycotoxins led to the death of 125 people in 2004, after consumption of contaminated grains.<ref>{{cite web | url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5334a4.htm | title=Outbreak of Aflatoxin Poisoning --- Eastern and Central Provinces, Kenya, January--July 2004 }}</ref> In animals, mycotoxicosis targets organ systems such as liver and digestive system. Other effects can include reduced productivity and suppression of the immune system, thus pre-disposing the animals to other secondary infections.<ref>{{cite journal | doi=10.3390/pr9112035 | doi-access=free | title=Mycotoxins—Prevention, Detection, Impact on Animal Health | date=2021 | last1=Kępińska-Pacelik | first1=Jagoda | last2=Biel | first2=Wioletta | journal=Processes | volume=9 | issue=11 | page=2035 }}</ref> | |||
| The common foodborne ] include: | |||
| * ]s – originating from '']'' and '']''. They are frequently found in tree nuts, peanuts, maize, sorghum and other oilseeds, including corn and cottonseeds. The pronounced forms of aflatoxins are those of B1, B2, G1, and G2, amongst which Aflatoxin B1 predominantly targets the liver, which will result in ], ], and ]. Other forms of aflatoxins exist as ] such as Aflatoxin M1.<ref name=afltx> | |||
| {{cite web| work= Center for Food Safety & Applied Nutrition| title = Aflatoxins | access-date = August 12, 2007| url = https://www.fda.gov/Food/FoodSafety/FoodborneIllness/FoodborneIllnessFoodbornePathogensNaturalToxins/BadBugBook/ucm071020.htm}}</ref><ref name="gtlmg">{{cite web|url=http://www.fao.org/Wairdocs/X5008E/X5008e01.htm|title=GASGA Technical Leaflet – 3 Mycotoxins in Grain|work=Food and Agriculture Organization of the United Nations|archive-url=https://web.archive.org/web/20170112143005/http://www.fao.org/Wairdocs/X5008E/X5008e01.htm|archive-date=January 12, 2017|access-date=August 12, 2007}}</ref> In the US, the acceptable level of total aflatoxins in foods is less than 20'' ''μg/kg, except for Aflatoxin M1 in milk, which should be less than 0.5'' ''μg/kg The official document can be found at ]'s website.<ref name=sec683100>{{cite web| work = Food and Drug Administration| title = Sec. 683.100 Action Levels for Aflatoxins in Animal Feeds (CPG 7126.33) | access-date = August 13, 2007| url = https://www.fda.gov/ora/compliance_ref/cpg/cpgvet/cpg683-100.html}}</ref><ref name=mfcvmp>{{cite web| last = Henry| first = Michael H. | name-list-style = vanc | title = Mycotoxins in Feeds: CVM's Perspective|work=FDA.gov| access-date = January 1, 2012| url = https://www.fda.gov/AnimalVeterinary/Products/AnimalFoodFeeds/Contaminants/ucm050974.htm}}</ref> The European union has more stringent standards, set at 10 μg/kg in cereals and cereal products. These references are also adopted in other countries.<ref>{{cite journal | doi=10.2903/sp.efsa.2013.EN-406 | title=Aflatoxins (Sum of B1, B2, G1, G2) in cereals and cereal-derived food products | journal=EFSA Supporting Publications | date=2013 | volume=10 | issue=3 | doi-access=free }}</ref><ref name=cfh> | |||
| {{cite web| work = World Health Organization| title = Chapter 2 Foodborne Hazards in ''Basic Food Safety for Health Workers'' | access-date = August 12, 2007| url =https://www.who.int/entity/foodsafety/publications/capacity/en/2.pdf| archive-url =https://wayback.archive-it.org/all/20070927001355/http://www.who.int/entity/foodsafety/publications/capacity/en/2.pdf| url-status =dead| archive-date =September 27, 2007}}</ref> | |||
| * ]s – are those of ] (AOH), ] (AME), ] (ALT), ] (ATX-1), ] (TeA), and ] (RAD), originating from '']'' spp. Some of the toxins can be present in sorghum, ], wheat and tomatoes.<ref name=atwdw> | |||
| {{cite journal |vauthors=Webley DJ, Jackson KL, Mullins JD, Hocking AD, Pitt JI |title=''Alternaria'' toxins in weather-damaged wheat and sorghum in the 1995–1996 Australian harvest |journal=Australian Journal of Agricultural Research |volume=48 |issue=8 |pages=1249–56 |year=1997 |doi=10.1071/A97005 }}</ref><ref name=amwwc>{{cite journal | vauthors = Li FQ, Yoshizawa T | title = Alternaria mycotoxins in weathered wheat from China | journal = Journal of Agricultural and Food Chemistry | volume = 48 | issue = 7 | pages = 2920–2924 | date = July 2000 | pmid = 10898645 | doi = 10.1021/jf0000171 }}</ref><ref name=sbtp>{{cite journal | vauthors = Motta SD, Valente Soares LM | title = Survey of Brazilian tomato products for alternariol, alternariol monomethyl ether, tenuazonic acid and cyclopiazonic acid | journal = Food Additives and Contaminants | volume = 18 | issue = 7 | pages = 630–634 | date = July 2001 | pmid = 11469319 | doi = 10.1080/02652030117707 | s2cid = 45938351 }}</ref> Some research has shown that the toxins can be easily cross-contaminated between grain commodities, suggesting that manufacturing and storage of grain commodities is a critical practice.<ref name=pamaa>{{cite journal | vauthors = Li FQ, Toyazaki N, Yoshizawa T | title = Production of alternaria mycotoxins by Alternaria alternata isolated from weather-damaged wheat | journal = Journal of Food Protection | volume = 64 | issue = 4 | pages = 567–571 | date = April 2001 | pmid = 11307900 | doi = 10.4315/0362-028X-64.4.567 | doi-access = free }} | |||
| </ref> | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ]s | |||
| * ]s / ] ] – ] | |||
| * ]s – Crop corn can be easily contaminated by the fungi '']'', and its ] will cause ] (LEM) in horses, ] (PES) in pigs, liver cancer in rats and ] in humans.<ref name=ftihah>{{cite journal | vauthors = Marasas WF | title = Fumonisins: their implications for human and animal health | journal = Natural Toxins | volume = 3 | issue = 4 | pages = 193–8; discussion 221 | year = 1995 | pmid = 7582616 | doi = 10.1002/nt.2620030405 }}</ref><ref name=off>{{cite journal |doi=10.1016/j.foodres.2004.06.009 | title=Occurrence of fumonisins in foods | journal=Food Research International | date=2004 | volume=37 | issue=10 | pages=985–1000 | vauthors = Soriano JM }}</ref> For human and animal health, both the ] and the ] have regulated the content levels of toxins in food and animal feed.<ref name=CVMF>{{cite web| work = Food and Drug Administration| title = CVM and Fumonisins | access-date = August 13, 2007| url = https://www.fda.gov/cvm/fumonisin.htm |archive-url = https://web.archive.org/web/20070812000712/https://www.fda.gov/cvm/fumonisin.htm <!-- Bot retrieved archive --> |archive-date = August 12, 2007}}</ref><ref name=mcmmp>{{cite web| work = Food Standards Agency| title = More contaminated maize meal products withdrawn from sale| access-date = August 12, 2007| url = http://www.food.gov.uk/news/newsarchive/2003/sep/moremaize| archive-date = August 13, 2007| archive-url = https://web.archive.org/web/20070813075444/http://www.food.gov.uk/news/newsarchive/2003/sep/moremaize| url-status = dead}}</ref> | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ]s | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ]s – In Australia, The Limit of Reporting (LOR) level for ] (OTA) analyses in 20th Australian Total Diet Survey was 1 μg/kg,<ref name=2atds>{{cite web| work = Food Standards Australia New Zealand| title = 20th Australian Total Diet Survey – Part B| access-date = August 13, 2007| url = http://www.foodstandards.gov.au/newsroom/publications/20thaustraliantotaldietsurveyjanuary2003/20thaustraliantotaldietsurveyfullreport/partb20thatds/partbmetals.cfm| archive-url = https://web.archive.org/web/20070902112319/http://www.foodstandards.gov.au/newsroom/publications/20thaustraliantotaldietsurveyjanuary2003/20thaustraliantotaldietsurveyfullreport/partb20thatds/partbmetals.cfm| archive-date = September 2, 2007| url-status = dead}}</ref> whereas the ] restricts the content of OTA to 5 μg/kg in cereal commodities, 3 μg/kg in processed products and 10 μg/kg in dried vine fruits.<ref name=wrmff>{{cite web| work = FAO FOOD AND NUTRITION PAPER 81| title = Worldwide regulations for mycotoxins in food and feed in 2003 | access-date = August 13, 2007| url = http://www.fao.org/docrep/007/y5499e/y5499e0f.htm}}</ref> | |||
| * ] | |||
| * ] – Currently, this toxin has been advisably regulated on fruit products. The ] and the ] have limited it to under 50 μg/kg for fruit juice and fruit nectar, while limits of 25 μg/kg for solid-contained fruit products and 10 μg/kg for baby foods were specified by the EC.<ref name="wrmff"/><ref name=pajajc>{{cite web| work = Food and Drug Administration| title = Patulin in Apple Juice, Apple Juice Concentrates and Apple Juice Products| access-date = August 16, 2007| url = http://vm.cfsan.fda.gov/~dms/patubckg.html| archive-url = https://web.archive.org/web/20070912062502/http://vm.cfsan.fda.gov/~dms/patubckg.html| archive-date = September 12, 2007| url-status = dead}}</ref> | |||
| * ]s | |||
| * ] | |||
| * ] | |||
| * Tremorgenic mycotoxins – Five of them have been reported to be associated with molds found in fermented meats. These are ], ], ], ], and ].<ref name=gaftm>{{cite journal | vauthors = Sabater-Vilar M, Nijmeijer S, Fink-Gremmels J | title = Genotoxicity assessment of five tremorgenic mycotoxins (fumitremorgen B, paxilline, penitrem A, verruculogen, and verrucosidin) produced by molds isolated from fermented meats | journal = Journal of Food Protection | volume = 66 | issue = 11 | pages = 2123–2129 | date = November 2003 | pmid = 14627292 | doi = 10.4315/0362-028X-66.11.2123 | doi-access = free }}</ref> | |||
| * ]s – sourced from ''Cephalosporium'', '']'', ''Myrothecium'', '']'', and '']''. The toxins are usually found in molded maize, wheat, corn, peanuts and rice, or animal feed of hay and straw.<ref name=ofst>{{cite journal | vauthors = Adejumo TO, Hettwer U, Karlovsky P | title = Occurrence of Fusarium species and trichothecenes in Nigerian maize | journal = International Journal of Food Microbiology | volume = 116 | issue = 3 | pages = 350–357 | date = May 2007 | pmid = 17412440 | doi = 10.1016/j.ijfoodmicro.2007.02.009 }}</ref><ref name=snhe> | |||
| {{cite journal | vauthors = Mazur LJ, Kim J | title = Spectrum of noninfectious health effects from molds | journal = Pediatrics | volume = 118 | issue = 6 | pages = e1909–e1926 | date = December 2006 | pmid = 17142508 | doi = 10.1542/peds.2006-2829 | doi-access = free }}</ref> Four trichothecenes, ], ], ] (DAS), and ] (DON) have been most commonly encountered by humans and animals. The consequences of oral intake of, or dermal exposure to, the toxins will result in alimentary toxic aleukia, ], ], ] and/or skin irritation.<ref name=tthm>{{cite journal | vauthors = Froquet R, Sibiril Y, Parent-Massin D | title = Trichothecene toxicity on human megakaryocyte progenitors (CFU-MK) | journal = Human & Experimental Toxicology | volume = 20 | issue = 2 | pages = 84–89 | date = February 2001 | pmid = 11327514 | doi = 10.1191/096032701677428611 | bibcode = 2001HETox..20...84F | s2cid = 37767457 }}</ref><ref name=csytt>{{cite journal | vauthors = Joffe AZ, Yagen B | title = Comparative study of the yield of T-2 toxic produced by Fusarium poae, F. sporotrichioides and F. sporotrichioides var. tricinctum strains from different sources | journal = Mycopathologia | volume = 60 | issue = 2 | pages = 93–97 | date = February 1977 | pmid = 846559 | doi = 10.1007/bf00490378 | s2cid = 39431820 }}</ref><ref name=fis>{{cite journal | vauthors = Hay RJ | title = Fusarium infections of the skin | journal = Current Opinion in Infectious Diseases | volume = 20 | issue = 2 | pages = 115–117 | date = April 2007 | pmid = 17496567 | doi = 10.1097/QCO.0b013e328014392d }}</ref> In 1993, the ] issued a document for the content limits of DON in food and animal feed at an advisory level.<ref name=gifda>{{cite web| work = Food and Drug Administration| title = Guidance for Industry and FDA – Letter to State Agricultural Directors, State Feed Control Officials, and Food, Feed, and Grain Trade Organizations | access-date = August 13, 2007| url = http://www.cfsan.fda.gov/~dms/graingui.html |archive-url = https://web.archive.org/web/20070609034256/http://www.cfsan.fda.gov/~dms/graingui.html <!-- Bot retrieved archive --> |archive-date = June 9, 2007}}</ref> In 2003, US published a patent that is very promising for farmers to produce a trichothecene-resistant crop.<ref name=trtp>Hohn, Thomas M. "Trichothecene-resistant transgenic plants". {{US Patent|6646184}}. Priority date March 31, 1999.</ref> | |||
| * ] | |||
| * ]s | |||
| ===Viruses=== | ===Viruses=== | ||
| ] infections make up perhaps one third of cases of food poisoning in developed countries. In the US, more than 50% of cases are viral and ] are the most common foodborne illness, causing 57% of outbreaks in 2004. Foodborne viral infection are usually of intermediate (1–3 days) ], causing illnesses which are self-limited in otherwise healthy individuals |
] infections make up perhaps one third of cases of food poisoning in developed countries. In the US, more than 50% of cases are viral and ] are the most common foodborne illness, causing 57% of outbreaks in 2004. Foodborne viral infection are usually of intermediate (1–3 days) ], causing illnesses which are self-limited in otherwise healthy individuals; they are similar to the bacterial forms described above.{{citation needed|date=January 2021}} | ||
| ] | |||
| * ] | * ] | ||
| * ] is distinguished from other viral causes by its prolonged (2–6 week) |
* ] is distinguished from other viral causes by its prolonged (2–6 week) incubation period and its ability to spread beyond the stomach and intestines into the ]. It often results in ], or yellowing of the skin, but rarely leads to chronic liver dysfunction. The virus has been found to cause infection due to the consumption of fresh-cut produce which has fecal contamination.<ref name=ivcma> | ||
| {{cite journal | vauthors = Dubois E, Hennechart C, Deboosère N, Merle G, Legeay O, Burger C, Le Calvé M, Lombard B, Ferré V, Traoré O | display-authors = 6 | title = Intra-laboratory validation of a concentration method adapted for the enumeration of infectious F-specific RNA coliphage, enterovirus, and hepatitis A virus from inoculated leaves of salad vegetables | journal = International Journal of Food Microbiology | volume = 108 | issue = 2 | pages = 164–171 | date = April 2006 | pmid = 16387377 | doi = 10.1016/j.ijfoodmicro.2005.11.007 }} | |||
| | last = Dubois | |||
| </ref><ref name=imqsf>{{cite thesis | last = Schmidt| first = Heather Martin | name-list-style = vanc | title = Improving the microbiological quality and safety of fresh-cut tomatoes by low dose electron beam irradiation |type=MS thesis |publisher=Texas A&M University |date=2004 | access-date = December 14, 2022| url =https://oaktrust.library.tamu.edu/handle/1969.1/2767 |hdl=1969.1/2767}}</ref> | |||
| | first = Eric ''et al.'' | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Intra-laboratory validation of a concentration method adapted for the enumeration of infectious F-specific RNA coliphage, enterovirus, and hepatitis A virus from inoculated leaves of salad vegetables spt on from mexican migrant workers. <internet> | |||
| | publisher = | |||
| | accessdaymonth = 11 August | |||
| | accessyear = 2007 | |||
| | url = http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T7K-4HYMVXK-4&_user=10&_coverDate=04%2F25%2F2006&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=29d010eafc89179a9a66fd24a4b44e21}}</ref><sup>,</sup> <ref name=imqsf>{{cite web | |||
| | last = Schmidt | |||
| | first = Heather Martin | |||
| | authorlink = | |||
| | coauthors = | |||
| | title = Improving the microbilological quality and safety of fresh-cut tomatoes by low dose dlectron beam irradiation - Master thesis <internet> | |||
| | publisher = | |||
| | accessdaymonth = 11 August | |||
| | accessyear = 2007 | |||
| | url = http://txspace.tamu.edu/bitstream/1969.1/2767/1/etd-tamu-2004B-FSTC-Schmidt.pdf}}</ref>. | |||
| * ] | * ] | ||
| * ] | * ] | ||
| * ] | * ] ] | ||
| ===Parasites=== | ===Parasites=== | ||
| Most foodborne ]s are ].<ref>{{cite journal | vauthors = Murrell KD | title = Zoonotic foodborne parasites and their surveillance | journal = Revue Scientifique et Technique | volume = 32 | issue = 2 | pages = 559–569 | date = August 2013 | pmid = 24547659 | doi = 10.20506/rst.32.2.2239 | doi-access = free }}</ref> | |||
| Most foodborne ]s are ]. | |||
| * ]:{{citation needed|date=January 2021}} | |||
| ** '']'' sp. | |||
| ]: | |||
| * '' |
** ''Nanophyetus'' sp. | ||
| ** '']'' | |||
| ] | |||
| ** '']'' | |||
| *''Nanophyetus'' sp. | |||
| *'']'' | ** '']'' | ||
| ** See also: ] and ] | |||
| *'']'' | |||
| * ]:<ref>{{Cite web| url= https://www.britannica.com/animal/nematode| author=Britannica | title= Nematode| date = 2021}}</ref> | |||
| *'']'' | |||
| ** '']'' sp. | |||
| ''See also: ] and ]'' | |||
| ** '']'' | |||
| ** '']'' sp. | |||
| ]: | |||
| *'']'' |
** '']'' | ||
| *'']'' | ** '']'' | ||
| ** '']'' | |||
| *''Eustrongylides'' sp. | |||
| * ]:{{citation needed|date=January 2021}} | |||
| *'']'' | |||
| ** '']'' and other free-living ]e | |||
| *'']'' | |||
| ** '']'' | |||
| ** '']'' | |||
| ]: | |||
| ** '']'' | |||
| ] | |||
| ** '']''] | |||
| * '']'' and other free-living ]e | |||
| ** ''Sarcocystis hominis'' | |||
| * '']'' | |||
| * '' |
** ''Sarcocystis suihominis'' | ||
| * '']'' | ** '']'' | ||
| * '']'' | |||
| * ''Sarcocystis hominis'' | |||
| * ''Sarcocystis suihominis'' | |||
| * '']'' | |||
| ===Natural toxins=== | ===Natural toxins=== | ||
| Several foods can naturally contain ], many of which are not produced by bacteria. Plants in particular may be toxic; animals which are naturally poisonous to eat are rare. In evolutionary terms, animals can escape being eaten by fleeing; plants can use only passive defenses such as poisons and distasteful substances, for example ] in ]s and pungent ] compounds in ] and ]s. Most animal poisons are not synthesised by the animal, but acquired by eating poisonous plants to which the animal is immune, or by bacterial action. | Several foods can naturally contain ], many of which are not produced by bacteria. Plants in particular may be toxic; animals which are naturally poisonous to eat are rare. In evolutionary terms, animals can escape being eaten by fleeing; plants can use only passive defenses such as poisons and distasteful substances, for example ] in ]s and pungent ] compounds in ] and ]s. Most animal poisons are not synthesised by the animal, but acquired by eating poisonous plants to which the animal is immune, or by bacterial action.{{citation needed|date=January 2021}} | ||
| * ]s | * ]s | ||
| * ] | * ] | ||
| * ] (] intoxication) | * ] (] intoxication) | ||
| * Hormones from the ]s of slaughtered animals (especially ] in cases of ''hamburger thyrotoxicosis'' or ''alimentary thyrotoxicosis'')<ref>{{cite journal | vauthors = Wartique L, Pothen L, Pirson N, Hermans MP, Lambert M, Yildiz H | title = An unusual cause of epidemic thyrotoxicosis | journal = Acta Clinica Belgica | volume = 72 | issue = 6 | pages = 451–453 | date = December 2017 | pmid = 28361645 | doi = 10.1080/17843286.2017.1309336 | s2cid = 24489342 }}</ref><ref name="pmid3561455">{{cite journal | vauthors = Hedberg CW, Fishbein DB, Janssen RS, Meyers B, McMillen JM, MacDonald KL, White KE, Huss LJ, Hurwitz ES, Farhie JR | display-authors = 6 | title = An outbreak of thyrotoxicosis caused by the consumption of bovine thyroid gland in ground beef | journal = The New England Journal of Medicine | volume = 316 | issue = 16 | pages = 993–998 | date = April 1987 | pmid = 3561455 | doi = 10.1056/NEJM198704163161605 }}</ref><ref name="pmid12952802">{{cite journal | vauthors = Parmar MS, Sturge C | title = Recurrent hamburger thyrotoxicosis | journal = CMAJ | volume = 169 | issue = 5 | pages = 415–417 | date = September 2003 | pmid = 12952802 | pmc = 183292 }}</ref><ref name="pmid25517332">{{cite journal | vauthors = Broome MR, Peterson ME, Kemppainen RJ, Parker VJ, Richter KP | title = Exogenous thyrotoxicosis in dogs attributable to consumption of all-meat commercial dog food or treats containing excessive thyroid hormone: 14 cases (2008-2013) | journal = Journal of the American Veterinary Medical Association | volume = 246 | issue = 1 | pages = 105–111 | date = January 2015 | pmid = 25517332 | doi = 10.2460/javma.246.1.105 | doi-access = free }}</ref><ref name="pmid20308711">{{cite journal | vauthors = Hendriks LE, Looij BJ | title = Hyperthyroidism caused by excessive consumption of sausages | journal = The Netherlands Journal of Medicine | volume = 68 | issue = 3 | pages = 135–137 | date = March 2010 | pmid = 20308711 }}</ref><ref name="pmid3257352">{{cite journal | vauthors = Kinney JS, Hurwitz ES, Fishbein DB, Woolf PD, Pinsky PF, Lawrence DN, Anderson LJ, Holmes GP, Wilson CK, Loschen DJ | display-authors = 6 | title = Community outbreak of thyrotoxicosis: epidemiology, immunogenetic characteristics, and long-term outcome | journal = The American Journal of Medicine | volume = 84 | issue = 1 | pages = 10–18 | date = January 1988 | pmid = 3257352 | doi = 10.1016/0002-9343(88)90002-2 }}</ref> | |||
| * ] toxins | |||
| * ] | |||
| * ] (red ] poisoning; destroyed by boiling) | * ] (red ] poisoning; destroyed by boiling) | ||
| * ]s | * ]s | ||
| * Shellfish toxin, including ], diarrhetic shellfish poisoning, neurotoxic shellfish poisoning, ] and ] fish poisoning | * Shellfish toxin, including ], diarrhetic shellfish poisoning, neurotoxic shellfish poisoning, ] and ] fish poisoning | ||
| * ] | * ] | ||
| * ] (green ] poisoning) | |||
| * ] (] poisoning) | * ] (] poisoning) | ||
| Some plants contain substances which are toxic in large doses, but have therapeutic properties in appropriate dosages. | Some plants contain substances which are toxic in large doses, but have therapeutic properties in appropriate dosages. | ||
| * ] contains ]. | * ] contains ]. | ||
| * Poisonous hemlock (]) has medicinal uses. | * Poisonous hemlock (]) has medicinal uses. {{Citation needed|date=March 2020}} | ||
| ===Other pathogenic agents=== | ===Other pathogenic agents=== | ||
| * ]s, resulting in ] | * ]s, resulting in ] (CJD) and its variant (]) | ||
| ==="Ptomaine poisoning"=== | ==="Ptomaine poisoning" misconception {{anchor|ptomaine}}=== | ||
| Ptomaine poisoning was a myth that persisted in the public consciousness, in newspaper headlines, and legal cases as an official diagnosis, decades after it had been scientifically disproven in the 1910s.<ref>{{cite magazine|magazine=The Spectator|title=The Ptomaine-Poisoning Myth|date=1934-05-25|author1-first=W. A.|author1-last=Brend|url=http://archive.spectator.co.uk/article/25th-may-1934/9/the-ptomaine-poisoning-myth}}</ref> | |||
| An early theory on the causes of food poisoning involved ''ptomaines'' (from Greek ''ptōma'', "fall, fallen body, corpse"), ]s found in decaying animal and vegetable matter. While some alkaloids do cause poisoning, the discovery of bacteria left the ptomaine theory obsolete and the word "ptomaine" is no longer used scientifically. | |||
| In the 19th century, the Italian chemist ], of Bologna, introduced the generic name ''{{linktext|ptomaine}}'' (from Greek ''ptōma'', "fall, fallen body, corpse") for ]s found in decaying animal and vegetable matter, especially (as reflected in their names) ] and ].<ref name="oed" | |||
| ==Global Impact== | |||
| >{{cite book|title=Oxford English Dictionary|date=1933|publisher=Oxford University Press|location=London|page=1557|edition=First}}</ref> The 1892 ''Merck's Bulletin'' stated, "We name such products of bacterial origin ptomaines; and the special ] produced by the ] is variously named Cadaverine, Putrescine, etc."<ref>, William Henry Porter, 1892.</ref> while '']'' stated, "The chemical ferments produced in the system, the... ptomaines which may exercise so disastrous an influence."<ref>Lancet, 3 Oct 1891, page 752</ref> It is now known that the "disastrous... influence" is due to the direct action of ] and only slightly due to the alkaloids. Thus, the use of the phrase "ptomaine poisoning" is now largely obsolete.{{cn|date=August 2023}} | |||
| At a ] political convention in ],<ref> ''Evening Independent'' (Massillon, OH), July 22, 1932, pg. 6</ref> and aboard a cruise ship in Washington, D.C., hundreds of people were sickened in separate incidents by tainted ], during a single week in 1932, drawing national attention to the dangers of so-called "ptomaine poisoning" in the pages of the American news weekly, ''].''<ref>"Medicine: Potato Salad," ''Time,'' August 1, 1932.</ref> In 1944, another newspaper article reported that over 150 people in Chicago were hospitalized with ptomaine poisoning, apparently from ] served by a restaurant chain.<ref>{{cite news|title=Poisoning Hits 150 in Chicago|url=http://ken.stparchive.com/Archive/KEN/KEN05271944p01.php|work=Kenosha Evening News|date=May 27, 1944|access-date=March 9, 2015|archive-date=April 27, 2021|archive-url=https://web.archive.org/web/20210427133354/http://ken.stparchive.com/Archive/KEN/KEN05271944p01.php|url-status=dead}}</ref> | |||
| In modern times, rapid globalization of food production and trade has increased the potential likelihood of food contamination. Many outbreaks of foodborne diseases that were once contained within a small community may now take place on global dimensions. ] authorities all over the world have acknowledged that ensuring food safety must not only be tackled at the national level but also through closer linkages among food safety authorities at the international level. This is important for exchanging routine information on food safety issues and to have rapid access to information in case of food safety emergencies." | |||
| ==Mechanism== | |||
| It is difficult to estimate the global incidence of foodborne disease, but it has been reported that in the year 2000 about 2.1 million people died from diarrhoeal diseases. Many of these cases have been attributed to contamination of food and drinking water. Additionally, diarrhoea is a major cause of malnutrition in infants and young children. | |||
| ===Incubation period=== | |||
| Even in industrialized countries, up to 30% of the population of people have been reported to suffer from foodborne diseases every year. In the U.S, around 76 million cases of foodborne diseases, which resulted in 325,000 hospitalizations and 5,000 deaths, are estimated to occur each year. Developing countries in particular, are worst affected by foodborne illnesses due to the presence of a wide range of diseases, including those caused by parasites. Foodborne illnesses can and did inflict serious and extensive harm on society. In 1994, an outbreak of salmonellosis due to contaminated ice cream occurred in the USA, affecting an estimated 224,000 persons. In 1988, an outbreak of hepatitis A, resulting from the consumption of contaminated clams, affected some 300,000 individuals in China. | |||
| The delay between the consumption of contaminated food and the appearance of the first ]s of illness is called the ]. This ranges from hours to days (and rarely months or even years, such as in the case of ] or ]), depending on the agent, and on how much was consumed. If symptoms occur within one to six hours after eating the food, it suggests that it is caused by a bacterial toxin or a chemical rather than live bacteria.{{cn|date=August 2023}} | |||
| The long incubation period of many foodborne illnesses tends to cause those affected to attribute their symptoms to ].<ref>{{cite journal | vauthors = Lee RM, Lessler J, Lee RA, Rudolph KE, Reich NG, Perl TM, Cummings DA | title = Incubation periods of viral gastroenteritis: a systematic review | journal = BMC Infectious Diseases | volume = 13 | pages = 446 | date = September 2013 | pmid = 24066865 | pmc = 3849296 | doi = 10.1186/1471-2334-13-446 | doi-access = free }}</ref> | |||
| Food contamination creates an enormous social and economic strain on societies. In the U.S., diseases caused by the major pathogens alone are estimated to cost up to US $35 billion annually (1997) in medical costs and lost productivity. The re-emergence of cholera in Peru in 1991 resulted in the loss of US $500 million in fish and fishery product exports that year. | |||
| During the incubation period, ]s pass through the ] into the ], attach to the ] lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a ] that is absorbed into the ]stream, and some can directly invade the deeper body tissues. The symptoms produced depend on the type of microbe.<ref> | |||
| ==Statistics== | |||
| {{cite web|work=US Centers for Disease Control and Prevention|url=https://www.cdc.gov/ncidod/diseases/food/index.htm |title=Food-Related Diseases|date=2018-03-29 }} | |||
| Every year there are about 76 million foodborne illnesses in the ] (26,000 cases for 100,000 inhabitants), 2 million in the ] (3,400 cases for 100,000 inhabitants) and 750,000 in ] (1,210 cases for 100,000 inhabitants). | |||
| </ref> | |||
| ===Infectious dose=== | |||
| The ] is the amount of agent that must be consumed to give rise to symptoms of foodborne illness, and varies according to the agent and the consumer's age and overall health. Pathogens vary in minimum infectious dose; for example, '']'' has a low estimated minimum dose of < 500 ]s (CFU) while '']'' has a relatively high estimate.<ref name=":0">{{Cite web |vauthors=Greig JD |title=Infective Doses and Pathogen Carriage |url=https://www.researchgate.net/publication/265305465 |website=ResearchGate}}</ref> | |||
| In the case of '']'' a relatively large inoculum of 1'' ''million to 1'' ''billion organisms is necessary to produce symptoms in healthy human volunteers,<ref>Owens, Michael D (January 2014) . emedicine.com</ref> as ''Salmonellae'' are very sensitive to acid. An unusually high stomach ] level (low acidity) greatly reduces the number of bacteria required to cause symptoms by a factor of between 10 and 100.{{cn|date=August 2023}} | |||
| ===Gut microbiota unaccustomed to endemic organisms=== | |||
| Foodborne illness often occurs as ] in persons whose ] is unaccustomed to organisms endemic to the visited region. This effect of microbiologic naïveté is compounded by any ] lapses in the food's preparation.{{cn|date=August 2023}} | |||
| ==Epidemiology== | |||
| Asymptomatic ] may help spread these diseases, particularly '']'', ''], ], ], ], ],'' and ].<ref name=":0" /> For example, as of 1984 it was estimated that in the United States, 200,000 people were asymptomatic carriers of ''Salmonella''.<ref name=":0" /> | |||
| ===Infants=== | |||
| {{Main | Infant food safety}} | |||
| Globally, infants are a group that is especially vulnerable to foodborne disease. The World Health Organization has issued recommendations for the preparation, use and storage of prepared formulas. Breastfeeding remains the best preventive measure for protection from foodborne infections in infants.<ref>{{cite web | url=https://www.who.int/foodsafety/publications/mra10/en/ | archive-url=https://web.archive.org/web/20150402090052/http://www.who.int/foodsafety/publications/mra10/en/ | url-status=dead | archive-date=April 2, 2015 | title=Enterobacter sakazakii and Salmonella in powdered infant formula | date=2006 | author=FAO/WHO | editor=World Health Organization | type=Meeting report | series=Microbiological risk assessment series 10}}</ref> | |||
| ===United States=== | ===United States=== | ||
| In the United States, there are approximately 76 million foodborne illnesses (26,000 cases for 100,000 inhabitants):<ref>{{cite web | |||
| | url=http://www.who.int/mediacentre/factsheets/fs237/en/ | |||
| | title=Food safety and foodborne illness | |||
| | pulisher=WHO}}</ref> | |||
| * 325,000 were hospitalized (111 per 100,000 inhabitants); | |||
| * 5,000 people ] (1.7 per 100,000 inhabitants.). | |||
| * Major pathogens from food borne illness in the United States cost upwards of US $35 billion dollars in medical costs and lost productivity (1997) | |||
| A CDC report<ref></ref> for the period 2017–2019 found that 41% of outbreaks at restaurants were caused by a sick employee. Contributory factors identified included lack of written policy compliance with FDA recommendations for identifying red-flag symptoms, glove use, and hand washing; lack of ] at the majority of establishments; and social pressure to come to work even while sick.<ref></ref> The remaining outbreaks had a variety of causes, including inadequate cooking, improper temperature, and cross-contamination{{cn|date=August 2023}}. | |||
| ===France=== | |||
| In France, for 750,000 cases(1,210 per 100,000 inhabitants): | |||
| In the United States, using FoodNet data from 2000 to 2007, the CDC estimated there were 47.8'' ''million foodborne illnesses per year (16,000 cases for 100,000 inhabitants)<ref name=CDC11Unspec>{{cite journal | vauthors = Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM | title = Foodborne illness acquired in the United States--unspecified agents | journal = Emerging Infectious Diseases | volume = 17 | issue = 1 | pages = 16–22 | date = January 2011 | pmid = 21192849 | pmc = 3204615 | doi = 10.3201/eid1701.P21101 }}</ref> with 9.4'' ''million of these caused by 31 known identified pathogens.<ref name=CDC11Spec /> | |||
| * 70,000 people consulted in the emergency department of an hospital (113 per 100,000 inhab.); | |||
| * 113,000 people were hospitalized (24 per 100,000 inhabitants); | |||
| <!-- orphan reference: surely useful for some fact, just not these<ref> | |||
| * 400 people died (0.9 per 100,000 inhabitants). | |||
| {{cite web | |||
| | url=https://www.who.int/mediacentre/factsheets/fs237/en/ | |||
| | archive-url=https://web.archive.org/web/20040227020759/http://www.who.int/mediacentre/factsheets/fs237/en/ | |||
| | url-status=dead | |||
| | archive-date=February 27, 2004 | |||
| | title=Food safety and foodborne illness | |||
| | publisher=WHO}} | |||
| </ref> --> | |||
| * 127,839 were hospitalized (43 per 100,000 inhabitants per year).<ref>{{cite news |title=Obama Proposes Single Overseer for Food Safety |url=https://www.nytimes.com/2015/02/21/us/obama-proposes-single-overseer-for-food-safety.html |quote=According to the C.D.C., an estimated 87 million Americans are sickened each year by contaminated food, 371,000 are hospitalized with food-related illness and 5,700 die from food-related disease |newspaper=] |date=February 20, 2015 |access-date=2015-02-22 }}</ref><ref name=six/><ref name=strom>{{cite news |author=Stephanie Strom |title=F.D.A. Offers Sweeping Rules to Fight Food Contamination |url=https://www.nytimes.com/2013/01/05/business/fda-offers-rules-to-stop-food-contamination.html |quote=One in six Americans becomes ill from eating contaminated food each year, the government estimates; of those, roughly 130,000 are hospitalized and 3,000 die. |newspaper=The New York Times |date=January 4, 2013 |access-date=January 5, 2013 |author-link=Stephanie Strom }}</ref> | |||
| * 3,037 people ] (1.0 per 100,000 inhabitants per year).<ref name=six>{{cite news |author=Sabrina Tavernise |title=F.D.A. Says Importers Must Audit Food Safety |url=https://www.nytimes.com/2013/07/27/health/fda-proposes-rules-to-ensure-safety-of-imported-food.html |quote=One in every six Americans becomes ill from eating contaminated food each year, Dr. Margaret A. Hamburg, F.D.A. commissioner, estimated. About 130,000 are hospitalized and 3,000 die. |newspaper=The New York Times |date=July 26, 2013 |access-date=July 27, 2013 |author-link=Sabrina Tavernise }}</ref><ref name=strom/> | |||
| {{Col-begin}} | {{Col-begin}} | ||
| {{Col-2}} | {{Col-2}} | ||
| {|class="wikitable" style="font-size:95%" | {|class="wikitable" style="font-size:95%" | ||
| |+ Causes of foodborne illness in US<ref name=CDC11Spec>{{cite journal | vauthors = Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM | display-authors = 6 | title = Foodborne illness acquired in the United States--major pathogens | journal = Emerging Infectious Diseases | volume = 17 | issue = 1 | pages = 7–15 | date = January 2011 | pmid = 21192848 | pmc = 3375761 | doi = 10.3201/eid1701.P11101 }} | |||
| |+ Causes of foodborne illness in ]<ref>{{cite web | |||
| | url=http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/inf_origine_alimentaire.pdf | |||
| | title=Report of the French sanitary agencies | |||
| | publisher=INVS/Afssa | |||
| | language=French}} | |||
| </ref><ref>{{cite web | |||
| | url=http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/grilleLecture.pdf | |||
| | title=Summary of Report of the French sanitary agencies | |||
| | publisher=INVS/Afssa | |||
| | language=French}} | |||
| </ref> | </ref> | ||
| |- | |- | ||
| ! !! Cause !! Annual cases !! Rate<br /><small>(per 100,000 inhabitants)</small> | ! !! Cause !! Annual cases !! Rate<br /><small>(per 100,000 inhabitants)</small> | ||
| |- | |||
| | 1 || '']'' || 5,461,731 cases || align="center"|X | |||
| |- | |||
| | 2 || '']'' || 1,027,561 cases || align="center"|X | |||
| |- | |||
| | 3 || '']'' || 965,958 cases || align="center"|X | |||
| |- | |||
| | 4 || '']'' || 845,024 cases || align="center"|X | |||
| |} | |||
| {{Col-2}} | |||
| {|class="wikitable" style="font-size:95%;" | |||
| |+ Causes of death by foodborne illness in US<ref name=CDC11Spec /> | |||
| |- | |||
| ! !! Cause !! Annual deaths!! Rate<br /><small>(per 100,000 inhabitants)</small> | |||
| |- | |||
| | 1 || '']'' || 378 cases || align="center"| 0.126 | |||
| |- | |||
| | 2 || '']'' || 327 cases || align="center"| 0.109 | |||
| |- | |||
| | 3 || '']'' || 255 cases || align="center"| 0.085 | |||
| |- | |||
| | 4 || '']'' || 149 cases || align="center"| 0.050 | |||
| |} | |||
| {{Col-end}} | |||
| === United Kingdom === | |||
| According to a 2012 report from the ], there were around a million cases of foodborne illness per year (1,580 cases for 100,000 inhabitants).<ref name=":2">{{cite web | title = Annual Report of the Chief Scientist 2012/13 | url = https://acss.food.gov.uk/sites/default/files/multimedia/pdfs/publication/cstar_2013.pdf | work = Food Standards Agency | location = England | date = 2013 }}</ref> | |||
| * 20,000 people were hospitalised (32 per 100,000 inhabitants);<ref name=":2" /><ref name=":3">{{Cite book |url= https://books.google.com/books?id=iJjJDgAAQBAJ&pg=PA290 |title=The Oxford Handbook of Criminology |last1=Liebling |first1=Alison |last2=Maruna |first2=Shadd |last3=McAra |first3=Lesley | name-list-style = vanc |date=2017|publisher=Oxford University Press|isbn=978-0-19-871944-1|pages=290|language=en}}</ref> | |||
| * 500 died (0.80 per 100,000 inhabitants).<ref name=":2" /><ref name=":3" /> | |||
| ===France=== | |||
| This data pertains to reported medical cases of 23 specific pathogens in the 1990s, as opposed to total population estimates of all foodborne illness for the United States.<ref name=inf_origine_alimentaire>{{cite web | url=http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/inf_origine_alimentaire.pdf | title=Report of the French sanitary agencies | publisher=INVS/Afssa | language=fr | access-date=October 6, 2004 | archive-date=March 3, 2016 | archive-url=https://web.archive.org/web/20160303221009/http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/inf_origine_alimentaire.pdf | url-status=dead }}</ref> | |||
| In France, for 735,590 to 769,615 cases of infection identified as being with the 23 specific pathogens, 238,836 to 269,085 were estimated to have been contracted from food: | |||
| * between 12,995 and 22,030 people were hospitalized (10,188 to 17,771 estimated to have contracted their infections from food); | |||
| * between 306 and 797 people died (228 to 691 estimated to have contracted their infections from food).<ref name=inf_origine_alimentaire /> | |||
| {{Col-begin}} | |||
| {{Col-2}} | |||
| {|class="wikitable" style="font-size:95%" | |||
| |+ Causes of foodborne illness in ]<ref name=inf_origine_alimentaire /><ref>{{cite web | url=http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/grilleLecture.pdf | title=Summary of Report of the French sanitary agencies | publisher=INVS/Afssa | language=fr | access-date=October 6, 2004 | archive-date=March 3, 2016 | archive-url=https://web.archive.org/web/20160303184200/http://www.invs.sante.fr/publications/2004/inf_origine_alimentaire/grilleLecture.pdf | url-status=dead }}</ref> | |||
| |- | |||
| ! !! Cause !! Annual hospitalizations !! Rate<br /><small>(per 100,000 inhabitants)</small> | |||
| |- | |- | ||
| | 1 || '']'' || ~8,000 cases || align="center"|13 | | 1 || '']'' || ~8,000 cases || align="center"|13 | ||
| Line 551: | Line 325: | ||
| |} | |} | ||
| {{Col-end}} | {{Col-end}} | ||
| ===Australia=== | ===Australia=== | ||
| In Australia, there are an estimated 5.4 million cases of food-borne illness every year, causing:<ref>{{cite web | |||
| A study by the Australian National University published in 2022 for Food Standards Australia New Zealand estimated there are 4.67 million cases of food poisoning in Australia each year that result in 47,900 hospitalisations, 38 deaths and a cost to the economy of $2.1 billion.<ref>{{cite web |title=The Annual Cost of Foodborne Illness in Australia Final Report September 2022 |url=https://www.foodstandards.gov.au/publications/Documents/ANU%20Foodborne%20Disease%20Final%20Report.pdf |website=Food Standards Australia New Zealand |publisher=Australian National University |access-date=8 April 2023}}</ref> | |||
| | url=http://www.ozfoodnet.org.au/internet/ozfoodnet/publishing.nsf/Content/reports-1/$FILE/foodborne_report.pdf | |||
| | title=Food borne illness in Australia | |||
| A previous study using different methodology and published in November 2014, found in 2010 that there were an estimated 4.1 million cases of foodborne gastroenteritis acquired in Australia on average each year, along with 5,140 cases of non-gastrointestinal illness.<ref>{{cite journal |last1=Kirk |first1=Martyn |title=Foodborne Illness, Australia, Circa 2000 and Circa 2010 |journal=Emerging Infectious Diseases |year=2014 |volume=20 |issue=11 |pages=1857–1864 |publisher=Emerging Infectious Diseases v 20:11 |doi=10.3201/eid2011.131315 |pmid=25340705 |pmc=4214288 }}</ref> | |||
| | pulisher=OzFoodNet}}</ref> | |||
| * 18,000 hospitalisations | |||
| The main causes were norovirus, pathogenic ''Escherichia coli'', ''Campylobacter'' spp. and non-typhoidal ''Salmonella'' spp., although the causes of approximately 80% of illnesses were unknown. Approximately 25% (90% ]: 13%–42%) of the 15.9 million episodes of gastroenteritis that occur in Australia were estimated to be transmitted by contaminated food. This equates to an average of approximately one episode of foodborne gastroenteritis every five years per person. Data on the number of hospitalisations and deaths represent the occurrence of serious foodborne illness. Including gastroenteritis, non-gastroenteritis and sequelae, there were an estimated annual 31,920 (90% CrI: 29,500–35,500) hospitalisations due to foodborne illness and 86 (90% CrI: 70–105) deaths due to foodborne illness circa 2010. This study concludes that these rates are similar to recent estimates in the US and Canada.{{citation needed|date=January 2021}} | |||
| * 120 deaths | |||
| A main aim of this study was to compare if foodborne illness incidence had increased over time. In this study, similar methods of assessment were applied to data from circa 2000, which showed that the rate of foodborne gastroenteritis had not changed significantly over time. Two key estimates were the total number of gastroenteritis episodes each year, and the proportion considered foodborne. In circa 2010, it was estimated that 25% of all episodes of gastroenteritis were foodborne. By applying this proportion of episodes due to food to the incidence of gastroenteritis circa 2000, there were an estimated 4.3 million (90% CrI: 2.2–7.3 million) episodes of foodborne gastroenteritis circa 2000, although credible intervals overlap with 2010. Taking into account changes in population size, applying these equivalent methods suggests a 17% decrease in the rate of foodborne gastroenteritis between 2000 and 2010, with considerable overlap of the 90% credible intervals.{{citation needed|date=January 2021}} | |||
| This study replaces a previous estimate of 5.4 million cases of foodborne illness in Australia every year, causing:<ref> | |||
| {{cite web | url=http://www.ozfoodnet.gov.au/internet/ozfoodnet/publishing.nsf/Content/reports-1/$FILE/foodborne_report.pdf | title=Foodborne illness in Australia. Annual incidence circa 2000 | publisher=OzFoodNet |page=10 |archiveurl=https://webarchive.nla.gov.au/awa/20140125145815/http://ozfoodnet.gov.au/internet/ozfoodnet/publishing.nsf/Content/7BDEF9F8EC3835D9CA257165001AB31D/$File/foodborne_report.pdf |archivedate=2014-01-25 |url-status=dead}}</ref> | |||
| * 18,000 hospitalizations | |||
| * 120 deaths (0.5 deaths per 100,000 inhabitants) | |||
| * 2.1 million lost days off work | * 2.1 million lost days off work | ||
| * 1.2 million doctor consultations | * 1.2 million doctor consultations | ||
| * 300,000 prescriptions for antibiotics | * 300,000 prescriptions for antibiotics. | ||
| Most foodborne disease outbreaks in Australia have been linked to raw or minimally cooked eggs or poultry.<ref>{{cite journal| vauthors = Astridge K, McPherson M, Knope K, Gregory J, Kardamanidis K, Bell E, Kirk M |title=Foodborne disease outbreaks in Australia 2001-2009|journal=Food Australia|date=2011|volume=63 |issue=12|pages=44–50|display-authors=6}}</ref> The ] estimates that one third of cases of food poisoning occur in the home.<ref>{{cite web|title=Food Hygiene|url=https://www.bupa.com.au/health-and-wellness/health-information/healthy-living/nutrition/eating/doc/food-hygiene|website=BUPA|access-date=13 September 2015|url-status=dead|archive-url=https://web.archive.org/web/20151211131645/https://www.bupa.com.au/health-and-wellness/health-information/healthy-living/nutrition/eating/doc/food-hygiene|archive-date=December 11, 2015|df=mdy-all}}</ref> | |||
| ===Outbreaks=== | |||
| {{Main article|Deadliest foodborne illness incidents}} | |||
| The vast majority of reported cases of foodborne illness occur as individual or sporadic cases. The origin of most sporadic cases is undetermined. In the United States, where people eat outside the home frequently, 58% of cases originate from commercial food facilities (2004 FoodNet data). An outbreak is defined as occurring when two or more people experience similar illness after consuming food from a common source.{{citation needed|date=January 2021}} | |||
| Often, a combination of events contributes to an outbreak, for example, food might be left at room temperature for many hours, allowing bacteria to ] which is compounded by inadequate cooking which results in a failure to kill the dangerously elevated bacterial levels.{{citation needed|date=January 2021}} | |||
| ==Outbreaks== | |||
| The vast majority of reported cases of foodborne illness occur as individual or ] cases. The origin of most ] cases is undetermined. In the United States, where people eat outside the home frequently, most outbreaks (58%) originate from commercial food facilities (2004 FoodNet data). An outbreak is defined as occurring when two or more people experience similar illness after consuming food from a common source. | |||
| Outbreaks are usually identified when those affected know each other. Outbreaks can also be identified by ] staff when there are unexpected increases in laboratory results for certain strains of bacteria. Outbreak detection and investigation in the United States is primarily handled by local health jurisdictions and is inconsistent from district to district. It is estimated that 1–2% of outbreaks are detected.{{citation needed|date=January 2021}} | |||
| Often, a combination of events contributes to an outbreak, for example, food might be left at room temperature for many hours, allowing bacteria to ] which is compounded by inadequate cooking which results in a failure to kill the dangerously elevated bacterial levels. | |||
| ==Society and culture== | |||
| Outbreaks are usually identified when those affected know each other. However, more and more, outbreaks are identified by ] staff from unexpected increases in laboratory results for certain strains of bacteria. Outbreak detection and investigation in the United States is primarily handled by local health jurisdictions and is inconsistent from district to district. It is estimated that 1–2% of outbreaks are detected. | |||
| ==Political issues== | |||
| ===United Kingdom=== | ===United Kingdom=== | ||
| In |
In Aberdeen, in 1964, a large-scale (>400 cases) outbreak of ] occurred, caused by contaminated ] which had been imported from ].<ref> | ||
| Smith, David F.; Diack, H. Lesley and Pennington, T. Hugh (2005) ''Food Poisoning, Policy and Politics : Corned Beef and Typhoid in Britain in the 1960s''. Boydell Press. {{ISBN|1-84383-138-4}}{{page needed|date=November 2013}} | |||
| </ref> The corned beef was placed in cans and because the cooling plant had failed, cold river water from the ] was used to cool the cans. One of the cans had a defect and the meat inside was contaminated. That meat was then sliced using a meat slicer in a shop in Aberdeen, and a lack of machinery-cleaning led to the spreading of the contamination to other meats cut in the slicer. Those meats were eaten by people in Aberdeen who then became ill.{{citation needed|date=January 2021}} | |||
| Serious outbreaks of foodborne illness since the 1970s prompted key changes in UK ] law. The outbreaks included the deaths of 19 patients in the Stanley Royd Hospital outbreak<ref>{{cite web|url=http://briandeer.com/social/stanley-royd.htm|title=Food poison deaths probe may reveal NHS flaws|date=February 24, 1985|author=Brian Deer|work=The Sunday Times}}</ref> and the ] (BSE, mad cow disease) outbreak identified in the 1980s. The deaths of 21 people in the ] of ''E. coli'' O157<ref>{{cite web|url=http://news.bbc.co.uk/1/hi/health/154107.stm|title=BBC News - Health - Sheriff criticises E. coli butcher}}</ref><ref>{{cite journal | vauthors = Cowden JM, Ahmed S, Donaghy M, Riley A | title = Epidemiological investigation of the central Scotland outbreak of Escherichia coli O157 infection, November to December 1996 | journal = Epidemiology and Infection | volume = 126 | issue = 3 | pages = 335–341 | date = June 2001 | pmid = 11467789 | pmc = 2869700 | doi = 10.1017/S0950268801005520 }}</ref> was a precursor to the establishment of the ] which, according to ] in the 1998 ] ''A Force for Change'' Cm 3830, "would be powerful, open and dedicated to the interests of consumers".<ref>{{cite web|url=http://www.archive.official-documents.co.uk/document/maffdh/fsa/fsa.htm |title=The Food Standards Agency: A Force for Change |website=gov.uk |publisher=Food Standards Agency, United Kingdom |date=January 14, 1998 |access-date=14 August 2016}}</ref> | |||
| In May 2015, for the second year running, England's Food Standards Agency devoted its annual Food Safety Week to "The Chicken Challenge". The focus was on the handling of raw chicken in the home and in catering facilities in a drive to reduce the high levels of food poisoning from the ''campylobacter'' bacterium. Anne Hardy argues that widespread public education of food hygiene can be useful, particularly through media (TV cookery programmes) and advertisement. She points to the examples set by ]n societies.<ref>{{Cite web|url=http://www.historyandpolicy.org/policy-papers/papers/food-poisoning-an-on-going-saga|title=Food Poisoning: An On-going Saga |last=Hardy |first=Anne | name-list-style = vanc |date=13 January 2016|website=History and Policy|access-date=4 July 2016}}</ref> | |||
| ===United States=== | ===United States=== | ||
| {{Main|Food safety in the United States}} | |||
| In 2001, the petitioned the ] to require meat packers to remove ]s before processing cattle carcasses for human consumption, a measure designed to lessen the risk of infection by variant ]. The petition was supported by the ], the ], the ], the ], and Safe Tables Our Priority. This was opposed by the ], the National Renderers Association, the ], the Pork Producers Council, sheep raisers, milk producers, the Turkey Federation, and eight other organizations from the animal-derived food industry. This was part of a larger controversy regarding the United States' violation of ] proscriptions to lessen the risk of infection by variant Creutzfeldt-Jakob disease.{{Fact|date=September 2007}} | |||
| In 2001, the ] petitioned the ] to require meat packers to remove ]s before processing cattle carcasses for human consumption, a measure designed to lessen the risk of infection by variant ]. The petition was supported by the ], the ], the ], the ], and Safe Tables Our Priority.<ref>{{cite web|url=https://www.federalregister.gov/articles/2004/01/12/04-626/meat-produced-by-advanced-meatbone-separation-machinery-and-meat-recovery-amr-systems#footnote-10 |access-date=3 July 2016 |title=Meat Produced by Advanced Meat/Bone Separation Machinery and Meat Recovery (AMR) Systems |website=Federal Register |publisher=U.S. National Archive and Records Administration|date=2004-01-12 }}</ref> | |||
| None of the US Department of Health and Human Services targets |
None of the US Department of Health and Human Services targets<ref>{{cite web|url=http://www.healthypeople.gov|title=Healthy People 2010 Home Page}}</ref> regarding incidence of foodborne infections were reached in 2007.<ref>{{cite journal | title = Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food--10 states, 2007 | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 57 | issue = 14 | pages = 366–370 | date = April 2008 | pmid = 18401330 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5714a2.htm | author1 = Centers for Disease Control Prevention (CDC) }}</ref> | ||
| A report issued in June 2018 by NBC's Minneapolis station using research by both the CDC and the Minnesota Department of Health concluded that foodborne illness is on the rise in the U.S.<ref>{{cite web|url=https://www.kare11.com/article/news/why-are-we-seeing-so-many-food-recalls/89-564858966|title=Why are we seeing so many food recalls?|publisher=KARE 11|first1=Gordon|last1=Severson | name-list-style = vanc |date=June 15, 2018|access-date=June 19, 2018}}</ref> | |||
| ==Organizations== | |||
| === India === | |||
| '''World Health Organization Food Safety Department''' | |||
| In India, '']'' is the most common cause of food illness, followed by '']'' bacteria, '']'' bacteria, ] bacteria, and ].<ref name=":1">{{Cite news |title=Symptoms of food poisoning |work=The Times of India |url=https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/how-fast-does-food-poisoning-set-in-what-are-the-symptoms-one-should-know/photostory/79493562.cms?picid=79493721 |access-date=2023-05-29 |issn=0971-8257}}</ref> According to statistics, food poisoning was the second most common cause of infectious disease outbreak in India in 2017. The numbers of outbreaks have increased from 50 in 2008 to 242 in 2017. <ref name=":1" /> | |||
| The WHO provides scientific advice for organizations and the public on issues concerning the safety of food. It serves as a medium linking the ] systems in countries around the world. Food safety is currently one of WHO's top ten priorities. Food Safety is one of the major issues in our world today, and the Organization calls for more systematic and aggressive steps to be taken to significantly reduce the risk of foodborne diseases. | |||
| ===Organizations=== | |||
| '''The Department of Food Safety, Zoonoses and Foodborne Diseases''' | |||
| The Department of Food Safety, Zoonoses and Foodborne Diseases is a department under the WHO. Its mission is to: to reduce the serious negative impact of foodborne diseases worldwide. According to the WHO website, food and waterborne diarrhoeal diseases are leading causes of illness and death in less developed countries, killing approximately 3.8 million people annually, most of whom are children | |||
| "WHO works closely with the Food and Agriculture Organization of the United Nations (FAO) to address food safety issues along the entire food production chain--from production to consumption--using new methods of risk analysis. These methods provide efficient, science-based tools to improve food safety, thereby benefiting both public health and economic development." | |||
| The ] Department of Food Safety and Zoonoses (FOS) provides scientific advice for organizations and the public on issues concerning the safety of food. Its mission is to lower the burden of foodborne disease, thereby strengthening the health security and sustainable development of Member States. Foodborne and waterborne diarrhoeal diseases kill an estimated 2.2'' ''million people annually, most of whom are children. WHO works closely with the Food and Agriculture Organization of the United Nations (FAO) to address food safety issues along the entire food production chain—from production to consumption—using new methods of risk analysis. These methods provide efficient, science-based tools to improve food safety, thereby benefiting both public health and economic development.{{citation needed|date=January 2021}} | |||
| '''The International Food Safety Authorities Network (INFOSAN)''' | |||
| This Network is intended to complement and support the existing WHO Global Outbreak Alert and Response Network (GOARN) which includes a Chemical Alert and Response component. | |||
| ===International Food Safety Authorities Network (INFOSAN)=== | |||
| == Academic resources == | |||
| === Periodicals === | |||
| * , ISSN: 0168-1605, Elsevier | |||
| * Foodborne Pathogens and Disease, ISSN: 1535-3141, ] | |||
| * Mycopathologia, ISSN: (electronic) 0301-486X (paper), Springer | |||
| The International Food Safety Authorities Network (INFOSAN) is a joint program of the WHO and FAO. INFOSAN has been connecting national authorities from around the globe since 2004, with the goal of preventing the international spread of contaminated food and foodborne disease and strengthening food safety systems globally. This is done by:{{citation needed|date=January 2021}} | |||
| === Books === | |||
| * Advances in Food Mycology (Advances in Experimental Medicine and Biology) (2006) by A.D. Hocking ''et al.'', ISBN-13: 978-0387283913 (electronic) 978-0387283852 (paper), Springer | |||
| * Foodborne Infections and Intoxications (2006) by Hans P. Riemann and Dean O. Cliver, ISBN 012588365X, Elsevier | |||
| * Foodborne Pathogens: Microbiology And Molecular Biology (2005) by Pina M. Fratamico ''et al.'', ISBN-10: 190445500X ISBN-13: 978-1904455004, Caister Academic Press | |||
| # Promoting the rapid exchange of information during food safety events; | |||
| ==See also== | |||
| # Sharing information on important food safety issues of global interest; | |||
| {{col-begin}} | |||
| # Promoting partnership and collaboration between countries; and | |||
| {{col-3}} | |||
| # Helping countries strengthen their capacity to manage food safety risks. | |||
| * ] | |||
| * ] | |||
| Membership to INFOSAN is voluntary, but is restricted to representatives from national and regional government authorities and requires an official letter of designation. INFOSAN seeks to reflect the multidisciplinary nature of food safety and promote intersectoral collaboration by requesting the designation of Focal Points in each of the respective national authorities with a stake in food safety, and a single Emergency Contact Point in the national authority with the responsibility for coordinating national food safety emergencies; countries choosing to be members of INFOSAN are committed to sharing information between their respective food safety authorities and other INFOSAN members. The operational definition of a food safety authority includes those authorities involved in: food policy; risk assessment; food control and management; food inspection services; foodborne disease surveillance and response; laboratory services for monitoring and surveillance of foods and foodborne diseases; and food safety information, education and communication across the ] continuum.{{citation needed|date=January 2021}} | |||
| * ] | |||
| * ] | |||
| ===Prioritisation of foodborne pathogens=== | |||
| * ] | |||
| * ] | |||
| The Food and Agriculture Organization of the United Nations and The World Health Organization have published a global ranking of foodborne parasites using a multicriteria ranking tool concluding that ''Taenia solium'' was the most relevant, followed by ''Echinococcus granulosus'', ''Echinococcus multilocularis'', and ''Toxoplasma gondii''.<ref name=fao>{{cite book |publisher=FAO/WHO |title=Multicriteria-based ranking for risk management of foodborne parasites |series=Microbiological Risk Assessment Series No. 23 |date=2014 |isbn=978-92-5-108199-0 |url=http://www.fao.org/publications/card/en/c/ee07c6ae-b86c-4d5f-915c-94c93ded7d9e/}}</ref> The same method was used regionally to rank the most important foodborne parasites in Europe ranking ''Echinococcus multilocularis'' of highest relevance, followed by ''Toxoplasma gondii'' and ''Trichinella spiralis''.<ref name=eur>{{cite journal | vauthors = Bouwknegt M, Devleesschauwer B, Graham H, Robertson LJ, van der Giessen JW | title = Prioritisation of food-borne parasites in Europe, 2016 | journal = Euro Surveillance | volume = 23 | issue = 9 | date = March 2018 | pmid = 29510783 | pmc = 5840924 | doi = 10.2807/1560-7917.ES.2018.23.9.17-00161 }}</ref> | |||
| ===Regulatory steps=== | |||
| Food may be contaminated during all stages of food production and retailing. In order to prevent viral contamination, regulatory authorities in Europe have enacted several measures:{{citation needed|date=January 2021}} | |||
| * European Commission Regulation (EC) No 2073/2005 of November 15, 2005 | |||
| * ] (CEN): Standard method for the detection of norovirus and hepatitis A virus in food products (shellfish, fruits and vegetables, surfaces and bottled water) | |||
| * CODEX Committee on Food Hygiene (CCFH): Guideline for the application of general principles of food hygiene for the control of viruses in food<ref>, European Commission, Retrieved April 7, 2015</ref> | |||
| == See also == | |||
| {{div col|colwidth=22em}} | |||
| * '']'' | |||
| * ] | * ] | ||
| * ] | |||
| {{col-3}} | |||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| * ] | * ] | ||
| * ] | * ] | ||
| * ] | |||
| * ] | * ] | ||
| * ] | |||
| {{col-3}} | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | * ] | ||
| * ] | * ] | ||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | * ] | ||
| {{col |
{{div col end}} | ||
| ==References== | == References == | ||
| {{CDC}} | |||
| <references/> | |||
| {{Reflist|30em}} | |||
| == Further reading == | |||
| === Periodicals === | |||
| * , {{ISSN|0168-1605}}, Elsevier | |||
| * , {{ISSN|1535-3141}}, ] | |||
| * '']'', {{ISSN|1573-0832}} (electronic), {{ISSN|0301-486X}} (paper), Springer | |||
| === Books === | |||
| * {{cite book |first1=Ailsa D. |last1=Hocking |first2=John I. |last2=Pitt |first3=Robert A. |last3=Samson |first4=Ulf |last4=Thrane | name-list-style = vanc |title=Advances in Food Mycology |url=https://books.google.com/books?id=9xlIicZfQ5IC |date= 2005 |publisher=Springer |isbn=978-0-387-28385-2}} {{ISBN|978-0-387-28391-3}} (electronic). | |||
| * {{cite book |first=Betty C. |last=Hobbs | name-list-style = vanc |title=Food Poisoning and Food Hygiene |journal=British Medical Bulletin |volume=7 |issue=3 |pages=167–70 |publisher=Edward Arnold |year=1993 |isbn=978-0-340-53740-4|pmid=14821218 |doi=10.1093/oxfordjournals.bmb.a073825 }} | |||
| * {{cite book |first1=Hans P. |last1=Riemann |first2=Dean O. |last2=Cliver | name-list-style = vanc |title=FoodBorne Infections and Intoxications |url=https://books.google.com/books?id=_OsZ9TcQTSsC&pg=PA485 |year=2006 |publisher=Academic Press |isbn=978-0-12-588365-8}} | |||
| * {{cite book |first=James L. |last=Smith | name-list-style = vanc |title=Foodborne Pathogens: Microbiology And Molecular Biology |url=https://books.google.com/books?id=-HNavPPs-JoC |year=2005 |publisher=Horizon Scientific Press |isbn=978-1-904455-00-4 |editor1-first=Pina M. |editor1-last=Fratamico |editor2-first=Arun K. |editor2-last=Bhunia |editor3-first=James L. |editor3-last=Smith}} | |||
| ==External links== | == External links == | ||
| <!--==========================({{NoMoreLinks}})============================ | <!--==========================({{NoMoreLinks}})============================ | ||
| | PLEASE BE CAUTIOUS IN ADDING MORE LINKS TO THIS ARTICLE. WIKIPEDIA | | | PLEASE BE CAUTIOUS IN ADDING MORE LINKS TO THIS ARTICLE. WIKIPEDIA | | ||
| Line 650: | Line 451: | ||
| | and link back to that category using the {{dmoz}} template. | | | and link back to that category using the {{dmoz}} template. | | ||
| =========================({{NoMoreLinks}})=============================--> | =========================({{NoMoreLinks}})=============================--> | ||
| {{Commons category}} | |||
| * | |||
| * , ], Fact sheet N°124, revised January |
* , ], Fact sheet N°124, revised January 2002 | ||
| * , NSW Food Authority | * {{Webarchive|url=https://web.archive.org/web/20191230124336/http://www.foodauthority.nsw.gov.au/fb-foodborne-illness.htm |date=December 30, 2019 }}, NSW Food Authority | ||
| * , ], Fact sheet N°237, revised January |
* , ], Fact sheet N°237, revised January 2002 | ||
| * | * | ||
| * | * | ||
| * from ] | * from ] | ||
| * hosted at the University of Guelph, Canada. | * hosted at the University of Guelph, Canada. | ||
| * | |||
| * | |||
| * | |||
| * | |||
| {{Concepts in infectious disease}} | |||
| {{CDC}} | |||
| {{Consumer Food Safety}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Foodborne Illness}} | |||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 18:33, 29 October 2024
Illness from eating spoiled food
| Food safety |
|---|
 |
| Terms |
| Critical factors |
| Bacterial pathogens |
| Viral pathogens |
| Parasitic pathogens |
Foodborne illness (also known as foodborne disease and food poisoning) is any illness resulting from the contamination of food by pathogenic bacteria, viruses, or parasites, as well as prions (the agents of mad cow disease), and toxins such as aflatoxins in peanuts, poisonous mushrooms, and various species of beans that have not been boiled for at least 10 minutes.
Symptoms vary depending on the cause. They often include vomiting, fever, and aches, and may include diarrhea. Bouts of vomiting can be repeated with an extended delay in between. This is because even if infected food was eliminated from the stomach in the first bout, microbes, like bacteria (if applicable), can pass through the stomach into the intestine and begin to multiply. Some types of microbes stay in the intestine.
For contaminants requiring an incubation period, symptoms may not manifest for hours to days, depending on the cause and on the quantity of consumption. Longer incubation periods tend to cause those affected to not associate the symptoms with the item consumed, so they may misattribute the symptoms to gastroenteritis, for example.
Causes
See also: Pathogen
Foodborne illness usually arises from improper handling, preparation, or food storage. Good hygiene practices before, during, and after food preparation can reduce the chances of contracting an illness. There is a consensus in the public health community that regular hand-washing is one of the most effective defenses against the spread of foodborne illness. The action of monitoring food to ensure that it will not cause foodborne illness is known as food safety. Foodborne disease can also be caused by a large variety of toxins that affect the environment.
Furthermore, foodborne illness can be caused by a number of chemicals, such as pesticides, medicines, and natural toxic substances such as vomitoxin, poisonous mushrooms or reef fish.
Bacteria
Bacteria are a common cause of foodborne illness. In 2000, the United Kingdom reported the individual bacteria involved as the following: Campylobacter jejuni 77.3%, Salmonella 20.9%, Escherichia coli O157:H7 1.4%, and all others less than 0.56%.
In the past, bacterial infections were thought to be more prevalent because few places had the capability to test for norovirus and no active surveillance was being done for this particular agent. Toxins from bacterial infections are delayed because the bacteria need time to multiply. As a result, symptoms associated with intoxication are usually not seen until 12–72 hours or more after eating contaminated food. However, in some cases, such as Staphylococcal food poisoning, the onset of illness can be as soon as 30 minutes after ingesting contaminated food.

A 2022 study concluded that washing uncooked chicken could increase the risk of pathogen transfer, and that specific washing conditions can decrease the risk of transfer.
Most common bacterial foodborne pathogens are:
- Campylobacter jejuni which can lead to secondary Guillain–Barré syndrome and periodontitis
- Clostridium perfringens, the "cafeteria germ"
- Salmonella spp. – its S. typhimurium infection is caused by consumption of eggs or poultry that are not adequately cooked or by other interactive human-animal pathogens
- Escherichia coli O157:H7 enterohemorrhagic (EHEC) which can cause hemolytic-uremic syndrome
Other common bacterial foodborne pathogens are:
- Bacillus cereus
- Escherichia coli, other virulence properties, such as enteroinvasive (EIEC), enteropathogenic (EPEC), enterotoxigenic (ETEC), enteroaggregative (EAEC or EAgEC)
- Listeria monocytogenes
- Shigella spp.
- Staphylococcus aureus
- Streptococcus
- Vibrio cholerae, including O1 and non-O1
- Vibrio parahaemolyticus
- Vibrio vulnificus
- Yersinia enterocolitica and Yersinia pseudotuberculosis
Less common bacterial agents:
- Brucella spp.
- Corynebacterium ulcerans
- Coxiella burnetii or Q fever
- Plesiomonas shigelloides
Enterotoxins
See also: BotulismIn addition to disease caused by direct bacterial infection, some foodborne illnesses are caused by enterotoxins (exotoxins targeting the intestines). Enterotoxins can produce illness even when the microbes that produced them have been killed. Symptom onset varies with the toxin but may be rapid in onset, as in the case of enterotoxins of Staphylococcus aureus in which symptoms appear in one to six hours. This causes intense vomiting including or not including diarrhea (resulting in staphylococcal enteritis), and staphylococcal enterotoxins (most commonly staphylococcal enterotoxin A but also including staphylococcal enterotoxin B) are the most commonly reported enterotoxins although cases of poisoning are likely underestimated. It occurs mainly in cooked and processed foods due to competition with other biota in raw foods, and humans are the main cause of contamination as a substantial percentage of humans are persistent carriers of S. aureus. The CDC has estimated about 240,000 cases per year in the United States.
The rare but potentially deadly disease botulism occurs when the anaerobic bacterium Clostridium botulinum grows in improperly canned low-acid foods and produces botulin, a powerful paralytic toxin.
Pseudoalteromonas tetraodonis, certain species of Pseudomonas and Vibrio, and some other bacteria, produce the lethal tetrodotoxin, which is present in the tissues of some living animal species rather than being a product of decomposition.
Emerging foodborne pathogens
- Aeromonas hydrophila, Aeromonas caviae, Aeromonas sobria
Scandinavian outbreaks of Yersinia enterocolitica have recently increased to an annual basis, connected to the non-canonical contamination of pre-washed salad.
Preventing bacterial food poisoning

Governments have the primary mandate of ensuring safe food for all, however all actors in the food chain are responsible to ensure only safe food reaches the consumer, thus preventing foodborne illnesses. This is achieved through the implementation of strict hygiene rules and a public veterinary and phytosanitary service that monitors animal products throughout the food chain, from farming to delivery in shops and restaurants. This regulation includes:
- traceability: the origin of the ingredients (farm of origin, identification of the crop or animal) and where and when it has been processed must be known in the final product; in this way, the origin of the disease can be traced and resolved (and possibly penalized), and the final products can be removed from sale if a problem is detected;
- enforcement of hygiene procedures such as HACCP and the "cold chain";
- power of control and of law enforcement of veterinarians.
In August 2006, the United States Food and Drug Administration approved phage therapy which involves spraying meat with viruses that infect bacteria, and thus preventing infection. This has raised concerns because without mandatory labeling, consumers would not know that meat and poultry products have been treated with the spray.
At home, prevention mainly consists of good food safety practices. Many forms of bacterial poisoning can be prevented by cooking food sufficiently, and either eating it quickly or refrigerating it effectively. Many toxins, however, are not destroyed by heat treatment.
Techniques that help prevent food borne illness in the kitchen are hand washing, rinsing produce, preventing cross-contamination, proper storage, and maintaining cooking temperatures. In general, freezing or refrigerating prevents virtually all bacteria from growing, and heating food sufficiently kills parasites, viruses, and most bacteria. Bacteria grow most rapidly at the range of temperatures between 40 and 140 °F (4 and 60 °C), called the "danger zone". Storing food below or above the "danger zone" can effectively limit the production of toxins. For storing leftovers, the food must be put in shallow containers for quick cooling and must be refrigerated within two hours. When food is reheated, it must reach an internal temperature of 165 °F (74 °C) or until hot or steaming to kill bacteria.
Mycotoxins and alimentary mycotoxicoses
The term alimentary mycotoxicosis refers to the effect of poisoning by mycotoxins through food consumption. The term mycotoxin is usually reserved for the toxic chemical compounds naturally produced by fungi that readily colonize crops under given temperature and moisture conditions. Mycotoxins can have important effects on human and animal health. For example, an outbreak which occurred in the UK during 1960 caused the death of 100,000 turkeys which had consumed aflatoxin-contaminated peanut meal. In the USSR in World War II, 5,000 people died due to alimentary toxic aleukia (ALA). In Kenya, mycotoxins led to the death of 125 people in 2004, after consumption of contaminated grains. In animals, mycotoxicosis targets organ systems such as liver and digestive system. Other effects can include reduced productivity and suppression of the immune system, thus pre-disposing the animals to other secondary infections. The common foodborne Mycotoxins include:
- Aflatoxins – originating from Aspergillus parasiticus and Aspergillus flavus. They are frequently found in tree nuts, peanuts, maize, sorghum and other oilseeds, including corn and cottonseeds. The pronounced forms of aflatoxins are those of B1, B2, G1, and G2, amongst which Aflatoxin B1 predominantly targets the liver, which will result in necrosis, cirrhosis, and carcinoma. Other forms of aflatoxins exist as metabolites such as Aflatoxin M1. In the US, the acceptable level of total aflatoxins in foods is less than 20 μg/kg, except for Aflatoxin M1 in milk, which should be less than 0.5 μg/kg The official document can be found at FDA's website. The European union has more stringent standards, set at 10 μg/kg in cereals and cereal products. These references are also adopted in other countries.
- Altertoxins – are those of alternariol (AOH), alternariol methyl ether (AME), altenuene (ALT), altertoxin-1 (ATX-1), tenuazonic acid (TeA), and radicinin (RAD), originating from Alternaria spp. Some of the toxins can be present in sorghum, ragi, wheat and tomatoes. Some research has shown that the toxins can be easily cross-contaminated between grain commodities, suggesting that manufacturing and storage of grain commodities is a critical practice.
- Citrinin
- Citreoviridin
- Cyclopiazonic acid
- Cytochalasins
- Ergot alkaloids / ergopeptine alkaloids – ergotamine
- Fumonisins – Crop corn can be easily contaminated by the fungi Fusarium moniliforme, and its fumonisin B1 will cause leukoencephalomalacia (LEM) in horses, pulmonary edema syndrome (PES) in pigs, liver cancer in rats and esophageal cancer in humans. For human and animal health, both the FDA and the EC have regulated the content levels of toxins in food and animal feed.
- Fusaric acid
- Fusarochromanone
- Kojic acid
- Lolitrem alkaloids
- Moniliformin
- 3-Nitropropionic acid
- Nivalenol
- Ochratoxins – In Australia, The Limit of Reporting (LOR) level for ochratoxin A (OTA) analyses in 20th Australian Total Diet Survey was 1 μg/kg, whereas the EC restricts the content of OTA to 5 μg/kg in cereal commodities, 3 μg/kg in processed products and 10 μg/kg in dried vine fruits.
- Oosporeine
- Patulin – Currently, this toxin has been advisably regulated on fruit products. The EC and the FDA have limited it to under 50 μg/kg for fruit juice and fruit nectar, while limits of 25 μg/kg for solid-contained fruit products and 10 μg/kg for baby foods were specified by the EC.
- Phomopsins
- Sporidesmin A
- Sterigmatocystin
- Tremorgenic mycotoxins – Five of them have been reported to be associated with molds found in fermented meats. These are fumitremorgen B, paxilline, penitrem A, verrucosidin, and verruculogen.
- Trichothecenes – sourced from Cephalosporium, Fusarium, Myrothecium, Stachybotrys, and Trichoderma. The toxins are usually found in molded maize, wheat, corn, peanuts and rice, or animal feed of hay and straw. Four trichothecenes, T-2 toxin, HT-2 toxin, diacetoxyscirpenol (DAS), and deoxynivalenol (DON) have been most commonly encountered by humans and animals. The consequences of oral intake of, or dermal exposure to, the toxins will result in alimentary toxic aleukia, neutropenia, aplastic anemia, thrombocytopenia and/or skin irritation. In 1993, the FDA issued a document for the content limits of DON in food and animal feed at an advisory level. In 2003, US published a patent that is very promising for farmers to produce a trichothecene-resistant crop.
- Zearalenone
- Zearalenols
Viruses
Viral infections make up perhaps one third of cases of food poisoning in developed countries. In the US, more than 50% of cases are viral and noroviruses are the most common foodborne illness, causing 57% of outbreaks in 2004. Foodborne viral infection are usually of intermediate (1–3 days) incubation period, causing illnesses which are self-limited in otherwise healthy individuals; they are similar to the bacterial forms described above.
- Enterovirus
- Hepatitis A is distinguished from other viral causes by its prolonged (2–6 week) incubation period and its ability to spread beyond the stomach and intestines into the liver. It often results in jaundice, or yellowing of the skin, but rarely leads to chronic liver dysfunction. The virus has been found to cause infection due to the consumption of fresh-cut produce which has fecal contamination.
- Hepatitis E
- Norovirus
- Rotavirus
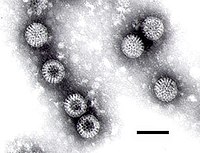
Rotavirus
Parasites
Most foodborne parasites are zoonoses.
- Platyhelminthes:
- Diphyllobothrium sp.
- Nanophyetus sp.
- Taenia saginata
- Taenia solium
- Fasciola hepatica
- See also: Tapeworm and Flatworm
- Nematode:
- Protozoa:
- Acanthamoeba and other free-living amoebae
- Cryptosporidiosis
- Cyclospora cayetanensis
- Entamoeba histolytica
- Giardia lamblia

Giardia lamblia - Sarcocystis hominis
- Sarcocystis suihominis
- Toxoplasma
Natural toxins
Several foods can naturally contain toxins, many of which are not produced by bacteria. Plants in particular may be toxic; animals which are naturally poisonous to eat are rare. In evolutionary terms, animals can escape being eaten by fleeing; plants can use only passive defenses such as poisons and distasteful substances, for example capsaicin in chili peppers and pungent sulfur compounds in garlic and onions. Most animal poisons are not synthesised by the animal, but acquired by eating poisonous plants to which the animal is immune, or by bacterial action.
- Alkaloids
- Ciguatera poisoning
- Grayanotoxin (honey intoxication)
- Hormones from the thyroid glands of slaughtered animals (especially triiodothyronine in cases of hamburger thyrotoxicosis or alimentary thyrotoxicosis)
- Mushroom toxins
- Phytohaemagglutinin (red kidney bean poisoning; destroyed by boiling)
- Pyrrolizidine alkaloids
- Shellfish toxin, including paralytic shellfish poisoning, diarrhetic shellfish poisoning, neurotoxic shellfish poisoning, amnesic shellfish poisoning and ciguatera fish poisoning
- Scombrotoxin
- Solanine (green potato poisoning)
- Tetrodotoxin (fugu fish poisoning)
Some plants contain substances which are toxic in large doses, but have therapeutic properties in appropriate dosages.
- Foxglove contains cardiac glycosides.
- Poisonous hemlock (conium) has medicinal uses.
Other pathogenic agents
- Prions, resulting in Creutzfeldt–Jakob disease (CJD) and its variant (vCJD)
"Ptomaine poisoning" misconception
Ptomaine poisoning was a myth that persisted in the public consciousness, in newspaper headlines, and legal cases as an official diagnosis, decades after it had been scientifically disproven in the 1910s.
In the 19th century, the Italian chemist Francesco Selmi, of Bologna, introduced the generic name ptomaine (from Greek ptōma, "fall, fallen body, corpse") for alkaloids found in decaying animal and vegetable matter, especially (as reflected in their names) putrescine and cadaverine. The 1892 Merck's Bulletin stated, "We name such products of bacterial origin ptomaines; and the special alkaloid produced by the comma bacillus is variously named Cadaverine, Putrescine, etc." while The Lancet stated, "The chemical ferments produced in the system, the... ptomaines which may exercise so disastrous an influence." It is now known that the "disastrous... influence" is due to the direct action of bacteria and only slightly due to the alkaloids. Thus, the use of the phrase "ptomaine poisoning" is now largely obsolete.
At a Communist political convention in Massillon, Ohio, and aboard a cruise ship in Washington, D.C., hundreds of people were sickened in separate incidents by tainted potato salad, during a single week in 1932, drawing national attention to the dangers of so-called "ptomaine poisoning" in the pages of the American news weekly, Time. In 1944, another newspaper article reported that over 150 people in Chicago were hospitalized with ptomaine poisoning, apparently from rice pudding served by a restaurant chain.
Mechanism
Incubation period
The delay between the consumption of contaminated food and the appearance of the first symptoms of illness is called the incubation period. This ranges from hours to days (and rarely months or even years, such as in the case of listeriosis or bovine spongiform encephalopathy), depending on the agent, and on how much was consumed. If symptoms occur within one to six hours after eating the food, it suggests that it is caused by a bacterial toxin or a chemical rather than live bacteria.
The long incubation period of many foodborne illnesses tends to cause those affected to attribute their symptoms to gastroenteritis.
During the incubation period, microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade the deeper body tissues. The symptoms produced depend on the type of microbe.
Infectious dose
The infectious dose is the amount of agent that must be consumed to give rise to symptoms of foodborne illness, and varies according to the agent and the consumer's age and overall health. Pathogens vary in minimum infectious dose; for example, Shigella sonnei has a low estimated minimum dose of < 500 colony-forming units (CFU) while Staphylococcus aureus has a relatively high estimate.
In the case of Salmonella a relatively large inoculum of 1 million to 1 billion organisms is necessary to produce symptoms in healthy human volunteers, as Salmonellae are very sensitive to acid. An unusually high stomach pH level (low acidity) greatly reduces the number of bacteria required to cause symptoms by a factor of between 10 and 100.
Gut microbiota unaccustomed to endemic organisms
Foodborne illness often occurs as travelers' diarrhea in persons whose gut microbiota is unaccustomed to organisms endemic to the visited region. This effect of microbiologic naïveté is compounded by any food safety lapses in the food's preparation.
Epidemiology
Asymptomatic subclinical infection may help spread these diseases, particularly Staphylococcus aureus, Campylobacter, Salmonella, Shigella, Enterobacter, Vibrio cholerae, and Yersinia. For example, as of 1984 it was estimated that in the United States, 200,000 people were asymptomatic carriers of Salmonella.
Infants
Main article: Infant food safetyGlobally, infants are a group that is especially vulnerable to foodborne disease. The World Health Organization has issued recommendations for the preparation, use and storage of prepared formulas. Breastfeeding remains the best preventive measure for protection from foodborne infections in infants.
United States
A CDC report for the period 2017–2019 found that 41% of outbreaks at restaurants were caused by a sick employee. Contributory factors identified included lack of written policy compliance with FDA recommendations for identifying red-flag symptoms, glove use, and hand washing; lack of paid sick leave at the majority of establishments; and social pressure to come to work even while sick. The remaining outbreaks had a variety of causes, including inadequate cooking, improper temperature, and cross-contamination.
In the United States, using FoodNet data from 2000 to 2007, the CDC estimated there were 47.8 million foodborne illnesses per year (16,000 cases for 100,000 inhabitants) with 9.4 million of these caused by 31 known identified pathogens.
- 127,839 were hospitalized (43 per 100,000 inhabitants per year).
- 3,037 people died (1.0 per 100,000 inhabitants per year).
|
|
United Kingdom
According to a 2012 report from the Food Standards Agency, there were around a million cases of foodborne illness per year (1,580 cases for 100,000 inhabitants).
- 20,000 people were hospitalised (32 per 100,000 inhabitants);
- 500 died (0.80 per 100,000 inhabitants).
France
This data pertains to reported medical cases of 23 specific pathogens in the 1990s, as opposed to total population estimates of all foodborne illness for the United States.
In France, for 735,590 to 769,615 cases of infection identified as being with the 23 specific pathogens, 238,836 to 269,085 were estimated to have been contracted from food:
- between 12,995 and 22,030 people were hospitalized (10,188 to 17,771 estimated to have contracted their infections from food);
- between 306 and 797 people died (228 to 691 estimated to have contracted their infections from food).
|
|
Australia
A study by the Australian National University published in 2022 for Food Standards Australia New Zealand estimated there are 4.67 million cases of food poisoning in Australia each year that result in 47,900 hospitalisations, 38 deaths and a cost to the economy of $2.1 billion.
A previous study using different methodology and published in November 2014, found in 2010 that there were an estimated 4.1 million cases of foodborne gastroenteritis acquired in Australia on average each year, along with 5,140 cases of non-gastrointestinal illness.
The main causes were norovirus, pathogenic Escherichia coli, Campylobacter spp. and non-typhoidal Salmonella spp., although the causes of approximately 80% of illnesses were unknown. Approximately 25% (90% CrI: 13%–42%) of the 15.9 million episodes of gastroenteritis that occur in Australia were estimated to be transmitted by contaminated food. This equates to an average of approximately one episode of foodborne gastroenteritis every five years per person. Data on the number of hospitalisations and deaths represent the occurrence of serious foodborne illness. Including gastroenteritis, non-gastroenteritis and sequelae, there were an estimated annual 31,920 (90% CrI: 29,500–35,500) hospitalisations due to foodborne illness and 86 (90% CrI: 70–105) deaths due to foodborne illness circa 2010. This study concludes that these rates are similar to recent estimates in the US and Canada.
A main aim of this study was to compare if foodborne illness incidence had increased over time. In this study, similar methods of assessment were applied to data from circa 2000, which showed that the rate of foodborne gastroenteritis had not changed significantly over time. Two key estimates were the total number of gastroenteritis episodes each year, and the proportion considered foodborne. In circa 2010, it was estimated that 25% of all episodes of gastroenteritis were foodborne. By applying this proportion of episodes due to food to the incidence of gastroenteritis circa 2000, there were an estimated 4.3 million (90% CrI: 2.2–7.3 million) episodes of foodborne gastroenteritis circa 2000, although credible intervals overlap with 2010. Taking into account changes in population size, applying these equivalent methods suggests a 17% decrease in the rate of foodborne gastroenteritis between 2000 and 2010, with considerable overlap of the 90% credible intervals.
This study replaces a previous estimate of 5.4 million cases of foodborne illness in Australia every year, causing:
- 18,000 hospitalizations
- 120 deaths (0.5 deaths per 100,000 inhabitants)
- 2.1 million lost days off work
- 1.2 million doctor consultations
- 300,000 prescriptions for antibiotics.
Most foodborne disease outbreaks in Australia have been linked to raw or minimally cooked eggs or poultry. The Australian Food Safety Information Council estimates that one third of cases of food poisoning occur in the home.
Outbreaks
Main article: Deadliest foodborne illness incidentsThe vast majority of reported cases of foodborne illness occur as individual or sporadic cases. The origin of most sporadic cases is undetermined. In the United States, where people eat outside the home frequently, 58% of cases originate from commercial food facilities (2004 FoodNet data). An outbreak is defined as occurring when two or more people experience similar illness after consuming food from a common source.
Often, a combination of events contributes to an outbreak, for example, food might be left at room temperature for many hours, allowing bacteria to multiply which is compounded by inadequate cooking which results in a failure to kill the dangerously elevated bacterial levels.
Outbreaks are usually identified when those affected know each other. Outbreaks can also be identified by public health staff when there are unexpected increases in laboratory results for certain strains of bacteria. Outbreak detection and investigation in the United States is primarily handled by local health jurisdictions and is inconsistent from district to district. It is estimated that 1–2% of outbreaks are detected.
Society and culture
United Kingdom
In Aberdeen, in 1964, a large-scale (>400 cases) outbreak of typhoid occurred, caused by contaminated corned beef which had been imported from Argentina. The corned beef was placed in cans and because the cooling plant had failed, cold river water from the Plate estuary was used to cool the cans. One of the cans had a defect and the meat inside was contaminated. That meat was then sliced using a meat slicer in a shop in Aberdeen, and a lack of machinery-cleaning led to the spreading of the contamination to other meats cut in the slicer. Those meats were eaten by people in Aberdeen who then became ill.
Serious outbreaks of foodborne illness since the 1970s prompted key changes in UK food safety law. The outbreaks included the deaths of 19 patients in the Stanley Royd Hospital outbreak and the bovine spongiform encephalopathy (BSE, mad cow disease) outbreak identified in the 1980s. The deaths of 21 people in the 1996 Wishaw outbreak of E. coli O157 was a precursor to the establishment of the Food Standards Agency which, according to Tony Blair in the 1998 white paper A Force for Change Cm 3830, "would be powerful, open and dedicated to the interests of consumers".
In May 2015, for the second year running, England's Food Standards Agency devoted its annual Food Safety Week to "The Chicken Challenge". The focus was on the handling of raw chicken in the home and in catering facilities in a drive to reduce the high levels of food poisoning from the campylobacter bacterium. Anne Hardy argues that widespread public education of food hygiene can be useful, particularly through media (TV cookery programmes) and advertisement. She points to the examples set by Scandinavian societies.
United States
Main article: Food safety in the United StatesIn 2001, the Center for Science in the Public Interest petitioned the United States Department of Agriculture to require meat packers to remove spinal cords before processing cattle carcasses for human consumption, a measure designed to lessen the risk of infection by variant Creutzfeldt–Jakob disease. The petition was supported by the American Public Health Association, the Consumer Federation of America, the Government Accountability Project, the National Consumers League, and Safe Tables Our Priority.
None of the US Department of Health and Human Services targets regarding incidence of foodborne infections were reached in 2007.
A report issued in June 2018 by NBC's Minneapolis station using research by both the CDC and the Minnesota Department of Health concluded that foodborne illness is on the rise in the U.S.
India
In India, Entamoeba is the most common cause of food illness, followed by Campylobacter bacteria, Salmonella bacteria, E. coli bacteria, and norovirus. According to statistics, food poisoning was the second most common cause of infectious disease outbreak in India in 2017. The numbers of outbreaks have increased from 50 in 2008 to 242 in 2017.
Organizations
The World Health Organization Department of Food Safety and Zoonoses (FOS) provides scientific advice for organizations and the public on issues concerning the safety of food. Its mission is to lower the burden of foodborne disease, thereby strengthening the health security and sustainable development of Member States. Foodborne and waterborne diarrhoeal diseases kill an estimated 2.2 million people annually, most of whom are children. WHO works closely with the Food and Agriculture Organization of the United Nations (FAO) to address food safety issues along the entire food production chain—from production to consumption—using new methods of risk analysis. These methods provide efficient, science-based tools to improve food safety, thereby benefiting both public health and economic development.
International Food Safety Authorities Network (INFOSAN)
The International Food Safety Authorities Network (INFOSAN) is a joint program of the WHO and FAO. INFOSAN has been connecting national authorities from around the globe since 2004, with the goal of preventing the international spread of contaminated food and foodborne disease and strengthening food safety systems globally. This is done by:
- Promoting the rapid exchange of information during food safety events;
- Sharing information on important food safety issues of global interest;
- Promoting partnership and collaboration between countries; and
- Helping countries strengthen their capacity to manage food safety risks.
Membership to INFOSAN is voluntary, but is restricted to representatives from national and regional government authorities and requires an official letter of designation. INFOSAN seeks to reflect the multidisciplinary nature of food safety and promote intersectoral collaboration by requesting the designation of Focal Points in each of the respective national authorities with a stake in food safety, and a single Emergency Contact Point in the national authority with the responsibility for coordinating national food safety emergencies; countries choosing to be members of INFOSAN are committed to sharing information between their respective food safety authorities and other INFOSAN members. The operational definition of a food safety authority includes those authorities involved in: food policy; risk assessment; food control and management; food inspection services; foodborne disease surveillance and response; laboratory services for monitoring and surveillance of foods and foodborne diseases; and food safety information, education and communication across the farm-to-table continuum.
Prioritisation of foodborne pathogens
The Food and Agriculture Organization of the United Nations and The World Health Organization have published a global ranking of foodborne parasites using a multicriteria ranking tool concluding that Taenia solium was the most relevant, followed by Echinococcus granulosus, Echinococcus multilocularis, and Toxoplasma gondii. The same method was used regionally to rank the most important foodborne parasites in Europe ranking Echinococcus multilocularis of highest relevance, followed by Toxoplasma gondii and Trichinella spiralis.
Regulatory steps
Food may be contaminated during all stages of food production and retailing. In order to prevent viral contamination, regulatory authorities in Europe have enacted several measures:
- European Commission Regulation (EC) No 2073/2005 of November 15, 2005
- European Committee for Standardization (CEN): Standard method for the detection of norovirus and hepatitis A virus in food products (shellfish, fruits and vegetables, surfaces and bottled water)
- CODEX Committee on Food Hygiene (CCFH): Guideline for the application of general principles of food hygiene for the control of viruses in food
See also
- American Public Health Association v. Butz
- Food allergy
- Food microbiology
- Food quality
- Food safety
- Food spoilage
- Food testing strips
- Gastroenteritis
- List of foodborne illness outbreaks by country
- List of food contamination incidents
- Mycotoxicology
- STOP Foodborne Illness
- United States Disease Control and Prevention
- Zoonotic pathogens
References
![]() This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
- "food poisoning" at Dorland's Medical Dictionary
- ^ "Foodborne Illness - Frequently Asked Questions". US Centers for Disease Control and Prevention. Archived from the original on March 3, 2011. Retrieved July 3, 2016.
- For foodborne illness caused by chemicals, see Food contaminants.
- "Chemicals, Metals & Pesticides in Food". Food and Drug Administration. 2021.
- "Reducing the risk from E. coli 0157 – controlling cross-contamination". Food Standards Agency, United Kingdom. February 2011. Archived from the original on April 16, 2014. Retrieved 14 August 2016.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - "Staphylococcal Food Poisoning". U.S. Centers for Disease Control and Prevention. Retrieved July 3, 2016.
- Chemistry, University of; Prague, Technology. "Chickensplash! Exploring the health concerns of washing raw chicken". phys.org. Retrieved October 3, 2022.
- Carmody CD, Mueller RC, Grodner BM, Chlumsky O, Wilking JN, McCalla SG (March 2022). "Chickensplash! Exploring the health concerns of washing raw chicken". Physics of Fluids. 34 (3): 031910. Bibcode:2022PhFl...34c1910C. doi:10.1063/5.0083979. PMC 8958727. PMID 35392485.
- Humphrey T, O'Brien S, Madsen M (July 2007). "Campylobacters as zoonotic pathogens: a food production perspective". International Journal of Food Microbiology. 117 (3): 237–257. doi:10.1016/j.ijfoodmicro.2007.01.006. PMID 17368847.
- "Foodborne Illness: What Consumers Need to Know". USDA.gov. Retrieved August 14, 2016.
- Kiu R, Caim S, Painset A, Pickard D, Swift C, Dougan G, et al. (October 2019). "Phylogenomic analysis of gastroenteritis-associated Clostridium perfringens in England and Wales over a 7-year period indicates distribution of clonal toxigenic strains in multiple outbreaks and extensive involvement of enterotoxin-encoding (CPE) plasmids". Microbial Genomics. 5 (10): e000297. doi:10.1099/mgen.0.000297. PMC 6861862. PMID 31553300.
- Tribe IG, Cowell D, Cameron P, Cameron S (2002). "An outbreak of Salmonella typhimurium phage type 135 infection linked to the consumption of raw shell eggs in an aged care facility". Communicable Diseases Intelligence Quarterly Report. 26 (1): 38–39. PMID 11950200. Archived from the original on February 17, 2014.
- "Salmonella Infection (salmonellosis) and Animals". Centers for Disease Control and Prevention. Archived from the original on July 4, 2007. Retrieved August 12, 2007.
- Doyle MP, Erickson MC (June 2006). "Reducing the carriage of foodborne pathogens in livestock and poultry". Poultry Science. 85 (6): 960–973. doi:10.1093/ps/85.6.960. PMID 16776463.
- CDC (March 18, 2020). "Foodborne Germs and Illnesses".
- Food poisoning: Causes. Mayo Clinic.
- ^ Argudín MÁ, Mendoza MC, Rodicio MR (July 2010). "Food poisoning and Staphylococcus aureus enterotoxins". Toxins. 2 (7): 1751–1773. doi:10.3390/toxins2071751. PMC 3153270. PMID 22069659.
- Staphylococcus aureus: A Problem When Food Is Left Out Too Long. Ohio State University Extension HYG-5564-11].
- Karlsson PA, Tano E, Jernberg C, Hickman RA, Guy L, Järhult JD, Wang H (May 13, 2021). "Molecular Characterization of Multidrug-Resistant Yersinia enterocolitica From Foodborne Outbreaks in Sweden". Frontiers in Microbiology. 12: 664665. doi:10.3389/fmicb.2021.664665. PMC 8155512. PMID 34054769.
- "FDA Says Viruses Safe for Treating Meat". Archived from the original on August 25, 2006. Retrieved September 2, 2014.
- DeRusha J (November 9, 2010). "Good Question: Does Washing Fruit Do Anything?". Retrieved September 18, 2016.
- How Temperatures Affect Food. U.D. Department of Agriculture
- Mount M. "Fungi and Mycotoxins" (PDF). vetmed.ucdavis.edu. Archived from the original (PDF) on September 27, 2007. Retrieved August 11, 2007.
- "Outbreak of Aflatoxin Poisoning --- Eastern and Central Provinces, Kenya, January--July 2004".
- Kępińska-Pacelik, Jagoda; Biel, Wioletta (2021). "Mycotoxins—Prevention, Detection, Impact on Animal Health". Processes. 9 (11): 2035. doi:10.3390/pr9112035.
- "Aflatoxins". Center for Food Safety & Applied Nutrition. Retrieved August 12, 2007.
- "GASGA Technical Leaflet – 3 Mycotoxins in Grain". Food and Agriculture Organization of the United Nations. Archived from the original on January 12, 2017. Retrieved August 12, 2007.
- "Sec. 683.100 Action Levels for Aflatoxins in Animal Feeds (CPG 7126.33)". Food and Drug Administration. Retrieved August 13, 2007.
- Henry MH. "Mycotoxins in Feeds: CVM's Perspective". FDA.gov. Retrieved January 1, 2012.
- "Aflatoxins (Sum of B1, B2, G1, G2) in cereals and cereal-derived food products". EFSA Supporting Publications. 10 (3). 2013. doi:10.2903/sp.efsa.2013.EN-406.
- "Chapter 2 Foodborne Hazards in Basic Food Safety for Health Workers" (PDF). World Health Organization. Archived from the original (PDF) on September 27, 2007. Retrieved August 12, 2007.
- Webley DJ, Jackson KL, Mullins JD, Hocking AD, Pitt JI (1997). "Alternaria toxins in weather-damaged wheat and sorghum in the 1995–1996 Australian harvest". Australian Journal of Agricultural Research. 48 (8): 1249–56. doi:10.1071/A97005.
- Li FQ, Yoshizawa T (July 2000). "Alternaria mycotoxins in weathered wheat from China". Journal of Agricultural and Food Chemistry. 48 (7): 2920–2924. doi:10.1021/jf0000171. PMID 10898645.
- Motta SD, Valente Soares LM (July 2001). "Survey of Brazilian tomato products for alternariol, alternariol monomethyl ether, tenuazonic acid and cyclopiazonic acid". Food Additives and Contaminants. 18 (7): 630–634. doi:10.1080/02652030117707. PMID 11469319. S2CID 45938351.
- Li FQ, Toyazaki N, Yoshizawa T (April 2001). "Production of alternaria mycotoxins by Alternaria alternata isolated from weather-damaged wheat". Journal of Food Protection. 64 (4): 567–571. doi:10.4315/0362-028X-64.4.567. PMID 11307900.
- Marasas WF (1995). "Fumonisins: their implications for human and animal health". Natural Toxins. 3 (4): 193–8, discussion 221. doi:10.1002/nt.2620030405. PMID 7582616.
- Soriano JM (2004). "Occurrence of fumonisins in foods". Food Research International. 37 (10): 985–1000. doi:10.1016/j.foodres.2004.06.009.
- "CVM and Fumonisins". Food and Drug Administration. Archived from the original on August 12, 2007. Retrieved August 13, 2007.
- "More contaminated maize meal products withdrawn from sale". Food Standards Agency. Archived from the original on August 13, 2007. Retrieved August 12, 2007.
- "20th Australian Total Diet Survey – Part B". Food Standards Australia New Zealand. Archived from the original on September 2, 2007. Retrieved August 13, 2007.
- ^ "Worldwide regulations for mycotoxins in food and feed in 2003". FAO FOOD AND NUTRITION PAPER 81. Retrieved August 13, 2007.
- "Patulin in Apple Juice, Apple Juice Concentrates and Apple Juice Products". Food and Drug Administration. Archived from the original on September 12, 2007. Retrieved August 16, 2007.
- Sabater-Vilar M, Nijmeijer S, Fink-Gremmels J (November 2003). "Genotoxicity assessment of five tremorgenic mycotoxins (fumitremorgen B, paxilline, penitrem A, verruculogen, and verrucosidin) produced by molds isolated from fermented meats". Journal of Food Protection. 66 (11): 2123–2129. doi:10.4315/0362-028X-66.11.2123. PMID 14627292.
- Adejumo TO, Hettwer U, Karlovsky P (May 2007). "Occurrence of Fusarium species and trichothecenes in Nigerian maize". International Journal of Food Microbiology. 116 (3): 350–357. doi:10.1016/j.ijfoodmicro.2007.02.009. PMID 17412440.
- Mazur LJ, Kim J (December 2006). "Spectrum of noninfectious health effects from molds". Pediatrics. 118 (6): e1909 – e1926. doi:10.1542/peds.2006-2829. PMID 17142508.
- Froquet R, Sibiril Y, Parent-Massin D (February 2001). "Trichothecene toxicity on human megakaryocyte progenitors (CFU-MK)". Human & Experimental Toxicology. 20 (2): 84–89. Bibcode:2001HETox..20...84F. doi:10.1191/096032701677428611. PMID 11327514. S2CID 37767457.
- Joffe AZ, Yagen B (February 1977). "Comparative study of the yield of T-2 toxic produced by Fusarium poae, F. sporotrichioides and F. sporotrichioides var. tricinctum strains from different sources". Mycopathologia. 60 (2): 93–97. doi:10.1007/bf00490378. PMID 846559. S2CID 39431820.
- Hay RJ (April 2007). "Fusarium infections of the skin". Current Opinion in Infectious Diseases. 20 (2): 115–117. doi:10.1097/QCO.0b013e328014392d. PMID 17496567.
- "Guidance for Industry and FDA – Letter to State Agricultural Directors, State Feed Control Officials, and Food, Feed, and Grain Trade Organizations". Food and Drug Administration. Archived from the original on June 9, 2007. Retrieved August 13, 2007.
- Hohn, Thomas M. "Trichothecene-resistant transgenic plants". U.S. patent 6,646,184. Priority date March 31, 1999.
- Dubois E, Hennechart C, Deboosère N, Merle G, Legeay O, Burger C, et al. (April 2006). "Intra-laboratory validation of a concentration method adapted for the enumeration of infectious F-specific RNA coliphage, enterovirus, and hepatitis A virus from inoculated leaves of salad vegetables". International Journal of Food Microbiology. 108 (2): 164–171. doi:10.1016/j.ijfoodmicro.2005.11.007. PMID 16387377.
- Schmidt HM (2004). Improving the microbiological quality and safety of fresh-cut tomatoes by low dose electron beam irradiation (MS thesis). Texas A&M University. hdl:1969.1/2767. Retrieved December 14, 2022.
- Murrell KD (August 2013). "Zoonotic foodborne parasites and their surveillance". Revue Scientifique et Technique. 32 (2): 559–569. doi:10.20506/rst.32.2.2239. PMID 24547659.
- Britannica (2021). "Nematode".
- Wartique L, Pothen L, Pirson N, Hermans MP, Lambert M, Yildiz H (December 2017). "An unusual cause of epidemic thyrotoxicosis". Acta Clinica Belgica. 72 (6): 451–453. doi:10.1080/17843286.2017.1309336. PMID 28361645. S2CID 24489342.
- Hedberg CW, Fishbein DB, Janssen RS, Meyers B, McMillen JM, MacDonald KL, et al. (April 1987). "An outbreak of thyrotoxicosis caused by the consumption of bovine thyroid gland in ground beef". The New England Journal of Medicine. 316 (16): 993–998. doi:10.1056/NEJM198704163161605. PMID 3561455.
- Parmar MS, Sturge C (September 2003). "Recurrent hamburger thyrotoxicosis". CMAJ. 169 (5): 415–417. PMC 183292. PMID 12952802.
- Broome MR, Peterson ME, Kemppainen RJ, Parker VJ, Richter KP (January 2015). "Exogenous thyrotoxicosis in dogs attributable to consumption of all-meat commercial dog food or treats containing excessive thyroid hormone: 14 cases (2008-2013)". Journal of the American Veterinary Medical Association. 246 (1): 105–111. doi:10.2460/javma.246.1.105. PMID 25517332.
- Hendriks LE, Looij BJ (March 2010). "Hyperthyroidism caused by excessive consumption of sausages". The Netherlands Journal of Medicine. 68 (3): 135–137. PMID 20308711.
- Kinney JS, Hurwitz ES, Fishbein DB, Woolf PD, Pinsky PF, Lawrence DN, et al. (January 1988). "Community outbreak of thyrotoxicosis: epidemiology, immunogenetic characteristics, and long-term outcome". The American Journal of Medicine. 84 (1): 10–18. doi:10.1016/0002-9343(88)90002-2. PMID 3257352.
- Brend, W. A. (May 25, 1934). "The Ptomaine-Poisoning Myth". The Spectator.
- Oxford English Dictionary (First ed.). London: Oxford University Press. 1933. p. 1557.
- Merck's Bulletin, Volume 5, William Henry Porter, 1892.
- Lancet, 3 Oct 1891, page 752
- "Report Next Week," Evening Independent (Massillon, OH), July 22, 1932, pg. 6
- "Medicine: Potato Salad," Time, August 1, 1932.
- "Poisoning Hits 150 in Chicago". Kenosha Evening News. May 27, 1944. Archived from the original on April 27, 2021. Retrieved March 9, 2015.
- Lee RM, Lessler J, Lee RA, Rudolph KE, Reich NG, Perl TM, Cummings DA (September 2013). "Incubation periods of viral gastroenteritis: a systematic review". BMC Infectious Diseases. 13: 446. doi:10.1186/1471-2334-13-446. PMC 3849296. PMID 24066865.
- "Food-Related Diseases". US Centers for Disease Control and Prevention. March 29, 2018.
- ^ Greig JD. "Infective Doses and Pathogen Carriage". ResearchGate.
- Owens, Michael D (January 2014) Salmonella Infection in Emergency Medicine. emedicine.com
- FAO/WHO (2006). World Health Organization (ed.). "Enterobacter sakazakii and Salmonella in powdered infant formula" (Meeting report). Microbiological risk assessment series 10. Archived from the original on April 2, 2015.
- Foodborne Illness Outbreaks at Retail Food Establishments — National Environmental Assessment Reporting System, 25 State and Local Health Departments, 2017–2019
- Food poisoning often caused by sick restaurant workers, CDC says
- Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM (January 2011). "Foodborne illness acquired in the United States--unspecified agents". Emerging Infectious Diseases. 17 (1): 16–22. doi:10.3201/eid1701.P21101. PMC 3204615. PMID 21192849.
- ^ Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al. (January 2011). "Foodborne illness acquired in the United States--major pathogens". Emerging Infectious Diseases. 17 (1): 7–15. doi:10.3201/eid1701.P11101. PMC 3375761. PMID 21192848.
- "Obama Proposes Single Overseer for Food Safety". The New York Times. February 20, 2015. Retrieved February 22, 2015.
According to the C.D.C., an estimated 87 million Americans are sickened each year by contaminated food, 371,000 are hospitalized with food-related illness and 5,700 die from food-related disease
- ^ Sabrina Tavernise (July 26, 2013). "F.D.A. Says Importers Must Audit Food Safety". The New York Times. Retrieved July 27, 2013.
One in every six Americans becomes ill from eating contaminated food each year, Dr. Margaret A. Hamburg, F.D.A. commissioner, estimated. About 130,000 are hospitalized and 3,000 die.
- ^ Stephanie Strom (January 4, 2013). "F.D.A. Offers Sweeping Rules to Fight Food Contamination". The New York Times. Retrieved January 5, 2013.
One in six Americans becomes ill from eating contaminated food each year, the government estimates; of those, roughly 130,000 are hospitalized and 3,000 die.
- ^ "Annual Report of the Chief Scientist 2012/13" (PDF). Food Standards Agency. England. 2013.
- ^ Liebling A, Maruna S, McAra L (2017). The Oxford Handbook of Criminology. Oxford University Press. p. 290. ISBN 978-0-19-871944-1.
- ^ "Report of the French sanitary agencies" (PDF) (in French). INVS/Afssa. Archived from the original (PDF) on March 3, 2016. Retrieved October 6, 2004.
- "Summary of Report of the French sanitary agencies" (PDF) (in French). INVS/Afssa. Archived from the original (PDF) on March 3, 2016. Retrieved October 6, 2004.
- "The Annual Cost of Foodborne Illness in Australia Final Report September 2022" (PDF). Food Standards Australia New Zealand. Australian National University. Retrieved April 8, 2023.
- Kirk, Martyn (2014). "Foodborne Illness, Australia, Circa 2000 and Circa 2010". Emerging Infectious Diseases. 20 (11). Emerging Infectious Diseases v 20:11: 1857–1864. doi:10.3201/eid2011.131315. PMC 4214288. PMID 25340705.
- "Foodborne illness in Australia. Annual incidence circa 2000" (PDF). OzFoodNet. p. 10. Archived from the original (PDF) on January 25, 2014.
- Astridge K, McPherson M, Knope K, Gregory J, Kardamanidis K, Bell E, et al. (2011). "Foodborne disease outbreaks in Australia 2001-2009". Food Australia. 63 (12): 44–50.
- "Food Hygiene". BUPA. Archived from the original on December 11, 2015. Retrieved September 13, 2015.
- Smith, David F.; Diack, H. Lesley and Pennington, T. Hugh (2005) Food Poisoning, Policy and Politics : Corned Beef and Typhoid in Britain in the 1960s. Boydell Press. ISBN 1-84383-138-4
- Brian Deer (February 24, 1985). "Food poison deaths probe may reveal NHS flaws". The Sunday Times.
- "BBC News - Health - Sheriff criticises E. coli butcher".
- Cowden JM, Ahmed S, Donaghy M, Riley A (June 2001). "Epidemiological investigation of the central Scotland outbreak of Escherichia coli O157 infection, November to December 1996". Epidemiology and Infection. 126 (3): 335–341. doi:10.1017/S0950268801005520. PMC 2869700. PMID 11467789.
- "The Food Standards Agency: A Force for Change". gov.uk. Food Standards Agency, United Kingdom. January 14, 1998. Retrieved August 14, 2016.
- Hardy A (January 13, 2016). "Food Poisoning: An On-going Saga". History and Policy. Retrieved July 4, 2016.
- "Meat Produced by Advanced Meat/Bone Separation Machinery and Meat Recovery (AMR) Systems". Federal Register. U.S. National Archive and Records Administration. January 12, 2004. Retrieved July 3, 2016.
- "Healthy People 2010 Home Page".
- Centers for Disease Control Prevention (CDC) (April 2008). "Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food--10 states, 2007". MMWR. Morbidity and Mortality Weekly Report. 57 (14): 366–370. PMID 18401330.
- Severson G (June 15, 2018). "Why are we seeing so many food recalls?". KARE 11. Retrieved June 19, 2018.
- ^ "Symptoms of food poisoning". The Times of India. ISSN 0971-8257. Retrieved May 29, 2023.
- Multicriteria-based ranking for risk management of foodborne parasites. Microbiological Risk Assessment Series No. 23. FAO/WHO. 2014. ISBN 978-92-5-108199-0.
- Bouwknegt M, Devleesschauwer B, Graham H, Robertson LJ, van der Giessen JW (March 2018). "Prioritisation of food-borne parasites in Europe, 2016". Euro Surveillance. 23 (9). doi:10.2807/1560-7917.ES.2018.23.9.17-00161. PMC 5840924. PMID 29510783.
- "Codex Committee on Food Hygiene (CCFH)", European Commission, Retrieved April 7, 2015
Further reading
Periodicals
- International Journal of Food Microbiology, ISSN 0168-1605, Elsevier
- Foodborne Pathogens and Disease, ISSN 1535-3141, Mary Ann Liebert, Inc.
- Mycopathologia, ISSN 1573-0832 (electronic), ISSN 0301-486X (paper), Springer
Books
- Hocking AD, Pitt JI, Samson RA, Thrane U (2005). Advances in Food Mycology. Springer. ISBN 978-0-387-28385-2. ISBN 978-0-387-28391-3 (electronic).
- Hobbs BC (1993). Food Poisoning and Food Hygiene. Vol. 7. Edward Arnold. pp. 167–70. doi:10.1093/oxfordjournals.bmb.a073825. ISBN 978-0-340-53740-4. PMID 14821218.
{{cite book}}:|journal=ignored (help) - Riemann HP, Cliver DO (2006). FoodBorne Infections and Intoxications. Academic Press. ISBN 978-0-12-588365-8.
- Smith JL (2005). Fratamico PM, Bhunia AK, Smith JL (eds.). Foodborne Pathogens: Microbiology And Molecular Biology. Horizon Scientific Press. ISBN 978-1-904455-00-4.
External links
- Foodborne diseases, emerging, WHO, Fact sheet N°124, revised January 2002
- Foodborne illness information pages Archived December 30, 2019, at the Wayback Machine, NSW Food Authority
- Food safety and foodborne illness, WHO, Fact sheet N°237, revised January 2002
- UK Health protection Agency
- US PulseNet
- Food poisoning from NHS Direct Online
- Food Safety Network hosted at the University of Guelph, Canada.
- Food Standard Agency website
| Consumer food safety | |
|---|---|
| Adulterants, food contaminants | |
| Food additives | |
| Intestinal parasites, parasitic disease | |
| Microorganisms | |
| Pesticides | |
| Preservatives | |
| Sugar substitutes | |
| Toxins, poisons, environment pollution | |
| Food fraud | |
| Food processing | |
| Food contamination incidents |
|
| Regulation, standards, watchdogs | |
| Institutions |
|
| Related topics | |