| Revision as of 00:42, 12 December 2008 editLegobot (talk | contribs)Bots1,668,137 editsm Robot - Moving category Diseases to Diseases and disorders per CFD at Misplaced Pages:Categories for discussion/Log/2008 December 2.← Previous edit | Latest revision as of 08:20, 15 August 2024 edit undoIntentionallyDense (talk | contribs)Extended confirmed users, New page reviewers, Pending changes reviewers34,530 edits Adding/improving reference(s) | ||
| (315 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Human disease caused by long-term exposure to coal dust}} | |||
| {{DiseaseDisorder infobox | | |||
| {{Infobox medical condition | |||
| Name = Coalworker's pneumoconiosis| | |||
| |
| name = Black lung disease | ||
| | image = BIRMINGHAM COAL MINER'S LUNG SHOWING EFFECT OF BLACK LUNG DISEASE. (FROM THE SITES EXHIBITION. FOR OTHER IMAGES IN... - NARA - 553848.jpg | |||
| ICD9 = {{ICD9|500}} | | |||
| |
| caption = Lung affected by black lung disease | ||
| | pronounce = | |||
| Image = Coal anthracite.jpg | | |||
| |
| field = ] | ||
| | synonyms = Coal workers' pneumoconiosis, anthracosis, black lung, coal mine dust lung disease | |||
| OMIM = | | |||
| |
| symptoms = | ||
| | complications = ] | |||
| eMedicineSubj = med | | |||
| | onset = | |||
| eMedicineTopic = 398 | | |||
| |
| duration = | ||
| |
| types = {{flatlist|*Anthracosis | ||
| *Simple coal workers’ pneumoconiosis | |||
| *Progressive massive fibrosis}} | |||
| | causes = Prolonged exposure to ] | |||
| | risks = | |||
| | diagnosis = | |||
| | differential = | |||
| | prevention = | |||
| | treatment = | |||
| | medication = | |||
| | prognosis = | |||
| | frequency = | |||
| | deaths = 25,000 per year (2013) | |||
| }} | }} | ||
| {{Coal sidebar|state=collapsed}} | |||
| '''Black lung disease''', also known as ''coal workers' ]'' (CWP), is caused by long exposure to ]. It is a common affliction of coal miners and others who work with coal, similar to both ] from inhaling silica dust, and to the long term effects of ] smoking. Inhaled coal dust progressively builds up in the lungs and is unable to be removed by the body, leading to ], ], and in the worst case ]. | |||
| '''Black lung disease''' ('''BLD'''), also known as '''coal workers' pneumoconiosis''',<ref>{{Cite web |date=2023-05-05 |title=Coal Workers’ Pneumoconiosis, Simple CWP {{!}} NIOSH {{!}} CDC |url=https://www.cdc.gov/niosh/learning/b-reader/pathology/pneumoconiosis/1.html |access-date=2024-06-18 |website=www.cdc.gov |language=en-us}}</ref> or simply '''black lung''', is an ] type of ] caused by long-term inhalation and deposition of ] in the lungs and the consequent lung tissue's reaction to its presence.<ref>{{Cite web |date=2019-11-19 |title=Pneumoconiosis |url=https://www.hopkinsmedicine.org/health/conditions-and-diseases/pneumoconiosis |access-date=2024-04-28 |website=www.hopkinsmedicine.org |language=en}}</ref> It is common in coal miners and others who work with coal. It is similar to both ] from inhaling ] and ] from inhaling ] dust.<ref>{{Cite web|url=https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/pneumoconiosis/pneumoconiosis-symptoms-causes-risks.html|title=Pneumoconiosis Symptoms, Causes and Risk Factors|website=American Lung Association|language=en|access-date=2019-04-25}}</ref> Inhaled coal dust progressively builds up in the ]s and leads to ], ], and in worse cases, ]. | |||
| Black lung disease develops after the initial, milder form of the disease known as '''anthracosis''' (from the Greek {{lang|grc|ἄνθραξ}}, or {{transliteration|grc|ánthrax}} – coal, carbon). This is often asymptomatic and is found to at least some extent in all urban dwellers<ref name="robspath">{{cite book | title=Robbins Pathologic Basis of Disease| last=Cotran|author2=Kumar, Collins| publisher=W.B Saunders Company| location=Philadelphia| isbn=978-0-7216-7335-6| year=1999}}</ref> due to ]. Prolonged exposure to large amounts of coal dust can result in more serious forms of the disease, ''simple coal workers' pneumoconiosis'' and ''complicated coal workers' pneumoconiosis'' (or ], PMF).<ref>{{Cite web|url=https://medlineplus.gov/ency/article/000130.htm|title=Coal worker's pneumoconiosis: MedlinePlus Medical Encyclopedia|website=medlineplus.gov|language=en|access-date=2019-04-25}}</ref><ref>{{Cite web |last=Says |first=Stephen Smyth |date=2023-02-27 |title=Modern Coal Miners Have Higher Death Rates From Lung Diseases Than Their Predecessors {{!}} Blogs {{!}} CDC |url=https://blogs.cdc.gov/niosh-science-blog/2023/02/27/mining-lung-disease/ |access-date=2023-05-28 |language=en-us}}</ref> More commonly, workers exposed to coal dust develop industrial bronchitis,<ref>{{cite journal |author=Morgan WK |title=Industrial bronchitis |journal=Br J Ind Med |volume=35 |issue=4 |pages=285–91 |date=November 1978 |doi=10.1136/oem.35.4.285 |pmid=367424 |pmc=1008445 }}</ref> clinically defined as ] (i.e. a productive cough for three months per year for at least two years) associated with workplace dust exposure. The incidence of industrial bronchitis varies with age, job, exposure, and smoking. In non-smokers (who are less prone to develop bronchitis than smokers), studies of coal miners have shown a 16%<ref>{{cite journal |vauthors=Seixas NS, Robins TG, Attfield MD, Moulton LH |title=Exposure-response relationships for coal mine dust and obstructive lung disease following enactment of the Federal Coal Mine Health and Safety Act of 1969 |journal=Am. J. Ind. Med. |volume=21 |issue=5 |pages=715–34 |year=1992 |pmid=1609817 |doi=10.1002/ajim.4700210511}}</ref> to 17%<ref>{{cite journal |vauthors=Marine WM, Gurr D, Jacobsen M |title=Clinically important respiratory effects of dust exposure and smoking in British coal miners |journal=Am. Rev. Respir. Dis. |volume=137 |issue=1 |pages=106–12 |date=January 1988 |pmid=3337449 |doi=10.1164/ajrccm/137.1.106}}</ref> incidence of industrial bronchitis.<!-- Epidemiology --> | |||
| In 2013, BLD resulted in 25,000 deaths globally—down from 29,000 deaths in 1990.<ref name="GDB2013">{{cite journal|title=Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013.|journal=Lancet|date=17 December 2014|pmid=25530442|doi=10.1016/S0140-6736(14)61682-2|volume=385|issue=9963|pages=117–71|pmc=4340604}}</ref> In the US, a 2018 study by the National Institute of Occupational Safety and Health shows a resurgence among veteran coalminers, recording the highest rate of BLD in roughly two decades.<ref>{{cite web | |||
| ==History and prevention efforts== | |||
| |url=https://www.reuters.com/article/us-usa-coal-blacklung/a-tenth-of-us-veteran-coal-miners-have-black-lung-disease-niosh-idUSKBN1K92W1 | |||
| There are currently about 42,000 underground coal miners actively working in the United States. The mining and production of coal is a major part of the economy in several developed countries. In the past 10 years, over 10,000 American miners have died from CWP. Although this disease is preventable, many miners are still developing advanced and severe cases. | |||
| |title=A tenth of U.S. veteran coal miners have black lung disease:NIOSH | |||
| |author=Richard Valdmanis | |||
| |date=19 July 2018 | |||
| |publisher=] | |||
| }}</ref> | |||
| == Pathogenesis == | |||
| In the 25 years since the Federal Coal Mine Health and Safety Act of 1969 became law, the proportion of miners with black lung disease has gone down by about 90%. But the downward trend of this disease in coal miners has stopped. Rates of black lung are on the rise and have almost doubled in the last 10 years. From 2000 to 2004, over 4,000 miners died from black lung disease in the United States. | |||
| Coal dust is not as ] as silica dust.<ref>{{cite journal |vauthors=Castranova V, Vallyathan V |title=Silicosis and coal workers' pneumoconiosis |journal=Environ. Health Perspect. |volume=108 |issue=Suppl 4|pages=675–84 |date=August 2000 |pmid=10931786 |pmc=1637684 |doi=10.1289/ehp.00108s4675}}</ref> Coal dust that enters the lungs can neither be destroyed nor removed by the body. The particles are engulfed by resident ] or interstitial ] and remain in the lungs, residing in the connective tissue or pulmonary ]s. Coal dust provides a sufficient stimulus for the macrophage to release various products, including enzymes, ], ], and ],<ref>{{cite journal |vauthors=Vanhée D, Gosset P, Boitelle A, Wallaert B, Tonnel AB |title=Cytokines and cytokine network in silicosis and coal workers' pneumoconiosis |journal=Eur. Respir. J. |volume=8 |issue=5 |pages=834–42 |date=May 1995 |doi=10.1183/09031936.95.08050834 |pmid=7656959 |s2cid=33011018 |url=http://erj.ersjournals.com/cgi/pmidlookup?view=long&pmid=7656959|doi-access=free }}</ref> which are important in the development of inflammation and fibrosis in BLD. Aggregations of carbon-laden macrophages can be visualized under a microscope as granular, black areas. In serious cases, the lung may grossly appear black. These aggregations can cause inflammation and fibrosis, as well as the formation of nodular ]s within the lungs. The centers of dense lesions may become necrotic due to ], leading to large cavities within the lung. | |||
| === Appearance === | |||
| The National Institute for Occupational Safety and Health (NIOSH), with support of the Mine Safety and Health Administration (MSHA), has started a Mobile Health Screening Program. This Mobile Unit travels to mining regions around the United States. Miners who participate in the Program receive health evaluations once every five years, at no cost to themselves. Chest x-rays can detect the early signs of and changes in CWP, often before the miner is aware of any lung problems. The screening program is only available to current miners.<ref>{{cite web | title = Enhanced Coal Workers' Health Surveillance Program | publisher = National Institute for Occupational Safety and Health | date = November 12, 2008 | url = http://www.cdc.gov/niosh/topics/surveillance/ORDS/ecwhsp.html | accessdate = November 24, 2008}}</ref> | |||
| Simple BLD is marked by the presence of {{convert|1|–|2|mm|abbr=on}} nodular aggregations of anthracotic macrophages, supported by a fine collagen network, within the lungs. Those 1–2 mm in diameter are known as ''coal macules'', with larger aggregations known as ''coal nodules''. These structures occur most frequently around the initial site of coal dust accumulation—the upper regions of the lungs around ]s.<ref name="robspath"/> The coal macule is the basic pathological feature of BLD and has a surrounding area of enlargement of the ], known as ].<ref>{{cite journal |title=Pathology standards for coal workers' pneumoconiosis. Report of the Pneumoconiosis Committee of the College of American Pathologists to the National Institute for Occupational Safety and Health |journal=Arch. Pathol. Lab. Med. |volume=103 |issue=8 |pages=375–432 |date=July 1979 |pmid=378179 }}</ref><ref name="Weinberger">{{cite book |last1=Weinberger |first1=S |last2=Cockrill |first2=B |last3=Mandel |first3=J |title=Principles of pulmonary medicine |date=2019 |isbn=9780323523714 |page=147 |publisher=Elsevier |edition=Seventh}}</ref> Focal emphysema extends into progressive ]. Less commonly a variant of ] develops.<ref name="NIOSH">{{cite web |title=Pathology Basis of Occupational Lung Disease, Pneumoconiosis {{!}} NIOSH {{!}} CDC |url=https://www.cdc.gov/niosh/learning/b-reader/pathology/pneumoconiosis/1.html |website=www.cdc.gov |access-date=29 July 2021 |language=en-us |date=5 August 2020}}</ref> | |||
| Continued exposure to coal dust following the development of simple BLD may progress to complicated BLD with ] (PMF), wherein large masses of dense fibrosis develop, usually in the upper lung zones, measuring greater than {{convert|1|cm|abbr=on}} in diameter, with accompanying decreased lung function. These cases generally require a number of years to develop. Grossly, the lung itself appears blackened. Pathologically, these consist of fibrosis with haphazardly-arranged collagen and many pigment-laden macrophages and abundant free pigment. Radiographically, BLD can appear strikingly similar to ]. In simple BLD, small rounded nodules predominate, tending to first appear in the upper lung zones. The nodules may coalesce and form large opacities (>1 cm), characterizing complicated BLD, or PMF. | |||
| == Pathogenesis == | |||
| Coal dust that enters the lungs can neither be destroyed nor removed by the body. The particles are engulfed by resident alveolar or interstitial ]s and remain in the lungs, residing in the connective tissue or pulmonary ]s. Aggregations of carbon-laden macrophages can be visualised under a microscope as granular, black areas. In serious cases, the lung may grossly appear black. These aggregations can cause inflammation and fibrosis, as well as the formation of nodular ]s within the lungs. The centres of dense lesions may become necrotic due to ], leading to large cavities within the lung | |||
| == |
==Diagnosis== | ||
| {{See also|ILO Classification}}] of anthracosis, with interstitial pigment deposition (black arrow) and an anthracotic ] (white arrow)]] | |||
| <!-- Image with unknown copyright status removed: ] --> | |||
| There are three basic criteria for the diagnosis of BLD: | |||
| Simple CWP is marked by the presence of 1-2mm nodular aggregations of anthracotic macrophages, supported by a fine collagen network, within the lungs. Those 1-2mm in diameter are known as ''coal macules'', with larger aggregations known as ''coal nodules''. These structures occur most frequently around the initial site of coal dust accumulation - the upper regions of the lungs around ]s<ref name="robspath">{{cite book | title=Robbins Pathologic Basis of Disease| last=Cotran| coauthors=Kumar, Collins| publisher=W.B Saunders Company| location=Philadelphia| id=0-7216-7335-X}}</ref>. | |||
| #] consistent with BLD | |||
| #An exposure history to coal dust (typically underground coal mining) of sufficient amount and latency | |||
| #Exclusion of alternative diagnoses (mimics of BLD) | |||
| Symptoms and ] relate to the degree of respiratory impairment but are not part of the diagnostic criteria. As noted above, the chest X-ray appearance for BLD can be virtually indistinguishable from silicosis. ], particularly ] (HRCT), are more sensitive than plain X-ray for detecting the small round opacities. | |||
| Continued exposure to coal dust following the development of simple CWP may result in its progression to complicated CWP, which generally requires a number of years to develop. Large, black, fibrotic scars 2-10cm in diameter are present, with accompanying decreased lung function. The lung itself appears blackened. A minority of these cases progresses to ] (PMF), the most serious form of CWP. | |||
| == |
=== Treatment === | ||
| There is no cure or discovered treatments for pneumoconiosis. The treatments that are available only relieve the symptoms but do not reverse or stop the illness. Some patients are given supplemental oxygen to help with their breathing and are advised to stop smoking to prevent further decline in lung function. In the most extreme cases, a ] could be done to help prolong the patient's life expectancy.<ref>{{Cite web|url=https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/pneumoconiosis/diagnosing-treating-pneumoconiosis.html|title=Diagnosing and Treating Pneumoconiosis|website=American Lung Association|language=en|access-date=2019-04-25}}</ref> | |||
| Both CWP and mild complicated CWP are often unsymptomatic or only affect lung function slightly. Shortness of breath and pain may be felt. However, progression to PMF is marked by lung dysfunction, ], and ]. | |||
| === Prevention of pneumoconiosis === | |||
| == See also == | |||
| The main way to avoid contracting coal worker's pneumoconiosis is to avoid the inhalation of coal dust. Some of the ways to prevent this disease include: wearing ventilated masks, such as NIOSH-certified respirators, when coming in contact with potentially dangerous airborne particles; regular pulmonary exams; and becoming educated about the risks of lung diseases in your work environment.<ref>{{Cite web|url=https://www.hopkinsmedicine.org/health/conditions-and-diseases/occupational-lung-diseases|title=Occupational Lung Diseases|website=Johns Hopkins Medicine Health Library|language=en|access-date=2019-04-25}}</ref> Pneumoconiosis can also be caused by inhaling other dusts including aluminum, antimony, barium, graphite, iron, kaolin, mica, and talc.<ref>{{Cite web |date=2023-05-23 |title=Pneumoconioses {{!}} NIOSH {{!}} CDC |url=https://www.cdc.gov/niosh/topics/pneumoconioses/default.html |access-date=2024-04-28 |website=www.cdc.gov |language=en-us}}</ref> | |||
| * ] | |||
| == Epidemiology == | |||
| ==Additional resources== | |||
| ] | |||
| * | |||
| In 2013, BLD resulted in 25,000 deaths down from 29,000 deaths in 1990.<ref name=GDB2013/> Between 1970 and 1974, prevalence of BLD among US coal miners who had worked over 25 years was 32%; the same group saw a prevalence of 9% in 2005–2006.<ref name=NIOSHResp>{{cite web |url = https://www.cdc.gov/niosh/programs/resp/risks.html |title = Respiratory Diseases: Occupational Risks |date = 21 December 2012 |access-date = 23 March 2015 |publisher = National Institute for Occupational Safety and Health}}</ref> | |||
| * video | |||
| In Australia, BLD was considered to be eliminated in the 1970s due to strict hazard control measures. However, there has been a resurgence of BLD in Australia, with the first new cases being detected in May 2015.<ref>Sim, M., Glass, D., Hoy, R., Roberts, M., Thompson, B., Cohen, R., ... & Deponte, K. (2016). Review of Respiratory Component of the Coal Mine Workers Health Scheme for Queensland Department of Natural Resources and Mines. Final Report. Melbourne, Victoria, Australia: Monash Centre for Occupational and Environmental Health, Monash University</ref> From 1999 to 2016, the average years of life lost due to BLD increased from 8.1 to 12.6 years, most likely due to the increased severity and progression of BLD.<ref>{{Cite journal|last=Mazurek|first=Jacek M.|date=2018|title=Coal Workers' Pneumoconiosis–Attributable Years of Potential Life Lost to Life Expectancy and Potential Life Lost Before Age 65 Years — United States, 1999–2016|url=https://www.cdc.gov/mmwr/volumes/67/wr/mm6730a3.htm|journal=MMWR. Morbidity and Mortality Weekly Report|language=en-us|volume=67|issue=30 |doi=10.15585/mmwr.mm6730a3|issn=0149-2195|pmc=6072058|pmid=30070982|pages=819–824}}</ref> | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * The Courier-Journal (Louisville, Ky): | |||
| == |
==History== | ||
| {{Globalize|article|USA|2name=the United States|date=August 2015}} | |||
| {{reflist|1}} | |||
| ] in 1970]] | |||
| Black lung is actually a set of conditions and until the 1950s its dangers were not well understood. Over time this disease has taken a large toll on the mining industry and the workers involved.<ref>{{Cite journal |last=Colinet |first=Jay F. |date=2020-12-01 |title=The Impact of Black Lung and a Methodology for Controlling Respirable Dust |url=https://doi.org/10.1007/s42461-020-00278-7 |journal=Mining, Metallurgy & Exploration |language=en |volume=37 |issue=6 |pages=1847–1856 |doi=10.1007/s42461-020-00278-7 |issn=2524-3470 |pmc=7885287 |pmid=33598636}}</ref> The prevailing view was that silicosis was very serious but it was solely caused by silica and not coal dust. The miners' union, the ], realized that rapid mechanization meant drills that produced much more dust, but under ] they decided not to raise the black lung issue because it might impede the mechanization that was producing higher productivity and higher wages. Union priorities were to maintain the viability of the long-fought-for welfare and retirement fund, which would be sustained by higher outputs of coal. After the death of Lewis, the union dropped its opposition to calling black lung a disease and realized the financial advantages of a fund for its disabled members. | |||
| In the ], the US Congress set up standards to reduce dust and created the Black Lung Disability Trust. The mining companies agreed to a clause, by which a ten-year history of mine work, coupled with X-ray or autopsy evidence of severe lung damage, guaranteed compensation. Equally important was a "rate retention" clause that allowed workers with progressive lung disease to transfer to jobs with lower exposure without loss of pay, seniority, or benefits. Financed by a federal tax on coal, the Trust by 2009 had distributed over $44 billion in benefits to miners disabled by the disease and their widows. A miner who has spent 25 years in underground coal mines has a 5–10% risk of contracting the disease.<ref>{{cite book |first=Alan |last=Derickson |title=Black lung: anatomy of a public health disaster |url=https://archive.org/details/blacklunganatomy0000deri |url-access=registration |date=January 1998 |publisher=]|isbn=978-0-8014-3186-9}}</ref> | |||
| <br>{{Respiratory pathology}} | |||
| ===21st century=== | |||
| ] | |||
| {{Globalize|article|USA|2name=the United States|date=September 2014}} | |||
| After the Federal Coal Mine Health and Safety Act of 1969 became law in the United States, the percentage of American miners with black lung disease decreased by about 90 percent.<ref>{{cite web|url=https://www.theguardian.com/us-news/2018/dec/13/dr-dust-the-man-who-discovered-a-hidden-black-lung-epidemic|title=Dr Dust: the man who discovered a hidden black lung epidemic|first=Elyssa|last=East|date=13 December 2018|access-date=13 December 2018|website=Theguardian.com}}</ref> More recently, however, rates of the disease have been on the rise. The ] (NIOSH) reported that close to 9 percent of miners with 25 years or more experience tested positive for black lung in 2005–2006, compared with 4 percent in the late 1990s.<ref>{{cite web | title = Black lung on the rise among US coal miners | publisher = World Socialist Web Site | date = January 11, 2010 | url = http://wsws.org/articles/2010/jan2010/blac-j11.shtml | access-date = January 11, 2010}}</ref><ref>{{cite journal |journal=Current Intelligence Bulletin |volume=64 | |||
| |title=Coal Mine Dust Exposures and Associated Health Outcomes: A Review of Information Published Since 1995 | year = 2011 | url = https://www.cdc.gov/niosh/docs/2011-172/pdfs/2011-172.pdf | access-date = August 18, 2011}}</ref> | |||
| New findings have shown that BLD can be a risk for surface coal miners, who are 48% of the workforce. Data from the Coal Workers' Health Surveillance Program of NIOSH, which examined chest X-rays from more than 2,000 miners in 16 US states from 2010 to 2011, showed that 2% of miners with greater than one year of surface mining experience developed BLD.<ref>{{cite journal |vauthors=Laney AS, Wolfe AL, Petsonk EL, Halldin CN |title=Pneumoconiosis and advanced occupational lung disease among surface coal miners – 16 states, 2010–2011 |journal=MMWR |volume=61 |issue=23 |pages=431–4 |date=June 2012 |pmid=22695382 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6123a2.htm | access-date = July 6, 2012 }}</ref> 0.5% of these miners had PMF. Most of these workers had never worked in an underground mine prior to surface mining. A high proportion of the X-rays suggested that these miners had developed silicosis. | |||
| NIOSH, with support from the ] (MSHA), operates a Mobile Health Screening Program, which travels to mining regions around the United States. Miners who participate in the Program receive health evaluations once every five years, at no cost to themselves. Chest x-rays can detect the early signs of and changes in BLD, often before the miner is aware of any lung problems.<ref>{{cite web | title = Enhanced Coal Workers' Health Surveillance Program | publisher = National Institute for Occupational Safety and Health | date = November 12, 2008 | url = https://www.cdc.gov/niosh/topics/surveillance/ORDS/ecwhsp.html | access-date = November 24, 2008}}</ref> | |||
| ] | |||
| ] | |||
| ] | |||
| A 2016–17 investigation by ] found that NIOSH had under-reported cases of PMF (a complication of black lung) by at least a factor of 20. NPR identified over 2,000 cases at certain clinics in Kentucky, Virginia, West Virginia, Pennsylvania, and Ohio, compared to 99 that NIOSH reported.<ref>{{cite web|url=https://www.npr.org/2016/12/15/505577680/advanced-black-lung-cases-surge-in-appalachia|title=Advanced Black Lung Cases Surge In Appalachia|website=Npr.org|access-date=13 December 2018}}</ref><ref>{{cite web|url=https://www.npr.org/sections/thetwo-way/2017/07/01/535082619/npr-continues-to-find-hundreds-of-cases-of-advanced-black-lung|title=NPR Continues To Find Hundreds Of Cases Of Advanced Black Lung|website=Npr.org|date=July 2017 |access-date=13 December 2018|last1=Berkes |first1=Howard }}</ref> NIOSH confirmed in 2018 the largest cluster of PMF ever scientifically documented, despite near-elimination of the disease in the 1990s. The causes of the spike are believed to include longer working shifts, mining of thinner coal seams (which causes mining machines to put more non-coal silica dust in the air), and retirements and layoffs that have prompted more former employees to visit health clinics.<ref>{{cite web|url=https://www.npr.org/2018/02/06/583456129/black-lung-study-biggest-cluster-ever-of-fatal-coal-miners-disease|title=Black Lung Study Finds Biggest Cluster Ever Of Fatal Coal Miners' Disease|website=Npr.org|access-date=13 December 2018}}</ref> | |||
| ==History and prevention efforts== | |||
| There are currently about 42,000 underground coal miners actively working in the United States. The mining and production of coal is a major part of the economy in several developed countries. In the past 10 years, over 10,000 American miners have died from CWP. Although this disease is preventable, many miners are still developing advanced and severe cases. | |||
| New U.S. MSHA rules took effect in August 2016 that lowered maximum allowed dust concentrations for surface and underground mines, and exposure by miners who have been found to be developing pneumoconiosis.<ref>{{cite web|url=https://www.msha.gov/news-media/special-initiatives/2016/09/28/respirable-dust-rule-historic-step-forward-effort-end|title=Respirable Dust Rule: A Historic Step Forward in the Effort to End Black Lung Disease - Mine Safety and Health Administration (MSHA)|website=Msha.gov|access-date=13 December 2018}}</ref> | |||
| In the 25 years since the Federal Coal Mine Health and Safety Act of 1969 became law, the proportion of miners with black lung disease has gone down by about 90%. But the downward trend of this disease in coal miners has stopped. Rates of black lung are on the rise and have almost doubled in the last 10 years. From 2000 to 2004, over 4,000 miners died from black lung disease in the United States. | |||
| ==Research== | |||
| The National Institute for Occupational Safety and Health (NIOSH), with support of the Mine Safety and Health Administration (MSHA), has started a Mobile Health Screening Program. This Mobile Unit travels to mining regions around the United States. Miners who participate in the Program receive health evaluations once every five years, at no cost to themselves. Chest x-rays can detect the early signs of and changes in CWP, often before the miner is aware of any lung problems. The screening program is only available to current miners.<ref>{{cite web | title = Enhanced Coal Workers' Health Surveillance Program | publisher = National Institute for Occupational Safety and Health | date = November 12, 2008 | url = http://www.cdc.gov/niosh/topics/surveillance/ORDS/ecwhsp.html | accessdate = November 24, 2008}}</ref> | |||
| Work to investigate the relationship between respirable dust exposure and coal worker's pneumoconiosis was carried out in the United Kingdom by the ]. This research was known as the Pneumoconiosis Field Research (PFR). The research underpinned the recommendations for more stringent airborne dust standards in British coalmines and the PFR was ultimately used as the basis for many national dust standards around the world. | |||
| In October of 2023 Summit Consulting LLC did research for the US Department of Labor about incidents of black lung disease. The point of their research was to answer some key questions that would shed some light on the prevalence and danger of black lung disease in specific subpopulations. The sub populations researched included miners, mining communities, the Navajo Nation, and Appalachia residents.<ref name=":0">{{Cite web |date=October 2023 |title=Black Lung Incidence Study |url=https://www.dol.gov/sites/dolgov/files/OASP/evaluation/pdf/Black-Lung-Incidence-Study-Final-Report-508.pdf |access-date=April 7, 2024}}</ref> The data sets that Summit used were compiled from the US Census Bureau American Community Survey, US Energy Information Administration, US Census Bureau County Business Patters, the CDC, online data for Epidemiologic Research, Coal Workers Health and Surveillance programs, and the MSHA Mines Data Set. These statistics were used to determine if the increasing number of cases can be abated, and to design predictions for future numbers of the disease. | |||
| == Pathogenesis == | |||
| Coal dust that enters the lungs can neither be destroyed nor removed by the body. The particles are engulfed by resident alveolar or interstitial ]s and remain in the lungs, residing in the connective tissue or pulmonary ]s. Aggregations of carbon-laden macrophages can be visualised under a microscope as granular, black areas. In serious cases, the lung may grossly appear black. These aggregations can cause inflammation and fibrosis, as well as the formation of nodular ]s within the lungs. The centres of dense lesions may become necrotic due to ], leading to large cavities within the lung | |||
| The report's first finding was the rate of black lung disease across the United States, with an average of 4.34 cases and 3.44 deaths per county. In certain areas of the country, these numbers go up dramatically. In Appalachia it was discovered that there were 28.79 cases and 10.88 deaths per county<ref name=":0" /> due to the larger mining populations in the Appalachia region. There were 103 counties in America that reported the disease during the entire data acquisition process which lasted from 1970 to 2014. However, 333 counties reported deaths from black lung disease during this time, indicating that where people worked and developed the disease may not match where people seek treatment or die afterwards. The research also led to the discovery that since 1990s CWP (Coal Workers Pneumoconiosis) has been increasing.<ref name=":0" /> The numbers collected may even be undercounted as the Coal Workers Health Surveillance Programs had a low output of screenings, and compensation approval rates were very slow. Despite these issues, the numbers still show an increase in cases which is concerning.<ref>{{Cite web |last=Association |first=American Lung |title=Coal Worker's Pneumoconiosis (Black Lung Disease) |url=https://www.lung.org/lung-health-diseases/lung-disease-lookup/black-lung |access-date=2024-04-28 |website=www.lung.org |language=en}}</ref> A study released in May of 2018 showed that 4,600 coal miners developed the worst kind of the disease with over half of these cases happening since 2000.<ref>{{Cite web |title=Doctors hired by employers to examine miner X-rays for black lung show 'alarming' bias: study {{!}} 2021-04-28 {{!}} Safety+Health |url=https://www.safetyandhealthmagazine.com/articles/21163-doctors-hired-by-employers-to-examine-miner-x-rays-for-black-lung-show-alarming-bias-study |access-date=2024-04-28 |website=www.safetyandhealthmagazine.com |language=en}}</ref> | |||
| == Appearance == | |||
| <!-- Image with unknown copyright status removed: ] --> | |||
| Simple CWP is marked by the presence of 1-2mm nodular aggregations of anthracotic macrophages, supported by a fine collagen network, within the lungs. Those 1-2mm in diameter are known as ''coal macules'', with larger aggregations known as ''coal nodules''. These structures occur most frequently around the initial site of coal dust accumulation - the upper regions of the lungs around ]s<ref name="robspath">{{cite book | title=Robbins Pathologic Basis of Disease| last=Cotran| coauthors=Kumar, Collins| publisher=W.B Saunders Company| location=Philadelphia| id=0-7216-7335-X}}</ref>. | |||
| The report's second finding involved a comparison of black lung disease rates in mining communities, former mining communities, and non-mining communities. The results indicate black lung disease rates are highest in current mining communities and significantly lower in former mining communities.<ref name=":0" /> Non-mining communities reported low rates of black lung disease cases or deaths. | |||
| Continued exposure to coal dust following the development of simple CWP may result in its progression to complicated CWP, which generally requires a number of years to develop. Large, black, fibrotic scars 2-10cm in diameter are present, with accompanying decreased lung function. The lung itself appears blackened. A minority of these cases progresses to ] (PMF), the most serious form of CWP. | |||
| A third finding of the study compared rates of black lung disease in the Navajo nation to the residents of Appalachia and the rest of the country. While the residents of Appalachia suffered much higher rates of the disease and deaths from the disease compared to other areas of the country, the Navajo nation didn't report major differences compared to the rest of the country with just ten deaths being reported over the course of the collection period from 1970-2020.<ref name=":0" /> This may be due to underreporting in the Navajo nation. | |||
| == Symptoms == | |||
| Both CWP and mild complicated CWP are often unsymptomatic or only affect lung function slightly. Shortness of breath and pain may be felt. However, progression to PMF is marked by lung dysfunction, ], and ]. | |||
| The last finding of the study was to determine the correlation of residential coal burning and instances of black lung disease. In comparison to the rest of the US outside Appalachia, an increase of cases and deaths was found in residential areas where coal is burned.<ref name=":0" /> Residential coal burning may be a contributing factor and not the main cause though, as these areas also have more mines and miners that could develop the disease from their occupation. | |||
| There is ongoing research and data is being collected in states all over the country.<ref>{{Cite web |title=NIOSH black lung screening program to visit 4 states {{!}} Safety+Health |url=https://www.safetyandhealthmagazine.com/articles/25283-niosh-black-lung-screening-program-to-visit-4-states |access-date=2024-04-28 |website=www.safetyandhealthmagazine.com |language=en}}</ref> | |||
| == See also == | == See also == | ||
| {{Portal|Medicine}} | |||
| * ] | |||
| * ] | * ] | ||
| ==Additional resources== | |||
| * | |||
| * video | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * The Courier-Journal (Louisville, Ky): | |||
| == References == | == References == | ||
| {{reflist| |
{{reflist|30em}} | ||
| ==External links== | |||
| <br>{{Respiratory pathology}} | |||
| * {{youTube |bTcfVNuNAL0|Faces of Black Lung - USDHHS}} | |||
| * | |||
| ] | |||
| * | |||
| * | |||
| * | |||
| {{Respiratory pathology}} | |||
| {{Occupational safety and health}} | |||
| {{authority control}} | |||
| {{DEFAULTSORT:Coal Worker's Pneumoconiosis}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 08:20, 15 August 2024
Human disease caused by long-term exposure to coal dust Medical condition| Black lung disease | |
|---|---|
| Other names | Coal workers' pneumoconiosis, anthracosis, black lung, coal mine dust lung disease |
 | |
| Lung affected by black lung disease | |
| Specialty | Pulmonology |
| Complications | Chronic obstructive pulmonary disease |
| Types |
|
| Causes | Prolonged exposure to coal dust |
| Deaths | 25,000 per year (2013) |
| Part of a series on |
| Coal |
|---|
 |
| Economic use |
| Externalities |
| Related articles |
Black lung disease (BLD), also known as coal workers' pneumoconiosis, or simply black lung, is an occupational type of pneumoconiosis caused by long-term inhalation and deposition of coal dust in the lungs and the consequent lung tissue's reaction to its presence. It is common in coal miners and others who work with coal. It is similar to both silicosis from inhaling silica dust and asbestosis from inhaling asbestos dust. Inhaled coal dust progressively builds up in the lungs and leads to inflammation, fibrosis, and in worse cases, necrosis.
Black lung disease develops after the initial, milder form of the disease known as anthracosis (from the Greek ἄνθραξ, or ánthrax – coal, carbon). This is often asymptomatic and is found to at least some extent in all urban dwellers due to air pollution. Prolonged exposure to large amounts of coal dust can result in more serious forms of the disease, simple coal workers' pneumoconiosis and complicated coal workers' pneumoconiosis (or progressive massive fibrosis, PMF). More commonly, workers exposed to coal dust develop industrial bronchitis, clinically defined as chronic bronchitis (i.e. a productive cough for three months per year for at least two years) associated with workplace dust exposure. The incidence of industrial bronchitis varies with age, job, exposure, and smoking. In non-smokers (who are less prone to develop bronchitis than smokers), studies of coal miners have shown a 16% to 17% incidence of industrial bronchitis.
In 2013, BLD resulted in 25,000 deaths globally—down from 29,000 deaths in 1990. In the US, a 2018 study by the National Institute of Occupational Safety and Health shows a resurgence among veteran coalminers, recording the highest rate of BLD in roughly two decades.
Pathogenesis
Coal dust is not as fibrogenic as silica dust. Coal dust that enters the lungs can neither be destroyed nor removed by the body. The particles are engulfed by resident alveolar macrophages or interstitial macrophages and remain in the lungs, residing in the connective tissue or pulmonary lymph nodes. Coal dust provides a sufficient stimulus for the macrophage to release various products, including enzymes, cytokines, oxygen radicals, and fibroblast growth factors, which are important in the development of inflammation and fibrosis in BLD. Aggregations of carbon-laden macrophages can be visualized under a microscope as granular, black areas. In serious cases, the lung may grossly appear black. These aggregations can cause inflammation and fibrosis, as well as the formation of nodular lesions within the lungs. The centers of dense lesions may become necrotic due to ischemia, leading to large cavities within the lung.
Appearance
Simple BLD is marked by the presence of 1–2 mm (0.039–0.079 in) nodular aggregations of anthracotic macrophages, supported by a fine collagen network, within the lungs. Those 1–2 mm in diameter are known as coal macules, with larger aggregations known as coal nodules. These structures occur most frequently around the initial site of coal dust accumulation—the upper regions of the lungs around respiratory bronchioles. The coal macule is the basic pathological feature of BLD and has a surrounding area of enlargement of the airspace, known as focal emphysema. Focal emphysema extends into progressive centrilobular emphysema. Less commonly a variant of panacinar emphysema develops.
Continued exposure to coal dust following the development of simple BLD may progress to complicated BLD with progressive massive fibrosis (PMF), wherein large masses of dense fibrosis develop, usually in the upper lung zones, measuring greater than 1 cm (0.39 in) in diameter, with accompanying decreased lung function. These cases generally require a number of years to develop. Grossly, the lung itself appears blackened. Pathologically, these consist of fibrosis with haphazardly-arranged collagen and many pigment-laden macrophages and abundant free pigment. Radiographically, BLD can appear strikingly similar to silicosis. In simple BLD, small rounded nodules predominate, tending to first appear in the upper lung zones. The nodules may coalesce and form large opacities (>1 cm), characterizing complicated BLD, or PMF.
Diagnosis
See also: ILO Classification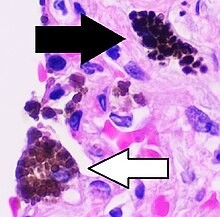
There are three basic criteria for the diagnosis of BLD:
- Chest radiography consistent with BLD
- An exposure history to coal dust (typically underground coal mining) of sufficient amount and latency
- Exclusion of alternative diagnoses (mimics of BLD)
Symptoms and pulmonary function testing relate to the degree of respiratory impairment but are not part of the diagnostic criteria. As noted above, the chest X-ray appearance for BLD can be virtually indistinguishable from silicosis. Chest CT, particularly high-resolution scanning (HRCT), are more sensitive than plain X-ray for detecting the small round opacities.
Treatment
There is no cure or discovered treatments for pneumoconiosis. The treatments that are available only relieve the symptoms but do not reverse or stop the illness. Some patients are given supplemental oxygen to help with their breathing and are advised to stop smoking to prevent further decline in lung function. In the most extreme cases, a lung transplant could be done to help prolong the patient's life expectancy.
Prevention of pneumoconiosis
The main way to avoid contracting coal worker's pneumoconiosis is to avoid the inhalation of coal dust. Some of the ways to prevent this disease include: wearing ventilated masks, such as NIOSH-certified respirators, when coming in contact with potentially dangerous airborne particles; regular pulmonary exams; and becoming educated about the risks of lung diseases in your work environment. Pneumoconiosis can also be caused by inhaling other dusts including aluminum, antimony, barium, graphite, iron, kaolin, mica, and talc.
Epidemiology
In 2013, BLD resulted in 25,000 deaths down from 29,000 deaths in 1990. Between 1970 and 1974, prevalence of BLD among US coal miners who had worked over 25 years was 32%; the same group saw a prevalence of 9% in 2005–2006. In Australia, BLD was considered to be eliminated in the 1970s due to strict hazard control measures. However, there has been a resurgence of BLD in Australia, with the first new cases being detected in May 2015. From 1999 to 2016, the average years of life lost due to BLD increased from 8.1 to 12.6 years, most likely due to the increased severity and progression of BLD.
History
| The examples and perspective in this article deal primarily with the United States and do not represent a worldwide view of the subject. You may improve this article, discuss the issue on the talk page, or create a new article, as appropriate. (August 2015) (Learn how and when to remove this message) |

Black lung is actually a set of conditions and until the 1950s its dangers were not well understood. Over time this disease has taken a large toll on the mining industry and the workers involved. The prevailing view was that silicosis was very serious but it was solely caused by silica and not coal dust. The miners' union, the United Mine Workers of America, realized that rapid mechanization meant drills that produced much more dust, but under John L. Lewis they decided not to raise the black lung issue because it might impede the mechanization that was producing higher productivity and higher wages. Union priorities were to maintain the viability of the long-fought-for welfare and retirement fund, which would be sustained by higher outputs of coal. After the death of Lewis, the union dropped its opposition to calling black lung a disease and realized the financial advantages of a fund for its disabled members.
In the Federal Coal Mine Health and Safety Act of 1969, the US Congress set up standards to reduce dust and created the Black Lung Disability Trust. The mining companies agreed to a clause, by which a ten-year history of mine work, coupled with X-ray or autopsy evidence of severe lung damage, guaranteed compensation. Equally important was a "rate retention" clause that allowed workers with progressive lung disease to transfer to jobs with lower exposure without loss of pay, seniority, or benefits. Financed by a federal tax on coal, the Trust by 2009 had distributed over $44 billion in benefits to miners disabled by the disease and their widows. A miner who has spent 25 years in underground coal mines has a 5–10% risk of contracting the disease.
21st century
| The examples and perspective in this article deal primarily with the United States and do not represent a worldwide view of the subject. You may improve this article, discuss the issue on the talk page, or create a new article, as appropriate. (September 2014) (Learn how and when to remove this message) |
After the Federal Coal Mine Health and Safety Act of 1969 became law in the United States, the percentage of American miners with black lung disease decreased by about 90 percent. More recently, however, rates of the disease have been on the rise. The National Institute for Occupational Safety and Health (NIOSH) reported that close to 9 percent of miners with 25 years or more experience tested positive for black lung in 2005–2006, compared with 4 percent in the late 1990s.
New findings have shown that BLD can be a risk for surface coal miners, who are 48% of the workforce. Data from the Coal Workers' Health Surveillance Program of NIOSH, which examined chest X-rays from more than 2,000 miners in 16 US states from 2010 to 2011, showed that 2% of miners with greater than one year of surface mining experience developed BLD. 0.5% of these miners had PMF. Most of these workers had never worked in an underground mine prior to surface mining. A high proportion of the X-rays suggested that these miners had developed silicosis.
NIOSH, with support from the Mine Safety and Health Administration (MSHA), operates a Mobile Health Screening Program, which travels to mining regions around the United States. Miners who participate in the Program receive health evaluations once every five years, at no cost to themselves. Chest x-rays can detect the early signs of and changes in BLD, often before the miner is aware of any lung problems.
A 2016–17 investigation by National Public Radio found that NIOSH had under-reported cases of PMF (a complication of black lung) by at least a factor of 20. NPR identified over 2,000 cases at certain clinics in Kentucky, Virginia, West Virginia, Pennsylvania, and Ohio, compared to 99 that NIOSH reported. NIOSH confirmed in 2018 the largest cluster of PMF ever scientifically documented, despite near-elimination of the disease in the 1990s. The causes of the spike are believed to include longer working shifts, mining of thinner coal seams (which causes mining machines to put more non-coal silica dust in the air), and retirements and layoffs that have prompted more former employees to visit health clinics.
New U.S. MSHA rules took effect in August 2016 that lowered maximum allowed dust concentrations for surface and underground mines, and exposure by miners who have been found to be developing pneumoconiosis.
Research
Work to investigate the relationship between respirable dust exposure and coal worker's pneumoconiosis was carried out in the United Kingdom by the Institute of Occupational Medicine. This research was known as the Pneumoconiosis Field Research (PFR). The research underpinned the recommendations for more stringent airborne dust standards in British coalmines and the PFR was ultimately used as the basis for many national dust standards around the world.
In October of 2023 Summit Consulting LLC did research for the US Department of Labor about incidents of black lung disease. The point of their research was to answer some key questions that would shed some light on the prevalence and danger of black lung disease in specific subpopulations. The sub populations researched included miners, mining communities, the Navajo Nation, and Appalachia residents. The data sets that Summit used were compiled from the US Census Bureau American Community Survey, US Energy Information Administration, US Census Bureau County Business Patters, the CDC, online data for Epidemiologic Research, Coal Workers Health and Surveillance programs, and the MSHA Mines Data Set. These statistics were used to determine if the increasing number of cases can be abated, and to design predictions for future numbers of the disease.
The report's first finding was the rate of black lung disease across the United States, with an average of 4.34 cases and 3.44 deaths per county. In certain areas of the country, these numbers go up dramatically. In Appalachia it was discovered that there were 28.79 cases and 10.88 deaths per county due to the larger mining populations in the Appalachia region. There were 103 counties in America that reported the disease during the entire data acquisition process which lasted from 1970 to 2014. However, 333 counties reported deaths from black lung disease during this time, indicating that where people worked and developed the disease may not match where people seek treatment or die afterwards. The research also led to the discovery that since 1990s CWP (Coal Workers Pneumoconiosis) has been increasing. The numbers collected may even be undercounted as the Coal Workers Health Surveillance Programs had a low output of screenings, and compensation approval rates were very slow. Despite these issues, the numbers still show an increase in cases which is concerning. A study released in May of 2018 showed that 4,600 coal miners developed the worst kind of the disease with over half of these cases happening since 2000.
The report's second finding involved a comparison of black lung disease rates in mining communities, former mining communities, and non-mining communities. The results indicate black lung disease rates are highest in current mining communities and significantly lower in former mining communities. Non-mining communities reported low rates of black lung disease cases or deaths.
A third finding of the study compared rates of black lung disease in the Navajo nation to the residents of Appalachia and the rest of the country. While the residents of Appalachia suffered much higher rates of the disease and deaths from the disease compared to other areas of the country, the Navajo nation didn't report major differences compared to the rest of the country with just ten deaths being reported over the course of the collection period from 1970-2020. This may be due to underreporting in the Navajo nation.
The last finding of the study was to determine the correlation of residential coal burning and instances of black lung disease. In comparison to the rest of the US outside Appalachia, an increase of cases and deaths was found in residential areas where coal is burned. Residential coal burning may be a contributing factor and not the main cause though, as these areas also have more mines and miners that could develop the disease from their occupation.
There is ongoing research and data is being collected in states all over the country.
See also
References
- "Coal Workers' Pneumoconiosis, Simple CWP | NIOSH | CDC". www.cdc.gov. 2023-05-05. Retrieved 2024-06-18.
- "Pneumoconiosis". www.hopkinsmedicine.org. 2019-11-19. Retrieved 2024-04-28.
- "Pneumoconiosis Symptoms, Causes and Risk Factors". American Lung Association. Retrieved 2019-04-25.
- ^ Cotran; Kumar, Collins (1999). Robbins Pathologic Basis of Disease. Philadelphia: W.B Saunders Company. ISBN 978-0-7216-7335-6.
- "Coal worker's pneumoconiosis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-04-25.
- Says, Stephen Smyth (2023-02-27). "Modern Coal Miners Have Higher Death Rates From Lung Diseases Than Their Predecessors | Blogs | CDC". Retrieved 2023-05-28.
- Morgan WK (November 1978). "Industrial bronchitis". Br J Ind Med. 35 (4): 285–91. doi:10.1136/oem.35.4.285. PMC 1008445. PMID 367424.
- Seixas NS, Robins TG, Attfield MD, Moulton LH (1992). "Exposure-response relationships for coal mine dust and obstructive lung disease following enactment of the Federal Coal Mine Health and Safety Act of 1969". Am. J. Ind. Med. 21 (5): 715–34. doi:10.1002/ajim.4700210511. PMID 1609817.
- Marine WM, Gurr D, Jacobsen M (January 1988). "Clinically important respiratory effects of dust exposure and smoking in British coal miners". Am. Rev. Respir. Dis. 137 (1): 106–12. doi:10.1164/ajrccm/137.1.106. PMID 3337449.
- ^ "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. 17 December 2014. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- Richard Valdmanis (19 July 2018). "A tenth of U.S. veteran coal miners have black lung disease:NIOSH". Reuters.
- Castranova V, Vallyathan V (August 2000). "Silicosis and coal workers' pneumoconiosis". Environ. Health Perspect. 108 (Suppl 4): 675–84. doi:10.1289/ehp.00108s4675. PMC 1637684. PMID 10931786.
- Vanhée D, Gosset P, Boitelle A, Wallaert B, Tonnel AB (May 1995). "Cytokines and cytokine network in silicosis and coal workers' pneumoconiosis". Eur. Respir. J. 8 (5): 834–42. doi:10.1183/09031936.95.08050834. PMID 7656959. S2CID 33011018.
- "Pathology standards for coal workers' pneumoconiosis. Report of the Pneumoconiosis Committee of the College of American Pathologists to the National Institute for Occupational Safety and Health". Arch. Pathol. Lab. Med. 103 (8): 375–432. July 1979. PMID 378179.
- Weinberger, S; Cockrill, B; Mandel, J (2019). Principles of pulmonary medicine (Seventh ed.). Elsevier. p. 147. ISBN 9780323523714.
- "Pathology Basis of Occupational Lung Disease, Pneumoconiosis | NIOSH | CDC". www.cdc.gov. 5 August 2020. Retrieved 29 July 2021.
- "Diagnosing and Treating Pneumoconiosis". American Lung Association. Retrieved 2019-04-25.
- "Occupational Lung Diseases". Johns Hopkins Medicine Health Library. Retrieved 2019-04-25.
- "Pneumoconioses | NIOSH | CDC". www.cdc.gov. 2023-05-23. Retrieved 2024-04-28.
- "Respiratory Diseases: Occupational Risks". National Institute for Occupational Safety and Health. 21 December 2012. Retrieved 23 March 2015.
- Sim, M., Glass, D., Hoy, R., Roberts, M., Thompson, B., Cohen, R., ... & Deponte, K. (2016). Review of Respiratory Component of the Coal Mine Workers Health Scheme for Queensland Department of Natural Resources and Mines. Final Report. Melbourne, Victoria, Australia: Monash Centre for Occupational and Environmental Health, Monash University
- Mazurek, Jacek M. (2018). "Coal Workers' Pneumoconiosis–Attributable Years of Potential Life Lost to Life Expectancy and Potential Life Lost Before Age 65 Years — United States, 1999–2016". MMWR. Morbidity and Mortality Weekly Report. 67 (30): 819–824. doi:10.15585/mmwr.mm6730a3. ISSN 0149-2195. PMC 6072058. PMID 30070982.
- Colinet, Jay F. (2020-12-01). "The Impact of Black Lung and a Methodology for Controlling Respirable Dust". Mining, Metallurgy & Exploration. 37 (6): 1847–1856. doi:10.1007/s42461-020-00278-7. ISSN 2524-3470. PMC 7885287. PMID 33598636.
- Derickson, Alan (January 1998). Black lung: anatomy of a public health disaster. Cornell University Press. ISBN 978-0-8014-3186-9.
- East, Elyssa (13 December 2018). "Dr Dust: the man who discovered a hidden black lung epidemic". Theguardian.com. Retrieved 13 December 2018.
- "Black lung on the rise among US coal miners". World Socialist Web Site. January 11, 2010. Retrieved January 11, 2010.
- "Coal Mine Dust Exposures and Associated Health Outcomes: A Review of Information Published Since 1995" (PDF). Current Intelligence Bulletin. 64. 2011. Retrieved August 18, 2011.
- Laney AS, Wolfe AL, Petsonk EL, Halldin CN (June 2012). "Pneumoconiosis and advanced occupational lung disease among surface coal miners – 16 states, 2010–2011". MMWR. 61 (23): 431–4. PMID 22695382. Retrieved July 6, 2012.
- "Enhanced Coal Workers' Health Surveillance Program". National Institute for Occupational Safety and Health. November 12, 2008. Retrieved November 24, 2008.
- "Advanced Black Lung Cases Surge In Appalachia". Npr.org. Retrieved 13 December 2018.
- Berkes, Howard (July 2017). "NPR Continues To Find Hundreds Of Cases Of Advanced Black Lung". Npr.org. Retrieved 13 December 2018.
- "Black Lung Study Finds Biggest Cluster Ever Of Fatal Coal Miners' Disease". Npr.org. Retrieved 13 December 2018.
- "Respirable Dust Rule: A Historic Step Forward in the Effort to End Black Lung Disease - Mine Safety and Health Administration (MSHA)". Msha.gov. Retrieved 13 December 2018.
- ^ "Black Lung Incidence Study" (PDF). October 2023. Retrieved April 7, 2024.
- Association, American Lung. "Coal Worker's Pneumoconiosis (Black Lung Disease)". www.lung.org. Retrieved 2024-04-28.
- "Doctors hired by employers to examine miner X-rays for black lung show 'alarming' bias: study | 2021-04-28 | Safety+Health". www.safetyandhealthmagazine.com. Retrieved 2024-04-28.
- "NIOSH black lung screening program to visit 4 states | Safety+Health". www.safetyandhealthmagazine.com. Retrieved 2024-04-28.
External links
- Faces of Black Lung - USDHHS on YouTube
- NIOSH Coal Workers' Health Surveillance Program
- Mine Safety and Health Administration
- 42CFR27 Specifications of Medical Examinations of Underground Coal Miners
- Institute of Occupational Medicine's pneumoconiosis research
| Diseases of the respiratory system | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Upper RT (including URTIs, common cold) |
| ||||||||||||||||||||||
| Lower RT/ lung disease (including LRTIs) |
| ||||||||||||||||||||||
| Pleural cavity/ mediastinum |
| ||||||||||||||||||||||
| Other/general | |||||||||||||||||||||||