| Revision as of 20:38, 3 February 2009 editRichard Arthur Norton (1958- ) (talk | contribs)Extended confirmed users195,161 edits The presence of an intact hymen has historically been used to determination of a woman's virginity.← Previous edit | Latest revision as of 07:40, 20 November 2024 edit undoKNHaw (talk | contribs)Extended confirmed users, Rollbackers28,569 editsm Reverted 1 edit by 68.14.184.54 (talk) to last revision by EquivampTags: Twinkle Undo | ||
| Line 1: | Line 1: | ||
| {{short description|Membrane that surrounds or partially covers the vaginal opening}} | |||
| {{otheruses4|the vaginal mucous membrane fold|the god and other uses}} | |||
| {{about|the vaginal membrane|4=other uses}} | |||
| {{Cleanup|date=January 2009}} | |||
| {{Use mdy dates|date=November 2016}} | |||
| {{Infobox |
{{Infobox anatomy | ||
| | Name = Hymen | |||
| | Latin = hymen | |||
| | Greek = ὑμήν | |||
| GraySubject = 270 | | |||
| |
| Width = | ||
| | Image = Hymen en.svg | |||
| | Caption = Various hymen defects (the shaded areas represent the vaginal opening) | |||
| | Image2 = Haultain_and_Ferguson_-_external_female_genital_organs.svg | |||
| Image2 = | | |||
| | Caption2 = External genitals of a human female | |||
| | Precursor= | |||
| System = | | |||
| |
| System = | ||
| MeshNumber = | | |||
| }} | }} | ||
| The '''hymen''' is a thin piece of ] that surrounds or partially covers the ]. A small percentage are born with hymens that are ] and completely obstruct the vaginal canal. It forms part of the ] and is similar in structure to the vagina.<ref name=emans /><ref name="Perlman">{{Cite book|last1=Perlman|first1=Sally E.|last2=Nakajyma | first2=Steven T.| last3=Hertweck| first3=S. Paige |title=Clinical protocols in pediatric and adolescent gynecology|year=2004|publisher=Parthenon |page=131 |isbn=978-1-84214-199-1 }}</ref> The term comes straight from the Greek, for 'membrane'. | |||
| The '''hymen''' is a fold of ] which surrounds or partially covers the external ]l opening. It forms part of the ], or external genitalia.<ref name=emans>Emans, S. Jean. "Physical Examination of the Child and Adolescent" (2000) in ''Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas'', Second edition, Oxford University Press. pages 62-64</ref><ref name="autogenerated1">{{cite book |last=Perlman |first=Sally E. |coauthors=Nakajima, Steven T. and Hertweck, S. Paige |title=Clinical protocols in pediatric and adolescent gynecology |year=2004|publisher=Parthenon |pages=131 }}</ref> Slang terms are maidenhead and "cherry", as in "popping one's cherry" (losing one's ]). The presence of an intact hymen has historically been used to determination of a woman's virginity. However, it is not always possible to confirm that a ] or post-] girl is a virgin by examining her hymen.<ref name=discovery/><ref name="autogenerated1" /> In cases of suspected ] or ], a detailed examination of the hymen may be carried out; but the condition of the hymen alone is often inconclusive or open to misinterpretation, especially if the patient has reached puberty.<ref name=emans/> In children, although a common appearance of the hymen is ]-shaped, many variations are possible.<ref name=emans/> After a woman ] she may be left with remnants of the hymen called ''carunculae myrtiformes'' or the hymen may be completely absent.<ref>{{cite book |last=Knight |first=Bernard |title=Simpson's Forensic Medicine |edition=11th edition |year=1997 |publisher=Arnold |location=London |pages=114 }}</ref> Although some women are born without a hymen, most have one. <ref name=discovery>{{cite web |url=http://health.discovery.com/centers/sex/sexpedia/hymen.html |title=Hymen |accessdate=2009-02-02 |quote=Knowing the facts about the hymen can help women dispel the myth that it proves virginity, freeing them from the negative effects of popular mythology. Having accurate information about the hymen can assist in normalizing a woman's fears about her body and help promote greater self-acceptance. |publisher=] }}</ref> | |||
| In children, a common appearance of the hymen is ]-shaped, although many shapes are possible. Each shape in the ] has a Latinate name. During ], ] causes the hymen to change in appearance and become very elastic.<ref name=":1" /><ref name=":2" /> Normal variations of the post-pubertal hymen range from thin and stretchy to thick and somewhat rigid.<ref name="emans" /> Very rarely, it may be completely absent.<ref>{{Cite journal |date=3 June 2019 |title=The little tissue that couldn't – dispelling myths about the Hymen's role in determining sexual history and assault - Fact 1A |pmc=6547601 |language=en|last1=Mishori |first1=R. |last2=Ferdowsian |first2=H. |last3=Naimer |first3=K. |last4=Volpellier |first4=M. |last5=McHale |first5=T. |journal=Reproductive Health |volume=16 |issue=1 |page=74 |doi=10.1186/s12978-019-0731-8 |pmid=31159818 |doi-access=free }}</ref> | |||
| == Hymenal Development == | |||
| The hymen can rip or tear during first ], which usually results in pain and, sometimes, mild temporary bleeding or spotting. Minor injuries to the hymen may heal on their own, and not require surgical intervention.<ref>{{Cite journal |last1=Hegazy |first1=Abdelmonem |last2=Al-Rukban |first2=Mohammed |date=2012-01-01 |title=Hymen: Facts and conceptions |url=https://www.researchgate.net/publication/260578888 |journal=The Health |language=en |volume=3 |issue=4 |issn=2219-8083 |quote=Possible explanations for the lack of genital trauma include... acute injuries occur but heal completely.}}</ref> Historically, it was believed that first penetration was necessarily traumatic, but now sources differ on how common tearing or bleeding are as a result of first intercourse.<ref name="ucsb sexinfo">{{cite web |url=https://sexinfoonline.com/the-hymen/ |title=The Hymen |publisher=] |access-date=2020-09-19 |quote=While some females bleed the first time they have penetrative intercourse, not every female does. This depends on many factors, such as how much hymenal tissue a female has, whether her hymen has already been stretched or torn, or how thick and elastic it is.}}</ref><ref name=":3">{{Cite journal |last1=Rogers |first1=Deborah J|last2=Stark |first2=Margaret |date=1998-08-08 |title=The hymen is not necessarily torn after sexual intercourse |journal=BMJ: British Medical Journal |volume=317 |issue=7155 |page=414 |issn=0959-8138 |pmc=1113684 |pmid=9694770 |doi=10.1136/bmj.317.7155.414}}</ref><ref name=":4">{{Cite journal |last=Emma Curtis, Camille San Lazaro |date=1999-02-27 |title=Appearance of the hymen in adolescents is not well documented |journal=BMJ: British Medical Journal |language=en |volume=318 |issue=7183 |page=605 |quote=We agree with Rogers and Stark that so called rupture and bleeding of the hymen is not to be routinely expected after first sexual intercourse. |pmc=1115047 |pmid=10037658 |doi=10.1136/bmj.318.7183.605}}</ref> Therefore, the state of the hymen is not a reliable indicator of ],<ref name="Perlman"/><ref name="Knight"/> though "]ing" remains a common practice in some cultures, sometimes accompanied by ] to give the appearance of virginity. | |||
| The genital tract develops during embryogenesis, from 3 weeks' gestation to the second trimester, and the hymen is formed following the vagina. | |||
| ==Development and histology== | |||
| At week seven, the urorectal septum forms and separates the rectum from the urogenital sinus. | |||
| The ] during ], from the third week of ] to the ], and the hymen is formed following the ]. At week seven, the ] forms and separates the ] from the ]. At week nine, the ]s move downwards to reach the urogenital sinus, forming the uterovaginal canal and inserting into the urogenital sinus. At week twelve, the Müllerian ducts fuse to create a primitive uterovaginal canal called unaleria. At month five, the vaginal canalization is complete and the fetal hymen is formed from the proliferation of the sinovaginal bulbs (where Müllerian ducts meet the urogenital sinus), and normally becomes perforate before or shortly after birth.<ref name="healey">{{cite book |last=Healey |first=Andrew |editor-last1=Mann |editor-first1=Gurdeep S. |editor-last2=Blair |editor-first2=Joanne C. |editor-last3=Garden |editor-first3=Anne S. |title=Imaging of Gynecological Disorders in Infants and Children |publisher=Springer |date=2012 |pages=21–30 |chapter=Embryology of the female reproductive tract |isbn=978-3-540-85602-3 |doi=10.1007/978-3-540-85602-3|series=Medical Radiology }}</ref> | |||
| The hymen has dense innervation. In newborn babies, still under the influence of the mother's ], the hymen is thick, pale pink, and redundant (folds in on itself and may protrude). For the first two to four years of life, the infant produces hormones that continue this effect.<ref name="McCann">McCann, J; Rosas, A. and Boos, S. (2003) "Child and adolescent sexual assaults (childhood sexual abuse)" in Payne-James, Jason; Busuttil, Anthony and Smock, William (eds). Forensic Medicine: Clinical and Pathological Aspects, Greenwich Medical Media: London, a)p.453, b)p.455 c)p.460. {{isbn|978-1-84-110026-5}}</ref> Their hymenal opening tends to be annular (circumferential).<ref name=heger>{{Cite book | last1=Heger | first1=Astrid | author-link = Astrid Heppenstall Heger | last2=Emans | first2=S. Jean | last3=Muram | first3=David |title=Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas |edition=Second |year=2000 |publisher=Oxford University Press |page=116 |isbn=978-0-19-507425-3 }}</ref> | |||
| At week nine, the müllerian ducts move downwards to reach the urogenital sinus, forming the uterovaginal canal and inserting into the urogenital sinus. | |||
| Post ] stage, the diameter of the hymenal opening (measured within the '''hymenal ring''') widens by approximately 1 mm for each year of age.<ref>{{Cite CiteSeerX |last=Pugno |first=Perry |title=Genital Findings in Prepubertal Girls Evaluated for Sexual Abuse |date=1999|citeseerx=10.1.1.522.1894 }}</ref> During ], ] causes the hymen to become very elastic and ]d.<ref name=":1">{{Cite journal|last1=Lahoti|first1=Sheela L.|last2=McClain|first2=Natalie|last3=Girardet|first3=Rebecca|last4=McNeese|first4=Margaret|last5=Cheung|first5=Kim|date=2001-03-01|title=Evaluating the Child for Sexual Abuse|url=http://www.aafp.org/afp/2001/0301/p883.html|journal=American Family Physician|language=en|volume=63|issue=5|pages=883–92|pmid=11261865|issn=0002-838X}}</ref><ref name=":2">{{Cite book|url=https://the-eye.eu/public/Books/Medical/texts/Evaluation%20of%20the%20Sexually%20Abused%20Child%202nd%20ed%20-%20A.%20Heger%2C%20et%20al.%2C%20%28Oxford%2C%202000%29%20WW.pdf|title=Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas|date=2000|publisher=Oxford University Press|isbn=978-0-19-507425-3|editor-last=Heger|editor-first=Astrid H.|edition=2nd|location=New York|page=122|language=en|editor-last2=Emans|editor-first2=S. Jean|access-date=July 8, 2018|archive-date=July 8, 2018|archive-url=https://web.archive.org/web/20180708104703/https://the-eye.eu/public/Books/Medical/texts/Evaluation%20of%20the%20Sexually%20Abused%20Child%202nd%20ed%20-%20A.%20Heger,%20et%20al.,%20(Oxford,%202000)%20WW.pdf}}</ref><gallery> | |||
| At week 12, the müllerian ducts fuse to create a primitive uterovaginal canal. | |||
| File:Carunculae myrtiformes.png|Arrows point to carunculae myrtiformes ("remnants") of the hymen in a post-pubertal individual. | |||
| </gallery>The hymen can stretch or tear as a result of various behaviors, by the use of ]s<ref name="ucsb sexinfo"/> or ]s, ]s with a ], or sexual intercourse.<ref name="emans" /> Remnants of the hymen are called carunculae myrtiformes.<ref name="Knight">{{cite book|last=Knight|first=Bernard|title=Simpson's Forensic Medicine|edition=11th|year=1997|publisher=Arnold|location=London|page=114|isbn=978-0-7131-4452-9}}</ref> | |||
| A glass or plastic rod of 6 mm diameter having a globe on one end with varying diameter from 10 to 25 mm, called a Glaister Keen rod, is used for close examination of the hymen or the degree of its rupture. In ], it is recommended by health authorities that a physician who must swab near this area of a ] girl avoid the hymen and swab the outer ] instead.<ref name=McCann/> In cases of suspected ] or ], a detailed examination of the hymen may be performed, but the condition of the hymen alone is often inconclusive.<ref name="Perlman"/> | |||
| At month 5, the vaginal canalization is complete and the fetal hymen is formed from the proliferation of the sinovaginal bulbs (where müllerian ducts meet the urogenital sinus), and becomes perforate before or shortly after birth.<ref name="WebMD">{{cite web |url=http://emedicine.medscape.com/article/269050-overview |title=Imperforate Hymen |accessdate=2009-02-02 |quote=Different normal variants in hymenal configuration are described, varying from the common annular, to crescentic, to navicular ("boatlike" with an anteriorly displaced hymenal orifice). Hymenal variations are rarely clinically significant before menarche. In the case of a navicular configuration, urinary complaints (eg, dribbling, retention, urinary tract infections) may result. Sometimes, a cribriform (fenestrated), septate, or navicular configuration to the hymen can be associated with retention of vaginal secretions and prolongation of the common condition of a mixed bacterial vulvovaginitis. |publisher=] }}</ref> | |||
| ==Anatomic variations== | |||
| In newborn babies, still under the influence of the mother's ], the hymen is thick, pale pink, and redundant (folds in on itself and may protrude). For the first two to four years of life, the infant produces hormones which continue this effect.<ref name="McCann">McCann, J; Rosas, A. and Boos, S. (2003) "Child and adolescent sexual assaults (childhood sexual abuse)" in Payne-James, Jason; Busuttil, Anthony and Smock, William (eds). Forensic Medicine: Clinical and Pathological Aspects, Greenwich Medical Media: London, a)p.453, b)p.455 c)p.460.</ref>. Their hymenal opening tends to be annular (circumferential).<ref name=emans/> | |||
| Normal variations of the hymen range from thin and stretchy to thick and somewhat rigid.<ref name=emans>{{Cite book|url=https://the-eye.eu/public/Books/Medical/texts/Evaluation%20of%20the%20Sexually%20Abused%20Child%202nd%20ed%20-%20A.%20Heger%2C%20et%20al.%2C%20%28Oxford%2C%202000%29%20WW.pdf|title=Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas|date=2000|publisher=Oxford University Press|isbn=978-0-19-507425-3|editor-last=Heger|editor-first=Astrid H.|edition=2nd|location=New York|pages=61–65|language=en|editor-last2=Emans|editor-first2=S. Jean|access-date=July 8, 2018|archive-date=July 8, 2018|archive-url=https://web.archive.org/web/20180708104703/https://the-eye.eu/public/Books/Medical/texts/Evaluation%20of%20the%20Sexually%20Abused%20Child%202nd%20ed%20-%20A.%20Heger,%20et%20al.,%20(Oxford,%202000)%20WW.pdf}}</ref><ref name="McCann"/> An ] occurs in 1-2 out of 1,000 infants.<ref>{{Cite book|url=https://books.google.com/books?id=H7Z-lD9cXBEC&q=vaginal+labial+fusion&pg=PA139|title=Blueprints Obstetrics and Gynecology|last1=Callahan|first1=Tamara L.|last2=Caughey|first2=Aaron B.|date=2009|publisher=Lippincott Williams & Wilkins|isbn=978-0-7817-8249-4|language=en}}</ref><ref>{{Cite journal|last1=Lardenoije|first1=Céline|last2=Aardenburg|first2=Robert|last3=Mertens|first3=Helen|date=2009-05-26|title=Imperforate hymen: a cause of abdominal pain in female adolescents|journal=BMJ Case Reports|volume=2009|pages=bcr0820080722|doi=10.1136/bcr.08.2008.0722|issn=1757-790X|pmc=3029536|pmid=21686660}}</ref> The only variation that may require medical intervention is the imperforate hymen, which either completely prevents the passage of menstrual fluid or slows it significantly. In either case, surgical intervention may be needed to allow menstrual fluid to pass or intercourse to take place at all.<ref>{{Cite web|title=Imperforate hymen |year=2021 |publisher=] |website=medlineplus.gov |url=https://medlineplus.gov/ency/patientinstructions/000708.htm}}</ref> | |||
| == Hymenal resorption == | |||
| Prepubescent hymenal openings come in many shapes, depending on hormonal and activity level, the most common being crescentic (posterior rim): no tissue at the 12 ]; crescent-shaped band of tissue from 1–2 to 10–11 o'clock, at its widest around 6 o'clock. From puberty onwards, depending on ] and activity levels, the hymenal tissue may be thicker, and the opening is often fimbriated or erratically shaped.<ref name=heger/> In younger children, a torn hymen will typically heal very quickly. In adolescents, the hymenal opening can naturally extend and variation in shape and appearance increases.<ref name=emans/> | |||
| Past neonatal stage, the diameter of the hymenal opening (measured within the hymenal ring) has historically been proposed to be approximately 1 mm for each year of age. <ref name="WebMD" /> In children, to make this measurement, a doctor may place a Foley catheter into the vagina and inflate the balloon behind the hymen to stretch the hymenal margin and allow for a better examination. In the normal course of life the hymenal opening can also be enlarged by ] use, pelvic examinations, regular physical activity or sexual intercourse.<ref name=emans/> Once a girl reaches puberty the hymen tends to become so elastic that it's not possible to determine whether a woman uses tampons or not by examining a hymen. In one survey only 43% of women reported bleeding the first time they had sex; indicating that the vagina of a majority of women is sufficiently opened.<ref name=emans/><ref name="McCann" /> | |||
| Variations of the female reproductive tract can result from ] or hypoplasia, canalization defects, lateral fusion and failure of resorption, resulting in various complications.<ref>{{Cite web|title=Congenital Anomalies of the Hymen |publisher=] |website=brighamandwomens.org |url=https://www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/congenital-anomalies/hymen-anomalies}}</ref> | |||
| The hymen is most apparent in young girls: at this time their hymen is thin and less likely to be ''redundant'', that is to protrude or fold over on itself.<ref>Muram, David. "Anatomical and Physiologic Changes" (2000) in ''Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas'', Second edition, ] Press. 105-7.</ref> In instances of suspected child abuse, doctors use the ] system to describe the hymenal opening. The 12 o'clock position is below the ], and 6 o'clock is towards the ], with the patient lying on her back.<ref name=pokorny>Pokorny, Susan. "Anatomical Terms of Female External Genitalia" (2000) in ''Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas'', Second edition, Oxford University Press. 110.</ref> | |||
| * ]: hymenal opening nonexistent; will require minor surgery if it has not corrected itself by puberty to allow menstrual fluids to escape.<ref>{{Cite web|title= Imperforate Hymen|publisher=] |website=mountsinai.org |url=https://www.mountsinai.org/health-library/special-topic/imperforate-hymen}}</ref> | |||
| * Cribriform, or microperforate: sometimes confused for imperforate, the hymenal opening appears to be nonexistent, but has, under close examination, small perforations.<ref>{{Cite web|title= Cribriform Hymen|publisher=] |website=texaschildrens.org |url=https://www.texaschildrens.org/health/cribriform-hymen}}</ref> | |||
| * Septate: the hymenal opening has one or more bands of tissue extending across the opening.<ref>{{Cite web|title=Septate Hymen |publisher=] |website=childrenshospital.org |url=https://www.childrenshospital.org/conditions-and-treatments/conditions/s/septate-hymen}}</ref> | |||
| == Trauma == | |||
| Infants' hymenal opening tends be redundant (sleeve-like, folding in on itself), and may be combined with annular shaped.<ref name=pokorny/> | |||
| ] | |||
| Historically, it was believed that first sexual intercourse was necessarily traumatic to the hymen and always resulted in the hymen being "broken" or torn, causing bleeding. However, research on women in Western populations has found that bleeding during first intercourse does not invariably occur.<ref name=":3" /><ref name=":4" /><ref name=":5">{{Cite news|url=https://www.tijdschriftvoorseksuologie.nl/media/k2/attachments/loeberZtvsZ32-3.pdf|title=Over het zwaard en de schede; bloedverlies en pijn bij de eerste coïtus Een onderzoek bij vrouwen uit diverse culturen|last=Loeber|first=Olga|date=2008|work=Tijdschrift voor Seksuologie|access-date=2018-09-07|volume=32|pages=129–137|language=nl-nl|archive-date=November 5, 2019|archive-url=https://web.archive.org/web/20191105174514/https://www.tijdschriftvoorseksuologie.nl/media/k2/attachments/loeberZtvsZ32-3.pdf|url-status=dead}}</ref> In one cross-cultural study, slightly more than half of all women self-reported bleeding during first intercourse, with significantly different levels of pain and bleeding reported depending on their region of origin.<ref>{{Cite journal|last=Amy|first=Jean-Jacques|date=January 2008|title=Certificates of virginity and reconstruction of the hymen|journal=The European Journal of Contraception & Reproductive Health Care|language=en|volume=13|issue=2|pages=111–113|doi=10.1080/13625180802106045|pmid=18465471|s2cid=37484764|issn=1362-5187}}</ref><ref name=":5" /> Not all women experience pain, and one study found a correlation between the experience of strong emotions – such as excitement, nervousness, or fear – with experiencing pain during first intercourse.<ref name="Pain">{{Cite journal |doi = 10.1007/BF01542003|title = The experience of pain during women's first sexual intercourse: Cultural mythology about female sexual initiation|year = 1985|last1 = Weis|first1 = David L.|journal = Archives of Sexual Behavior|volume = 14|issue = 5|pages = 421–438|pmid = 4062539|s2cid = 6427129}}</ref> | |||
| By the time a girl reaches school-age, this hormonal influence has stopped and the hymen becomes thin, smooth, delicate and almost ]. It is also very sensitive to touch; a physician who needed to swab the area would avoid the hymen and swab the outer ] instead.<ref name="McCann" /> | |||
| In several studies of adolescent female rape victims, where patients were examined at a hospital following sexual assault, half or fewer of virgin victims had any injury to the hymen.<ref name=":6">{{Cite journal |vauthors=White C, McLean I |date=2006-05-01|title=Adolescent complainants of sexual assault; injury patterns in virgin and non-virgin groups|journal=Journal of Clinical Forensic Medicine|language=en|volume=13|issue=4|pages=172–180|doi=10.1016/j.jcfm.2006.02.006|pmid=16564196|issn=1353-1131|quote=Hymen injury was noted in 40 (50.6%) participants of the virgin group, but only 11 (12.4%) of the non-virgin group}}</ref><ref>{{Cite journal|last1=Adams|first1=Joyce A.|last2=Girardin|first2=Barbara|last3=Faugno|first3=Diana|date=May 2000|title=Signs of genital trauma in adolescent rape victims examined acutely|url=https://www.jpagonline.org/article/S1083-3188(00)00015-2/abstract|journal=Journal of Pediatric and Adolescent Gynecology|language=en|volume=13|issue=2|page=88|doi=10.1016/S1083-3188(00)00015-2|pmid=10869972|issn=1083-3188}}</ref><ref name=":7">{{Cite journal|date=2001-11-01|title=Adolescent Sexual Assault: Documentation of Acute Injuries Using Photo-colposcopy|journal=Journal of Pediatric and Adolescent Gynecology|language=en|volume=14|issue=4|pages=175–180|doi=10.1016/S1083-3188(01)00126-7|issn=1083-3188|quote=The incidence of hymenal tears in self-described virgins was higher than in nonvirgins (19% vs. 3%, P .008);|last1=Adams|first1=Joyce A.|last2=Girardin|first2=Barbara|last3=Faugno|first3=Diana|pmid=11748013}}</ref> Tears of the hymen occurred in less than a quarter of cases.<ref name=":7" /> However, virgins were significantly more likely to have injuries to the hymen than non-virgins.<ref name=":6" /><ref name=":7" /> | |||
| Prepubescent girls' hymenal opening comes in a many shapes, depending on hormonal and activity level, the most common being crescentic (posterior rim): no tissue at the 12 o'clock position; crescent shaped band of tissue from 1-2 to 10-11 o'clock at its' widest around 6 o'clock. From puberty onwards, depending on ] and activity levels, the hymenal tissue may be thicker and the opening is often fimbriated or erratically shaped<ref>Heger, Astrid; Emans, S. Jean and Muram, David (2000). ''Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas'', Second edition, Oxford University Press, 116.</ref> | |||
| In a study of adolescents who had previously had consensual sex, approximately half showed evidence of trauma to the hymen.<ref>{{Cite journal|last1=Adams|first1=Joyce A.|last2=Botash|first2=Ann S.|last3=Kellogg|first3=Nancy|date=March 2004|title=Differences in hymenal morphology between adolescent girls with and without a history of consensual sexual intercourse|journal=Archives of Pediatrics & Adolescent Medicine|volume=158|issue=3|pages=280–285|doi=10.1001/archpedi.158.3.280|issn=1072-4710|pmid=14993089|quote=Subjects who admitted having past intercourse still had non disrupted, intact hymens in 52% of cases.|doi-access=free}}</ref><ref name=":8">{{Cite web|url=https://www.psychologytoday.com/gb/blog/you-it/200806/new-york-times-is-wrong-about-hymens-they-are-not-alone|title=New York Times Is Wrong about Hymens--But They Are Not Alone|website=Psychology Today|language=en-GB|access-date=2018-09-08}}</ref> Trauma to the hymen may also occur in adult non-virgins following consensual sex, although it is rare.<ref>{{Cite journal|last1=Slaughter|first1=Laura|last2=Brown|first2=Carl R.V.|last3=Crowley|first3=Sharon|last4=Peck|first4=Roxy|date=March 1997|title=Patterns of genital injury in female sexual assault victims|journal=American Journal of Obstetrics and Gynecology|volume=176|issue=3|pages=609–616|doi=10.1016/s0002-9378(97)70556-8|pmid=9077615|issn=0002-9378}}</ref> Trauma to the hymen may heal without any visible sign of injury.<ref name=":6" /><ref name=":8" /><ref name="emans" /> An observational study of adolescent sexual assault victims found that majority of wounds to the hymen healed without any visible sign of injury having occurred.<ref>{{Cite journal|last=Reading|first=Richard|date=2007-12-12|title=Healing of hymenal injuries in prepubertal and adolescent girls: a descriptive study|journal=Child: Care, Health and Development|language=en|volume=34|issue=1|pages=137–138|doi=10.1111/j.1365-2214.2007.00818_7.x|issn=0305-1862|quote=Of the girls who sustained 'superficial', 'intermediate,' or 'deep' lacerations, 15 of 18 prepubertal girls had smooth and continuous appearing hymenal rims, whereas 24 of 41 adolescents' hymens had a normal, 'scalloped' appearance and 30 of 34 had no disruption of continuity on healing. The final 'width' of a hymenal rim was dependent on the initial depth of the laceration. No scar tissue formation was observed in either group of girls.}}</ref> | |||
| After giving birth, the vaginal opening usually has nothing left but hymenal tags (carunculae mytriformes) and is called "parous introitus".{{Fact|date=February 2009}} | |||
| Trauma to the hymen is hypothesized to occur as a result of various other behaviors, such as ] or ] use, ]s with a ], masturbation, gymnastics, or horseback riding, although the true prevalence of trauma as a result of these activities is unclear.<ref name="ucsb sexinfo" /><ref>{{Cite journal|date=1998-06-08|title=Can tampon use cause hymen changes in girls who have not had sexual intercourse? A review of the literature|journal=Forensic Science International|language=en|volume=94|issue=1–2|pages=147–153|doi=10.1016/S0379-0738(98)00053-X|issn=0379-0738|last1=Goodyear-Smith|first1=Felicity A.|last2=Laidlaw|first2=Tannis M.|pmid=9670493}}</ref><ref>{{Cite journal|date=1994-07-01|title=Hymenal findings in adolescent women: Impact of tampon use and consensual sexual activity|journal=The Journal of Pediatrics|language=en|volume=125|issue=1|pages=153–160|doi=10.1016/S0022-3476(94)70144-X|issn=0022-3476|quote=Contrary to the popular belief that transections of the hymen are associated with gymnastics, horseback riding, and other vigorous sports, we found no relation between sports or gymnastics and hymenal changes. There was also no relation to prior gynecologic examination.|last1=Emans|first1=S.Jean|last2=Woods|first2=Elizabeth R.|last3=Allred|first3=Elizabeth N.|last4=Grace|first4=Estherann|pmid=8021768}}</ref> | |||
| == Anatomic anomalies == | |||
| Anomalies of the female reproductive tract can result from agenesis or hypoplasia, canalization defects, lateral fusion and failure of resorption, resulting in various complications.<ref name="WebMD" /> | |||
| * Imperforate:<ref>{{cite book |last= |first= |authorlink= |coauthors= |title=Encyclopedia of Jewish Medical Ethics |year=2003 |publisher= |quote=Occasionally, the hymen is harder than normal or it is complete and sealed | |||
| without there being ... This condition is called imperforate hymen and, at times ... | url=http://books.google.com/books?id=aaklGZAID08C&pg=PA1115&dq=hymen&lr=&ei=SFeDSbi_H4buMqrIjbgF |isbn=1583305920 }}</ref><ref>Ergun, E. "Social, Medical, and Legal Control of Female Sexuality Through Construction of Virginity in Turkey" (2006). Unpublished masters thesis, Towson University, MD, USA. Accessed 01.17.2007 at </ref> hymenal opening non existent; will require minor surgery if it has not corrected itself by puberty to allow menstrual fluids to escape. | |||
| * Cribriform, or microperforate: sometimes confused for imperforate, the hymenal opening appears to be non existent, but has, under close examination, small openings. | |||
| * Septate: the hymenal opening has one or more bands extending across the opening. | |||
| ==Cultural and religious significance== | |||
| == Hymens in other animals == | |||
| {{further|Virginity test}} | |||
| The hymen is often attributed important cultural significance in certain communities because of its association with a woman's ]. In those cultures, an intact hymen is highly valued at marriage in the belief that this is a proof of virginity.<ref name="ucsb sexinfo" /><ref>{{cite news|url=https://www.reuters.com/article/us-muslimwomen-europe-virginity-idUSL2532025120070430?pageNumber=2&sp=true |title=Muslim women in France regain virginity in clinics |work=Reuters |quote='Many of my patients are caught between two worlds,' said Abecassis. They have had sex already but are expected to be virgins at marriage according to a custom that he called 'cultural and traditional, with enormous family pressure'. | date=April 30, 2007}}</ref><ref name=europe/> Some women undergo ] to restore their hymen for this reason.<ref name="europe">{{Cite news|last1=Sciolino|first1=Elaine|last2=Mekhennet|first2=Souad|date=June 11, 2008|title=In Europe, Debate Over Islam and Virginity|work=]|url=https://www.nytimes.com/2008/06/11/world/europe/11virgin.html?_r=1&scp=1&sq=hymen&st=nyt&oref=slogin|access-date=2008-06-13|quote='In my culture, not to be a virgin is to be dirt,' said the student, perched on a hospital bed as she awaited surgery on Thursday. 'Right now, virginity is more important to me than life.'}}</ref> In October 2018, the ], ] and the ] (WHO) stated that virginity testing must end as "it is a painful, humiliating and traumatic practice, constituting ]".<ref>{{Cite web|url=https://www.who.int/news-room/detail/17-10-2018-united-nations-agencies-call-for-ban-on-virginity-testing|title=United Nations agencies call for ban on virginity testing|date=17 October 2018|publisher=World Health Organization|access-date=22 October 2018}}</ref> | |||
| Some traditional ] state that it is intended by God for the husband to be the one to break his wife's hymen, and that the bleeding the hymen, believed occur during first intercourse (but see above), is a ] that seals the bond of ] between husband and wife (cf. '']'').<ref name="Gentry2021">{{cite book |last1=Gentry |first1=Harold |title=Intimacy |date=21 January 2021 |publisher=] |isbn=978-1-6642-1232-9 |language=en}}</ref> | |||
| Due to similar reproductive system development, many mammals, from chimpanzees and elephants to manatees and whales, retain hymens. <ref>{{cite book |last=Blank |first=Hanne|authorlink=Hanne Blank|url=http://books.google.com/books?ei=GX-AScSHI4rONcO9oEw&id=shq1AAAAIAAJ&dq=Virgin%3A+The+Untouched+History&q=toothed+whales&pgis=1#search_anchor | title=Virgin: The Untouched History |year=2007|publisher=] |pages=23}}</ref><ref>, ], 02 October, 1992, ]</ref><ref>{{cite book |last=Blackledge |first=Catherine |authorlink= |coauthors= |title=The Story of V |year=2004 |publisher=] |quote=Hymens, or vaginal closure membranes or vaginal constrictions, as they are often referred to, are found in a number of mammals, including llamas, ... | url=http://books.google.com/books?id=f2d-11Y_u3cC&pg=PP250&dq=guinea+pig+hymen&ei=ocSAScWgCaasNZivuZgO |isbn=0813534550 }}</ref> | |||
| == |
==Womb fury== | ||
| In the 16th and 17th centuries, medical researchers mistakenly saw the presence or absence of the hymen as founding evidence of physical diseases such as "womb-fury", i.e., ]. If not cured, womb-fury would, according to doctors practicing at the time, result in death.<ref>{{cite journal | last1 = Berrios | first1 = GE | last2 = Rivière | first2 = L | year = 2006 | title = Madness from the womb | journal = History of Psychiatry | volume = 17 | issue = 66 Pt 2 | pages = 223–35 | doi=10.1177/0957154x06065699| pmid = 17146991 | s2cid = 148179899 | url = https://hal.science/hal-00570861 }}</ref><ref>The linkage between the hymen and social elements of control has been taken up in Marie Loughlin's book published in 1997</ref> | |||
| {{main|Hymenorrhaphy}} | |||
| <!--==Modern perspective==In late 2005, Monica Christiansson, former maternity ward nurse and Carola Eriksson, a PhD student at ] announced that according to studies of medical literature and practical experience, the hymen should be considered a social and cultural myth, based on deeply rooted stereotypes of women's roles in sexual relations with men. Christiansson and Eriksson support their claims by pointing out that there are no accurate medical descriptions of what a hymen actually consists of. Statistics presented by the two state that fewer than 30% of women who have gone through puberty and have consensual intercourse bleed the first time. Christiansson has expressed an opinion that the use of the term "hymen" should be discontinued and that it should be considered an integral part of the vaginal opening.<ref> {{sv icon}}</ref>--> | |||
| ==Other animals== | |||
| In some cultures the concept of an intact hymen is highly valued at marriage and an increasing number of Muslim women in Europe undergo a ] to restore their hymens.<ref name=debate>{{cite news |first= |last= |authorlink= |coauthors= |title=In Europe, Debate Over Islam and Virginity |url=http://www.nytimes.com/2008/06/11/world/europe/11virgin.html?_r=1&scp=1&sq=hymen&st=nyt&oref=slogin |quote=Like an increasing number of Muslim women in Europe, she had a hymenoplasty, a restoration of her hymen, the vaginal membrane that normally breaks in the first act of intercourse. |publisher=] |date=], ] |accessdate=2008-06-13 }}</ref> In Korea the word for hymen translates literally as “virgin-skin” and a small industry has grown up around its surgical construction through plastic surgery. In 1994 the Korean Medical Research Center was made to pay compensation to a 40-year-old woman for extreme psychological distress after she lost her hymen during a Pap smear test. The court found that, “it is clear that the hymen is still recognized as a symbol of ‘virginity’ and keeping virginity is valued in society". <ref>Park, J. I., Compensation for hymen lost: Not loss of virginity but a medical accident. Chosun Daily Aug 1994</ref> Some Korean prenatal clinics offers STD tests with hymenorrhaphy, in order to "free" women from their history of sexual experiences in the past. <ref>http://www.yunlee.co.kr</ref> These surgeries are not even approved by the Korean medical association because they are based on myths and efforts at re-education are being made. <ref>International Encyclopedia of Sexuality, South Korea by Hyung-Ki Choi, M.D., Ph.D., and Huso Yi, Ph.D.</ref> | |||
| Due to similar reproductive system development, many mammals have hymens, including ]s, ]s, ]s, whales, horses and ]s.<ref>{{Cite book|last=Blank |first=Hanne|author-link=Hanne Blank|url=https://books.google.com/books?id=shq1AAAAIAAJ&q=toothed+whales | title=Virgin: The Untouched History |year=2007|publisher=] |page=23 |isbn=978-1-59691-010-2 |access-date=2013-11-09}}</ref><ref>{{Cite book|last=Blackledge |first=Catherine |title=The Story of V |year=2004 |publisher=] |quote=Hymens, or vaginal closure membranes or vaginal constrictions, as they are often referred to, are found in a number of mammals, including llamas, ... | url=https://archive.org/details/storyofv00cath |url-access=registration |isbn=978-0-8135-3455-8 }}</ref> | |||
| == |
==See also== | ||
| <!-- THIS SECTION IS ONLY FOR LINKS TO OTHER WIKIPEDIA ARTICLES --> | |||
| *As early as the late sixteenth century, ] and Andreas Laurentius asserted to have never seen the hymen and that it was "a primitive myth, unworthy of a civilized nation like France."<ref name=loughlin/> | |||
| *] | |||
| * In the sixteenth and seventeenth centuries, medical researchers have used the presence of the hymen, or lack thereof, as founding evidence of physical diseases such as "womb-fury". If not cured, womb-fury would, according to these early doctors, result in death.<ref name=loughlin>{{cite book |last=Loughlin |first=Marie |authorlink=Marie Loughlin |coauthors= |title=Hymeneutics: Interpreting Virginity on the Early Modern Stage |year=1997 |publisher=] |quote= | url=http://books.google.com/books?id=3wqNbrYPNn8C&pg |isbn= }}</ref> | |||
| ==References== | |||
| ==Modern perspectives== | |||
| {{Reflist|2}} | |||
| ==External links== | |||
| In late 2005, Monica Christiansson, former maternity ward nurse and Carola Eriksson, a PhD student at ] announced that according to studies of medical literature and practical experience, the hymen should be considered a social and cultural myth, based on deeply rooted stereotypes of women's roles in sexual relations with men. Christiansson and Eriksson support their claims by pointing out that there are no accurate medical descriptions of what a hymen actually consists of. Statistics presented by the two state that fewer than 30% of women who have gone through puberty and have consensual intercourse bleed the first time. Christiansson has expressed an opinion that the use of the term "hymen" should be discontinued and that it should be considered an integral part of the vaginal opening.<ref> {{sv icon}}</ref> | |||
| {{commons category|Hymen}} | |||
| {{wikiquote}} | |||
| {{Prone to spam|date=September 2011}} | |||
| <!-- ======================== {{No more links}} ============================ | |||
| PLEASE BE CAUTIOUS IN ADDING MORE LINKS TO THIS ARTICLE. | |||
| By examining women's bodies for the existence of the hymen, researchers{{who}} have used it to determine whether or not women are "virtuous." ], professor at the ], explains how "the hymen itself emerges physiologically with the development of sexual purity codes" as an element of patriarchy.<ref>{{cite journal |authorlink=Sherry Beth Ortner |title=The Virgin and the State | last =Ortner | first =Sherry Beth | journal =] | volume =4 | issue =3 | pages =19-35 |accessdate=2009-02-03 |quote= |year=1987 }}</ref> | |||
| Misplaced Pages is not a collection of links and should not be used for advertising. | |||
| Excessive or inappropriate links WILL BE DELETED. | |||
| ==References== | |||
| {{reflist|2}} | |||
| See ] and ] for details. | |||
| ==External links== | |||
| * | |||
| * - Illustrations of hymen types | |||
| * the historical context of ] in a frank and easy-to-understand manner. | |||
| * - Interview with Hanne Blank, author of "Virgin: The Untouched History". Discusses relationship between hymen and concept of virginity. | |||
| * Explanation of the hymen, myths on first-time sex, Hymenectomies and Vaginismus (Painful sex or Fear of Penetration) | |||
| {{Female reproductive system}} | |||
| If there are already plentiful links, please propose additions | |||
| ] | |||
| or replacements on the article's discussion page. | |||
| ======================== {{No more links}} ============================ | |||
| --> | |||
| *—the historical context of ] | |||
| *—Interview with Hanne Blank, author of ''Virgin: The Untouched History''. Discusses relationship between hymen and concept of virginity. | |||
| * Radiology (US – ultrasound) of Hydrocolpos | |||
| * at the American Family Physician | |||
| * {{Webarchive|url=https://web.archive.org/web/20130117005752/http://www.scarleteen.com/article/body/my_corona_the_anatomy_formerly_known_as_the_hymen_the_myths_that_surround_it |date=January 17, 2013 }}, Scarleteen, Sex education for the real world | |||
| * | |||
| *. {{Webarchive|url=https://web.archive.org/web/20170110225148/http://www.rfsu.se/en/Engelska/About-rfsu/Resources/Publications/Vagnial-Corona/ |date=January 10, 2017 }}. | |||
| * | |||
| {{Female reproductive system}} | |||
| {{Authority control}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 07:40, 20 November 2024
Membrane that surrounds or partially covers the vaginal opening This article is about the vaginal membrane. For other uses, see Hymen (disambiguation).
| Hymen | |
|---|---|
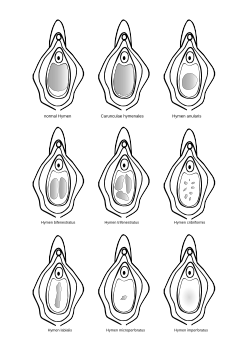 Various hymen defects (the shaded areas represent the vaginal opening) Various hymen defects (the shaded areas represent the vaginal opening) | |
 External genitals of a human female External genitals of a human female | |
| Details | |
| Identifiers | |
| Latin | hymen |
| Greek | ὑμήν |
| MeSH | D006924 |
| TA98 | A09.1.04.008 |
| TA2 | 3530 |
| FMA | 20005 |
| Anatomical terminology[edit on Wikidata] | |
The hymen is a thin piece of mucosal tissue that surrounds or partially covers the vaginal introitus. A small percentage are born with hymens that are imperforate and completely obstruct the vaginal canal. It forms part of the vulva and is similar in structure to the vagina. The term comes straight from the Greek, for 'membrane'.
In children, a common appearance of the hymen is crescent-shaped, although many shapes are possible. Each shape in the natural range has a Latinate name. During puberty, estrogen causes the hymen to change in appearance and become very elastic. Normal variations of the post-pubertal hymen range from thin and stretchy to thick and somewhat rigid. Very rarely, it may be completely absent.
The hymen can rip or tear during first penetrative intercourse, which usually results in pain and, sometimes, mild temporary bleeding or spotting. Minor injuries to the hymen may heal on their own, and not require surgical intervention. Historically, it was believed that first penetration was necessarily traumatic, but now sources differ on how common tearing or bleeding are as a result of first intercourse. Therefore, the state of the hymen is not a reliable indicator of virginity, though "virginity testing" remains a common practice in some cultures, sometimes accompanied by hymen reconstruction surgery to give the appearance of virginity.
Development and histology
The genital tract develops during embryogenesis, from the third week of gestation to the second trimester, and the hymen is formed following the vagina. At week seven, the urorectal septum forms and separates the rectum from the urogenital sinus. At week nine, the Müllerian ducts move downwards to reach the urogenital sinus, forming the uterovaginal canal and inserting into the urogenital sinus. At week twelve, the Müllerian ducts fuse to create a primitive uterovaginal canal called unaleria. At month five, the vaginal canalization is complete and the fetal hymen is formed from the proliferation of the sinovaginal bulbs (where Müllerian ducts meet the urogenital sinus), and normally becomes perforate before or shortly after birth.
The hymen has dense innervation. In newborn babies, still under the influence of the mother's hormones, the hymen is thick, pale pink, and redundant (folds in on itself and may protrude). For the first two to four years of life, the infant produces hormones that continue this effect. Their hymenal opening tends to be annular (circumferential).
Post neonatal stage, the diameter of the hymenal opening (measured within the hymenal ring) widens by approximately 1 mm for each year of age. During puberty, estrogen causes the hymen to become very elastic and fimbriated.
The hymen can stretch or tear as a result of various behaviors, by the use of tampons or menstrual cups, pelvic examinations with a speculum, or sexual intercourse. Remnants of the hymen are called carunculae myrtiformes.
A glass or plastic rod of 6 mm diameter having a globe on one end with varying diameter from 10 to 25 mm, called a Glaister Keen rod, is used for close examination of the hymen or the degree of its rupture. In forensic medicine, it is recommended by health authorities that a physician who must swab near this area of a prepubescent girl avoid the hymen and swab the outer vulval vestibule instead. In cases of suspected rape or child sexual abuse, a detailed examination of the hymen may be performed, but the condition of the hymen alone is often inconclusive.
Anatomic variations
Normal variations of the hymen range from thin and stretchy to thick and somewhat rigid. An imperforate hymen occurs in 1-2 out of 1,000 infants. The only variation that may require medical intervention is the imperforate hymen, which either completely prevents the passage of menstrual fluid or slows it significantly. In either case, surgical intervention may be needed to allow menstrual fluid to pass or intercourse to take place at all.
Prepubescent hymenal openings come in many shapes, depending on hormonal and activity level, the most common being crescentic (posterior rim): no tissue at the 12 o'clock position; crescent-shaped band of tissue from 1–2 to 10–11 o'clock, at its widest around 6 o'clock. From puberty onwards, depending on estrogen and activity levels, the hymenal tissue may be thicker, and the opening is often fimbriated or erratically shaped. In younger children, a torn hymen will typically heal very quickly. In adolescents, the hymenal opening can naturally extend and variation in shape and appearance increases.
Variations of the female reproductive tract can result from agenesis or hypoplasia, canalization defects, lateral fusion and failure of resorption, resulting in various complications.
- Imperforate: hymenal opening nonexistent; will require minor surgery if it has not corrected itself by puberty to allow menstrual fluids to escape.
- Cribriform, or microperforate: sometimes confused for imperforate, the hymenal opening appears to be nonexistent, but has, under close examination, small perforations.
- Septate: the hymenal opening has one or more bands of tissue extending across the opening.
Trauma

Historically, it was believed that first sexual intercourse was necessarily traumatic to the hymen and always resulted in the hymen being "broken" or torn, causing bleeding. However, research on women in Western populations has found that bleeding during first intercourse does not invariably occur. In one cross-cultural study, slightly more than half of all women self-reported bleeding during first intercourse, with significantly different levels of pain and bleeding reported depending on their region of origin. Not all women experience pain, and one study found a correlation between the experience of strong emotions – such as excitement, nervousness, or fear – with experiencing pain during first intercourse.
In several studies of adolescent female rape victims, where patients were examined at a hospital following sexual assault, half or fewer of virgin victims had any injury to the hymen. Tears of the hymen occurred in less than a quarter of cases. However, virgins were significantly more likely to have injuries to the hymen than non-virgins.
In a study of adolescents who had previously had consensual sex, approximately half showed evidence of trauma to the hymen. Trauma to the hymen may also occur in adult non-virgins following consensual sex, although it is rare. Trauma to the hymen may heal without any visible sign of injury. An observational study of adolescent sexual assault victims found that majority of wounds to the hymen healed without any visible sign of injury having occurred.
Trauma to the hymen is hypothesized to occur as a result of various other behaviors, such as tampon or menstrual cup use, pelvic examinations with a speculum, masturbation, gymnastics, or horseback riding, although the true prevalence of trauma as a result of these activities is unclear.
Cultural and religious significance
Further information: Virginity testThe hymen is often attributed important cultural significance in certain communities because of its association with a woman's virginity. In those cultures, an intact hymen is highly valued at marriage in the belief that this is a proof of virginity. Some women undergo hymenorrhaphy to restore their hymen for this reason. In October 2018, the UN Human Rights Council, UN Women and the World Health Organization (WHO) stated that virginity testing must end as "it is a painful, humiliating and traumatic practice, constituting violence against women".
Some traditional Christian theological interpretations state that it is intended by God for the husband to be the one to break his wife's hymen, and that the bleeding the hymen, believed occur during first intercourse (but see above), is a blood covenant that seals the bond of holy matrimony between husband and wife (cf. consummation).
Womb fury
In the 16th and 17th centuries, medical researchers mistakenly saw the presence or absence of the hymen as founding evidence of physical diseases such as "womb-fury", i.e., (female) hysteria. If not cured, womb-fury would, according to doctors practicing at the time, result in death.
Other animals
Due to similar reproductive system development, many mammals have hymens, including chimpanzees, elephants, manatees, whales, horses and llamas.
See also
References
- ^ Heger, Astrid H.; Emans, S. Jean, eds. (2000). Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas (PDF) (2nd ed.). New York: Oxford University Press. pp. 61–65. ISBN 978-0-19-507425-3. Archived from the original (PDF) on July 8, 2018. Retrieved July 8, 2018.
- ^ Perlman, Sally E.; Nakajyma, Steven T.; Hertweck, S. Paige (2004). Clinical protocols in pediatric and adolescent gynecology. Parthenon. p. 131. ISBN 978-1-84214-199-1.
- ^ Lahoti, Sheela L.; McClain, Natalie; Girardet, Rebecca; McNeese, Margaret; Cheung, Kim (March 1, 2001). "Evaluating the Child for Sexual Abuse". American Family Physician. 63 (5): 883–92. ISSN 0002-838X. PMID 11261865.
- ^ Heger, Astrid H.; Emans, S. Jean, eds. (2000). Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas (PDF) (2nd ed.). New York: Oxford University Press. p. 122. ISBN 978-0-19-507425-3. Archived from the original (PDF) on July 8, 2018. Retrieved July 8, 2018.
- Mishori, R.; Ferdowsian, H.; Naimer, K.; Volpellier, M.; McHale, T. (June 3, 2019). "The little tissue that couldn't – dispelling myths about the Hymen's role in determining sexual history and assault - Fact 1A". Reproductive Health. 16 (1): 74. doi:10.1186/s12978-019-0731-8. PMC 6547601. PMID 31159818.
- Hegazy, Abdelmonem; Al-Rukban, Mohammed (January 1, 2012). "Hymen: Facts and conceptions". The Health. 3 (4). ISSN 2219-8083.
Possible explanations for the lack of genital trauma include... acute injuries occur but heal completely.
- ^ "The Hymen". University of California, Santa Barbara. Retrieved September 19, 2020.
While some females bleed the first time they have penetrative intercourse, not every female does. This depends on many factors, such as how much hymenal tissue a female has, whether her hymen has already been stretched or torn, or how thick and elastic it is.
- ^ Rogers, Deborah J; Stark, Margaret (August 8, 1998). "The hymen is not necessarily torn after sexual intercourse". BMJ: British Medical Journal. 317 (7155): 414. doi:10.1136/bmj.317.7155.414. ISSN 0959-8138. PMC 1113684. PMID 9694770.
- ^ Emma Curtis, Camille San Lazaro (February 27, 1999). "Appearance of the hymen in adolescents is not well documented". BMJ: British Medical Journal. 318 (7183): 605. doi:10.1136/bmj.318.7183.605. PMC 1115047. PMID 10037658.
We agree with Rogers and Stark that so called rupture and bleeding of the hymen is not to be routinely expected after first sexual intercourse.
- ^ Knight, Bernard (1997). Simpson's Forensic Medicine (11th ed.). London: Arnold. p. 114. ISBN 978-0-7131-4452-9.
- Healey, Andrew (2012). "Embryology of the female reproductive tract". In Mann, Gurdeep S.; Blair, Joanne C.; Garden, Anne S. (eds.). Imaging of Gynecological Disorders in Infants and Children. Medical Radiology. Springer. pp. 21–30. doi:10.1007/978-3-540-85602-3. ISBN 978-3-540-85602-3.
- ^ McCann, J; Rosas, A. and Boos, S. (2003) "Child and adolescent sexual assaults (childhood sexual abuse)" in Payne-James, Jason; Busuttil, Anthony and Smock, William (eds). Forensic Medicine: Clinical and Pathological Aspects, Greenwich Medical Media: London, a)p.453, b)p.455 c)p.460. ISBN 978-1-84-110026-5
- ^ Heger, Astrid; Emans, S. Jean; Muram, David (2000). Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas (Second ed.). Oxford University Press. p. 116. ISBN 978-0-19-507425-3.
- Pugno, Perry (1999). "Genital Findings in Prepubertal Girls Evaluated for Sexual Abuse". CiteSeerX 10.1.1.522.1894.
- Callahan, Tamara L.; Caughey, Aaron B. (2009). Blueprints Obstetrics and Gynecology. Lippincott Williams & Wilkins. ISBN 978-0-7817-8249-4.
- Lardenoije, Céline; Aardenburg, Robert; Mertens, Helen (May 26, 2009). "Imperforate hymen: a cause of abdominal pain in female adolescents". BMJ Case Reports. 2009: bcr0820080722. doi:10.1136/bcr.08.2008.0722. ISSN 1757-790X. PMC 3029536. PMID 21686660.
- "Imperforate hymen". medlineplus.gov. United States National Library of Medicine. 2021.
- "Congenital Anomalies of the Hymen". brighamandwomens.org. Brigham and Women's Hospital.
- "Imperforate Hymen". mountsinai.org. Mount Sinai Hospital (Brooklyn).
- "Cribriform Hymen". texaschildrens.org. Texas Children's Hospital.
- "Septate Hymen". childrenshospital.org. Boston Children's Hospital.
- ^ Loeber, Olga (2008). "Over het zwaard en de schede; bloedverlies en pijn bij de eerste coïtus Een onderzoek bij vrouwen uit diverse culturen" (PDF). Tijdschrift voor Seksuologie (in Dutch). Vol. 32. pp. 129–137. Archived from the original (PDF) on November 5, 2019. Retrieved September 7, 2018.
- Amy, Jean-Jacques (January 2008). "Certificates of virginity and reconstruction of the hymen". The European Journal of Contraception & Reproductive Health Care. 13 (2): 111–113. doi:10.1080/13625180802106045. ISSN 1362-5187. PMID 18465471. S2CID 37484764.
- Weis, David L. (1985). "The experience of pain during women's first sexual intercourse: Cultural mythology about female sexual initiation". Archives of Sexual Behavior. 14 (5): 421–438. doi:10.1007/BF01542003. PMID 4062539. S2CID 6427129.
- ^ White C, McLean I (May 1, 2006). "Adolescent complainants of sexual assault; injury patterns in virgin and non-virgin groups". Journal of Clinical Forensic Medicine. 13 (4): 172–180. doi:10.1016/j.jcfm.2006.02.006. ISSN 1353-1131. PMID 16564196.
Hymen injury was noted in 40 (50.6%) participants of the virgin group, but only 11 (12.4%) of the non-virgin group
- Adams, Joyce A.; Girardin, Barbara; Faugno, Diana (May 2000). "Signs of genital trauma in adolescent rape victims examined acutely". Journal of Pediatric and Adolescent Gynecology. 13 (2): 88. doi:10.1016/S1083-3188(00)00015-2. ISSN 1083-3188. PMID 10869972.
- ^ Adams, Joyce A.; Girardin, Barbara; Faugno, Diana (November 1, 2001). "Adolescent Sexual Assault: Documentation of Acute Injuries Using Photo-colposcopy". Journal of Pediatric and Adolescent Gynecology. 14 (4): 175–180. doi:10.1016/S1083-3188(01)00126-7. ISSN 1083-3188. PMID 11748013.
The incidence of hymenal tears in self-described virgins was higher than in nonvirgins (19% vs. 3%, P .008);
- Adams, Joyce A.; Botash, Ann S.; Kellogg, Nancy (March 2004). "Differences in hymenal morphology between adolescent girls with and without a history of consensual sexual intercourse". Archives of Pediatrics & Adolescent Medicine. 158 (3): 280–285. doi:10.1001/archpedi.158.3.280. ISSN 1072-4710. PMID 14993089.
Subjects who admitted having past intercourse still had non disrupted, intact hymens in 52% of cases.
- ^ "New York Times Is Wrong about Hymens--But They Are Not Alone". Psychology Today. Retrieved September 8, 2018.
- Slaughter, Laura; Brown, Carl R.V.; Crowley, Sharon; Peck, Roxy (March 1997). "Patterns of genital injury in female sexual assault victims". American Journal of Obstetrics and Gynecology. 176 (3): 609–616. doi:10.1016/s0002-9378(97)70556-8. ISSN 0002-9378. PMID 9077615.
- Reading, Richard (December 12, 2007). "Healing of hymenal injuries in prepubertal and adolescent girls: a descriptive study". Child: Care, Health and Development. 34 (1): 137–138. doi:10.1111/j.1365-2214.2007.00818_7.x. ISSN 0305-1862.
Of the girls who sustained 'superficial', 'intermediate,' or 'deep' lacerations, 15 of 18 prepubertal girls had smooth and continuous appearing hymenal rims, whereas 24 of 41 adolescents' hymens had a normal, 'scalloped' appearance and 30 of 34 had no disruption of continuity on healing. The final 'width' of a hymenal rim was dependent on the initial depth of the laceration. No scar tissue formation was observed in either group of girls.
- Goodyear-Smith, Felicity A.; Laidlaw, Tannis M. (June 8, 1998). "Can tampon use cause hymen changes in girls who have not had sexual intercourse? A review of the literature". Forensic Science International. 94 (1–2): 147–153. doi:10.1016/S0379-0738(98)00053-X. ISSN 0379-0738. PMID 9670493.
- Emans, S.Jean; Woods, Elizabeth R.; Allred, Elizabeth N.; Grace, Estherann (July 1, 1994). "Hymenal findings in adolescent women: Impact of tampon use and consensual sexual activity". The Journal of Pediatrics. 125 (1): 153–160. doi:10.1016/S0022-3476(94)70144-X. ISSN 0022-3476. PMID 8021768.
Contrary to the popular belief that transections of the hymen are associated with gymnastics, horseback riding, and other vigorous sports, we found no relation between sports or gymnastics and hymenal changes. There was also no relation to prior gynecologic examination.
- "Muslim women in France regain virginity in clinics". Reuters. April 30, 2007.
'Many of my patients are caught between two worlds,' said Abecassis. They have had sex already but are expected to be virgins at marriage according to a custom that he called 'cultural and traditional, with enormous family pressure'.
- ^ Sciolino, Elaine; Mekhennet, Souad (June 11, 2008). "In Europe, Debate Over Islam and Virginity". The New York Times. Retrieved June 13, 2008.
'In my culture, not to be a virgin is to be dirt,' said the student, perched on a hospital bed as she awaited surgery on Thursday. 'Right now, virginity is more important to me than life.'
- "United Nations agencies call for ban on virginity testing". World Health Organization. October 17, 2018. Retrieved October 22, 2018.
- Gentry, Harold (January 21, 2021). Intimacy. WestBow Press. ISBN 978-1-6642-1232-9.
- Berrios, GE; Rivière, L (2006). "Madness from the womb". History of Psychiatry. 17 (66 Pt 2): 223–35. doi:10.1177/0957154x06065699. PMID 17146991. S2CID 148179899.
- The linkage between the hymen and social elements of control has been taken up in Marie Loughlin's book Hymeneutics: Interpreting Virginity on the Early Modern Stage published in 1997
- Blank, Hanne (2007). Virgin: The Untouched History. Bloomsbury Publishing. p. 23. ISBN 978-1-59691-010-2. Retrieved November 9, 2013.
- Blackledge, Catherine (2004). The Story of V. Rutgers University Press. ISBN 978-0-8135-3455-8.
Hymens, or vaginal closure membranes or vaginal constrictions, as they are often referred to, are found in a number of mammals, including llamas, ...
External links
- Magical Cups and Bloody Brides—the historical context of virginity
- 20 Questions About Virginity—Interview with Hanne Blank, author of Virgin: The Untouched History. Discusses relationship between hymen and concept of virginity.
- Putting tampon in painlessly Radiology (US – ultrasound) of Hydrocolpos
- Evaluating the Child for Sexual Abuse at the American Family Physician
- My Corona: The Anatomy Formerly Known as the Hymen & the Myths That Surround It Archived January 17, 2013, at the Wayback Machine, Scarleteen, Sex education for the real world
- The Hymen Myth
- Vaginal Corona. Archived January 10, 2017, at the Wayback Machine.
- 5 Myths about Virginity, Busted
| Female reproductive system | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal |
| ||||||||||||||||||||||||||||||
| External |
| ||||||||||||||||||||||||||||||
| Blood supply | |||||||||||||||||||||||||||||||
| Other | |||||||||||||||||||||||||||||||
