| Revision as of 11:05, 14 December 2005 editBrisvegas (talk | contribs)Extended confirmed users4,604 edits re-worked article← Previous edit | Latest revision as of 11:52, 12 December 2024 edit undo2604:2000:2fc0:f:e123:5ff5:2949:5def (talk)No edit summary | ||
| (673 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Study of the different types of sensory perception of fetuses during pregnancy}} | |||
| ⚫ | |||
| {{expert needed|biology|date=August 2009|reason=discrepancy between abortion subsection and rest of the article, and lacking scientific consensus in article overall}} | |||
| {{mergeto|List of political epithets}} | |||
| '''Prenatal perception''' is the study of the extent of ] and other types of ] during ]. In practical terms, this means the study of ]es; none of the accepted indicators of perception are present in ]s. Studies of this type inform the ], along with certain related pieces of legislation in countries affected by that debate. As of 2022, there is not any ] on whether a fetus can feel pain.<ref>{{Cite news |last=Belluck |first=Pam |date=2013-09-17 |title=Complex Science at Issue in Politics of Fetal Pain |language=en-US |work=The New York Times |url=https://www.nytimes.com/2013/09/17/health/complex-science-at-issue-in-politics-of-fetal-pain.html |access-date=2022-09-20 |issn=0362-4331}}</ref><ref>{{Cite web |last=Levitan |first=Dave |date=2015-05-18 |title=Does a Fetus Feel Pain at 20 Weeks? |url=https://www.factcheck.org/2015/05/does-a-fetus-feel-pain-at-20-weeks/ |access-date=2022-09-20 |website=FactCheck.org |language=en-US}}</ref><ref>{{Cite news |last=Karni |first=Annie |date=2022-09-13 |title=Graham Proposes 15-Week Abortion Ban, Splitting Republicans |language=en-US |work=The New York Times |url=https://www.nytimes.com/2022/09/13/us/politics/lindsey-graham-abortion.html |access-date=2022-09-20 |issn=0362-4331}}</ref> | |||
| <!-- Unsourced image Image:Baby_in_the_womb.jpg removed --> | |||
| ==Prenatal hearing== | |||
| The issue of when a fetus can feel pain is a highly divisive and keenly debated one when considering the effects of ] on the ]. While scientists have acknowledged that a foetus can indeed feel physical pain, professional opinion is still divided as to when the foetus has the necessary sensory perception to experience pain. Several academics, usually those supporting abortion, contend that only once connections to the ] are made can the fetus experience pain; this usually occurs during the third trimester of the pregnancy, when only 1% of abortions are carried out. Other scientists, who mainly hold pro-life convictions, argue that a fetus can feel pain as early as 7 weeks, during the first trimester. The personal bias of many researchers is believed to influence their analysis of any experiments they undertake into the phenomenon. The topic has also been hotly debated by many politicians of both persuasions. | |||
| Numerous studies have found evidence indicating a fetus's ability to respond to auditory stimuli. The earliest fetal response to a sound stimulus has been observed at 16 weeks' gestational age, while the auditory system is fully functional at 25–29 weeks' gestation.<ref>{{cite journal |last1=Graven |first1=Stanley N. |last2=Browne |first2=Joy V. |title=Auditory Development in the Fetus and Infant |journal=Newborn and Infant Nursing Reviews |date=December 2008 |volume=8 |issue=4 |pages=187–193 |doi=10.1053/j.nainr.2008.10.010 |s2cid=6361226 |url=https://www.sciencedirect.com/science/article/pii/S1527336908001347 |access-date=31 May 2022 |language=en |issn=1527-3369}}</ref> At 33–41 weeks' gestation, the fetus is able to distinguish its mother's voice from others.<ref>{{cite journal |doi=10.1016/j.infbeh.2008.10.002 |pmid=19058856 |title=Fetal sensitivity to properties of maternal speech and language |journal=Infant Behavior and Development |volume=32 |issue=1 |pages=59–71 |year=2009 |last1=Kisilevsky |first1=B.S. |last2=Hains |first2=S.M.J. |last3=Brown |first3=C.A. |last4=Lee |first4=C.T. |last5=Cowperthwaite |first5=B. |last6=Stutzman |first6=S.S. |last7=Swansburg |first7=M.L. |last8=Lee |first8=K. |last9=Xie |first9=X. |last10=Huang |first10=H. |last11=Ye |first11=H.-H. |last12=Zhang |first12=K. |last13=Wang |first13=Z. }}</ref><ref>{{cite journal |doi=10.1002/dev.20229 |pmid=17577240 |title=Estimated cardiac vagal tone predicts fetal responses to mother's and stranger's voices |journal=Developmental Psychobiology |volume=49 |issue=5 |pages=543–7 |year=2007 |last1=Smith |first1=Laura S. |last2=Dmochowski |first2=Pawel A. |last3=Muir |first3=Darwin W. |last4=Kisilevsky |first4=Barbara S. }}</ref> | |||
| ==Prenatal pain== | |||
| Pain in an adult, child, newborn or late-term fetus originates as an electrical impulse in a body's ]s. This signal is sent via nerve pathways to the ], and then to the ] - a part of the brain that relays signals from the ] to the ], where it is sensed as pain. | |||
| ] | |||
| The hypothesis that human fetuses are capable of perceiving ] during the first trimester has little evidence, although fetuses at 14 weeks may respond to touch.<ref>{{Cite journal|last1=Marx|first1=Viola|last2=Nagy|first2=Emese|date=2015-06-08|title=Fetal Behavioural Responses to Maternal Voice and Touch|journal=PLOS ONE|volume=10|issue=6|pages=e0129118|doi=10.1371/journal.pone.0129118|issn=1932-6203|pmc=4460088|pmid=26053388|bibcode=2015PLoSO..1029118M|doi-access=free}}</ref>{{Additional citation needed|date=May 2022|reason=Source is just a single article and not a review; The 8-week figure was only mentioned in passing as a figure from a popular book instead of being an experimental result.}} A multidisciplinary ] from 2005 found limited evidence that thalamocortical pathways begin to function "around 29 to 30 weeks' gestational age", only after which a fetus is capable of feeling pain.<ref name="Lee">{{cite journal|last1=Lee|first1=Susan J.|last2=Ralston|first2=Henry J. Peter|last3=Drey|first3=Eleanor A.|last4=Partridge|first4=John Colin|last5=Rosen|first5=Mark A.|year=2005|title=Fetal Pain|journal=JAMA|volume=294|issue=8|pages=947–54|doi=10.1001/jama.294.8.947|pmid=16118385|doi-access=free}}</ref><ref>{{cite journal |doi=10.1136/bmj.332.7546.909 |pmid=16613970 |pmc=1440624 |title=Can fetuses feel pain? |journal=BMJ |volume=332 |issue=7546 |pages=909–12 |year=2006 |last1=Derbyshire |first1=S. W G }}</ref> | |||
| In March 2010, the Royal College of Obstetricians and Gynecologists submitted a report,<ref name="royalcollege">{{Cite web|date=March 2010|title=Fetal Awareness – Review of Research and Recommendations for Practice|url=http://www.rcog.org.uk/files/rcog-corp/RCOGFetalAwarenessWPR0610.pdf|url-status=dead|archive-url=https://web.archive.org/web/20111002222748/http://www.rcog.org.uk/files/rcog-corp/RCOGFetalAwarenessWPR0610.pdf|archive-date=2011-10-02|publisher=]|via=Internet Archive|access-date=2019-03-27}}</ref> concluding that "Current research shows that the sensory structures are not developed or specialized enough to respond to pain in a fetus of less than 24 weeks",<ref name="royalcollege" />{{rp|22}} | |||
| In a fetus, pain receptors develop around 7 weeks after conception; the ] at about 13 weeks. However, the connections to the cortex are established only after about 26 weeks into pregnancy. Most pro-life advocates believe that pain can be felt by the fetus when these systems are only partly formed. Most pro-choice advocates believe that only once all the connections between the receptors and brain can pain be felt - i.e. sometime after about 26 weeks into pregnancy. | |||
| {{blockquote|The neural regions and pathways that are responsible for pain experience remain under debate but it is generally accepted that pain from physical trauma requires an intact pathway from the periphery, through the spinal cord, into the thalamus and on to regions of the cerebral cortex including the primary sensory cortex (S1), the insular cortex and the anterior cingulated cortex. Fetal pain is not possible before these necessary neural pathways and structures have developed.<ref name="royalcollege" />{{rp|3}}}} | |||
| In ], Dr. Robert White, director of the Division of Neurosurgery and Brain Research Laboratory at Case Western Reserve School of Medicine, gave testimony before the House Constitution Subcommittee of the ]. He stated that, at 20 weeks' gestation, the fetus "is fully capable of experiencing pain...Without question, all of this is a dreadfully painful experience for any infant subjected to such a surgical procedure." | |||
| The report specifically identified the ] as the area of the ] responsible for processing of pain. The anterior cingulate is part of the cerebral cortex, which begins to develop in the fetus at week 26. A co-author of that report reviewed the evidence in 2020, specifically the functionality of the thalamic projections into the cortical ], and posited "an immediate and unreflective pain experience...from as early as 12 weeks."<ref>{{Cite journal|last1=Derbyshire|first1=Stuart WG|last2=Bockmann|first2=John C.|date=2020-01-01|title=Reconsidering fetal pain|url=https://jme.bmj.com/content/46/1/3|journal=Journal of Medical Ethics|language=en|volume=46|issue=1|pages=3–6|doi=10.1136/medethics-2019-105701|issn=0306-6800|pmid=31937669|doi-access=free}}</ref> | |||
| His assertions were supported by Dr. Paul Ranalli, a ] at the ], who has cited several observations to support the belief that a fetus can experience pain. These include observing a fetus "withdraw from painful stimulation", and the fact that ]s detected in adults observing pain has also been found in the blood samples of aborted fetuses. | |||
| There is a consensus among ] that the establishment of ] connections (at weeks 22–34, reliably at 29) is a critical event with regard to fetal perception of pain, as they allow peripheral sensory information to arrive at the cortex.<ref>Johnson, Martin and Everitt, Barry. '''' (Blackwell 2000), p. 235. Retrieved 2007-02-21.</ref> | |||
| In ], a working group appointed by the ] in the ] contradicted these findings, stating that "little sensory input" reaches the brain of the developing fetus before 26 weeks. "Therefore reactions to noxious stimuli cannot be interpreted as feeling or perceiving pain." | |||
| Electroencephalography indicates that the capacity for functional pain perception in premature infants does not exist before 29 or 30 weeks; a 2005 meta-analysis states that withdrawal reflexes and changes of heart rates and hormone levels in response to invasive procedures are reflexes that do not indicate fetal pain.<ref name="Lee"/> | |||
| In ], a ] of existing experiments concluded that the lack of functioning neurological pathways to a fetus' cererbral cortex before 26 weeks meant that it could not experience pain before then. The meta-study was criticised by pro-life groups who were suspicious of the prior involvement of several authors of the report. One directs an abortion clinic at ], while the lead author undertook legal work with ], an pro-choice group for six months. | |||
| Several types of evidence suggest that a fetus does not awaken during its time in the womb. Much of the literature concerning fetal pain simply extrapolates from findings and research of premature babies. The presence of such chemicals as ], ], and ]-D<sub>2</sub> in both human and animal fetuses, indicate that the fetus is both ] and ] when in the womb. These chemicals are oxidized with the newborn's first few breaths and washed out of the tissues, increasing consciousness.<ref>{{Cite journal|last1=Lagercrantz|first1=Hugo|last2=Changeux|first2=Jean-Pierre|date=March 2009|title=The Emergence of Human Consciousness: From Fetal to Neonatal Life|journal=Pediatric Research|volume=65|issue=3|pages=255–260|doi=10.1203/PDR.0b013e3181973b0d|pmid=19092726|s2cid=39391626|issn=0031-3998|quote=The delivery from the mother's womb thus causes arousal from a "resting," sleeping, state in utero. After birth, electrophysiological signs on EEG scalp recordings indicate an intense flow of novel sensory stimuli after birth… In addition, arousal is enhanced by the release from endogenous analgesia possibly caused by removal of the mentioned placental "suppressors" which in utero selectively inhibit neural activity of the fetus…. The catecholamine surge triggered by vaginal delivery may also be critical for the arousal at birth.|doi-access=free}}</ref> If the fetus is asleep throughout gestation then the possibility of fetal pain is greatly minimized,<ref name="Diesch">{{cite journal |doi=10.1016/j.brainresrev.2005.01.006 |pmid=16269314 |title=The importance of 'awareness' for understanding fetal pain |journal=Brain Research Reviews |volume=49 |issue=3 |pages=455–71 |year=2005 |last1=Mellor |first1=David J. |last2=Diesch |first2=Tamara J. |last3=Gunn |first3=Alistair J. |last4=Bennet |first4=Laura |s2cid=9833426 }}</ref><ref>{{cite news|last=Paul|first=AM|title=The First Ache|url=https://www.nytimes.com/2008/02/10/magazine/10Fetal-t.html|newspaper=The New York Times|date=2008-02-10}}</ref> although some studies found that the adenosine levels in third-trimester fetuses are only slightly greater than those in adults' blood.<ref>{{cite journal |doi=10.3109/14767058.2011.632040 |title=Is fetal pain a real evidence? |journal=] |volume=25 |issue=8 |pages=1203–8 |year=2012 |last1=Bellieni |first1=Carlo Valerio |last2=Buonocore |first2=Giuseppe |pmid=22023261 |s2cid=20578842 }}</ref> | |||
| Given the lack of irrefutable evidence, women will have to rely on their own convictions and conscience when choosing whether or not to abort their pregnancy. | |||
| === |
===Fetal anesthesia=== | ||
| Direct fetal ] is used for only a minority of prenatal surgeries.<ref>{{cite journal |doi=10.3109/14767058.2012.718392 |title=Use of fetal analgesia during prenatal surgery |journal=The Journal of Maternal-Fetal & Neonatal Medicine |volume=26 |pages=90–5 |year=2012 |last1=Bellieni |first1=Carlo V. |last2=Tei |first2=M. |last3=Stazzoni |first3=G. |last4=Bertrando |first4=S. |last5=Cornacchione |first5=S. |last6=Buonocore |first6=G. |issue=1 |pmid=22881840 |s2cid=46355976 }}</ref> | |||
| ⚫ | * Anti-abortion site presenting case for fetal pain from second month of pregnancy: |
||
| * A review of clinical evidence concerning fetal pain, JAMA. 2005;294:947-954. | |||
| Some caution that unnecessary use of fetal anesthetic may pose potential health risks to the mother. "In the context of abortion, fetal analgesia would be used solely for beneficence toward the fetus, assuming fetal pain exists. This interest must be considered in concert with maternal safety and fetal effectiveness of any proposed anesthetic or analgesic technique. For instance, general anesthesia increases abortion morbidity and mortality for women and substantially increases the cost of abortion. Although placental transfer of many opioids and sedative-hypnotics has been determined, the maternal dose required for fetal analgesia is unknown, as is the safety for women at such doses.<ref name="Lee"/> Given the maternal risk involved and the lack of evidence of any potential benefit to the fetus, administering fetal anesthesia for abortion is not recommended.<ref>{{Cite journal|last1=Society for Maternal-Fetal Medicine|last2=Society of Family Planning|last3=Norton|first3=Mary E.|last4=Cassidy|first4=Arianna|last5=Ralston|first5=Steven J.|last6=Chatterjee|first6=Debnath|last7=Farmer|first7=Diana|last8=Beasley|first8=Anitra D.|last9=Dragoman|first9=Monica|date=2022-02-01|title=Society for Maternal-Fetal Medicine Consult Series #59: The use of analgesia and anesthesia for maternal-fetal procedures|url=https://www.contraceptionjournal.org/article/S0010-7824(21)00441-8/abstract|journal=Contraception|language=English|volume=106|pages=10–15|doi=10.1016/j.contraception.2021.10.003|issn=0010-7824|pmid=34740602|s2cid=243477250|doi-access=free}}</ref> | |||
| Fetal pain legislation may make abortions more difficult to obtain, because abortion clinics lack the equipment and expertise to supply fetal anesthesia. Currently, anesthesia is administered directly to fetuses only while they are undergoing surgery.<ref name="paul">{{cite news |last=Paul |first=Annie Murphy |url=https://www.nytimes.com/2008/02/10/magazine/10Fetal-t.html |title=The First Ache |work=New York Times |date=February 10, 2008}}</ref> | |||
| Doctors for a Woman's Choice on Abortion state that the majority of surgical abortions in Britain are already performed with general anesthesia, which also affects the fetus. In a letter to the ''British Medical Journal'' in April 1997, they deemed the discussion "unhelpful to women and to the scientific debate"<ref>{{cite journal |doi=10.1136/bmj.314.7088.1201 |title=Do fetuses feel pain? |journal=BMJ |volume=314 |issue=7088 |pages=1201 |year=1997 |last1=Savage |first1=W. |last2=Wall |first2=P. D |last3=Derbyshire |first3=S. W. |pmc=2126513 |pmid=9146414 }}</ref> despite a report in the ''British Medical Journal'' that "the theoretical possibility that the fetus may feel pain (albeit much earlier than most embryologists and physiologists consider likely) with the procedure of legal abortion".<ref>{{cite journal |doi=10.1136/bmj.314.7076.302a |title=Do fetuses feel pain? |journal=BMJ |volume=314 |issue=7076 |pages=302–3 |year=1997 |last1=McCullagh |first1=P. |last2=Saunders |first2=P J |pmc=2125716 |pmid=9022510 }}</ref> Yet if mothers' general anesthesia were enough to anesthetise the fetus, all fetuses would be born sleepy after a cesarean section performed in general anesthesia, which is not the case.<ref>{{cite journal |doi=10.1097/ACO.0000000000000185 |title=General anesthesia for caesarean section |journal=Curr Opin Anesthesiol |volume=28 |issue=3 |pages=240–246 |year=2015 |last1=Devroe |first1=S.|pmid=25827280 |s2cid=38558311 }}</ref> Dr. Carlo V. Bellieni also agrees that the anesthesia that women receive for fetal surgery is not sufficient to anesthetize the fetus.<ref>Bellieni, Carlo V. (2021-05). . ''Pediatric Research'' '''89''' (7): 1612-1618. {{ISSN|1530-0447}}. {{doi|10.1038/s41390-020-01170-2}}.</ref> | |||
| ==United States legislation== | |||
| ===Federal legislation=== | |||
| In 1985, questions about fetal pain were raised during congressional hearings concerning the movie '']''.<ref>Hearing Before the Subcommittee on the Constitution of the Committee on the Judiciary, United States Senate, Ninety-Ninth Congress. (May 21, 1985). S. Hrg. 99–429; Serial No. J-99-28, pages 10 and following</ref> | |||
| In 2013 during the ], ] introduced a bill named the "]" (H.R. 1797). It passed in the House on June 18, 2013, and was received in the U.S. Senate, read twice, and referred to the Judiciary Committee.<ref>''{{Dead link|date=August 2021 |bot=InternetArchiveBot |fix-attempted=yes }}'' H.R.1797, 113th Cong., 1st Sess. (2013)</ref> | |||
| In 2004 during the ], ] introduced a bill named the "]" for the stated purpose of "ensur that women seeking an abortion are fully informed regarding the pain experienced by their unborn child", which was read twice and referred to committee.<ref>'' {{Webarchive|url=https://web.archive.org/web/20081014160455/http://thomas.loc.gov/cgi-bin/query/z?c108:S.2466: |date=2008-10-14 }},'' S.2466, 108t Cong., 2nd Sess. (2004)</ref><ref>Weisman, Jonathan. "", ''Washington Post'' 2006-12-05. Retrieved 2007-02-06.</ref> | |||
| ===State legislation=== | |||
| Subsequently, 25 states have examined similar legislation related to fetal pain and/or fetal anesthesia,<ref name="paul"/> and in 2010 ] banned abortions after 20 weeks on the basis of fetal pain.<ref>Kliff, Sarah '''' The Daily Beast Apr 13, 2010</ref> Eight states – Arkansas, Georgia, Louisiana, Minnesota, Oklahoma, Alaska, South Dakota, and Texas – have passed laws which introduced information on fetal pain in their state-issued abortion-counseling literature, which one opponent of these laws, the ] founded by Planned Parenthood, has termed "generally irrelevant" and not in line "with the current medical literature".<ref>{{cite journal |author1=Gold Rachel Benson |author2=Nash Elizabeth | year = 2007 | title = State Abortion Counseling Policies and the Fundamental Principles of Informed Consent | url = http://www.guttmacher.org/pubs/gpr/10/4/gpr100406.html | journal = Guttmacher Policy Review | volume = 10 | issue = 4 }}</ref> ], director of the Center for Bioethics at the University of Pennsylvania, said laws such as these "reduce ... the process of informed consent to the reading of a fixed script created and mandated by politicians not doctors."<ref>]. "" ''MSNBC.com'', November 30, 2005</ref> | |||
| ==See also== | |||
| * ] | |||
| ⚫ | * ] | ||
| * ] | |||
| ==References== | |||
| {{Reflist|30em}} | |||
| ==External links== | |||
| * from U.S. Congress, House Judiciary Committee, Subcommittee on the Constitution, Civil Rights, and Civil Liberties (2005). This includes testimony both for and against proposed legislation dealing with fetal pain. | |||
| * from Ontario Consultants on Religious Tolerance. This site : "We feel that all women considering an abortion should be fully informed and as free as possible from outside pressure." | |||
| ⚫ | * ] site presenting case for fetal pain from second month of pregnancy: . | ||
| * Statement of National Abortion Federation Opposing H.R. 3442, the "Unborn Child Pain Awareness Act" (2008) and . | |||
| * National Right to Life Committee's webpage of testimonies regarding fetal pain: | |||
| * by Eric Schulzke in ''Deseret News'' | |||
| {{Pain}} | |||
| {{Neuroscience}} | |||
| {{Mental processes}} | |||
| {{abortion}} | |||
| {{Pregnancy}} | |||
| {{Humandevelopment}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 11:52, 12 December 2024
Study of the different types of sensory perception of fetuses during pregnancy| This article needs attention from an expert in biology. The specific problem is: discrepancy between abortion subsection and rest of the article, and lacking scientific consensus in article overall. WikiProject Biology may be able to help recruit an expert. (August 2009) |
Prenatal perception is the study of the extent of somatosensory and other types of perception during pregnancy. In practical terms, this means the study of fetuses; none of the accepted indicators of perception are present in embryos. Studies of this type inform the abortion controversy, along with certain related pieces of legislation in countries affected by that debate. As of 2022, there is not any scientific consensus on whether a fetus can feel pain.
Prenatal hearing
Numerous studies have found evidence indicating a fetus's ability to respond to auditory stimuli. The earliest fetal response to a sound stimulus has been observed at 16 weeks' gestational age, while the auditory system is fully functional at 25–29 weeks' gestation. At 33–41 weeks' gestation, the fetus is able to distinguish its mother's voice from others.
Prenatal pain
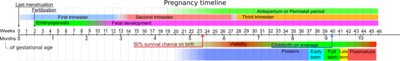
The hypothesis that human fetuses are capable of perceiving pain during the first trimester has little evidence, although fetuses at 14 weeks may respond to touch. A multidisciplinary systematic review from 2005 found limited evidence that thalamocortical pathways begin to function "around 29 to 30 weeks' gestational age", only after which a fetus is capable of feeling pain.
In March 2010, the Royal College of Obstetricians and Gynecologists submitted a report, concluding that "Current research shows that the sensory structures are not developed or specialized enough to respond to pain in a fetus of less than 24 weeks",
The neural regions and pathways that are responsible for pain experience remain under debate but it is generally accepted that pain from physical trauma requires an intact pathway from the periphery, through the spinal cord, into the thalamus and on to regions of the cerebral cortex including the primary sensory cortex (S1), the insular cortex and the anterior cingulated cortex. Fetal pain is not possible before these necessary neural pathways and structures have developed.
The report specifically identified the anterior cingulate as the area of the cerebral cortex responsible for processing of pain. The anterior cingulate is part of the cerebral cortex, which begins to develop in the fetus at week 26. A co-author of that report reviewed the evidence in 2020, specifically the functionality of the thalamic projections into the cortical subplate, and posited "an immediate and unreflective pain experience...from as early as 12 weeks."
There is a consensus among developmental neurobiologists that the establishment of thalamocortical connections (at weeks 22–34, reliably at 29) is a critical event with regard to fetal perception of pain, as they allow peripheral sensory information to arrive at the cortex.
Electroencephalography indicates that the capacity for functional pain perception in premature infants does not exist before 29 or 30 weeks; a 2005 meta-analysis states that withdrawal reflexes and changes of heart rates and hormone levels in response to invasive procedures are reflexes that do not indicate fetal pain.
Several types of evidence suggest that a fetus does not awaken during its time in the womb. Much of the literature concerning fetal pain simply extrapolates from findings and research of premature babies. The presence of such chemicals as adenosine, pregnanolone, and prostaglandin-D2 in both human and animal fetuses, indicate that the fetus is both sedated and anesthetized when in the womb. These chemicals are oxidized with the newborn's first few breaths and washed out of the tissues, increasing consciousness. If the fetus is asleep throughout gestation then the possibility of fetal pain is greatly minimized, although some studies found that the adenosine levels in third-trimester fetuses are only slightly greater than those in adults' blood.
Fetal anesthesia
Direct fetal analgesia is used for only a minority of prenatal surgeries.
Some caution that unnecessary use of fetal anesthetic may pose potential health risks to the mother. "In the context of abortion, fetal analgesia would be used solely for beneficence toward the fetus, assuming fetal pain exists. This interest must be considered in concert with maternal safety and fetal effectiveness of any proposed anesthetic or analgesic technique. For instance, general anesthesia increases abortion morbidity and mortality for women and substantially increases the cost of abortion. Although placental transfer of many opioids and sedative-hypnotics has been determined, the maternal dose required for fetal analgesia is unknown, as is the safety for women at such doses. Given the maternal risk involved and the lack of evidence of any potential benefit to the fetus, administering fetal anesthesia for abortion is not recommended.
Fetal pain legislation may make abortions more difficult to obtain, because abortion clinics lack the equipment and expertise to supply fetal anesthesia. Currently, anesthesia is administered directly to fetuses only while they are undergoing surgery.
Doctors for a Woman's Choice on Abortion state that the majority of surgical abortions in Britain are already performed with general anesthesia, which also affects the fetus. In a letter to the British Medical Journal in April 1997, they deemed the discussion "unhelpful to women and to the scientific debate" despite a report in the British Medical Journal that "the theoretical possibility that the fetus may feel pain (albeit much earlier than most embryologists and physiologists consider likely) with the procedure of legal abortion". Yet if mothers' general anesthesia were enough to anesthetise the fetus, all fetuses would be born sleepy after a cesarean section performed in general anesthesia, which is not the case. Dr. Carlo V. Bellieni also agrees that the anesthesia that women receive for fetal surgery is not sufficient to anesthetize the fetus.
United States legislation
Federal legislation
In 1985, questions about fetal pain were raised during congressional hearings concerning the movie The Silent Scream.
In 2013 during the 113th Congress, Representative Trent Franks introduced a bill named the "Pain-Capable Unborn Child Protection Act" (H.R. 1797). It passed in the House on June 18, 2013, and was received in the U.S. Senate, read twice, and referred to the Judiciary Committee.
In 2004 during the 108th Congress, Senator Sam Brownback introduced a bill named the "Unborn Child Pain Awareness Act" for the stated purpose of "ensur that women seeking an abortion are fully informed regarding the pain experienced by their unborn child", which was read twice and referred to committee.
State legislation
Subsequently, 25 states have examined similar legislation related to fetal pain and/or fetal anesthesia, and in 2010 Nebraska banned abortions after 20 weeks on the basis of fetal pain. Eight states – Arkansas, Georgia, Louisiana, Minnesota, Oklahoma, Alaska, South Dakota, and Texas – have passed laws which introduced information on fetal pain in their state-issued abortion-counseling literature, which one opponent of these laws, the Guttmacher Institute founded by Planned Parenthood, has termed "generally irrelevant" and not in line "with the current medical literature". Arthur Caplan, director of the Center for Bioethics at the University of Pennsylvania, said laws such as these "reduce ... the process of informed consent to the reading of a fixed script created and mandated by politicians not doctors."
See also
References
- Belluck, Pam (2013-09-17). "Complex Science at Issue in Politics of Fetal Pain". The New York Times. ISSN 0362-4331. Retrieved 2022-09-20.
- Levitan, Dave (2015-05-18). "Does a Fetus Feel Pain at 20 Weeks?". FactCheck.org. Retrieved 2022-09-20.
- Karni, Annie (2022-09-13). "Graham Proposes 15-Week Abortion Ban, Splitting Republicans". The New York Times. ISSN 0362-4331. Retrieved 2022-09-20.
- Graven, Stanley N.; Browne, Joy V. (December 2008). "Auditory Development in the Fetus and Infant". Newborn and Infant Nursing Reviews. 8 (4): 187–193. doi:10.1053/j.nainr.2008.10.010. ISSN 1527-3369. S2CID 6361226. Retrieved 31 May 2022.
- Kisilevsky, B.S.; Hains, S.M.J.; Brown, C.A.; Lee, C.T.; Cowperthwaite, B.; Stutzman, S.S.; Swansburg, M.L.; Lee, K.; Xie, X.; Huang, H.; Ye, H.-H.; Zhang, K.; Wang, Z. (2009). "Fetal sensitivity to properties of maternal speech and language". Infant Behavior and Development. 32 (1): 59–71. doi:10.1016/j.infbeh.2008.10.002. PMID 19058856.
- Smith, Laura S.; Dmochowski, Pawel A.; Muir, Darwin W.; Kisilevsky, Barbara S. (2007). "Estimated cardiac vagal tone predicts fetal responses to mother's and stranger's voices". Developmental Psychobiology. 49 (5): 543–7. doi:10.1002/dev.20229. PMID 17577240.
- Marx, Viola; Nagy, Emese (2015-06-08). "Fetal Behavioural Responses to Maternal Voice and Touch". PLOS ONE. 10 (6): e0129118. Bibcode:2015PLoSO..1029118M. doi:10.1371/journal.pone.0129118. ISSN 1932-6203. PMC 4460088. PMID 26053388.
- ^ Lee, Susan J.; Ralston, Henry J. Peter; Drey, Eleanor A.; Partridge, John Colin; Rosen, Mark A. (2005). "Fetal Pain". JAMA. 294 (8): 947–54. doi:10.1001/jama.294.8.947. PMID 16118385.
- Derbyshire, S. W G (2006). "Can fetuses feel pain?". BMJ. 332 (7546): 909–12. doi:10.1136/bmj.332.7546.909. PMC 1440624. PMID 16613970.
- ^ "Fetal Awareness – Review of Research and Recommendations for Practice" (PDF). Royal College of Obstetricians and Gynaecologists. March 2010. Archived from the original (PDF) on 2011-10-02. Retrieved 2019-03-27 – via Internet Archive.
- Derbyshire, Stuart WG; Bockmann, John C. (2020-01-01). "Reconsidering fetal pain". Journal of Medical Ethics. 46 (1): 3–6. doi:10.1136/medethics-2019-105701. ISSN 0306-6800. PMID 31937669.
- Johnson, Martin and Everitt, Barry. Essential reproduction (Blackwell 2000), p. 235. Retrieved 2007-02-21.
- Lagercrantz, Hugo; Changeux, Jean-Pierre (March 2009). "The Emergence of Human Consciousness: From Fetal to Neonatal Life". Pediatric Research. 65 (3): 255–260. doi:10.1203/PDR.0b013e3181973b0d. ISSN 0031-3998. PMID 19092726. S2CID 39391626.
The delivery from the mother's womb thus causes arousal from a "resting," sleeping, state in utero. After birth, electrophysiological signs on EEG scalp recordings indicate an intense flow of novel sensory stimuli after birth… In addition, arousal is enhanced by the release from endogenous analgesia possibly caused by removal of the mentioned placental "suppressors" which in utero selectively inhibit neural activity of the fetus…. The catecholamine surge triggered by vaginal delivery may also be critical for the arousal at birth.
- Mellor, David J.; Diesch, Tamara J.; Gunn, Alistair J.; Bennet, Laura (2005). "The importance of 'awareness' for understanding fetal pain". Brain Research Reviews. 49 (3): 455–71. doi:10.1016/j.brainresrev.2005.01.006. PMID 16269314. S2CID 9833426.
- Paul, AM (2008-02-10). "The First Ache". The New York Times.
- Bellieni, Carlo Valerio; Buonocore, Giuseppe (2012). "Is fetal pain a real evidence?". The Journal of Maternal-Fetal & Neonatal Medicine. 25 (8): 1203–8. doi:10.3109/14767058.2011.632040. PMID 22023261. S2CID 20578842.
- Bellieni, Carlo V.; Tei, M.; Stazzoni, G.; Bertrando, S.; Cornacchione, S.; Buonocore, G. (2012). "Use of fetal analgesia during prenatal surgery". The Journal of Maternal-Fetal & Neonatal Medicine. 26 (1): 90–5. doi:10.3109/14767058.2012.718392. PMID 22881840. S2CID 46355976.
- Society for Maternal-Fetal Medicine; Society of Family Planning; Norton, Mary E.; Cassidy, Arianna; Ralston, Steven J.; Chatterjee, Debnath; Farmer, Diana; Beasley, Anitra D.; Dragoman, Monica (2022-02-01). "Society for Maternal-Fetal Medicine Consult Series #59: The use of analgesia and anesthesia for maternal-fetal procedures". Contraception. 106: 10–15. doi:10.1016/j.contraception.2021.10.003. ISSN 0010-7824. PMID 34740602. S2CID 243477250.
- ^ Paul, Annie Murphy (February 10, 2008). "The First Ache". New York Times.
- Savage, W.; Wall, P. D; Derbyshire, S. W. (1997). "Do fetuses feel pain?". BMJ. 314 (7088): 1201. doi:10.1136/bmj.314.7088.1201. PMC 2126513. PMID 9146414.
- McCullagh, P.; Saunders, P J (1997). "Do fetuses feel pain?". BMJ. 314 (7076): 302–3. doi:10.1136/bmj.314.7076.302a. PMC 2125716. PMID 9022510.
- Devroe, S. (2015). "General anesthesia for caesarean section". Curr Opin Anesthesiol. 28 (3): 240–246. doi:10.1097/ACO.0000000000000185. PMID 25827280. S2CID 38558311.
- Bellieni, Carlo V. (2021-05). "Analgesia for fetal pain during prenatal surgery: 10 years of progress". Pediatric Research 89 (7): 1612-1618. ISSN 1530-0447. doi:10.1038/s41390-020-01170-2.
- Hearing Before the Subcommittee on the Constitution of the Committee on the Judiciary, United States Senate, Ninety-Ninth Congress. (May 21, 1985). First session on: The medical evidence concerning fetal pain. S. Hrg. 99–429; Serial No. J-99-28, pages 10 and following
- Pain-Capable Unborn Child Protection Act of 2013 H.R.1797, 113th Cong., 1st Sess. (2013)
- Unborn Child Pain Awareness Act of 2005 Archived 2008-10-14 at the Wayback Machine, S.2466, 108t Cong., 2nd Sess. (2004)
- Weisman, Jonathan. "House to Consider Abortion Anesthesia Bill", Washington Post 2006-12-05. Retrieved 2007-02-06.
- Kliff, Sarah Newly Passed 'Fetal Pain' Bill in Nebraska Is a Big Deal The Daily Beast Apr 13, 2010
- Gold Rachel Benson; Nash Elizabeth (2007). "State Abortion Counseling Policies and the Fundamental Principles of Informed Consent". Guttmacher Policy Review. 10 (4).
- Caplan, Arthur. "Abortion politics twist facts in fetal pain laws" MSNBC.com, November 30, 2005
External links
- "Oversight Hearing on Pain of the Unborn" from U.S. Congress, House Judiciary Committee, Subcommittee on the Constitution, Civil Rights, and Civil Liberties (2005). This includes testimony both for and against proposed legislation dealing with fetal pain.
- "Can a embryo or fetus feel pain? Various opinions and studies" from Ontario Consultants on Religious Tolerance. This site states: "We feel that all women considering an abortion should be fully informed and as free as possible from outside pressure."
- Anti-abortion site presenting case for fetal pain from second month of pregnancy: HTML version.
- Statement of National Abortion Federation Opposing H.R. 3442, the "Unborn Child Pain Awareness Act" (2008) PDF version and HTML version.
- National Right to Life Committee's webpage of testimonies regarding fetal pain: HTML version
- Small survivors: How the disputed science of fetal pain is reshaping abortion law by Eric Schulzke in Deseret News
| Pain | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| By region/system |
| ||||||||||
| Measurement and testing | |||||||||||
| Pathophysiology | |||||||||||
| Management | |||||||||||
| Related concepts | |||||||||||
| Mental processes | |
|---|---|
| Cognition | |
| Perception | |
| Memory | |
| Other | |
| Pregnancy and childbirth | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Planning | |||||||||
| Conception | |||||||||
| Testing | |||||||||
| Types | |||||||||
| Childbirth |
| ||||||||
| Prenatal |
| ||||||||
| Postpartum |
| ||||||||
| Obstetric history | |||||||||
| Development of the human body | |
|---|---|
| Before birth | |
| Birth and after | |
| Phases | |
| Social and legal | |
