| Revision as of 05:26, 20 September 2009 editNutriveg (talk | contribs)3,676 edits →Abstinence as an alternative to safe sex: removed text not associated with safer sex, by the intro definition← Previous edit | Latest revision as of 10:18, 17 November 2024 edit undoGreenC bot (talk | contribs)Bots2,547,812 edits Rescued 1 archive link; reformat 1 link. Wayback Medic 2.5 per WP:URLREQ#time.com | ||
| Line 1: | Line 1: | ||
| {{Short description|Ways to reduce the risk of acquiring STIs}} | |||
| ] education campaign in ]]] | |||
| {{For|the film|Safe Sex (film)}} | |||
| '''Safer sex''' is a term used to specify sexual practices and sexual behaviors that reduce the risk of contracting and transmitting ].<ref>Pan American Health Organization (PAHO)/World Association of Sexology (WAS) (2000). Promotion of Sexual | |||
| {{Use dmy dates|date=February 2019}} | |||
| Health: Recommendation for Action. Washington, DC.</ref>. The term '''safe sex''' was the first term coined for that purpose but its use has been replaced by health officials.<ref>" Assimilating safer sex: young heterosexual men's understanding of "safer sex" In: AIDS: foundations for the future, edited by Peter Aggleton, Peter Davies and Graham Hart. London, England, Taylor and Francis, 1994. :97-109. (Social Aspects of AIDS)</ref> | |||
| ]s can be used to cover the ] for safer sex during ] or ] insertion or ].]] | |||
| ]s can be used to cover the ] or ] when engaging in ] or ], respectively, for safer sex.]] | |||
| ]s ("internal" condoms) can be used by receptive partners for safer sex.]] | |||
| '''Safe sex''' is ] using methods or contraceptive devices (such as ]) to reduce the risk of transmitting or acquiring ]s (STIs), especially ].<ref>, Oxford University Press, 2009, Accessed 23 September 2009</ref> "Safe sex" is also sometimes referred to as '''safer sex''' or '''protected sex''' to indicate that some safe sex practices do not eliminate STI risks. It is also sometimes used colloquially to describe methods aimed at ] that may or may not also lower STI risks. | |||
| Promotion of safer sex became more prominent in the late 1980s as a result of the ] epidemic. Promoting safer sex is now a principal aim of ]. From the viewpoint of society, safe sex can be regarded as a ] strategy aimed at reducing risks. | |||
| The concept of "safe sex" emerged in the 1980s as a response to the global ], and possibly more specifically to the ] in the ]. Promoting safe sex is now one of the main aims of ] and STI prevention, especially reducing new HIV infections. Safe sex is regarded as a ] strategy aimed at reducing the risk of STI transmission.<ref name="Who">{{cite web| title = Global strategy for the prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission| publisher = ]| year = 2007| access-date = 26 November 2011| url = http://whqlibdoc.who.int/publications/2007/9789241563475_eng.pdf| archive-date = 23 March 2014| archive-url = https://web.archive.org/web/20140323122753/http://whqlibdoc.who.int/publications/2007/9789241563475_eng.pdf| url-status = dead}}</ref><ref name="Mercer">{{cite journal | vauthors = Chin HB, Sipe TA, Elder R, Mercer SL, Chattopadhyay SK, Jacob V, Wethington HR, Kirby D, Elliston DB, Griffith M, Chuke SO, Briss SC, Ericksen I, Galbraith JS, Herbst JH, Johnson RL, Kraft JM, Noar SM, Romero LM, Santelli J | display-authors = 6 | title = The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the Guide to Community Preventive Services | journal = American Journal of Preventive Medicine | volume = 42 | issue = 3 | pages = 272–94 | date = March 2012 | pmid = 22341164 | doi = 10.1016/j.amepre.2011.11.006 | url = http://www.ajpmonline.org/article/S0749-3797(11)00906-8/abstract | collaboration = Community Preventive Services Task Force }}</ref> | |||
| The risk reduction of safer sex is not absolute; for example the reduced risk to the receptive partner of acquiring HIV from HIV seropositive partners not wearing condoms compared to when they wear them is estimated to be about a four- to five-fold.<ref name="Vittinghoff">Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP. (1999). . Am J Epidemiol. 150(3):306-11. PMID 10430236 </ref> | |||
| Although some safe sex practices can be used as ], most forms of contraception |
Although some safe sex practices (like ]) can also be used as ] (''contraception''), most forms of contraception do not protect against STIs. Likewise, some safe sex practices, such as partner selection and low-risk sex behavior,{{Example needed|date=June 2019}} might not be effective forms of contraception. | ||
| == |
==History== | ||
| {{More citations needed|section|date=March 2018}} | |||
| Recently, and mainly within ] and the ], the use of the term ''safer sex'' rather than ''safe sex'' has gained greater use by health workers, with the realization the grounds that risk of transmission of sexually transmitted infections in various ] is a continuum rather than a simple dichotomy between risky and safe. However, in most other countries, including the ] and ], the term ''safe sex'' is still mostly used by sex educators. | |||
| Although strategies for avoiding STIs like ] and ] have existed for centuries and the term "safe sex" existed in English as early as the 1930s, the use of the term to refer to STI-risk reduction dates to the mid-1980s in the United States. It emerged in response to the ].<ref>{{cite magazine | vauthors = Stephey MJ |title=A Brief History of Safe Sex |url=http://content.time.com/time/health/article/0,8599,1866044,00.html |magazine=Time |access-date=14 September 2018 |date=11 December 2008 |quote=In the 1540s, an Italian doctor named Gabriele Fallopius — the same man who discovered and subsequently named the Fallopian tubes of the female anatomy — wrote about syphilis, advocating the use of layered linen during intercourse for more "adventurous" (read: promiscuous) men. Legendary lover Casanova wrote about his pitfalls with medieval condoms made of dried sheep gut, referring to them as "dead skins" in his memoir. Even so, condoms made of animal intestine — known as "French letters" in England and la capote anglaise (English riding coats) in France — remained popular for centuries, though always expensive and never easy to obtain, meaning the devices were often reused.}}</ref><ref name="phrases.org.uk">{{cite web |title=The meaning and origin of the expression: Safe sex |url=https://www.phrases.org.uk/meanings/309375.html |website=The Phrase Finder |access-date=14 September 2018}}</ref> | |||
| A year before the HIV virus was isolated and named, the San Francisco chapter of the ] published a small pamphlet titled ''Play Fair!'' out of concern over widespread STIs among the city's gay male population. It specifically named illnesses (Kaposi's sarcoma and pneumocystis pneumonia) that would later be understood as symptoms of advanced HIV disease (or ]). The pamphlet advocated a range of safe-sex practices, including abstinence, condoms, personal hygiene, use of personal lubricants, and STI testing/treatment. It took a casual, sex-positive approach while also emphasizing personal and social responsibility. In May 1983—the same month HIV was isolated and named in France—the New York City-based HIV/AIDS activists Richard Berkowitz and Michael Callen published similar advice in their booklet, '']''. Both publications included recommendations that are now standard advice for reducing STI (including HIV) risks.<ref>{{cite web | vauthors = Sonnabend J |title=How to have sex in an epidemic: 30th anniversary |url=https://www.poz.com/blog/how-to-have-sex-in-a |website=POZ |access-date=14 September 2018|date=17 May 2013 }}</ref><ref>{{cite journal | vauthors = Merson MH, O'Malley J, Serwadda D, Apisuk C | title = The history and challenge of HIV prevention | journal = Lancet | volume = 372 | issue = 9637 | pages = 475–88 | date = August 2008 | pmid = 18687461 | doi = 10.1016/S0140-6736(08)60884-3 | url = https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)60884-3 | s2cid = 26554589 }}</ref><ref name="Berkowitz 2">{{cite book | vauthors = Berkowitz R |title=Stayin' Alive: The Invention of Safe Sex |date=2003 |publisher=WestView |location=Boulder, CO |isbn=9780813340920}}</ref> | |||
| ==Focus on condoms and HIV control== | |||
| ] | |||
| Much attention has focused on controlling ], the ] that causes AIDS, through the use of barrier protection for the penis, specially ]. However, the HIV is a delicate virus, so protections focused on HIV may not protect against other STIs, which can also be transmitted through other areas of the body where the pathogen (virus or bacteria) has higher prevalence and resistance. Thus some ]s recommend the use of barrier protection for any sexual contact with anal or vaginal cavities, or oral stimulation of those cavities or penis.{{Citation needed|date=September 2009}} | |||
| Safe sex as a form of STI risk reduction appeared in journalism as early as 1984, in the British publication ''The Daily Intelligencer'': "The goal is to reach about 50 million people with messages about safe sex and AIDS education."<ref name="phrases.org.uk"/> | |||
| Although ''safe sex'' is used by individuals to refer to protection against both ] and HIV/AIDS or other STI transmissions, the term was born in response to the HIV/AIDS epidemic. It is believed that the term ''safe sex'' was used in the professional literature in 1984, in the content of a paper on the psychological effect that HIV/AIDS may have on gay and bisexual men.<ref>{{cite journal | vauthors = Blair TR | title = Safe Sex in the 1970s: Community Practitioners on the Eve of AIDS | journal = American Journal of Public Health | volume = 107 | issue = 6 | pages = 872–879 | date = June 2017 | pmid = 28426312 | pmc = 5425850 | doi = 10.2105/AJPH.2017.303704 }}</ref> | |||
| ==Safe sex precautions== | |||
| ] | |||
| ] print by ] depicting masturbation]] | |||
| A year later, the same term appeared in an article in ''].'' This article emphasized that most specialists advised their AIDS patients to practice safe sex. The concept included limiting the number of sexual partners, using prophylactics, avoiding bodily fluid exchange, and resisting the use of ]s that reduced inhibitions for high-risk sexual behavior.<ref name="A">{{cite web|url=http://www.csuchico.edu/cjhp/4/1/109-118-moskowitz.pdf|archive-url=https://web.archive.org/web/20060812073450/http://www.csuchico.edu/cjhp/4/1/109-118-moskowitz.pdf|url-status=dead|archive-date=12 August 2006|title=How Do Californians Define Safe Sex?|access-date=28 July 2010}}</ref> Moreover, in 1985, the first safe sex guidelines were established by the 'Coalition for Sexual Responsibilities'.{{Who|date=August 2010}} According to these guidelines, safe sex was practiced by using ]s also when engaging in ] or ].<ref>{{cite news | vauthors = Gross J |title= Homosexuals Stepping Up AIDS Education |url= https://www.nytimes.com/1985/09/22/nyregion/homosexuals-stepping-up-aids-education.html |access-date=26 September 2021 |work=The New York Times |date=22 September 1985}}</ref> | |||
| Although the term ''safe sex'' was primarily used in reference to sexual activity between men, in 1986 the concept was spread to the general population. Various programs were developed with the aim of promoting safe sex practices among college students. These programs were focused on promoting the use of the condom, a better knowledge about the partner's sexual history and limiting the number of ]s. The first book on this subject appeared in the same year. The book was entitled "Safe Sex in the Age of AIDS", and had 88 pages that described both positive and negative approaches to sexual life.{{Citation needed|date=August 2010}} Sexual behavior could be safe (]ing, ]ging, ], ], ], ], ], and use of separate ]s); possibly safe (use of condoms); or unsafe.<ref name="A"/> | |||
| ===Sex by yourself=== | |||
| Known as '']'', solitary sexual activity is relatively safe. ], the simple act of stimulating one's own genitalia, is safe{{Citation needed|date=September 2009}} so long as contact is not made with other people's discharged bodily fluids. | |||
| In 1997, specialists in this matter promoted the use of condoms as the most accessible safe sex method (besides abstinence) and they called for ] featuring condoms. During the same year, the ] in the United States issued their own "safer sex" guidelines on which condoms were listed, though two years later the ] urged ] and ] marriage, attacking the American Catholic bishops' guidelines.{{citation needed|date=October 2020}} | |||
| Modern technology does permit some activities, such as "]" and "]", that allow for partners to engage in sexual activity without being in the same room, eliminating the risks involved with exchanging bodily fluids. | |||
| A study carried out in 2006 by Californian specialists showed that the most common definitions of safe sex are condom use (68% of the interviewed subjects), abstinence (31.1% of the interviewed subjects), monogamy (28.4% of the interviewed subjects) and safe partner (18.7% of the interviewed subjects).<ref name="A"/> | |||
| The term ''safer sex'' in Canada and the United States has gained greater use by health workers, reflecting that risk of transmission of sexually transmitted infections in various ] is a ]. The term ''safe sex'' is still in common use in the United Kingdom,<ref>{{cite web|url=https://www.nhs.uk/live-well/sexual-health/|title=Sexual Health|date=26 April 2018|publisher=]|access-date=2019-04-08}}</ref> Australia and New Zealand. | |||
| "Safer sex" is thought to be a more aggressive term which may make it more obvious to individuals that any type of sexual activity carries a certain degree of risk. | |||
| The term ''safe love'' has also been used, notably by the French ] in the promotion of men's underpants incorporating a condom pocket and including the red ribbon symbol in the design, which were sold to support the charity. | |||
| ==Practices== | |||
| A range of safe-sex practices are commonly recommended by Sexual Health Educators and Public Health Agencies. Many of these practices can reduce (but not eliminate) risk of transmitting or acquiring STIs.<ref>{{cite web |title=How You Can Prevent Sexually Transmitted Diseases |date=30 March 2020 |url=https://www.cdc.gov/std/prevention/default.htm |publisher=Centers for Disease Control |access-date=2 April 2021}}</ref> | |||
| ===Phone sex/cybersex/sexting=== | |||
| Sexual activities, such as phone sex, ], and ], that do not include direct contact with the skin or bodily fluids of sexual partners, carry no STI risks and, thus, are forms of safe sex.<ref name=plannedparenthood>{{cite web |url = http://www.plannedparenthood.org/health-topics/stds-hiv-safer-sex/safer-sex-4263.htm |title = Safer Sex ("Safe Sex") |access-date = 23 September 2009 |archive-date = 29 March 2008 |archive-url = https://web.archive.org/web/20080329023107/http://www.plannedparenthood.org/health-topics/stds-hiv-safer-sex/safer-sex-4263.htm |url-status = dead }}</ref> | |||
| ===Non-penetrative sex=== | |||
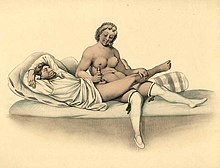
| ] of ] of the penis, ], 1840]] | |||
| === Non-penetrative sex === | |||
| ] of manual stimulation of the penis, ], 1840.]] | |||
| {{Main|Non-penetrative sex}} | {{Main|Non-penetrative sex}} | ||
| A range of sex acts called "non-penetrative sex" or "outercourse" can significantly reduce STI risks. Non-penetrative sex includes practices such as kissing, mutual masturbation, manual sex, rubbing or stroking.<ref name="LaRosa">{{cite book | vauthors = LaRosa J, Bader H, Garfield S |title=New Dimensions In Women's Health |publisher=] |year=2009 |page=91 |access-date=31 August 2013 |isbn=978-0763765927 |url=https://books.google.com/books?id=2X03PXd4JSoC&pg=PA91 |quote=Outercourse is the sharing of sexual intimacy with behaviors such as private part kissing, petting, and mutual masturbation. The advantages of outercourse include no risk of pregnancy without penile-vaginal penetration and the behaviors permit emotional bonding and closeness.}}</ref><ref name="White">{{Cite book | vauthors = White L, Duncan G, Baumle W |title=Medical Surgical Nursing: An Integrated Approach |edition=3rd |publisher=] |year=2011 |access-date=1 September 2013 |page=1161 |isbn=978-1133707141 |url=https://books.google.com/books?id=LWEJAAAAQBAJ&pg=PA1161|quote=Some people consider outercourse to mean sex play without vaginal intercourse, while others consider this to mean sex play with no penetration at all (vaginal, oral, or anal).}}</ref> According to the Health Department of Western Australia, this sexual practice may prevent pregnancy and most STIs. However, non-penetrative sex may not protect against infections that can be transmitted via skin-to-skin contact, such as ] and ].<ref>{{cite web|title=STDs (Sexually Transmitted Diseases) |url=http://www.mckinley.illinois.edu/handouts/sexually_transmitted_infections.html|access-date=23 January 2014|archive-date=2 February 2014|archive-url=https://web.archive.org/web/20140202144530/http://www.mckinley.illinois.edu/handouts/sexually_transmitted_infections.html|url-status=dead}}</ref> Mutual masturbation and manual sex carry some STI risk, especially if there is skin contact or shared bodily fluids with sexual partners, although the risks are significantly lower than many other sexual activities.<ref name=plannedparenthood/> | |||
| ===Condoms, dental dams, gloves=== | |||
| A range of sex acts,{{Which?|date=September 2009}} sometimes called "outercourse", can be enjoyed by lovers with significantly reduced risks of infection{{Citation needed|date=September 2009}} and pregnancy. U.S. President ]'s surgeon general, Dr. ], tried to encourage the use of these practices among young people, but her position encountered opposition from a number of outlets, including the White House itself, and resulted in her being fired by President Clinton in December 1994.<ref>{{cite web|url=http://www.time.com/time/magazine/article/0,9171,982008,00.html|title=Getting Out the Wrecking Ball|publisher=Time|date=1994-12-19|accessdate=2009-03-08}}</ref><ref></ref><ref>{{cite web|url=http://query.nytimes.com/gst/fullpage.html?res=9C02E0D81038F935A35752C1A960958260|title=President Clinton Makes a Celebratory Return to His Starting Point in Arkansas|publisher=New York Times|date=1996-11-06|accessdate=2009-03-08}}</ref> | |||
| {{anchor|Barrier protection}} | |||
| Barriers, such as condoms, dental dams, and medical gloves can prevent contact with body fluids (such as ], ], ], rectal mucus), and other means of transmitting STIs (like skin, hair and shared objects) during sexual activity.<ref>{{cite journal | vauthors = Gil-Llario MD, Morell-Mengual V, García-Barba M, Nebot-García JE, Ballester-Arnal R | title = HIV and STI Prevention Among Spanish Women Who have Sex with Women: Factors Associated with Dental Dam and Condom Use | journal = AIDS and Behavior | volume = 27 | issue = 1 | pages = 161–170 | date = January 2023 | pmid = 35788924 | pmc = 9852118 | doi = 10.1007/s10461-022-03752-z }}</ref><ref>{{cite journal | vauthors = Claure I, Anderson D, Klapperich CM, Kuohung W, Wong JY | title = Biomaterials and Contraception: Promises and Pitfalls | journal = Annals of Biomedical Engineering | volume = 48 | issue = 7 | pages = 2113–2131 | date = July 2020 | pmid = 31701311 | doi = 10.1007/s10439-019-02402-1 | s2cid = 254185613 | pmc = 7202983 }}</ref> | |||
| ] | |||
| === Barrier protection === | |||
| * External ]s can be used to cover the penis, hands, fingers, or other body parts during sexual penetration or ].<ref name="Corinna" /> They are most frequently made of ], and can also be made out of synthetic materials including ] and ]. | |||
| Various protective devices are used to avoid contact with ], ], ] or other contaminant agents (like skin, hair and shared objects) during sexual activity. | |||
| * Internal condoms (also called ]s) are inserted into the ] or ] prior to sexual penetration. These condoms are made of either polyurethane or ]. If external and internal condoms are used at the same time, they may break due to friction between the materials during sexual activity. | |||
| Practice of ] using this devices is called '''protected sex'''. | |||
| * A ] (originally used in dentistry) is a sheet of latex typically used for protection between the mouth and the ] or anus when engaging in oral sex. | |||
| * ]s and ]s made out of latex, vinyl, ], or polyurethane can cover hands or fingers during ] or may be used as a makeshift dental dam during oral sex.<ref name="Corinna">{{cite book |vauthors=Corinna H |title=S.E.X.: The All-You-Need-to-Know Sexuality Guide to Get You Through Your Teens and Twenties |date=2016 |publisher=Da Capo Lifelong Press |location=New York |isbn=978-0738218847}}</ref><ref name="Moon">{{cite book | vauthors = Moon A |title=Girl Sex 101 |date=2018 |publisher=Lunatic Ink |isbn=978-0983830900}}</ref> | |||
| * Condoms, dental dams, and gloves can also be used to cover ] such as ]s during sexual stimulation or penetration.<ref name="Corinna" /><ref name="Moon" /> If a sex toy is to be used in more than one orifice or partner, a condom/dental dam/glove can be used over it and changed when the toy is moved. | |||
| Oil-based ] can break down the structure of latex condoms, dental dams or gloves, reducing their effectiveness for STI protection.<ref>{{cite book | vauthors = Corinna H |title=S.E.X.: The All-You-Need-to-Know Sexuality Guide to Get You Through Your Teens and Twenties |date=2016 |publisher=Da Capo Lifelong Press |location=New York |isbn=978-0738218847 |page=294 |edition=2nd}}</ref> | |||
| ]]] | |||
| *]s cover the penis during sexual activity. They are most frequently made of ], but can also be made out of ]<!-- removed animal intestine condoms from the list, because they "have larger microscopic openings and may allow the organisms that cause STDs to pass through and infect either partner". Also just you don't need to say "for those with latex allergies". If someone has a latex allergy they will naturally use polyurethane and not latex... -->. Polyurethane is thought to be a safe material for use in condoms, since it is nonporous and viruses cannot pass through it. However, there is less research on its effectiveness than there is on latex. <!-- the same reasoning as the above statement. --> | |||
| *]s are inserted into the ] prior to intercourse. They may also be used for ], although they are less effective.{{Citation needed|date=September 2009}} | |||
| *A ] (originally used in dentistry) is a sheet of latex used for protection when engaging in ]. It is typically used as a barrier between the mouth and the ] during ] or between the mouth and the anus during ]. | |||
| *] made out of latex, vinyl, ], or polyurethane may be used as an makeshift dental dam during oral sex, or to protect the hands during sexual stimulation, like in ]. Hands may have invisible cuts on them that may admit pathogens or, more usually, serve as vehicle for contamination of other body part or partner. | |||
| *Another way to protect against pathogen transmission is the use of protected or properly cleaned ]s or other ]s. If a sex toy is to be used in more than one orifice or partner, a condom can be used over it and changed when the toy is moved. | |||
| While use of external condoms can reduce STI risks during sexual activity, they are not 100% effective. One study has suggested condoms might reduce HIV transmission by 85% to 95%; effectiveness beyond 95% was deemed unlikely because of slippage, breakage, and incorrect use.<ref name="Varghese">{{cite journal |vauthors=Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW |title=Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use |journal=Sexually Transmitted Diseases |volume=29 |issue=1 |pages=38–43 |date=January 2002 |pmid=11773877 |doi=10.1097/00007435-200201000-00007 |s2cid=45262002 |url=http://ww2.aegis.org/files/AskDoc_refs/varghese2002-29-1.pdf |url-status=dead |archive-url=https://web.archive.org/web/20110724224853/http://ww2.aegis.org/files/AskDoc_refs/varghese2002-29-1.pdf |archive-date=24 July 2011}}</ref> It also said, "In practice, inconsistent use may reduce the overall effectiveness of condoms to as low as 60–70%".<ref name="Varghese"/><sup>p. 40.</sup> | |||
| If any latex barrier is being used, oil-based ] should not be used, as this can break down the structure of the latex and remove the protection it provides. | |||
| ===Pre-exposure prophylaxis (PrEP)=== | |||
| Condoms (male or female) may be used to protect against STDs, and used with other forms of contraception to improve contraceptive effectiveness. For example, simultaneously using both the male condom and spermicide (applied separately, not pre-lubricated) is believed to reduce perfect-use pregnancy rates to those seen among implant users.<ref>{{cite journal |author=Kestelman P, Trussell J |title=Efficacy of the simultaneous use of condoms and spermicides. | journal = Fam Plann Perspect | volume = 23 | issue = 5 |pages=226–7, 232 |year=1991| pmid = 1743276 | doi = 10.2307/2135759}}</ref> However, two condoms should not be used simultaneously (male condom on top of male condom, or male condom inside female condom), since this increases the chance of condom failure.<ref>{{cite web |title=Does using two condoms provide more protection than using just one condom? |work=Condoms and Dental Dams |publisher=New York University Student Health Center |url=http://www.nyu.edu/shc/promotion/condoms.dental.dams.html |accessdate=2008-06-30}}</ref><ref>{{cite web |title=Are two condoms better than one? |work=] |publisher=Columbia University |date=2005-01-21 |url=http://www.goaskalice.columbia.edu/1139.html |accessdate=2008-06-30}}</ref> | |||
| {{Main|Pre-exposure prophylaxis}} | |||
| ] (often abbreviated as ''PrEP'') is the use of prescription drugs by those who do not have HIV to prevent HIV infection. PrEP drugs are taken ''prior'' to HIV exposure to prevent the transmission of the virus, usually between sexual partners. PrEP drugs do not prevent other STI infections or pregnancy.<ref>{{Cite journal |last1=Kumar |first1=Sagar |last2=Haderxhanaj |first2=Laura T. |last3=Spicknall |first3=Ian H. |date=June 2021 |title=Reviewing PrEP's Effect on STI Incidence Among Men Who Have sex with Men-Balancing Increased STI Screening and Potential Behavioral Sexual Risk Compensation |journal=AIDS and Behavior |volume=25 |issue=6 |pages=1810–1818 |doi=10.1007/s10461-020-03110-x |issn=1573-3254 |pmc=8085068 |pmid=33242186}}</ref> | |||
| As of 2018, the most-widely approved form of ''PrEP'' combines two drugs (tenofovir and emtricitabine) in one pill. That drug combination is sold under the brand name ] by Gilead Sciences. It is also sold in generic formulations worldwide. Other drugs and modalities are being studied for use as PrEP.<ref>{{Cite web |title=Pre-exposure Prophylaxis (PrEP) to Reduce HIV Risk | work = National Institute of Allergy and Infectious Diseases | date = 10 December 2020 |url=https://www.niaid.nih.gov/diseases-conditions/pre-exposure-prophylaxis-prep |access-date=2022-06-27 |language=en}}</ref><ref>{{cite journal | vauthors = Beymer MR, Holloway IW, Pulsipher C, Landovitz RJ | title = Current and Future PrEP Medications and Modalities: On-demand, Injectables, and Topicals | journal = Current HIV/AIDS Reports | volume = 16 | issue = 4 | pages = 349–358 | date = August 2019 | pmid = 31222499 | pmc = 6719717 | doi = 10.1007/s11904-019-00450-9 }}</ref> | |||
| Proper use of barriers, such as condoms, depends on the cleanness of surfaces of the barrier, care should be taken to avoid contamination of the barrier when handling it and to control contamination from used surfaces of a barrier. | |||
| Different countries have approved different protocols for using the tenofovir/emtricitabine-combination drug as ''PrEP''. That two-drug combination has been shown to prevent HIV infection in different populations when taken daily, intermittently, and on demand. Numerous studies have found the tenofovir/emtricitabine combination to be over 90% effective at preventing HIV transmission between sexual partners.<ref>{{cite web |url=https://www.cdc.gov/hiv/risk/prep/ |title=Pre-Exposure Prophylaxis (PrEP) |date=19 September 2016 |publisher=Centers for Disease Control and Prevention |access-date=14 March 2017}}</ref> AVAC has developed a tool to track trends in PrEP uptake across the globe.<ref>{{Cite web |title=PrEP {{!}} AVAC |url=https://avac.org/prevention-option/prep/ |access-date=2024-02-07 |website=avac.org}}</ref> | |||
| === Other Precautions === | |||
| Acknowledging that it is usually impossible to have entirely risk-free sex with another person, proponents of safe sex recommend that some of the following methods be used to minimize the risks of STD transmission and unwanted pregnancy. | |||
| * ] is now backed by the ] as a preventative measure against HIV. African studies have found that circumcision can reduce the transmission rate of HIV by up to 60%<ref>{{cite web |url=http://news.bbc.co.uk/2/hi/health/6502855.stm |title=WHO agrees HIV circumcision plan |accessdate=2008-07-12 |work=BBC World News |publisher=BBC |date=2007-03-03 }}</ref>. Some advocacy groups dispute these findings.<ref></ref><ref></ref> | |||
| * Periodic STD testing has been used to reduce STD infections in Cuba and among pornographic film actors. Cuba implemented a program of mandatory testing and quarantine early in the AIDS epidemic.<ref>{{cite web |url=http://www.thebody.com/content/art32967.html |title=Cuba fights AIDS in its Own Way |accessdate=2009-06-13 |work=The Body |publisher=The Body|date=2009-06-13 }}</ref> In the US pornographic film industry in the US, many production companies will not hire actors without tests for Chlamydia, HIV and Gonorrhea that are no more than 30 days old-and tests for other STD's no more than 6 months old. AIM Medical foundation claims that program of testing has reduced the incidence of STD infection to 20% of that of the general population. | |||
| * ] and ] can reduce ] of HIV on devices, such as barrier contraceptives<ref name=soap> | |||
| {{cite journal | |||
| |title=Virucidal Efficacy of Soap and Water against Human Immunodeficiency Virus in Genital Secretions | |||
| |author=Li, J. Z. | |||
| |coauthors=E. C. Mack, and J. A. Levy. | |||
| |year=2003 | |||
| |pmid=14506048 | |||
| |pmc=201149 | |||
| |volume=47 | |||
| |issue=10 | |||
| |doi=10.1128/AAC.47.10.3321-3322.2003 | |||
| |pages=3321–3322 | |||
| |journal=Antimicrobial Agents and Chemotherapy | |||
| }}</ref>. Douching with soap and water should be avoided because it has not been studied and by disrupting the vaginal flora it might increase risk of infection.<ref name=soap /> | |||
| * ] , practiced faithfully, is very safe (as far as STDs are concerned) when all partners are non-infected. However, many monogamous people have been infected with sexually transmitted diseases by partners who are ], have used injection drugs, or were infected by previous sexual partners. | |||
| * For those who are not monogamous, reducing the number of one's sexual partners, particularly anonymous sexual partners, may also reduce one's potential exposure to STDs. Similarly, one may restrict one's sexual contact to a community of trusted individuals - this is the approach taken by some ]s . | |||
| *When selecting a sexual parter, some characteristics can increase the risks for contracting sexually transmitted diseases.<ref name="partner">{{cite doi|10.1097/OLQ.0b013e3181901e32}}</ref> These include:- an age discordance of more than five years<ref name="partner"/>; having STD in the past year<ref name="partner"/>; problems with marijuana or alcohol<ref name="partner"/>; having had sex with other people in the past year<ref name="partner"/>. | |||
| * ] with one's sexual partner(s) makes for greater safety. Before initiating sexual activities, partners may discuss what activities they will and will not engage in, and what precautions they will take. This can reduce the chance of risky decisions being made "in the heat of passion". | |||
| * Refraining from the use of ]s, including ], before and during sexual activity can protect against associated risks such as lowered inhibitions, decreased immune response, impaired judgment, and loss of consciousness. | |||
| * If a person is sexually active with a number of partners, it is important that they get regular ] check-ups from a doctor. Anyone noticing unusual symptoms should get medical advice quickly as ] is sometimes ] or symptoms will have a nonspecific nature and can even be misdiagnosed.<ref name=Kahn>{{cite journal | |||
| | author=Kahn, J. O. and Walker, B. D. | title=Acute Human Immunodeficiency Virus type 1 infection | journal=N. Engl. J. Med. | year=1998 | pages=33–39 | volume=331 | issue=1 | pmid=9647878 | doi=10.1056/NEJM199807023390107}}</ref><ref name="pmid11187417">{{cite journal |author=Daar ES, Little S, Pitt J, ''et al.'' |title=Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network |journal=Ann. Intern. Med. |volume=134 |issue=1 |pages=25–9 |year=2001 |pmid=11187417 |doi=}}</ref> | |||
| === |
===Treatment as prevention=== | ||
| {{Main|Treatment as prevention}} | |||
| Treatment as Prevention (often abbreviated as ''TasP'') is the practice of testing for and treating HIV infection as a way to prevent further spread of the virus. Those having knowledge of their HIV-positive status can use safe-sex practices to protect themselves and their partners (such as using condoms, sero-sorting partners, or choosing less-risky sexual activities). And, because HIV-positive people with durably suppressed or undetectable amounts of HIV in their blood ''cannot transmit HIV to sexual partners'', sexual activity with HIV-positive partners on effective treatment is a form of safe sex (to prevent HIV infection). This fact has given rise to the concept of "U=U" ("Undetectable = Untransmittable").<ref>{{cite web |url=https://www.preventionaccess.org/ |title=U=U|date=2017|publisher=Prevention Access Campaign|access-date=11 September 2018}}</ref> | |||
| ===Other forms of safe sex=== | |||
| While the use of condoms can reduce HIV transmission, it does not do so completely. One study has suggested it might be around by a factor of 85% to 95% and questioned that effectiveness beyond 95% would be unlikely because of slippage, breakage, and incorrect use.<ref name="Varghese">Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW. (2002). . Sex Transm Dis. 29(1):38-43. PMID 11773877</ref> It also noted "In practice, inconsistent use may reduce the overall effectiveness of condoms to as low as 60–70%".<ref name="Varghese"/><sup>p. 40.</sup> | |||
| Other methods proven effective at reducing STI risks during sexual activity are: | |||
| * ] against certain sexually-transmitted viruses. The most common vaccines protect against ] and ], which can cause ], ], ], and ]. Immunization before initiation of sexual activity increases effectiveness of these vaccines. HPV vaccines are recommended for all teen girls and women as well as teen boys and men through age 26 and 21 respectively.<ref>{{Cite web|url=https://www.cdc.gov/std/prevention/default.htm|title=Prevention - STD Information from CDC|date=2019-05-28|website=www.cdc.gov|language=en-us|access-date=2019-08-05}}</ref> | |||
| * Limiting numbers of sexual partners, particularly casual sexual partners, or restricting sexual activity to those who know and share their STI status, can also reduce STI risks. ] or ], practiced faithfully, is very safe (as far as STIs are concerned) when all partners are non-infected. However, many monogamous people have been infected with sexually transmitted infections by partners who are ], have used injection drugs, or were infected by previous sexual partners. The same risks apply to polyfidelitous people, who face higher risks depending on how many people are in the polyfidelitous group. | |||
| * ] with sexual partners about sexual history and STI status, preferred safe sex practices, and acceptable risks for partnered sexual activities. | |||
| * Engaging in less-risky sexual activities. In general, solo sexual activities are less risky than partnered activities. Sexual penetration of orifices (mouth, vagina, anus) and sharing body fluids (such as semen, blood, vaginal fluids, and rectal mucus) between sexual partners carry the most risk for STIs. | |||
| * Regular STI testing and treatment, especially by those who are sexually active with more than one casual sexual partner.<ref name=Kahn>{{cite journal | vauthors = Kahn JO, Walker BD | title = Acute human immunodeficiency virus type 1 infection | journal = The New England Journal of Medicine | volume = 339 | issue = 1 | pages = 33–9 | date = July 1998 | pmid = 9647878 | doi = 10.1056/NEJM199807023390107 }}</ref><ref name="pmid11187417">{{cite journal | vauthors = Daar ES, Little S, Pitt J, Santangelo J, Ho P, Harawa N, Kerndt P, Glorgi JV, Bai J, Gaut P, Richman DD, Mandel S, Nichols S | display-authors = 6 | title = Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network | journal = Annals of Internal Medicine | volume = 134 | issue = 1 | pages = 25–9 | date = January 2001 | pmid = 11187417 | doi = 10.7326/0003-4819-134-1-200101020-00010 | s2cid = 34714025 | first14 = Network }}</ref> It is possible to attain and show proof of STD-free-verification through ] and websites.<ref>{{cite web| url = https://www.sheknows.com/health-and-wellness/articles/985207/app-for-finding-out-std-status/| title = Do you know his STD status? There's an app for that| date = 3 April 2013}}</ref><ref>{{cite web| url = https://medcitynews.com/2016/01/tinder-healthvana-std/| title = Tinder adds link to healthvana for STD-checking purposes| date = 22 January 2016}}</ref> | |||
| * ]. Some research suggests that circumcising (removing) the foreskin of the penis can reduce the risk of contracting HIV.<ref>{{cite web | title = Circumcision (male) | publisher = Mayo Clinic | url = https://www.mayoclinic.org/tests-procedures/circumcision/about/pac-20393550 | access-date = 10 May 2020}}</ref><ref>{{cite news |url=http://news.bbc.co.uk/2/hi/health/6502855.stm |title=WHO agrees HIV circumcision plan |access-date=12 July 2008 |work=BBC World News |publisher=BBC |date=3 March 2007 }}</ref> Some advocacy groups dispute these findings.<ref>{{cite web|url=http://www.circumstitions.com/HIV-SA.html|title=Circumcision and HIV - the Randomised Controlled Trials|website=www.circumstitions.com}}</ref><ref>{{cite web|url=http://mgmbill.org/aids.htm|title=Circumcision and AIDS<!-- Bot generated title -->|url-status=dead|archive-url=https://web.archive.org/web/20080723220755/http://mgmbill.org/aids.htm|archive-date=23 July 2008}}</ref> | |||
| ==Ineffective methods== | |||
| The risk of the receptive partner acquiring HIV from HIV seropositive partners not wearing condoms is 0.82% and from those wearing condoms is 0.18%, a four- to five-fold reduction.<ref name="Vittinghoff"/> Where the partner's HIV status is unknown, "Estimated per-contact risk of protected receptive anal intercourse with HIV-positive and unknown serostatus partners, including episodes in which condoms failed, was two thirds the risk of unprotected receptive anal intercourse with the comparable set of partners."<ref name="Vittinghoff"/><sup>p. 310.</sup> | |||
| Most methods of contraception are not effective at preventing the spread of ]s. This includes ], ], ], ], ]s and many non-barrier methods of pregnancy prevention. However, ], when used correctly, significantly reduces the risks of STI transmission and unwanted pregnancy.<ref>{{Cite web |title=Condom Effectiveness |author=Centers for Disease Control and Prevention |work=cdc.gov |date=2 February 2022 |access-date=13 April 2022 |url= https://www.cdc.gov/condomeffectiveness/index.html |quote=Correctly using male (also called external) condoms and other barriers like female (also called internal) condoms and dental dams, every time, can reduce (though not eliminate) the risk of sexually transmitted diseases (STDs), including human immunodeficiency virus (HIV) and viral hepatitis. They can also provide protection against other diseases that may be transmitted through sex like Zika and Ebola. Using male (external) and female (internal) condoms correctly, every time, can also help prevent pregnancy. }}</ref> | |||
| The ] ] has been claimed to reduce the likelihood of STI transmission. However, a technical report from 2001<ref name=":0">{{Cite web|url=http://apps.who.int/iris/bitstream/10665/68510/1/WHO_RHR_03.08.pdf|title=Technical Consultation on Nonoxynol-9 |date=October 2001|website=WHO|access-date=10 March 2018}}</ref> by the ] has shown that nonoxynol-9 is an irritant and can produce tiny tears in mucous membranes, which may increase the risk of transmission by offering ]s more easy points of entry into the system. They reported that nonoxynol-9 lubricant do not have enough spermicide to increase contraceptive effectiveness cautioned they should not be promoted. There is no evidence that spermicidal condoms are better at preventing STD transmission compared to condoms that do not have spermicide. If used properly, spermicidal condoms can prevent pregnancy, but there is still an increased risk that nonoxynyl-9 can irritate the skin, making it more susceptible for infections.<ref name=":0" /><ref>{{Cite web|url=https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/safer-sex/how-do-i-make-sex-safer|title=How Do I Make Sex Safer? {{!}} Common Questions and Answers|website=www.plannedparenthood.org|language=en|access-date=2019-08-02}}</ref> | |||
| == Ineffective methods == | |||
| Note that most methods of contraception<!-- removed (birth control) because unless I'm wrong - which I may well be - contraception is a specific type of birth control barrier methods not falling under this category --> other than the barrier methods mentioned above are ''not'' effective at preventing the spread of STDs. This includes the "]". | |||
| The use of a ] or ] provides some women with better protection against certain sexually transmitted infections,<ref name="TechInd">{{cite news |url= http://findarticles.com/p/articles/mi_m1200/is_n19_v141/ai_12248743/ |title=Diaphragm and sponge protect against STDs - sexually transmitted diseases |access-date=5 April 2010 |work=Science News | vauthors = Fackelmann KA |year=1992 |url-status=dead |archive-url= https://web.archive.org/web/20100404015828/http://findarticles.com/p/articles/mi_m1200/is_n19_v141/ai_12248743/ |archive-date=4 April 2010 }}</ref> but they are not effective for all STIs. | |||
| The ] ] has been claimed to reduce the likelihood of STD transmission. However a recent study by the ] <ref></ref> has shown that Nonoxynol-9 is an irritant and can produce tiny tears in mucous membranes, which may increase the risk of transmission by offering ] more easy points of entry into the system. Condoms with Nonoxynol-9 lubricant do not have enough spermicide to increase contraceptive effectiveness and are not to be promoted.{{Citation needed|date=August 2009}} | |||
| Hormonal methods of preventing pregnancy (such as oral contraceptives , depoprogesterone, hormonal IUDs, the vaginal ring, and the patch) offer no protection against STIs. The copper intrauterine device and the hormonal intrauterine device provide an up to 99% protection against pregnancies but no protection against STIs. Women with copper intrauterine device ''may'' be subject to greater risk of infection from bacterial infectious such as ] or ], although this is debated.<ref>{{cite journal | vauthors = Hubacher D | title = Intrauterine devices & infection: review of the literature | journal = The Indian Journal of Medical Research | volume = 140 | issue = Suppl 1 | pages = S53-7 | date = November 2014 | pmid = 25673543 | pmc = 4345753 }}</ref> | |||
| ] (or "pulling out"), in which the penis is removed from the vagina, ], or ] before ], is not safe sex and can result in STD transmission. This is because {{fact}} of the formation of ], a fluid that oozes from the ] before actual ejaculation. Pre-ejaculate ''can'' contain pathogens such as HIV.<ref name="HIV study">. ''Contraceptive Technology Update''. Volume 14, Number 10, October 1993, pp.154-6.</ref><!-- | |||
| --><ref>Zukerman, Z. et al. ''Journal of Assisted Reproduction and Genetics''. Volume 20, Number 4, April 2003, pp. 157-159(3).</ref> | |||
| ] (or "pulling out"), in which the penis is removed from the ] or ] before ], may reduce transmission of STIs but still carries significant risk. This is because ], a fluid that oozes from the penile ] before ejaculation, may contain STI pathogens. Additionally, the microbes responsible for some diseases, including ]s and ], can be transmitted through skin-to-skin or mucous membrane contact.<ref>{{Cite web |title=Safe Sex: Better Health Channel |url=https://www.betterhealth.vic.gov.au/health/healthyliving/safe-sex |access-date=7 April 2024 |website=better health.vic.gov.au}}</ref> | |||
| ==Dangers of anal sex== | |||
| Unprotected anal sex is a high risk activity regardless of sexual orientation. Research suggests that although gay men are more likely to engage in anal sex, heterosexual couples are more likely not to use condoms when doing so.<ref>"Gay men's dream: A 'magic' lube: Researchers discuss rectal microbicide development at NIAID workshop", Bob Roehr, (June 15, 2001) ''Bay Area Reporter'' </ref> | |||
| ==Anal sex== | |||
| Anal sex is a higer risk activity than vaginal, because very thin tissues of anus and ] can be easily damaged; this includes by the use of anal ]. Even slight injuries can become "open gates" for various bacteria and viruses, including HIV. This implies that anal sex does require some certain safety measures. First of all, any partners who practice anal sex should be aware of the necessity of using a condom. The condom must be put on properly, otherwise it does not provide reliable protection. Users should keep in mind that oil-based lubricants damage latex. For this reason water-based ]s should be used for anal sex. Those who have allergy to latex should consider use of non-latex condoms, for instance polyurethane condoms that are compatible with both oil-based and water-based lubricants. | |||
| Unprotected ] is considered a high-risk sexual activity because the thin tissues of the anus and ] can be easily damaged.<ref name="Dean and Delvin">{{cite web|title=Anal sex|vauthors=Dean J, Delvin D|publisher=Netdoctor.co.uk|access-date=29 April 2010|url=http://www.netdoctor.co.uk/sexandrelationships/analsex.htm|archive-date=7 May 2010|archive-url=https://web.archive.org/web/20100507161735/http://www.netdoctor.co.uk/sexandrelationships/analsex.htm|url-status=dead}}</ref><ref>{{cite journal | vauthors = Voeller B | title = AIDS and heterosexual anal intercourse | journal = Archives of Sexual Behavior | volume = 20 | issue = 3 | pages = 233–276 | date = June 1991 | pmid = 2059146 | doi = 10.1007/BF01541846 | s2cid = 13387947 }} as cited in {{cite journal | vauthors = Leichliter JS | title = Heterosexual anal sex: part of an expanding sexual repertoire? | journal = Sexually Transmitted Diseases | volume = 35 | issue = 11 | pages = 910–1 | date = November 2008 | pmid = 18813143 | doi = 10.1097/OLQ.0b013e31818af12f | s2cid = 27348658 | doi-access = free }}</ref> Slight injuries can allow the passage of bacteria and viruses, including HIV. This includes penetration of the anus by fingers, hands, or sex ] such as ]s. Also, condoms may be more likely to break during anal sex than during vaginal sex, increasing the risk of STI transmission.<ref>{{cite web | title = Can I get HIV from anal sex? | url = http://aids.about.com/od/technicalquestions/f/oral.htm | access-date = 19 August 2011 | archive-date = 3 October 2011 | archive-url = https://web.archive.org/web/20111003004931/http://aids.about.com/od/technicalquestions/f/oral.htm | url-status = dead }}</ref> | |||
| The main risk that individuals are exposed to when performing anal sex is the transmission of ]. Other possible infections include ], ] and ]; ]s like '']''; and bacterial infections such as ''].''<ref>{{Cite web|url=https://www.cdc.gov/hiv/risk/analsex.html|title=Anal Sex |website=CDC|access-date=10 March 2018}}</ref> | |||
| Condoms should also be used with sex toys. By putting a condom on the sex toy, the user provides better hygiene and prevents transmission of infections if the sex toy is shared. However, the condom must be replaced when switching between partners. Cleaning of anal sex toys is also a very important matter as many anal sex toys are made of porous materials. Pores retain viruses and bacteria. For this reason users should clean anal toys (plugs, anal vibrators) thoroughly, preferably with use of special sex toy cleaners. Glass sex toys are more preferred for sexual uses because of their non-porous nature and ability to be sterilized between uses. | |||
| Anal sex should be avoided by couples in which one of the partners has been diagnosed with an STI until the treatment has proven to be effective. | |||
| ==Abstinence as an alternative== | |||
| Refraining from any sexual contact with another individual is the surest way to avoid the risk of sexually contracting ].<ref name="CDC condoms"/> In that context complete ],<ref name="CDC condoms">{{cite web|url=http://www.cdc.gov/condomeffectiveness/latex.htm|title=Condoms and STDs: Fact Sheet for Public Health Personnel|date=July 15, 2009|publisher=Centers for Disease Control and Prevention|accessdate=2009-09-13}}</ref> like ], is one of those practices that fit that definition. | |||
| In order to make anal sex safer, the couple must ensure that the anal area is clean and the bowel empty and the partner on whom anal penetration occurs should be able to relax. Regardless of whether anal penetration occurs by using a finger or the penis, the condom is the best barrier method to prevent transmission of STI. ]s should not be used as they can increase the risk of HIV infection<ref>{{cite journal |vauthors=Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH |title=The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides | journal=AIDS and Behavior |volume=12 |issue=6 |pages=860–866 |date=November 2008 |pmid=17705033 |pmc=2953367 |doi=10.1007/s10461-007-9301-0 }}</ref> and ] ].<ref>{{cite journal |vauthors=de Vries HJ, van der Bij AK, Fennema JS, Smit C, de Wolf F, Prins M, Coutinho RA, Morré SA |display-authors=6 |title=Lymphogranuloma venereum proctitis in men who have sex with men is associated with anal enema use and high-risk behavior |journal=Sexually Transmitted Diseases |volume=35 |issue=2 |pages=203–208 |date=February 2008 |pmid=18091565 |doi=10.1097/OLQ.0b013e31815abb08 |s2cid=2065170 |url=https://dare.uva.nl/personal/pure/en/publications/lymphogranuloma-venereum-proctitis-in-men-who-have-sex-with-men-is-associated-with-anal-enema-use-and-highrisk-behavior(6b9b21d8-9369-4f55-a0e5-c6804db29083).html|doi-access=free }}</ref> | |||
| However, sexual abstinence is seen by critics as repressive, it is difficult to maintain for prolonged periods of time and practitioners may restrict the abstinence only to specific sexual practices they see associated with increased STD risk or with other purposes of sexual abstinence, like ] and some definitions of ]. | |||
| Since the rectum can be easily damaged, the use of lubricants is highly recommended even when penetration occurs by using the finger. Especially for beginners, using a condom on the finger is both a protection measure against STI and a lubricant source. Most condoms are lubricated and they allow less painful and easier penetration. Oil-based lubricants damage latex and should not be used with condoms;<ref>{{cite journal |vauthors=Steiner M, Piedrahita C, Glover L, Joanis C, Spruyt A, Foldesy R |title=The impact of lubricants on latex condoms during vaginal intercourse |journal=International Journal of STD & AIDS |volume=5 |issue=1 |pages=29–36 |year=1993 |pmid=8142525 |doi=10.1177/095646249400500108 |url=http://pdf.usaid.gov/pdf_docs/PNACA620.pdf |s2cid=9271973 |citeseerx=10.1.1.574.1501}}</ref> water-based and silicone-based ]s are available instead. Non-latex condoms are available for people who are ] made out of ] or ].<ref>{{Cite web|title=Condoms|date=21 December 2017 |website=NHS |url=https://www.nhs.uk/conditions/contraception/male-condoms/ |access-date=10 March 2018}}</ref> Polyurethane condoms can safely be used with oil-based lubricant.<ref>{{Cite web |title=Clinical Prevention Guidance - 2015 STD Treatment Guidelines|date=10 October 2017 |website=www.cdc.gov |url=https://www.cdc.gov/std/tg2015/clinical.htm|access-date=10 March 2018}}</ref> The "]" may also be used effectively by the anal receiving partner. | |||
| ==See also== | |||
| * ] | |||
| Anal stimulation with a sex toy requires similar safety measures to anal penetration with a penis, in this case using a condom on the sex toy in a similar way. | |||
| * ] | |||
| * ] | |||
| It is important that the man washes and cleans his penis after anal intercourse if he intends to penetrate the vagina. Bacteria from the rectum are easily transferred to the vagina, which may cause ] and ]s.<ref name="SHR">{{cite web |title=Anal Sex - Facts and Safe Sex Information |url=http://www.sexual-health-resource.org/anal_sex.htm#aidsanal |access-date=5 April 2010 |archive-url=https://web.archive.org/web/20100404055257/http://www.sexual-health-resource.org/anal_sex.htm#aidsanal |archive-date=4 April 2010 |url-status=dead}}</ref> | |||
| * ] | |||
| * ] | |||
| When anal–oral contact occurs, protection is required since this is a ] in which illnesses such as hepatitis A or STIs can be easily transmitted, as well as enteric infections. The dental dam or plastic wrap<ref>{{Cite book|title=HIVAIDS care & counselling : a multidisciplinary approach | vauthors = Van Dyk AC |date=2008 |publisher=Pearson Education South Africa |isbn=9781770251717 |edition=4th |location=Cape Town |oclc=225855360|page=157}}</ref> are effective protection means whenever anilingus is performed. | |||
| * ] | |||
| * ] | |||
| ==Sex toys== | |||
| ] (note the flared bases)]] | |||
| Putting a condom on a ] provides better sexual hygiene and can help to prevent transmission of infections if the sex toy is shared, provided the condom is replaced when used by a different partner. Some ]s are made of porous materials, and pores retain viruses and bacteria, which makes it necessary to clean sex toys thoroughly, preferably with use of cleaners specifically for sex toys. Glass is non-porous and medical grade glass sex toys more easily sterilized between uses.<ref>{{Cite news |url=https://kinseyconfidential.org/safety-dance-sex-toy-safety-generation/|title=The Safety Dance: Sex Toy Safety for a New Generation|work=Kinsey Confidential |access-date=9 May 2017|archive-date=4 June 2017|archive-url=https://web.archive.org/web/20170604194306/https://kinseyconfidential.org/safety-dance-sex-toy-safety-generation/|url-status=dead}}</ref> | |||
| In cases in which one of the partners is treated for an STI, it is recommended that the couple not use sex toys until the treatment has proved to be effective. | |||
| All sex toys have to be properly cleaned after use. The way in which a sex toy is cleaned varies on the type of material it is made of. Some sex toys can be boiled or cleaned in a dishwasher. Most of the sex toys come with advice on the best way to clean and store them and these instructions should be carefully followed.<ref name="NHS">{{cite web|url=http://www.nhs.uk/chq/Pages/1690.aspx?CategoryID=118&SubCategoryID=122 |title=Are sex toys safe? |publisher=NHS |access-date=31 March 2010}}</ref> A sex toy should be cleaned not only when it is shared with other individuals but also when it is used on different parts of the body (such as mouth, vagina or anus). | |||
| A sex toy should regularly be checked for scratches or breaks that can be breeding ground for ]. It is best if the damaged sex toy is replaced by a new undamaged one. Even more ] protection should be considered by pregnant women when using sex toys. Sharing any type of sex toy that may draw ], like whips or needles, is not recommended, and is not safe.<ref name="NHS"/> | |||
| When using sex toys in the anus, sex toys "...can easily get lost" as "rectal muscles contract and can suck an object up and up, potentially obstructing the colon"; to prevent this serious problem, sex toy users are advised to use sex "...toys with a flared base or a string".<ref>{{cite web |url=https://www.scientificamerican.com/article/good-vibrations-us-consumer-web-site-aims-to-enhance-sex-toy-safety/|title=Good Vibrations: U.S. Consumer Web Site Aims to Enhance Sex Toy Safety| vauthors=Nuzzo R |website=] |author-link=Regina Nuzzo}}</ref> | |||
| ==Abstinence== | |||
| ] reduces STIs and pregnancy risks associated with ], but STIs may also be transmitted through non-sexual means, or by ]. HIV may be transmitted through contaminated needles used in ]ing, ], or ]. Medical or dental procedures using contaminated instruments can also spread HIV, while some health-care workers have acquired HIV through occupational exposure to accidental injuries with needles.<!-- | |||
| - --><ref name="HIV">{{cite journal |vauthors=Do AN, Ciesielski CA, Metler RP, Hammett TA, Li J, Fleming PL |title=Occupationally acquired human immunodeficiency virus (HIV) infection: national case surveillance data during 20 years of the HIV epidemic in the United States |journal=Infection Control and Hospital Epidemiology |volume=24 |issue=2 |pages=86–96 |date=February 2003 |pmid=12602690 |doi=10.1086/502178 |s2cid=20112502 |url=https://zenodo.org/record/1235694}}</ref> Evidence does not support the use of ].<ref name=Obs07>{{cite journal |vauthors=Ott MA, Santelli JS |title=Abstinence and abstinence-only education |journal=Current Opinion in Obstetrics & Gynecology |volume=19 |issue=5 |pages=446–452 |date=October 2007 |pmid=17885460 |pmc=5913747 |doi=10.1097/GCO.0b013e3282efdc0b }}</ref> Abstinence-only sex education programs have been found to be ineffective in decreasing rates of ] infection in the developed world<ref>{{cite journal |vauthors=Underhill K, Operario D, Montgomery P |title=Abstinence-only programs for HIV infection prevention in high-income countries |journal=The Cochrane Database of Systematic Reviews |issue=4 |pages=CD005421 |date=October 2007 |pmid=17943855 |doi=10.1002/14651858.CD005421.pub2 |veditors=Operario D}}</ref> and ].<ref name=Obs07/> Abstinence-only sex education primarily relies on the consequences of character and morality while health care professionals are concerned about matters regarding health outcomes and behaviors.<ref name=":1">{{cite journal |vauthors=Santelli JS, Kantor LM, Grilo SA, Speizer IS, Lindberg LD, Heitel J, Schalet AT, Lyon ME, Mason-Jones AJ, McGovern T, Heck CJ, Rogers J, Ott MA |display-authors=6 |title=Abstinence-Only-Until-Marriage: An Updated Review of U.S. Policies and Programs and Their Impact |language=en |journal=The Journal of Adolescent Health |volume=61 |issue=3 |pages=273–280 |date=September 2017 |pmid=28842065 |doi=10.1016/j.jadohealth.2017.05.031 |url=https://www.jahonline.org/article/S1054-139X(17)30260-4/abstract |doi-access=free|hdl=1805/15683 |hdl-access=free }}</ref> Though abstinence is the best course to prevent pregnancy and STIs, in reality, it leaves young people without the information and skills they need to avoid unwanted pregnancies and STIs.<ref name=":1" /> | |||
| == See also == | |||
| {{Portal|Human sexuality}} | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | * ] | ||
| * ] | * ] | ||
| * ] | * ] | ||
| * ] | * ] | ||
| ==References== | == References == | ||
| {{ |
{{Reflist|35em}} | ||
| ==External links== | == External links == | ||
| {{Commons category|Safer sex}} | {{Commons category|Safer sex}} | ||
| * {{Webarchive|url=https://web.archive.org/web/20200218012445/http://www.agum.org.uk/std/prevention-std.html |date=18 February 2020 }} | |||
| * - 10 articles about condoms. | |||
| * | |||
| * "Guide to Safer Sex" from the ]'s sexuality.org site. Very explicit information on making various sexual practices safer: | |||
| ** | |||
| ** | |||
| * from HIV InSite | |||
| * - Detailed information on contraception (also includes a step-by-step guide with pictures on how to make a dental dam out of a condom) | |||
| * - Presents risk levels of a variety of sexual activities and most major STDs. | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| *{{fr icon}} — with many pictures. | |||
| * Useful links to other organisations are available, as well as information on women's sexual and reproductive health and rights in the Asian-Pacific region | |||
| {{Reproductive health}} | {{Reproductive health}} | ||
| {{Human sexuality}} | |||
| {{Sex}} | {{Sex}} | ||
| {{condom}} | {{condom}} | ||
| {{AIDS|state=autocollapse}} | {{AIDS|state=autocollapse}} | ||
| {{STD/STI}} | {{STD/STI}} | ||
| {{Public health}} | |||
| {{Authority control}} | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| <!-- The below are interlanguage links. --> | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 10:18, 17 November 2024
Ways to reduce the risk of acquiring STIs For the film, see Safe Sex (film).



Safe sex is sexual activity using methods or contraceptive devices (such as condoms) to reduce the risk of transmitting or acquiring sexually transmitted infections (STIs), especially HIV. "Safe sex" is also sometimes referred to as safer sex or protected sex to indicate that some safe sex practices do not eliminate STI risks. It is also sometimes used colloquially to describe methods aimed at preventing pregnancy that may or may not also lower STI risks.
The concept of "safe sex" emerged in the 1980s as a response to the global AIDS epidemic, and possibly more specifically to the AIDS crisis in the United States. Promoting safe sex is now one of the main aims of sex education and STI prevention, especially reducing new HIV infections. Safe sex is regarded as a harm reduction strategy aimed at reducing the risk of STI transmission.
Although some safe sex practices (like condoms) can also be used as birth control (contraception), most forms of contraception do not protect against STIs. Likewise, some safe sex practices, such as partner selection and low-risk sex behavior, might not be effective forms of contraception.
History
| This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources in this section. Unsourced material may be challenged and removed. Find sources: "Safe sex" – news · newspapers · books · scholar · JSTOR (March 2018) (Learn how and when to remove this message) |
Although strategies for avoiding STIs like syphilis and gonorrhea have existed for centuries and the term "safe sex" existed in English as early as the 1930s, the use of the term to refer to STI-risk reduction dates to the mid-1980s in the United States. It emerged in response to the HIV/AIDS crisis.
A year before the HIV virus was isolated and named, the San Francisco chapter of the Sisters of Perpetual Indulgence published a small pamphlet titled Play Fair! out of concern over widespread STIs among the city's gay male population. It specifically named illnesses (Kaposi's sarcoma and pneumocystis pneumonia) that would later be understood as symptoms of advanced HIV disease (or AIDS). The pamphlet advocated a range of safe-sex practices, including abstinence, condoms, personal hygiene, use of personal lubricants, and STI testing/treatment. It took a casual, sex-positive approach while also emphasizing personal and social responsibility. In May 1983—the same month HIV was isolated and named in France—the New York City-based HIV/AIDS activists Richard Berkowitz and Michael Callen published similar advice in their booklet, How to Have Sex in an Epidemic: One Approach. Both publications included recommendations that are now standard advice for reducing STI (including HIV) risks.

Safe sex as a form of STI risk reduction appeared in journalism as early as 1984, in the British publication The Daily Intelligencer: "The goal is to reach about 50 million people with messages about safe sex and AIDS education."
Although safe sex is used by individuals to refer to protection against both pregnancy and HIV/AIDS or other STI transmissions, the term was born in response to the HIV/AIDS epidemic. It is believed that the term safe sex was used in the professional literature in 1984, in the content of a paper on the psychological effect that HIV/AIDS may have on gay and bisexual men.

A year later, the same term appeared in an article in The New York Times. This article emphasized that most specialists advised their AIDS patients to practice safe sex. The concept included limiting the number of sexual partners, using prophylactics, avoiding bodily fluid exchange, and resisting the use of drugs that reduced inhibitions for high-risk sexual behavior. Moreover, in 1985, the first safe sex guidelines were established by the 'Coalition for Sexual Responsibilities'. According to these guidelines, safe sex was practiced by using condoms also when engaging in anal or oral sex.
Although the term safe sex was primarily used in reference to sexual activity between men, in 1986 the concept was spread to the general population. Various programs were developed with the aim of promoting safe sex practices among college students. These programs were focused on promoting the use of the condom, a better knowledge about the partner's sexual history and limiting the number of sexual partners. The first book on this subject appeared in the same year. The book was entitled "Safe Sex in the Age of AIDS", and had 88 pages that described both positive and negative approaches to sexual life. Sexual behavior could be safe (kissing, hugging, massage, body-to-body rubbing, mutual masturbation, exhibitionism, phone sex, and use of separate sex toys); possibly safe (use of condoms); or unsafe.
In 1997, specialists in this matter promoted the use of condoms as the most accessible safe sex method (besides abstinence) and they called for TV commercials featuring condoms. During the same year, the Catholic Church in the United States issued their own "safer sex" guidelines on which condoms were listed, though two years later the Vatican urged chastity and heterosexual marriage, attacking the American Catholic bishops' guidelines.
A study carried out in 2006 by Californian specialists showed that the most common definitions of safe sex are condom use (68% of the interviewed subjects), abstinence (31.1% of the interviewed subjects), monogamy (28.4% of the interviewed subjects) and safe partner (18.7% of the interviewed subjects).
The term safer sex in Canada and the United States has gained greater use by health workers, reflecting that risk of transmission of sexually transmitted infections in various sexual activities is a continuum. The term safe sex is still in common use in the United Kingdom, Australia and New Zealand.
"Safer sex" is thought to be a more aggressive term which may make it more obvious to individuals that any type of sexual activity carries a certain degree of risk.
The term safe love has also been used, notably by the French Sidaction in the promotion of men's underpants incorporating a condom pocket and including the red ribbon symbol in the design, which were sold to support the charity.
Practices
A range of safe-sex practices are commonly recommended by Sexual Health Educators and Public Health Agencies. Many of these practices can reduce (but not eliminate) risk of transmitting or acquiring STIs.
Phone sex/cybersex/sexting
Sexual activities, such as phone sex, cybersex, and sexting, that do not include direct contact with the skin or bodily fluids of sexual partners, carry no STI risks and, thus, are forms of safe sex.
Non-penetrative sex
A range of sex acts called "non-penetrative sex" or "outercourse" can significantly reduce STI risks. Non-penetrative sex includes practices such as kissing, mutual masturbation, manual sex, rubbing or stroking. According to the Health Department of Western Australia, this sexual practice may prevent pregnancy and most STIs. However, non-penetrative sex may not protect against infections that can be transmitted via skin-to-skin contact, such as herpes and human papilloma virus. Mutual masturbation and manual sex carry some STI risk, especially if there is skin contact or shared bodily fluids with sexual partners, although the risks are significantly lower than many other sexual activities.
Condoms, dental dams, gloves
Barriers, such as condoms, dental dams, and medical gloves can prevent contact with body fluids (such as blood, vaginal fluid, semen, rectal mucus), and other means of transmitting STIs (like skin, hair and shared objects) during sexual activity.

- External condoms can be used to cover the penis, hands, fingers, or other body parts during sexual penetration or oral sex. They are most frequently made of latex, and can also be made out of synthetic materials including polyurethane and polyisoprene.
- Internal condoms (also called female condoms) are inserted into the vagina or anus prior to sexual penetration. These condoms are made of either polyurethane or nitrile. If external and internal condoms are used at the same time, they may break due to friction between the materials during sexual activity.
- A dental dam (originally used in dentistry) is a sheet of latex typically used for protection between the mouth and the vulva or anus when engaging in oral sex.
- Medical gloves and finger cots made out of latex, vinyl, nitrile, or polyurethane can cover hands or fingers during manual sex or may be used as a makeshift dental dam during oral sex.
- Condoms, dental dams, and gloves can also be used to cover sex toys such as dildos during sexual stimulation or penetration. If a sex toy is to be used in more than one orifice or partner, a condom/dental dam/glove can be used over it and changed when the toy is moved.
Oil-based lubrication can break down the structure of latex condoms, dental dams or gloves, reducing their effectiveness for STI protection.
While use of external condoms can reduce STI risks during sexual activity, they are not 100% effective. One study has suggested condoms might reduce HIV transmission by 85% to 95%; effectiveness beyond 95% was deemed unlikely because of slippage, breakage, and incorrect use. It also said, "In practice, inconsistent use may reduce the overall effectiveness of condoms to as low as 60–70%".
Pre-exposure prophylaxis (PrEP)
Main article: Pre-exposure prophylaxisPre-exposure prophylaxis (often abbreviated as PrEP) is the use of prescription drugs by those who do not have HIV to prevent HIV infection. PrEP drugs are taken prior to HIV exposure to prevent the transmission of the virus, usually between sexual partners. PrEP drugs do not prevent other STI infections or pregnancy.
As of 2018, the most-widely approved form of PrEP combines two drugs (tenofovir and emtricitabine) in one pill. That drug combination is sold under the brand name Truvada by Gilead Sciences. It is also sold in generic formulations worldwide. Other drugs and modalities are being studied for use as PrEP.
Different countries have approved different protocols for using the tenofovir/emtricitabine-combination drug as PrEP. That two-drug combination has been shown to prevent HIV infection in different populations when taken daily, intermittently, and on demand. Numerous studies have found the tenofovir/emtricitabine combination to be over 90% effective at preventing HIV transmission between sexual partners. AVAC has developed a tool to track trends in PrEP uptake across the globe.
Treatment as prevention
Main article: Treatment as preventionTreatment as Prevention (often abbreviated as TasP) is the practice of testing for and treating HIV infection as a way to prevent further spread of the virus. Those having knowledge of their HIV-positive status can use safe-sex practices to protect themselves and their partners (such as using condoms, sero-sorting partners, or choosing less-risky sexual activities). And, because HIV-positive people with durably suppressed or undetectable amounts of HIV in their blood cannot transmit HIV to sexual partners, sexual activity with HIV-positive partners on effective treatment is a form of safe sex (to prevent HIV infection). This fact has given rise to the concept of "U=U" ("Undetectable = Untransmittable").
Other forms of safe sex
Other methods proven effective at reducing STI risks during sexual activity are:
- Immunization against certain sexually-transmitted viruses. The most common vaccines protect against hepatitis B and human papilloma virus (HPV), which can cause cervical cancer, penile cancer, oral cancer, and genital warts. Immunization before initiation of sexual activity increases effectiveness of these vaccines. HPV vaccines are recommended for all teen girls and women as well as teen boys and men through age 26 and 21 respectively.
- Limiting numbers of sexual partners, particularly casual sexual partners, or restricting sexual activity to those who know and share their STI status, can also reduce STI risks. Monogamy or polyfidelity, practiced faithfully, is very safe (as far as STIs are concerned) when all partners are non-infected. However, many monogamous people have been infected with sexually transmitted infections by partners who are sexually unfaithful, have used injection drugs, or were infected by previous sexual partners. The same risks apply to polyfidelitous people, who face higher risks depending on how many people are in the polyfidelitous group.
- Communication with sexual partners about sexual history and STI status, preferred safe sex practices, and acceptable risks for partnered sexual activities.
- Engaging in less-risky sexual activities. In general, solo sexual activities are less risky than partnered activities. Sexual penetration of orifices (mouth, vagina, anus) and sharing body fluids (such as semen, blood, vaginal fluids, and rectal mucus) between sexual partners carry the most risk for STIs.
- Regular STI testing and treatment, especially by those who are sexually active with more than one casual sexual partner. It is possible to attain and show proof of STD-free-verification through online dating apps and websites.
- Penile circumcision. Some research suggests that circumcising (removing) the foreskin of the penis can reduce the risk of contracting HIV. Some advocacy groups dispute these findings.
Ineffective methods
Most methods of contraception are not effective at preventing the spread of STIs. This includes birth control pills, vasectomy, tubal ligation, periodic abstinence, IUDs and many non-barrier methods of pregnancy prevention. However, condoms, when used correctly, significantly reduces the risks of STI transmission and unwanted pregnancy.
The spermicide nonoxynol-9 has been claimed to reduce the likelihood of STI transmission. However, a technical report from 2001 by the World Health Organization has shown that nonoxynol-9 is an irritant and can produce tiny tears in mucous membranes, which may increase the risk of transmission by offering pathogens more easy points of entry into the system. They reported that nonoxynol-9 lubricant do not have enough spermicide to increase contraceptive effectiveness cautioned they should not be promoted. There is no evidence that spermicidal condoms are better at preventing STD transmission compared to condoms that do not have spermicide. If used properly, spermicidal condoms can prevent pregnancy, but there is still an increased risk that nonoxynyl-9 can irritate the skin, making it more susceptible for infections.
The use of a diaphragm or contraceptive sponge provides some women with better protection against certain sexually transmitted infections, but they are not effective for all STIs.
Hormonal methods of preventing pregnancy (such as oral contraceptives , depoprogesterone, hormonal IUDs, the vaginal ring, and the patch) offer no protection against STIs. The copper intrauterine device and the hormonal intrauterine device provide an up to 99% protection against pregnancies but no protection against STIs. Women with copper intrauterine device may be subject to greater risk of infection from bacterial infectious such as gonorrhea or chlamydia, although this is debated.
Coitus interruptus (or "pulling out"), in which the penis is removed from the vagina or mouth before ejaculation, may reduce transmission of STIs but still carries significant risk. This is because pre-ejaculate, a fluid that oozes from the penile urethra before ejaculation, may contain STI pathogens. Additionally, the microbes responsible for some diseases, including genital warts and syphilis, can be transmitted through skin-to-skin or mucous membrane contact.
Anal sex
Unprotected anal penetration is considered a high-risk sexual activity because the thin tissues of the anus and rectum can be easily damaged. Slight injuries can allow the passage of bacteria and viruses, including HIV. This includes penetration of the anus by fingers, hands, or sex toys such as dildos. Also, condoms may be more likely to break during anal sex than during vaginal sex, increasing the risk of STI transmission.
The main risk that individuals are exposed to when performing anal sex is the transmission of HIV. Other possible infections include hepatitis A, B and C; intestinal parasite infections like Giardia; and bacterial infections such as Escherichia coli.
Anal sex should be avoided by couples in which one of the partners has been diagnosed with an STI until the treatment has proven to be effective.
In order to make anal sex safer, the couple must ensure that the anal area is clean and the bowel empty and the partner on whom anal penetration occurs should be able to relax. Regardless of whether anal penetration occurs by using a finger or the penis, the condom is the best barrier method to prevent transmission of STI. Enemas should not be used as they can increase the risk of HIV infection and lymphogranuloma venereum proctitis.
Since the rectum can be easily damaged, the use of lubricants is highly recommended even when penetration occurs by using the finger. Especially for beginners, using a condom on the finger is both a protection measure against STI and a lubricant source. Most condoms are lubricated and they allow less painful and easier penetration. Oil-based lubricants damage latex and should not be used with condoms; water-based and silicone-based lubricants are available instead. Non-latex condoms are available for people who are allergic to latex made out of polyurethane or polyisoprene. Polyurethane condoms can safely be used with oil-based lubricant. The "female condom" may also be used effectively by the anal receiving partner.
Anal stimulation with a sex toy requires similar safety measures to anal penetration with a penis, in this case using a condom on the sex toy in a similar way.
It is important that the man washes and cleans his penis after anal intercourse if he intends to penetrate the vagina. Bacteria from the rectum are easily transferred to the vagina, which may cause vaginal and urinary tract infections.
When anal–oral contact occurs, protection is required since this is a risky sexual behavior in which illnesses such as hepatitis A or STIs can be easily transmitted, as well as enteric infections. The dental dam or plastic wrap are effective protection means whenever anilingus is performed.
Sex toys

Putting a condom on a sex toy provides better sexual hygiene and can help to prevent transmission of infections if the sex toy is shared, provided the condom is replaced when used by a different partner. Some sex toys are made of porous materials, and pores retain viruses and bacteria, which makes it necessary to clean sex toys thoroughly, preferably with use of cleaners specifically for sex toys. Glass is non-porous and medical grade glass sex toys more easily sterilized between uses.
In cases in which one of the partners is treated for an STI, it is recommended that the couple not use sex toys until the treatment has proved to be effective.
All sex toys have to be properly cleaned after use. The way in which a sex toy is cleaned varies on the type of material it is made of. Some sex toys can be boiled or cleaned in a dishwasher. Most of the sex toys come with advice on the best way to clean and store them and these instructions should be carefully followed. A sex toy should be cleaned not only when it is shared with other individuals but also when it is used on different parts of the body (such as mouth, vagina or anus).
A sex toy should regularly be checked for scratches or breaks that can be breeding ground for bacteria. It is best if the damaged sex toy is replaced by a new undamaged one. Even more hygiene protection should be considered by pregnant women when using sex toys. Sharing any type of sex toy that may draw blood, like whips or needles, is not recommended, and is not safe.
When using sex toys in the anus, sex toys "...can easily get lost" as "rectal muscles contract and can suck an object up and up, potentially obstructing the colon"; to prevent this serious problem, sex toy users are advised to use sex "...toys with a flared base or a string".
Abstinence
Sexual abstinence reduces STIs and pregnancy risks associated with sexual contact, but STIs may also be transmitted through non-sexual means, or by rape. HIV may be transmitted through contaminated needles used in tattooing, body piercing, or injections. Medical or dental procedures using contaminated instruments can also spread HIV, while some health-care workers have acquired HIV through occupational exposure to accidental injuries with needles. Evidence does not support the use of abstinence-only sex education. Abstinence-only sex education programs have been found to be ineffective in decreasing rates of HIV infection in the developed world and unplanned pregnancy. Abstinence-only sex education primarily relies on the consequences of character and morality while health care professionals are concerned about matters regarding health outcomes and behaviors. Though abstinence is the best course to prevent pregnancy and STIs, in reality, it leaves young people without the information and skills they need to avoid unwanted pregnancies and STIs.
See also
- Bareback (sex)
- Celibacy
- Human sexual activity
- Masturbation
- Misconceptions about HIV/AIDS
- Party and play
- Post-exposure prophylaxis
- Sisters of Perpetual Indulgence
- Terrence Higgins Trust
References
- Compact Oxford English Dictionary, Oxford University Press, 2009, Accessed 23 September 2009
- "Global strategy for the prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission" (PDF). World Health Organization. 2007. Archived from the original (PDF) on 23 March 2014. Retrieved 26 November 2011.
- Chin HB, Sipe TA, Elder R, Mercer SL, Chattopadhyay SK, Jacob V, et al. (Community Preventive Services Task Force) (March 2012). "The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the Guide to Community Preventive Services". American Journal of Preventive Medicine. 42 (3): 272–94. doi:10.1016/j.amepre.2011.11.006. PMID 22341164.
- Stephey MJ (11 December 2008). "A Brief History of Safe Sex". Time. Retrieved 14 September 2018.
In the 1540s, an Italian doctor named Gabriele Fallopius — the same man who discovered and subsequently named the Fallopian tubes of the female anatomy — wrote about syphilis, advocating the use of layered linen during intercourse for more "adventurous" (read: promiscuous) men. Legendary lover Casanova wrote about his pitfalls with medieval condoms made of dried sheep gut, referring to them as "dead skins" in his memoir. Even so, condoms made of animal intestine — known as "French letters" in England and la capote anglaise (English riding coats) in France — remained popular for centuries, though always expensive and never easy to obtain, meaning the devices were often reused.
- ^ "The meaning and origin of the expression: Safe sex". The Phrase Finder. Retrieved 14 September 2018.
- Sonnabend J (17 May 2013). "How to have sex in an epidemic: 30th anniversary". POZ. Retrieved 14 September 2018.
- Merson MH, O'Malley J, Serwadda D, Apisuk C (August 2008). "The history and challenge of HIV prevention". Lancet. 372 (9637): 475–88. doi:10.1016/S0140-6736(08)60884-3. PMID 18687461. S2CID 26554589.
- Berkowitz R (2003). Stayin' Alive: The Invention of Safe Sex. Boulder, CO: WestView. ISBN 9780813340920.
- Blair TR (June 2017). "Safe Sex in the 1970s: Community Practitioners on the Eve of AIDS". American Journal of Public Health. 107 (6): 872–879. doi:10.2105/AJPH.2017.303704. PMC 5425850. PMID 28426312.
- ^ "How Do Californians Define Safe Sex?" (PDF). Archived from the original (PDF) on 12 August 2006. Retrieved 28 July 2010.
- Gross J (22 September 1985). "Homosexuals Stepping Up AIDS Education". The New York Times. Retrieved 26 September 2021.
- "Sexual Health". NHS. 26 April 2018. Retrieved 8 April 2019.
- "How You Can Prevent Sexually Transmitted Diseases". Centers for Disease Control. 30 March 2020. Retrieved 2 April 2021.
- ^ "Safer Sex ("Safe Sex")". Archived from the original on 29 March 2008. Retrieved 23 September 2009.
- LaRosa J, Bader H, Garfield S (2009). New Dimensions In Women's Health. Jones & Bartlett Learning. p. 91. ISBN 978-0763765927. Retrieved 31 August 2013.
Outercourse is the sharing of sexual intimacy with behaviors such as private part kissing, petting, and mutual masturbation. The advantages of outercourse include no risk of pregnancy without penile-vaginal penetration and the behaviors permit emotional bonding and closeness.
- White L, Duncan G, Baumle W (2011). Medical Surgical Nursing: An Integrated Approach (3rd ed.). Cengage Learning. p. 1161. ISBN 978-1133707141. Retrieved 1 September 2013.
Some people consider outercourse to mean sex play without vaginal intercourse, while others consider this to mean sex play with no penetration at all (vaginal, oral, or anal).
- "STDs (Sexually Transmitted Diseases)". Archived from the original on 2 February 2014. Retrieved 23 January 2014.
- Gil-Llario MD, Morell-Mengual V, García-Barba M, Nebot-García JE, Ballester-Arnal R (January 2023). "HIV and STI Prevention Among Spanish Women Who have Sex with Women: Factors Associated with Dental Dam and Condom Use". AIDS and Behavior. 27 (1): 161–170. doi:10.1007/s10461-022-03752-z. PMC 9852118. PMID 35788924.
- Claure I, Anderson D, Klapperich CM, Kuohung W, Wong JY (July 2020). "Biomaterials and Contraception: Promises and Pitfalls". Annals of Biomedical Engineering. 48 (7): 2113–2131. doi:10.1007/s10439-019-02402-1. PMC 7202983. PMID 31701311. S2CID 254185613.
- ^ Corinna H (2016). S.E.X.: The All-You-Need-to-Know Sexuality Guide to Get You Through Your Teens and Twenties. New York: Da Capo Lifelong Press. ISBN 978-0738218847.
- ^ Moon A (2018). Girl Sex 101. Lunatic Ink. ISBN 978-0983830900.
- Corinna H (2016). S.E.X.: The All-You-Need-to-Know Sexuality Guide to Get You Through Your Teens and Twenties (2nd ed.). New York: Da Capo Lifelong Press. p. 294. ISBN 978-0738218847.
- ^ Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW (January 2002). "Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use" (PDF). Sexually Transmitted Diseases. 29 (1): 38–43. doi:10.1097/00007435-200201000-00007. PMID 11773877. S2CID 45262002. Archived from the original (PDF) on 24 July 2011.
- Kumar, Sagar; Haderxhanaj, Laura T.; Spicknall, Ian H. (June 2021). "Reviewing PrEP's Effect on STI Incidence Among Men Who Have sex with Men-Balancing Increased STI Screening and Potential Behavioral Sexual Risk Compensation". AIDS and Behavior. 25 (6): 1810–1818. doi:10.1007/s10461-020-03110-x. ISSN 1573-3254. PMC 8085068. PMID 33242186.
- "Pre-exposure Prophylaxis (PrEP) to Reduce HIV Risk". National Institute of Allergy and Infectious Diseases. 10 December 2020. Retrieved 27 June 2022.
- Beymer MR, Holloway IW, Pulsipher C, Landovitz RJ (August 2019). "Current and Future PrEP Medications and Modalities: On-demand, Injectables, and Topicals". Current HIV/AIDS Reports. 16 (4): 349–358. doi:10.1007/s11904-019-00450-9. PMC 6719717. PMID 31222499.
- "Pre-Exposure Prophylaxis (PrEP)". Centers for Disease Control and Prevention. 19 September 2016. Retrieved 14 March 2017.
- "PrEP | AVAC". avac.org. Retrieved 7 February 2024.
- "U=U". Prevention Access Campaign. 2017. Retrieved 11 September 2018.
- "Prevention - STD Information from CDC". www.cdc.gov. 28 May 2019. Retrieved 5 August 2019.
- Kahn JO, Walker BD (July 1998). "Acute human immunodeficiency virus type 1 infection". The New England Journal of Medicine. 339 (1): 33–9. doi:10.1056/NEJM199807023390107. PMID 9647878.
- Daar ES, Little S, Pitt J, Santangelo J, Ho P, Harawa N, et al. (January 2001). "Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network". Annals of Internal Medicine. 134 (1): 25–9. doi:10.7326/0003-4819-134-1-200101020-00010. PMID 11187417. S2CID 34714025.
- "Do you know his STD status? There's an app for that". 3 April 2013.
- "Tinder adds link to healthvana for STD-checking purposes". 22 January 2016.
- "Circumcision (male)". Mayo Clinic. Retrieved 10 May 2020.
- "WHO agrees HIV circumcision plan". BBC World News. BBC. 3 March 2007. Retrieved 12 July 2008.
- "Circumcision and HIV - the Randomised Controlled Trials". www.circumstitions.com.
- "Circumcision and AIDS". Archived from the original on 23 July 2008.
- Centers for Disease Control and Prevention (2 February 2022). "Condom Effectiveness". cdc.gov. Retrieved 13 April 2022.
Correctly using male (also called external) condoms and other barriers like female (also called internal) condoms and dental dams, every time, can reduce (though not eliminate) the risk of sexually transmitted diseases (STDs), including human immunodeficiency virus (HIV) and viral hepatitis. They can also provide protection against other diseases that may be transmitted through sex like Zika and Ebola. Using male (external) and female (internal) condoms correctly, every time, can also help prevent pregnancy.
- ^ "Technical Consultation on Nonoxynol-9" (PDF). WHO. October 2001. Retrieved 10 March 2018.
- "How Do I Make Sex Safer? | Common Questions and Answers". www.plannedparenthood.org. Retrieved 2 August 2019.
- Fackelmann KA (1992). "Diaphragm and sponge protect against STDs - sexually transmitted diseases". Science News. Archived from the original on 4 April 2010. Retrieved 5 April 2010.
- Hubacher D (November 2014). "Intrauterine devices & infection: review of the literature". The Indian Journal of Medical Research. 140 (Suppl 1): S53-7. PMC 4345753. PMID 25673543.
- "Safe Sex: Better Health Channel". better health.vic.gov.au. Retrieved 7 April 2024.
- Dean J, Delvin D. "Anal sex". Netdoctor.co.uk. Archived from the original on 7 May 2010. Retrieved 29 April 2010.
- Voeller B (June 1991). "AIDS and heterosexual anal intercourse". Archives of Sexual Behavior. 20 (3): 233–276. doi:10.1007/BF01541846. PMID 2059146. S2CID 13387947. as cited in Leichliter JS (November 2008). "Heterosexual anal sex: part of an expanding sexual repertoire?". Sexually Transmitted Diseases. 35 (11): 910–1. doi:10.1097/OLQ.0b013e31818af12f. PMID 18813143. S2CID 27348658.
- "Can I get HIV from anal sex?". Archived from the original on 3 October 2011. Retrieved 19 August 2011.
- "Anal Sex". CDC. Retrieved 10 March 2018.
- Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH (November 2008). "The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides". AIDS and Behavior. 12 (6): 860–866. doi:10.1007/s10461-007-9301-0. PMC 2953367. PMID 17705033.
- de Vries HJ, van der Bij AK, Fennema JS, Smit C, de Wolf F, Prins M, et al. (February 2008). "Lymphogranuloma venereum proctitis in men who have sex with men is associated with anal enema use and high-risk behavior". Sexually Transmitted Diseases. 35 (2): 203–208. doi:10.1097/OLQ.0b013e31815abb08. PMID 18091565. S2CID 2065170.
- Steiner M, Piedrahita C, Glover L, Joanis C, Spruyt A, Foldesy R (1993). "The impact of lubricants on latex condoms during vaginal intercourse" (PDF). International Journal of STD & AIDS. 5 (1): 29–36. CiteSeerX 10.1.1.574.1501. doi:10.1177/095646249400500108. PMID 8142525. S2CID 9271973.
- "Condoms". NHS. 21 December 2017. Retrieved 10 March 2018.
- "Clinical Prevention Guidance - 2015 STD Treatment Guidelines". www.cdc.gov. 10 October 2017. Retrieved 10 March 2018.
- "Anal Sex - Facts and Safe Sex Information". Archived from the original on 4 April 2010. Retrieved 5 April 2010.
- Van Dyk AC (2008). HIVAIDS care & counselling : a multidisciplinary approach (4th ed.). Cape Town: Pearson Education South Africa. p. 157. ISBN 9781770251717. OCLC 225855360.
- "The Safety Dance: Sex Toy Safety for a New Generation". Kinsey Confidential. Archived from the original on 4 June 2017. Retrieved 9 May 2017.
- ^ "Are sex toys safe?". NHS. Retrieved 31 March 2010.
- Nuzzo R. "Good Vibrations: U.S. Consumer Web Site Aims to Enhance Sex Toy Safety". Scientific American.
- Do AN, Ciesielski CA, Metler RP, Hammett TA, Li J, Fleming PL (February 2003). "Occupationally acquired human immunodeficiency virus (HIV) infection: national case surveillance data during 20 years of the HIV epidemic in the United States". Infection Control and Hospital Epidemiology. 24 (2): 86–96. doi:10.1086/502178. PMID 12602690. S2CID 20112502.
- ^ Ott MA, Santelli JS (October 2007). "Abstinence and abstinence-only education". Current Opinion in Obstetrics & Gynecology. 19 (5): 446–452. doi:10.1097/GCO.0b013e3282efdc0b. PMC 5913747. PMID 17885460.
- Underhill K, Operario D, Montgomery P (October 2007). Operario D (ed.). "Abstinence-only programs for HIV infection prevention in high-income countries". The Cochrane Database of Systematic Reviews (4): CD005421. doi:10.1002/14651858.CD005421.pub2. PMID 17943855.
- ^ Santelli JS, Kantor LM, Grilo SA, Speizer IS, Lindberg LD, Heitel J, et al. (September 2017). "Abstinence-Only-Until-Marriage: An Updated Review of U.S. Policies and Programs and Their Impact". The Journal of Adolescent Health. 61 (3): 273–280. doi:10.1016/j.jadohealth.2017.05.031. hdl:1805/15683. PMID 28842065.
External links
- "Prevention – Sexually Transmitted Disease, AGUM (Association of Genital Urinary Medicine) Archived 18 February 2020 at the Wayback Machine
- "Guidelines", British Association for Sexual health and HIV (BASHH)
| Sexual and reproductive health | |
|---|---|
| Rights | |
| Education | |
| Planning | |
| Contraception | |
| Assisted reproduction |
|
| Health | |
| Pregnancy | |
| Identity | |
| Medicine | |
| Disorders | |
| By country |
|
| History | |
| Policy | |
| Condom | |
|---|---|
| Brand names | |
| Uses | |
| Social issues | |
| History | |
| Related topics | |
| Sexually transmitted infections (STI) | |
|---|---|
| Bacterial | |
| Protozoal | |
| Parasitic | |
| Viral | |
| General inflammation |
|
| Public health | |||||||
|---|---|---|---|---|---|---|---|
| General |
| ||||||
| Preventive healthcare | |||||||
| Population health | |||||||
| Biological and epidemiological statistics | |||||||
| Infectious and epidemic disease prevention | |||||||
| Food hygiene and safety management | |||||||
| Health behavioral sciences | |||||||
| Organizations, education and history |
| ||||||
