| Revision as of 14:47, 17 May 2010 view sourceAjax151 (talk | contribs)Extended confirmed users1,113 edits →Substance Abuse: uncertainty← Previous edit | Latest revision as of 21:08, 22 December 2024 view source Slothwizard (talk | contribs)Extended confirmed users1,239 edits Unnecessary template for SCZTags: Visual edit Mobile edit Mobile web edit | ||
| Line 1: | Line 1: | ||
| {{Short description|Mental disorder with psychotic symptoms}} | |||
| {{Otheruses}} | |||
| {{Other uses}} | |||
| {{pp-semi-protected|small=yes}} | |||
| {{Pp|small=yes}} | |||
| {{Infobox disease | | |||
| {{pp-move}} | |||
| Name = Schizophrenia | | |||
| {{Use dmy dates|date=March 2023}} | |||
| Width = | | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| DiseasesDB = 11890 | | |||
| {{Infobox medical condition | |||
| ICD10 = {{ICD10|F|20||f|20}} | | |||
| | name = Schizophrenia | |||
| ICD9 = {{ICD9|295}} | | |||
| | image = Cloth embroidered by a schizophrenia sufferer.jpg | |||
| ICDO = | | |||
| | alt = Embroidery art with nonlinear text sewn into it with multiple colors of thread | |||
| OMIM = 181500 | | |||
| | caption = Cloth ] by a person diagnosed with schizophrenia | |||
| MedlinePlus = 000928 | | |||
| | field = ]<ref>{{cite book | vauthors = Jones D | author-link = Daniel Jones (phonetician) | title = English Pronouncing Dictionary |veditors= Roach P, Hartmann J, Setter J |publisher=Cambridge University Press |orig-date=1917 |year=2003 | isbn = 978-3-12-539683-8}}</ref> | |||
| eMedicineSubj = med | | |||
| | symptoms = ]s, ]s, ], ]<ref name=WHO2022/><ref name=NIH2022>{{cite web |title=Schizophrenia |work= Health topics |url=https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml |publisher= US ] |date=April 2022|access-date=22 August 2022}}</ref> | |||
| eMedicineTopic = 2072 | | |||
| | complications = Harm to self or others, social isolation, cognitive issues, ], ]s,<ref name=SBU2012>{{Cite web|url=http://www.sbu.se/en/publications/sbu-assesses/schizophrenia--pharmacological-treatments-patient-involvement-and-organization-of-care/|title=Medicinal treatment of psychosis/schizophrenia|date=21 November 2012 |publisher=] (SBU)|archive-url=https://web.archive.org/web/20170629092226/http://www.sbu.se/en/publications/sbu-assesses/schizophrenia--pharmacological-treatments-patient-involvement-and-organization-of-care/|archive-date=29 June 2017|url-status=live|access-date=26 June 2017}}</ref> ] and ] arising from ] medication<ref>{{cite web | vauthors = Proietto Sr J |title=Diabetes and Antipsychotic Drugs |url=https://www.medsafe.govt.nz/profs/puarticles/antipsychdiabetes.htm |publisher=] |date=November 2004}}</ref><ref>{{cite journal | vauthors = Holt RI | title = Association Between Antipsychotic Medication Use and Diabetes | journal = Current Diabetes Reports | volume = 19 | issue = 10 | pages = 96 | date = September 2019 | pmid = 31478094 | pmc = 6718373 | doi = 10.1007/s11892-019-1220-8 | publisher = ] |issn=1534-4827}}</ref> | |||
| eMedicine_mult = {{eMedicine2|emerg|520}} | | |||
| | onset = Ages 16 to 30<ref name=NIH2022/> | |||
| MeshName = Schizophrenia | | |||
| | duration = Chronic<ref name=NIH2022/> | |||
| MeshNumber = F03.700.750 |}} | |||
| | causes = Environmental and genetic factors<ref name=Lancet2016/> | |||
| <!--Para1: Definition, symptoms and diagnosis--> | |||
| | risks = ], ] use in adolescence, ]- or ]-associated psychosis,<ref>{{cite journal |title=Transition of Substance-Induced, Brief, and Atypical Psychoses to Schizophrenia: A Systematic Review and Meta-analysis|url=https://academic.oup.com/schizophreniabulletin/article/46/3/505/5588638 |journal=] |date=May 2020}}</ref> problems during pregnancy, ], being born or raised in a city<ref name=Lancet2016/><ref>{{cite journal | vauthors = Gruebner O, Rapp MA, Adli M, Kluge U, Galea S, Heinz A | title = Cities and Mental Health | journal = Deutsches Ärzteblatt International | volume = 114 | issue = 8 | pages = 121–127 | date = February 2017 | pmid = 28302261 | pmc = 5374256 | doi = 10.3238/arztebl.2017.0121 }}</ref> | |||
| '''Schizophrenia''' ({{pron-en|ˌskɪtsɵˈfrɛniə}} or {{IPA-en|ˌskɪtsɵˈfriːniə|}}) is a ] characterized by abnormalities in the perception or expression of reality. It most commonly manifests as auditory ]s, ] or bizarre ]s, or ] with significant social or occupational dysfunction. Onset of symptoms typically occurs in young adulthood,<ref name="castle1991">{{cite journal |author=Castle D, Wessely S, Der G, Murray RM |title=The incidence of operationally defined schizophrenia in Camberwell, 1965-84 |journal=The British Journal of Psychiatry |volume=159 |issue= |pages=790–4 |year=1991 |month=December |pmid=1790446 |doi=10.1192/bjp.159.6.790}}</ref> with around 0.4–0.6%<ref>{{cite journal |author=Bhugra D |title=The global prevalence of schizophrenia |journal=PLoS Medicine |volume=2 |issue=5 |pages=e151; quiz e175 |year=2005 |month=May |pmid=15916460 |pmc=1140960 |doi=10.1371/journal.pmed.0020151}}</ref><ref name="fn_34">{{cite journal |author=Goldner EM, Hsu L, Waraich P, Somers JM |title=Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature |journal=Canadian Journal of Psychiatry |volume=47 |issue=9 |pages=833–43 |year=2002 |month=November |pmid=12500753}}</ref> of the population affected. Diagnosis is based on the patient's self-reported experiences and observed behavior. No laboratory test for schizophrenia currently exists.<ref name="DSM-IV-TR" /> | |||
| | diagnosis = Based on observed behavior, reported experiences, and reports of others familiar with the person<ref name=DSM5/> | |||
| | differential = ], ], ] (], ]), ],<ref name=Ferri2010>{{cite book|vauthors=Ferri FF |title=Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders |date=2010 |publisher=Elsevier/Mosby |location=Philadelphia |isbn=978-0-323-07699-9 |chapter=Chapter S |edition=2nd}}</ref> ],<ref name=Paris2018/> ], ], ], ], ], ], ], ] | |||
| | prevention = | |||
| | management = Counseling, ] training<ref name=WHO2022/><ref name=Lancet2016/> | |||
| | medication = ]<ref name=Lancet2016/> | |||
| | prognosis = 20–28 years shorter ]<ref name=Laursen2014/><ref name=NIHStat/> | |||
| | frequency = ~0.32% (1 in 300) of the global population is affected.<ref name=WHO_FACT_SHEET>{{cite web |title=Schizophrenia Fact Sheet and Information |url=https://www.who.int/news-room/fact-sheets/detail/schizophrenia |publisher=]}}</ref> | |||
| | deaths = ~17,000 (2015)<ref name=GBD2015/> | |||
| }} | |||
| <!-- Definition, symptoms, and diagnosis--> | |||
| '''Schizophrenia''' is a ]<ref>{{cite web |title=ICD-11: 6A20 Schizophrenia |url=https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1683919430 |publisher=] |access-date= 23 August 2022 }}</ref><ref name= Lancet2016/> characterized variously by ]s (typically, ]), ]s, ] and behavior,<ref name=DSM5/> and ].<ref name= Lancet2016/> Symptoms ] and typically begin during young adulthood and are never resolved.<ref name=NIH2022/><ref name=DSM5/> There is no objective diagnostic test; diagnosis is based on observed behavior, a ] that includes the person's reported experiences, and reports of others familiar with the person.<ref name=DSM5/> For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months (according to the ]) or one month (according to the ]).<ref name=DSM5>{{cite book |title=Diagnostic and Statistical Manual of Mental Disorders: DSM-5 |edition=5th |date=2013 |publisher=American Psychiatric Association |location=Arlington, VA |isbn=978-0-89042-555-8 |pages=99–105}}</ref><ref name=Ferri2019/> Many people with schizophrenia have other mental disorders, especially ]s, ]s, and ].<ref name=DSM5/> | |||
| <!-- Epidemiology and causes --> | |||
| <!--Para2:lack of validity/controversies--> | |||
| About 0.3% to 0.7% of people are diagnosed with schizophrenia during their lifetime.<ref name=Javitt2014>{{cite journal |vauthors=Javitt DC |title=Balancing therapeutic safety and efficacy to improve clinical and economic outcomes in schizophrenia: a clinical overview |journal=The American Journal of Managed Care |volume=20 |issue=8 Suppl |pages=S160-165 |date=June 2014 |pmid=25180705}}</ref> In 2017, there were an estimated 1.1 million new cases and in 2022 a total of 24 million cases globally.<ref name=WHO2022/><ref name=GBD2018>{{cite journal |vauthors=James SL, Abate D |title=Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017 |journal=The Lancet |date=November 2018 |volume=392 |issue=10159 |pages=1789–1858 |doi=10.1016/S0140-6736(18)32279-7 |pmid=30496104 |pmc=6227754 }}</ref> Males are more often affected and on average have an earlier onset than females.<ref name=WHO2022>{{cite web |title=Schizophrenia Fact sheet | url = https://www.who.int/news-room/fact-sheets/detail/schizophrenia | publisher = ] | date = 10 January 2022 | access-date = 23 August 2022 }}</ref> The causes of schizophrenia may include ] and ] factors.<ref name=Lancet2016/> Genetic factors include a variety of common and rare ].<ref name=vandeLeemput2016>{{cite book|vauthors=van de Leemput J, Hess JL, Glatt SJ, Tsuang MT|date=2016|title=Genetics of Schizophrenia: Historical Insights and Prevailing Evidence |series=Advances in Genetics|volume=96|pages=99–141|doi=10.1016/bs.adgen.2016.08.001|pmid=27968732|isbn=978-0-12-809672-7 }}</ref> Possible environmental factors include ], childhood adversity, ] use during adolescence, infections, the ], and poor ].<ref name=Lancet2016/><ref name=Parakh2013/> | |||
| Studies suggest that ], early environment, ], ] and social processes are important contributory factors; some recreational and prescription drugs appear to cause or worsen symptoms. Current psychiatric research is focused on the role of neurobiology, but no single organic cause has been found. As a result of the many possible combinations of symptoms, there is debate about whether the diagnosis represents a single disorder or a number of discrete syndromes. Despite the ] of the term from the ] roots ''skhizein'' (''σχίζειν'', "to split") and ''phrēn, phren-'' (''φρήν, φρεν-''; "mind"), schizophrenia does not imply a "split mind" and it is not the same as ] (previously known as multiple personality disorder or split personality), a condition with which it is often confused in public perception.<ref>{{cite book|title=Abnormal Psychology|page=228|last=Rathus|first=Spencer|coauthors=Jeffrey Nevid|year=1991|publisher=Prentice Hall|isbn=0130052167}}</ref> | |||
| <!-- |
<!-- Course and prognosis --> | ||
| About half of those diagnosed with schizophrenia will have a significant improvement over the long term with no further relapses, and a small proportion of these will recover completely.<ref name=DSM5/><!-- Quote: "The course appears to be favorable in about 20% of those with schizophrenia, and a small number of individuals are reported to recover completely." --><ref name=Vita2018>{{cite journal | vauthors = Vita A, Barlati S | s2cid = 35299996 | title = Recovery from schizophrenia: is it possible? | journal = Current Opinion in Psychiatry | date = May 2018 |volume = 31 | issue = 3 | pages = 246–255 | doi = 10.1097/YCO.0000000000000407 | pmid = 29474266}}</ref> The other half will have a lifelong impairment.<ref name=Law2015>{{cite book | vauthors= Lawrence RE, First MB, Lieberman JA | chapter = Chapter 48: Schizophrenia and Other Psychoses | veditors= Tasman A, Kay J, Lieberman JA, First MB, Riba MB | title = Psychiatry | edition = fourth | date = 2015 | pages = 798, 816, 819 | doi = 10.1002/9781118753378.ch48 | publisher=John Wiley & Sons, Ltd. | isbn = 978-1-118-84547-9 }}</ref> In severe cases, people may be admitted to hospitals.<ref name=Vita2018/> Social problems such as ], poverty, ], exploitation, and victimization are commonly correlated with schizophrenia.<ref name=Killaspy2014/><ref name=Charleson2018>{{cite journal | vauthors = Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, McGrath JJ, Whiteford HA | title = Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016 | journal = Schizophrenia Bulletin | volume = 44 | issue = 6 | pages = 1195–1203 | date = October 2018 | pmid = 29762765 | pmc = 6192504 | doi = 10.1093/schbul/sby058 }}</ref> Compared to the general population, people with schizophrenia have a higher suicide rate (about 5% overall) and more ],<ref name=Lancet2009>{{cite journal | vauthors = ], ] | s2cid = 208792724 | title = Schizophrenia | journal = Lancet | volume = 374 | issue = 9690 | pages = 635–645 | date = August 2009 | pmid = 19700006 | doi = 10.1016/S0140-6736(09)60995-8 | url = http://xa.yimg.com/kq/groups/19525360/611943554/name/Schizophrenia+-+The+Lancet.pdf | archive-url = https://web.archive.org/web/20130623065810/http://xa.yimg.com/kq/groups/19525360/611943554/name/Schizophrenia+-+The+Lancet.pdf | df = dmy-all | archive-date = 23 June 2013 | access-date = 23 December 2011 }}</ref><ref name=Jop2010>{{cite journal | vauthors = Hor K, Taylor M | title = Suicide and schizophrenia: a systematic review of rates and risk factors | journal = Journal of Psychopharmacology | volume = 24 | issue = 4 Suppl | pages = 81–90 | date = November 2010 | pmid = 20923923 | pmc = 2951591 | doi = 10.1177/1359786810385490 }}</ref> leading to an average decrease in ] by 20<ref name=Laursen2014>{{cite journal | vauthors = Laursen TM, Nordentoft M, Mortensen PB | title = Excess early mortality in schizophrenia| journal = Annual Review of Clinical Psychology | date = 2014 | volume = 10 | pages=425–448 | doi = 10.1146/annurev-clinpsy-032813-153657 | pmid = 24313570| doi-access = free }}</ref> to 28 years.<ref name=NIHStat/> In 2015, an estimated 17,000 deaths were linked to schizophrenia.<ref name=GBD2015>{{cite journal | vauthors = Wang H, Naghavi M, Allen C, etal | collaboration = GBD 2015 Mortality and Causes of Death Collaborators | title = Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015 | journal = Lancet | volume = 388 | issue = 10053 | pages = 1459–1544 | date = October 2016 | pmid = 27733281 | pmc = 5388903 | doi = 10.1016/S0140-6736(16)31012-1 }}</ref> | |||
| Increased ] activity in the ] of the brain is consistently found in schizophrenic individuals. The mainstay of treatment is ] medication; this type of drug primarily works by suppressing dopamine activity. Dosages of antipsychotics are generally lower than in the early decades of their use. ], and vocational and social rehabilitation are also important. In more serious cases—where there is risk to self and others—involuntary hospitalization may be necessary, although hospital stays are less frequent and for shorter periods than they were in previous times.<ref name="BeckerKilian2006">{{cite journal |author=Becker T, Kilian R|year=2006 |title=Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care? |journal=] Supplement |volume=429 |pages=9–16 |pmid=16445476 |doi=10.1111/j.1600-0447.2005.00711.x |issue=429}}</ref> | |||
| <!-- Treatment --> | |||
| <!--Para4: Impairment/chronicity and Comorbidity--> | |||
| The mainstay of treatment is ] medication, including ] and ], along with ], job training, and ].<ref name=Lancet2016>{{cite journal | vauthors = Owen MJ, Sawa A, Mortensen PB | title = Schizophrenia | journal = The Lancet | volume = 388 | issue = 10039 | pages = 86–97 | date = July 2016 | pmid = 26777917 | pmc = 4940219 | doi = 10.1016/S0140-6736(15)01121-6 }}</ref> Up to a third of people do not respond to initial antipsychotics, in which case ] is offered.<ref name=Siskind2017>{{cite journal |vauthors=Siskind D, Siskind V, Kisely S |title=Clozapine Response Rates among People with Treatment-Resistant Schizophrenia: Data from a Systematic Review and Meta-Analysis |journal=Canadian Journal of Psychiatry |volume=62 |issue=11 |pages=772–777 |date=November 2017 |pmid=28655284|doi=10.1177/0706743717718167|pmc=5697625 }}</ref> In a network comparative meta-analysis of 15 antipsychotic drugs, clozapine was significantly more effective than all other drugs, although clozapine's heavily multimodal action may cause more significant side effects.<ref>{{cite journal | vauthors = Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM | title = Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis | journal = Lancet | volume = 382 | issue = 9896 | pages = 951–962 | date = September 2013 | pmid = 23810019 | doi = 10.1016/S0140-6736(13)60733-3 | s2cid = 32085212 }}</ref> In situations where doctors judge that there is a risk of harm to self or others, they may impose short ].<ref name=BeckerKilian2006>{{cite journal | vauthors = Becker T, Kilian R | title = Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care? | journal = Acta Psychiatrica Scandinavica. Supplementum | volume = 113 | issue = 429 | pages = 9–16 | year = 2006 | pmid = 16445476 | doi = 10.1111/j.1600-0447.2005.00711.x | s2cid = 34615961 }}</ref> Long-term hospitalization is used on a small number of people with severe schizophrenia.<ref name=Capdevielle2009>{{cite journal |vauthors=Capdevielle D, Boulenger JP, Villebrun D, Ritchie K |title=Durées d'hospitalisation des patients souffrant de schizophrénie: implication des systèmes de soin et conséquences médicoéconomiques |trans-title=Schizophrenic patients' length of stay: mental health care implication and medicoeconomic consequences |language=fr |journal=L'Encéphale |volume=35 |issue=4 |pages=394–399 |date=September 2009 |pmid=19748377 |doi=10.1016/j.encep.2008.11.005 }}</ref> In some countries where supportive services are limited or unavailable, long-term hospital stays are more common.<ref name=Narayan2012>{{cite journal | vauthors = Narayan KK, Kumar DS | title = Disability in a Group of Long-stay Patients with Schizophrenia: Experience from a Mental Hospital. | journal = Indian Journal of Psychological Medicine | date = January 2012 | volume = 34 | issue = 1 | pages = 70–75 | doi = 10.4103/0253-7176.96164 | pmid = 22661812| pmc = 3361848 | doi-access = free }}</ref> | |||
| The disorder is thought to mainly affect ], but it also usually contributes to chronic problems with behavior and emotion. People with schizophrenia are likely to have additional (]) conditions, including ] and ]s;<ref name="Sim_et_al_2006">{{cite journal |author=Sim K, Chua TH, Chan YH, Mahendran R, Chong SA |title=Psychiatric comorbidity in first episode schizophrenia: a 2 year, longitudinal outcome study |journal=Journal of Psychiatric Research |volume=40 |issue=7 |pages=656–63 |year=2006 |month=October |pmid=16904688 |doi=10.1016/j.jpsychires.2006.06.008}}</ref> the lifetime occurrence of ] is around 40%. Social problems, such as long-term unemployment, poverty and homelessness, are common. Furthermore, the average ] of people with the disorder is 10 to 12 years less than those without, due to increased physical health problems and a higher ] rate ( about 5% ).<ref name="Brown_Barraclough_2000">{{cite journal |author=Brown S, Barraclough B, Inskip H|year=2000 |title=Causes of the excess mortality of schizophrenia |journal=] |volume=177 |pages=212–7 |pmid=11040880 |doi=10.1192/bjp.177.3.212}}</ref><ref>{{cite journal |author=Palmer BA, Pankratz VS, Bostwick JM |title=The lifetime risk of suicide in schizophrenia: a reexamination |journal=Archives of General Psychiatry |volume=62 |issue=3 |pages=247–53 |year=2005 |month=March |pmid=15753237 |doi=10.1001/archpsyc.62.3.247}}</ref> | |||
| {{TOC limit}} | |||
| ]]] | |||
| ==Signs and symptoms== | ==Signs and symptoms== | ||
| ], who had schizophrenia]] | |||
| Depending on the individual, a person diagnosed with schizophrenia may experience ]s (most commonly ]), ]s (often bizarre or ] in nature), and ]. The latter may range from loss of train of thought, to sentences only loosely connected in meaning, to incoherence known as ] in severe cases. There is often an observable pattern of ] difficulty, for example lack of responsiveness or motivation. Impairment in ] is associated with schizophrenia, as are symptoms of ], and ] commonly occurs. In one uncommon subtype, the person may be largely mute, remain motionless in bizarre postures, or exhibit purposeless agitation; these are signs of ]. | |||
| Schizophrenia is a ] characterized by significant alterations in ], thoughts, mood, and behavior.<ref name=NICE2014/> Symptoms are described in terms of ], negative, and ].<ref name=NIH2022/><ref>{{cite journal |vauthors=Stępnicki P, Kondej M, Kaczor AA |title=Current Concepts and Treatments of Schizophrenia |journal= Molecules|volume=23 |issue=8 |date=20 August 2018 |pmid=30127324|doi=10.3390/molecules23082087 |pmc=6222385 |page=2087|doi-access=free }}</ref> The positive symptoms of schizophrenia are the same for any ] and are sometimes referred to as psychotic symptoms. These may be present in any of the different psychoses and are often transient, making early diagnosis of schizophrenia problematic. Psychosis noted for the first time in a person who is later diagnosed with schizophrenia is referred to as a first-episode psychosis (FEP).<ref name=RAISE>{{cite web |title=RAISE Questions and Answers |url=https://www.nimh.nih.gov/health/topics/schizophrenia/raise/raise-questions-and-answers.shtml#4 |publisher= US ]|access-date=29 December 2019}}</ref><ref>{{cite journal | vauthors = Marshall M | title = Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review | journal = Archives of General Psychiatry | date = September 2005 | volume = 62 | issue = 9 | pages = 975–983 | doi = 10.1001/archpsyc.62.9.975 | pmid = 16143729| s2cid = 13504781 | doi-access = }}</ref> | |||
| ===Positive symptoms=== | |||
| Late adolescence and early adulthood are peak years for the onset of schizophrenia. In 40% of men and 23% of women diagnosed with schizophrenia, the condition arose before the age of 19.<ref name=Cullen>{{cite journal |author=Cullen KR, Kumra S, Regan J ''et al.'' |title=Atypical Antipsychotics for Treatment of Schizophrenia Spectrum Disorders |journal=Psychiatric Times |volume=25 |issue=3 |year=2008 |url=http://www.psychiatrictimes.com/schizophrenia/article/10168/1147536}}</ref> These are critical periods in a young adult's social and vocational development. To minimize the developmental disruption associated with schizophrenia, much work has recently been done to identify and treat the ] phase of the illness, which has been detected up to 30 months before the onset of symptoms, but may be present longer.<ref name="Addington_et_al_2007">{{cite journal |author=Addington J |coauthors=Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, Heinssen R |year=2007|title=North American prodrome longitudinal study: a collaborative multisite approach to prodromal schizophrenia research |journal=] |volume=33 | issue=3 |pages=665–72 |pmid=17255119|doi=10.1093/schbul/sbl075 |pmc=2526151}}</ref> Those who go on to develop schizophrenia may experience the non-specific symptoms of social withdrawal, irritability and ] in the prodromal period,<ref name="ParnasJorgensen1989">{{cite journal |author=Parnas J |coauthors=Jorgensen A |year=1989 |title=Pre-morbid psychopathology in schizophrenia spectrum |journal=] |volume=115 |pages=623–7 |pmid=2611591}}</ref> and transient or self-limiting psychotic symptoms in the prodromal phase before psychosis becomes apparent.<ref name="Amminger_et_al_2006">{{cite journal |author=Amminger GP |coauthors=Leicester S, Yung AR, Phillips LJ, Berger GE, Francey SM, Yuen HP, McGorry PD |year=2006 |title=Early-onset of symptoms predicts conversion to non-affective psychosis in ultra-high risk individuals |journal=] |volume=84 | issue=1 |pages=67–76 |pmid=16677803 |doi=10.1016/j.schres.2006.02.018}}</ref> | |||
| Positive symptoms are those symptoms that are not normally experienced, but are present in people during a psychotic episode in schizophrenia, including ]s, ]s, and disorganized thoughts, speech and behavior or inappropriate affect, typically regarded as manifestations of psychosis.<ref name=RAISE/> Hallucinations occur at some point in the lifetimes of 80% of those with schizophrenia<ref name=Montagnese2021>{{cite journal |vauthors=Montagnese M, Leptourgos P, Fernyhough C, et al |title=A Review of Multimodal Hallucinations: Categorization, Assessment, Theoretical Perspectives, and Clinical Recommendations |journal=Schizophr Bull |volume=47 |issue=1 |pages=237–248 |date=January 2021 |pmid=32772114 |pmc=7825001 |doi=10.1093/schbul/sbaa101 }}</ref> and most commonly involve the sense of ] (most often ]), but can sometimes involve any of the other ]s such as ], ], ], and ].<ref>{{cite journal |vauthors=Császár N, Kapócs G, Bókkon I |s2cid=52813070 |title=A possible key role of vision in the development of schizophrenia |journal=Reviews in the Neurosciences |volume=30 |issue=4 |pages=359–379 |date=27 May 2019 |pmid=30244235 |doi=10.1515/revneuro-2018-0022|doi-broken-date=3 December 2024 }}</ref> The frequency of hallucinations involving multiple senses is double the rate of those involving only one sense.<ref name=Montagnese2021/> They are also typically related to the content of the delusional theme.<ref name=DSMIV>{{cite book | author = American Psychiatric Association. Task Force on DSM-IV. | year = 2000 | title = Diagnostic and statistical manual of mental disorders: DSM-IV-TR. | publisher = American Psychiatric Pub. | isbn = 978-0-89042-025-6 | pages = 299–304 }}</ref> ]s are ] or ] in nature. ] such as feeling that ] or that ], sometimes termed passivity phenomena, are also common.<ref name=Heinz2016>{{cite journal | vauthors = Heinz A, Voss M, Lawrie SM, Mishara A, Bauer M, Gallinat J, Juckel G, Lang U, Rapp M, Falkai P, Strik W, Krystal J, Abi-Dargham A, Galderisi S | title = Shall we really say goodbye to first rank symptoms? | journal = European Psychiatry | volume = 37 | pages = 8–13 | date = September 2016 | pmid = 27429167 | doi = 10.1016/j.eurpsy.2016.04.010 | s2cid = 13761854 }}</ref><ref name=NIH2022/> Positive symptoms generally respond well to medication<ref name=Lancet2016/> and become reduced over the course of the illness, perhaps linked to the age-related decline in dopamine activity.<ref name=DSM5/> | |||
| === |
===Negative symptoms=== | ||
| Negative symptoms are deficits of normal emotional responses, or of other thought processes. The five recognized domains of negative symptoms are: ] – showing flat expressions (monotone) or little emotion; ] – a poverty of speech; ] – an inability to feel pleasure; ] – the lack of desire to form relationships, and ] – a lack of motivation and ].<ref name=Adida2015>{{cite journal |vauthors=Adida M, Azorin JM, Belzeaux R, Fakra E |title= |journal=L'Encephale |volume=41 |issue=6 Suppl 1 |pages=6S15–17 |date=December 2015 |pmid=26776385 |doi=10.1016/S0013-7006(16)30004-5}}</ref><ref>{{cite journal |vauthors=Mach C, Dollfus S |title= |journal=L'Encephale |volume=42 |issue=2 |pages=165–171 |date=April 2016 |pmid=26923997 |doi=10.1016/j.encep.2015.12.020}}</ref> Avolition and anhedonia are seen as motivational deficits resulting from impaired reward processing.<ref>{{cite journal |vauthors=Waltz JA, Gold JM |title=Motivational Deficits in Schizophrenia and the Representation of Expected Value |journal=Current Topics in Behavioral Neurosciences |volume=27 |pages=375–410 |date=2016 |pmid=26370946 |doi=10.1007/7854_2015_385 |pmc=4792780 |isbn=978-3-319-26933-7 }}</ref><ref name=Husain2018>{{cite journal |vauthors=Husain M, Roiser JP |s2cid=49428707 |title=Neuroscience of apathy and anhedonia: a transdiagnostic approach. |journal=Nature Reviews. Neuroscience|volume=19 |issue=8 |pages=470–484 |date=August 2018 |pmid=29946157 |doi=10.1038/s41583-018-0029-9|url=https://ora.ox.ac.uk/objects/uuid:3e481f87-0ede-47dd-bdd8-2db78dfd3694 }}</ref> Reward is the main driver of motivation and this is mostly mediated by dopamine.<ref name=Husain2018/> It has been suggested that negative symptoms are multidimensional and they have been categorised into two subdomains of apathy or lack of motivation, and diminished expression.<ref name=Adida2015/><ref name=Galderisi2018>{{cite journal |vauthors=Galderisi S, Mucci A, Buchanan RW, Arango C |title=Negative symptoms of schizophrenia: new developments and unanswered research questions |journal=The Lancet. Psychiatry |volume=5 |issue=8 |pages=664–677 |date=August 2018 |pmid=29602739 |doi=10.1016/S2215-0366(18)30050-6 |s2cid=4483198 }}</ref> Apathy includes avolition, anhedonia, and social withdrawal; diminished expression includes blunt affect and alogia.<ref>{{cite journal |vauthors=Klaus F, Dorsaz O, Kaiser S |title= |journal=Revue médicale suisse |volume=14 |issue=619 |pages=1660–1664 |date=19 September 2018 |doi=10.53738/REVMED.2018.14.619.1660 |pmid=30230774|s2cid=246764656 }}</ref> Sometimes diminished expression is treated as both verbal and non-verbal.<ref>{{cite journal |vauthors=Batinic B |title=Cognitive Models of Positive and Negative Symptoms of Schizophrenia and Implications for Treatment. |journal=Psychiatria Danubina |volume=31 |issue=Suppl 2 |pages=181–184 |date=June 2019 |pmid=31158119}}</ref> | |||
| The psychiatrist ] (1887–1967) listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called ''first-rank symptoms'' or ], and they include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices.<ref name="SchneiderClinicalPsychopathology">{{cite book |last1=Schneider |first1=K |authorlink1=Kurt Schneider |title=Clinical Psychopathology |url=http://books.google.co.uk/books?id=ofzOAAAAMAAJ |edition=5 |year=1959 |publisher=Grune & Stratton |location=New York }}</ref> Although they have significantly contributed to the current diagnostic criteria, the ] of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that these studies allow neither a reconfirmation nor a rejection of Schneider's claims, and suggested that first-rank symptoms be de-emphasized in future revisions of diagnostic systems.<ref name="pmid17562695">{{cite journal |author=Nordgaard J, Arnfred SM, Handest P, Parnas J |title=The diagnostic status of first-rank symptoms |journal=Schizophrenia Bulletin |volume=34 |issue=1 |pages=137–54 |year=2008 |month=January |pmid=17562695 |pmc=2632385 |doi=10.1093/schbul/sbm044}}</ref> | |||
| Apathy accounts for around 50% of the most often found negative symptoms and affects functional outcome and subsequent quality of life. Apathy is related to disrupted cognitive processing affecting memory and planning including goal-directed behaviour.<ref>{{cite journal |vauthors=Bortolon C, Macgregor A, Capdevielle D, Raffard S |s2cid=13411386 |title=Apathy in schizophrenia: A review of neuropsychological and neuroanatomical studies. |journal=Neuropsychologia |volume=118 |issue=Pt B |pages=22–33 |date=September 2018 |pmid=28966139 |doi=10.1016/j.neuropsychologia.2017.09.033}}</ref> The two subdomains have suggested a need for separate treatment approaches.<ref name=Marder2014>{{cite journal |vauthors=Marder SR, Kirkpatrick B |s2cid=5172022 |title=Defining and measuring negative symptoms of schizophrenia in clinical trials |journal=European Neuropsychopharmacology|volume=24 |issue=5 |pages=737–743 |date=May 2014 |pmid=24275698 |doi=10.1016/j.euroneuro.2013.10.016}}</ref> A lack of distress is another noted negative symptom.<ref name=Tatsumi2020>{{cite journal |vauthors=Tatsumi K, Kirkpatrick B, Strauss GP, Opler M |s2cid=211141678 |title=The brief negative symptom scale in translation: A review of psychometric properties and beyond |journal=European Neuropsychopharmacology |date=April 2020 |volume=33 |pages=36–44 |doi=10.1016/j.euroneuro.2020.01.018 |pmid=32081498}}</ref> A distinction is often made between those negative symptoms that are inherent to schizophrenia, termed primary; and those that result from positive symptoms, from the side effects of antipsychotics, substance use disorder, and social deprivation – termed secondary negative symptoms.<ref>{{cite journal |vauthors=Klaus F, Kaiser S, Kirschner M |title=. |journal=Therapeutische Umschau |volume=75 |issue=1 |pages=51–56 |date=June 2018 |pmid=29909762 |doi=10.1024/0040-5930/a000966|s2cid=196502392 }}</ref> Negative symptoms are less responsive to medication and the most difficult to treat.<ref name=Marder2014/> However, if properly assessed, secondary negative symptoms are amenable to treatment.<ref name=Galderisi2018/> There is some evidence that the negative symptoms of schizophrenia are amenable to psychostimulant medication, although such drugs have varying degrees of risk for causing positive psychotic symptoms.<ref>{{Cite journal |last1=Lindenmayer |first1=Jean-Pierre |last2=Nasrallah |first2=Henry |last3=Pucci |first3=Michael |last4=James |first4=Steven |last5=Citrome |first5=Leslie |date=2013-07-01 |title=A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities |url=https://www.sciencedirect.com/science/article/abs/pii/S0920996413001655 |journal=Schizophrenia Research |volume=147 |issue=2 |pages=241–252 |doi=10.1016/j.schres.2013.03.019 |pmid=23619055 |issn=0920-9964}}</ref> | |||
| ===Positive and negative symptoms=== | |||
| Schizophrenia is often described in terms of ''positive'' and ''negative'' (or deficit) symptoms.<ref name="Sims_2002">{{cite book |author=Sims A |title=Symptoms in the mind: an introduction to descriptive psychopathology |publisher=W. B. Saunders |location=Philadelphia |year=2002 |isbn=0-7020-2627-1 }}</ref> The term ''positive symptoms'' refers to symptoms that most individuals do not normally experience but are present in schizophrenia. They include ]s, ], and ], and are typically regarded as manifestations of ]. ''Negative symptoms'' are things that are not present in schizophrenic persons but are normally found in healthy persons, that is, symptoms that reflect the loss or absence of normal traits or abilities. Common negative symptoms include flat or ] and emotion, poverty of speech (]), inability to experience pleasure (]), lack of desire to form relationships (]), and lack of motivation (]). Research suggests that negative symptoms contribute more to poor quality of life, functional disability, and the burden on others than do positive symptoms.<ref>{{cite journal |author=Velligan DI and Alphs LD|title=Negative Symptoms in Schizophrenia: The Importance of Identification and Treatment |journal=Psychiatric Times |volume=25 |issue=3 |date=March 1, 2008 |url=http://www.psychiatrictimes.com/schizophrenia/article/10168/1147581}}</ref> | |||
| Scales for specifically assessing the presence of negative symptoms, and for measuring their severity, and their changes have been introduced since the earlier scales such as the ] that deals with all types of symptoms.<ref name=Marder2014/> These scales are the ''Clinical Assessment Interview for Negative Symptoms'' (CAINS), and the ''Brief Negative Symptom Scale'' (BNSS) also known as second-generation scales.<ref name=Marder2014/><ref name=Tatsumi2020/><ref>{{cite journal |vauthors=Wójciak P, Rybakowski J |title=Clinical picture, pathogenesis and psychometric assessment of negative symptoms of schizophrenia. |journal=Psychiatria Polska |volume=52 |issue=2 |pages=185–197 |date=30 April 2018 |pmid=29975360 |doi=10.12740/PP/70610|doi-access=free }}</ref> In 2020, ten years after its introduction, a cross-cultural study of the use of BNSS found valid and reliable ] evidence for its five-domain structure cross-culturally. The BNSS can assess both the presence and severity of negative symptoms of the five recognized domains and an additional item of reduced normal distress. It has been used to measure changes in negative symptoms in trials of psychosocial and pharmacological interventions.<ref name=Tatsumi2020/> | |||
| A third symptom grouping, the ''disorganization syndrome'', is sometimes described, and includes chaotic speech, thought, and behavior. There is evidence for a number of other symptom classifications.<ref name="Peralta_Cuesta_2001">{{cite journal |author=Peralta V |coauthors=Cuesta MJ |year=2001 |title=How many and which are the psychopathological dimensions in schizophrenia? Issues influencing their ascertainment |journal=] |volume=49 | issue=3 |pages=269–85 |pmid=11356588 |doi=10.1016/S0920-9964(00)00071-2}}</ref> | |||
| ===Cognitive symptoms=== | |||
| ==Diagnosis== | |||
| {{See also |Visual processing abnormalities in schizophrenia}} | |||
| Schizophrenia is diagnosed on the basis of ]. ] correlates do not provide sufficiently useful criteria.<ref>{{cite journal | doi = 10.1126/stke.2003.207.pe49 | year = 2003 | month = Nov | author = Manji, Hk; Gottesman, Ii; Gould, Td | title = Signal transduction and genes-to-behaviors pathways in psychiatric diseases. | volume = 2003 | issue = 207 | pages = pe49 | pmid = 14600293 | journal = Science's STKE: signal transduction knowledge environment}}</ref> Diagnosis is based on the self-reported experiences of the person, and abnormalities in behavior reported by family members, friends or co-workers, followed by a clinical assessment by a ], ], ] or other ]. Psychiatric assessment includes a ] and some form of ].{{Citation needed|date=November 2009}} | |||
| ] throughout the human brain in a patient with schizophrenia. The most deficient areas are magenta, while the least deficient areas are blue.]] | |||
| An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early-onset and late-onset illness.<ref name=Murante2017/><ref name=Kar2016>{{cite journal |vauthors=Kar SK, Jain M |title=Current understandings about cognition and the neurobiological correlates in schizophrenia |journal=Journal of Neurosciences in Rural Practice |volume=7 |issue=3 |pages=412–418 |date=July 2016 |pmid=27365960 |doi=10.4103/0976-3147.176185 |pmc=4898111 |doi-access=free }}</ref> These are often evident long before the onset of illness in the ], and may be present in childhood or early adolescence.<ref name=Bozikas2011/><ref>{{cite journal | vauthors = Shah JN, Qureshi SU, Jawaid A, Schulz PE | s2cid = 10970088 | title = Is there evidence for late cognitive decline in chronic schizophrenia? | journal = The Psychiatric Quarterly | volume = 83 | issue = 2 | pages = 127–144 | date = June 2012 | pmid = 21863346 | doi = 10.1007/s11126-011-9189-8 }}</ref> They are a core feature but not considered to be core symptoms, as are positive and negative symptoms.<ref name=Biedermann2016>{{cite journal |vauthors = Biedermann F, Fleischhacker WW | title = Psychotic disorders in DSM-5 and ICD-11 | journal = CNS Spectrums | date = August 2016 | volume = 21 | issue = 4 | pages = 349–354 | doi = 10.1017/S1092852916000316 | pmid = 27418328| s2cid = 24728447 }}</ref><ref name=Vidailhet2013/> However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms.<ref name=Bozikas2011>{{cite journal | vauthors = Bozikas VP, Andreou C | s2cid = 26135485 | title = Longitudinal studies of cognition in first episode psychosis: a systematic review of the literature | journal = The Australian and New Zealand Journal of Psychiatry | volume = 45 | issue = 2 | pages = 93–108 | date = February 2011 | pmid = 21320033 | doi = 10.3109/00048674.2010.541418 }}</ref> Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.<ref name=Hashimoto2019/><ref name=Green2019/> | |||
| The deficits in ] are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed{{By whom|date=March 2024}} to equate to a possible reduction in IQ from the norm of 100 to 70–85.<ref>{{cite journal | vauthors=Javitt DC, Sweet RA |title=Auditory dysfunction in schizophrenia: integrating clinical and basic features. |journal=Nature Reviews. Neuroscience|volume=16 |issue=9 |pages=535–550 |date=September 2015|pmid=26289573|doi=10.1038/nrn4002|pmc=4692466 }}</ref><ref name=Megreya2016>{{cite journal |vauthors=Megreya AM |s2cid=26125559 |title=Face perception in schizophrenia: a specific deficit |journal=Cognitive Neuropsychiatry |volume=21 |issue=1 |pages=60–72 |date=2016 |pmid=26816133|doi=10.1080/13546805.2015.1133407}}</ref> Cognitive deficits may be of ] (nonsocial) or of ].<ref name=Murante2017>{{cite journal |vauthors=Murante T, Cohen CI |title=Cognitive Functioning in Older Adults With Schizophrenia |journal=Focus (American Psychiatric Publishing) |volume=15 |issue=1 |pages=26–34 |date=January 2017 |pmid=31975837 |doi=10.1176/appi.focus.20160032|pmc=6519630 }}</ref> Neurocognition is the ability to receive and remember information, and includes verbal fluency, ], ]ing, ], ], and ] and visual perception.<ref name=Green2019/> ] and attention are seen to be the most affected.<ref name=Megreya2016/><ref>{{cite journal |vauthors=Eack SM |title=Cognitive remediation: a new generation of psychosocial interventions for people with schizophrenia |journal=Social Work |volume=57 |issue=3 |pages=235–246 |date=July 2012 |pmid=23252315 |doi=10.1093/sw/sws008|pmc=3683242 }}</ref> Verbal memory impairment is associated with a decreased level of ] (relating meaning to words).<ref>{{cite journal | |||
| ===Standardized criteria=== | |||
| |vauthors=Pomarol-Clotet E, Oh M, Laws KR, McKenna PJ | title=Semantic priming in schizophrenia: systematic review and meta-analysis |journal=The British Journal of Psychiatry |volume=192 |issue=2 | pages=92–97 |date=February 2008 |pmid=18245021 |doi=10.1192/bjp.bp.106.032102 | hdl=2299/2735 |doi-access=free |hdl-access=free }}</ref> Another memory impairment is that of ].<ref>{{cite journal | vauthors = Goldberg TE, Keefe RS, Goldman RS, Robinson DG, Harvey PD | title = Circumstances under which practice does not make perfect: a review of the practice effect literature in schizophrenia and its relevance to clinical treatment studies | journal = Neuropsychopharmacology | volume = 35 | issue = 5 | pages = 1053–1062 | date = April 2010 | pmid = 20090669 | pmc = 3055399 | doi = 10.1038/npp.2009.211 | df = dmy-all }}</ref> An impairment in visual perception that is consistently found in schizophrenia is that of ].<ref name=Green2019/> ] impairments include an inability to perceive complex ]s.<ref>{{cite journal |vauthors=King DJ, Hodgekins J, Chouinard PA, Chouinard VA, Sperandio I |title=A review of abnormalities in the perception of visual illusions in schizophrenia. |journal=Psychonomic Bulletin and Review |volume=24 |issue=3 |pages=734–751 |date=June 2017 |pmid=27730532 |doi=10.3758/s13423-016-1168-5 |pmc = 5486866}}</ref> Social cognition is concerned with the mental operations needed to interpret, and understand the self and others in the social world.<ref name=Green2019>{{cite journal |vauthors=Green MF, Horan WP, Lee J |title=Nonsocial and social cognition in schizophrenia: current evidence and future directions |journal=World Psychiatry|volume=18 |issue=2 |pages=146–161 |date=June 2019 |pmid=31059632 |doi=10.1002/wps.20624|pmc=6502429 }}</ref><ref name=Murante2017/> This is also an associated impairment, and ] is often found to be difficult.<ref>{{cite journal | vauthors = Kohler CG, Walker JB, Martin EA, Healey KM, Moberg PJ | title = Facial emotion perception in schizophrenia: a meta-analytic review | journal = Schizophrenia Bulletin | volume = 36 | issue = 5 | pages = 1009–1019 | date = September 2010 | pmid = 19329561 | pmc = 2930336 | doi = 10.1093/schbul/sbn192 | df = dmy-all }}</ref><ref>{{cite journal | vauthors = Le Gall E, Iakimova G | title = | journal = L'Encéphale | volume = 44 | issue = 6 | pages = 523–537 | date = December 2018 | pmid = 30122298 | doi = 10.1016/j.encep.2018.03.004 | s2cid = 150099236 }}</ref> Facial perception is critical for ordinary social interaction.<ref>{{cite journal | vauthors = Grill-Spector K, Weiner KS, Kay K, Gomez J | title = The Functional Neuroanatomy of Human Face Perception | journal = Annual Review of Vision Science | volume = 3 | pages = 167–196 | date = September 2017 | pmid = 28715955 | pmc = 6345578 | doi = 10.1146/annurev-vision-102016-061214 }}</ref> Cognitive impairments do not usually respond to antipsychotics, and there are a number of ] that are used to try to improve them; ] is of particular help.<ref name=Vidailhet2013/> | |||
| The most widely used standardized criteria for diagnosing schizophrenia come from the ]'s '']'', version DSM-IV-TR, and the ]'s ], the ICD-10. The latter criteria are typically used in European countries, while the DSM criteria are used in the United States and the rest of the world, as well as prevailing in research studies. The ICD-10 criteria put more emphasis on Schneiderian ], although, in practice, agreement between the two systems is high.<ref name="Jakobsen_et_al_2005">{{cite journal |author=Jakobsen KD |coauthors=Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T |year=2005 |title=Reliability of clinical ICD-10 schizophrenia diagnoses |journal=Nordic Journal of Psychiatry |volume=59 | issue=3 |pages=209–12 |pmid=16195122 | doi = 10.1080/08039480510027698}}</ref> | |||
| ] of clumsiness and loss of fine motor movement are often found in schizophrenia, which may resolve with effective treatment of FEP.<ref name=Ferri2019/><ref>{{cite journal |vauthors=Fountoulakis KN, Panagiotidis P, Kimiskidis V, Nimatoudis I, Gonda X |s2cid=56476015 |title=Neurological soft signs in familial and sporadic schizophrenia |journal=Psychiatry Research |volume=272 |pages=222–229 |date=February 2019 |pmid=30590276 |doi=10.1016/j.psychres.2018.12.105 }}</ref> | |||
| According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:<ref name="DSM-IV-TR" /> | |||
| # '''Characteristic symptoms''': Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment). | |||
| #* ]s | |||
| #* ]s | |||
| #* Disorganized speech, which is a manifestation of ] | |||
| #* Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or ] behavior | |||
| #* Negative symptoms: ] (lack or decline in emotional response), ] (lack or decline in speech), or ] (lack or decline in motivation) | |||
| #:If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication. | |||
| # '''Social/occupational dysfunction''': For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset. | |||
| # '''Duration''': Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment). | |||
| ===Onset=== | |||
| If signs of disturbance are present for more than a month but less than six months, the diagnosis of ] is applied.<ref name="DSM-IV-TR">{{cite book |title=Diagnostic and statistical manual of mental disorders: DSM-IV |author=American Psychiatric Association |publisher=American Psychiatric Publishing, Inc. |location=Washington, DC |year=2000 |chapter=Schizophrenia |chapterurl=http://www.behavenet.com/capsules/disorders/schiz.htm |isbn=0-89042-024-6 |accessdate=2008-07-04}}</ref> Psychotic symptoms lasting less than a month may be diagnosed as ], and various conditions may be classed as ]. Schizophrenia cannot be diagnosed if symptoms of ] are substantially present (although ] could be diagnosed), or if symptoms of ] are present unless prominent delusions or hallucinations are also present, or if the symptoms are the direct physiological result of a general medical condition or a substance, such as abuse of a drug or medication. | |||
| {{Further|Basic symptoms of schizophrenia}} | |||
| {{See also|Childhood schizophrenia|Adolescence#Changes in the brain}} | |||
| Onset typically occurs between the late teens and early 30s, with the peak incidence occurring in males in the early to mid-twenties, and in females in the late twenties.<ref name=NIH2022/><ref name=DSM5/><ref name=Ferri2019/> Onset before the age of 17 is known as early-onset,<ref>{{cite journal |vauthors=Bourgou Gaha S, Halayem Dhouib S, Amado I, Bouden A |title= |journal=L'Encephale |volume=41 |issue=3 |pages=209–214 |date=June 2015 |pmid=24854724 |doi=10.1016/j.encep.2014.01.005}}</ref> and before the age of 13, as can sometimes occur, is known as ] or very early-onset.<ref name=DSM5 /><ref name=DaFonseca2018>{{cite journal |vauthors=Da Fonseca D, Fourneret P |title= |journal=L'Encephale |volume=44 |issue=6S |pages=S8–S11 |date=December 2018 |pmid=30935493 |doi=10.1016/S0013-7006(19)30071-5|s2cid=150798223 }}</ref> Onset can occur between the ages of 40 and 60, known as late-onset schizophrenia.<ref name=Murante2017/> Onset over the age of 60, which may be difficult to differentiate as schizophrenia, is known as very-late-onset schizophrenia-like psychosis.<ref name=Murante2017/> Late onset has shown that a higher rate of females are affected; they have less severe symptoms and need lower doses of antipsychotics.<ref name=Murante2017/> The tendency for earlier onset in males is later seen to be balanced by a ] increase in the development in females. ] produced pre-menopause has a dampening effect on dopamine receptors but its protection can be overridden by a genetic overload.<ref>{{cite journal |vauthors=Häfner H |title=From Onset and Prodromal Stage to a Life-Long Course of Schizophrenia and Its Symptom Dimensions: How Sex, Age, and Other Risk Factors Influence Incidence and Course of Illness |journal=Psychiatry Journal |volume=2019 |page=9804836 |date=2019 |pmid=31139639 |doi=10.1155/2019/9804836 |pmc=6500669 |doi-access=free }}</ref> There has been a dramatic increase in the numbers of older adults with schizophrenia.<ref>{{cite journal | vauthors = Cohen CI, Freeman K, Ghoneim D, Vengassery A, Ghezelaiagh B, Reinhardt MM | title = Advances in the Conceptualization and Study of Schizophrenia in Later Life | journal = The Psychiatric Clinics of North America | volume = 41 | issue = 1 | pages = 39–53 | date = March 2018 | pmid = 29412847 | doi = 10.1016/j.psc.2017.10.004 }}</ref> | |||
| Onset may happen suddenly or may occur after the slow and gradual development of a number of signs and symptoms, a period known as the ].<ref name=DSM5 /> Up to 75% of those with schizophrenia go through a prodromal stage.<ref name=George2017>{{cite journal |vauthors=George M, Maheshwari S, Chandran S, Manohar JS, Sathyanarayana Rao TS |title=Understanding the schizophrenia prodrome |journal=Indian Journal of Psychiatry |volume=59 |issue=4 |pages=505–509 |date=October 2017 |pmid=29497198 |doi=10.4103/psychiatry.IndianJPsychiatry_464_17|doi-broken-date=1 November 2024 |doi-access=free|pmc=5806335 }}</ref> The negative and cognitive symptoms in the prodrome stage can precede FEP (first episode psychosis) by many months and up to five years.<ref name=Hashimoto2019>{{cite journal |vauthors=Hashimoto K |s2cid=195814019 |title=Recent Advances in the Early Intervention in Schizophrenia: Future Direction from Preclinical Findings |journal=Current Psychiatry Reports |volume=21 |issue=8 |page=75 |date=5 July 2019 |pmid=31278495 |doi=10.1007/s11920-019-1063-7}}</ref><ref name=Conroy2018>{{cite journal |vauthors=Conroy S, Francis M, Hulvershorn LA |title=Identifying and treating the prodromal phases of bipolar disorder and schizophrenia |journal=Current Treatment Options in Psychiatry |volume=5 |issue=1 |pages=113–128 |date=March 2018 |pmid=30364516 |doi=10.1007/s40501-018-0138-0|pmc=6196741 }}</ref> The period from FEP and treatment is known as the duration of untreated psychosis (DUP) which is seen to be a factor in functional outcome. The prodromal stage is the high-risk stage for the development of psychosis.<ref name=Green2019/> Since the progression to first episode psychosis is not inevitable, an alternative term is often preferred of ].<ref name=Green2019/> Cognitive dysfunction at an early age impacts a young person's usual cognitive development.<ref>{{cite journal |vauthors=Lecardeur L, Meunier-Cussac S, Dollfus S |title= |journal=L'Encephale |volume=39 |pages=S64-71 |date=May 2013 |issue=Suppl 1 |pmid=23528322 |doi=10.1016/j.encep.2012.10.011}}</ref> Recognition and early intervention at the prodromal stage would minimize the associated disruption to educational and social development and has been the focus of many studies.<ref name=Hashimoto2019/><ref name=Conroy2018/> | |||
| ===Confusion with other conditions=== | |||
| There is a ] of disorders that share similarities with schizophrenia but which are diagnosed as separate conditions, including ], ], ] and ] (related to the concept of ]). ] is also generally considered to be related.<ref>Bowie, C.R. (2005) Current Psychosis and Therapeutics Reports, Volume 3, Number 4, Pages 147-151 DOI 10.1007/BF02629446</ref> | |||
| ==Risk factors== | |||
| Psychotic symptoms may be present in several other mental disorders, including ],<ref>{{cite journal |author=Pope HG |year=1983 |title=Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports |journal=Hospital and Community Psychiatry |volume=34 |pages=322–28 |url=http://psychservices.psychiatryonline.org/cgi/reprint/34/4/322.pdf|format=PDF |accessdate= 2008-02-24}}</ref> ],<ref>{{cite journal |author=McGlashan TH |title=Testing DSM-III symptom criteria for schizotypal and borderline personality disorders |journal=] |volume=44 |issue=2 |pages=143–8 |year=1987 |month=February |pmid=3813809 |accessdate=2008-07-03}}</ref>, drug intoxication and drug-induced psychosis. Delusions ("non-bizarre") are also present in ], and social withdrawal in ] or ]. Schizophrenia is complicated with ] (OCD) considerably more often than could be explained by pure chance, although it can be difficult to distinguish compulsions that represent OCD from the delusions of schizophrenia.<ref>{{cite journal |author=Bottas A |title=Comorbidity: Schizophrenia With Obsessive-Compulsive Disorder |journal=Psychiatric Times |volume=26 |issue=4 |date=April 15, 2009 |url=http://www.psychiatrictimes.com/display/article/10168/1402540 }}</ref> | |||
| {{Main|Risk factors of schizophrenia}} | |||
| Schizophrenia is described as a ] with no precise boundary, or single cause, and is thought to develop from ]s with involved vulnerability factors.<ref name=Lancet2016/><ref>{{cite journal | vauthors = Mullin AP, Gokhale A, Moreno-De-Luca A, Sanyal S, Waddington JL, Faundez V | title = Neurodevelopmental disorders: mechanisms and boundary definitions from genomes, interactomes and proteomes | journal = Translational Psychiatry | volume = 3 | issue = 12 | pages = e329 | date = December 2013 | pmid = 24301647 | pmc = 4030327 | doi = 10.1038/tp.2013.108 }}</ref><ref name= Davis2016/> The interactions of these ]s are complex, as numerous and diverse ] from conception to adulthood can be involved.<ref name=Davis2016>{{cite journal | vauthors = Davis J, Eyre H, Jacka FN, Dodd S, Dean O, McEwen S, Debnath M, McGrath J, Maes M, Amminger P, McGorry PD, Pantelis C, Berk M | title = A review of vulnerability and risks for schizophrenia: Beyond the two hit hypothesis | journal = Neuroscience and Biobehavioral Reviews | volume = 65 | pages = 185–194 | date = June 2016 | pmid = 27073049 | pmc = 4876729 | doi = 10.1016/j.neubiorev.2016.03.017 }}</ref> A genetic predisposition on its own, without interacting environmental factors, will not give rise to the development of schizophrenia.<ref name=Davis2016/><ref name=Perkovic2017>{{cite journal | vauthors = Perkovic MN, Erjavec GN, Strac DS, Uzun S, Kozumplik O, Pivac N | title = Theranostic Biomarkers for Schizophrenia | journal = International Journal of Molecular Sciences | volume = 18 | issue = 4 | page = 733 | date = March 2017 | pmid = 28358316 | pmc = 5412319 | doi = 10.3390/ijms18040733 | doi-access = free }}</ref> The genetic component means that ] brain development is disturbed, and environmental influence affects the postnatal development of the brain.<ref name= Suvisaari2010>{{cite journal | vauthors = Suvisaari J | title = | language = Finnish | journal = Duodecim; Laaketieteellinen Aikakauskirja | volume = 126 | issue = 8 | pages = 869–876 | date = 2010 | pmid = 20597333 }}</ref> Evidence suggests that genetically susceptible children are more likely to be vulnerable to the effects of environmental risk factors.<ref name= Suvisaari2010/> | |||
| ===Genetic=== | |||
| A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms,<ref name="DSM-IV-TR" /> such as ], ], ], ] infection, ], and brain lesions. It may be necessary to rule out a ], which can be distinguished by visual hallucinations, acute onset and fluctuating ], and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific ''medical'' indication or possible ] from ]. | |||
| Estimates of the ] of schizophrenia are between 70% and 80%, which implies that 70% to 80% of the individual differences in risk of schizophrenia are associated with genetics.<ref name=vandeLeemput2016/><ref name=Her2011/> These estimates vary because of the ] genetic and environmental influences, and their accuracy has been queried.<ref>{{cite journal | vauthors = O'Donovan MC, Williams NM, Owen MJ | title = Recent advances in the genetics of schizophrenia | journal = Human Molecular Genetics | volume = 12 Spec No 2 | pages = R125–133 | date = October 2003 | pmid = 12952866 | doi = 10.1093/hmg/ddg302 | doi-access = free }}</ref><ref name=Torrey2019>{{Cite journal |vauthors=Torrey EF, Yolken RH |s2cid=173991937 |date=August 2019 |title=Schizophrenia as a pseudogenetic disease: A call for more gene-environmental studies |journal=Psychiatry Research |volume=278 |pages=146–150 |doi=10.1016/j.psychres.2019.06.006|pmid=31200193 }}</ref> The greatest risk factor for developing schizophrenia is having a ] with the disease (risk is 6.5%); more than 40% of ] of those with schizophrenia are also affected.<ref name=BMJ07>{{cite journal | vauthors = Picchioni MM, Murray RM | title = Schizophrenia | journal = BMJ | volume = 335 | issue = 7610 | pages = 91–95 | date = July 2007 | pmid = 17626963 | pmc = 1914490 | doi = 10.1136/bmj.39227.616447.BE }}</ref> If one parent is affected the risk is about 13% and if both are affected the risk is nearly 50%.<ref name=Her2011>{{cite book|title=Adult psychopathology and diagnosis |year=2011 |publisher=John Wiley & Sons |isbn=978-1-118-13884-7 |chapter-url= https://books.google.com/books?id=iJtzm1KfU5oC&pg=PT282 |chapter= Chapter 8: Schizophrenia: Etiological considerations| veditors = Hersen M, Beidel DC |edition=6th| vauthors = Combs DR, Mueser KT, Gutierrez MM }}</ref> However, the ''DSM-5'' indicates that most people with schizophrenia have no family history of psychosis.<ref name=DSM5/> Results of ] studies of schizophrenia have generally failed to find consistent associations,<ref>{{cite journal | vauthors = Farrell MS, Werge T, Sklar P, Owen MJ, Ophoff RA, O'Donovan MC, Corvin A, Cichon S, Sullivan PF | title = Evaluating historical candidate genes for schizophrenia | journal = Molecular Psychiatry | volume = 20 | issue = 5 | pages = 555–562 | date = May 2015 | pmid = 25754081 | pmc = 4414705 | doi = 10.1038/mp.2015.16 }}</ref> and the ] identified by ] explain only a small fraction of the variation in the disease.<ref>{{Cite book |url= https://books.google.com/books?id=7ukmDAAAQBAJ |title=Schizophrenia and Psychotic Spectrum Disorders | vauthors = Schulz SC, Green MF, Nelson KJ |date=2016 |publisher=Oxford University Press |isbn=9780199378067 |pages=124–125 }}</ref> | |||
| Many ] are known to be involved in schizophrenia, each with small effects and unknown ] and ].<ref name=vandeLeemput2016/><ref>{{cite journal | vauthors = Schork AJ, Wang Y, Thompson WK, Dale AM, Andreassen OA | title = New statistical approaches exploit the polygenic architecture of schizophrenia—implications for the underlying neurobiology | journal = Current Opinion in Neurobiology | volume = 36 | pages = 89–98 | date = February 2016 | pmid = 26555806 | pmc = 5380793 | doi = 10.1016/j.conb.2015.10.008 }}</ref><ref>{{cite journal|vauthors= Coelewij L, Curtis D|title=Mini-review: Update on the genetics of schizophrenia|journal=Annals of Human Genetics|volume=82|issue=5|year= 2018|pages=239–243|issn=0003-4800|doi=10.1111/ahg.12259|pmid= 29923609|s2cid=49311660|url=https://discovery.ucl.ac.uk/id/eprint/10064654/ |doi-access=free}}</ref> The summation of these effect sizes into a ] can explain at least 7% of the variability in liability for schizophrenia.<ref>{{cite journal | vauthors = Kendler KS | title = The Schizophrenia Polygenic Risk Score: To What Does It Predispose in Adolescence? | journal = JAMA Psychiatry | volume = 73 | issue = 3 | pages = 193–194 | date = March 2016 | pmid = 26817666 | doi = 10.1001/jamapsychiatry.2015.2964 }}</ref> Around 5% of cases of schizophrenia are understood to be at least partially attributable to rare ]s (CNVs); these ]s are associated with known genomic disorders involving ] at ] (]) and ] (]), duplications at ] (most frequently found) and deletions at ] (]).<ref name=Lowther2017p82>{{cite journal | vauthors = Lowther C, Costain G, Baribeau DA, Bassett AS | s2cid = 4776174 | title = Genomic Disorders in Psychiatry—What Does the Clinician Need to Know? | journal = Current Psychiatry Reports | volume = 19 | issue = 11 | page = 82 | date = September 2017 | doi = 10.1007/s11920-017-0831-5 | pmid = 28929285 }}</ref> Some of these CNVs increase the risk of developing schizophrenia by as much as 20-fold, and are frequently comorbid with autism and intellectual disabilities.<ref name=Lowther2017p82/> | |||
| "Schizophrenia" does '''''not''''' mean ]—formerly and still widely known as "multiple personalities"—despite the ] of the word (Greek σχίζω = "I split").<!-- A common layman's error --> | |||
| The genes ] and ] are associated with the severity of suicidal behavior. These genes code for stress response proteins needed in the control of the ], and their interaction can affect this axis. Response to stress can cause lasting changes in the ] possibly disrupting the negative feedback mechanism, ], and the regulation of emotion leading to altered behaviors.<ref name=Perkovic2017/> | |||
| ===Subtypes=== | |||
| The ] contains five sub-classifications of schizophrenia (the ] developers are planning to drop them<ref>] DSM-5 Work Groups (2010) Retrieved 17 February 2010</ref>): | |||
| * ]: Where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent. (DSM code 295.3/ICD code F20.0) | |||
| * ]: Named ''hebephrenic schizophrenia'' in the ICD. Where thought disorder and ] are present together. (DSM code 295.1/ICD code F20.1) | |||
| * ]: The subject may be almost immobile or exhibit agitated, purposeless movement. Symptoms can include catatonic stupor and ]. (DSM code 295.2/ICD code F20.2) | |||
| * '''Undifferentiated type''': Psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met. (DSM code 295.9/ICD code F20.3) | |||
| * '''Residual type''': Where positive symptoms are present at a low intensity only. (DSM code 295.6/ICD code F20.5) | |||
| The question of how schizophrenia could be primarily genetically influenced, given that people with schizophrenia have lower fertility rates, is a paradox. It is expected that ] that increase the risk of schizophrenia would be selected against, due to their negative effects on ]. A number of potential explanations have been proposed, including that ]s associated with schizophrenia risk confers a fitness advantage in unaffected individuals.<ref>{{Cite journal |vauthors= Bundy H, Stahl D, MacCabe JH |date=February 2011 |title=A systematic review and meta-analysis of the fertility of patients with schizophrenia and their unaffected relatives: Fertility in schizophrenia |journal=Acta Psychiatrica Scandinavica |volume=123 |issue=2 |pages=98–106 |doi= 10.1111/j.1600-0447.2010.01623.x|pmid=20958271 |s2cid=45179016 }}</ref><ref>{{Cite journal |vauthors= van Dongen J, Boomsma DI |date=March 2013 |title=The evolutionary paradox and the missing heritability of schizophrenia |journal=American Journal of Medical Genetics Part B: Neuropsychiatric Genetics |volume=162 |issue=2 |pages=122–136 |doi= 10.1002/ajmg.b.32135|pmid=23355297 |s2cid=9648115 }}</ref> While some evidence has not supported this idea,<ref name=Torrey2019/> others propose that a large number of alleles each contributing a small amount can persist.<ref>{{cite journal |vauthors= Owen MJ, Sawa A, Mortensen PB |title=Schizophrenia |journal=Lancet |date=2 July 2016 |volume=388 |issue=10039 |pages=86–97 |doi=10.1016/S0140-6736(15)01121-6 |pmid= 26777917|pmc=4940219}}</ref> | |||
| The ] defines two additional subtypes. | |||
| * '''Post-schizophrenic depression''': A depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present. (ICD code F20.4) | |||
| * '''Simple schizophrenia''': Insidious and progressive development of prominent negative symptoms with no history of psychotic episodes. (ICD code F20.6) | |||
| A meta-analysis found that oxidative ] was significantly increased in schizophrenia.<ref name = Goh2021>{{cite journal |vauthors=Goh XX, Tang PY, Tee SF |title= 8-Hydroxy-2'-Deoxyguanosine and Reactive Oxygen Species as Biomarkers of Oxidative Stress in Mental Illnesses: A Meta-Analysis |journal= Psychiatry Investig |volume=18 |issue=7 |pages=603–618 |date=July 2021 |pmid=34340273 |pmc=8328836 |doi=10.30773/pi.2020.0417 |type= Meta-analysis}}</ref> | |||
| ===Controversies and research directions=== | |||
| The scientific ] of schizophrenia, and its defining symptoms such as delusions and hallucinations, have been criticised.<ref name="Boyle2002">{{cite book |author=Boyle, Mary |title=Schizophrenia: a scientific delusion? |publisher=Routledge |location=New York |year=2002 |isbn=0-415-22718-6}}</ref><ref name="fn_8">{{cite book |author=Bentall, Richard P.; Read, John E; Mosher, Loren R. |title=Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia |publisher=Brunner-Routledge |location=Philadelphia |year=2004|isbn=1-58391-906-6}}</ref> In 2006, a group of consumers and mental health professionals from the UK, under the banner of Campaign for Abolition of the Schizophrenia Label, argued for a rejection of the diagnosis of schizophrenia based on its heterogeneity and associated stigma, and called for the adoption of a ]. Other UK psychiatrists opposed the move arguing that the term schizophrenia is a useful, even if provisional concept.<ref name="schizophrenia_invalid">{{cite news |title=Schizophrenia term use 'invalid' |url=http://news.bbc.co.uk/2/hi/health/6033013.stm |agency=BBC |publisher=BBC News online |location=United Kingdom |date=9 October 2006 |accessdate=16 May 2007 }}</ref><ref>{{cite web|url=http://www.caslcampaign.com/aboutus_biography.php|title=CASL Biography|accessdate=2009-02-01}} and {{cite web|url=http://www.caslcampaign.com/aboutus.php|title=CASL History|accessdate=2009-02-01}}</ref> | |||
| ===Environmental=== | |||
| Similarly, there is an argument that the underlying issues would be better addressed as a spectrum of conditions<ref name=Tsuang00/> or as individual dimensions along which everyone varies rather than by a diagnostic category based on an arbitrary cut-off between normal and ill.<ref name="pmid18235866">{{cite journal |author=Peralta V, Cuesta MJ |title=A dimensional and categorical architecture for the classification of psychotic disorders |journal=World Psychiatry |volume=6 |issue=2 |pages=100–1 |year=2007 |month=June |pmid=18235866 |pmc=2219908 |doi= |url=}}</ref> This approach appears consistent with research on ], and with a relatively high prevalence of psychotic experiences, mostly non-distressing delusional beliefs, among the general public.<ref name="fn_5">{{cite journal |author=Verdoux H |coauthors=van Os J |year=2002 |title=Psychotic symptoms in non-clinical populations and the continuum of psychosis |journal=] |volume=54 | issue=1–2 |pages=59–65 |pmid=11853979 |doi=10.1016/S0920-9964(01)00352–8 |doi_brokendate=2009-12-08}}</ref><ref name="fn_65">{{cite journal |author=Johns LC |coauthors=van Os J |year=2001 |title=The continuity of psychotic experiences in the general population |journal=Clinical Psychology Review |volume=21 | issue=8 |pages=1125–41 |pmid=11702510 |doi=10.1016/S0272-7358(01)00103–9 |doi_brokendate=2010-03-22}}</ref><ref name="fn_67">{{cite journal |author=Peters ER |coauthors=Day S, McKenna J, Orbach G |year=2005 |title=Measuring delusional ideation: the 21-item Peters et al. Delusions Inventory (PDI) |journal=] |volume=30 |pages=1005–22 |pmid=15954204 |issue=4}}</ref> In concordance with this observation, psychologist Edgar Jones<!-- do not link, he is none of those guys-->, and psychiatrists ] and ], surveying the existing literature on delusions, pointed out that the consistency and completeness of the definition of delusion have been found wanting by many; delusions are neither necessarily fixed, nor false, nor involve the presence of incontrovertible evidence.<ref name="Jones1999">{{cite journal |author=Edgar Jones |year=1999 |title=The Phenomenology of Abnormal Belief: A Philosophical and Psychiatric Inquiry |journal=Philosophy, Psychiatry and Psychology |volume=6 | issue=1 |pages=1–16 |url=http://muse.jhu.edu/journals/philosophy_psychiatry_and_psychology/v006/6.1jones01.html |accessdate=2008-02-24 |doi=10.1353/ppp.1999.0004 |doi_brokendate=2009-12-08}}</ref><ref name="David1999">{{cite journal |author=David AS |year=1999 |title=On the impossibility of defining delusions |journal=Philosophy, Psychiatry and Psychology |volume=6 | issue=1 |pages=17–20 |url=http://muse.jhu.edu/journals/philosophy_psychiatry_and_psychology/v006/6.1david.html |accessdate=2008-02-24 |doi=10.1353/ppp.1999.0006 |doi_brokendate=2009-12-08}}</ref><ref name="Ghaemi1999">{{cite journal |author=S. Nassir Ghaemi |year=1999 |title=An Empirical Approach to Understanding Delusions |journal=Philosophy, Psychiatry and Psychology |volume=6 | issue=1 |pages=21–24 |url=http://muse.jhu.edu/journals/philosophy_psychiatry_and_psychology/v006/6.1ghaemi.html |accessdate=2008-02-24 |doi=10.1353/ppp.1999.0007 |doi_brokendate=2009-12-08}}</ref> | |||
| {{Further|Prenatal nutrition|Prenatal stress|Neuroplastic effects of pollution}} | |||
| Environmental factors, each associated with a slight risk of developing schizophrenia in later life include ], infection, ], and malnutrition in the mother during prenatal development.<ref name=Stilo2019>{{cite journal |vauthors=Stilo SA, Murray RM |title=Non-Genetic Factors in Schizophrenia |journal=Current Psychiatry Reports |volume=21 |issue=10 |page=100 |date=14 September 2019 |pmid=31522306 |doi=10.1007/s11920-019-1091-3 |pmc=6745031 }}</ref> A risk is associated with maternal obesity, in increasing ], and dysregulating the dopamine and serotonin pathways.<ref>{{cite journal |vauthors=Cirulli F, Musillo C, Berry A |s2cid=211029692 |title=Maternal Obesity as a Risk Factor for Brain Development and Mental Health in the Offspring |journal=Neuroscience|date= 5 February 2020 |volume=447 |pages=122–135 |pmid=32032668|doi= 10.1016/j.neuroscience.2020.01.023|hdl=11573/1387747 |hdl-access=free }}</ref> Both maternal stress and infection have been demonstrated to alter fetal ] through an increase of pro-inflammatory ]s.<ref name=Upthegrove2020>{{cite journal |vauthors=Upthegrove R, Khandaker GM |title=Cytokines, Oxidative Stress and Cellular Markers of Inflammation in Schizophrenia |journal=Current Topics in Behavioral Neurosciences |volume=44 |pages=49–66 |date=2020 |pmid=31115797 |doi= 10.1007/7854_2018_88|isbn=978-3-030-39140-9 |s2cid=162169817 |url= http://pure-oai.bham.ac.uk/ws/files/74984176/Upthegrove_Khandaker_Cytokines_oxidative_stress_and_cellular_markers_of_inflammation_in_schizophrenia_Current_Topics_in_Behavioral_Neurosciences_2019.pdf }}</ref> There is a slighter risk associated with being born in the winter or spring possibly due to ]<ref name=Chiang2016>{{cite journal |vauthors=Chiang M, Natarajan R, Fan X |s2cid= 206926835 |title=Vitamin D in schizophrenia: a clinical review |journal= Evidence-Based Mental Health |volume=19 |issue=1 |pages=6–9 |date= February 2016 |pmid=26767392 |doi=10.1136/eb-2015-102117 |pmc=10699337 }}</ref> or a prenatal ].<ref name=BMJ07/> Other infections during pregnancy or around the time of birth that have been linked to an increased risk include infections by '']'' and '']''.<ref>{{cite journal | vauthors = Arias I, Sorlozano A, Villegas E, de Dios Luna J, McKenney K, Cervilla J, Gutierrez B, Gutierrez J | title = Infectious agents associated with schizophrenia: a meta-analysis | journal = Schizophrenia Research | volume = 136 | issue = 1–3 | pages = 128–136 | date = April 2012 | pmid = 22104141 | doi = 10.1016/j.schres.2011.10.026 | hdl-access = free | s2cid = 2687441 | hdl = 10481/90076 }}</ref> The increased risk is about five to eight percent.<ref name=yolken>{{cite journal | vauthors = Yolken R | title = Viruses and schizophrenia: a focus on herpes simplex virus | journal = Herpes | volume = 11 | issue = Suppl 2 | pages = 83A–88A | date = June 2004 | pmid = 15319094 }}</ref> Viral infections of the brain during childhood are also linked to a risk of schizophrenia during adulthood.<ref>{{cite journal | vauthors = Khandaker GM | title = Childhood infection and adult schizophrenia: a meta-analysis of population-based studies. | journal = Schizophr. Res. | volume = 139 | issue = 1–3 | pages = 161–168 |date = August 2012 | pmid = 22704639 | pmc = 3485564 | doi = 10.1016/j.schres.2012.05.023}}</ref> ] is also associated with an increased risk of broadly defined schizophrenia-related disorders, with an ] of 2.4.<ref>{{cite journal | title = Cat Ownership and Schizophrenia-Related Disorders and Psychotic-Like Experiences: A Systematic Review and Meta-Analysis | journal = Schizophrenia Bulletin | volume = 50 | issue = 3 | pages = 489–495 | date = May 2024 | pmid = 38491934 | pmc = 11059805 | doi = 10.1093/schbul/sbad168 | vauthors = McGrath JJ, Lim CC, Saha S }}</ref> | |||
| ], a leading figure in schizophrenia research, has criticized the current DSM-IV and ICD-10 criteria for sacrificing diagnostic ] for the sake of artificially improving ]. She argues that overemphasis on psychosis in the diagnostic criteria, while improving diagnostic reliability, ignores more fundamental cognitive impairments that are harder to assess due to large variations in presentation.<ref name="pmid10719138">{{cite journal |author=Andreasen NC |title=Schizophrenia: the fundamental questions |journal=] |volume=31 |issue=2–3 |pages=106–12 |year=2000 |month=March |pmid=10719138 |doi= 10.1016/S0165-0173(99)00027-2|url=http://linkinghub.elsevier.com/retrieve/pii/S0165017399000272}}</ref><ref name="pmid12884883">{{cite journal |author=Andreasen NC |title=A unitary model of schizophrenia: Bleuler's "fragmented phrene" as schizencephaly |journal=] |volume=56 |issue=9 |pages=781–7 |year=1999 |month=September |pmid=12884883 |doi= 10.1001/archpsyc.56.9.781|url=http://archpsyc.ama-assn.org/cgi/pmidlookup?view=long&pmid=12884883}}</ref> This view is supported by other psychiatrists.<ref name=competing07>{{cite journal |author=Jansson LB, Parnas J |title=Competing definitions of schizophrenia: what can be learned from polydiagnostic studies? |journal=] |volume=33 |issue=5 |pages=1178–200 |year=2007 |month=September |pmid=17158508 |doi=10.1093/schbul/sbl065 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17158508}}</ref> In the same vein, ] and colleagues argue that psychotic symptoms may be a common end-state in a variety of disorders, including schizophrenia, rather than a reflection of the specific etiology of schizophrenia, and warn that there is little basis for regarding DSM’s operational definition as the "true" construct of schizophrenia.<ref name=Tsuang00>{{cite journal |author=Tsuang MT |coauthors=Stone WS, Faraone SV |year=2000 |title=Toward reformulating the diagnosis of schizophrenia |journal=] |volume=157 | issue=7 |pages=1041–50 |pmid=10873908 |doi=10.1176/appi.ajp.157.7.1041}}</ref> Neuropsychologist ] went further in suggesting the presence of specific ]s may be used to construct ] that are alternatives to those that are purely symptom-based. These deficits take the form of a reduction or impairment in basic psychological functions such as ], ], ] and ].<ref name="pmid10416733">{{cite journal |author=Green MF, Nuechterlein KH |title=Should schizophrenia be treated as a neurocognitive disorder? |journal=] |volume=25 |issue=2 |pages=309–19 |year=1999 |pmid=10416733 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=10416733}}</ref><ref name="GreenSchizophreniaBook">{{cite book |author=Green, Michael |title=Schizophrenia revealed: from neurons to social interactions |publisher=W.W. Norton |location=New York |year=2001|isbn=0-393-70334-7|laysummary=https://content.nejm.org/cgi/content/full/345/24/1782|laysource=NEJM book review}}</ref> | |||
| ] (ACEs), severe forms of which are classed as ], range from being bullied or abused, to the death of a parent.<ref name=Pearce2019>{{cite journal |vauthors=Pearce J, Murray C, Larkin W |title=Childhood adversity and trauma:experiences of professionals trained to routinely enquire about childhood adversity |journal=Heliyon |volume=5 |issue=7 |page=e01900 |date=July 2019 |pmid=31372522 |doi=10.1016/j.heliyon.2019.e01900|doi-access=free |pmc=6658729 |bibcode=2019Heliy...501900P }}</ref> Many adverse childhood experiences can cause ] and increase the risk of psychosis.<ref name=Pearce2019/><ref>{{cite journal | vauthors = Dvir Y, Denietolis B, Frazier JA | title = Childhood trauma and psychosis | journal = Child and Adolescent Psychiatric Clinics of North America | volume = 22 | issue = 4 | pages = 629–641 | date = October 2013 | pmid = 24012077 | doi = 10.1016/j.chc.2013.04.006 | s2cid = 40053289 }}</ref><ref>{{cite journal | vauthors = Misiak B, Krefft M, Bielawski T, Moustafa AA, Sąsiadek MM, Frydecka D | s2cid = 21614845 | title = Toward a unified theory of childhood trauma and psychosis: A comprehensive review of epidemiological, clinical, neuropsychological and biological findings | journal = Neuroscience and Biobehavioral Reviews | volume = 75 | pages = 393–406 | date = April 2017 | pmid = 28216171 | doi = 10.1016/j.neubiorev.2017.02.015 }}</ref> Chronic trauma, including ACEs, can promote lasting inflammatory dysregulation throughout the nervous system.<ref name=Nettis2020>{{cite journal | vauthors = Nettis MA, Pariante CM, Mondelli V | title = Early-Life Adversity, Systemic Inflammation and Comorbid Physical and Psychiatric Illnesses of Adult Life | journal = Current Topics in Behavioral Neurosciences | volume = 44 | pages = 207–225 | date = 2020 | pmid = 30895531 | doi = 10.1007/7854_2019_89 | isbn = 978-3-030-39140-9 | s2cid = 84842249 | url = https://kclpure.kcl.ac.uk/portal/en/publications/earlylife-adversity-systemic-inflammation-and-comorbid-physical-and-psychiatric-illnesses-of-adult-life(d2cdfc38-19e7-4918-80f1-5525e6ff45bf).html}}</ref> It is suggested that early stress may contribute to the development of schizophrenia through these alterations in the immune system.<ref name= Nettis2020/> Schizophrenia was the last diagnosis to benefit from the link made between ACEs and adult mental health outcomes.<ref>{{cite journal |vauthors=Guloksuz S, van Os J |title=The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum |journal=Psychological Medicine |volume=48 |issue=2 |pages=229–244 |date=January 2018 |pmid=28689498 |doi=10.1017/S0033291717001775|doi-access=free }}</ref> | |||
| The exclusion of affective components from the criteria for schizophrenia, despite their ubiquity in clinical settings, has also caused contention. This exclusion in the DSM has resulted in a "rather convoluted" separate disorder—].<ref name=competing07/> Citing poor ], some psychiatrists have totally contested the concept of schizoaffective disorder as a separate entity.<ref name="pmid17551352">{{cite journal |author=Lake CR, Hurwitz N |title=Schizoaffective disorder merges schizophrenia and bipolar disorders as one disease—there is no schizoaffective disorder |journal=] |volume=20 |issue=4 |pages=365–79 |year=2007 |month=July |pmid=17551352 |doi=10.1097/YCO.0b013e3281a305ab |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?an=00001504-200707000-00011}}</ref><ref name="pmid18199238">{{cite journal |author=Malhi GS, Green M, Fagiolini A, Peselow ED, Kumari V |title=Schizoaffective disorder: diagnostic issues and future recommendations |journal=Bipolar Disorders |volume=10 |issue=1 Pt 2 |pages=215–30 |year=2008 |month=February |pmid=18199238 |doi=10.1111/j.1399-5618.2007.00564.x}}</ref> The categorical distinction between mood disorders and schizophrenia, known as the ]ian dichotomy, has also been challenged by data from genetic epidemiology.<ref name="pmid15863738">{{cite journal |author=Craddock N, Owen MJ |title=The beginning of the end for the Kraepelinian dichotomy |journal=] |volume=186 |pages=364–6 |year=2005 |month=May |pmid=15863738 |doi=10.1192/bjp.186.5.364 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=15863738}}</ref> | |||
| Living in an ] during childhood or as an adult has consistently been found to increase the risk of schizophrenia by a factor of two,<ref name= Lancet2009/><ref>{{cite journal |vauthors= Costa E, Silva JA, Steffen RE |title=Urban environment and psychiatric disorders: a review of the neuroscience and biology |journal=Metabolism: Clinical and Experimental |volume=100S |page=153940 |date=November 2019 |pmid=31610855|doi=10.1016/j.metabol.2019.07.004|s2cid=204704312 }}</ref> even after taking into account ], ], and size of ].<ref>{{cite journal | vauthors = van Os J | title = Does the urban environment cause psychosis? | journal = The British Journal of Psychiatry | volume = 184 | issue = 4 | pages = 287–8 | date = April 2004 | pmid = 15056569 | doi = 10.1192/bjp.184.4.287 | doi-access = free }}</ref> A possible link between the ] has been suggested to be the cause of the elevated risk of schizophrenia.<ref>{{cite journal |vauthors=Attademo L, Bernardini F, Garinella R, Compton MT |s2cid=25505446 |title= Environmental pollution and risk of psychotic disorders: A review of the science to date |journal=Schizophrenia Research |volume=181 |pages=55–59 |date=March 2017 |pmid=27720315 |doi=10.1016/j.schres.2016.10.003}}</ref> Other risk factors include ], immigration related to social adversity and racial discrimination, family dysfunction, unemployment, and poor housing conditions.<ref name=BMJ07/><ref>{{cite journal | vauthors = Selten JP, Cantor-Graae E, Kahn RS | s2cid = 21391349 | title = Migration and schizophrenia | journal = Current Opinion in Psychiatry | volume = 20 | issue = 2 | pages = 111–115 | date = March 2007 | pmid = 17278906 | doi = 10.1097/YCO.0b013e328017f68e }}</ref> Having a ], or parents younger than 20 years are also associated with schizophrenia.<ref name= Lancet2016 /><ref>{{cite journal | vauthors = Sharma R, Agarwal A, Rohra VK, Assidi M, Abu-Elmagd M, Turki RF | title = Effects of increased paternal age on sperm quality, reproductive outcome and associated epigenetic risks to offspring | journal = Reproductive Biology and Endocrinology | volume = 13 | pages = 35 | date = April 2015 | pmid = 25928123 | pmc = 4455614 | doi = 10.1186/s12958-015-0028-x | doi-access = free }}</ref> | |||
| An approach broadly known as the ] movement, most active in the 1960s, opposes the orthodox medical view of schizophrenia as an illness.<ref name="Cooper1969">{{cite book |author=Cooper, David A. |title=The Dialectics of Liberation (Pelican) |publisher=Penguin Books Ltd |location=London, England |year=1969 |isbn=0-14-021029-6}}</ref>{{pn}} Psychiatrist ] argues that psychiatric patients are individuals with unconventional thoughts and behavior that society diagnoses as a method of ], and therefore the diagnosis of "schizophrenia" is merely a form of ].<ref name="Szasz1984">{{cite book |author=Szasz, Thomas Stephen |title=The myth of mental illness: foundations of a theory of personal conduct |publisher=Harper & Row |location=San Francisco |year=1974|isbn=0-06-091151-4}}</ref> The ] argues that many people diagnosed as psychotic need their experiences to be accepted and valued rather than ]. | |||
| ====Substance use==== | |||
| ==Causes== | |||
| {{ |
{{Further|Risk factors of schizophrenia#Substance use|Substance-induced psychosis}} | ||
| ] study<ref name="fn_25">;{{cite journal |author=Meyer-Lindenberg A |coauthors=Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, Weinberger DR, Berman KF |year=2002 |title=Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia |journal=] |volume=5 |pages=267–71 |pmid=11865311 |doi=10.1038/nn804 |issue=3}}</ref> suggests that the less the ]s are activated (<font color="red">red</font>) during a ] task, the greater the increase in abnormal ] activity in the ] (<font color="green">green</font>), thought to be related to the ]s in schizophrenia.]] | |||
| While the reliability of the diagnosis introduces difficulties in measuring the relative effect of genes and environment (for example, symptoms overlap to some extent with severe ] or ]), evidence suggests that genetic and ]s can act in combination to result in schizophrenia.<ref name="fn_12">{{cite journal |author=Harrison PJ |coauthors=Owen MJ |year=2003 |title=Genes for schizophrenia? Recent findings and their pathophysiological implications |journal=] |volume=361 | issue=9355 |pages=417–19 |pmid=12573388 |doi=10.1016/S0140-6736(03)12379–3 |doi_brokendate=2009-12-08}}</ref> Evidence suggests that the diagnosis of schizophrenia has a significant heritable component but that onset is significantly influenced by environmental factors or stressors.<ref name="fn_15">{{cite journal |author=Day R |coauthors=Nielsen JA, Korten A, Ernberg G, Dube KC, Gebhart J, Jablensky A, Leon C, Marsella A, Olatawura M, et al. |year=1987 |title=Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization |journal=Culture, Medicine and Psychiatry |volume=11 | issue=2 |pages=123–205 |pmid=3595169 | doi = 10.1007/BF00122563}}</ref> The idea of an inherent vulnerability (or ''diathesis'') in some people, which can be unmasked by biological, psychological or environmental stressors, is known as the ''stress-diathesis model''.<ref name="Corcoran_et_al_2003">{{cite journal |author=Corcoran C |coauthors=Walker E, Huot R, Mittal V, Tessner K, Kestler L, Malaspina D |year=2003 |title=The stress cascade and schizophrenia: etiology and onset |journal=] |volume=29 | issue=4 |pages=671–92 |pmid=14989406}}</ref> An alternative idea that biological, psychological and social factors are all important is known as the "biopsychosocial" model. | |||
| About half of those with schizophrenia use ] including ], tobacco, and ] excessively.<ref name=Gregg2007/><ref>{{cite journal | vauthors = Sagud M, Mihaljević-Peles A, Mück-Seler D, Pivac N, Vuksan-Cusa B, Brataljenović T, Jakovljević M | title = Smoking and schizophrenia | journal = Psychiatria Danubina | volume = 21 | issue = 3 | pages = 371–375 | date = September 2009 | pmid = 19794359 }}</ref> Use of ]s such as ] and ] can lead to a temporary ], which presents very similarly to schizophrenia. Rarely, alcohol use can also result in a similar ].<ref name= BMJ07/><ref name=alcohol>{{Cite journal |url= http://www.emedicine.com/med/topic3113.htm |title=Alcohol-Related Psychosis |access-date=27 September 2006 | vauthors = Larson M |date=30 March 2006 |journal=EMedicine |url-status=live |archive-url= https://web.archive.org/web/20081109011819/http://www.emedicine.com/MED/topic3113.htm |archive-date=9 November 2008}}</ref> Drugs may also be used as coping mechanisms by people who have schizophrenia, to deal with depression, ], boredom, and ].<ref name=Gregg2007>{{cite journal | vauthors = Gregg L, Barrowclough C, Haddock G | title = Reasons for increased substance use in psychosis | journal = Clinical Psychology Review | volume = 27 | issue = 4 | pages = 494–510 | date = May 2007 | pmid = 17240501 | doi = 10.1016/j.cpr.2006.09.004 }}</ref><ref name=Leweke08>{{cite journal | vauthors = Leweke FM, Koethe D | title = Cannabis and psychiatric disorders: it is not only addiction | journal = Addiction Biology | volume = 13 | issue = 2 | pages = 264–75 | date = June 2008 | pmid = 18482435 | doi = 10.1111/j.1369-1600.2008.00106.x | s2cid = 205400285 }}</ref> The use of cannabis and tobacco are not associated with the development of cognitive deficits, and sometimes a reverse relationship is found where their use improves these symptoms.<ref name=Vidailhet2013>{{cite journal | vauthors = Vidailhet P | title = . | journal = L'Encéphale | date = September 2013 | volume = 39 | issue = Suppl 2 | language= fr| pages = S83-92 | doi = 10.1016/S0013-7006(13)70101-5 | pmid=24084427}}</ref> However, ]s are associated with an increased risk of suicide, and a poor response to treatment.<ref name= Khokhar2018>{{cite book |vauthors=Khokhar JY, Henricks AM, Sullivan ED, Green AI |title=Apprentices to Genius: A tribute to Solomon H. Snyder |chapter=Unique Effects of Clozapine: A Pharmacological Perspective |series=Advances in Pharmacology |volume=82 |pages=137–162 |date=2018 |pmid=29413518|doi=10.1016/bs.apha.2017.09.009|pmc=7197512 |isbn=978-0128140871 }}</ref><ref>{{cite journal |vauthors=Bighelli I, Rodolico A, García-Mieres H, et al |title=Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis |journal=Lancet Psychiatry |volume=8 |issue=11 |pages=969–980 |date=November 2021 |pmid=34653393 |doi=10.1016/S2215-0366(21)00243-1 |s2cid=239003358 |doi-access=free |url=https://boris.unibe.ch/160225/8/Bighelli_LancetPsychiatry_2021.pdf }}</ref> | |||
| ===Genetic=== | |||
| ] and adoption studies have suggested a high level of ] (the proportion of variation between individuals in a population that is influenced by genetic factors).<ref name="ODonovan_et_al_2003">{{cite journal |author=O'Donovan MC |coauthors=Williams NM, Owen MJ |year=2003 |title=Recent advances in the genetics of schizophrenia |journal=] |volume=12 Spec No 2 |pages=R125–33 |pmid=12952866 |doi=10.1093/hmg/ddg302}}</ref> It has been suggested that schizophrenia is a condition of complex inheritance, with many different potential ] each of small effect, with different pathways for different individuals. Some have suggested that several genetic and other risk factors need to be present before a person becomes affected but this is still uncertain.<ref name="fn_75">{{cite journal |author=Owen MJ |coauthors=Craddock N, O'Donovan MC |year=2005 |title=Schizophrenia: genes at last? |journal=] |volume=21 | issue=9 |pages=518–25 |pmid=16009449 |doi=10.1016/j.tig.2005.06.011}}</ref> Candidate genes linked to an increased risk of schizophrenia and bipolar disorder as found in recent genome wide association studies appear to be partly separate and partly overlapping between the two disorders<ref name="Craddock_et_al_2006">{{cite journal |author=Craddock N |coauthors=O'Donovan MC, Owen MJ |year=2006 |title=Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology|journal=] |volume=32 | issue=1 |pages=9–16 |pmid=16319375 |doi=10.1093/schbul/sbj033 |pmc=2632175}}</ref> ] of ] studies have produced evidence of chromosomal regions increasing susceptibility,<ref>{{Cite journal | last1 = Datta | first1 = SR. | last2 = McQuillin | first2 = A. | last3 = Rizig | first3 = M. | last4 = Blaveri | first4 = E. | last5 = Thirumalai | first5 = S. | last6 = Kalsi | first6 = G. | last7 = Lawrence | first7 = J. | last8 = Bass | first8 = NJ. | last9 = Puri | first9 = V. | title = A threonine to isoleucine missense mutation in the pericentriolar material 1 gene is strongly associated with schizophrenia. | journal = Mol Psychiatry | month = Dec | year = 2008 | doi = 10.1038/mp.2008.128 | pmid = 19048012 }}</ref> which interacts directly with the Disrupted in Schizophrenia 1 (DISC1) gene protein<ref>{{Cite journal | last1 = Hennah | first1 = W. | last2 = Thomson | first2 = P. | last3 = McQuillin | first3 = A. | last4 = Bass | first4 = N. | last5 = Loukola | first5 = A. | last6 = Anjorin | first6 = A. | last7 = Blackwood | first7 = D. | last8 = Curtis | first8 = D. | last9 = Deary | first9 = IJ. | title = DISC1 association, heterogeneity and interplay in schizophrenia and bipolar disorder. | journal = Mol Psychiatry | volume = 14 | issue = 9 | pages = 865–73 | month = Sep | year = 2009 | doi = 10.1038/mp.2008.22 | pmid = 18317464 }}</ref> more recently the ].<ref>{{cite journal |author= O'Donovan MC, Craddock NJ, Owen MJ |title= Genetics of psychosis; insights from views across the genome |journal= Hum Genet |volume= 126|issue= 1|pages= 3–12|year=2009 |pmid=19521722 |doi=10.1007/s00439-009-0703-0}}</ref> has been implicated as well as the chromosome 6 HLA region.<ref>{{Cite journal | last1 = Purcell | first1 = SM. | last2 = Wray | first2 = NR. | last3 = Stone | first3 = JL. | last4 = Visscher | first4 = PM. | last5 = O'Donovan | first5 = MC. | last6 = Sullivan | first6 = PF. | last7 = Sklar | first7 = P. | last8 = Purcell | first8 = SM. | last9 = Wray | first9 = NR. | title = Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. | journal = Nature | volume = 460 | issue = 7256 | pages = 748–52 | month = Aug | year = 2009 | doi = 10.1038/nature08185 | pmid = 19571811 }}</ref> However, a large and comprehensive genetic study found no evidence of any significant association with any of 14 previously identified ]s.<ref name="pmid18198266">{{cite journal |author=Sanders AR, Duan J, Levinson DF, ''et al.'' |title=No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics |journal=Am J Psychiatry |volume=165 |issue=4 |pages=497–506 |year=2008 |month=April |pmid=18198266 |doi=10.1176/appi.ajp.2007.07101573 |url=}}</ref> Schizophrenia, in a small minority of cases, has been associated with rare deletions or duplications of tiny DNA sequences (known as ]) disproportionately occurring within genes involved in neuronal signaling and brain development/human cognitive, behavioral, and psychological variation.<ref name="Walsh T_et_al_2008">{{cite journal |author= Walsh T, McClellan JM, McCarthy SE ''et al.'' |title= Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia |journal=] |volume=320 |issue=5875 |pages=539–43 |year=2008 |pmid=18369103 |doi=10.1126/science.1155174}}</ref><ref>{{cite journal |author= Kirov G, Grozeva D, Norton N ''et al.'' |title= Support for the involvement of large CNVs in the pathogenesis of schizophrenia |journal= Hum Mol Genet |volume= 18|issue= 8|pages= 1497|year=2009 |pmid=19181681 |doi=10.1093/hmg/ddp043 |pmc= 2664144}}</ref><ref>{{cite journal |author=The International Schizophrenia Consortium |title=Rare chromosomal deletions and duplications increase risk of schizophrenia |journal=Nature|date=11 September 2008 |volume=455 |issue=7210 |pages=237–41 |pmid=18668038 |doi=10.1038/nature07239}}</ref> | |||
| ] may be a contributory factor in the development of schizophrenia, potentially increasing the risk of the disease in those who are already at risk.<ref name= Patel2020>{{cite journal |vauthors=Patel S, Khan S, M S, Hamid P |title=The Association Between Cannabis Use and Schizophrenia: Causative or Curative? A Systematic Review |journal= ] |volume=12 |issue=7 |pages=e9309 |date=July 2020 |pmid=32839678 |pmc=7442038 |doi=10.7759/cureus.9309 |doi-access=free |url=}}</ref><ref name= Hasan2020>{{cite journal |vauthors=Hasan A, von Keller R, Friemel CM, Hall W, Schneider M, Koethe D, Leweke FM, Strube W, Hoch E |title=Cannabis use and psychosis: a review of reviews |journal=Eur Arch Psychiatry Clin Neurosci |volume=270 |issue=4 |pages= 403–412 |date=June 2020 |pmid=31563981 |doi=10.1007/s00406-019-01068-z |s2cid=203567900 |url=}}</ref><ref>{{cite web |title=Causes — Schizophrenia | url= https://www.nhs.uk/mental-health/conditions/schizophrenia/causes/ |publisher= UK ] |date=11 November 2019 |access-date= 8 December 2021}}</ref> The increased risk may require the presence of certain genes within an individual.<ref name= Parakh2013>{{cite journal | vauthors = Parakh P, Basu D | title = Cannabis and psychosis: have we found the missing links? | journal = ] | volume = 6 | issue = 4 | pages = 281–287 | date = August 2013 | pmid = 23810133 | doi = 10.1016/j.ajp.2013.03.012 | type = Review | quote = Cannabis acts as a component cause of psychosis, that is, it increases the risk of psychosis in people with certain genetic or environmental vulnerabilities, though by itself, it is neither a sufficient nor a necessary cause of psychosis. }}</ref> Its use is associated with doubling the rate.<ref>{{cite journal | vauthors = Ortiz-Medina MB, Perea M, Torales J, Ventriglio A, Vitrani G, Aguilar L, Roncero C | title = Cannabis consumption and psychosis or schizophrenia development | journal = The International Journal of Social Psychiatry | volume = 64 | issue = 7 | pages = 690–704 | date = November 2018 | pmid = 30442059 | doi = 10.1177/0020764018801690 | s2cid = 53563635 }}</ref> | |||
| Assuming a ] genetic basis, one question for ] is why genes that increase the likelihood of the condition evolved, assuming the condition would have been ] from an evolutionary/reproductive point of view. One theory implicates genes involved in the evolution of language and ], but so far all theories have been disproved or remain unsubstantiated.<ref name="pmid18502103">{{cite journal |author=Crow TJ |title=The 'big bang' theory of the origin of psychosis and the faculty of language |journal=] |volume=102 |issue=1–3 |pages=31–52 |year=2008 |month=July |pmid=18502103 |doi=10.1016/j.schres.2008.03.010 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920-9964(08)00149–7}}</ref><ref>{{cite book|title=Clinical Handbook of Schizophrenia | |||
| |year=2008|isbn=1593856520|page=22–23|author=Mueser KT, Jeste DV|publisher=Guilford Press|location=New York}}</ref> | |||
| == |
==Causes== | ||
| {{Main|Causes of schizophrenia}}{{See also|Aberrant salience}} | |||
| Causal factors are thought to initially come together in early ] to increase the risk of later developing schizophrenia. One curious finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring, (at least in the ]).<ref name="fn_21">{{cite journal |author=Davies G |coauthors=Welham J, Chant D, Torrey EF, McGrath J |year=2003 |title=A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia |journal=] |volume=29 | issue=3|pages=587–93 |pmid=14609251}}</ref> There is now evidence that ] exposure to infections increases the risk for developing schizophrenia later in life, providing additional evidence for a link between in utero developmental pathology and risk of developing the condition.<ref name="fn_73">{{cite journal |author=Brown AS |year=2006 |title=Prenatal infection as a risk factor for schizophrenia |journal=] |volume=32 | issue=2 |pages=200–2 |pmid=16469941 |doi= 10.1093/schbul/sbj052 |pmc=2632220}}</ref> | |||
| The causes of schizophrenia are still unknown. Several models have been put forward to explain the link between altered brain function and schizophrenia.<ref name=Lancet2009/> The prevailing model of schizophrenia is that of a neurodevelopmental disorder, and the underlying changes that occur before symptoms become evident are seen as arising from the ].<ref>{{cite journal |vauthors=Hayes D, Kyriakopoulos M |title=Dilemmas in the treatment of early-onset first-episode psychosis |journal=Therapeutic Advances in Psychopharmacology |volume=8 |issue=8 |pages=231–239 |date=August 2018 |pmid=30065814 |doi=10.1177/2045125318765725|pmc=6058451 |doi-access= free }}</ref> Extensive studies support this model.<ref name=George2017/> Maternal infections, malnutrition and ] and ] are known risk factors for the development of schizophrenia, which usually emerges between the ages of 18 and 25, a period that overlaps with certain stages of neurodevelopment.<ref>{{cite journal |vauthors=Cannon TD |title=How Schizophrenia Develops: Cognitive and Brain Mechanisms Underlying Onset of Psychosis |journal=Trends Cogn Sci |volume=19 |issue=12 |pages=744–756 |date= December 2015 |pmid=26493362 |pmc=4673025 |doi=10.1016/j.tics.2015.09.009 }}</ref> Gene-environment interactions lead to deficits in the ]ry that affect sensory and cognitive functions.<ref name=George2017/> | |||
| The common dopamine and glutamate models proposed are not mutually exclusive; each is seen to have a role in the neurobiology of schizophrenia.<ref>{{cite journal |vauthors=Correll CU, Schooler NR |title=Negative Symptoms in Schizophrenia: A Review and Clinical Guide for Recognition, Assessment, and Treatment |journal= Neuropsychiatric Disease and Treatment |volume=16 |pages=519–534 |date=2020 |pmid=32110026 |doi=10.2147/NDT.S225643 |pmc=7041437 |doi-access=free }}</ref> The most common model put forward was the ], which attributes psychosis to the mind's faulty interpretation of the misfiring of ].<ref>{{cite journal | vauthors = Howes OD | title = The Role of Genes, Stress, and Dopamine in the Development of Schizophrenia | journal = Biological Psychiatry | date = 1 January 2017 | volume = 81 | issue = 1 | pages = 9–20 | doi = 10.1016/j.biopsych.2016.07.014 | pmid = 27720198| pmc = 5675052 }}</ref> This has been directly related to the symptoms of delusions and hallucinations.<ref>{{cite journal|vauthors=Broyd A, Balzan RP, Woodward TS, Allen P|date=June 2017|title=Dopamine, cognitive biases and assessment of certainty: A neurocognitive model of delusions| url= https://kclpure.kcl.ac.uk/portal/en/publications/dopamine-cognitive-biases-and-assessment-of-certainty-a-neurocognitive-model-of-delusions(138513dd-3a44-4deb-bac1-be45767ef51b).html|journal=Clinical Psychology Review|volume=54|pages=96–106|doi= 10.1016/j.cpr.2017.04.006 |pmid= 28448827|s2cid=3729566 }}</ref><ref name=Lancet2014>{{cite journal | vauthors = Howes OD, Murray RM | title = Schizophrenia: an integrated sociodevelopmental-cognitive model | journal = Lancet | volume = 383 | issue = 9929 | pages = 1677–1687 | date = May 2014 | pmid = 24315522 | pmc = 4127444 | doi = 10.1016/S0140-6736(13)62036-X }}</ref><ref>{{cite journal | vauthors = Grace AA | title = Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression | journal = Nature Reviews. Neuroscience | volume = 17 | issue = 8 | pages = 524–532 | date = August 2016 | pmid = 27256556 | pmc = 5166560 | doi = 10.1038/nrn.2016.57 }}</ref> Abnormal dopamine signaling has been implicated in schizophrenia based on the usefulness of medications that affect the dopamine receptor and the observation that dopamine levels are increased during acute psychosis.<ref>{{cite journal | vauthors = Fusar-Poli P, Meyer-Lindenberg A | title = Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of -DOPA PET studies | journal = Schizophrenia Bulletin | volume = 39 | issue = 1 | pages = 33–42 | date = January 2013 | pmid = 22282454 | pmc = 3523905 | doi = 10.1093/schbul/sbr180 }}</ref><ref>{{cite journal | vauthors = Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, Kapur S | title = The nature of dopamine dysfunction in schizophrenia and what this means for treatment | journal = Archives of General Psychiatry | volume = 69 | issue = 8 | pages = 776–786 | date = August 2012 | pmid = 22474070 | pmc = 3730746 | doi = 10.1001/archgenpsychiatry.2012.169 }}</ref> A decrease in ] in the ] may also be responsible for deficits in ].<ref>{{cite journal | vauthors = Arnsten AF, Girgis RR, Gray DL, Mailman RB | title = Novel Dopamine Therapeutics for Cognitive Deficits in Schizophrenia | journal = Biological Psychiatry | volume = 81 | issue = 1 | pages = 67–77 | date = January 2017 | pmid = 26946382 | pmc = 4949134 | doi = 10.1016/j.biopsych.2015.12.028 }}</ref><ref>{{cite journal | vauthors = Maia TV, Frank MJ | title = An Integrative Perspective on the Role of Dopamine in Schizophrenia | journal = Biological Psychiatry | volume = 81 | issue = 1 | pages = 52–66 | date = January 2017 | pmid = 27452791 | pmc = 5486232 | doi = 10.1016/j.biopsych.2016.05.021 }}</ref> | |||
| ===Social=== | |||
| Living in an ] environment has been consistently found to be a risk factor for schizophrenia.<ref name="fn_19" /><ref name="vanOs_et_al_2005">{{cite journal |author=van Os J, Krabbendam L, Myin-Germeys I, Delespaul P |title=The schizophrenia envirome |journal=Current Opinion in Psychiatry |volume=18 |issue=2 |pages=141–5 |year=2005 |month=March |pmid=16639166 |url=http://www.co-psychiatry.com/pt/re/copsych/abstract.00001504-200503000-00006.htm |accessdate=2008-07-06}}</ref> Social disadvantage has been found to be a risk factor, including poverty<ref>{{cite journal |author=Mueser KT, McGurk SR |year=2004 |title=Schizophrenia |journal=] |volume=363 |issue=9426 |pages=2063–72 |pmid=15207959 |doi=10.1016/S0140-6736(04)16458–1 |doi_brokendate=2009-12-08}}</ref> and migration related to social adversity, racial discrimination, family dysfunction, unemployment or poor housing conditions.<ref name="Selten_et_al_2007">{{cite journal |author=Selten JP, Cantor-Graae E, Kahn RS |year=2007 |month=March |title=Migration and schizophrenia |journal=Current Opinion in Psychiatry |volume=20 |issue=2 |pages=111–115 |pmid=17278906 |url=http://www.co-psychiatry.com/pt/re/copsych/abstract.00001504-200703000-00003.htm |accessdate=2008-07-06 |doi=10.1097/YCO.0b013e328017f68e}}</ref> Childhood experiences of abuse or trauma have also been implicated as risk factors for a diagnosis of schizophrenia later in life.<ref name="Schenkel_et_al_2005">{{cite journal |author=Schenkel LS |coauthors=Spaulding WD, Dilillo D, Silverstein SM |year=2005 |title=Histories of childhood maltreatment in schizophrenia: Relationships with premorbid functioning, symptomatology, and cognitive deficits |journal=] |volume=76 |issue=2–3 |pages=273–286 |pmid=15949659 |doi=10.1016/j.schres.2005.03.003}}</ref><ref name="Janssen_et_al_2004">{{cite journal |author=Janssen |coauthors=Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, van Os J |year=2004 |title=Childhood abuse as a risk factor for psychotic experiences |journal=] |volume=109 |pages=38–45 |pmid=14674957 |doi=10.1046/j.0001–690X.2003.00217.x |issue=1 |doi_brokendate=2009-12-08}}</ref> Parenting is not held responsible for schizophrenia but unsupportive dysfunctional relationships may contribute to an increased risk.<ref name="Bentall_et_al_2007"/><ref>{{cite journal |author=Subotnik, KL |coauthors=Goldstein, MJ, Nuechterlein, KH, Woo, SM and Mintz, J |year=2002 |title=Are Communication Deviance and Expressed Emotion Related to Family History of Psychiatric Disorders in Schizophrenia? |journal=] |volume=28 |issue=4 |pages=719–29 |pmid=12795501}}</ref> | |||
| The ] links alterations between ] and the ]s that affect ].<ref name=Pratt2017/> Studies have shown that a reduced expression of a ] – ], and glutamate blocking drugs such as ] and ] can mimic the symptoms and cognitive problems associated with schizophrenia.<ref name=Pratt2017>{{cite journal | vauthors = Pratt J, Dawson N, Morris BJ, Grent-'t-Jong T, Roux F, Uhlhaas PJ | title = Thalamo-cortical communication, glutamatergic neurotransmission and neural oscillations: A unique window into the origins of ScZ? | journal = Schizophrenia Research | volume = 180 | pages = 4–12 | date = February 2017 | pmid = 27317361 | doi = 10.1016/j.schres.2016.05.013 | s2cid = 205075178 | url = https://eprints.gla.ac.uk/132874/1/132874.pdf }}</ref><ref>{{cite journal | vauthors = Catts VS, Lai YL, Weickert CS, Weickert TW, Catts SV | title = A quantitative review of the post-mortem evidence for decreased cortical N-methyl-D-aspartate receptor expression levels in schizophrenia: How can we link molecular abnormalities to mismatch negativity deficits? | journal = Biological Psychology | volume = 116 | pages = 57–67 | date = April 2016 | pmid = 26549579 | doi = 10.1016/j.biopsycho.2015.10.013 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Michie PT, Malmierca MS, Harms L, Todd J | s2cid = 41179430 | title = The neurobiology of MMN and implications for schizophrenia | journal = Biological Psychology | volume = 116 | pages = 90–97 | date = April 2016 | pmid = 26826620 | doi = 10.1016/j.biopsycho.2016.01.011 }}</ref> Post-mortem studies consistently find that a subset of these neurons fail to express ] (]),<ref name = Marin2012>{{cite journal | vauthors = Marín O | s2cid = 205507186 | title = Interneuron dysfunction in psychiatric disorders | journal = Nature Reviews. Neuroscience | volume = 13 | issue = 2 | pages = 107–120 | date = January 2012 | pmid = 22251963 | doi = 10.1038/nrn3155 }}</ref> in addition to abnormalities in ]. The subsets of interneurons that are abnormal in schizophrenia are responsible for the synchronizing of neural ensembles needed during working memory tasks. These give the neural oscillations produced as ]s that have a frequency of between 30 and 80 ]. Both working memory tasks and gamma waves are impaired in schizophrenia, which may reflect abnormal interneuron functionality.<ref name = Marin2012 /><ref>{{cite journal | vauthors = Lewis DA, Hashimoto T, Volk DW | s2cid = 3335493 | title = Cortical inhibitory neurons and schizophrenia | journal = Nature Reviews. Neuroscience | volume = 6 | issue = 4 | pages = 312–324 | date = April 2005 | pmid = 15803162 | doi = 10.1038/nrn1648 }}</ref><ref>{{cite journal | vauthors = Senkowski D, Gallinat J | s2cid = 206104940 | title = Dysfunctional prefrontal gamma-band oscillations reflect working memory and other cognitive deficits in schizophrenia | journal = Biological Psychiatry | volume = 77 | issue = 12 | pages = 1010–1019 | date = June 2015 | pmid = 25847179 | doi = 10.1016/j.biopsych.2015.02.034 |quote=Several studies that investigated perceptual processes found impaired GBR in ScZ patients over sensory areas, such as the auditory and visual cortex. Moreover, studies examining steady-state auditory-evoked potentials showed deficits in the gen- eration of oscillations in the gamma band.}}</ref><ref>{{cite journal | vauthors = Reilly TJ, Nottage JF, Studerus E, Rutigliano G, Micheli AI, Fusar-Poli P, McGuire P | title = Gamma band oscillations in the early phase of psychosis: A systematic review | journal = Neuroscience and Biobehavioral Reviews | volume = 90 | pages = 381–399 | date = July 2018 | pmid = 29656029 | doi = 10.1016/j.neubiorev.2018.04.006 | quote = Decreased gamma power in response to a task was a relatively consistent finding, with 5 out of 6 studies reported reduced evoked or induced power. | s2cid = 4891072 | url = https://kclpure.kcl.ac.uk/portal/en/publications/e2f500b7-f358-433d-9f9c-7f6b9c52bb2f }}</ref> An important process that may be disrupted in neurodevelopment is astrogenesis – the formation of ]s. Astrocytes are crucial in contributing to the formation and maintenance of neural circuits and it is believed that disruption in this role can result in a number of neurodevelopmental disorders including schizophrenia.<ref name=Sloan2014>{{cite journal |vauthors=Sloan SA, Barres BA |title=Mechanisms of astrocyte development and their contributions to neurodevelopmental disorders |journal=Curr Opin Neurobiol |volume=27 |pages=75–81 |date=August 2014 |pmid=24694749 |pmc=4433289 |doi=10.1016/j.conb.2014.03.005 }}</ref> Evidence suggests that reduced numbers of astrocytes in deeper cortical layers are assocociated with a diminished expression of ], a ] in astrocytes; supporting the glutamate hypothesis.<ref name=Sloan2014/> | |||
| ===Substance Abuse=== | |||
| {{See also|Dual diagnosis}} | |||
| {{seealso|Schizophrenia and smoking}} | |||
| In a recent study of people with schizophrenia and a substance abuse disorder, over a ten year period, "substantial proportions were above cutoffs selected by dual diagnosis clients as indicators of recovery."<ref>http://schizophreniabulletin.oxfordjournals.org/cgi/content/abstract/32/3/464</ref> Although about half of all patients with schizophrenia use drugs or alcohol, a clear causal connection between drug use and schizophrenia has been difficult to prove. The two most often used explanations for this are "substance use causes schizophrenia" and "substance use is a consequence of schizophrenia", and they both may be correct.<ref>{{cite journal |author=Ferdinand RF, Sondeijker F, van der Ende J, Selten JP, Huizink A, Verhulst FC |year=2005 |title=Cannabis use predicts future psychotic symptoms, and vice versa |journal=] |volume=100 |issue=5 |pages=612–8 |doi=10.1111/j.1360–0443.2005.01070.x |pmid=15847618 |doi_brokendate=2009-12-08}}</ref> A 2007 ] estimated that cannabis use is ] with a ] increase in risk of development of psychotic disorders, including schizophrenia, though the authors admit that some uncertainty about ''causality'' still remains.<ref>{{cite journal |author=Moore THM, Zammit S, Lingford-Hughes A ''et al.'' |year=2007 |title= Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review |journal=Lancet |volume=370 |issue=9584 |pages=319–328 |doi=10.1016/S0140-6736(07)61162-3 |pmid=17662880}}</ref> There is little evidence to suggest that other drugs including alcohol cause schizophrenia, or that psychotic individuals choose specific drugs to self-medicate; there is some support for the hypothesis that they use drugs to cope with unpleasant states such as depression, anxiety, boredom and loneliness.<ref name="Gregg_et_al_2007">{{cite journal |author=Gregg L, Barrowclough C, Haddock G |year=2007 |title= Reasons for increased substance use in psychosis |journal= Clin Psychol Rev |volume=27 |issue=4 |pages=494–510 |pmid=17240501 |doi=10.1016/j.cpr.2006.09.004}}</ref> However, regarding ] itself, it is well understood that ] and ] use can result in methamphetamine- or cocaine-induced psychoses that present very similar symptomatology and may persist even when users remain abstinent.<ref>{{cite journal |author=Mahoney JJ, Kalechstein AD, De La Garza R, Newton TF |title=Presence and persistence of psychotic symptoms in cocaine- versus methamphetamine-dependent participants |journal=The American Journal on Addictions |volume=17 |issue=2 |pages=83–98 |year=2008 |pmid=18393050 |doi=10.1080/10550490701861201}}</ref> | |||
| Deficits in ]s, such as planning, inhibition, and working memory, are pervasive in schizophrenia. Although these functions are separable, their dysfunction in schizophrenia may reflect an underlying deficit in the ability to represent goal related information in working memory, and to use this to direct cognition and behavior.<ref>{{cite journal | vauthors = Lesh TA, Niendam TA, Minzenberg MJ, Carter CS | title = Cognitive control deficits in schizophrenia: mechanisms and meaning |journal=Neuropsychopharmacology | volume = 36 | issue = 1 | pages = 316–338 | date = January 2011 | pmid = 20844478 |pmc = 3052853 |doi =10.1038/npp.2010.156 }}</ref><ref>{{cite journal | vauthors = Barch DM, Ceaser A | title = Cognition in schizophrenia: core psychological and neural mechanisms | journal = Trends in Cognitive Sciences | volume = 16 | issue = 1 | pages = 27–34 | date = January 2012 | pmid = 22169777 | pmc = 3860986 | doi = 10.1016/j.tics.2011.11.015 }}</ref> These impairments have been linked to a number of neuroimaging and neuropathological abnormalities. For example, functional neuroimaging studies report evidence of reduced neural processing efficiency, whereby the dorsolateral prefrontal cortex is activated to a greater degree to achieve a certain level of performance relative to controls on working memory tasks. These abnormalities may be linked to the consistent post-mortem finding of reduced ], evidenced by increased ] density and reduced ] density. These cellular and functional abnormalities may also be reflected in structural neuroimaging studies that find reduced ] volume in association with deficits in working memory tasks.<ref>{{cite journal | vauthors = Eisenberg DP, Berman KF | title = Executive function, neural circuitry, and genetic mechanisms in schizophrenia | journal = Neuropsychopharmacology | volume = 35 |issue = 1 | pages = 258–277 | date = January 2010 | pmid = 19693005 | pmc = 2794926 | doi = 10.1038/npp.2009.111}}</ref> | |||
| ==Mechanisms== | |||
| ===Psychological=== | |||
| A number of psychological mechanisms have been implicated in the development and maintenance of schizophrenia. ]es that have been identified in those with a diagnosis or those at risk, especially when under stress or in confusing situations, include excessive attention to potential threats, jumping to conclusions, making external ], impaired reasoning about social situations and ], difficulty distinguishing inner speech from speech from an external source, and difficulties with early visual processing and maintaining concentration.<ref>{{cite journal |author=Broome MR |coauthors=Woolley JB, Tabraham P, Johns LC, Bramon E, Murray GK, Pariante C, McGuire PK, Murray RM |year=2005 |title=What causes the onset of psychosis? |journal=] |volume=79 | issue=1 |pages=23–34 |pmid=16198238 |doi=10.1016/j.schres.2005.02.007}}</ref><ref>{{cite journal |author= Lewis R|year=2004 |title=Should cognitive deficit be a diagnostic criterion for schizophrenia? |journal=Journal of Psychiatry and Neuroscience |volume=29 | issue=2 |pages=102–113 |pmid=15069464 |pmc= 383342}}</ref><ref>{{cite journal |author=Brune M |coauthors=Abdel-Hamid M, Lehmkamper C, Sonntag C |year=2007 |title=Mental state attribution, neurocognitive functioning, and psychopathology: What predicts poor social competence in schizophrenia best? |journal=] |volume=92| issue=1–2 |pages=151–9 |pmid=17346931 |doi=10.1016/j.schres.2007.01.006}}</ref><ref>{{cite journal |author=Sitskoorn MM |coauthors=Aleman A, Ebisch SJH, Appels MCM, Khan RS |year=2004 |title=Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis |journal=] |volume=71 | issue=2 |pages=285–295 |pmid= 15474899 |doi=10.1016/j.schres.2004.03.007}}</ref> Some cognitive features may reflect global ]s in ], ], ], ] or ], while others may be related to particular issues and experiences.<ref name="Bentall_et_al_2007">{{cite journal |author=Bentall RP |coauthors=Fernyhough C, Morrison AP, Lewis S, Corcoran R |year=2007 |title=Prospects for a cognitive-developmental account of psychotic experiences |journal=Br J Clin Psychol |volume=46 | issue=Pt 2 |pages=155–73 |pmid=17524210 | doi = 10.1348/014466506X123011}}</ref><ref name="Kurtz_2005">{{cite journal |author=Kurtz MM |year=2005 |title=Neurocognitive impairment across the lifespan in schizophrenia: an update |journal=] |volume=74 | issue=1 |pages=15–26 |pmid=15694750 |doi=10.1016/j.schres.2004.07.005}}</ref> | |||
| Positive symptoms have been linked to cortical thinning in the ].<ref>{{cite journal | vauthors = Walton E, Hibar DP, van Erp TG, Potkin SG, Roiz-Santiañez R, Crespo-Facorro B, Suarez-Pinilla P, Van Haren NE, de Zwarte SM, Kahn RS, Cahn W, Doan NT, Jørgensen KN, Gurholt TP, Agartz I, Andreassen OA, Westlye LT, Melle I, Berg AO, Mørch-Johnsen L, Faerden A, Flyckt L, Fatouros-Bergman H, Jönsson EG, Hashimoto R, Yamamori H, Fukunaga M, Preda A, De Rossi P, Piras F, Banaj N, Ciullo V, Spalletta G, Gur RE, Gur RC, Wolf DH, Satterthwaite TD, Beard LM, Sommer IE, Koops S, Gruber O, Richter A, Krämer B, Kelly S, Donohoe G, McDonald C, Cannon DM, Corvin A, Gill M, Di Giorgio A, Bertolino A, Lawrie S, Nickson T, Whalley HC, Neilson E, Calhoun VD, Thompson PM, Turner JA, Ehrlich S | title = Positive symptoms associate with cortical thinning in the superior temporal gyrus via the ENIGMA Schizophrenia consortium | journal = Acta Psychiatrica Scandinavica | volume = 135 | issue = 5 | pages = 439–447 | date = May 2017 | pmid = 28369804 | pmc = 5399182 | doi = 10.1111/acps.12718 }}</ref> The severity of negative symptoms has been linked to reduced thickness in the left medial ].<ref>{{cite journal | vauthors = Walton E, Hibar DP, van Erp TG, Potkin SG, Roiz-Santiañez R, Crespo-Facorro B, Suarez-Pinilla P, van Haren NE, de Zwarte SM, Kahn RS, Cahn W, Doan NT, Jørgensen KN, Gurholt TP, Agartz I, Andreassen OA, Westlye LT, Melle I, Berg AO, Morch-Johnsen L, Færden A, Flyckt L, Fatouros-Bergman H, Jönsson EG, Hashimoto R, Yamamori H, Fukunaga M, Jahanshad N, De Rossi P, Piras F, Banaj N, Spalletta G, Gur RE, Gur RC, Wolf DH, Satterthwaite TD, Beard LM, Sommer IE, Koops S, Gruber O, Richter A, Krämer B, Kelly S, Donohoe G, McDonald C, Cannon DM, Corvin A, Gill M, Di Giorgio A, Bertolino A, Lawrie S, Nickson T, Whalley HC, Neilson E, Calhoun VD, Thompson PM, Turner JA, Ehrlich S | title = Prefrontal cortical thinning links to negative symptoms in schizophrenia via the ENIGMA consortium | journal = Psychological Medicine | volume = 48 | issue = 1 | pages = 82–94 | date = January 2018 | pmid = 28545597 | pmc = 5826665 | doi = 10.1017/S0033291717001283 | collaboration = Karolinska Schizophrenia Project Consortium (KaSP) }}</ref> Anhedonia, traditionally defined as a reduced capacity to experience pleasure, is frequently reported in schizophrenia. However, a large body of evidence suggests that ] are intact in schizophrenia,<ref>{{cite journal | vauthors = Cohen AS, Minor KS | title = Emotional experience in patients with schizophrenia revisited: meta-analysis of laboratory studies | journal = Schizophrenia Bulletin | volume = 36 | issue = 1 | pages = 143–150 | date = January 2010 | pmid = 18562345 | pmc = 2800132 | doi = 10.1093/schbul/sbn061 }}</ref> and that what is reported to be anhedonia is a reflection of dysfunction in other processes related to reward.<ref>{{cite journal | vauthors = Strauss GP, Gold JM | title = A new perspective on anhedonia in schizophrenia | journal = The American Journal of Psychiatry | volume = 169 | issue = 4 | pages = 364–373 | date = April 2012 | pmid = 22407079 | pmc = 3732829 | doi = 10.1176/appi.ajp.2011.11030447 }}</ref> Overall, a failure of reward prediction is thought to lead to impairment in the generation of cognition and behavior required to obtain rewards, despite normal hedonic responses.<ref>{{cite book | vauthors = Young J, Anticevic A, Barch D | veditors = Charney D, Buxbaum J, Sklar P, Nestler E |title=Charney & Nestler's Neurobiology of Mental Illness |date=2018 |publisher=Oxford University Press. |location=New York |isbn=9780190681425 |pages=215, 217 |edition=5th |chapter=Cognitive and Motivational Neuroscience of Psychotic Disorders |quote=Several recent reviews (e.g., Cohen and Minor, 2010) have found that individuals with schizophrenia show relatively intact self-reported emotional responses to affect-eliciting stimuli as well as other indicators of intact response(215)...Taken together, the literature increasingly suggests that there may be a deficit in putatively DA-mediated reward learning and/ or reward prediction functions in schizophrenia. Such findings suggest that impairment in striatal reward prediction mechanisms may influence "wanting" in schizophrenia in a way that reduces the ability of individuals with schizophrenia to use anticipated rewards to drive motivated behavior.(217)}}</ref> | |||
| Despite a common appearance of "blunted affect", recent findings indicate that many individuals diagnosed with schizophrenia are emotionally responsive, particularly to stressful or negative stimuli, and that such sensitivity may cause vulnerability to symptoms or to the disorder.<ref name="schizophrenia1"/><ref>{{cite journal |author=Horan WP |coauthors=Blanchard JJ |year=2003 |title=Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping |journal=] |volume=60 | issue=2–3 |pages=271–83 |pmid=12591589 |doi=10.1016/S0920-9964(02)00227-X}}</ref><ref>{{cite journal |author=Barrowclough C |coauthors=Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B |year=2003 |title=Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology |journal=J Abnorm Psychol |volume=112 | issue=1 |pages=92–9 |pmid=12653417 | doi = 10.1037/0021–843X.112.1.92 |doi_brokendate=2009-12-08}}</ref><ref name="schizophrenia1">{{cite journal |author=Cohen AS |coauthors=Docherty NM |year=2004 |title=Affective reactivity of speech and emotional experience in patients with schizophrenia |journal=] |volume=69 | issue=1 |pages=7–14 |pmid=15145465 |doi=10.1016/S0920-9964(03)00069–0 |last2=Docherty |first2=NM |doi_brokendate=2009-12-08}}</ref> Some evidence suggests that the content of delusional beliefs and psychotic experiences can reflect emotional causes of the disorder, and that how a person interprets such experiences can influence symptomatology.<ref>{{cite journal |author=Birchwood M |coauthors=Meaden A, Trower P, Gilbert P, Plaistow J |year=2000 |title=The power and omnipotence of voices: subordination and entrapment by voices and significant others |journal=Psychol Med |volume=30 | issue=2 |pages=337–44 |pmid=10824654 | doi = 10.1017/S0033291799001828}}</ref><ref>{{cite journal |author=Smith B |coauthors=Fowler DG, Freeman D, Bebbington P, Bashforth H, Garety P, Dunn G, Kuipers E |year=2006 |title=Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations |journal=] |volume=86 | issue=1–3 |pages=181–8 |pmid=16857346 |doi=10.1016/j.schres.2006.06.018}}</ref><ref>{{cite journal |author=Beck, AT |year=2004 |title=A Cognitive Model of Schizophrenia |journal=Journal of Cognitive Psychotherapy |volume=18 | issue=3 |pages=281–88 | doi = 10.1891/jcop.18.3.281.65649}}</ref><ref>{{cite journal |author=Bell V |coauthors=Halligan PW, Ellis HD |year=2006 |title=Explaining delusions: a cognitive perspective |journal=] |volume=10 | issue=5 |pages=219–26 |pmid=16600666 |doi=10.1016/j.tics.2006.03.004}}</ref> The use of "]" to avoid imagined threats may contribute to the chronicity of delusions.<ref name="Freeman_BRT_2007">{{cite journal |author=Freeman D |coauthors=Garety PA, Kuipers E, Fowler D, Bebbington PE, Dunn G |year=2007 |title=Acting on persecutory delusions: the importance of safety seeking |journal=Behaviour Research and Therapy |volume=45 | issue=1 |pages=89–99 |pmid=16530161 |doi=10.1016/j.brat.2006.01.014}}</ref> Further evidence for the role of psychological mechanisms comes from the effects of ] on symptoms of schizophrenia.<ref>{{cite journal |author=Kuipers E |coauthors=Garety P, Fowler D, Freeman D, Dunn G, Bebbington P |year=2006 |title=Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms |journal=] |volume=32 | issue=Suppl 1 |pages=S24–31 |pmid=16885206 |doi=10.1093/schbul/sbl014 |pmc=2632539}}</ref> | |||
| Another theory links abnormal ] to the development of ] which is significantly more common in those with schizophrenia.<ref name=Wilberg2019>{{cite journal | vauthors = Wiberg A, Ng M, Al Omran Y, Alfaro-Almagro F, McCarthy P, Marchini J, Bennett DL, Smith S, Douaud G, Furniss D | title = Handedness, language areas and neuropsychiatric diseases: insights from brain imaging and genetics | journal = Brain | volume = 142 | issue = 10 | pages = 2938–2947 | date = October 2019 | pmid = 31504236 | pmc = 6763735 | doi = 10.1093/brain/awz257 }}</ref> This abnormal development of hemispheric asymmetry is noted in schizophrenia.<ref>{{cite book |vauthors=Tzourio-Mazoyer N, Kennedy H, Van Essen DC, Christen Y |title=Micro-, Meso- and Macro-Connectomics of the Brain |chapter=Intra- and Inter-hemispheric Connectivity Supporting Hemispheric Specialization |series=Research and Perspectives in Neurosciences |date=2016 |pages=129–146 |doi=10.1007/978-3-319-27777-6_9 |pmid=28590670|isbn=978-3-319-27776-9 |s2cid=147813648 }}</ref> Studies have concluded that the link is a true and verifiable effect that may reflect a genetic link between lateralization and schizophrenia.<ref name=Wilberg2019/><ref>{{cite journal | vauthors = Ocklenburg S, Güntürkün O, Hugdahl K, Hirnstein M | title = Laterality and mental disorders in the postgenomic age—A closer look at schizophrenia and language lateralization | journal = Neuroscience and Biobehavioral Reviews | volume = 59 | pages = 100–110 | date = December 2015 | pmid = 26598216 | doi = 10.1016/j.neubiorev.2015.08.019 | s2cid = 15983622 }}</ref> | |||
| ===Neural=== | |||
| Studies using ]s and ] technologies such as ] and ] to examine functional differences in brain activity have shown that differences seem to most commonly occur in the ]s, ] and ]s.<ref>{{cite book|year=2006|last=Kircher|first=Tilo|coauthors=Renate Thienel|title=The Boundaries of Consciousness|isbn=0444528768|page=302|url=http://books.google.com/books?hl=en&lr=&id=YHGacGKyVbYC&oi=fnd&pg=PA302|chapter=Functional brain imaging of symptoms and cognition in schizophrenia|publisher=Elsevier|location=Amsterdam}}</ref> These differences have been linked to the ]s often associated with schizophrenia.<ref name="Green2006">{{cite journal |author=Green MF|year=2006|title=Cognitive impairment and functional outcome in schizophrenia and bipolar disorder|journal=Journal of Clinical Psychiatry |volume=67 | issue=Suppl 9 |pages=3–8|pmid=16965182}}</ref> | |||
| ] have been used to link abnormalities in cellular functioning to symptoms.<ref>{{cite journal | vauthors = Friston KJ, Stephan KE, Montague R, Dolan RJ | title = Computational psychiatry: the brain as a phantastic organ | journal = The Lancet. Psychiatry | volume = 1 | issue = 2 | pages = 148–158 | date = July 2014 | pmid = 26360579 | doi = 10.1016/S2215-0366(14)70275-5 | s2cid = 15504512 }}</ref><ref>{{cite journal | vauthors = Griffin JD, Fletcher PC | title = Predictive Processing, Source Monitoring, and Psychosis | journal = Annual Review of Clinical Psychology | volume = 13 | pages = 265–289 | date = May 2017 | pmid = 28375719 | pmc = 5424073 | doi = 10.1146/annurev-clinpsy-032816-045145}}</ref> Both hallucinations and delusions have been suggested to reflect improper encoding of ], thereby causing expectation to excessively influence sensory perception and the formation of beliefs. In approved models of ] that mediate ], reduced NMDA receptor activation, could in theory result in the positive symptoms of delusions and hallucinations.<ref>{{cite journal | vauthors = Fletcher PC, Frith CD | s2cid = 6219485 | title = Perceiving is believing: a Bayesian approach to explaining the positive symptoms of schizophrenia | journal = Nature Reviews. Neuroscience | volume = 10 | issue = 1 | pages = 48–58 | date = January 2009 | pmid = 19050712 | doi = 10.1038/nrn2536 | url = https://pure.au.dk/ws/files/48560345/fletcher_frithNRN.pdf }}</ref><ref>{{cite journal | vauthors = Corlett PR, Taylor JR, Wang XJ, Fletcher PC, Krystal JH | title = Toward a neurobiology of delusions | journal = Progress in Neurobiology | volume = 92 | issue = 3 | pages = 345–369 | date = November 2010 | pmid = 20558235 | pmc = 3676875 | doi = 10.1016/j.pneurobio.2010.06.007 }}</ref><ref>{{cite journal | vauthors = Bastos AM, Usrey WM, Adams RA, Mangun GR, Fries P, Friston KJ | title = Canonical microcircuits for predictive coding | journal = Neuron | volume = 76 | issue = 4 | pages = 695–711 | date = November 2012 | pmid = 23177956 | pmc = 3777738 | doi = 10.1016/j.neuron.2012.10.038 }}</ref> | |||
| ] and other ] technologies allow for the study of differences in brain activity among people diagnosed with schizophrenia]] | |||
| Particular focus has been placed upon the function of dopamine in the ] of the brain. This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the ], could reduce psychotic symptoms. It is also supported by the fact that ]s, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia.<ref name="Laruelle_et_al_1996">{{cite journal |author=Laruelle M |coauthors=Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J, McCance E, Rosenblatt W, Fingado C, Zoghbi SS, Baldwin RM, Seibyl JP, Krystal JH, Charney DS, Innis RB |year=1996 |title=Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects |journal=Proceedings of the National Academy of Sciences of the USA |volume=93 |doi= 10.1073/pnas.93.17.9235 |pages=9235–40 |pmid=8799184 |issue=17 |pmc=38625}}</ref> An influential theory, known as the ], proposed that excess activation of ] was the cause of (the positive symptoms of) schizophrenia. Although postulated for about 20 years based on the D<sub>2</sub> blockade effect common to all antipsychotics, it was not until the mid-1990s that ] and ] imaging studies provided supporting evidence. This explanation is now thought to be simplistic, partly because newer antipsychotic medication (called ] medication) can be equally effective as older medication (called ] medication), but also affects ] function and may have slightly less of a ] blocking effect.<ref name="JonesPilowsky2002">{{cite journal |author=Jones HM |coauthors=Pilowsky LS |year=2002 |title=Dopamine and antipsychotic drug action revisited |journal=] |volume=181 |pages=271–275 |pmid=12356650 |doi=10.1192/bjp.181.4.271}}</ref> | |||
| ==Diagnosis== | |||
| Interest has also focused on the neurotransmitter ] and the reduced function of the ] in schizophrenia. This has largely been suggested by abnormally low levels of ]s found in postmortem brains of people previously diagnosed with schizophrenia<ref name="fn_27">{{cite journal |author=Konradi C |coauthors=Heckers S |year=2003 |title=Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment |journal=Pharmacology and Therapeutics |volume=97 |issue=2 |pages=153–79 |pmid=12559388 |doi=10.1016/S0163-7258(02)00328–5 |doi_brokendate=2009-12-08}}</ref> and the discovery that the glutamate blocking drugs such as ] and ] can mimic the symptoms and cognitive problems associated with the condition.<ref name="fn_59">{{cite journal |author=Lahti AC |coauthors=Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA |year=2001 |title=Effects of ketamine in normal and schizophrenic volunteers |journal=] |volume=25 |issue=4 |pages=455–67 |pmid=11557159 |doi=10.1016/S0893-133X(01)00243–3 |doi_brokendate=2009-12-08}}</ref> The fact that reduced glutamate function is linked to poor performance on tests requiring ] and ] function and that glutamate can affect ] function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia.<ref name="fn_28">{{cite journal |author=Coyle JT |coauthors=Tsai G, Goff D |year=2003 |title=Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia |journal=Annals of the ] |volume=1003 |pages=318–27 |pmid=14684455 |doi=10.1196/annals.1300.020}}</ref> Positive symptoms fail however to respond to glutamatergic medication.<ref name="fn_60">{{cite journal |author=Tuominen HJ |coauthors=Tiihonen J, Wahlbeck K |year=2005 |title=Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis |journal=] |volume=72 |pages=225–34 |pmid=15560967 |doi=10.1016/j.schres.2004.05.005 |issue=2-3}}</ref> | |||
| {{Main|Diagnosis of schizophrenia}} | |||
| ===Criteria=== | |||
| There have also been findings of differences in the size and structure of certain brain areas in schizophrenia. A 2006 metaanlaysis of MRI studies found that whole brain and ] volume are reduced and that ] volume is increased in patients with a first psychotic episode relative to healthy controls. The average volumetric changes in these studies are however close to the limit of detection by MRI methods, so it remains to be determined whether schizophrenia is a neurodegenerative process that begins at about the time of symptom onset, or whether it is better characterised as a neurodevelopmental process that produces abnormal brain volumes at an early age.<ref name="pmid16738340">{{cite journal |author=Steen RG, Mull C, McClure R, Hamer RM, Lieberman JA |title=Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies |journal=] |volume=188 |pages=510–8 |year=2006 |month=June |pmid=16738340 |doi=10.1192/bjp.188.6.510 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=16738340}}</ref> In first episode psychosis typical antipsychotics like haloperidol were associated with significant reductions in gray matter volume, whereas atypical antipsychotics like olanzapine were not.<ref name="pmid18922967">{{cite journal |author=Lieberman JA, Bymaster FP, Meltzer HY, Deutch AY, Duncan GE, Marx CE, Aprille JR, Dwyer DS, Li XM, Mahadik SP, Duman RS, Porter JH, Modica-Napolitano JS, Newton SS, Csernansky JG |title=Antipsychotic drugs: comparison in animal models of efficacy, neurotransmitter regulation, and neuroprotection |journal=] |volume=60 |issue=3 |pages=358–403 |year=2008 |month=September |pmid=18922967 |doi=10.1124/pr.107.00107 }}</ref> Studies in non-human primates found gray and white matter reductions for both typical and atypical antipsychotics.<ref name="pmid18263882">{{cite journal |author=DeLisi LE |title=The concept of progressive brain change in schizophrenia: implications for understanding schizophrenia |journal=] |volume=34 |issue=2 |pages=312–21 |year=2008 |month=March |pmid=18263882 |doi=10.1093/schbul/sbm164 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=18263882 |pmc=2632405}}</ref> | |||
| Schizophrenia is diagnosed based on criteria in either the '']'' (DSM) published by the ] or the ] (ICD) published by the ] (WHO). These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by a ]. The ] is an important part of the assessment.<ref>{{cite journal | vauthors = Soltan M, Girguis J | title = How to approach the mental state examination | url = https://www.bmj.com/content/357/sbmj.j1821 | journal = BMJ | volume = 357 | page = j1821 | access-date = 9 January 2020 | doi = 10.1136/sbmj.j1821 | pmid = 31055448 | date = 8 May 2017| s2cid = 145820368 }}</ref> An established tool for assessing the severity of positive and negative symptoms is the Positive and Negative Syndrome Scale (PANSS).<ref>{{cite journal | vauthors = Lindenmayer JP | title = Are Shorter Versions of the Positive and Negative Syndrome Scale (PANSS) Doable? A Critical Review. | journal = Innovations in Clinical Neuroscience | date = 1 December 2017 | volume = 14 | issue = 11–12 |pages=73–76 | pmid = 29410940| pmc = 5788254 }}</ref> This has been seen to have shortcomings relating to negative symptoms, and other scales – the ''Clinical Assessment Interview for Negative Symptoms'' (CAINS), and the ''Brief Negative Symptoms Scale'' (BNSS) have been introduced.<ref name=Marder2014/> The ], published in 2013, gives a ''Scale to Assess the Severity of Symptom Dimensions'' outlining eight dimensions of symptoms.<ref name=Biedermann2016/> | |||
| DSM-5 states that to be diagnosed with schizophrenia, two diagnostic criteria have to be met over the period of one month, with a significant impact on social or occupational functioning for at least six months. One of the symptoms needs to be either delusions, hallucinations, or disorganized speech. A second symptom could be one of the negative symptoms, or severely disorganized or ].<ref name=DSM5/> A different diagnosis of ] can be made before the six months needed for the diagnosis of schizophrenia.<ref name=DSM5/> | |||
| A 2009 meta-analysis of ] studies identified two consistent locations of reduced ] (roughly the level of organization of neural connections) in schizophrenia. The authors suggest that two networks of ] tracts may be affected in schizophrenia, with the potential for "disconnection" of the ] regions which they link.<ref name="pmid19128945">{{cite journal |author=Ellison-Wright I, Bullmore E |title=Meta-analysis of diffusion tensor imaging studies in schizophrenia |journal=] |volume=108 |issue=1–3 |pages=3–10 |year=2009 |month=March |pmid=19128945 |doi=10.1016/j.schres.2008.11.021 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920-9964(08)00527–6}}</ref> During ] studies, greater connectivity in the brain's ] and ] has been observed in patients diagnosed with schizophrenia, and may reflect excessive attentional orientation toward ] and toward ], respectively. The greater anti-correlation between the two networks suggests excessive rivalry between the networks.<ref>{{cite journal |author= Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJS |title= Default-mode brain dysfunction in mental disorders: a systematic review |journal= Neurosci Biobehav Rev |year=2008 |pmid=18824195 |doi=10.1016/j.neubiorev.2008.09.002 |volume= 33 |pages= 279 |issue= 3}}</ref> | |||
| In Australia, the guideline for diagnosis is for six months or more with symptoms severe enough to affect ordinary functioning.<ref>{{cite web |title=Diagnosis of schizophrenia |url=https://www.healthdirect.gov.au/diagnosis-of-schizophrenia |publisher= Australian Department of Health |access-date=28 January 2020 |date=10 January 2019}}</ref> In the UK diagnosis is based on having the symptoms for most of the time for one month, with symptoms that significantly affect the ability to work, study, or carry on ordinary daily living, and with other similar conditions ruled out.<ref>{{cite web |title=Schizophrenia – Diagnosis |url=https://www.nhs.uk/conditions/schizophrenia/diagnosis/ |publisher= UK ] |access-date=28 January 2020 |date=23 October 2017}}</ref> | |||
| ==Screening and prevention== | |||
| There are no reliable markers for the later development of schizophrenia although research is being conducted into how well a combination of genetic risk plus non-disabling psychosis-like experience predicts later diagnosis.<ref name="Cannon_et_al_2007">{{cite journal |author=Cannon TD, Cornblatt B, McGorry P |title=The empirical status of the ultra high-risk (prodromal) research paradigm |journal=Schizophrenia Bulletin |volume=33 |issue=3 |pages=661–4 |year=2007 |month=May |pmid=17470445 |doi=10.1093/schbul/sbm031 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17470445 |accessdate=2008-07-06 |pmc=2526144}}</ref> People who fulfill the 'ultra high-risk mental state' criteria, that include a family history of schizophrenia plus the presence of transient or self-limiting psychotic experiences, have a 20–40% chance of being diagnosed with the condition after one year.<ref name="Drake_Lewis_2005">{{cite journal |author=Drake RJ, Lewis SW |title=Early detection of schizophrenia |journal=Current Opinion in Psychiatry |volume=18 |issue=2 |pages=147–50 |year=2005 |month=March |pmid=16639167|url=http://www.co-psychiatry.com/pt/re/copsych/abstract.00001504-200503000-00007.htm |accessdate=2008-07-06 |doi=10.1097/00001504-200503000-00007}}</ref> The use of psychological treatments and medication has been found effective in reducing the chances of people who fulfill the 'high-risk' criteria from developing full-blown schizophrenia.<ref name="vanOs_Delespaul_2005">{{cite journal |author=Van Os J, Delespaul P |title=Toward a world consensus on prevention of schizophrenia |journal=Dialogues Clin Neurosci |volume=7 |issue=1 |pages=53–67 |year=2005 |pmid=16060596}}</ref> However, the treatment of people who may never develop schizophrenia is controversial,<ref>{{Cite journal | last1 = McGorry | first1 = PD. | last2 = Yung | first2 = A. | last3 = Phillips | first3 = L. | title = Ethics and early intervention in psychosis: keeping up the pace and staying in step. | journal = Schizophr Res | volume = 51 | issue = 1 | pages = 17–29 | month = Aug | year = 2001 | pmid = 11479062 | doi = 10.1016/S0920-9964(01)00235-3 }}</ref> in light of the side-effects of antipsychotic medication; particularly with respect to the potentially disfiguring ] and the rare but potentially lethal ].<ref name="Haroun_et_al_2006">{{cite journal |author=Haroun N, Dunn L, Haroun A, Cadenhead KS |title=Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research |journal=Schizophrenia Bulletin |volume=32 |issue=1 |pages=166–78 |year=2006 |month=January |pmid=16207892 |doi=10.1093/schbul/sbj007 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16207892 |accessdate=2008-07-06 |pmc=2632176}}</ref> The most widely used form of preventative health care for schizophrenia takes the form of public education campaigns that provide information on risk factors and early symptoms, with the aim to improve detection and provide treatment earlier for those experiencing delays.<ref name="Hafner_et_al_2004">{{cite journal |author=Häfner H, Maurer K, Ruhrmann S, ''et al.'' |title=Early detection and secondary prevention of psychosis: facts and visions |journal=European Archives of Psychiatry and Clinical Neuroscience |volume=254 |issue=2 |pages=117–28 |year=2004 |month=April |pmid=15146341 |doi=10.1007/s00406-004-0508-z |accessdate=2008-07-06}}</ref> The new clinical approach ] is a secondary ] strategy to prevent further episodes and prevent the long term disability associated with schizophrenia. | |||
| The ICD criteria are typically used in European countries; the DSM criteria are used predominantly in the United States and Canada, and are prevailing in research studies. In practice, agreement between the two systems is high.<ref>{{cite journal | vauthors = Jakobsen KD, Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T | title = Reliability of clinical ICD-10 schizophrenia diagnoses | journal = Nordic Journal of Psychiatry | volume = 59 | issue = 3 | pages = 209–212 | year = 2005 | pmid = 16195122 | doi = 10.1080/08039480510027698 | s2cid = 24590483 }}</ref> The current proposal for the ] criteria for schizophrenia recommends adding self-disorder as a symptom.<ref name=Heinz2016/> | |||
| ==Management== | |||
| {{Main|Treatment of schizophrenia}} | |||
| ], which revolutionized treatment of schizophrenia in the 1950s]] | |||
| The concept of a cure as such remains controversial, as there is no consensus on the definition, although some criteria for the remission of symptoms have recently been suggested.<ref name="fn_63">{{Cite journal | last1 = van Os | first1 = J. | last2 = Burns | first2 = T. | last3 = Cavallaro | first3 = R. | last4 = Leucht | first4 = S. | last5 = Peuskens | first5 = J. | last6 = Helldin | first6 = L. | last7 = Bernardo | first7 = M. | last8 = Arango | first8 = C. | last9 = Fleischhacker | first9 = W. | title = Standardized remission criteria in schizophrenia. | journal = Acta Psychiatr Scand | volume = 113 | issue = 2 | pages = 91–5 | month = Feb | year = 2006 | doi = 10.1111/j.1600-0447.2005.00659.x | pmid = 16423159 }}</ref> <!-- and they are...?--> The effectiveness of schizophrenia treatment is often assessed using standardized methods, one of the most common being the ] (PANSS).<ref name="fn_68">{{Cite journal | last1 = Kay | first1 = SR. | last2 = Fiszbein | first2 = A. | last3 = Opler | first3 = LA. | title = The positive and negative syndrome scale (PANSS) for schizophrenia. | journal = Schizophr Bull | volume = 13 | issue = 2 | pages = 261–76 | year = 1987 | pmid = 3616518 }}</ref> | |||
| Management of symptoms and improving function is thought to be more achievable than a cure. Treatment was revolutionized in the mid-1950s with the development and introduction of ].<ref name="Turner2007">{{cite journal | author=Turner T. | title=Unlocking psychosis | journal=Brit J Med | year=2007 | volume=334 | issue=suppl | pages=s7 | doi=10.1136/bmj.39034.609074.94 | pmid=17204765 }}</ref> A ] is increasingly adopted, emphasizing hope, empowerment and social inclusion.<ref name="Bellack06">{{cite journal |author=Bellack AS |title=Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications |journal=Schizophrenia Bulletin |volume=32 |issue=3 |pages=432–42 |year=2006 |month=July |pmid=16461575 |pmc=2632241 |doi=10.1093/schbul/sbj044}}</ref> | |||
| A major unresolved difference between the two diagnostic systems is that of the requirement in DSM of an impaired functional outcome. WHO for ICD argues that not all people with schizophrenia have functional deficits and so these are not specific for the diagnosis.<ref name=Biedermann2016/> | |||
| Hospitalization may occur with severe episodes of schizophrenia. This can be voluntary or (if mental health legislation allows it) involuntary (called civil or ]). Long-term inpatient stays are now less common due to ], although can still occur.<ref name="BeckerKilian2006" /> Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or ] team, supported employment<ref>{{Cite journal | last1 = McGurk | first1 = SR. | last2 = Mueser | first2 = KT. | last3 = Feldman | first3 = K. | last4 = Wolfe | first4 = R. | last5 = Pascaris | first5 = A. | title = Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. | journal = Am J Psychiatry | volume = 164 | issue = 3 | pages = 437–41 | month = Mar | year = 2007 | url = http://ajp.psychiatryonline.org/cgi/content/full/164/3/437 | doi = 10.1176/appi.ajp.164.3.437 | pmid = 17329468 }}</ref> and patient-led support groups. | |||
| === Neuroimaging techniques === | |||
| In many non-Western societies, schizophrenia may only be treated with more informal, community-led methods. Multiple international surveys by the World Health Organization over several decades have indicated that the outcome for people diagnosed with schizophrenia in non-Western countries is on average better there than for people in the West.<ref name="fn_41">{{Cite journal | last1 = Kulhara | first1 = P. | title = Outcome of schizophrenia: some transcultural observations with particular reference to developing countries. | journal = Eur Arch Psychiatry Clin Neurosci | volume = 244 | issue = 5 | pages = 227–35 | year = 1994 | pmid = 7893767 | doi = 10.1007/BF02190374 }}</ref> Many clinicians and researchers suspect the relative levels of social connectedness and acceptance are the difference,<ref> {{cite web |url=http://www.washingtonpost.com/wp-dyn/content/article/2005/06/26/AR2005062601091.html |title=Social Network's Healing Power Is Borne Out in Poorer Nations |author=Shankar Vedantam |date=27 June 2005 |publisher=Washington Post |location=USA }}</ref> although further ] are seeking to clarify the findings. | |||
| ] has become a tool in understanding brain activity and connectivity differences in individuals with schizophrenia. Through resting-state fMRI, researchers have observed altered connectivity patterns within several key brain networks, such as the default mode network (DMN),<ref>{{Cite journal |last1=Whitfield-Gabrieli |first1=Susan |last2=Ford |first2=Judith M. |date=2012-04-27 |title=Default Mode Network Activity and Connectivity in Psychopathology |url=https://www.annualreviews.org/doi/10.1146/annurev-clinpsy-032511-143049 |journal=Annual Review of Clinical Psychology |language=en |volume=8 |issue=1 |pages=49–76 |doi=10.1146/annurev-clinpsy-032511-143049 |pmid=22224834 |issn=1548-5943}}</ref> salience network (SN),<ref>{{Cite journal |last=Menon |first=Vinod |date=October 2011 |title=Large-scale brain networks and psychopathology: a unifying triple network model |url=https://linkinghub.elsevier.com/retrieve/pii/S1364661311001719 |journal=Trends in Cognitive Sciences |language=en |volume=15 |issue=10 |pages=483–506 |doi=10.1016/j.tics.2011.08.003|pmid=21908230 }}</ref> and central executive network (CEN).<ref>{{Cite journal |last1=Baker |first1=Justin T. |last2=Holmes |first2=Avram J. |last3=Masters |first3=Grace A. |last4=Yeo |first4=B. T. Thomas |last5=Krienen |first5=Fenna |last6=Buckner |first6=Randy L. |last7=Öngür |first7=Dost |date=2014-02-01 |title=Disruption of Cortical Association Networks in Schizophrenia and Psychotic Bipolar Disorder |journal=JAMA Psychiatry |language=en |volume=71 |issue=2 |pages=109–118 |doi=10.1001/jamapsychiatry.2013.3469 |issn=2168-622X |pmc=4435541 |pmid=24306091}}</ref> Alterations may underlie cognitive and emotional symptoms in schizophrenia, such as disorganized thinking, impaired attention, and emotional dysregulation. | |||
| === |
===Comorbidities=== | ||
| ] showing overlapping ]s in genes associated with ] of ] (ASD), ], ] and schizophrenia: | |||
| The first line psychiatric treatment for schizophrenia is ] medication.<ref name="fn_72">{{cite web |url=http://www.nice.org.uk/nicemedia/pdf/CG82FullGuideline.pdf |format=PDF|title=Schizophrenia: Full national clinical guideline on core interventions in primary and secondary care |accessdate=2009-11-25 |author=National Collaborating Centre for Mental Health |date=2009-03-25 |publisher=Gaskell and the British Psychological Society}}</ref> These can reduce the positive symptoms of psychosis. Most antipsychotics take around 7–14 days to have their main effect. Currently available antipsychotics fail, however, to significantly ameliorate the negative symptoms, and the improvements on cognition may be attributed to the practice effect.<ref name="pmid16930948">{{cite journal |author=Murphy BP, Chung YC, Park TW, McGorry PD |title=Pharmacological treatment of primary negative symptoms in schizophrenia: a systematic review |journal=] |volume=88 |issue=1–3 |pages=5–25 |year=2006 |month=December |pmid=16930948 |doi=10.1016/j.schres.2006.07.002 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920-9964(06)00311–2}}</ref><ref name="pmid17667958">{{cite journal |author=Gray JA, Roth BL |title=The pipeline and future of drug development in schizophrenia |journal=] |volume=12 |issue=10 |pages=904–22 |year=2007 |month=October |pmid=17667958 |doi=10.1038/sj.mp.4002062}}</ref><ref name="pmid16903799">{{cite journal |author=Jarskog LF, Miyamoto S, Lieberman JA |title=Schizophrenia: new pathological insights and therapies |journal=] |volume=58 |pages=49–61 |year=2007 |pmid=16903799 |doi=10.1146/annurev.med.58.060904.084114 |url=http://arjournals.annualreviews.org/doi/abs/10.1146/annurev.med.58.060904.084114?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov}}</ref><ref name="pmid18291627">{{cite journal |author=Tandon R, Keshavan MS, Nasrallah HA |title=Schizophrenia, "Just the Facts": what we know in 2008 part 1: overview |journal=] |volume=100 |issue=1-3 |pages=4–19 |year=2008 |month=March |pmid=18291627 |doi=10.1016/j.schres.2008.01.022 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920-9964(08)00071-6}}</ref> | |||
| {{legend|#007fff|Genes associated with epilepsy}} | |||
| {{legend|#007f7f|Genes associated with schizophrenia}} | |||
| {{legend|#d4aaff|Genes associated with autism spectrum disorder}} | |||
| {{legend|#ff0000|Genes associated with dystonia}}]] | |||
| Many people with schizophrenia may have one or more ], such as ], ], or substance use disorder. These are separate disorders that require treatment.<ref name=DSM5/> When comorbid with schizophrenia, substance use disorder and ] both increase the risk for violence.<ref name=Richard-Devantoy2009/> Comorbid substance use disorder also increases the risk of suicide.<ref name=Khokhar2018/> | |||
| ]s often co-occur with schizophrenia, and may be an early sign of relapse.<ref name=Staedt2010/> Sleep disorders are linked with positive symptoms such as ] and can adversely affect ] and cognition.<ref name=Staedt2010>{{cite journal |vauthors=Staedt J, Hauser M, Gudlowski Y, Stoppe G |title=Sleep disorders in schizophrenia |journal=Fortschritte der Neurologie-Psychiatrie |volume=78 |issue=2 |pages=70–80 |date=February 2010 |pmid=20066610 |doi=10.1055/s-0028-1109967|s2cid=260137215 }}</ref> The consolidation of memories is disrupted in sleep disorders.<ref name=Pocivavsek2018/> They are associated with severity of illness, a poor prognosis, and poor quality of life.<ref name=Monti2013/><ref>{{cite journal |vauthors=Faulkner SM, Bee PE, Meyer N, Dijk DJ, Drake RJ |title=Light therapies to improve sleep in intrinsic circadian rhythm sleep disorders and neuro-psychiatric illness: A systematic review and meta-analysis |journal=Sleep Medicine Reviews |volume=46 |pages=108–123 |date=August 2019 |pmid=31108433|doi=10.1016/j.smrv.2019.04.012|doi-access=free }}</ref> Sleep onset and maintenance insomnia is a common symptom, regardless of whether treatment has been received or not.<ref name=Monti2013>{{cite journal | vauthors = Monti JM, BaHammam AS, Pandi-Perumal SR, Bromundt V, Spence DW, Cardinali DP, Brown GM | title = Sleep and circadian rhythm dysregulation in schizophrenia | journal = Progress in Neuro-Psychopharmacology & Biological Psychiatry | volume = 43 | pages = 209–216 | date = June 2013 | pmid = 23318689 | doi = 10.1016/j.pnpbp.2012.12.021 | hdl-access = free | s2cid = 19626589 | hdl = 11336/3858 }}</ref> Genetic variations have been found associated with these conditions involving the ], dopamine and ], and signal transduction.<ref>{{cite journal | vauthors = Assimakopoulos K, Karaivazoglou K, Skokou M, Kalogeropoulou M, Kolios P, Gourzis P, Patrinos GP, Tsermpini EE | title = Genetic Variations Associated with Sleep Disorders in Patients with Schizophrenia: A Systematic Review | journal = Medicines | volume = 5 | issue = 2 | page = 27 | date = March 2018 | pmid = 29587340 | pmc = 6023503 | doi = 10.3390/medicines5020027 | doi-access = free }}</ref> | |||
| ] (trade name Risperdal) is a common ] medication]] | |||
| The newer ] drugs are usually preferred for ] over the older ], although they are expensive and are more likely to induce weight gain and ]-related diseases.<ref name="fn_62">{{cite journal |author=Lieberman JA, Stroup TS, McEvoy JP, ''et al.'' |title=Effectiveness of antipsychotic drugs in patients with chronic schizophrenia |journal=New England Journal of Medicine |volume=353 |issue=12 |pages=1209–23 |year=2005 |month=September |pmid=16172203 |doi=10.1056/NEJMoa051688 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=16172203&promo=ONFLNS19 |accessdate=2008-07-04}}</ref> In 2008, results from a major randomized trial sponsored by the US National Institute of Mental Health (Clinical Antipsychotic Trials of Intervention Effectiveness, or CATIE) found that a representative first-generation antipsychotic, perphenazine, was as effective as and more cost-effective than several newer drugs (olanzapine, perphenazine, quetiapine, risperidone, or ziprasidone) taken for up to 18 months. The atypical antipsychotic which patients were willing to continue for the longest, olanzapine, was associated with considerable weight gain and risk of metabolic syndrome. ] was most effective for people with a poor response to other drugs, but it had troublesome side effects. Because the trial excluded patients with ], its relevance to these people is unclear.<ref>{{cite journal |author=Swartz MS, Stroup TS ''et al.'' |title=What CATIE Found: Results From the Schizophrenia Trial |journal=Psychiatr Serv |volume=59 |pages=500–506 |year=2008 |doi=10.1176/appi.ps.59.5.500|url=http://ps.psychiatryonline.org/cgi/content/full/59/5/500 |pmid=18451005 |issue=5}}</ref> | |||
| Schizophrenia is also associated with a number of somatic comorbidities including ], ]s, and ]s. The association of these with schizophrenia may be partially due to medications (e.g. ] from antipsychotics), environmental factors (e.g. complications from an increased rate of cigarette smoking), or associated with the disorder itself (e.g. diabetes mellitus type 2 and some cardiovascular diseases are thought to be genetically linked). These somatic comorbidities contribute to reduced life expectancy among persons with the disorder.<ref>{{cite journal |vauthors=Dieset I, Andreassen O, Haukvik U|title=Somatic Comorbidity in Schizophrenia: Some Possible Biological Mechanisms Across the Life Span |journal= Schizophrenia Bulletin|volume=42 |issue=6 |date=2016 |pages=1316–1319 | pmid=27033328|doi=10.1093/schbul/sbw028 |pmc=5049521 |doi-access=free }}</ref> | |||
| Because of their reportedly lower risk of side effects that affect mobility, atypical antipsychotics have been first-line treatment for early-onset schizophrenia for many years before certain drugs in this class were approved by the ] for use in children and teenagers with schizophrenia. This advantage comes at the cost of an increased risk of ] and ], which is of concern in the context of long-term use begun at an early age. Especially in the case of children and teenagers who have schizophrenia, medication should be used in combination with individual therapy and family-based interventions.<ref name=Cullen/> | |||
| ===Differential diagnosis=== | |||
| Recent reviews have refuted the claim that atypical antipsychotics have fewer extrapyramidal side effects than typical antipsychotics, especially when the latter are used in low doses or when low potency antipsychotics are chosen.<ref name="fn_36">{{cite journal |author=Leucht S, Wahlbeck K, Hamann J, Kissling W |title=New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis |journal=Lancet |volume=361 |issue=9369 |pages=1581–89 |year=2003 |month=May |pmid=12747876 |doi=10.1016/S0140-6736(03)13306-5 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(03)13306-5 |accessdate=2008-07-04}}</ref> | |||
| {{see also|Dual diagnosis|Comparison of bipolar disorder and schizophrenia}} | |||
| To make a diagnosis of schizophrenia ].<ref>{{cite journal |vauthors=Schrimpf LA, Aggarwal A, Lauriello J |title=Psychosis |journal=Continuum (Minneap Minn) |volume=24 |issue=3 |pages=845–860 |date=June 2018 |pmid=29851881 |doi=10.1212/CON.0000000000000602|s2cid=243933980 }}</ref>{{Rp|page=858|quote=Psychosis as a primary mental health disorder is a diagnosis of exclusion. Many different manifestations of psychotic symptoms are directly related to an underlying medical or neurologic disorder. Delirium and dementia are the two most important disorders to rule out and can present in a very subtle fashion.}} Psychotic symptoms lasting less than a month may be diagnosed as ], or as schizophreniform disorder. Psychosis is noted in ''Other specified schizophrenia spectrum and other psychotic disorders'' as a DSM-5 category. ] is diagnosed if symptoms of ] are substantially present alongside psychotic symptoms. Psychosis that results from a general medical condition or substance is termed secondary psychosis.<ref name=DSM5/><!-- cites previous four sentences --> | |||
| Psychotic symptoms may be present in several other conditions, including ],<ref name=Ferri2010/> ],<ref name=Paris2018>{{cite journal | vauthors = Paris J | title = Differential Diagnosis of Borderline Personality Disorder | journal = The Psychiatric Clinics of North America | date = December 2018 | volume = 41 | issue = 4 | pages=575–582 | doi = 10.1016/j.psc.2018.07.001 | pmid = 30447725| s2cid = 53951650 }}</ref> ], ], and a number of ]s. Non-bizarre delusions are also present in ], and social withdrawal in ], ] and ]. Schizotypal personality disorder has symptoms that are similar but less severe than those of schizophrenia.<ref name=DSM5/> Schizophrenia occurs along with obsessive–compulsive disorder (OCD) considerably more often than could be explained by chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia.<ref>{{cite journal | vauthors = Bottas A |title=Comorbidity: Schizophrenia With Obsessive-Compulsive Disorder |journal=Psychiatric Times |volume=26 |issue=4 |date=15 April 2009 |url=http://www.psychiatrictimes.com/display/article/10168/1402540 |url-status=live |archive-url=https://web.archive.org/web/20130403064649/http://www.psychiatrictimes.com/display/article/10168/1402540 |archive-date=3 April 2013}}</ref> There can be considerable overlap with the symptoms of ].<ref>{{cite journal |vauthors=OConghaile A, DeLisi LE |title=Distinguishing schizophrenia from posttraumatic stress disorder with psychosis |journal=Curr Opin Psychiatry |volume=28 |issue=3 |pages=249–255 |date=May 2015 |pmid=25785709 |doi=10.1097/YCO.0000000000000158 |s2cid=12523516 }}</ref> | |||
| Prolactin elevations have been reported in women with schizophrenia taking atypical antipsychotics.<ref name="Dickson_et_al_1995">{{cite journal |author=Dickson RA, Dalby JT, Williams R, Edwards AL |title=Risperidone-induced prolactin elevations in premenopausal women with schizophrenia |journal=American Journal of Psychiatry |volume=152 |issue=7 |pages=1102–03 |year=1995 |month=July |pmid=7540803}}</ref> It remains unclear whether the newer antipsychotics reduce the chances of developing ], a rare but serious and potentially fatal neurological disorder most often caused by an adverse reaction to ] or antipsychotic drugs.<ref name="Ananth_et_al_2004">{{cite journal |author=Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T |title=Neuroleptic malignant syndrome and atypical antipsychotic drugs |journal=Journal of Clinical Psychiatry |volume=65 |issue=4 |pages=464–70 |year=2004 |month=April |pmid=15119907 |url=http://article.psychiatrist.com/?ContentType=START&ID=10000823 |accessdate=2008-07-04 |doi=10.4088/JCP.v65n0403}}</ref> | |||
| A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms, such as ], ], ], ], ], ], and brain lesions. Stroke, ], ], ], and ]s such as ], ], ], and the ]s may also be associated with schizophrenia-like psychotic symptoms.<ref>{{cite book|title=Bradley's neurology in clinical practice|year=2012|publisher=Elsevier/Saunders|location=Philadelphia, PA|isbn=978-1-4377-0434-1| vauthors= Murray ED, Buttner N, Price BH | volume = 1 | edition=6th|pages=92–111| veditors = Bradley WG, Daroff RB, Fenichel GM, Jankovic J |chapter=Depression and Psychosis in Neurological Practice}}</ref> It may be necessary to rule out a ], which can be distinguished by visual hallucinations, acute onset and fluctuating ], and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific ''medical'' indication or possible ] from ].<ref>{{cite journal |vauthors=Leucht S, Bauer S, Siafis S, Hamza T, Wu H, Schneider-Thoma J, Salanti G, Davis JM |title=Examination of Dosing of Antipsychotic Drugs for Relapse Prevention in Patients With Stable Schizophrenia: A Meta-analysis |journal=JAMA Psychiatry |volume=78 |issue=11 |pages=1238–1248 |date=November 2021 |pmid=34406325 |pmc=8374744 |doi=10.1001/jamapsychiatry.2021.2130}}</ref> In children hallucinations must be separated from typical childhood fantasies.<ref name=DSM5/> It is difficult to distinguish childhood schizophrenia from autism.<ref name=DaFonseca2018/> | |||
| Response of symptoms to medication is variable: treatment-resistant schizophrenia is a term used for the failure of symptoms to respond satisfactorily to at least two different antipsychotics.<ref>{{cite journal |author=Meltzer HY |title=Treatment-resistant schizophrenia—the role of clozapine |journal=Current Medical Research and Opinion |volume=14 |issue=1 |pages=1–20 |year=1997 |pmid=9524789 |doi=10.1185/03007999709113338 |doi_brokendate=2009-12-08}}</ref> Patients in this category may be prescribed ],<ref>{{cite journal |author=Wahlbeck K, Cheine MV, Essali A |title=Clozapine versus typical neuroleptic medication for schizophrenia |journal=The Cochrane Database of Systematic Reviews |issue=2 |pages=CD000059 |publisher=John Wiley and Sons, Ltd. |year=2007 |pmid=10796289 |doi=10.1002/14651858.CD000059}}</ref> a medication of superior effectiveness but several potentially lethal side effects including ] and ].<ref>{{cite journal | author = Haas SJ, Hill R, Krum H | title = Clozapine-associated myocarditis: a review of 116 cases of suspected myocarditis associated with the use of clozapine in Australia during 1993–2003 | journal = Drug Safety | volume = 30 | pages = 47–57 | year = 2007 | pmid=17194170 | doi = 10.2165/00002018-200730010-00005 | issue = 1 }}</ref> Clozapine may have the additional benefit of reducing propensity for substance abuse in schizophrenic patients.<ref>{{cite journal |author = Lee M, Dickson RA, Campbell M, Oliphant J, Gretton H, Dalby JT. |title = Clozapine and substance abuse in patients with schizophrenia |journal = Canadian Journal of Psychiatry |volume = 43 |pages = 855–856 |year = 1998 }}</ref> For other patients who are unwilling or unable to take medication regularly, long-acting ] preparations of antipsychotics may be given every two weeks to achieve control. The United States and Australia are two countries with ] allowing the forced administration of this type of medication on those who refuse but are otherwise stable and living in the community. At least one study suggested that in the longer-term some individuals may do better not taking antipsychotics.<ref>{{cite journal |author=Harrow M, Jobe TH |title=Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study |journal=] |volume=195 |issue=5 |pages=406–414 |year=2007 |month=May |pmid=17502806 |doi=10.1097/01.nmd.0000253783.32338.6e |doi_brokendate=2009-12-08}}</ref> | |||
| ==Prevention== | |||
| ===Psychological and social interventions=== | |||
| ] of schizophrenia is difficult as there are no reliable markers for the later development of the disorder.<ref>{{cite journal | vauthors = Cannon TD, Cornblatt B, McGorry P | title = The empirical status of the ultra high-risk (prodromal) research paradigm | journal = Schizophrenia Bulletin | volume = 33 | issue = 3 | pages = 661–664 | date = May 2007 | pmid = 17470445 | pmc = 2526144 | doi = 10.1093/schbul/sbm031 }}</ref> | |||
| ] is also widely recommended and used in the treatment of schizophrenia, although services may often be confined to pharmacotherapy because of reimbursement problems or lack of training.<ref>{{cite journal |author=Moran, M |date=18 November 2005 |title=Psychosocial Treatment Often Missing From Schizophrenia Regimens |journal=Psychiatric News |volume=40 |issue=22 |page=24 |publisher=Psychiatry Online |location=USA |url=http://pn.psychiatryonline.org/cgi/content/full/40/22/24-b |accessdate=17 May 2007 }}</ref> | |||
| ] diagnose and treat patients in the prodromal phase of the illness. There is some evidence that these programs reduce symptoms. Patients tend to prefer early treatment programs to ordinary treatment and are less likely to disengage from them. As of 2020, it is unclear whether the benefits of early treatment persist once the treatment is terminated.<ref>{{cite journal |vauthors=Puntis S, Minichino A, De Crescenzo F, Cipriani A, Lennox B, Harrison R |title=Specialised early intervention teams for recent-onset psychosis |journal=Cochrane Database Syst Rev |volume=11 |issue=11 |pages=CD013288 |date=November 2020 |pmid=33135811 |doi=10.1002/14651858.CD013288.pub2 |pmc=8092671 | quote=p. 22: There is low-certainty evidence for the use of SEl services in comparison to TAU for a small reduction in psychiatric hospitalisation, and moderate-certainty evidence of a large effect of reduction in disengagement from mental health services. There is moderate-certainty evidence that SEI results in a small reduction of positive (hallucinations, delusions and disordered thinking) and negative symptoms (social withdrawal, flat or blunted affect, and poverty of speech) and low-certainty evidence that it greatly increases satisfaction in care, while there is low-certainty evidence that it improves general functioning and the likelihood of recovery. These effects were only observed during treatment and there was no evidence that outcomes are improved after the treatment has finished, although these were based on only one trial.}}</ref> | |||
| ] (CBT) is used to target specific symptoms<ref>{{cite journal |author=Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, O'Carroll M, Barnes TR |title=A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication |journal=Arch. Gen. Psychiatry |volume=57 |issue=2 |pages=165–72 |year=2000 |month=February |pmid=10665619 |doi= 10.1001/archpsyc.57.2.165}}</ref><ref>{{cite journal |author=Kuipers E, Garety P, Fowler D, Dunn G, Bebbington P, Freeman D, Hadley C |title=London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis. I: effects of the treatment phase |journal=Br J Psychiatry |volume=171 |pages=319–27 |year=1997 |month=October |pmid=9373419 |doi= 10.1192/bjp.171.4.319}}</ref><ref>{{cite journal |author=Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P, Kingdon D, Siddle R, Drake R, Everitt J, Leadley K, Benn A, Grazebrook K, Haley C, Akhtar S, Davies L, Palmer S, Faragher B, Dunn G |title=Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes |journal=Br J Psychiatry Suppl |volume=43 |pages=s91–7 |year=2002 |month=September |pmid=12271807 }}</ref> and improve related issues such as ], social functioning, and insight. Although the results of early trials were inconclusive<ref name="fn_38">{{cite journal |author=Cormac I, Jones C, Campbell C |title=Cognitive behaviour therapy for schizophrenia |journal=Cochrane Database of ]s |issue=1 |pages=CD000524 |year=2002 |pmid=11869579 |doi=10.1002/14651858.CD000524|accessdate=2008-07-03}}</ref> as the therapy advanced from its initial applications in the mid 1990s, more recent reviews clearly show CBT is an effective treatment for the psychotic symptoms of schizophrenia.<ref>{{cite journal |author=Wykes T, Steel C, Everitt B, Tarrier N |title=Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor |journal=Schizophr Bull |volume=34 |issue=3 |pages=523–37 |year=2008 |month=May |pmid=17962231 |doi=10.1093/schbul/sbm114 |pmc=2632426}}</ref><ref name="fn_39">{{cite journal |author=Zimmermann G, Favrod J, Trieu VH, Pomini V |title=The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis |journal=Schizophrenia Research |volume=77 |issue=1 |pages=1–9 |year=2005 |month=September |pmid=16005380 |doi=10.1016/j.schres.2005.02.018 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920-9964(05)00084-8|accessdate=2008-07-03}}</ref> | |||
| ] may reduce the risk of psychosis in those at high risk after a year<ref>{{cite journal | vauthors = Stafford MR, Jackson H, Mayo-Wilson E, Morrison AP, Kendall T | title = Early interventions to prevent psychosis: systematic review and meta-analysis | journal = BMJ | volume = 346 | page = f185 | date = January 2013 | pmid = 23335473 | pmc = 3548617 | doi = 10.1136/bmj.f185 }}</ref> and is recommended in this group, by the ] (NICE).<ref name="NICE2014">{{cite web|title=Psychosis and schizophrenia in adults: treatment and management |url=http://www.nice.org.uk/nicemedia/live/14382/66534/66534.pdf |publisher = ] (NICE) |access-date=19 April 2014 |pages=4–34|date=March 2014 |archive-url=https://web.archive.org/web/20140420070946/http://www.nice.org.uk/nicemedia/live/14382/66534/66534.pdf |archive-date=20 April 2014 }}</ref> Another preventive measure is to avoid drugs that have been associated with development of the disorder, including ], cocaine, and ].<ref name="BMJ07" /> | |||
| Another approach is cognitive remediation, a technique aimed at remediating the ]s sometimes present in schizophrenia. Based on techniques of ], early evidence has shown it to be cognitively effective, with some improvements related to measurable changes in brain activation as measured by ].<ref name="fn_40">{{cite journal |author=Wykes T, Brammer M, Mellers J, ''et al.'' |title=Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia |journal=] |volume=181 |pages=144–52 |year=2002 |month=August |pmid=12151286 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=12151286 |accessdate=2008-07-03 |doi=10.1192/bjp.181.2.144 |doi_brokendate=2009-12-08 }}</ref><ref>{{cite journal |author=Medalia A |title=Cognitive Remediation for Psychiatric Patients: Improving Functional Outcomes for Patients With Schizophrenia |journal=Psychiatric Times |volume=26 |issue=3 |year=2009 |url=http://www.psychiatrictimes.com/display/article/10168/1386195}}</ref> A similar approach known as cognitive enhancement therapy, which focuses on social cognition as well as neurocognition, has shown efficacy.<ref>{{cite journal |author=Hogarty GE, Flesher S, Ulrich R, ''et al.'' |title=Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior |journal=Arch. Gen. Psychiatry |volume=61 |issue=9 |pages=866–76 |year=2004 |month=September |pmid=15351765 |doi=10.1001/archpsyc.61.9.866 |url=http://archpsyc.ama-assn.org/cgi/pmidlookup?view=long&pmid=15351765|accessdate=2008-07-03}}</ref> | |||
| Antipsychotics are prescribed following a first-episode psychosis, and following remission, a preventive maintenance use is continued to avoid relapse. However, it is recognized that some people do recover following a single episode and that long-term use of antipsychotics will not be needed but there is no way of identifying this group.<ref name=Taylor2019>{{cite journal |vauthors=Taylor M, Jauhar S |title=Are we getting any better at staying better? The long view on relapse and recovery in first episode nonaffective psychosis and schizophrenia |journal=Therapeutic Advances in Psychopharmacology |volume=9 |date=September 2019|page=204512531987003 |pmid=31523418|doi=10.1177/2045125319870033 |pmc=6732843 }}</ref> | |||
| ] or education, which addresses the whole family system of an individual with a diagnosis of schizophrenia, has been consistently found to be beneficial, at least if the duration of intervention is longer-term.<ref>{{cite journal |author=McFarlane WR, Dixon L, Lukens E, Lucksted A |title=Family psychoeducation and schizophrenia: a review of the literature |journal=J Marital Fam Ther |volume=29 |issue=2 |pages=223–45 |year=2003 |month=April |pmid=12728780 |doi=10.1111/j.1752–0606.2003.tb01202.x |doi_brokendate=2009-12-08 }}</ref><ref>{{cite journal |author=Glynn SM, Cohen AN, Niv N |title=New challenges in family interventions for schizophrenia |journal=Expert Review of Neurotherapeutics |volume=7 |issue=1 |pages=33–43 |year=2007 |month=January |pmid=17187495 |doi=10.1586/14737175.7.1.33 |url=http://www.future-drugs.com/doi/abs/10.1586/14737175.7.1.33?url_ver=Z39.88–2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov|accessdate=2008-07-03}}</ref><ref>{{Cite journal | last1 = Pharoah | first1 = F. | last2 = Mari | first2 = J. | last3 = Rathbone | first3 = J. | last4 = Wong | first4 = W. | title = Family intervention for schizophrenia. | journal = Cochrane Database Syst Rev | issue = 4 | pages = CD000088 | year = 2006 | url = http://www.cochrane.org/reviews/en/ab000088.html | doi = 10.1002/14651858.CD000088.pub2 | pmid = 17054127 | last5 = Pharoah | first5 = Fiona }}</ref> Aside from therapy, the effect of schizophrenia on families and the burden on carers has been recognized, with the increasing availability of self-help books on the subject.<ref>{{cite book |author=Jones S, Hayward P |title=Coping with Schizophrenia: A Guide for Patients, Families and Caregivers | publisher = Oneworld Pub. | year = 2004 | location = Oxford, England |isbn=1-85168-344-5}}</ref><ref>{{cite book |author=] |title=Surviving Schizophrenia: A Manual for Families, Consumers, and Providers |edition=5th |publisher=HarperCollins |year=2006 | isbn=0-06-084259-8}}</ref> There is also some evidence for benefits from social skills training, although there have also been significant negative findings.<ref>{{cite journal |author=Kopelowicz A, Liberman RP, Zarate R |title=Recent advances in social skills training for schizophrenia |journal=] |volume=32 Suppl 1 |pages=S12–23 |year=2006 |month=October |pmid=16885207 |doi=10.1093/schbul/sbl023 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16885207|accessdate=2008-07-03 |pmc=2632540}}</ref><ref>{{cite web |url=http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=5217 |title=Practice Guideline for the Treatment of Patients With Schizophrenia. Second Edition |author=American Psychiatric Association |authorlink=American Psychiatric Association |month=February |year=2004 |publisher=National Guideline Clearinghouse |location=USA }}</ref> Some studies have explored the possible benefits of music therapy and other creative therapies.<ref>{{cite journal |author=Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S |title=Music therapy for in-patients with schizophrenia: exploratory randomised controlled trial |journal=The British Journal of Psychiatry |volume=189 |pages=405–9 |year=2006 |month=November |pmid=17077429 |doi=10.1192/bjp.bp.105.015073 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=17077429|accessdate=2008-07-03}}</ref><ref>{{Cite journal | last1 = Ruddy | first1 = R. | last2 = Milnes | first2 = D. | title = Art therapy for schizophrenia or schizophrenia-like illnesses. | journal = Cochrane Database Syst Rev | issue = 4 | pages = CD003728 | url = http://www.cochrane.org/reviews/en/ab003728.html | year = 2005 | doi = 10.1002/14651858.CD003728.pub2 | pmid = 16235338 | last3 = Ruddy | first3 = Rachel }}</ref><ref name="Ruddy-2007">{{Cite journal | last1 = Ruddy | first1 = RA. | last2 = Dent-Brown | first2 = K. | title = Drama therapy for schizophrenia or schizophrenia-like illnesses. | journal = Cochrane Database Syst Rev | url = http://www.cochrane.org/reviews/en/ab005378.html | issue = 1 | pages = CD005378 | year = 2007 | doi = 10.1002/14651858.CD005378.pub2 | pmid = 17253555 | last3 = Ruddy | first3 = Rachel }}</ref> | |||
| ==Management== | |||
| The ] model is alternative to inpatient hospital treatment using a minimal medication approach. It is described as a ]-therapeutic ] method, characterized by its founder as "the 24 hour a day application of interpersonal phenomenologic interventions by a nonprofessional staff, usually without neuroleptic drug treatment, in the context of a small, homelike, quiet, supportive, protective, and tolerant social environment."<ref name="mosh99">{{cite journal |author=Mosher LR |title=Soteria and other alternatives to acute psychiatric hospitalization: a personal and professional review |journal=] |volume=187 |issue=3 |pages=142–9 |year=1999 |month=March |pmid=10086470 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0022–3018&volume=187&issue=3&spage=142|accessdate=2008-07-03 |doi=10.1097/00005053-199903000-00003}}</ref> Although research evidence is limited, a 2008 systematic review found the programme equally as effective as treatment with medication in people diagnosed with first and second episode schizophrenia.<ref name="Calton_et_al_2008">{{cite journal |author=Calton T, Ferriter M, Huband N, Spandler H |title=A systematic review of the Soteria paradigm for the treatment of people diagnosed with schizophrenia |journal=] |volume=34 |issue=1 |pages=181–92 |year=2008 |month=January |pmid=17573357 |doi=10.1093/schbul/sbm047 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17573357|accessdate=2008-07-03 |pmc=2632384}}</ref> | |||
| {{Main|Management of schizophrenia}} | |||
| The primary treatment of schizophrenia is the use of ], often in combination with ] and ]s.<ref name=Lancet2009/><ref>{{cite journal | vauthors = Weiden PJ |title=Beyond Psychopharmacology: Emerging Psychosocial Interventions for Core Symptoms of Schizophrenia. |journal=Focus (American Psychiatric Publishing) |volume=14 |issue=3 |pages=315–327 |date=July 2016 |pmid=31975812|doi=10.1176/appi.focus.20160014|pmc=6526802 }}</ref> Community support services including drop-in centers, visits by members of a ], ],<ref>{{cite journal | vauthors = McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A | title = Cognitive training for supported employment: 2–3 year outcomes of a randomized controlled trial | journal = The American Journal of Psychiatry | volume = 164 | issue = 3 | pages = 437–441 | date = March 2007 | pmid = 17329468 | doi = 10.1176/appi.ajp.164.3.437 }}</ref> and support groups are common. The time between the onset of psychotic symptoms to being given treatment – the duration of untreated psychosis (DUP) – is associated with a poorer outcome in both the short term and the long term.<ref>{{cite journal | vauthors = Souaiby L, Gaillard R, Krebs MO |title= |journal=Encephale |volume=42 |issue=4 |pages=361–366 |date=August 2016|pmid=27161262 |doi=10.1016/j.encep.2015.09.007 }}</ref> | |||
| ] or ] admission to hospital may be imposed by doctors and courts who deem a person to be having a severe episode. In the UK, large mental hospitals termed asylums began to be closed down in the 1950s with the advent of antipsychotics, and with an awareness of the negative impact of long-term hospital stays on recovery.<ref name=Killaspy2014>{{cite journal |vauthors=Killaspy H|title= Contemporary mental health rehabilitation|journal=East Asian Archives of Psychiatry|volume=24 | issue=3|pages=89–94|date=September 2014|pmid = 25316799}}</ref> This process was known as ], and community and supportive services were developed to support this change. Many other countries followed suit with the US starting in the 60s.<ref>{{cite journal | vauthors = Fuller Torrey E | title = Deinstitutionalization and the rise of violence. | journal = CNS Spectrums | date = June 2015 | volume = 20 | issue = 3 | pages = 207–214 | doi = 10.1017/S1092852914000753 | pmid = 25683467| s2cid = 22210482 }}</ref> There still remain a smaller group of people who do not improve enough to be discharged.<ref name=Killaspy2014/><ref name=Capdevielle2009/> In some countries that lack the necessary supportive and social services, long-term hospital stays are more usual.<ref name=Narayan2012/> | |||
| ===Other=== | |||
| ] is not considered a ] but may be prescribed in cases where other treatments have failed. It is more effective where symptoms of catatonia are present,<ref>{{cite journal |author=Greenhalgh J, Knight C, Hind D, Beverley C, Walters S |year=2005 |month=March |title= Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies|journal= Health Technol Assess.|volume= 9|issue=9 |pages=1–156 |accessdate= 2007-06-17 |pmid=15774232}}</ref> and is recommended for use under ] guidelines in the UK for catatonia if previously effective, though there is no recommendation for use for schizophrenia otherwise.<ref>{{cite web |url=http://www.nice.org.uk/page.aspx?o=TA059 |title= The clinical effectiveness and cost effectiveness of electroconvulsive Therapy (ECT) for depressive illness, schizophrenia, catatonia and mania.|accessdate=2007-06-17 |year= 2003|month=April |publisher= National Institute for Health and Clinical Excellence}}</ref> ] has now become a rare procedure and is not a recommended treatment.<ref name="Mashour_et_al_2005">{{cite journal |author=Mashour GA, Walker EE, Martuza RL |title=Psychosurgery: past, present, and future |journal=Brain Res. Brain Res. Rev. |volume=48 |issue=3 |pages=409–19 |year=2005 |month=June |pmid=15914249 |doi=10.1016/j.brainresrev.2004.09.002 |url=http://linkinghub.elsevier.com/retrieve/pii/S0165-0173(04)00129-8 |accessdate=2008-07-04}}</ref> | |||
| ===Medication=== | |||
| Service-user led movements have become integral to the recovery process in Europe and the United States; groups such as the ] and the ] have developed a self-help approach that aims to provide support and assistance outside the traditional medical model adopted by mainstream psychiatry. By avoiding framing personal experience in terms of criteria for ] or ], they aim to destigmatize the experience and encourage individual responsibility and a positive self-image. Partnerships between hospitals and consumer-run groups are becoming more common, with services working toward remediating social withdrawal, building social skills and reducing rehospitalization.<ref>{{cite journal |author=Goering P, Durbin J, Sheldon CT, Ochocka J, Nelson G, Krupa T |title=Who uses consumer-run self-help organizations? |journal=American Journal of Orthopsychiatry |volume=76 |issue=3 |pages=367–73 |year=2006 |month=July |pmid=16981815 |doi=10.1037/0002-9432.76.3.367 |url=http://content.apa.org/journals/ort/76/3/367 |accessdate=2008-07-04}}</ref> | |||
| ] (trade name Risperdal) is a common ] medication.]] | |||
| The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called ], like ], are ]s that block D<sub>2</sub> receptors, and affect the ] of ]. Those brought out later, the second-generation antipsychotics known as ], including ] and ], can also have an effect on another neurotransmitter, ]. Antipsychotics can reduce the symptoms of anxiety within hours of their use, but, for other symptoms, they may take several days or weeks to reach their full effect.<ref name=RAISE/><ref name=nhsTreatment/> They have little effect on negative and cognitive symptoms, which may be helped by additional psychotherapies and medications.<ref>{{cite journal | vauthors = Ortiz-Orendain J, Covarrubias-Castillo SA, Vazquez-Alvarez AO, Castiello-de Obeso S, Arias Quiñones GE, Seegers M, Colunga-Lozano LE | title = Modafinil for people with schizophrenia or related disorders | journal = The Cochrane Database of Systematic Reviews | volume = 12 | page = CD008661 | date = December 2019 | issue = 12 | pmid = 31828767 | pmc = 6906203 | doi = 10.1002/14651858.CD008661.pub2 }}</ref> There is no single antipsychotic suitable for first-line treatment for everyone, as responses and tolerances vary between people.<ref>{{cite journal | vauthors = Lally J, MacCabe JH | title = Antipsychotic medication in schizophrenia: a review | journal = British Medical Bulletin | volume = 114 | issue = 1 | pages = 169–179 | date = June 2015 | pmid = 25957394 | doi = 10.1093/bmb/ldv017 | doi-access = }}</ref> Stopping medication may be considered after a single psychotic episode where there has been a full recovery with no symptoms for twelve months. Repeated relapses worsen the long-term outlook and the risk of relapse following a second episode is high, and long-term treatment is usually recommended.<ref>{{cite journal | vauthors = Keks N, Schwartz D, Hope J | title = Stopping and switching antipsychotic drugs | journal = Australian Prescriber | volume = 42 | issue = 5 | pages = 152–157 | date = October 2019 | pmid = 31631928 | pmc = 6787301 | doi = 10.18773/austprescr.2019.052 }}</ref><ref name=Harrow2013>{{cite journal | vauthors = Harrow M, Jobe TH | title = Does long-term treatment of schizophrenia with antipsychotic medications facilitate recovery? | journal = Schizophrenia Bulletin | volume = 39 | issue = 5 | pages = 962–5 | date = September 2013 | pmid = 23512950 | pmc = 3756791 | doi = 10.1093/schbul/sbt034 }}</ref> | |||
| Regular exercise can have healthful effects on both the physical and mental health and well-being of individuals with schizophrenia.<ref>{{cite doi|10.1002/14651858.CD004412.pub2}}</ref> | |||
| About half of those with schizophrenia will respond favourably to antipsychotics, and have a good return of functioning.<ref>{{cite journal |vauthors=Elkis H, Buckley PF |title=Treatment-Resistant Schizophrenia |journal=The Psychiatric Clinics of North America |volume=39 |issue=2 |pages=239–65 |date=June 2016 |pmid=27216902|doi=10.1016/j.psc.2016.01.006}}</ref> However, positive symptoms persist in up to a third of people. Following two trials of different antipsychotics over six weeks, that also prove ineffective, they will be classed as having treatment-resistant schizophrenia (TRS), and ] will be offered.<ref>{{cite journal |vauthors=Gillespie AL, Samanaite R, Mill J, Egerton A, MacCabe JH |title=Is treatment-resistant schizophrenia categorically distinct from treatment-responsive schizophrenia? a systematic review |journal=BMC Psychiatry |volume=17 |issue=1 |page=12 |date=13 January 2017 |pmid=28086761 |doi=10.1186/s12888-016-1177-y|pmc=5237235 |doi-access=free }}</ref><ref name=Siskind2017/> Clozapine is of benefit to around half of this group although it has the potentially serious side effect of ] (lowered ] count) in less than 4% of people.<ref name=Lancet2009/><ref name=BMJ07/><ref>{{cite journal | vauthors = Essali A, Al-Haj Haasan N, Li C, Rathbone J | title = Clozapine versus typical neuroleptic medication for schizophrenia | journal = The Cochrane Database of Systematic Reviews | issue = 1 | page = CD000059 | date = January 2009 | volume = 2009 | pmid = 19160174 | doi = 10.1002/14651858.CD000059.pub2 | pmc = 7065592 }}</ref> | |||
| ==Prognosis== | |||
| ===Course=== | |||
| ], a US ], began showing signs of paranoid schizophrenia during his college years. Despite having stopped taking his prescribed medication, Nash continued his studies and was awarded the ] in 1994. His life was depicted in the 2001 film '']''.]] | |||
| Coordinated by the ] and published in 2001, The International Study of Schizophrenia (ISoS) was a long-term follow-up study of 1633 individuals diagnosed with schizophrenia around the world. Of the 75% who were available for follow-up, half had a favourable outcome, and 16% had a delayed recovery after an early unremitting course. More usually, the course in the first two years predicted the long-term course. Early social intervention was also related to a better outcome. The findings were held as important in moving patients, carers and clinicians away from the prevalent belief of the chronic nature of the condition.<ref>{{cite journal |author=Harrison G, Hopper K, Craig T, ''et al.'' |title=Recovery from psychotic illness: a 15- and 25-year international follow-up study |journal=British Journal of Psychiatry |volume=178 |pages=506–17 |year=2001 |month=June |pmid=11388966 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=11388966 |accessdate=2008-07-04 |doi=10.1192/bjp.178.6.506}}</ref> A review of major ] in North America noted this variation in outcomes, although outcome was on average worse than for other psychotic and psychiatric disorders. A moderate number of patients with schizophrenia were seen to remit and remain well; the review raised the question that some may not require maintenance medication.<ref name="Jobe2005">{{cite journal |author=Jobe TH, Harrow M |title=Long-term outcome of patients with schizophrenia: a review |journal=Canadian Journal of Psychiatry |volume=50 |issue=14 |pages=892–900 |year=2005 |month=December |pmid=16494258 |url=http://ww1.cpa-apc.org/Publications/Archives/CJP/2005/december/cjp-dec-05-Harrow-IR.pdf|format=PDF |accessdate=2008-07-05}}</ref> | |||
| About 30 to 50 percent of people with schizophrenia do not accept that they have an illness or comply with their recommended treatment.<ref>{{cite journal | vauthors = Baier M | title = Insight in schizophrenia: a review | journal = Current Psychiatry Reports | volume = 12 | issue = 4 | pages = 356–361 | date = August 2010 | pmid = 20526897 | doi = 10.1007/s11920-010-0125-7 | s2cid = 29323212 }}</ref> For those who are unwilling or unable to take medication regularly, ] of antipsychotics may be used,<ref>{{cite journal | vauthors = Peters L, Krogmann A, von Hardenberg L, Bödeker K, Nöhles VB, Correll CU | title = Long-Acting Injections in Schizophrenia: a 3-Year Update on Randomized Controlled Trials Published January 2016 – March 2019 | journal = Current Psychiatry Reports | volume = 21 | issue = 12 | pages = 124 | date = November 2019 | pmid = 31745659 | doi = 10.1007/s11920-019-1114-0 | s2cid = 208144438 }}</ref> which reduce the risk of relapse to a greater degree than oral medications.<ref>{{cite journal | vauthors = Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, Davis JM | title = Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis | journal = Lancet | volume = 379 | issue = 9831 | pages = 2063–2071 | date = June 2012 | pmid = 22560607 | doi = 10.1016/S0140-6736(12)60239-6 | s2cid = 2018124 }}</ref> When used in combination with psychosocial interventions, they may improve long-term ] to treatment.<ref name=Depo06>{{cite journal | vauthors = McEvoy JP | title = Risks versus benefits of different types of long-acting injectable antipsychotics | journal = The Journal of Clinical Psychiatry | volume = 67 | issue = Suppl 5 | pages = 15–18 | year = 2006 | pmid = 16822092 }}</ref> | |||
| A clinical study using strict recovery criteria (concurrent remission of positive and negative symptoms and adequate social and vocational functioning continuously for two years) found a recovery rate of 14% within the first five years.<ref name="fn_43">{{cite journal |author=Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM |title=Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder |journal=American Journal of Psychiatry |volume=161 |issue=3 |pages=473–9 |year=2004 |month=March |pmid=14992973 |url=http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=14992973 |accessdate=2008-07-04 |doi=10.1176/appi.ajp.161.3.473}}</ref> A 5-year community study found that 62% showed overall improvement on a composite measure of clinical and functional outcomes.<ref>{{cite journal |author=Harvey CA, Jeffreys SE, McNaught AS, Blizard RA, King MB |year=2007 |title=The Camden Schizophrenia Surveys III: Five-Year Outcome of a Sample of Individuals From a Prevalence Survey and the Importance of Social Relationships |journal=International Journal of Social Psychiatry |volume=53 |issue=4 |pages=340–356 |url=http://isp.sagepub.com/cgi/content/abstract/53/4/340 |accessdate=2008-07-04 |doi=10.1177/0020764006074529 |pmid=17703650}}</ref> | |||
| The ] medication ] (Cobenfy) was approved for medical use in the United States in September 2024.<ref name="FDA PR 20240926">{{cite press release | title=FDA Approves Drug with New Mechanism of Action for Treatment of Schizophrenia | website=U.S. ] (FDA) | date=26 September 2024 | url=https://www.fda.gov/news-events/press-announcements/fda-approves-drug-new-mechanism-action-treatment-schizophrenia | access-date=27 September 2024 | archive-date=27 September 2024 | archive-url=https://web.archive.org/web/20240927004824/https://www.fda.gov/news-events/press-announcements/fda-approves-drug-new-mechanism-action-treatment-schizophrenia | url-status=live }} {{PD-notice}}</ref><ref>{{cite press release | title=U.S. Food and Drug Administration Approves Bristol Myers Squibb's Cobenfy (xanomeline and trospium chloride), a First-In-Class Muscarinic Agonist for the Treatment of Schizophrenia in Adults | publisher=Bristol Myers Squibb | via=Business Wire | date=27 September 2024 | url=https://www.businesswire.com/news/home/20240925382351/en/U.S.-Food-and-Drug-Administration-Approves-Bristol-Myers-Squibb%E2%80%99s-COBENFY%E2%84%A2-xanomeline-and-trospium-chloride-a-First-In-Class-Muscarinic-Agonist-for-the-Treatment-of-Schizophrenia-in-Adults | access-date=27 September 2024}}</ref> It is the first ] approved by the US ] (FDA) to treat schizophrenia.<ref name="FDA PR 20240926" /> | |||
| ] studies have noted that individuals diagnosed with schizophrenia have much better long-term outcomes in ] (India, Colombia and Nigeria) than in ] (United States, United Kingdom, Ireland, Denmark, Czech Republic, Slovakia, Japan, and Russia),<ref name="fn_44">{{cite journal |author=Hopper K, Wanderling J |title=Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia |journal=Schizophrenia Bulletin |volume=26 |issue=4 |pages=835–46 |date=1 January 2000|pmid=11087016 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=11087016 |accessdate=2008-07-04 }}</ref> despite antipsychotic drugs not being widely available. | |||
| Negative and cognitive symptoms are an unmet clinical need in antipsychotic-based treatment approaches. Psychostimulant drugs have been found effective in the treatment of negative symptoms, but are rarely prescribed due to concerns about the excacerbation of positive symptoms.<ref>{{Cite journal |last1=Lindenmayer |first1=Jean-Pierre |last2=Nasrallah |first2=Henry |last3=Pucci |first3=Michael |last4=James |first4=Steven |last5=Citrome |first5=Leslie |date=2013-07-01 |title=A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities |url=https://www.sciencedirect.com/science/article/abs/pii/S0920996413001655 |journal=Schizophrenia Research |volume=147 |issue=2 |pages=241–252 |doi=10.1016/j.schres.2013.03.019 |issn=0920-9964}}</ref> It is possible that low-dose psychedelic therapies could be of benefit in schizophrenia through their prosocial and procognitive effects, although there is a serious risk that high dose psychedelic therapies could lead to worsening of positive symptoms.<ref>{{Cite journal |last1=Sapienza |first1=Jacopo |last2=Martini |first2=Francesca |last3=Comai |first3=Stefano |last4=Cavallaro |first4=Roberto |last5=Spangaro |first5=Marco |last6=De Gregorio |first6=Danilo |last7=Bosia |first7=Marta |date=2024-09-18 |title=Psychedelics and schizophrenia: a double-edged sword |url=https://www.nature.com/articles/s41380-024-02743-x |journal=Molecular Psychiatry |language=en |pages=1–14 |doi=10.1038/s41380-024-02743-x |pmid=39294303 |issn=1476-5578}}</ref> | |||
| ===Defining recovery=== | |||
| Rates are not always comparable across studies because exact definitions of remission and recovery have not been widely established. A "Remission in Schizophrenia Working Group" has proposed standardized remission criteria involving "improvements in core signs and symptoms to the extent that any remaining symptoms are of such low intensity that they no longer interfere significantly with behavior and are below the threshold typically utilized in justifying an initial diagnosis of schizophrenia".<ref>{{cite journal |author=Andreasen NC, Carpenter WT, Kane JM, Lasser RA, Marder SR, Weinberger DR |title=Remission in schizophrenia: proposed criteria and rationale for consensus |journal=The American Journal of Psychiatry |volume=162 |issue=3 |pages=441–9 |year=2005 |month=March |pmid=15741458 |doi=10.1176/appi.ajp.162.3.441 |url=http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=15741458 |accessdate=2008-07-07}}</ref> Standardized recovery criteria have also been proposed by a number of different researchers, with the stated DSM definitions of a "complete return to premorbid levels of functioning” or "complete return to full functioning" seen as inadequate, impossible to measure, incompatible with the variability in how society defines normal psychosocial functioning, and contributing to self-fulfilling pessimism and stigma.<ref>{{cite journal |author=Liberman RP, Kopelowicz A|year=2005 |month=June |title=Recovery From Schizophrenia: A Concept in Search of Research |journal=Psychiatric Services |volume=56 |issue=6 |pages=735–742 |url=http://psychservices.psychiatryonline.org/cgi/content/full/56/6/735 |accessdate=2008-07-07 |doi=10.1176/appi.ps.56.6.735 |pmid=15939952}}</ref> Some ]s may have quite different basic perceptions and concepts of recovery than individuals with the diagnosis, including those in the ].<ref>{{cite journal |author=Davidson L, Schmutte T, Dinzeo T, Andres-Hyman R |title=Remission and recovery in schizophrenia: practitioner and patient perspectives |journal=Schizophrenia Bulletin |volume=34 |issue=1 |pages=5–8 |year=2008 |month=January |pmid=17984297 |doi=10.1093/schbul/sbm122 |url=http://schizophreniabulletin.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17984297 |accessdate=2008-07-07 |pmc=2632379}}</ref> One notable limitation of nearly all the research criteria is failure to address the person's own evaluations and feelings about their life. Schizophrenia and recovery often involve a continuing loss of self-esteem, alienation from friends and family, interruption of school and career, and social stigma, "experiences that cannot just be reversed or forgotten".<ref name="Bellack06"/> An increasingly influential ] defines recovery as a process, similar to being "in recovery" from drug and alcohol problems, and emphasizes a personal journey involving factors such as hope, choice, empowerment, social inclusion and achievement.<ref name="Bellack06"/> | |||
| === |
====Adverse effects==== | ||
| {{Further information|Antipsychotic#Adverse effects}} | |||
| Several factors have been associated with a better overall prognosis: Being female, rapid (vs. insidious) onset of symptoms, older age of first episode, predominantly positive (rather than negative) symptoms, presence of mood symptoms, and good pre-illness functioning.<ref name="Davidson_Glashan_1997">{{cite journal |author=Davidson L, McGlashan TH |title=The varied outcomes of schizophrenia |journal=Canadian Journal of Psychiatry |volume=42 |issue=1 |pages=34–43 |year=1997 |month=February |pmid=9040921 }}</ref><ref name="Lieberman_et_al_1996">{{cite journal |author=Lieberman JA, Koreen AR, Chakos M, ''et al.'' |title=Factors influencing treatment response and outcome of first-episode schizophrenia: implications for understanding the pathophysiology of schizophrenia |journal=Journal of Clinical Psychiatry |volume=57 Suppl 9 |pages=5–9 |year=1996 |pmid=8823344}}</ref> The strengths and internal resources of the individual concerned, such as determination or ], have also been associated with better prognosis.<ref name="Jobe2005"/> The attitude and level of support from people in the individual's life can have a significant impact; research framed in terms of the negative aspects of this—the level of critical comments, hostility, and intrusive or controlling attitudes, termed high ']'—has consistently indicated links to relapse.<ref name="fn_70">{{cite journal |author=Bebbington P, Kuipers L |title=The predictive utility of expressed emotion in schizophrenia: an aggregate analysis |journal=Psychological Medicine |volume=24 |issue=3 |pages=707–18 |year=1994 |month=August |pmid=7991753 |doi=10.1017/S0033291700027860}}</ref> Most research on predictive factors is correlational in nature, however, and a clear cause-and-effect relationship is often difficult to establish. | |||
| ], including ], are associated with all commercially available ] to varying degrees.<ref name=Chow2020>{{cite journal |vauthors=Chow CL, Kadouh NK, Bostwick JR, VandenBerg AM |date=June 2020 |title=Akathisia and Newer Second-Generation Antipsychotic Drugs: A Review of Current Evidence |url= |journal=Pharmacotherapy |volume=40 |issue=6 |pages=565–574 |doi=10.1002/phar.2404 |pmid=32342999|hdl=2027.42/155998 |s2cid=216596357 |hdl-access=free }}</ref>{{Rp|page=566|quote=However, EPS, particularly akathisia, occurs, to some degree, with all commercially available SGAs.}} There is little evidence that second generation antipsychotics have reduced levels of extrapyramidical symptoms compared to typical antipsychotics.<ref name=Chow2020/>{{Rp|page=566|quote=Furthermore, previous meta-analyses and systematic reviews comparing the safety and tolerability of FGAs and SGAs have found little evidence to support the notion that as a class, SGAs pose a reduced risk for EPS com- pared with FGAs. However, high-potency FGAs do tend to pose the greatest risk for EPS.}} ] can occur due to long-term use of antipsychotics, developing after months or years of use.<ref>{{cite journal |vauthors=Carbon M, Kane JM, Leucht S, Correll CU |date=October 2018 |title=Tardive dyskinesia risk with first- and second-generation antipsychotics in comparative randomized controlled trials: a meta-analysis |journal=World Psychiatry |volume=17 |issue=3 |pages=330–340 |doi=10.1002/wps.20579 |pmc=6127753 |pmid=30192088}}</ref> The antipsychotic ] is also associated with ] (including ]), ], and ]. | |||
| ===Mortality=== | |||
| {{seealso|Physical health in schizophrenia}} | |||
| In a study of over 168,000 Swedish citizens undergoing psychiatric treatment, schizophrenia was associated with an average life expectancy of approximately 80–85% of that of the general population; women were found to have a slightly better life expectancy than men, and a diagnosis of schizophrenia was associated with an overall better life expectancy than ], ], ] and ].<ref name="fn_45">{{cite journal |author=Hannerz H, Borgå P, Borritz M |title=Life expectancies for individuals with psychiatric diagnoses |journal=Public Health |volume=115 |issue=5 |pages=328–37 |year=2001 |month=September |pmid=11593442 |doi=10.1038/sj.ph.1900785 }}</ref> Other identified factors include smoking,<ref>{{cite journal |author=Evins AE|title=Nicotine Dependence in Schizophrenia: Prevalence, Mechanisms, and Implications for Treatment |journal=Psychiatric Times |volume=25 |issue=3 |date=March 1, 2008|url=http://www.psychiatrictimes.com/schizophrenia/article/10168/1147496 | |||
| }}</ref> poor diet, little exercise and the negative health effects of psychiatric drugs.<ref name="Brown_Barraclough_2000" /> | |||
| ===Psychosocial interventions=== | |||
| There is a higher than average ] rate associated with schizophrenia. This has been cited at 10%, but a more recent analysis of studies and statistics revises the estimate at 4.9%, most often occurring in the period following onset or first hospital admission.<ref>{{Cite journal | last1 = Palmer | first1 = BA. | last2 = Pankratz | first2 = VS. | last3 = Bostwick | first3 = JM. | title = The lifetime risk of suicide in schizophrenia: a reexamination. | journal = Arch Gen Psychiatry | volume = 62 | issue = 3 | pages = 247–53 | month = Mar | year = 2005 | doi = 10.1001/archpsyc.62.3.247 | pmid = 15753237 }}</ref> Several times more attempt suicide.<ref name="fn_46">{{cite journal |author=Radomsky ED, Haas GL, Mann JJ, Sweeney JA |title=Suicidal behavior in patients with schizophrenia and other psychotic disorders |journal=American Journal of Psychiatry |volume=156 |issue=10 |pages=1590–5 |date=1 October 1999|pmid=10518171 |url=http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=10518171 |accessdate=2008-07-04 }}</ref> There are a variety of reasons and risk factors.<ref name="fn_47">{{cite journal |author=Caldwell CB, Gottesman II |title=Schizophrenics kill themselves too: a review of risk factors for suicide |journal=Schizophr Bull |volume=16 |issue=4 |pages=571–89 |year=1990 |pmid=2077636}}</ref><ref name="fn_128">{{cite book |author=Dalby JT, Williams RJ |title=Depression in schizophrenics |publisher=Plenum Press |location=New York |year=1989 |isbn=0-306-43240-4}}</ref> | |||
| {{Further|Management of schizophrenia#Psychosocial}} | |||
| A number of psychosocial interventions that include several types of ] may be useful in the treatment of schizophrenia such as: ],<ref name=Pharoah2010>{{cite journal | vauthors = Pharoah F, Mari J, Rathbone J, Wong W | title = Family intervention for schizophrenia | journal = The Cochrane Database of Systematic Reviews | volume = 12 | issue = 12 | pages = CD000088 | date = December 2010 | pmid = 21154340 | pmc = 4204509 | doi = 10.1002/14651858.CD000088.pub2 | veditors = Pharoah F }}</ref> ], cognitive remediation therapy (CRT),<ref>{{cite journal | vauthors = Bellani M, Ricciardi C, Rossetti MG, Zovetti N, Perlini C, Brambilla P | title = Cognitive remediation in schizophrenia: the earlier the better? | journal = Epidemiology and Psychiatric Sciences | volume = 29 | issue = | pages = e57 | date = September 2019 | pmid = 31556864 | pmc = 8061237 | doi = 10.1017/S2045796019000532 }}</ref> cognitive behavioral therapy (CBT), and ].<ref>{{cite journal | vauthors = Philipp R, Kriston L, Lanio J, Kühne F, Härter M, Moritz S, Meister R | title = Effectiveness of metacognitive interventions for mental disorders in adults-A systematic review and meta-analysis (METACOG) | journal = Clinical Psychology & Psychotherapy | volume = 26 | issue = 2 | pages = 227–240 | date = March 2019 | pmid = 30456821 | doi = 10.1002/cpp.2345 | s2cid = 53872643 }}</ref><ref>{{cite journal | vauthors = Rouy M, Saliou P, Nalborczyk L, Pereira M, Roux P, Faivre N | title = Systematic review and meta-analysis of metacognitive abilities in individuals with schizophrenia spectrum disorders | journal = Neuroscience and Biobehavioral Reviews | volume = 126 | issue = | pages = 329–337 | date = July 2021 | pmid = 33757817 | doi = 10.1016/j.neubiorev.2021.03.017 | s2cid = 232288918 | url = https://hal.archives-ouvertes.fr/hal-03178486/file/2020.12.03.20243113v1.full.pdf }}</ref> Skills training, help with substance use, and weight management – often needed as a side effect of an antipsychotic – are also offered.<ref>{{cite journal | vauthors = Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Lehman A, Tenhula WN, Calmes C, Pasillas RM, Peer J, Kreyenbuhl J | title = The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements | journal = Schizophrenia Bulletin | volume = 36 | issue = 1 | pages = 48–70 | date = January 2010 | pmid = 19955389 | pmc = 2800143 | doi = 10.1093/schbul/sbp115 }}</ref> In the US, interventions for first episode psychosis have been brought together in an overall approach known as ] (CSC) and also includes support for education.<ref name=RAISE/> In the UK ''care across all phases'' is a similar approach that covers many of the treatment guidelines recommended.<ref name=NICE2014/> The aim is to reduce the number of relapses and stays in the hospital.<ref name=Pharoah2010/> | |||
| Other support services for education, employment, and housing are usually offered. For people with severe schizophrenia, who are discharged from a stay in the hospital, these services are often brought together in an integrated approach to offer support in the community away from the hospital setting. In addition to medicine management, housing, and finances, assistance is given for more routine matters such as help with shopping and using public transport. This approach is known as ] (ACT) and has been shown to achieve positive results in symptoms, social functioning and quality of life.<ref>{{cite journal | vauthors = Bond GR, Drake RE | title = The critical ingredients of assertive community treatment. | journal = World Psychiatry | date = June 2015 | volume = 14 | issue = 2 | pages = 240–242 | doi = 10.1002/wps.20234 | pmid = 26043344| pmc = 4471983 }}</ref><ref>{{cite journal | vauthors = Smeerdijk M | title = . | journal = Tijdschrift voor Psychiatrie | date = 2017 | volume = 59 | issue = 8 | pages = 466–473 | pmid = 28880347}}</ref> Another more intense approach is known as ''intensive care management'' (ICM). ICM is a stage further than ACT and emphasises support of high intensity in smaller caseloads, (less than twenty). This approach is to provide long-term care in the community. Studies show that ICM improves many of the relevant outcomes including social functioning.<ref>{{cite journal | vauthors = Dieterich M | title = Intensive case management for severe mental illness | journal=The Cochrane Database of Systematic Reviews | date = 6 January 2017 | volume = 1 | issue = 1 | page = CD007906 | doi = 10.1002/14651858.CD007906.pub3 | pmid = 28067944| pmc = 6472672 }}</ref> | |||
| ===Violence=== | |||
| The relationship between violent acts and schizophrenia is a contentious topic. Current research indicates that the percentage of people with schizophrenia who commit violent acts is higher than the percentage of people without any disorder, but lower than is found for disorders such as ], and the difference is reduced or not found in same-neighbourhood comparisons when related factors are taken into account, notably sociodemographic variables and ].<ref>Violence and schizophrenia: | |||
| * {{cite journal |author=Walsh E, Buchanan A, Fahy T |title=Violence and schizophrenia: examining the evidence |journal=British Journal of Psychiatry |volume=180 |pages=490–5 |year=2002 |month=June |pmid=12042226 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=12042226 |accessdate=2008-07-04 |doi=10.1192/bjp.180.6.490}} | |||
| * {{cite journal |author=Stuart H |title=Violence and mental illness: an overview |journal=World Psychiatry |volume=2 |issue=2 |pages=121–24 |year=2003 |month=June |pmid=16946914 |pmc=1525086}} | |||
| * {{cite journal |author=Steadman HJ, Mulvey EP, Monahan J, ''et al.'' |title=Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods |journal=Archives of General Psychiatry |volume=55 |issue=5 |pages=393–401 |year=1998 |month=May |pmid=9596041 |url=http://archpsyc.ama-assn.org/cgi/pmidlookup?view=long&pmid=9596041 |accessdate=2008-07-04 |doi=10.1001/archpsyc.55.5.393}} | |||
| * {{cite journal |author=Swanson JW, Swartz MS, Van Dorn RA, ''et al.'' |title=A national study of violent behavior in persons with schizophrenia |journal=Archives of General Psychiatry |volume=63 |issue=5 |pages=490–9 |year=2006 |month=May |pmid=16651506 |doi=10.1001/archpsyc.63.5.490 |url=http://archpsyc.ama-assn.org/cgi/pmidlookup?view=long&pmid=16651506 |accessdate=2008-07-04}} | |||
| * {{cite journal |author=Swanson JW, Holzer CE, Ganju VK, Jono RT |title=Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys |journal=Hospital and Community Psychiatry |volume=41 |issue=7 |pages=761–70 |year=1990 |month=July |pmid=2142118 |url=http://ps.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=2142118 |accessdate=2008-07-04}}</ref> Studies have indicated that 5% to 10% of those charged with murder in Western countries have a schizophrenia spectrum disorder.<ref name="Mullen 06">{{cite journal |author=Mullen PE |year=2006 |title=Schizophrenia and violence: from correlations to preventive strategies |journal=Advances in Psychiatric Treatment |volume=12 |pages=239–248 |url=http://apt.rcpsych.org/cgi/content/abstract/12/4/239 |accessdate=2008-07-04 |doi=10.1192/apt.12.4.239}}</ref><ref name="fn_52">{{cite journal |author=Simpson AI, McKenna B, Moskowitz A, Skipworth J, Barry-Walsh J |title=Homicide and mental illness in New Zealand, 1970–2000 |journal=British Journal of Psychiatry |volume=185 |pages=394–8 |year=2004 |month=November |pmid=15516547 |doi=10.1192/bjp.185.5.394 |url=http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=15516547 |accessdate=2008-07-04}}</ref><ref name="fn_53">{{cite journal |author=Fazel S, Grann M |title=Psychiatric morbidity among homicide offenders: a Swedish population study |journal=American Journal of Psychiatry |volume=161 |issue=11 |pages=2129–31 |year=2004 |month=November |pmid=15514419 |doi=10.1176/appi.ajp.161.11.2129 |url=http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=15514419 |accessdate=2008-07-04}}</ref> | |||
| Some studies have shown little evidence for the effectiveness of CBT in either reducing symptoms or preventing relapse.<ref>{{cite journal | vauthors = Jauhar S, McKenna PJ, Radua J, Fung E, Salvador R, Laws KR | title = Cognitive-behavioural therapy for the symptoms of schizophrenia: systematic review and meta-analysis with examination of potential bias | journal = The British Journal of Psychiatry | volume = 204 | issue = 1 | pages = 20–29 | date = January 2014 | pmid = 24385461 | doi = 10.1192/bjp.bp.112.116285 | type = Review | doi-access = free }}</ref><ref name=Jones2018>{{cite journal | vauthors = Jones C, Hacker D, Meaden A, Cormac I, Irving CB, Xia J, Zhao S, Shi C, Chen J | title = Cognitive behavioural therapy plus standard care versus standard care plus other psychosocial treatments for people with schizophrenia | journal = The Cochrane Database of Systematic Reviews | volume = 11 | issue = 11 | pages = CD008712 | date = November 2018 | pmid = 30480760 | pmc = 6516879 | doi = 10.1002/14651858.CD008712.pub3 }}</ref> However, other studies have found that CBT does improve overall psychotic symptoms (when in use with medication) and it has been recommended in Canada, but has been seen to have no effect on social function, relapse, or quality of life.<ref>{{cite journal | title = Cognitive Behavioural Therapy for Psychosis: A Health Technology Assessment| journal = Ontario Health Technology Assessment Series | date = 2018 |volume = 18 | issue = 5 |pages = 1–141 | pmid = 30443277 | pmc = 6235075 | author = Health Quality Ontario }}</ref> In the UK it is recommended as an add-on therapy in the treatment of schizophrenia.<ref name=nhsTreatment/><ref name=Jones2018/> ] are seen to improve negative symptoms in some people, and are recommended by NICE in the UK.<ref name=nhsTreatment>{{cite web | title = Schizophrenia – Treatment | url = https://www.nhs.uk/conditions/schizophrenia/treatment/ | publisher= UK ] | access-date = 8 January 2020 | date = 23 October 2017}}</ref> This approach is criticised as having not been well-researched,<ref>{{cite journal | vauthors = Ruddy R, Milnes D | title = Art therapy for schizophrenia or schizophrenia-like illnesses | journal = The Cochrane Database of Systematic Reviews | issue = 4 | page = CD003728 | date = October 2005 | pmid = 16235338 | doi = 10.1002/14651858.CD003728.pub2 | url = http://www.cochrane.org/reviews/en/ab003728.html | archive-url = https://web.archive.org/web/20111027132811/http://www2.cochrane.org/reviews/en/ab003728.html | df = dmy-all | url-status=live | archive-date = 27 October 2011 }}</ref><ref>{{cite journal | vauthors = Ruddy RA, Dent-Brown K | title = Drama therapy for schizophrenia or schizophrenia-like illnesses | journal = The Cochrane Database of Systematic Reviews | issue = 1 | page = CD005378 | date = January 2007 | pmid = 17253555 | doi = 10.1002/14651858.CD005378.pub2 | url = http://www.cochrane.org/reviews/en/ab005378.html | archive-url = https://web.archive.org/web/20110825024045/http://www2.cochrane.org/reviews/en/ab005378.html | df = dmy-all | url-status=live | archive-date = 25 August 2011 }}</ref> and arts therapies are not recommended in Australian guidelines for example.<ref>{{cite journal |vauthors=Galletly C, Castle D, Dark F, et al |title=Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders |journal=Aust N Z J Psychiatry |volume=50 |issue=5 |pages=410–472 |date=May 2016 |pmid=27106681 |doi=10.1177/0004867416641195 |s2cid=6536743 |url=|doi-access=free }}</ref> ], in which people with ] of schizophrenia, provide help to each other, is of unclear benefit.<ref>{{cite journal |vauthors= Chien WT, Clifton AV, Zhao S, Lui S |title=Peer support for people with schizophrenia or other serious mental illness. |journal=The Cochrane Database of Systematic Reviews |date=4 April 2019 |volume=4 |issue=6 |page=CD010880 |doi=10.1002/14651858.CD010880.pub2 |pmid=30946482|pmc=6448529 }}</ref> | |||
| The occurrence of ] in schizophrenia has sometimes been linked to a higher risk of violent acts. Findings on the specific role of delusions or hallucinations have been inconsistent, but have focused on delusional jealousy, perception of threat and command hallucinations. It has been proposed that a certain type of individual with schizophrenia may be most likely to offend, characterized by a history of educational difficulties, low ], conduct disorder, early-onset substance misuse and offending prior to diagnosis.<ref name= "Mullen 06"/> | |||
| ===Other=== | |||
| Individuals with a diagnosis of schizophrenia are often the ] of violent crime—at least 14 times more often than they are perpetrators.<ref>{{cite journal |author=Brekke JS, Prindle C, Bae SW, Long JD |title=Risks for individuals with schizophrenia who are living in the community |journal=Psychiatr Serv |volume=52 |issue=10 |pages=1358–66 |year=2001 |month=October |pmid=11585953 |doi= 10.1176/appi.ps.52.10.1358|url=http://ps.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=11585953 |accessdate=2008-07-04}}</ref><ref name="fn_55">{{cite journal |author=Fitzgerald PB, de Castella AR, Filia KM, Filia SL, Benitez J, Kulkarni J |title=Victimization of patients with schizophrenia and related disorders |journal=The Australian and New Zealand Journal of Psychiatry |volume=39 |issue=3 |pages=169–74 |year=2005 |month=March |pmid=15701066 |doi=10.1111/j.1440-1614.2005.01539.x}}</ref> Another consistent finding is a link to substance misuse, particularly alcohol,<ref name="fn_51">{{cite journal |author=Walsh E, Gilvarry C, Samele C, ''et al.'' |title=Predicting violence in schizophrenia: a prospective study |journal=Schizophrenia Research |volume=67 |issue=2–3 |pages=247–52 |year=2004 |month=April |pmid=14984884 |doi=10.1016/S0920-9964(03)00091-4 |url=http://linkinghub.elsevier.com/retrieve/pii/S0920996403000914 |accessdate=2008-07-04}}</ref> among the minority who commit violent acts. Violence by or against individuals with schizophrenia typically occurs in the context of complex social interactions within a family setting,<ref>{{cite journal |author=Solomon PL, Cavanaugh MM, Gelles RJ |title=Family violence among adults with severe mental illness: a neglected area of research |journal=Trauma Violence Abuse |volume=6 |issue=1 |pages=40–54 |year=2005 |month=January |pmid=15574672 |doi=10.1177/1524838004272464 |url=http://tva.sagepub.com/cgi/pmidlookup?view=long&pmid=15574672 |accessdate=2008-07-04}}{subscription required)</ref> and is also an issue in clinical services<ref>{{cite journal |author=Chou KR, Lu RB, Chang M |title=Assaultive behavior by psychiatric in-patients and its related factors |journal=J Nurs Res |volume=9 |issue=5 |pages=139–51 |year=2001 |month=December |pmid=11779087}}</ref> and in the wider community.<ref>{{cite journal |author=Lögdberg B, Nilsson LL, Levander MT, Levander S |title=Schizophrenia, neighbourhood, and crime |journal=Acta Psychiatrica Scandinavica |volume=110 |issue=2 |pages=92–7 |year=2004 |month=August |pmid=15233709 |doi=10.1111/j.1600-0047.2004.00322.x}}</ref> | |||
| Exercise including aerobic exercise has been shown to improve positive and negative symptoms, cognition, working memory, and improve quality of life.<ref name=Girdler2019>{{cite journal | vauthors =Girdler SJ, Confino JE, Woesner ME | title = Exercise as a Treatment for Schizophrenia: A Review. |journal= Psychopharmacology Bulletin | date = 15 February 2019 | volume = 49 | issue = 1 | pages=56–69 | pmid=30858639| pmc = 6386427 }}</ref><ref name=Firth2017>{{cite journal | vauthors = Firth J | title = Aerobic Exercise Improves Cognitive Functioning in People With Schizophrenia: A Systematic Review and Meta-Analysis | journal = Schizophrenia Bulletin | date = 1 May 2017 | volume = 43 | issue = 3 | pages = 546–556 | doi = 10.1093/schbul/sbw115 | pmid = 27521348| pmc = 5464163 }}</ref> Exercise has also been shown to increase the volume of the ] in those with schizophrenia. A decrease in hippocampal volume is one of the factors linked to the development of the disease.<ref name=Girdler2019/> However, there still remains the problem of increasing motivation for, and maintaining participation in physical activity.<ref>{{cite journal | vauthors = Tréhout M, Dollfus S |title = . | journal = L'Encéphale | date = December 2018 | volume = 44 | issue = 6 | pages = 538–547 | doi=10.1016/j.encep.2018.05.005 | pmid = 29983176|s2cid = 150334210 }}</ref> Supervised sessions are recommended.<ref name=Firth2017/> In the UK healthy eating advice is offered alongside exercise programs.<ref>{{cite web |title=Quality statement 7: Promoting healthy eating, physical activity and smoking cessation {{!}} Psychosis and schizophrenia in adults |date=12 February 2015 |url=https://www.nice.org.uk/guidance/qs80/chapter/Quality-statement-7-Promoting-healthy-eating-physical-activity-and-smoking-cessation |publisher= UK ]}}</ref> | |||
| An inadequate diet is often found in schizophrenia, and associated vitamin deficiencies including those of ], and ] are linked to the risk factors for the development of schizophrenia and for early death including heart disease.<ref name=Firth2018>{{cite journal | vauthors = Firth J, Carney R, Stubbs B, Teasdale SB, Vancampfort D, Ward PB, Berk M, Sarris J | title = Nutritional Deficiencies and Clinical Correlates in First-Episode Psychosis: A Systematic Review and Meta-analysis | journal = Schizophrenia Bulletin | volume = 44 | issue = 6 | pages = 1275–1292 | date = October 2018 | pmid = 29206972 | pmc = 6192507 | doi = 10.1093/schbul/sbx162 }}</ref><ref name=Rastogi2020>{{cite journal | vauthors = Rastogi A, Viani-Walsh D, Akbari S, Gall N, Gaughran F, Lally J | title = Pathogenesis and management of Brugada syndrome in schizophrenia: A scoping review | journal = General Hospital Psychiatry | volume = 67 | pages = 83–91 | date = October 2020 | pmid = 33065406 | pmc = 7537626 | doi = 10.1016/j.genhosppsych.2020.09.003 }}</ref> Those with schizophrenia possibly have the worst diet of all the mental disorders. Lower levels of folate and vitamin D have been noted as significantly lower in first episode psychosis.<ref name=Firth2018/> The use of supplemental folate is recommended.<ref>{{cite journal | vauthors = Martone G | title = Enhancement of recovery from mental illness with l-methylfolate supplementation | journal = Perspectives in Psychiatric Care | volume = 54 | issue = 2 | pages = 331–334 | date = April 2018 | pmid = 28597528 | doi = 10.1111/ppc.12227 | doi-access = free }}</ref> A ] has also been noted.<ref name=Firth2019>{{cite journal | vauthors = Firth J, Teasdale SB, Allott K, Siskind D, Marx W, Cotter J, Veronese N, Schuch F, Smith L, Solmi M, Carvalho AF, Vancampfort D, Berk M, Stubbs B, Sarris J | title = The efficacy and safety of nutrient supplements in the treatment of mental disorders: a meta-review of meta-analyses of randomized controlled trials | journal = World Psychiatry | volume = 18 | issue = 3 | pages = 308–324 | date = October 2019 | pmid = 31496103 | pmc = 6732706 | doi = 10.1002/wps.20672 }}</ref> ] is also often deficient and this is linked to worse symptoms. Supplementation with B vitamins has been shown to significantly improve symptoms, and to put in reverse some of the cognitive deficits.<ref name=Firth2018/> It is also suggested that the noted dysfunction in gut microbiota might benefit from the use of ].<ref name=Firth2019/> | |||
| ==Epidemiology== | |||
| ] for schizophrenia per 100,000 inhabitants in 2002.<div class="references-small" style="-moz-column-count:3; column-count:3;"> | |||
| ==Prognosis== | |||
| {{Main|Prognosis of schizophrenia}}{{See also|Physical health in schizophrenia}} | |||
| ]s lost due to schizophrenia per 100,000 inhabitants in 2004 | |||
| {{Col-begin}} | |||
| {{Col-break}} | |||
| {{legend|#b3b3b3|no data}} | {{legend|#b3b3b3|no data}} | ||
| {{legend|#ffff65|≤ 185}} | {{legend|#ffff65|≤ 185}} | ||
| Line 220: | Line 212: | ||
| {{legend|#ffb000|218–229}} | {{legend|#ffb000|218–229}} | ||
| {{legend|#ff9a00|229–240}} | {{legend|#ff9a00|229–240}} | ||
| {{Col-break}} | |||
| {{legend|#ff8400|240–251}} | {{legend|#ff8400|240–251}} | ||
| {{legend|#ff6e00|251–262}} | {{legend|#ff6e00|251–262}} | ||
| Line 226: | Line 219: | ||
| {{legend|#ff2c00|284–295}} | {{legend|#ff2c00|284–295}} | ||
| {{legend|#cb0000|≥ 295}} | {{legend|#cb0000|≥ 295}} | ||
| {{col-end}}]] | |||
| </div>]] | |||
| <!-- Life expectancy --> | |||
| Schizophrenia occurs equally in males and females, although typically appears earlier in men—the peak ages of onset are 20–28 years for males and 26–32 years for females.<ref name="castle1991" /> Onset in childhood is much rarer,<ref name="Kumra_et_al_2001">{{cite journal |author=Kumra S |coauthors=Shaw M, Merka P, Nakayama E, Augustin R |year=2001 |title=Childhood-onset schizophrenia: research update |journal=Canadian Journal of Psychiatry |volume=46 | issue=10 |pages=923–30 |pmid=11816313}}</ref> as is onset in middle- or old age.<ref>{{cite book | last = Hassett | first = Anne, et al. (eds) | title = Psychosis in the Elderly | publisher = London: Taylor and Francis. |isbn=1841843946 | date = 2005 | pages = 6 | url = http://books.google.com/books?id=eLaMOJ9oj28C&printsec=frontcover&dq=Psychosis+in+the+Elderly&ei=LC3tSYCYH4G4M9Sz6OkN | isbn = 1841843946}}</ref> The ] of schizophrenia—the proportion of individuals expected to experience the disease at any time in their lives—is commonly given at 1%. However, a 2002 ] of many studies found a lifetime prevalence of 0.55%.<ref name="fn_34" /> Despite the received wisdom that schizophrenia occurs at similar rates worldwide, its prevalence varies across the world,<ref name="Jablensky_et_al_1992">{{cite journal |author=Jablensky A |coauthors=Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, Day R, Bertelsen A |year=1992 |title=Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study |journal=Psychological Medicine Monograph Supplement |volume=20 |pages=1–97 |pmid=1565705 |doi=10.1017/S0264180100000904}}</ref> within countries,<ref name="Kirkbride_et_al_2006">{{cite journal |author=Kirkbride JB |coauthors=Fearon P, Morgan C, Dazzan P, Morgan K, Tarrant J, Lloyd T, Holloway J, Hutchinson G, Leff JP, Mallett RM, Harrison GL, Murray RM, Jones PB |year=2006 |title=Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings From the 3-center ÆSOP study |journal=] |volume=63 | issue=3 |pages=250–58 |pmid=16520429 |doi=10.1001/archpsyc.63.3.250}}</ref> and at the local and neighbourhood level.<ref name="Kirkbride_et_al_2007">{{cite journal |author=Kirkbride JB |coauthors=Fearon P, Morgan C, Dazzan P, Morgan K, Murray RM, Jones PB |year=2007 |title=Neighbourhood variation in the incidence of psychotic disorders in Southeast London |journal=Social Psychiatry and Psychiatric Epidemiology |volume=42 | issue=6 |pages=438–45 |pmid=17473901 | doi = 10.1007/s00127-007-0193-0}}</ref> One particularly stable and replicable finding has been the association between living in an ] environment and schizophrenia diagnosis, even after factors such as ], ] and size of ] have been controlled for.<ref name="fn_19">{{cite journal |author=Van Os J |year=2004 |title=Does the urban environment cause psychosis? |journal=] |volume=184 | issue=4 |pages=287–288 |pmid=15056569 |doi=10.1192/bjp.184.4.287}}</ref> Schizophrenia is known to be a major cause of ]. In a 1999 study of 14 countries, active ] was ranked the third-most-disabling condition after ] and ] and ahead of ] and ].<ref name="fn_35">{{cite journal |author=Ustun TB |coauthors=Rehm J, Chatterji S, Saxena S, Trotter R, Room R, Bickenbach J, and the ]/] Joint Project CAR Study Group |year=1999 |title=Multiple-informant ranking of the disabling effects of different health conditions in 14 countries |journal=] |volume=354 | issue=9173 |pages=111–15 |pmid=10408486 |doi=10.1016/S0140-6736(98)07507-2}}</ref> | |||
| Schizophrenia has great human and economic costs.<ref name=Lancet2016/> It decreases life expectancy by between 10<ref name=Laursen2014/><!-- Laursen2014 shows a range of 10-25 in the article text--> and 28 years.<ref name=NIHStat/> This is primarily because of its association with heart disease,<ref name=Kritharides2017>{{cite journal |vauthors=Kritharides L, Chow V, Lambert TJ |date=6 February 2017 |title=Cardiovascular disease in patients with schizophrenia |journal=The Medical Journal of Australia |volume=206 |issue=2 |pages=91–95 |doi=10.5694/mja16.00650 |pmid=28152356 |s2cid=5388097}}</ref> diabetes,<ref name=NIHStat/> ], poor diet, a ], and smoking, with an increased rate of suicide playing a lesser role.<ref name=Laursen2014/><ref>{{cite journal | vauthors = Erlangsen A, Eaton WW, Mortensen PB, Conwell Y | title = Schizophrenia—a predictor of suicide during the second half of life? | journal = Schizophrenia Research | volume = 134 | issue = 2–3 | pages = 111–117 | date = February 2012 | pmid = 22018943 | pmc = 3266451 | doi = 10.1016/j.schres.2011.09.032 }}</ref> Side effects of antipsychotics may also increase the risk.<ref name=Laursen2014/> | |||
| Almost 40% of those with schizophrenia die from complications of cardiovascular disease which is seen to be increasingly associated.<ref name=Rastogi2020/> An underlying factor of sudden cardiac death may be ] (BrS) – BrS mutations that overlap with those linked with schizophrenia are the ] mutations.<ref name=Rastogi2020/> BrS may also be drug-induced from certain antipsychotics and antidepressants.<ref name=Rastogi2020/> ], or excessive fluid intake, is relatively common in people with chronic schizophrenia.<ref>{{cite book| vauthors = Goroll AH, Mulley AG |title=Primary Care Medicine: Office Evaluation and Management of The Adult Patient |edition=Sixth|date=2011|publisher=Lippincott Williams & Wilkins|isbn=978-1-4511-2159-9|page=Chapter 101|url=https://books.google.com/books?id=fXpKo1afC2YC&pg=PT1766}}</ref><ref name=Rizvi2019>{{cite journal | vauthors = Rizvi S, Gold J, Khan AM | title = Role of Naltrexone in Improving Compulsive Drinking in Psychogenic Polydipsia. | journal = Cureus | date = 5 August 2019 | volume = 11 | issue = 8 | page =e5320 | doi = 10.7759/cureus.5320 | doi-access = free | pmid = 31598428| pmc = 6777931 }}</ref> This may lead to ] which can be life-threatening. Antipsychotics can lead to a ], but there are several other factors that may contribute to the disorder; it may reduce life expectancy by 13 percent.<ref name=Rizvi2019/> Barriers to improving the mortality rate in schizophrenia are poverty, overlooking the symptoms of other illnesses, stress, stigma, and medication side effects.<ref>{{cite journal |vauthors=Seeman MV |s2cid=170078453 |title=Schizophrenia Mortality: Barriers to Progress |journal=The Psychiatric Quarterly |volume=90 |issue=3 |pages=553–563 |date=September 2019 |pmid=31147816 |doi=10.1007/s11126-019-09645-0}}</ref> | |||
| <!-- Disability --> | |||
| Schizophrenia is a major cause of ]. In 2016, it was classed as the 12th most disabling condition.<ref>{{cite journal | vauthors = Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, McGrath JJ, Whiteford HA | title = Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016 | journal = Schizophrenia Bulletin | volume = 44 | issue = 6 | pages = 1195–1203 | date = October 2018 | pmid = 29762765 | pmc = 6192504 | doi = 10.1093/schbul/sby058 }}</ref> Approximately 75% of people with schizophrenia have ongoing disability with relapses.<ref>{{cite journal | vauthors = Smith T, Weston C, Lieberman J | title = Schizophrenia (maintenance treatment) | journal = American Family Physician | volume = 82 | issue = 4 | pages = 338–339 | date = August 2010 | pmid = 20704164}}</ref> Some people do recover completely and others function well in society.<ref>{{cite journal | vauthors = Warner R | s2cid = 26666000 | title = Recovery from schizophrenia and the recovery model | journal = Current Opinion in Psychiatry | volume = 22 | issue = 4 | pages = 374–380 | date = July 2009 | pmid = 19417668 | doi = 10.1097/YCO.0b013e32832c920b }}</ref> Most people with schizophrenia live independently with community support.<ref name=Lancet2009/> About 85% are unemployed.<ref name=Lancet2016/> In people with a first episode of psychosis in schizophrenia a good long-term outcome occurs in 31%, an intermediate outcome in 42% and a poor outcome in 31%.<ref>{{cite journal | vauthors = Menezes NM, Arenovich T, Zipursky RB | s2cid = 23475454 | title = A systematic review of longitudinal outcome studies of first-episode psychosis | journal = Psychological Medicine | volume = 36 | issue = 10 | pages = 1349–62 | date = October 2006 | pmid = 16756689 | doi = 10.1017/S0033291706007951 | url = https://pdfs.semanticscholar.org/8539/923c1b4f6bacb128d478b9ec7f6e95559210.pdf | archive-url = https://web.archive.org/web/20200922015257/https://pdfs.semanticscholar.org/8539/923c1b4f6bacb128d478b9ec7f6e95559210.pdf | archive-date = 22 September 2020}}</ref> Males are affected more often than females, and have a worse outcome.<ref>{{cite book |vauthors=Coyle JT |title=Neurodegenerative Diseases |chapter=Schizophrenia: Basic and Clinical |series=Advances in Neurobiology |volume=15 |pages=255–280 |date=2017 |pmid=28674984 |doi=10.1007/978-3-319-57193-5_9|isbn=978-3-319-57191-1 }}</ref> Studies showing that outcomes for schizophrenia appear better in the ] than the ]<ref name=Isa07>{{cite journal | vauthors = Isaac M, Chand P, Murthy P | title = Schizophrenia outcome measures in the wider international community | journal = The British Journal of Psychiatry. Supplement | volume = 50 | pages = s71–77 | date = August 2007 | pmid = 18019048 | doi = 10.1192/bjp.191.50.s71 | doi-access = free }}</ref> have been questioned.<ref>{{cite journal | vauthors = Cohen A, Patel V, Thara R, Gureje O | title = Questioning an axiom: better prognosis for schizophrenia in the developing world? | journal = Schizophrenia Bulletin | volume = 34 | issue = 2 | pages = 229–244 | date = March 2008 | pmid = 17905787 | pmc = 2632419 | doi = 10.1093/schbul/sbm105 }}</ref> Social problems, such as long-term unemployment, poverty, homelessness, exploitation, ] and victimization are common consequences, and lead to ].<ref name=Killaspy2014/><ref name=Charleson2018/> | |||
| <!-- Suicide --> | |||
| There is a higher than average ] associated with schizophrenia estimated at 5% to 6%, most often occurring in the period following onset or first hospital admission.<ref name=Ferri2019>{{cite book |title=Ferri's clinical advisor 2019: 5 books in 1 |pages=1225–1226|date=2019 |isbn=9780323530422 | vauthors = Ferri FF |publisher=Elsevier }}</ref><ref name=Jop2010/> Several times more (20 to 40%) attempt suicide at least once.<ref name=DSM5/><ref name=Chiang2016/> There are a variety of risk factors, including male sex, depression, a high ],<ref>{{cite journal | vauthors = Carlborg A, Winnerbäck K, Jönsson EG, Jokinen J, Nordström P | s2cid = 204385719 | title = Suicide in schizophrenia | journal = Expert Review of Neurotherapeutics | volume = 10 | issue = 7 | pages = 1153–1164 | date = July 2010 | pmid = 20586695 | doi = 10.1586/ern.10.82 | doi-access = free }}</ref> heavy smoking,<ref>{{cite journal |vauthors=Tsoi DT, Porwal M, Webster AC |title=Interventions for smoking cessation and reduction in individuals with schizophrenia |journal=The Cochrane Database of Systematic Reviews |issue=2 |page=CD007253 |date=28 February 2013 |volume=2013 |pmid=23450574|doi=10.1002/14651858.CD007253.pub3|pmc=6486303 }}</ref> and substance use.<ref name=Khokhar2018/> Repeated relapse is linked to an increased risk of suicidal behavior.<ref name=Taylor2019/> The use of clozapine can reduce the risk of suicide, and of aggression.<ref>{{cite journal |vauthors=Sriretnakumar V, Huang E, Müller DJ |date=2015 |title=Pharmacogenetics of clozapine treatment response and side-effects in schizophrenia: an update |journal=Expert Opinion on Drug Metabolism & Toxicology |volume=11 |issue=11 |pages=1709–1731 |doi=10.1517/17425255.2015.1075003 |pmid=26364648 |s2cid=207492339}}</ref> | |||
| <!-- Drug use --> | |||
| A strong association between ] has been shown in worldwide studies.<ref>{{cite journal | vauthors = de Leon J, Diaz FJ | s2cid = 32975940 | title = A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors | journal = Schizophrenia Research | volume = 76 | issue = 2–3 | pages = 135–157 | date = July 2005 | pmid = 15949648 | doi = 10.1016/j.schres.2005.02.010 }}</ref><ref name=Keltner2006>{{cite journal | vauthors = Keltner NL, Grant JS | title = Smoke, smoke, smoke that cigarette | journal = Perspectives in Psychiatric Care | volume = 42 | issue = 4 | pages = 256–261 | date = November 2006 | pmid = 17107571 | doi = 10.1111/j.1744-6163.2006.00085.x }}</ref> ] is especially high in those diagnosed with schizophrenia, with estimates ranging from 80 to 90% being regular smokers, as compared to 20% of the general population.<ref name=Keltner2006/> Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content.<ref name=DSMIV/> Some propose that this is in an effort to improve symptoms.<ref>{{cite journal | vauthors = Kumari V, Postma P | s2cid = 15581894 | title = Nicotine use in schizophrenia: the self medication hypotheses | journal = Neuroscience and Biobehavioral Reviews | volume = 29 | issue = 6 | pages = 1021–1034 | date = January 2005 | pmid = 15964073 | doi = 10.1016/j.neubiorev.2005.02.006 }}</ref> Among people with schizophrenia use of cannabis is also common.<ref name=Khokhar2018/> | |||
| Schizophrenia leads to an increased risk of dementia.<ref>{{cite journal |vauthors=Cai L, Huang J |title=Schizophrenia and risk of dementia: a meta-analysis study |journal=Neuropsychiatr Dis Treat |volume=14 |issue= |pages=2047–2055 |date=2018 |pmid=30147318 |pmc=6095111 |doi=10.2147/NDT.S172933 |doi-access=free }}</ref> | |||
| ===Violence=== | |||
| Most people with schizophrenia are not aggressive, and are more likely to be victims of violence rather than perpetrators.<ref name=DSM5/> People with schizophrenia are commonly exploited and victimized by violent crime as part of a broader dynamic of social exclusion.<ref name=Killaspy2014/><ref name=Charleson2018/> People diagnosed with schizophrenia are also subject to forced drug injections, seclusion, and restraint at high rates.<ref name=BeckerKilian2006/><ref name=Capdevielle2009/> | |||
| The risk of violence by people with schizophrenia is small. There are minor subgroups where the risk is high.<ref name=Richard-Devantoy2009>{{cite journal |vauthors=Richard-Devantoy S, Olie JP, Gourevitch R |title= |journal=L'Encephale |volume=35 |issue=6 |pages=521–530 |date=December 2009 |pmid=20004282 |doi=10.1016/j.encep.2008.10.009}}</ref> This risk is usually associated with a comorbid disorder such as a substance use disorder – in particular alcohol, or with antisocial personality disorder.<ref name=Richard-Devantoy2009/> Substance use disorder is strongly linked, and other risk factors are linked to deficits in cognition and social cognition including facial perception and insight that are in part included in ] impairments.<ref>{{cite journal |vauthors=Ng R, Fish S, Granholm E |title=Insight and theory of mind in schizophrenia. |journal=Psychiatry Research |volume=225 |issue=1–2 |pages=169–174 |date=30 January 2015 |pmid=25467703 |doi=10.1016/j.psychres.2014.11.010|pmc=4269286 }}</ref><ref>{{cite journal |vauthors=Bora E |title=Relationship between insight and theory of mind in schizophrenia: A meta-analysis |journal=Schizophrenia Research |volume=190 |pages=11–17 |date=December 2017 |pmid=28302393 |doi=10.1016/j.schres.2017.03.029|s2cid=36263370 }}</ref> Poor cognitive functioning, decision-making, and facial perception may contribute to making a wrong judgement of a situation that could result in an inappropriate response such as violence.<ref>{{cite journal |vauthors=Darmedru C, Demily C, Franck N |title= |journal=L'Encephale |volume=44 |issue=2 |pages=158–167 |date=April 2018 |pmid=28641817 |doi=10.1016/j.encep.2017.05.001}}</ref> These associated risk factors are also present in antisocial personality disorder which when present as a comorbid disorder greatly increases the risk of violence.<ref>{{cite journal | vauthors = Richard-Devantoy S, Bouyer-Richard AI, Jollant F, Mondoloni A, Voyer M, Senon JL | title = | journal = Revue d'Épidemiologie et de Santé Publique | volume = 61 | issue = 4 | pages = 339–350 | date = August 2013 | pmid = 23816066 | doi = 10.1016/j.respe.2013.01.096 }}</ref><ref>{{cite journal | vauthors = Sedgwick O, Young S, Baumeister D, Greer B, Das M, Kumari V | title = Neuropsychology and emotion processing in violent individuals with antisocial personality disorder or schizophrenia: The same or different? A systematic review and meta-analysis | journal = The Australian and New Zealand Journal of Psychiatry | volume = 51 | issue = 12 | pages = 1178–1197 | date = December 2017 | pmid = 28992741 | doi = 10.1177/0004867417731525 | s2cid = 206401875 | doi-access = free }}</ref> | |||
| ==Epidemiology== | |||
| {{Main|Epidemiology of schizophrenia}} | |||
| [[File:Schizophrenia world map-Deaths per million persons-WHO2012.svg|thumb|upright=1.3|Deaths per million persons due to schizophrenia in 2012 | |||
| {{Div col|small=yes|colwidth=10em}} | |||
| {{legend|#ffff20|0–0}}{{legend|#ffc020|1–1}}{{legend|#ff9a20|2–2}}{{legend|#f08015|3–3}}{{legend|#d85010|4–6}}{{legend|#d02010|7–20}}{{div col end}}]] | |||
| In 2017,{{update after|2022|8|22}} the ] estimated there were 1.1 million new cases;<ref name=GBD2018/> in 2022 the World Health Organization (WHO) reported a total of 24 million cases globally.<ref name=WHO2022/> Schizophrenia affects around 0.3–0.7% of people at some point in their life.<ref name=Javitt2014/><ref name=NIHStat>{{cite web|title=Schizophrenia |url= http://www.nimh.nih.gov/health/statistics/prevalence/schizophrenia.shtml |date= 22 April 2022 |access-date= 23 August 2022 |publisher= US ] (NIMH)|work= Statistics}}</ref> In areas of conflict this figure can rise to between 4.0 and 6.5%.<ref>{{cite journal | vauthors = Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S | title = New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis | journal = Lancet | volume = 394 | issue = 10194 | pages = 240–248 | date = July 2019 | pmid = 31200992 | pmc = 6657025 | doi = 10.1016/S0140-6736(19)30934-1 }}</ref> It occurs 1.4 times more frequently in males than females and typically appears earlier in men.<ref name=BMJ07/> | |||
| Worldwide, schizophrenia is the most common ].<ref name=Kar2016/> The frequency of schizophrenia varies across the world,<ref name=DSM5/> within countries,<ref>{{cite journal | vauthors = Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Tarrant J, Lloyd T, Holloway J, Hutchinson G, Leff JP, Mallett RM, Harrison GL, Murray RM, Jones PB | title = Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study | journal = Archives of General Psychiatry | volume = 63 | issue = 3 | pages = 250–258 | date = March 2006 | pmid = 16520429 | doi = 10.1001/archpsyc.63.3.250 | doi-access = free }}</ref> and at the local and neighborhood level;<ref>{{cite journal | vauthors = Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Murray RM, Jones PB | title = Neighbourhood variation in the incidence of psychotic disorders in Southeast London | journal = Social Psychiatry and Psychiatric Epidemiology | volume = 42 | issue = 6 | pages = 438–445 | date = June 2007 | pmid = 17473901 | doi = 10.1007/s00127-007-0193-0 | s2cid = 19655724 }}</ref> this variation in ] between studies over time, across geographical locations, and by gender is as high as fivefold.<ref name=Lancet2016/> | |||
| Schizophrenia causes approximately one percent of worldwide ]{{update after|2022|8|24}}<ref name=BMJ07/> and resulted in 17,000 deaths in 2015.<ref name=GBD2015/> | |||
| In 2000,{{update after|2022|8|22}} WHO found the percentage of people affected and the number of new cases that develop each year is roughly similar around the world, with age-standardized prevalence per 100,000 ranging from 343 in Africa to 544 in Japan and Oceania for men, and from 378 in Africa to 527 in Southeastern Europe for women.<ref>{{update after|2022|8|22}} {{cite web|title=Global burden of schizophrenia in the year 2000|date= 15 August 2006| url=https://www.who.int/healthinfo/statistics/bod_schizophrenia.pdf|publisher=] | vauthors = Ayuso-Mateos JL |access-date=27 February 2013|url-status=live|archive-url=https://web.archive.org/web/20160304075113/http://www.who.int/healthinfo/statistics/bod_schizophrenia.pdf|archive-date=4 March 2016}}</ref> | |||
| ==History== | ==History== | ||
| {{Main|History of schizophrenia}} | {{Main|History of schizophrenia}} | ||
| Accounts of a schizophrenia-like ] are thought to be rare in the historical record before the 1800s, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning ], and accounts by ] published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature.<ref name="Heinrichs2003">{{cite journal |author=Heinrichs RW |title=Historical origins of schizophrenia: two early madmen and their illness |journal=J Hist Behav Sci |volume=39 |issue=4 |pages=349–63 |year=2003 |pmid=14601041 |doi=10.1002/jhbs.10152}}</ref> Schizophrenia was first described as a distinct syndrome affecting teenagers and young adults by ] in 1853, termed ''démence précoce'' (literally 'early dementia'). The term ] was used in 1891 by ] to in a case report of a psychotic disorder. In 1893 ] introduced a broad new distinction in the ] between '']'' and ] (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that ''dementia praecox'' was primarily a disease of the brain,<ref name="fn_2">{{cite book |last1=Kraepelin |first1=E. |others=Diefendorf A.R. |title=Text book of psychiatry |edition=7 |year=1907 |publisher=Macmillan |location=London }}</ref> and particularly a form of ], distinguished from other forms of dementia, such as ], which typically occur later in life.<ref name="fn_49">{{cite book |author=Hansen RA, Atchison B |title=Conditions in occupational therapy: effect on occupational performance |publisher=Lippincott Williams & Wilkins |location=Hagerstown, MD |year=2000 |isbn=0-683-30417-8}}</ref> | |||
| ===Conceptual development=== | |||
| The word ''schizophrenia''—which translates roughly as "splitting of the mind" and comes from the ] roots ''schizein'' (σχίζειν, "to split") and ''phrēn'', ''phren-'' (φρήν, φρεν-, "]")<ref>{{cite journal |author=Kuhn R; |title=Eugen Bleuler's concepts of psychopathology |journal=Hist Psychiatry |volume=15 |issue=3 |year=2004 |pages=361–6 |doi=10.1177/0957154X04044603 |pmid=15386868 |others=tr. Cahn CH}}</ref>—was coined by ] in 1908 and was intended to describe the separation of function between ], ], ], and ]. Bleuler described the main symptoms as 4 ''A'''s: flattened ''Affect'', ''Autism'', impaired ''Association'' of ideas and ''Ambivalence''.<ref name="fn_78">{{cite journal |author=Stotz-Ingenlath G |title=Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911 |journal=Medicine, Health Care and Philosophy |volume=3 |issue=2 |pages=153–9 |year=2000 |pmid=11079343|url=http://www.kluweronline.com/art.pdf?issn=1386-7423&volume=3&page=153|format=PDF |accessdate=2008-07-03 |doi=10.1023/A:1009919309015}}</ref> Bleuler realized that the illness was not a ] as some of his patients improved rather than deteriorated and hence proposed the term schizophrenia instead. | |||
| {{Main|History of schizophrenia#Conceptual development}} | |||
| {{Further|Dementia praecox}} | |||
| ].]] | |||
| Accounts of a schizophrenia-like ] are rare in records before the 19th century; the earliest case reports were in 1797 and 1809.<ref>{{cite journal | vauthors = Heinrichs RW | title = Historical origins of schizophrenia: two early madmen and their illness | journal = Journal of the History of the Behavioral Sciences | volume = 39 | issue = 4 | pages = 349–363 | year = 2003 | pmid = 14601041 | doi = 10.1002/jhbs.10152 | doi-access = free }}</ref> The term '']'' ("premature dementia") was used by German psychiatrist Heinrich Schüle in 1886 and then in 1891 by ] in a case report of ]. In 1893 ] used the term in making a distinction, known as the ], between the two psychoses: dementia praecox and ] (now called ]).<ref name=Laursen2014/> When it became evident that the disorder was not a degenerative dementia, it was renamed ''schizophrenia'' by ] in 1908.<ref name=Kuhn2004>{{cite journal | vauthors = Kuhn R, Cahn CH | title = Eugen Bleuler's concepts of psychopathology | journal = History of Psychiatry | volume = 15 | issue = 59 Pt 3 | pages = 361–366 | date = September 2004 | pmid = 15386868 | doi = 10.1177/0957154X04044603 | s2cid = 5317716 }}</ref> | |||
| The word ''schizophrenia'' ("splitting of the mind") is ], derived from the ] ''schizein'' ({{Langx|grc|σχίζειν|lit=to split}}) and ''phrēn'' ({{langx|grc|φρήν|lit=mind}}).<ref>{{cite web |title=Schizophrenia {{!}} Definition of Schizophrenia by Lexico |url=https://www.lexico.com/en/definition/schizophrenia |archive-url=https://web.archive.org/web/20200310144713/https://www.lexico.com/en/definition/schizophrenia |archive-date=10 March 2020 |publisher=Lexico Dictionaries {{!}} English }}</ref> Its use was intended to describe the separation of function between ], ], memory, and perception.<ref name=Kuhn2004/> | |||
| In the early 20th century, the psychiatrist ] categorized the psychotic symptoms of schizophrenia into two groups: hallucinations and delusions. The hallucinations were listed as specific to auditory and the delusions included thought disorders. These were seen as important symptoms, termed ]. The most common first-rank symptom was found to belong to thought disorders.{{page needed|date=August 2022}}<ref>{{page needed|date=August 2022}} {{cite book| vauthors = Schneider K |author-link1=Kurt Schneider |title=Clinical Psychopathology |edition=5th |year=1959 |publisher=Grune & Stratton |location=New York }}</ref>{{page needed|date=August 2022}}<ref>{{page needed|date=August 2022}} {{cite book | vauthors = Moore D |title=Textbook of Clinical Neuropsychiatry |edition=Second |publisher=CRC Press |date=25 April 2008|isbn=9781444109740 }}</ref> In 2013 the first-rank symptoms were excluded from the DSM-5 criteria;<ref>{{cite journal | vauthors = Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W | title = Definition and description of schizophrenia in the DSM-5 | journal = Schizophrenia Research | volume = 150 | issue = 1 | pages = 3–10 | date = October 2013 | pmid = 23800613 | doi = 10.1016/j.schres.2013.05.028 | s2cid = 17314600 }}</ref> while they may not be useful in diagnosing schizophrenia, they can assist in ].<ref>{{cite journal | vauthors = Picardi A | title = The Two Faces of First-Rank Symptoms | journal = Psychopathology | volume = 52 | issue = 4 | pages = 221–231 | date = 2019 | pmid = 31610542 | doi = 10.1159/000503152 | s2cid = 204702486 | doi-access = free }}</ref> | |||
| Subtypes of schizophrenia—classified as paranoid, disorganized, ], undifferentiated, and residual—were difficult to distinguish and are no longer recognized as separate conditions by DSM-5 (2013) or ICD-11.<ref name=Reed2019>{{cite journal | vauthors = Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, Maj M, Stein DJ, Maercker A, Tyrer P, Claudino A, Garralda E, Salvador-Carulla L, Ray R, Saunders JB, Dua T, Poznyak V, Medina-Mora ME, Pike KM, Ayuso-Mateos JL, Kanba S, Keeley JW, Khoury B, Krasnov VN, Kulygina M, Lovell AM, de Jesus Mari J, Maruta T, Matsumoto C, Rebello TJ, Roberts MC, Robles R, Sharan P, Zhao M, Jablensky A, Udomratn P, Rahimi-Movaghar A, Rydelius PA, Bährer-Kohler S, Watts AD, Saxena S | title = Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders | journal = World Psychiatry | volume = 18 | issue = 1 | pages = 3–19 | date = February 2019 | pmid = 30600616 | pmc = 6313247 | doi = 10.1002/wps.20611 }}</ref><ref>{{Cite web |title=Updates to DSM-5 Criteria & Text |url=https://www.psychiatry.org/psychiatrists/practice/dsm/updates-to-dsm-5/updates-to-dsm-5-criteria-text |access-date=21 February 2019 |publisher=www.psychiatry.org}}</ref><ref>{{cite journal | vauthors = Tandon R | title = Schizophrenia and Other Psychotic Disorders in Diagnostic and Statistical Manual of Mental Disorders (DSM)-5: Clinical Implications of Revisions from DSM-IV | journal = Indian Journal of Psychological Medicine | volume = 36 | issue = 3 | pages = 223–225 | date = July 2014 | pmid = 25035542 | pmc = 4100404 | doi = 10.4103/0253-7176.135365 | doi-access = free }}</ref> | |||
| === Breadth of diagnosis === | |||
| Before the 1960s, nonviolent ]s and women were sometimes diagnosed with schizophrenia, categorizing the latter as ill for not performing their duties as wives and mothers.<ref name= Lane2010/> In the mid- to late 1960s, black men were categorized as "hostile and aggressive" and diagnosed as schizophrenic at much higher rates, their ] and ] activism labeled as delusions.<ref name=Lane2010>{{Cite web |vauthors= Lane C |date= 5 May 2010|title=How Schizophrenia Became a Black Disease: An Interview With Jonathan Metzl|url=http://www.psychologytoday.com/blog/side-effects/201005/how-schizophrenia-became-black-disease-interview-jonathan-metzl|access-date=5 April 2021|work=]}}</ref><ref>{{page needed|date=August 2022}} {{Cite book|vauthors=Metz J|title=]|year=2010|isbn=978-0-8070-8592-9| publisher = Beacon Press}}</ref> | |||
| In the early 1970s in the United States, the diagnostic model for schizophrenia was broad and clinically based using ]. Schizophrenia was diagnosed far more in the United States than in Europe, where the ] criteria were followed. The US model was criticised for failing to demarcate clearly those people with a mental illness. In 1980 DSM III was published and showed a shift in focus from the clinically based ] to a reason-based medical model.{{what|date=December 2024}}<ref>{{cite journal |vauthors=Wilson M |date=March 1993 |title=DSM-III and the transformation of American psychiatry: a history |journal=The American Journal of Psychiatry |volume=150 |issue=3 |pages=399–410 |doi=10.1176/ajp.150.3.399 |pmid=8434655}}</ref> DSM IV brought an increased focus on an evidence-based medical model.<ref>{{cite journal |vauthors=Fischer BA |date=December 2012 |title=A review of American psychiatry through its diagnoses: the history and development of the Diagnostic and Statistical Manual of Mental Disorders. |journal=The Journal of Nervous and Mental Disease |volume=200 |issue=12 |pages=1022–1030 |doi=10.1097/NMD.0b013e318275cf19 |pmid=23197117 |s2cid=41939669}}</ref> | |||
| === Historical treatment === | |||
| {{Main|History of schizophrenia#Development of treatments in the 20th century}} | |||
| ], the first antipsychotic developed in the 1950s]] | |||
| In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia.<ref name=Jones2000>{{cite journal |vauthors=Jones K |date=March 2000 |title=Insulin coma therapy in schizophrenia |journal=Journal of the Royal Society of Medicine |volume=93 |issue=3 |pages=147–149 |doi=10.1177/014107680009300313 |pmc=1297956 |pmid=10741319}}</ref> ] involved injecting large doses of ] to induce comas, which in turn produced ] and convulsions.<ref name=Jones2000/><ref>{{cite journal |vauthors=Jobes DA, Chalker SA |date=26 September 2019 |title=One Size Does Not Fit All: A Comprehensive Clinical Approach to Reducing Suicidal Ideation, Attempts, and Deaths. |journal=International Journal of Environmental Research and Public Health |volume=16 |issue=19 |page=3606 |doi=10.3390/ijerph16193606 |pmc=6801408 |pmid=31561488 |doi-access=free}}</ref> The use of electricity to induce seizures was in use as ] (ECT) by 1938.<ref>{{cite journal |vauthors=Ali SA, Mathur N, Malhotra AK, Braga RJ |date=April 2019 |title=Electroconvulsive Therapy and Schizophrenia: A Systematic Review |journal=Molecular Neuropsychiatry |volume=5 |issue=2 |pages=75–83 |doi=10.1159/000497376 |pmc=6528094 |pmid=31192220}}</ref> | |||
| Carried out from the 1930s until the 1970s in the United States and until the 1980s in France, ], including such modalities as the ], is recognized as a ].<ref>{{cite journal |vauthors=Mashour GA, Walker EE, Martuza RL |date=June 2005 |title=Psychosurgery: past, present, and future |journal=Brain Research. Brain Research Reviews |volume=48 |issue=3 |pages=409–419 |doi=10.1016/j.brainresrev.2004.09.002 |pmid=15914249 |s2cid=10303872}}</ref><ref>{{Cite web |vauthors=Mendez J |date=1 February 2013|title=Report of the Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment |url= https://www.ohchr.org/sites/default/files/Documents/HRBodies/HRCouncil/RegularSession/Session22/A.HRC.22.53_English.pdf |access-date= 22 August 2022 |publisher=Office of the High Commissioner for Human Rights}}</ref> In the mid-1950s, ], the first ], was introduced,<ref>{{cite journal |vauthors=Turner T |date=January 2007 |title=Chlorpromazine: unlocking psychosis |journal=BMJ |volume=334 Suppl 1 |issue=suppl |page=s7 |doi=10.1136/bmj.39034.609074.94 |pmid=17204765 |s2cid=33739419}}</ref> followed in the 1970s by clozapine, the first ].<ref>{{cite journal |vauthors=Aringhieri S |date=December 2018 |title=Molecular targets of atypical antipsychotics: From mechanism of action to clinical differences. |journal=Pharmacology & Therapeutics |volume=192 |pages=20–41 |doi=10.1016/j.pharmthera.2018.06.012 |pmid=29953902 |s2cid=49602956}}</ref> | |||
| In the early 1970s, the diagnostic criteria for schizophrenia was the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe.<ref name="Wing1971">{{cite journal |author=Wing JK |title=International comparisons in the study of the functional psychoses |journal=British Medical Bulletin |volume=27 |issue=1 |pages=77–81 |year=1971 |month=January |pmid=4926366}}</ref> This was partly due to looser diagnostic criteria in the US, which used the ] manual, contrasting with Europe and its ]. ] 1972 study, published in the journal '']'' under the title '']'', concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable.<ref>{{cite journal |author=Rosenhan D |year=1973 |title=On being sane in insane places |journal=] |volume=179 |pages=250–8 |pmid=4683124| doi=10.1126/science.179.4070.250 |issue=70}}</ref> These were some of the factors in leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the ] in 1980.{subscription required}<ref name="Wilson1993">{{cite journal |author=Wilson M |title=DSM-III and the transformation of American psychiatry: a history |journal=] |volume=150 |issue=3 |pages=399–410 |year=1993 |month=March |pmid=8434655 |url=http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=8434655 |accessdate=2008-07-03}}{subscription required}</ref> | |||
| === Political abuse === | |||
| The term ''schizophrenia'' is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion arises in part due to the literal interpretation of Bleuler's term ''schizophrenia''. The first known misuse of the term to mean "split personality" was in an article by the poet ] in 1933.<ref name="fn_3">{{cite book |author=Porter, Roy; Berrios, G. E. |title=A history of clinical psychiatry: the origin and history of psychiatric disorders |publisher=Athlone Press |location=London |year=1995 |isbn=0-485-24211-7}}</ref> | |||
| {{Further information|Political abuse of psychiatry}} | |||
| From the 1960s until 1989, psychiatrists in the ] and ] diagnosed thousands of people with ],<ref>{{Cite journal|vauthors=Park YS, Sang M, Jun JY, Kim SJ|date=2014|title=Psychiatry in former socialist countries: implications for north korean psychiatry|journal=Psychiatry Investigation|volume=11|issue=4|pages=363–370|doi=10.4306/pi.2014.11.4.363|issn=1738-3684|pmc=4225199|pmid=25395966}}</ref><ref>{{page needed|date=August 2022}} {{Cite book|vauthors=Gosden R|title=Punishing the patient: how psychiatrists misunderstand and mistreat schizophrenia|date=2001|publisher=Scribe Publications|isbn=0-908011-52-0|location=Melbourne|oclc=47177633}}</ref> without signs of psychosis, based on "the assumption that symptoms would later appear".<ref>{{cite journal | vauthors = Sfera A | title = Can Psychiatry be Misused Again? | journal = Frontiers in Psychiatry | volume = 4 | pages = 101 | date = September 2013 | pmid = 24058348 | pmc = 3766833 | doi = 10.3389/fpsyt.2013.00101 | doi-access = free }}</ref> Now discredited, the diagnosis provided a convenient way to confine political dissidents.<ref name=Merskey1988>{{Cite journal| vauthors = Merskey H |date=15 October 1988|title=IPPNW: Forum for Soviet anti-American propaganda?|journal=CMAJ: Canadian Medical Association Journal|volume=139|issue=8|pages=699–700|issn=0820-3946|pmc=1268271}}</ref> | |||
| ==Society and culture== | ==Society and culture== | ||
| {{See also|List of people with schizophrenia|Religion and schizophrenia|}}In the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002.<ref>{{cite journal | vauthors = Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J | title = The economic burden of schizophrenia in the United States in 2002 | journal = The Journal of Clinical Psychiatry | volume = 66 | issue = 9 | pages = 1122–1129 | date = September 2005 | pmid = 16187769 | doi = 10.4088/jcp.v66n0906 }}</ref>{{efn|A 2007 review stated that the 2002 estimate was still the best available,<ref>{{cite journal | vauthors = McEvoy JP | title = The costs of schizophrenia | journal = The Journal of Clinical Psychiatry | volume = 68 | issue = Suppl 14 | pages = 4–7 | date = 2007 | pmid = 18284271 | doi = }}</ref> and a 2018 review cited the same $62.7 billion.<ref> | |||
| ===Stigma=== | |||
| {{cite journal |vauthors=Zhang W, Amos TB, Gutkin SW, et al |title=A systematic literature review of the clinical and health economic burden of schizophrenia in privately insured patients in the United States |journal=Clinicoecon Outcomes Res |volume=10 |issue= |pages=309–320 |date=2018 |pmid=29922078 |pmc=5997131 |doi=10.2147/CEOR.S156308 |doi-access=free }}</ref>}} In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.<ref name="Lancet2016" /> | |||
| ] has been identified as a major obstacle in the recovery of patients with schizophrenia.<ref>{{Cite book | last1 = Maj | first1 = Mario | last2 = Sartorius | first2 = N. | title = Schizophrenia | date = 15 September 1999 | publisher = Wiley | location = Chichester | isbn = 978-0-471-99906-5 | page = 292 }}</ref> In a large, representative sample from a 1999 study, 12.8% of Americans believed that individuals with schizophrenia were "very likely" to do something violent against others, and 48.1% said that they were "somewhat likely" to. Over 74% said that people with schizophrenia were either "not very able" or "not able at all" to make decisions concerning their treatment, and 70.2% said the same of money management decisions.<ref>{{cite journal |author=Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S |title=The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems |journal=American Journal of Public Health |volume=89 |issue=9 |pages=1339–45 |year=1999 |month=September |pmid=10474550 |pmc=1508769 |doi= 10.2105/AJPH.89.9.1339|url=http://www.ajph.org/cgi/pmidlookup?view=long&pmid=10474550 |accessdate=2008-07-03}}</ref> The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.<ref>{{cite journal |author=Phelan JC, Link BG, Stueve A, Pescosolido BA|year=2000 |month=June |title=Public Conceptions of Mental Illness in 1950 and 1996: What Is Mental Illness and Is It to be Feared? |journal=Journal of Health and Social Behavior |volume=41 |issue=2 |pages=188–207 |doi=10.2307/2676305}}</ref> | |||
| === Stigma === | |||
| In 2002, the ] changed the term for schizophrenia from ''Seishin-Bunretsu-Byo'' 精神分裂病 (mind-split-disease) to ''Tōgō-shitchō-shō'' 統合失調症 (]) to reduce stigma,<ref>{{Cite journal | last1 = Kim | first1 = Y. | last2 = Berrios | first2 = GE. | title = Impact of the term schizophrenia on the culture of ideograph: the Japanese experience. | journal = Schizophr Bull | volume = 27 | issue = 2 | pages = 181–5 | year = 2001 | pmid = 11354585 }}</ref> The new name was inspired by the biopsychosocial model, and it increased the percentage of cases in which patients were informed of the diagnosis from 36.7% to 69.7% over three years.<ref name="Sato">{{cite journal |author=Sato M |year=2004 |title=Renaming schizophrenia: a Japanese perspective |journal=World Psychiatry |volume=5 | issue=1 |pages=53–55 |pmid=16757998 |pmc=1472254}}</ref> | |||
| ], an American mathematician and joint recipient of the 1994 ], had schizophrenia. His life was the subject of the 1998 book, '']'', by ].]] | |||
| In 2002, the term for schizophrenia in Japan was changed from {{nihongo||精神分裂病|seishin-bunretsu-byō|lit. 'mind-split disease'}} to {{nihongo||統合失調症|tōgō-shitchō-shō|lit. 'integration–dysregulation syndrome'}} to reduce ].<ref>{{cite journal | vauthors = Yamaguchi S, Mizuno M, Ojio Y, Sawada U, Matsunaga A, Ando S, Koike S | title = Associations between renaming schizophrenia and stigma-related outcomes: A systematic review | journal = Psychiatry and Clinical Neurosciences | volume = 71 | issue = 6 | pages = 347–362 | date = June 2017 | pmid = 28177184 | doi = 10.1111/pcn.12510 | doi-access = free }}</ref> The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model.<ref>{{cite journal | vauthors = Sato M | title = Renaming schizophrenia: a Japanese perspective | journal = World Psychiatry | volume = 5 | issue = 1 | pages = 53–55 | date = February 2006 | pmid = 16757998 | pmc = 1472254 }}</ref> A similar change was made in South Korea in 2012 to attunement disorder.<ref>{{cite journal | vauthors = Park SC, Park YC | title = Korea in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition | journal = Journal of Korean Medical Science | volume = 35 | issue = 2 | pages = e6 | date = January 2020 | pmid = 31920014 | pmc = 6955430 | doi = 10.3346/jkms.2020.35.e6 | edition = Fifth }}</ref> | |||
| ===Iconic cultural depictions=== | |||
| === Cultural depictions === | |||
| The book and film '']'' chronicled the life of ], a ]-winning mathematician who was diagnosed with schizophrenia. The ] film ''Devrai'' (featuring ]) is a presentation of a patient with schizophrenia. The film, set in Western ], shows the behavior, mentality, and struggle of the patient as well as his loved-ones. Other factual books have been written by relatives on family members; Australian journalist ] told the story of her son's battle with schizophrenia in ''Tell me I'm Here'',<ref>{{cite book |author=] |title=Tell Me I'm Here |publisher=Penguin |year=1991 |isbn=0-14-027257-7}}</ref> later made into a movie. | |||
| Media coverage, especially movies, reinforce the public perception of an association between schizophrenia and violence.<ref>{{cite journal | vauthors = Fazel S, Gulati G, Linsell L, Geddes JR, Grann M | title = Schizophrenia and violence: systematic review and meta-analysis | journal = PLOS Medicine | volume = 6 | issue = 8 | pages = e1000120 | date = August 2009 | pmid = 19668362 | pmc = 2718581 | doi = 10.1371/journal.pmed.1000120 | doi-access = free }}</ref> A majority of movies have historically depicted characters with schizophrenia as criminal, dangerous, violent, unpredictable and homicidal, and depicted delusions and hallucinations as the main symptoms of schizophrenic characters, ignoring other common symptoms,<ref name= Owen2012>{{cite journal |vauthors=Owen PR |title=Portrayals of schizophrenia by entertainment media: a content analysis of contemporary movies |journal=Psychiatr Serv |volume=63 |issue=7 |pages=655–9 |date=July 2012 |pmid=22555313 |doi=10.1176/appi.ps.201100371}}</ref> furthering stereotypes of schizophrenia including the idea of a split personality.<ref>{{cite journal |vauthors=Katschnig H |title=Psychiatry's contribution to the public stereotype of schizophrenia: Historical considerations |journal=J Eval Clin Pract |volume=24 |issue=5 |pages=1093–1100 |date=October 2018 |pmid=30112785 |pmc=6174929 |doi=10.1111/jep.13011 }}</ref> | |||
| The book '']'' chronicled the life of ] who had been diagnosed with schizophrenia and won the ]. The book was made into a ]; an earlier documentary film was '']''. | |||
| In the UK, guidelines for reporting conditions and award campaigns have shown a reduction in negative reporting since 2013.<ref>{{cite journal |vauthors=Chen M, Lawrie S |title=Newspaper depictions of mental and physical health. |journal=BJPsych Bulletin |volume=41 |issue=6 |pages=308–313 |date=December 2017 |pmid=29234506 |doi=10.1192/pb.bp.116.054775|pmc=5709678 }}</ref> | |||
| ==See also== | |||
| *] | |||
| *] | |||
| *] | |||
| In 1964 a ] of three males diagnosed with schizophrenia who each had the delusional belief that they were ] was published as '']''; a film with the title '']'' was released in 2020.<ref>{{cite journal | vauthors = Dyga K, Stupak R | title = Ways of understanding of religious delusions associated with a change of identity on the example of identification with Jesus Christ. | journal=Psychiatria Polska | date = 28 February 2018 | volume = 52 | issue = 1 | pages = 69–80 | doi=10.12740/PP/64378 | pmid=29704415| doi-access = free }}</ref><ref>{{cite journal | vauthors = Dein S, Littlewood R | title = Religion and psychosis: a common evolutionary trajectory? | journal = Transcultural Psychiatry | date = July 2011 | volume = 48 | issue = 3 | pages =318–335 | doi = 10.1177/1363461511402723 | pmid = 21742955| s2cid = 12991391 }}</ref> | |||
| ==References== | |||
| {{Reflist|colwidth=30em}} | |||
| == |
==Research directions== | ||
| {{See also|Animal models of schizophrenia}} | |||
| <!-- Please only include material which addresses schizophrenia in general, rather than specific aspects, or related topics --> | |||
| A 2015 Cochrane review found unclear evidence of benefit from brain stimulation techniques to treat the positive symptoms of schizophrenia, in particular auditory verbal hallucinations (AVHs).<ref>{{cite journal |vauthors =Dougall N, Maayan N, Soares-Weiser K, McDermott LM, McIntosh A |title=Transcranial magnetic stimulation (TMS) for schizophrenia. |journal=The Cochrane Database of Systematic Reviews |volume=2015 |date=20 August 2015 |issue=8 |pages=CD006081 |doi=10.1002/14651858.CD006081.pub2 |pmid=26289586|pmc=9395125 |hdl=1893/22520 |hdl-access=free }}</ref> Most studies focus on ] (tDCM), and ] (rTMS).<ref name=Nathou2019>{{cite journal |vauthors=Nathou C, Etard O, Dollfus S |date=2019 |title=Auditory verbal hallucinations in schizophrenia: current perspectives in brain stimulation treatments. |journal=Neuropsychiatric Disease and Treatment|volume=15 |pages=2105–2117 |pmid=31413576 |pmc=6662171 |doi=10.2147/NDT.S168801 |doi-access=free }}</ref> Techniques based on focused ultrasound for ] could provide insight for the treatment of AVHs.<ref name=Nathou2019/> | |||
| <div class="references-small"> | |||
| *{{cite book |author=] |title=Madness explained: psychosis and human nature |publisher=Allen Lane |location=London |year=2003 |isbn=0-7139-9249-2}} | |||
| *{{cite book |last=Dalby |first=J. Thomas |title=Mental disease in history: a selection of translated readings |publisher=Peter Lang |location=Bern |year=1996 |isbn=0-8204-3056-0 }} | |||
| *{{cite journal |last=Fallon |first=James H. |authorlink=James Fallon |year=2003 |title=The Neuroanatomy of Schizophrenia: Circuitry and Neurotransmitter Systems |journal=Clinical Neuroscience Research |volume=3 |pages=77–107 |doi=10.1016/S1566-2772(03)00022-7 |accessdate=2008-07-07}} | |||
| *{{cite book |last=Fleck |first=Stephen |authorlink=Theodore Lidz |coauthors=] and Alice Cornelison |title=Schizophrenia and the family |publisher=International Universities Press |location=New York |year=1985 |isbn=0-8236-6001-X}} | |||
| *{{cite journal |author=Keen TM |title=Schizophrenia: orthodoxy and heresies. A review of alternative possibilities |journal=Journal of Psychiatric and Mental Health Nursing |volume=6 |issue=6 |pages=415–24 |year=1999 |month=December |pmid=10818864 |doi=10.1046/j.1365-2850.1999.00237.x}} | |||
| *{{cite book |last=Laing |first=Ronald D. |authorlink=Ronald David Laing |title=The divided self: an existential study in sanity and madness |publisher=Penguin Books |location=New York |year=1990|isbn=0-14-013537-5 }} | |||
| *{{cite book |author=Noll, Richard |title=The Encyclopedia of Schizophrenia And Other Psychotic Disorders (Facts on File Library of Health and Living) |publisher=Facts on File |location=New York |year=2006 |isbn=0-8160-6405-9}} | |||
| *{{cite book |last=Roazen |first=Paul |authorlink=Paul Roazen |coauthors=] |title=Sexuality, war, and schizophrenia: collected psychoanalytic papers |publisher=Transaction Publishers |location=New Brunswick, N.J., U.S.A |year=1991 |isbn=0-88738-365-3}} (On the Origin of the 'Influencing Machine' in Schizophrenia.) | |||
| *{{cite journal |author=Shaner A, Miller G, Mintz J |title=Schizophrenia as one extreme of a sexually selected fitness indicator |journal=Schizophr. Res. |volume=70 |issue=1 |pages=101–9 |year=2004 |month=September |pmid=15246469 |doi=10.1016/j.schres.2003.09.014 |url=http://www.unm.edu/~gfmiller/new_papers/shaner%20miller%202004%20schizo.pdf|format=PDF|accessdate=2008-07-07}} | |||
| *{{cite book |last=Szasz |first=Thomas Stephen |authorlink=Thomas Szasz |title=Schizophrenia: the sacred symbol of psychiatry |publisher=Basic Books |location=New York |year=1976 |isbn=0-465-07222-4}} | |||
| *{{cite journal |title=Schizophrenia: Etiology and Course |journal=Annual Review of Psychology |author=Walker Elaine, et al |volume=55 |pages=401-30 |year=2004 |url=http://arjournals.annualreviews.org/doi/abs/10.1146/annurev.psych.55.090902.141950 |doi=10.1146/annurev.psych.55.090902.141950}} | |||
| </div> | |||
| The study of potential ] that would help in diagnosis and treatment of schizophrenia is an active area of research as of 2020. Possible biomarkers include markers of inflammation,<ref name=Upthegrove2020/> ],<ref>{{cite journal |vauthors=Kraguljac NV, McDonald WM, Widge AS, Rodriguez CI, Tohen M, Nemeroff CB |title=Neuroimaging Biomarkers in Schizophrenia |journal=Am J Psychiatry |pages=509–521 |date=January 2021 |volume=178 |issue=6 |pmid=33397140 |doi=10.1176/appi.ajp.2020.20030340|pmc=8222104 }}</ref> ] (BDNF),<ref>{{cite journal |vauthors=Khavari B, Cairns MJ |title=Epigenomic Dysregulation in Schizophrenia: In Search of Disease Etiology and Biomarkers |journal=Cells |volume=9 |issue=8 |date=August 2020 |page=1837 |pmid=32764320 |doi=10.3390/cells9081837|pmc=7463953 |doi-access=free }}</ref> and speech analysis. Some markers such as ] are useful in detecting levels of inflammation implicated in some psychiatric disorders but they are not disorder-specific. Other inflammatory cytokines are found to be elevated in first episode psychosis and acute relapse that are normalized after treatment with antipsychotics, and these may be considered as state markers.<ref>{{cite journal |vauthors=Goldsmith DR, Crooks CL, Walker EF, Cotes RO |title=An Update on Promising Biomarkers in Schizophrenia |journal=Focus (American Psychiatric Publishing)|volume=16 |issue=2 |pages=153–163 |date=April 2018 |doi=10.1176/appi.focus.20170046 |pmid=31975910|pmc=6526854 }}</ref> Deficits in ]s in schizophrenia may serve as a marker of an impaired thalamocortical circuit, and a mechanism for memory impairment.<ref name=Pocivavsek2018>{{cite journal |vauthors=Pocivavsek A, Rowland LM |title=Basic Neuroscience Illuminates Causal Relationship Between Sleep and Memory: Translating to Schizophrenia |journal=Schizophrenia Bulletin |volume=44 |issue=1 |pages=7–14 |date=13 January 2018 |pmid=29136236|doi=10.1093/schbul/sbx151|pmc=5768044 |doi-access=free }}</ref> ]s are highly influential in early neuronal development, and their disruption is implicated in several ] disorders; ]s (cimiRNAs) are found in ]s such as blood and cerebrospinal fluid, and changes in their levels are seen to relate to changes in microRNA levels in specific regions of brain tissue. These studies suggest that cimiRNAs have the potential to be early and accurate biomarkers in a number of disorders including schizophrenia.<ref>{{cite journal |vauthors=Kumar S, Reddy PH |title=Are circulating microRNAs peripheral biomarkers for Alzheimer's disease? |journal=Biochim Biophys Acta |volume=1862 |issue=9 |pages=1617–1627 |date=September 2016 |pmid=27264337 |pmc=5343750 |doi=10.1016/j.bbadis.2016.06.001 |url=}}</ref><ref>{{cite journal |vauthors=van den Berg MM, Krauskopf J, Ramaekers JG, et al. |title=Circulating microRNAs as potential biomarkers for psychiatric and neurodegenerative disorders |journal=Prog Neurobiol |volume=185 |pages=101732 |date=February 2020 |pmid=31816349 |doi=10.1016/j.pneurobio.2019.101732 |s2cid=208790466|doi-access=free }}</ref> | |||
| ==External links== | |||
| *{{dmoz|Health/Mental_Health/Disorders/Schizophrenia/}} | |||
| * | |||
| * | |||
| * Film made in 1940 showing some of the symptoms of Schizophrenia. | |||
| {{featured article}} | |||
| {{Mental and behavioural disorders|selected = schizophrenia}} | |||
| ] aims to identify biomarkers within these brain networks,<ref>{{Cite journal |last1=Palaniyappan |first1=Lena |last2=Liddle |first2=Peter F. |date=2013-04-24 |title=Diagnostic Discontinuity in Psychosis: A Combined Study of Cortical Gyrification and Functional Connectivity |url=https://academic.oup.com/schizophreniabulletin/article-abstract/40/3/675/1903745?redirectedFrom=fulltext |journal=Schizophrenia Bulletin |volume=40 |issue=3 |pages=675–684 |doi=10.1093/schbul/sbt050 |issn=1745-1701 |pmc=3984507 |pmid=23615812}}</ref> potentially aiding in earlier diagnosis and better tracking of treatment responses in schizophrenia. | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| == Explanatory notes == | |||
| {{Link FA|ro}} | |||
| {{ |
{{Notelist}} | ||
| == References == | |||
| ] | |||
| {{Reflist}} | |||
| ] | |||
| ] | |||
| == External links == | |||
| ] | |||
| {{Medical condition classification and resources | |||
| ] | |||
| | DiseasesDB = 11890 | |||
| ] | |||
| | ICD11 = {{ICD11|6A20}} | |||
| ] | |||
| | ICD10 = {{ICD10|F|20||f|20}} | |||
| ] | |||
| | ICD9 = {{ICD9|295}} | |||
| ] | |||
| | ICDO = | |||
| ] | |||
| | OMIM = 181500 | |||
| ] | |||
| | MedlinePlus = 000928 | |||
| ] | |||
| | eMedicineSubj = med | |||
| ] | |||
| | eMedicineTopic = 2072 | |||
| ] | |||
| | eMedicine_mult = {{eMedicine2|emerg|520}} | |||
| ] | |||
| | MeshName = Schizophrenia | |||
| ] | |||
| | MeshNumber = F03.700.750 | |||
| ] | |||
| | Scholia = Q41112 | |||
| ] | |||
| }} | |||
| ] | |||
| {{Schizophrenia}} | |||
| ] | |||
| {{Mental and behavioural disorders|selected = schizophrenia}} | |||
| ] | |||
| {{Subject bar | |||
| ] | |||
| | b = | |||
| ] | |||
| | commons = yes | |||
| ] | |||
| | d = yes | |||
| ] | |||
| | n = yes | |||
| ] | |||
| | q = yes | |||
| ] | |||
| | s = | |||
| ] | |||
| | species = | |||
| ] | |||
| | v = | |||
| ] | |||
| | voy = | |||
| ] | |||
| | wikt = yes | |||
| ] | |||
| |Psychiatry|Psychology}} | |||
| ] | |||
| {{Authority control}} | |||
| ] | |||
| ] | |||
| {{Featured article}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 21:08, 22 December 2024
Mental disorder with psychotic symptoms For other uses, see Schizophrenia (disambiguation).Medical condition
Schizophrenia is a mental disorder characterized variously by hallucinations (typically, hearing voices), delusions, disorganized thinking and behavior, and flat or inappropriate affect. Symptoms develop gradually and typically begin during young adulthood and are never resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months (according to the DSM-5) or one month (according to the ICD-11). Many people with schizophrenia have other mental disorders, especially mood disorders, anxiety disorders, and obsessive–compulsive disorder.
About 0.3% to 0.7% of people are diagnosed with schizophrenia during their lifetime. In 2017, there were an estimated 1.1 million new cases and in 2022 a total of 24 million cases globally. Males are more often affected and on average have an earlier onset than females. The causes of schizophrenia may include genetic and environmental factors. Genetic factors include a variety of common and rare genetic variants. Possible environmental factors include being raised in a city, childhood adversity, cannabis use during adolescence, infections, the age of a person's mother or father, and poor nutrition during pregnancy.
About half of those diagnosed with schizophrenia will have a significant improvement over the long term with no further relapses, and a small proportion of these will recover completely. The other half will have a lifelong impairment. In severe cases, people may be admitted to hospitals. Social problems such as long-term unemployment, poverty, homelessness, exploitation, and victimization are commonly correlated with schizophrenia. Compared to the general population, people with schizophrenia have a higher suicide rate (about 5% overall) and more physical health problems, leading to an average decrease in life expectancy by 20 to 28 years. In 2015, an estimated 17,000 deaths were linked to schizophrenia.
The mainstay of treatment is antipsychotic medication, including olanzapine and risperidone, along with counseling, job training, and social rehabilitation. Up to a third of people do not respond to initial antipsychotics, in which case clozapine is offered. In a network comparative meta-analysis of 15 antipsychotic drugs, clozapine was significantly more effective than all other drugs, although clozapine's heavily multimodal action may cause more significant side effects. In situations where doctors judge that there is a risk of harm to self or others, they may impose short involuntary hospitalization. Long-term hospitalization is used on a small number of people with severe schizophrenia. In some countries where supportive services are limited or unavailable, long-term hospital stays are more common.
Signs and symptoms

Schizophrenia is a mental disorder characterized by significant alterations in perception, thoughts, mood, and behavior. Symptoms are described in terms of positive, negative, and cognitive symptoms. The positive symptoms of schizophrenia are the same for any psychosis and are sometimes referred to as psychotic symptoms. These may be present in any of the different psychoses and are often transient, making early diagnosis of schizophrenia problematic. Psychosis noted for the first time in a person who is later diagnosed with schizophrenia is referred to as a first-episode psychosis (FEP).
Positive symptoms
Positive symptoms are those symptoms that are not normally experienced, but are present in people during a psychotic episode in schizophrenia, including delusions, hallucinations, and disorganized thoughts, speech and behavior or inappropriate affect, typically regarded as manifestations of psychosis. Hallucinations occur at some point in the lifetimes of 80% of those with schizophrenia and most commonly involve the sense of hearing (most often hearing voices), but can sometimes involve any of the other senses such as taste, sight, smell, and touch. The frequency of hallucinations involving multiple senses is double the rate of those involving only one sense. They are also typically related to the content of the delusional theme. Delusions are bizarre or persecutory in nature. Distortions of self-experience such as feeling that others can hear one's thoughts or that thoughts are being inserted into one's mind, sometimes termed passivity phenomena, are also common. Positive symptoms generally respond well to medication and become reduced over the course of the illness, perhaps linked to the age-related decline in dopamine activity.
Negative symptoms
Negative symptoms are deficits of normal emotional responses, or of other thought processes. The five recognized domains of negative symptoms are: blunted affect – showing flat expressions (monotone) or little emotion; alogia – a poverty of speech; anhedonia – an inability to feel pleasure; asociality – the lack of desire to form relationships, and avolition – a lack of motivation and apathy. Avolition and anhedonia are seen as motivational deficits resulting from impaired reward processing. Reward is the main driver of motivation and this is mostly mediated by dopamine. It has been suggested that negative symptoms are multidimensional and they have been categorised into two subdomains of apathy or lack of motivation, and diminished expression. Apathy includes avolition, anhedonia, and social withdrawal; diminished expression includes blunt affect and alogia. Sometimes diminished expression is treated as both verbal and non-verbal.
Apathy accounts for around 50% of the most often found negative symptoms and affects functional outcome and subsequent quality of life. Apathy is related to disrupted cognitive processing affecting memory and planning including goal-directed behaviour. The two subdomains have suggested a need for separate treatment approaches. A lack of distress is another noted negative symptom. A distinction is often made between those negative symptoms that are inherent to schizophrenia, termed primary; and those that result from positive symptoms, from the side effects of antipsychotics, substance use disorder, and social deprivation – termed secondary negative symptoms. Negative symptoms are less responsive to medication and the most difficult to treat. However, if properly assessed, secondary negative symptoms are amenable to treatment. There is some evidence that the negative symptoms of schizophrenia are amenable to psychostimulant medication, although such drugs have varying degrees of risk for causing positive psychotic symptoms.
Scales for specifically assessing the presence of negative symptoms, and for measuring their severity, and their changes have been introduced since the earlier scales such as the PANNS that deals with all types of symptoms. These scales are the Clinical Assessment Interview for Negative Symptoms (CAINS), and the Brief Negative Symptom Scale (BNSS) also known as second-generation scales. In 2020, ten years after its introduction, a cross-cultural study of the use of BNSS found valid and reliable psychometric evidence for its five-domain structure cross-culturally. The BNSS can assess both the presence and severity of negative symptoms of the five recognized domains and an additional item of reduced normal distress. It has been used to measure changes in negative symptoms in trials of psychosocial and pharmacological interventions.
Cognitive symptoms
See also: Visual processing abnormalities in schizophrenia
An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early-onset and late-onset illness. These are often evident long before the onset of illness in the prodromal stage, and may be present in childhood or early adolescence. They are a core feature but not considered to be core symptoms, as are positive and negative symptoms. However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms. Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.
The deficits in cognition are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed to equate to a possible reduction in IQ from the norm of 100 to 70–85. Cognitive deficits may be of neurocognition (nonsocial) or of social cognition. Neurocognition is the ability to receive and remember information, and includes verbal fluency, memory, reasoning, problem solving, speed of processing, and auditory and visual perception. Verbal memory and attention are seen to be the most affected. Verbal memory impairment is associated with a decreased level of semantic processing (relating meaning to words). Another memory impairment is that of episodic memory. An impairment in visual perception that is consistently found in schizophrenia is that of visual backward masking. Visual processing impairments include an inability to perceive complex visual illusions. Social cognition is concerned with the mental operations needed to interpret, and understand the self and others in the social world. This is also an associated impairment, and facial emotion perception is often found to be difficult. Facial perception is critical for ordinary social interaction. Cognitive impairments do not usually respond to antipsychotics, and there are a number of interventions that are used to try to improve them; cognitive remediation therapy is of particular help.
Neurological soft signs of clumsiness and loss of fine motor movement are often found in schizophrenia, which may resolve with effective treatment of FEP.
Onset
Further information: Basic symptoms of schizophrenia See also: Childhood schizophrenia and Adolescence § Changes in the brainOnset typically occurs between the late teens and early 30s, with the peak incidence occurring in males in the early to mid-twenties, and in females in the late twenties. Onset before the age of 17 is known as early-onset, and before the age of 13, as can sometimes occur, is known as childhood schizophrenia or very early-onset. Onset can occur between the ages of 40 and 60, known as late-onset schizophrenia. Onset over the age of 60, which may be difficult to differentiate as schizophrenia, is known as very-late-onset schizophrenia-like psychosis. Late onset has shown that a higher rate of females are affected; they have less severe symptoms and need lower doses of antipsychotics. The tendency for earlier onset in males is later seen to be balanced by a post-menopausal increase in the development in females. Estrogen produced pre-menopause has a dampening effect on dopamine receptors but its protection can be overridden by a genetic overload. There has been a dramatic increase in the numbers of older adults with schizophrenia.
Onset may happen suddenly or may occur after the slow and gradual development of a number of signs and symptoms, a period known as the prodromal stage. Up to 75% of those with schizophrenia go through a prodromal stage. The negative and cognitive symptoms in the prodrome stage can precede FEP (first episode psychosis) by many months and up to five years. The period from FEP and treatment is known as the duration of untreated psychosis (DUP) which is seen to be a factor in functional outcome. The prodromal stage is the high-risk stage for the development of psychosis. Since the progression to first episode psychosis is not inevitable, an alternative term is often preferred of at risk mental state. Cognitive dysfunction at an early age impacts a young person's usual cognitive development. Recognition and early intervention at the prodromal stage would minimize the associated disruption to educational and social development and has been the focus of many studies.
Risk factors
Main article: Risk factors of schizophreniaSchizophrenia is described as a neurodevelopmental disorder with no precise boundary, or single cause, and is thought to develop from gene–environment interactions with involved vulnerability factors. The interactions of these risk factors are complex, as numerous and diverse insults from conception to adulthood can be involved. A genetic predisposition on its own, without interacting environmental factors, will not give rise to the development of schizophrenia. The genetic component means that prenatal brain development is disturbed, and environmental influence affects the postnatal development of the brain. Evidence suggests that genetically susceptible children are more likely to be vulnerable to the effects of environmental risk factors.
Genetic
Estimates of the heritability of schizophrenia are between 70% and 80%, which implies that 70% to 80% of the individual differences in risk of schizophrenia are associated with genetics. These estimates vary because of the difficulty in separating genetic and environmental influences, and their accuracy has been queried. The greatest risk factor for developing schizophrenia is having a first-degree relative with the disease (risk is 6.5%); more than 40% of identical twins of those with schizophrenia are also affected. If one parent is affected the risk is about 13% and if both are affected the risk is nearly 50%. However, the DSM-5 indicates that most people with schizophrenia have no family history of psychosis. Results of candidate gene studies of schizophrenia have generally failed to find consistent associations, and the genetic loci identified by genome-wide association studies explain only a small fraction of the variation in the disease.
Many genes are known to be involved in schizophrenia, each with small effects and unknown transmission and expression. The summation of these effect sizes into a polygenic risk score can explain at least 7% of the variability in liability for schizophrenia. Around 5% of cases of schizophrenia are understood to be at least partially attributable to rare copy number variations (CNVs); these structural variations are associated with known genomic disorders involving deletions at 22q11.2 (DiGeorge syndrome) and 17q12 (17q12 microdeletion syndrome), duplications at 16p11.2 (most frequently found) and deletions at 15q11.2 (Burnside–Butler syndrome). Some of these CNVs increase the risk of developing schizophrenia by as much as 20-fold, and are frequently comorbid with autism and intellectual disabilities.
The genes CRHR1 and CRHBP are associated with the severity of suicidal behavior. These genes code for stress response proteins needed in the control of the HPA axis, and their interaction can affect this axis. Response to stress can cause lasting changes in the function of the HPA axis possibly disrupting the negative feedback mechanism, homeostasis, and the regulation of emotion leading to altered behaviors.
The question of how schizophrenia could be primarily genetically influenced, given that people with schizophrenia have lower fertility rates, is a paradox. It is expected that genetic variants that increase the risk of schizophrenia would be selected against, due to their negative effects on reproductive fitness. A number of potential explanations have been proposed, including that alleles associated with schizophrenia risk confers a fitness advantage in unaffected individuals. While some evidence has not supported this idea, others propose that a large number of alleles each contributing a small amount can persist.
A meta-analysis found that oxidative DNA damage was significantly increased in schizophrenia.
Environmental
Further information: Prenatal nutrition, Prenatal stress, and Neuroplastic effects of pollutionEnvironmental factors, each associated with a slight risk of developing schizophrenia in later life include oxygen deprivation, infection, prenatal maternal stress, and malnutrition in the mother during prenatal development. A risk is associated with maternal obesity, in increasing oxidative stress, and dysregulating the dopamine and serotonin pathways. Both maternal stress and infection have been demonstrated to alter fetal neurodevelopment through an increase of pro-inflammatory cytokines. There is a slighter risk associated with being born in the winter or spring possibly due to vitamin D deficiency or a prenatal viral infection. Other infections during pregnancy or around the time of birth that have been linked to an increased risk include infections by Toxoplasma gondii and Chlamydia. The increased risk is about five to eight percent. Viral infections of the brain during childhood are also linked to a risk of schizophrenia during adulthood. Cat exposure is also associated with an increased risk of broadly defined schizophrenia-related disorders, with an odds ratio of 2.4.
Adverse childhood experiences (ACEs), severe forms of which are classed as childhood trauma, range from being bullied or abused, to the death of a parent. Many adverse childhood experiences can cause toxic stress and increase the risk of psychosis. Chronic trauma, including ACEs, can promote lasting inflammatory dysregulation throughout the nervous system. It is suggested that early stress may contribute to the development of schizophrenia through these alterations in the immune system. Schizophrenia was the last diagnosis to benefit from the link made between ACEs and adult mental health outcomes.
Living in an urban environment during childhood or as an adult has consistently been found to increase the risk of schizophrenia by a factor of two, even after taking into account drug use, ethnic group, and size of social group. A possible link between the urban environment and pollution has been suggested to be the cause of the elevated risk of schizophrenia. Other risk factors include social isolation, immigration related to social adversity and racial discrimination, family dysfunction, unemployment, and poor housing conditions. Having a father older than 40 years, or parents younger than 20 years are also associated with schizophrenia.
Substance use
Further information: Risk factors of schizophrenia § Substance use, and Substance-induced psychosisAbout half of those with schizophrenia use recreational drugs including alcohol, tobacco, and cannabis excessively. Use of stimulants such as amphetamine and cocaine can lead to a temporary stimulant psychosis, which presents very similarly to schizophrenia. Rarely, alcohol use can also result in a similar alcohol-related psychosis. Drugs may also be used as coping mechanisms by people who have schizophrenia, to deal with depression, anxiety, boredom, and loneliness. The use of cannabis and tobacco are not associated with the development of cognitive deficits, and sometimes a reverse relationship is found where their use improves these symptoms. However, substance use disorders are associated with an increased risk of suicide, and a poor response to treatment.
Cannabis use may be a contributory factor in the development of schizophrenia, potentially increasing the risk of the disease in those who are already at risk. The increased risk may require the presence of certain genes within an individual. Its use is associated with doubling the rate.
Causes
Main article: Causes of schizophreniaSee also: Aberrant salienceThe causes of schizophrenia are still unknown. Several models have been put forward to explain the link between altered brain function and schizophrenia. The prevailing model of schizophrenia is that of a neurodevelopmental disorder, and the underlying changes that occur before symptoms become evident are seen as arising from the interaction between genes and the environment. Extensive studies support this model. Maternal infections, malnutrition and complications during pregnancy and childbirth are known risk factors for the development of schizophrenia, which usually emerges between the ages of 18 and 25, a period that overlaps with certain stages of neurodevelopment. Gene-environment interactions lead to deficits in the neural circuitry that affect sensory and cognitive functions.
The common dopamine and glutamate models proposed are not mutually exclusive; each is seen to have a role in the neurobiology of schizophrenia. The most common model put forward was the dopamine hypothesis of schizophrenia, which attributes psychosis to the mind's faulty interpretation of the misfiring of dopaminergic neurons. This has been directly related to the symptoms of delusions and hallucinations. Abnormal dopamine signaling has been implicated in schizophrenia based on the usefulness of medications that affect the dopamine receptor and the observation that dopamine levels are increased during acute psychosis. A decrease in D1 receptors in the dorsolateral prefrontal cortex may also be responsible for deficits in working memory.
The glutamate hypothesis of schizophrenia links alterations between glutamatergic neurotransmission and the neural oscillations that affect connections between the thalamus and the cortex. Studies have shown that a reduced expression of a glutamate receptor – NMDA receptor, and glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with schizophrenia. Post-mortem studies consistently find that a subset of these neurons fail to express GAD67 (GAD1), in addition to abnormalities in brain morphometry. The subsets of interneurons that are abnormal in schizophrenia are responsible for the synchronizing of neural ensembles needed during working memory tasks. These give the neural oscillations produced as gamma waves that have a frequency of between 30 and 80 hertz. Both working memory tasks and gamma waves are impaired in schizophrenia, which may reflect abnormal interneuron functionality. An important process that may be disrupted in neurodevelopment is astrogenesis – the formation of astrocytes. Astrocytes are crucial in contributing to the formation and maintenance of neural circuits and it is believed that disruption in this role can result in a number of neurodevelopmental disorders including schizophrenia. Evidence suggests that reduced numbers of astrocytes in deeper cortical layers are assocociated with a diminished expression of EAAT2, a glutamate transporter in astrocytes; supporting the glutamate hypothesis.
Deficits in executive functions, such as planning, inhibition, and working memory, are pervasive in schizophrenia. Although these functions are separable, their dysfunction in schizophrenia may reflect an underlying deficit in the ability to represent goal related information in working memory, and to use this to direct cognition and behavior. These impairments have been linked to a number of neuroimaging and neuropathological abnormalities. For example, functional neuroimaging studies report evidence of reduced neural processing efficiency, whereby the dorsolateral prefrontal cortex is activated to a greater degree to achieve a certain level of performance relative to controls on working memory tasks. These abnormalities may be linked to the consistent post-mortem finding of reduced neuropil, evidenced by increased pyramidal cell density and reduced dendritic spine density. These cellular and functional abnormalities may also be reflected in structural neuroimaging studies that find reduced grey matter volume in association with deficits in working memory tasks.
Positive symptoms have been linked to cortical thinning in the superior temporal gyrus. The severity of negative symptoms has been linked to reduced thickness in the left medial orbitofrontal cortex. Anhedonia, traditionally defined as a reduced capacity to experience pleasure, is frequently reported in schizophrenia. However, a large body of evidence suggests that hedonic responses are intact in schizophrenia, and that what is reported to be anhedonia is a reflection of dysfunction in other processes related to reward. Overall, a failure of reward prediction is thought to lead to impairment in the generation of cognition and behavior required to obtain rewards, despite normal hedonic responses.
Another theory links abnormal brain lateralization to the development of being left-handed which is significantly more common in those with schizophrenia. This abnormal development of hemispheric asymmetry is noted in schizophrenia. Studies have concluded that the link is a true and verifiable effect that may reflect a genetic link between lateralization and schizophrenia.
Bayesian models of brain functioning have been used to link abnormalities in cellular functioning to symptoms. Both hallucinations and delusions have been suggested to reflect improper encoding of prior expectations, thereby causing expectation to excessively influence sensory perception and the formation of beliefs. In approved models of circuits that mediate predictive coding, reduced NMDA receptor activation, could in theory result in the positive symptoms of delusions and hallucinations.
Diagnosis
Main article: Diagnosis of schizophreniaCriteria
Schizophrenia is diagnosed based on criteria in either the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association or the International Statistical Classification of Diseases and Related Health Problems (ICD) published by the World Health Organization (WHO). These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by a psychiatric assessment. The mental status examination is an important part of the assessment. An established tool for assessing the severity of positive and negative symptoms is the Positive and Negative Syndrome Scale (PANSS). This has been seen to have shortcomings relating to negative symptoms, and other scales – the Clinical Assessment Interview for Negative Symptoms (CAINS), and the Brief Negative Symptoms Scale (BNSS) have been introduced. The DSM-5, published in 2013, gives a Scale to Assess the Severity of Symptom Dimensions outlining eight dimensions of symptoms.
DSM-5 states that to be diagnosed with schizophrenia, two diagnostic criteria have to be met over the period of one month, with a significant impact on social or occupational functioning for at least six months. One of the symptoms needs to be either delusions, hallucinations, or disorganized speech. A second symptom could be one of the negative symptoms, or severely disorganized or catatonic behaviour. A different diagnosis of schizophreniform disorder can be made before the six months needed for the diagnosis of schizophrenia.
In Australia, the guideline for diagnosis is for six months or more with symptoms severe enough to affect ordinary functioning. In the UK diagnosis is based on having the symptoms for most of the time for one month, with symptoms that significantly affect the ability to work, study, or carry on ordinary daily living, and with other similar conditions ruled out.
The ICD criteria are typically used in European countries; the DSM criteria are used predominantly in the United States and Canada, and are prevailing in research studies. In practice, agreement between the two systems is high. The current proposal for the ICD-11 criteria for schizophrenia recommends adding self-disorder as a symptom.
A major unresolved difference between the two diagnostic systems is that of the requirement in DSM of an impaired functional outcome. WHO for ICD argues that not all people with schizophrenia have functional deficits and so these are not specific for the diagnosis.
Neuroimaging techniques
Functional magnetic resonance imaging (fMRI) has become a tool in understanding brain activity and connectivity differences in individuals with schizophrenia. Through resting-state fMRI, researchers have observed altered connectivity patterns within several key brain networks, such as the default mode network (DMN), salience network (SN), and central executive network (CEN). Alterations may underlie cognitive and emotional symptoms in schizophrenia, such as disorganized thinking, impaired attention, and emotional dysregulation.
Comorbidities

Many people with schizophrenia may have one or more other mental disorders, such as anxiety disorders, obsessive–compulsive disorder, or substance use disorder. These are separate disorders that require treatment. When comorbid with schizophrenia, substance use disorder and antisocial personality disorder both increase the risk for violence. Comorbid substance use disorder also increases the risk of suicide.
Sleep disorders often co-occur with schizophrenia, and may be an early sign of relapse. Sleep disorders are linked with positive symptoms such as disorganized thinking and can adversely affect cortical plasticity and cognition. The consolidation of memories is disrupted in sleep disorders. They are associated with severity of illness, a poor prognosis, and poor quality of life. Sleep onset and maintenance insomnia is a common symptom, regardless of whether treatment has been received or not. Genetic variations have been found associated with these conditions involving the circadian rhythm, dopamine and histamine metabolism, and signal transduction.
Schizophrenia is also associated with a number of somatic comorbidities including diabetes mellitus type 2, autoimmune diseases, and cardiovascular diseases. The association of these with schizophrenia may be partially due to medications (e.g. dyslipidemia from antipsychotics), environmental factors (e.g. complications from an increased rate of cigarette smoking), or associated with the disorder itself (e.g. diabetes mellitus type 2 and some cardiovascular diseases are thought to be genetically linked). These somatic comorbidities contribute to reduced life expectancy among persons with the disorder.
Differential diagnosis
See also: Dual diagnosis and Comparison of bipolar disorder and schizophreniaTo make a diagnosis of schizophrenia other possible causes of psychosis need to be excluded. Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, or as schizophreniform disorder. Psychosis is noted in Other specified schizophrenia spectrum and other psychotic disorders as a DSM-5 category. Schizoaffective disorder is diagnosed if symptoms of mood disorder are substantially present alongside psychotic symptoms. Psychosis that results from a general medical condition or substance is termed secondary psychosis.
Psychotic symptoms may be present in several other conditions, including bipolar disorder, borderline personality disorder, substance intoxication, substance-induced psychosis, and a number of drug withdrawal syndromes. Non-bizarre delusions are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. Schizotypal personality disorder has symptoms that are similar but less severe than those of schizophrenia. Schizophrenia occurs along with obsessive–compulsive disorder (OCD) considerably more often than could be explained by chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia. There can be considerable overlap with the symptoms of post-traumatic stress disorder.
A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms, such as metabolic disturbance, systemic infection, syphilis, HIV-associated neurocognitive disorder, epilepsy, limbic encephalitis, and brain lesions. Stroke, multiple sclerosis, hyperthyroidism, hypothyroidism, and dementias such as Alzheimer's disease, Huntington's disease, frontotemporal dementia, and the Lewy body dementias may also be associated with schizophrenia-like psychotic symptoms. It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific medical indication or possible adverse effects from antipsychotic medication. In children hallucinations must be separated from typical childhood fantasies. It is difficult to distinguish childhood schizophrenia from autism.
Prevention
Prevention of schizophrenia is difficult as there are no reliable markers for the later development of the disorder.
Early intervention programs diagnose and treat patients in the prodromal phase of the illness. There is some evidence that these programs reduce symptoms. Patients tend to prefer early treatment programs to ordinary treatment and are less likely to disengage from them. As of 2020, it is unclear whether the benefits of early treatment persist once the treatment is terminated.
Cognitive behavioral therapy may reduce the risk of psychosis in those at high risk after a year and is recommended in this group, by the National Institute for Health and Care Excellence (NICE). Another preventive measure is to avoid drugs that have been associated with development of the disorder, including cannabis, cocaine, and amphetamines.
Antipsychotics are prescribed following a first-episode psychosis, and following remission, a preventive maintenance use is continued to avoid relapse. However, it is recognized that some people do recover following a single episode and that long-term use of antipsychotics will not be needed but there is no way of identifying this group.
Management
Main article: Management of schizophreniaThe primary treatment of schizophrenia is the use of antipsychotic medications, often in combination with psychosocial interventions and social supports. Community support services including drop-in centers, visits by members of a community mental health team, supported employment, and support groups are common. The time between the onset of psychotic symptoms to being given treatment – the duration of untreated psychosis (DUP) – is associated with a poorer outcome in both the short term and the long term.
Voluntary or involuntary admission to hospital may be imposed by doctors and courts who deem a person to be having a severe episode. In the UK, large mental hospitals termed asylums began to be closed down in the 1950s with the advent of antipsychotics, and with an awareness of the negative impact of long-term hospital stays on recovery. This process was known as deinstitutionalization, and community and supportive services were developed to support this change. Many other countries followed suit with the US starting in the 60s. There still remain a smaller group of people who do not improve enough to be discharged. In some countries that lack the necessary supportive and social services, long-term hospital stays are more usual.
Medication

The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called typical antipsychotics, like haloperidol, are dopamine antagonists that block D2 receptors, and affect the neurotransmission of dopamine. Those brought out later, the second-generation antipsychotics known as atypical antipsychotics, including olanzapine and risperidone, can also have an effect on another neurotransmitter, serotonin. Antipsychotics can reduce the symptoms of anxiety within hours of their use, but, for other symptoms, they may take several days or weeks to reach their full effect. They have little effect on negative and cognitive symptoms, which may be helped by additional psychotherapies and medications. There is no single antipsychotic suitable for first-line treatment for everyone, as responses and tolerances vary between people. Stopping medication may be considered after a single psychotic episode where there has been a full recovery with no symptoms for twelve months. Repeated relapses worsen the long-term outlook and the risk of relapse following a second episode is high, and long-term treatment is usually recommended.
About half of those with schizophrenia will respond favourably to antipsychotics, and have a good return of functioning. However, positive symptoms persist in up to a third of people. Following two trials of different antipsychotics over six weeks, that also prove ineffective, they will be classed as having treatment-resistant schizophrenia (TRS), and clozapine will be offered. Clozapine is of benefit to around half of this group although it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in less than 4% of people.
About 30 to 50 percent of people with schizophrenia do not accept that they have an illness or comply with their recommended treatment. For those who are unwilling or unable to take medication regularly, long-acting injections of antipsychotics may be used, which reduce the risk of relapse to a greater degree than oral medications. When used in combination with psychosocial interventions, they may improve long-term adherence to treatment.
The fixed-dose combination medication xanomeline/trospium chloride (Cobenfy) was approved for medical use in the United States in September 2024. It is the first cholinergic agonist approved by the US Food and Drug Administration (FDA) to treat schizophrenia.
Negative and cognitive symptoms are an unmet clinical need in antipsychotic-based treatment approaches. Psychostimulant drugs have been found effective in the treatment of negative symptoms, but are rarely prescribed due to concerns about the excacerbation of positive symptoms. It is possible that low-dose psychedelic therapies could be of benefit in schizophrenia through their prosocial and procognitive effects, although there is a serious risk that high dose psychedelic therapies could lead to worsening of positive symptoms.
Adverse effects
Further information: Antipsychotic § Adverse effectsExtrapyramidal symptoms, including akathisia, are associated with all commercially available antipsychotic to varying degrees. There is little evidence that second generation antipsychotics have reduced levels of extrapyramidical symptoms compared to typical antipsychotics. Tardive dyskinesia can occur due to long-term use of antipsychotics, developing after months or years of use. The antipsychotic clozapine is also associated with thromboembolism (including pulmonary embolism), myocarditis, and cardiomyopathy.
Psychosocial interventions
Further information: Management of schizophrenia § PsychosocialA number of psychosocial interventions that include several types of psychotherapy may be useful in the treatment of schizophrenia such as: family therapy, group therapy, cognitive remediation therapy (CRT), cognitive behavioral therapy (CBT), and metacognitive training. Skills training, help with substance use, and weight management – often needed as a side effect of an antipsychotic – are also offered. In the US, interventions for first episode psychosis have been brought together in an overall approach known as coordinated speciality care (CSC) and also includes support for education. In the UK care across all phases is a similar approach that covers many of the treatment guidelines recommended. The aim is to reduce the number of relapses and stays in the hospital.
Other support services for education, employment, and housing are usually offered. For people with severe schizophrenia, who are discharged from a stay in the hospital, these services are often brought together in an integrated approach to offer support in the community away from the hospital setting. In addition to medicine management, housing, and finances, assistance is given for more routine matters such as help with shopping and using public transport. This approach is known as assertive community treatment (ACT) and has been shown to achieve positive results in symptoms, social functioning and quality of life. Another more intense approach is known as intensive care management (ICM). ICM is a stage further than ACT and emphasises support of high intensity in smaller caseloads, (less than twenty). This approach is to provide long-term care in the community. Studies show that ICM improves many of the relevant outcomes including social functioning.
Some studies have shown little evidence for the effectiveness of CBT in either reducing symptoms or preventing relapse. However, other studies have found that CBT does improve overall psychotic symptoms (when in use with medication) and it has been recommended in Canada, but has been seen to have no effect on social function, relapse, or quality of life. In the UK it is recommended as an add-on therapy in the treatment of schizophrenia. Arts therapies are seen to improve negative symptoms in some people, and are recommended by NICE in the UK. This approach is criticised as having not been well-researched, and arts therapies are not recommended in Australian guidelines for example. Peer support, in which people with personal experience of schizophrenia, provide help to each other, is of unclear benefit.
Other
Exercise including aerobic exercise has been shown to improve positive and negative symptoms, cognition, working memory, and improve quality of life. Exercise has also been shown to increase the volume of the hippocampus in those with schizophrenia. A decrease in hippocampal volume is one of the factors linked to the development of the disease. However, there still remains the problem of increasing motivation for, and maintaining participation in physical activity. Supervised sessions are recommended. In the UK healthy eating advice is offered alongside exercise programs.
An inadequate diet is often found in schizophrenia, and associated vitamin deficiencies including those of folate, and vitamin D are linked to the risk factors for the development of schizophrenia and for early death including heart disease. Those with schizophrenia possibly have the worst diet of all the mental disorders. Lower levels of folate and vitamin D have been noted as significantly lower in first episode psychosis. The use of supplemental folate is recommended. A zinc deficiency has also been noted. Vitamin B12 is also often deficient and this is linked to worse symptoms. Supplementation with B vitamins has been shown to significantly improve symptoms, and to put in reverse some of the cognitive deficits. It is also suggested that the noted dysfunction in gut microbiota might benefit from the use of probiotics.
Prognosis
Main article: Prognosis of schizophreniaSee also: Physical health in schizophrenia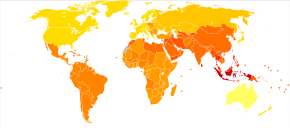
| no data ≤ 185 185–197 197–207 207–218 218–229 229–240 | 240–251 251–262 262–273 273–284 284–295 ≥ 295 |
Schizophrenia has great human and economic costs. It decreases life expectancy by between 10 and 28 years. This is primarily because of its association with heart disease, diabetes, obesity, poor diet, a sedentary lifestyle, and smoking, with an increased rate of suicide playing a lesser role. Side effects of antipsychotics may also increase the risk.
Almost 40% of those with schizophrenia die from complications of cardiovascular disease which is seen to be increasingly associated. An underlying factor of sudden cardiac death may be Brugada syndrome (BrS) – BrS mutations that overlap with those linked with schizophrenia are the calcium channel mutations. BrS may also be drug-induced from certain antipsychotics and antidepressants. Primary polydipsia, or excessive fluid intake, is relatively common in people with chronic schizophrenia. This may lead to hyponatremia which can be life-threatening. Antipsychotics can lead to a dry mouth, but there are several other factors that may contribute to the disorder; it may reduce life expectancy by 13 percent. Barriers to improving the mortality rate in schizophrenia are poverty, overlooking the symptoms of other illnesses, stress, stigma, and medication side effects.
Schizophrenia is a major cause of disability. In 2016, it was classed as the 12th most disabling condition. Approximately 75% of people with schizophrenia have ongoing disability with relapses. Some people do recover completely and others function well in society. Most people with schizophrenia live independently with community support. About 85% are unemployed. In people with a first episode of psychosis in schizophrenia a good long-term outcome occurs in 31%, an intermediate outcome in 42% and a poor outcome in 31%. Males are affected more often than females, and have a worse outcome. Studies showing that outcomes for schizophrenia appear better in the developing than the developed world have been questioned. Social problems, such as long-term unemployment, poverty, homelessness, exploitation, stigmatization and victimization are common consequences, and lead to social exclusion.
There is a higher than average suicide rate associated with schizophrenia estimated at 5% to 6%, most often occurring in the period following onset or first hospital admission. Several times more (20 to 40%) attempt suicide at least once. There are a variety of risk factors, including male sex, depression, a high IQ, heavy smoking, and substance use. Repeated relapse is linked to an increased risk of suicidal behavior. The use of clozapine can reduce the risk of suicide, and of aggression.
A strong association between schizophrenia and tobacco smoking has been shown in worldwide studies. Smoking is especially high in those diagnosed with schizophrenia, with estimates ranging from 80 to 90% being regular smokers, as compared to 20% of the general population. Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content. Some propose that this is in an effort to improve symptoms. Among people with schizophrenia use of cannabis is also common.
Schizophrenia leads to an increased risk of dementia.
Violence
Most people with schizophrenia are not aggressive, and are more likely to be victims of violence rather than perpetrators. People with schizophrenia are commonly exploited and victimized by violent crime as part of a broader dynamic of social exclusion. People diagnosed with schizophrenia are also subject to forced drug injections, seclusion, and restraint at high rates.
The risk of violence by people with schizophrenia is small. There are minor subgroups where the risk is high. This risk is usually associated with a comorbid disorder such as a substance use disorder – in particular alcohol, or with antisocial personality disorder. Substance use disorder is strongly linked, and other risk factors are linked to deficits in cognition and social cognition including facial perception and insight that are in part included in theory of mind impairments. Poor cognitive functioning, decision-making, and facial perception may contribute to making a wrong judgement of a situation that could result in an inappropriate response such as violence. These associated risk factors are also present in antisocial personality disorder which when present as a comorbid disorder greatly increases the risk of violence.
Epidemiology
Main article: Epidemiology of schizophrenia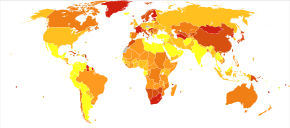
In 2017, the Global Burden of Disease Study estimated there were 1.1 million new cases; in 2022 the World Health Organization (WHO) reported a total of 24 million cases globally. Schizophrenia affects around 0.3–0.7% of people at some point in their life. In areas of conflict this figure can rise to between 4.0 and 6.5%. It occurs 1.4 times more frequently in males than females and typically appears earlier in men.
Worldwide, schizophrenia is the most common psychotic disorder. The frequency of schizophrenia varies across the world, within countries, and at the local and neighborhood level; this variation in prevalence between studies over time, across geographical locations, and by gender is as high as fivefold.
Schizophrenia causes approximately one percent of worldwide disability adjusted life years and resulted in 17,000 deaths in 2015.
In 2000, WHO found the percentage of people affected and the number of new cases that develop each year is roughly similar around the world, with age-standardized prevalence per 100,000 ranging from 343 in Africa to 544 in Japan and Oceania for men, and from 378 in Africa to 527 in Southeastern Europe for women.
History
Main article: History of schizophreniaConceptual development
Main article: History of schizophrenia § Conceptual development Further information: Dementia praecox
Accounts of a schizophrenia-like syndrome are rare in records before the 19th century; the earliest case reports were in 1797 and 1809. The term dementia praecox ("premature dementia") was used by German psychiatrist Heinrich Schüle in 1886 and then in 1891 by Arnold Pick in a case report of hebephrenia. In 1893 Emil Kraepelin used the term in making a distinction, known as the Kraepelinian dichotomy, between the two psychoses: dementia praecox and manic depression (now called bipolar disorder). When it became evident that the disorder was not a degenerative dementia, it was renamed schizophrenia by Eugen Bleuler in 1908.
The word schizophrenia ("splitting of the mind") is Modern Latin, derived from the Greek schizein (Ancient Greek: σχίζειν, lit. 'to split') and phrēn (Ancient Greek: φρήν, lit. 'mind'). Its use was intended to describe the separation of function between personality, thinking, memory, and perception.
In the early 20th century, the psychiatrist Kurt Schneider categorized the psychotic symptoms of schizophrenia into two groups: hallucinations and delusions. The hallucinations were listed as specific to auditory and the delusions included thought disorders. These were seen as important symptoms, termed first-rank. The most common first-rank symptom was found to belong to thought disorders. In 2013 the first-rank symptoms were excluded from the DSM-5 criteria; while they may not be useful in diagnosing schizophrenia, they can assist in differential diagnosis.
Subtypes of schizophrenia—classified as paranoid, disorganized, catatonic, undifferentiated, and residual—were difficult to distinguish and are no longer recognized as separate conditions by DSM-5 (2013) or ICD-11.
Breadth of diagnosis
Before the 1960s, nonviolent petty criminals and women were sometimes diagnosed with schizophrenia, categorizing the latter as ill for not performing their duties as wives and mothers. In the mid- to late 1960s, black men were categorized as "hostile and aggressive" and diagnosed as schizophrenic at much higher rates, their civil rights and Black Power activism labeled as delusions.
In the early 1970s in the United States, the diagnostic model for schizophrenia was broad and clinically based using DSM II. Schizophrenia was diagnosed far more in the United States than in Europe, where the ICD-9 criteria were followed. The US model was criticised for failing to demarcate clearly those people with a mental illness. In 1980 DSM III was published and showed a shift in focus from the clinically based biopsychosocial model to a reason-based medical model. DSM IV brought an increased focus on an evidence-based medical model.
Historical treatment
Main article: History of schizophrenia § Development of treatments in the 20th century
In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia. Insulin shock involved injecting large doses of insulin to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was in use as electroconvulsive therapy (ECT) by 1938.
Carried out from the 1930s until the 1970s in the United States and until the 1980s in France, psychosurgery, including such modalities as the lobotomy, is recognized as a human rights abuse. In the mid-1950s, chlorpromazine, the first typical antipsychotic, was introduced, followed in the 1970s by clozapine, the first atypical antipsychotic.
Political abuse
Further information: Political abuse of psychiatryFrom the 1960s until 1989, psychiatrists in the USSR and Eastern Bloc diagnosed thousands of people with sluggish schizophrenia, without signs of psychosis, based on "the assumption that symptoms would later appear". Now discredited, the diagnosis provided a convenient way to confine political dissidents.
Society and culture
See also: List of people with schizophrenia and Religion and schizophreniaIn the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002. In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.
Stigma

In 2002, the term for schizophrenia in Japan was changed from seishin-bunretsu-byō (精神分裂病, lit. 'mind-split disease') to tōgō-shitchō-shō (統合失調症, lit. 'integration–dysregulation syndrome') to reduce stigma. The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model. A similar change was made in South Korea in 2012 to attunement disorder.
Cultural depictions
Media coverage, especially movies, reinforce the public perception of an association between schizophrenia and violence. A majority of movies have historically depicted characters with schizophrenia as criminal, dangerous, violent, unpredictable and homicidal, and depicted delusions and hallucinations as the main symptoms of schizophrenic characters, ignoring other common symptoms, furthering stereotypes of schizophrenia including the idea of a split personality.
The book A Beautiful Mind chronicled the life of John Forbes Nash who had been diagnosed with schizophrenia and won the Nobel Memorial Prize in Economic Sciences. The book was made into a film with the same name; an earlier documentary film was A Brilliant Madness.
In the UK, guidelines for reporting conditions and award campaigns have shown a reduction in negative reporting since 2013.
In 1964 a case study of three males diagnosed with schizophrenia who each had the delusional belief that they were Jesus Christ was published as The Three Christs of Ypsilanti; a film with the title Three Christs was released in 2020.
Research directions
See also: Animal models of schizophreniaA 2015 Cochrane review found unclear evidence of benefit from brain stimulation techniques to treat the positive symptoms of schizophrenia, in particular auditory verbal hallucinations (AVHs). Most studies focus on transcranial direct-current stimulation (tDCM), and repetitive transcranial magnetic stimulation (rTMS). Techniques based on focused ultrasound for deep brain stimulation could provide insight for the treatment of AVHs.
The study of potential biomarkers that would help in diagnosis and treatment of schizophrenia is an active area of research as of 2020. Possible biomarkers include markers of inflammation, neuroimaging, brain-derived neurotrophic factor (BDNF), and speech analysis. Some markers such as C-reactive protein are useful in detecting levels of inflammation implicated in some psychiatric disorders but they are not disorder-specific. Other inflammatory cytokines are found to be elevated in first episode psychosis and acute relapse that are normalized after treatment with antipsychotics, and these may be considered as state markers. Deficits in sleep spindles in schizophrenia may serve as a marker of an impaired thalamocortical circuit, and a mechanism for memory impairment. MicroRNAs are highly influential in early neuronal development, and their disruption is implicated in several CNS disorders; circulating microRNAs (cimiRNAs) are found in body fluids such as blood and cerebrospinal fluid, and changes in their levels are seen to relate to changes in microRNA levels in specific regions of brain tissue. These studies suggest that cimiRNAs have the potential to be early and accurate biomarkers in a number of disorders including schizophrenia.
Ongoing fMRI research aims to identify biomarkers within these brain networks, potentially aiding in earlier diagnosis and better tracking of treatment responses in schizophrenia.
Explanatory notes
- A 2007 review stated that the 2002 estimate was still the best available, and a 2018 review cited the same $62.7 billion.
References
- Jones D (2003) . Roach P, Hartmann J, Setter J (eds.). English Pronouncing Dictionary. Cambridge University Press. ISBN 978-3-12-539683-8.
- ^ "Schizophrenia Fact sheet". World Health Organization. 10 January 2022. Retrieved 23 August 2022.
- ^ "Schizophrenia". Health topics. US National Institute of Mental Health. April 2022. Retrieved 22 August 2022.
- "Medicinal treatment of psychosis/schizophrenia". Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). 21 November 2012. Archived from the original on 29 June 2017. Retrieved 26 June 2017.
- Proietto Sr J (November 2004). "Diabetes and Antipsychotic Drugs". Medsafe.
- Holt RI (September 2019). "Association Between Antipsychotic Medication Use and Diabetes". Current Diabetes Reports. 19 (10). National Center for Biotechnology Information: 96. doi:10.1007/s11892-019-1220-8. ISSN 1534-4827. PMC 6718373. PMID 31478094.
- ^ Owen MJ, Sawa A, Mortensen PB (July 2016). "Schizophrenia". The Lancet. 388 (10039): 86–97. doi:10.1016/S0140-6736(15)01121-6. PMC 4940219. PMID 26777917.
- "Transition of Substance-Induced, Brief, and Atypical Psychoses to Schizophrenia: A Systematic Review and Meta-analysis". Schizophrenia Bulletin. May 2020.
- Gruebner O, Rapp MA, Adli M, Kluge U, Galea S, Heinz A (February 2017). "Cities and Mental Health". Deutsches Ärzteblatt International. 114 (8): 121–127. doi:10.3238/arztebl.2017.0121. PMC 5374256. PMID 28302261.
- ^ Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Association. 2013. pp. 99–105. ISBN 978-0-89042-555-8.
- ^ Ferri FF (2010). "Chapter S". Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia: Elsevier/Mosby. ISBN 978-0-323-07699-9.
- ^ Paris J (December 2018). "Differential Diagnosis of Borderline Personality Disorder". The Psychiatric Clinics of North America. 41 (4): 575–582. doi:10.1016/j.psc.2018.07.001. PMID 30447725. S2CID 53951650.
- ^ Laursen TM, Nordentoft M, Mortensen PB (2014). "Excess early mortality in schizophrenia". Annual Review of Clinical Psychology. 10: 425–448. doi:10.1146/annurev-clinpsy-032813-153657. PMID 24313570.
- ^ "Schizophrenia". Statistics. US National Institute of Mental Health (NIMH). 22 April 2022. Retrieved 23 August 2022.
- "Schizophrenia Fact Sheet and Information". World Health Organization.
- ^ Wang H, Naghavi M, Allen C, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- "ICD-11: 6A20 Schizophrenia". World Health Organization. Retrieved 23 August 2022.
- ^ Ferri FF (2019). Ferri's clinical advisor 2019: 5 books in 1. Elsevier. pp. 1225–1226. ISBN 9780323530422.
- ^ Javitt DC (June 2014). "Balancing therapeutic safety and efficacy to improve clinical and economic outcomes in schizophrenia: a clinical overview". The American Journal of Managed Care. 20 (8 Suppl): S160-165. PMID 25180705.
- ^ James SL, Abate D (November 2018). "Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017". The Lancet. 392 (10159): 1789–1858. doi:10.1016/S0140-6736(18)32279-7. PMC 6227754. PMID 30496104.
- ^ van de Leemput J, Hess JL, Glatt SJ, Tsuang MT (2016). Genetics of Schizophrenia: Historical Insights and Prevailing Evidence. Advances in Genetics. Vol. 96. pp. 99–141. doi:10.1016/bs.adgen.2016.08.001. ISBN 978-0-12-809672-7. PMID 27968732.
- ^ Parakh P, Basu D (August 2013). "Cannabis and psychosis: have we found the missing links?". Asian Journal of Psychiatry (Review). 6 (4): 281–287. doi:10.1016/j.ajp.2013.03.012. PMID 23810133.
Cannabis acts as a component cause of psychosis, that is, it increases the risk of psychosis in people with certain genetic or environmental vulnerabilities, though by itself, it is neither a sufficient nor a necessary cause of psychosis.
- ^ Vita A, Barlati S (May 2018). "Recovery from schizophrenia: is it possible?". Current Opinion in Psychiatry. 31 (3): 246–255. doi:10.1097/YCO.0000000000000407. PMID 29474266. S2CID 35299996.
- Lawrence RE, First MB, Lieberman JA (2015). "Chapter 48: Schizophrenia and Other Psychoses". In Tasman A, Kay J, Lieberman JA, First MB, Riba MB (eds.). Psychiatry (fourth ed.). John Wiley & Sons, Ltd. pp. 798, 816, 819. doi:10.1002/9781118753378.ch48. ISBN 978-1-118-84547-9.
- ^ Killaspy H (September 2014). "Contemporary mental health rehabilitation". East Asian Archives of Psychiatry. 24 (3): 89–94. PMID 25316799.
- ^ Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. (October 2018). "Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016". Schizophrenia Bulletin. 44 (6): 1195–1203. doi:10.1093/schbul/sby058. PMC 6192504. PMID 29762765.
- ^ van Os J, Kapur S (August 2009). "Schizophrenia" (PDF). Lancet. 374 (9690): 635–645. doi:10.1016/S0140-6736(09)60995-8. PMID 19700006. S2CID 208792724. Archived from the original (PDF) on 23 June 2013. Retrieved 23 December 2011.
- ^ Hor K, Taylor M (November 2010). "Suicide and schizophrenia: a systematic review of rates and risk factors". Journal of Psychopharmacology. 24 (4 Suppl): 81–90. doi:10.1177/1359786810385490. PMC 2951591. PMID 20923923.
- ^ Siskind D, Siskind V, Kisely S (November 2017). "Clozapine Response Rates among People with Treatment-Resistant Schizophrenia: Data from a Systematic Review and Meta-Analysis". Canadian Journal of Psychiatry. 62 (11): 772–777. doi:10.1177/0706743717718167. PMC 5697625. PMID 28655284.
- Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. (September 2013). "Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis". Lancet. 382 (9896): 951–962. doi:10.1016/S0140-6736(13)60733-3. PMID 23810019. S2CID 32085212.
- ^ Becker T, Kilian R (2006). "Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?". Acta Psychiatrica Scandinavica. Supplementum. 113 (429): 9–16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476. S2CID 34615961.
- ^ Capdevielle D, Boulenger JP, Villebrun D, Ritchie K (September 2009). "Durées d'hospitalisation des patients souffrant de schizophrénie: implication des systèmes de soin et conséquences médicoéconomiques" [Schizophrenic patients' length of stay: mental health care implication and medicoeconomic consequences]. L'Encéphale (in French). 35 (4): 394–399. doi:10.1016/j.encep.2008.11.005. PMID 19748377.
- ^ Narayan KK, Kumar DS (January 2012). "Disability in a Group of Long-stay Patients with Schizophrenia: Experience from a Mental Hospital". Indian Journal of Psychological Medicine. 34 (1): 70–75. doi:10.4103/0253-7176.96164. PMC 3361848. PMID 22661812.
- ^ "Psychosis and schizophrenia in adults: treatment and management" (PDF). National Institute for Health and Care Excellence (NICE). March 2014. pp. 4–34. Archived from the original (PDF) on 20 April 2014. Retrieved 19 April 2014.
- Stępnicki P, Kondej M, Kaczor AA (20 August 2018). "Current Concepts and Treatments of Schizophrenia". Molecules. 23 (8): 2087. doi:10.3390/molecules23082087. PMC 6222385. PMID 30127324.
- ^ "RAISE Questions and Answers". US National Institute of Mental Health. Retrieved 29 December 2019.
- Marshall M (September 2005). "Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review". Archives of General Psychiatry. 62 (9): 975–983. doi:10.1001/archpsyc.62.9.975. PMID 16143729. S2CID 13504781.
- ^ Montagnese M, Leptourgos P, Fernyhough C, et al. (January 2021). "A Review of Multimodal Hallucinations: Categorization, Assessment, Theoretical Perspectives, and Clinical Recommendations". Schizophr Bull. 47 (1): 237–248. doi:10.1093/schbul/sbaa101. PMC 7825001. PMID 32772114.
- Császár N, Kapócs G, Bókkon I (27 May 2019). "A possible key role of vision in the development of schizophrenia". Reviews in the Neurosciences. 30 (4): 359–379. doi:10.1515/revneuro-2018-0022 (inactive 3 December 2024). PMID 30244235. S2CID 52813070.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - ^ American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. pp. 299–304. ISBN 978-0-89042-025-6.
- ^ Heinz A, Voss M, Lawrie SM, Mishara A, Bauer M, Gallinat J, et al. (September 2016). "Shall we really say goodbye to first rank symptoms?". European Psychiatry. 37: 8–13. doi:10.1016/j.eurpsy.2016.04.010. PMID 27429167. S2CID 13761854.
- ^ Adida M, Azorin JM, Belzeaux R, Fakra E (December 2015). "". L'Encephale. 41 (6 Suppl 1): 6S15–17. doi:10.1016/S0013-7006(16)30004-5. PMID 26776385.
- Mach C, Dollfus S (April 2016). "". L'Encephale. 42 (2): 165–171. doi:10.1016/j.encep.2015.12.020. PMID 26923997.
- Waltz JA, Gold JM (2016). "Motivational Deficits in Schizophrenia and the Representation of Expected Value". Current Topics in Behavioral Neurosciences. 27: 375–410. doi:10.1007/7854_2015_385. ISBN 978-3-319-26933-7. PMC 4792780. PMID 26370946.
- ^ Husain M, Roiser JP (August 2018). "Neuroscience of apathy and anhedonia: a transdiagnostic approach". Nature Reviews. Neuroscience. 19 (8): 470–484. doi:10.1038/s41583-018-0029-9. PMID 29946157. S2CID 49428707.
- ^ Galderisi S, Mucci A, Buchanan RW, Arango C (August 2018). "Negative symptoms of schizophrenia: new developments and unanswered research questions". The Lancet. Psychiatry. 5 (8): 664–677. doi:10.1016/S2215-0366(18)30050-6. PMID 29602739. S2CID 4483198.
- Klaus F, Dorsaz O, Kaiser S (19 September 2018). "". Revue médicale suisse. 14 (619): 1660–1664. doi:10.53738/REVMED.2018.14.619.1660. PMID 30230774. S2CID 246764656.
- Batinic B (June 2019). "Cognitive Models of Positive and Negative Symptoms of Schizophrenia and Implications for Treatment". Psychiatria Danubina. 31 (Suppl 2): 181–184. PMID 31158119.
- Bortolon C, Macgregor A, Capdevielle D, Raffard S (September 2018). "Apathy in schizophrenia: A review of neuropsychological and neuroanatomical studies". Neuropsychologia. 118 (Pt B): 22–33. doi:10.1016/j.neuropsychologia.2017.09.033. PMID 28966139. S2CID 13411386.
- ^ Marder SR, Kirkpatrick B (May 2014). "Defining and measuring negative symptoms of schizophrenia in clinical trials". European Neuropsychopharmacology. 24 (5): 737–743. doi:10.1016/j.euroneuro.2013.10.016. PMID 24275698. S2CID 5172022.
- ^ Tatsumi K, Kirkpatrick B, Strauss GP, Opler M (April 2020). "The brief negative symptom scale in translation: A review of psychometric properties and beyond". European Neuropsychopharmacology. 33: 36–44. doi:10.1016/j.euroneuro.2020.01.018. PMID 32081498. S2CID 211141678.
- Klaus F, Kaiser S, Kirschner M (June 2018). "". Therapeutische Umschau. 75 (1): 51–56. doi:10.1024/0040-5930/a000966. PMID 29909762. S2CID 196502392.
- Lindenmayer JP, Nasrallah H, Pucci M, James S, Citrome L (1 July 2013). "A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities". Schizophrenia Research. 147 (2): 241–252. doi:10.1016/j.schres.2013.03.019. ISSN 0920-9964. PMID 23619055.
- Wójciak P, Rybakowski J (30 April 2018). "Clinical picture, pathogenesis and psychometric assessment of negative symptoms of schizophrenia". Psychiatria Polska. 52 (2): 185–197. doi:10.12740/PP/70610. PMID 29975360.
- ^ Murante T, Cohen CI (January 2017). "Cognitive Functioning in Older Adults With Schizophrenia". Focus (American Psychiatric Publishing). 15 (1): 26–34. doi:10.1176/appi.focus.20160032. PMC 6519630. PMID 31975837.
- ^ Kar SK, Jain M (July 2016). "Current understandings about cognition and the neurobiological correlates in schizophrenia". Journal of Neurosciences in Rural Practice. 7 (3): 412–418. doi:10.4103/0976-3147.176185. PMC 4898111. PMID 27365960.
- ^ Bozikas VP, Andreou C (February 2011). "Longitudinal studies of cognition in first episode psychosis: a systematic review of the literature". The Australian and New Zealand Journal of Psychiatry. 45 (2): 93–108. doi:10.3109/00048674.2010.541418. PMID 21320033. S2CID 26135485.
- Shah JN, Qureshi SU, Jawaid A, Schulz PE (June 2012). "Is there evidence for late cognitive decline in chronic schizophrenia?". The Psychiatric Quarterly. 83 (2): 127–144. doi:10.1007/s11126-011-9189-8. PMID 21863346. S2CID 10970088.
- ^ Biedermann F, Fleischhacker WW (August 2016). "Psychotic disorders in DSM-5 and ICD-11". CNS Spectrums. 21 (4): 349–354. doi:10.1017/S1092852916000316. PMID 27418328. S2CID 24728447.
- ^ Vidailhet P (September 2013). "". L'Encéphale (in French). 39 (Suppl 2): S83-92. doi:10.1016/S0013-7006(13)70101-5. PMID 24084427.
- ^ Hashimoto K (5 July 2019). "Recent Advances in the Early Intervention in Schizophrenia: Future Direction from Preclinical Findings". Current Psychiatry Reports. 21 (8): 75. doi:10.1007/s11920-019-1063-7. PMID 31278495. S2CID 195814019.
- ^ Green MF, Horan WP, Lee J (June 2019). "Nonsocial and social cognition in schizophrenia: current evidence and future directions". World Psychiatry. 18 (2): 146–161. doi:10.1002/wps.20624. PMC 6502429. PMID 31059632.
- Javitt DC, Sweet RA (September 2015). "Auditory dysfunction in schizophrenia: integrating clinical and basic features". Nature Reviews. Neuroscience. 16 (9): 535–550. doi:10.1038/nrn4002. PMC 4692466. PMID 26289573.
- ^ Megreya AM (2016). "Face perception in schizophrenia: a specific deficit". Cognitive Neuropsychiatry. 21 (1): 60–72. doi:10.1080/13546805.2015.1133407. PMID 26816133. S2CID 26125559.
- Eack SM (July 2012). "Cognitive remediation: a new generation of psychosocial interventions for people with schizophrenia". Social Work. 57 (3): 235–246. doi:10.1093/sw/sws008. PMC 3683242. PMID 23252315.
- Pomarol-Clotet E, Oh M, Laws KR, McKenna PJ (February 2008). "Semantic priming in schizophrenia: systematic review and meta-analysis". The British Journal of Psychiatry. 192 (2): 92–97. doi:10.1192/bjp.bp.106.032102. hdl:2299/2735. PMID 18245021.
- Goldberg TE, Keefe RS, Goldman RS, Robinson DG, Harvey PD (April 2010). "Circumstances under which practice does not make perfect: a review of the practice effect literature in schizophrenia and its relevance to clinical treatment studies". Neuropsychopharmacology. 35 (5): 1053–1062. doi:10.1038/npp.2009.211. PMC 3055399. PMID 20090669.
- King DJ, Hodgekins J, Chouinard PA, Chouinard VA, Sperandio I (June 2017). "A review of abnormalities in the perception of visual illusions in schizophrenia". Psychonomic Bulletin and Review. 24 (3): 734–751. doi:10.3758/s13423-016-1168-5. PMC 5486866. PMID 27730532.
- Kohler CG, Walker JB, Martin EA, Healey KM, Moberg PJ (September 2010). "Facial emotion perception in schizophrenia: a meta-analytic review". Schizophrenia Bulletin. 36 (5): 1009–1019. doi:10.1093/schbul/sbn192. PMC 2930336. PMID 19329561.
- Le Gall E, Iakimova G (December 2018). "". L'Encéphale. 44 (6): 523–537. doi:10.1016/j.encep.2018.03.004. PMID 30122298. S2CID 150099236.
- Grill-Spector K, Weiner KS, Kay K, Gomez J (September 2017). "The Functional Neuroanatomy of Human Face Perception". Annual Review of Vision Science. 3: 167–196. doi:10.1146/annurev-vision-102016-061214. PMC 6345578. PMID 28715955.
- Fountoulakis KN, Panagiotidis P, Kimiskidis V, Nimatoudis I, Gonda X (February 2019). "Neurological soft signs in familial and sporadic schizophrenia". Psychiatry Research. 272: 222–229. doi:10.1016/j.psychres.2018.12.105. PMID 30590276. S2CID 56476015.
- Bourgou Gaha S, Halayem Dhouib S, Amado I, Bouden A (June 2015). "". L'Encephale. 41 (3): 209–214. doi:10.1016/j.encep.2014.01.005. PMID 24854724.
- ^ Da Fonseca D, Fourneret P (December 2018). "". L'Encephale. 44 (6S): S8–S11. doi:10.1016/S0013-7006(19)30071-5. PMID 30935493. S2CID 150798223.
- Häfner H (2019). "From Onset and Prodromal Stage to a Life-Long Course of Schizophrenia and Its Symptom Dimensions: How Sex, Age, and Other Risk Factors Influence Incidence and Course of Illness". Psychiatry Journal. 2019: 9804836. doi:10.1155/2019/9804836. PMC 6500669. PMID 31139639.
- Cohen CI, Freeman K, Ghoneim D, Vengassery A, Ghezelaiagh B, Reinhardt MM (March 2018). "Advances in the Conceptualization and Study of Schizophrenia in Later Life". The Psychiatric Clinics of North America. 41 (1): 39–53. doi:10.1016/j.psc.2017.10.004. PMID 29412847.
- ^ George M, Maheshwari S, Chandran S, Manohar JS, Sathyanarayana Rao TS (October 2017). "Understanding the schizophrenia prodrome". Indian Journal of Psychiatry. 59 (4): 505–509. doi:10.4103/psychiatry.IndianJPsychiatry_464_17 (inactive 1 November 2024). PMC 5806335. PMID 29497198.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Conroy S, Francis M, Hulvershorn LA (March 2018). "Identifying and treating the prodromal phases of bipolar disorder and schizophrenia". Current Treatment Options in Psychiatry. 5 (1): 113–128. doi:10.1007/s40501-018-0138-0. PMC 6196741. PMID 30364516.
- Lecardeur L, Meunier-Cussac S, Dollfus S (May 2013). "". L'Encephale. 39 (Suppl 1): S64-71. doi:10.1016/j.encep.2012.10.011. PMID 23528322.
- Mullin AP, Gokhale A, Moreno-De-Luca A, Sanyal S, Waddington JL, Faundez V (December 2013). "Neurodevelopmental disorders: mechanisms and boundary definitions from genomes, interactomes and proteomes". Translational Psychiatry. 3 (12): e329. doi:10.1038/tp.2013.108. PMC 4030327. PMID 24301647.
- ^ Davis J, Eyre H, Jacka FN, Dodd S, Dean O, McEwen S, et al. (June 2016). "A review of vulnerability and risks for schizophrenia: Beyond the two hit hypothesis". Neuroscience and Biobehavioral Reviews. 65: 185–194. doi:10.1016/j.neubiorev.2016.03.017. PMC 4876729. PMID 27073049.
- ^ Perkovic MN, Erjavec GN, Strac DS, Uzun S, Kozumplik O, Pivac N (March 2017). "Theranostic Biomarkers for Schizophrenia". International Journal of Molecular Sciences. 18 (4): 733. doi:10.3390/ijms18040733. PMC 5412319. PMID 28358316.
- ^ Suvisaari J (2010). "". Duodecim; Laaketieteellinen Aikakauskirja (in Finnish). 126 (8): 869–876. PMID 20597333.
- ^ Combs DR, Mueser KT, Gutierrez MM (2011). "Chapter 8: Schizophrenia: Etiological considerations". In Hersen M, Beidel DC (eds.). Adult psychopathology and diagnosis (6th ed.). John Wiley & Sons. ISBN 978-1-118-13884-7.
- O'Donovan MC, Williams NM, Owen MJ (October 2003). "Recent advances in the genetics of schizophrenia". Human Molecular Genetics. 12 Spec No 2: R125–133. doi:10.1093/hmg/ddg302. PMID 12952866.
- ^ Torrey EF, Yolken RH (August 2019). "Schizophrenia as a pseudogenetic disease: A call for more gene-environmental studies". Psychiatry Research. 278: 146–150. doi:10.1016/j.psychres.2019.06.006. PMID 31200193. S2CID 173991937.
- ^ Picchioni MM, Murray RM (July 2007). "Schizophrenia". BMJ. 335 (7610): 91–95. doi:10.1136/bmj.39227.616447.BE. PMC 1914490. PMID 17626963.
- Farrell MS, Werge T, Sklar P, Owen MJ, Ophoff RA, O'Donovan MC, et al. (May 2015). "Evaluating historical candidate genes for schizophrenia". Molecular Psychiatry. 20 (5): 555–562. doi:10.1038/mp.2015.16. PMC 4414705. PMID 25754081.
- Schulz SC, Green MF, Nelson KJ (2016). Schizophrenia and Psychotic Spectrum Disorders. Oxford University Press. pp. 124–125. ISBN 9780199378067.
- Schork AJ, Wang Y, Thompson WK, Dale AM, Andreassen OA (February 2016). "New statistical approaches exploit the polygenic architecture of schizophrenia—implications for the underlying neurobiology". Current Opinion in Neurobiology. 36: 89–98. doi:10.1016/j.conb.2015.10.008. PMC 5380793. PMID 26555806.
- Coelewij L, Curtis D (2018). "Mini-review: Update on the genetics of schizophrenia". Annals of Human Genetics. 82 (5): 239–243. doi:10.1111/ahg.12259. ISSN 0003-4800. PMID 29923609. S2CID 49311660.
- Kendler KS (March 2016). "The Schizophrenia Polygenic Risk Score: To What Does It Predispose in Adolescence?". JAMA Psychiatry. 73 (3): 193–194. doi:10.1001/jamapsychiatry.2015.2964. PMID 26817666.
- ^ Lowther C, Costain G, Baribeau DA, Bassett AS (September 2017). "Genomic Disorders in Psychiatry—What Does the Clinician Need to Know?". Current Psychiatry Reports. 19 (11): 82. doi:10.1007/s11920-017-0831-5. PMID 28929285. S2CID 4776174.
- Bundy H, Stahl D, MacCabe JH (February 2011). "A systematic review and meta-analysis of the fertility of patients with schizophrenia and their unaffected relatives: Fertility in schizophrenia". Acta Psychiatrica Scandinavica. 123 (2): 98–106. doi:10.1111/j.1600-0447.2010.01623.x. PMID 20958271. S2CID 45179016.
- van Dongen J, Boomsma DI (March 2013). "The evolutionary paradox and the missing heritability of schizophrenia". American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 162 (2): 122–136. doi:10.1002/ajmg.b.32135. PMID 23355297. S2CID 9648115.
- Owen MJ, Sawa A, Mortensen PB (2 July 2016). "Schizophrenia". Lancet. 388 (10039): 86–97. doi:10.1016/S0140-6736(15)01121-6. PMC 4940219. PMID 26777917.
- Goh XX, Tang PY, Tee SF (July 2021). "8-Hydroxy-2'-Deoxyguanosine and Reactive Oxygen Species as Biomarkers of Oxidative Stress in Mental Illnesses: A Meta-Analysis". Psychiatry Investig (Meta-analysis). 18 (7): 603–618. doi:10.30773/pi.2020.0417. PMC 8328836. PMID 34340273.
- Stilo SA, Murray RM (14 September 2019). "Non-Genetic Factors in Schizophrenia". Current Psychiatry Reports. 21 (10): 100. doi:10.1007/s11920-019-1091-3. PMC 6745031. PMID 31522306.
- Cirulli F, Musillo C, Berry A (5 February 2020). "Maternal Obesity as a Risk Factor for Brain Development and Mental Health in the Offspring". Neuroscience. 447: 122–135. doi:10.1016/j.neuroscience.2020.01.023. hdl:11573/1387747. PMID 32032668. S2CID 211029692.
- ^ Upthegrove R, Khandaker GM (2020). "Cytokines, Oxidative Stress and Cellular Markers of Inflammation in Schizophrenia" (PDF). Current Topics in Behavioral Neurosciences. 44: 49–66. doi:10.1007/7854_2018_88. ISBN 978-3-030-39140-9. PMID 31115797. S2CID 162169817.
- ^ Chiang M, Natarajan R, Fan X (February 2016). "Vitamin D in schizophrenia: a clinical review". Evidence-Based Mental Health. 19 (1): 6–9. doi:10.1136/eb-2015-102117. PMC 10699337. PMID 26767392. S2CID 206926835.
- Arias I, Sorlozano A, Villegas E, de Dios Luna J, McKenney K, Cervilla J, et al. (April 2012). "Infectious agents associated with schizophrenia: a meta-analysis". Schizophrenia Research. 136 (1–3): 128–136. doi:10.1016/j.schres.2011.10.026. hdl:10481/90076. PMID 22104141. S2CID 2687441.
- Yolken R (June 2004). "Viruses and schizophrenia: a focus on herpes simplex virus". Herpes. 11 (Suppl 2): 83A–88A. PMID 15319094.
- Khandaker GM (August 2012). "Childhood infection and adult schizophrenia: a meta-analysis of population-based studies". Schizophr. Res. 139 (1–3): 161–168. doi:10.1016/j.schres.2012.05.023. PMC 3485564. PMID 22704639.
- McGrath JJ, Lim CC, Saha S (May 2024). "Cat Ownership and Schizophrenia-Related Disorders and Psychotic-Like Experiences: A Systematic Review and Meta-Analysis". Schizophrenia Bulletin. 50 (3): 489–495. doi:10.1093/schbul/sbad168. PMC 11059805. PMID 38491934.
- ^ Pearce J, Murray C, Larkin W (July 2019). "Childhood adversity and trauma:experiences of professionals trained to routinely enquire about childhood adversity". Heliyon. 5 (7): e01900. Bibcode:2019Heliy...501900P. doi:10.1016/j.heliyon.2019.e01900. PMC 6658729. PMID 31372522.
- Dvir Y, Denietolis B, Frazier JA (October 2013). "Childhood trauma and psychosis". Child and Adolescent Psychiatric Clinics of North America. 22 (4): 629–641. doi:10.1016/j.chc.2013.04.006. PMID 24012077. S2CID 40053289.
- Misiak B, Krefft M, Bielawski T, Moustafa AA, Sąsiadek MM, Frydecka D (April 2017). "Toward a unified theory of childhood trauma and psychosis: A comprehensive review of epidemiological, clinical, neuropsychological and biological findings". Neuroscience and Biobehavioral Reviews. 75: 393–406. doi:10.1016/j.neubiorev.2017.02.015. PMID 28216171. S2CID 21614845.
- ^ Nettis MA, Pariante CM, Mondelli V (2020). "Early-Life Adversity, Systemic Inflammation and Comorbid Physical and Psychiatric Illnesses of Adult Life". Current Topics in Behavioral Neurosciences. 44: 207–225. doi:10.1007/7854_2019_89. ISBN 978-3-030-39140-9. PMID 30895531. S2CID 84842249.
- Guloksuz S, van Os J (January 2018). "The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum". Psychological Medicine. 48 (2): 229–244. doi:10.1017/S0033291717001775. PMID 28689498.
- Costa E, Silva JA, Steffen RE (November 2019). "Urban environment and psychiatric disorders: a review of the neuroscience and biology". Metabolism: Clinical and Experimental. 100S: 153940. doi:10.1016/j.metabol.2019.07.004. PMID 31610855. S2CID 204704312.
- van Os J (April 2004). "Does the urban environment cause psychosis?". The British Journal of Psychiatry. 184 (4): 287–8. doi:10.1192/bjp.184.4.287. PMID 15056569.
- Attademo L, Bernardini F, Garinella R, Compton MT (March 2017). "Environmental pollution and risk of psychotic disorders: A review of the science to date". Schizophrenia Research. 181: 55–59. doi:10.1016/j.schres.2016.10.003. PMID 27720315. S2CID 25505446.
- Selten JP, Cantor-Graae E, Kahn RS (March 2007). "Migration and schizophrenia". Current Opinion in Psychiatry. 20 (2): 111–115. doi:10.1097/YCO.0b013e328017f68e. PMID 17278906. S2CID 21391349.
- Sharma R, Agarwal A, Rohra VK, Assidi M, Abu-Elmagd M, Turki RF (April 2015). "Effects of increased paternal age on sperm quality, reproductive outcome and associated epigenetic risks to offspring". Reproductive Biology and Endocrinology. 13: 35. doi:10.1186/s12958-015-0028-x. PMC 4455614. PMID 25928123.
- ^ Gregg L, Barrowclough C, Haddock G (May 2007). "Reasons for increased substance use in psychosis". Clinical Psychology Review. 27 (4): 494–510. doi:10.1016/j.cpr.2006.09.004. PMID 17240501.
- Sagud M, Mihaljević-Peles A, Mück-Seler D, Pivac N, Vuksan-Cusa B, Brataljenović T, et al. (September 2009). "Smoking and schizophrenia". Psychiatria Danubina. 21 (3): 371–375. PMID 19794359.
- Larson M (30 March 2006). "Alcohol-Related Psychosis". EMedicine. Archived from the original on 9 November 2008. Retrieved 27 September 2006.
- Leweke FM, Koethe D (June 2008). "Cannabis and psychiatric disorders: it is not only addiction". Addiction Biology. 13 (2): 264–75. doi:10.1111/j.1369-1600.2008.00106.x. PMID 18482435. S2CID 205400285.
- ^ Khokhar JY, Henricks AM, Sullivan ED, Green AI (2018). "Unique Effects of Clozapine: A Pharmacological Perspective". Apprentices to Genius: A tribute to Solomon H. Snyder. Advances in Pharmacology. Vol. 82. pp. 137–162. doi:10.1016/bs.apha.2017.09.009. ISBN 978-0128140871. PMC 7197512. PMID 29413518.
- Bighelli I, Rodolico A, García-Mieres H, et al. (November 2021). "Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis" (PDF). Lancet Psychiatry. 8 (11): 969–980. doi:10.1016/S2215-0366(21)00243-1. PMID 34653393. S2CID 239003358.
- Patel S, Khan S, M S, Hamid P (July 2020). "The Association Between Cannabis Use and Schizophrenia: Causative or Curative? A Systematic Review". Cureus. 12 (7): e9309. doi:10.7759/cureus.9309. PMC 7442038. PMID 32839678.
- Hasan A, von Keller R, Friemel CM, Hall W, Schneider M, Koethe D, et al. (June 2020). "Cannabis use and psychosis: a review of reviews". Eur Arch Psychiatry Clin Neurosci. 270 (4): 403–412. doi:10.1007/s00406-019-01068-z. PMID 31563981. S2CID 203567900.
- "Causes — Schizophrenia". UK National Health Service. 11 November 2019. Retrieved 8 December 2021.
- Ortiz-Medina MB, Perea M, Torales J, Ventriglio A, Vitrani G, Aguilar L, et al. (November 2018). "Cannabis consumption and psychosis or schizophrenia development". The International Journal of Social Psychiatry. 64 (7): 690–704. doi:10.1177/0020764018801690. PMID 30442059. S2CID 53563635.
- Hayes D, Kyriakopoulos M (August 2018). "Dilemmas in the treatment of early-onset first-episode psychosis". Therapeutic Advances in Psychopharmacology. 8 (8): 231–239. doi:10.1177/2045125318765725. PMC 6058451. PMID 30065814.
- Cannon TD (December 2015). "How Schizophrenia Develops: Cognitive and Brain Mechanisms Underlying Onset of Psychosis". Trends Cogn Sci. 19 (12): 744–756. doi:10.1016/j.tics.2015.09.009. PMC 4673025. PMID 26493362.
- Correll CU, Schooler NR (2020). "Negative Symptoms in Schizophrenia: A Review and Clinical Guide for Recognition, Assessment, and Treatment". Neuropsychiatric Disease and Treatment. 16: 519–534. doi:10.2147/NDT.S225643. PMC 7041437. PMID 32110026.
- Howes OD (1 January 2017). "The Role of Genes, Stress, and Dopamine in the Development of Schizophrenia". Biological Psychiatry. 81 (1): 9–20. doi:10.1016/j.biopsych.2016.07.014. PMC 5675052. PMID 27720198.
- Broyd A, Balzan RP, Woodward TS, Allen P (June 2017). "Dopamine, cognitive biases and assessment of certainty: A neurocognitive model of delusions". Clinical Psychology Review. 54: 96–106. doi:10.1016/j.cpr.2017.04.006. PMID 28448827. S2CID 3729566.
- Howes OD, Murray RM (May 2014). "Schizophrenia: an integrated sociodevelopmental-cognitive model". Lancet. 383 (9929): 1677–1687. doi:10.1016/S0140-6736(13)62036-X. PMC 4127444. PMID 24315522.
- Grace AA (August 2016). "Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression". Nature Reviews. Neuroscience. 17 (8): 524–532. doi:10.1038/nrn.2016.57. PMC 5166560. PMID 27256556.
- Fusar-Poli P, Meyer-Lindenberg A (January 2013). "Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of [(18)F/(11)C]-DOPA PET studies". Schizophrenia Bulletin. 39 (1): 33–42. doi:10.1093/schbul/sbr180. PMC 3523905. PMID 22282454.
- Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, et al. (August 2012). "The nature of dopamine dysfunction in schizophrenia and what this means for treatment". Archives of General Psychiatry. 69 (8): 776–786. doi:10.1001/archgenpsychiatry.2012.169. PMC 3730746. PMID 22474070.
- Arnsten AF, Girgis RR, Gray DL, Mailman RB (January 2017). "Novel Dopamine Therapeutics for Cognitive Deficits in Schizophrenia". Biological Psychiatry. 81 (1): 67–77. doi:10.1016/j.biopsych.2015.12.028. PMC 4949134. PMID 26946382.
- Maia TV, Frank MJ (January 2017). "An Integrative Perspective on the Role of Dopamine in Schizophrenia". Biological Psychiatry. 81 (1): 52–66. doi:10.1016/j.biopsych.2016.05.021. PMC 5486232. PMID 27452791.
- ^ Pratt J, Dawson N, Morris BJ, Grent-'t-Jong T, Roux F, Uhlhaas PJ (February 2017). "Thalamo-cortical communication, glutamatergic neurotransmission and neural oscillations: A unique window into the origins of ScZ?" (PDF). Schizophrenia Research. 180: 4–12. doi:10.1016/j.schres.2016.05.013. PMID 27317361. S2CID 205075178.
- Catts VS, Lai YL, Weickert CS, Weickert TW, Catts SV (April 2016). "A quantitative review of the post-mortem evidence for decreased cortical N-methyl-D-aspartate receptor expression levels in schizophrenia: How can we link molecular abnormalities to mismatch negativity deficits?". Biological Psychology. 116: 57–67. doi:10.1016/j.biopsycho.2015.10.013. PMID 26549579.
- Michie PT, Malmierca MS, Harms L, Todd J (April 2016). "The neurobiology of MMN and implications for schizophrenia". Biological Psychology. 116: 90–97. doi:10.1016/j.biopsycho.2016.01.011. PMID 26826620. S2CID 41179430.
- ^ Marín O (January 2012). "Interneuron dysfunction in psychiatric disorders". Nature Reviews. Neuroscience. 13 (2): 107–120. doi:10.1038/nrn3155. PMID 22251963. S2CID 205507186.
- Lewis DA, Hashimoto T, Volk DW (April 2005). "Cortical inhibitory neurons and schizophrenia". Nature Reviews. Neuroscience. 6 (4): 312–324. doi:10.1038/nrn1648. PMID 15803162. S2CID 3335493.
- Senkowski D, Gallinat J (June 2015). "Dysfunctional prefrontal gamma-band oscillations reflect working memory and other cognitive deficits in schizophrenia". Biological Psychiatry. 77 (12): 1010–1019. doi:10.1016/j.biopsych.2015.02.034. PMID 25847179. S2CID 206104940.
Several studies that investigated perceptual processes found impaired GBR in ScZ patients over sensory areas, such as the auditory and visual cortex. Moreover, studies examining steady-state auditory-evoked potentials showed deficits in the gen- eration of oscillations in the gamma band.
- Reilly TJ, Nottage JF, Studerus E, Rutigliano G, Micheli AI, Fusar-Poli P, et al. (July 2018). "Gamma band oscillations in the early phase of psychosis: A systematic review". Neuroscience and Biobehavioral Reviews. 90: 381–399. doi:10.1016/j.neubiorev.2018.04.006. PMID 29656029. S2CID 4891072.
Decreased gamma power in response to a task was a relatively consistent finding, with 5 out of 6 studies reported reduced evoked or induced power.
- ^ Sloan SA, Barres BA (August 2014). "Mechanisms of astrocyte development and their contributions to neurodevelopmental disorders". Curr Opin Neurobiol. 27: 75–81. doi:10.1016/j.conb.2014.03.005. PMC 4433289. PMID 24694749.
- Lesh TA, Niendam TA, Minzenberg MJ, Carter CS (January 2011). "Cognitive control deficits in schizophrenia: mechanisms and meaning". Neuropsychopharmacology. 36 (1): 316–338. doi:10.1038/npp.2010.156. PMC 3052853. PMID 20844478.
- Barch DM, Ceaser A (January 2012). "Cognition in schizophrenia: core psychological and neural mechanisms". Trends in Cognitive Sciences. 16 (1): 27–34. doi:10.1016/j.tics.2011.11.015. PMC 3860986. PMID 22169777.
- Eisenberg DP, Berman KF (January 2010). "Executive function, neural circuitry, and genetic mechanisms in schizophrenia". Neuropsychopharmacology. 35 (1): 258–277. doi:10.1038/npp.2009.111. PMC 2794926. PMID 19693005.
- Walton E, Hibar DP, van Erp TG, Potkin SG, Roiz-Santiañez R, Crespo-Facorro B, et al. (May 2017). "Positive symptoms associate with cortical thinning in the superior temporal gyrus via the ENIGMA Schizophrenia consortium". Acta Psychiatrica Scandinavica. 135 (5): 439–447. doi:10.1111/acps.12718. PMC 5399182. PMID 28369804.
- Walton E, Hibar DP, van Erp TG, Potkin SG, Roiz-Santiañez R, Crespo-Facorro B, et al. (Karolinska Schizophrenia Project Consortium (KaSP)) (January 2018). "Prefrontal cortical thinning links to negative symptoms in schizophrenia via the ENIGMA consortium". Psychological Medicine. 48 (1): 82–94. doi:10.1017/S0033291717001283. PMC 5826665. PMID 28545597.
- Cohen AS, Minor KS (January 2010). "Emotional experience in patients with schizophrenia revisited: meta-analysis of laboratory studies". Schizophrenia Bulletin. 36 (1): 143–150. doi:10.1093/schbul/sbn061. PMC 2800132. PMID 18562345.
- Strauss GP, Gold JM (April 2012). "A new perspective on anhedonia in schizophrenia". The American Journal of Psychiatry. 169 (4): 364–373. doi:10.1176/appi.ajp.2011.11030447. PMC 3732829. PMID 22407079.
- Young J, Anticevic A, Barch D (2018). "Cognitive and Motivational Neuroscience of Psychotic Disorders". In Charney D, Buxbaum J, Sklar P, Nestler E (eds.). Charney & Nestler's Neurobiology of Mental Illness (5th ed.). New York: Oxford University Press. pp. 215, 217. ISBN 9780190681425.
Several recent reviews (e.g., Cohen and Minor, 2010) have found that individuals with schizophrenia show relatively intact self-reported emotional responses to affect-eliciting stimuli as well as other indicators of intact response(215)...Taken together, the literature increasingly suggests that there may be a deficit in putatively DA-mediated reward learning and/ or reward prediction functions in schizophrenia. Such findings suggest that impairment in striatal reward prediction mechanisms may influence "wanting" in schizophrenia in a way that reduces the ability of individuals with schizophrenia to use anticipated rewards to drive motivated behavior.(217)
- ^ Wiberg A, Ng M, Al Omran Y, Alfaro-Almagro F, McCarthy P, Marchini J, et al. (October 2019). "Handedness, language areas and neuropsychiatric diseases: insights from brain imaging and genetics". Brain. 142 (10): 2938–2947. doi:10.1093/brain/awz257. PMC 6763735. PMID 31504236.
- Tzourio-Mazoyer N, Kennedy H, Van Essen DC, Christen Y (2016). "Intra- and Inter-hemispheric Connectivity Supporting Hemispheric Specialization". Micro-, Meso- and Macro-Connectomics of the Brain. Research and Perspectives in Neurosciences. pp. 129–146. doi:10.1007/978-3-319-27777-6_9. ISBN 978-3-319-27776-9. PMID 28590670. S2CID 147813648.
- Ocklenburg S, Güntürkün O, Hugdahl K, Hirnstein M (December 2015). "Laterality and mental disorders in the postgenomic age—A closer look at schizophrenia and language lateralization". Neuroscience and Biobehavioral Reviews. 59: 100–110. doi:10.1016/j.neubiorev.2015.08.019. PMID 26598216. S2CID 15983622.
- Friston KJ, Stephan KE, Montague R, Dolan RJ (July 2014). "Computational psychiatry: the brain as a phantastic organ". The Lancet. Psychiatry. 1 (2): 148–158. doi:10.1016/S2215-0366(14)70275-5. PMID 26360579. S2CID 15504512.
- Griffin JD, Fletcher PC (May 2017). "Predictive Processing, Source Monitoring, and Psychosis". Annual Review of Clinical Psychology. 13: 265–289. doi:10.1146/annurev-clinpsy-032816-045145. PMC 5424073. PMID 28375719.
- Fletcher PC, Frith CD (January 2009). "Perceiving is believing: a Bayesian approach to explaining the positive symptoms of schizophrenia" (PDF). Nature Reviews. Neuroscience. 10 (1): 48–58. doi:10.1038/nrn2536. PMID 19050712. S2CID 6219485.
- Corlett PR, Taylor JR, Wang XJ, Fletcher PC, Krystal JH (November 2010). "Toward a neurobiology of delusions". Progress in Neurobiology. 92 (3): 345–369. doi:10.1016/j.pneurobio.2010.06.007. PMC 3676875. PMID 20558235.
- Bastos AM, Usrey WM, Adams RA, Mangun GR, Fries P, Friston KJ (November 2012). "Canonical microcircuits for predictive coding". Neuron. 76 (4): 695–711. doi:10.1016/j.neuron.2012.10.038. PMC 3777738. PMID 23177956.
- Soltan M, Girguis J (8 May 2017). "How to approach the mental state examination". BMJ. 357: j1821. doi:10.1136/sbmj.j1821. PMID 31055448. S2CID 145820368. Retrieved 9 January 2020.
- Lindenmayer JP (1 December 2017). "Are Shorter Versions of the Positive and Negative Syndrome Scale (PANSS) Doable? A Critical Review". Innovations in Clinical Neuroscience. 14 (11–12): 73–76. PMC 5788254. PMID 29410940.
- "Diagnosis of schizophrenia". Australian Department of Health. 10 January 2019. Retrieved 28 January 2020.
- "Schizophrenia – Diagnosis". UK National Health Service. 23 October 2017. Retrieved 28 January 2020.
- Jakobsen KD, Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T (2005). "Reliability of clinical ICD-10 schizophrenia diagnoses". Nordic Journal of Psychiatry. 59 (3): 209–212. doi:10.1080/08039480510027698. PMID 16195122. S2CID 24590483.
- Whitfield-Gabrieli S, Ford JM (27 April 2012). "Default Mode Network Activity and Connectivity in Psychopathology". Annual Review of Clinical Psychology. 8 (1): 49–76. doi:10.1146/annurev-clinpsy-032511-143049. ISSN 1548-5943. PMID 22224834.
- Menon V (October 2011). "Large-scale brain networks and psychopathology: a unifying triple network model". Trends in Cognitive Sciences. 15 (10): 483–506. doi:10.1016/j.tics.2011.08.003. PMID 21908230.
- Baker JT, Holmes AJ, Masters GA, Yeo BT, Krienen F, Buckner RL, et al. (1 February 2014). "Disruption of Cortical Association Networks in Schizophrenia and Psychotic Bipolar Disorder". JAMA Psychiatry. 71 (2): 109–118. doi:10.1001/jamapsychiatry.2013.3469. ISSN 2168-622X. PMC 4435541. PMID 24306091.
- ^ Richard-Devantoy S, Olie JP, Gourevitch R (December 2009). "". L'Encephale. 35 (6): 521–530. doi:10.1016/j.encep.2008.10.009. PMID 20004282.
- ^ Staedt J, Hauser M, Gudlowski Y, Stoppe G (February 2010). "Sleep disorders in schizophrenia". Fortschritte der Neurologie-Psychiatrie. 78 (2): 70–80. doi:10.1055/s-0028-1109967. PMID 20066610. S2CID 260137215.
- ^ Pocivavsek A, Rowland LM (13 January 2018). "Basic Neuroscience Illuminates Causal Relationship Between Sleep and Memory: Translating to Schizophrenia". Schizophrenia Bulletin. 44 (1): 7–14. doi:10.1093/schbul/sbx151. PMC 5768044. PMID 29136236.
- ^ Monti JM, BaHammam AS, Pandi-Perumal SR, Bromundt V, Spence DW, Cardinali DP, et al. (June 2013). "Sleep and circadian rhythm dysregulation in schizophrenia". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 43: 209–216. doi:10.1016/j.pnpbp.2012.12.021. hdl:11336/3858. PMID 23318689. S2CID 19626589.
- Faulkner SM, Bee PE, Meyer N, Dijk DJ, Drake RJ (August 2019). "Light therapies to improve sleep in intrinsic circadian rhythm sleep disorders and neuro-psychiatric illness: A systematic review and meta-analysis". Sleep Medicine Reviews. 46: 108–123. doi:10.1016/j.smrv.2019.04.012. PMID 31108433.
- Assimakopoulos K, Karaivazoglou K, Skokou M, Kalogeropoulou M, Kolios P, Gourzis P, et al. (March 2018). "Genetic Variations Associated with Sleep Disorders in Patients with Schizophrenia: A Systematic Review". Medicines. 5 (2): 27. doi:10.3390/medicines5020027. PMC 6023503. PMID 29587340.
- Dieset I, Andreassen O, Haukvik U (2016). "Somatic Comorbidity in Schizophrenia: Some Possible Biological Mechanisms Across the Life Span". Schizophrenia Bulletin. 42 (6): 1316–1319. doi:10.1093/schbul/sbw028. PMC 5049521. PMID 27033328.
- Schrimpf LA, Aggarwal A, Lauriello J (June 2018). "Psychosis". Continuum (Minneap Minn). 24 (3): 845–860. doi:10.1212/CON.0000000000000602. PMID 29851881. S2CID 243933980.
- Bottas A (15 April 2009). "Comorbidity: Schizophrenia With Obsessive-Compulsive Disorder". Psychiatric Times. 26 (4). Archived from the original on 3 April 2013.
- OConghaile A, DeLisi LE (May 2015). "Distinguishing schizophrenia from posttraumatic stress disorder with psychosis". Curr Opin Psychiatry. 28 (3): 249–255. doi:10.1097/YCO.0000000000000158. PMID 25785709. S2CID 12523516.
- Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.). Bradley's neurology in clinical practice. Vol. 1 (6th ed.). Philadelphia, PA: Elsevier/Saunders. pp. 92–111. ISBN 978-1-4377-0434-1.
- Leucht S, Bauer S, Siafis S, Hamza T, Wu H, Schneider-Thoma J, et al. (November 2021). "Examination of Dosing of Antipsychotic Drugs for Relapse Prevention in Patients With Stable Schizophrenia: A Meta-analysis". JAMA Psychiatry. 78 (11): 1238–1248. doi:10.1001/jamapsychiatry.2021.2130. PMC 8374744. PMID 34406325.
- Cannon TD, Cornblatt B, McGorry P (May 2007). "The empirical status of the ultra high-risk (prodromal) research paradigm". Schizophrenia Bulletin. 33 (3): 661–664. doi:10.1093/schbul/sbm031. PMC 2526144. PMID 17470445.
- Puntis S, Minichino A, De Crescenzo F, Cipriani A, Lennox B, Harrison R (November 2020). "Specialised early intervention teams for recent-onset psychosis". Cochrane Database Syst Rev. 11 (11): CD013288. doi:10.1002/14651858.CD013288.pub2. PMC 8092671. PMID 33135811.
p. 22: There is low-certainty evidence for the use of SEl services in comparison to TAU for a small reduction in psychiatric hospitalisation, and moderate-certainty evidence of a large effect of reduction in disengagement from mental health services. There is moderate-certainty evidence that SEI results in a small reduction of positive (hallucinations, delusions and disordered thinking) and negative symptoms (social withdrawal, flat or blunted affect, and poverty of speech) and low-certainty evidence that it greatly increases satisfaction in care, while there is low-certainty evidence that it improves general functioning and the likelihood of recovery. These effects were only observed during treatment and there was no evidence that outcomes are improved after the treatment has finished, although these were based on only one trial.
- Stafford MR, Jackson H, Mayo-Wilson E, Morrison AP, Kendall T (January 2013). "Early interventions to prevent psychosis: systematic review and meta-analysis". BMJ. 346: f185. doi:10.1136/bmj.f185. PMC 3548617. PMID 23335473.
- ^ Taylor M, Jauhar S (September 2019). "Are we getting any better at staying better? The long view on relapse and recovery in first episode nonaffective psychosis and schizophrenia". Therapeutic Advances in Psychopharmacology. 9: 204512531987003. doi:10.1177/2045125319870033. PMC 6732843. PMID 31523418.
- Weiden PJ (July 2016). "Beyond Psychopharmacology: Emerging Psychosocial Interventions for Core Symptoms of Schizophrenia". Focus (American Psychiatric Publishing). 14 (3): 315–327. doi:10.1176/appi.focus.20160014. PMC 6526802. PMID 31975812.
- McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A (March 2007). "Cognitive training for supported employment: 2–3 year outcomes of a randomized controlled trial". The American Journal of Psychiatry. 164 (3): 437–441. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- Souaiby L, Gaillard R, Krebs MO (August 2016). "". Encephale. 42 (4): 361–366. doi:10.1016/j.encep.2015.09.007. PMID 27161262.
- Fuller Torrey E (June 2015). "Deinstitutionalization and the rise of violence". CNS Spectrums. 20 (3): 207–214. doi:10.1017/S1092852914000753. PMID 25683467. S2CID 22210482.
- ^ "Schizophrenia – Treatment". UK National Health Service. 23 October 2017. Retrieved 8 January 2020.
- Ortiz-Orendain J, Covarrubias-Castillo SA, Vazquez-Alvarez AO, Castiello-de Obeso S, Arias Quiñones GE, Seegers M, et al. (December 2019). "Modafinil for people with schizophrenia or related disorders". The Cochrane Database of Systematic Reviews. 12 (12): CD008661. doi:10.1002/14651858.CD008661.pub2. PMC 6906203. PMID 31828767.
- Lally J, MacCabe JH (June 2015). "Antipsychotic medication in schizophrenia: a review". British Medical Bulletin. 114 (1): 169–179. doi:10.1093/bmb/ldv017. PMID 25957394.
- Keks N, Schwartz D, Hope J (October 2019). "Stopping and switching antipsychotic drugs". Australian Prescriber. 42 (5): 152–157. doi:10.18773/austprescr.2019.052. PMC 6787301. PMID 31631928.
- Harrow M, Jobe TH (September 2013). "Does long-term treatment of schizophrenia with antipsychotic medications facilitate recovery?". Schizophrenia Bulletin. 39 (5): 962–5. doi:10.1093/schbul/sbt034. PMC 3756791. PMID 23512950.
- Elkis H, Buckley PF (June 2016). "Treatment-Resistant Schizophrenia". The Psychiatric Clinics of North America. 39 (2): 239–65. doi:10.1016/j.psc.2016.01.006. PMID 27216902.
- Gillespie AL, Samanaite R, Mill J, Egerton A, MacCabe JH (13 January 2017). "Is treatment-resistant schizophrenia categorically distinct from treatment-responsive schizophrenia? a systematic review". BMC Psychiatry. 17 (1): 12. doi:10.1186/s12888-016-1177-y. PMC 5237235. PMID 28086761.
- Essali A, Al-Haj Haasan N, Li C, Rathbone J (January 2009). "Clozapine versus typical neuroleptic medication for schizophrenia". The Cochrane Database of Systematic Reviews. 2009 (1): CD000059. doi:10.1002/14651858.CD000059.pub2. PMC 7065592. PMID 19160174.
- Baier M (August 2010). "Insight in schizophrenia: a review". Current Psychiatry Reports. 12 (4): 356–361. doi:10.1007/s11920-010-0125-7. PMID 20526897. S2CID 29323212.
- Peters L, Krogmann A, von Hardenberg L, Bödeker K, Nöhles VB, Correll CU (November 2019). "Long-Acting Injections in Schizophrenia: a 3-Year Update on Randomized Controlled Trials Published January 2016 – March 2019". Current Psychiatry Reports. 21 (12): 124. doi:10.1007/s11920-019-1114-0. PMID 31745659. S2CID 208144438.
- Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. (June 2012). "Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis". Lancet. 379 (9831): 2063–2071. doi:10.1016/S0140-6736(12)60239-6. PMID 22560607. S2CID 2018124.
- McEvoy JP (2006). "Risks versus benefits of different types of long-acting injectable antipsychotics". The Journal of Clinical Psychiatry. 67 (Suppl 5): 15–18. PMID 16822092.
- ^ "FDA Approves Drug with New Mechanism of Action for Treatment of Schizophrenia". U.S. Food and Drug Administration (FDA) (Press release). 26 September 2024. Archived from the original on 27 September 2024. Retrieved 27 September 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "U.S. Food and Drug Administration Approves Bristol Myers Squibb's Cobenfy (xanomeline and trospium chloride), a First-In-Class Muscarinic Agonist for the Treatment of Schizophrenia in Adults" (Press release). Bristol Myers Squibb. 27 September 2024. Retrieved 27 September 2024 – via Business Wire.
- Lindenmayer JP, Nasrallah H, Pucci M, James S, Citrome L (1 July 2013). "A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities". Schizophrenia Research. 147 (2): 241–252. doi:10.1016/j.schres.2013.03.019. ISSN 0920-9964.
- Sapienza J, Martini F, Comai S, Cavallaro R, Spangaro M, De Gregorio D, et al. (18 September 2024). "Psychedelics and schizophrenia: a double-edged sword". Molecular Psychiatry: 1–14. doi:10.1038/s41380-024-02743-x. ISSN 1476-5578. PMID 39294303.
- ^ Chow CL, Kadouh NK, Bostwick JR, VandenBerg AM (June 2020). "Akathisia and Newer Second-Generation Antipsychotic Drugs: A Review of Current Evidence". Pharmacotherapy. 40 (6): 565–574. doi:10.1002/phar.2404. hdl:2027.42/155998. PMID 32342999. S2CID 216596357.
- Carbon M, Kane JM, Leucht S, Correll CU (October 2018). "Tardive dyskinesia risk with first- and second-generation antipsychotics in comparative randomized controlled trials: a meta-analysis". World Psychiatry. 17 (3): 330–340. doi:10.1002/wps.20579. PMC 6127753. PMID 30192088.
- ^ Pharoah F, Mari J, Rathbone J, Wong W (December 2010). Pharoah F (ed.). "Family intervention for schizophrenia". The Cochrane Database of Systematic Reviews. 12 (12): CD000088. doi:10.1002/14651858.CD000088.pub2. PMC 4204509. PMID 21154340.
- Bellani M, Ricciardi C, Rossetti MG, Zovetti N, Perlini C, Brambilla P (September 2019). "Cognitive remediation in schizophrenia: the earlier the better?". Epidemiology and Psychiatric Sciences. 29: e57. doi:10.1017/S2045796019000532. PMC 8061237. PMID 31556864.
- Philipp R, Kriston L, Lanio J, Kühne F, Härter M, Moritz S, et al. (March 2019). "Effectiveness of metacognitive interventions for mental disorders in adults-A systematic review and meta-analysis (METACOG)". Clinical Psychology & Psychotherapy. 26 (2): 227–240. doi:10.1002/cpp.2345. PMID 30456821. S2CID 53872643.
- Rouy M, Saliou P, Nalborczyk L, Pereira M, Roux P, Faivre N (July 2021). "Systematic review and meta-analysis of metacognitive abilities in individuals with schizophrenia spectrum disorders" (PDF). Neuroscience and Biobehavioral Reviews. 126: 329–337. doi:10.1016/j.neubiorev.2021.03.017. PMID 33757817. S2CID 232288918.
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, et al. (January 2010). "The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements". Schizophrenia Bulletin. 36 (1): 48–70. doi:10.1093/schbul/sbp115. PMC 2800143. PMID 19955389.
- Bond GR, Drake RE (June 2015). "The critical ingredients of assertive community treatment". World Psychiatry. 14 (2): 240–242. doi:10.1002/wps.20234. PMC 4471983. PMID 26043344.
- Smeerdijk M (2017). "". Tijdschrift voor Psychiatrie. 59 (8): 466–473. PMID 28880347.
- Dieterich M (6 January 2017). "Intensive case management for severe mental illness". The Cochrane Database of Systematic Reviews. 1 (1): CD007906. doi:10.1002/14651858.CD007906.pub3. PMC 6472672. PMID 28067944.
- Jauhar S, McKenna PJ, Radua J, Fung E, Salvador R, Laws KR (January 2014). "Cognitive-behavioural therapy for the symptoms of schizophrenia: systematic review and meta-analysis with examination of potential bias". The British Journal of Psychiatry (Review). 204 (1): 20–29. doi:10.1192/bjp.bp.112.116285. PMID 24385461.
- ^ Jones C, Hacker D, Meaden A, Cormac I, Irving CB, Xia J, et al. (November 2018). "Cognitive behavioural therapy plus standard care versus standard care plus other psychosocial treatments for people with schizophrenia". The Cochrane Database of Systematic Reviews. 11 (11): CD008712. doi:10.1002/14651858.CD008712.pub3. PMC 6516879. PMID 30480760.
- Health Quality Ontario (2018). "Cognitive Behavioural Therapy for Psychosis: A Health Technology Assessment". Ontario Health Technology Assessment Series. 18 (5): 1–141. PMC 6235075. PMID 30443277.
- Ruddy R, Milnes D (October 2005). "Art therapy for schizophrenia or schizophrenia-like illnesses". The Cochrane Database of Systematic Reviews (4): CD003728. doi:10.1002/14651858.CD003728.pub2. PMID 16235338. Archived from the original on 27 October 2011.
- Ruddy RA, Dent-Brown K (January 2007). "Drama therapy for schizophrenia or schizophrenia-like illnesses". The Cochrane Database of Systematic Reviews (1): CD005378. doi:10.1002/14651858.CD005378.pub2. PMID 17253555. Archived from the original on 25 August 2011.
- Galletly C, Castle D, Dark F, et al. (May 2016). "Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders". Aust N Z J Psychiatry. 50 (5): 410–472. doi:10.1177/0004867416641195. PMID 27106681. S2CID 6536743.
- Chien WT, Clifton AV, Zhao S, Lui S (4 April 2019). "Peer support for people with schizophrenia or other serious mental illness". The Cochrane Database of Systematic Reviews. 4 (6): CD010880. doi:10.1002/14651858.CD010880.pub2. PMC 6448529. PMID 30946482.
- ^ Girdler SJ, Confino JE, Woesner ME (15 February 2019). "Exercise as a Treatment for Schizophrenia: A Review". Psychopharmacology Bulletin. 49 (1): 56–69. PMC 6386427. PMID 30858639.
- ^ Firth J (1 May 2017). "Aerobic Exercise Improves Cognitive Functioning in People With Schizophrenia: A Systematic Review and Meta-Analysis". Schizophrenia Bulletin. 43 (3): 546–556. doi:10.1093/schbul/sbw115. PMC 5464163. PMID 27521348.
- Tréhout M, Dollfus S (December 2018). "". L'Encéphale. 44 (6): 538–547. doi:10.1016/j.encep.2018.05.005. PMID 29983176. S2CID 150334210.
- "Quality statement 7: Promoting healthy eating, physical activity and smoking cessation | Psychosis and schizophrenia in adults". UK National Institute for Health and Care Excellence. 12 February 2015.
- ^ Firth J, Carney R, Stubbs B, Teasdale SB, Vancampfort D, Ward PB, et al. (October 2018). "Nutritional Deficiencies and Clinical Correlates in First-Episode Psychosis: A Systematic Review and Meta-analysis". Schizophrenia Bulletin. 44 (6): 1275–1292. doi:10.1093/schbul/sbx162. PMC 6192507. PMID 29206972.
- ^ Rastogi A, Viani-Walsh D, Akbari S, Gall N, Gaughran F, Lally J (October 2020). "Pathogenesis and management of Brugada syndrome in schizophrenia: A scoping review". General Hospital Psychiatry. 67: 83–91. doi:10.1016/j.genhosppsych.2020.09.003. PMC 7537626. PMID 33065406.
- Martone G (April 2018). "Enhancement of recovery from mental illness with l-methylfolate supplementation". Perspectives in Psychiatric Care. 54 (2): 331–334. doi:10.1111/ppc.12227. PMID 28597528.
- ^ Firth J, Teasdale SB, Allott K, Siskind D, Marx W, Cotter J, et al. (October 2019). "The efficacy and safety of nutrient supplements in the treatment of mental disorders: a meta-review of meta-analyses of randomized controlled trials". World Psychiatry. 18 (3): 308–324. doi:10.1002/wps.20672. PMC 6732706. PMID 31496103.
- Kritharides L, Chow V, Lambert TJ (6 February 2017). "Cardiovascular disease in patients with schizophrenia". The Medical Journal of Australia. 206 (2): 91–95. doi:10.5694/mja16.00650. PMID 28152356. S2CID 5388097.
- Erlangsen A, Eaton WW, Mortensen PB, Conwell Y (February 2012). "Schizophrenia—a predictor of suicide during the second half of life?". Schizophrenia Research. 134 (2–3): 111–117. doi:10.1016/j.schres.2011.09.032. PMC 3266451. PMID 22018943.
- Goroll AH, Mulley AG (2011). Primary Care Medicine: Office Evaluation and Management of The Adult Patient (Sixth ed.). Lippincott Williams & Wilkins. p. Chapter 101. ISBN 978-1-4511-2159-9.
- ^ Rizvi S, Gold J, Khan AM (5 August 2019). "Role of Naltrexone in Improving Compulsive Drinking in Psychogenic Polydipsia". Cureus. 11 (8): e5320. doi:10.7759/cureus.5320. PMC 6777931. PMID 31598428.
- Seeman MV (September 2019). "Schizophrenia Mortality: Barriers to Progress". The Psychiatric Quarterly. 90 (3): 553–563. doi:10.1007/s11126-019-09645-0. PMID 31147816. S2CID 170078453.
- Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. (October 2018). "Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016". Schizophrenia Bulletin. 44 (6): 1195–1203. doi:10.1093/schbul/sby058. PMC 6192504. PMID 29762765.
- Smith T, Weston C, Lieberman J (August 2010). "Schizophrenia (maintenance treatment)". American Family Physician. 82 (4): 338–339. PMID 20704164.
- Warner R (July 2009). "Recovery from schizophrenia and the recovery model". Current Opinion in Psychiatry. 22 (4): 374–380. doi:10.1097/YCO.0b013e32832c920b. PMID 19417668. S2CID 26666000.
- Menezes NM, Arenovich T, Zipursky RB (October 2006). "A systematic review of longitudinal outcome studies of first-episode psychosis" (PDF). Psychological Medicine. 36 (10): 1349–62. doi:10.1017/S0033291706007951. PMID 16756689. S2CID 23475454. Archived from the original (PDF) on 22 September 2020.
- Coyle JT (2017). "Schizophrenia: Basic and Clinical". Neurodegenerative Diseases. Advances in Neurobiology. Vol. 15. pp. 255–280. doi:10.1007/978-3-319-57193-5_9. ISBN 978-3-319-57191-1. PMID 28674984.
- Isaac M, Chand P, Murthy P (August 2007). "Schizophrenia outcome measures in the wider international community". The British Journal of Psychiatry. Supplement. 50: s71–77. doi:10.1192/bjp.191.50.s71. PMID 18019048.
- Cohen A, Patel V, Thara R, Gureje O (March 2008). "Questioning an axiom: better prognosis for schizophrenia in the developing world?". Schizophrenia Bulletin. 34 (2): 229–244. doi:10.1093/schbul/sbm105. PMC 2632419. PMID 17905787.
- Carlborg A, Winnerbäck K, Jönsson EG, Jokinen J, Nordström P (July 2010). "Suicide in schizophrenia". Expert Review of Neurotherapeutics. 10 (7): 1153–1164. doi:10.1586/ern.10.82. PMID 20586695. S2CID 204385719.
- Tsoi DT, Porwal M, Webster AC (28 February 2013). "Interventions for smoking cessation and reduction in individuals with schizophrenia". The Cochrane Database of Systematic Reviews. 2013 (2): CD007253. doi:10.1002/14651858.CD007253.pub3. PMC 6486303. PMID 23450574.
- Sriretnakumar V, Huang E, Müller DJ (2015). "Pharmacogenetics of clozapine treatment response and side-effects in schizophrenia: an update". Expert Opinion on Drug Metabolism & Toxicology. 11 (11): 1709–1731. doi:10.1517/17425255.2015.1075003. PMID 26364648. S2CID 207492339.
- de Leon J, Diaz FJ (July 2005). "A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors". Schizophrenia Research. 76 (2–3): 135–157. doi:10.1016/j.schres.2005.02.010. PMID 15949648. S2CID 32975940.
- ^ Keltner NL, Grant JS (November 2006). "Smoke, smoke, smoke that cigarette". Perspectives in Psychiatric Care. 42 (4): 256–261. doi:10.1111/j.1744-6163.2006.00085.x. PMID 17107571.
- Kumari V, Postma P (January 2005). "Nicotine use in schizophrenia: the self medication hypotheses". Neuroscience and Biobehavioral Reviews. 29 (6): 1021–1034. doi:10.1016/j.neubiorev.2005.02.006. PMID 15964073. S2CID 15581894.
- Cai L, Huang J (2018). "Schizophrenia and risk of dementia: a meta-analysis study". Neuropsychiatr Dis Treat. 14: 2047–2055. doi:10.2147/NDT.S172933. PMC 6095111. PMID 30147318.
- Ng R, Fish S, Granholm E (30 January 2015). "Insight and theory of mind in schizophrenia". Psychiatry Research. 225 (1–2): 169–174. doi:10.1016/j.psychres.2014.11.010. PMC 4269286. PMID 25467703.
- Bora E (December 2017). "Relationship between insight and theory of mind in schizophrenia: A meta-analysis". Schizophrenia Research. 190: 11–17. doi:10.1016/j.schres.2017.03.029. PMID 28302393. S2CID 36263370.
- Darmedru C, Demily C, Franck N (April 2018). "". L'Encephale. 44 (2): 158–167. doi:10.1016/j.encep.2017.05.001. PMID 28641817.
- Richard-Devantoy S, Bouyer-Richard AI, Jollant F, Mondoloni A, Voyer M, Senon JL (August 2013). "". Revue d'Épidemiologie et de Santé Publique. 61 (4): 339–350. doi:10.1016/j.respe.2013.01.096. PMID 23816066.
- Sedgwick O, Young S, Baumeister D, Greer B, Das M, Kumari V (December 2017). "Neuropsychology and emotion processing in violent individuals with antisocial personality disorder or schizophrenia: The same or different? A systematic review and meta-analysis". The Australian and New Zealand Journal of Psychiatry. 51 (12): 1178–1197. doi:10.1177/0004867417731525. PMID 28992741. S2CID 206401875.
- Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S (July 2019). "New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis". Lancet. 394 (10194): 240–248. doi:10.1016/S0140-6736(19)30934-1. PMC 6657025. PMID 31200992.
- Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Tarrant J, et al. (March 2006). "Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study". Archives of General Psychiatry. 63 (3): 250–258. doi:10.1001/archpsyc.63.3.250. PMID 16520429.
- Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Murray RM, et al. (June 2007). "Neighbourhood variation in the incidence of psychotic disorders in Southeast London". Social Psychiatry and Psychiatric Epidemiology. 42 (6): 438–445. doi:10.1007/s00127-007-0193-0. PMID 17473901. S2CID 19655724.
- Ayuso-Mateos JL (15 August 2006). "Global burden of schizophrenia in the year 2000" (PDF). World Health Organization. Archived (PDF) from the original on 4 March 2016. Retrieved 27 February 2013.
- Heinrichs RW (2003). "Historical origins of schizophrenia: two early madmen and their illness". Journal of the History of the Behavioral Sciences. 39 (4): 349–363. doi:10.1002/jhbs.10152. PMID 14601041.
- ^ Kuhn R, Cahn CH (September 2004). "Eugen Bleuler's concepts of psychopathology". History of Psychiatry. 15 (59 Pt 3): 361–366. doi:10.1177/0957154X04044603. PMID 15386868. S2CID 5317716.
- "Schizophrenia | Definition of Schizophrenia by Lexico". Lexico Dictionaries | English. Archived from the original on 10 March 2020.
- Schneider K (1959). Clinical Psychopathology (5th ed.). New York: Grune & Stratton.
- Moore D (25 April 2008). Textbook of Clinical Neuropsychiatry (Second ed.). CRC Press. ISBN 9781444109740.
- Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, et al. (October 2013). "Definition and description of schizophrenia in the DSM-5". Schizophrenia Research. 150 (1): 3–10. doi:10.1016/j.schres.2013.05.028. PMID 23800613. S2CID 17314600.
- Picardi A (2019). "The Two Faces of First-Rank Symptoms". Psychopathology. 52 (4): 221–231. doi:10.1159/000503152. PMID 31610542. S2CID 204702486.
- Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, et al. (February 2019). "Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders". World Psychiatry. 18 (1): 3–19. doi:10.1002/wps.20611. PMC 6313247. PMID 30600616.
- "Updates to DSM-5 Criteria & Text". www.psychiatry.org. Retrieved 21 February 2019.
- Tandon R (July 2014). "Schizophrenia and Other Psychotic Disorders in Diagnostic and Statistical Manual of Mental Disorders (DSM)-5: Clinical Implications of Revisions from DSM-IV". Indian Journal of Psychological Medicine. 36 (3): 223–225. doi:10.4103/0253-7176.135365. PMC 4100404. PMID 25035542.
- ^ Lane C (5 May 2010). "How Schizophrenia Became a Black Disease: An Interview With Jonathan Metzl". Psychology Today. Retrieved 5 April 2021.
- Metz J (2010). The Protest Psychosis. Beacon Press. ISBN 978-0-8070-8592-9.
- Wilson M (March 1993). "DSM-III and the transformation of American psychiatry: a history". The American Journal of Psychiatry. 150 (3): 399–410. doi:10.1176/ajp.150.3.399. PMID 8434655.
- Fischer BA (December 2012). "A review of American psychiatry through its diagnoses: the history and development of the Diagnostic and Statistical Manual of Mental Disorders". The Journal of Nervous and Mental Disease. 200 (12): 1022–1030. doi:10.1097/NMD.0b013e318275cf19. PMID 23197117. S2CID 41939669.
- ^ Jones K (March 2000). "Insulin coma therapy in schizophrenia". Journal of the Royal Society of Medicine. 93 (3): 147–149. doi:10.1177/014107680009300313. PMC 1297956. PMID 10741319.
- Jobes DA, Chalker SA (26 September 2019). "One Size Does Not Fit All: A Comprehensive Clinical Approach to Reducing Suicidal Ideation, Attempts, and Deaths". International Journal of Environmental Research and Public Health. 16 (19): 3606. doi:10.3390/ijerph16193606. PMC 6801408. PMID 31561488.
- Ali SA, Mathur N, Malhotra AK, Braga RJ (April 2019). "Electroconvulsive Therapy and Schizophrenia: A Systematic Review". Molecular Neuropsychiatry. 5 (2): 75–83. doi:10.1159/000497376. PMC 6528094. PMID 31192220.
- Mashour GA, Walker EE, Martuza RL (June 2005). "Psychosurgery: past, present, and future". Brain Research. Brain Research Reviews. 48 (3): 409–419. doi:10.1016/j.brainresrev.2004.09.002. PMID 15914249. S2CID 10303872.
- Mendez J (1 February 2013). "Report of the Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment" (PDF). Office of the High Commissioner for Human Rights. Retrieved 22 August 2022.
- Turner T (January 2007). "Chlorpromazine: unlocking psychosis". BMJ. 334 Suppl 1 (suppl): s7. doi:10.1136/bmj.39034.609074.94. PMID 17204765. S2CID 33739419.
- Aringhieri S (December 2018). "Molecular targets of atypical antipsychotics: From mechanism of action to clinical differences". Pharmacology & Therapeutics. 192: 20–41. doi:10.1016/j.pharmthera.2018.06.012. PMID 29953902. S2CID 49602956.
- Park YS, Sang M, Jun JY, Kim SJ (2014). "Psychiatry in former socialist countries: implications for north korean psychiatry". Psychiatry Investigation. 11 (4): 363–370. doi:10.4306/pi.2014.11.4.363. ISSN 1738-3684. PMC 4225199. PMID 25395966.
- Gosden R (2001). Punishing the patient: how psychiatrists misunderstand and mistreat schizophrenia. Melbourne: Scribe Publications. ISBN 0-908011-52-0. OCLC 47177633.
- Sfera A (September 2013). "Can Psychiatry be Misused Again?". Frontiers in Psychiatry. 4: 101. doi:10.3389/fpsyt.2013.00101. PMC 3766833. PMID 24058348.
- Merskey H (15 October 1988). "IPPNW: Forum for Soviet anti-American propaganda?". CMAJ: Canadian Medical Association Journal. 139 (8): 699–700. ISSN 0820-3946. PMC 1268271.
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, et al. (September 2005). "The economic burden of schizophrenia in the United States in 2002". The Journal of Clinical Psychiatry. 66 (9): 1122–1129. doi:10.4088/jcp.v66n0906. PMID 16187769.
- McEvoy JP (2007). "The costs of schizophrenia". The Journal of Clinical Psychiatry. 68 (Suppl 14): 4–7. PMID 18284271.
- Zhang W, Amos TB, Gutkin SW, et al. (2018). "A systematic literature review of the clinical and health economic burden of schizophrenia in privately insured patients in the United States". Clinicoecon Outcomes Res. 10: 309–320. doi:10.2147/CEOR.S156308. PMC 5997131. PMID 29922078.
- Yamaguchi S, Mizuno M, Ojio Y, Sawada U, Matsunaga A, Ando S, et al. (June 2017). "Associations between renaming schizophrenia and stigma-related outcomes: A systematic review". Psychiatry and Clinical Neurosciences. 71 (6): 347–362. doi:10.1111/pcn.12510. PMID 28177184.
- Sato M (February 2006). "Renaming schizophrenia: a Japanese perspective". World Psychiatry. 5 (1): 53–55. PMC 1472254. PMID 16757998.
- Park SC, Park YC (January 2020). "Korea in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition". Journal of Korean Medical Science. 35 (2) (Fifth ed.): e6. doi:10.3346/jkms.2020.35.e6. PMC 6955430. PMID 31920014.
- Fazel S, Gulati G, Linsell L, Geddes JR, Grann M (August 2009). "Schizophrenia and violence: systematic review and meta-analysis". PLOS Medicine. 6 (8): e1000120. doi:10.1371/journal.pmed.1000120. PMC 2718581. PMID 19668362.
- Owen PR (July 2012). "Portrayals of schizophrenia by entertainment media: a content analysis of contemporary movies". Psychiatr Serv. 63 (7): 655–9. doi:10.1176/appi.ps.201100371. PMID 22555313.
- Katschnig H (October 2018). "Psychiatry's contribution to the public stereotype of schizophrenia: Historical considerations". J Eval Clin Pract. 24 (5): 1093–1100. doi:10.1111/jep.13011. PMC 6174929. PMID 30112785.
- Chen M, Lawrie S (December 2017). "Newspaper depictions of mental and physical health". BJPsych Bulletin. 41 (6): 308–313. doi:10.1192/pb.bp.116.054775. PMC 5709678. PMID 29234506.
- Dyga K, Stupak R (28 February 2018). "Ways of understanding of religious delusions associated with a change of identity on the example of identification with Jesus Christ". Psychiatria Polska. 52 (1): 69–80. doi:10.12740/PP/64378. PMID 29704415.
- Dein S, Littlewood R (July 2011). "Religion and psychosis: a common evolutionary trajectory?". Transcultural Psychiatry. 48 (3): 318–335. doi:10.1177/1363461511402723. PMID 21742955. S2CID 12991391.
- Dougall N, Maayan N, Soares-Weiser K, McDermott LM, McIntosh A (20 August 2015). "Transcranial magnetic stimulation (TMS) for schizophrenia". The Cochrane Database of Systematic Reviews. 2015 (8): CD006081. doi:10.1002/14651858.CD006081.pub2. hdl:1893/22520. PMC 9395125. PMID 26289586.
- ^ Nathou C, Etard O, Dollfus S (2019). "Auditory verbal hallucinations in schizophrenia: current perspectives in brain stimulation treatments". Neuropsychiatric Disease and Treatment. 15: 2105–2117. doi:10.2147/NDT.S168801. PMC 6662171. PMID 31413576.
- Kraguljac NV, McDonald WM, Widge AS, Rodriguez CI, Tohen M, Nemeroff CB (January 2021). "Neuroimaging Biomarkers in Schizophrenia". Am J Psychiatry. 178 (6): 509–521. doi:10.1176/appi.ajp.2020.20030340. PMC 8222104. PMID 33397140.
- Khavari B, Cairns MJ (August 2020). "Epigenomic Dysregulation in Schizophrenia: In Search of Disease Etiology and Biomarkers". Cells. 9 (8): 1837. doi:10.3390/cells9081837. PMC 7463953. PMID 32764320.
- Goldsmith DR, Crooks CL, Walker EF, Cotes RO (April 2018). "An Update on Promising Biomarkers in Schizophrenia". Focus (American Psychiatric Publishing). 16 (2): 153–163. doi:10.1176/appi.focus.20170046. PMC 6526854. PMID 31975910.
- Kumar S, Reddy PH (September 2016). "Are circulating microRNAs peripheral biomarkers for Alzheimer's disease?". Biochim Biophys Acta. 1862 (9): 1617–1627. doi:10.1016/j.bbadis.2016.06.001. PMC 5343750. PMID 27264337.
- van den Berg MM, Krauskopf J, Ramaekers JG, et al. (February 2020). "Circulating microRNAs as potential biomarkers for psychiatric and neurodegenerative disorders". Prog Neurobiol. 185: 101732. doi:10.1016/j.pneurobio.2019.101732. PMID 31816349. S2CID 208790466.
- Palaniyappan L, Liddle PF (24 April 2013). "Diagnostic Discontinuity in Psychosis: A Combined Study of Cortical Gyrification and Functional Connectivity". Schizophrenia Bulletin. 40 (3): 675–684. doi:10.1093/schbul/sbt050. ISSN 1745-1701. PMC 3984507. PMID 23615812.
External links
| Classification | D |
|---|---|
| External resources |
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
 Definitions from Wiktionary
Definitions from Wiktionary Media from Commons
Media from Commons News from Wikinews
News from Wikinews Quotations from Wikiquote
Quotations from Wikiquote Data from Wikidata
Data from Wikidata
Categories:
