| Revision as of 15:36, 18 December 2011 editWhywhenwhohow (talk | contribs)Autopatrolled, Extended confirmed users, Pending changes reviewers49,119 edits update drugbox, refs← Previous edit | Latest revision as of 08:08, 19 November 2024 edit undoWikiCleanerBot (talk | contribs)Bots926,203 editsm v2.05b - Bot T20 CW#61 - Fix errors for CW project (Reference before punctuation)Tag: WPCleaner | ||
| (342 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Medication and metabolite of cholesterol}} | |||
| {{Refimprove|date=January 2009}} | |||
| {{Use dmy dates|date=February 2020}} | |||
| '''Ursodiol''', also known as '''ursodeoxycholic acid''' and the ] '''UDCA''', is one of the secondary ]s, which are metabolic byproducts of intestinal bacteria. | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| {{Infobox drug | |||
| {{Drugbox | |||
| | verifiedrevid = 470620651 | |||
| | Verifiedfields = changed | |||
| | verifiedrevid = 425146856 | |||
| | IUPAC_name = 3α,7β-dihydroxy-5β-cholan-24-oic acid<br />OR<br />(''R'')-4-((3''R'',5''S'',7''S'',8''R'',9''S'',10''S'',13''R'',14''S'',17''R'')-3,7-dihydroxy-<br />10,13-dimethylhexadecahydro-<br />1''H''-cyclopentaphenanthren-17-yl)pentanoic acid | |||
| | image = Ursodeoxycholic acid acsv.svg | | image = Ursodeoxycholic acid acsv.svg | ||
| | width = |
| width = 250 | ||
| | alt = | |||
| | image2 = | |||
| | image2 = Ursodeoxycholic acid ball-and-stick.png | |||
| | width2 = | |||
| | width2 = 250 | |||
| | drug_name = Ursodeoxycholic acid | |||
| | alt2 = | |||
| | caption = | |||
| <!--Clinical data--> | <!-- Clinical data --> | ||
| | pronounce = | |||
| | tradename = Actigall | |||
| | tradename = Actigall, Urso, others | |||
| | Drugs.com = {{drugs.com|monograph|ursodiol}} | | Drugs.com = {{drugs.com|monograph|ursodiol}} | ||
| | licence_EU = <!-- EMEA requires brand name --> | |||
| | licence_US = Ursodiol | |||
| | pregnancy_AU = <!-- A / B1 / B2 / B3 / C / D / X --> | |||
| | pregnancy_US = B | |||
| | pregnancy_category = | |||
| | legal_AU = <!-- Unscheduled / S2 / S3 / S4 / S8 --> | |||
| | legal_CA = <!-- / Schedule I, II, III, IV, V, VI, VII, VIII --> | |||
| | legal_UK = <!-- GSL / P / POM / CD / Class A, B, C --> | |||
| | legal_US = Rx-only | |||
| | legal_status = | |||
| | dependency_liability = | |||
| | routes_of_administration = oral | |||
| | MedlinePlus = a699047 | | MedlinePlus = a699047 | ||
| | DailyMedID = |
| DailyMedID = Ursodiol | ||
| | pregnancy_AU = B3 | |||
| | pregnancy_AU_comment = <ref name="Drugs.com pregnancy">{{cite web | title=Ursodiol, Heptiza 300/150 Use During Pregnancy | website=Drugs.com | date=4 November 2019 | url=https://www.drugs.com/pregnancy/ursodiol.html | access-date=20 February 2020}}</ref> | |||
| | pregnancy_category = | |||
| | routes_of_administration = ] | |||
| | class = | |||
| | ATC_prefix = A05 | |||
| | ATC_suffix = AA02 | |||
| | ATC_supplemental = | |||
| <!-- |
<!-- Legal status --> | ||
| | |
| legal_AU = S4 | ||
| | legal_AU_comment = <ref>{{cite web | title=Prescription medicines: registration of new generic medicines and biosimilar medicines, 2017 | website=Therapeutic Goods Administration (TGA) | date=21 June 2022 | url=https://www.tga.gov.au/resources/publication/publications/prescription-medicines-registration-new-generic-medicines-and-biosimilar-medicines-2017 | access-date=30 March 2024}}</ref> | |||
| | protein_bound = | |||
| | legal_BR = <!-- OTC, A1, A2, A3, B1, B2, C1, C2, C3, C4, C5, D1, D2, E, F--> | |||
| | metabolism = | |||
| | legal_BR_comment = | |||
| | elimination_half-life = | |||
| | |
| legal_CA = Rx-only | ||
| | legal_CA_comment = <ref>{{cite web | title=Product information | website=] | date=3 August 2000 | url=https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=11967 | access-date=3 March 2024}}</ref><ref>{{cite web | title=Details for: Ursodiol C | website=] | date=25 October 2021 | url=https://dhpp.hpfb-dgpsa.ca/dhpp/resource/100493 | access-date=3 March 2024}}</ref> | |||
| | legal_DE = <!-- Anlage I, II, III or Unscheduled--> | |||
| | legal_DE_comment = | |||
| | legal_NZ = <!-- Class A, B, C --> | |||
| | legal_NZ_comment = | |||
| | legal_UK = POM | |||
| | legal_UK_comment = <ref>{{cite web | title=Ursodeoxycholic acid 300mg Tablets - Summary of Product Characteristics (SmPC) | website=(emc) | date=10 July 2019 | url=https://www.medicines.org.uk/emc/product/10064/smpc | access-date=29 April 2020}}</ref> | |||
| | legal_US = Rx-only | |||
| | legal_US_comment = <ref name="Actigall FDA label">{{cite web | title=Actigall- ursodiol capsule | website=DailyMed | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ad414461-262f-43fe-9a3d-bab300b719ed | access-date=25 September 2021}}</ref><ref>{{cite web | title=Urso 250- ursodiol tablet, film coated Urso Forte- ursodiol tablet, film coated | website=DailyMed | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e8fc4fc2-fe5c-4cba-b6e0-5ceaf2157a61 | access-date=25 September 2021}}</ref> | |||
| | legal_EU = | |||
| | legal_EU_comment = | |||
| | legal_UN = <!-- N I, II, III, IV / P I, II, III, IV--> | |||
| | legal_UN_comment = | |||
| | legal_status = Rx-only | |||
| <!-- |
<!-- Pharmacokinetic data --> | ||
| | bioavailability = | |||
| | CASNo_Ref = {{cascite|correct|CAS}} | |||
| | protein_bound = | |||
| | metabolism = | |||
| | metabolites = | |||
| | onset = | |||
| | elimination_half-life = | |||
| | duration_of_action = | |||
| | excretion = | |||
| <!-- Identifiers --> | |||
| | CAS_number_Ref = {{cascite|correct|??}} | | CAS_number_Ref = {{cascite|correct|??}} | ||
| | CAS_number = 128-13-2 | | CAS_number = 128-13-2 | ||
| | CAS_supplemental = | |||
| | ATC_prefix = A05 | |||
| | ATC_suffix = AA02 | |||
| | ATC_supplemental = | |||
| | PubChem = 31401 | | PubChem = 31401 | ||
| | IUPHAR_ligand = 7104 | |||
| | DrugBank_Ref = {{drugbankcite|changed|drugbank}} | |||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| | DrugBank = DB01586 | | DrugBank = DB01586 | ||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| Line 51: | Line 70: | ||
| | UNII_Ref = {{fdacite|correct|FDA}} | | UNII_Ref = {{fdacite|correct|FDA}} | ||
| | UNII = 724L30Y2QR | | UNII = 724L30Y2QR | ||
| | KEGG_Ref = {{keggcite| |
| KEGG_Ref = {{keggcite|correct|kegg}} | ||
| | KEGG = D00734 | | KEGG = D00734 | ||
| | ChEBI_Ref = {{ebicite| |
| ChEBI_Ref = {{ebicite|correct|EBI}} | ||
| | ChEBI = 9907 | | ChEBI = 9907 | ||
| | ChEMBL_Ref = {{ebicite|correct|EBI}} | | ChEMBL_Ref = {{ebicite|correct|EBI}} | ||
| | ChEMBL = 1551 | | ChEMBL = 1551 | ||
| | NIAID_ChemDB = | |||
| | PDB_ligand = IU5 | |||
| | synonyms = Ursodiol | |||
| <!--Chemical data--> | <!-- Chemical and physical data --> | ||
| | IUPAC_name = 3α,7β-dihydroxy-5β-cholan-24-oic acid<br />OR<br />(''R'')-4-((3''R'',5''S'',7''S'',8''R'',9''S'',10''S'',13''R'',14''S'',17''R'')-3,7-dihydroxy-<br />10,13-dimethylhexadecahydro-<br />1''H''-cyclopentaphenanthren-17-yl)pentanoic acid | |||
| | C=24 | H=40 | O=4 | |||
| | C=24 | H=40 | O=4 | |||
| | molecular_weight = 392.56 g/mol | |||
| | |
| SMILES = O=C(O)CC(1CC21(C)CC42(O)C3C(O)CC34C)C | ||
| | InChI = 1/C24H40O4/c1-14(4-7-21(27)28)17-5-6-18-22-19(9-11-24(17,18)3)23(2)10-8-16(25)12-15(23)13-20(22)26/h14-20,22,25-26H,4-13H2,1-3H3,(H,27,28)/t14-,15+,16-,17-,18+,19+,20+,22+,23+,24-/m1/s1 | |||
| | InChIKey = RUDATBOHQWOJDD-UZVSRGJWBC | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChI = 1S/C24H40O4/c1-14(4-7-21(27)28)17-5-6-18-22-19(9-11-24(17,18)3)23(2)10-8-16(25)12-15(23)13-20(22)26/h14-20,22,25-26H,4-13H2,1-3H3,(H,27,28)/t14-,15+,16-,17-,18+,19+,20+,22+,23+,24-/m1/s1 | | StdInChI = 1S/C24H40O4/c1-14(4-7-21(27)28)17-5-6-18-22-19(9-11-24(17,18)3)23(2)10-8-16(25)12-15(23)13-20(22)26/h14-20,22,25-26H,4-13H2,1-3H3,(H,27,28)/t14-,15+,16-,17-,18+,19+,20+,22+,23+,24-/m1/s1 | ||
| | StdInChI_comment = | |||
| | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChIKey = RUDATBOHQWOJDD-UZVSRGJWSA-N | | StdInChIKey = RUDATBOHQWOJDD-UZVSRGJWSA-N | ||
| | density = | |||
| | synonyms = ursodeoxycholic acid, Actigall, Ursosan, Urso, Urso Forte | |||
| | |
| density_notes = | ||
| | melting_point = 203 | | melting_point = 203 | ||
| | |
| melting_high = | ||
| | |
| melting_notes = | ||
| | boiling_point = | |||
| | specific_rotation = | |||
| | |
| boiling_notes = | ||
| | solubility = | |||
| | sol_units = | |||
| | specific_rotation = | |||
| }} | }} | ||
| '''Ursodeoxycholic acid''' ('''UDCA'''), also known as '''ursodiol''', is a secondary ], produced in humans and most other species from metabolism by intestinal bacteria. It is synthesized in the liver in some species, and was first identified in ] of genus '']'', from which its name derived.<ref name="pmid8263415">{{cite journal | vauthors = Hagey LR, Crombie DL, Espinosa E, Carey MC, Igimi H, Hofmann AF | title = Ursodeoxycholic acid in the Ursidae: biliary bile acids of bears, pandas, and related carnivores | journal = Journal of Lipid Research | volume = 34 | issue = 11 | pages = 1911–1917 | date = November 1993 | pmid = 8263415 | doi = 10.1016/S0022-2275(20)35109-9 | doi-access = free }}</ref> In purified form, it has been used to treat or prevent several diseases of the ] or ]. | |||
| ==Endogenous effects== | |||
| Primary bile acids are produced by the ] and stored in the ]. When secreted into the colon, primary bile acids can be metabolized into secondary bile acids by intestinal bacteria. Primary and secondary bile acids help the body ] ]s. Ursodeoxycholic acid helps regulate ] by reducing the rate at which the ] absorbs cholesterol molecules while breaking up ]s containing cholesterol. Because of this property, ursodeoxycholic acid is used to treat (cholesterol) ]s non-surgically. | |||
| It is available as a ].<ref>{{cite web | title=2020 First Generic Drug Approvals | website=U.S. ] (FDA) | date=23 February 2021 | url=https://www.fda.gov/drugs/first-generic-drug-approvals/2020-first-generic-drug-approvals | access-date=25 September 2021}}</ref><ref>{{cite web | title=Ursodiol: FDA-Approved Drugs | website=U.S. ] (FDA) | url=https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=205789 | access-date=25 September 2021}}</ref> | |||
| While some bile acids are known to be colon tumor promoters (e.g. deoxycholic acid), others such as ursodeoxycholic acid are thought to be chemopreventive, perhaps by inducing cellular differentiation and/or cellular senescence in colon epithelial cells.<ref>{{cite journal |author=Akare S, Jean-Louis S, Chen W, Wood DJ, Powell AA, Martinez JD |title=Ursodeoxycholic acid modulates histone acetylation and induces differentiation and senescence |journal=International Journal of Cancer. Journal International Du Cancer |volume=119 |issue=12 |pages=2958–69 |year=2006 |month=December |pmid=17019713 |doi=10.1002/ijc.22231}}</ref> | |||
| ==Medical uses== | |||
| It is believed to inhibit ].<ref name="pmid19417220">{{cite journal |author=Amaral JD, Viana RJ, Ramalho RM, Steer CJ, Rodrigues CM |title=Bile acids: regulation of apoptosis by ursodeoxycholic acid |journal=Journal of Lipid Research |volume=50 |issue=9 |pages=1721–34 |year=2009 |month=September |pmid=19417220 |doi=10.1194/jlr.R900011-JLR200 |pmc=2724780}}</ref> | |||
| UDCA has been used as medical therapy in ] disease (cholelithiasis) and for ].<ref name="PMID2672842">{{cite journal | vauthors = Hofmann AF | title = Medical dissolution of gallstones by oral bile acid therapy | journal = American Journal of Surgery | volume = 158 | issue = 3 | pages = 198–204 | date = September 1989 | pmid = 2672842 | doi = 10.1016/0002-9610(89)90252-3 }}</ref><ref>{{cite journal | vauthors = Jüngst C, Kullak-Ublick GA, Jüngst D | title = Gallstone disease: Microlithiasis and sludge | journal = Best Practice & Research. Clinical Gastroenterology | volume = 20 | issue = 6 | pages = 1053–1062 | date = 2006 | pmid = 17127187 | doi = 10.1016/j.bpg.2006.03.007 }}</ref> UDCA helps reduce the ] saturation of bile and leads to gradual dissolution of cholesterol-rich gallstones.<ref name=PMID2672842/> | |||
| UDCA may be given after bariatric surgery to prevent cholelithiasis, which commonly occurs due to the rapid weight loss producing biliary cholesterol oversaturation and also biliary dyskinesia secondary to hormonal changes.<ref>{{cite journal | vauthors = Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Chatedaki C, Sioka E, Zacharoulis D | title = Ursodeoxycholic Acid in the Prevention of Gallstone Formation After Bariatric Surgery: an Updated Systematic Review and Meta-analysis | journal = Obesity Surgery | volume = 27 | issue = 11 | pages = 3021–3030 | date = November 2017 | pmid = 28889240 | doi = 10.1007/s11695-017-2924-y | s2cid = 4622165 }}</ref> | |||
| Ursodeoxycholic acid has also been shown experimentally to suppress ] such as immune cell ]. Prolonged exposure and/or increased quantities of systemic (throughout the body, not just in the digestive system) ursodeoxycholic acid can be toxic.<ref>Material Safety Data Sheet on Ursodiol MSDS. https://fscimage.fishersci.com/msds/70916.htm</ref> | |||
| ===Primary biliary cholangitis=== | |||
| ==As a pharmaceutical== | |||
| UDCA is used as therapy in ] (PBC; previously known as primary biliary cirrhosis) where it can produce an improvement in biomarkers.<ref>{{cite journal | vauthors = Poupon RE, Balkau B, Eschwège E, Poupon R | title = A multicenter, controlled trial of ursodiol for the treatment of primary biliary cirrhosis. UDCA-PBC Study Group | journal = The New England Journal of Medicine | volume = 324 | issue = 22 | pages = 1548–1554 | date = May 1991 | pmid = 1674105 | doi = 10.1056/NEJM199105303242204 | doi-access = free }}</ref> Meta-analyses have borne out conflicting results on the mortality benefit.<ref>{{cite journal | vauthors = Goulis J, Leandro G, Burroughs AK | title = Randomised controlled trials of ursodeoxycholic-acid therapy for primary biliary cirrhosis: a meta-analysis | journal = Lancet | volume = 354 | issue = 9184 | pages = 1053–1060 | date = September 1999 | pmid = 10509495 | doi = 10.1016/S0140-6736(98)11293-X | s2cid = 25562983 }}</ref> However analyses that exclude trials of short duration (i.e. < 2 years) have demonstrated a survival benefit and are generally considered more clinically relevant.<ref>{{cite journal | vauthors = Shi J, Wu C, Lin Y, Chen YX, Zhu L, Xie WF | title = Long-term effects of mid-dose ursodeoxycholic acid in primary biliary cirrhosis: a meta-analysis of randomized controlled trials | journal = The American Journal of Gastroenterology | volume = 101 | issue = 7 | pages = 1529–1538 | date = July 2006 | pmid = 16863557 | doi = 10.1111/j.1572-0241.2006.00634.x | s2cid = 32076958 }}</ref> A Cochrane systematic review in 2012 found no significant benefit in reducing mortality, the rate of liver transplantation, ] or fatigue.<ref>{{cite journal | vauthors = Rudic JS, Poropat G, Krstic MN, Bjelakovic G, Gluud C | title = Ursodeoxycholic acid for primary biliary cirrhosis | journal = The Cochrane Database of Systematic Reviews | volume = 12 | issue = 12 | pages = CD000551 | date = December 2012 | pmid = 23235576 | pmc = 7045744 | doi = 10.1002/14651858.CD000551.pub3 }}</ref> Ursodiol and ] are FDA-approved for the treatment of primary biliary cholangitis.<ref>{{cite journal | vauthors = Bowlus CL, Kenney JT, Rice G, Navarro R | title = Primary Biliary Cholangitis: Medical and Specialty Pharmacy Management Update | journal = Journal of Managed Care & Specialty Pharmacy | volume = 22 | issue = 10-a-s Suppl | pages = S3–S15 | date = October 2016 | pmid = 27700211 | doi = 10.18553/jmcp.2016.22.10-a-s.s3 | pmc = 10408407 | doi-access = free }}</ref> | |||
| Ursodeoxycholic acid goes by the trade names '''Actigall''', '''Ursosan''', '''Egyurso'''( Egyphar Egypt), '''Urso''', and '''Urso Forte'''. In Italy and Switzerland, it is marketed under the name '''Deursil'''. In ] it is marketed in capsules of 250 mg under the name '''Coric''' by ] pharmaceutical Landsteiner Scientific. | |||
| ===Primary sclerosing cholangitis=== | |||
| Ursodeoxycholic acid can be chemically synthesized and was brought to market by the Montreal-based ] in 1998,{{Citation needed|date=January 2009}} which continues to market the drug. | |||
| UDCA use is associated with improved serum liver tests that do not always correlate with improved liver disease status.<ref>{{cite journal | vauthors = Poropat G, Giljaca V, Stimac D, Gluud C | title = Bile acids for primary sclerosing cholangitis | journal = The Cochrane Database of Systematic Reviews | volume = 2011 | issue = 1 | pages = CD003626 | date = January 2011 | pmid = 21249655 | pmc = 7163275 | doi = 10.1002/14651858.CD003626.pub2 }}</ref> WHO Drug Information advises against its use in primary sclerosing cholangitis in unapproved doses beyond 13–15 mg/kg/day.<ref>{{cite journal | journal = WHO Drug Information | volume = 26 | issue = 1 | date = 2012 | title = Ursodeoxycholic acid: serious hepatic events | url =https://www.who.int/medicines/publications/druginformation/issues/26-1.pdf }}</ref> | |||
| UDCA in a dose of 28–30 mg/kg/day increases risk of death and need for liver transplant by 2.3-fold among those with primary sclerosing cholangitis, despite decrease in liver enzymes.<ref>{{cite journal | vauthors = Lindor KD, Kowdley KV, Luketic VA, Harrison ME, McCashland T, Befeler AS, Harnois D, Jorgensen R, Petz J, Keach J, Mooney J, Sargeant C, Braaten J, Bernard T, King D, Miceli E, Schmoll J, Hoskin T, Thapa P, Enders F | title = High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis | journal = Hepatology | volume = 50 | issue = 3 | pages = 808–814 | date = September 2009 | pmid = 19585548 | pmc = 2758780 | doi = 10.1002/hep.23082 }}</ref> | |||
| The drug reduces ] absorption and is used to dissolve (cholesterol) ]s in ]s who want an alternative to ]. The drug is very expensive, however, and if the patient stops taking it, the gallstones tend to recur if the condition that gave rise to their formation does not change. For these reasons, it has not supplanted surgical treatment by ]. | |||
| ===Intrahepatic cholestasis of pregnancy=== | |||
| It is the only FDA approved drug to treat ].<ref>{{cite journal |author=Jackson H, Solaymani-Dodaran M, Card TR, Aithal GP, Logan R, West J |title=Influence of ursodeoxycholic acid on the mortality and malignancy associated with primary biliary cirrhosis: a population-based cohort study |journal=Hepatology |volume=46 |issue=4 |pages=1131–7 |year=2007 |month=October |pmid=17685473 |doi=10.1002/hep.21795}}</ref> | |||
| UDCA has been used for ]. UDCA lessens itching in the mother and may reduce the number of preterm births. Effects on fetal distress and other adverse outcomes are unlikely to be great.<ref>{{cite journal | vauthors = Walker KF, Chappell LC, Hague WM, Middleton P, Thornton JG | title = Pharmacological interventions for treating intrahepatic cholestasis of pregnancy | journal = The Cochrane Database of Systematic Reviews | volume = 2020 | issue = 7 | pages = CD000493 | date = July 2020 | pmid = 32716060 | pmc = 7389072 | doi = 10.1002/14651858.CD000493.pub3 }}</ref><ref>{{cite journal | vauthors = Chappell LC, Bell JL, Smith A, Linsell L, Juszczak E, Dixon PH, Chambers J, Hunter R, Dorling J, Williamson C, Thornton JG | title = Ursodeoxycholic acid versus placebo in women with intrahepatic cholestasis of pregnancy (PITCHES): a randomised controlled trial | journal = Lancet | volume = 394 | issue = 10201 | pages = 849–860 | date = September 2019 | pmid = 31378395 | pmc = 6739598 | doi = 10.1016/S0140-6736(19)31270-X }}</ref> | |||
| ===Cholestasis=== | |||
| A Cochrane review to evaluate if ursodeoxycholic acid has any beneficial effect in primary biliary cirrhosis patients included 16 randomized clinical trials with a total of 1447 patients. The primary outcome measures were mortality and mortality or liver transplantation. Although treatment with ursodeoxycholic acid showed a reduction in liver biochemistry, jaundice, and ascites, it did not decrease mortality or liver transplantation.<ref>{{cite journal |author=Gong Y, Huang ZB, Christensen E, Gluud C |editor1-last=Gong |editor1-first=Yan |title=Ursodeoxycholic acid for primary biliary cirrhosis |journal=Cochrane Database of Systematic Reviews |volume= |issue=3 |pages=CD000551 |year=2008 |pmid=18677775 |doi=10.1002/14651858.CD000551.pub2}}</ref> | |||
| UDCA use is not licensed in children, as its safety and effectiveness have not been established. Evidence is accumulating that ursodeoxycholic acid is ineffective, unsafe and its use is associated with significant risk of morbidity and mortality in neonatal hepatitis and neonatal cholestasis.<ref>{{cite journal | vauthors = Kotb MA | title = Review of historical cohort: ursodeoxycholic acid in extrahepatic biliary atresia | journal = Journal of Pediatric Surgery | volume = 43 | issue = 7 | pages = 1321–1327 | date = July 2008 | pmid = 18639689 | doi = 10.1016/j.jpedsurg.2007.11.043 }}</ref><ref>{{cite book |author=Paediatric Formulary Committee |title=British National Formulary for Children 2008 |publisher=Pharmaceutical Press |location=London |year=2008 |page=91 |isbn=978-0-85369-780-0}}</ref><ref>{{cite web | title = Urso package insert. | location = Birmingham, AL | publisher = Axcan Pharma U.S. | date = January 2000 | url = http://www.axcan.com/pdf/urso_patient_brochure.pdf | access-date = 25 April 2009 | archive-date = 17 October 2006 | archive-url = https://web.archive.org/web/20061017072157/http://www.axcan.com/pdf/urso_patient_brochure.pdf | url-status = dead }}</ref><ref>{{cite journal | vauthors = Kotb MA, Mosallam D, Basanti CW, El Sorogy ST, Badr AM, Abd El Baky HE, Draz IH | title = Ursodeoxycholic acid use is associated with significant risk of morbidity and mortality in infants with cholestasis: A strobe compliant study | journal = Medicine | volume = 99 | issue = 7 | pages = e18730 | date = February 2020 | pmid = 32049781 | pmc = 7035015 | doi = 10.1097/MD.0000000000018730 }}</ref> | |||
| ===Other conditions=== | |||
| In absence of biochemical response to 13-15mg/kg/day ursodeoxycholic acid, the 15 year incidence of hepatocellular carcinoma in patients with primary biliary cirrhosis is 20%.<ref name="pmid21389798">{{cite journal | |||
| UDCA has been suggested to be an adequate treatment of bile reflux ].<ref name=newprb>{{cite journal | vauthors = McCabe ME, Dilly CK | title = New Causes for the Old Problem of Bile Reflux Gastritis | journal = Clinical Gastroenterology and Hepatology | volume = 16 | issue = 9 | pages = 1389–1392 | date = September 2018 | pmid = 29505908 | doi = 10.1016/j.cgh.2018.02.034 | hdl-access = free | s2cid = 3748071 | hdl = 1805/15771 }}</ref> | |||
| | author = Kuiper EM, Hansen BE, Adang RP, van Nieuwkerk CM, Timmer R, Drenth JP, Spoelstra P, Brouwer HT, Kuyvenhoven JP, van Buuren HR | |||
| | title = Relatively high risk for hepatocellular carcinoma in patients with primary biliary cirrhosis not responding to ursodeoxycholic acid | |||
| | journal = ] | |||
| | volume = 22 | |||
| | issue = 12 | |||
| | pages = 1495–502 | |||
| | year = 2010 | |||
| | month = December | |||
| | pmid = 21389798 | |||
| | doi = 10.1097/MEG.0b013e32834059e7 | |||
| }}</ref> | |||
| In ] there is insufficient evidence to justify routine use of UDCA, especially as there is a lack of available data for long-term outcomes such as death or need for liver transplantation.<ref>{{cite journal | vauthors = Cheng K, Ashby D, Smyth RL | title = Ursodeoxycholic acid for cystic fibrosis-related liver disease | journal = The Cochrane Database of Systematic Reviews | volume = 9 | issue = 9 | pages = CD000222 | date = September 2017 | pmid = 28891588 | pmc = 6483662 | doi = 10.1002/14651858.CD000222.pub4 | collaboration = Cochrane Cystic Fibrosis and Genetic Disorders Group }}</ref> | |||
| In children, its use is not licensed, as its safety and effectiveness are not established.<ref>{{cite journal |author=Kotb MA |title=Review of historical cohort: ursodeoxycholic acid in extrahepatic biliary atresia |journal=Journal of Pediatric Surgery |volume=43 |issue=7 |pages=1321–7 |year=2008 |month=July |pmid=18639689 |doi=10.1016/j.jpedsurg.2007.11.043}}</ref><ref>{{cite book |author=Paediatric Formulary Committee |title=British National Formulary for Children 2008 |publisher=Pharmaceutical Press |location=London |year=2008 |page=91 |isbn=0-85369-780-9}}</ref><ref>Urso package insert. Birmingham, AL: Axcan Pharma U.S.; 2000 Jan.http://www.axcan.com/pdf/urso_patient_brochure.pdf</ref> | |||
| In double the recommended daily dose ursodeoxycholic acid reduces elevated liver enzyme levels in patients with primary sclerosing cholangitis, but its use was associated with an increased risk of serious adverse events (the development of cirrhosis, varices, death or liver transplantation) in patients who received ursodeoxycholic acid compared with those who received placebo). After adjustment for baseline stratification characteristics, the risk was 2.1 times greater for death,transplantation, or minimal listing criteria in patients on ursodeoxycholic acid than for those on placebo (P = 0.038). Serious adverse events, were more common in the ursodeoxycholic acid group than the placebo group (63% versus 37% )).<ref>{{cite journal |author=Lindor KD, Kowdley KV, Luketic VA, ''et al.'' |title=High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis |journal=Hepatology |volume=50 |issue=3 |pages=808–14 |year=2009 |month=September |pmid=19585548 |pmc=2758780 |doi=10.1002/hep.23082}}</ref> | |||
| UDCA has also been in effective in ], in liver bile duct-paucity syndromes. It is contraindicated in obstruction of biliary tracts such as ]. It is not effective in liver allograft rejection, and in ] involving the liver.{{medical citation needed|date=October 2023}} | |||
| Research by the ] has produced promising results in the treatment of ], both in patients who have suffered a heart attack and in foetuses, by using ursodiol to change the electrical properties of ] cells. Myofibroblasts disrupt the transmission of electrical signals controlling heart rhythm. <ref></ref> | |||
| == |
==Adverse effects== | ||
| Diarrhea was the most frequent adverse event seen in trial of UDCA in gallstone dissolution, occurring in 2 to 9%, which is less frequent than with ] therapy. Bacterial conversion of UDCA to chenodeoxycholic acid may be the mechanism for this side effect. Right upper quadrant abdominal pain and exacerbation of pruritus was occasionally reported in trials in patients with PBC.<ref name="pmid14616161">{{cite journal | vauthors = Hempfling W, Dilger K, Beuers U | title = Systematic review: ursodeoxycholic acid--adverse effects and drug interactions | journal = Alimentary Pharmacology & Therapeutics | volume = 18 | issue = 10 | pages = 963–972 | date = November 2003 | pmid = 14616161 | doi = 10.1046/j.1365-2036.2003.01792.x | s2cid = 25738560 | doi-access = free }}</ref> Additional symptoms may include bloating, weight gain, and occasionally, thinning of hair.<ref name=Lleo>{{cite journal | vauthors = Lleo A, Wang GQ, Gershwin ME, Hirschfield GM | title = Primary biliary cholangitis | journal = Lancet | volume = 396 | issue = 10266 | pages = 1915–1926 | date = December 2020 | pmid = 33308474 | doi = 10.1016/S0140-6736(20)31607-X | s2cid = 228086916 }}</ref> | |||
| The drug is generally not derived from animals.{{cn}} However, it is believed{{by whom}} more than 12,000 ]s are kept on farms in China, Vietnam and South Korea for the purpose of harvesting ursodeoxycholic acid.<ref name="BBC">{{cite news| author = Richard Black | date = 11 June 2007 | publisher = ] | url= http://news.bbc.co.uk/2/hi/science/nature/6742671.stm|title=BBC Test kit targets cruel bear trade}}</ref> Ursodeoxycholic acid is found in large quantities in bear bile.{{cn}} | |||
| ==Mechanisms of action== | |||
| ==References== | |||
| {{reflist|30em}} | |||
| == |
===Choleretic effects=== | ||
| Primary bile acids are produced by the ] and stored in the ]. When secreted into the intestine, primary bile acids can be metabolized into secondary bile acids by intestinal bacteria. Primary and secondary bile acids help the body ] ]s. Ursodeoxycholic acid helps regulate ] by reducing the rate at which the ] absorbs cholesterol molecules while breaking up ]s containing cholesterol. The drug reduces cholesterol absorption and is used to dissolve (cholesterol) ]s in ]s who want an alternative to ].<ref>{{cite journal | vauthors = Tint GS, Salen G, Shefer S | title = Effect of ursodeoxycholic acid and chenodeoxycholic acid on cholesterol and bile acid metabolism | journal = Gastroenterology | volume = 91 | issue = 4 | pages = 1007–1018 | date = October 1986 | pmid = 3527851 | doi = 10.1016/0016-5085(86)90708-0 | doi-access = free }}</ref> There are multiple mechanisms involved in cholestatic liver diseases.<ref name="PMID12198643">{{cite journal | vauthors = Paumgartner G, Beuers U | title = Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited | journal = Hepatology | volume = 36 | issue = 3 | pages = 525–531 | date = September 2002 | pmid = 12198643 | doi = 10.1053/jhep.2002.36088 | s2cid = 28282761 | doi-access = free }}</ref> | |||
| * at ] | |||
| ===Immunomodulating effects=== | |||
| Ursodeoxycholic acid has also been shown experimentally to suppress ] such as immune cell ]. Prolonged exposure and/or increased quantities of systemic (throughout the body, not just in the digestive system) ursodeoxycholic acid can be toxic.<ref>Material Safety Data Sheet on Ursodiol MSDS. https://fscimage.fishersci.com/msds/70916.htm</ref> | |||
| ===Anti-inflammatory effects=== | |||
| Ursodeoxycholic acid has been shown to exert anti-inflammatory and protective effects in human epithelial cells of the ]. It has been linked to regulation of immunoregulatory responses by regulation of ]s,<ref>{{cite journal | vauthors = Ward JB, Lajczak NK, Kelly OB, O'Dwyer AM, Giddam AK, Ní Gabhann J, Franco P, Tambuwala MM, Jefferies CA, Keely S, Roda A, Keely SJ | title = Ursodeoxycholic acid and lithocholic acid exert anti-inflammatory actions in the colon | journal = American Journal of Physiology. Gastrointestinal and Liver Physiology | volume = 312 | issue = 6 | pages = G550–G558 | date = June 2017 | pmid = 28360029 | doi = 10.1152/ajpgi.00256.2016 | doi-access = free }}</ref> antimicrobial peptides ]s,<ref>{{cite journal | vauthors = Lajczak NK, Saint-Criq V, O'Dwyer AM, Perino A, Adorini L, Schoonjans K, Keely SJ | title = Bile acids deoxycholic acid and ursodeoxycholic acid differentially regulate human β-defensin-1 and -2 secretion by colonic epithelial cells | journal = FASEB Journal | volume = 31 | issue = 9 | pages = 3848–3857 | date = September 2017 | pmid = 28487283 | doi = 10.1096/fj.201601365R | s2cid = 46877147 | doi-access = free}}</ref> and take an active part in increased restitution of wound in the colon.<ref>{{cite journal | vauthors = Mroz MS, Lajczak NK, Goggins BJ, Keely S, Keely SJ | title = The bile acids, deoxycholic acid and ursodeoxycholic acid, regulate colonic epithelial wound healing | journal = American Journal of Physiology. Gastrointestinal and Liver Physiology | volume = 314 | issue = 3 | pages = G378–G387 | date = March 2018 | pmid = 29351391 | doi = 10.1152/ajpgi.00435.2016 | s2cid = 3767047 }}</ref> Moreover, UDCA's effects has been shown to have exert actions outside the epithelial cells.<ref>{{cite journal | vauthors = O'Dwyer AM, Lajczak NK, Keyes JA, Ward JB, Greene CM, Keely SJ | title = Ursodeoxycholic acid inhibits TNFα-induced IL-8 release from monocytes | journal = American Journal of Physiology. Gastrointestinal and Liver Physiology | volume = 311 | issue = 2 | pages = G334–G341 | date = August 2016 | pmid = 27340129 | doi = 10.1152/ajpgi.00406.2015 | doi-access = free }}</ref> | |||
| While some bile acids are known to be colon tumor promoters (''e.g.'' ]), others such as ursodeoxycholic acid are thought to be ], perhaps by inducing cellular differentiation and/or cellular senescence in colon epithelial cells.<ref>{{cite journal | vauthors = Akare S, Jean-Louis S, Chen W, Wood DJ, Powell AA, Martinez JD | title = Ursodeoxycholic acid modulates histone acetylation and induces differentiation and senescence | journal = International Journal of Cancer | volume = 119 | issue = 12 | pages = 2958–2969 | date = December 2006 | pmid = 17019713 | doi = 10.1002/ijc.22231 | s2cid = 21187798 | doi-access = }}</ref> | |||
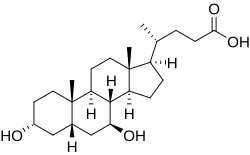
| == Chemistry == | |||
| Ursodeoxycholic acid is an ] of ], which has similar choleretic effects and a wider species distribution. However, CDCA is not as well-tolerated in humans and it does not show immunomodulating or chemoprotective effects. Both are 7-hydroxyl derivatives of deoxycholic acid, but UDCA has the group in the beta instead of the alpha orientation.<ref name="Feng"/> | |||
| === Biosynthesis === | |||
| Among mammals, only bears (]; excluding ]s) produce UDCA at useful amounts<ref name="Feng"/> (>30%). It is produced in the bear liver, but the pathway remains unknown.<ref name="pmid8263415" /> | |||
| Other vertebrates produce UDCA in much smaller amounts by gut bacteria. CDCA is oxidized into 7-oxo-CDCA then reduced into UDCA.<ref>{{cite journal | vauthors = Devlin AS, Fischbach MA | title = A biosynthetic pathway for a prominent class of microbiota-derived bile acids | journal = Nature Chemical Biology | volume = 11 | issue = 9 | pages = 685–690 | date = September 2015 | pmid = 26192599 | pmc = 4543561 | doi = 10.1038/nchembio.1864 }}</ref> | |||
| === Industrial production === | |||
| UDCA is most commonly produced from ] (CA) derived from bovine bile, a by-product of the beef industry. The current yield of this ] is about 30%.<ref>{{cite journal | vauthors = Tonin F, Arends IW | title = Latest development in the synthesis of ursodeoxycholic acid (UDCA): a critical review | journal = Beilstein Journal of Organic Chemistry | volume = 14 | pages = 470–483 | date = 2018 | pmid = 29520309 | pmc = 5827811 | doi = 10.3762/bjoc.14.33 | doi-access = free }}</ref> | |||
| == Society and culture == | |||
| ===Names=== | |||
| The term is from the Latin noun '']'' meaning bear, as ] contains the substance.<ref>https://pubchem.ncbi.nlm.nih.gov/compound/Ursodiol</ref> | |||
| Ursodeoxycholic acid can be chemically synthesized and is marketed under multiple trade names, including Ursetor, Udikast, Actibile, Actigall, Biliver, Deursil, Egyurso, Heptiza 300/150, Stener, Udcasid, Udiliv, Udinorm, Udoxyl, Urso, Urso Forte, Ursocol, Ursoliv, Ursofalk,<ref>https://prehledy.sukl.cz/prehled_leciv.html#/detail-reg/0148926</ref> Ursosan, Ursoserinox, Udimarin, and Ursonova.{{citation needed|date=February 2020}} | |||
| === History === | |||
| Bear bile, a natural source of UDCA, is used in ] since the seventh century. Japanese scientists successfully synthesized UDCA chemically in 1955.<ref name="Feng">{{cite journal | vauthors = Feng Y, Siu K, Wang N, Ng KM, Tsao SW, Nagamatsu T, Tong Y | title = Bear bile: dilemma of traditional medicinal use and animal protection | journal = Journal of Ethnobiology and Ethnomedicine | volume = 5 | issue = 1 | pages = 2 | date = January 2009 | pmid = 19138420 | pmc = 2630947 | doi = 10.1186/1746-4269-5-2 | doi-access = free }}</ref> The earliest reference to UDCA in ] dates to 1957 under an alternative spelling "ursodesoxycholic acid", in a small-scale clinical trial.<ref>{{cite journal | vauthors = Arakawa T, Kagaya A, Inaba Y | title = Ursodesoxycholic acid as in accelerator for riboflavin phosphorylation in children with nutritional dystrophy | journal = The Journal of Vitaminology | volume = 3 | issue = 3 | pages = 165–167 | date = September 1957 | pmid = 13476545 | doi = 10.5925/jnsv1954.3.165 | doi-access = free }}</ref> | |||
| Ursodeoxycholic acid (application filed by ]) was approved for use in the United States in December 1987,<ref>{{cite web | title=Actigall: FDA-Approved Drugs | website=U.S. ] (FDA) | url=https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=019594 | access-date=29 April 2020}}</ref> and was designated an ].<ref>{{cite web | title=Actigall Orphan Drug Designation and Approval | website=U.S. ] (FDA) | url=https://www.accessdata.fda.gov/scripts/opdlisting/oopd/detailedIndex.cfm?cfgridkey=55390 | access-date=29 April 2020}}</ref> | |||
| == References == | |||
| {{Reflist}} | |||
| {{Bile and liver therapy}} | {{Bile and liver therapy}} | ||
| {{Portal bar | Medicine}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Ursodeoxycholic Acid}} | |||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 08:08, 19 November 2024
Medication and metabolite of cholesterolPharmaceutical compound
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Actigall, Urso, others |
| Other names | Ursodiol |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a699047 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.437 |
| Chemical and physical data | |
| Formula | C24H40O4 |
| Molar mass | 392.580 g·mol |
| 3D model (JSmol) | |
| Melting point | 203 °C (397 °F) |
SMILES
| |
InChI
| |
| (verify) | |
Ursodeoxycholic acid (UDCA), also known as ursodiol, is a secondary bile acid, produced in humans and most other species from metabolism by intestinal bacteria. It is synthesized in the liver in some species, and was first identified in bile of bears of genus Ursus, from which its name derived. In purified form, it has been used to treat or prevent several diseases of the liver or bile ducts.
It is available as a generic medication.
Medical uses
UDCA has been used as medical therapy in gallstone disease (cholelithiasis) and for biliary sludge. UDCA helps reduce the cholesterol saturation of bile and leads to gradual dissolution of cholesterol-rich gallstones.
UDCA may be given after bariatric surgery to prevent cholelithiasis, which commonly occurs due to the rapid weight loss producing biliary cholesterol oversaturation and also biliary dyskinesia secondary to hormonal changes.
Primary biliary cholangitis
UDCA is used as therapy in primary biliary cholangitis (PBC; previously known as primary biliary cirrhosis) where it can produce an improvement in biomarkers. Meta-analyses have borne out conflicting results on the mortality benefit. However analyses that exclude trials of short duration (i.e. < 2 years) have demonstrated a survival benefit and are generally considered more clinically relevant. A Cochrane systematic review in 2012 found no significant benefit in reducing mortality, the rate of liver transplantation, pruritus or fatigue. Ursodiol and obeticholic acid are FDA-approved for the treatment of primary biliary cholangitis.
Primary sclerosing cholangitis
UDCA use is associated with improved serum liver tests that do not always correlate with improved liver disease status. WHO Drug Information advises against its use in primary sclerosing cholangitis in unapproved doses beyond 13–15 mg/kg/day.
UDCA in a dose of 28–30 mg/kg/day increases risk of death and need for liver transplant by 2.3-fold among those with primary sclerosing cholangitis, despite decrease in liver enzymes.
Intrahepatic cholestasis of pregnancy
UDCA has been used for intrahepatic cholestasis of pregnancy. UDCA lessens itching in the mother and may reduce the number of preterm births. Effects on fetal distress and other adverse outcomes are unlikely to be great.
Cholestasis
UDCA use is not licensed in children, as its safety and effectiveness have not been established. Evidence is accumulating that ursodeoxycholic acid is ineffective, unsafe and its use is associated with significant risk of morbidity and mortality in neonatal hepatitis and neonatal cholestasis.
Other conditions
UDCA has been suggested to be an adequate treatment of bile reflux gastritis.
In cystic fibrosis there is insufficient evidence to justify routine use of UDCA, especially as there is a lack of available data for long-term outcomes such as death or need for liver transplantation.
UDCA has also been in effective in non-alcoholic fatty liver disease, in liver bile duct-paucity syndromes. It is contraindicated in obstruction of biliary tracts such as biliary atresia. It is not effective in liver allograft rejection, and in Graft-versus-host disease involving the liver.
Adverse effects
Diarrhea was the most frequent adverse event seen in trial of UDCA in gallstone dissolution, occurring in 2 to 9%, which is less frequent than with chenodeoxycholic acid therapy. Bacterial conversion of UDCA to chenodeoxycholic acid may be the mechanism for this side effect. Right upper quadrant abdominal pain and exacerbation of pruritus was occasionally reported in trials in patients with PBC. Additional symptoms may include bloating, weight gain, and occasionally, thinning of hair.
Mechanisms of action
Choleretic effects
Primary bile acids are produced by the liver and stored in the gall bladder. When secreted into the intestine, primary bile acids can be metabolized into secondary bile acids by intestinal bacteria. Primary and secondary bile acids help the body digest fats. Ursodeoxycholic acid helps regulate cholesterol by reducing the rate at which the intestine absorbs cholesterol molecules while breaking up micelles containing cholesterol. The drug reduces cholesterol absorption and is used to dissolve (cholesterol) gallstones in patients who want an alternative to surgery. There are multiple mechanisms involved in cholestatic liver diseases.
Immunomodulating effects
Ursodeoxycholic acid has also been shown experimentally to suppress immune response such as immune cell phagocytosis. Prolonged exposure and/or increased quantities of systemic (throughout the body, not just in the digestive system) ursodeoxycholic acid can be toxic.
Anti-inflammatory effects
Ursodeoxycholic acid has been shown to exert anti-inflammatory and protective effects in human epithelial cells of the gastrointestinal tract. It has been linked to regulation of immunoregulatory responses by regulation of cytokines, antimicrobial peptides defensins, and take an active part in increased restitution of wound in the colon. Moreover, UDCA's effects has been shown to have exert actions outside the epithelial cells.
While some bile acids are known to be colon tumor promoters (e.g. deoxycholic acid), others such as ursodeoxycholic acid are thought to be chemopreventive, perhaps by inducing cellular differentiation and/or cellular senescence in colon epithelial cells.
Chemistry
Ursodeoxycholic acid is an epimer of chenodeoxycholic acid, which has similar choleretic effects and a wider species distribution. However, CDCA is not as well-tolerated in humans and it does not show immunomodulating or chemoprotective effects. Both are 7-hydroxyl derivatives of deoxycholic acid, but UDCA has the group in the beta instead of the alpha orientation.
Biosynthesis
Among mammals, only bears (Ursidae; excluding giant pandas) produce UDCA at useful amounts (>30%). It is produced in the bear liver, but the pathway remains unknown.
Other vertebrates produce UDCA in much smaller amounts by gut bacteria. CDCA is oxidized into 7-oxo-CDCA then reduced into UDCA.
Industrial production
UDCA is most commonly produced from cholic acid (CA) derived from bovine bile, a by-product of the beef industry. The current yield of this semisynthesis is about 30%.
Society and culture
Names
The term is from the Latin noun ursus meaning bear, as bear bile contains the substance.
Ursodeoxycholic acid can be chemically synthesized and is marketed under multiple trade names, including Ursetor, Udikast, Actibile, Actigall, Biliver, Deursil, Egyurso, Heptiza 300/150, Stener, Udcasid, Udiliv, Udinorm, Udoxyl, Urso, Urso Forte, Ursocol, Ursoliv, Ursofalk, Ursosan, Ursoserinox, Udimarin, and Ursonova.
History
Bear bile, a natural source of UDCA, is used in traditional Chinese medicine since the seventh century. Japanese scientists successfully synthesized UDCA chemically in 1955. The earliest reference to UDCA in PubMed dates to 1957 under an alternative spelling "ursodesoxycholic acid", in a small-scale clinical trial.
Ursodeoxycholic acid (application filed by Allergan) was approved for use in the United States in December 1987, and was designated an orphan drug.
References
- "Ursodiol, Heptiza 300/150 Use During Pregnancy". Drugs.com. 4 November 2019. Retrieved 20 February 2020.
- "Prescription medicines: registration of new generic medicines and biosimilar medicines, 2017". Therapeutic Goods Administration (TGA). 21 June 2022. Retrieved 30 March 2024.
- "Product information". Health Canada. 3 August 2000. Retrieved 3 March 2024.
- "Details for: Ursodiol C". Health Canada. 25 October 2021. Retrieved 3 March 2024.
- "Ursodeoxycholic acid 300mg Tablets - Summary of Product Characteristics (SmPC)". (emc). 10 July 2019. Retrieved 29 April 2020.
- "Actigall- ursodiol capsule". DailyMed. Retrieved 25 September 2021.
- "Urso 250- ursodiol tablet, film coated Urso Forte- ursodiol tablet, film coated". DailyMed. Retrieved 25 September 2021.
- ^ Hagey LR, Crombie DL, Espinosa E, Carey MC, Igimi H, Hofmann AF (November 1993). "Ursodeoxycholic acid in the Ursidae: biliary bile acids of bears, pandas, and related carnivores". Journal of Lipid Research. 34 (11): 1911–1917. doi:10.1016/S0022-2275(20)35109-9. PMID 8263415.
- "2020 First Generic Drug Approvals". U.S. Food and Drug Administration (FDA). 23 February 2021. Retrieved 25 September 2021.
- "Ursodiol: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 25 September 2021.
- ^ Hofmann AF (September 1989). "Medical dissolution of gallstones by oral bile acid therapy". American Journal of Surgery. 158 (3): 198–204. doi:10.1016/0002-9610(89)90252-3. PMID 2672842.
- Jüngst C, Kullak-Ublick GA, Jüngst D (2006). "Gallstone disease: Microlithiasis and sludge". Best Practice & Research. Clinical Gastroenterology. 20 (6): 1053–1062. doi:10.1016/j.bpg.2006.03.007. PMID 17127187.
- Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Chatedaki C, Sioka E, et al. (November 2017). "Ursodeoxycholic Acid in the Prevention of Gallstone Formation After Bariatric Surgery: an Updated Systematic Review and Meta-analysis". Obesity Surgery. 27 (11): 3021–3030. doi:10.1007/s11695-017-2924-y. PMID 28889240. S2CID 4622165.
- Poupon RE, Balkau B, Eschwège E, Poupon R (May 1991). "A multicenter, controlled trial of ursodiol for the treatment of primary biliary cirrhosis. UDCA-PBC Study Group". The New England Journal of Medicine. 324 (22): 1548–1554. doi:10.1056/NEJM199105303242204. PMID 1674105.
- Goulis J, Leandro G, Burroughs AK (September 1999). "Randomised controlled trials of ursodeoxycholic-acid therapy for primary biliary cirrhosis: a meta-analysis". Lancet. 354 (9184): 1053–1060. doi:10.1016/S0140-6736(98)11293-X. PMID 10509495. S2CID 25562983.
- Shi J, Wu C, Lin Y, Chen YX, Zhu L, Xie WF (July 2006). "Long-term effects of mid-dose ursodeoxycholic acid in primary biliary cirrhosis: a meta-analysis of randomized controlled trials". The American Journal of Gastroenterology. 101 (7): 1529–1538. doi:10.1111/j.1572-0241.2006.00634.x. PMID 16863557. S2CID 32076958.
- Rudic JS, Poropat G, Krstic MN, Bjelakovic G, Gluud C (December 2012). "Ursodeoxycholic acid for primary biliary cirrhosis". The Cochrane Database of Systematic Reviews. 12 (12): CD000551. doi:10.1002/14651858.CD000551.pub3. PMC 7045744. PMID 23235576.
- Bowlus CL, Kenney JT, Rice G, Navarro R (October 2016). "Primary Biliary Cholangitis: Medical and Specialty Pharmacy Management Update". Journal of Managed Care & Specialty Pharmacy. 22 (10-a-s Suppl): S3 – S15. doi:10.18553/jmcp.2016.22.10-a-s.s3. PMC 10408407. PMID 27700211.
- Poropat G, Giljaca V, Stimac D, Gluud C (January 2011). "Bile acids for primary sclerosing cholangitis". The Cochrane Database of Systematic Reviews. 2011 (1): CD003626. doi:10.1002/14651858.CD003626.pub2. PMC 7163275. PMID 21249655.
- "Ursodeoxycholic acid: serious hepatic events" (PDF). WHO Drug Information. 26 (1). 2012.
- Lindor KD, Kowdley KV, Luketic VA, Harrison ME, McCashland T, Befeler AS, et al. (September 2009). "High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis". Hepatology. 50 (3): 808–814. doi:10.1002/hep.23082. PMC 2758780. PMID 19585548.
- Walker KF, Chappell LC, Hague WM, Middleton P, Thornton JG (July 2020). "Pharmacological interventions for treating intrahepatic cholestasis of pregnancy". The Cochrane Database of Systematic Reviews. 2020 (7): CD000493. doi:10.1002/14651858.CD000493.pub3. PMC 7389072. PMID 32716060.
- Chappell LC, Bell JL, Smith A, Linsell L, Juszczak E, Dixon PH, et al. (September 2019). "Ursodeoxycholic acid versus placebo in women with intrahepatic cholestasis of pregnancy (PITCHES): a randomised controlled trial". Lancet. 394 (10201): 849–860. doi:10.1016/S0140-6736(19)31270-X. PMC 6739598. PMID 31378395.
- Kotb MA (July 2008). "Review of historical cohort: ursodeoxycholic acid in extrahepatic biliary atresia". Journal of Pediatric Surgery. 43 (7): 1321–1327. doi:10.1016/j.jpedsurg.2007.11.043. PMID 18639689.
- Paediatric Formulary Committee (2008). British National Formulary for Children 2008. London: Pharmaceutical Press. p. 91. ISBN 978-0-85369-780-0.
- "Urso package insert" (PDF). Birmingham, AL: Axcan Pharma U.S. January 2000. Archived from the original (PDF) on 17 October 2006. Retrieved 25 April 2009.
- Kotb MA, Mosallam D, Basanti CW, El Sorogy ST, Badr AM, Abd El Baky HE, et al. (February 2020). "Ursodeoxycholic acid use is associated with significant risk of morbidity and mortality in infants with cholestasis: A strobe compliant study". Medicine. 99 (7): e18730. doi:10.1097/MD.0000000000018730. PMC 7035015. PMID 32049781.
- McCabe ME, Dilly CK (September 2018). "New Causes for the Old Problem of Bile Reflux Gastritis". Clinical Gastroenterology and Hepatology. 16 (9): 1389–1392. doi:10.1016/j.cgh.2018.02.034. hdl:1805/15771. PMID 29505908. S2CID 3748071.
- Cheng K, Ashby D, Smyth RL, et al. (Cochrane Cystic Fibrosis and Genetic Disorders Group) (September 2017). "Ursodeoxycholic acid for cystic fibrosis-related liver disease". The Cochrane Database of Systematic Reviews. 9 (9): CD000222. doi:10.1002/14651858.CD000222.pub4. PMC 6483662. PMID 28891588.
- Hempfling W, Dilger K, Beuers U (November 2003). "Systematic review: ursodeoxycholic acid--adverse effects and drug interactions". Alimentary Pharmacology & Therapeutics. 18 (10): 963–972. doi:10.1046/j.1365-2036.2003.01792.x. PMID 14616161. S2CID 25738560.
- Lleo A, Wang GQ, Gershwin ME, Hirschfield GM (December 2020). "Primary biliary cholangitis". Lancet. 396 (10266): 1915–1926. doi:10.1016/S0140-6736(20)31607-X. PMID 33308474. S2CID 228086916.
- Tint GS, Salen G, Shefer S (October 1986). "Effect of ursodeoxycholic acid and chenodeoxycholic acid on cholesterol and bile acid metabolism". Gastroenterology. 91 (4): 1007–1018. doi:10.1016/0016-5085(86)90708-0. PMID 3527851.
- Paumgartner G, Beuers U (September 2002). "Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited". Hepatology. 36 (3): 525–531. doi:10.1053/jhep.2002.36088. PMID 12198643. S2CID 28282761.
- Material Safety Data Sheet on Ursodiol MSDS. https://fscimage.fishersci.com/msds/70916.htm
- Ward JB, Lajczak NK, Kelly OB, O'Dwyer AM, Giddam AK, Ní Gabhann J, et al. (June 2017). "Ursodeoxycholic acid and lithocholic acid exert anti-inflammatory actions in the colon". American Journal of Physiology. Gastrointestinal and Liver Physiology. 312 (6): G550 – G558. doi:10.1152/ajpgi.00256.2016. PMID 28360029.
- Lajczak NK, Saint-Criq V, O'Dwyer AM, Perino A, Adorini L, Schoonjans K, et al. (September 2017). "Bile acids deoxycholic acid and ursodeoxycholic acid differentially regulate human β-defensin-1 and -2 secretion by colonic epithelial cells". FASEB Journal. 31 (9): 3848–3857. doi:10.1096/fj.201601365R. PMID 28487283. S2CID 46877147.
- Mroz MS, Lajczak NK, Goggins BJ, Keely S, Keely SJ (March 2018). "The bile acids, deoxycholic acid and ursodeoxycholic acid, regulate colonic epithelial wound healing". American Journal of Physiology. Gastrointestinal and Liver Physiology. 314 (3): G378 – G387. doi:10.1152/ajpgi.00435.2016. PMID 29351391. S2CID 3767047.
- O'Dwyer AM, Lajczak NK, Keyes JA, Ward JB, Greene CM, Keely SJ (August 2016). "Ursodeoxycholic acid inhibits TNFα-induced IL-8 release from monocytes". American Journal of Physiology. Gastrointestinal and Liver Physiology. 311 (2): G334 – G341. doi:10.1152/ajpgi.00406.2015. PMID 27340129.
- Akare S, Jean-Louis S, Chen W, Wood DJ, Powell AA, Martinez JD (December 2006). "Ursodeoxycholic acid modulates histone acetylation and induces differentiation and senescence". International Journal of Cancer. 119 (12): 2958–2969. doi:10.1002/ijc.22231. PMID 17019713. S2CID 21187798.
- ^ Feng Y, Siu K, Wang N, Ng KM, Tsao SW, Nagamatsu T, et al. (January 2009). "Bear bile: dilemma of traditional medicinal use and animal protection". Journal of Ethnobiology and Ethnomedicine. 5 (1): 2. doi:10.1186/1746-4269-5-2. PMC 2630947. PMID 19138420.
- Devlin AS, Fischbach MA (September 2015). "A biosynthetic pathway for a prominent class of microbiota-derived bile acids". Nature Chemical Biology. 11 (9): 685–690. doi:10.1038/nchembio.1864. PMC 4543561. PMID 26192599.
- Tonin F, Arends IW (2018). "Latest development in the synthesis of ursodeoxycholic acid (UDCA): a critical review". Beilstein Journal of Organic Chemistry. 14: 470–483. doi:10.3762/bjoc.14.33. PMC 5827811. PMID 29520309.
- https://pubchem.ncbi.nlm.nih.gov/compound/Ursodiol
- https://prehledy.sukl.cz/prehled_leciv.html#/detail-reg/0148926
- Arakawa T, Kagaya A, Inaba Y (September 1957). "Ursodesoxycholic acid as in accelerator for riboflavin phosphorylation in children with nutritional dystrophy". The Journal of Vitaminology. 3 (3): 165–167. doi:10.5925/jnsv1954.3.165. PMID 13476545.
- "Actigall: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 29 April 2020.
- "Actigall Orphan Drug Designation and Approval". U.S. Food and Drug Administration (FDA). Retrieved 29 April 2020.
| Bile and liver therapy (A05) | |
|---|---|
| Bile therapy | |
| Liver therapy | |