| Revision as of 01:21, 29 September 2016 editChaya5260 (talk | contribs)Extended confirmed users2,727 edits describing source of driver mutations← Previous edit | Latest revision as of 22:49, 25 April 2024 edit undoCoolieCoolster (talk | contribs)Extended confirmed users49,705 editsm Added non-breaking space to non-template file size, frequency, bitrate, and bandwidth values (via WP:JWB) | ||
| (100 intermediate revisions by 52 users not shown) | |||
| Line 1: | Line 1: | ||
| {{short description|Sub-field of genomics}} | |||
| {{Redirect|Genetics in cancer|inheritable genetic syndromes predisposing affected individuals to cancer|Hereditary cancer syndrome}} | |||
| '''Oncogenomics''' is a sub-field of ] that characterizes ]-associated ]s. It focuses on genomic, epigenomic and transcript alterations in cancer. | '''Oncogenomics''' is a sub-field of ] that characterizes ]-associated ]s. It focuses on genomic, epigenomic and transcript alterations in cancer. | ||
| ] is a genetic disease caused by accumulation of ] |
] is a genetic disease caused by accumulation of ]s and ] alterations leading to unrestrained cell proliferation and ] formation. The goal of oncogenomics is to identify new ] or ] that may provide new insights into cancer diagnosis, predicting clinical outcome of cancers and new targets for cancer therapies. The success of targeted cancer therapies such as ], ] and ] raised the hope for oncogenomics to elucidate new targets for cancer treatment.<ref name="Strausberg2004">{{cite journal | vauthors = Strausberg RL, Simpson AJ, Old LJ, Riggins GJ | title = Oncogenomics and the development of new cancer therapies | journal = Nature | volume = 429 | issue = 6990 | pages = 469–74 | date = May 2004 | pmid = 15164073 | doi = 10.1038/nature02627 | bibcode = 2004Natur.429..469S | s2cid = 37628107 }}</ref> | ||
| ] | ] | ||
| Besides understanding the underlying genetic mechanisms that initiate or drive cancer progression, oncogenomics targets personalized cancer treatment. Cancer develops due to DNA mutations that accumulate randomly. Identifying and targeting the mutations in an individual patient may lead to increased treatment efficacy. | Besides understanding the underlying genetic mechanisms that initiate or drive cancer progression, oncogenomics targets personalized cancer treatment. Cancer develops due to ] and epigenetic alterations that accumulate randomly. Identifying and targeting the mutations in an individual patient may lead to increased treatment efficacy. | ||
| The completion of the ] facilitated the field of oncogenomics and increased the abilities of researchers to find oncogenes. Sequencing technologies have been applied to the study of oncogenomics. | The completion of the ] facilitated the field of oncogenomics and increased the abilities of researchers to find oncogenes. Sequencing technologies and global methylation profiling techniques have been applied to the study of oncogenomics. | ||
| ==History== | ==History== | ||
| The genomics era began in the 1990s, with the generation of DNA sequences of many organisms. In the 21st century, the completion of the ] enabled the study of functional genomics and examining tumor genomes. Cancer is a main focus. | The genomics era began in the 1990s, with the generation of DNA sequences of many organisms. In the 21st century, the completion of the ] enabled the study of functional genomics and examining tumor genomes. Cancer is a main focus. | ||
| The epigenomics era largely began more recently, about 2000.<ref name="pmid17158741">{{cite journal |vauthors=Ting AH, McGarvey KM, Baylin SB |title=The cancer |
The epigenomics era largely began more recently, about 2000.<ref name="pmid17158741">{{cite journal|author-link3=Stephen B. Baylin |vauthors=Ting AH, McGarvey KM, Baylin SB |title=The cancer epigenome—components and functional correlates |journal=Genes Dev. |volume=20 |issue=23 |pages=3215–31 |year=2006 |pmid=17158741 |doi=10.1101/gad.1464906 |doi-access=free }}</ref><ref name="pmid17320506">{{cite journal |vauthors=Jones PA, Baylin SB |title=The epigenomics of cancer |journal=Cell |volume=128 |issue=4 |pages=683–92 |year=2007 |pmid=17320506 |pmc=3894624 |doi=10.1016/j.cell.2007.01.029 }}</ref> One major source of epigenetic change is altered methylation of ] at the ] region of genes (see ]). A number of recently devised methods can assess the DNA methylation status in cancers versus normal tissues.<ref name="pmid25448294">{{cite journal |vauthors=Li D, Zhang B, Xing X, Wang T |title=Combining MeDIP-seq and MRE-seq to investigate genome-wide CpG methylation |journal=Methods |volume=72 |pages=29–40 |year=2015 |pmid=25448294 |pmc=4300244 |doi=10.1016/j.ymeth.2014.10.032 }}</ref> Some methods assess methylation of CpGs located in different classes of loci, including CpG islands, shores, and shelves as well as promoters, gene bodies, and intergenic regions.<ref name="pmid27493446">{{cite journal |vauthors=Wei J, Li G, Dang S, Zhou Y, Zeng K, Liu M |title=Discovery and Validation of Hypermethylated Markers for Colorectal Cancer |journal=Dis. Markers |volume=2016 |pages=2192853 |year=2016 |pmid=27493446 |pmc=4963574 |doi=10.1155/2016/2192853 |doi-access=free }}</ref> Cancer is also a major focus of epigenetic studies. | ||
| Access to whole ] is important to cancer (or cancer genome) research because: | Access to whole ] is important to cancer (or cancer genome) research because: | ||
| *Mutations are the immediate cause of cancer and define the tumor ]. | * Mutations are the immediate cause of cancer and define the tumor ]. | ||
| *Access to cancerous and normal tissue samples from the same patient and the fact that most cancer mutations represent ] events, allow the identification of cancer-specific mutations. | * Access to cancerous and normal tissue samples from the same patient and the fact that most cancer mutations represent ] events, allow the identification of cancer-specific mutations. | ||
| *Cancer mutations are cumulative and sometimes are related to disease stage. ] and drug resistance are distinguishable.<ref name="overview">{{cite journal| |
* Cancer mutations are cumulative and sometimes are related to disease stage. ] and drug resistance are distinguishable.<ref name="overview">{{cite journal | vauthors = Strausberg RL, Simpson AJ | title = Whole-genome cancer analysis as an approach to deeper understanding of tumour biology | journal = Br. J. Cancer | volume = 102 | issue = 2 | pages = 243–8 | date = January 2010 | pmid = 20029419 | pmc = 2816661 | doi = 10.1038/sj.bjc.6605497 }}</ref> | ||
| Access to methylation profiling is important to cancer research because: | Access to methylation profiling is important to cancer research because: | ||
| *Epi-drivers, along with Mut-drivers, can act as immediate causes of cancers<ref name="pmid23539594">{{cite journal |vauthors=Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW |title=Cancer genome landscapes |journal=Science |volume=339 |issue=6127 |pages=1546–58 |year=2013 |pmid=23539594 |pmc=3749880 |doi=10.1126/science.1235122 | |
* Epi-drivers, along with Mut-drivers, can act as immediate causes of cancers<ref name="pmid23539594">{{cite journal |vauthors=Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW |title=Cancer genome landscapes |journal=Science |volume=339 |issue=6127 |pages=1546–58 |year=2013 |pmid=23539594 |pmc=3749880 |doi=10.1126/science.1235122 |bibcode=2013Sci...339.1546V }}</ref> | ||
| *Cancer epimutations are cumulative and sometimes related to disease stage<ref name="pmid24793120">{{cite journal |vauthors=Luo Y, Wong CJ, Kaz AM, Dzieciatkowski S, Carter KT, Morris SM, Wang J, Willis JE, Makar KW, Ulrich CM, Lutterbaugh JD, Shrubsole MJ, Zheng W, Markowitz SD, Grady WM |title=Differences in DNA methylation signatures reveal multiple pathways of progression from adenoma to colorectal cancer |journal=Gastroenterology |volume=147 |issue=2 |pages=418–29.e8 |year=2014 |pmid=24793120 |pmc=4107146 |doi=10.1053/j.gastro.2014.04.039 |
* Cancer epimutations are cumulative and sometimes related to disease stage<ref name="pmid24793120">{{cite journal |vauthors=Luo Y, Wong CJ, Kaz AM, Dzieciatkowski S, Carter KT, Morris SM, Wang J, Willis JE, Makar KW, Ulrich CM, Lutterbaugh JD, Shrubsole MJ, Zheng W, Markowitz SD, Grady WM |title=Differences in DNA methylation signatures reveal multiple pathways of progression from adenoma to colorectal cancer |journal=Gastroenterology |volume=147 |issue=2 |pages=418–29.e8 |year=2014 |pmid=24793120 |pmc=4107146 |doi=10.1053/j.gastro.2014.04.039 }}</ref> | ||
| === Whole genome sequencing === | === Whole genome sequencing === | ||
| The first cancer genome was sequenced in 2008.<ref name="overview" /> This study sequenced a typical ] (AML) genome and its normal counterpart genome obtained from the same patient. The comparison revealed ten mutated genes. Two were already thought to contribute to tumor progression: an internal tandem duplication of the ] receptor ] gene, which activates kinase signaling and is associated with a poor prognosis and a four base insertion in exon 12 of the ] gene (NPMc). These mutations are found in |
The first cancer genome was sequenced in 2008.<ref name="overview" /> This study sequenced a typical ] (AML) genome and its normal counterpart genome obtained from the same patient. The comparison revealed ten mutated genes. Two were already thought to contribute to tumor progression: an internal tandem duplication of the ] receptor ] gene, which activates kinase signaling and is associated with a poor prognosis and a four base insertion in exon 12 of the ] gene (NPMc). These mutations are found in 25–30% of AML tumors and are thought to contribute to disease progression rather than to cause it directly. | ||
| The remaining 8 were new mutations and all were single base changes: Four were in families that are strongly associated with cancer pathogenesis (], CDH24, ] and ]). The other four had no previous association with cancer pathogenesis. They did have potential functions in ]s that suggested mechanisms by which they could act to promote cancer (KNDC1, ], EB12, GRINC1B) | The remaining 8 were new mutations and all were single base changes: Four were in families that are strongly associated with cancer pathogenesis (], CDH24, ] and ]). The other four had no previous association with cancer pathogenesis. They did have potential functions in ]s that suggested mechanisms by which they could act to promote cancer (KNDC1, ], EB12, GRINC1B) | ||
| These genes are involved in pathways known to contribute to cancer pathogenesis, but before this study most would not have been candidates for targeted gene therapy. This analysis validated the approach of whole ] in identifying somatic mutations and the importance of parallel sequencing of normal and tumor cell genomes.<ref>{{cite journal | |
These genes are involved in pathways known to contribute to cancer pathogenesis, but before this study most would not have been candidates for targeted gene therapy. This analysis validated the approach of whole ] in identifying somatic mutations and the importance of parallel sequencing of normal and tumor cell genomes.<ref name="pmid18987736">{{cite journal | vauthors = Ley TJ, Mardis ER, Ding L, Fulton B, McLellan MD, Chen K, Dooling D, Dunford-Shore BH, McGrath S, Hickenbotham M, Cook L, Abbott R, Larson DE, Koboldt DC, Pohl C, Smith S, Hawkins A, Abbott S, Locke D, Hillier LW, Miner T, Fulton L, Magrini V, Wylie T, Glasscock J, Conyers J, Sander N, Shi X, Osborne JR, Minx P, Gordon D, Chinwalla A, Zhao Y, Ries RE, Payton JE, Westervelt P, Tomasson MH, Watson M, Baty J, Ivanovich J, Heath S, Shannon WD, Nagarajan R, Walter MJ, Link DC, Graubert TA, DiPersio JF, Wilson RK|display-authors = 6 | title = DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome | journal = Nature | volume = 456 | issue = 7218 | pages = 66–72 | date = November 2008 | pmid = 18987736 | pmc = 2603574 | doi = 10.1038/nature07485 |bibcode=2008Natur.456...66L }}</ref> | ||
| In 2011, the genome of an exceptional bladder cancer patient whose tumor had been eliminated by the drug ] was sequenced, revealing mutations in two genes, '']'' and '']''. The mutations disregulated ], the protein inhibited by everolimus, allowing it to reproduce without limit. As a result, in 2015, the Exceptional Responders Initiative was created at the National Cancer Institute. The initiative allows such exceptional patients (who have responded positively for at least six months to a cancer drug that usually fails) to have their genomes sequenced to identify the relevant mutations. Once identified, other patients could be screened for those mutations and then be given the drug. In 2016 To that end, a nationwide cancer drug trial began in 2015, involving up to twenty-four hundred centers. Patients with appropriate mutations are matched with one of more than forty drugs.<ref name=":0">{{Cite web|url=http://www.popularmechanics.com/science/health/a17577/exceptional-breakthrough-awards-2015/|title=What Miraculous Recoveries Tell Us About Beating Cancer|last=Peikoff|first=Kira|date=2015-10-16|website=Popular Mechanics|access-date=2016-04-28}}</ref> | In 2011, the genome of an exceptional bladder cancer patient whose tumor had been eliminated by the drug ] was sequenced, revealing mutations in two genes, '']'' and '']''. The mutations disregulated ], the protein inhibited by everolimus, allowing it to reproduce without limit. As a result, in 2015, the Exceptional Responders Initiative was created at the National Cancer Institute. The initiative allows such exceptional patients (who have responded positively for at least six months to a cancer drug that usually fails) to have their genomes sequenced to identify the relevant mutations. Once identified, other patients could be screened for those mutations and then be given the drug. In 2016 To that end, a nationwide cancer drug trial began in 2015, involving up to twenty-four hundred centers. Patients with appropriate mutations are matched with one of more than forty drugs.<ref name=":0">{{Cite web|url=http://www.popularmechanics.com/science/health/a17577/exceptional-breakthrough-awards-2015/|title=What Miraculous Recoveries Tell Us About Beating Cancer|last=Peikoff|first=Kira|date=2015-10-16|website=Popular Mechanics|access-date=2016-04-28}}</ref> | ||
| Line 39: | Line 41: | ||
| ===Genome sequencing=== | ===Genome sequencing=== | ||
| {{Further|Cancer genome sequencing}} | {{Further|Cancer genome sequencing}} | ||
| * '']'': ]-based sequencers offer a relatively low-cost method to generate sequence data.<ref name=Strausberg2004 /><ref>{{cite journal |author1=Bardelli A. |author2=Velculescu V.E. | year = 2005 | title = Mutational analysis of gene families in human cancer |
* '']'': ]-based sequencers offer a relatively low-cost method to generate sequence data.<ref name=Strausberg2004 /><ref>{{cite journal|author1-link=Alberto Bardelli|author1=Bardelli A. |author2=Velculescu V.E. | year = 2005 | title = Mutational analysis of gene families in human cancer | journal = Current Opinion in Genetics & Development | volume = 15 | issue = 1| pages = 5–12 | doi = 10.1016/j.gde.2004.12.009 |pmid=15661527 }}</ref><ref>{{cite journal |author1=Benvenuti S. |author2=Arena S. |author3=Bardelli A. | year = 2005 | title = Identification of cancer genes by mutational profiling of tumor genomes | journal = FEBS Letters | volume = 579 | issue = 8| pages = 1884–1890 | doi = 10.1016/j.febslet.2005.02.015 | pmid = 15763568 |s2cid=31708201 | doi-access = }}</ref> | ||
| * '']'': This technique measures the ] differences between normal and cancer genomes. It uses the fluorescence intensity from fluorescent-labeled samples, which are hybridized to known probes on a microarray.<ref>{{cite journal |author1=Shih I.M. |author2=Wang T.L. | year = 2005 | title = Apply innovative technologies to explore cancer genome |
* '']'': This technique measures the ] differences between normal and cancer genomes. It uses the fluorescence intensity from fluorescent-labeled samples, which are hybridized to known probes on a microarray.<ref>{{cite journal |author1=Shih I.M. |author2=Wang T.L. | year = 2005 | title = Apply innovative technologies to explore cancer genome | journal = Current Opinion in Oncology | volume = 17 | issue = 1| pages = 33–38 | doi = 10.1097/01.cco.0000147382.97085.e4 | pmid = 15608510 |s2cid=39104975 }}</ref><ref name="pmid14672980">{{cite journal | vauthors = Greshock J, Naylor TL, Margolin A, Diskin S, Cleaver SH, Futreal PA, deJong PJ, Zhao S, Liebman M, Weber BL|display-authors = 6 | title = 1-Mb resolution array-based comparative genomic hybridization using a BAC clone set optimized for cancer gene analysis | journal = Genome Res. | volume = 14 | issue = 1 | pages = 179–87 | date = January 2004 | pmid = 14672980 | pmc = 314295 | doi = 10.1101/gr.1847304 }}</ref> | ||
| * ''Representational ] ] analysis'': Detects copy number variation using amplified restriction-digested genomic fragments that are hybridized to human oligonucleotides, achieving a resolution between 30 and 35 |
* ''Representational ] ] analysis'': Detects copy number variation using amplified restriction-digested genomic fragments that are hybridized to human oligonucleotides, achieving a resolution between 30 and 35 kbit/s.<ref name="pmid12975311">{{cite journal | vauthors = Lucito R, Healy J, Alexander J, Reiner A, Esposito D, Chi M, Rodgers L, Brady A, Sebat J, Troge J, West JA, Rostan S, Nguyen KC, Powers S, Ye KQ, Olshen A, Venkatraman E, Norton L, Wigler M |display-authors = 6| title = Representational oligonucleotide microarray analysis: a high-resolution method to detect genome copy number variation | journal = Genome Res. | volume = 13 | issue = 10 | pages = 2291–305 | date = October 2003 | pmid = 12975311 | pmc = 403708 | doi = 10.1101/gr.1349003 }}</ref> | ||
| * ''Digital ]'': Detects copy number variation using genomics tags obtained via ] digests. These tags are then linked to into ditags, concatenated, cloned, sequenced and mapped back to the ] to evaluate tag density.<ref>{{cite journal | |
* ''Digital ]'': Detects copy number variation using genomics tags obtained via ] digests. These tags are then linked to into ditags, concatenated, cloned, sequenced and mapped back to the ] to evaluate tag density.<ref name="pmid17406428">{{cite journal | vauthors = Hu M, Yao J, Polyak K | title = Methylation-specific digital karyotyping | journal = Nat Protoc | volume = 1 | issue = 3 | pages = 1621–36 | date = 2006 | pmid = 17406428 | doi = 10.1038/nprot.2006.278 | s2cid = 10554933 }}</ref><ref name="pmid17314512">{{cite journal | vauthors = Körner H, Epanchintsev A, Berking C, Schuler-Thurner B, Speicher MR, Menssen A, Hermeking H | title = Digital karyotyping reveals frequent inactivation of the dystrophin/DMD gene in malignant melanoma | journal = Cell Cycle | volume = 6 | issue = 2 | pages = 189–98 | date = January 2007 | pmid = 17314512 | doi = 10.4161/cc.6.2.3733 | doi-access = free }}</ref> | ||
| * ''] (BAC)-end sequencing (])'': Identifies ] breakpoints by generating a BAC library from a cancer genome and sequencing their ends. The BAC clones that contain chromosome aberrations have end sequences that do not map to a similar region of the reference genome, thus identifying a chromosomal breakpoint.<ref>{{cite journal | |
* ''] (BAC)-end sequencing (])'': Identifies ] breakpoints by generating a BAC library from a cancer genome and sequencing their ends. The BAC clones that contain chromosome aberrations have end sequences that do not map to a similar region of the reference genome, thus identifying a chromosomal breakpoint.<ref name="pmid12788976">{{cite journal | vauthors = Volik S, Zhao S, Chin K, Brebner JH, Herndon DR, Tao Q, Kowbel D, Huang G, Lapuk A, Kuo WL, Magrane G, De Jong P, Gray JW, Collins C|display-authors = 6 | title = End-sequence profiling: sequence-based analysis of aberrant genomes | journal = Proc. Natl. Acad. Sci. U.S.A. | volume = 100 | issue = 13 | pages = 7696–701 | date = June 2003 | pmid = 12788976 | pmc = 164650 | doi = 10.1073/pnas.1232418100 |bibcode = 2003PNAS..100.7696V |doi-access = free }}</ref> | ||
| ===Transcriptomes=== | ===Transcriptomes=== | ||
| {{Further|Transcriptomics technologies}} | |||
| * ''Microarrays'': Assess ] abundance. Useful in classification, prognosis, raise the possibility of differential treatment approaches and aid identification of mutations in the proteins' coding regions.<ref>{{cite journal | author = Van |
* ''Microarrays'': Assess ] abundance. Useful in classification, prognosis, raise the possibility of differential treatment approaches and aid identification of mutations in the proteins' coding regions.<ref>{{cite journal | author = Van, de Vijver M.J.| year = 2002 | title = A gene-expression signature as a predictor of survival in breast cancer | journal = New England Journal of Medicine | volume = 347 | issue = 25| pages = 1999–2009 | doi = 10.1056/NEJMoa021967 | pmid = 12490681 | hdl = 1874/15577 |display-authors=etal| hdl-access = free }}</ref><ref name="pmid12559048">{{cite journal | vauthors = van 't Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Bernards R, Friend SH | title = Expression profiling predicts outcome in breast cancer | journal = Breast Cancer Res. | volume = 5 | issue = 1 | pages = 57–8 | date = 2003 | pmid = 12559048 | pmc = 154139 | doi = 10.1186/bcr562 | doi-access = free }}</ref> The relative abundance of alternative transcripts has become an important feature of cancer research. Particular alternative transcript forms correlate with specific cancer types.<ref>{{cite journal |author1=Xu Q. |author2=Lee C. | year = 2003 | title = Discovery of novel splice forms and functional analysis of cancer-specific alternative splicing in human expressed sequences | journal = Nucleic Acids Research | volume = 31 | issue = 19| pages = 5635–5643 | doi = 10.1093/nar/gkg786 | pmid = 14500827 | pmc = 206480 }}</ref> | ||
| * ''RNA-Seq'' | |||
| ===Bioinformatics and functional analysis of oncogenes=== | ===Bioinformatics and functional analysis of oncogenes=== | ||
| ] technologies allow the statistical analysis of genomic data. The functional characteristics of oncogenes has yet to be established. Potential functions include their transformational capabilities relating to tumour formation and specific roles at each stage of cancer development. | ] technologies allow the statistical analysis of genomic data. The functional characteristics of oncogenes has yet to be established. Potential functions include their transformational capabilities relating to tumour formation and specific roles at each stage of cancer development. | ||
| After the detection of ] cancer mutations across a cohort of cancer samples, bioinformatic computational analyses can be carried out to identify likely functional and likely driver mutations. There are three main approaches routinely used for this identification: mapping mutations, assessing the effect of mutation of the function of a protein or a ] and finding signs of positive selection across a cohort of tumors. The approaches are not necessarily sequential however, there are important relationships of precedence between elements from the different approaches. Different tools are used at each step.<ref name="pmid23900255">{{cite journal | vauthors = Gonzalez-Perez A, Mustonen V, Reva B, Ritchie GR, Creixell P, Karchin R, Vazquez M, Fink JL, Kassahn KS, Pearson JV, Bader GD, Boutros PC, Muthuswamy L, Ouellette BF, Reimand J, Linding R, Shibata T, Valencia A, Butler A, Dronov S, Flicek P, Shannon NB, Carter H, Ding L, Sander C, Stuart JM, Stein LD, Lopez-Bigas N|display-authors = 6 | title = Computational approaches to identify functional genetic variants in cancer genomes | journal = Nat. Methods | volume = 10 | issue = 8 | pages = 723–9 | date = August 2013 | pmid = 23900255 | pmc = 3919555 | doi = 10.1038/nmeth.2562 }}</ref> | |||
| ===Operomics=== | ===Operomics=== | ||
| Operomics aims to integrate genomics, transcriptomics and ] to understand the molecular mechanisms that underlie the cancer development.<ref>{{cite journal | |
Operomics aims to integrate genomics, transcriptomics and ] to understand the molecular mechanisms that underlie the cancer development.<ref name="pmid11097332">{{cite journal | vauthors = Hanash SM | title = Operomics: molecular analysis of tissues from DNA to RNA to protein | journal = Clin. Chem. Lab. Med. | volume = 38 | issue = 9 | pages = 805–13 | date = September 2000 | pmid = 11097332 | doi = 10.1515/CCLM.2000.116 | s2cid = 34163524 }}</ref> | ||
| ==Comparative oncogenomics== | ==Comparative oncogenomics== | ||
| Comparative oncogenomics uses cross-species comparisons to identify oncogenes. This research involves studying cancer genomes, transcriptomes and proteomes in model organisms such as mice, identifying potential oncogenes and referring back to human cancer samples to see whether homologues of these oncogenes are important in causing human cancers.<ref>{{cite journal | |
Comparative oncogenomics uses cross-species comparisons to identify oncogenes. This research involves studying cancer genomes, transcriptomes and proteomes in model organisms such as mice, identifying potential oncogenes and referring back to human cancer samples to see whether homologues of these oncogenes are important in causing human cancers.<ref name="pmid16814709">{{cite journal | vauthors = Peeper D, Berns A | title = Cross-species oncogenomics in cancer gene identification | journal = Cell | volume = 125 | issue = 7 | pages = 1230–3 | date = June 2006 | pmid = 16814709 | doi = 10.1016/j.cell.2006.06.018 | doi-access = free }}</ref> Genetic alterations in mouse models are similar to those found in human cancers. These models are generated by methods including ] insertion ] or graft transplantation of cancerous cells. | ||
| ==Source of |
==Source of cancer driver mutations, cancer mutagenesis== | ||
| Mutations provide the raw material for natural selection in evolution and can be caused by errors of DNA replication, the action of exogenous mutagens or endogenous DNA damage. The machinery of replication and genome maintenance can be damaged by mutations, or altered by physiological conditions and differential levels of expression in cancer (see references in<ref name="pmid28498882">{{cite journal | vauthors = Rogozin IB, Pavlov YI, Goncearenco A, De S, Lada AG, Poliakov E, Panchenko AR, Cooper DN | title = Mutational signatures and mutable motifs in cancer genomes | journal = Brief. Bioinformatics | volume = 19 | issue = 6 | pages = 1085–1101 | date = November 2018 | pmid = 28498882 | doi = 10.1093/bib/bbx049 | pmc = 6454500 }}</ref>). | |||
| ⚫ | As pointed out by Gao et al.,<ref name="pmid26967246">{{cite journal |vauthors=Gao D, Herman JG, Guo M |title=The clinical value of aberrant epigenetic changes of DNA damage repair genes in human cancer |journal=Oncotarget |volume= |issue= |pages= |year=2016 |pmid=26967246 |doi=10.18632/oncotarget.7949 | |
||
| ⚫ | As pointed out by Gao et al.,<ref name="pmid26967246">{{cite journal|author-link2=James G. Herman |vauthors=Gao D, Herman JG, Guo M |title=The clinical value of aberrant epigenetic changes of DNA damage repair genes in human cancer |journal=Oncotarget |volume= 7|issue= 24|pages= 37331–37346|year=2016 |pmid=26967246 |doi=10.18632/oncotarget.7949 |pmc=5095080}}</ref> the stability and integrity of the human genome are maintained by the ] (DDR) system. Un-repaired DNA damage is a major cause of mutations that drive carcinogenesis.<ref name="pmid18403632">{{cite journal |vauthors=Kastan MB |title=DNA damage responses: mechanisms and roles in human disease: 2007 G.H.A. Clowes Memorial Award Lecture |journal=Mol. Cancer Res. |volume=6 |issue=4 |pages=517–24 |year=2008 |pmid=18403632 |doi=10.1158/1541-7786.MCR-08-0020 |doi-access=free |url=http://www.tau.ac.il/~yossih/download/Michael_B_Kastan_11.pdf }}</ref><ref name="BernsteinPrasad">{{cite book |last1= Bernstein |first1=C |last2=Prasad |first2=AR |last3=Nfonsam |first3=V |last4=Bernstein |first4=H. |year=2013 |chapter= Chapter 16: DNA Damage, DNA Repair and Cancer |title= New Research Directions in DNA Repair |editor-first=Clark |editor-last=Chen |isbn=978-953-51-1114-6|page=413|publisher=BoD – Books on Demand }}</ref> If DNA repair is deficient, DNA damage tends to accumulate. Such excess DNA damage can increase ] errors during ] due to error-prone ]. Excess DNA damage can also increase ] alterations due to errors during DNA repair.<ref name="Hagan">{{cite journal |vauthors=O'Hagan HM, Mohammad HP, Baylin SB |title=Double strand breaks can initiate gene silencing and SIRT1-dependent onset of DNA methylation in an exogenous promoter CpG island |journal=PLOS Genetics |volume=4 |issue=8 |pages=e1000155 |year=2008 |pmid=18704159 |pmc=2491723 |doi=10.1371/journal.pgen.1000155 |doi-access=free }}</ref><ref name="Cuozzo">{{cite journal |vauthors=Cuozzo C, Porcellini A, Angrisano T |title=DNA damage, homology-directed repair, and DNA methylation |journal=PLOS Genetics |volume=3 |issue=7 |pages=e110 | date=July 2007 |pmid=17616978 |pmc=1913100 |doi=10.1371/journal.pgen.0030110|display-authors=etal |doi-access=free }}</ref> Such mutations and epigenetic alterations can give rise to ]. DDR genes are often repressed in human cancer by epigenetic mechanisms. Such repression may involve DNA methylation of promoter regions or repression of DDR genes by a microRNA. Epigenetic repression of DDR genes occurs more frequently than gene mutation in many types of cancer (see ]). Thus, epigenetic repression often plays a more important role than mutation in reducing expression of DDR genes. This reduced expression of DDR genes is likely an important driver of carcinogenesis. | ||
| DDR genes are often repressed in human cancer by epigenetic mechanisms. Such repression may involve DNA methylation of promoter regions or repression of DDR genes by a microRNA. Epigenetic repression of DDR genes occurs more frequently than gene mutation in many types of cancer (see ]). Thus, epigenetic repression often plays a more important role than mutation in reducing expression of DDR genes. This reduced expression of DDR genes is likely an important driver of carcinogenesis. | |||
| Nucleotide sequence context influences mutation probability<ref name="pmid355893">{{cite journal | vauthors = Coulondre C, Miller JH, Farabaugh PJ, Gilbert W | title = Molecular basis of base substitution hotspots in Escherichia coli | journal = Nature | volume = 274 | issue = 5673 | pages = 775–80 | date = August 1978 | pmid = 355893 |doi= 10.1038/274775a0|bibcode=1978Natur.274..775C| s2cid = 4165194 }}</ref><ref name="pmid3338800">{{cite journal | vauthors = Cooper DN, Youssoufian H | title = The CpG dinucleotide and human genetic disease | journal = Hum. Genet. | volume = 78 | issue = 2 | pages = 151–5 | date = February 1988 | pmid = 3338800 | doi = 10.1007/bf00278187 | s2cid = 41948691 }}</ref><ref name=":1">{{cite journal | vauthors = Rogozin IB, Kolchanov NA | title = Somatic hypermutagenesis in immunoglobulin genes. II. Influence of neighbouring base sequences on mutagenesis | journal = Biochim. Biophys. Acta | volume = 1171 | issue = 1 | pages = 11–8 | date = November 1992 | pmid = 1420357 | doi = 10.1016/0167-4781(92)90134-l |issn=0006-3002}}</ref> and analysis of mutational (mutable) DNA motifs can be essential for understanding the mechanisms of mutagenesis in cancer. Such motifs represent the fingerprints of interactions between DNA and mutagens, between DNA and repair/replication/modification enzymes. Examples of motifs are the AID motif WRCY/RGYW (W = A or T, R = purine and Y = pyrimidine) with C to T/G/A mutations,<ref name=":1" /> and error-prone DNA pol η attributed AID-related mutations (A to G/C/G) in WA/TW motifs.<ref name="pmid11376340">{{cite journal | vauthors = Rogozin IB, Pavlov YI, Bebenek K, Matsuda T, Kunkel TA | title = Somatic mutation hotspots correlate with DNA polymerase eta error spectrum | journal = Nat. Immunol. | volume = 2 | issue = 6 | pages = 530–6 | date = June 2001 | pmid = 11376340 | doi = 10.1038/88732 | s2cid = 12807889 | issn=1529-2908}}</ref> | |||
| Another (agnostic) way to analyze the observed mutational spectra and DNA sequence context of mutations in tumors involves pooling all mutations of different types and contexts from cancer samples into a discrete distribution. If multiple cancer samples are available, their context-dependent mutations can be represented in the form of a nonnegative matrix. This matrix can be further decomposed into components (mutational signatures) which ideally should describe individual mutagenic factors.<ref name="pmid22608084">{{cite journal | vauthors = Nik-Zainal S, Alexandrov LB, Wedge DC, Van Loo P, Greenman CD, Raine K, Jones D, Hinton J, Marshall J, Stebbings LA, Menzies A, Martin S, Leung K, Chen L, Leroy C, Ramakrishna M, Rance R, Lau KW, Mudie LJ, Varela I, McBride DJ, Bignell GR, Cooke SL, Shlien A, Gamble J, Whitmore I, Maddison M, Tarpey PS, Davies HR, Papaemmanuil E, Stephens PJ, McLaren S, Butler AP, Teague JW, Jönsson G, Garber JE, Silver D, Miron P, Fatima A, Boyault S, Langerød A, Tutt A, Martens JW, Aparicio SA, Borg Å, Salomon AV, Thomas G, Børresen-Dale AL, Richardson AL, Neuberger MS, Futreal PA, Campbell PJ, Stratton MR|display-authors = 6 | title = Mutational processes molding the genomes of 21 breast cancers | journal = Cell | volume = 149 | issue = 5 | pages = 979–93 | date = May 2012 | pmid = 22608084 | pmc = 3414841 | doi = 10.1016/j.cell.2012.04.024 }}</ref> Several computational methods have been proposed for solving this decomposition problem. The first implementation of Non-negative Matrix Factorization (NMF) method is available in Sanger Institute Mutational Signature Framework in the form of a MATLAB package.<ref name="pmid23318258">{{cite journal | vauthors = Alexandrov LB, Nik-Zainal S, Wedge DC, Campbell PJ, Stratton MR | title = Deciphering signatures of mutational processes operative in human cancer | journal = Cell Rep | volume = 3 | issue = 1 | pages = 246–59 | date = January 2013 | pmid = 23318258 | pmc = 3588146 | doi = 10.1016/j.celrep.2012.12.008 }}</ref> On the other hand, if mutations from a single tumor sample are only available, the DeconstructSigs R package<ref name="pmid26899170">{{cite journal | vauthors = Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C | title = DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution | journal = Genome Biol. | volume = 17 | pages = 31 | date = February 2016 | pmid = 26899170 | pmc = 4762164 | doi = 10.1186/s13059-016-0893-4 | doi-access = free }}</ref> and <ref name="pmid28472504">{{cite journal | vauthors = Goncearenco A, Rager SL, Li M, Sang QX, Rogozin IB, Panchenko AR | title = Exploring background mutational processes to decipher cancer genetic heterogeneity | journal = Nucleic Acids Res. | volume = 45 | issue = W1 | pages = W514–W522 | date = July 2017 | pmid = 28472504 | pmc = 5793731 | doi = 10.1093/nar/gkx367 }}</ref> may provide the identification of contributions of different mutational signatures for a single tumor sample. In addition, MutaGene server provides mutagen or cancer-specific mutational background models and signatures that can be applied to calculate expected DNA and protein site mutability to decouple relative contributions of mutagenesis and selection in carcinogenesis. | |||
| ==Synthetic lethality== | ==Synthetic lethality== | ||
| Synthetic lethality arises when a combination of deficiencies in the expression of two or more genes leads to cell death, whereas a deficiency in only one of these genes does not. The deficiencies can arise through mutations, epigenetic alterations or inhibitors of one of the genes. | |||
| ⚫ | |||
| The therapeutic potential of synthetic lethality as an efficacious anti-cancer strategy is continually improving. Recently, the applicability of synthetic lethality to targeted cancer therapy has heightened due to the recent work of scientists including ] and colleagues, in what is termed 'collateral lethality'. Muller et al. found that passenger genes, with chromosomal proximity to tumor suppressor genes, are collaterally deleted in some cancers.<ref name="ReferenceA">{{cite journal | vauthors = Muller FL, Colla S, Aquilanti E, Manzo VE, Genovese G, Lee J, Eisenson D, Narurkar R, Deng P, Nezi L, Lee MA, Hu B, Hu J, Sahin E, Ong D, Fletcher-Sananikone E, Ho D, Kwong L, Brennan C, Wang YA, Chin L, DePinho RA|display-authors = 6 | title = Passenger deletions generate therapeutic vulnerabilities in cancer | journal = Nature | volume = 488 | issue = 7411 | pages = 337–42 | date = August 2012 | pmid = 22895339 | pmc = 3712624 | doi = 10.1038/nature11331 |bibcode=2012Natur.488..337M }}</ref> Thus, the identification of collaterally deleted redundant genes carrying out an essential cellular function may be the untapped reservoir for then pursuing a ] approach. Collateral lethality therefore holds great potential in identification of novel and selective therapeutic targets in oncology.<ref name="pmid26870836">{{cite journal | vauthors = Muller FL, Aquilanti EA, DePinho RA | title = Collateral Lethality: A new therapeutic strategy in oncology | journal = Trends Cancer | volume = 1 | issue = 3 | pages = 161–173 | date = November 2015 | pmid = 26870836 | pmc = 4746004 | doi = 10.1016/j.trecan.2015.10.002 }}</ref> In 2012, Muller et al. identified that homozygous deletion of redundant-essential glycolytic ] gene in human ] (GBM) is the consequence of proximity to 1p36 tumor suppressor locus deletions and may hold potential for a synthetic lethality approach to GBM inhibition.<ref name="ReferenceA"/> ENO1 is one of three homologous genes (], ]) that encodes the mammalian ] enzyme.<ref name="pmid1322695">{{cite journal | vauthors = Poyner RR, Reed GH | title = Structure of the bis divalent cation complex with phosphonoacetohydroxamate at the active site of enolase | journal = Biochemistry | volume = 31 | issue = 31 | pages = 7166–73 | date = August 1992 | pmid = 1322695 | doi = 10.1021/bi00146a020 }}</ref> ENO2, which encodes ], is mostly expressed in neural tissues, leading to the postulation that in ]-deleted GBM, ENO2 may be the ideal target as the redundant homologue of ENO1.<ref name="pmid8632173">{{cite journal | vauthors = Joseph J, Cruz-Sánchez FF, Carreras J | title = Enolase activity and isoenzyme distribution in human brain regions and tumors | journal = J. Neurochem. | volume = 66 | issue = 6 | pages = 2484–90 | date = June 1996 | pmid = 8632173 | doi = 10.1046/j.1471-4159.1996.66062484.x | s2cid = 24655147 }}</ref> Muller found that both genetic and pharmacological ENO2 inhibition in GBM cells with homozygous ENO1 deletion elicits a synthetic lethality outcome by selective killing of GBM cells.<ref name="ReferenceA"/> In 2016, Muller and colleagues discovered antibiotic SF2312 as a highly potent nanomolar-range ] inhibitor which preferentially inhibits glioma cell proliferation and glycolytic flux in ENO1-deleted cells.<ref name="pmid27723749"/> SF2312 was shown to be more efficacious than pan-enolase inhibitor PhAH and have more specificity for ENO2 inhibition over ENO1.<ref name="pmid27723749">{{cite journal | vauthors = Leonard PG, Satani N, Maxwell D, Lin YH, Hammoudi N, Peng Z, Pisaneschi F, Link TM, Lee GR, Sun D, Prasad BB, Di Francesco ME, Czako B, Asara JM, Wang YA, Bornmann W, DePinho RA, Muller FL|display-authors = 6 | title = SF2312 is a natural phosphonate inhibitor of enolase | journal = Nat. Chem. Biol. | volume = 12 | issue = 12 | pages = 1053–1058 | date = December 2016 | pmid = 27723749 | pmc = 5110371 | doi = 10.1038/nchembio.2195 }}</ref> Subsequent work by the same team showed that the same approach could be applied to ], whereby homozygously deleted ] results in the collateral deletion of mitochondrial malic enzyme 2 (]), an oxidative decarboxylase essential for ] homeostasis.<ref name="ReferenceB">{{cite journal | vauthors = Dey P, Baddour J, Muller F, Wu CC, Wang H, Liao WT, Lan Z, Chen A, Gutschner T, Kang Y, Fleming J, Satani N, Zhao D, Achreja A, Yang L, Lee J, Chang E, Genovese G, Viale A, Ying H, Draetta G, Maitra A, Wang YA, Nagrath D, DePinho RA|display-authors = 6 | title = Genomic deletion of malic enzyme 2 confers collateral lethality in pancreatic cancer | journal = Nature | volume = 542 | issue = 7639 | pages = 119–123 | date = February 2017 | pmid = 28099419 | pmc = 5398413 | doi = 10.1038/nature21052 |bibcode=2017Natur.542..119D}}</ref> Dey et al. show that ME2 genomic deletion in pancreatic ductal adenocarcinoma cells results in high endogenous reactive oxygen species, consistent with KRAS-driven ], and essentially primes ME2-null cells for synthetic lethality by depletion of redundant NAD(P)+-dependent isoform ME3. The effects of ME3 depletion were found to be mediated by inhibition of de novo nucleotide synthesis resulting from AMPK activation and mitochondrial ROS-mediated apoptosis.<ref name="pmid26947075">{{cite journal | vauthors = Liou GY, Döppler H, DelGiorno KE, Zhang L, Leitges M, Crawford HC, Murphy MP, Storz P | title = Mutant KRas-Induced Mitochondrial Oxidative Stress in Acinar Cells Upregulates EGFR Signaling to Drive Formation of Pancreatic Precancerous Lesions | journal = Cell Rep | volume = 14 | issue = 10 | pages = 2325–36 | date = March 2016 | pmid = 26947075 | pmc = 4794374 | doi = 10.1016/j.celrep.2016.02.029 }}</ref><ref name="ReferenceB"/> Meanwhile, Oike et al. demonstrated the generalizability of the concept by targeting redundant essential-genes in process other than metabolism, namely the ] and ] subunits in the chromatin-remodeling ] complex.<ref name="pmid23872584">{{cite journal | vauthors = Oike T, Ogiwara H, Tominaga Y, Ito K, Ando O, Tsuta K, Mizukami T, Shimada Y, Isomura H, Komachi M, Furuta K, Watanabe S, Nakano T, Yokota J, Kohno T|display-authors = 6 | title = A synthetic lethality-based strategy to treat cancers harboring a genetic deficiency in the chromatin remodeling factor BRG1 | journal = Cancer Res. | volume = 73 | issue = 17 | pages = 5508–18 | date = September 2013 | pmid = 23872584 | doi = 10.1158/0008-5472.CAN-12-4593 | doi-access = free }}</ref> | |||
| ⚫ | Some oncogenes are essential for survival of all cells (not only cancer cells). Thus, drugs that knock out these oncogenes (and thereby kill cancer cells) may also damage normal cells, inducing significant illness. However, other genes may be essential to cancer cells but not to healthy cells. | ||
| Treatments based on the principle of synthetic lethality have prolonged the survival of cancer patients, and show promise for future advances in reversal of carcinogenesis. A major type of synthetic lethality operates on the DNA repair defect that often initiates a cancer, and is still present in the tumor cells. Some examples are given here. | |||
| ] or ] expression is deficient in a majority of high-grade breast and ovarian cancers, usually due to epigenetic methylation of its promoter or epigenetic repression by an over-expressed microRNA (see articles ] and ]). BRCA1 and BRCA2 are important components of the major pathway for ]al repair of double-strand breaks. If one or the other is deficient, it increases the risk of cancer, especially breast or ovarian cancer. A back-up DNA repair pathway, for some of the damages usually repaired by BRCA1 and BRCA2, depends on ]. Thus, many ovarian cancers respond to an FDA-approved treatment with a PARP inhibitor, causing synthetic lethality to cancer cells deficient in BRCA1 or BRCA2. This treatment is also being evaluated for breast cancer and numerous other cancers in Phase III clinical trials in 2016.<ref name="pmid27642590">{{cite journal |vauthors=Murata S, Zhang C, Finch N, Zhang K, Campo L, Breuer EK |title=Predictors and Modulators of Synthetic Lethality: An Update on PARP Inhibitors and Personalized Medicine |journal=Biomed Res Int |volume=2016 |pages=2346585 |year=2016 |pmid=27642590 |pmc=5013223 |doi=10.1155/2016/2346585 |doi-access=free }}</ref> | |||
| There are two pathways for ]al repair of double-strand breaks. The major pathway depends on BRCA1, ] and BRCA2 while an alternative pathway depends on RAD52.<ref name="pmid22964643">{{cite journal |vauthors=Lok BH, Carley AC, Tchang B, Powell SN |title=RAD52 inactivation is synthetically lethal with deficiencies in BRCA1 and PALB2 in addition to BRCA2 through RAD51-mediated homologous recombination |journal=Oncogene |volume=32 |issue=30 |pages=3552–8 |year=2013 |pmid=22964643 |doi=10.1038/onc.2012.391 |pmc=5730454 }}</ref> Pre-clinical studies, involving epigenetically reduced or mutated BRCA-deficient cells (in culture or injected into mice), show that inhibition of RAD52 is synthetically lethal with BRCA-deficiency.<ref name="pmid23836560">{{cite journal |vauthors=Cramer-Morales K, Nieborowska-Skorska M, Scheibner K, Padget M, Irvine DA, Sliwinski T, Haas K, Lee J, Geng H, Roy D, Slupianek A, Rassool FV, Wasik MA, Childers W, Copland M, Müschen M, Civin CI, Skorski T |title=Personalized synthetic lethality induced by targeting RAD52 in leukemias identified by gene mutation and expression profile |journal=Blood |volume=122 |issue=7 |pages=1293–304 |year=2013 |pmid=23836560 |pmc=3744994 |doi=10.1182/blood-2013-05-501072 }}</ref> | |||
| Mutations in genes employed in DNA mismatch repair (MMR) cause a high mutation rate.<ref name="pmid7824277">{{cite journal |vauthors=Eshleman JR, Lang EZ, Bowerfind GK, Parsons R, Vogelstein B, Willson JK, Veigl ML, Sedwick WD, Markowitz SD |title=Increased mutation rate at the hprt locus accompanies microsatellite instability in colon cancer |journal=Oncogene |volume=10 |issue=1 |pages=33–7 |year=1995 |pmid=7824277 }}</ref> In tumors, such frequent subsequent mutations often generate "non-self" immunogenic antigens. A human Phase II clinical trial, with 41 patients, evaluated one synthetic lethal approach for tumors with or without MMR defects.<ref name="pmid26028255">{{cite journal |vauthors=Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, Biedrzycki B, Donehower RC, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Duffy SM, Goldberg RM, de la Chapelle A, Koshiji M, Bhaijee F, Huebner T, Hruban RH, Wood LD, Cuka N, Pardoll DM, Papadopoulos N, Kinzler KW, Zhou S, Cornish TC, Taube JM, Anders RA, Eshleman JR, Vogelstein B, Diaz LA |display-authors = 6|title=PD-1 Blockade in Tumors with Mismatch-Repair Deficiency |journal=N. Engl. J. Med. |volume=372 |issue=26 |pages=2509–20 |year=2015 |pmid=26028255 |pmc=4481136 |doi=10.1056/NEJMoa1500596 }}</ref> The product of gene ''PD-1'' ordinarily represses cytotoxic immune responses. Inhibition of this gene allows a greater immune response. When cancer patients with a defect in MMR in their tumors were exposed to an inhibitor of PD-1, 67–78% of patients experienced immune-related progression-free survival. In contrast, for patients without defective MMR, addition of PD-1 inhibitor generated only 11% of patients with immune-related progression-free survival. Thus inhibition of PD-1 is primarily synthetically lethal with MMR defects. | |||
| ], a chromatin modifier, is required for ], a major pathway that repairs double-strand breaks in DNA,<ref name="pmid24788099">{{cite journal |vauthors=Watanabe R, Ui A, Kanno S, Ogiwara H, Nagase T, Kohno T, Yasui A |title=SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability |journal=Cancer Res. |volume=74 |issue=9 |pages=2465–75 |year=2014 |pmid=24788099 |doi=10.1158/0008-5472.CAN-13-3608 |doi-access=free }}</ref> and also has transcription regulatory roles.<ref name="pmid26716708">{{cite journal |vauthors=Raab JR, Resnick S, Magnuson T |title=Genome-Wide Transcriptional Regulation Mediated by Biochemically Distinct SWI/SNF Complexes |journal=PLOS Genet. |volume=11 |issue=12 |pages=e1005748 |year=2015 |pmid=26716708 |pmc=4699898 |doi=10.1371/journal.pgen.1005748 |doi-access=free }}</ref> ARID1A mutations are one of the 12 most common carcinogenic mutations.<ref name="pmid24390350">{{cite journal |vauthors=Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander ES, Getz G |title=Discovery and saturation analysis of cancer genes across 21 tumour types |journal=Nature |volume=505 |issue=7484 |pages=495–501 |year=2014 |pmid=24390350 |pmc=4048962 |doi=10.1038/nature12912 |bibcode=2014Natur.505..495L }}</ref> Mutation or epigenetically decreased expression<ref name="pmid23349767">{{cite journal |vauthors=Zhang X, Sun Q, Shan M, Niu M, Liu T, Xia B, Liang X, Wei W, Sun S, Zhang Y, Liu XS, Song Q, Yang Y, Ma Y, Liu Y, Yang L, Ren Y, Zhang G, Pang D |title=Promoter hypermethylation of ARID1A gene is responsible for its low mRNA expression in many invasive breast cancers |journal=PLOS ONE |volume=8 |issue=1 |pages=e53931 |year=2013 |pmid=23349767 |pmc=3549982 |doi=10.1371/journal.pone.0053931 |bibcode=2013PLoSO...853931Z |doi-access=free }}</ref> of ARID1A has been found in 17 types of cancer.<ref name="pmid23208470">{{cite journal |vauthors=Wu JN, Roberts CW |title=ARID1A mutations in cancer: another epigenetic tumor suppressor? |journal=Cancer Discov |volume=3 |issue=1 |pages=35–43 |year=2013 |pmid=23208470 |pmc=3546152 |doi=10.1158/2159-8290.CD-12-0361 }}</ref> Pre-clinical studies in cells and in mice show that synthetic lethality for ARID1A deficiency occurs by either inhibition of the methyltransferase activity of EZH2,<ref name="pmid25686104">{{cite journal |vauthors=Bitler BG, Aird KM, Garipov A, Li H, Amatangelo M, Kossenkov AV, Schultz DC, Liu Q, ((Shih IeM)), Conejo-Garcia JR, Speicher DW, Zhang R |title=Synthetic lethality by targeting EZH2 methyltransferase activity in ARID1A-mutated cancers |journal=Nat. Med. |volume=21 |issue=3 |pages=231–8 |year=2015 |pmid=25686104 |pmc=4352133 |doi=10.1038/nm.3799 }}</ref><ref name="pmid26552009">{{cite journal |vauthors=Kim KH, Kim W, Howard TP, Vazquez F, Tsherniak A, Wu JN, Wang W, Haswell JR, Walensky LD, Hahn WC, Orkin SH, Roberts CW |title=SWI/SNF-mutant cancers depend on catalytic and non-catalytic activity of EZH2 |journal=Nat. Med. |volume=21 |issue=12 |pages=1491–6 |year=2015 |pmid=26552009 |pmc=4886303 |doi=10.1038/nm.3968 }}</ref> or with addition of the kinase inhibitor dasatinib.<ref name="pmid27364904">{{cite journal |vauthors=Miller RE, Brough R, Bajrami I, Williamson CT, McDade S, Campbell J, Kigozi A, Rafiq R, Pemberton H, Natrajan R, Joel J, Astley H, Mahoney C, Moore JD, Torrance C, Gordan JD, Webber JT, Levin RS, Shokat KM, Bandyopadhyay S, Lord CJ, Ashworth A|display-authors = 6 |title=Synthetic Lethal Targeting of ARID1A-Mutant Ovarian Clear Cell Tumors with Dasatinib |journal=Mol. Cancer Ther. |volume=15 |issue=7 |pages=1472–84 |year=2016 |pmid=27364904 |doi=10.1158/1535-7163.MCT-15-0554 |url=https://pure.qub.ac.uk/portal/files/82797193/Miller_et_al.pdf|doi-access=free }}</ref> | |||
| Another approach is to individually knock out each gene in a genome and observe the effect on normal and cancerous cells.<ref>{{cite journal | author = Kaelin W.G. | year = 2005 | title = The concept of synthetic lethality in the context of anticancer therapy | journal = Nature Reviews Cancer | volume = 5 | issue = 9| pages = 689–698 | doi = 10.1038/nrc1691 | pmid = 16110319 | s2cid = 3218512 }}</ref><ref>{{cite journal |author1=O'Connor M.J. |author2=Martin N.M.B. |author3=Smith G.C.M. | year = 2007 | title = Targeted cancer therapies based on the inhibition of DNA strand break repair | journal = Oncogene | volume = 26 | issue = 56| pages = 7816–7824 | doi = 10.1038/sj.onc.1210879 | pmid = 18066095 |s2cid=33955861 | doi-access = }}</ref> If the knockout of an otherwise nonessential gene has little or no effect on healthy cells, but is lethal to cancerous cells containing a mutated oncogene, then the system-wide suppression of the suppressed gene can destroy cancerous cells while leaving healthy ones relatively undamaged. The technique was used to identify ] inhibitors to treat BRCA1/BRCA2-associated cancers.<ref name="pmid15829967">{{cite journal | vauthors = Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A | title = Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy | journal = Nature | volume = 434 | issue = 7035 | pages = 917–21 | date = April 2005 | pmid = 15829967 | doi = 10.1038/nature03445 | bibcode = 2005Natur.434..917F | s2cid = 4364706 }}</ref><ref>{{cite journal | author = Bryant H.E. | year = 2005 | title = Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase | journal = Nature | volume = 434 | issue = 7035| pages = 913–917 | doi = 10.1038/nature03443 | pmid = 15829966 |bibcode = 2005Natur.434..913B | last2 = Schultz | first2 = Niklas | last3 = Thomas | first3 = Huw D. | last4 = Parker | first4 = Kayan M. | last5 = Flower | first5 = Dan | last6 = Lopez | first6 = Elena | last7 = Kyle | first7 = Suzanne | last8 = Meuth | first8 = Mark | last9 = Curtin | first9 = Nicola J. | last10 = Helleday | first10 = Thomas | s2cid = 4391043 |display-authors=etal}}</ref> In this case, the combined presence of PARP-1 inhibition and of the cancer-associated mutations in BRCA genes is lethal only to the cancerous cells. | |||
| ==Databases for cancer research== | ==Databases for cancer research== | ||
| {{See also|Databases for oncogenomic research}} | {{See also|Databases for oncogenomic research}} | ||
| The ] is an initiative to map out all somatic mutations in cancer. The project systematically sequences the exons and flanking splice junctions of the genomes of primary tumors and cancerous cell lines. |
The ] is an initiative to map out all somatic mutations in cancer. The project systematically sequences the exons and flanking splice junctions of the genomes of primary tumors and cancerous cell lines. COSMIC software displays the data generated from these experiments. As of February 2008, the CGP had identified 4,746 genes and 2,985 mutations in 1,848 tumours. | ||
| The includes information of research on cancer genomes, transcriptomes and proteomes. | The ] includes information of research on cancer genomes, transcriptomes and proteomes. | ||
| Progenetix is an oncogenomic reference database, presenting cytogenetic and molecular-cytogenetic tumor data. | |||
| Oncomine has compiled data from cancer transcriptome profiles. | |||
| The integrative oncogenomics database IntOGen and the Gitools datasets integrate multidimensional human oncogenomic data classified by tumor type. The first version of IntOGen focused on the role of deregulated ] and ] in cancer.<ref>{{cite journal | |
The integrative oncogenomics database IntOGen and the Gitools datasets integrate multidimensional human oncogenomic data classified by tumor type. The first version of IntOGen focused on the role of deregulated ] and ] in cancer.<ref name="pmid20111033">{{cite journal | vauthors = Gundem G, Perez-Llamas C, Jene-Sanz A, Kedzierska A, Islam A, Deu-Pons J, Furney SJ, Lopez-Bigas N | title = IntOGen: integration and data mining of multidimensional oncogenomic data | journal = Nat. Methods | volume = 7 | issue = 2 | pages = 92–3 | date = February 2010 | pmid = 20111033 | doi = 10.1038/nmeth0210-92 | hdl = 10230/28107 | s2cid = 205417208 | hdl-access = free }}</ref> A later version emphasized mutational cancer driver genes across 28 tumor types,.<ref name="pmid24037244">{{cite journal | vauthors = Gonzalez-Perez A, Perez-Llamas C, Deu-Pons J, Tamborero D, Schroeder MP, Jene-Sanz A, Santos A, Lopez-Bigas N | title = IntOGen-mutations identifies cancer drivers across tumor types | journal = Nat. Methods | volume = 10 | issue = 11 | pages = 1081–2 | date = November 2013 | pmid = 24037244 | pmc = 5758042 | doi = 10.1038/nmeth.2642 }}</ref><ref name="pmid25759023">{{cite journal | vauthors = Rubio-Perez C, Tamborero D, Schroeder MP, Antolín AA, Deu-Pons J, Perez-Llamas C, Mestres J, Gonzalez-Perez A, Lopez-Bigas N | title = In silico prescription of anticancer drugs to cohorts of 28 tumor types reveals targeting opportunities | journal = Cancer Cell | volume = 27 | issue = 3 | pages = 382–96 | date = March 2015 | pmid = 25759023 | doi = 10.1016/j.ccell.2015.02.007 | doi-access = free | hdl = 10230/33093 | hdl-access = free }}</ref> All releases of IntOGen data are made available at the IntOGen database. | ||
| The ] is the biggest project to collect human cancer genome data. The data is accessible through the |
The ] is the biggest project to collect human cancer genome data. The data is accessible through the ICGC website. The BioExpress® Oncology Suite contains gene expression data from primary, metastatic and benign tumor samples and normal samples, including matched adjacent controls. The suite includes hematological malignancy samples for many well-known cancers. | ||
| Specific databases for model animals include the |
Specific databases for model animals include the Retrovirus Tagged Cancer Gene Database (RTCGD) that compiled research on retroviral and transposon insertional mutagenesis in mouse tumors. | ||
| ==Gene families== | ==Gene families== | ||
| Mutational analysis of entire gene families revealed that genes of the same family have similar functions, as predicted by similar coding sequences and ]. Two such classes are the ] family, involved in adding phosphate groups to proteins and the ] family, involved with removing phosphate groups from proteins.<ref>{{cite journal | |
Mutational analysis of entire gene families revealed that genes of the same family have similar functions, as predicted by similar coding sequences and ]. Two such classes are the ] family, involved in adding phosphate groups to proteins and the ] family, involved with removing phosphate groups from proteins.<ref name="pmid11357143">{{cite journal | vauthors = Blume-Jensen P, Hunter T | title = Oncogenic kinase signalling | journal = Nature | volume = 411 | issue = 6835 | pages = 355–65 | date = May 2001 | pmid = 11357143 | doi = 10.1038/35077225 | bibcode = 2001Natur.411..355B | s2cid = 4428819 }}</ref> These families were first examined because of their apparent role in transducing cellular signals of cell growth or death. In particular, more than 50% of colorectal cancers carry a mutation in a kinase or phosphatase gene. ] (]) gene encodes for lipid kinases that commonly contain mutations in colorectal, breast, gastric, lung and various other cancers.<ref>{{cite journal |vauthors=Bardelli A, etal | year = 2003 | title = Mutational analysis of the tyrosine kinome in colorectal cancers | journal = Science | volume = 300 | issue = 5621| pages = 949 | doi = 10.1126/science.1082596 | pmid=12738854| s2cid = 85934154 }}</ref><ref name="pmid15016963">{{cite journal | vauthors = ], Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S, Yan H, Gazdar A, Powell SM, Riggins GJ, Willson JK, Markowitz S, Kinzler KW, Vogelstein B, Velculescu VE | title = High frequency of mutations of the PIK3CA gene in human cancers | journal = Science | volume = 304 | issue = 5670 | pages = 554 | date = April 2004 | pmid = 15016963 | doi = 10.1126/science.1096502 | s2cid = 10147415 }}</ref> Drug therapies can inhibit PIK3CA. Another example is the ] gene, one of the first to be implicated in melanomas.<ref name="pmid12068308">{{cite journal | vauthors = Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S, Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G, Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL, Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR, Futreal PA|display-authors = 6 | title = Mutations of the BRAF gene in human cancer | journal = Nature | volume = 417 | issue = 6892 | pages = 949–54 | date = June 2002 | pmid = 12068308 | doi = 10.1038/nature00766 | url = http://eprints.gla.ac.uk/121/1/Davis%2CH_2002_pdf.pdf | bibcode = 2002Natur.417..949D |s2cid = 3071547 }}</ref> BRAF encodes a ]/] kinase that is involved in the RAS-RAF-] growth signaling pathway. Mutations in BRAF cause constitutive phosphorylation and activity in 59% of melanomas. Before BRAF, the genetic mechanism of melanoma development was unknown and therefore prognosis for patients was poor.<ref>{{cite journal |author1=Danson S. |author2=Lorigan P. | year = 2005 | title = Improving outcomes in advanced malignant melanoma – Update on systemic therapy | journal = Drugs | volume = 65 | issue = 6| pages = 733–743 | doi = 10.2165/00003495-200565060-00002 | pmid = 15819587 |s2cid=46969987 }}</ref> | ||
| ==Mitochondrial DNA == | == Mitochondrial DNA == | ||
| ] (mtDNA) mutations are linked the formation of tumors. Four types of mtDNA mutations have been identified:<ref name="mito">{{cite |
] (mtDNA) mutations are linked the formation of tumors. Four types of mtDNA mutations have been identified:<ref name="mito">{{cite book|last=Yu|first=Man|title=Somatic Mitochondrial DNA Mutations in Human Cancers|year=2012|volume=57|pages=99–138|doi=10.1016/B978-0-12-394384-2.00004-8|pmid=22870588|series=Advances in Clinical Chemistry|isbn=9780123943842}}</ref> | ||
| ===Point mutations=== | ===Point mutations=== | ||
| Point mutations have been observed in the coding and non-coding region of the mtDNA contained in cancer cells. In individuals with bladder, head/neck and lung cancers, the point mutations within the coding region show signs of resembling each other. This suggests that when a healthy cell transforms into a tumor cell (a neoplastic transformation) the ] seem to become homogenous. Abundant point mutations located within the non-coding region, ], of the cancerous mitochondria suggest that mutations within this region might be an important characteristic in some cancers.<ref name="mito"/> | Point mutations have been observed in the ] and ] region of the mtDNA contained in cancer cells. In individuals with bladder, head/neck and lung cancers, the point mutations within the coding region show signs of resembling each other. This suggests that when a healthy cell transforms into a tumor cell (a neoplastic transformation) the ] seem to become homogenous. Abundant point mutations located within the non-coding region, ], of the cancerous mitochondria suggest that mutations within this region might be an important characteristic in some cancers.<ref name="mito"/> | ||
| ===Deletions=== | ===Deletions=== | ||
| This type of mutation is sporadically detected due to its small size ( < |
This type of mutation is sporadically detected due to its small size ( < 1 kb). The appearance of certain specific mtDNA mutations (264-bp deletion and 66-bp deletion in the complex 1 subunit gene ND1) in multiple types of cancer provide some evidence that small mtDNA deletions might appear at the beginning of ]. It also suggests that the amount of mitochondria containing these deletions increases as the tumor progresses. An exception is a relatively large deletion that appears in many cancers (known as the "common deletion"), but more mtDNA large scale deletions have been found in normal cells compared to tumor cells. This may be due to a seemingly adaptive process of tumor cells to eliminate any mitochondria that contain these large scale deletions (the "common deletion" is > 4 kb).<ref name="mito"/> | ||
| ===Insertions=== | ===Insertions=== | ||
| Two small mtDNA insertions of ~260 and ~520 bp can be present in breast cancer, gastric cancer, hepatocellular carcinoma (HCC) and colon cancer and in normal cells. No correlation between these insertions and cancer are established.<ref>{{cite journal|last=Hung|first=W.Y. |author2=J.C. Lin |author3=L.M. Lee|title=Tandem duplication/triplication correlated with poly-cytosine stretch variation in human mitochondrial DNA D-loop region|journal=Mutagenesis|year=2008|volume=23|pages=137–142|doi=10.1093/mutage/gen002|pmid=18252697|issue=2|display-authors=etal}}</ref> | Two small mtDNA insertions of ~260 and ~520 bp can be present in breast cancer, gastric cancer, hepatocellular carcinoma (HCC) and colon cancer and in normal cells. No correlation between these insertions and cancer are established.<ref>{{cite journal|last=Hung|first=W.Y. |author2=J.C. Lin |author3=L.M. Lee|title=Tandem duplication/triplication correlated with poly-cytosine stretch variation in human mitochondrial DNA D-loop region|journal=Mutagenesis|year=2008|volume=23|pages=137–142|doi=10.1093/mutage/gen002|pmid=18252697|issue=2|display-authors=etal|doi-access=free}}</ref> | ||
| ===Copy number mutations=== | ===Copy number mutations=== | ||
| Line 118: | Line 141: | ||
| !rRNAs | !rRNAs | ||
| |- | |- | ||
| |Bladder<ref>{{cite journal |last1=Fliss |first1=M. S. |last2=Usadel |first2=H. |last3=Caballero |first3=O. L. |last4=Wu |first4=L. |last5=Buta |first5=M. R. |last6=Eleff |first6=S. M. |last7=Jen |first7=J. |last8=Sidransky |first8=D. |display-authors=3 |title=Facile detection of mitochondrial DNA mutations in tumors and bodily fluids |journal=Science |year=2000 |volume=287 |pages=2017–2019 |bibcode=2000Sci...287.2017F |doi=10.1126/science.287.5460.2017 |pmid=10720328 |issue=5460}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| ||style="text-align: center;"|X||15,642-15,662|| || | |Bladder<ref>{{cite journal |last1=Fliss |first1=M. S. |last2=Usadel |first2=H. |last3=Caballero |first3=O. L. |last4=Wu |first4=L. |last5=Buta |first5=M. R. |last6=Eleff |first6=S. M. |last7=Jen |first7=J. |last8=Sidransky |first8=D. |display-authors=3 |title=Facile detection of mitochondrial DNA mutations in tumors and bodily fluids |journal=Science |year=2000 |volume=287 |pages=2017–2019 |bibcode=2000Sci...287.2017F |doi=10.1126/science.287.5460.2017 |pmid=10720328 |issue=5460|s2cid=24438279 }}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| ||style="text-align: center;"|X||15,642-15,662|| || | ||
| |- | |- | ||
| |Breast<ref name="Dani">{{cite journal|last=Dani|first=M.A. |author2=S.U. Dani |author3=S.P. Lima|title=Less ΔmtDNA4977 than normal in various types of tumors suggests that cancer cells are essentially free of this mutation|journal=Genet. Mol. Res|year=2004|volume=3|pages=395–409|pmid=15614730|issue=3|display-authors=etal}}</ref><ref>{{cite journal|last=Ye|first=C. |author2=X.O. Shu |author3=W. Wen|title=Quantitative analysis of mitochondrial DNA 4977-bp deletion in sporadic breast cancer and benign breast diseases|journal=Breast Cancer Res. Treat.|year=2008|volume=108|pages=427–434|doi=10.1007/s10549-007-9613-9|pmid=17541740|issue=3|display-authors=etal}}</ref><ref>{{cite journal|last=Tseng|first=L.M. |author2=P.H. Yin |author3=C.W. Chi|title=Mitochondrial DNA mutations and mitochondrial DNA depletion in breast cancer|journal=Genes Chromosomes Cancer|year=2006|volume=45|pages=629–638|doi=10.1002/gcc.20326|pmid=16568452|issue=7|display-authors=etal}}</ref><ref>{{cite journal|last=Zhu|first=W. |author2=W. Qin |author3=P. Bradley |author4=A. Wessel |author5=C.L. Puckett |author6=E.R. Sauter|title=Mitochondrial DNA mutations in breast cancer tissue and in matched nipple aspirate fluid|journal=Carcinogenesis|year=2005|volume=26|issue=1|pages=145–152|doi=10.1093/carcin/bgh282|pmid=15375011}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||8470-13,447 and 8482-13459|| ||style="text-align: center;"|X | |Breast<ref name="Dani">{{cite journal|last=Dani|first=M.A. |author2=S.U. Dani |author3=S.P. Lima|title=Less ΔmtDNA4977 than normal in various types of tumors suggests that cancer cells are essentially free of this mutation|journal=Genet. Mol. Res.|year=2004|volume=3|pages=395–409|pmid=15614730|issue=3|display-authors=etal}}</ref><ref>{{cite journal|last=Ye|first=C. |author2=X.O. Shu |author3=W. Wen|title=Quantitative analysis of mitochondrial DNA 4977-bp deletion in sporadic breast cancer and benign breast diseases|journal=Breast Cancer Res. Treat.|year=2008|volume=108|pages=427–434|doi=10.1007/s10549-007-9613-9|pmid=17541740|issue=3|display-authors=etal|pmc=3836503}}</ref><ref>{{cite journal|last=Tseng|first=L.M. |author2=P.H. Yin |author3=C.W. Chi|title=Mitochondrial DNA mutations and mitochondrial DNA depletion in breast cancer|journal=Genes Chromosomes Cancer|year=2006|volume=45|pages=629–638|doi=10.1002/gcc.20326|pmid=16568452|issue=7|s2cid=21181048 |display-authors=etal}}</ref><ref>{{cite journal|last=Zhu|first=W. |author2=W. Qin |author3=P. Bradley |author4=A. Wessel |author5=C.L. Puckett |author6=E.R. Sauter|title=Mitochondrial DNA mutations in breast cancer tissue and in matched nipple aspirate fluid|journal=Carcinogenesis|year=2005|volume=26|issue=1|pages=145–152|doi=10.1093/carcin/bgh282|pmid=15375011|doi-access=free}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||8470-13,447 and 8482-13459|| ||style="text-align: center;"|X | ||
| |- | |- | ||
| |Head and neck<ref name="Dani" /><ref>{{cite journal | |
|Head and neck<ref name="Dani" /><ref name="pmid17456604">{{cite journal | vauthors = Zhou S, Kachhap S, Sun W, Wu G, Chuang A, Poeta L, Grumbine L, Mithani SK, Chatterjee A, Koch W, Westra WH, Maitra A, Glazer C, Carducci M, Sidransky D, McFate T, Verma A, Califano JA | title = Frequency and phenotypic implications of mitochondrial DNA mutations in human squamous cell cancers of the head and neck | journal = Proc. Natl. Acad. Sci. U.S.A. | volume = 104 | issue = 18 | pages = 7540–5 | date = May 2007 | pmid = 17456604 | pmc = 1863503 | doi = 10.1073/pnas.0610818104 | bibcode = 2007PNAS..104.7540Z | doi-access = free }}</ref><ref name="pmid15163006">{{cite journal | vauthors = Poetsch M, Petersmann A, Lignitz E, Kleist B | title = Relationship between mitochondrial DNA instability, mitochondrial DNA large deletions, and nuclear microsatellite instability in head and neck squamous cell carcinomas | journal = Diagn. Mol. Pathol. | volume = 13 | issue = 1 | pages = 26–32 | date = March 2004 | pmid = 15163006 | doi = 10.1097/00019606-200403000-00005 | s2cid = 21271445 }}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||8470-13,447 and 8482-13459||style="text-align: center;"|X|| | ||
| |- | |- | ||
| |Oral<ref>{{cite journal|last=Tan|first=D.J. |author2=J. Chang |author3=W.L. Chen|title=Somatic mitochondrial DNA mutations in oral cancer of betel quid chewers|journal=Ann. N. Y. Acad. Sci.|year=2004|volume=1011|pages=310–316|bibcode=2004NYASA1011..310T|doi=10.1196/annals.1293.030|pmid=15126307|display-authors=etal}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| || ||8470-13,447 and 8482-13459|| || | |Oral<ref>{{cite journal|last=Tan|first=D.J. |author2=J. Chang |author3=W.L. Chen|title=Somatic mitochondrial DNA mutations in oral cancer of betel quid chewers|journal=Ann. N. Y. Acad. Sci.|year=2004|volume=1011|issue=1 |pages=310–316|bibcode=2004NYASA1011..310T|doi=10.1196/annals.1293.030|pmid=15126307|s2cid=19794015 |display-authors=etal}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| || ||8470-13,447 and 8482-13459|| || | ||
| |- | |- | ||
| |Hepatocellular carcinoma (HCC)<ref>{{cite journal|last=Lee|first=H.C. |author2=S.H. Li |author3=J.C. Lin |author4=C.C. Wu |author5=D.C. Yeh |author6=Y.H. Wei|title=Somatic mutations in the D-loop and decrease in the copy number of mitochondrial DNA in human hepatocellular carcinoma|journal=Mutation Research|year=2004|volume=547|pages=71–78|doi=10.1016/j.mrfmmm.2003.12.011|pmid=15013701|issue=1–2}}</ref><ref>{{cite journal|last=Yin|first=P.H. |author2=C.C. Wu |author3=J.C. Lin |author4=C.W. Chi |author5=Y.H. Wei |author6=H.C. Lee|title=Somatic mutations of mitochondrial genome in hepatocellular carcinoma|journal=Mitochondrion|year=2010|volume=10|pages=174–182|doi=10.1016/j.mito.2009.12.147|pmid=20006738|issue=2}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X|| 306-556 and 3894-3960 || ||style="text-align: center;"|X | |Hepatocellular carcinoma (HCC)<ref>{{cite journal|last=Lee|first=H.C. |author2=S.H. Li |author3=J.C. Lin |author4=C.C. Wu |author5=D.C. Yeh |author6=Y.H. Wei|title=Somatic mutations in the D-loop and decrease in the copy number of mitochondrial DNA in human hepatocellular carcinoma|journal=Mutation Research|year=2004|volume=547|pages=71–78|doi=10.1016/j.mrfmmm.2003.12.011|pmid=15013701|issue=1–2}}</ref><ref>{{cite journal|last=Yin|first=P.H. |author2=C.C. Wu |author3=J.C. Lin |author4=C.W. Chi |author5=Y.H. Wei |author6=H.C. Lee|title=Somatic mutations of mitochondrial genome in hepatocellular carcinoma|journal=Mitochondrion|year=2010|volume=10|pages=174–182|doi=10.1016/j.mito.2009.12.147|pmid=20006738|issue=2}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X|| 306-556 and 3894-3960 || ||style="text-align: center;"|X | ||
| |- | |- | ||
| |Esophageal<ref>{{cite journal|last=Tan|first=D.J. |author2=J. Chang |author3=L.L. Liu|title=Significance of somatic mutations and content alteration of mitochondrial DNA in esophageal cancer|journal=BMC Cancer|year=2006|volume=6|pages=93|doi=10.1186/1471-2407-6-93|pmid=16620376|pmc=1459869|display-authors=etal}}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| ||style="text-align: center;"|X||8470-13,447 and 8482-13459||style="text-align: center;"|X|| | |Esophageal<ref>{{cite journal|last=Tan|first=D.J. |author2=J. Chang |author3=L.L. Liu|title=Significance of somatic mutations and content alteration of mitochondrial DNA in esophageal cancer|journal=BMC Cancer|year=2006|volume=6|pages=93|doi=10.1186/1471-2407-6-93|pmid=16620376|pmc=1459869|display-authors=etal |doi-access=free }}</ref>||style="text-align: center;"|X||style="text-align: center;"|X|| ||style="text-align: center;"|X||8470-13,447 and 8482-13459||style="text-align: center;"|X|| | ||
| |- | |- | ||
| |Gastric<ref>{{cite journal| |
|Gastric<ref name="pmid17827523">{{cite journal | vauthors = Kassauei K, Habbe N, Mullendore ME, Karikari CA, Maitra A, Feldmann G | title = Mitochondrial DNA mutations in pancreatic cancer | journal = Int J Gastrointest Cancer | volume = 37 | issue = 2–3 | pages = 57–64 | date = 2006 | pmid = 17827523 | doi = 10.1007/s12029-007-0008-2 | s2cid = 9716204 }}</ref><ref name="pmid19527772">{{cite journal | vauthors = Hung WY, Wu CW, Yin PH, Chang CJ, Li AF, Chi CW, Wei YH, Lee HC | title = Somatic mutations in mitochondrial genome and their potential roles in the progression of human gastric cancer | journal = Biochim. Biophys. Acta | volume = 1800 | issue = 3 | pages = 264–70 | date = March 2010 | pmid = 19527772 | doi = 10.1016/j.bbagen.2009.06.006 }}</ref><ref name="pmid15892105">{{cite journal | vauthors = Wu CW, Yin PH, Hung WY, Li AF, Li SH, Chi CW, Wei YH, Lee HC | title = Mitochondrial DNA mutations and mitochondrial DNA depletion in gastric cancer | journal = Genes Chromosomes Cancer | volume = 44 | issue = 1 | pages = 19–28 | date = September 2005 | pmid = 15892105 | doi = 10.1002/gcc.20213 | s2cid = 11009518 }}</ref>||style="text-align: center;"|X||style="text-align: center;"|X||style="text-align: center;"|X|| || 298-348|| || style="text-align: center;"|X | ||
| |- | |- | ||
| |Prostate<ref>{{cite journal|last=Yu|first=J.J.|author2=T. Yan|title=Effect of mtDNA mutation on tumor malignant degree in patients with prostate cancer|journal=Aging Male|year=2010|volume=13|pages=159–165|doi=10.3109/13685530903536668|pmid=20136572|issue=3}}</ref><ref>{{cite journal|last=Gomez-Zaera|first=M. |author2=J. Abril |author3=L. Gonzalez|title=Identification of somatic and germline mitochondrial DNA sequence variants in prostate cancer patients|journal=Mutation Research|year=2006|volume=595|pages=42–51|doi=10.1016/j.mrfmmm.2005.10.012|pmid=16472830|issue=1–2|display-authors=etal}}</ref>||style="text-align: center;"|X|| || ||style="text-align: center;"|X||8470-13,447 and 8482-13459||style="text-align: center;"|X|| | |Prostate<ref>{{cite journal|last=Yu|first=J.J.|author2=T. Yan|title=Effect of mtDNA mutation on tumor malignant degree in patients with prostate cancer|journal=Aging Male|year=2010|volume=13|pages=159–165|doi=10.3109/13685530903536668|pmid=20136572|issue=3|s2cid=22017823}}</ref><ref>{{cite journal|last=Gomez-Zaera|first=M. |author2=J. Abril |author3=L. Gonzalez|title=Identification of somatic and germline mitochondrial DNA sequence variants in prostate cancer patients|journal=Mutation Research|year=2006|volume=595|pages=42–51|doi=10.1016/j.mrfmmm.2005.10.012|pmid=16472830|issue=1–2|display-authors=etal}}</ref>||style="text-align: center;"|X|| || ||style="text-align: center;"|X||8470-13,447 and 8482-13459||style="text-align: center;"|X|| | ||
| |} | |} | ||
| 57.7% (500/867) contained somatic point putations and of the 1172 mutations surveyed 37.8% (443/1127) were located in the D-loop control region, 13.1% (154/1172) were located in the tRNA or rRNA genes and 49.1% (575/1127) were found in the mRNA genes needed for producing complexes required for mitochondrial respiration. | 57.7% (500/867) contained somatic point putations and of the 1172 mutations surveyed 37.8% (443/1127) were located in the D-loop control region, 13.1% (154/1172) were located in the tRNA or rRNA genes and 49.1% (575/1127) were found in the mRNA genes needed for producing complexes required for mitochondrial respiration. | ||
| Line 140: | Line 163: | ||
| ==Cancer biomarkers== | ==Cancer biomarkers== | ||
| Several ] can be useful in cancer staging, prognosis and treatment. They can range from ]s (SNPs), ], changes in DNA copy number, microsatellite instability, promoter region ], or even high or low protein levels.<ref>{{cite journal| |
Several ] can be useful in cancer staging, prognosis and treatment. They can range from ]s (SNPs), ], changes in DNA copy number, microsatellite instability, promoter region ], or even high or low protein levels.<ref name="pmid16239904">{{cite journal | vauthors = Ludwig JA, Weinstein JN | title = Biomarkers in cancer staging, prognosis and treatment selection | journal = Nat. Rev. Cancer | volume = 5 | issue = 11 | pages = 845–56 | date = November 2005 | pmid = 16239904 | doi = 10.1038/nrc1739 | s2cid = 25540232 | url = https://zenodo.org/record/1233488 }}</ref> Between 2013 and 2019 only 6.8% of people with cancer in 2 US states underwent genetic testing, suggesting broad under-utilization of information that could improve treatment decisions and patient outcomes.<ref>{{cite journal |last1=Kurian |title=Germline Genetic Testing After Cancer Diagnosis |journal=JAMA |date=July 3, 2023 |volume=330 |issue=1 |pages=43–51 |doi=10.1001/jama.2023.9526 |pmid=37276540 |pmc=10242510 |url=https://jamanetwork.com/journals/jama/article-abstract/2805796 |access-date=4 July 2023 }}</ref> | ||
| == |
== See also == | ||
| * ] | |||
| ⚫ | {{reflist| |
||
| * ] | |||
| * ] | |||
| == |
== References == | ||
| ⚫ | {{reflist|30em}} | ||
| *: an oncogenomic reference database from the Wellcome Trust Sanger Institute | |||
| *: an oncogenomic reference database from the National Cancer Institute | |||
| *: an oncogenomic reference database, presenting cytogenetic and molecular-cytogenetic tumor data | |||
| * | |||
| * | |||
| * | |||
| * Integration and data mining of multidimensional oncogenomic data | |||
| ] | ] | ||
Latest revision as of 22:49, 25 April 2024
Sub-field of genomics "Genetics in cancer" redirects here. For inheritable genetic syndromes predisposing affected individuals to cancer, see Hereditary cancer syndrome.Oncogenomics is a sub-field of genomics that characterizes cancer-associated genes. It focuses on genomic, epigenomic and transcript alterations in cancer.
Cancer is a genetic disease caused by accumulation of DNA mutations and epigenetic alterations leading to unrestrained cell proliferation and neoplasm formation. The goal of oncogenomics is to identify new oncogenes or tumor suppressor genes that may provide new insights into cancer diagnosis, predicting clinical outcome of cancers and new targets for cancer therapies. The success of targeted cancer therapies such as Gleevec, Herceptin and Avastin raised the hope for oncogenomics to elucidate new targets for cancer treatment.

Besides understanding the underlying genetic mechanisms that initiate or drive cancer progression, oncogenomics targets personalized cancer treatment. Cancer develops due to DNA mutations and epigenetic alterations that accumulate randomly. Identifying and targeting the mutations in an individual patient may lead to increased treatment efficacy.
The completion of the Human Genome Project facilitated the field of oncogenomics and increased the abilities of researchers to find oncogenes. Sequencing technologies and global methylation profiling techniques have been applied to the study of oncogenomics.
History
The genomics era began in the 1990s, with the generation of DNA sequences of many organisms. In the 21st century, the completion of the Human Genome Project enabled the study of functional genomics and examining tumor genomes. Cancer is a main focus.
The epigenomics era largely began more recently, about 2000. One major source of epigenetic change is altered methylation of CpG islands at the promoter region of genes (see DNA methylation in cancer). A number of recently devised methods can assess the DNA methylation status in cancers versus normal tissues. Some methods assess methylation of CpGs located in different classes of loci, including CpG islands, shores, and shelves as well as promoters, gene bodies, and intergenic regions. Cancer is also a major focus of epigenetic studies.
Access to whole cancer genome sequencing is important to cancer (or cancer genome) research because:
- Mutations are the immediate cause of cancer and define the tumor phenotype.
- Access to cancerous and normal tissue samples from the same patient and the fact that most cancer mutations represent somatic events, allow the identification of cancer-specific mutations.
- Cancer mutations are cumulative and sometimes are related to disease stage. Metastasis and drug resistance are distinguishable.
Access to methylation profiling is important to cancer research because:
- Epi-drivers, along with Mut-drivers, can act as immediate causes of cancers
- Cancer epimutations are cumulative and sometimes related to disease stage
Whole genome sequencing
The first cancer genome was sequenced in 2008. This study sequenced a typical acute myeloid leukaemia (AML) genome and its normal counterpart genome obtained from the same patient. The comparison revealed ten mutated genes. Two were already thought to contribute to tumor progression: an internal tandem duplication of the FLT3 receptor tyrosine kinase gene, which activates kinase signaling and is associated with a poor prognosis and a four base insertion in exon 12 of the NPM1 gene (NPMc). These mutations are found in 25–30% of AML tumors and are thought to contribute to disease progression rather than to cause it directly.
The remaining 8 were new mutations and all were single base changes: Four were in families that are strongly associated with cancer pathogenesis (PTPRT, CDH24, PCLKC and SLC15A1). The other four had no previous association with cancer pathogenesis. They did have potential functions in metabolic pathways that suggested mechanisms by which they could act to promote cancer (KNDC1, GPR124, EB12, GRINC1B)
These genes are involved in pathways known to contribute to cancer pathogenesis, but before this study most would not have been candidates for targeted gene therapy. This analysis validated the approach of whole cancer genome sequencing in identifying somatic mutations and the importance of parallel sequencing of normal and tumor cell genomes.
In 2011, the genome of an exceptional bladder cancer patient whose tumor had been eliminated by the drug everolimus was sequenced, revealing mutations in two genes, TSC1 and NF2. The mutations disregulated mTOR, the protein inhibited by everolimus, allowing it to reproduce without limit. As a result, in 2015, the Exceptional Responders Initiative was created at the National Cancer Institute. The initiative allows such exceptional patients (who have responded positively for at least six months to a cancer drug that usually fails) to have their genomes sequenced to identify the relevant mutations. Once identified, other patients could be screened for those mutations and then be given the drug. In 2016 To that end, a nationwide cancer drug trial began in 2015, involving up to twenty-four hundred centers. Patients with appropriate mutations are matched with one of more than forty drugs.
In 2014 the Center for Molecular Oncology rolled out the MSK-IMPACT test, a screening tool that looks for mutations in 341 cancer-associated genes. By 2015 more than five thousand patients had been screened. Patients with appropriate mutations are eligible to enroll in clinical trials that provide targeted therapy.
Technologies
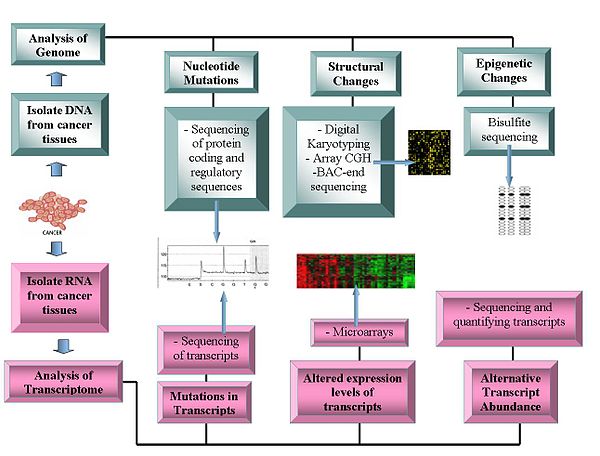
Genomics technologies include:
Genome sequencing
Further information: Cancer genome sequencing- DNA sequencing: Pyrosequencing-based sequencers offer a relatively low-cost method to generate sequence data.
- Array Comparative Genome Hybridization: This technique measures the DNA copy number differences between normal and cancer genomes. It uses the fluorescence intensity from fluorescent-labeled samples, which are hybridized to known probes on a microarray.
- Representational oligonucleotide microarray analysis: Detects copy number variation using amplified restriction-digested genomic fragments that are hybridized to human oligonucleotides, achieving a resolution between 30 and 35 kbit/s.
- Digital karyotyping: Detects copy number variation using genomics tags obtained via restriction enzyme digests. These tags are then linked to into ditags, concatenated, cloned, sequenced and mapped back to the reference genome to evaluate tag density.
- Bacterial artificial chromosome (BAC)-end sequencing (end-sequence profiling): Identifies chromosomal breakpoints by generating a BAC library from a cancer genome and sequencing their ends. The BAC clones that contain chromosome aberrations have end sequences that do not map to a similar region of the reference genome, thus identifying a chromosomal breakpoint.
Transcriptomes
Further information: Transcriptomics technologies- Microarrays: Assess transcript abundance. Useful in classification, prognosis, raise the possibility of differential treatment approaches and aid identification of mutations in the proteins' coding regions. The relative abundance of alternative transcripts has become an important feature of cancer research. Particular alternative transcript forms correlate with specific cancer types.
- RNA-Seq
Bioinformatics and functional analysis of oncogenes
Bioinformatics technologies allow the statistical analysis of genomic data. The functional characteristics of oncogenes has yet to be established. Potential functions include their transformational capabilities relating to tumour formation and specific roles at each stage of cancer development.
After the detection of somatic cancer mutations across a cohort of cancer samples, bioinformatic computational analyses can be carried out to identify likely functional and likely driver mutations. There are three main approaches routinely used for this identification: mapping mutations, assessing the effect of mutation of the function of a protein or a regulatory element and finding signs of positive selection across a cohort of tumors. The approaches are not necessarily sequential however, there are important relationships of precedence between elements from the different approaches. Different tools are used at each step.
Operomics
Operomics aims to integrate genomics, transcriptomics and proteomics to understand the molecular mechanisms that underlie the cancer development.
Comparative oncogenomics
Comparative oncogenomics uses cross-species comparisons to identify oncogenes. This research involves studying cancer genomes, transcriptomes and proteomes in model organisms such as mice, identifying potential oncogenes and referring back to human cancer samples to see whether homologues of these oncogenes are important in causing human cancers. Genetic alterations in mouse models are similar to those found in human cancers. These models are generated by methods including retroviral insertion mutagenesis or graft transplantation of cancerous cells.
Source of cancer driver mutations, cancer mutagenesis
Mutations provide the raw material for natural selection in evolution and can be caused by errors of DNA replication, the action of exogenous mutagens or endogenous DNA damage. The machinery of replication and genome maintenance can be damaged by mutations, or altered by physiological conditions and differential levels of expression in cancer (see references in).
As pointed out by Gao et al., the stability and integrity of the human genome are maintained by the DNA-damage response (DDR) system. Un-repaired DNA damage is a major cause of mutations that drive carcinogenesis. If DNA repair is deficient, DNA damage tends to accumulate. Such excess DNA damage can increase mutational errors during DNA replication due to error-prone translesion synthesis. Excess DNA damage can also increase epigenetic alterations due to errors during DNA repair. Such mutations and epigenetic alterations can give rise to cancer. DDR genes are often repressed in human cancer by epigenetic mechanisms. Such repression may involve DNA methylation of promoter regions or repression of DDR genes by a microRNA. Epigenetic repression of DDR genes occurs more frequently than gene mutation in many types of cancer (see Cancer epigenetics). Thus, epigenetic repression often plays a more important role than mutation in reducing expression of DDR genes. This reduced expression of DDR genes is likely an important driver of carcinogenesis.
Nucleotide sequence context influences mutation probability and analysis of mutational (mutable) DNA motifs can be essential for understanding the mechanisms of mutagenesis in cancer. Such motifs represent the fingerprints of interactions between DNA and mutagens, between DNA and repair/replication/modification enzymes. Examples of motifs are the AID motif WRCY/RGYW (W = A or T, R = purine and Y = pyrimidine) with C to T/G/A mutations, and error-prone DNA pol η attributed AID-related mutations (A to G/C/G) in WA/TW motifs.
Another (agnostic) way to analyze the observed mutational spectra and DNA sequence context of mutations in tumors involves pooling all mutations of different types and contexts from cancer samples into a discrete distribution. If multiple cancer samples are available, their context-dependent mutations can be represented in the form of a nonnegative matrix. This matrix can be further decomposed into components (mutational signatures) which ideally should describe individual mutagenic factors. Several computational methods have been proposed for solving this decomposition problem. The first implementation of Non-negative Matrix Factorization (NMF) method is available in Sanger Institute Mutational Signature Framework in the form of a MATLAB package. On the other hand, if mutations from a single tumor sample are only available, the DeconstructSigs R package and MutaGene server may provide the identification of contributions of different mutational signatures for a single tumor sample. In addition, MutaGene server provides mutagen or cancer-specific mutational background models and signatures that can be applied to calculate expected DNA and protein site mutability to decouple relative contributions of mutagenesis and selection in carcinogenesis.
Synthetic lethality
Synthetic lethality arises when a combination of deficiencies in the expression of two or more genes leads to cell death, whereas a deficiency in only one of these genes does not. The deficiencies can arise through mutations, epigenetic alterations or inhibitors of one of the genes.
The therapeutic potential of synthetic lethality as an efficacious anti-cancer strategy is continually improving. Recently, the applicability of synthetic lethality to targeted cancer therapy has heightened due to the recent work of scientists including Ronald A. DePinho and colleagues, in what is termed 'collateral lethality'. Muller et al. found that passenger genes, with chromosomal proximity to tumor suppressor genes, are collaterally deleted in some cancers. Thus, the identification of collaterally deleted redundant genes carrying out an essential cellular function may be the untapped reservoir for then pursuing a synthetic lethality approach. Collateral lethality therefore holds great potential in identification of novel and selective therapeutic targets in oncology. In 2012, Muller et al. identified that homozygous deletion of redundant-essential glycolytic ENO1 gene in human glioblastoma (GBM) is the consequence of proximity to 1p36 tumor suppressor locus deletions and may hold potential for a synthetic lethality approach to GBM inhibition. ENO1 is one of three homologous genes (ENO2, ENO3) that encodes the mammalian alpha-enolase enzyme. ENO2, which encodes enolase 2, is mostly expressed in neural tissues, leading to the postulation that in ENO1-deleted GBM, ENO2 may be the ideal target as the redundant homologue of ENO1. Muller found that both genetic and pharmacological ENO2 inhibition in GBM cells with homozygous ENO1 deletion elicits a synthetic lethality outcome by selective killing of GBM cells. In 2016, Muller and colleagues discovered antibiotic SF2312 as a highly potent nanomolar-range enolase inhibitor which preferentially inhibits glioma cell proliferation and glycolytic flux in ENO1-deleted cells. SF2312 was shown to be more efficacious than pan-enolase inhibitor PhAH and have more specificity for ENO2 inhibition over ENO1. Subsequent work by the same team showed that the same approach could be applied to pancreatic cancer, whereby homozygously deleted SMAD4 results in the collateral deletion of mitochondrial malic enzyme 2 (ME2), an oxidative decarboxylase essential for redox homeostasis. Dey et al. show that ME2 genomic deletion in pancreatic ductal adenocarcinoma cells results in high endogenous reactive oxygen species, consistent with KRAS-driven pancreatic cancer, and essentially primes ME2-null cells for synthetic lethality by depletion of redundant NAD(P)+-dependent isoform ME3. The effects of ME3 depletion were found to be mediated by inhibition of de novo nucleotide synthesis resulting from AMPK activation and mitochondrial ROS-mediated apoptosis. Meanwhile, Oike et al. demonstrated the generalizability of the concept by targeting redundant essential-genes in process other than metabolism, namely the SMARCA4 and SMARCA2 subunits in the chromatin-remodeling SWI/SNF complex.
Some oncogenes are essential for survival of all cells (not only cancer cells). Thus, drugs that knock out these oncogenes (and thereby kill cancer cells) may also damage normal cells, inducing significant illness. However, other genes may be essential to cancer cells but not to healthy cells.
Treatments based on the principle of synthetic lethality have prolonged the survival of cancer patients, and show promise for future advances in reversal of carcinogenesis. A major type of synthetic lethality operates on the DNA repair defect that often initiates a cancer, and is still present in the tumor cells. Some examples are given here.
BRCA1 or BRCA2 expression is deficient in a majority of high-grade breast and ovarian cancers, usually due to epigenetic methylation of its promoter or epigenetic repression by an over-expressed microRNA (see articles BRCA1 and BRCA2). BRCA1 and BRCA2 are important components of the major pathway for homologous recombinational repair of double-strand breaks. If one or the other is deficient, it increases the risk of cancer, especially breast or ovarian cancer. A back-up DNA repair pathway, for some of the damages usually repaired by BRCA1 and BRCA2, depends on PARP1. Thus, many ovarian cancers respond to an FDA-approved treatment with a PARP inhibitor, causing synthetic lethality to cancer cells deficient in BRCA1 or BRCA2. This treatment is also being evaluated for breast cancer and numerous other cancers in Phase III clinical trials in 2016.
There are two pathways for homologous recombinational repair of double-strand breaks. The major pathway depends on BRCA1, PALB2 and BRCA2 while an alternative pathway depends on RAD52. Pre-clinical studies, involving epigenetically reduced or mutated BRCA-deficient cells (in culture or injected into mice), show that inhibition of RAD52 is synthetically lethal with BRCA-deficiency.
Mutations in genes employed in DNA mismatch repair (MMR) cause a high mutation rate. In tumors, such frequent subsequent mutations often generate "non-self" immunogenic antigens. A human Phase II clinical trial, with 41 patients, evaluated one synthetic lethal approach for tumors with or without MMR defects. The product of gene PD-1 ordinarily represses cytotoxic immune responses. Inhibition of this gene allows a greater immune response. When cancer patients with a defect in MMR in their tumors were exposed to an inhibitor of PD-1, 67–78% of patients experienced immune-related progression-free survival. In contrast, for patients without defective MMR, addition of PD-1 inhibitor generated only 11% of patients with immune-related progression-free survival. Thus inhibition of PD-1 is primarily synthetically lethal with MMR defects.
ARID1A, a chromatin modifier, is required for non-homologous end joining, a major pathway that repairs double-strand breaks in DNA, and also has transcription regulatory roles. ARID1A mutations are one of the 12 most common carcinogenic mutations. Mutation or epigenetically decreased expression of ARID1A has been found in 17 types of cancer. Pre-clinical studies in cells and in mice show that synthetic lethality for ARID1A deficiency occurs by either inhibition of the methyltransferase activity of EZH2, or with addition of the kinase inhibitor dasatinib.
Another approach is to individually knock out each gene in a genome and observe the effect on normal and cancerous cells. If the knockout of an otherwise nonessential gene has little or no effect on healthy cells, but is lethal to cancerous cells containing a mutated oncogene, then the system-wide suppression of the suppressed gene can destroy cancerous cells while leaving healthy ones relatively undamaged. The technique was used to identify PARP-1 inhibitors to treat BRCA1/BRCA2-associated cancers. In this case, the combined presence of PARP-1 inhibition and of the cancer-associated mutations in BRCA genes is lethal only to the cancerous cells.
Databases for cancer research
See also: Databases for oncogenomic researchThe Cancer Genome Project is an initiative to map out all somatic mutations in cancer. The project systematically sequences the exons and flanking splice junctions of the genomes of primary tumors and cancerous cell lines. COSMIC software displays the data generated from these experiments. As of February 2008, the CGP had identified 4,746 genes and 2,985 mutations in 1,848 tumours.
The Cancer Genome Anatomy Project includes information of research on cancer genomes, transcriptomes and proteomes.
Progenetix is an oncogenomic reference database, presenting cytogenetic and molecular-cytogenetic tumor data.
Oncomine has compiled data from cancer transcriptome profiles.
The integrative oncogenomics database IntOGen and the Gitools datasets integrate multidimensional human oncogenomic data classified by tumor type. The first version of IntOGen focused on the role of deregulated gene expression and CNV in cancer. A later version emphasized mutational cancer driver genes across 28 tumor types,. All releases of IntOGen data are made available at the IntOGen database.
The International Cancer Genome Consortium is the biggest project to collect human cancer genome data. The data is accessible through the ICGC website. The BioExpress® Oncology Suite contains gene expression data from primary, metastatic and benign tumor samples and normal samples, including matched adjacent controls. The suite includes hematological malignancy samples for many well-known cancers.
Specific databases for model animals include the Retrovirus Tagged Cancer Gene Database (RTCGD) that compiled research on retroviral and transposon insertional mutagenesis in mouse tumors.
Gene families
Mutational analysis of entire gene families revealed that genes of the same family have similar functions, as predicted by similar coding sequences and protein domains. Two such classes are the kinase family, involved in adding phosphate groups to proteins and the phosphatase family, involved with removing phosphate groups from proteins. These families were first examined because of their apparent role in transducing cellular signals of cell growth or death. In particular, more than 50% of colorectal cancers carry a mutation in a kinase or phosphatase gene. Phosphatidylinositold 3-kinases (PIK3CA) gene encodes for lipid kinases that commonly contain mutations in colorectal, breast, gastric, lung and various other cancers. Drug therapies can inhibit PIK3CA. Another example is the BRAF gene, one of the first to be implicated in melanomas. BRAF encodes a serine/threonine kinase that is involved in the RAS-RAF-MAPK growth signaling pathway. Mutations in BRAF cause constitutive phosphorylation and activity in 59% of melanomas. Before BRAF, the genetic mechanism of melanoma development was unknown and therefore prognosis for patients was poor.
Mitochondrial DNA
Mitochondrial DNA (mtDNA) mutations are linked the formation of tumors. Four types of mtDNA mutations have been identified:
Point mutations
Point mutations have been observed in the coding and non-coding region of the mtDNA contained in cancer cells. In individuals with bladder, head/neck and lung cancers, the point mutations within the coding region show signs of resembling each other. This suggests that when a healthy cell transforms into a tumor cell (a neoplastic transformation) the mitochondria seem to become homogenous. Abundant point mutations located within the non-coding region, D-loop, of the cancerous mitochondria suggest that mutations within this region might be an important characteristic in some cancers.
Deletions
This type of mutation is sporadically detected due to its small size ( < 1 kb). The appearance of certain specific mtDNA mutations (264-bp deletion and 66-bp deletion in the complex 1 subunit gene ND1) in multiple types of cancer provide some evidence that small mtDNA deletions might appear at the beginning of tumorigenesis. It also suggests that the amount of mitochondria containing these deletions increases as the tumor progresses. An exception is a relatively large deletion that appears in many cancers (known as the "common deletion"), but more mtDNA large scale deletions have been found in normal cells compared to tumor cells. This may be due to a seemingly adaptive process of tumor cells to eliminate any mitochondria that contain these large scale deletions (the "common deletion" is > 4 kb).
Insertions
Two small mtDNA insertions of ~260 and ~520 bp can be present in breast cancer, gastric cancer, hepatocellular carcinoma (HCC) and colon cancer and in normal cells. No correlation between these insertions and cancer are established.
Copy number mutations
The characterization of mtDNA via real-time polymerase chain reaction assays shows the presence of quantitative alteration of mtDNA copy number in many cancers. Increase in copy number is expected to occur because of oxidative stress. On the other hand, decrease is thought to be caused by somatic point mutations in the replication origin site of the H-strand and/or the D310 homopolymeric c-stretch in the D-loop region, mutations in the p53 (tumor suppressor gene) mediated pathway and/or inefficient enzyme activity due to POLG mutations. Any increase/decrease in copy number then remains constant within tumor cells. The fact that the amount of mtDNA is constant in tumor cells suggests that the amount of mtDNA is controlled by a much more complicated system in tumor cells, rather than simply altered as a consequence of abnormal cell proliferation. The role of mtDNA content in human cancers apparently varies for particular tumor types or sites.
| Cancer Type | Location of Point mutations | Nucleotide Position of Deletions | Increase of mtDNA copy # | Decrease of mtDNA copy # | |||
|---|---|---|---|---|---|---|---|
| D-Loop | mRNAs | tRNAs | rRNAs | ||||
| Bladder | X | X | X | 15,642-15,662 | |||
| Breast | X | X | X | X | 8470-13,447 and 8482-13459 | X | |
| Head and neck | X | X | X | X | 8470-13,447 and 8482-13459 | X | |
| Oral | X | X | 8470-13,447 and 8482-13459 | ||||
| Hepatocellular carcinoma (HCC) | X | X | X | X | 306-556 and 3894-3960 | X | |
| Esophageal | X | X | X | 8470-13,447 and 8482-13459 | X | ||
| Gastric | X | X | X | 298-348 | X | ||
| Prostate | X | X | 8470-13,447 and 8482-13459 | X | |||
57.7% (500/867) contained somatic point putations and of the 1172 mutations surveyed 37.8% (443/1127) were located in the D-loop control region, 13.1% (154/1172) were located in the tRNA or rRNA genes and 49.1% (575/1127) were found in the mRNA genes needed for producing complexes required for mitochondrial respiration.
Diagnostic applications
Some anticancer drugs target mtDNA and have shown positive results in killing tumor cells. Research has used mitochondrial mutations as biomarkers for cancer cell therapy. It is easier to target mutation within mitochondrial DNA versus nuclear DNA because the mitochondrial genome is much smaller and easier to screen for specific mutations. MtDNA content alterations found in blood samples might be able to serve as a screening marker for predicting future cancer susceptibility as well as tracking malignant tumor progression. Along with these potential helpful characteristics of mtDNA, it is not under the control of the cell cycle and is important for maintaining ATP generation and mitochondrial homeostasis. These characteristics make targeting mtDNA a practical therapeutic strategy.
Cancer biomarkers
Several biomarkers can be useful in cancer staging, prognosis and treatment. They can range from single-nucleotide polymorphisms (SNPs), chromosomal aberrations, changes in DNA copy number, microsatellite instability, promoter region methylation, or even high or low protein levels. Between 2013 and 2019 only 6.8% of people with cancer in 2 US states underwent genetic testing, suggesting broad under-utilization of information that could improve treatment decisions and patient outcomes.
See also
References
- ^ Strausberg RL, Simpson AJ, Old LJ, Riggins GJ (May 2004). "Oncogenomics and the development of new cancer therapies". Nature. 429 (6990): 469–74. Bibcode:2004Natur.429..469S. doi:10.1038/nature02627. PMID 15164073. S2CID 37628107.
- Ting AH, McGarvey KM, Baylin SB (2006). "The cancer epigenome—components and functional correlates". Genes Dev. 20 (23): 3215–31. doi:10.1101/gad.1464906. PMID 17158741.
- Jones PA, Baylin SB (2007). "The epigenomics of cancer". Cell. 128 (4): 683–92. doi:10.1016/j.cell.2007.01.029. PMC 3894624. PMID 17320506.
- Li D, Zhang B, Xing X, Wang T (2015). "Combining MeDIP-seq and MRE-seq to investigate genome-wide CpG methylation". Methods. 72: 29–40. doi:10.1016/j.ymeth.2014.10.032. PMC 4300244. PMID 25448294.
- Wei J, Li G, Dang S, Zhou Y, Zeng K, Liu M (2016). "Discovery and Validation of Hypermethylated Markers for Colorectal Cancer". Dis. Markers. 2016: 2192853. doi:10.1155/2016/2192853. PMC 4963574. PMID 27493446.
- ^ Strausberg RL, Simpson AJ (January 2010). "Whole-genome cancer analysis as an approach to deeper understanding of tumour biology". Br. J. Cancer. 102 (2): 243–8. doi:10.1038/sj.bjc.6605497. PMC 2816661. PMID 20029419.
- Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW (2013). "Cancer genome landscapes". Science. 339 (6127): 1546–58. Bibcode:2013Sci...339.1546V. doi:10.1126/science.1235122. PMC 3749880. PMID 23539594.
- Luo Y, Wong CJ, Kaz AM, Dzieciatkowski S, Carter KT, Morris SM, Wang J, Willis JE, Makar KW, Ulrich CM, Lutterbaugh JD, Shrubsole MJ, Zheng W, Markowitz SD, Grady WM (2014). "Differences in DNA methylation signatures reveal multiple pathways of progression from adenoma to colorectal cancer". Gastroenterology. 147 (2): 418–29.e8. doi:10.1053/j.gastro.2014.04.039. PMC 4107146. PMID 24793120.
- Ley TJ, Mardis ER, Ding L, Fulton B, McLellan MD, Chen K, et al. (November 2008). "DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome". Nature. 456 (7218): 66–72. Bibcode:2008Natur.456...66L. doi:10.1038/nature07485. PMC 2603574. PMID 18987736.
- ^ Peikoff, Kira (2015-10-16). "What Miraculous Recoveries Tell Us About Beating Cancer". Popular Mechanics. Retrieved 2016-04-28.
- Bardelli A.; Velculescu V.E. (2005). "Mutational analysis of gene families in human cancer". Current Opinion in Genetics & Development. 15 (1): 5–12. doi:10.1016/j.gde.2004.12.009. PMID 15661527.
- Benvenuti S.; Arena S.; Bardelli A. (2005). "Identification of cancer genes by mutational profiling of tumor genomes". FEBS Letters. 579 (8): 1884–1890. doi:10.1016/j.febslet.2005.02.015. PMID 15763568. S2CID 31708201.
- Shih I.M.; Wang T.L. (2005). "Apply innovative technologies to explore cancer genome". Current Opinion in Oncology. 17 (1): 33–38. doi:10.1097/01.cco.0000147382.97085.e4. PMID 15608510. S2CID 39104975.
- Greshock J, Naylor TL, Margolin A, Diskin S, Cleaver SH, Futreal PA, et al. (January 2004). "1-Mb resolution array-based comparative genomic hybridization using a BAC clone set optimized for cancer gene analysis". Genome Res. 14 (1): 179–87. doi:10.1101/gr.1847304. PMC 314295. PMID 14672980.
- Lucito R, Healy J, Alexander J, Reiner A, Esposito D, Chi M, et al. (October 2003). "Representational oligonucleotide microarray analysis: a high-resolution method to detect genome copy number variation". Genome Res. 13 (10): 2291–305. doi:10.1101/gr.1349003. PMC 403708. PMID 12975311.
- Hu M, Yao J, Polyak K (2006). "Methylation-specific digital karyotyping". Nat Protoc. 1 (3): 1621–36. doi:10.1038/nprot.2006.278. PMID 17406428. S2CID 10554933.
- Körner H, Epanchintsev A, Berking C, Schuler-Thurner B, Speicher MR, Menssen A, Hermeking H (January 2007). "Digital karyotyping reveals frequent inactivation of the dystrophin/DMD gene in malignant melanoma". Cell Cycle. 6 (2): 189–98. doi:10.4161/cc.6.2.3733. PMID 17314512.
- Volik S, Zhao S, Chin K, Brebner JH, Herndon DR, Tao Q, et al. (June 2003). "End-sequence profiling: sequence-based analysis of aberrant genomes". Proc. Natl. Acad. Sci. U.S.A. 100 (13): 7696–701. Bibcode:2003PNAS..100.7696V. doi:10.1073/pnas.1232418100. PMC 164650. PMID 12788976.
- Van, de Vijver M.J.; et al. (2002). "A gene-expression signature as a predictor of survival in breast cancer". New England Journal of Medicine. 347 (25): 1999–2009. doi:10.1056/NEJMoa021967. hdl:1874/15577. PMID 12490681.
- van 't Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Bernards R, Friend SH (2003). "Expression profiling predicts outcome in breast cancer". Breast Cancer Res. 5 (1): 57–8. doi:10.1186/bcr562. PMC 154139. PMID 12559048.
- Xu Q.; Lee C. (2003). "Discovery of novel splice forms and functional analysis of cancer-specific alternative splicing in human expressed sequences". Nucleic Acids Research. 31 (19): 5635–5643. doi:10.1093/nar/gkg786. PMC 206480. PMID 14500827.
- Gonzalez-Perez A, Mustonen V, Reva B, Ritchie GR, Creixell P, Karchin R, et al. (August 2013). "Computational approaches to identify functional genetic variants in cancer genomes". Nat. Methods. 10 (8): 723–9. doi:10.1038/nmeth.2562. PMC 3919555. PMID 23900255.
- Hanash SM (September 2000). "Operomics: molecular analysis of tissues from DNA to RNA to protein". Clin. Chem. Lab. Med. 38 (9): 805–13. doi:10.1515/CCLM.2000.116. PMID 11097332. S2CID 34163524.
- Peeper D, Berns A (June 2006). "Cross-species oncogenomics in cancer gene identification". Cell. 125 (7): 1230–3. doi:10.1016/j.cell.2006.06.018. PMID 16814709.
- Rogozin IB, Pavlov YI, Goncearenco A, De S, Lada AG, Poliakov E, Panchenko AR, Cooper DN (November 2018). "Mutational signatures and mutable motifs in cancer genomes". Brief. Bioinformatics. 19 (6): 1085–1101. doi:10.1093/bib/bbx049. PMC 6454500. PMID 28498882.
- Gao D, Herman JG, Guo M (2016). "The clinical value of aberrant epigenetic changes of DNA damage repair genes in human cancer". Oncotarget. 7 (24): 37331–37346. doi:10.18632/oncotarget.7949. PMC 5095080. PMID 26967246.
- Kastan MB (2008). "DNA damage responses: mechanisms and roles in human disease: 2007 G.H.A. Clowes Memorial Award Lecture" (PDF). Mol. Cancer Res. 6 (4): 517–24. doi:10.1158/1541-7786.MCR-08-0020. PMID 18403632.
- Bernstein, C; Prasad, AR; Nfonsam, V; Bernstein, H. (2013). "Chapter 16: DNA Damage, DNA Repair and Cancer". In Chen, Clark (ed.). New Research Directions in DNA Repair. BoD – Books on Demand. p. 413. ISBN 978-953-51-1114-6.
- O'Hagan HM, Mohammad HP, Baylin SB (2008). "Double strand breaks can initiate gene silencing and SIRT1-dependent onset of DNA methylation in an exogenous promoter CpG island". PLOS Genetics. 4 (8): e1000155. doi:10.1371/journal.pgen.1000155. PMC 2491723. PMID 18704159.
- Cuozzo C, Porcellini A, Angrisano T, et al. (July 2007). "DNA damage, homology-directed repair, and DNA methylation". PLOS Genetics. 3 (7): e110. doi:10.1371/journal.pgen.0030110. PMC 1913100. PMID 17616978.
- Coulondre C, Miller JH, Farabaugh PJ, Gilbert W (August 1978). "Molecular basis of base substitution hotspots in Escherichia coli". Nature. 274 (5673): 775–80. Bibcode:1978Natur.274..775C. doi:10.1038/274775a0. PMID 355893. S2CID 4165194.
- Cooper DN, Youssoufian H (February 1988). "The CpG dinucleotide and human genetic disease". Hum. Genet. 78 (2): 151–5. doi:10.1007/bf00278187. PMID 3338800. S2CID 41948691.
- ^ Rogozin IB, Kolchanov NA (November 1992). "Somatic hypermutagenesis in immunoglobulin genes. II. Influence of neighbouring base sequences on mutagenesis". Biochim. Biophys. Acta. 1171 (1): 11–8. doi:10.1016/0167-4781(92)90134-l. ISSN 0006-3002. PMID 1420357.
- Rogozin IB, Pavlov YI, Bebenek K, Matsuda T, Kunkel TA (June 2001). "Somatic mutation hotspots correlate with DNA polymerase eta error spectrum". Nat. Immunol. 2 (6): 530–6. doi:10.1038/88732. ISSN 1529-2908. PMID 11376340. S2CID 12807889.
- Nik-Zainal S, Alexandrov LB, Wedge DC, Van Loo P, Greenman CD, Raine K, et al. (May 2012). "Mutational processes molding the genomes of 21 breast cancers". Cell. 149 (5): 979–93. doi:10.1016/j.cell.2012.04.024. PMC 3414841. PMID 22608084.
- Alexandrov LB, Nik-Zainal S, Wedge DC, Campbell PJ, Stratton MR (January 2013). "Deciphering signatures of mutational processes operative in human cancer". Cell Rep. 3 (1): 246–59. doi:10.1016/j.celrep.2012.12.008. PMC 3588146. PMID 23318258.
- Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C (February 2016). "DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution". Genome Biol. 17: 31. doi:10.1186/s13059-016-0893-4. PMC 4762164. PMID 26899170.
- Goncearenco A, Rager SL, Li M, Sang QX, Rogozin IB, Panchenko AR (July 2017). "Exploring background mutational processes to decipher cancer genetic heterogeneity". Nucleic Acids Res. 45 (W1): W514 – W522. doi:10.1093/nar/gkx367. PMC 5793731. PMID 28472504.
- ^ Muller FL, Colla S, Aquilanti E, Manzo VE, Genovese G, Lee J, et al. (August 2012). "Passenger deletions generate therapeutic vulnerabilities in cancer". Nature. 488 (7411): 337–42. Bibcode:2012Natur.488..337M. doi:10.1038/nature11331. PMC 3712624. PMID 22895339.
- Muller FL, Aquilanti EA, DePinho RA (November 2015). "Collateral Lethality: A new therapeutic strategy in oncology". Trends Cancer. 1 (3): 161–173. doi:10.1016/j.trecan.2015.10.002. PMC 4746004. PMID 26870836.
- Poyner RR, Reed GH (August 1992). "Structure of the bis divalent cation complex with phosphonoacetohydroxamate at the active site of enolase". Biochemistry. 31 (31): 7166–73. doi:10.1021/bi00146a020. PMID 1322695.
- Joseph J, Cruz-Sánchez FF, Carreras J (June 1996). "Enolase activity and isoenzyme distribution in human brain regions and tumors". J. Neurochem. 66 (6): 2484–90. doi:10.1046/j.1471-4159.1996.66062484.x. PMID 8632173. S2CID 24655147.
- ^ Leonard PG, Satani N, Maxwell D, Lin YH, Hammoudi N, Peng Z, et al. (December 2016). "SF2312 is a natural phosphonate inhibitor of enolase". Nat. Chem. Biol. 12 (12): 1053–1058. doi:10.1038/nchembio.2195. PMC 5110371. PMID 27723749.
- ^ Dey P, Baddour J, Muller F, Wu CC, Wang H, Liao WT, et al. (February 2017). "Genomic deletion of malic enzyme 2 confers collateral lethality in pancreatic cancer". Nature. 542 (7639): 119–123. Bibcode:2017Natur.542..119D. doi:10.1038/nature21052. PMC 5398413. PMID 28099419.
- Liou GY, Döppler H, DelGiorno KE, Zhang L, Leitges M, Crawford HC, Murphy MP, Storz P (March 2016). "Mutant KRas-Induced Mitochondrial Oxidative Stress in Acinar Cells Upregulates EGFR Signaling to Drive Formation of Pancreatic Precancerous Lesions". Cell Rep. 14 (10): 2325–36. doi:10.1016/j.celrep.2016.02.029. PMC 4794374. PMID 26947075.
- Oike T, Ogiwara H, Tominaga Y, Ito K, Ando O, Tsuta K, et al. (September 2013). "A synthetic lethality-based strategy to treat cancers harboring a genetic deficiency in the chromatin remodeling factor BRG1". Cancer Res. 73 (17): 5508–18. doi:10.1158/0008-5472.CAN-12-4593. PMID 23872584.
- Murata S, Zhang C, Finch N, Zhang K, Campo L, Breuer EK (2016). "Predictors and Modulators of Synthetic Lethality: An Update on PARP Inhibitors and Personalized Medicine". Biomed Res Int. 2016: 2346585. doi:10.1155/2016/2346585. PMC 5013223. PMID 27642590.
- Lok BH, Carley AC, Tchang B, Powell SN (2013). "RAD52 inactivation is synthetically lethal with deficiencies in BRCA1 and PALB2 in addition to BRCA2 through RAD51-mediated homologous recombination". Oncogene. 32 (30): 3552–8. doi:10.1038/onc.2012.391. PMC 5730454. PMID 22964643.
- Cramer-Morales K, Nieborowska-Skorska M, Scheibner K, Padget M, Irvine DA, Sliwinski T, Haas K, Lee J, Geng H, Roy D, Slupianek A, Rassool FV, Wasik MA, Childers W, Copland M, Müschen M, Civin CI, Skorski T (2013). "Personalized synthetic lethality induced by targeting RAD52 in leukemias identified by gene mutation and expression profile". Blood. 122 (7): 1293–304. doi:10.1182/blood-2013-05-501072. PMC 3744994. PMID 23836560.
- Eshleman JR, Lang EZ, Bowerfind GK, Parsons R, Vogelstein B, Willson JK, Veigl ML, Sedwick WD, Markowitz SD (1995). "Increased mutation rate at the hprt locus accompanies microsatellite instability in colon cancer". Oncogene. 10 (1): 33–7. PMID 7824277.
- Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. (2015). "PD-1 Blockade in Tumors with Mismatch-Repair Deficiency". N. Engl. J. Med. 372 (26): 2509–20. doi:10.1056/NEJMoa1500596. PMC 4481136. PMID 26028255.
- Watanabe R, Ui A, Kanno S, Ogiwara H, Nagase T, Kohno T, Yasui A (2014). "SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability". Cancer Res. 74 (9): 2465–75. doi:10.1158/0008-5472.CAN-13-3608. PMID 24788099.
- Raab JR, Resnick S, Magnuson T (2015). "Genome-Wide Transcriptional Regulation Mediated by Biochemically Distinct SWI/SNF Complexes". PLOS Genet. 11 (12): e1005748. doi:10.1371/journal.pgen.1005748. PMC 4699898. PMID 26716708.
- Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander ES, Getz G (2014). "Discovery and saturation analysis of cancer genes across 21 tumour types". Nature. 505 (7484): 495–501. Bibcode:2014Natur.505..495L. doi:10.1038/nature12912. PMC 4048962. PMID 24390350.
- Zhang X, Sun Q, Shan M, Niu M, Liu T, Xia B, Liang X, Wei W, Sun S, Zhang Y, Liu XS, Song Q, Yang Y, Ma Y, Liu Y, Yang L, Ren Y, Zhang G, Pang D (2013). "Promoter hypermethylation of ARID1A gene is responsible for its low mRNA expression in many invasive breast cancers". PLOS ONE. 8 (1): e53931. Bibcode:2013PLoSO...853931Z. doi:10.1371/journal.pone.0053931. PMC 3549982. PMID 23349767.
- Wu JN, Roberts CW (2013). "ARID1A mutations in cancer: another epigenetic tumor suppressor?". Cancer Discov. 3 (1): 35–43. doi:10.1158/2159-8290.CD-12-0361. PMC 3546152. PMID 23208470.
- Bitler BG, Aird KM, Garipov A, Li H, Amatangelo M, Kossenkov AV, Schultz DC, Liu Q, Shih IeM, Conejo-Garcia JR, Speicher DW, Zhang R (2015). "Synthetic lethality by targeting EZH2 methyltransferase activity in ARID1A-mutated cancers". Nat. Med. 21 (3): 231–8. doi:10.1038/nm.3799. PMC 4352133. PMID 25686104.
- Kim KH, Kim W, Howard TP, Vazquez F, Tsherniak A, Wu JN, Wang W, Haswell JR, Walensky LD, Hahn WC, Orkin SH, Roberts CW (2015). "SWI/SNF-mutant cancers depend on catalytic and non-catalytic activity of EZH2". Nat. Med. 21 (12): 1491–6. doi:10.1038/nm.3968. PMC 4886303. PMID 26552009.
- Miller RE, Brough R, Bajrami I, Williamson CT, McDade S, Campbell J, et al. (2016). "Synthetic Lethal Targeting of ARID1A-Mutant Ovarian Clear Cell Tumors with Dasatinib" (PDF). Mol. Cancer Ther. 15 (7): 1472–84. doi:10.1158/1535-7163.MCT-15-0554. PMID 27364904.
- Kaelin W.G. (2005). "The concept of synthetic lethality in the context of anticancer therapy". Nature Reviews Cancer. 5 (9): 689–698. doi:10.1038/nrc1691. PMID 16110319. S2CID 3218512.
- O'Connor M.J.; Martin N.M.B.; Smith G.C.M. (2007). "Targeted cancer therapies based on the inhibition of DNA strand break repair". Oncogene. 26 (56): 7816–7824. doi:10.1038/sj.onc.1210879. PMID 18066095. S2CID 33955861.
- Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A (April 2005). "Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy". Nature. 434 (7035): 917–21. Bibcode:2005Natur.434..917F. doi:10.1038/nature03445. PMID 15829967. S2CID 4364706.
- Bryant H.E.; Schultz, Niklas; Thomas, Huw D.; Parker, Kayan M.; Flower, Dan; Lopez, Elena; Kyle, Suzanne; Meuth, Mark; Curtin, Nicola J.; Helleday, Thomas; et al. (2005). "Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase". Nature. 434 (7035): 913–917. Bibcode:2005Natur.434..913B. doi:10.1038/nature03443. PMID 15829966. S2CID 4391043.
- Gundem G, Perez-Llamas C, Jene-Sanz A, Kedzierska A, Islam A, Deu-Pons J, Furney SJ, Lopez-Bigas N (February 2010). "IntOGen: integration and data mining of multidimensional oncogenomic data". Nat. Methods. 7 (2): 92–3. doi:10.1038/nmeth0210-92. hdl:10230/28107. PMID 20111033. S2CID 205417208.
- Gonzalez-Perez A, Perez-Llamas C, Deu-Pons J, Tamborero D, Schroeder MP, Jene-Sanz A, Santos A, Lopez-Bigas N (November 2013). "IntOGen-mutations identifies cancer drivers across tumor types". Nat. Methods. 10 (11): 1081–2. doi:10.1038/nmeth.2642. PMC 5758042. PMID 24037244.
- Rubio-Perez C, Tamborero D, Schroeder MP, Antolín AA, Deu-Pons J, Perez-Llamas C, Mestres J, Gonzalez-Perez A, Lopez-Bigas N (March 2015). "In silico prescription of anticancer drugs to cohorts of 28 tumor types reveals targeting opportunities". Cancer Cell. 27 (3): 382–96. doi:10.1016/j.ccell.2015.02.007. hdl:10230/33093. PMID 25759023.
- Blume-Jensen P, Hunter T (May 2001). "Oncogenic kinase signalling". Nature. 411 (6835): 355–65. Bibcode:2001Natur.411..355B. doi:10.1038/35077225. PMID 11357143. S2CID 4428819.
- Bardelli A, et al. (2003). "Mutational analysis of the tyrosine kinome in colorectal cancers". Science. 300 (5621): 949. doi:10.1126/science.1082596. PMID 12738854. S2CID 85934154.
- Samuels Y, Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S, Yan H, Gazdar A, Powell SM, Riggins GJ, Willson JK, Markowitz S, Kinzler KW, Vogelstein B, Velculescu VE (April 2004). "High frequency of mutations of the PIK3CA gene in human cancers". Science. 304 (5670): 554. doi:10.1126/science.1096502. PMID 15016963. S2CID 10147415.
- Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. (June 2002). "Mutations of the BRAF gene in human cancer" (PDF). Nature. 417 (6892): 949–54. Bibcode:2002Natur.417..949D. doi:10.1038/nature00766. PMID 12068308. S2CID 3071547.
- Danson S.; Lorigan P. (2005). "Improving outcomes in advanced malignant melanoma – Update on systemic therapy". Drugs. 65 (6): 733–743. doi:10.2165/00003495-200565060-00002. PMID 15819587. S2CID 46969987.
- ^ Yu, Man (2012). Somatic Mitochondrial DNA Mutations in Human Cancers. Advances in Clinical Chemistry. Vol. 57. pp. 99–138. doi:10.1016/B978-0-12-394384-2.00004-8. ISBN 9780123943842. PMID 22870588.
- Hung, W.Y.; J.C. Lin; L.M. Lee; et al. (2008). "Tandem duplication/triplication correlated with poly-cytosine stretch variation in human mitochondrial DNA D-loop region". Mutagenesis. 23 (2): 137–142. doi:10.1093/mutage/gen002. PMID 18252697.
- Fliss, M. S.; Usadel, H.; Caballero, O. L.; et al. (2000). "Facile detection of mitochondrial DNA mutations in tumors and bodily fluids". Science. 287 (5460): 2017–2019. Bibcode:2000Sci...287.2017F. doi:10.1126/science.287.5460.2017. PMID 10720328. S2CID 24438279.
- ^ Dani, M.A.; S.U. Dani; S.P. Lima; et al. (2004). "Less ΔmtDNA4977 than normal in various types of tumors suggests that cancer cells are essentially free of this mutation". Genet. Mol. Res. 3 (3): 395–409. PMID 15614730.
- Ye, C.; X.O. Shu; W. Wen; et al. (2008). "Quantitative analysis of mitochondrial DNA 4977-bp deletion in sporadic breast cancer and benign breast diseases". Breast Cancer Res. Treat. 108 (3): 427–434. doi:10.1007/s10549-007-9613-9. PMC 3836503. PMID 17541740.
- Tseng, L.M.; P.H. Yin; C.W. Chi; et al. (2006). "Mitochondrial DNA mutations and mitochondrial DNA depletion in breast cancer". Genes Chromosomes Cancer. 45 (7): 629–638. doi:10.1002/gcc.20326. PMID 16568452. S2CID 21181048.
- Zhu, W.; W. Qin; P. Bradley; A. Wessel; C.L. Puckett; E.R. Sauter (2005). "Mitochondrial DNA mutations in breast cancer tissue and in matched nipple aspirate fluid". Carcinogenesis. 26 (1): 145–152. doi:10.1093/carcin/bgh282. PMID 15375011.
- Zhou S, Kachhap S, Sun W, Wu G, Chuang A, Poeta L, Grumbine L, Mithani SK, Chatterjee A, Koch W, Westra WH, Maitra A, Glazer C, Carducci M, Sidransky D, McFate T, Verma A, Califano JA (May 2007). "Frequency and phenotypic implications of mitochondrial DNA mutations in human squamous cell cancers of the head and neck". Proc. Natl. Acad. Sci. U.S.A. 104 (18): 7540–5. Bibcode:2007PNAS..104.7540Z. doi:10.1073/pnas.0610818104. PMC 1863503. PMID 17456604.
- Poetsch M, Petersmann A, Lignitz E, Kleist B (March 2004). "Relationship between mitochondrial DNA instability, mitochondrial DNA large deletions, and nuclear microsatellite instability in head and neck squamous cell carcinomas". Diagn. Mol. Pathol. 13 (1): 26–32. doi:10.1097/00019606-200403000-00005. PMID 15163006. S2CID 21271445.
- Tan, D.J.; J. Chang; W.L. Chen; et al. (2004). "Somatic mitochondrial DNA mutations in oral cancer of betel quid chewers". Ann. N. Y. Acad. Sci. 1011 (1): 310–316. Bibcode:2004NYASA1011..310T. doi:10.1196/annals.1293.030. PMID 15126307. S2CID 19794015.
- Lee, H.C.; S.H. Li; J.C. Lin; C.C. Wu; D.C. Yeh; Y.H. Wei (2004). "Somatic mutations in the D-loop and decrease in the copy number of mitochondrial DNA in human hepatocellular carcinoma". Mutation Research. 547 (1–2): 71–78. doi:10.1016/j.mrfmmm.2003.12.011. PMID 15013701.
- Yin, P.H.; C.C. Wu; J.C. Lin; C.W. Chi; Y.H. Wei; H.C. Lee (2010). "Somatic mutations of mitochondrial genome in hepatocellular carcinoma". Mitochondrion. 10 (2): 174–182. doi:10.1016/j.mito.2009.12.147. PMID 20006738.
- Tan, D.J.; J. Chang; L.L. Liu; et al. (2006). "Significance of somatic mutations and content alteration of mitochondrial DNA in esophageal cancer". BMC Cancer. 6: 93. doi:10.1186/1471-2407-6-93. PMC 1459869. PMID 16620376.
- Kassauei K, Habbe N, Mullendore ME, Karikari CA, Maitra A, Feldmann G (2006). "Mitochondrial DNA mutations in pancreatic cancer". Int J Gastrointest Cancer. 37 (2–3): 57–64. doi:10.1007/s12029-007-0008-2. PMID 17827523. S2CID 9716204.
- Hung WY, Wu CW, Yin PH, Chang CJ, Li AF, Chi CW, Wei YH, Lee HC (March 2010). "Somatic mutations in mitochondrial genome and their potential roles in the progression of human gastric cancer". Biochim. Biophys. Acta. 1800 (3): 264–70. doi:10.1016/j.bbagen.2009.06.006. PMID 19527772.
- Wu CW, Yin PH, Hung WY, Li AF, Li SH, Chi CW, Wei YH, Lee HC (September 2005). "Mitochondrial DNA mutations and mitochondrial DNA depletion in gastric cancer". Genes Chromosomes Cancer. 44 (1): 19–28. doi:10.1002/gcc.20213. PMID 15892105. S2CID 11009518.
- Yu, J.J.; T. Yan (2010). "Effect of mtDNA mutation on tumor malignant degree in patients with prostate cancer". Aging Male. 13 (3): 159–165. doi:10.3109/13685530903536668. PMID 20136572. S2CID 22017823.
- Gomez-Zaera, M.; J. Abril; L. Gonzalez; et al. (2006). "Identification of somatic and germline mitochondrial DNA sequence variants in prostate cancer patients". Mutation Research. 595 (1–2): 42–51. doi:10.1016/j.mrfmmm.2005.10.012. PMID 16472830.
- Ludwig JA, Weinstein JN (November 2005). "Biomarkers in cancer staging, prognosis and treatment selection". Nat. Rev. Cancer. 5 (11): 845–56. doi:10.1038/nrc1739. PMID 16239904. S2CID 25540232.
- Kurian (July 3, 2023). "Germline Genetic Testing After Cancer Diagnosis". JAMA. 330 (1): 43–51. doi:10.1001/jama.2023.9526. PMC 10242510. PMID 37276540. Retrieved 4 July 2023.