| Revision as of 00:53, 7 October 2007 editArcadian (talk | contribs)163,050 edits {{Urogenital surgical procedures}}← Previous edit | Revision as of 17:58, 26 October 2007 edit undoRussBot (talk | contribs)Bots1,405,741 editsm Robot-assisted fix links to disambiguation page SterilizationNext edit → | ||
| Line 45: | Line 45: | ||
| The doctor will gently insert the tip of the cystoscope into the urethra and slowly glide it up into the bladder. Men may feel a couple of pinches as the scope passes through the prostate into the bladder. | The doctor will gently insert the tip of the cystoscope into the urethra and slowly glide it up into the bladder. Men may feel a couple of pinches as the scope passes through the prostate into the bladder. | ||
| Relaxing the pelvic muscles helps make this part of the test easier. | Relaxing the pelvic muscles helps make this part of the test easier. | ||
| A ] liquid (water, ], or ] solution) will flow through the cystoscope to slowly fill the bladder and stretch it so that the doctor has a better view of the bladder wall. | A ] liquid (water, ], or ] solution) will flow through the cystoscope to slowly fill the bladder and stretch it so that the doctor has a better view of the bladder wall. | ||
| As the bladder reaches capacity, patients typically feel some discomfort and the urge to urinate. | As the bladder reaches capacity, patients typically feel some discomfort and the urge to urinate. | ||
Revision as of 17:58, 26 October 2007

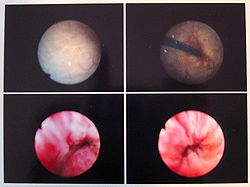
Endoscopy of the urinary bladder via the urethra is called cystoscopy. Diagnostic cystoscopy is usually carried out with local anaesthesia. General anaesthesia is sometimes used for operative cystoscopic procedures.
When a patient has a urinary problem, the doctor may use a cystoscope to see the inside of the bladder and urethra.
The urethra is the tube that carries urine from the bladder to the outside of the body. The cystoscope has lenses like a telescope or microscope. These lenses let the doctor focus on the inner surfaces of the urinary tract. Some cystoscopes use optical fibres (flexible glass fibres) that carry an image from the tip of the instrument to a viewing piece at the other end. The cystoscope is as thick as a pencil and has a light at the tip. Many cystoscopes have extra tubes to guide other instruments for surgical procedures to treat urinary problems.
There are two main types of cystoscopy - flexible and rigid - differing in the flexibility of the cystoscope. Flexible cystoscopy is carried out using local anaesthesia on both sexes. Typically, lidocaine gel (such as the brand name Instillagel) is used as an anaesthetic, instilled in the urethra. Rigid cystoscopy can be performed under the same conditions, but is generally carried out under general anaesthesia, particularly in male subjects, due to the pain caused by the probe.
A doctor may recommend cystoscopy for any of the following conditions:
- Interstitial Cystitis
- Frequent urinary tract infections
- Blood in the urine (hematuria)
- Loss of bladder control (incontinence) or overactive bladder
- Unusual cells found in urine sample
- Need for a bladder catheter
- Painful urination, chronic pelvic pain, or interstitial cystitis
- Urinary blockage such as from prostate enlargement, stricture, or narrowing of the urinary tract
- Stone in the urinary tract
- Unusual growth, polyp, tumor, or cancer
Male and female urinary tracts
If a patient has a stone lodged higher in the urinary tract, the doctor may use a much finer calibre scope called a ureteroscope through the bladder and up into the ureter. (The ureter is the tube that carries urine from the kidney to the bladder). The doctor can then see the stone and remove it with a small basket at the end of a wire which is inserted through an extra tube in the ureteroscope. For larger stones, the doctor may also use the extra tube in the ureteroscope to extend a flexible fiber that carries a laser beam to break the stone into smaller pieces that can then pass out of the body in the urine.
Test Procedures
Doctors may have special instructions, but in most cases, patients are able to eat normally and return to normal activities after the test. Patients are sometimes asked to give a urine sample before the test to check for infection. These patients should avoid urinating for an hour before this part of the test.
Patients generally wear a hospital gown for the examination, and the lower part of the body will be covered with a sterile drape. In most cases, patients lie on their backs with knees raised and apart. A nurse or technician will clean the area around the urethral opening and apply a local anesthetic.
Patients receiving a ureteroscopy may receive a spinal or general anaesthetic. (If you know this will be the case, you will want to arrange a lift home after the test.)
The doctor will gently insert the tip of the cystoscope into the urethra and slowly glide it up into the bladder. Men may feel a couple of pinches as the scope passes through the prostate into the bladder. Relaxing the pelvic muscles helps make this part of the test easier. A sterile liquid (water, saline, or glycine solution) will flow through the cystoscope to slowly fill the bladder and stretch it so that the doctor has a better view of the bladder wall.
As the bladder reaches capacity, patients typically feel some discomfort and the urge to urinate.
The time from insertion of the cystoscope to removal may be only a few minutes, or it may be longer if the doctor finds a stone and decides to remove it. Taking a biopsy (a small tissue sample for examination under a microscope) will also make the procedure last longer. In most cases, the entire examination, including preparation, will take about 15 to 20 minutes.
After the test, patients often have some burning feeling when they urinate and often see small amounts of blood in their urine. Occasionally, patients may feel some lower abdominal pains, reflecting bladder muscle spasms, but these are not common. (These problems should not last more than 24 hours. Tell your doctor if bleeding or pain is severe or if problems last more than a couple of days.)
Common prescriptions to relieve discomfort after the test include:
- Drink 32 fluid ounces (1 L) of water over 2 hours.
- Ask your doctor if you can take a warm bath to relieve the burning feeling.
- Hold a warm, damp washcloth over the urethral opening.
Some doctors will prescribe an antibiotic to take for 1 or 2 days to prevent an infection. However, recent trends have been to discourage this kind of prophylactic treatment (prescribing antibiotics as a preventative when there is no other evidence of infection) because it tends to increase the rate at which bacteria develop resistance to the antibiotic drug. (If you have signs of infection - including pain, chills or fever - call your doctor.)
External links and references
An earlier version of this article was adapted from the public domain NIH Publication No. 01-4800, at http://www.niddk.nih.gov/health/kidney/pubs/cystoscopy/cystoscopy.htm which says, "This e-text is not copyrighted. The clearinghouse encourages users of this e-pub to duplicate and distribute as many copies as desired."
| Tests and procedures involving the female reproductive system | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gynecological surgery | |||||||||||
| Ovaries | |||||||||||
| Fallopian tubes | |||||||||||
| Uterus |
| ||||||||||
| Vagina | |||||||||||
| Vulva | |||||||||||
| Medical imaging | |||||||||||