| Revision as of 10:55, 15 July 2005 editDozenist (talk | contribs)4,869 editsm I think "seen" is better than "known as" because it refers to what is viewed in a clinical setting (as opposed to a microscope)← Previous edit | Revision as of 21:16, 15 July 2005 edit undoEvilphoenix (talk | contribs)Extended confirmed users6,023 edits →Development: copyeditingNext edit → | ||
| Line 22: | Line 22: | ||
| ==Development== | ==Development== | ||
| Enamel formation is part of the overall process of ]. When the tissues of the developing tooth are seen under a microscope, different cellular aggregations can be identified, including structures known as the ], ], and ] {{ref|ross_enamelorgan}}. The generally recognized stages of tooth development are the bud stage, cap stage, bell stage, and crown |
Enamel formation is part of the overall process of ]. When the tissues of the developing tooth are seen under a microscope, different cellular aggregations can be identified, including structures known as the ], ], and ] {{ref|ross_enamelorgan}}. The generally recognized stages of tooth development are the bud stage, cap stage, bell stage, and crown, or calcification, stage. Enamel formation is first seen <!--under the microscope--><!--would it only be seen under the microscope?-->in the crown stage. | ||
| ], or enamel formation, occurs after the first establishment of dentin |
], or enamel formation, occurs after the first establishment of dentin, via cells known as ameloblasts. Human enamel forms at a rate of around 4 ] per day, beginning at the future location of cusps, around the third or fourth month of pregnancy {{ref|cate_formationrate}}. As in all human processes, the creation of enamel is complex, but can generally be divided into two stages {{ref|cate_stages}}. The first stage, called the secretory stage, involves proteins and an organic matrix forming a partially mineralized enamel. The second stage, called the maturation stage, completes enamel mineralization. | ||
| In the secretory stage, |
In the secretory stage, ameloblasts are polarized columnar ]. In the ] of these cells, enamel proteins are released into the surrounding area and contribute to what is known as the enamel matrix, which is then partially mineralized by the enzyme ] {{ref|ross_phosphatase}}. When this first layer is formed, the ameloblasts move away from the dentin, allowing for the development of Tomes’ processes <!--what exactly are tomes processes? A clause of explanation would be helpful here -->at the apical<!--better word?--> pole of the cell. Enamel formation continues around the adjoining ameloblasts, resulting in a walled area, or pit, that houses a Tomes’ process, and also around the end of each Tomes’ process, resulting in a deposition of enamel matrix inside of each pit {{ref|cate_pits}}. The matrix within the pit will eventually become an enamel rod, and the walls will eventually become interrod enamel. The only distinguishing factor between the two is the orientation of the calcium crystals. | ||
| In the maturation stage, the ameloblasts |
In the maturation stage, the ameloblasts transport substances used in the formation of enamel<!--from where to where?-->. Histologically<!--this is a high level vocabulary word, is there a better synonym?-->, the most notable aspect of this phase is that these cells become striated, or have a ruffled border {{ref|ross_ruffled}}. These signs demonstrate that the ameloblasts have changed their function from production, as in the secretory stage, to transportation. Proteins used for the final mineralization process compose most of the transported material. The noteworthy proteins involved are ], ], ], and ] {{ref|ross_proteins}}. During this process, amelogenins and ameloblastins are removed after use, leaving enamelins and tuftelin in the enamel {{ref|ross_proteins2}}. By the end of this stage, the enamel has completed its mineralization. | ||
| At some point before the tooth erupts into the mouth, but after the maturation stage, the ameloblasts are broken down. Consequently, enamel, unlike many other tissues of the body, has no way to regenerate itself {{ref|ross_regenerating}}. After destruction of enamel from decay or injury, neither the body nor a dentist can restore the enamel tissue. Enamel can be affected further by non-pathologic processes. The discoloration of teeth over time can result from exposure to substances such as ], ], and ] {{ref|adha_staining}}. This is partly due to material building up in the enamel, but is also an effect of the underlying dentin becoming sclerotic {{ref|summit_scleroticdentin}}. As a result, tooth color gradually darkens with age. Additionally, enamel becomes less permeable to fluids, less soluble to acid, and contains less water {{ref|summit_enamelless}}. | At some point before the tooth erupts into the mouth, but after the maturation stage, the ameloblasts are broken down. Consequently, enamel, unlike many other tissues of the body, has no way to regenerate itself {{ref|ross_regenerating}}. After destruction of enamel from decay or injury, neither the body nor a dentist can restore the enamel tissue. Enamel can be affected further by non-pathologic processes. The discoloration of teeth over time can result from exposure to substances such as ], ], and ] {{ref|adha_staining}}. This is partly due to material building up in the enamel, but is also an effect of the underlying dentin becoming sclerotic<!--sclerotic? please define briefly--> {{ref|summit_scleroticdentin}}. As a result, tooth color gradually darkens with age. Additionally, enamel becomes less permeable to fluids, less soluble to acid, and contains less water {{ref|summit_enamelless}}. | ||
| {| border="BORDER" | {| border="BORDER" | ||
Revision as of 21:16, 15 July 2005
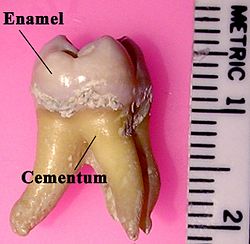
Tooth enamel is the most highly mineralized and hardest substance of the body . Enamel is one of the three major parts of the human tooth, the others being dentin and cementum. It is the normally visible dental tissue of a tooth, and must be supported by underlying dentin. Minerals compose 96% of enamel, with water and organic material composing the rest . Since enamel is semi-translucent, the color of dentin and any restorative dental material underneath the enamel highly affects the outer appearance of the tooth. The color of enamel is a light yellow to grayish white. It varies in thickness over the surface of the tooth. Often, enamel is thickest at the cusp, up to 2.5 mm, and the thickness tapers down to a miniscule amount at its border, which is seen clinically as the cementoenamel junction (CEJ).
Enamel's primary mineral component is hydroxyapatite, which is a crystalline calcium phosphate . The large amount of minerals in enamel accounts for its strength, but also for its brittleness . Thus, dentin, which is less mineralized and less brittle, compensates for enamel and is necessary as a support .
The organic portion of enamel does not contain collagen, as do dentin and bone. Instead, it has two unique classes of proteins called amelogenins and enamelins. While the role of these proteins is not fully understood, it is believed that they aid in the development of enamel by serving as a framework support, among other functions .
Structure

The basic unit of enamel is called an enamel rod . Measuring 4 μm wide to 8 μm high, an enamel rod, formerly called an enamel prism, is a tightly packed mass of hydroxyapatite crystals in an organized pattern . In cross section, it is best compared to a keyhole, with the top, or head, oriented toward the crown of the tooth, and the bottom, or tail, oriented toward the root of the tooth.
The arrangement of the crystals within each enamel rod is highly complex. Both ameloblasts (the cells which initiate enamel formation) and Tomes' processes affect the crystals' pattern. Enamel crystals in the head of the enamel rod are oriented parallel to the long axis of the rod . When found in the tail of the enamel rod, the crystals' orientation diverges slightly from the long axis .
The arrangement of enamel rods is understood more clearly than their internal structure. Enamel rods are found in rows along the tooth, and within each row, the long axis of the enamel rod is generally perpendicular to the underlying dentin . In permanent teeth, the enamel rods near the cementoenamel junction (CEJ) tilt slightly toward the root of the tooth. Understanding enamel orientation is very important in restorative dentistry, because enamel unsupported by underlying dentin is prone to fracture .
The area around the enamel rod is known as interrod enamel. Interrod enamel has the same composition as enamel rod, however a histologic distinction is made between the two because crystal orientation is different in each . The border where the crystals of enamel rods and crystals of interrod enamel meet is called the rod sheath .
Striae of Retzius are stripes that appear on enamel when viewed microscopically in cross-section . Formed from changes in diameter of Tomes’ processes, these stripes demonstrate the growth of enamel, similar to the annual rings on a tree. Perikymata are shallow furrows where the striae of Retzius end . Darker than the other stripes, the neonatal line is a stripe that separates enamel formed before and after birth .
Gnarled enamel is found at the cusps of teeth . Its twisted appearance results from the orientation of enamel rods and the rows in which they lie.
Development
Enamel formation is part of the overall process of tooth development. When the tissues of the developing tooth are seen under a microscope, different cellular aggregations can be identified, including structures known as the enamel organ, dental lamina, and dental papilla . The generally recognized stages of tooth development are the bud stage, cap stage, bell stage, and crown, or calcification, stage. Enamel formation is first seen in the crown stage.
Amelogenesis, or enamel formation, occurs after the first establishment of dentin, via cells known as ameloblasts. Human enamel forms at a rate of around 4 μm per day, beginning at the future location of cusps, around the third or fourth month of pregnancy . As in all human processes, the creation of enamel is complex, but can generally be divided into two stages . The first stage, called the secretory stage, involves proteins and an organic matrix forming a partially mineralized enamel. The second stage, called the maturation stage, completes enamel mineralization.
In the secretory stage, ameloblasts are polarized columnar cells. In the rough endoplasmic reticulum of these cells, enamel proteins are released into the surrounding area and contribute to what is known as the enamel matrix, which is then partially mineralized by the enzyme alkaline phosphatase . When this first layer is formed, the ameloblasts move away from the dentin, allowing for the development of Tomes’ processes at the apical pole of the cell. Enamel formation continues around the adjoining ameloblasts, resulting in a walled area, or pit, that houses a Tomes’ process, and also around the end of each Tomes’ process, resulting in a deposition of enamel matrix inside of each pit . The matrix within the pit will eventually become an enamel rod, and the walls will eventually become interrod enamel. The only distinguishing factor between the two is the orientation of the calcium crystals.
In the maturation stage, the ameloblasts transport substances used in the formation of enamel. Histologically, the most notable aspect of this phase is that these cells become striated, or have a ruffled border . These signs demonstrate that the ameloblasts have changed their function from production, as in the secretory stage, to transportation. Proteins used for the final mineralization process compose most of the transported material. The noteworthy proteins involved are amelogenins, ameloblastins, enamelins, and tuftelins . During this process, amelogenins and ameloblastins are removed after use, leaving enamelins and tuftelin in the enamel . By the end of this stage, the enamel has completed its mineralization.
At some point before the tooth erupts into the mouth, but after the maturation stage, the ameloblasts are broken down. Consequently, enamel, unlike many other tissues of the body, has no way to regenerate itself . After destruction of enamel from decay or injury, neither the body nor a dentist can restore the enamel tissue. Enamel can be affected further by non-pathologic processes. The discoloration of teeth over time can result from exposure to substances such as tobacco, coffee, and tea . This is partly due to material building up in the enamel, but is also an effect of the underlying dentin becoming sclerotic . As a result, tooth color gradually darkens with age. Additionally, enamel becomes less permeable to fluids, less soluble to acid, and contains less water .
| Amount of Enamel Formed at Birth | Enamel Mineralization Completed | ||
|---|---|---|---|
| Primary Maxillary Tooth |
Central Incisor | 5/6 | 1.5 months after birth |
| Lateral Incisor | 2/3 | 2.5 months after birth | |
| Canine | 1/3 | 9 months after birth | |
| 1st Molar | Cusps united; occlusal completely calcified and 1/2 to 3/4 crown height |
6 months after birth | |
| 2nd Molar | Cusps united; occlusal incompletely calcified; calcified tissue covers 1/5 to 1⁄4 crown height |
11 months after birth | |
| Primary Mandibular Tooth |
Central Incisor | 3/5 | 2.5 months after birth |
| Lateral Incisor | 3/5 | 3 months after birth | |
| Canine | 1/3 | 9 months after birth | |
| 1st Molar | cusps united; occlusal completely calcified |
5.5 months after birth | |
| 2nd Molar | cusps united; occlusal incompletely calcified |
10 months after birth |
Destruction
The high mineral content of enamel, which makes this tissue the hardest in the human body, also makes it susceptible to a demineralization process which often occurs as dental caries, otherwise known as cavities . Demineralization occurs for several reasons, but the most important cause of tooth decay is the ingestion of sugars.
Sugars from candies, soft drinks, and even fruit juices play a significant role in tooth decay, and consequently in enamel destruction. The mouth contains a great number and variety of bacteria, and when sucrose, the most common of sugars, coats the surface of the mouth, some intraoral bacteria interact with it and form lactic acid, which decreases the pH in the mouth. . Then, the hydroxyapatite crystals of enamel demineralize, allowing for greater bacterial invasion deeper into the tooth. The most important bacteria involved with tooth decay is Streptococcus mutans, but the number and type of bacteria varies with the progress of tooth destruction .
Furthermore, tooth morphology dictates that the most common site for the initiation of dental caries is in the deep grooves, pits, and fissures of enamel. This is expected because these locations are impossible to reach with a toothbrush and allow for bacteria to reside there. When demineralization of enamel occurs, a dentist can use a sharp instrument, such as a dental explorer, and "feel a stick" at the location of the decay. As enamel continues to become less mineralized and is unable to prevent the encroachment of bacteria, the underlying dentin becomes affected as well. When dentin, which normally supports enamel, is destroyed by a physiologic condition or by decay, enamel is unable to compensate for its brittleness and breaks away from the tooth easily.

The extent to which tooth decay is likely, known as cariogenicity, depends on factors such as how retentive the sugar is to the teeth. Contrary to common belief, it is not the amount of sugar ingested but the frequency of sugar ingestion that is the most important factor in the causation of tooth decay. When the pH in the mouth initially decreases from the ingestion of sugars, the enamel is demineralized and left vulnerable for about 30 minutes. Eating a greater quantity of sugar in one sitting does not increase the time of demineralization. Similarly, eating a lesser quantity of sugar in one sitting does not decrease the time of demineralization. Thus, eating a great quantity of sugar at one time in the day is less detrimental than is a very small quantity ingested in many intervals throughout the day. For example, in terms of oral health, it is better to eat a very large dessert at dinnertime than to snack on a single, small bag of candy throughout the entire workday.
In addition to bacterial invasion, enamel is also susceptible to other destructive forces. Bruxism, also known as clenching of or grinding on teeth, destroys enamel very quickly. The wear rate of enamel, called attrition, is 8 micrometers a year from normal factors. A common misperception is that enamel wears away mostly from chewing, but actually teeth rarely touch during chewing. Furthermore, normal tooth contact is compensated physiologically by the periodontal ligaments (pdl) and the arrangement of dental occlusion. The truly destructive forces are the parafunctional movements, as found in bruxism, which can cause irreversible damage to the enamel.
Other non-bacterial processes of enamel destruction include abrasion (involving foreign elements, such as a toothbrushes), erosion (involving chemical processes, such as lemon juice), and possibly abfraction (involving compressive and tensile forces) .
Oral hygiene and fluoride
Considering the vulnerability of enamel to demineralization and the daily menace of sugar ingestion, prevention of tooth decay is the best way to maintain the health of teeth. Most countries have wide use of toothbrushes, which can reduce the number of bacteria and food particles on enamel. Some isolated societies do not have access to toothbrushes, but it is common for those people to use other objects, such as sticks, to clean their teeth. In between two adjacent teeth, floss is used to wipe the enamel surfaces free of plaque and food particles to discourage bacterial growth. Although neither floss nor toothbrushes can penetrate the deep grooves and pits of enamel, good general oral health habits can usually prevent enough bacterial growth to keep tooth decay from starting.

These methods of oral hygiene have been helped greatly by the use of fluoride. Fluoride can be found in many locations naturally, such as the ocean and other water sources. Consequently, many seafood dishes contain fluoride. The recommended dosage of fluoride in drinking water is 1 part per million (ppm) . Fluoride helps prevent dental decay by binding to the hydroxyapatite crystals in enamel . The incorporated fluoride makes enamel more resistant to demineralization and, thus, resistant to decay . Fluoride therapy is used to help teeth prevent dental decay.
Many groups of people have spoken out against fluorinated drinking water. One example used by these advocates is the damage fluoride can do as fluorosis. Fluorosis is a condition resulting from the overexposure to fluoride, especially between the ages of 6 months to 5 years, and appears as mottled enamel . Consequently, the teeth look unsightly and, indeed, the incidence of dental decay in those teeth is very small. However, it is important to note that most substances, even beneficial ones, are detrimental when taken in extreme doses. Where fluoride is found naturally in high concentrations, filters are often used to decrease the amount of fluoride in water. For this reason, codes have been developed by dental professionals to limit the amount of fluoride a person should take . These codes are supported by the American Dental Association and the American Academy of Pediatric Dentistry. The acute toxic dose of fluoride is ~5 mg/kg of body weight. Furthermore, whereas topical fluoride, found in toothpaste and mouthwashes, does not cause fluorosis, its effects are also less pervasive and not as long-lasting as those of systemic fluoride, such as when drinking fluorinated water . For instance, all of a tooth's enamel gains the benefits of fluoride when it is ingested systemically, through fluorinated water or salt fluoridation (a common alternative in Europe). Only some of the outer surfaces of enamel can be reached by topical fluoride. Thus, despite fluoridation's detractors, most dental health care professionals and organizations agree that the inclusion of fluoride in public water has been one of the most effective methods of decreasing the prevalence of tooth decay.
Effects of Dental Procedures on Enamel

Dental Restorations
Most dental restorations involve the removal of enamel. Frequently, the purpose of removal is to gain access to the underlying decay in the dentin or inflammation in the pulp. This is typically the case in amalgam restorations and endodontic treatment.
Nonetheless, enamel can sometimes be removed before there is any decay present. The process of placing dental sealants involves removing healthy enamel in the deep fissures and grooves of a tooth and replacing it with a restorative material . Sealants are unique in that they are preventative restorations for protection from future decay and have shown to reduce the risk of decay by 55% over 7 years .
Aesthetics is another reason for the removal of enamel. Removing enamel is necessary when placing crowns and veneers to enhance the appearance of teeth. In both of these instances, it is important to keep in mind the orientation of enamel rods because it is possible to leave enamel unsupported by underlying dentin, leaving that portion of the prepared teeth more vulnerable to fracture .
Acid-Etching Techniques
Invented in 1955, acid-etching employs dental etchants and is used frequently when bonding dental restoration to teeth . This is important for long-term use of some materials, such as composites and sealants . By dissolving minerals in enamel, etchants remove the outer 10 micrometers on the enamel surface and makes a porous layer 5–50 micrometers deep . This roughens the enamel microscopically and results in a greater surface area on which to bond.
The effects of acid-etching on enamel can vary. Important variables are the amount of time the etchant is applied, the type of etchant used, and the current condition of the enamel .
There are three types of patterns formed by acid-etching . Type 1 is a pattern where predominantly the enamel rods are dissolved; type 2 is a pattern where predominantly the area around the enamel rods are dissolved; and type 3 is a pattern where there is no evidence left of any enamel rods. Besides concluding that type 1 is the most favorable pattern and type 3 the least, the explanation for these different patterns is not known for certain but is most commonly attributed to different crystal orientation in the enamel .
Tooth Whitening
Tooth whitening, or tooth bleaching, procedures attempt to lighten a tooth's color in either of two ways: by chemical or mechanical action .
Working chemically, a bleaching agent is used to carry out an oxidation reaction in the enamel and dentin . The agents most commonly used to intrinsically change the color of teeth are hydrogen peroxide and carbamide peroxide . A tooth whitening product with an overall low pH can put enamel at risk for decay or destruction by demineralization. Consequently, care should be taken and risk evaluated when choosing a product which is very acidic .
Tooth whiteners in toothpastes work through a mechanical action. They have mild abrasives which aid in the removal of stains on enamel. Although this can be an effective method, it does not alter the intrinsic color of teeth .
Microabrasion techniques employ both methods. An acid is used first to weaken the outer 22–27 micrometers of enamel in order to weaken it enough for the subsequent abrasive force . This allows for removal of superficial stains in the enamel. If the discoloration is deeper or in the dentin, this method of tooth whitening will not be successful.
Systemic Conditions Affecting Enamel
There are many different types of Amelogenesis imperfecta. The hypocalcification type, which is the most common, is an autosomal dominant condition that results in enamel that is not completely mineralized . Consequently, enamel easily flakes off the teeth, which appear yellow because of the revealed dentin. The hypoplastic type is X-linked and results in normal enamel that appears in too little quantity, having the same effect as the most common type .
Chronic bilirubin encephalopathy, which can result from erythroblastosis fetalis, is a disease which has numerous effects on an infant, but it can also cause enamel hypoplasia and green staining of enamel .
Enamel hypoplasia is broadly defined to encompass all deviations from normal enamel in its various degrees of absence . The missing enamel could be localized, forming a small pit, or it could be completely absent.
Erythropoietic porphyria is a genetic disease resulting in the deposition of porphyrins throughout the body. These deposits also occur in enamel and leave an appearance described as red in color and fluorescent .
Fluorosis leads to mottled enamel and occurs from overexposure to fluoride .
Tetracycline staining leads to brown bands on the areas of developing enamel. As a result, tetracycline is contraindicated in pregnant women.
Enamel in non-human Animals
For the most part, research has shown that enamel does not vary consistently between humans and non-humans. Enamel formation in animals is almost identical to formation in humans. The enamel organ, including the dental papilla, and ameloblasts function similarly . The variations of enamel that are present are infrequent but sometimes important. Differences exist, certainly, in the morphology, number, and types of teeth among animals.

Dogs are less likely than humans to have tooth decay due to the very high pH of dog saliva, which prevents an acidic environment from forming and the subsequent demineralization of enamel which would occur . In the event that tooth decay does occur (usually from trauma), dogs can receive dental fillings just as humans do. Similar to human teeth, the enamel of dogs is vulnerable to tetracycline staining. Consequently, this risk must be accounted for when tetracycline antibiotic therapy is administered to young dogs . Enamel hypoplasia may also occur in dogs .
The mineral distribution in rodent enamel is different than that of monkeys, dogs, pigs, and humans . In horse teeth, the enamel and dentin layers are intertwined with each other, which increases the strength and decreases the wear rate of those teeth .
See also
Notes
- Michael H. Ross, Gordon I. Kaye, and Wojciech Pawlina, Histology: a Text and Atlas, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2002), p. 441.
- A. R. Ten Cate, Oral Histology: Development, Structure, and Function, 5th ed. (Saint Louis: Mosby-Year Book, 1998), p. 1.
- Ibid., p. 219.
- "Biology of the Human Dentition"
- Cate, Oral Histology, p. 218.
- "Biology of the Human Dentition"
- Cate, Oral Histology, p. 198.
- "Biology of the Human Dentition"
- See note 1 above.
- Cate, Oral Histology, p. 219; Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 441.
- See note 1 above.
- Cate, Oral Histology, p. 224.
- Ibid., p. 224.
- Ibid., p. 219.
- Cate, Oral Histology, p. 221.
- Ibid., p. 224.
- Ibid., p. 230.
- Cate, Oral Histology, p. 76; Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 441.
- Cate, Oral Histology, p. 229.
- Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 443.
- See note 12 above.
- Ibid., p. 197.
- Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 445.
- Cate, Oral Histology, p. 208.
- Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 445.
- Ibid., p. 447.
- Ibid., p. 448.
- Ibid., p. 3.
- American Dental Hygienists' Association, accessed here
- James B. Summitt, J. William Robbins, and Richard S. Schwartz, eds., Fundamentals of Operative Dentistry: A Contemporary Approach, 2nd ed. (Carol Stream , IL: Quintessence Publishing, 2001), p. 2.
- Ibid.
- Major M. Ash and Stanley Nelson, Wheeler’s Dental Anatomy, Physiology, and Occlusion 8th ed. (Philadelphia: W.B. Saunders Co., 2003), p. 54.
- Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 443.
- Ibid., p. 453.
- Ibid.
- Gandara & Truelove. Information found on chart titled, "Definitions of Tooth Surface Loss," and the specific page can be accessed here.
- Dean, Arnold, and Elvove, "Domestic water and dental caries," Public Health Reports 52, no. 32 (1942): 1155–79.
- Cate, Oral Histology, p. 223.
- Ross, Kaye, and Pawlina, Histology: Text and Atlas, p. 453.
- Cate, Oral Histology, p. 216.
- American Dental Association
- E. Newbrun, Fluorides and dental caries (Springfield, IL: Charles C. Thomas publisher, 1986).
- Summitt, Robbins, and Schwartz, Fundamentals of Operative Dentistry, p. 273.
- Ibid., p. 274.
- Ibid., p. 7.
- Ibid., p. 191.
- See note 33 above.
- Summitt, Robbins, and Schwartz, Fundamentals of Operative Dentistry, p. 193.
- Ibid.
- Ibid.
- Cate, Oral Histology, p. 235.
- American Dental Assocation's whitening page found here
- Summitt, Robbins, and Schwartz, Fundamentals of Operative Dentistry, p. 402.
- American Dental Assocation's whitening page notes the intrinsic change and can be accessed here, and Summit et al. lists the two most common agents, p. 403.
- Summitt, Robbins, and Schwartz, Fundamentals of Operative Dentistry, p. 404.
- American Dental Assocation's whitening page found here
- Summitt, Robbins, and Schwartz, Fundamentals of Operative Dentistry, p. 420.
- Edward F. Harris, see section titled "X-Linked Inheritance," in Craniofacial Growth and Development 2002, p. 7.
- Ibid.
- eMedicine. Shelley C. Springer and David J. Annibale. "Kernicterus", page accessed . Last updated November 6, 2004.
- Ash and Stanley, Wheeler’s Dental Anatomy, p. 31.
- eMedicine. Jeanette L. Hebel and Maureen B Poh-Fitzpatrick. "Erythropoietic Porphyria", page accessed . Last updated June 3, 2005.
- See note 35 above.
- R. D. Frandson et al., Anatomy and Physiology of Farm Animals, 5th ed. (Baltimore: Lippincott Williams & Wilkins, 1992), p. 305.
- Chris C. Pinney, The Illustrated Veterinary Guide for Dogs, Cats, Birds, and Exotic Pets (Blue Ridge Summit, PA: TAB Books, 1992), p. 187.
- Ibid.
- Ibid., p. 186.
- Fejerskov, O. on Pubmed. Link can be found here
- Encarta article found here and Randall-Bowman, whose link can be found here
References
- American Dental Association, Council on Access Prevention and Interprofessional Relations., 1995. "Caries diagnosis and risk assessment: a review of preventive strategies and management." Journal of the American Dental Association: 126.
- American Dental Association Website, page on tooth whitening found here
- American Dental Hygienists' Association. "The Oral Health Information page."
- Ash, Major M. and Stanley J. Nelson, 2003. Wheeler’s Dental Anatomy, Physiology, and Occlusion. 8th edition.
- Blackwell, Bonnie, 1996. "Why Teeth Fossilize Better Than Bone."
- Cate, A.R. Ten. Oral Histology: development, structure, and function. 5th ed. 1998. ISBN 0815129521.
- Dean, H.T., F.A. Arnold, and E. Elvove, 1942. "Domestic water and dental caries." Public Health Reports, 57(32): pages 1155-79.
- Encarta Online Encyclopedia. "Teeth." Chris Martin.
- eMedicine homepage
- Fejerskov, O., 1979 "Human dentition and experimental animals." Journal of Dental Research. 58, special issue B, March, 1979: pages 725-734. Abstract found at PubMed
- Frandson, R.D. & T.L. Spurgeon, 1992. Anatomy and Physiology of Farm Animals. 5th edition. Philadelphia, Lea & Febiger. ISBN 0812114353.
- Gandara,B.K. & E.L. Truelove, 1999. "Diagnosis and Management of Dental Erosion." Journal of Contemporary Dental Practice, volume 1 (number 1), October 1999: pages 016-023. Copy of article found here.
- Harris, Edward F., 2002. Craniofacial Growth and Development.
- Johnson, Clarke, 1998. "Biology of the Human Dentition"
- Newbrun, E., 1986. Fluorides and dental caries. 3rd edition. Springfield, Illinois, Charles C. Thomas.
- Pinney, Chris C., 1992. The Illustrated Veterinary Guide for Dogs, Cats, Birds, and Exotic Pets. TAB Books, 1992. ISBN 0070501793.
- Randall-Bowman, 2004. "Gummed Out: Young Horses Lose Many Teeth, Vet Says." April 2004. Article found here.
- Ross, Michael H., Gordon I. Kaye, and Wojciech Pawlina, 2003. Histology: a text and atlas. 4th edition. ISBN 0683302426.
- Summit, James B., J. William Robbins, and Richard S. Schwartz, 2001. Fundamentals of Operative Dentistry: A Contemporary Approach. 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc. ISBN 0867153822.