| Revision as of 19:12, 7 January 2007 view sourceEverSince (talk | contribs)Extended confirmed users7,837 edits →Research findings on violence and schizophrenia: just fixing ref. Not rewording again despite source about general non-adherence not "ceasing" meds + cited source found no main sig effect← Previous edit | Revision as of 20:07, 7 January 2007 view source 75.24.94.219 (talk) →Psychosocial factors: fix spelling errorNext edit → | ||
| Line 172: | Line 172: | ||
| A number of ]es or deficits have been found in people with schizophrenia (and their relatives<ref> Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. ''Schizophrenia Research'', Volume 71, Issue 2, Pages 285-295.</ref>). These include jumping to conclusions when faced with limited or contradictory information; specific biases in reasoning about social situations, for example assuming other people cause things that go wrong (external attribution); difficulty distinguishing inner speech from speech from an external source (source monitoring); difficulty in adjusting speech to the needs of the hearer, related to ] difficulties; difficulties in the very earliest stages of processing visual information (including reduced ]); difficulty with attention e.g. being more easily distracted, ] towards threat. Some of these tendencies have been shown to worsen or appear when under emotional stress or in confusing situations. As with the related neurological findings, they are not shown by all individuals with a diagnosis of schizophrenia and it is not clear how specific they are to schizophrenia or to particular symptoms<ref> What causes the onset of psychosis? ''Schizophr Res'', 79(1), 23-34.</ref>. The findings regarding schizophrenia are reliable and consistent, however, to the extent that they can be viewed as diagnostic<ref> Should cognitive deficit be a diagnostic criterion for schizophrenia? ''Journal of Psychiatry and Neuroscience'' March; 29(2): 102–113.</ref> | A number of ]es or deficits have been found in people with schizophrenia (and their relatives<ref> Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. ''Schizophrenia Research'', Volume 71, Issue 2, Pages 285-295.</ref>). These include jumping to conclusions when faced with limited or contradictory information; specific biases in reasoning about social situations, for example assuming other people cause things that go wrong (external attribution); difficulty distinguishing inner speech from speech from an external source (source monitoring); difficulty in adjusting speech to the needs of the hearer, related to ] difficulties; difficulties in the very earliest stages of processing visual information (including reduced ]); difficulty with attention e.g. being more easily distracted, ] towards threat. Some of these tendencies have been shown to worsen or appear when under emotional stress or in confusing situations. As with the related neurological findings, they are not shown by all individuals with a diagnosis of schizophrenia and it is not clear how specific they are to schizophrenia or to particular symptoms<ref> What causes the onset of psychosis? ''Schizophr Res'', 79(1), 23-34.</ref>. The findings regarding schizophrenia are reliable and consistent, however, to the extent that they can be viewed as diagnostic<ref> Should cognitive deficit be a diagnostic criterion for schizophrenia? ''Journal of Psychiatry and Neuroscience'' March; 29(2): 102–113.</ref> | ||
| A number of emotional factors have been implicated in schizophrenia, with some models putting them at the core of the disorder. It was thought that the appearance of blunted affect meant that sufferers did not experience strong emotions, but more recent studies indicate there is often a normal or even heightened level of emotionality, particularly in response to negative events or stressful social situations.<ref> Affective reactivity of speech and emotional experience in patients with schizophrenia. ''Schizophr Res'', 1;69(1):7-14.</ref> Some theories suggest positive symptoms of schizophrenia can result from or be worsened by negative emotions, including depressed feelings and low ]<ref> Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. ''Schizophr Res''. Sep;86(1-3):181-8.</ref> and feelings of |
A number of emotional factors have been implicated in schizophrenia, with some models putting them at the core of the disorder. It was thought that the appearance of blunted affect meant that sufferers did not experience strong emotions, but more recent studies indicate there is often a normal or even heightened level of emotionality, particularly in response to negative events or stressful social situations.<ref> Affective reactivity of speech and emotional experience in patients with schizophrenia. ''Schizophr Res'', 1;69(1):7-14.</ref> Some theories suggest positive symptoms of schizophrenia can result from or be worsened by negative emotions, including depressed feelings and low ]<ref> Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. ''Schizophr Res''. Sep;86(1-3):181-8.</ref> and feelings of vulnerability, inferiority or ].<ref> A Cognitive Model of Schizophrenia, ''Journal of Cognitive Psychotherapy'', 18 (3), 281-288.</ref> Chronic negative feelings and maladaptive coping skills may explain some of the association between psychosocial stressors and symptomology.<ref> Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping. | ||
| Schizophr Res. Apr 1;60(2-3):271-83.</ref> Critical and controlling behaviour by significant others (high ]) causes increased emotional arousal<ref> Psychosocial factors, arousal and schizophrenic relapse. The psychophysiological data. | Schizophr Res. Apr 1;60(2-3):271-83.</ref> Critical and controlling behaviour by significant others (high ]) causes increased emotional arousal<ref> Psychosocial factors, arousal and schizophrenic relapse. The psychophysiological data. | ||
| ''Br J Psychiatry''. 161:3-11</ref> and lowered self-esteem<ref> Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. | ''Br J Psychiatry''. 161:3-11</ref> and lowered self-esteem<ref> Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. | ||
Revision as of 20:07, 7 January 2007
Medical condition| Schizophrenia | |
|---|---|
| Specialty | Psychiatry, clinical psychology |
Schizophrenia (from the Greek word σχιζοφρένεια, "split mind") is a psychiatric diagnosis that describes a mental disorder characterized by impairments in the perception or expression of reality and by significant social or occupational dysfunction. A person experiencing schizophrenia is typically characterized as demonstrating disorganized thinking, and as experiencing delusions or auditory hallucinations.
Although the disorder is primarily thought to affect cognition, it can also contribute to chronic problems with behavior and emotion. Due to the many possible combinations of symptoms, heated debate is ongoing about whether the diagnosis necessarily or adequately describes a disorder, or alternatively whether it might represent a number of disorders. For this reason, Eugen Bleuler deliberately called the disease "the schizophrenias" plural, when he coined the present name.
Diagnosis is based on the self-reported experiences of the patient, in combination with secondary signs observed by a psychiatrist, clinical psychologist or other clinician. No medical test for schizophrenia exists. Studies suggest that genetics, early environment, neurobiology and psychological and social processes are important contributory factors. Current psychiatric research into the development of the disorder often focuses on the role of neurobiology, although a reliable and identifiable organic cause has not been found. In the absence of a confirmed specific pathology underlying the diagnosis, some question the legitimacy of schizophrenia's status as a disease. Furthermore, some propose that the perceptions and feelings involved are meaningful and do not necessarily involve impairment.
The term schizophrenia translates roughly as "splitting of the mind", and comes from the Greek σχίζω (schizo, "to split" or "to divide") and φρήν (phrēn, "mind"). Despite its etymology, schizophrenia is not synonymous with dissociative identity disorder, also known as multiple personality disorder or "split personality"; in popular culture the two are often confused. People with schizophrenia are generally not more violent or dangerous than other members of the population.
Patients diagnosed with schizophrenia are highly likely to be diagnosed with other disorders. The lifetime prevalence of substance abuse is typically around 40%. Comorbidity is also high with clinical depression, anxiety disorders, and social problems, and a generally decreased life expectancy is also present. Patients diagnosed with schizophrenia typically live 10-12 years less than their healthy counterparts, owing to increased physical health problems and a high suicide rate. Unemployment and poverty are common.
Overview
Schizophrenia is often described in terms of "positive" and "negative" symptoms. Positive symptoms include delusions, auditory hallucinations and thought disorder and are typically regarded as manifestations of psychosis. Negative symptoms are so named because they are considered to be the loss or absence of normal traits or abilities, and include features such as flat, blunted or constricted affect and emotion, poverty of speech and lack of motivation. Some models of schizophrenia include formal thought disorder and planning difficulties in a third group, a "disorganization syndrome".
Additionally, neurocognitive deficits may be present. These may take the form of reduced or impaired psychological functions such as memory, attention, problem-solving, executive function or social cognition.
Onset of schizophrenia typically occurs in late adolescence or early adulthood, with males tending to show symptoms earlier than females.
In 1893 psychiatrist Emil Kraepelin was the first to draw a distinction between what he termed dementia praecox ("premature dementia") and other psychotic illnesses. In 1908, "dementia praecox" was renamed "schizophrenia" by psychiatrist Eugen Bleuler, who discovered that the disorder is not a form of dementia.
The diagnostic category of schizophrenia has been widely criticised as lacking in scientific validity or reliability, consistent with evidence of poor levels of consistency in diagnostic practices and the use of criteria. One alternative suggests that the problems and issues making up the diagnosis of schizophrenia would be better addressed as individual dimensions along which everyone varies, such that there is a spectrum or continuum rather than a cut-off between normal and ill. This approach appears consistent with research on schizotypy and of a relatively high prevalence of psychotic experiences and delusional beliefs amongst the general public.
Although no common cause of schizophrenia has been identified in all individuals diagnosed with the condition, currently most researchers and clinicians believe it results from a combination of both brain vulnerabilities (either inherited or acquired) and stressful life-events. This widely-adopted approach is known as the 'stress-vulnerability' model, and much scientific debate now focuses on how much each of these factors contributes to the development and maintenance of schizophrenia.
It is also thought that processes in early neurodevelopment are important, particularly prenatal processes. In adult life, particular importance has been placed upon the function (or malfunction) of dopamine in the mesolimbic pathway in the brain. This theory, known as the dopamine hypothesis of schizophrenia largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, reduced psychotic symptoms. However, this theory is now thought to be overly simplistic as a complete explanation. These drugs have now been developed further and antipsychotic medication is commonly used as a first-line treatment. Although effective in many cases, these medications are not well tolerated by some patients due to significant side-effects. The positive symptoms are more responsive to medications; negative symptoms being less so.
Differences in brain structure have been found between people with schizophrenia and those without. However, these tend only to be reliable on the group level and, due to the significant variability between individuals, may not be reliably present in any particular individual. Significant brain atrophy and enlarged ventricles are the most conspicuous of such differences.
History
Accounts that may relate to symptoms of schizophrenia date back as far as 2000 BC in the Book of Hearts, part of the ancient Ebers papyrus. However, a recent study into the ancient Greek and Roman literature showed that, while the general population probably had an awareness of psychotic disorders, there was no recorded condition that would meet the modern diagnostic criteria for schizophrenia in these societies.
This nonspecific concept of "madness" has been around for many thousands of years, but schizophrenia was only classified as a distinct mental disorder by Kraepelin in 1893. He was the first to make a distinction in the psychotic disorders between what he called dementia praecox (a term first used by psychiatrist Benedict A. Morel) and manic depression. Kraepelin believed that dementia praecox was primarily a disease of the brain, and particularly a form of dementia. Kraepelin named the disorder 'dementia praecox' (early dementia) to distinguish it from other forms of dementia (such as Alzheimer's disease) which typically occur late in life. He used this term because his studies focused on young adults with dementia.
The term schizophrenia is derived from the Greek words σχίζειν (split) and φρήν (mind) and was coined by Eugene Bleuler in 1908 to refer to the lack of interaction between thought processes and perception. He was also the first to describe the symptoms as "positive" or "negative." Blueler described the main symptoms as 4 "A"'s: flattened Affect, Autism, impaired Association of ideas and Ambivalence. Bleuler suggested the name schizophrenia, as it was obvious that Kraepelin's name was misleading. The word "praecox" implied precocious or early onset, hence premature dementia, as opposed to senile dementia from old age. Bleuler realized the illness was not a dementia as some of his patients improved rather than following a deteriorating course.
With the name 'schizophrenia' Bleuler intended to capture the separation of function between personality, thinking, memory, and perception, however it is commonly misunderstood to mean that affected persons have a 'split personality' (something akin to the character in Robert Louis Stevenson's The Strange Case of Dr Jekyll and Mr Hyde). Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion perhaps arises in part due to the meaning of Bleuler's term 'schizophrenia' (literally 'split' or 'shattered mind'). Interestingly, the first known misuse of this word schizophrenia to mean 'split personality' (in the Jekyll and Hyde sense) was in an article by the poet T. S. Eliot in 1933.
In the first half of the twentieth century schizophrenia was considered by many to be a "hereditary defect", and individuals affected by schizophrenia became subject to eugenics in many countries. Hundreds of thousands were sterilized, with or without consent, the majority in Nazi Germany, the United States, and Scandinavian countries, Many people diagnosed with schizophrenia, together with other people labeled "mentally unfit", were murdered in the Nazi "Operation T-4" program.
Diagnosis
Criteria (signs and symptoms)
Like many mental illnesses, the diagnosis of schizophrenia is based upon the behavior of the person being assessed. There is a list of criteria that must be met for someone to be so diagnosed. These depend on both the presence and duration of certain signs and symptoms.
The most commonly used criteria for diagnosing schizophrenia are from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD). The most recent versions are ICD-10 and DSM-IV-TR.
Below is an abbreviated version of the diagnostic criteria from the DSM-IV-TR; the full version is available here.
To be diagnosed as having schizophrenia, a person must display:
- A) Characteristic symptoms: Two or more of the following, each present for a significant portion of time during a one-month period (or less, if successfully treated)
- delusions
- hallucinations
- disorganized speech (e.g., frequent derailment or incoherence; speaking in abstracts). See thought disorder.
- grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- negative symptoms, i.e., affective flattening (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation).
- Note: Only one Criterion A symptom is required if delusions are bizarre or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other.
- B) Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- C) Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if successfully treated) that meet Criterion A.
Additional criteria (D, E and F) are also given that exclude a diagnosis of schizophrenia if symptoms of mood disorder or pervasive developmental disorder are present. Additionally a diagnosis of schizophrenia is excluded if the symptoms are the direct result of a substance (e.g., abuse of a drug, medication) or a general medical condition.
Subtypes
Historically, schizophrenia in the West was classified into simple, catatonic, hebephrenic, and paranoid. The DSM now contains five sub-classifications of schizophrenia, the ICD-10 identifies 7:
- (295.2/F20.2) catatonic type (prominent psychomotor disturbances are evident. Symptoms can include catatonic stupor and waxy flexibility).
- (295.1/F20.1) disorganized type (where thought disorder and flat affect are present together),
- (295.3/F20.0) paranoid type (where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening is absent),
- (295.6/F20.5) residual type (where positive symptoms are present at a low intensity only) and
- (295.9/F20.3) undifferentiated type (psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types has not been met).
NB: Brackets indicate codes for DSM and ICD-10 diagnostic manuals, respectively. Some older classifications still use "Hebephrenic schizophrenia" instead of "Disorganized schizophrenia".
Deficit Syndrome
Currently, there is debate in the field about a new subtype known as the deficit syndrome. It is not currently included in the DSM-IV-TR, however it has been receiving a great deal of attention in the last 20 years. This subtype is more expansive than the other subtypes as a person can be diagnosed with both paranoid schizophrenia and the deficit syndrome. It is characterized by primary negative symptoms (which means that they cannot be caused by such things as the side-effects of medication or depression). People with the deficit syndrome tend to have extremely flat affect (do not appear to be very emotional), do not have good eye contact, do not enjoy normally pleasurable activities (see dysphoria), and seem to be uninterested in social interaction. (There is, however, conflict in the research on this last point. While people who have been diagnosed with the deficit syndrome report being uninterested in social interaction, in the laboratory, they often report normal reactions to the situations.) Patients who have been diagnosed with the deficit syndrome tend to have a worse prognosis as these symptoms tend to be resistant to medication. This fact has brought much needed attention to negative symptoms (which have traditionally not been viewed as important as the positive symptoms).
Presentation
Symptoms may also be described as 'positive symptoms' (those additional to normal experience and behavior) and 'negative symptoms' (the lack or decline in normal experience or behavior). 'Positive symptoms' describe psychosis and typically include delusions, hallucinations and thought disorder. 'Negative symptoms' describe inappropriate or nonpresent emotion, poverty of speech, and lack of motivation. In three-factor models of schizophrenia, a third symptom grouping, the so-called 'disorganization syndrome', is also given. This considers thought disorder and related disorganized behavior to be in a separate symptom cluster from delusions and hallucinations.
Some symptoms, such as social isolation, may be caused by a number of factors. One possible factor is impairment in social cognition, which is associated with schizophrenia, but isolation may also result from an individual reacting to psychotic symptoms (such as paranoia) or avoiding potentially stressful social situations which may exacerbate mental distress in some people.
It is worth noting that many of the positive or psychotic symptoms may occur in a variety of disorders and not only in schizophrenia. The psychiatrist Kurt Schneider tried to list the particular forms of psychotic symptoms that he thought were particularly useful in distinguishing between schizophrenia and other disorders that could produce psychosis. These are called first rank symptoms or Schneiderian first rank symptoms and include delusions of being controlled by an external force, the belief that thoughts are being inserted into or withdrawn from one's conscious mind, the belief that one's thoughts are being broadcast to other people and hearing hallucinated voices which comment on one's thoughts or actions, or may have a conversation with other hallucinated voices. As with other diagnostic methods, the reliability of 'first rank symptoms' has been questioned, although they remain in use as diagnostic criteria in many countries.
Diagnostic issues and controversies
It has been argued that the diagnostic approach to schizophrenia is flawed, as it relies on an assumption of a clear dividing line between what is considered to be mental illness (fulfilling the diagnostic criteria) and mental health (not fulfilling the criteria). Recently it has been argued, notably by psychiatrist Jim van Os and psychologist Richard Bentall, that this makes little sense, as studies have shown that many people have psychotic experiences and have delusion-like ideas without becoming distressed, disabled or diagnosable by the categorical system (potentially because they interpret their experiences in more positive ways, or hold more pragmatic and commonly accepted beliefs).
Of particular concern is that the decision as to whether a symptom is present is a subjective decision by the person making the diagnosis or relies on an incoherent definition (for example, see the entries on delusions and thought disorder for a discussion of this issue). More recently, it has been argued that psychotic symptoms are not a good basis for making a diagnosis of schizophrenia as "psychosis is the 'fever' of mental illness — a serious but nonspecific indicator".
Perhaps because of these factors, studies examining the diagnosis of schizophrenia have typically shown relatively low or inconsistent levels of diagnostic reliability. Most famously, David Rosenhan's 1972 study, published as On being sane in insane places, demonstrated that the diagnosis of schizophrenia was (at least at the time) often subjective and unreliable. More recent studies have found agreement between any two psychiatrists when diagnosing schizophrenia tends to reach about 65% at best. This, and the results of earlier studies of diagnostic reliability (which typically reported even lower levels of agreement) have led some critics to argue that the diagnosis of schizophrenia should be abandoned.
In 2004 in Japan, the category of schizophrenia was abandoned and replaced with integration disorder. In 2006, campaigners in the UK, under the banner of Campaign for Abolition of the Schizophrenia Label, argued for a similar rejection of the diagnosis of schizophrenia and a different approach to the treatment and understanding of the symptoms currently associated with it.
Alternatively, other proponents have argued for a new approach that would use the presence of specific neurocognitive deficits to make a diagnosis. These often accompany schizophrenia and take the form of a reduction or impairment in basic psychological functions such as memory, attention, executive function and problem solving. It is these sorts of difficulties, rather than the psychotic symptoms (which can in many cases be controlled by antipsychotic medication), which seem to be the cause of most disability in schizophrenia. However, this argument is relatively new and it is unlikely that the method of diagnosing schizophrenia will change radically in the near future.
The diagnostic approach to schizophrenia has also been opposed by the proponents of the anti-psychiatry movement, who argue that classifying specific thoughts and behaviors as an illness allows social control of people that society finds undesirable but who have committed no crime. They argue that this is a way of unjustly classifying a social problem as a medical one to allow the forcible detention and treatment of people displaying these behaviors, which is something which can be done under mental health legislation in most Western countries.
An example of this can be seen in the Soviet Union, where an additional sub-classification of sluggishly progressing schizophrenia was created. Particularly in the RSFSR (Russian Soviet Federated Socialist Republic), this diagnosis was used for the purpose of silencing political dissidents or forcing them to recant their ideas by the use of forcible confinement and treatment. In 2000 similar concerns about the abuse of psychiatry to unjustly silence and detain practitioners of the Falun Gong movement by the Chinese government led the American Psychiatric Association's Committee on the Abuse of Psychiatry and Psychiatrists to pass a resolution to urge the World Psychiatric Association to investigate the situation in China.
Western psychiatric medicine tends to favor a definition of symptoms that depends on form rather than content (an innovation first argued for by psychiatrists Karl Jaspers and Kurt Schneider). Therefore, a subject should be able to believe anything, however unusual or socially unacceptable, without being diagnosed delusional, unless their belief is held in a particular way. In principle, this would stop people being forcibly detained or treated simply for what they believe. However, the distinction between form and content is not easy, or always possible, to make in practice (see delusion). This had led to accusations by anti-psychiatry, surrealist and mental health system survivor groups that psychiatric abuses exist in the West as well.
Causes
While the reliability of the schizophrenia diagnosis introduces difficulties in measuring the relative effect of genes and environment (for example, symptoms overlap to some extent with severe bipolar disorder or major depression), evidence suggests that genetic vulnerability and environmental stressors can act in combination to result in diagnosis of schizophrenia.
The extent to which these factors influence the likelihood of being diagnosed with schizophrenia is debated widely, and currently, controversial. Schizophrenia is likely to be a diagnosis of complex inheritance. Thus, it is likely that several genes interact to generate risk for schizophrenia or for the separate components that can co-occur to lead to a diagnosis. This, combined with disagreements over which research methods are best, or how data from genetic research should be interpreted, has led to differing estimates over genetic contribution.
Genetic
Substantial evidence suggests that the diagnosis of schizophrenia has a heritable component (some estimates are as high as 80%). Current research suggests that environmental factors play a significant role in the expression of any genetic disposition towards schizophrenia (i.e. if someone has the genes that increase risk, this will not automatically result in a diagnosis of schizophrenia later in life). A recent review of the genetic evidence has suggested a more than 28% chance of one identical twin obtaining the diagnosis if the other already has it (see twin studies), but such studies are not noted for pondering the likelihood of similarities of social class and/or other socio-psychological factors between the twins. The estimates of heritability of schizophrenia from twin studies varies a great deal, with some notable studies showing rates as low as 11.0%–13.8% among monozygotic twins, and 1.8%–4.1% among dizygotic twins. However, some scientists criticise the methodology of the twin studies, and have argued that the genetic basis of schizophrenia is still largely unknown or open to different interpretations.
There is currently a great deal of effort being put into molecular genetic studies of schizophrenia, which attempt to identify specific genes which may increase risk. Because of this, the genes that are thought to be most involved can change as new evidence is gathered. A 2003 review of linkage studies listed seven genes as likely to increase risk for a later diagnosis of the disorder. Two more recent reviews have suggested that the evidence is currently strongest for two genes known as dysbindin (DTNBP1) and neuregulin (NRG1), with a number of other genes (such as COMT, RGS4, PPP3CC, ZDHHC8, DISC1, and AKT1) showing some early promising results that have not yet been fully replicated.
Environmental
Considerable evidence indicates that stressful life events cause or trigger schizophrenia. Childhood experiences of abuse or trauma have also been implicated as risk factors for a diagnosis of schizophrenia later in life.
Evidence is also consistent that negative attitudes towards individuals with (or with a risk of developing) schizophrenia can have a significant adverse impact. In particular, critical comments, hostility, authoritarian and intrusive or controlling attitudes (termed 'high expressed emotion' by researchers) from family members have been found to correlate with a higher risk of relapse in schizophrenia across cultures. It is not clear whether such attitudes play a causal role in the onset of schizophrenia, although those diagnosed in this way may claim it to be the primary causal factor. The research has focused on family members but also appears to relate to professional staff in regular contact with clients. While initial work addressed those diagnosed as schizophrenic, these attitudes have also been found to play a significant role in other mental health problems. This approach does not blame 'bad parenting' or staffing, but addresses the attitudes, behaviors and interactions of all parties. Some go as far as to criticise the whole approach of seeking to localise 'mental illness' within one individual - the patient - rather than his/her group and its functionality, citing a scapegoat effect.
Factors such as poverty and discrimination also appear to be involved in increasing the risk of schizophrenia or schizophrenia relapse, perhaps due to the high levels of stress they engender, or faults in diagnostic procedure/assumptions. Racism in society, including in diagnostic practices, and/or the stress of living in a different culture, may explain why minority communities have shown higher rates of schizophrenia than members of the same ethnic groups resident in their home country. The "social drift hypothesis" suggests that the functional problems related to schizophrenia, or the stigma and prejudice attached to them, can result in more limited employment and financial opportunities, so that the causal pathway goes from mental health problems to poverty, rather than, or in addition to, the other direction. Some argue that unemployment and the long-term unemployed and homeless are simply being stigmatised.
One particularly stable and replicable finding has been the association between living in an urban environment and schizophrenia diagnosis, even after factors such as drug use, ethnic group and size of social group have been controlled for. A recent study of 4.4 million men and women in Sweden found an alleged 68%–77% increased risk of diagnosed psychosis for people living in the most urbanized environments, a significant proportion of which is likely to be described as schizophrenia.
Perinatal brain development
It is thought that causal factors can initially come together in early neurodevelopment, including during pregnancy, to increase the risk of later developing schizophrenia. One curious finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring (at least in the northern hemisphere). However, the effect is not large. Some researchers postulate that the correlation is due to viral infections during the third trimester (4-6 months) of pregnancy. There is now significant evidence that prenatal exposure to infections increases the risk for developing schizophrenia later in life, providing additional evidence for a link between in utero developmental pathology and risk of developing the condition.
A study by Sweden's Karolinska Institute and Bristol University in the UK, looked at the medical records of over 700,000 people and calculated that 15.5% of cases of schizophrenia seen in the group may have been due to the patient having a father who was aged over 30 years at their birth, the researchers argue this is due to build up of mutations in the sperm of elder fathers.
Women who were pregnant during the Dutch famine of 1944, where many people were close to starvation, had a higher chance of having a child who would later develop schizophrenia. Similarly, studies of Finnish mothers who were pregnant when they found out that their husbands had been killed during the Winter War of 1939–1940 have shown that their children were much more likely to develop schizophrenia when compared with mothers who found out about their husbands' death after pregnancy, suggesting that even psychological trauma in the mother may have an effect.
Childhood and adolescent development
Schizophrenia is most commonly first diagnosed during late adolescence or early adulthood suggesting it is often the end process of childhood and adolescent development. Studies have indicated that genetic dispositions can interact with early environment to increase the risk of developing schizophrenia, including through global neurobehavioral deficits, a poorer family environment and disruptive school behaviour, poor peer engagement, immaturity or unpopularity or poorer social competence and increasing schizophrenic symptomology emerging during adolescence These developmental problems have also been linked to socioeconomic disadvantage or early experiences of traumatic events.
There is on average a somewhat earlier onset for men than women, with the possible protective influence of the female hormone oestrogen being one hypothesis made and sociocultural influences another.
Adult brain structure
Differences in the size and structure of certain brain areas have been found in some adults diagnosed with schizophrenia. Early findings came from the discovery of ventricular enlargement in people diagnosed with schizophrenia with negative symptoms most prominent. However, this finding has not proved particularly reliable on the level of the individual person, with considerable variation between patients. The role of antipsychotic medication, which nearly all those studied had taken, in causing such abnormalities is also unclear
More recent studies have shown a large number of differences in brain structure between people with and without diagnoses of schizophrenia. However, as with earlier studies, many of these differences are only reliably detected when comparing groups of people, and are unlikely to predict any differences in brain structure of an individual person with schizophrenia.
Neuropsychology and brain function
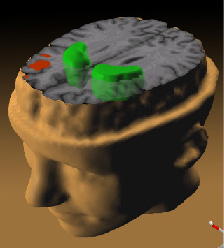
Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus, and temporal lobes. These differences are heavily linked to the neurocognitive deficits which often occur with schizophrenia, particularly in areas of memory, attention, problem solving, executive function and social cognition.
Electroencephalograph (EEG) recordings of persons with schizophrenia performing perception oriented tasks showed an absence of gamma band activity in the brain, indicating weak integration of critical neural networks in the brain. Those who experienced intense hallucinations, delusions and disorganized thinking showed the lowest frequency synchronization. None of the drugs taken by the persons scanned had moved neural synchrony back into the gamma frequency range. Gamma band and working memory alterations may be related to alterations in interneurons that produced the neurotransmitter GABA.
Neurochemical pathways
Particular focus has been placed upon the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, could reduce psychotic symptoms. An influential theory, known as the "dopamine hypothesis of schizophrenia", proposed that a malfunction involving dopamine pathways was therefore the cause of (the positive symptoms of) schizophrenia. This theory is now thought to be overly simplistic as a complete explanation, partly because newer antipsychotic medication (called atypical antipsychotic medication) can be equally effective as older medication (called typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect. In addition dopamine pathway dysfunction has not been reliably shown to correlate with symptom onset or severity.
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia. This has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition. The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia. Further support of this theory has come from preliminary trials suggesting the efficacy of coagonists at the NMDA receptor complex in reducing some of the positive schizophrenic symptoms
Psychosocial factors
A number of cognitive biases or deficits have been found in people with schizophrenia (and their relatives). These include jumping to conclusions when faced with limited or contradictory information; specific biases in reasoning about social situations, for example assuming other people cause things that go wrong (external attribution); difficulty distinguishing inner speech from speech from an external source (source monitoring); difficulty in adjusting speech to the needs of the hearer, related to theory of mind difficulties; difficulties in the very earliest stages of processing visual information (including reduced latent inhibition); difficulty with attention e.g. being more easily distracted, attentional bias towards threat. Some of these tendencies have been shown to worsen or appear when under emotional stress or in confusing situations. As with the related neurological findings, they are not shown by all individuals with a diagnosis of schizophrenia and it is not clear how specific they are to schizophrenia or to particular symptoms. The findings regarding schizophrenia are reliable and consistent, however, to the extent that they can be viewed as diagnostic
A number of emotional factors have been implicated in schizophrenia, with some models putting them at the core of the disorder. It was thought that the appearance of blunted affect meant that sufferers did not experience strong emotions, but more recent studies indicate there is often a normal or even heightened level of emotionality, particularly in response to negative events or stressful social situations. Some theories suggest positive symptoms of schizophrenia can result from or be worsened by negative emotions, including depressed feelings and low self-esteem and feelings of vulnerability, inferiority or loneliness. Chronic negative feelings and maladaptive coping skills may explain some of the association between psychosocial stressors and symptomology. Critical and controlling behaviour by significant others (high expressed emotion) causes increased emotional arousal and lowered self-esteem and a subsequent increase in positive symptoms such as unusual thoughts. Countries or cultures where schizotypal personalities or schizophrenia symptoms are more accepted or valued appear to be associated with reduced onset of, or increased recovery from, schizophrenia.
Related studies suggest that the content of delusional and psychotic beliefs in schizophrenia can be meaningful and play a causal or mediating role in reflecting the life history or social circumstances of the individual. Holding minority or poorly understood sociocultural beliefs, for example due to ethnic background, has been linked to increased diagnosis of schizophrenia. The way an individual personally understands and attributes their delusions or hallucinations (e.g. as threatening or as potentially positive) has also been found to influence functioning and recovery.
Incidence and prevalence
In the western world, schizophrenia is typically diagnosed in late adolescence or early adulthood. In the western world, it is found approximately equally in men and women, though the onset tends to be later in women, who also tend to have a better course and outcome. Although rare, there are also instances of childhood onset schizophrenia and late-onset schizophrenia that occurs in the elderly.
The lifetime prevalence of schizophrenia is commonly given at 1%; however, a recent review of studies from around the world estimated it to be 0.55%. The same study also found that prevalence may vary greatly from country to country, despite the received wisdom that schizophrenia occurs at the same rate throughout the world. It is worth noting however, that this may be in part due to differences in the way schizophrenia is diagnosed. The incidence of schizophrenia was given as a range of between 7.5 and 16.3 cases per year per 100,000 population.
Schizophrenia is also a major cause of disability. In a recent 14-country study, active psychosis was ranked the third most disabling condition after quadriplegia and dementia and before paraplegia and blindness.
Research findings on violence and schizophrenia
Although schizophrenia is sometimes associated with violence in the media only a small minority of people with schizophrenia commit an act of violence, and only a minority of people who commit criminal violence have been diagnosed with schizophrenia.
Research has suggested that schizophrenia is associated with a slight increase in risk of violence, although this risk is largely due to a small sub-group of individuals for whom violence is associated with active psychotic symptoms, concurrent substance abuse and ceasing psychiatric drugs, additionally, those having a history of violence and educational difficulties in childhood showed additional risk.
For the most serious acts of violence, long-term independent studies of convicted murderers in both New Zealand and Sweden found that 3.7%–8.9% had been given a previous diagnosis of schizophrenia.
There is some evidence to suggest that in some people, the drugs used to treat schizophrenia may produce an increased risk for violence, largely due to agitation induced by akathisia, a side effect sometimes associated with antipsychotic medication. Similarly, abuse experienced in childhood may contribute both to a slight increase in risk for violence in adulthood, as well as the development of schizophrenia.
Research has shown that a person diagnosed with schizophrenia is more likely to be a victim of violence (4.3% in a one month period) than a perpetrator.
Treatment
Medication and hospitalization
Currently schizophrenia has not been cured although many psychiatrists and psychologists believe that it can be managed. The first line pharmacological therapy for schizophrenia is usually the use of antipsychotic medication. The concept of 'curing' schizophrenia is controversial as there are no clear criteria for what might constitute a cure, although some criteria for the remission of symptoms have recently been suggested. Therefore, antipsychotic drugs are only thought to provide symptomatic relief from the positive symptoms of psychosis. The newer atypical antipsychotic medications (such as clozapine, risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and amisulpride) are usually preferred over older typical antipsychotic medications (such as chlorpromazine and haloperidol) due to their favorable side-effect profile. Compared to the typical antipsychotics, the atypicals are associated with a lower incident rate of extrapyramidal side effects (EPS) and tardive dyskinesia (TD) although they are more likely to induce weight gain and so increase risk for obesity-related diseases. It is still unclear whether newer drugs reduce the chances of developing the rare but potentially life-threatening neuroleptic malignant syndrome (NMS). While the atypical antipsychotics are associated with less EPS and TD than the conventional antipsychotics, some of the agents in this class (especially olanzapine and clozapine) appear to be associated with metabolic side effects such as weight gain, hyperglycemia and hypertriglyceridemia that must be considered when choosing appropriate pharmacotherapy.
Atypical and typical antipsychotics are generally thought to be equivalent for the treatment of the positive symptoms of schizophrenia. It has been suggested by some researchers that the atypicals have some beneficial effects on negative symptoms and cognitive deficits associated with schizophrenia, although the clinical significance of these effects has yet to be established. However, recent reviews have suggested that typical antipsychotics, when dosed conservatively, may have similar effects to atypicals. The atypical antipsychotics are much more costly as they are still within patent, whereas the older drugs are available in inexpensive generic forms. Aripiprazole is a drug from a new class of antipsychotic drugs (variously named 'dopamine system stabilizers' or 'partial dopamine agonists') that have recently been developed and is now widely licensed to treat schizophrenia.
The efficacy of schizophrenia treatment is often assessed by using standardized assessment methods, one of the most common being the positive and negative syndrome scale (PANSS).
Hospitalization may occur with severe episodes. This can be voluntary or (if mental health legislation allows it) involuntary (called civil or involuntary commitment). Mental health legislation may also allow people to be treated against their will. However, in many countries such legislation does not exist, or does not have the power to enforce involuntary hospitalization or treatment.
Therapy and community support
Psychotherapy or other forms of talk therapy may be offered, with cognitive behavioral therapy being the most frequently used. This may focus on the direct reduction of the symptoms, or on related aspects, such as issues of self-esteem, social functioning, and insight. Although the results of early trials with cognitive behavioral therapy (CBT) were inconclusive, more recent reviews suggest that CBT can be an effective treatment for the psychotic symptoms of schizophrenia.
A relatively new approach has been the use of cognitive remediation therapy, a technique aimed at remediating the neurocognitive deficits sometimes present in schizophrenia. Based on techniques of neuropsychological rehabilitation, early evidence has shown it to be cognitively effective, with some improvements related to measurable changes in brain activation as measured by fMRI.
Electroconvulsive therapy (also known as ECT or 'electroshock therapy') may be used in countries where it is legal. It is not considered a first line treatment but may be prescribed in cases where other treatments have failed. Psychosurgery has now become a rare procedure and is not a recommended treatment for schizophrenia.
Other support services may also be available, such as drop-in centers, visits from members of a 'community mental health team' or assertive community treatment team, and patient-led support groups. In recent years the importance of service-user led recovery based movements has grown substantially throughout Europe and America. Groups such as the Hearing Voices Network and more recently, the Paranoia Network, have developed a self-help approach that aims to provide support and assistance outside of the traditional medical model adopted by mainstream psychiatry. By avoiding framing personal experience in terms of criteria for mental illness or mental health, they aim to destigmatize the experience and encourage individual responsibility and a positive self-image. Peer-to-peer suppport is also developing a professional footing with partnerships between hospitals and consumer run groups becoming more common. These services work towards remediating social withdrawal, building social skills and reducing rehospitalization.
In many non-Western societies, schizophrenia may be treated with more informal, community-led methods. A particularly sobering thought for Western psychiatry is that the outcome for people diagnosed with schizophrenia in non-Western countries may actually be much better than for people in the West. The reasons for this recently discovered effect are still far from clear, although cross-cultural studies are being conducted to find out why.
A recent randomised controlled trial found that music therapy significantly improved symptom scores in a group of patients diagnosed with schizophrenia. A notable early mention of the beneficial effect of music on mental illness was in 1621 by Robert Burton in The Anatomy of Melancholy.
Dietary supplements
Omega-3 fatty acids (found naturally in foods such as oily fish, flax seeds, hemp seeds, walnuts and canola oil) have recently been studied as a treatment for schizophrenia. Although the number of research trials has been limited, the majority of randomized controlled trials have found omega-3 supplements to be effective when used as a dietary supplement.
Prognosis
Prognosis for any particular individual affected by schizophrenia is particularly hard to judge as treatment and access to treatment is continually changing, as new methods become available and medical recommendations change.
One retrospective study has shown that about a third of people make a full recovery, about a third show improvement but not a full recovery, and a third remain ill. A more recent study using stricter recovery criteria (i.e. concurrent remission of positive and negative symptoms and specific instances of adequate social / vocational functioning) reported a recovery rate of 13.7%.
The exact definition of what constitutes a recovery has not been widely defined, however, although criteria have recently been suggested to define a remission in symptoms. Therefore, this makes it difficult to give an exact estimate as recovery and remission rates are not always comparable across studies.
The World Health Organization conducted two long-term follow-up studies involving more than 2,000 people suffering from schizophrenia in different countries. These studies' findings were that these patients have much better long-term outcomes in developing countries (India, Colombia and Nigeria) than in developed countries (USA, UK, Ireland, Denmark, Czech Republic, Slovakia, Japan, and Russia), despite the fact antipsychotic drugs are typically not widely available in poorer countries, thus raising questions about the effectiveness of such drug-based treatments.
Prognosis also depends on some other factors. Females tend to show recovery rates higher than males, and acute and sudden onset of schizophrenia is associated with higher rates of recovery, while gradual onset is associated with lower rates. Most studies done on this subject, however, are correlational in nature, and a clear cause-and-effect relationship is difficult to establish. Pre-morbid functioning and positive prognosis also seem to be correlated.
In a study of over 168,000 Swedish citizens undergoing psychiatric treatment, schizophrenia was associated with an average life expectancy of approximately 80-85% of that of the general population. Women with a diagnosis of schizophrenia were found to have a slightly better life expectancy than that of men, and as a whole, a diagnosis of schizophrenia was associated with a better life expectancy than substance abuse, personality disorder, heart attack and stroke.
There is an extremely high suicide rate associated with schizophrenia. A recent study showed that 30% of patients diagnosed with this condition had attempted suicide at least once during their lifetime. Another study suggested that 10% of persons with schizophrenia die by suicide.
Recovery and Rehabilitation
Just as the diagnosis itself is mired in controversy and counter-accusation, it is difficult to establish a clear picture of recovery and rehabilitation. Both long ago and in the recent past, patients in developed countries were told that chances of recovery were limited, with statistics being quoted to support this negative prognosis. Today, with the advent of a vocal "Recovery Movement" in mental health, statistics are quoted in a conflicting fashion, and attention is drawn to cultural and local factors in impeding or accelerating recovery. Rehabilitation provision is uneven and strongly dependent on local political culture and/or resources.
Schizophrenia and drug use
The relationship between schizophrenia and drug use is complex, meaning that a clear causal connection between drug use and schizophrenia has been difficult to tease apart. There is strong evidence that using certain drugs can trigger either the onset or relapse of schizophrenia in some people. It may also be the case, however, that people with schizophrenia use drugs to overcome negative feelings associated with both the commonly prescribed antipsychotic medication and the condition itself, where negative emotion, paranoia and anhedonia are all considered to be core features.
The rate of substance use is known to be particularly high in this group. In a recent study, 60% of people with schizophrenia were found to use substances and 37% would be diagnosable with a substance use disorder.
Amphetamines
As amphetamines trigger the release of dopamine and excessive dopamine function is believed to be responsible for many symptoms of schizophrenia (known as the dopamine hypothesis of schizophrenia), amphetamines may worsen schizophrenia symptoms.
Hallucinogens
Schizophrenia can sometimes be triggered by heavy use of hallucinogenic drugs , although some claim that a predisposition towards developing schizophrenia is needed for this to occur. There is also some evidence suggesting that people suffering schizophrenia but responding to treatment can have relapse because of subsequent drug use. Some widely known cases where hallucinogens have been suspected of precipitating schizophrenia are Pink Floyd founder-member Syd Barrett and The Beach Boys producer, arranger and songwriter Brian Wilson.
Drugs such as ketamine, PCP, and LSD have been used to mimic schizophrenia for research purposes, although this has now fallen out of favor with the scientific research community, as the differences between the drug induced states and the typical presentation of schizophrenia have become clear.
Hallucinogenic drugs were also briefly tested as possible treatments for schizophrenia by psychiatrists such as Humphry Osmond and Abram Hoffer in the 1950s. It was mainly for this experimental treatment of schizophrenia that LSD administration was legal, briefly before its use as a recreational drug led to its criminalization.
Cannabis
There is evidence that cannabis use can contribute to schizophrenia. Some studies suggest that cannabis is neither a sufficient nor necessary factor in developing schizophrenia, but that cannabis may significantly increase the risk of developing schizophrenia and may be, among other things, a significant causal factor. Nevertheless, some previous research in this area has been criticised as it has often not been clear whether cannabis use is a cause or effect of schizophrenia. To address this issue, a recent review of studies from which a causal contribution to schizophrenia can be assessed has suggested that cannabis statistically doubles the risk of developing schizophrenia on the individual level, and may, assuming a causal relationship, be responsible for up to 8% of cases in the population.
Tobacco
People with schizophrenia smoke significantly more tobacco than the general population. The rates are exceptionally high amongst institutionalized patients and homeless people. In a UK census from 1993, 74% of people with schizophrenia living in institutions were found to be smokers. A 1999 study that covered all people with schizophrenia in Nithsdale, Scotland found a 58% prevalence rate of cigarette smoking, to compare with 28% in the general population. An older study found that as much as 88% of outpatients with schizophrenia were smokers.
Despite the higher prevalence of tobacco smoking, people diagnosed with schizophrenia have a much lower than average chance of developing and dying from lung cancer. While the reason for this is unknown, it may be because of a genetic resistance to the cancer, a side-effect of drugs being taken, or a statistical effect of increased likelihood of dying from causes other than lung cancer.
A recent study of over 50,000 Swedish conscripts found that there was a small but significant protective effect of smoking cigarettes on the risk of developing schizophrenia later in life. While the authors of the study stressed that the risks of smoking far outweigh these minor benefits, this study provides further evidence for the 'self-medication' theory of smoking in schizophrenia and may give clues as to how schizophrenia might develop at the molecular level. Furthermore, many people with schizophrenia have smoked tobacco products long before they are diagnosed with the illness, and some groups advocate that the chemicals in tobacco have actually contributed to the onset of the illness and have no benefit of any kind.
It is of interest that cigarette smoking affects liver function such that the antipsychotic drugs used to treat schizophrenia are broken down in the blood stream more quickly. This means that smokers with schizophrenia need slightly higher doses of antipsychotic drugs in order for them to be effective than do their non-smoking counterparts.
The increased rate of smoking in schizophrenia may be due to a desire to self-medicate with nicotine. One possible reason is that smoking produces a short term effect to improve alertness and cognitive functioning in persons who suffer this illness. It has been postulated that the mechanism of this effect is that schizophrenics have a disturbance of nicotinic receptor functioning which is temporarily abated by tobacco use.
Alternative approaches to schizophrenia
An approach broadly known as the anti-psychiatry movement, notably most active in the 1960s, has opposed the orthodox medical view of schizophrenia as an illness.
Psychiatrist Thomas Szasz argues that psychiatric patients are not ill but are just individuals with unconventional thoughts and behavior that make society uncomfortable. He argues that society unjustly seeks to control such individuals by classifying their behavior as an illness and forcibly treating them as a method of social control. It is worth noting that Szasz has never considered himself to be "anti-psychiatry" in the sense of being against psychiatric treatment, but simply believes that it should be conducted between consenting adults, rather than imposed upon anyone against his or her will.
Similarly, psychiatrists R. D. Laing, Silvano Arieti, Theodore Lidz and other mental health professionals have argued that the symptoms of what is normally called mental illness are comprehensible reactions to impossible demands that society and particularly family life places on some sensitive individuals. Laing, Arieti and Lidz were revolutionary in valuing the content of psychotic experience as worthy of interpretation, rather than considering it simply as a secondary but essentially meaningless marker of underlying psychological or neurological distress. Laing's work, co-authored with Aaron Esterson, Sanity, Madness and the Family (1964) described eleven case studies of people diagnosed with schizophrenia and argued that the content of their actions and statements was meaningful and logical in the context of their family and life situations. Arieti's Interpretation of Schizophrenia won the 1975 scientific National Book Award in the United States. In the books Schizophrenia and the Family and The Origin and Treatment of Schizophrenic Disorders Lidz and his colleagues explain their belief that parental behaviour can result in mental illness in children.
In the 1976 book The Origin of Consciousness in the Breakdown of the Bicameral Mind, psychologist Julian Jaynes proposed that until the beginning of historic times, schizophrenia or a similar condition was the normal state of human consciousness. This would take the form of a "bicameral mind" where a normal state of low affect, suitable for routine activities, would be interrupted in moments of crisis by "mysterious voices" giving instructions, which early people characterized as interventions from the gods. This theory was briefly controversial. Continuing research has failed to either further confirm or refute the thesis.
Psychiatrist Tim Crow has argued that schizophrenia may be the evolutionary price we pay for a left brain hemisphere specialization for language. Since psychosis is associated with greater levels of right brain hemisphere activation and a reduction in the usual left brain hemisphere dominance, our language abilities may have evolved at the cost of causing schizophrenia when this system breaks down.
Researchers into shamanism have speculated that in some cultures schizophrenia or related conditions may predispose an individual to becoming a shaman. Certainly, the experience of having access to multiple realities is not uncommon in schizophrenia, and is a core experience in many shamanic traditions. Equally, the shaman may have the skill to bring on and direct some of the altered states of consciousness psychiatrists label as illness. Speculations regarding primary and important religious figures as having schizophrenia abound. Some commentators have endorsed the idea that major religious figures experienced psychosis, heard voices and displayed delusions of grandeur.
Alternative medicine tends to hold the view that schizophrenia is primarily caused by imbalances in the body's reserves and absorption of dietary minerals, vitamins, fats, and/or the presence of excessive levels of toxic heavy metals. The body's adverse reactions to gluten are also strongly implicated in some alternative theories (see gluten-free, casein-free diet).
One theory put forward by psychiatrists E. Fuller Torrey and R.H. Yolken is that the parasite Toxoplasma gondii leads to some, if not many, cases of schizophrenia. This is supported by evidence that significantly higher levels of Toxoplasma antibodies in schizophrenia patients compared to the general population.
An additional approach is suggested by the work of Richard Bandler who argues that "The usual difference between someone who hallucinates and someone who visualizes normally, is that the person who hallucinates doesn't know he's doing it or doesn't have any choice about it." (Time for a Change, p107). He suggests that because visualization is a sophisticated mental capability, schizophrenia is a skill, albeit an involuntary and dysfunctional one that is being used but not controlled. He therefore suggests that a significant route to treating schizophrenia might be to teach the missing skill - how to distinguish created reality from consensus external reality, to reduce its maladaptive impact, and ultimately how to exercise appropriate control over the vizualization or auditory process. Hypnotic approaches have been explored by the physician Milton H. Erickson as a means of facilitating this.
Regarding schizophrenia as a waking dreamer syndrome, Jie Zhang hypothesizes that the hallucinations of schizophrenia are caused by the activation of the continual-activation mechanism during waking, a mechanism that induces dreaming while asleep, due to the malfunction of the continual-activation thresholds in the conscious part of brain.
Portrayals of schizophrenia in the arts
The book and film A Beautiful Mind chronicled the life of John Nash, a Nobel-Prize-winning mathematician who was diagnosed with schizophrenia.
In Bulgakov's Master and Margarita the poet Ivan Bezdomnyj is institutionalized and diagnosed with schizophrenia after witnessing the devil (Woland) predict Berlioz's death.
The book The Eden Express by Mark Vonnegut accounts his struggle into schizophrenia and his journey back to sanity.
EastEnders featured a very successful storyline in 1996 that involved a character suffering from schizophrenia, triggered by the loss of a relative.
The effects of untreated schizophrenia on the family are documented in Virginia Holman's autobiography, Rescuing Patty Hearst (Simon & Schuster 2003). The book also discusses the legal impediments to treatment that face many schizophrenics and their families.
See also
|
Further reading
- Bentall, R. (2003) Madness explained: Psychosis and Human Nature. London: Penguin Books Ltd. ISBN 0-7139-9249-2
- Boyle, Mary, (1993), Schizophrenia: A Scientific Delusion, Routledge, ISBN 0-415-09700-2
- Deveson, Anne (1991), Tell Me I'm Here. Penguin. ISBN 0-14-027257-7
- Fallon, J.H. et. al. (2003) The Neuroanatomy of Schizophrenia: Circuitry and Neurotransmitter Systems. Clinical Neuroscience Research 3:77-107.
- Green, M.F. (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- Jones, S. and Hayward, P. (2004) Coping with Schizophrenia: A Guide for Patients, Families and Caregivers. ISBN 1-85168-344-5
- Keen, T. M. (1999) Schizophrenia: orthodoxy and heresies. A review of alternative possibilities. Journal of Psychiatric and Mental Health Nursing, 1999, 6, 415-424. pdf
- Noll, Richard (2007) The Encyclopedia of Schizophrenia and Other Psychotic Disorders, Third Edition ISBN 0-8160-6405-9
- Read, J., Mosher, L.R., Bentall, R. (2004) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6. A critical approach to biological and genetic theories, and a review of social influences on schizophrenia.
- Szasz, T. (1976) Schizophrenia: The Sacred Symbol of Psychiatry. New York: Basic Books. ISBN 0-465-07222-4
- Tausk, V. : "Sexuality, War, and Schizophrenia: Collected Psychoanalytic Papers", Publisher: Transaction Publishers 1991, ISBN 0-88738-365-3 (On the Origin of the 'Influencing Machine' in Schizophrenia.)
- Torrey, E.F., M.D. (2006) Surviving Schizophrenia: A Manual for Families, Consumers, and Providers (5th Edition). Quill (HarperCollins Publishers) ISBN 0-06-084259-8
- Vonnegut, M. The Eden Express. ISBN 0-553-02755-7. A personal account of schizophrenia.
- Wiencke, Markus (2006) Schizophrenie als Ergebnis von Wechselwirkungen: Georg Simmels Individualitätskonzept in der Klinischen Psychologie. In David Kim (ed.), Georg Simmel in Translation: Interdisciplinary Border-Crossings in Culture and Modernity (pp. 123-155). Cambridge Scholars Press, Cambridge, ISBN 1-84718-060-5
External links
News, information and further description
- - DSM V scholarly debates on schizophrenia
- - NPR: the sight and sounds of schizophrenia
- National Mental Health Association fact sheet on schizophrenia
- Understanding Schizophrenia - A factsheet from the mental health charity Mind
- DSM-IV-TR Full diagnostic criteria for schizophrenia
- World Health Organisation data on schizophrenia from 'The World Health Report 2001. Mental Health: New Understanding, New Hope'
- National Institute of Mental Health (USA) Schizophrenia information
- Childhood Schizophrenia Summary
- National Mental Health Consumers' Self-Help Clearinghouse
- UCLA Laboratory of Neuro Imaging definition
- The current World Health Organisation definition of Schizophrenia
- A directory of free full-text articles on diagnosis and management of schizophrenia
- Schizophrenia by WebMD (pharmaceutical company sponsored).
- Schizophrenia.com - information and support site. Sponsored by Janssen Pharmaceuticals .
- Schizophrenia in history
- Symptoms in Schizophrenia Film made in 1940 showing some of the symptoms of Schizophrenia.
- http://www.sciencedaily.com/news/mind_brain/schizophrenia/
- Open The Doors - information on global programme to fight stigma and discrimination because of Schizophrenia. The World Psychiatric Association (WPA)
- Scientific American Magazine (January 2004 Issue) Decoding Schizophrenia
- Alternative view on schizophrenia as a mental healing process
Charities and support groups
- Schizophrenics Anonymous
- SANE UK mental health charity focused on schizophrenia that supports sufferers, runs a helpline and carries out research into mental illness
- The Schizophrenia Association of Great Britain
- CASL The Campaign for Abolition of the Schizophrenia Label.
- WFSAD The World Fellowship for Schizophrenia and Allied Disorders is an education and support network for families of people with schizophrenia.
Critical approaches to schizophrenia
- Successfulschizophrenia.org A website critical of Schizophrenia as a disorder, with many links and resources, by Al Siebert, psychologist Ph.D.
- Schizophrenia: A Nonexsistent Disease by Lawrence Stevens, J.D
- Loren Mosher, M.D. (Chief of the Center for Studies of Schizophrenia at the U.S. National Institute of Mental Health 1969-1980) Still Crazy After All These Years
- Bola, John R., Ph.D.; & Mosher, Loren R., M.D. (2003). Treatment of Acute Psychosis Without Neuroleptics: Two-Year Outcomes From the Soteria Project. The Journal of Nervous and Mental Disease, (191: 219-229). Available as PDF.
- Boyle, Mary (2002). Schizophrenia: A Scientific Delusion? (second edition) Hove, East Sussex: Routledge. A detailed and comperehensive critical review and rebuttal of almost all the major evidence presented for the existence of schizophrenia as a brain disorder.
- Jonathan Leo, Ph.D., & Jay Joseph, Psy.D. Schizophrenia: Medical students are taught it's all in the genes, but are they hearing the whole story?
- The Rosenhan experiment, famous experiment into the validity of psychiatric diagnosis conducted by David Rosenhan in 1972.
References
- Evans, K., McGrath, J., & Milns, R. (2003) Searching for schizophrenia in ancient Greek and Roman literature: a systematic review. Acta Psychiatrica Scandanavica, 107(5), 323–330.
- ^ Kraepelin, E. (1907) Text book of psychiatry (7th ed) (trans. A.R. Diefendorf). London: Macmillan.
- ^ "Conditions in Occupational Therapy: effect on occupational performance." ed. Ruth A. Hansen and Ben Atchison (Baltimore: Lippincott Williams & Williams, 2000), 54–74. ISBN 0-683-30417-8
- Stotz-Ingenlath G. (2000) Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911. Medicine, Health Care, and Philosophy, 3(2), 153-9.
- Turner, T. (1999) 'Schizophrenia'. In G.E. Berrios and R. Porter (eds) A History of Clinical Psychiatry. London: Athlone Press. ISBN 0-485-24211-7
- Allen GE. (1997) The social and economic origins of genetic determinism: a case history of the American Eugenics Movement, 1900-1940 and its lessons for today. Genetica, 99, 77-88.
- Read, J., Masson, J. (2004) Genetics, eugenics and mass murder. In J. Read, L.R. Mosher, R.P. Bentall (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Bertelsen, A. (2002) Schizophrenia and Related Disorders: Experience with Current Diagnostic Systems. Psychopathology, 35, 89–93.
- Verdoux, H., & van Os, J. (2002) Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research, 54(1–2), 59–65.
- Johns LC, van Os J. (2001) The continuity of psychotic experiences in the general population. Clinical Psychology Review, 21 (8),1125-41.
- E.R. Peters, S. Day, J. McKenna, G. Orbach (2005) Measuring delusional ideation: the 21-item Peters et al. Delusions Inventory (PDI). Schizophrenia Bulletin, 30, 1005-22.
- Tsuang, M. T., Stone, W. S., & Faraone, S. V. (2000) Toward reformulating the diagnosis of schizophrenia. American Journal of Psychiatry, 157(7), 1041–1050.
- McGorry PD, Mihalopoulos C, Henry L, Dakis J, Jackson HJ, Flaum M, Harrigan S, McKenzie D, Kulkarni J, Karoly R. (1995) Spurious precision: procedural validity of diagnostic assessment in psychotic disorders. American Journal of Psychiatry, 152 (2), 220–3.
- Read, J. (2004) Does 'schizophrenia' exist? Reliability and validity. In J. Read, L.R. Mosher, R.P. Bentall (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Sato, M. (2004) Renaming schizophrenia: a Japanese perspective. World Psychiatry, 5(1), 53-5.
- BBC News Online, (9 October 2006) Schizophrenia term use 'invalid'
- ^ Harrison PJ, Owen MJ. (2003) Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet, 361(9355), 417–9.
- ^ Owen MJ, Craddock N, O'Donovan MC. (2005) Schizophrenia: genes at last? Trends in Genetics, 21(9), 518-25.
- Torrey, E.F., Bowler, A.E., Taylor, E.H. & Gottesman, I.I (1994) Schizophrenia and manic depressive disorder. New York: Basic books. ISBN 0-465-07285-2
- Koskenvuo M, Langinvainio H, Kaprio J, Lonnqvist J, Tienari P (1984) Psychiatric hospitalization in twins. Acta Genet Med Gemellol (Roma), 33(2),321-32.
- Hoeffer A, Pollin W. (1970) Schizophrenia in the NAS-NRC panel of 15,909 veteran twin pairs. Archives of General Psychiatry, 1970 Nov; 23(5):469-77.
- ^ Riley B, Kendler KS (2006) Molecular genetic studies of schizophrenia. Eur J Hum Genet, 14 (6), 669-80.
- Day R, Nielsen JA, Korten A, Ernberg G, Dube KC, Gebhart J, Jablensky A, Leon C, Marsella A, Olatawura M et al (1987). Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization. Culture, Medicine and Psychiatry, 11 (2), 123–205
- ^ Harriet L. MacMillan, Jan E. Fleming, David L. Streiner, Elizabeth Lin, Michael H. Boyle, Ellen Jamieson, Eric K. Duku, Christine A. Walsh, Maria Y.-Y. Wong, William R. Beardslee. (2001) Childhood Abuse and Lifetime Psychopathology in a Community Sample. American Journal of Psychiatry,158, 1878-83.
- Schenkel, L.S., Spaulding, W.D., Dilillo, D., Silverstein, S.M. (2005) Histories of childhood maltreatment in schizophrenia: Relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophrenia Research
- Janssen I., Krabbendam L., Bak M., Hanssen M., Vollebergh W., De Graaf R., Van Os, J. (2004) Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica, 109, 38-45.
- Bebbington P E, Kuipers E (1994) The predictive utility of expressed emotion in schizophrenia: an aggregate analysis. Psychological Medicine, 24, 707-718.
- Van Humbeeck G, Van Audenhove C. (2003) Expressed emotion of professionals towards mental health patients. Epidemiologia e Psychiatria Sociale, 12(4), 232-235. (full text)
- Wearden AJ, Tarrier N, Barrowclough C, Zastowny TR, Rahill AA. (2000) A review of expressed emotion research in health care. Clinical Psychology Review, 20, 633-66.
- Van Os J. (2004) Does the urban environment cause psychosis? British Journal of Psychiatry, 184 (4), 287–288.
- Sundquist K, Frank G, Sundquist J. (2004) Urbanisation and incidence of psychosis and depression: Follow-up study of 4.4 million women and men in Sweden. British Journal of Psychiatry, 184 (4), 293–298.
- Davies G, Welham J, Chant D, Torrey EF, McGrath J. (2003) A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophrenia Bulletin, 29 (3), 587–93.
- Brown, A.S. (2006) Prenatal infection as a risk factor for schizophrenia. Schizophrenia Bulletin, 32 (2), 200-2.
- Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM (1996) Schizophrenia after prenatal famine. Further evidence. Archives of General Psychiatry, 53(1), 25–31.
- Huttunen MO, Niskanen P. (1978) Prenatal loss of father and psychiatric disorders. Archives of General Psychiatry, 35(4), 429–31.
- Hans SL, Marcus J, Nuechterlein KH, Asarnow RF, Styr B, Auerbach JG. (1999) Neurobehavioral deficits at adolescence in children at risk for schizophrenia: The Jerusalem Infant Development Study. Arch Gen Psychiatry. 56(8):741-8.
- Carter JW, Schulsinger F, Parnas J, Cannon T, Mednick SA. (2002) A multivariate prediction model of schizophrenia. Schizophrenia Bulletin 28(4):649-82.
- Hans SL, Auerbach JG, Asarnow JR, Styr B, Marcus J. (2000) Social adjustment of adolescents at risk for schizophrenia: the Jerusalem Infant Development Study. J Am Acad Child Adolesc Psychiatry. 39(11):1406-14.
- Dworkin RH, Bernstein G, Kaplansky LM, Lipsitz JD, Rinaldi A, Slater SL, Cornblatt BA, Erlenmeyer-Kimling L. (1991) Social competence and positive and negative symptoms: a longitudinal study of children and adolescents at risk for schizophrenia and affective disorder. Am J Psychiatry. Sep;148(9):1182-8.
- Read J, Perry BD, Moskowitz A, Connolly J (2001) The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry, 64, 319-45. (full text)
- Meyer-Lindenberg A, Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, Weinberger DR, Berman KF (2002) Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nature Neuroscience, 5, 267-71.
- Johnstone EC, Crow TJ, Frith CD, Husband J, Kreel L. (1976) Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet, 30;2 (7992), 924-6.
- http://ajp.psychiatryonline.org/cgi/content/full/156/11/1843-b
- Flashman LA, Green MF (2004) Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment. Psychiatric Clinics of North America, 27 (1), 1-18, vii.
- Green, M.F. (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- Spencer KM, Nestor PG, Perlmutter R, Niznikiewicz MA, Klump MC, Frumin M, Shenton ME, McCarley (2004) Neural synchrony indexes disordered perception and cognition in schizophrenia. Proceedings of the National Academy of Sciences, 101, 17288-93. (full text)
- Konradi C, Heckers S. (2003) Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics, 97(2), 153-79.
- Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA. (2001) Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology, 25(4), 455-67.
- Coyle JT, Tsai G, Goff D. (2003) Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences, 1003, 318-27.
- Tuominen HJ, Tiihonen J, Wahlbeck K. (2005) Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res, 72:225-34.
- Sitskoorn, M.M., Aleman, A., Ebisch, S.J.H., Appels, M.C.M. & Khan, R.S. (2004) Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. Schizophrenia Research, Volume 71, Issue 2, Pages 285-295.
- Broome MR, Woolley JB, Tabraham P, Johns LC, Bramon E, Murray GK, Pariante C, McGuire PK, Murray RM. (2005) What causes the onset of psychosis? Schizophr Res, 79(1), 23-34.
- Lewis, R. (2004) Should cognitive deficit be a diagnostic criterion for schizophrenia? Journal of Psychiatry and Neuroscience March; 29(2): 102–113.
- Cohen & Docherty (2004) Affective reactivity of speech and emotional experience in patients with schizophrenia. Schizophr Res, 1;69(1):7-14.
- Smith B, Fowler DG, Freeman D, Bebbington P, Bashforth H, Garety P, Dunn G, Kuipers E. (2006) Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr Res. Sep;86(1-3):181-8.
- Beck, AT (2004) A Cognitive Model of Schizophrenia, Journal of Cognitive Psychotherapy, 18 (3), 281-288.
- Horan WP, Blanchard JJ. (2003) Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping. Schizophr Res. Apr 1;60(2-3):271-83.
- Tarrier & Turpin (1992) Psychosocial factors, arousal and schizophrenic relapse. The psychophysiological data. Br J Psychiatry. 161:3-11
- Barrowclough C, Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B. (2003) Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 112(1):92-9.
- Birchwood M, Meaden A, Trower P, Gilbert P, Plaistow J. (2000) The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med. Mar;30(2):337-44
- Honig A, Romme MA, Ensink BJ, Escher SD, Pennings MH, deVries MW. (1998) Auditory hallucinations: a comparison between patients and nonpatients J Nerv Ment Dis. Oct;186(10):646-51.
- Goldner EM, Hsu L, Waraich P, Somers JM (2002) Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature. Canadian Journal of Psychiatry, 47(9), 833–43.
- Ustun TB, Rehm J, Chatterji S, Saxena S, Trotter R, Room R, Bickenbach J, and the WHO/NIH Joint Project CAR Study Group (1999). Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. Lancet, 354(9173), 111–115.
- Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tattan T, Tyrer P, Creed F, Murray R, Fahy T (2004) Predicting violence in schizophrenia: a prospective study. Schizophrenia Research, 67(2-3), 247-52.
- Simpson AI, McKenna B, Moskowitz A, Skipworth J, Barry-Walsh J. (2004) Homicide and mental illness in New Zealand, 1970-2000. British Journal of Psychiatry, 185, 394-8.
- Fazel S, Grann M. (2004) Psychiatric morbidity among homicide offenders: a Swedish population study. American Journal of Psychiatry, 161(11), 2129-31.
- Leong GB, Silva JA. (2003) Neuroleptic-induced akathisia and violence: a review. Journal of Forensic Science, 48
- Fitzgerald PB, de Castella AR, Filia KM, Filia SL, Benitez J, Kulkarni J. (2005) Victimization of patients with schizophrenia and related disorders. Australia and New Zealand Journal of Psychiatry, 39(3), 169-74. (1), 187-9.
- The Royal College of Psychiatrists & The British Psychological Society (2003) Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care. London: Gaskell and the British Psychological Society.
- ^ van Os J, Burns T, Cavallaro R, Leucht S, Peuskens J, Helldin L, Bernardo M, Arango C, Fleischhacker W, Lachaux B, Kane JM. (2006) Standardized remission criteria in schizophrenia. Acta Psychiatrica Scandinavica, 113(2), 91-5.
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. (2005) Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. The New England Journal of Medicine, 353 (12), 1209-23.
- Leucht S, Wahlbeck K, Hamann J, Kissling W. (2003) New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet, 361(9369), 1581-9.
- Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E, Stringfellow J, Ingenito G, Marder SR (2003) Aripiprazole, an Antipsychotic With a Novel Mechanism of Action, and Risperidone vs Placebo in Patients With Schizophrenia and Schizoaffective Disorder. Archives of General Psychiatry, 60(7), 681–90.
- Kay SR, Fiszbein A, Opler LA. (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261-76.
- Cormac I, Jones C, Campbell C. (2002) Cognitive behaviour therapy for schizophrenia. Cochrane Database of systematic reviews, (1), CD000524.
- Zimmermann, G., Favrod, J., Trieu, V. H., & Pomini, V. (2005) The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophrenia Research, 77, 1-9.
- Wykes T, Brammer M, Mellers J, Bray P, Reeder C, Williams C, Corner J. (2002) Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia. British Journal of Psychiatry, 181, 144-52.
- Kulhara P. (1994) Outcome of schizophrenia: some transcultural observations with particular reference to developing countries. European Archives of Psychiatry and Clinical Neuroscience, 244(5), 227–35.
-
Crawford, Mike J. (2006). "Music therapy for in-patients with schizophrenia: Exploratory randomised controlled trial". The British Journal of Psychiatry (2006). 189: 405–409.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help); Unknown parameter|quotes=ignored (help) - Burton, R. The Anatomy of Melancholy. Cf. especially subsection 3, on and after line 3480, "Music a Remedy".
- Peet M, Stokes C. (2005) Omega-3 fatty acids in the treatment of psychiatric disorders. Drugs, 65(8), 1051-9.
- Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A. (1987) The Vermont longitudinal study of persons with severe mental illness, II: Long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. American Journal of Psychiatry, 144(6), 727–35.
- Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM (2004) Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. American Journal of Psychiatry, 161, 473-479.
- Hopper K, Wanderling J (2000) Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia. Schizophrenia Bulletin, 26 (4), 835-46.
- Hannerz H, Borga P, Borritz M. (2001) Life expectancies for individuals with psychiatric diagnoses. Public Health, 115 (5), 328-37.
- Radomsky ED, Haas GL, Mann JJ, Sweeney JA (1999) Suicidal behavior in patients with schizophrenia and other psychotic disorders. American Journal of Psychiatry, 156(10), 1590–5.
- Caldwell CB, Gottesman II. (1990) Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophrenia Bulletin, 16(4), 571–89.
- Swartz MS, Wagner HR, Swanson JW, Stroup TS, McEvoy JP, Canive JM, Miller del D, Reimherr F, McGee M, Khan A, Van Dorn R, Rosenheck RA, Lieberman JA. (2006) Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study. Journal of Nervous and Mental Disease, 194(3), 164-72.
- Arseneault L, Cannon M, Witton J, Murray RM. (2004) Causal association between cannabis and psychosis: examination of the evidence. British Journal of Psychiatry, 184, 110-7. (full text)
- McNeill, Ann (2001). "Smoking and mental health - a review of the literature" (PDF). SmokeFree London Programme. Retrieved 2006-12-14.
{{cite journal}}: Cite journal requires|journal=(help) - Meltzer, H., Gill, B., Petticrew, M., Hinds. K. (1995). "OPCS Surveys of Psychiatric Morbidity Report 3: Economic Activity and Social Functioning of Adults With Psychiatric Disorders". London, Her Majesty’s Stationery Office.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - Kelly, Ciara (1999). "Smoking Habits, Current Symptoms, and Premorbid Characteristics of Schizophrenic Patients in Nithsdale, Scotland". The American Journal of Psychiatry. 156. American Psychiatric Association: 1751–1757. Retrieved 2006-12-14.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Hughes, J.R. (1986). "Prevalence of smoking among psychiatric outpatients". The American Journal of Psychiatry. 143. American Psychiatric Association: 993–997. Retrieved 2006-12-14.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Zammit S, Allebeck P, Dalman C, Lundberg I, Hemmingsson T, Lewis (2003) Investigating the association between cigarette smoking and schizophrenia in a cohort study. American Journal of Psychiatry, 160 (12), 2216–21.
- ^ Compton, Michael T. (2004-07-30). "Cigarette Smoking in Individuals with Schizophrenia". Medscape Psychiatry & Mental Health. Retrieved 2006-12-17.
- Crow, T. J. (1997) Schizophrenia as failure of hemispheric dominance for language. Trends in Neurosciences, 20(8), 339–343.
- Polimeni J, Reiss JP. (2002) How shamanism and group selection may reveal the origins of schizophrenia. Medical Hypothesis, 58(3), 244–8.
- Torrey EF, Yolken RH. (2003) Toxoplasma gondii and schizophrenia. Emerging Infectious Diseases, 9 (11), 1375-80.
- Wang HL, et al. (2006) Prevalence of Toxoplasma infection in first-episode schizophrenia and comparison between Toxoplasma-seropositive and Toxoplasma-seronegative schizophrenia, Acta Psychiatrica Scandinavica, 114 (1), 40-48.
- Zhang, Jie (2005) Continual-activation theories of schizophrenia and restless legs syndrome, Dynamical Psychology.
Categories: