| Revision as of 21:32, 5 August 2022 editYerachmiel C (talk | contribs)Extended confirmed users652 editsNo edit summaryTag: Visual edit← Previous edit | Revision as of 21:32, 5 August 2022 edit undoYerachmiel C (talk | contribs)Extended confirmed users652 editsmNo edit summaryTag: Visual editNext edit → | ||
| Line 6: | Line 6: | ||
| == Physiology == | == Physiology == | ||
| {{refimprove|date=February 2016}} | {{refimprove|date=February 2016}} | ||
| The P wave is a summation wave generated by the depolarization front as it transits the atria. Normally the right atrium depolarizes slightly earlier than left atrium since the depolarization wave originates in the ], in the high right atrium and then travels to and through the left atrium. |
The P wave is a summation wave generated by the depolarization front as it transits the atria. Normally the right atrium depolarizes slightly earlier than left atrium since the depolarization wave originates in the ], in the high right atrium and then travels to and through the left atrium. The depolarization front is carried through the atria along semi-specialized conduction pathways including ] resulting in uniform shaped waves. Depolarization originating elsewhere in the atria (atrial ectopics) result in P waves with a different morphology from normal. | ||
| ==Pathology== | ==Pathology== | ||
| Line 19: | Line 19: | ||
| }}</ref> or hypertrophy.<ref name="Lungmore2004" /> | }}</ref> or hypertrophy.<ref name="Lungmore2004" /> | ||
| If at least three different shaped P waves can be seen in a given ECG lead tracing, this implies that even if one of them arises from the SA node, at least two others are arising elsewhere. |
If at least three different shaped P waves can be seen in a given ECG lead tracing, this implies that even if one of them arises from the SA node, at least two others are arising elsewhere. This is taken as evidence of multiple (i.e. at least two) ], and is called multifocal (or more correctly, multiform) atrial rhythm if the rate is ≤100) or ] if the rate is over 100.<ref name="Kastor_1990">{{cite journal |author = Kastor JA |title = Multifocal Atrial Tachycardia |journal = N Engl J Med |volume = 322 |issue = 24 |pages = 1713–1717 |year = 1990 |pmid = 2188131 | doi = 10.1056/NEJM199006143222405}}</ref> This appears particularly commonly in exacerbations of ].<ref name="Seema_2006">{{cite journal |vauthors=Kothari SA, Apiyasawat S, Asad N, Spodick DH |title = Evidence supporting a new rate threshold for multifocal atrial tachycardia |journal = Clin Cardiol |volume = 28 |issue = 12 |pages = 3561–3563 |year = 2006 |pmid = 16405199 | doi = 10.1002/clc.4960281205|pmc = 6654295 }}</ref> | ||
| If the baseline has a totally irregular form, this suggests fibrillatory waves of ] or possibly artefact; a saw tooth shaped baseline suggests the flutter waves of ]. |
If the baseline has a totally irregular form, this suggests fibrillatory waves of ] or possibly artefact; a saw tooth shaped baseline suggests the flutter waves of ]. With either of these rhythms, if the ventricular rate is fast, the fibrillatory or flutter waves can easily be misinterpreted as P waves. | ||
| Absence of the '''P wave''' with a flat ] may indicate: | Absence of the '''P wave''' with a flat ] may indicate: | ||
Revision as of 21:32, 5 August 2022
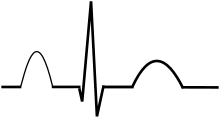
Represents atrial depolarization, which results in atrial contraction

The P wave on the ECG represents atrial depolarization, which results in atrial contraction, or atrial systole.
Physiology
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "P wave" electrocardiography – news · newspapers · books · scholar · JSTOR (February 2016) (Learn how and when to remove this message) |
The P wave is a summation wave generated by the depolarization front as it transits the atria. Normally the right atrium depolarizes slightly earlier than left atrium since the depolarization wave originates in the sinoatrial node, in the high right atrium and then travels to and through the left atrium. The depolarization front is carried through the atria along semi-specialized conduction pathways including Bachmann's bundle resulting in uniform shaped waves. Depolarization originating elsewhere in the atria (atrial ectopics) result in P waves with a different morphology from normal.
Pathology
Peaked P waves (> 0.25 mV) suggest right atrial enlargement, cor pulmonale, (P pulmonale rhythm), but have a low predictive value (~20%).
A P wave with increased amplitude can indicate hypokalemia. It can also indicate right atrial enlargement.
A P wave with decreased amplitude can indicate hyperkalemia.

Bifid P waves (known as P mitrale) indicate left-atrial abnormality - e.g. dilatation or hypertrophy.
If at least three different shaped P waves can be seen in a given ECG lead tracing, this implies that even if one of them arises from the SA node, at least two others are arising elsewhere. This is taken as evidence of multiple (i.e. at least two) ectopic foci, and is called multifocal (or more correctly, multiform) atrial rhythm if the rate is ≤100) or multifocal atrial tachycardia if the rate is over 100. This appears particularly commonly in exacerbations of chronic obstructive lung disease.
If the baseline has a totally irregular form, this suggests fibrillatory waves of atrial fibrillation or possibly artefact; a saw tooth shaped baseline suggests the flutter waves of atrial flutter. With either of these rhythms, if the ventricular rate is fast, the fibrillatory or flutter waves can easily be misinterpreted as P waves.
Absence of the P wave with a flat baseline may indicate:
- Fine atrial fibrillation
- Sinoatrial arrest (with a secondary escape rhythm)
If P waves are not clearly delineated in the surface ECG, a Lewis lead may be used to better visualize P waves.
Atrial repolarization
This occurs a mean of 320 ms after the end of the P wave, with a duration of 2-3 times that of the P wave and a polarity always opposite to that of the P wave. It is represented on the surface ECG by a so-called Ta wave. The clinical relevance of this is that, although a normal phenomenon, the nadir of the Ta wave can occur just after the QRS complex and cause ST depression similar to (and easily mistaken with) that occurring with disease states such as cardiac ischaemia.
Related pages
References
- ^ Longmore, Murray (2004). Oxford Handbook of Clinical Medicine 8th edition page 90. Oxford University Press. ISBN 978-0-19-852558-5.
- Reeves WC, Hallahan W, Schwiter EJ, Ciotola TJ, Buonocore E, Davidson W (1981). "Two-dimensional echocardiographic assessment of electrocardiographic criteria for right atrial enlargement". Circulation. 64 (2): 387–391. doi:10.1161/01.CIR.64.2.387. PMID 6454512.
- "Hypokalaemia".
- Yanowitz, Frank G. "VII. Atrial Enlargement". ECG Learning Center. Archived from the original on 2010-03-29. Retrieved 2009-09-05.
- Levis, Joel T (2013). "ECG Diagnosis: Hyperkalemia". The Permanente Journal. 17 (1): 69. doi:10.7812/TPP/12-088. ISSN 1552-5767. PMC 3627796. PMID 23596374.
- Munuswamy K, Alpert MA, Martin RH, Whiting RB, Mechlin NJ (1983). "Sensitivity and specificity of commonly used electrocardiographic criteria for left atrial enlargement determined by m-mode echocardiography". Am J Cardiol. 53 (6): 829–832. doi:10.1016/0002-9149(84)90413-2. PMID 6230922.
- Kastor JA (1990). "Multifocal Atrial Tachycardia". N Engl J Med. 322 (24): 1713–1717. doi:10.1056/NEJM199006143222405. PMID 2188131.
- Kothari SA, Apiyasawat S, Asad N, Spodick DH (2006). "Evidence supporting a new rate threshold for multifocal atrial tachycardia". Clin Cardiol. 28 (12): 3561–3563. doi:10.1002/clc.4960281205. PMC 6654295. PMID 16405199.
- Smith, SW. "Atrial Repolarization Wave Mimicking ST Depression". Retrieved 22 October 2014.
| Physiology of the cardiovascular system | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heart |
| ||||||||||||
| Vascular system/ hemodynamics |
| ||||||||||||