| Revision as of 04:09, 7 March 2009 edit64.149.82.230 (talk)No edit summary← Previous edit | Revision as of 14:40, 14 March 2009 edit undoTransity (talk | contribs)Pending changes reviewers8,358 edits →Alternative therapies: If you can't CITE evidence, then you can't say that it exists.Next edit → | ||
| Line 87: | Line 87: | ||
| ===Alternative therapies=== | ===Alternative therapies=== | ||
| Alternatives to conventional medical approaches include ] |
Alternatives to conventional medical approaches include ] manipulations of the jaw, targeted to produce lymphatic flow and allow normal opening of the Eustachian tube.<ref>http://www.jaoa.org/cgi/content/abstract/100/10/635</ref> There is no known evidence of the effectiveness of this treatment. | ||
| ==History== | ==History== | ||
Revision as of 14:40, 14 March 2009
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Otitis media" – news · newspapers · books · scholar · JSTOR (February 2008) (Learn how and when to remove this message) |
| This article needs attention from an expert on the subject. Please add a reason or a talk parameter to this template to explain the issue with the article. When placing this tag, consider associating this request with a WikiProject. (September 2008) |
| Otitis media | |
|---|---|
| Specialty | Otorhinolaryngology, audiology |
Otitis media is inflammation of the middle ear, or middle ear infection (the word otitis is Greek and it means “inflammation of the ear”, and media means middle).
Otitis media occurs in the area between the ear drum (the end of the outer ear) and the inner ear, including a duct known as the Eustachian tube. It is one of the two categories of ear inflammation that can underly what is commonly called an earache, the other being otitis externa. Diseases other than ear infections can also cause ear pain, including cancers of any structure that shares nerve supply with the ear.
Otitis media is very common in childhood, with the average toddler having two to three episodes a year, almost always accompanied by a viral upper respiratory infection (URI), mostly the common cold. The rhinoviruses (nose viruses) that cause the common cold infect the Eustachian tube that goes from the back of the nose to the middle ear, causing swelling and compromise of pressure equalization, which is the normal function of the tube. In general, the more severe and prolonged the compromise of Eustachian tube function, the more severe the consequences are to the middle ear and its delicate structures. If a person is born with poor Eustachian tube function, this greatly increases the likelihood of more frequent and severe episodes of otitis media. Progression to chronic otitis media is much more common in this group of people, who often have a family history of middle ear disease.
Types
Otitis media has many degrees of severity, and various names are used to describe each. The terminology is sometimes confusing because of multiple terms being used to describe the same condition. A common misconception with ear infection is that sufferers think that a symptom is itchy ear. Although sufferers may feel discomfort, an itchy ear is not a symptom of ear infection.
Acute otitis media
Acute otitis media (AOM) is most often purely viral and self-limited, as is its usual accompanying viral URI. There is congestion of the ears and perhaps mild discomfort and popping, but the symptoms resolve with the underlying URI. If the middle ear, which is normally sterile, becomes contaminated with bacteria, pus and pressure in the middle ear can result, and this is called acute bacterial otitis media. Viral acute otitis media can lead to bacterial otitis media in a very short time, especially in children, but it usually does not. The individual with bacterial acute otitis media has the classic "earache", pain that is more severe and continuous and is often accompanied by fever of 102 °F (39 °C) or more.. Bacterial cases may result in perforation of the ear drum, infection of the mastoid space (mastoiditis) and in very rare cases further spread to cause meningitis.
Otitis media with effusion
Otitis media with effusion (OME), also called serous or secretory otitis media (SOM), is simply a collection of fluid that occurs within the middle ear space as a result of the negative pressure produced by altered Eustachian tube function. This can occur purely from a viral URI, with no pain or bacterial infection, or it can precede and/or follow acute bacterial otitis media. Fluid in the middle ear sometimes causes conductive hearing impairment, but only when it interferes with the normal vibration of the eardrum by sound waves. Over weeks and months, middle ear fluid can become very thick and glue-like (thus the name glue ear), which increases the likelihood of its causing conductive hearing impairment. Early-onset OME is associated with feeding while lying down and early entry into group child care, while parental smoking, too short a period of breastfeeding and greater amounts of time spent in group child care increased the duration of OME in the first two years of life.
Chronic suppurative otitis media
Chronic suppurative otitis media involves a perforation (hole) in the eardrum and active bacterial infection within the middle ear space for several weeks or more. There may be enough pus that it drains to the outside of the ear (otorrhea), or the purulence may be minimal enough to only be seen on examination using a binocular microscope. This disease is much more common in persons with poor Eustachian tube function. Hearing impairment often accompanies this disease.
Symptoms
When the middle ear becomes acutely infected by bacteria, pressure builds up behind the ear drum, usually but not always causing pain. In severe or untreated cases, the tympanic membrane may rupture, allowing the pus in the middle ear space to drain into the ear canal. If there is enough of it, this drainage may be obvious. Even though the rupture of the tympanic membrane suggests a traumatic process, it is almost always associated with the dramatic relief of pressure and pain. In a simple case of acute otitis media in an otherwise healthy person, the body's defenses are likely to resolve the infection and the ear drum nearly always heals. Antibiotic administration can prevent perforation of the eardrum and hasten recovery of the ear.
Instead of the infection and eardrum perforation resolving, however, drainage from the middle ear can become a chronic condition. As long as there is active middle ear infection, the eardrum will not heal. The World Health Organization defines Chronic Suppurative Otitis Media (CSOM) as "a stage of ear disease in which there is chronic infection of the middle ear cleft, a non-intact tympanic membrane (i.e. perforated eardrum) and discharge (otorrhoea), for at least the preceding two weeks" (WHO 1998). (Notice WHO's use of the term serous to denote a bacterial process, whereas the same term is generally used by ear physicians in the United States to denote simple fluid collection within the middle ear behind an intact eardrum. Chronic otitis media is the term used by most ear physicians worldwide to describe a chronically infected middle ear with eardrum perforation.)
Causes
Streptococcus pneumoniae and nontypable Haemophilus influenzae are the most common bacterial causes of otitis media. Tubal dysfunction leads to the ineffective clearing of bacteria from the middle ear. In older adolescents and young adults, the most common cause of ear infections during their childhoods was Haemophilus influenzae. The role of the anti-H. influenzae vaccine that children are regularly given in changing patterns of ear infections is unclear, as this vaccine is active only against strains of serotype b, which rarely cause otitis media.
As well as being caused by Streptococcus pneumoniae and Haemophilus influenzae it can also be caused by the common cold. Colds indirectly cause many cases of otitis media by damaging the normal defenses of the epithelial cells in the upper respiratory tract.
Another common culprit of otitis media includes Moraxella catarrhalis, a gram-negative, aerobic, oxidase positive diplococcus. Less commonly otitis media can be caused by Mycobacterium tuberculosis.
Progression
Typically, acute otitis media follows a cold: after a few days of a stuffy nose the ear becomes involved and can cause severe pain. The pain will usually settle within a day or two, but can last over a week. Sometimes the ear drum ruptures, discharging pus from the ear, but the ruptured drum will usually heal rapidly.
At an anatomic level, the typical progression of acute otitis media occurs as follows: the tissues surrounding the Eustachian tube swell due to an upper respiratory infection, allergies, or dysfunction of the tubes. The Eustachian tube remains blocked most of the time. The air present in the middle ear is slowly absorbed into the surrounding tissues. A strong negative pressure creates a vacuum in the middle ear, and eventually the vacuum reaches a point where fluid from the surrounding tissues accumulates in the middle ear. This is seen as a progression from a Type A tympanogram to a Type C to a Type B tympanogram. The fluid may become infected. It has been found that dormant bacteria behind the Tympanum (eardrum) multiply when the conditions are ideal, infecting the middle ear fluid.
Susceptibility in children
Children below the age of seven years are much more prone to otitis media since the Eustachian tube is shorter and at more of a horizontal angle than in the adult ear. They also have not developed the same resistance to viruses and bacteria as adults. Numerous studies have correlated the incidence of acute otitis media in children with various factors such as nursing in infancy, bottle feeding when supine, parental smoking, diet, allergies, and automobile emissions; but the most obvious weakness of such studies is the inability to control the variable of exposure to viral agents during the studies. One must also keep in mind that correlation does not establish causation. Breastfeeding for the first twelve months of life is associated with a reduction in the number, and duration of all OM infections. Well pacifier use is associated with more frequent episoids of AOM.
Treatment
Acute otitis media
Management of pain
To treat the pain caused by otitis media oral as well as topical analgesics are often used. Oral agents may include ibuprofen, acetaminophen, and / or narcotics. Topical agents have also been shown to be effective, such as antipyrine and benzocaine ear drops.
Antibiotics
Many guidelines suggest deferring the start of antibiotics for one to three days avoiding the need for antibiotics for two out of three children without adverse effect on longterm outcomes for those whose treatment is deferred. First line antibiotic treatment, if warranted, is amoxicillin. If the bacteria is resistant, then amoxicillin-clavulanate or another penicillin derivative plus beta lactamase inhibitor is second line.
Treatment of acute otitis media however is controversial. Much of the controversy centers around the difficulty of distinguishing viral infection from bacterial infection and the fact that viral infection can progress to bacterial infection at any time. Primary care providers, such as general practitioners and pediatricians, often have a monocular otoscope and perhaps a tympanometer as their only diagnostic tools, which makes this distinction difficult, especially if the canal is small and there is wax in the ear that obscures a clear view of the eardrum. Also, an upset child's crying can cause the eardrum to look inflamed due to causing distention of the small blood vessels on it, mimicking the redness associated with otitis media. Because of a tradition of inappropriate prescribing of antibiotics for viral acute otitis media, their use has recently been condemned by many primary care practitioners for most cases of acute otitis media. Ear specialists tend to disagree with this philosophy and promote efforts to distinguish between viral and bacterial infection, so as to optimize treatment results by giving antibiotics only for bacterial infection. Acute bacterial otitis media can cause pain that leads to sleepless nights for both children and parents, can cause eardrum perforations, not all of which heal, and can spread to cause mastoiditis and/or meningitis, brain abscess, and even death if a severe infection goes untreated long enough. High fever can occur and can cause febrile seizures. Appropriate antibiotic administration prevents most such complications. On the other hand, it is generally agreed that acute otitis media that is purely viral will usually resolve without antibiotic treatment, although associated persistent middle ear effusions may require medical intervention.
Chronic cases or with effusion
In chronic cases or with effusions present for months, surgery is sometimes performed by an otolaryngologist (ear, nose, and throat specialist) or by an otologist (ear specialist), to insert a tympanostomy tube (called a "grommet") into the eardrum to allow air to pass through into the middle ear, and thus release any pressure buildup and help clear excess fluid within.
Alternative therapies
Alternatives to conventional medical approaches include osteopathic manipulations of the jaw, targeted to produce lymphatic flow and allow normal opening of the Eustachian tube. There is no known evidence of the effectiveness of this treatment.
History
Prior to the invention of antibiotics, severe acute otits media was mainly remedied surgically by Myringotomy. An outpatient procedure, it consists of making a small incision in the tympanic membrane to relieve pressure build-up.
Gallery
-
 Otitis media acuta - Myringitis bullosa
Otitis media acuta - Myringitis bullosa
-
-
 Influenza
Influenza
-
 Otitis media acuta
Otitis media acuta
-
 Otitis media acuta
Otitis media acuta
-
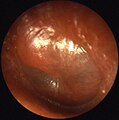
 Otitis media chronica mesotympanalis
Otitis media chronica mesotympanalis
-
 Otitis media chronica mesotympanalis
Otitis media chronica mesotympanalis
-
 Otitis media chronica mesotympanalis
Otitis media chronica mesotympanalis
-
 Otitis media chronica mesotympanalis
Otitis media chronica mesotympanalis
References
- Owen MJ, Baldwin CD, Swank PR, Pannu AK, Johnson DL, Howie VM (1993). "Relation of infant feeding practices, cigarette smoke exposure, and group child care to the onset and duration of otitis media with effusion in the first two years of life". J. Pediatr. 123 (5): 702–11. doi:10.1016/S0022-3476(05)80843-1. PMID 8229477.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Dewey KG, Heinig MJ, Nommsen-Rivers LA (1995). "Differences in morbidity between breast-fed and formula-fed infants". J. Pediatr. 126 (5 Pt 1): 696–702. doi:10.1016/S0022-3476(95)70395-0. PMID 7751991.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Rovers MM, Numans ME, Langenbach E, Grobbee DE, Verheij TJ, Schilder AG (2008). "Is pacifier use a risk factor for acute otitis media? A dynamic cohort study". Fam Pract. 25 (4): 233–6. doi:10.1093/fampra/cmn030. PMID 18562333.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "BestBets: Role of topical analgesia in acute otitis media".
- Damoiseaux R (2005). "Antibiotic treatment for acute otitis media: time to think again". CMAJ. 172 (5): 657–8. PMID 15738492.
- Marchetti F, Ronfani L, Nibali S, Tamburlini G (2005). "Delayed prescription may reduce the use of antibiotics for acute otitis media: a prospective observational study in primary care". Arch Pediatr Adolesc Med. 159 (7): 679–84. doi:10.1001/archpedi.159.7.679. PMID 15997003.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Little P, Moore M, Warner G, Dunleavy J, Williamson I (2006). "Longer term outcomes from a randomised trial of prescribing strategies in otitis media". Br J Gen Pract. 56 (524): 176–82. PMID 16536957.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Damoiseaux R, van Balen F, Hoes A, Verheij T, de Melker R (2000). "Primary care based randomised, double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years". BMJ. 320 (7231): 350–4. doi:10.1136/bmj.320.7231.350. PMID 10657332.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Arroll B (2005). "Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews". Respir Med. 99 (3): 255–61. doi:10.1016/j.rmed.2004.11.004. PMID 15733498.
- Rovers MM, Glasziou P, Appelman CL, Burke P, McCormick DP, Damoiseaux RA, Gaboury I, Little P, Hoes AW. (2006). "Antibiotics for acute otitis media: a meta-analysis with individual patient data". Lancet. 368 (9545): 1429–35. doi:10.1016/S0140-6736(06)69606-2. PMID 17055944.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - http://www.jaoa.org/cgi/content/abstract/100/10/635
External links
- Specialist Library for ENT and Audiology High quality research and patient information on otitis media
- More on otitis media information on otitis media
| Diseases of the outer and middle ear | |
|---|---|
| Outer ear | |
| Middle ear and mastoid | |
| Symptoms | |
| Tests | |
| Common cold | |
|---|---|
| Viruses | |
| Symptoms | |
| Complications | |
| Drugs | |