| Revision as of 18:01, 22 October 2011 editCheMoBot (talk | contribs)Bots141,565 edits Updating {{drugbox}} (changes to verified and watched fields - updated 'CAS_number_Ref') per Chem/Drugbox validation (report errors or bugs)← Previous edit | Revision as of 22:48, 10 November 2011 edit undoBeetstra (talk | contribs)Edit filter managers, Administrators172,055 edits Script assisted update of identifiers for the Chem/Drugbox validation project (updated: 'DrugBank').Next edit → | ||
| Line 29: | Line 29: | ||
| | PubChem = 119182 | | PubChem = 119182 | ||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | ||
| | DrugBank = |
| DrugBank = DB00631 | ||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| | ChemSpiderID = 106472 | | ChemSpiderID = 106472 | ||
Revision as of 22:48, 10 November 2011
Pharmaceutical compound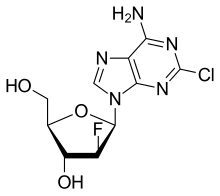 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607012 |
| ATC code | |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.159.663 |
| Chemical and physical data | |
| Formula | C10H11ClFN5O3 |
| Molar mass | 303.677 g/mol g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (what is this?) (verify) | |
Clofarabine is a purine nucleoside antimetabolite marketed in the U.S. and Canada as Clolar. In Europe and Australia/New Zealand the product is marketed under the name Evoltra. It is FDA-approved for treating a type of leukaemia called relapsed or refractory acute lymphoblastic leukaemia (ALL) in children, after at least two other types of treatment have failed. It is not known if it extends life expectancy. Some investigations of effectiveness in cases of acute myeloid leukaemia (AML) and juvenile myelomonocytic leukaemia (JMML) have been carried out. Ongoing trials are assessing its efficacy, if any, for managing other cancers.
Side effects
- Tumor lysis syndrome (TLS). Clofarabine quickly kills leukaemia cells in the blood. The body may react to this. Signs include hyperkalemia, hyperuricemia, and hyperphosphatemia. TLS is very serious and can lead to death if it is not treated right away.
- Systemic Inflammatory Response Syndrome (SIRS): Symptoms include fast breathing, fast heartbeat, low blood pressure, and fluid in the lungs.
- Bone marrow problems (suppression). Clofarabine can stop the bone marrow from making enough red blood cells, white blood cells, and platelets. Serious side effects that can happen because of bone marrow suppression include severe infection (sepsis), bleeding, and anemia.
- Effects on pregnancy and breastfeeding. Girls and women should not become pregnant or breastfeed during treatment which may harm the baby.
- Dehydration and low blood pressure. Clofarabine can cause vomiting and diarrhea which may lead to low body fluid (dehydration). Signs and symptoms of dehydration include dizziness, lightheadedness, fainting spells, or decreased urination.
- Other side effects. The most common side effects are stomach problems (including vomiting, diarrhea, and nausea), and effects on blood cells (including low red blood cells count, low white blood cell count, low platelet count, fever, and infection. Clofarabine can also cause tachycardia and can affect the liver and kidneys.
Contraindications
- pregnancy or planned pregnancy
- breast-feeding
- liver problems
- kidney problems
Drug interactions
- nephrotoxic drugs
- hepatotoxic drugs
Delivery
- By intravenous infusion.
- Dosage is a 2 hour infusion (52 mg/m²) every day for five days. The cycle is repeated every 2 to 6 weeks.
- Regular blood tests to monitor his or her blood cells, kidney function, and liver function.
Results of clinical trials
Efficacy and safety were demonstrated in a single multi-center trial that enrolled 40 patients aged 2-19. The patients were suffering with relapsed or refractory acute lymphoblastic leukaemia (ALL) (An additional 9 patients suffering with acute myelogenous leukaemia (AML) had similar pharmacokinetics but are not included in the figure below.) Most patients had received 2 to 4 prior regimens and 15/49 (31%) had undergone at least one transplant. The median age was 12 years. Clofarabine was given at a dose of 52 mg/m, intravenously, over 2 hours daily x 5 repeated every 2 to 6 weeks following recovery or return to baseline organ function. The study endpoints were the rate of complete response (CR) and the rate of complete response without platelet recovery (CRp). The former was defined as no evidence of circulating blasts or extramedullary disease, an M1 bone marrow, and recovery of peripheral platelet and absolute neutrophil counts; the latter was defined as meeting all criteria for CR except for platelet count recovery. Response rates were determined by an Independent Response Review Panel (IRRP).
Six patients (12%) achieved a CR and 4 patients (8%) achieved a CRp, and 5 patients (10%) achieved a PR. Of the 15 responding patients, 6 had post-clofarabine bone marrow transplantation. Hence, response durations could not be determined. In the patients who were not transplanted, the response durations for CR were 43, 50, 82, 93+, and 160+ days; for CRp the response duration was 32 days.
The principal clofarabine toxicities were nausea, vomiting, hematologic toxicity, febrile neutropenia, hepatobiliary toxicity, infections and renal toxicity. Clofarabine can produce systemic inflammatory response syndrome/capillary leak syndrome (SIRS), manifested by the rapid development of tachypnea, tachycardia, hypotension, shock, and multi-organ failure. Cardiac toxicity was characterized as left ventricular systolic dysfunction; tachycardia may also occur.
Approval
Clolar was Food and Drug Administration (FDA) Approved 28 December 2004. (Under accelerated approval regulations requiring further clinical studies.)
External links
- Clofarabine information on Cancerbackup.
- FDA usage leaflet.
- Clolar.com homepage.
- FDA approval notice.