This is an old revision of this page, as edited by AntiVandalBot (talk | contribs) at 03:30, 12 October 2006 (BOT - rv 204.244.150.7 (talk) to last version by Khukri). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 03:30, 12 October 2006 by AntiVandalBot (talk | contribs) (BOT - rv 204.244.150.7 (talk) to last version by Khukri)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)The testicles, or testes (singular testis), are the male generative glands in animals. Male mammals have two testicles, which are often contained within an extension of the abdomen called the scrotum.
In land mammals, with the exception of the elephant the testes are located outside of the body, as they are suspended by the spermatic cord and within the scrotum. This is due to the fact that fertile spermatogenesis in mammals is more efficient at a temperature somewhat less than the core body temperature (37°C or 98.6°F for humans). The cremasteric muscle is part of the spermatic cord. When this muscle contracts, the cord is shortened and the testicle is moved closer up toward the body, which provides slightly more warmth to maintain optimal testicular temperature. When cooling is required, the cremasteric muscle relaxes and the testicle is lowered away from the warm body and are able to cool. This phenomenon is known as the cremasteric reflex. It also occurs in response to stress (the testicles rise up toward the body in an evolutionary effort to protect them in a fight), and there are persistent reports that relaxation indicates approach of orgasm. There is a noticeable tendency to also retract during orgasm.
The testicles can also be lifted voluntarily using the pubococcygeus muscle, which partially activates related muscles. This can sometimes be triggered by tightening or sucking in the stomach or abdomen.
Animals other than mammals do not have externalized testicles. Birds, despite having very high core body temperatures have internal testes: it was once theorized that birds used their air sacs to cool the testes internally, but later studies revealed that birds' testes function at core body temperature. Marine mammals also have internal testes, but it has recently been shown (eg, for dolphins) that they use elaborate vascular networks to provide the necessary temperature lowering for proper operation.
During puberty, the testicles grow in response to the start of spermatogenesis. Size depends on lytic function, sperm production (amount of spermatogenisis present in testis), interstitial fluid, and Sertoli cell fluid production. After puberty, the volume of the testicles can be increased by over 500% as compared to the pre-pubertal size.
It is most common for one testicle to hang lower than the other. The percentage of men with a lower hanging right testicle or left testicle is about equal. This is due to differences in the vascular anatomical structure on the right and left sides.
Function
Like the ovaries (to which they are homologous), testicles are components of both the reproductive system (being gonads) and the endocrine system (being endocrine glands). The respective functions of the testicles are:
- producing sperm (spermatozoa)
- producing male sex hormones, of which testosterone is the best-known
Both functions of the testicle, sperm-forming and endocrine, are under control of gonadotropic hormones produced by the anterior pituitary:
- luteinizing hormone (LH)
- follicle-stimulating hormone (FSH)
Structure
Under a tough membraneous shell, the tunica albuginea, the testis contains very fine coiled tubes called the seminiferous tubules. The tubes are lined with a layer of cells that, from puberty into old-age, produce sperm cells. The sperm travel from the seminiferous tubules to the rete testis, the efferent ducts, and then to the epididymis where newly-created sperm cells mature (see spermatogenesis). The sperm move into the vas deferens (also called the ductus deferens), which opens into the prostate. Upon sufficient sexual arousal, the process of emission is initiated: mature sperm move from the ampulla of the vas deferens into the ejaculatory duct, where they mix with secretions of the seminal vesicles and exit into the prostatic urethra. The resulting fluid is now called semen, and contains additional secretions from the prostate and bulbourethral glands. The process of ejaculation expels the sperm through the urethra and out of the urethral orifice through muscular contractions.
The genital anatomy described here, along with the neuroanatomy and hormonal systems that enable it to perform ejaculation, have as primary functions the impregnation of a fertile female of the same species, via sexual intercourse with her.
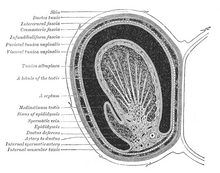
Between the seminiferous tubules are special cells called interstitial cells (Leydig cells) where testosterone and other androgens are formed.
Many anatomical features of the adult testis reflect its developmental origin in the abdomen. Blood supply and lympatic drainage of the testes and scrotum are distinct:
- The paired testicular arteries arise directly from the abdominal aorta and descend through the inguinal canal, while the scrotum and the rest of the external genitalia is supplied by the internal pudendal artery (itself a branch of the internal iliac artery).
- Lymphatic drainage of the testes follows the testicular arteries back to the paraaortic lymph nodes, while lymph from the scrotum drains to the inguinal lymph nodes.
Similarly, the layers of tissue enclosing each testicle are derived from the layers of the anterior abdominal wall. Notably, the cremasteric muscle arises from the internal oblique muscle.
The Blood-Testis Barrier
Large molecules cannot pass from the blood into the lumen of a seminiferous tubule due to the presence of tight junctions between adjacent Sertoli cells. The spermatogonia are in the basal compartment (deep to the level of the tight junctions) and the more mature forms such as primary and secondary spermatocytes and spermatids are in the adluminal compartment. The function of the blood-testis barrier (red highlight in diagram above) may be to prevent an auto-immune reaction. Mature sperm (and their antigens) arise long after immune tolerance is established in infancy. Therefore, since sperm are antigenically different than self tissue, a male animal can react immunologically to his own sperm. In fact, he is capable of making antibodies against them. Injection of sperm antigens causes inflammation of the testis (autoimmune orchitis) and reduced fertility. Thus, the blood-testis barrier may reduce the likelihood that sperm proteins will induce an immune response, reducing fertility and so progeny.
Testicular size
Testicular size as a proportion of body weight varies widely. In the mammalian kingdom, there is a tendency for testicular size to correspond with multiple mates (ie, harems, polygamy). Production of testicular output sperm and spermatic fluid is also larger in polygamous animals, possibly a spermatogenic competition for survival. In normal adult human males, testicular size ranges from the lower end of around 14 cm³ to the upper end larger than 35 cm³. Measurement in the living adult is done in two basic ways: (1) comparing the testicle with ellipsoids of known sizes (orchidometer), or (2) measuring the length, depth and width with a ruler, a pair of calipers or ultrasound imaging. The volume is then calculated, e.g., using the formula for ellipsoids: 4/3 π × r (length) × r (width) x r (depth). Usually right and left testicles are about the same size.
To some extent, it is possible to change testicular size. Short of direct injury or subjecting them to adverse conditions, e.g., higher temperature than they are normally accustomed to, they can be shrunk by competing against their intrinsic hormonal function through the use of externally administered steroidal hormones. Steroids taken for muscle enhancement often have the undesired side effect of testicular shrinkage. Similarly, stimulation of testicular functions via gonadotropic-like hormones may enlarge their size. Testicles may shrink or atrophy during hormone replacement therapy.
Health issues
The testicles are well-known to be very sensitive to impact and injury. The most prominent diseases of testicles are:
- testicular cancer and other neoplasms
- swelling of a testicle, caused by hydrocele testis
- inflammation of the testicles, called orchitis
- inflammation of the epididymis, called epididymitis
- spermatic cord torsion also called testicular torsion
- varicocele - swollen vein from the testes, usually affecting the left testicle
- Anorchidism is the absence of one or both testicles.
The removal of one or both testicles is termed
- orchidectomy, in medicine (where orchiectomy and orchectomy are synonymous), and
- castration in general use, especially when done as punishment or torture
Testicular prostheses are available to mimic the appearance and feel of one or both testicles, when absent as from injury or as treatment for gender identity disorder. There have also been some instances of their implanting in dogs.
Consumption of testicles
See also
- Anorchia
- cryptorchidism (cryptorchismus)
- Polyorchidism
- infertility
- List of homologues of the human reproductive system
- orchidometer
- spermatogenesis
- sterilization (surgical procedure), vasectomy
- Epididymis
- Spermatic cord
- Penis
- Ovary
- Geier Hitch
- WikiSaurus:testicles — the WikiSaurus list of synonyms and slang words for testicles in many languages
External links
- Queries related to Testicle Answered by Physicians and Andrologists
| Female reproductive system | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal |
| ||||||||||||||||||||||||||||||
| External |
| ||||||||||||||||||||||||||||||
| Blood supply | |||||||||||||||||||||||||||||||
| Other | |||||||||||||||||||||||||||||||
| Anatomy of the endocrine system | |||||
|---|---|---|---|---|---|
| Pituitary gland |
| ||||
| Thyroid | |||||
| Parathyroid gland | |||||
| Adrenal gland |
| ||||
| Gonads | |||||
| Islets of pancreas | |||||
| Pineal gland | |||||
| Other | |||||