This is an old revision of this page, as edited by 64.180.230.40 (talk) at 23:23, 5 November 2006. The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 23:23, 5 November 2006 by 64.180.230.40 (talk)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) Medical condition| Schizophrenia | |
|---|---|
| Specialty | Psychiatry, clinical psychology |
Schizophrenia is a psychiatric diagnosis that describes a mental disorder characterized by impairments in the perception or expression of reality and by significant social or occupational dysfunction. A person experiencing untreated schizophrenia is typically characterized as demonstrating disorganized thinking, and as experiencing delusions or auditory hallucinations.
Although the disorder is primarily thought to affect cognition, it can also contribute to chronic problems with behavior and emotion. Due to the many possible combinations of symptoms, heated debate is ongoing about whether the diagnosis necessarily or adequately describes a disorder, or alternatively whether it might represent a number of disorders. For this reason, Eugen Bleuler deliberately called the disease "the schizophrenias" plural, when he coined the present name.
Diagnosis is based on the self-reported experiences of the patient, in combination with secondary signs observed by a psychiatrist, clinical psychologist or other competent clinician. No objective biological test for schizophrenia exists, though studies suggest that genetics, neurobiology and social environment are important contributing factors. Current research into the development of the disorder often focuses on the role of neurobiology, although a reliable and identifiable organic cause has not been found. In the absence of objective laboratory tests to confirm the diagnosis, some question the legitimacy of schizophrenia's status as a disease. Furthermore, some question the status of schizophrenia as a disease on the basis that they do not consider the condition to be an impairment.
The term schizophrenia translates roughly as "shattered mind," and comes from the Greek σχίζω (schizo, "to split" or "to divide") and φρήν (phrēn, "mind"). Despite its etymology, schizophrenia is not synonymous with dissociative identity disorder, also known as multiple personality disorder or "split personality"; in popular culture the two are often confused. Although schizophrenia often leads to social or occupational dysfunction, a predisposition toward aggressive behavior is little associated with the illness.
Patients diagnosed with schizophrenia are highly likely to be diagnosed with other disorders. The lifetime prevalence of substance abuse is typically around 40%. Comorbidity is also high with clinical depression, anxiety disorders, and social problems, and a generally decreased life expectancy is also present. Patients diagnosed with schizophrenia typically live 10-12 years less than their healthy counterparts, owing to increased physical health problems and a high suicide rate.
Overview
Schizophrenia is often described in terms of "positive" and "negative" symptoms. Positive symptoms include delusions, auditory hallucinations and thought disorder and are typically regarded as manifestations of psychosis. Negative symptoms are so named because they are considered to be the loss or absence of normal traits or abilities, and include features such as flat, blunted or constricted affect and emotion, poverty of speech and lack of motivation. Some models of schizophrenia include formal thought disorder and planning difficulties in a third group, a "disorganization syndrome".
Additionally, neurocognitive deficits may be present. These may take the form of reduced or impaired psychological functions such as memory, attention, problem-solving, executive function or social cognition.
Onset of schizophrenia typically occurs in late adolescence or early adulthood, with males tending to show symptoms earlier than females.
In 1893 Psychiatrist Emil Kraepelin was the first to draw a distinction between what he termed dementia praecox ("premature dementia") and other psychotic illnesses. In 1908, "dementia praecox" was renamed "schizophrenia" by psychiatrist Eugen Bleuler, who discovered that the disorder is not a form of dementia nor premature.
The diagnostic category of schizophrenia has been widely criticised as lacking in scientific validity or reliability, consistent with evidence of poor levels of consistency in diagnostic practices and the use of criteria. One alternative suggests that the problems and issues making up the diagnosis of schizophrenia would be better addressed as individual dimensions along which everyone varies, such that there is a spectrum or continuum rather than a cut-off between normal and ill. This approach appears consistent with research on schizotypy and of a relatively high prevalence of psychotic experiences and delusional beliefs amongst the general public.
The wider anti-psychiatry movement also often argues against the diagnosis, for example arguing that classifying unusual thoughts, feelings and behaviors as a medical illness in this way is unscientific, stigmatizing, and legitimises the social control of people whom society finds undesirable but who have committed no crime.
Although no common cause of schizophrenia has been identified in all individuals diagnosed with the condition, currently most researchers and clinicians believe it results from a combination of both brain vulnerabilities (either inherited or acquired) and stressful life-events. This widely-adopted approach is known as the 'stress-vulnerability' model, and much scientific debate now focuses on how much each of these factors contributes to the development and maintenance of schizophrenia.
It is also thought that processes in early neurodevelopment are important, particularly prenatal processes. In adult life, particular importance has been placed upon the function (or malfunction) of dopamine in the mesolimbic pathway in the brain. This theory, known as the dopamine hypothesis of schizophrenia largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, reduced psychotic symptoms. However, this theory is now thought to be overly simplistic as a complete explanation. These drugs have now been developed further and antipsychotic medication is commonly used as a first-line treatment. Although effective in many cases, these medications are not well tolerated by many patients due to significant side-effects, and have little positive effect on some individuals.
Differences in brain structure have been found between people with schizophrenia and those without. However, these tend only to be reliable on the group level and, due to the significant variability between individuals, may not be reliably present in any particular individual.
History
Accounts that may relate to symptoms of schizophrenia date back as far as 2000 BC in the Book of Hearts, part of the ancient Ebers papyrus. However, a recent study into the ancient Greek and Roman literature showed that, while the general population probably had an awareness of psychotic disorders, there was no recorded condition that would meet the modern diagnostic criteria for schizophrenia in these societies.
This nonspecific concept of "madness" has been around for many thousands of years, but schizophrenia was only classified as a distinct mental disorder by Kraepelin in 1893. He was the first to make a distinction in the psychotic disorders between what he called dementia praecox (a term first used by psychiatrist Benedict A. Morel) and manic depression. Kraepelin believed that dementia praecox was primarily a disease of the brain, and particularly a form of dementia. Kraepelin named the disorder 'dementia praecox' (early dementia) to distinguish it from other forms of dementia (such as Alzheimer's disease) which typically occur late in life. He used this term because his studies focused on young adults with dementia.
The term schizophrenia is derived from the Greek words σχίζειν (split) and φρήν (mind) and was coined by Eugene Bleuler in 1908 to refer to the lack of interaction between thought processes and perception. He was also the first to describe the symptoms as "positive" or "negative." Blueler described the main symptoms as 4 "A"'s: flattened Affect, Autism, impaired Association of ideas and Ambivalence. Bleuler suggested the name schizophrenia, as it was obvious that Kraepelin's name was misleading. The word "praecox" implied precocious or early onset, hence premature dementia, as opposed to senile dementia from old age. Bleuler realized the illness was not a dementia, as it did not lead to mental deterioration and could occur early or late in life. Rather, schizophrenia led to a sharpening of the senses and a greater awareness of memories and experiences.
With the name 'schizophrenia' Bleuler intended to capture the separation of function between personality, thinking, memory, and perception, however it is commonly misunderstood to mean that affected persons have a 'split personality' (something akin to the character in Robert Louis Stevenson's The Strange Case of Dr Jekyll and Mr Hyde). Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion perhaps arises in part due to the meaning of Bleuler's term 'schizophrenia' (literally 'split mind'). Interestingly, the first known misuse of this word schizophrenia to mean 'split personality' (in the Jekyll and Hyde sense) was in an article by the poet T. S. Eliot in 1933.
In the first half of the twentieth century schizophrenia was considered by many to be a "hereditary defect", and individuals affected by schizophrenia became subject to eugenics in many countries. Hundreds of thousands were sterilized, with or without consent, the majority in Nazi Germany, the United States, and Scandinavian countries., Many people diagnosed with schizophrenia, together with other people labeled "mentally unfit", were murdered in the Nazi "Operation T-4" program.
Diagnosis
Criteria (signs and symptoms)
Like many mental illnesses, the diagnosis of schizophrenia is based upon the behavior of the person being assessed. There is a list of criteria that must be met for someone to be so diagnosed. These depend on both the presence and duration of certain signs and symptoms.
The most commonly used criteria for diagnosing schizophrenia are from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD). The most recent versions are ICD-10 and DSM-IV-TR.
Below is an abbreviated version of the diagnostic criteria from the DSM-IV-TR; the full version is available here.
To be diagnosed as having schizophrenia, a person must display:
- A) Characteristic symptoms: Two or more of the following, each present for a significant portion of time during a one-month period (or less, if successfully treated)
- delusions
- hallucinations
- disorganized speech (e.g., frequent derailment or incoherence; speaking in abstracts). See thought disorder.
- grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- negative symptoms, i.e., affective flattening (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation).
- Note: Only one Criterion A symptom is required if delusions are bizarre or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other.
- B) Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- C) Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if successfully treated) that meet Criterion A.
Additional criteria (D, E and F) are also given that exclude a diagnosis of schizophrenia if symptoms of mood disorder or pervasive developmental disorder are present. Additionally a diagnosis of schizophrenia is excluded if the symptoms are the direct result of a substance (e.g., abuse of a drug, medication) or a general medical condition.
Subtypes
Historically, schizophrenia in the West was classified into simple, catatonic, hebephrenic, and paranoid. The DSM now contains five sub-classifications of schizophrenia, the ICD-10 identifies 7:
- (295.2/F20.2) catatonic type (where marked absences or peculiarities of movement are present),
- (295.1/F20.1) disorganized type (where thought disorder and flat affect are present together),
- (295.3/F20.0) paranoid type (where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening is absent),
- (295.6/F20.5) residual type (where positive symptoms are present at a low intensity only) and
- (295.9/F20.3) undifferentiated type (psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types has not been met).
NB: Brackets indicate codes for DSM and ICD-10 diagnostic manuals, respectively. Some older classifications still use "Hebephrenic schizophrenia" instead of "Disorganized schizophrenia".
Deficit Syndrome
Currently, there is debate in the field about a new subtype known as the deficit syndrome. It is not currently included in the DSM-IV-TR, however it has been receiving a great deal of attention in the last 20 years. This subtype is more expansive than the other subtypes as a person can be diagnosed with both paranoid schizophrenia and the deficit syndrome. It is characterized by primary negative symptoms (which means that they cannot be caused by such things as the side-effects of medication or depression). People with the deficit syndrome tend to have extremely flat affect (do not appear to be very emotional), do not have good eye contact, do not enjoy normally pleasurable activities (see dysphoria), and seem to be uninterested in social interaction. (There is, however, conflict in the research on this last point. While people who have been diagnosed with the deficit syndrome report being uninterested in social interaction, in the laboratory, they often report normal reactions to the situations.) Patients who have been diagnosed with the deficit syndrome tend to have a worse prognosis as these symptoms tend to be resistant to medication. This fact has brought much needed attention to negative symptoms (which have traditionally not been viewed as important as the positive symptoms).
Presentation
Symptoms may also be described as 'positive symptoms' (those additional to normal experience and behavior) and 'negative symptoms' (the lack or decline in normal experience or behavior). 'Positive symptoms' describe psychosis and typically include delusions, hallucinations and thought disorder. 'Negative symptoms' describe inappropriate or nonpresent emotion, poverty of speech, and lack of motivation. In three-factor models of schizophrenia, a third symptom grouping, the so-called 'disorganization syndrome', is also given. This considers thought disorder and related disorganized behavior to be in a separate symptom cluster from delusions and hallucinations.
Some symptoms, such as social isolation, may be caused by a number of factors. One possible factor is impairment in social cognition, which is associated with schizophrenia, but isolation may also result from an individual reacting to psychotic symptoms (such as paranoia) or avoiding potentially stressful social situations which may exacerbate mental distress in some people.
It is worth noting that many of the positive or psychotic symptoms may occur in a variety of disorders and not only in schizophrenia. The psychiatrist Kurt Schneider tried to list the particular forms of psychotic symptoms that he thought were particularly useful in distinguishing between schizophrenia and other disorders that could produce psychosis. These are called first rank symptoms or Schneiderian first rank symptoms and include delusions of being controlled by an external force, the belief that thoughts are being inserted into or withdrawn from your conscious mind, the belief that your thoughts are being broadcast to other people and hearing hallucinated voices which comment on your thoughts or actions, or may have a conversation with other hallucinated voices. As with other diagnostic methods, the reliability of 'first rank symptoms' has been questioned, although they remain in use as diagnostic criteria in many countries.
Diagnostic issues and controversies
It has been argued that the diagnostic approach to schizophrenia is flawed, as it relies on an assumption of a clear dividing line between what is considered to be mental illness (fulfilling the diagnostic criteria) and mental health (not fulfilling the criteria). Recently it has been argued, notably by psychiatrist Jim van Os and psychologist Richard Bentall, that this makes little sense, as studies have shown that many people have psychotic experiences and have delusion-like ideas without becoming distressed, disabled or diagnosable by the categorical system (potentially because they interpret their experiences in more positive ways, or hold more pragmatic and commonly accepted beliefs).
Of particular concern is that the decision as to whether a symptom is present is a subjective decision by the person making the diagnosis or relies on an incoherent definition (for example, see the entries on delusions and thought disorder for a discussion of this issue). More recently, it has been argued that psychotic symptoms are not a good basis for making a diagnosis of schizophrenia as "psychosis is the 'fever' of mental illness — a serious but nonspecific indicator".
Perhaps because of these factors, studies examining the diagnosis of schizophrenia have typically shown relatively low or inconsistent levels of diagnostic reliability. Most famously, David Rosenhan's 1972 study, published as On being sane in insane places, demonstrated that the diagnosis of schizophrenia was (at least at the time) often subjective and unreliable. More recent studies have found agreement between any two psychiatrists when diagnosing schizophrenia tends to reach about 65% at best. This, and the results of earlier studies of diagnostic reliability (which typically reported even lower levels of agreement) have led some critics to argue that the diagnosis of schizophrenia should be abandoned.
In 2004 in Japan, the category of schizophrenia was abandoned and replaced with integration disorder. In 2006, campaigners in the UK, under the banner of Campaign for Abolition of the Schizophrenia Label, argued for a similar rejection of the diagnosis of schizophrenia and a different approach to the treatment and understanding of the symptoms currently associated with it.
Alternatively, other proponents have argued for a new approach that would use the presence of specific neurocognitive deficits to make a diagnosis. These often accompany schizophrenia and take the form of a reduction or impairment in basic psychological functions such as memory, attention, executive function and problem solving. It is these sorts of difficulties, rather than the psychotic symptoms (which can in many cases be controlled by antipsychotic medication), which seem to be the cause of most disability in schizophrenia. However, this argument is relatively new and it is unlikely that the method of diagnosing schizophrenia will change radically in the near future.
The diagnostic approach to schizophrenia has also been opposed by the proponents of the anti-psychiatry movement, who argue that classifying specific thoughts and behaviors as an illness allows social control of people that society finds undesirable but who have committed no crime. They argue that this is a way of unjustly classifying a social problem as a medical one to allow the forcible detention and treatment of people displaying these behaviors, which is something which can be done under mental health legislation in most Western countries.
An example of this can be seen in the Soviet Union, where an additional sub-classification of sluggishly progressing schizophrenia was created. Particularly in the RSFSR (Russian Soviet Federated Socialist Republic), this diagnosis was used for the purpose of silencing political dissidents or forcing them to recant their ideas by the use of forcible confinement and treatment. In 2000 similar concerns about the abuse of psychiatry to unjustly silence and detain practitioners of the Falun Gong movement by the Chinese government led the American Psychiatric Association's Committee on the Abuse of Psychiatry and Psychiatrists to pass a resolution to urge the World Psychiatric Association to investigate the situation in China.
Western psychiatric medicine tends to favor a definition of symptoms that depends on form rather than content (an innovation first argued for by psychiatrists Karl Jaspers and Kurt Schneider). Therefore, a subject should be able to believe anything, however unusual or socially unacceptable, without being diagnosed delusional, unless their belief is held in a particular way. In principle, this would stop people being forcibly detained or treated simply for what they believe. However, the distinction between form and content is not easy, or always possible, to make in practice (see delusion). This had led to accusations by anti-psychiatry, surrealist and mental health system survivor groups that psychiatric abuses exist in the West as well.
Causes
Genetic and environmental influences
While the reliability of the schizophrenia diagnosis introduces difficulties in measuring the relative effect of genes and environment (for example, symptoms overlap to some extent with severe bipolar disorder or major depression), evidence suggests that genetic vulnerability and environmental stressors can act in combination to result in diagnosis of schizophrenia.
The extent to which these factors influence the likelihood of being diagnosed with schizophrenia is debated widely, and currently, controversial. Schizophrenia is likely to be a diagnosis of complex inheritance (analogous to diabetes or high blood pressure). Thus, it is likely that several genes interact to generate risk for it. This, combined with disagreements over which research methods are best, or how data from genetic research should be interpreted, has led to differing estimates over genetic contribution.
Genetic
Substantial evidence suggests that the diagnosis of schizophrenia has a heritable component (some estimates are as high as 80%). Current research suggests that environmental factors play a significant role in the expression of any genetic disposition towards schizophrenia (i.e. if someone has the genes that increase risk, this will not automatically result in a diagnosis of schizophrenia later in life). A recent review of the genetic evidence has suggested a more than 28% chance of one identical twin obtaining the diagnosis if the other already has it (see twin studies), but such studies are not noted for pondering the likelihood of similarities of social class and/or other socio-psychological factors between the twins. The estimates of heritability of schizophrenia from twin studies varies a great deal, with some notable studies showing rates as low as 11.0%–13.8% among monozygotic twins, and 1.8%–4.1% among dizygotic twins. However, Jay Joseph and a vocal lobby of psychiatrists and scientists who are at present in the minority have taken to task the twin studies, and have argued that the genetic basis of schizophrenia is open to question.
There is currently a great deal of effort being put into molecular genetic studies of schizophrenia, which attempt to identify specific genes which may increase risk. Because of this, the genes that are thought to be most involved can change as new evidence is gathered. A 2003 review of linkage studies listed seven genes as likely to increase risk for a later diagnosis of the disorder. Two more recent reviews have suggested that the evidence is currently strongest for two genes known as dysbindin (DTNBP1) and neuregulin (NRG1), with a number of other genes (such as COMT, RGS4, PPP3CC, ZDHHC8, DISC1, and AKT1) showing some early promising results that have not yet been fully replicated.
Environmental
Considerable evidence indicates that stressful life events cause or trigger schizophrenia. Childhood experiences of abuse or trauma have also been implicated as risk factors for a diagnosis of schizophrenia later in life.
Evidence is also consistent that negative attitudes towards individuals with (or with a risk of developing) schizophrenia can have a significant adverse impact. In particular, critical comments, hostility, authoritarian and intrusive or controlling attitudes (termed 'high expressed emotion' by researchers) from family members have been found to correlate with a higher risk of relapse in schizophrenia across cultures. It is not clear whether such attitudes play a causal role in the onset of schizophrenia, although those diagnosed in this way may claim it to be the primary causal factor. The research has focused on family members but also appears to relate to professional staff in regular contact with clients. While initial work addressed those diagnosed as schizophrenic, these attitudes have also been found to play a significant role in other mental health problems. This approach does not blame 'bad parenting' or staffing, but addresses the attitudes, behaviors and interactions of all parties. Some go as far as to criticise the whole approach of seeking to localise 'mental illness' within one individual - the patient - rather than his/her group and its functionality, citing a scapegoat effect.
Factors such as poverty and discrimination also appear to be involved in increasing the risk of schizophrenia or schizophrenia relapse, perhaps due to the high levels of stress they engender, or faults in diagnostic procedure/assumptions. Racism in society, including in diagnostic practices, and/or the stress of living in a different culture, may explain why minority communities have shown higher rates of schizophrenia than members of the same ethnic groups resident in their home country. The "social drift hypothesis" suggests that the functional problems related to schizophrenia, or the stigma and prejudice attached to them, can result in more limited employment and financial opportunities, so that the causal pathway goes from mental health problems to poverty, rather than, or in addition to, the other direction. Some argue that unemployment and the long-term unemployed and homeless are simply being stigmatised.
One particularly stable and replicable finding has been the association between living in an urban environment and schizophrenia diagnosis, even after factors such as drug use, ethnic group and size of social group have been controlled for. A recent study of 4.4 million men and women in Sweden found an alleged 68%–77% increased risk of diagnosed psychosis for people living in the most urbanized environments, a significant proportion of which is likely to be described as schizophrenia.
One curious finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring (at least in the northern hemisphere). However, the effect is not large. Some researchers postulate that the correlation is due to viral infections during the third trimester (4-6 months) of pregnancy.
A study by Sweden's Karolinska Institute and Bristol University in the UK, looked at the medical records of over 700,000 people and calculated that 15.5% of cases of schizophrenia seen in the group may have been due to the patient having a father who was aged over 30 years at their birth, the researchers argue this is due to build up of mutations in the sperm of elder fathers.
Neurobiological influences
Early neurodevelopment
It is also thought that processes in early neurodevelopment are important, particularly during pregnancy. For example, women who were pregnant during the Dutch famine of 1944, where many people were close to starvation, had a higher chance of having a child who would later develop schizophrenia. Similarly, studies of Finnish mothers who were pregnant when they found out that their husbands had been killed during the Winter War of 1939–1940 have shown that their children were much more likely to develop schizophrenia when compared with mothers who found out about their husbands' death after pregnancy, suggesting that even psychological trauma in the mother may have an effect. Furthermore, there is now significant evidence that prenatal exposure to infections increases the risk for developing schizophrenia later in life, providing additional evidence for a link between developmental pathology and risk of developing the condition.
Some researchers have proposed that environmental influences during childhood also interact with neurobiological risk factors to influence the likelihood of developing schizophrenia later in life. The neurological development of children is considered sensitive to features of dysfunctional social settings, such as trauma, violence, lack of warmth in personal relationships and hostility. These have all been found to be risk factors for the later development of schizophrenia. Research has suggested that effects of the childhood environment, favorable or unfavorable, interact with genetics and the processes of neurodevelopment, with long-term consequences for brain function. Consequently, this is thought to influence the underlying vulnerability for psychosis later in life, particularly during the adult years.
Role of dopamine
In adult life, particular importance has been placed upon the function (or malfunction) of dopamine in the mesolimbic pathway in the brain. This theory, known as the dopamine hypothesis of schizophrenia, largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, reduced psychotic symptoms. These drugs have now been developed further and antipsychotic medication is commonly used as a first line treatment.
However, this theory is now thought to be overly simplistic as a complete explanation, partly because newer antipsychotic medication (called atypical antipsychotic medication) is equally effective as older medication (called typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect. Psychiatrist David Healy has also argued that pharmaceutical companies have promoted certain oversimplified biological theories of mental illness to promote their own sales of biological treatments.
Role of glutamate and the NMDA receptor
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in the development of schizophrenia. This theory has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition. The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested the glutamate hypothesis of schizophrenia as an increasingly popular explanation. Further support of this theory has come from trials showing the efficacy of molecules, which are coagonists at the NMDA receptor complex, in reducing schizophrenic symptoms. The precursors D-serine, glycine, and D-cycloserine all enhance NMDA function through the glycine co-agonist site. Several placebo controlled trials have shown a reduction mainly in negative symptoms with high dose therapy. Currently type 1 glycine transporter inhibitors are in late-state preclinical for the treatment of schizophrenia. They increase glycine concentrations in the brain thus causing increased NMDA receptor activation and a reduction in symptoms.
Anatomy and physiology of the brain
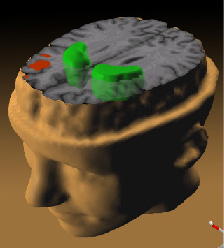
Much recent research has focused on differences in structure or function in certain brain areas in people diagnosed with schizophrenia.
Early evidence for differences in the neural structure came from the discovery of ventricular enlargement in people diagnosed with schizophrenia, for whom negative symptoms were most prominent. However, this finding has not proved particularly reliable on the level of the individual person, with considerable variation between patients. A letter to the editor of the American Journal of Psychiatry links ventricular enlargement with exposure to antipsychotic drugs.
More recent studies have shown a large number of differences in brain structure between people with and without diagnoses of schizophrenia. However, as with earlier studies, many of these differences are only reliably detected when comparing groups of people, and are unlikely to predict any differences in brain structure of an individual person with schizophrenia.
Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus, and temporal lobes. These differences are heavily linked to the neurocognitive deficits which often occur with schizophrenia, particularly in areas of memory, attention, problem solving, executive function and social cognition.
Electroencephalograph (EEG) recordings of persons with schizophrenia performing perception oriented tasks showed an absence of gamma band activity in the brain, indicating weak integration of critical neural networks in the brain. Those who experienced intense hallucinations, delusions and disorganized thinking showed the lowest frequency synchronization. None of the drugs taken by the persons scanned had moved neural synchrony back into the gamma frequency range. Gamma band and working memory alterations may be related to alterations in interneurons that produced the neurotransmitter GABA. Alterations in a subclass of GABAergic interneurons which produce the calcium-binding protein parvalbumin have been shown to exist in the dorsolateral prefrontal cortex in schizophrenia.
Incidence and prevalence
In the western world, schizophrenia is typically diagnosed in late adolescence or early adulthood. In the western world, it is found approximately equally in men and women, though the onset tends to be later in women, who also tend to have a better course and outcome. Although rare, there are also instances of childhood onset schizophrenia and late-onset schizophrenia that occurs in the elderly.
The lifetime prevalence of schizophrenia is commonly given at 1%; however, a recent review of studies from around the world estimated it to be 0.55%. The same study also found that prevalence may vary greatly from country to country, despite the received wisdom that schizophrenia occurs at the same rate throughout the world. It is worth noting however, that this may be in part due to differences in the way schizophrenia is diagnosed. The incidence of schizophrenia was given as a range of between 7.5 and 16.3 cases per year per 100,000 population.
Schizophrenia is also a major cause of disability. In a recent 14-country study, active psychosis was ranked the third most disabling condition after quadriplegia and dementia and before paraplegia and blindness.
Treatment
Medication and hospitalization
Currently schizophrenia has not been cured although many psychiatrists and psychologists believe that it can be managed. The first line pharmacological therapy for schizophrenia is usually the use of antipsychotic medication . The concept of 'curing' schizophrenia is controversial as there are no clear criteria for what might constitute a cure, although some criteria for the remission of symptoms have recently been suggested. Therefore, antipsychotic drugs are only thought to provide symptomatic relief from the positive symptoms of psychosis. The newer atypical antipsychotic medications (such as clozapine, risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and amisulpride) are usually preferred over older typical antipsychotic medications (such as chlorpromazine and haloperidol) due to their favorable side-effect profile. Compared to the typical antipsychotics, the atypicals are associated with a lower incident rate of extrapyramidal side effects (EPS) and tardive dyskinesia (TD) although they are more likely to induce weight gain and so increase risk for obesity-related diseases. It is still unclear whether newer drugs reduce the chances of developing the rare but potentially life-threatening neuroleptic malignant syndrome (NMS). While the atypical antipsychotics are associated with less EPS and TD than the conventional antipsychotics, some of the agents in this class (especially olanzapine and clozapine) appear to be associated with metabolic side effects such as weight gain, hyperglycemia and hypertriglyceridemia that must be considered when choosing appropriate pharmacotherapy.
Atypical and typical antipsychotics are generally thought to be equivalent for the treatment of the positive symptoms of schizophrenia. It has been suggested by some researchers that the atypicals have some beneficial effects on negative symptoms and cognitive deficits associated with schizophrenia, although the clinical significance of these effects has yet to be established. However, recent reviews have suggested that typical antipsychotics, when dosed conservatively, may have similar effects to atypicals. The atypical antipsychotics are much more costly as they are still within patent, whereas the older drugs are available in inexpensive generic forms. Aripiprazole is a drug from a new class of antipsychotic drugs (variously named 'dopamine system stabilizers' or 'partial dopamine agonists'<ref name="fn_37">[http://www.ncbi.nlm.nih.gov:80/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12860772&dopt=
- Evans, K., McGrath, J., & Milns, R. (2003) Searching for schizophrenia in ancient Greek and Roman literature: a systematic review. Acta Psychiatrica Scandanavica, 107(5), 323–330.
- ^ Kraepelin, E. (1907) Text book of psychiatry (7th ed) (trans. A.R. Diefendorf). London: Macmillan.
- "Conditions in Occupational Therapy: effect on occupational performance." ed. Ruth A. Hansen and Ben Atchison (Baltimore: Lippincott Williams & Williams, 2000), 54–74. ISBN 0-683-30417-8
- Stotz-Ingenlath G. (2000) Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911. Medicine, Health Care, and Philosophy, 3(2), 153-9.
- Turner, T. (1999) 'Schizophrenia'. In G.E. Berrios and R. Porter (eds) A History of Clinical Psychiatry. London: Athlone Press. ISBN 0-485-24211-7
- Allen GE. (1997) The social and economic origins of genetic determinism: a case history of the American Eugenics Movement, 1900-1940 and its lessons for today. Genetica, 99, 77-88.
- Read, J., Masson, J. (2004) Genetics, eugenics and mass murder. In J. Read, L.R. Mosher, R.P. Bentall (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Bertelsen, A. (2002) Schizophrenia and Related Disorders: Experience with Current Diagnostic Systems. Psychopathology, 35, 89–93.
- Verdoux, H., & van Os, J. (2002) Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research, 54(1–2), 59–65.
- Johns LC, van Os J. (2001) The continuity of psychotic experiences in the general population. Clinical Psychology Review, 21 (8),1125-41.
- E.R. Peters, S. Day, J. McKenna, G. Orbach (2005) Measuring delusional ideation: the 21-item Peters et al. Delusions Inventory (PDI). Schizophrenia Bulletin, 30, 1005-22.
- Tsuang, M. T., Stone, W. S., & Faraone, S. V. (2000) Toward reformulating the diagnosis of schizophrenia. American Journal of Psychiatry, 157(7), 1041–1050.
- McGorry PD, Mihalopoulos C, Henry L, Dakis J, Jackson HJ, Flaum M, Harrigan S, McKenzie D, Kulkarni J, Karoly R. (1995) Spurious precision: procedural validity of diagnostic assessment in psychotic disorders. American Journal of Psychiatry, 152 (2), 220–3.
- Read, J. (2004) Does 'schizophrenia' exist? Reliability and validity. In J. Read, L.R. Mosher, R.P. Bentall (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Sato, M. (2004) Renaming schizophrenia: a Japanese perspective. World Psychiatry, 5(1), 53-5.
- BBC News Online, (9 October 2006) Schizophrenia term use 'invalid'
- ^ Harrison PJ, Owen MJ. (2003) Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet, 361(9355), 417–9.
- ^ Owen MJ, Craddock N, O'Donovan MC. (2005) Schizophrenia: genes at last? Trends in Genetics, 21(9), 518-25.
- Torrey, E.F., Bowler, A.E., Taylor, E.H. & Gottesman, I.I (1994) Schizophrenia and manic depressive disorder. New York: Basic books. ISBN 0-465-07285-2
- Koskenvuo M, Langinvainio H, Kaprio J, Lonnqvist J, Tienari P (1984) Psychiatric hospitalization in twins. Acta Genet Med Gemellol (Roma), 33(2),321-32.
- Hoeffer A, Pollin W. (1970) Schizophrenia in the NAS-NRC panel of 15,909 veteran twin pairs. Archives of General Psychiatry, 1970 Nov; 23(5):469-77.
- ^ Riley B, Kendler KS (2006) Molecular genetic studies of schizophrenia. Eur J Hum Genet, 14 (6), 669-80.
- Day R, Nielsen JA, Korten A, Ernberg G, Dube KC, Gebhart J, Jablensky A, Leon C, Marsella A, Olatawura M et al (1987). Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization. Culture, Medicine and Psychiatry, 11 (2), 123–205
- Harriet L. MacMillan, Jan E. Fleming, David L. Streiner, Elizabeth Lin, Michael H. Boyle, Ellen Jamieson, Eric K. Duku, Christine A. Walsh, Maria Y.-Y. Wong, William R. Beardslee. (2001) Childhood Abuse and Lifetime Psychopathology in a Community Sample. American Journal of Psychiatry,158, 1878-83.
- Schenkel, L.S., Spaulding, W.D., Dilillo, D., Silverstein, S.M. (2005) Histories of childhood maltreatment in schizophrenia: Relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophrenia Research
- Janssen I., Krabbendam L., Bak M., Hanssen M., Vollebergh W., De Graaf R., Van Os, J. (2004) Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica, 109, 38-45.
- Bebbington P E, Kuipers E (1994) The predictive utility of expressed emotion in schizophrenia: an aggregate analysis. Psychological Medicine, 24, 707-718.
- Van Humbeeck G, Van Audenhove C. (2003) Expressed emotion of professionals towards mental health patients. Epidemiologia e Psychiatria Sociale, 12(4), 232-235. (full text)
- Wearden AJ, Tarrier N, Barrowclough C, Zastowny TR, Rahill AA. (2000) A review of expressed emotion research in health care. Clinical Psychology Review, 20, 633-66.
- Van Os J. (2004) Does the urban environment cause psychosis? British Journal of Psychiatry, 184 (4), 287–288.
- Sundquist K, Frank G, Sundquist J. (2004) Urbanisation and incidence of psychosis and depression: Follow-up study of 4.4 million women and men in Sweden. British Journal of Psychiatry, 184 (4), 293–298.
- Davies G, Welham J, Chant D, Torrey EF, McGrath J. (2003) A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophrenia Bulletin, 29 (3), 587–93.
- Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM (1996) Schizophrenia after prenatal famine. Further evidence. Archives of General Psychiatry, 53(1), 25–31.
- Huttunen MO, Niskanen P. (1978) Prenatal loss of father and psychiatric disorders. Archives of General Psychiatry, 35(4), 429–31.
- Brown, A.S. (2006) Prenatal infection as a risk factor for schizophrenia. Schizophrenia Bulletin, 32 (2), 200-2.
- Read J, Perry BD, Moskowitz A, Connolly J (2001) The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry, 64, 319-45. (full text)
- Meyer-Lindenberg A, Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, Weinberger DR, Berman KF (2002) Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nature Neuroscience, 5, 267-71.
- Healy, D. (2002) The Creation of Psychopharmacology. Cambridge, MA: Harvard University Press. ISBN 0-674-00619-4
- Konradi C, Heckers S. (2003) Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics, 97(2), 153-79.
- Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA. (2001) Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology, 25(4), 455-67.
- Coyle JT, Tsai G, Goff D. (2003) Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences, 1003, 318-27.
- Tuominen HJ, Tiihonen J, Wahlbeck K. (2005) Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res, 72:225-34.
- Kinney GG, Sur C, Burno M, Mallorga PJ, Williams JB, Figueroa DJ, Wittmann M, Lemaire W, Conn PJ. (2003) The Glycine Transporter Type 1 Inhibitor. The Journal of Neuroscience, 23 (20), 7586-7591.
- Johnstone EC, Crow TJ, Frith CD, Husband J, Kreel L. (1976) Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet, 30;2 (7992), 924-6.
- http://ajp.psychiatryonline.org/cgi/content/full/156/11/1843-b
- Flashman LA, Green MF (2004) Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment. Psychiatric Clinics of North America, 27 (1), 1-18, vii.
- Green, M.F. (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- Spencer KM, Nestor PG, Perlmutter R, Niznikiewicz MA, Klump MC, Frumin M, Shenton ME, McCarley (2004) Neural synchrony indexes disordered perception and cognition in schizophrenia. Proceedings of the National Academy of Sciences, 101, 17288-93. (full text)
- Lewis DA, Hashimoto T, Volk DW (2005) Cortical inhibitory neurons and schizophrenia. Nature Reviews Neuroscience, 6, 312-324.
- Goldner EM, Hsu L, Waraich P, Somers JM (2002) Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature. Canadian Journal of Psychiatry, 47(9), 833–43.
- Ustun TB, Rehm J, Chatterji S, Saxena S, Trotter R, Room R, Bickenbach J, and the WHO/NIH Joint Project CAR Study Group (1999). Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. Lancet, 354(9173), 111–115.
- The Royal College of Psychiatrists & The British Psychological Society (2003) Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care. London: Gaskell and the British Psychological Society.
- van Os J, Burns T, Cavallaro R, Leucht S, Peuskens J, Helldin L, Bernardo M, Arango C, Fleischhacker W, Lachaux B, Kane JM. (2006) Standardized remission criteria in schizophrenia. Acta Psychiatrica Scandinavica, 113(2), 91-5.
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. (2005) Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. The New England Journal of Medicine, 353 (12), 1209-23.
- Leucht S, Wahlbeck K, Hamann J, Kissling W. (2003) New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet, 361(9369), 1581-9.