This is an old revision of this page, as edited by Michael Devore (talk | contribs) at 01:17, 11 February 2008 (typo in ref title, checked at source). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 01:17, 11 February 2008 by Michael Devore (talk | contribs) (typo in ref title, checked at source)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) For other uses, see Schizophrenia (disambiguation).Medical condition
| Schizophrenia | |
|---|---|
| Specialty | Psychiatry, clinical psychology |
Schizophrenia, from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind"), is a psychiatric diagnosis that describes a mental illness characterized by impairments in the perception or expression of reality, most commonly manifesting as auditory hallucinations, paranoid or bizarre delusions or disorganized speech and thinking in the context of significant social or occupational dysfunction. Onset of symptoms typically occurs in young adulthood, with approximately 0.4–0.6% of the population affected. Diagnosis is based on the patient's self-reported experiences and observed behavior. No laboratory test for schizophrenia exists.
Studies suggest that genetics, early environment, neurobiology and psychological and social processes are important contributory factors. Current psychiatric research is focused on the role of neurobiology, but a clear organic cause has not been found. Due to the many possible combinations of symptoms, there is debate about whether the diagnosis represents a single disorder or a number of discrete syndromes. For this reason, Eugen Bleuler termed the disease the schizophrenias (plural) when he coined the name. Despite its etymology, schizophrenia is not synonymous with dissociative identity disorder, previously known as multiple personality disorder or split personality; in popular culture the two are often confused.
Increased dopaminergic activity in the mesolimbic pathway of the brain is a consistent finding. The mainstay of treatment is pharmacotherapy with antipsychotic medications; these primarily work by suppressing dopamine activity. Dosages of antipsychotics are generally lower than in the early decades of their use. Psychotherapy, vocational and social rehabilitation are also important. In more serious cases—where there is risk to self and others—involuntary hospitalization may be necessary, though hospital stays are less frequent and for shorter periods than they were in previous years.
The disorder is primarily thought to affect cognition, but it also usually contributes to chronic problems with behavior and emotion. People diagnosed with schizophrenia are likely to be diagnosed with comorbid conditions, including clinical depression and anxiety disorders; the lifetime prevalence of substance abuse is typically around 40%. Social problems, such as long-term unemployment, poverty and homelessness, are common and life expectancy is decreased; the average life expectancy of people with the disorder is 10 to 12 years less than those without, owing to increased physical health problems and a high suicide rate.
Signs and symptoms
A person experiencing schizophrenia may demonstrate symptoms such as disorganized thinking, auditory hallucinations, and delusions. In severe cases, the person may be largely mute, remain motionless in bizarre postures, or exhibit purposeless agitation; these are signs of catatonia. The current classification of psychoses holds that symptoms need to have been present for at least one month in a period of at least six months of disturbed functioning. A schizophrenia-like psychosis of shorter duration is termed a schizophreniform disorder. No one sign is diagnostic of schizophrenia, and all can occur in other medical and psychiatric conditions.
Social isolation commonly occurs and may be due to a number of factors. Impairment in social cognition is associated with schizophrenia, as are the active symptoms of paranoia from delusions and hallucinations, and the negative symptoms of apathy and avolition. Many people diagnosed with schizophrenia avoid potentially stressful social situations that may exacerbate mental distress.
Late adolescence and early adulthood are peak years for the onset of schizophrenia. These are critical periods in a young adult's social and vocational development, and they can be severely disrupted by disease onset. To minimize the effect of schizophrenia, much work has recently been done to identify and treat the prodromal (pre-onset) phase of the illness, which has been detected up to 30 months before the onset of symptoms, but may be present longer. Those who go on to develop schizophrenia may experience the non-specific symptoms of social withdrawal, irritability and dysphoria in the prodromal period, and transient or self-limiting psychotic symptoms in the prodromal phase before psychosis becomes apparent.
Schneiderian classification
The psychiatrist Kurt Schneider (1887–1967) listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider's first-rank symptoms, and they include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices. The reliability of first-rank symptoms has been questioned, although they have contributed to the current diagnostic criteria.
Positive and negative symptoms
Schizophrenia is often described in terms of positive (or productive) and negative (or deficit) symptoms. Positive symptoms include delusions, auditory hallucinations, and thought disorder, and are typically regarded as manifestations of psychosis. Negative symptoms are so-named because they are considered to be the loss or absence of normal traits or abilities, and include features such as flat or blunted affect and emotion, poverty of speech (alogia), anhedonia, and lack of motivation (avolition). Despite the appearance of blunted affect, recent studies indicate that there is often a normal or even heightened level of emotionality in Schizophrenia especially in response to stressful or negative events. A third symptom grouping, the disorganization syndrome, is commonly described, and includes chaotic speech, thought, and behaviour. There is evidence for a number of other symptom classifications.
Diagnosis
Diagnosis is based on the self-reported experiences of the person as well as abnormalities in behavior reported by family members, friends or co-workers, followed by secondary signs observed by a psychiatrist, social worker, clinical psychologist or other clinician in a clinical assessment. There is a list of criteria that must be met for someone to be so diagnosed. These depend on both the presence and duration of certain signs and symptoms.
An initial assessment includes a comprehensive history and physical examination by a physician. Although there are no biological tests which confirm schizophrenia, tests are carried out to exclude medical illnesses which may rarely present with psychotic schizophrenia-like symptoms. These include blood tests measuring TSH to exclude hypo- or hyperthyroidism, basic electrolytes and serum calcium to rule out a metabolic disturbance, full blood count including ESR to rule out a systemic infection or chronic disease, and serology to exclude syphilis or HIV infection; two commonly ordered investigations are EEG to exclude epilepsy, and a CT scan of the head to exclude brain lesions. It is important to rule out a delirium which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness and indicates an underlying medical illness. There are several psychiatric illnesses which may present with psychotic symptoms other than schizophrenia. These include bipolar disorder, borderline personality disorder, drug intoxication, brief drug-induced psychosis, and schizophreniform disorder.
Investigations are not generally repeated for relapse unless there is a specific medical indication. These may include serum blood sugar level (BSL) if olanzapine has been prescribed previously, liver function tests if chlorpromazine, or creatine phosphokinase (CPK) to exclude neuroleptic malignant syndrome. Assessment and treatment are usually done on an outpatient basis; admission to an inpatient facility is considered if there is a risk to self or others.
The most widely used criteria for diagnosing schizophrenia are from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, the current version being DSM-IV-TR, and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems, currently the ICD-10. The latter criteria are typically used in European countries while the DSM criteria are used in the USA or the rest of the world, as well as prevailing in research studies. The ICD-10 criteria put more emphasis on Schneiderian first rank symptoms although, in practice, agreement between the two systems is high. The WHO has developed the tool SCAN (Schedules for Clinical Assessment in Neuropsychiatry) which can be used for diagnosing a number of psychiatric conditions, including schizophrenia.
DSM IV-TR Criteria
To be diagnosed with schizophrenia, a person must display:
- Characteristic symptoms: Two or more of the following, each present for a significant portion of time during a one-month period (or less, if successfully treated)
- delusions
- hallucinations
- disorganized speech (e.g., frequent derailment or incoherence; speaking in abstracts). See thought disorder.
- grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- negative symptoms, i.e., affective flattening (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation).
- Note: Only one of these symptoms is required if delusions are bizarre or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other.
- Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if successfully treated).
Additional criteria are also given that exclude the diagnosis; thus schizophrenia cannot be diagnosed if symptoms of mood disorder or pervasive developmental disorder are present, or the symptoms are the direct result of a substance (e.g., abuse of a drug/medication) or a general medical condition.
Subtypes
Historically, schizophrenia in the West was classified into simple, catatonic, hebephrenic (now known as disorganized), and paranoid. The DSM contains five sub-classifications of schizophrenia:
- paranoid type: where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent (DSM code 295.3/ICD code F20.0)
- disorganized type: named 'hebephrenic schizophrenia' in the ICD. Where thought disorder and flat affect are present together (DSM code 295.1/ICD code F20.1)
- catatonic type: prominent psychomotor disturbances are evident. Symptoms can include catatonic stupor and waxy flexibility (DSM code 295.2/ICD code F20.2)
- undifferentiated type: psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met (DSM code 295.9/ICD code F20.3)
- residual type: where positive symptoms are present at a low intensity only (DSM code 295.6/ICD code F20.5)
The ICD-10 recognises a further two subtypes:
- post-schizophrenic depression: a depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present (ICD code F20.4)
- simple schizophrenia: insidious but progressive development of prominent negative symptoms with no history of psychotic episodes (ICD code F20.6)
Diagnostic issues and controversies
Schizophrenia as a diagnostic entity has been criticised as lacking in scientific validity or reliability, part of a larger criticism of the validity of psychiatric diagnoses in general. One alternative suggests that the issues with the diagnosis would be better addressed as individual dimensions along which everyone varies, such that there is a spectrum or continuum rather than a cut-off between normal and ill. This approach appears consistent with research on schizotypy and of a relatively high prevalence of psychotic experiences and often non-distressing delusional beliefs amongst the general public.
Another criticism is that the definitions used for criteria lack consistency; this is particularly relevant to the evaluation of delusions and thought disorder. More recently, it has been argued that psychotic symptoms are not a good basis for making a diagnosis of schizophrenia as "psychosis is the 'fever' of mental illness — a serious but nonspecific indicator".
Perhaps because of these factors, studies examining the diagnosis of schizophrenia have typically shown relatively low or inconsistent levels of diagnostic reliability. Most famously, David Rosenhan's 1972 study, published as On being sane in insane places, demonstrated that the diagnosis of schizophrenia was (at least at the time) often subjective and unreliable. More recent studies have found agreement between any two psychiatrists when diagnosing schizophrenia tends to reach about 65% at best. This, and the results of earlier studies of diagnostic reliability (which typically reported even lower levels of agreement) have led some critics to argue that the diagnosis of schizophrenia should be abandoned.
In 2004 in Japan, the Japanese term for schizophrenia was changed from Seishin-Bunretsu-Byo (mind-split-disease) to Tōgō-shitchō-shō (integration disorder). In 2006, campaigners in the UK, under the banner of Campaign for Abolition of the Schizophrenia Label, argued for a similar rejection of the diagnosis of schizophrenia and a different approach to the treatment and understanding of the symptoms currently associated with it.
Alternatively, other proponents have put forward using the presence of specific neurocognitive deficits to make a diagnosis. These take the form of a reduction or impairment in basic psychological functions such as memory, attention, executive function and problem solving. It is these sorts of difficulties, rather than the psychotic symptoms (which can in many cases be controlled by antipsychotic medication), which seem to be the cause of most disability in schizophrenia. However, this argument is relatively new and it is unlikely that the method of diagnosing schizophrenia will change radically in the near future.
The diagnosis of schizophrenia has been used for political rather than therapeutic purposes; in the Soviet Union an additional sub-classification of sluggishly progressing schizophrenia was created. Particularly in the RSFSR (Russian Soviet Federated Socialist Republic), this diagnosis was used for the purpose of silencing political dissidents or forcing them to recant their ideas by the use of forcible confinement and treatment. In 2000 there were similar concerns regarding detention and 'treatment' of practitioners of the Falun Gong movement by the Chinese government. This led the American Psychiatric Association's Committee on the Abuse of Psychiatry and Psychiatrists to pass a resolution to urge the World Psychiatric Association to investigate the situation in China.
Epidemiology
Schizophrenia occurs equally in males and females although typically appears earlier in men with the peak ages of onset being 20–28 years for males and 26–32 years for females. Much rarer are instances of childhood-onset and late- (middle age) or very-late-onset (old age) schizophrenia. The lifetime prevalence of schizophrenia, that is, the proportion of individuals expected to experience the disease at any time in their lives, is commonly given at 1%. A 2002 systematic review of many studies, however, found a lifetime prevalence of 0.55%. Despite the received wisdom that schizophrenia occurs at similar rates throughout the world, its prevalence varies across the world, within countries, and at the local and neighbourhood level. One particularly stable and replicable finding has been the association between living in an urban environment and schizophrenia diagnosis, even after factors such as drug use, ethnic group and size of social group have been controlled for. Schizophrenia is known to be a major cause of disability. In a 1999 study of 14 countries, active psychosis was ranked the third-most-disabling condition, after quadriplegia and dementia and before paraplegia and blindness.
Causes
Main article: Causes of schizophrenia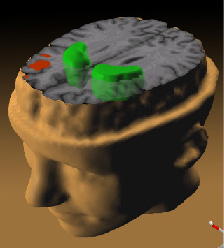
While the reliability of the diagnosis introduces difficulties in measuring the relative effect of genes and environment (for example, symptoms overlap to some extent with severe bipolar disorder or major depression), evidence suggests that genetic and environmental factors can act in combination to result in schizophrenia. Evidence suggests that the diagnosis of schizophrenia has a significant heritable component but that onset is significantly influenced by environmental factors or stressors. The idea of an inherent vulnerability (or diathesis) in some people, which can be unmasked by biological, psychological or environmental stressors, is known as the stress-diathesis model. The idea that biological, psychological and social factors are all important is known as the "biopsychosocial" model.
Genetic
Estimates of the heritability of schizophrenia tend to vary owing to the difficulty of separating the effects of genetics and the environment although twin studies have suggested a high level of heritability. It is likely that schizophrenia is a condition of complex inheritance, with several genes possibly interacting to generate risk for schizophrenia or the separate components that can co-occur leading to a diagnosis. Recent work has suggested that genes that raise the risk for developing schizophrenia are non-specific, and may also raise the risk of developing other psychotic disorders such as bipolar disorder.
Prenatal
It is thought that causal factors can initially come together in early neurodevelopment, including during pregnancy, to increase the risk of later developing schizophrenia. One curious finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring, (at least in the northern hemisphere). There is now evidence that prenatal exposure to infections increases the risk for developing schizophrenia later in life, providing additional evidence for a link between in utero developmental pathology and risk of developing the condition.
Social
Living in an urban environment has been consistently found to be a risk factor for schizophrenia. Social disadvantage has been found to be a risk factor, including poverty and migration related to social adversity, racial discrimination, family dysfunction, unemployment or poor housing conditions. Childhood experiences of abuse or trauma have also been implicated as risk factors for a diagnosis of schizophrenia later in life. Parenting is not held responsible for schizophrenia but unsupportive dysfunctional relationships may contribute to an increased risk.
Substance use
The relationship between schizophrenia and drug use is complex, meaning that a clear causal connection between drug use and schizophrenia has been difficult to tease apart. There is strong evidence that using certain drugs can trigger either the onset or relapse of schizophrenia in some people. It may also be the case, however, that people with schizophrenia use drugs to overcome negative feelings associated with both the commonly prescribed antipsychotic medication and the condition itself, where negative emotion, paranoia and anhedonia are all considered to be core features. Amphetamines trigger the release of dopamine and excessive dopamine function is believed to be responsible for many symptoms of schizophrenia (known as the dopamine hypothesis of schizophrenia), amphetamines may worsen schizophrenia symptoms. Schizophrenia can be triggered by heavy use of hallucinogenic or stimulant drugs. One study suggests that cannabis use can contribute to psychosis, though the researchers suspected cannabis use was only a small component in a broad range of factors that can cause psychosis.
Psychological
A number of psychological mechanisms have been implicated in the development and maintenance of schizophrenia. Cognitive biases that have been identified in those with a diagnosis or those at risk, especially when under stress or in confusing situations, include excessive attention to potential threats, jumping to conclusions, making external attributions, impaired reasoning about social situations and mental states, difficulty distinguishing inner speech from speech from an external source, and difficulties with early visual processing and maintaining concentration. Some cognitive features may reflect global neurocognitive deficits in memory, attention, problem-solving, executive function or social cognition, while others may be related to particular issues and experiences. Despite a common appearance of "blunted affect", recent findings indicate that many individuals diagnosed with schizophrenia are highly emotionally responsive, particularly to stressful or negative stimuli, and that such sensitivity may cause vulnerability to symptoms or to the disorder. Some evidence suggests that the content of delusional beliefs and psychotic experiences can reflect emotional causes of the disorder, and that how a person interprets such experiences can influence symptomology. Further evidence for the role of psychological mechanisms comes from the effects of therapies on symptoms of schizophrenia.
Neural
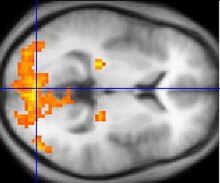
Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus, and temporal lobes. These differences have been linked to the neurocognitive deficits often associated with schizophrenia. The role of antipsychotic medication, which nearly all those studied had taken, in causing such abnormalities is also unclear.
Particular focus has been placed upon the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, could reduce psychotic symptoms. An influential theory, known as the Dopamine hypothesis of schizophrenia, proposed that a malfunction involving dopamine pathways was the cause of (the positive symptoms of) schizophrenia. This theory is now thought to be overly simplistic as a complete explanation, partly because newer antipsychotic medication (called atypical antipsychotic medication) can be equally effective as older medication (called typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect.
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia. This has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition. The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia. Further support of this theory has come from preliminary trials suggesting the efficacy of coagonists at the NMDA receptor complex in reducing some of the positive symptoms of schizophrenia.
There have also been findings of differences in the size and structure of certain brain areas in schizophrenia, starting with the discovery of ventricular enlargement in those for whom negative symptoms were most prominent. However, this has not proven particularly reliable on the level of the individual person, with considerable variation between patients. More recent studies have shown various differences in brain structure between people with and without diagnoses of schizophrenia. However, as with earlier studies, many of these differences are only reliably detected when comparing groups of people, and are unlikely to predict any differences in brain structure of an individual person with schizophrenia.
Treatment and services
Main article: Treatment of schizophrenia
The concept of a cure as such remains controversial, as there is no consensus on the definition, although some criteria for the remission of symptoms have recently been suggested. The effectiveness of schizophrenia treatment is often assessed using standardized methods, one of the most common being the positive and negative syndrome scale (PANSS). Management of symptoms and improving function is thought to be more achievable than a cure. Treatment was revolutionized in the mid 1950s with the development and introduction of chlorpromazine. A recovery model is increasingly adopted, emphasizing hope, empowerment and social inclusion.
Hospitalization may occur with severe episodes of schizophrenia. This can be voluntary or (if mental health legislation allows it) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although can still occur. Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or Assertive Community Treatment team, supported employment and patient-led support groups.
In many non-Western societies, schizophrenia may only be treated with more informal, community-led methods. The outcome for people diagnosed with schizophrenia in non-Western countries may actually be better than for people in the West. The reasons for this effect are not clear, although cross-cultural studies are being conducted.
Medication
The mainstay of psychiatric treatment for schizophrenia is an antipsychotic medication. These can reduce the "positive" symptoms of psychosis. Most antipsychotics take around 7–14 days to have their main effect.

Though expensive, the newer atypical antipsychotic drugs are usually preferred for initial treatment over the older typical antipsychotics; they are often better tolerated and associated with lower rates of tardive dyskinesia, although they are more likely to induce weight gain and obesity-related diseases. Prolactin elevations have been reported in women with schizophrenia taking atypical antipsychotics.It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome, a rare but serious and potentially fatal neurological disorder most often caused by an adverse reaction to neuroleptic or antipsychotic drugs.
The two classes of antipsychotics are generally thought equally effective for the treatment of the positive symptoms. Some researchers have suggested that the atypicals offer additional benefit for the negative symptoms and cognitive deficits associated with schizophrenia, although the clinical significance of these effects has yet to be established. Recent reviews have refuted the claim that atypical antipsychotics have fewer extrapyramidal side effects than typical antipsychotics, especially when the latter are used in low doses or when low potency antipsychotics are chosen.
Response of symptoms to medication is variable; "Treatment-resistant schizophrenia" is a term used for the failure of symptoms to respond satisfactorily to at least two different antipsychotics. Patients in this category may be prescribed clozapine, a medication of superior effectiveness but several potentially lethal side effects including agranulocytosis and myocarditis. Clozapine may have the additional benefit of reducing propensity for substance abuse in schizophrenic patients. For other patients who are unwilling or unable to take medication regularly, long-acting depot preparations of antipsychotics may be given every two weeks to achieve control. America and Australia are two countries with laws allowing the forced administration of this type of medication on those who refuse but are otherwise stable and living in the community. Some findings have found that in the longer-term some individuals may do better not taking antipsychotics. Despite the promising results of early pilot trials, omega-3 fatty acids failed to improve schizophrenic symptoms, according to the most recent meta-analysis.
Psychological and social interventions
Psychotherapy is also widely recommended and used in the treatment of schizophrenia, although services may often be confined to pharmacotherapy because of reimbursement problems or lack of training.
Cognitive behavioral therapy (CBT) is used to reduce symptoms and improve related issues such as self-esteem, social functioning, and insight. Although the results of early trials were inconclusive, more recent reviews suggest that CBT can be an effective treatment for the psychotic symptoms of schizophrenia. Another approach is cognitive remediation therapy, a technique aimed at remediating the neurocognitive deficits sometimes present in schizophrenia. Based on techniques of neuropsychological rehabilitation, early evidence has shown it to be cognitively effective, with some improvements related to measurable changes in brain activation as measured by fMRI. A similar approach known as cognitive enhancement therapy, which focuses on social cognition as well as neurocognition, has shown efficacy.
Family Therapy or Education, which addresses the whole family system of an individual with a diagnosis of schizophrenia, has been consistently found to be beneficial, at least if the duration of intervention is longer-term. Aside from therapy, the impact of schizophrenia on families and the burden on carers has been recognized, with the increasing availability of self-help books on the subject. There is also some evidence for benefits from social skills training, although there have also been significant negative findings. Some studies have explored the possible benefits of music therapy and other creative therapies.
Other
Electroconvulsive therapy is not considered a first line treatment but may be prescribed in cases where other treatments have failed. It is more effective where symptoms of catatonia are present, and is recommended for use under NICE guidelines in the UK for catatonia if previously effective, though there is no recommendation for use for schizophrenia otherwise. Psychosurgery has now become a rare procedure and is not a recommended treatment for schizophrenia.
Service-user led movements have become integral to the recovery process in Europe and America; groups such as the Hearing Voices Network and the Paranoia Network have developed a self-help approach that aims to provide support and assistance outside the traditional medical model adopted by mainstream psychiatry. By avoiding framing personal experience in terms of criteria for mental illness or mental health, they aim to destigmatize the experience and encourage individual responsibility and a positive self-image. Partnerships between hospitals and consumer-run groups are becoming more common, with services working toward remediating social withdrawal, building social skills and reducing rehospitalization.
Prognosis
Numerous international studies have demonstrated favorable long-term outcomes for around half of those diagnosed with schizophrenia, with substantial variation between individuals and regions. One retrospective study found that about a third of people made a full recovery, about a third showed improvement but not a full recovery, and a third remained ill. A clinical study using strict recovery criteria (concurrent remission of positive and negative symptoms and adequate social and vocational functioning continuously for two years) found a recovery rate of 14% within the first five years. A 5-year community study found that 62% showed overall improvement on a composite measure of symptomatic, clinical and functional outcomes. Rates are not always comparable across studies because an exact definition of what constitutes recovery has not been widely accepted, although standardized criteria have been suggested.
The World Health Organization conducted two long-term follow-up studies involving more than 2,000 people suffering from schizophrenia in different countries. These studies found patients have much better long-term outcomes in developing countries (India, Colombia and Nigeria) than in developed countries (USA, UK, Ireland, Denmark, Czech Republic, Slovakia, Japan, and Russia), despite the fact antipsychotic drugs are typically not widely available in poorer countries, raising questions about the effectiveness of such drug-based treatments.
Several factors are associated with a better prognosis: Being female, acute (vs. insidious) onset of symptoms, older age of first episode, predominantly positive (rather than negative) symptoms, presence of mood symptoms and good premorbid functioning. Most studies done on this subject, however, are correlational in nature, and a clear cause-and-effect relationship is difficult to establish. Evidence is also consistent that negative attitudes towards individuals with schizophrenia can have a significant adverse impact. In particular, critical comments, hostility, authoritarian and intrusive or controlling attitudes (termed high 'Expressed emotion' or 'EE' by researchers) from family members have been found to correlate with a higher risk of relapse in schizophrenia across cultures.
Mortality
In a study of over 168,000 Swedish citizens undergoing psychiatric treatment, schizophrenia was associated with an average life expectancy of approximately 80–85% of that of the general population. Women with a diagnosis of schizophrenia were found to have a slightly better life expectancy than that of men, and as a whole, a diagnosis of schizophrenia was associated with a better life expectancy than substance abuse, personality disorder, heart attack and stroke. There is a high suicide rate associated with schizophrenia; a recent study showed that 30% of patients diagnosed with this condition had attempted suicide at least once during their lifetime. Another study suggested that 10% of persons with schizophrenia die by suicide. Other identified factors include smoking, poor diet, little exercise and the negative health effects of psychiatric drugs.
Violence
The relationship between violent acts and schizophrenia is a contentious topic. Current research indicates that the percentage of people with schizophrenia who commit violent acts is higher than the percentage of people without any disorder, but lower than is found for disorders such as alcoholism, and the difference is reduced or not found in same-neighbourhood comparisons when related factors are taken into account, notably sociodemographic variables and substance misuse. Studies have indicated that 5 to 10% of those charged with murder in Western countries have a schizophrenia spectrum disorder.
The occurrence of psychosis in schizophrenia has sometimes been linked to a higher risk of violent acts. Findings on the specific role of delusions or hallucinations have been inconsistent, but have focused on delusional jealousy, perception of threat and command hallucinations. It has been proposed that a certain type of individual with schizophrenia may be most likely to offend, characterized by a history of educational difficulties, low IQ, conduct disorder, early-onset substance misuse and offending prior to diagnosis.
A consistent finding is that individuals with a diagnosis of schizophrenia are often the victims of violent crime—at least 14 times more often than they are perpetrators. Another consistent finding is a link to substance misuse, particularly alcohol, among the minority who commit violent acts. Violence by or against individuals with schizophrenia typically occurs in the context of complex social interactions within a family setting, and is also an issue in clinical services and in the wider community.
Screening and prevention
There are no reliable markers for the later development of schizophrenia although research is being conducted into how well a combination of genetic risk plus non-disabling psychosis-like experience predicts later diagnosis. People who fulfil the 'ultra high-risk mental state' criteria, that include a family history of schizophrenia plus the presence of transient or self-limiting psychotic experiences, have a 20–40% chance of being diagnosed with the condition after one year. The use of psychological treatments and medication has been found effective in reducing the chances of people who fulfill the 'high-risk' criteria from developing full-blown schizophrenia. However, the treatment of people who may never develop schizophrenia is controversial, in light of the side-effects of antipsychotic medication; particularly with respect to the potentially disfiguring tardive dyskinesia and the rare but potentially lethal neuroleptic malignant syndrome. The most widely used form of preventative health care for schizophrenia takes the form of public education campaigns that provide information on risk factors, early detection and treatment options.
Popular views and misconceptions
Stigma has been identified as a major obstacle in the recovery of patients with schizophrenia. 12.8% of a large, representative sample of Americans in a 1999 study believed that individuals with schizophrenia were "very likely" to do something violent against others, and 48.1% said that they were "somewhat likely" to. Over 74% said that people with schizophrenia were either "not very able" or "not able at all" to make decisions concerning their treatment, and 70.2% said the same of money management decisions. The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.
As public understanding of mental illness as a biological disorder is yet developing, patients may be discouraged by friends or family members from taking prescribed medication. Consumers' views on treatment and recovery may differ from those of mental health professionals.
Alternative approaches
An approach broadly known as the anti-psychiatry movement, most active in the 1960s, opposes the orthodox medical view of schizophrenia as an illness. Psychiatrist Thomas Szasz argued that psychiatric patients are not ill, but rather individuals with unconventional thoughts and behavior that make society uncomfortable. He argues that society unjustly seeks to control them by classifying their behavior as an illness and forcibly treating them as a method of social control. According to this view, "schizophrenia" does not actually exist but is merely a form of social construction, created by society's concept of what constitutes normality and abnormality. Szasz has never considered himself to be "anti-psychiatry" in the sense of being against psychiatric treatment, but simply believes that treatment should be conducted between consenting adults, rather than imposed upon anyone against his or her will. Similarly, psychiatrists R. D. Laing, Silvano Arieti, Theodore Lidz and Colin Ross have argued that the symptoms of what is called mental illness are comprehensible reactions to impossible demands that society and particularly family life places on some sensitive individuals. Laing, Arieti, Lidz and Ross were notable in valuing the content of psychotic experience as worthy of interpretation, rather than considering it simply as a secondary but essentially meaningless marker of underlying psychological or neurological distress. Laing described eleven case studies of people diagnosed with schizophrenia and argued that the content of their actions and statements was meaningful and logical in the context of their family and life situations. In 1956, Palo Alto, Gregory Bateson and his colleagues Paul Watzlawick, Donald Jackson, and Jay Haley articulated a theory of schizophrenia, related to Laing's work, as stemming from double bind situations where a person receives different or contradictory messages. Madness was therefore an expression of this distress, and should be valued as a cathartic and trans-formative experience. In the books Schizophrenia and the Family and The Origin and Treatment of Schizophrenic Disorders Lidz and his colleagues explain their belief that parental behaviour can result in mental illness in children. Arieti's Interpretation of Schizophrenia won the 1975 scientific National Book Award in the United States.
The concept of schizophrenia as a result of civilization has been developed further by psychologist Julian Jaynes in his 1976 book The Origin of Consciousness in the Breakdown of the Bicameral Mind; he proposed that until the beginning of historic times, schizophrenia or a similar condition was the normal state of human consciousness. This would take the form of a "bicameral mind" where a normal state of low affect, suitable for routine activities, would be interrupted in moments of crisis by "mysterious voices" giving instructions, which early people characterized as interventions from the gods. Researchers into shamanism have speculated that in some cultures schizophrenia or related conditions may predispose an individual to becoming a shaman; the experience of having access to multiple realities is not uncommon in schizophrenia, and is a core experience in many shamanic traditions. Equally, the shaman may have the skill to bring on and direct some of the altered states of consciousness psychiatrists label as illness. Psychohistorians, on the other hand, accept the psychiatric diagnoses. However, unlike the current medical model of mental disorders they argue that poor parenting in tribal societies causes the shaman's schizoid personalities. Speculation regarding primary and important religious figures as having schizophrenia abound. Commentators such as Paul Kurtz and others have endorsed the idea that major religious figures experienced psychosis, heard voices and displayed delusions of grandeur.
Psychiatrist Tim Crow has argued that schizophrenia may be the evolutionary price we pay for a left brain hemisphere specialization for language. Since psychosis is associated with greater levels of right brain hemisphere activation and a reduction in the usual left brain hemisphere dominance, our language abilities may have evolved at the cost of causing schizophrenia when this system breaks down.
The Soteria model is an alternative treatment to institutionalization and early use of antipsychotics. It is described as a milieu-therapeutic recovery method, characterized by its founder as "the 24 hour a day application of interpersonal phenomenologic interventions by a nonprofessional staff, usually without neuroleptic drug treatment, in the context of a small, homelike, quiet, supportive, protective, and tolerant social environment."
A branch of alternative medicine that deals with schizophrenia is known as orthomolecular psychiatry. Vitamin B-3 (Niacin) has been proposed as an effective treatment. Orthomolecular psychiatry considers the schizophrenias to be a group of disorders; management entails performing the appropriate diagnostic tests and then providing the appropriate therapy. Nobel Laureate Linus Pauling was a strong supporter of orthomolecular psychiatry. The body's adverse reactions to gluten are implicated in some alternative theories, including orthomolecular psychiatry. This theory—discussed by one author in three British journals in the 1970s—is unproven. A 2006 literature review suggests that gluten may be a factor for patients with both schizophrenia and celiac disease, but further study is needed to confirm the association between gluten and schizophrenia.
History
Descriptions of schizophrenia-like symptoms date back to circa 2000 BC in the Book of Hearts—part of the ancient Egyptian Ebers Papyrus. However, study of the ancient Greek and Roman literature shows that although the general population probably had an awareness of psychotic disorders, there was no recorded condition that would meet the modern criteria for schizophrenia. Symptoms resembling schizophrenia were, however, reported in Arabic medical and psychological literature during the Middle Ages. In The Canon of Medicine, for example, Avicenna described a condition somewhat resembling schizophrenia which he called Junun Mufrit (severe madness), which he distinguished from other forms of madness (Junun) such as mania, rabies, and manic depressive psychosis.

Although a broad concept of madness has existed for thousands of years, schizophrenia was only classified as a distinct mental disorder by Emil Kraepelin in 1893. He was the first to make a distinction in the psychotic disorders between what he called dementia praecox (early dementia—a term first used by psychiatrist Bénédict Morel ) and manic depression. Kraepelin believed that dementia praecox was primarily a disease of the brain, and particularly a form of dementia, distinguished from other forms of dementia, such as Alzheimer's disease, which typically occur later in life.
The word schizophrenia—which translates roughly as "splitting of the mind" and comes from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind")—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. Bleuler described the main symptoms as 4 A's: flattened Affect, Autism, impaired Association of ideas and Ambivalence. Bleuler realized that the illness was not a dementia as some of his patients improved rather than deteriorated and hence proposed the term schizophrenia instead.
The term schizophrenia is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion arises in part due to the meaning of Bleuler's term schizophrenia (literally "split" or "shattered mind"). The first known misuse of the term to mean "split personality" was in an article by the poet T. S. Eliot in 1933.
In the first half of the twentieth century schizophrenia was considered to be a hereditary defect, and sufferers were subject to eugenics in many countries. Hundreds of thousands were sterilized, with or without consent—the majority in Nazi Germany, the United States, and Scandinavian countries. Along with other people labeled "mentally unfit", many diagnosed with schizophrenia were murdered in the Nazi "Action T4" program.
The diagnostic description of schizophrenia has changed over time. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe. This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. This was one of the factors in leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III.
Cultural references
The book and film A Beautiful Mind chronicled the life of John Forbes Nash, a Nobel-Prize-winning mathematician who was diagnosed with schizophrenia. The Marathi film Devrai (Featuring Atul Kulkarni) is a presentation of a patient with schizophrenia. The film, set in the Konkan region of Maharashtra in Western India, shows the behavior, mentality, and struggle of the patient as well as his loved-ones. It also portrays the treatment of this mental illness using medication, dedication and plenty of patience by the close relatives of the patient. Other factual books have been written by relatives on family members; Australian journalist Anne Deveson told the story of her son's battle with schizophrenia in Tell me I'm Here, later made into a movie.
In Bulgakov's Master and Margarita the poet Ivan Bezdomnyj is institutionalized and diagnosed with schizophrenia after witnessing the devil (Woland) predict Berlioz's death. The book The Eden Express by Mark Vonnegut accounts his struggle into schizophrenia and his journey back to sanity.
References
- ^ Castle E, Wessely S, Der G, Murray RM (1991). "The incidence of operationally defined schizophrenia in Camberwell 1965–84," British Journal of Psychiatry 159: 790–794. PMID 1790446
- Bhugra, D. (2005). The global prevalence of schizophrenia. PLoS Medicine, 2 (5), 372–373. PMID 15916460
- ^ Goldner EM, Hsu L, Waraich P, Somers JM (2002). Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature. Canadian Journal of Psychiatry, 47(9), 833–43. PMID 12500753
- ^ American Psychiatric Association (2004) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision). American Psychiatric Association. ISBN 0890420246. DSM-IV & DSM-IV-TR Schizophrenia criteria
- ^ Brown S, Inskip H, Barraclough B. (2000) Causes of the excess mortality of schizophrenia. Br J Psychiatry, 177, 212-7. PMID 11040880
- Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE, Dunn G. (2007) Acting on persecutory delusions: the importance of safety seeking. Behaviour Research and Therapy, 45 (1), 89–99. PMID 16530161
- Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, Heinssen R. (2007) North American prodrome longitudinal study: a collaborative multisite approach to prodromal schizophrenia research. Schizophrenia Bulletin, 33 (3), 665-72. PMID 17255119
- Parnas J, Jorgensen A. (1989) Pre-morbid psychopathology in schizophrenia spectrum. British Journal of Psychiatry, 155, 623–7.
- Amminger GP, Leicester S, Yung AR, Phillips LJ, Berger GE, Francey SM, Yuen HP, McGorry PD. (2006) Early-onset of symptoms predicts conversion to non-affective psychosis in ultra-high risk individuals. Schizophrenia Research, 84 (1), 67–76. PMID 16677803
- Schneider, K. (1959) Clinical Psychopathology. New York: Grune and Stratton.
- Bertelsen, A. (2002). Schizophrenia and Related Disorders: Experience with Current Diagnostic Systems. Psychopathology, 35, 89–93. PMID 12145490
- Sims A (2002) Symptoms in the Mind: An Introduction to Descriptive Psychopathology (3rd edition). Edinburgh: Elsevier Science Ltd. ISBN 0-7020-2627-1
- Cohen & Docherty (2004). Affective reactivity of speech and emotional experience in patients with schizophrenia. Schizophr Res, 1;69(1):7–14. PMID 15145465
- Peralta V, Cuesta MJ. (2001) How many and which are the psychopathological dimensions in schizophrenia? Issues influencing their ascertainment. Schizophrenia Research, 30, 49(3), 269-85. PMID 11356588
- Pope HG (1983). Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports. Hospital and Community Psychiatry, 34: 322–328.
- McGlashan TH (1987) Testing DSM-III symptom criteria for schizotypal and borderline personality disorders. Archives of General Psychiatry, 44: 15–22.
- Jakobsen KD, Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T (2005) Reliability of clinical ICD-10 schizophrenia diagnoses. Nordic Journal of Psychiatry, 59 (3), 209-12. PMID 16195122
- Bentall RP (1992) Reconstructing Schizophrenia. London: Routledge. ISBN 0415075246
- Boyle M (2002) Schizophrenia: A Scientific Delusion?. London: Routledge. ISBN 0415227186
- Verdoux H, van Os J (2002). Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research, 54(1–2), 59–65. PMID 11853979
- LC, van Os J. (2001). The continuity of psychotic experiences in the general population. Clinical Psychology Review, 21 (8),1125–41. PMID 11702510
- Peters ER, Day S, McKenna J, Orbach G(2005). Measuring delusional ideation: the 21-item Peters et al. Delusions Inventory (PDI). Schizophrenia Bulletin, 30, 1005–22. PMID 15954204
- Johns LC, van Os J (2001) The continuity of psychotic experiences in the general population. Clinical Psychology Review, 21 (8), 1125–41. PMID 11702510.
- David AS (1999) On the impossibility of defining delusions. Philosophy, Psychiatry and Psychology, 6 (1), 17–20
- Tsuang MT, Stone WS, Faraone SV (2000). Toward reformulating the diagnosis of schizophrenia. American Journal of Psychiatry, 157(7), 1041–1050. PMID 10873908
- Rosenhan D (1973). On being sane in insane places. Science, 179, 250-8. PMID 4683124Full text as PDF
- McGorry PD, Mihalopoulos C, Henry L, Dakis J, Jackson HJ, Flaum M, Harrigan S, McKenzie D, Kulkarni J, Karoly R (1995). Spurious precision: procedural validity of diagnostic assessment in psychotic disorders. American Journal of Psychiatry, 152 (2), 220–3. PMID 7840355
- Read J (2004) Does 'schizophrenia' exist? Reliability and validity. In Read J, Mosher LR, Bentall RP (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Sato M (2004). Renaming schizophrenia: a Japanese perspective. World Psychiatry, 5(1), 53–5. PMID 16757998
- Schizophrenia term use 'invalid'. BBC News Online, (9 October 2006). Retrieved on 2007-05-16.
- Green MF (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0393703347
- Wilkinson G (1986) Political dissent and "sluggish" schizophrenia in the Soviet Union. Br Med J (Clin Res Ed), 293(6548), 641-2. PMID 3092963
- Lyons D (2001). Soviet-style psychiatry is alive and well in the People's Republic. British Journal of Psychiatry, 178, 380–381. PMID 11282823
- Kumra S, Shaw M, Merka P, Nakayama E, Augustin R. (2001) Childhood-onset schizophrenia: research update. Canadian Journal of Psychiatry, 46 (10), 923–30.
- Hassett A, Ames D, Chiu E (eds) (2005) Psychosis in the Elderly. London: Taylor and Francis. ISBN 18418439446
- Jablensky A, Sartorius N, Ernberg G, et al. (1992) Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychological Medicine Monograph Supplement, 20, 1–97. PMID 1565705
- Kirkbride JB, Fearon P, Morgan C, et al. (2006) Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings From the 3-center ÆSOP study. Archives of General Psychiatry, 63, 250–258. PMID 16520429
- Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Murray RM, Jones PB. (2007) Neighbourhood variation in the incidence of psychotic disorders in Southeast London. Social Psychiatry and Psychiatric Epidemiology, 42(6), 438-45. PMID 17473901
- ^ Van Os J. (2004). Does the urban environment cause psychosis? British Journal of Psychiatry, 184 (4), 287–288. PMID 15056569
- Ustun TB, Rehm J, Chatterji S, Saxena S, Trotter R, Room R, Bickenbach J, and the WHO/NIH Joint Project CAR Study Group (1999). Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. The Lancet, 354(9173), 111–115. PMID 10408486
- Meyer-Lindenberg A, Miletich RS, Kohn PD, et al (2002). Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nature Neuroscience, 5, 267–71. PMID 11865311
- Harrison PJ, Owen MJ. (2003). Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet, 361(9355), 417–9. PMID 12573388
- Day R, Nielsen JA, Korten A, Ernberg G, et al (1987). Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization. Culture, Medicine and Psychiatry, 11 (2), 123–205. PMID 3595169
- Corcoran C, Walker E, Huot R, Mittal V, Tessner K, Kestler L, Malaspina D. (2003) The stress cascade and schizophrenia: etiology and onset. Schizophr Bull, 29 (4), 671-92. PMID 14989406
- O'Donovan MC, Williams NM, Owen MJ. (2003) Recent advances in the genetics of schizophrenia. Human Molecular Genetics, 12 Spec No 2, R125-33. PMID 12952866
- Owen MJ, Craddock N, O'Donovan MC. (2005). Schizophrenia: genes at last? Trends in Genetics, 21(9), 518–25. PMID 16009449
- Craddock N, O'Donovan MC, Owen MJ. (2006) Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophrenia Bulletin, 32 (1), 9–16. PMID 16319375
- Dalby JT, Morgan D, Lee M. (1986) Schizophrenia and mania in identical twin brothers.Journal of Nervous and Mental Disease,174,304-308. PMID 3701318
- Davies G, Welham J, Chant D, Torrey EF, McGrath J. (2003). A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophrenia Bulletin, 29 (3), 587–93. PMID 14609251
- Brown AS (2006). Prenatal infection as a risk factor for schizophrenia. Schizophr Bull 32 (2), 200–2. PMID 16469941
- van Os J, Krabbendam L, Myin-Germeys I, Delespaul P (2005) The schizophrenia envirome. Current Opinion in Psychiatry, 18 (2), 141-5. PMID 16639166
- Mueser KT & McGurk SR. (2004) Schizophrenia. Lancet. June 19;363(9426):2063-72. PMID 15207959
- Selten JP, Cantor-Graae E, Kahn RS. (2007) Migration and schizophrenia. Current Opinion in Psychiatry, 20 (2), 111-5. PMID 17278906
- Schenkel LS, Spaulding WD, Dilillo D, Silverstein SM (2005). Histories of childhood maltreatment in schizophrenia: Relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophrenia Research, 76(2–3), 273–286. PMID 15949659
- Janssen I, Krabbendam L, Bak M, Hanssen M, et al (2004). Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica, 109, 38–45. PMID 14674957
- ^ Bentall RP, Fernyhough C, Morrison AP, Lewis S, Corcoran R. (2007) Prospects for a cognitive-developmental account of psychotic experiences. Br J Clin Psychol. Jun;46(Pt 2):155-73. PMID 17524210
- Subotnik, KL, Goldstein, MJ, Nuechterlein, KH, Woo, SM and Mintz, J. (2002) Are Communication Deviance and Expressed Emotion Related to Family History of Psychiatric Disorders in Schizophrenia? Schizophr Bull. 28(4):719-29 PMID 12795501
- Gregg L, Barrowclough C, Haddock G. (2007) Reasons for increased substance use in psychosis. Clinical Psychology Review, 27 (4), 494–510. PMID 17240501
- Laruelle, M., Abi-Dargham, A., Van-Dyck, C. H., et al (1996) Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proceedings of the National Academy of Sciences of the USA, 93, 9235–9240. PMID 8799184 Full text
- Mueser KT, Yarnold PR, Levinson DF, et al (1990). Prevalence of substance abuse in schizophrenia: demographic and clinical correlates. Schizophrenic Bulletin, 16(1), 31–56. PMID 2333480
- Arseneault L, Cannon M, Witton J, Murray RM (2004). Causal association between cannabis and psychosis: examination of the evidence. British Journal of Psychiatry, 184, 110-7. PMID 14754822 Full text
- Broome MR, Woolley JB, Tabraham P, Johns LC, et al (2005). What causes the onset of psychosis? Schizophr Res, 79(1), 23–34. PMID 16198238
- Lewis R (2004). Should cognitive deficit be a diagnostic criterion for schizophrenia? Journal of Psychiatry and Neuroscience March; 29(2): 102–113. PMID 15069464
- Brune M, Abdel-Hamid M, Lehmkamper C, Sonntag C (2007). Mental state attribution, neurocognitive functioning, and psychopathology: What predicts poor social competence in schizophrenia best? Schizophr Res. March 6 PMID 17346931
- Sitskoorn MM, Aleman A, Ebisch SJH, Appels MCM, Khan RS (2004). Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. Schizophrenia Research, Volume 71, Issue 2, Pages 285–295. PMID 15474899
- Kurtz MM. (2005) Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophrenia Research, 74 (1), 15–26. PMID 15694750
- Cohen & Docherty (2004). Affective reactivity of speech and emotional experience in patients with schizophrenia. Schizophr Res, 1;69(1):7–14. PMID 15145465
- Horan WP, Blanchard JJ. (2003) Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping. Schizophr Res. April 1;60(2-3):271-83. PMID 12591589
- Barrowclough C, Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B (2003). Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 112(1):92–9. PMID 12653417
- Birchwood M, Meaden A, Trower P, Gilbert P, Plaistow J (2000). The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med. Mar;30(2):337–44. PMID 10824654
- Smith B, Fowler DG, Freeman D, et al (2006). Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr Res. Sep;86(1–3):181–8. PMID 16857346
- Beck, AT (2004). A Cognitive Model of Schizophrenia, Journal of Cognitive Psychotherapy, 18 (3), 281–288. Retrieved on 2007-05-16.
- Bell V, Halligan PW, Ellis HD. (2006) Explaining delusions: a cognitive perspective. Trends Cogn Sci. May;10(5):219-26. PMID 16600666
- Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P. (2006) Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms. Schizophr Bull. Oct;32 Suppl 1:S24-31. PMID 16885206
- Green MF (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- Green MF. (2006) Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. Journal of Clinical Psychiatry, 67, Suppl 9, 3–8. PMID 16965182
- http://ajp.psychiatryonline.org/cgi/content/full/156/11/1843-b
- Jones HM, Pilowsky LS (2002) Dopamine and antipsychotic drug action revisited. British Journal of Psychiatry, 181, 271–275. PMID 12356650
- Konradi C, Heckers S. (2003). Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics, 97(2), 153–79. PMID 12559388
- Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA. (2001). Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology, 25(4), 455–67. PMID 11557159
- Coyle JT, Tsai G, Goff D. (2003). Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences, 1003, 318–27. PMID 14684455
- Tuominen HJ, Tiihonen J, Wahlbeck K. (2005). Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res, 72:225–34. PMID 15560967
- Johnstone EC, Crow TJ, Frith CD, Husband J, Kreel L. (1976). Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet, 30;2 (7992), 924–6. PMID 62160
- Flashman LA, Green MF (2004). Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment. Psychiatric Clinics of North America, 27 (1), 1–18, vii. PMID 15062627
- ^ van Os J, Burns T, Cavallaro R, et al (2006). Standardized remission criteria in schizophrenia. Acta Psychiatrica Scandinavica, 113(2), 91–5. PMID 16423159
- Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261–76. PMID 3616518
- Turner T. (2007). "Unlocking psychosis". Brit J Med. 334 (suppl): s7.
- ^ Bellack AS. (2006) Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull. Jul;32(3):432-42. PMID 16461575
- Becker T, Kilian R. (2006) Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care? Acta Psychiatrica Scandinavica Supplement, 429, 9–16. PMID 16445476
- McGurk, SR, Mueser KT, Feldman K, Wolfe R, Pascaris A (2007). Cognitive training for supported employment: 2–3 year outcomes of a randomized controlled trial. Am J Psychiatry. Mar;164(3):437–41. PMID 17329468
- Kulhara P (1994). Outcome of schizophrenia: some transcultural observations with particular reference to developing countries. European Archives of Psychiatry and Clinical Neuroscience, 244(5), 227–35. PMID 7893767
- The Royal College of Psychiatrists & The British Psychological Society (2003). Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care (PDF). London: Gaskell and the British Psychological Society. Retrieved on 2007-05-17.
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. The New England Journal of Medicine, 353 (12), 1209–23. PMID 16172203
- Dickson RA, Dalby JT, Williams R, Edwards AL. (1995) Risperidone induced prolactin elevations in premenopausal women with schizophrenia. American Journal of Psychiatry,152,1102-1103. PMID 7540803
- Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. (2004) Neuroleptic malignant syndrome and atypical antipsychotic drugs. Journal of Clinical Psychiatry, 65 (4), 464-70. PMID 15119907
- Leucht S, Wahlbeck K, Hamann J, Kissling W (2003). New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. The Lancet, 361(9369), 1581–9. PMID 12747876
- Meltzer HY (1997). "Treatment-resistant schizophrenia--the role of clozapine". Current Medical Research and Opinion. 14 (1): 1–20. PMID 9524789.
- Wahlbeck K, Cheine MV, Essali A (2007). "Clozapine versus typical neuroleptic medication for schizophrenia". The Cochrane Database of Systematic Reviews (2). John Wiley and Sons, Ltd. doi:10.1002/14651858.CD000059. PMID 10796289. ISSN 1464-780X.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Haas SJ, Hill R, Krum H (2007). "Clozapine-associated myocarditis: a review of 116 cases of suspected myocarditis associated with the use of clozapine in Australia during 1993–2003". Drug Safety. 30: 47–57. PMID 17194170.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lee M, Dickson RA, Campbell M, Oliphant J, Gretton H, Dalby JT. (1998). "Clozapine and substance abuse in patients with schizophrenia". Canadian Journal of Psychiatry. 43: 855–856.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Harrow M, Jobe TH. (2007) Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study. J Nerv Ment Dis. May;195(5):406-14. PMID 17502806
- Peet M, Brind J, Ramchand CN, Shah S, Vankar GK (2001). "Two double-blind placebo-controlled pilot studies of eicosapentaenoic acid in the treatment of schizophrenia". Schizophr. Res. 49 (3): 243–51. PMID 11356585.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Freeman MP, Hibbeln JR, Wisner KL, Davis JM, Mischoulon D, Peet M, Keck PE, Marangell LB, Richardson AJ, Lake J, Stoll AL (2006). "Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry". The Journal of clinical psychiatry. 67 (12): 1954–67. PMID 17194275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Moran, M (2005). Psychosocial Treatment Often Missing From Schizophrenia Regimens. Psychiatr News November 18 2005, Volume 40, Number 22, page 24. Retrieved on 2007-05-17.
- Cormac I, Jones C, Campbell C (2002). Cognitive behaviour therapy for schizophrenia. Cochrane Database of systematic reviews, (1), CD000524. PMID 11869579
- Zimmermann G, Favrod J, Trieu VH, Pomini V (2005). The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophrenia Research, 77, 1–9. PMID 16005380
- Wykes T, Brammer M, Mellers J, et al (2002). Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia. British Journal of Psychiatry, 181, 144–52. PMID 12151286
- Hogarty GE, Flesher S, Ulrich R, Carter M, et al (2004). Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. Sep;61(9):866–76.PMID 15351765
- McFarlane WR, Dixon L, Lukens E, Lucksted A (2003). Family psychoeducation and schizophrenia: a review of the literature. J Marital Fam Ther. Apr;29(2):223–45. PMID 12728780
- Glynn SM, Cohen AN, Niv N (2007). New challenges in family interventions for schizophrenia. Expert Rev Neurother. Jan;7(1):33–43. PMID 17187495
- Pharoah F, Mari J, Rathbone J, Wong W. (2006) Family intervention for schizophrenia Cochrane Database of Systematic Reviews, Issue 4
- Jones, S., Hayward, P. (2004). Coping with Schizophrenia: A Guide for Patients, Families and Caregivers. Oxford, England: Oneworld Pub. ISBN 1-85168-344-5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Torrey, EF (2006). Surviving Schizophrenia: A Manual for Families, Consumers, and Providers (5th Edition). HarperCollins. ISBN 0-06-084259-8.
- Kopelowicz A, Liberman RP, Zarate R (2006). Recent advances in social skills training for schizophrenia. Schizophr Bull. 2006 Oct;32 Suppl 1:S12–23. PMID 16885207
- American Psychiatric Association (2004) Practice Guideline for the Treatment of Patients With Schizophrenia. Second Edition.
- Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S (2006). Music therapy for in-patients with schizophrenia: Exploratory randomised controlled trial. The British Journal of Psychiatry. Nov;189:405–9. PMID 17077429 Full text available.
- Ruddy R, Milnes D. (2005) Art therapy for schizophrenia or schizophrenia-like illnesses. Cochrane Database of Systematic Reviews, Issue 4
- Ruddy RA, Dent-Brown K. (2007) Drama therapy for schizophrenia or schizophrenia-like illnesses. Cochrane Database of Systematic Reviews, Issue 1.
- Greenhalgh J, Knight C, Hind D, Beverley C, Walters S (2005). (abstract) "Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies". Health Technol Assess. 9 (9): 1–156. Retrieved 2007-06-17.
{{cite journal}}: Check|url=value (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - National Institute for Health and Clinical Excellence (2003). "The clinical effectiveness and cost effectiveness of electroconvulsive Therapy (ECT) for depressive illness, schizophrenia, catatonia and mania". National Institute for Health and Clinical Excellence. Retrieved 2007-06-17.
{{cite web}}: Unknown parameter|month=ignored (help) - Mashour GA, Walker EE, Martuza RL. (2005) Psychosurgery: past, present, and future. Brain Research: Brain Research Reviews, 48 (3), 409-19. PMID 15914249
- Goering P, Durbin J, Sheldon CT, Ochocka J, Nelson G, Krupa T. Who uses consumer-run self-help organizations? American Journal of Orthopsychiatry, 76 (3), 367-73. PMID 16981815
- Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, Dube KC, Ganev K, Giel R, an der Heiden W, Holmberg SK, Janca A, Lee PW, León CA, Malhotra S, Marsella AJ, Nakane Y, Sartorius N, Shen Y, Skoda C, Thara R, Tsirkin SJ, Varma VK, Walsh D, Wiersma D. (2001) Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. Jun;178:506-17. PMID 11388966
- Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A (1987). The Vermont longitudinal study of persons with severe mental illness, II: Long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. American Journal of Psychiatry, 144(6), 727–35. PMID 3591992
- Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM (2004). Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. American Journal of Psychiatry, 161, 473–479. PMID 14992973
- Harvey, C.A., Jeffreys, S.E., McNaught, A.S., Blizard, R.A., King, M.B.(2007) The Camden Schizophrenia Surveys III: Five-Year Outcome of a Sample of Individuals From a Prevalence Survey and the Importance of Social Relationships. International Journal of Social Psychiatry, Vol. 53, No. 4, 340-356
- Hopper K, Wanderling J (2000). Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia. Schizophrenia Bulletin, 26 (4), 835–46. PMID 11087016
- Davidson L, McGlashan TH. (1997) The varied outcomes of schizophrenia. Canadian Journal of Psychiatry, 42 (1), 34–43. PMID 9040921
- Lieberman JA, Koreen AR, Chakos M, Sheitman B, Woerner M, Alvir JM, Bilder R. (1996) Factors influencing treatment response and outcome of first-episode schizophrenia: implications for understanding the pathophysiology of schizophrenia. Journal of Clinical Psychiatry, 57 Suppl 9, 5–9. PMID 8823344
- Bebbington PE, Kuipers E (1994). The predictive utility of expressed emotion in schizophrenia: an aggregate analysis. Psychological Medicine, 24, 707–718. PMID 7991753
- Hannerz H, Borga P, Borritz M (2001). Life expectancies for individuals with psychiatric diagnoses. Public Health, 115 (5), 328–37. PMID 11593442
- Radomsky ED, Haas GL, Mann JJ, Sweeney JA (1999). Suicidal behavior in patients with schizophrenia and other psychotic disorders. American Journal of Psychiatry, 156(10), 1590–5. PMID 10518171
- Williams R, Dalby JT. Eds. (1989). Depression in Schizophrenics. New York: Plenum Publishing.
- Caldwell CB, Gottesman II. (1990). Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophrenia Bulletin, 16(4), 571–89. PMID 2077636
- Walsh E, Buchanan A, Fahy T (2002). Violence and schizophrenia: examining the evidence. British Journal of Psychiatry. 2002 Jun;180:490–5. PMID 12042226
- Stuart, H (2003). Violence and mental illness: an overview. World Psychiatry. June; 2(2): 121–124. PMID 16946914 Full text, Retrieved on 2007-05-17.
- Steadman HJ, Mulvey EP, Monahan J, et al (1998). Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry. May;55(5):393–401. PMID 9596041
- Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, et al (2006). A national study of violent behavior in persons with schizophrenia. Archives of General Psychiatry. May;63(5):490–9. PMID 16651506
- Swanson JW, Holzer CE, Ganju VK, Jono RT. (1990) Violence and Psychiatric Disorder in the Community: Evidence From the Epidemiologic Catchment Area Surveys Hosp Community Psychiatry 41:761-770, July 1990 PMID 2142118
- ^ Mullen PE (2006). Schizophrenia and violence: from correlations to preventive strategies. Advances in Psychiatric Treatment 12: 239–248. Full text available, Retrieved on 2007-05-17.
- Simpson AI, McKenna B, Moskowitz A, Skipworth J, Barry-Walsh J (2004). Homicide and mental illness in New Zealand, 1970–2000. British Journal of Psychiatry, 185, 394–8. PMID 15516547
- Fazel S, Grann M (2004). Psychiatric morbidity among homicide offenders: a Swedish population study. American Journal of Psychiatry, 161(11), 2129–31. PMID 15514419
- Brekke JS, Prindle C, Bae SW, Long JD (2001). Risks for individuals with schizophrenia who are living in the community. Psychiatric Services. Oct;52(10):1358–66. PMID 11585953
- Fitzgerald PB, de Castella AR, Filia KM, Filia SL, Benitez J, Kulkarni J (2005). Victimization of patients with schizophrenia and related disorders. Australia and New Zealand Journal of Psychiatry, 39(3), 169-74. (1), 187–9. PMID 15701066
- Walsh E, Gilvarry C, Samele C, et al (2004). Predicting violence in schizophrenia: a prospective study. Schizophrenia Research, 67(2–3), 247-52. PMID 14984884
- Solomon PL, Cavanaugh MM, Gelles RJ (2005). Family Violence among Adults with Severe Mental Illness. Trauma, Violence, & Abuse, Vol. 6, No. 1, 40–54. PMID 15574672Full text available.
- Chou KR, Lu RB, Chang M (2001). Assaultive behavior by psychiatric in-patients and its related factors. Journal of Nursing Research. Dec;9(5):139–51. PMID 11779087
- Logdberg B, Nilsson LL, Levander MT, Levander S (2004). Schizophrenia, neighbourhood, and crime. Acta Psychiatrica Scandinavica, 110(2) Page 92. PMID 15233709 Full text available, Retrieved on 2007-05-16
- Cannon TD, Cornblatt B, McGorry P. (2007) Editor's Introduction: The Empirical Status of the Ultra High-Risk (Prodromal) Research Paradigm. Schizophrenia Bulletin, 33 (3), 661–4. PMID 17470445
- Drake RJ, Lewis SW. (2005) Early detection of schizophrenia. Current Opinion in Psychiatry, 18 (2), 147–50. PMID 16639167
- Van Os J, Delespaul P. (2005) Toward a world consensus on prevention of schizophrenia. Dialogues in Clinical Neuroscience, 7 (1), 53–67.
- Haroun N, Dunn L, Haroun A, Cadenhead KS. (2006) Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophrenia Bulletin, 32 (1), 166–78. PMID 16207892. Full text
- Hafner H, Maurer K, Ruhrmann S, et al. (2004) "Early detection and secondary prevention of psychosis: facts and visions". European Archives of Psychiatry and Clinical Neuroscience, 254 (2), 117–28. PMID 15146341
- McGorry, Patrick (2003). "The Influence of Stigma on Preventive Efforts in Psychotic Disorders," in Schizophrenia (WPA Series in Evidence & Experience in Psychiatry), p. 292.
- Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S (1999). "The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems," American Journal of Public Health, 89(9):1339–45. PMID 10474550
- Phelan, Jo C., Link, Bruce G., Stueve, Ann, Pescosolido, Bernice A. (1997). "Public Conceptions of Mental Illness in 1950 and 1996: What Is Mental Illness and Is It to be Feared?," Journal of Health and Social Behavior, 41(2):188-207
- American Psychiatric Association. Americans Still Cling to Myths About Mental Illness, Survey Finds. Psychiatric News. December 7, 2001 Volume 36 Number 23 Full text
- Cooper D (1969) The Dialectics of Liberation. London: Penguin Books Ltd. ISBN 0140210296
- Szasz T (1984) The Myth of Mental Illness: Foundations of a Theory of Personal Contact (revised edition. New York: Harper and Row. ISBN 0060911514
- Colin, Ross (2004). Schizophrenia: Innovations in Diagnosis and Treatment. Haworth Press. ISBN 0789022699.
- R.D. Laing's and Aaron Esterson. Sanity, Madness and the Family (1964)
- Bateson, G., Jackson, D. D., Haley, J. & Weakland, J., 1956, Toward a theory of schizophrenia. (in: 'Behavioral Science', vol.1, 251-264)
- Jaynes J (1976) The Origin of Consciousness in the Breakdown of the Bicameral Mind. Houghton Mifflin. ISBN 0395207290
- Polimeni J, Reiss JP (2002). How shamanism and group selection may reveal the origins of schizophrenia. Medical Hypothesis, 58(3), 244–8. PMID 12018978
- DeMause, Lloyd, "The seven stages of historical personality" in The Emotional Life of Nations (Karnac, 2002). Available at primal-page.com, Retrieved on 2007-05-17.
- Kurtz, Paul (1986). The Transcendental Temptation: A Critique of Religion and the Paranormal (Prometheus Books) ISBN 0-87975-645-4
- Crow TJ (1997). Schizophrenia as failure of hemispheric dominance for language. Trends in Neurosciences, 20(8), 339–343. PMID 9246721
- Bola JR, Mosher LR (April 2003). "Treatment of Acute Psychosis Without Neuroleptics: Two-Year Outcomes From the Soteria Project" (PDF). The Journal of Nervous and Mental Disease. 191. Lippincott Williams & Wilkins, Inc: 219–229. PMID 12695732. Retrieved 2007-06-13.
- Mosher LR (1999). "Soteria and Other Alternatives to Acute Psychiatric Hospitalization: A Personal and Professional Review." Journal of Nervous and Mental Disease, 187, 142–149.
- Hoffer and Walker, Orthomolecular Nutrition. Keats Publishing, 1978
- Pfeiffer, Carl C. Nutrition and Mental Illness: An Orthomolecular Approach to Balancing Body Chemistry. Healing Art Press. ISBN 0-89281-226-5.
- Pauling, L (1973). Orthomolecular Psychiatry: Treatment of Schizophrenia. San Francisco: Freeman. p. 697. ISBN ??.
{{cite book}}: Check|isbn=value: invalid character (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Dohan FC (1970). Coeliac disease and schizophrenia. Lancet, 1970 April 25;1(7652):897–8. PMID 4191543
*Dohan FC (1973). Coeliac disease and schizophrenia. British Medical Journal, 3(5870): 51–52. PMID 4740433
* Dohan FC (1979). Celiac-type diets in schizophrenia. Am J Psychiatry, 1979 May;136(5):732–3. PMID 434265 - Kalaydjian AE, Eaton W, Cascella N, Fasano A (2006). The gluten connection: the association between schizophrenia and celiac disease. Acta Psychiatr Scand. 2006 Feb;113(2):82–90. PMID 16423158
- Evans K, McGrath J, Milns R. (2003). Searching for schizophrenia in ancient Greek and Roman literature: a systematic review. Acta Psychiatrica Scandanavica, 107(5), 323–330. PMID 12752027
- Hanafy A. Youssef, Fatma A. Youssef and T. R. Dening (1996), "Evidence for the existence of schizophrenia in medieval Islamic society", History of Psychiatry 7: 55-62 .
- Kraepelin E. (1907) Text book of psychiatry (7th ed) (trans. A.R. Diefendorf). London: Macmillan.
- "Conditions in Occupational Therapy: effect on occupational performance." ed. Ruth A. Hansen and Ben Atchison (Baltimore: Lippincott, Williams & Williams, 2000), 54–74. ISBN 0-683-30417-8
- Kuhn R; tr. Cahn CH (2004). "Eugen Bleuler's concepts of psychopathology". Hist Psychiatry. 15 (3): 361–6. doi:10.1177/0957154X04044603. PMID 15386868.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Stotz-Ingenlath G. (2000). Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911. Medicine, Health Care, and Philosophy, 3(2), 153–9. PMID 11079343
- Turner T. (1999) 'Schizophrenia'. In G. E. Berrios and R. Porter (eds) A History of Clinical Psychiatry. London: Athlone Press. ISBN 0-485-24211-7
- Allen GE. (1997). The social and economic origins of genetic determinism: a case history of the American Eugenics Movement, 1900–1940 and its lessons for today. Genetica, 99, 77–88. PMID 9463076
- Read J, Masson J. (2004) Genetics, eugenics and mass murder. In J. Read, L.R. Mosher, R.P. Bentall (eds) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6
- Lifton RJ. (2000) The Nazi Doctors: Medical Killing and the Psychology of Genocide. Basic Books. ISBN 0465049052
- Wing JK (1971) International comparisons in the study of the functional psychoses. British Medical Bulletin, 27 (1), 77–81. PMID 4926366
- Wilson M. (1993) DSM-III and the transformation of American psychiatry: a history. American Journal of Psychiatry, 150 (3), 399–410. PMID 8434655
- Deveson, Anne (1991). Tell Me I'm Here. Penguin. ISBN 0-14-027257-7.
Further reading
- Bentall, R. (2003) Madness explained: Psychosis and Human Nature. London: Penguin Books Ltd. ISBN 0-7139-9249-2
- Dalby, J.T. (1997) Mental Disease in History: A selection of translated readings. New York: Peter Lang Publishing. ISBN 0-8204-3056-0
- Fallon, James H. et al. (2003) The Neuroanatomy of Schizophrenia: Circuitry and Neurotransmitter Systems. Clinical Neuroscience Research 3:77–107. Available at Elsevier article locater.
- Green, M.F. (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- Keen, T. M. (1999) Schizophrenia: orthodoxy and heresies. A review of alternative possibilities. Journal of Psychiatric and Mental Health Nursing, 1999, 6, 415–424. PMID 10818864
- Lidz, Theodore, Stephen Fleck & Alice Cornelison, Schizophrenia and the Family. International Universities Press, 1965. ISBN 978-0823660018
- Noll, Richard (2007) The Encyclopedia of Schizophrenia and Other Psychotic Disorders, Third Edition ISBN 0-8160-6405-9
- Open The Doors - information on global programme to fight stigma and discrimination because of Schizophrenia. The World Psychiatric Association (WPA)
- Read, J., Mosher, L.R., Bentall, R. (2004) Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. ISBN 1-58391-906-6. A critical approach to biological and genetic theories, and a review of social influences on schizophrenia.
- Scientific American Magazine (January 2004 Issue) Decoding Schizophrenia
- Shaner, A., Miller, G. F., & Mintz, J. (2004). Schizophrenia as one extreme of a sexually selected fitness indicator. Schizophrenia Research, 70(1), 101–109. PMID 15246469Full text (PDF), Retrieved on 2007-05-17.
- Szasz, T. (1976) Schizophrenia: The Sacred Symbol of Psychiatry. New York: Basic Books. ISBN 0-465-07222-4
- Tausk, V. : "Sexuality, War, and Schizophrenia: Collected Psychoanalytic Papers", Publisher: Transaction Publishers 1991, ISBN 0-88738-365-3 (On the Origin of the 'Influencing Machine' in Schizophrenia.)
- Wiencke, Markus (2006) Schizophrenie als Ergebnis von Wechselwirkungen: Georg Simmels Individualitätskonzept in der Klinischen Psychologie. In David Kim (ed.), Georg Simmel in Translation: Interdisciplinary Border-Crossings in Culture and Modernity (pp. 123–155). Cambridge Scholars Press, Cambridge, ISBN 1-84718-060-5
External links
- Template:Dmoz
- Bibliography of scholarly histories on schizophrenia and dementia praecox, part 1 (2000-mid 2007).
- News, information and further description
- NPR: the sight and sounds of schizophrenia
- The current World Health Organisation definition of Schizophrenia
- Symptoms in Schizophrenia Film made in 1940 showing some of the symptoms of Schizophrenia.
- Schizophrenics call to Church for understanding, Western Catholic Reporter
- World Fellowship for Schizophrenia and Allied Disorders - 'Information for families caring for people with mental illness'
- Critical approaches to schizophrenia
- Leo, Jonathan Ph.D., & Jay Joseph, Psy. D. Schizophrenia: Medical students are taught it's all in the genes, but are they hearing the whole story?
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
Template:Link FA Template:Link FA
Categories: