This is an old revision of this page, as edited by Sailsbystars (talk | contribs) at 02:21, 10 October 2010 (Reverted 1 edit by 184.32.140.145 identified as vandalism to last revision by 98.219.150.123. (TW)). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 02:21, 10 October 2010 by Sailsbystars (talk | contribs) (Reverted 1 edit by 184.32.140.145 identified as vandalism to last revision by 98.219.150.123. (TW))(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) Medical condition| Attention deficit hyperactivity disorder | |
|---|---|
| Specialty | Psychiatry, child and adolescent psychiatry |
Attention-Deficit Hyperactivity Disorder (ADHD or AD/HD or ADD) is a neurobehavioral developmental disorder. It is primarily characterized by "the co-existence of attentional problems and hyperactivity, with each behavior occurring infrequently alone" and symptoms starting before seven years of age.
ADHD is the most commonly studied and diagnosed psychiatric disorder in children, affecting about 3% to 5% of children globally and diagnosed in about 2% to 16% of school aged children. It is a chronic disorder with 30% to 50% of those individuals diagnosed in childhood continuing to have symptoms into adulthood. Adolescents and adults with ADHD tend to develop coping mechanisms to compensate for some or all of their impairments. 4.7% of American adults are estimated to live with ADHD.
ADHD is diagnosed two to four times as frequently in boys as in girls, though studies suggest this discrepancy may be due to subjective bias of referring teachers. ADHD management usually involves some combination of medications, behavior modifications, lifestyle changes, and counseling. Its symptoms can be difficult to differentiate from other disorders, increasing the likelihood that the diagnosis of ADHD will be missed. Additionally, most clinicians have not received formal training in the assessment and treatment of ADHD, particularly in adult patients.
ADHD and its diagnosis and treatment have been considered controversial since the 1970s. The controversies have involved clinicians, teachers, policymakers, parents and the media. Topics include the actuality of the disorder, its causes, and the use of stimulant medications in its treatment. Most healthcare providers accept that ADHD is a genuine disorder with debate in the scientific community centering mainly around how it is diagnosed and treated. The American Medical Association concluded in 1998 that the diagnostic criteria for ADHD are based on extensive research and, if applied appropriately, lead to the diagnosis with high reliability.
Classification
ADHD may be seen as one or more continuous traits found normally throughout the general population. ADHD is a developmental disorder in which certain traits such as impulse control lag in development. Using magnetic resonance imaging of the prefrontal cortex, this developmental lag has been estimated to range from 3 to 5 years. These delays are considered to cause impairment. A diagnosis of ADHD does not, however, imply a neurological disease.
ADHD is classified as a disruptive behavior disorder along with oppositional defiant disorder, conduct disorder and antisocial disorder.
Subtypes
ADHD has three subtypes:
- Predominantly hyperactive-impulsive
- Most symptoms (six or more) are in the hyperactivity-impulsivity categories.
- Fewer than six symptoms of inattention are present, although inattention may still be present to some degree.
- Predominantly inattentive
- The majority of symptoms (six or more) are in the inattention category and fewer than six symptoms of hyperactivity-impulsivity are present, although hyperactivity-impulsivity may still be present to some degree.
- Children with this subtype are less likely to act out or have difficulties getting along with other children. They may sit quietly, but they are not paying attention to what they are doing. Therefore, the child may be overlooked, and parents and teachers may not notice symptoms of ADHD.
- Combined hyperactive-impulsive and inattentive
- Six or more symptoms of inattention and six or more symptoms of hyperactivity-impulsivity are present.
- Most children with ADHD have the combined type.
Childhood ADHD
Attention-deficit hyperactivity disorder or ADHD is a common childhood condition that can be treated. ADHD may affect certain areas of the brain that allow problem solving, planning ahead, understanding others’ actions, and impulse control.
The American Academy of Child Adolescent Psychiatry (AACAP) considers it necessary that the following be present before attaching the label of ADHD to a child:
- The behaviors must appear before age 7.
- They must continue for at least six months.
- The symptoms must also create a real handicap in at least two of the following areas of the child’s life:
- in the classroom,
- on the playground,
- at home,
- in the community, or
- in social settings.
If a child seems too active on the playground but not elsewhere, the problem might not be ADHD. It might also not be ADHD if the behaviors occur in the classroom but nowhere else. A child who shows some symptoms would not be diagnosed with ADHD if his or her schoolwork or friendships are not impaired by the behaviors.
Even if a child’s behavior seems like ADHD, it might not actually be ADHD; careful attention to the process of differential diagnosis is mandatory. Many other conditions and situations can trigger behavior that resembles ADHD. For example, a child might show ADHD symptoms when experiencing:
- A death or divorce in the family, a parent’s job loss, or other sudden change
- Undetected seizures
- An ear infection that causes temporary hearing problems
- Problems with schoolwork caused by a learning disability
- Anxiety or depression
- Insufficient or poor quality sleep
- Child abuse
Adult ADHD
Main article: Adult attention-deficit disorderResearchers found that 60% of the children diagnosed with ADHD continue having symptoms well into adulthood. Many adults, however, remain untreated. Untreated adults with ADHD often have chaotic lifestyles, may appear to be disorganized and may rely on non-prescribed drugs and alcohol to get by. They often have such associated psychiatric comorbidities as depression, anxiety disorder, bipolar disorder, substance abuse, or a learning disability. A diagnosis of ADHD may offer adults insight into their behaviors and allow patients to become more aware and seek help with coping and treatment strategies. There is controversy amongst some experts on whether ADHD persists into adulthood. Recognized as occurring in adults in 1978, it is currently not addressed separately from ADHD in childhood. Obstacles that clinicians face when assessing adults who may have ADHD include developmentally inappropriate diagnostic criteria, age-related changes, comorbidities and the possibility that high intelligence or situational factors can mask ADHD.
Signs and symptoms
Inattention, hyperactivity, and impulsivity are the key behaviors of ADHD. The symptoms of ADHD are especially difficult to define because it is hard to draw the line at where normal levels of inattention, hyperactivity, and impulsivity end and clinically significant levels requiring intervention begin. To be diagnosed with ADHD, symptoms must be observed in two different settings for six months or more and to a degree that is greater than other children of the same age.
The symptom categories of ADHD in children yield three potential classifications of ADHD—predominantly inattentive type, predominantly hyperactive-impulsive type, or combined type if criteria for both subtypes are met:
Predominantly inattentive type symptoms may include:
- Be easily distracted, miss details, forget things, and frequently switch from one activity to another
- Have difficulty maintaining focus on one task
- Become bored with a task after only a few minutes, unless doing something enjoyable
- Have difficulty focusing attention on organizing and completing a task or learning something new or trouble completing or turning in homework assignments, often losing things (e.g., pencils, toys, assignments) needed to complete tasks or activities
- Not seem to listen when spoken to
- Daydream, become easily confused, and move slowly
- Have difficulty processing information as quickly and accurately as others
- Struggle to follow instructions.
Predominantly hyperactive-impulsive type symptoms may include:
- Fidget and squirm in their seats
- Talk nonstop
- Dash around, touching or playing with anything and everything in sight
- Have trouble sitting still during dinner, school, and story time
- Be constantly in motion
- Have difficulty doing quiet tasks or activities.
and also these manifestations primarily of impulsivity:
- Be very impatient
- Blurt out inappropriate comments, show their emotions without restraint, and act without regard for consequences
- Have difficulty waiting for things they want or waiting their turns in games
Most people exhibit some of these behaviors, but not to the degree where such behaviors significantly interfere with a person's work, relationships, or studies. The core impairments are consistent even in different cultural contexts.
Symptoms may persist into adulthood for up to half of children diagnosed with ADHD. Estimating this is difficult as there are no official diagnostic criteria for ADHD in adults. ADHD in adults remains a clinical diagnosis. The signs and symptoms may differ from those during childhood and adolescence due to the adaptive processes and avoidance mechanisms learned during the process of socialisation.
A 2009 study found that children with ADHD move around a lot because it helps them stay alert enough to complete challenging tasks.
Comorbidities
ADHD may accompany other disorders such as anxiety or depression. Such combinations can greatly complicate diagnosis and treatment. Academic studies and research in private practice suggest that depression in ADHD appears to be increasingly prevalent in children as they get older, with a higher rate of increase in girls than in boys, and to vary in prevalence with the subtype of ADHD. Where a mood disorder complicates ADHD it would be prudent to treat the mood disorder first, but parents of children who have ADHD often wish to have the ADHD treated first, because the response to treatment is quicker.
Inattention and "hyperactive" behavior are not the only problems in children with ADHD. ADHD exists alone in only about 1/3 of the children diagnosed with it. Many co-existing conditions require other courses of treatment and should be diagnosed separately instead of being grouped in the ADHD diagnosis. Some of the associated conditions are:
- Oppositional defiant disorder (35%) and conduct disorder (26%) which both are characterized by antisocial behaviors such as stubbornness, aggression, frequent temper tantrums, deceitfulness, lying, or stealing, inevitably linking these comorbid disorders with antisocial personality disorder (ASPD); about half of those with hyperactivity and ODD or CD develop ASPD in adulthood.
- Borderline personality disorder, which was according to a study on 120 female psychiatric patients diagnosed and treated for BPD associated with ADHD in 70% of those cases.
- Primary disorder of vigilance, which is characterized by poor attention and concentration, as well as difficulties staying awake. These children tend to fidget, yawn and stretch and appear to be hyperactive in order to remain alert and active.
- Mood disorders. Boys diagnosed with the combined subtype have been shown likely to suffer from a mood disorder.
- Bipolar disorder. As many as 25% of children with ADHD have bipolar disorder. Children with this combination may demonstrate more aggression and behavioral problems than those with ADHD alone.
- Anxiety disorder, which has been found to be common in girls diagnosed with the inattentive subtype of ADHD.
- Obsessive-compulsive disorder. OCD is believed to share a genetic component with ADHD and shares many of its characteristics.
Cause
A specific cause of ADHD is not known. There are, however, a number of factors that may contribute to, or exacerbate ADHD. They include genetics, diet and social and physical environments.
Genetics
Twin studies indicate that the disorder is highly heritable and that genetics are a factor in about 75% of ADHD cases. Hyperactivity also seems to be primarily a genetic condition; however, other causes do have an effect.
Researchers believe that a large majority of ADHD cases arise from a combination of various genes, many of which affect dopamine transporters. Candidate genes include α2A adrenergic receptor, dopamine transporter, dopamine receptors D2/D3, dopamine beta-hydroxylase monoamine oxidase A, catecholamine-methyl transferase, serotonin transporter promoter (SLC6A4), 5HT2A receptor, 5HT1B receptor, the 10-repeat allele of the DAT1 gene, the 7-repeat allele of the DRD4 gene, and the dopamine beta hydroxylase gene (DBH TaqI).
The broad selection of targets indicates that ADHD does not follow the traditional model of "a genetic disease" and should therefore be viewed as a complex interaction among genetic and environmental factors. Even though all these genes might play a role, to date no single gene has been shown to make a major contribution to ADHD.
Evolutionary theories
See also: Hunter vs. farmer theoryThe hunter vs. farmer theory is a hypothesis proposed by author Thom Hartmann about the origins of ADHD. The theory proposes that hyperactivity may be an adaptive behavior in pre-modern humans and that those with ADHD retain some of the older "hunter" characteristics associated with early pre-agricultural human society. According to this theory, individuals with ADHD may be more adept at searching and seeking and less adept at staying put and managing complex tasks over time. Further evidence showing hyperactivity may be evolutionarily beneficial was put forth in 2006 in a study which found it may carry specific benefits for certain forms of ancient society. In these societies, those with ADHD are hypothesized to have been more proficient in tasks involving risk or competition (i.e. hunting, mating rituals, etc.).
Environmental
Twin studies to date have suggested that approximately 9% to 20% of the variance in hyperactive-impulsive-inattentive behavior or ADHD symptoms can be attributed to nonshared environmental (nongenetic) factors. Environmental factors implicated include alcohol and tobacco smoke exposure during pregnancy and environmental exposure to lead in very early life. The relation of smoking to ADHD could be due to nicotine causing hypoxia (lack of oxygen) to the fetus in utero. It could also be that women with ADHD are more likely to smoke and therefore, due to the strong genetic component of ADHD, are more likely to have children with ADHD. Complications during pregnancy and birth—including premature birth—might also play a role. ADHD patients have been observed to have higher than average rates of head injuries; however, current evidence does not indicate that head injuries are the cause of ADHD in the patients observed. Infections during pregnancy, at birth, and in early childhood are linked to an increased risk of developing ADHD. These include various viruses (measles, varicella, rubella, enterovirus 71) and streptococcal bacterial infection.
A 2007 study linked the organophosphate insecticide chlorpyrifos, which is used on some fruits and vegetables, with delays in learning rates, reduced physical coordination, and behavioral problems in children, especially ADHD.
A 2010 study found that pesticide exposure is strongly associated with an increased risk of ADHD in children. Researchers analyzed the levels of organophosphate residues in the urine of more than 1,100 children aged 8 to 15 years old, and found that those with the highest levels of dialkyl phosphates, which are the breakdown products of organophosphate pesticides, also had the highest incidence of ADHD. Overall, they found a 35% increase in the odds of developing ADHD with every 10-fold increase in urinary concentration of the pesticide residues. The effect was seen even at the low end of exposure: children who had any detectable, above-average level of pesticide metabolite in their urine were twice as likely as those with undetectable levels to record symptoms of ADHD.
Diet
Main article: Diet and attention deficit hyperactivity disorderA study conducted by researchers at Southampton University in the United Kingdom and published in The Lancet on November 3, 2007 found a link between children’s ingestion of many commonly used artificial food colors, the preservative sodium benzoate and hyperactivity. In response to these findings, the British government took prompt action. According to the Food Standards Agency, the food regulatory agency in the UK, food manufacturers are being encouraged to voluntarily phase out the use of most artificial food colors by the end of 2009. Following the FSA’s actions, the European Commission ruled that any food products containing the “Southampton Six” (The contentious colourings are: sunset yellow FCF (E110), quinoline yellow (E104), carmoisine (E122), allura red (E129), tartrazine (E102) and ponceau 4R (E124)) must display warning labels on their packaging by 2010. In the US, little has been done to curb food manufacturer’s use of specific food colors, despite the new evidence presented by the Southampton study. However, the existing US Food Drug and Cosmetic Act had already required that artificial food colors be approved for use, that they must be given FD&C numbers by the FDA, and the use of these colors must be indicated on the package. This is why food packaging in the USA may state something like: "Contains FD&C Red #40."
Social
The World Health Organization states that the diagnosis of ADHD can represent family dysfunction or inadequacies in the educational system rather than individual psychopathology. Other researchers believe that relationships with caregivers have a profound effect on attentional and self-regulatory abilities. A study of foster children found that a high number of them had symptoms closely resembling ADHD. Researchers have found behavior typical of ADHD in children who have suffered violence and emotional abuse. Furthermore, Complex Post Traumatic Stress Disorder can result in attention problems that can look like ADHD. ADHD is also considered to be related to sensory integration dysfunction.
A 2010 article by CNN suggests that there is an increased risk for internationally adopted children to develop mental health disorders, such as ADHD and ODD. The risk may be related to the length of time the children spent in an orphanage, especially if they were neglected or abused. Many of these families who adopted the affected children feel overwhelmed and frustrated, since managing their children may entail more responsibilities than originally anticipated. The adoption agencies may be aware of the child's behavioral history, but decide to withhold the information prior to the adoption. This in turn has resulted in some parents suing adoption agencies, the abuse of children, and even the relinquishment of the child.
Neurodiversity
Main article: NeurodiversityProponents of the neurodiversity theory assert that atypical (neurodivergent) neurological development is a normal human difference that is to be tolerated and respected just like any other human difference. Social critics argue that while biological factors may play a large role in difficulties with sitting still in class and/or concentrating on schoolwork in some children, these children could have failed to integrate others' social expectations of their behavior for a variety of other reasons. It has been said that ADHD has a link with creativity. As genetic research into ADHD proceeds, it may become possible to integrate this information with the neurobiology in order to distinguish disability from varieties of normal or even exceptional functioning in people along the same spectrum of attention differences.
Social construct theory of ADHD
Main article: Social construct theory of ADHDSocial construction theory states that it is societies that determine where the line between normal and abnormal behavior is drawn. Thus society members including physicians, parents, teachers, and others are the ones who determine which diagnostic criteria are applied and thus determine the number of people affected. This is exemplified in the fact that the DSM IV arrives at levels of ADHD three to four times higher than those obtained with use of the ICD 10. Thomas Szasz, an extreme proponent of this theory, has gone so far as to state that ADHD was "invented and not discovered."
Low arousal theory
Main article: Low arousal theoryAccording to the low arousal theory, people with ADHD need excessive activity as self-stimulation because of their state of abnormally low arousal. The theory states that those with ADHD cannot self-moderate, and their attention can only be gained by means of environmental stimuli, which in turn results in disruption of attentional capacity and an increase in hyperactive behaviour.
Without enough stimulation coming from the environment, an ADHD child will create it him or herself by walking around, fidgeting, talking, etc. This theory also explains why stimulant medications have high success rates and can induce a calming effect at therapeutic dosages among children with ADHD. It establishes a strong link with scientific data that ADHD is connected to abnormalities with the neurochemical dopamine and a powerful link with low-stimulation PET scan results in ADHD subjects.
Pathophysiology

The pathophysiology of ADHD is unclear and there are a number of competing theories. Research on children with ADHD has shown a general reduction of brain volume, but with a proportionally greater reduction in the volume of the left-sided prefrontal cortex. These findings suggest that the core ADHD features of inattention, hyperactivity, and impulsivity may reflect frontal lobe dysfunction, but other brain regions particularly the cerebellum have also been implicated. Neuroimaging studies in ADHD have not always given consistent results and as of 2008 are only used for research not diagnostic purposes. A 2005 review of published studies involving neuroimaging, neuropsychological genetics, and neurochemistry found converging lines of evidence to suggest that four connected frontostriatal regions play a role in the pathophysiology of ADHD: The lateral prefrontal cortex, dorsal anterior cingulate cortex, caudate, and putamen.
In one study a delay in development of certain brain structures by an average of three years occurred in ADHD elementary school aged patients. The delay was most prominent in the frontal cortex and temporal lobe, which are believed to be responsible for the ability to control and focus thinking. In contrast, the motor cortex in the ADHD patients was seen to mature faster than normal, suggesting that both slower development of behavioral control and advanced motor development might be required for the fidgetiness that characterizes ADHD. It should be noted that stimulant medication itself may affect growth factors of the central nervous system.
The same laboratory had previously found involvement of the "7-repeat" variant of the dopamine D4 receptor gene, which accounts for about 30 percent of the genetic risk for ADHD, in unusual thinness of the cortex of the right side of the brain; however, in contrast to other variants of the gene found in ADHD patients, the region normalized in thickness during the teen years in these children, coinciding with clinical improvement.
Additionally, SPECT scans found people with ADHD to have reduced blood circulation (indicating low neural activity), and a significantly higher concentration of dopamine transporters in the striatum which is in charge of planning ahead. A study by the U.S. Department of Energy’s Brookhaven National Laboratory in collaboration with Mount Sinai School of Medicine in New York suggest that it is not the dopamine transporter levels that indicate ADHD, but the brain's ability to produce neurotransmitters like dopamine itself. The study was done by injecting 20 ADHD subjects and 25 control subjects with a radiotracer that attaches itself to dopamine transporters. The study found that it was not the transporter levels that indicated ADHD, but the dopamine itself. ADHD subjects showed lower levels of dopamine (hypodopaminergia) across the board. They speculated that since ADHD subjects had lower levels of dopamine to begin with, the number of transporters in the brain was not the telling factor. In support of this notion, plasma homovanillic acid, an index of dopamine levels, was found to be inversely related not only to childhood ADHD symptoms in adult psychiatric patients, but to "childhood learning problems" in healthy subjects as well. One interpretation of dopamine pathway tracers is that the biochemical "reward" mechanism works for those with ADHD only when the task performed is inherently motivating; low levels of dopamine raise the threshold at which someone can maintain focus on a task which is otherwise boring. Neuroimaging studies also found that neurotransmitters level (e.g. dopamine and serotonin) in the synaptic cleft goes down during depression.
A 1990 PET scan study by Alan J. Zametkin et al. found that global cerebral glucose metabolism was 8% lower in medication-naive adults who had been hyperactive since childhood. Further studies found that chronic stimulant treatment had little effect on global glucose metabolism, a 1993 study in girls failed to find a decreased global glucose metabolism, but found significant differences in glucose metabolism in 6 specific regions of the brains of ADHD girls as compared to control subjects. The study also found that differences in one specific region of the frontal lobe were statistically correlated with symptom severity. A further study in 1997 also failed to find global differences in glucose metabolism, but similarly found differences in glucose normalization in specific regions of the brain. The 1997 study also noted that their findings were somewhat different than those in the 1993 study, and concluded that sexual maturation may have played a role in this discrepancy. The significance of the research by Zametkin has not been determined and neither his group nor any other has been able to replicate the 1990 results.
Critics, such as Jonathan Leo and David Cohen, who reject the characterization of ADHD as a disorder, contend that the controls for stimulant medication usage were inadequate in some lobar volumetric studies which makes it impossible to determine whether ADHD itself or psychotropic medication used to treat ADHD is responsible for the decreased thickness observed in certain brain regions. While the main study in question used age-matched controls, it did not provide information on height and weight of the subjects. These variables it has been argued could account for the regional brain size differences rather than ADHD itself. They believe many neuroimaging studies are oversimplified in both popular and scientific discourse and given undue weight despite deficiencies in experimental methodology.
Diagnosis
ADHD is diagnosed via a psychiatric assessment; to rule out other potential causes or comorbidities, physical examination, radiological imaging, and laboratory tests may be used.
In North America, the DSM-IV criteria are often the basis for a diagnosis, while European countries usually use the ICD-10. If the DSM-IV criteria are used, rather than the ICD-10, a diagnosis of ADHD is 3–4 times more likely. Factors other than those within the DSM or ICD however have been found to affect the diagnosis in clinical practice. A child's social and school environment as well as academic pressures at school are likely to be of influence.
Many of the symptoms of ADHD occur from time to time in everyone; in patients with ADHD, the frequency of these symptoms is greater and patients' lives are significantly impaired. Impairment must occur in multiple settings to be classified as ADHD. As with many other psychiatric and medical disorders, the formal diagnosis is made by a qualified professional in the field based on a set number of criteria. In the USA these criteria are laid down by the American Psychiatric Association in their Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), 4th edition. Based on the DSM-IV criteria listed below, three types of ADHD are classified:
- ADHD, Combined Type: if both criteria 1A and 1B are met for the past 6 months
- ADHD Predominantly Inattentive Type: if criterion 1A is met but criterion 1B is not met for the past six months
- ADHD, Predominantly Hyperactive-Impulsive Type: if criterion 1B is met but criterion 1A is not met for the past six months.
The previously used term ADD expired with the most recent revision of the DSM. Consequently, ADHD is the current nomenclature used to describe the disorder as one distinct disorder which can manifest itself as being a primary deficit resulting in hyperactivity/impulsivity (ADHD, predominately hyperactive-impulsive type) or inattention (ADHD predominately inattentive type) or both (ADHD combined type).
DSM-IV criteria
IA. Six or more of the following signs of inattention have been present for at least 6 months to a point that is disruptive and inappropriate for developmental level:
- Inattention:
- Often does not give close attention to details or makes careless mistakes in schoolwork, work, or other activities.
- Often has trouble keeping attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow instructions and fails to finish schoolwork, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions).
- Often has trouble organizing activities.
- Often avoids, dislikes, or doesn't want to do things that take a lot of mental effort for a long period of time (such as schoolwork or homework).
- Often loses things needed for tasks and activities (such as toys, school assignments, pencils, books, or tools).
- Is often easily distracted.
- Often forgetful in daily activities.
IB. Six or more of the following signs of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for developmental level:
- Hyperactivity:
- Often fidgets with hands or feet or squirms in seat.
- Often gets up from seat when remaining in seat is expected.
- Often runs about or climbs when and where it is not appropriate (adolescents or adults may feel very restless).
- Often has trouble playing or enjoying leisure activities quietly.
- Is often "on the go" or often acts as if "driven by a motor".
- Often talks excessively.
- Impulsiveness:
- Often blurts out answers before questions have been finished.
- Often has trouble waiting one's turn.
- Often interrupts or intrudes on others (example: butts into conversations or games).
II. Some signs that cause impairment were present before age 7 years.
III. Some impairment from the signs is present in two or more settings (such as at school/work and at home).
IV. There must be clear evidence of significant impairment in social, school, or work functioning.
V. The signs do not happen only during the course of a Pervasive Developmental Disorder, Schizophrenia, or other Psychotic Disorder. The signs are not better accounted for by another mental disorder (such as Mood Disorder, Anxiety Disorder, Dissociative Identity Disorder, or a Personality Disorder).
ICD-10
In the tenth edition of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) the signs of ADHD are given the name "Hyperkinetic disorders". When a conduct disorder (as defined by ICD-10) is present, the condition is referred to as "Hyperkinetic conduct disorder". Otherwise the disorder is classified as "Disturbance of Activity and Attention", "Other Hyperkinetic Disorders" or "Hyperkinetic Disorders, Unspecified". The latter is sometimes referred to as, "Hyperkinetic Syndrome".
Other diagnostic guidelines
The American Academy of Pediatrics Clinical Practice Guideline for children with ADHD emphasizes that a reliable diagnosis is dependent upon the fulfillment of three criteria:
- The use of explicit criteria for the diagnosis using the DSM-IV-TR.
- The importance of obtaining information about the child’s signs in more than one setting.
- The search for coexisting conditions that may make the diagnosis more difficult or complicate treatment planning.
All three criteria are determined using the patient's history given by the parents, teachers and/or the patient.
Adults often continue to be impaired by ADHD. Adults with ADHD are diagnosed under the same criteria, including the stipulation that their signs must have been present prior to the age of seven. Adults face some of their greatest challenges in the areas of self-control and self-motivation, as well as executive functioning, usually having more signs of inattention and fewer of hyperactivity or impulsiveness than children do.
Comorbid conditions
Common comorbid conditions include oppositional defiant disorder (ODD). About 20% to 25% of children with ODD meet criteria for a learning disorder. Learning disorders are more common when there are inattention signs.
Comorbid disorders or substance abuse can make the diagnosis and treatment of ADHD more difficult. Psychosocial therapy is useful in treating some comorbid conditions. ADHD is not, in boys, associated with increased substance misuse unless there is comorbid conduct disorder; but "research needs to examine the extent to which ADHD in adulthood increases the risk of substance use disorders."
Depression may also coincide with ADHD, increasingly prevalent among girls and older children.
Epilepsy is a commonly found comorbid disorder in ADHD diagnosed individuals. Some forms of epilepsy can also cause ADHD like behaviour which can be misdiagnosed as ADHD.
Differential diagnoses
To make the diagnosis of ADHD, a number of other possible medical and psychological conditions must be excluded.
Medical conditions
Medical conditions that must be excluded include: hypothyroidism, anemia, lead poisoning, chronic illness, hearing or vision impairment, substance abuse, medication side effects, sleep impairment and child abuse, and cluttering (tachyphemia) among others.
Sleep conditions
As with other psychological and neurological issues, the relationship between ADHD and sleep is complex. In addition to clinical observations, there is substantial empirical evidence from a neuroanatomic standpoint to suggest that there is considerable overlap in the central nervous system centers that regulate sleep and those that regulate attention/arousal. Primary sleep disorders play a role in the clinical presentation of symptoms of inattention and behavioral dysregulation. There are multilevel and bidirectional relationships among sleep, neurobehavioral functioning and the clinical syndrome of ADHD.
Behavioral manifestations of sleepiness in children range from the classic ones (yawning, rubbing eyes), to externalizing behaviors (impulsivity, hyperactivity, aggressiveness), to mood lability and inattentiveness. Many sleep disorders are important causes of symptoms which may overlap with the cardinal symptoms of ADHD; children with ADHD should be regularly and systematically assessed for sleep problems.
From a clinical standpoint, mechanisms that account for the phenomenon of excessive daytime sleepiness include:
- Chronic sleep deprivation, that is insufficient sleep for physiologic sleep needs,
- Fragmented or disrupted sleep, caused by, for example, obstructive sleep apnea (OSA) or periodic limb movement disorder (PLMD),
- Primary clinical disorders of excessive daytime sleepiness, such as narcolepsy and
- Circadian rhythm disorders, such as delayed sleep phase syndrome (DSPS). A study in the Netherlands compared two groups of unmedicated 6-12-year-olds, all of them with "rigorously diagnosed ADHD". 87 of them had problems getting to sleep, 33 had no sleep problems. The larger group had a significantly later dim light melatonin onset (DLMO) than did the children with no sleep problems.
Management
Main article: Attention-deficit hyperactivity disorder managementMethods of treatment often involve some combination of behavior modification, life-style changes, counseling, and medication. A 2005 study found that medical management and behavioral treatment is the most effective ADHD management strategy, followed by medication alone, and then behavioral treatment. While medication has been shown to improve behavior when taken over the short term, they have not been shown to alter long term outcomes.
Behavioral interventions
A 2009 review concluded that the evidence is strong for the effectiveness of behavioral treatments in ADHD.
Psychological therapies used to treat ADHD include psychoeducational input, behavior therapy, cognitive behavioral therapy (CBT), interpersonal psychotherapy (IPT), family therapy, school-based interventions, social skills training and parent management training.
Parent training and education have been found to have short term benefits. Family therapy has shown to be of little use in the treatment of ADHD, though it may be worth noting that parents of children with ADHD are more likely to divorce than parents of children without ADHD, particularly when their children are younger than eight years old.
Several ADHD specific support groups exist as informational sources and to help families cope with challenges associated with dealing with ADHD.
A 2009 study found that children with ADHD move around a lot because it helps them stay alert enough to complete challenging tasks. The researcher advises that when they are doing homework, one should let them fidget, stand or chew gum since it may help them cope. Unless their behavior is destructive, severely limiting their activity could be counterproductive.
Medications
| This article may lend undue weight to certain ideas, incidents, or controversies. Please help improve it by rewriting it in a balanced fashion that contextualizes different points of view. (September 2010) (Learn how and when to remove this message) |
Management with medication was shown to be the most cost-effective, followed by behavioral treatment and combined treatment in a 14 month follow-up study. However, a follow-up study found that stimulant medication offered no benefits over behavioral therapy in children after their respective treatments allocations had been discontinued for two years. Stimulant medication or non-stimulant medication may be prescribed. A 2007 drug class review found that there are no good studies of comparative effectiveness between various drugs for ADHD and that there is a lack of quality evidence on their effects on overall academic performance and social behaviors. ADHD medications are not recommended for preschool children as their long term effects in such young people are unknown. There is very little data on the long-term adverse effects or benefits of stimulants for ADHD.
Stimulant medication

Stimulants are the most commonly prescribed medications for ADHD. The most common stimulant medications are the chain subsitituted amphetamine methylphenidate (Ritalin, Metadate, Concerta), dextroamphetamine (Dexedrine), mixed amphetamine salts (Adderall), dextromethamphetamine (Desoxyn) and lisdexamfetamine (Vyvanse). However, caution needs to be used when prescribing medications that increase levels of "feel-good" neurotransmitters like dopamine, because they can be addictive (see article: amphetamine dependence). According to several studies, use of stimulants (e.g. methylphenidate) can lead to development of drug tolerance to therapeutic doses; tolerance also occurs among high dose abusers of methylphenidate.
Stimulants used to treat ADHD raise the extracellular concentrations of the neurotransmitters dopamine and norepinephrine which causes an increase in neurotransmission. The therapeutic benefits are due to noradrenergic effects at the locus coeruleus and the prefrontal cortex and dopaminergic effects at the nucleus accumbens.
A meta analysis of clinical trials found that about 70% of children improve after being treated with stimulants in the short term but found that this conclusion may be biased due to the high number of low quality clinical trials in the literature. There have been no randomized placebo controlled clinical trials investigating the long term effectiveness of methylphenidate (Ritalin) beyond 4 weeks. Thus the long term effectiveness of methylphenidate has not been scientifically demonstrated. Serious concerns of publication bias regarding the use of methylphenidate for ADHD has also been noted.
Higher rates of schizophrenia and bipolar disorder as well as increased severity of these disorders occur in individuals with a past history of stimulant use for ADHD in childhood. Emergency room visits by children ages 10–14 involving Ritalin intoxication have now reached the same level as those for cocaine which indicates escalating abuse of this highly addictive drug. US and Canada account for a startling 95 percent of worldwide Ritalin consumption. In one study which looked at adult cocaine users, it was found that those individuals who used Ritalin between one and ten years of age had a percentage of cocaine abuse twice that of those who had been diagnosed with ADHD but had not utilized Ritalin.
Both children with and without ADHD abuse stimulants, with ADHD individuals being at the highest risk of abusing or diverting their stimulant prescriptions. Between 16 and 29 percent of students who are prescribed stimulants report diverting their prescriptions. Between 5 and 9 percent of grade/primary and high school children and between 5 and 35 percent of college students have used nonprescribed stimulants. Most often their motivation is to concentrate, improve alertness, "get high," or to experiment.
Although one review indicates that long-term use of methylphenidate has potential for abuse and addiction due to its similar pharmacologically to cocaine and amphetamines, the use of stimulant therapy for ADHD does not increase the risk of subsequent substance abuse and may be protective against it when treatment is started in childhood. However, when stimulant therapy is started during adolescence or adulthood, there is an increased risk of subsequent substance abuse.
One study found that children with ADHD actually need to move more to maintain the required level of alertness while performing tasks that challenge their working memory. Performing math problems mentally and remembering multi-step directions are examples of tasks that require working memory, which involves remembering and manipulating information for a short time. These findings may also explain why stimulant medications improve the behavior of most children with ADHD. Those medications improve the physiological arousal of children with ADHD, increasing their alertness. Previous studies have shown that stimulant medications temporarily improve working memory abilities.
Although "under medical supervision, stimulant medications are considered safe", the use of stimulant medications for the treatment of ADHD has generated controversy because of undesirable side effects, uncertain long term effects and social and ethical issues regarding their use and dispensation. The FDA has added black-box warnings to some ADHD medications, while the American Heart Association and the American Academy of Pediatrics feel that it is prudent to carefully assess children for heart conditions before treating them with stimulant medications.
A novel stimulant drug that has been used to treat ADHD is modafinil. There have been double-blind randomized controlled trials that have demonstrated the efficacy and tolerability of modafinil, however there are risks of serious side effects such as skin reactions and modafinil is not recommended for use in children.
Antipsychotic medication

In an odd contrast with the approved use of stimulant medication as a treatment for children with ADHD, the use of atypical antipsychotic drugs as an off-label treatment has been rising. Antipsychotics work by blocking dopamine, whereas stimulants trigger its release. Atypical antipsychotics have been approved for use in children and teenagers with schizophrenia spectrum disorders and autistic spectrum disorders by the U.S. Food and Drug Administration (FDA) since 1993.
Non-ADHD children do not respond differently to ADHD children when prescribed antipsychotic drugs, which are also increasingly prescribed off-label for children with aggression or defiant behavior. Social pressure to control a child's difficult and disruptive behavior, both at home and at school, may inadvertently change focus from what is in the best interest of the child's wellbeing; to how to render the child more compliant and easier to manage.
Careful approach needs to be taken when blocking dopamine function, which is responsible for the psychological reward system. Excessive blocking of this neurotransmitter can cause dysphoria. This may in turn cause suicidal ideation, or lead some teenagers to compensate for their dopamine deficiency with illicit drugs or alcohol. Atypical antipsychotics are preferred for this reason, because they are less likely to cause movement disorders, dysphoria, and increased drug cravings that have been associated with older typical antipsychotics. Weight gain, diabetes, lactation, gynecomastia, drooling, dysphoria, anhedonia (inability to experience pleasure), fatigue, sexual dysfunction, heart rhythm problems and the possibility of tardive dyskinesia, an irreversible movement disorder, are among the adverse events associated with antipsychotic drugs.
Other non-stimulant medications
Atomoxetine (Strattera) and Guanfacine (Intuniv) are the only non-stimulant drugs approved for the treatment of ADHD. Other medications which may be prescribed off-label include α2A adrenergic receptor agonists such as clonidine, certain antidepressants such as tricyclic antidepressants, SNRIs, SSRIs or MAOIs.
Prognosis
Children diagnosed with ADHD have significant difficulties in adolescence, regardless of treatment. In the United States, 37% of those with ADHD do not get a high school diploma even though many of them will receive special education services. A 1995 briefing citing a 1994 book review says the combined outcomes of the expulsion and dropout rates indicate that almost half of all ADHD students never finish high school. Also in the US, less than 5% of individuals with ADHD get a college degree compared to 28% of the general population. Those with ADHD as children are at increased risk of a number of adverse life outcomes once they become teenagers. These include a greater risk of auto crashes, injury and higher medical expenses, earlier sexual activity, and teen pregnancy. Russell Barkley states that adult ADHD impairments affect "education, occupation, social relationships, sexual activities, dating and marriage, parenting and offspring psychological morbidity, crime and drug abuse, health and related lifestyles, financial management, or driving. ADHD can be found to produce diverse and serious impairments". The proportion of children meeting the diagnostic criteria for ADHD drops by about 50% over three years after the diagnosis. This occurs regardless of the treatments used and also occurs in untreated children with ADHD. ADHD persists into adulthood in about 30-50% of cases. Those affected are likely to develop coping mechanisms as they mature, thus compensating for their previous ADHD.
Epidemiology
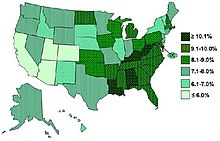
ADHD's global prevalence is estimated at 3-5% in people under the age of 19. There is, however, both geographical and local variability among studies. Geographically, children in North America appear to have a higher rate of ADHD than children in Africa and the Middle East, well published studies have found rates of ADHD as low as 2% and as high as 14% among school aged children. The rates of diagnosis and treatment of ADHD are also much higher on the East Coast of the USA than on the West Coast. The frequency of the diagnosis differs between male children (10%) and female children (4%) in the United States. This difference between genders may reflect either a difference in susceptibility or that females with ADHD are less likely to be diagnosed than males.
Rates of ADHD diagnosis and treatment have increased in both the UK and the USA since the 1970s. In the UK an estimated 0.5 per 1,000 children had ADHD in the 1970s, while 3 per 1,000 received ADHD medications in the late 1990s. In the USA in the 1970s 12 per 1,000 children had the diagnosis, while in the late 1990s 34 per 1,000 had the diagnosis and the numbers continue to increase.
Adults are likely not to be diagnosed or treated for ADHD. This may result in a substantial underestimation of prevalence in most populations. Awareness about Hyperactivity and ADHD or its signs and symptoms has been rudimentary until early 1990 across Europe.
In the UK in 2003 a prevalence of 3.6% is reported in male children and less than 1% is reported in female children.
As of 2009, eight percent of all Major League Baseball players have been diagnosed with ADHD, making the disorder epidemic among this population. The increase coincided with the League's 2006 ban on stimulants (q.v. Major League Baseball drug policy).
History
Main article: History of attention-deficit hyperactivity disorderHyperactivity has long been part of the human condition. Sir Alexander Crichton describes "mental restlessness" in his book An Inquiry Into the Nature and Origin of Mental Derangement written in 1798. The terminology used to describe the symptoms of ADHD has gone through many changes over history including: "minimal brain damage", "minimal brain dysfunction" (or disorder), "learning/behavioral disabilities" and "hyperactivity". In the DSM-II (1968) it was the "Hyperkinetic Reaction of Childhood". In the DSM-III "ADD (Attention-Deficit Disorder) with or without hyperactivity" was introduced. In 1987 this was changed to ADHD in the DSM-III-R and subsequent editions. The use of stimulants to treat ADHD was first described in 1937.
Society and culture
See also: List of people diagnosed with attention-deficit hyperactivity disorderThe media have reported on many issues related to ADHD. In 2001 PBS's Frontline aired a one-hour program about the effects of the diagnosis and treatment of ADHD in minors, entitled "Medicating Kids." The program included a selection of interviews with representatives of various points of view. In one segment, entitled Backlash, retired neurologist Fred Baughman and Peter Breggin whom PBS described as "outspoken critics who insist a fraud perpetrated by the psychiatric and pharmaceutical industries on families anxious to understand their children's behavior" were interviewed on the legitimacy of the disorder. Russell Barkley and Xavier Castellanos, then head of ADHD research at the National Institute of Mental Health (NIMH), defended the viability of the disorder. In the interview with Castellanos, he stated that little is scientifically understood. Lawrence Diller was interviewed on the business of ADHD along with a representative from Shire Plc.
A number of notable individuals have given controversial opinions on ADHD. Scientologist Tom Cruise's interview with Matt Lauer was widely watched by the public. In this interview he spoke about postpartum depression and also referred to Ritalin and Adderall as being "street drugs" rather than as ADHD medication. In England Baroness Susan Greenfield, a leading neuroscientist, spoke out publicly about the need for a wide-ranging inquiry in the House of Lords into the dramatic increase in the diagnosis of ADHD in the UK and possible causes following a 2007 BBC Panorama programme which highlighted US research (The Multimodal Treatment Study of Children with ADHD by the University of Buffalo showing treatment results of 600) suggesting drugs are no better than other forms of therapy for ADHD in the long term.
Controversies
Main article: Attention-deficit hyperactivity disorder controversiesADHD and its diagnosis and treatment have been considered controversial since the 1970s. The controversies have involved clinicians, teachers, policymakers, parents and the media. Opinions regarding ADHD range from not believing it exists at all to believing there are genetic and physiological bases for the condition as well as disagreement about the use of stimulant medications in treatment. Most healthcare providers accept that ADHD is a genuine disorder with debate in the scientific community centering mainly around how it is diagnosed and treated.
Others have included that it may stem from a misunderstanding of the diagnostic criteria and how they are utilized by clinicians, teachers, policymakers, parents and the media. Debates center around: whether ADHD is a disability or whether it is merely a neurological description, the cause of the disorder, the changing of the diagnostic criteria, and the rapid increase in diagnosis of ADHD and the use of stimulants to treat the disorder. Some do not believe it exists at all. Long term possible side effects of stimulants and their usefulness are largely unknown because of a lack of long term studies. Some research raises questions about the long term effectiveness and side effects of medications used to treat ADHD.
In 1998, the US National Institutes of Health (NIH) released a consensus statement on the diagnosis and treatment of ADHD. The statement, while recognizing that stimulant treatment is controversial, supports the validity of the ADHD diagnosis and the efficacy of stimulant treatment. It found controversy only in the lack of sufficient data on long-term use of medications, and in the need for more research in many areas.
Stimulants legal status was recently reviewed by several international organizations:
- Internationally, methylphenidate is a Schedule II drug under the Convention on Psychotropic Substances.
- In the United States, methylphenidate is classified as a Schedule II controlled substance, the designation used for substances that have a recognized medical value but present a high likelihood for abuse because of their addictive potential.
- In the United Kingdom, methylphenidate is a controlled 'Class B' substance, and possession without prescription is illegal, with a sentence up to 14 years and/or an unlimited fine.
- In New Zealand, it is a 'class B2 controlled substance'. unlawful possession is punishable by 6 month prison sentence and distribution of it is punishable by a 14 year sentence.
The British Psychological Society said in a 1997 report that physicians and psychiatrists should not follow the American example of applying medical labels to such a wide variety of attention-related disorders: "The idea that children who don’t attend or who don’t sit still in school have a mental disorder is not entertained by most British clinicians." However, several years later, in 2009, the British Psychological Society, in collaboration with the Royal College of Psychiatrists, released a set of guidelines for the diagnosis and treatment of ADHD.
With a "wide variation in diagnosis across states, races, and ethnicities" some investigators suspect that factors other than neurological conditions play a role when the diagnosis of ADHD is made. Two studies published in 2010 suggest that the diagnosis is more likely to be made in the younger children within a grade; the authors propose that such a misdiagnosis of ADHD within a grade may be due to different states of maturity and may lead to potentially inappropriate treatment.
References
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington DC.
- NINDS Attention Deficit-Hyperactivity Disorder Information Page. National Institute of Neurological Disorders and Stroke (NINDS/NIH) February 9, 2007. Retrieved on 2007-08-13.
- Zwi M, Ramchandani P, Joughin C (2000). "Evidence and belief in ADHD". BMJ. 321 (7267): 975–6. doi:10.1136/bmj.321.7267.975. PMC 1118810. PMID 11039942.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Biederman J (1998). "Attention-deficit/hyperactivity disorder: a life-span perspective". The Journal of Clinical Psychiatry. 59 Suppl 7: 4–16. PMID 9680048.
- "NIMH • ADHD • Complete Publication". Archived from the original on 2007-10-18.
- Nair J, Ehimare U, Beitman BD, Nair SS, Lavin A (2006). "Clinical review: evidence-based diagnosis and treatment of ADHD in children". Mo Med. 103 (6): 617–21. PMID 17256270.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Rader R, McCauley L, Callen EC (2009). "Current strategies in the diagnosis and treatment of childhood attention-deficit/hyperactivity disorder". Am Fam Physician. 79 (8): 657–65. PMID 19405409.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Van Cleave J, Leslie LK (2008). "Approaching ADHD as a chronic condition: implications for long-term adherence". Journal of Psychosocial Nursing and Mental Health Services. 46 (8): 28–37. PMID 18777966.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bálint S, Czobor P, Mészáros A, Simon V, Bitter I (2008). "". Psychiatr Hung (in Hungarian). 23 (5): 324–35. PMID 19129549.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Elia J, Ambrosini PJ, Rapoport JL (1999). "Treatment of attention-deficit-hyperactivity disorder". The New England Journal of Medicine. 340 (10): 780–8. doi:10.1056/NEJM199903113401007. PMID 10072414.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gentile, Julie (2004). "Adult ADHD: Diagnosis, Differential Diagnosis and Medication Management". Psychiatry. 3 (8): 24–30.
{{cite journal}}: Cite has empty unknown parameters:|month=and|coauthors=(help) - Barkley, Russell A. (2007). "ADHD in Adults: History, Diagnosis, and Impairments". ContinuingEdCourses.net. Retrieved July 27, 2009.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - Dulcan M (1997). "Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. American Academy of Child and Adolescent Psychiatry". Journal of the American Academy of Child and Adolescent Psychiatry. 36 (10 Suppl): 85S–121S. doi:10.1097/00004583-199710001-00007. PMID 9334567.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Singh I (2008). "Beyond polemics: science and ethics of ADHD". Nature Reviews. Neuroscience. 9 (12): 957–64. doi:10.1038/nrn2514. PMID 19020513.
{{cite journal}}: Unknown parameter|month=ignored (help) - Sciutto, M.J., Nolfi, C.J., & Bluhm, C. (2004). Effects of Child Gender and Symptom Type on Referrals for ADHD by Elementary School Teachers. Journal of Emotional and Behavioral Disorders, 12(4), 247-253.
- ^ Ramsay, J. Russell. Cognitive Behavioral Therapy for Adult ADHD. Routledge, 2007. ISBN 0-415-95501-7
- ^ Parrillo, Vincent (2008). Encyclopedia of Social Problems. SAGE. p. 63. ISBN 9781412941655. Retrieved 2009-05-02.
- ^ "Treatment of Attention-Deficit/Hyperactivity Disorder". US department of health and human services. 1999. Retrieved 2008-10-02.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Mayes R, Bagwell C, Erkulwater J (2008). "ADHD and the rise in stimulant use among children". Harv Rev Psychiatry. 16 (3): 151–66. doi:10.1080/10673220802167782. PMID 18569037.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cohen, Donald J.; Cicchetti, Dante (2006). Developmental psychopathology. Chichester: John Wiley & Sons. ISBN 0-471-23737-X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Sim MG, Hulse G, Khong E (2004). "When the child with ADHD grows up" (PDF). Aust Fam Physician. 33 (8): 615–8. PMID 15373378.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Silver, Larry B. Attention-deficit/hyperactivity disorder. American Psychiatric Publishing, Inc.; 3 edition (September 2003) ISBN 1-58562-131-5; Online July 20, 2009
- ^ Schonwald A, Lechner E (2006). "Attention deficit/hyperactivity disorder: complexities and controversies". Curr. Opin. Pediatr. 18 (2): 189–95. doi:10.1097/01.mop.0000193302.70882.70. PMID 16601502.
{{cite journal}}: Unknown parameter|month=ignored (help) - Goldman LS, Genel M, Bezman RJ, Slanetz PJ (1998). "Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Council on Scientific Affairs, American Medical Association". JAMA. 279 (14): 1100–7. PMID 9546570.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "CG72 Attention deficit hyperactivity disorder (ADHD): full guideline" (PDF). NHS. 24 September 2008. Retrieved 2008-10-08.
- "Brain Matures A Few Years Late In ADHD, But Follows Normal Pattern". Sciencedaily.com. 2007-11-13. Retrieved 2009-05-25.
- Wiener, Jerry M., Editor (2003). Textbook Of Child & Adolescent Psychiatry. Washington, DC: American Psychiatric Association. ISBN 1-58562-057-2.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - DSM-IV-TR workgroup. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association.
- ^ American Academy of Child Adolescent Psychiatry. "ADHD - A Guide for Families." June 27, 2009. http://www.aacap.org/cs/adhd_a_guide_for_families/what_is_adhd
- ^ http://www.webmd.com/add-adhd/guide/adhd-adults
- ^ Tom, Catherine M. (2005-01-15). "Recognizing and Treating ADHD in Adolescents and Adults". uspharmacist.com. Retrieved 2009-05-25.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Gentile, Julie. "Adult ADHD: Diagnosis, Differential Diagnosis, and Medication Management". 3 (8). Psychiatrymmc.com. Retrieved 2009-05-25.
{{cite journal}}: Cite journal requires|journal=(help) - ^ https://health.google.com/health/ref/Attention+deficit+hyperactivity+disorder+(ADHD)
- ^ "Attention Deficit Hyperactivity Disorder (ADHD)." Health & Outreach. Publications. http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/complete-index.shtml July 15, 2009
- Brewis, Alexandra; Schmidt, Karen L.; Meyer, Mary (2000-12). "ADHD-Type Behavior and Harmful Dysfunction in Childhood: A Cross-Cultural Model". American Anthropologist. 102 (4): 826. doi:10.1525/aa.2000.102.4.823.
{{cite journal}}:|access-date=requires|url=(help); Check date values in:|date=(help) - http://www.herbalfreak.com/medical-condition/ailments/attention-deficit-hyperactivity-disorder/2009/12/
- ^
- "UCF study: Hyperactivity enables children with ADHD to stay alert".
- Rapport MD, Bolden J, Kofler MJ, Sarver DE, Raiker JS, Alderson RM (2009). "Hyperactivity in boys with attention-deficit/hyperactivity disorder (ADHD): a ubiquitous core symptom or manifestation of working memory deficits?". J Abnorm Child Psychol. 37 (4): 521–34. doi:10.1007/s10802-008-9287-8. PMID 19083090.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
- ^ Brunsvold GL, Oepen G (2008). "Comorbid Depression in ADHD: Children and Adolescents". Psychiatric Times. 25 (10).
- ^ Krull, K.R. (December 5, 2007). "Evaluation and diagnosis of attention deficit hyperactivity disorder in children" (Subscription required). Uptodate. Retrieved 2008-09-12.
- PMID 19428109
- Philipsen A (2006). "Differential diagnosis and comorbidity of attention-deficit/hyperactivity disorder (ADHD) and borderline personality disorder (BPD) in adults". European Archives of Psychiatry and Clinical Neuroscience. 256 Suppl 1: i42–6. doi:10.1007/s00406-006-1006-2. PMID 16977551.
{{cite journal}}: Unknown parameter|month=ignored (help) - Bauermeister, J., Shrout, P., Chávez, L., Rubio-Stipec, M., Ramírez, R., Padilla, L., et al. (2007, August). ADHD and gender: are risks and sequela of ADHD the same for boys and girls?. Journal of Child Psychology & Psychiatry, 48(8), 831-839. Retrieved February 17, 2009, doi:10.1111/j.1469-7610.2007.01750.x
- Bauermeister, J., Shrout, P., Chávez, L., Rubio-Stipec, M., Ramírez, R., Padilla, L., et al. (2007, August). ADHD and gender: are risks and sequela of ADHD the same for boys and girls?. Journal of Child Psychology & Psychiatry, 48(8), 831-839.
- Bailly, Lionel (2005). "Stimulant medication for the treatment of attention-deficit hyperactivity disorder: evidence-b(i)ased practice?" (Full text). Psychiatric Bulletin. 29 (8). The Royal College of Psychiatrists: 284–287. doi:10.1192/pb.29.8.284.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - Barkley, Russel A. "Attention-Deficit/Hyperactivity Disorder: Nature, Course, Outcomes, and Comorbidity". Retrieved 2006-06-26.
- Volkow, ND; Wang, GJ; Kollins, SH; Wigal, TL; Newcorn, JH; Telang, F; Fowler, JS; Zhu, W; Logan, J (2009). "Evaluating Dopamine Reward Pathway in ADHD". JAMA. 302 (10): 1084–1091. doi:10.1001/jama.2009.1308. PMID 19738093.
{{cite journal}}: More than one of|author=and|last1=specified (help) - Roman T, Rohde LA, Hutz MH. (2004). "Polymorphisms of the dopamine transporter gene: influence on response to methylphenidate in attention deficit-hyperactivity disorder." American Journal of Pharmacogenomics 4(2):83–92 PMID 15059031
- ^ Swanson JM, Flodman P, Kennedy J, et al. "Dopamine Genes and ADHD." Neurosci Biobehav Rev. 2000 Jan;24(1):21–5. PMID 10654656
- Smith KM, Daly M, Fischer M, et al. "Association of the dopamine beta hydroxylase gene with attention deficit hyperactivity disorder: genetic analysis of the Milwaukee longitudinal study." Am J Med Genet B Neuropsychiatr Genet. 2003 May 15;119(1):77–85. PMID 12707943
- Acosta, MT; Arcos-Burgos, M; Muenke, M (2004). "Attention deficit/hyperactivity disorder (ADHD): Complex phenotype, simple genotype?". Genetics in Medicine. 6 (1): 1–15. doi:10.1097/01.GIM.0000110413.07490.0B. PMID 14726804.
{{cite journal}}: More than one of|author=and|last1=specified (help) - Arcos-Burgos M, Acosta MT (2007). "Tuning major gene variants conditioning human behavior: the anachronism of ADHD". Curr. Opin. Genet. Dev. 17 (3): 234–8. doi:10.1016/j.gde.2007.04.011. PMID 17467976.
{{cite journal}}: Unknown parameter|month=ignored (help) - Hartmann, Thom (2003). The Edison gene: ADHD and the gift of the hunter child. Rochester, Vt: Park Street Press. ISBN 0-89281-128-5.
- Williams J, Taylor E (2006). "The evolution of hyperactivity, impulsivity and cognitive diversity". J R Soc Interface. 3 (8): 399–413. doi:10.1098/rsif.2005.0102. PMC 1578754. PMID 16849269.
{{cite journal}}: Unknown parameter|month=ignored (help) - Levy et al., 1997
- Nigg, 2006
- Sherman, Silberg et al., 1996
- Sherman DK, Iacono WG, McGue MK (1997). "Attention-deficit hyperactivity disorder dimensions: a twin study of inattention and impulsivity-hyperactivity". Journal of the American Academy of Child and Adolescent Psychiatry. 36 (6): 745–53. doi:10.1097/00004583-199706000-00010. PMID 9183128.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Braun JM, Kahn RS, Froehlich T, Auinger P, Lanphear BP (2006). "Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children". Environ. Health Perspect. 114 (12): 1904–9. doi:10.1289/ehp.10274. PMC 1764142. PMID 17185283.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Bad behaviour 'linked to smoking'". BBC. 31 July 2005. Retrieved 2008-12-30.
- "Ability To Quit Smoking May Depend On ADHD Symptoms, Researchers Find". Science Daily. 24 November 2008. Retrieved 2008-12-30.
- "Prenatal Smoking Increases ADHD Risk In Some Children". Science Daily. 11 April 2007. Retrieved 2008-12-30.
- "ADHD 'linked to premature birth'". BBC. 4 June 2006. Retrieved 2008-12-30.
- Keenan HT, Hall GC, Marshall SW (2008). "Early head injury and attention deficit hyperactivity disorder: retrospective cohort study;". BMJ. 337: a1984. doi:10.1136/bmj.a1984. PMC 2590885. PMID 18988644.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Mental Health: A report of the surgeon general". 1999. Retrieved 2008-09-15.
- Millichap JG (2008). "Etiologic classification of attention-deficit/hyperactivity disorder". Pediatrics. 121 (2): e358–65. doi:10.1542/peds.2007-1332. PMID 18245408.
{{cite journal}}: Unknown parameter|month=ignored (help) - Millichap JG. Attention Deficit Hyperactivity Disorder Handbook: A Physician’s Guide to ADHD. New York: Springer-Verlag, 2010
- Study Links Organophosphate Insecticide Used on Corn With ADHD. Beyond Pesticides. 5 January 2007.
- Klein, Sarah. Study: ADHD linked to pesticide exposure. CNN. 17 May 2010.
- Maugh II, Thomas H. (2010-05-16). "Study links pesticide to ADHD in children". The Los Angeles Times.
- McCann D, Barrett A, Cooper A (2007). "Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomized, double-blinded, placebo-controlled trial". Lancet. 370 (9598): 1560–7. doi:10.1016/S0140-6736(07)61306-3. PMID 17825405.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - U.S. Food and Drug Administration
- U.S. Food and Drug Administration
- "www.euro.who.int" (PDF).
- Template:PDFlink
- Adam James (2004) Clinical psychology publishes critique of ADHD diagnosis and use of medication on children published on Psychminded.co.uk Psychminded Ltd
- Cuffe, S.P.; McCullough, Elizabeth L.; Pumariega, Andres J. (1994). "Comorbidity of attention Deficit Hyperactivity Disorder and Post-Traumatic Stress Disorder". Journal of Child and Family Studies. 3 (3): 327–336. doi:10.1007/BF02234689.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Sensory integration disorder". healthatoz.com. 2006-08-14. Retrieved 2008-12-30.
- Park, Madison (14 April 2010). / "Adopted children at greater risk for mental health disorders". CNN.com. Retrieved 24 May 2010.
{{cite web}}: Check|url=value (help) - Rethinking ADHD
- Bailey, Eileen (2007-11-23). "ADHD and Creativity". Healthcentral.com. Retrieved 2009-05-25.
- Susan Smalley (2008). "Reframing ADHD in the Genomic Era". Psychiatric Times. 25 (7).
- Parens E, Johnston J (2009). "Facts, values, and Attention-Deficit Hyperactivity Disorder (ADHD): an update on the controversies". Child Adolesc Psychiatry Ment Health. 3 (1): 1. doi:10.1186/1753-2000-3-1. PMC 2637252. PMID 19152690.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Chriss, James J. (2007). Social control: an introduction. Cambridge, UK: Polity. p. 230. ISBN 0-7456-3858-9.
- Szasz, Thomas Stephen (2001). Pharmacracy: medicine and politics in America. New York: Praeger. p. 212. ISBN 0-275-97196-1.
- ^ "Attention Deficit Hyperactivity Disorder is a neurologically based disorder". Incrediblehorizons.com. Retrieved 2009-05-25.
- "ADHD". Sci.csuhayward.edu. Retrieved 2009-05-25.
- Sikström S, Söderlund G (2007). "Stimulus-dependent dopamine release in attention-deficit/hyperactivity disorder". Psychol Rev. 114 (4): 1047–75. doi:10.1037/0033-295X.114.4.1047. PMID 17907872.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Evaluation and diagnosis of attention deficit hyperactivity disorder in children". December 5, 2007. Retrieved 2008-09-15.
- Krain, Amy; Castellanos, FX (2006). "Brain development and ADHD". Clinical Psychology Review. 26 (4): 433–444. doi:10.1016/j.cpr.2006.01.005. PMID 16480802.
{{cite journal}}:|access-date=requires|url=(help); Cite has empty unknown parameter:|month=(help); More than one of|first1=and|first=specified (help); More than one of|last1=and|last=specified (help) - "MerckMedicus Modules: ADHD - Pathophysiology".
- Bush G, Valera EM, Seidman LJ (2005). "Functional neuroimaging of attention-deficit/hyperactivity disorder: a review and suggested future directions". Biological Psychiatry. 57 (11): 1273–84. doi:10.1016/j.biopsych.2005.01.034. PMID 15949999.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Brain Matures a Few Years Late in ADHD, But Follows Normal Pattern NIMH Press Release, November 12, 2007
- Joshi SV; Adam, H. M. (2002). "ADHD, growth deficits, and relationships to psychostimulant use". Pediatrics in Review. 23 (2): 67–8, discussion 67–8. doi:10.1542/pir.23-2-67. PMID 11826259.
{{cite journal}}: Unknown parameter|month=ignored (help) - Gene Predicts Better Outcome as Cortex Normalizes in Teens with ADHD NIMH Press Release, August 6, 2007
- Lou HC, Andresen J, Steinberg B, McLaughlin T, Friberg L. "The striatum in a putative cerebral network activated by verbal awareness in normals and in ADHD children." Eur J Neurol. 1998 Jan;5(1):67–74. PMID 10210814
- Dougherty DD, Bonab AA, Spencer TJ, Rauch SL, Madras BK, Fischman AJ (1999). "Dopamine transporter density in patients with attention deficit hyperactivity disorder". Lancet. 354 (9196): 2132–-33. doi:10.1016/S0140-6736(99)04030-1. PMID 10609822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Dresel SH, Kung MP, Plössl K, Meegalla SK, Kung HF (1998). "Pharmacological effects of dopaminergic drugs on in vivo binding of TRODAT-1 to the central dopamine transporters in rats". European journal of nuclear medicine. 25 (1): 31–9. PMID 9396872.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Coccaro EF, Hirsch SL, Stein MA (2007). "Plasma homovanillic acid correlates inversely with history of learning problems in healthy volunteer and personality disordered subjects". Psychiatry research. 149 (1–3): 297–302. doi:10.1016/j.psychres.2006.05.009. PMID 17113158.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - http://www.npr.org/templates/story/story.php?storyId=112752252
- "The Role of Dopamine and Norepinephrine in Depression".
- "The Chemistry of Depression".
- Zametkin AJ, Nordahl TE, Gross M (1990). "Cerebral glucose metabolism in adults with hyperactivity of childhood onset". N. Engl. J. Med. 323 (20): 1361–6. doi:10.1056/NEJM199011153232001. PMID 2233902.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Matochik JA, Liebenauer LL, King AC, Szymanski HV, Cohen RM, Zametkin AJ (1994). "Cerebral glucose metabolism in adults with attention deficit hyperactivity disorder after chronic stimulant treatment". Am J Psychiatry. 151 (5): 658–64. PMID 8166305.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Zametkin AJ, Liebenauer LL, Fitzgerald GA (1993). "Brain metabolism in teenagers with attention-deficit hyperactivity disorder". Arch. Gen. Psychiatry. 50 (5): 333–40. PMID 8489322.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ernst M, Cohen RM, Liebenauer LL, Jons PH, Zametkin AJ (1997). "Cerebral glucose metabolism in adolescent girls with attention-deficit/hyperactivity disorder". J Am Acad Child Adolesc Psychiatry. 36 (10): 1399–406. doi:10.1097/00004583-199710000-00022. PMID 9334553.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Armstrong, Thomas (1999). Add/Adhd Alternatives in the Classroom. ASCD. pp. 3–5. ISBN 9780871203595. Retrieved 2009-05-02.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - Ernst M, Liebenauer LL, King AC, Fitzgerald GA, Cohen RM, Zametkin AJ (1994). "Reduced brain metabolism in hyperactive girls". J Am Acad Child Adolesc Psychiatry. 33 (6): 858–68. doi:10.1097/00004583-199407000-00012. PMID 8083143.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Díaz-Heijtz R, Mulas F, Forssberg H (2006). "[Alterations in the pattern of dopaminergic markers in attention-deficit/hyperactivity disorder]". Revista De Neurologia (in Spanish). 42 Suppl 2: S19–23. PMID 16555214.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Philip Shaw, MD; Jason Lerch, PhD; Deanna Greenstein, PhD; Wendy Sharp, MSW; Liv Clasen, PhD; Alan Evans, PhD; Jay Giedd, MD; F. Xavier Castellanos, MD; Judith Rapoport, MD (2006). "Longitudinal Mapping of Cortical Thickness and Clinical Outcome in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder". Arch Gen Psychiatry. 5 (63): 540–549. doi:10.1001/archpsyc.63.5.540. PMID 16651511.
- ^ David Cohen (2004). "An Update on ADHD Neuroimaging Research" (PDF). The Journal of Mind and Behavior. 25 (2). The Institute of Mind and Behavior, Inc: 161–166. ISSN 0271–0137. Retrieved 2009-05-25.
{{cite journal}}: Check|issn=value (help) - David Cohen (2003). "Broken brains or flawed studies? A critical review of ADHD neuroimaging studies". The Journal of Mind and Behavior. 24: 29–56.
- Joughin C, Ramchandani P, Zwi M (2003). "Attention-deficit/hyperactivity disorder". American Family Physician. 67 (9): 1969–70. PMID 12751659.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Schneider H, Eisenberg D (2006). "Who receives a diagnosis of attention-deficit/ hyperactivity disorder in the United States elementary school population?". Pediatrics. 117 (4): e601–9. doi:10.1542/peds.2005-1308. PMID 16585277.
{{cite journal}}: Unknown parameter|month=ignored (help) - http://www.adhd.org.au/
- http://www.psychnet-uk.com/dsm_iv/attention_deficit_disorder.htm
- ^ ICD Version 2006: F91. World Health Organization. Retrieved on December 11, 2006.
- ^ American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder and Committee on Quality Improvement (2001). "Clinical practice guideline: treatment of the school-aged child with attention-deficit/hyperactivity disorder". Pediatrics. 108 (4): 1033–44. doi:10.1542/peds.108.4.1033. PMID 11581465.
{{cite journal}}: Unknown parameter|month=ignored (help) - "PsychiatryOnline".
- Medscape.com (subscription required)
- Pliszka SR (2000). "Patterns of psychiatric comorbidity with attention-deficit/hyperactivity disorder". Child and Adolescent Psychiatric Clinics of North America. 9 (3): 525–40, vii. PMID 10944655.
{{cite journal}}: Unknown parameter|month=ignored (help) - Lamminmäky T (1995). "Attention deficit hyperactivity disorder subtypes: Are there differences in academic problems?". Dev neuropsychology (11): 297–310.
- Foster EM, Jensen PS, Schlander M; et al. (2007). "Treatment for ADHD: is more complex treatment cost-effective for more complex cases?". Health Services Research. 42 (1 Pt 1): 165–82. doi:10.1111/j.1475-6773.2006.00599.x. PMC 1955245. PMID 17355587.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Lynskey MT, Hall W (2001). "Attention deficit hyperactivity disorder and substance use disorders: Is there a causal link?". Addiction. 96 (6): 815–22. doi:10.1080/09652140020050988. PMID 11399213.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help) - Tan M, Appleton R (2005). "Attention deficit and hyperactivity disorder, methylphenidate, and epilepsy". Archives of Disease in Childhood. 90 (1): 57–9. doi:10.1136/adc.2003.048504. PMC 1720074. PMID 15613514.
{{cite journal}}: Unknown parameter|month=ignored (help) - Aldenkamp AP, Arzimanoglou A, Reijs R, Van Mil S (2006). "Optimizing therapy of seizures in children and adolescents with ADHD". Neurology. 67 (12 Suppl 4): S49–51. PMID 17190923.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Smucker WD, Hedayat M (2001). "Evaluation and treatment of ADHD". American Family Physician. 64 (5): 817–29. PMID 11563573.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Owens JA (2005). "The ADHD and sleep conundrum: a review". Journal of Developmental and Behavioral Pediatrics. 26 (4): 312–22. doi:10.1097/00004703-200508000-00011. PMID 16100507.
{{cite journal}}: Unknown parameter|month=ignored (help) - Owens JA (2008). "Sleep disorders and attention-deficit/hyperactivity disorder". Current Psychiatry Reports. 10 (5): 439–44. doi:10.1007/s11920-008-0070-x. PMID 18803919.
{{cite journal}}: Unknown parameter|month=ignored (help) - Golan N, Shahar E, Ravid S, Pillar G (2004). "Sleep disorders and daytime sleepiness in children with attention-deficit/hyperactive disorder". Sleep. 27 (2): 261–6. PMID 15124720.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hirshkowitz, Max (2004). "Neuropsychiatric Aspects of Sleep and Sleep Disorders". In Yudofsky, Stuart C. and Robert E. Hales, editors (ed.). Essentials of neuropsychiatry and clinical neurosciences (4 ed.). Arlington, Virginia, USA: American Psychiatric Publishing. pp. 315–40. ISBN 978-1-58562-005-0.
{{cite book}}:|access-date=requires|url=(help);|editor=has generic name (help);|format=requires|url=(help); Cite has empty unknown parameters:|origmonth=,|month=,|origdate=, and|coauthors=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)CS1 maint: multiple names: editors list (link) - Walters AS, Silvestri R, Zucconi M, Chandrashekariah R, Konofal E (2008). "Review of the possible relationship and hypothetical links between attention deficit hyperactivity disorder (ADHD) and the simple sleep related movement disorders, parasomnias, hypersomnias, and circadian rhythm disorders". Journal of Clinical Sleep Medicine. 4 (6): 591–600. PMC 2603539. PMID 19110891.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Van der Heijden KB, Smits MG, Van Someren EJ, Gunning WB (2005). "Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder". Chronobiology International. 22 (3): 559–70. doi:10.1081/CBI-200062410. PMID 16076654.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jensen PS, Garcia JA, Glied S (2005). "Cost-effectiveness of ADHD treatments: findings from the multimodal treatment study of children with ADHD". The American Journal of Psychiatry. 162 (9): 1628–36. doi:10.1176/appi.ajp.162.9.1628. PMID 16135621.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Yamada A, Takeuchi H, Miki H, Touge T, Deguchi K (1990). "". Rinshō Shinkeigaku (in Japanese). 30 (7): 784–6. PMID 2242635.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, O'Connor BC (2009). "A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder". Clinical Psychology Review. 29 (2): 129–40. doi:10.1016/j.cpr.2008.11.001. PMID 19131150.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Pliszka S; AACAP Work Group on Quality Issues (2007). "Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (7): 894–921. doi:10.1097/chi.0b013e318054e724. PMID 17581453.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Family therapy for attention-deficit disorder or attention-deficit/hyperactivity disorder in children and adolescents". The Cochrane Collaboration. April 20, 2005. Retrieved 2008-09-19.
- Wymbs BT, Pelham WE, Molina BS, Gnagy EM, Wilson TK, Greenhouse JB (2008). "Rate and predictors of divorce among parents of youths with ADHD". Journal of Consulting and Clinical Psychology. 76 (5): 735–44. doi:10.1037/a0012719. PMC 2631569. PMID 18837591.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jensen PS, Arnold LE, Swanson JM (2007). "3-year follow-up of the NIMH MTA study". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (8): 989–1002. doi:10.1097/CHI.0b013e3180686d48. PMID 17667478.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - McDonagh MS, Peterson K, Dana T, Thakurta S. (2007). Drug Class Review on Pharmacologic Treatments for ADHD. Results.
- Greenhill LL, Posner K, Vaughan BS, Kratochvil CJ (2008). "Attention deficit hyperactivity disorder in preschool children". Child and Adolescent Psychiatric Clinics of North America. 17 (2): 347–66, ix. doi:10.1016/j.chc.2007.11.004. PMID 18295150.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ King S, Griffin S, Hodges Z (2006). "A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents". Health Technology Assessment. 10 (23): iii–iv, xiii–146. PMID 16796929.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Stephen V. Faraone, P. (2003, September 18). Retrieved from Medscape Today: Medscape.com
- Sulzer D, Sonders MS, Poulsen NW, Galli A (2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Progress in Neurobiology. 75 (6): 406–33. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - National Toxicology, Program (2005). "NTP-CERHR monograph on the potential human reproductive and developmental effects of amphetamines". Ntp Cerhr Mon (16): vii–III1. PMID 16130031.
{{cite journal}}: Unknown parameter|month=ignored (help) - Howland RH (2008). "Lisdexamfetamine: a prodrug stimulant for ADHD". Journal of Psychosocial Nursing and Mental Health Services. 46 (8): 19–22. PMID 18777964.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Ritalin Abuse, Addiction and Treatment".
- "Dopamine".
- "Treatment of ADHD When Tolerance to Methylphenidate Develops".
- "Acute tolerance to methylphenidate in the treatment of attention deficit hyperactivity disorder in children".
- "Methylphenidate".
- Solanto MV (1998). "Neuropsychopharmacological mechanisms of stimulant drug action in attention-deficit hyperactivity disorder: a review and integration". Behavioural Brain Research. 94 (1): 127–52. doi:10.1016/S0166-4328(97)00175-7. PMID 9708845.
{{cite journal}}: Unknown parameter|month=ignored (help) - Schachter HM, Pham B, King J, Langford S, Moher D (2001). "How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis". CMAJ. 165 (11): 1475–88. PMC 81663. PMID 11762571.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ross RG (2006). "Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder". The American Journal of Psychiatry. 163 (7): 1149–52. doi:10.1176/appi.ajp.163.7.1149. PMID 16816217.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Ritalin Addiction".
- "The truth about North America's greatest drug problem: Ritalin".
- Wilens TE, Adler LA, Adams J (2008). "Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature". Journal of the American Academy of Child and Adolescent Psychiatry. 47 (1): 21–31. doi:10.1097/chi.0b013e31815a56f1. PMID 18174822.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Lerner M, Wigal T. Long-term safety of stimulant medications used to treat children with ADHD. Pediatr Ann. 2008 Jan;37(1):37-45.
- Zhu J, Reith ME (2008). "Role of the dopamine transporter in the action of psychostimulants, nicotine, and other drugs of abuse". CNS & Neurological Disorders Drug Targets. 7 (5): 393–409. doi:10.2174/187152708786927877. PMID 19128199.
{{cite journal}}: Unknown parameter|month=ignored (help) - Faraone SV, Wilens T (2003). "Does stimulant treatment lead to substance use disorders?". J Clin Psychiatry. 64 Suppl 11: 9–13. PMID 14529324.
- Faraone SV, Wilens TE (2007). "Effect of stimulant medications for attention-deficit/hyperactivity disorder on later substance use and the potential for stimulant misuse, abuse, and diversion". J Clin Psychiatry. 68 Suppl 11: 15–22. PMID 18307377.
- "NIMH · ADHD · The Treatment of ADHD".
- Stern HP, Stern TP (2002). "When children with attention-deficit/hyperactivity disorder become adults". South. Med. J. 95 (9): 985–91. PMID 12356139.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|month=ignored (help) - Murphy, Kevin R.; Barkley, Russell A. (2005). Attention-Deficit Hyperactivity Disorder, Third Edition : A Clinical Workbook. New York: The Guilford Press. ISBN 1-59385-227-4.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "What is the evidence for using CNS stimulants to treat ADHD in children? | Therapeutics Initiative".
- Lerner M, Wigal T (2008). "Long-term safety of stimulant medications used to treat children with ADHD". Pediatric annals. 37 (1): 37–45. doi:10.3928/00904481-20080101-11. PMID 18240852.
{{cite journal}}: Unknown parameter|month=ignored (help) - "FDA News". FDA. February 21, 2007. Retrieved 2009-08-14.
- "Drugs with Black Box Warnings - Comprehensive List". FormWeb. Joyce Generali. 05-04-2009. Retrieved 2009-05-19.
{{cite web}}: Check date values in:|date=(help) - American Academy of Pediatrics/American Heart Association (2008). "American Academy of Pediatrics/American Heart Association clarification of statement on cardiovascular evaluation and monitoring of children and adolescents with heart disease receiving medications for ADHD: May 16, 2008". Journal of Developmental and Behavioral Pediatrics. 29 (4): 335. doi:10.1097/DBP.0b013e31318185dc14. PMID 18698199.
{{cite journal}}: Unknown parameter|month=ignored (help) - Biederman J, Swanson JM, Wigal SB, Boellner SW, Earl CQ, Lopez FA (2006). "A comparison of once-daily and divided doses of modafinil in children with attention-deficit/hyperactivity disorder: a randomized, double-blind, and placebo-controlled study". The Journal of Clinical Psychiatry. 67 (5): 727–35. doi:10.4088/JCP.v67n0506. PMID 16841622.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Greenhill LL, Biederman J, Boellner SW (2006). "A randomized, double-blind, placebo-controlled study of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 45 (5): 503–11. doi:10.1097/01.chi.0000205709.63571.c9. PMID 16601402.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Modavigil Product Information". Retrieved 2008-07-02.
- Pharmalot - Florida Medicaid To Review Antipsychotics & ADHD
- "Atypical Antipsychotics for Treatment of Schizophrenia Spectrum Disorders".
- Physicians Postgraduate Press, Inc., Dosing of Atypical Antipsychotics in Children and Adolescents
- Department of Public Health, Guidelines for the use of atypical antipsychotics in adults
- Stein MA (2004). "Innovations in attention-deficit/hyperactivity disorder pharmacotherapy: long-acting stimulant and nonstimulant treatments". The American Journal of Managed Care. 10 (4 Suppl): S89–98. PMID 15352535.
{{cite journal}}: Unknown parameter|month=ignored (help) - Christman AK, Fermo JD, Markowitz JS (2004). "Atomoxetine, a novel treatment for attention-deficit-hyperactivity disorder". Pharmacotherapy. 24 (8): 1020–36. doi:10.1592/phco.24.11.1020.36146. PMID 15338851.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hazell P (2005). "Do adrenergically active drugs have a role in the first-line treatment of attention-deficit/hyperactivity disorder?". Expert Opinion on Pharmacotherapy. 6 (12): 1989–98. doi:10.1517/14656566.6.12.1989. PMID 16197353.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Atomoxetine (marketed as Strattera) Information". Retrieved 12 July 2009.
- Molina BS, Hinshaw SP, Swanson JM (2009). "The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study". Journal of the American Academy of Child and Adolescent Psychiatry. 48 (5): 484–500. doi:10.1097/CHI.0b013e31819c23d0. PMID 19318991.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Attention-Deficit/Hyperactivity Disorder: Nature, Course, Outcomes, and Comorbidity". Barkley, Russell. Retrieved 2008-09-19.
- Template:PDFlink
- Cimera, Robert (2002). Making ADHD a gift: teaching Superman how to fly. Lanham, Maryland: Scarecrow Press, Inc. p. 116. ISBN 0810843188. Retrieved 2009-05-02.
- College Degree Nearly Doubles Annual Earnings, Census Bureau Reports U.S. Census Bureau March 28, 2005. Retrieved on 2008-08-02.
- ContinuingEdCourses.net
- ContinuingEdCourses.net
- "CDC - ADHD, Prevalence - NCBDDD".
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007). "The worldwide prevalence of ADHD: a systematic review and metaregression analysis". The American Journal of Psychiatry. 164 (6): 942–8. doi:10.1176/appi.ajp.164.6.942. PMID 17541055.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "LONI: Laboratory of Neuro Imaging". Retrieved 2008-09-19.
- "ADHD Home".
- "CDC.gov" (PDF).
- Staller J, Faraone SV (2006). "Attention-deficit hyperactivity disorder in girls: epidemiology and management". CNS Drugs. 20 (2): 107–23. doi:10.2165/00023210-200620020-00003. PMID 16478287.
- NICE 2008 Pg. 134
- Saletan, William (2009-01-12). "Doping Deficit Disorder. Need performance-enhancing drugs? Claim ADHD". Slate. Retrieved 2009-05-02.
- An Early Description of ADHD (Inattentive Subtype): Dr Alexander Crichton and `Mental Restlessness' (1798) Child and Adolescent Mental Health, Volume 6, Number 2, May 2001 , pp. 66–73(8)
- p 271, An inquiry into the nature and origin of mental derangement: comprehending a concise system of the physiology and pathology of the human mind and a history of the passions and their effects.
- Bland, J.,(2002) About Gender: Testosterone and Aggression - Childhood. http://www.gender.org.uk/about/06encrn/63gaggrs.htm
- "Development of the DSM". Kadi.myweb.uga.edu. Retrieved 2009-05-25.
- Patrick KS, Straughn AB, Perkins JS, González MA (2009). "Evolution of stimulants to treat ADHD: transdermal methylphenidate". Human Psychopharmacology. 24 (1): 1–17. doi:10.1002/hup.992. PMC 2629554. PMID 19051222.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Defining and Diagnosing ADHD". PBS. Retrieved 2009-05-25.
- "Opponents and Backlash". PBS. Retrieved 2009-05-25.
- Castellanos, Xavier (2000-10-10). "Interviews: Xavier Castellanos, M.D." (Interview). Retrieved 2009-05-25.
{{cite interview}}: Unknown parameter|program=ignored (help) - "'I'm passionate about life'". msnbc.msn.com. Retrieved 2008-12-30.
- "Health | Peer calls for ADHD care review". BBC News. 2007-11-14. Retrieved 2009-05-25.
- "Baroness Susan Greenfield". Brunel.ac.uk. Retrieved 2009-05-25.
- Foreman DM (2006). "Attention deficit hyperactivity disorder: legal and ethical aspects". Archives of Disease in Childhood. 91 (2): 192–4. doi:10.1136/adc.2004.064576. PMC 2082674. PMID 16428370.
{{cite journal}}: Unknown parameter|month=ignored (help) - "Controversies Surrounding ADHD - (ADHD) Attention Deficit Hyperactivity Disorder Cause, Diagnosis, History".
- Ashton H, Gallagher P, Moore B (2006). "The adult psychiatrist's dilemma: psychostimulant use in attention deficit/hyperactivity disorder". J. Psychopharmacol. (Oxford). 20 (5): 602–10. doi:10.1177/0269881106061710. PMID 16478756.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Lakhan SE, Hagger-Johnson GE (2007). "The impact of prescribed psychotropics on youth". Clin Pract Epidemol Ment Health. 3: 21. doi:10.1186/1745-0179-3-21. PMC 2100041. PMID 17949504.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - National Institutes of Health (NIH) | title=Diagnosis and Treatment of Attention Deficit Hyperactivity Disorder (ADHD). NIH Consensus Statement 1998 Nov 16Ð18; 16(2): 1Ð37.
- Template:PDFlink 23rd edition. August 2003. International Narcotics Board, Vienna International Centre. Retrieved 2 March 2006
- http://www.homeoffice.gov.uk/drugs/drugs-law/Class-a-b-c/
- Reason R; Working Party of the British Psychological Society (1999). "ADHD: a psychological response to an evolving concept. (Report of a Working Party of the British Psychological Society)". Journal of Learning Disabilities. 32 (1): 85–91. doi:10.1177/002221949903200108. PMID 15499890.
- Encyclopedia - Britannica Online Encyclopedia
- Nice.org.uk, National Institute for Clinical Excellence (NICE)
- ^ Elder TE (2010). "The importance of relative standards in ADHD diagnoses: Evidence based on exact birth dates". J Health Econ. 2010 Jun 17. 29 (5): 641–56. doi:10.1016/j.jhealeco.2010.06.003. PMC 2933294. PMID 20638739.
- ^ Evans WN, Morrill MS, Parente ST (2010). "Measuring inappropriate medical diagnosis and treatment in survey data: The case of ADHD among school-age children". J Health Econ. 2010 Aug 4. 29 (5): 657–73. doi:10.1016/j.jhealeco.2010.07.005. PMID 20739076.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
Bibliography
- Dr Jennifer Erkulwater; Dr Rick Mayes; Dr Catherine Bagwell (2009). Medicating Children: ADHD and Pediatric Mental Health. Cambridge: Harvard University Press. p. 5. ISBN 0-674-03163-6.
{{cite book}}: CS1 maint: multiple names: authors list (link)
Further reading
- Barkley, Russell A. Take Charge of ADHD: The Complete Authoritative Guide for Parents (2005) New York: Guilford Publications.
- Conrad, Peter Identifying Hyperactive Children (Ashgate, 2006).
- Crawford, Teresa I'm Not Stupid! I'm ADHD!
- Faraone, Stephen V. (2005). The scientific foundation for understanding attention-deficit/hyperactivity disorder as a valid psychiatric disorder. Eur Child Adolesc Psychiatry 14, 1-10.
- Faraone, Stephen, V.Straight Talk about Your Child's Mental Health: What to Do When Something Seems Wrong (2003) New York:Guilford Press
- Green, Christopher, Kit Chee, Understanding ADD; Doubleday 1994; ISBN 0-86824-587-9
- Hanna, Mohab. (2006) Making the Connection: A Parent's Guide to Medication in ADHD, Washington D.C.: Ladner-Drysdale.
- Hartmann, Thom (2003). The Edison gene: ADHD and the gift of the hunter child. Rochester, Vt: Park Street Press. ISBN 0-89281-128-5.
- Mate, Gabor. Scattered Minds: A New Look at the Origins and Healing of Attention Deficit Disorder. Vintage Canada (1999). ISBN-10: 0676972594
- Matlen, Terry. (2005) "Survival Tips for Women with AD/HD". ISBN 1-886941-59-9
- Mellor, Nigel ADHD or Attention Seeking? Ways of Distinguishing Two Common Childhood Problems (2008)
- Millichap, J. Gordon, MD, FRCP Attention Deficit Hyperactivity Disorder Handbook: A Physician’s Guide to ADHD. New York: Springer, 2010 ISBN: 978-1441913968
- Ninivaggi, F.J. "Attention-Deficit/Hyperactivity Disorder in Children and Adolescents: Rethinking Diagnosis and Treatment Implications for Complicated Cases", Connecticut Medicine. September 1999; Vol. 63, No. 9, 515-521. PMID 10531701
- Southall, Angela (2007). The Other Side of ADHD:Attention Deficit Hyperactivity Disorder Exposed and Explained. Radcliffe Publishing Ltd. ISBN 1846190681. Retrieved 2009-05-02.
- Mohammed M. Alqahtani. The Comorbidity of ADHD in the General Population of Saudi Arabian School-Age Children. J Atten Disord. 2009 Oct 22.DOI:10.1177/1087054709347195.
- Mohammed M.J. Alqahtani. Attention-deficit hyperactive disorder in school-aged children in Saudi Arabia. Eur J Pediatr. 2010 Mar 27. DOI 10.1007/s00431-010-1190-y
Adult ADHD
- Kelly, Kate, Peggy Ramundo. (1993) You Mean I'm Not Lazy, Stupid or Crazy?! A Self-Help Book for Adults with Attention deficit Disorder. ISBN 0-684-81531-1
- Mate, Gabor. Scattered: How Attention Deficit Disorder Originates And What You Can Do About It. Plume (August 1, 2000). ISBN-10: 0452279631
- Ratey, Nancy. (2008) The Disorganized Mind: Coaching Your ADHD Brain to Take Control of Your Time, Tasks, and Talents. ISBN 0-312-35533-5
- Sarkis, Stephanie. (2006) 10 Simple Solutions to Adult ADD: How to Overcome Chronic Distraction & Accomplish Your Goals. ISBN 1-57224-434-8
- Weiss, Lynn. (2005) Attention Deficit Disorder in Adults, 4th Edition: A Different Way of Thinking ISBN 1-58979-237-8
External links
- National Institute of Mental Health on ADHD
- "CG72 Attention deficit hyperactivity disorder (ADHD): full guideline" (PDF). NHS. 09 March 2009. Retrieved 2009-01-08.
{{cite web}}: Check date values in:|date=(help) - New Zealand MOH Guidelines for the Assessment and Treatment of Attention-Deficit/Hyperactivity Disorder
- Functional Disconnection Identified Between Key Brain Areas in Children With ADHD
- Hellenic Society for the Study of ADHD
| Attention deficit hyperactivity disorder (ADHD) | |
|---|---|
| Main articles |
|
| Sub-types | |
| Medications |
|
| Related or outdated topics | |
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| Emotional and behavioral disorders | |
|---|---|
| Emotional/behavioral |
|
- Articles needing the year an event occurred from September 2010
- Misplaced Pages neutral point of view disputes from September 2010
- Attention
- Attention disorders
- Childhood psychiatric disorders
- Educational psychology
- Neurological disorders
- Attention-deficit hyperactivity disorder
- Emotional and behavioral disorders in childhood and adolescence