This is an old revision of this page, as edited by Forgottenfaces (talk | contribs) at 14:12, 2 February 2012 (it's only asserted that misused therapies such as hypnosis can cause alters - not that hypnosis itself would cause it, only improper use of hypnosis (for example). Changed the wording to reflect that.). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 14:12, 2 February 2012 by Forgottenfaces (talk | contribs) (it's only asserted that misused therapies such as hypnosis can cause alters - not that hypnosis itself would cause it, only improper use of hypnosis (for example). Changed the wording to reflect that.)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)| The accessibility of this article is in question. Relevant discussion may be found on the talk page. (February 2012) |
| The neutrality of this article is disputed. Relevant discussion may be found on the talk page. Please do not remove this message until conditions to do so are met. (January 2012) (Learn how and when to remove this message) |
| Dissociative identity disorder | |
|---|---|
| Specialty | Psychiatry, psychology |
| Frequency | 1.5% (United States of America) |
Dissociative identity disorder (DID, also known as multiple personality disorder in the ICD-10) is a psychiatric diagnosis whose essential feature, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM), "...is the presence of two or more distinct identities or personality states...that recurrently take control of behavior." The diagnosis requires that at least two personalities (one may be the host) routinely take control of the individual's behavior with an associated memory loss that goes beyond normal forgetfulness; in addition, symptoms cannot be the temporary effects of drug use or a general medical condition. Memory loss will occur in those with DID when an alternate part of the personality becomes dominant. DID is less common than other dissociative disorders, occurring in approximately 1% of dissociative cases, and diagnosis is often difficult as there is considerable comorbidity with other conditions and many symptoms overlap with other types of mental illness. It is diagnosed significantly more frequently in North America than in the rest of the world.
Individuals diagnosed with DID frequently report severe physical and sexual abuse as a child. The etiology of DID has been attributed to the experience of pathological levels of stress which disrupts normal functioning and forces some memories, thoughts and aspects of personality from consciousness, though some assert that multiple personalities are the product of certain misguided or misused psychological therapies, and the debate between the two positions is characterised by passionate disagreement.
Signs and symptoms
The Diagnostic and Statistical Manual of Mental Disorderscriteria for DID include the presence of two or more distinct identities or personality states, at least two of which take control of the individual's behavior on a recurrent basis, accompanied by inability to recall personal information beyond what is expected through normal forgetfulness. The diagnosis excludes symptoms caused by alcohol, drugs, medications or other medical conditions such as complex partial seizures and normal fantasy play in children.
Individuals diagnosed with DID demonstrate a variety of symptoms, with wide fluctuations across time. Daily functioning can vary from severely impaired, to normal, to a high level of functionality. Symptoms can include:
- Disruption of identity characterized by two or more distinct personality states
- Multiple mannerisms, attitudes and beliefs
- Pseudoseizures or other conversion symptoms
- Somatic symptoms that vary across identities
- Distortion or loss of subjective time (a long time)
- Current memory loss of everyday events
- Depersonalization
- Derealization
- Depression
- Flashbacks of abuse/trauma
- Sudden anger without a justified cause
- Frequent panic/anxiety attacks
- Unexplainable phobias
Patients may experience a broad array of other symptoms that may appear to resemble epilepsy, schizophrenia, anxiety disorders, mood disorders, posttraumatic stress disorder, personality disorders, and eating disorders. Individuals diagnosed with DID tend to be highly hypnotizable and dissociate easily.
Despite research on DID including structural and functional magnetic resonance imaging, positron emission tomography, single-photon emission computed tomography, event-related potential and electroencephalography, no convergent neuroimaging findings have been identified regarding DID making it difficult to hypothesize a biological basis for DID. In addition, many of the studies that do exist were performed from an explicitly trauma-based position, and did not consider the possibility of iatrogenic induction of DID. Studies have shown differences between cerebral blood flow and changes in visual parameters between alters, as well as support for amnesia between alters. There is no research to date regarding the neuroimaging and introduction of false memories in DID patients.
Causes
This disorder is theoretically linked with the interaction of overwhelming stress, traumatic antecedents, insufficient childhood nurturing and the innate ability of children in general to dissociate memories or experiences from consciousness. A high percentage of patients report child abuse others report an early loss, serious medical illness or other traumatic events. People diagnosed with DID often report that they have experienced severe physical and sexual abuse, especially during early to mid childhood. Several psychiatric rating scales of DID sufferers suggested that DID is strongly related to childhood trauma rather than to an underlying electrophysiological dysfunction.
Within the first six years of life young children are still developing a personality structure that allows integrative functioning. Early childhood trauma interferes with the the development of integrative functions (childhood trauma related dissociation). Repeated activation of trauma-related dissociative states (while the myelin in the hippocampus is still being formed) conditions the brain to function state-dependently (dissociative identities).
Developmental trauma
Severe sexual, physical, or psychological trauma in childhood by a primary caregiver has been proposed as an explanation for the development of DID. In this theory, awareness, memories and feelings of a harmful action or event caused by the caregiver is pushed into the subconscious and dissociation becomes a coping mechanism for the individual during times of stress. These memories and feelings are later experienced as a separate entity, and if this happens multiple times, multiple alters are created.
Iatrogenesis
Symptoms of DID may be created iatrogenically by therapists using techniques to "recover" memories with suggestible patients, but this idea is not universally accepted. The characteristics of patients diagnosed with DID (hypnotizability, suggestibility, frequent fantasization and mental absorption) contributed to these concerns and concerns regarding the validity of recovered memories. Skeptics have suggested that a small subset of doctors are responsible for diagnosing the majority of individuals with DID. Psychologist Nicholas Spanos and others skeptical of the condition have suggested that in addition to iatrogenesis, DID may be the result of role-playing rather than separate personalities, though others disagree, pointing to a lack of incentive to manufacture or maintain separate personalities and point to the claimed histories of abuse of these patients.
The iatrogenic position is strongly linked to ideas about false memories. There is little consensus between the iatrogenic and traumagenic positions regarding DID and debates are both passionate and diametrically opposed.
Diagnosis
The diagnosis of dissociative identity disorder is defined by criteria in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM-II used the term multiple personality disorder, the DSM-III grouped the diagnosis with the other four major dissociative disorders, and the DSM-IV-TR categorizes it as dissociative identity disorder. Dissociation is recognized as a symptomatic presentation in response to psychological trauma, extreme emotional stress, and, as noted, in association with emotional dysregulation and borderline personality disorder. The ICD-10 continues to list the condition as multiple personality disorder.
The diagnostic criteria in section 300.14 (dissociative disorders) of the DSM-IV require that an adult, for non-physiological reasons, be recurrently controlled by multiple discrete identity or personality states while also suffering extensive memory lapses. While otherwise similar, the diagnostic criteria for children requires also ruling out fantasy. Diagnosis is normally performed by a therapist, psychiatrist or psychologist clinically trained in the specific material who may use specially designed interviews (such as the SCID-D) and personality assessment tools to evaluate a person for a dissociative disorder. The psychiatric history of individuals diagnosed with DID frequently but not always contains multiple previous diagnoses of various mental disorders and treatment failures. Subjectivity in terms like personality, ego-state, identity and amnesia grants a certain degree of subjectivity to diagnosis. The diagnosis has been criticized, researchers Piper and Merskey described it as a culture-bound and often iatrogenic condition which they believe is in decline.
The proposed diagnostic criteria for DID in the DSM-5 is:
- Disruption of identity characterized by two or more distinct personality states (one can be the host) or an experience of possession, as evidenced by discontinuities in sense of self, cognition, behavior, affect, perceptions, and/or memories. This disruption may be observed by others, or reported by the patient.
- Inability to recall important personal information, for everyday events or traumatic events, that is inconsistent with ordinary forgetfulness.
- Causes clinically significant distress and impairment in social, occupational, or other important areas of functioning.
- The disturbance is not a normal part of a broadly accepted cultural or religious practice and is not due to the direct physiological effects of a substance (e.g., blackouts or chaotic behavior during alcohol intoxication) or a general medical condition (e.g., complex partial seizures). NOTE: In children, the symptoms are not attributable to imaginary playmates or other fantasy play.
These specifiers are under consideration:
a) With pseudoseizures or other conversion symptoms
b) With somatic symptoms that vary across identities
The proposed Criterion C is intended to "help differentiate normative cultural experiences from psychopathology." This phrase, which occurs in several other diagnostic criteria, is proposed for inclusion in 300.14 as part of a proposed merger of dissociative trance disorder with DID. For example, professionals would be able to take shamanism, which involves voluntary possession trance states, into consideration, and not have to diagnose those who report it as having a mental disorder.
Screening
Perhaps due to their rarity, the dissociative disorders including DID was not initially included in the Structured Clinical Interview for DSM-IV (SCID), designed to make psychiatric diagnoses more rigorous and reliable. Instead, shortly after the publication of the initial SCID a freestanding protocol for dissociative disorders (SCID-D) was published. This interview takes about 30 to 90 minutes depending on the subject's experiences. An alternative diagnostic instrument, the Dissociative Disorders Interview Schedule, also exists but the SCID-D is generally considered superior. The Dissociative Disorders Interview Schedule (DDIS) is a highly structured interview that discriminates among various DSM-IV diagnoses. The DDIS can usually be administered in 30–45 minutes.
Other questionnaires include the Dissociative Experiences Scale (DES), Perceptual Alterations Scale, Questionnaire on Experiences of Dissociation, Dissociation Questionnaire and the Mini-SCIDD. All are strongly intercorrelated and except the Mini-SCIDD, all incorporate absorption, a normal part of personality involving narrowing or broadening of attention. The DES is a simple, quick, and validated questionnaire that has been widely used to screen for dissociative symptoms, with variations for children and adolescents. Tests such as the DES provide a quick method of screening subjects so that the more time-consuming structured clinical interview can be used in the group with high DES scores. Depending on where the cutoff is set, people who would subsequently be diagnosed can be missed. An early recommended cutoff was 15-20. The reliability of the DES in non-clinical samples has been questioned.
Differential diagnoses
Due to overlap between symptoms, differential diagnosis between DID and a variety of other conditions (including schizophrenia, psychosis, normal and rapid-cycling bipolar disorder, anxiety disorders, somatization and personality disorders) can be complicated as delusions or auditory hallucinations can be mistaken for speech by other personalities and vice-versa, or sudden behavior changes being attributed to sudden mood fluctuations. Persistence and consistency of identities and behavior, amnesia, measures of dissociation or hypnotizability and reports from family members or other associates indicating a history of such changes can help distinguish DID from other conditions. A diagnosis of DID takes precedence over any other dissociative disorders. Distinguishing true DID from malingering is a concern when financial or legal gains are an issue, and factitious disorder may also be considered if there patient has a history or pattern help or attention seeking. Individuals who state that their symptoms are due to external spirits or entities entering their bodies are generally diagnosed with dissociative disorder not otherwise specified rather than DID due to the lack of internal personalities or alter states.
Conditions which may be present with similar symptoms include borderline personality disorder, and the dissociative conditions of dissociative amnesia and dissociative fugue. The clearest distinction is the lack of discrete formed personalities in these conditions. Individuals with schizophrenia will have some form of delusions, hallucinations or thought disorder. The condition is thought to be under-diagnosed due to skepticism and lack of awareness from mental health professionals, made difficult due to the lack of specific and reliable criteria for diagnosing DID as well as a lack of prevalence rates due to the failure to examine systematically selected and representative populations.
Treatment
There is a general lack of consensus in the diagnosis and treatment of DID. Treatment methods may include psychotherapy and medications for comorbid disorders and medications may also be used to treat specific symptoms. Treatment of DID is phase-oriented. The first phase focuses on symptoms and relieving the distressing aspects of the condition and ensuring the safety of the individual. The second phase focuses on stepwise exposure to traumatic memories and prevention of re-dissociation. The third phase focuses on reconnecting the identities of disparate alters into a single functioning identity with all its memories and experiences intact. Some behavior therapists initially use behavioral treatments such as only responding to a single identity, and using more traditional therapy once a consistent response is established.
Brief treatment due to managed care may be difficult, as individuals diagnosed with DID may have unusually difficulties in trusting their therapist or fear rejection and lengthy, regular contact (weekly or biweekly) is more common. Different alters may appear based on their greater ability to deal with specific situational stresses or threats, and some cognitive behavioral therapy strategies involve learning coping strategies other than transitioning between alters. While some patients may initially present with a large number of alters these number of alters may reduce during treatment, though it is considered important for the therapist to become familiar with at lesat the more prominent personality states as the "host" personality may not be the "true" identity of the patient. Specific alters may react negatively to therapy, fearing the therapists goal is to eliminate the alter (particularly those associated with illegal or violent activities). A more appropriate goal of treatment would be to integrate adaptive responses to abuse, injury or other threats into the overall personality structure.
Prognosis
DID does not resolve spontaneously, and symptoms vary over time. Individuals with primarily dissociative symptoms and features of post traumatic stress disorder normally recover with treatment. Those with comorbid addictions, personality, mood, or eating disorders face a longer, slower, and more complicated recovery process. Individuals still attached to abusers face the poorest prognosis; treatment may be long-term and consist solely of symptom relief rather than personality integration. Changes in identity, loss of memory, and awaking in unexplained locations and situations often leads to chaotic personal lives. Individuals with the condition commonly attempt suicide.
Epidemiology
The DSM does not provide an estimate of incidence for DID and dissociative disorders were excluded from the Epidemiological Catchment Area Project. As a result, there are no national statistics for incidence and prevalence of DID in the United States. Initially DID along with the rest of the dissociative disorders were considered the rarest of psychological conditions, numbering less than 100 by 1944, with only one further case added in the next two decades. In the late 1970s and 80s, the number of diagnoses rose sharply. Accompanying this rise was an increase in the number of alters, rising from only the primary and one alter personality in most cases, to an average of 13 in the mid-1980s (the increase in both number of cases and number of alters within each case are both factors in professional skepticism regarding the diagnosis). A possible explanation for the increase in incidence and prevalence of DID over time is that the condition was misdiagnosed as schizophrenia, bipolar disorder, or other such disorders in the past; another explanation is that an increase in awareness of DID and child sexual abuse has led to earlier, more accurate diagnosis. Others explain the increase as being due to the use of inappropriate therapeutic techniques in highly suggestible individuals, though this is itself controversial. Figures from psychiatric populations (inpatients and outpatients) show a wide diversity from different countries:
| Country | Prevalence in mentally ill populations | Source study |
|---|---|---|
| India | 0.015% | Chiku et al. (1989) |
| Switzerland | 0.05 - 0.1% | Modestin (1992) |
| China | 0.4% | Xiao et al. (2006) |
| Germany | 0.9% | Gast et al. (2001) |
| Netherlands | 2% | Friedl & Draijer (2000) |
| United States | 10% | Bliss & Jeppsen (1985) |
| United States | 6 - 8% | Ross et al. (1992) |
| United States | 6 - 10% | Foote et al. (2006) |
| Turkey | 14% | Sar et al. (2007) |
| Israel | 0.8% | Ginzburg et al. (2010) |
Figures from the general population show less diversity:
| Country | Prevalence | Source study |
|---|---|---|
| Canada | 1% | Ross (1991) |
| Turkey (male) | 0.4% | Akyuz et al. (1999) |
| Turkey (female) | 1.1% | Sar et al. (2007) |
Over-representation in North America
DID is a controversial diagnosis and condition, with much of the literature on DID still being generated and published in North America, to the extent that it was once regarded as a phenomenon confined to that continent though research has appeared discussing the appearance of DID in other countries and cultures. In a 1996 review, Joel Paris offered three possible causes for the sudden increase in people diagnosed with DID:
- The result of therapist suggestions to suggestible people, much as Charcot's hysterics acted in accordance with his expectations.
- Psychiatrists' past failure to recognize dissociation being redressed by new training and knowledge.
- Dissociative phenomena are actually increasing, but this increase only represents a new form of an old and protean entity: "hysteria".
Paris believes that the first possible cause is the most likely.
The debate over the validity of this condition, whether as a clinical diagnosis, a symptomatic presentation, a subjective misrepresentation on the part of the patient, or a case of unconscious collusion on the part of the patient and the professional is considerable. There are several main points of disagreement over the diagnosis.
One of the primary reasons for the ongoing recategorization of this condition is that there were once so few documented cases (research in 1944 showed only 76) of what was once referred to as multiple personality.
Comorbidity
Conditions frequently comorbid with DID include:
- bipolar disorder
- major depressive disorder
- posttraumatic stress disorder
- anxiety disorder
- somatization
- personality disorders
- psychotic disorder
In addition, higher incidences of substance abuse and eating disorders are found in individuals with a diagnosis of DID.
History

Before the 19th century, people exhibiting symptoms similar to those were believed to be possessed. The first case of DID was thought to be described by Paraclesus in 1646.
An intense interest in spiritualism, parapsychology, and hypnosis continued throughout the 19th and early 20th centuries, running in parallel with John Locke's views that there was an association of ideas requiring the coexistence of feelings with awareness of the feelings. Hypnosis, which was pioneered in the late 18th century by Franz Mesmer and Armand-Marie Jacques de Chastenet, Marques de Puységur, challenged Locke's association of ideas. Hypnotists reported what they thought were second personalities emerging during hypnosis and wondered how two minds could coexist.
The 19th century saw a number of reported cases of multiple personalities which Rieber estimated would be close to 100. Epilepsy was seen as a factor in some cases, and discussion of this connection continues into the present era.
By the late 19th century there was a general acceptance that emotionally traumatic experiences could cause long-term disorders which might display a variety of symptoms. These conversion disorders were found to occur in even the most resilient individuals, but with profound effect in someone with emotional instability like Louis Vivé (1863-?) who suffered a traumatic experience as a 13 year-old when he encountered a viper. Vivé was the subject of countless medical papers and became the most studied case of dissociation in the 19th century.
Between 1880 and 1920, many great international medical conferences devoted a lot of time to sessions on dissociation. It was in this climate that Jean-Martin Charcot introduced his ideas of the impact of nervous shocks as a cause for a variety of neurological conditions. One of Charcot's students, Pierre Janet, took these ideas and went on to develop his own theories of dissociation. One of the first individuals diagnosed with multiple personalities to be scientifically studied was Clara Norton Fowler, under the pseudonym Christine Beauchamp; American neurologist Morton Prince studied Fowler between 1898 and 1904, describing her case study in his 1906 monograph, Dissociation of a Personality.
In the early 20th century interest in dissociation and multiple personalities waned for a number of reasons. After Charcot's death in 1893, many of his so-called hysterical patients were exposed as frauds, and Janet's association with Charcot tarnished his theories of dissociation. Sigmund Freud recanted his earlier emphasis on dissociation and childhood trauma.

In 1910, Eugen Bleuler introduced the term schizophrenia to replace dementia praecox. A review of the Index medicus from 1903 through 1978 showed a dramatic decline in the number of reports of multiple personality after the diagnosis of schizophrenia became popular, especially in the United States. A number of factors helped create a large climate of skepticism and disbelief; paralleling the increased suspicion of DID was the decline of interest in dissociation as a laboratory and clinical phenomenon.
Starting in about 1927, there was a large increase in the number of reported cases of schizophrenia, which was matched by an equally large decrease in the number of multiple personality reports. Bleuler also included multiple personality in his category of schizophrenia. It was concluded in the 1980s that DID patients are often misdiagnosed as suffering from schizophrenia.
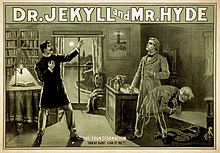
The public, however, was exposed to psychological ideas which took their interest. Mary Shelley's Frankenstein, Robert Louis Stevenson's Strange Case of Dr Jekyll and Mr Hyde, and many short stories by Edgar Allan Poe had a formidable impact. In 1957, with the publication of the book The Three Faces of Eve and the popular movie which followed it, the American public's interest in multiple personality was revived. During the 1970s an initially small number of clinicians campaigned to have it considered a legitimate diagnosis.
Between 1968 and 1980 the term that was used for dissocative identity disorder was "Hysterical neurosis, dissociative type". The APA wrote in the second edition of the DSM: "In the dissociative type, alterations may occur in the patient's state of consciousness or in his identity, to produce such symptoms as amnesia, somnambulism, fugue, and multiple personality." The number of cases sharply increased in the late 1970s and throughout the 80s, and the first scholarly monographs on the topic appeared in 1986.
In 1974 the highly influential book Sybil was published, and later made into a miniseries in 1976 and again in 2007. Describing what Robert Rieber called “the third most famous of multiple personality cases”, it presented a detailed discussion of the problems of treatment of “Sybil”, a pseudonym for Shirley Ardell Mason. Though the book and subsequent films helped popularize the diagnosis, later analysis of the case suggested different interpretations, ranging from Mason’s problems being iatrogenically induced through therapeutic methods or an inadvertent hoax due in part to the lucrative publishing rights, though this conclusions has itself been challenged.
With the publication of the DSM-III, which omitted the terms "hysteria" and "neurosis" (and thus the former categories for dissociative disorders), dissociative diagnoses became "orphans" with their own categories with dissociative identity disorder appearing as "multiple personality disorder". In the opinion of McGill University psychiatrist Joel Paris, this inadvertently legitimized them by forcing textbooks, which mimicked the structure of the DSM, to include a separate chapter on them and resulted in an increase in diagnosis of dissociative conditions. Once a rarely-occurring spontaneous phenomena, became "an artifact of bad (or naïve) psychotherapy" as patients capable of dissociating were accidentally encouraged to express their symptoms by "overly fascinated" therapists.
"Interpersonality amnesia" was removed as a diagnostic feature from the DSM III in 1987, which may have contributed to the increasing frequency of the diagnosis. There were 200 reported cases of DID as of 1980, and 20,000 from 1980 to 1990. Joan Acocella reports that 40,000 cases were diagnosed from 1985 to 1995. Scientific publications regarding DID peaked in the mid-1990s then rapidly declined.
In 1994, the fourth edition of the DSM replaced the criteria again and changed the name of the condition from "multiple personality disorder" to the current "dissociative identity disorder" to emphasize the importance of changes to consciousness and identity rather than personality. The inclusion of interpersonality amnesia helped to distinguish DID from dissociative disorder not otherwise specified, but the condition retains an inherent subjectivity due to difficulty in defining terms such as personality, identity, ego-state and even amnesia. The ICD-10 still classifies DID as a "Dissociative disorder" and retains the name "multiple personality disorder" with the classification number of F44.8.81.
Society and culture
Despite its rareness, DID is portrayed with remarkable frequency in popular culture, producing or appearing in numerous books, films and television shows.
Within legal circles, DID has been described as one of the most disputed psychiatric diagnoses and forensic assessments. The number of court cases involving DID has increased substantially since the 1990s. There are two main hypothesis for the etiology of DID, traumatic and iatrogenic. Legal systems must also distinguish true DID from pseudogenic DID, in which individuals imitate DID for personal gain in legal or social situations. Within jurisprudence, DID presents as three specific issues:
- those for which individuals accuse others of (generally severe) child sexual abuse but lack objective evidence and can only provide recovered memories
- individuals accused of crimes who deny culpability due to the crime being committed by a different identity state
- civil rights of different alters
Psychiatrist Colin A. Ross has stated that based on documents obtained through freedom of information legislation, psychiatrists linked to Project MKULTRA claimed to be able to deliberately induce dissociative identity disorder using a variety of aversive techniques.
Surveys of the attitudes of Canadian and American psychiatrists' attitudes towards dissociative disorders completed in 1999 and 2001 found considerable skepticism and disagreement regarding the research base of dissociative disorders in general and DID in specific, as well as whether the inclusion DID in the DSM was appropriate.
Research directions
A 2006 study compared scholarly research and publications on DID and dissociative amnesia to other mental health conditions, such as anorexia nervosa, alcohol abuse and schizophrenia from 1984 to 2003. The results were found to be unusually distributed, with a very low level of publications in the 1980s followed by a significant rise that peaked in the mid-1990s and subsequently rapidly declined in the decade following. Compared to 25 other diagnosis, the mid-90's "bubble" of publications regarding DID was unique. In the opinion of the authors of the review, the publication results suggest a period of "fashion" that waned, and that the two diagnoses " not command widespread scientific acceptance".
See also
Footnotes
- ^ "The ICD-10 Classification of Mental and Behavioural Disorders" (pdf). World Health Organization.
- ^ American Psychiatric Association (2000-06). Diagnostic and Statistical Manual of Mental Disorders-IV (Text Revision). Arlington, VA, USA: American Psychiatric Publishing, Inc. pp. 526–529. doi:10.1176/appi.books.9780890423349. ISBN 978-0890420249.
{{cite book}}: Check date values in:|date=(help) - Nijenhuis, E (2010). "Trauma-related structural dissociation of the personality" (pdf). Activitas Nervosa Superior. 52 (1): 1–23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15014580 , please use {{cite journal}} with
|pmid= 15014580instead. - ^ Paris J (1996). "Review-Essay : Dissociative Symptoms, Dissociative Disorders, and Cultural Psychiatry". Transcult Psychiatry. 33 (1): 55–68. doi:10.1177/136346159603300104.
- ^ Atchison M, McFarlane AC (1994). "A review of dissociation and dissociative disorders". The Australian and New Zealand journal of psychiatry. 28 (4): 591–9. doi:10.3109/00048679409080782. PMID 7794202.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17716088, please use {{cite journal}} with
|pmid= 17716088instead. - Howell, E (2010). "Dissociation and dissociative disorders: commentary and context". Knowing, not-knowing and sort-of-knowing: psychoanalysis and the experience of uncertainty. Karnac Books. pp. 83-98. ISBN 1855756579.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15503730 , please use {{cite journal}} with
|pmid= 15503730instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 9989574, please use {{cite journal}} with
|pmid= 9989574instead. - ^ Rubin, EH (2005). Adult psychiatry: Blackwell's neurology and psychiatry access series (2nd ed.). John Wiley & Sons. pp. 280. ISBN 1405117699.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ Weiten, W (2010). Psychology: Themes and Variations (8 ed.). Cengage Learning. pp. 461. ISBN 0495813109.
- ^ MacDonald, K (2008). "Dissociative disorders unclear? Think 'rainbows from pain blows'" (pdf). Current Psychiatry. 7 (5): 73–85.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18569730 , please use {{cite journal}} with
|pmid= 18569730instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15560314 , please use {{cite journal}} with
|pmid= 15560314instead. - ^ "Dissociative Identity Disorder". Merck.com. 2010.
- Reinders AA, Nijenhuis ER, Paans AM, Korf J, Willemsen AT, den Boer JA (2003). "One brain, two selves". Neuroimage. 20 (4): 2119–25. doi:10.1016/j.neuroimage.2003.08.021. PMID 14683715.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Birnbaum MH, Thomann K (1996). "Visual function in multiple personality disorder". Journal of the American Optometric Association. 67 (6): 327–34. PMID 8888853.
- Pearson, M.L. (1997). "Childhood trauma, adult trauma, and dissociation" (PDF). Dissociation. 10 (1): 58–62:. Retrieved 2008-06-01.
{{cite journal}}: CS1 maint: extra punctuation (link) - "Dissociative Identity Disorder, patient's reference". Merck.com. 2003-02-01. Retrieved 2007-12-07.
- ^ Kluft, RP (2003). "Current Issues in Dissociative Identity Disorder" (PDF). Bridging Eastern and Western Psychiatry. 1 (1): 71–87. Retrieved 2008-05-09.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - American Psychiatric Association (2000-06). Diagnostic and Statistical Manual of Mental Disorders DSM-IV TR (Text Revision). Arlington, VA, USA: American Psychiatric Publishing, Inc. p. 943. doi:10.1176/appi.books.9780890423349. ISBN 978-0890420249.
{{cite book}}: Check date values in:|date=(help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 3418321, please use {{cite journal}} with
|pmid= 3418321instead. - Putnam, F.W. (1997). Dissociation in children and adolescents: A developmental perspective. New York: Guilford.
- Perry, BD (1999). "The memory of states: How the brain stores and retrieves traumatic experience". Splintered reflections: Images of the body in treatment. New York: Basic Books. pp. 9–38. ISBN 0465095445.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1080/15299732.2011.537248, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1080/15299732.2011.537248instead. - Carson VB (2006). Foundations of Psychiatric Mental Health Nursing: A Clinical Approach (5 ed.). St. Louis: Saunders Elsevier. pp. 266–267. ISBN 1-4160-0088-7.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 7877901, please use {{cite journal}} with
|pmid=7877901instead. - American Psychiatric Association (2000). "Diagnostic criteria for 300.14 Dissociative Identity Disorder". Diagnostic and Statistical Manual of Mental Disorders (4th, text revision (DSM-IV-TR) ed.). ISBN 0-89042-025-4.
{{cite book}}:|access-date=requires|url=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ "Mental Health: Dissociative Identity Disorder (Multiple Personality Disorder)". Webmd.com. Retrieved 2007-12-10. Cite error: The named reference "webmd" was defined multiple times with different content (see the help page).
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20603761 , please use {{cite journal}} with
|pmid=20603761instead. - Dissociative identity disorder at the DSM-V showing proposed revision, page found 2011-06-05.
- Dissociative Trance Disorder at the DSM-V showing proposed merger with Dissociative Identity Disorder, page found 2011-06-05.
- Steinberg M, Rounsaville B, Cicchetti DV (1990). "The Structured Clinical Interview for DSM-III-R Dissociative Disorders: preliminary report on a new diagnostic instrument". The American journal of psychiatry. 147 (1): 76–82. PMID 2293792.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Steinberg, Marlene (1993). Structured clinical interview for DSM-IV dissociative disorders / Marlene Steinberg. Washington, DC: American Psychiatric Press. ISBN 0-88048-562-0.
- Ross CA, Ellason JW (2005). "Discriminating among diagnostic categories using the Dissociative Disorders Interview Schedule". Psychological reports. 96 (2): 445–53. doi:10.2466/PR0.96.2.445-453. PMID 15941122.
- Ross CA, Helier S, Norton R, Anderson D, Anderson G, Barchet P (198). "THE DISSOCIATIVE DISORDERS INTERVIEW SCHEDULE: A STRUCTURED INTERVIEW" (PDF). dissociation. 2 (3): 171.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bernstein EM, Putnam FW (1986). "Development, reliability, and validity of a dissociation scale". J. Nerv. Ment. Dis. 174 (12): 727–35. doi:10.1097/00005053-198612000-00004. PMID 3783140.
- Carlson EB; Putnam FW; Ross CA; et al. (1993). "Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study". The American journal of psychiatry. 150 (7): 1030–6. PMID 8317572.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Steinberg M, Rounsaville B, Cicchetti D (1991). "Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview". The American journal of psychiatry. 148 (8): 1050–4. PMID 1853955.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wright DB, Loftus EF (1999). "Measuring dissociation: comparison of alternative forms of the dissociative experiences scale". The American journal of psychology. 112 (4). The American Journal of Psychology, Vol. 112, No. 4: 497–519. doi:10.2307/1423648. JSTOR 1423648. PMID 10696264. Page 1
- ^ Sadock 2002, p. 683
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19893342 , please use {{cite journal}} with
|pmid= 19893342instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19724751, please use {{cite journal}} with
|pmid= 19724751instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21240739, please use {{cite journal}} with
|pmid= 21240739instead. - Kohlenberg, R.J. (1991). Functional Analytic Psychotherapy: Creating Intense and Curative Therapeutic Relationships. Springer. ISBN 0306438577.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Sadock 2002, p. 681
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18195639 , please use {{cite journal}} with
|pmid= 18195639instead. - Boon S, Draijer N (1991). "Diagnosing dissociative disorders in The Netherlands: a pilot study with the Structured Clinical Interview for DSM-III-R Dissociative Disorders". The American journal of psychiatry. 148 (4): 458–62. PMID 2006691.
- Adityanjee, Raju GS, Khandelwal SK (1989). "Current status of multiple personality disorder in India". The American journal of psychiatry. 146 (12): 1607–10. PMID 2589555.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Modestin J (1992). "Multiple personality disorder in Switzerland". The American journal of psychiatry. 149 (1): 88–92. PMID 1728191.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16877651, please use {{cite journal}} with
|pmid=16877651instead. - Gast U, Rodewald F, Nickel V, Emrich HM (2001). "Prevalence of dissociative disorders among psychiatric inpatients in a German university clinic". J. Nerv. Ment. Dis. 189 (4): 249–57. doi:10.1097/00005053-200104000-00007. PMID 11339321.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Friedl MC, Draijer N (2000). "Dissociative disorders in Dutch psychiatric inpatients". The American journal of psychiatry. 157 (6): 1012–3. doi:10.1176/appi.ajp.157.6.1012. PMID 10831486.
- Bliss EL, Jeppsen EA (1985). "Prevalence of multiple personality among inpatients and outpatients". The American journal of psychiatry. 142 (2): 250–1. PMID 3970252.
- Ross CA, Anderson G, Fleisher WP, Norton GR (1992). "Dissociative experiences among psychiatric inpatients". General hospital psychiatry. 14 (5): 350–4. doi:10.1016/0163-8343(92)90071-H. PMID 1521791.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Foote B, Smolin Y, Kaplan M, Legatt ME, Lipschitz D (2006). "Prevalence of dissociative disorders in psychiatric outpatients". The American journal of psychiatry. 163 (4): 623–9. doi:10.1176/appi.ajp.163.4.623. PMID 16585436.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sar V; Koyuncu A; Ozturk E; et al. (2007). "Dissociative disorders in the psychiatric emergency ward". General hospital psychiatry. 29 (1): 45–50. doi:10.1016/j.genhosppsych.2006.10.009. PMID 17189745.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20458202, please use {{cite journal}} with
|pmid= 20458202instead. - Ross CA (1991). "Epidemiology of multiple personality disorder and dissociation". Psychiatr. Clin. North Am. 14 (3): 503–17. PMID 1946021.
- Akyüz G, Doğan O, Sar V, Yargiç LI, Tutkun H (1999). "Frequency of dissociative identity disorder in the general population in Turkey". Comprehensive psychiatry. 40 (2): 151–9. doi:10.1016/S0010-440X(99)90120-7. PMID 10080263.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sar V, Akyüz G, Doğan O (2007). "Prevalence of dissociative disorders among women in the general population". Psychiatry Res. 149 (1–3): 169–76. doi:10.1016/j.psychres.2006.01.005. PMID 17157389.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Trauma And Dissociation in a Cross-cultural Perspective: Not Just a North American Phenomenon. Routledge. 2006. ISBN 978-0-7890-3407-6.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - "Creating Hysteria by Joan Acocella". The New York Times. 1999.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15912905, please use {{cite journal}} with
|pmid= 15912905instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21908758 , please use {{cite journal}} with
|pmid= 21908758instead. - ^ Rieber RW (2002). "The duality of the brain and the multiplicity of minds: can you have it both ways?". History of psychiatry. 13 (49 Pt 1): 3–17. doi:10.1177/0957154X0201304901. PMID 12094818.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6427406, please use {{cite journal}} with
|pmid= 6427406instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 2725878, please use {{cite journal}} with
|pmid= 2725878instead. - Borch-Jacobsen M, Brick D (2000). "How to predict the past: from trauma to repression". History of Psychiatry. 11 (41 Pt 1): 15–35. doi:10.1177/0957154X0001104102. PMID 11624606.
- ^ Putnam, Frank W. (1989). Diagnosis and Treatment of Multiple Personality Disorder. New York: The Guilford Press. p. 351. ISBN 0-89862-177-1.
- ^ van der Kolk BA, van der Hart O (1989). "Pierre Janet and the breakdown of adaptation in psychological trauma". Am J Psychiatry. 146 (12): 1530–40. PMID 2686473.
{{cite journal}}: Unknown parameter|month=ignored (help) - Rosenbaum M (1980). "The role of the term schizophrenia in the decline of diagnoses of multiple personality". Arch. Gen. Psychiatry. 37 (12): 1383–5. doi:10.1001/archpsyc.1980.01780250069008. PMID 7004385.
- American Psychiatric Association (1968). "Hysterical Neurosis". Diagnostic and statistical manual of mental disorders second edition. Washington, D.C. p. 40.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11623821, please use {{cite journal}} with
|pmid= 11623821instead. - Nathan, D (2011). Sybil Exposed. Free Press. ISBN 978-1439168271.
- Lawrence, M (2008). "Review of Bifurcation of the Self: The history and theory of dissociation and its disorders". American Journal of Clinical Hypnosis. 50 (3): 273–283.
- ^ Paris, J (2008). Prescriptions for the mind: a critical view of contemporary psychiatry. Oxford University Press. pp. 92. ISBN 0195313836.
- PMID 7788115
- Acocella, JR (1999). Creating hysteria: Women and multiple personality disorder. San Francisco: Jossey-Bass Publishers. ISBN 0-7879-4794-6.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16361871, please use {{cite journal}} with
|pmid=16361871instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19742237, please use {{cite journal}} with
|pmid= 19742237instead. - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16530592, please use {{cite journal}} with
|pmid= 16530592instead. - Ross, C (2000). Bluebird: Deliberate Creation of Multiple Personality Disorder by Psychiatrists. Manitou Communications. ISBN 978-0970452511.
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11441778, please use {{cite journal}} with
|pmid= 11441778instead.
References
- Sadock, Benjamin J. (2002). Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (9th ed.). Lippincott Williams & Wilkins. ISBN 0781731836.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: ref duplicates default (link)
External links
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||