This is an old revision of this page, as edited by Beno1000 (talk | contribs) at 11:02, 18 June 2012 (→Function). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 11:02, 18 June 2012 by Beno1000 (talk | contribs) (→Function)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Seminal vesicles" – news · newspapers · books · scholar · JSTOR (November 2009) (Learn how and when to remove this message) |
| Seminal vesicle | |
|---|---|
| File:Male anatomy en.svgHuman Male Anatomy | |
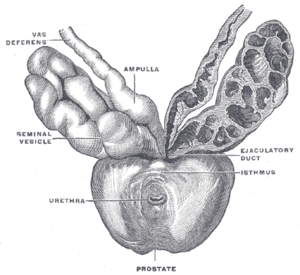 Prostate with seminal vesicles and seminal ducts, viewed from in front and above. Prostate with seminal vesicles and seminal ducts, viewed from in front and above. | |
| Details | |
| Precursor | Wolffian duct |
| Artery | Inferior vesical artery, middle rectal artery |
| Lymph | external iliac lymph nodes, internal iliac lymph nodes |
| Identifiers | |
| Latin | vesiculæ seminales |
| MeSH | D012669 |
| TA98 | A09.3.06.001 |
| TA2 | 3631 |
| FMA | 19386 |
| Anatomical terminology[edit on Wikidata] | |
The seminal vesicles (glandulae vesiculosae) or vesicular glands are a pair of simple tubular glands posteroinferior to the urinary bladder of male mammals. It is located within the pelvis.
Anatomy
Each seminal gland spreads approximately 5 cm, though the full length of seminal vesicle is approximately 10 cm, but it is curled up inside of the gland's structure. Each gland forms as an outpocketing of the wall of ampulla of each vas deferens.
The excretory duct of seminal gland opens into the vas deferens as it enters the prostate gland.
Function
The seminal vesicles secrete a significant proportion of the fluid that ultimately becomes semen. Lipofuscin granules from dead epithelial cells give the secretion its yellowish color. About 50-70% of the seminal fluid in humans originates from the seminal vesicles, but is not expelled in the first ejaculate fractions which are dominated by spermatozoa and zinc-rich prostatic fluid. The excretory duct of each seminal gland opens into the corresponding vas deferens as it enters the prostate gland. Seminal vesicle fluid is alkaline, resulting in human semen having a mildly alkaline pH. The alkalinity of semen helps neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm. Acidic ejaculate (pH <7.2) may be associated with Ejaculatory duct obstruction. The vesicle produces a substance that causes the semen to become sticky/jelly-like after ejaculation, which is thought to be useful in keeping the semen near the womb.
The thick secretions from the seminal vesicles contain proteins, enzymes, fructose, mucus, vitamin C, flavins, phosphorylcholine and prostaglandins. The high fructose concentrations provide nutrient energy for the spermatozoa when stored in semen in the laboratory. Spermatozoa ejaculated into the vagina are not likely to have contact with the seminal vesicular fluid but transfer directly from the prostatic fluid into the cervical mucus as the first step on their travel through the female reproductive system. The fluid is expelled under sympathetic contraction of the muscularis muscle coat.
In vitro studies have shown that sperm expelled together with seminal vesicular fluid show poor motility and survival, and the sperm chromatin is less protected. Therefore the exact physiological importance of seminal vesicular fluid is not clear. It has been speculated that it is a developmental rest, still seen among some rodents where the last part of the ejaculate form a spermicidal plug which reduces the chances for sperm from a later arriving male to proceed to the oocyte.
Histology


Histologically, the seminal vesicles are notable for their tortuous pathways, diverticula, pseudo-stratified columnar epithelium and cuboidal cells along the basal layer.

The height of these columnar cells, and therefore activity, is dependent upon testosterone levels in the blood.
The lumen is large and stores the fluid secretions (but not spermatozoa) between ejaculations.
From inside to out, the layers are:
- Mucosa - arranged into convoluted folds, significantly increasing surface area
- Muscular - well-developed layer composed of an inner circular and outer longitudinal layer of smooth muscle
- Connective tissue
Additional images
-
 Human male reproductive system.
Human male reproductive system.
-
 Seminal vesicles
Seminal vesicles
-
 Coronal section of pelvis, showing arrangement of fasciae. Viewed from behind.
Coronal section of pelvis, showing arrangement of fasciae. Viewed from behind.
-
 Male pelvic organs seen from right side.
Male pelvic organs seen from right side.
-
 Fundus of the bladder with the vesiculae seminales.
Fundus of the bladder with the vesiculae seminales.
-
 Vesiculae seminales and ampullae of ductus deferentes, seen from the front.
Vesiculae seminales and ampullae of ductus deferentes, seen from the front.
-
 Vertical section of bladder, penis, and urethra.
Vertical section of bladder, penis, and urethra.
-
Cross section of seminal vesicle through a microscope.
External links
- Histology image: 17501loa – Histology Learning System at Boston University - "Male Reproductive System: prostate, seminal vesicle"
- Anatomy photo:44:04-0202 at the SUNY Downstate Medical Center - "The Male Pelvis: The Urinary Bladder"
- Anatomy photo:44:08-0103 at the SUNY Downstate Medical Center - "The Male Pel
References
- Wilke (2009). Anatomy and Physiology of Farm Animals. John Wiley and Sons. ISBN 0-8138-1394-8.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Kierszenbaum, Abraham L. (2002). Histology and cell biology : an introduction to pathology. St. Louis : Mosby. p. 558. ISBN 0-323-01639-1.
-
"CHEMICAL COMPOSITION OF HUMAN SEMEN AND OF THE SECRETIONS OF THE PROSTATE AND SEMINAL VESICLES". http://ajplegacy.physiology.org. Retrieved 2010-08-10.
{{cite web}}: External link in|publisher= - reference needed
| Anatomy and morphology | ||
|---|---|---|
| Fields |  | |
| Bacteria and fungi | ||
| Protists | ||
| Plants | ||
| Invertebrates | ||
| Mammals | ||
| Other vertebrates | ||
| Glossaries | ||
| Related topics | ||