This is an old revision of this page, as edited by 121.218.77.212 (talk) at 11:41, 3 April 2013 (→Sexual dysfunction). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 11:41, 3 April 2013 by 121.218.77.212 (talk) (→Sexual dysfunction)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) "SSRI" redirects here. For other uses, see SSRI (disambiguation). See also: Serotonin reuptake inhibitor| Selective serotonin reuptake inhibitor | |
|---|---|
| Drug class | |
 Serotonin Serotonin | |
| Class identifiers | |
| Use | Depression |
| ATC code | N06AB |
| Biological target | Serotonin transporter |
| Clinical data | |
| Drugs.com | Drug Classes |
| Consumer Reports | Best Buy Drugs |
| External links | |
| MeSH | D017367 |
| Legal status | |
| In Wikidata | |
Selective serotonin re-uptake inhibitors or serotonin-specific reuptake inhibitor (SSRIs) are a class of compounds typically used as antidepressants in the treatment of depression, anxiety disorders, and some personality disorders.
SSRIs are believed to increase the extracellular level of the neurotransmitter serotonin by inhibiting its reuptake into the presynaptic cell, increasing the level of serotonin in the synaptic cleft available to bind to the postsynaptic receptor. They have varying degrees of selectivity for the other monoamine transporters, with pure SSRIs having only weak affinity for the noradrenaline and dopamine transporter.
SSRIs are the first class of psychotropic drugs discovered using the process called rational drug design, a process that starts with a specific biological target and then creates a molecule designed to affect it. They are the most widely prescribed antidepressants in many countries. The efficacy of SSRIs in mild or moderate cases of depression has been disputed.
Medical uses
The main indication for SSRIs is clinical depression. SSRIs are frequently prescribed for anxiety disorders, such as social anxiety, panic disorders, obsessive–compulsive disorder (OCD), eating disorders, chronic pain and occasionally, for posttraumatic stress disorder (PTSD). They are also frequently used to treat depersonalization disorder, although generally with poor results.
Depression
Antidepressants are recommended by the National Institute for Clinical Excellence (NICE) as a first-line treatment of severe depression and for the treatment of mild-to-moderate depression that persists after conservative measures such as cognitive therapy. They recommend against their routine use in those who have chronic health problems and mild depression. There has been controversy regarding the efficacy of antidepressants in treating depression depending on its severity and duration. A comprehensive review conducted by NICE concluded that antidepressants have no advantage over placebo in the treatment of short term mild depression, but that the available evidence supported the use of antidepressants in the treatment of dysthymia and other forms of chronic mild depression. Two meta-analyses of clinical trials published in 2008 and 2011 found that in mild and moderate depression, the effect of SSRIs is small or none compared to placebo, while in very severe depression the effect of SSRIs is between "relatively small " and "substantial". Unlike the NICE study, these studies did not discriminate between the acutely and chronically depressed. The 2008 meta-analysis combined 35 clinical trials submitted to the U.S. Food and Drug Administration (FDA) before licensing of four newer antidepressants (including the SSRIs paroxetine and fluoxetine, the non-SSRI antidepressant nefazodone, and the SNRI (serotonin and norepinephrine reuptake inhibitor) venlafaxine). The authors attributed the relationship between severity and efficacy to a reduction of the placebo effect in severely depressed patients, rather than an increase in the effect of the medication. Some researchers have questioned the statistical basis of this study suggesting that it underestimates the effect size of antidepressants. A 2010 review reached similar conclusions: in mild and moderate depression, specifically that the effect of SSRI is very small or none compared to placebo, while it is clinically significant in very severe depression. However, this analysis included only 6 studies out of the over 2,000 that have been done, involved just 2 medications, and did not involve studies with placebo washout periods typically used as controls.
SSRIs are recommended by NICE over tricyclics due to their superior tolerability. One study showed that SSRIs have greater adverse effects than TCAs in the elderly, though the authors caution that more research is needed. There does not appear to be a substantial differences in efficacy among the various second generation antidepressants (SSRIs and SNRIs).
Generalized anxiety disorder
SSRIs are recommended by the National Institute for Health and Clinical Excellence (NICE) for the treatment of generalized anxiety disorder (GAD) that has failed to respond to conservative measures such as education and self-help activities. GAD is a common disorder of which the central feature is excessive worry about a number of different events. Key symptoms include excessive anxiety about multiple events and issues, and difficulty controlling worrisome thoughts that persists for at least 6 months.
Antidepressants provide a modest-to-moderate reduction in anxiety in GAD, and are superior to placebo in treating GAD. The efficacy of different antidepressants is similar.
Obsessive compulsive disorder (OCD)
SSRIs are recommended for the second line treatment of adult obsessive compulsive disorder patients with mild functional impairment and as first line treatment for those with moderate or severe impairment. In children, SSRIs can be considered as a second line therapy in those with moderate-to-severe impairment, with close monitoring for psychiatric adverse effects. SSRIs are efficacious in the treatment of OCD; patients treated with SSRIs are about twice as likely to respond to treatment as those treated with placebo.
Eating disorders
Anti-depressants are recommended as an alternative or additional first step to self-help programs in the treatment of bulimia nervosa. SSRIs (fluoxetine in particular) are preferred over other anti-depressants due to their acceptability, tolerability, and superior reduction of symptoms in short term trials. Long term efficacy remains poorly characterized.
Similar recommendations apply to binge eating disorder. SSRIs provide short term reductions in binge eating behavior, but have not been associated with significant weight loss.
Clinical trials have generated mostly negative results for the use of SSRI's in the treatment of anorexia nervosa. Treatment guidelines from the National Institute of Health and Clinical Excellence recommend against the use of SSRIs in this disorder. Those from the American Psychiatric Association note that SSRIs confer no advantage regarding weight gain, but that they may be used for the treatment of co-existing depressive, anxiety, or obsessive-compulsive disorders.
Stroke recovery
SSRIs have been used in the treatment of stroke patients, including those with and without symptoms of depression. A recent meta analysis of randomized, controlled clinical trials found a statistically significant effect of SSRIs on dependence, neurological deficit, depression, and anxiety. There was no statistically significant effect on death, motor deficits, or cognition.
Premature ejaculation
A general disadvantage of SSRIs in treating premature ejaculation is that they require continuous daily treatment to delay ejaculation significantly. For the occasional "on-demand" treatment, a few hours before coitus, clomipramine gave better results than paroxetine in one study, while in another study both sertraline and clomipramine were indistinguishable from the pause–squeeze technique and inferior to paroxetine. The most recent research, conducted in 2007, suggests that on-demand treatment with sildenafil (Viagra) offers a dramatic improvement in ejaculation delay and sexual satisfaction as compared with daily paroxetine, with on-demand sertraline, paroxetine or clomipramine, and with the pause–squeeze technique.
Adverse effects
General side effects are mostly present during the first 1–4 weeks while the body adapts to the drug (with the exception of sexual side effects, which tend to occur later in treatment). In fact, it often takes 6–8 weeks for the drug to begin reaching its full potential (the slow onset is considered a downside to treatment with SSRIs). Almost all SSRIs are known to cause one or more of these symptoms:
- nausea/vomiting
- drowsiness or somnolence
- headache (very common as a short-term side effect)
- bruxism
- extremely vivid or strange dreams
- dizziness
- mydriasis (pupil dilation)
- changes in appetite
- insomnia and/or changes in sleep
- excessive diarrhea
- weight loss/gain (measured by a change in bodyweight of 7 pounds)
- increased risk of bone fractures by 1.7 fold
- changes in sexual behaviour (see the next section)
- increased feelings of depression and anxiety (which may sometimes provoke panic attacks)
- mania
- tremors
- autonomic dysfunction including orthostatic hypotension, increased or reduced sweating
- akathisia
- suicidal ideation (thoughts of suicide)
- photosensitivity
- paresthesia
- cognitive disorders
- Syndrome of inappropriate antidiuretic hormone hypersecretion
Many side effects disappear after the adaptation phase, when the antidepressant effects begin to come to prominence. However, despite being called general, the side effects and their durations are highly individual and drug-specific. Usually the treatment is begun with a small dose to see how the patient's body reacts to the drug, after that either the dose can be adjusted (e.g. Prozac in the UK is begun at a 20 mg dose, and then adjusted as necessary to 40 mg or 60 mg). Should the drug prove ineffective, or the side effects intolerable to the patient, another common route is to switch treatment to either another SSRI, or an SNRI.
Mania or hypomania is a possible side effect. Users with some type of bipolar disorder are at a much higher risk, however SSRI-induced mania in patients previously diagnosed with unipolar depression can trigger a bipolar episode; however, according to DSM IV-TR, the diagnosis of bipolar disorder requires that the individuals symptoms must not stem from medication side effects, toxins, drug abuse, or another general medical condition.
Sexual dysfunction
SSRIs can cause various types of sexual dysfunction such as anorgasmia, erectile dysfunction, and diminished libido. Initial studies found sexual side effects not significantly different from placebo, but since these studies relied on unprompted reporting, the frequency was probably underestimated. In more recent studies, doctors have specifically asked about sexual difficulties, and found that they are present in between 17% and 41% of patients, although the lack of placebo control in these studies means they are likely underestimates. This is because release of extracellular concentrations of serotonin in the brain decreases dopamine and norepinephrine leading to erectile and/or sexual dysfunction.
Release of postsynaptic 5-HT2 and 5-HT3 receptors decreases dopamine and norepinephrine release from the substantia nigra. A number of drugs are not associated with sexual side effects (such as bupropion, mirtazapine, reboxetine, tianeptine, agomelatine, trazodone, nefazodone, moclobemide and maprotiline, some of which are also not associated with weight gain). As a result, sexual dysfunction caused by SSRIs can sometimes be treated by several different medications including: bupropion, ropinirole and yohimbine among others.
A small number of case reports have appeared in the literature suggesting that in rare cases, sexual dysfunction may persist after discontinuing treatment.
On the other hand, the effect of SSRIs to slow down sexual stimulation may be used as treatment; SSRIs have been proposed as a drug to treat premature ejaculation. The Andean herbaceous biennial plant Lepidium meyenii (also known as "maca") was found to be effective for alleviating SSRI-induced sexual dysfunction on a small double-blind, randomized, parallel group dose-finding pilot study.
Cardiovascular
Cardiovascular side effects are very rare with SSRI use, with a reported incidence of less than 0.0003 percent. SSRIs inhibit cardiac and vascular sodium, calcium and potassium channels and prolong QT intervals. A number of large studies of patients without known pre-existing heart disease have reported no EKG changes related to SSRI use. More recently, however, concerns about cardiac problems have led to a reduction in the recommended maximum dose of two types of SSRI's. The recommended maximum daily dose of citalopram was reduced to 40 mg. for most people and 20 mg. for those older than age 60 and some others. The recommended maximum daily dose of escitalopram was reduced to 10 mg. for those older than age 65; the maximum daily dose for most other people remained unchanged at 20 mg. In overdose, fluoxetine has been reported to cause sinus tachycardia, myocardial infarction, junctional rhythms and trigeminy. Some authors have suggested electrocardiographic monitoring in patients with severe pre-existing cardiovascular disease who are taking SSRI's.
Discontinuation syndrome
Main article: SSRI discontinuation syndromeAntidepressants such as SSRIs have some dependence producing effects, most notably a withdrawal syndrome. Their dependence producing properties (depending on the antidepressant) may not be as significant as other psychotropic drugs such as benzodiazepines; however, withdrawal symptoms nonetheless may be quite severe and even debilitating. SSRIs have little abuse potential, but discontinuation can produce disturbing withdrawal symptoms that may be indistinguishable from a reoccurrence of the original illness. Since physical dependence is a reality, discontinuation should be discussed with a medical practitioner before beginning treatment with this class of drugs.
When discontinuing an SSRI or SNRI some doctors may switch the patient to fluoxetine due to its much longer half-life. This may avoid many of the severe withdrawal symptoms associated with SSRI/SNRI discontinuation. This can be done either by administering a single 20 mg dose of fluoxetine or by beginning on a low dosage of fluoxetine and slowly tapering down. Any SSRI or SNRI may be requested in liquid form, which allows very gradual tapering. Alternatively, a patient wishing to stop taking an SSRI/SNRI may visit a compounding pharmacy where his or her prescription may be re-arranged into progressively smaller dosages. For example the lowest dose of cymbalta that can normally be prescribed is 20 mg in gel capsules; a compounding pharmacist may divide this into doses of 20, 15, 10, 5 and 2.5 mg so that a proper tapered reduction may take place.
Suicide risk
Children and adolescents
Several studies have found that SSRI use is related to a higher risk of suicidal behavior in children and adolescents. For instance, a 2004 U.S. Food and Drug Administration (FDA) analysis of clinical trials on children with major depressive disorder found statistically significant increases of the risks of "possible suicidal ideation and suicidal behavior" by about 80%, and of agitation and hostility by about 130%; More infrequently, studies have been inconclusive. however, a recent comparison of aggression and hostility occurring during treatment with fluoxetine to placebo in children and adolescents found that no significant difference between the fluoxetine group and a placebo group. There is also evidence that higher rates of SSRI prescriptions are associated with lower rates of suicide in children, though since the evidence is correlational, the true nature of the relationship is unclear.
In 2004, the Medicines and Healthcare products Regulatory Agency (MHRA) in the United Kingdom judged fluoxetine (Prozac) to be the only antidepressant that offered a favorable risk-benefit ratio in children with depression, though it was also associated with a slight increase in the risk of self-harm and suicidal ideation. Only two SSRIs are licensed for use with children in the UK, sertraline (Zoloft) and fluvoxamine (Luvox), and only for the treatment of obsessive–compulsive disorder. Fluoxetine is not licensed for this use.
Adults
It is unclear whether or not SSRIs affect the risk of suicidal behavior for adults.
- A 2005 meta-analysis of drug company data found no evidence that SSRIs increased the risk of suicide; however, important protective or hazardous effects could not be excluded. Also among high-risk adult patients, antidepressant drug treatment does not seem related to suicide attempts and death.
- A 2005 review observed that suicide attempts are increased in those who use SSRIs as compared to placebo and compared to therapeutic interventions other than tricyclic antidepressants. No difference risk of suicide attempts was detected between SSRIs versus tricyclic antidepressants.
- On the other hand, a 2006 review suggests that the widespread use of antidepressants in the new "SSRI-era" appear to have led to highly significant decline in suicide rates in most countries with traditionally high baseline suicide rates. The decline is particularly striking for women who, compared with men, seek more help for depression. Recent clinical data on large samples in the US too have revealed a protective effect of antidepressant against suicide.
- A 2006 meta analysis of random controlled trials suggests that SSRIs increase suicide ideation compared with placebo. However, the observational studies suggests that SSRIs did not increase suicide risk more than older antidepressants. The researchers stated that if SSRIs increase suicide risk in some patients, the number of additional deaths is very small because ecological studies have generally found that suicide mortality has declined (or at least not increased) as SSRI use has increased.
- An additional meta-analysis by the FDA in 2006 found an age-related effect of SSRI's. Among adults younger than 25 years, results indicated that there was a higher risk for suicidal behavior. For adults between 25 and 64, the effect appears neutral on suicidal behavior but possibly protective for suicidal behavior for adults between the ages of 25 and 64. For adults older than 64, SSRI's seem to reduce the risk of both suicidal behavior.
Suicide warnings
The FDA findings resulted in a black box warning on SSRI and other antidepressant medications regarding the increased risk of suicidal behavior in patients younger than 24. Similar precautionary notice revisions were implemented by the Japanese Ministry of Health. In 2004 the Medicines and Healthcare products Regulatory Agency in the United Kingdom issued a warning about increases in 'insomnia, agitation, weight loss, headache, tremor, loss of appetite, self-harm and suicidal thoughts' when the medications are used with children and adolescents.
The introduction of a warning regarding the association between SSRIs and suicide by the FDA in 2004 led to a dramatic decrease in prescriptions of these medications to young people. Originally, there were concerns that the decrease in prescriptions caused by the warnings could increase the number of teenage suicides in the US. However, the most recent data from the US National Center for Health Statistics put these concerns to rest. The suicide rates for persons younger than 25 has actually decreased between 2004 and 2007.
Pregnancy and breastfeeding
SSRI use during pregnancy is associated with an increased rate of miscarriages, birth defects, persistent pulmonary hypertension of the newborn, newborn behavioral syndrome, and possibly long term behavioral problems. The risk of spontaneous abortion is increased about 1.7 fold.
The FDA issued a statement on July 19, 2006 stating nursing mothers on SSRIs must discuss treatment with their physicians. However, the medical literature on the safety of SSRIs has determined that some SSRIs like Sertraline and Paroxetine are considered safe for breastfeeding.
Maternal SSRI use may be associated with autism.
Neonatal abstinence syndrome
Neonatal abstinence syndrome is a withdrawal syndrome in newborn babies. It has been documented in SSRI treatment. By November 2003, a total of 93 cases of SSRI use associated with either neonatal convulsions or withdrawal syndrome had been reported. Subsequently, the authors of a Lancet study concluded that doctors should avoid or cautiously manage the prescribing of these drugs to pregnant women with psychiatric disorders.
Neuropsychological changes due to SSRI use in infancy
Since the early 80's scientists have used a technique called neonatal clomipramine to produce animals used in depression research. If rats are given the tricyclic antidepressant clomipramine when 8–21 days old, they develop behavioural changes in adulthood that resemble depression in humans. In 1997 Lundbeck found that treatment with the SSRI LU-10-134-C, which only differs from their product citalopram by two atoms could give similar results as clomipramine. Later it was found that neonatal citalopram and escitalopram makes persistent changes in the serotonergic transmission of the brain resulting in behavioral changes, which are reversed by treatment with antidepressants. By treating normal and knockout mice lacking the serotonin transporter with fluoxetine scientists showed that normal emotional reactions in adulthood, like a short latency to escape foot shocks and inclination to explore new environments were dependent on active serotonin transporters during the neonatal period.
But when young mice were treated with the SNRI desimipramine they developed to normal adults, which suggests that serotonin and noradrenaline have different effects in the developing brain. For humans, the developmental stage sensitive to SSRI:s corresponds with the last trimester to the first years of life. A study showed that 4-year old children perinatally exposed to SSRIs behave normally. However, the young mice and rats also seem normal until they reach puberty and develop behavioural disturbances.
The mechanism is currently unknown, but it seems that early life overstimulation of the 5HT-1 receptor that regulates serotonin production results in low serotonin production after puberty.
Persistent pulmonary hypertension
Persistent pulmonary hypertension (PPHN) is a serious and life-threatening, but rare, lung condition that occurs soon after birth of the newborn. Newborn babies with PPHN have high pressure in their lung blood vessels and are not able to get enough oxygen into their bloodstream. About 1 to 2 babies per 1000 babies born in the U.S. develop PPHN shortly after birth, and often they need intensive medical care. One study has found that PPHN is six times more common in babies whose mothers take an SSRI antidepressant after the 20th week of the pregnancy compared to babies whose mothers do not take an antidepressant.
A population-based cohort study, which included 1.6 million live births in five Nordic countries, of women with filled SSRI prescriptions later than the 20th week gestation by last menstrual period demonstrated an increased risk of persistent pulmonary hypertension (PPHN) compared to control infants (adjusted RR 2.1, 95% CI 1.5-3). The increased risk of PPHN was of similar magnitude for the SSRI class of drugs (Fluoxetine, Citalopram, Paroxetine, Sertraline, Escitalopram). This study showed that the absolute risk of PPHN would only increase the incidence from 0.1 to 0.3 percent of live-births with late prenatal SSRI exposure.
Bleeding tendencies
SSRIs appear to increase the risk of bleeding. This includes an increased risk of GI bleeding, post operative bleeding, and intracranial bleeding. SSRIs are known to cause platelet dysfunction.
Overdose
See also: Serotonin syndromeSSRIs appear safer in overdose when compared with traditional antidepressants, such as the tricyclic antidepressants. This relative safety is supported both by case series and studies of deaths per numbers of prescriptions. However, case reports of SSRI poisoning have indicated that severe toxicity can occur and deaths have been reported following massive single ingestions, although this is exceedingly uncommon when compared to the tricyclic antidepressants.
Because of the wide therapeutic index of the SSRIs, most patients will have mild or no symptoms following moderate overdoses. The most commonly reported severe effect following SSRI overdose is serotonin syndrome; serotonin toxicity is usually associated with very high overdoses or multiple drug ingestion. Other reported significant effects include coma, seizures, and cardiac toxicity.
Treatment for SSRI overdose is mainly based on symptomatic and supportive care. Medical care may be required for agitation, maintenance of the airways, and treatment for serotonin syndrome. ECG monitoring is usually indicated to detect any cardiac abnormalities.
Contraindications and drug interaction
One major contraindication of SSRIs is the concomitant use of MAOIs (monoamine oxidase inhibitors). This is likely to cause severe serotonin syndrome/toxidrome.
People taking SSRIs should also avoid taking pimozide (an antipsychotic diphenylbutylpiperidine derivative). Tramadol hydrochloride (or Ultram, Ultracet) can, in rare cases, produce seizures when taken in conjunction with an SSRI or tricyclic antidepressant. Liver impairment is another contraindication for medications of this type.
SSRIs may increase blood levels and risk of toxicities of certain medications:
- highly protein-bound medications like warfarin (coumadin) and digoxin
- antiarrhythmic agents like propafenone (Rythmol) or flecainide (Tambocor)
- beta blockers like metoprolol (Toprol xl) or propranolol (Inderal)
- Tricyclic antidepressants like amitriptyline (Elavil, Endep) etc.
- triptans like sumatriptan (Imitrex, Imigran) etc.
- benzodiazepines like alprazolam (Xanax) or diazepam (Valium)
- carbamazepine (Tegretol)
- cisapride (Propulsid)
- clozapine (Clozaril)
- ciclosporin (Neoral)
- haloperidol (Haldol)
- phenytoin (Dilantin)
- pimozide (Orap)
- theophylline (Theo-dur)
Certain drugs may increase toxicities of SSRIs:
- alcohol and other CNS depressants
- methylene blue dye
- diuretics (water pills)
- MAOIs – possibly fatal serotonin syndrome/toxidrome
- sympathomimetic drugs like pseudoephedrine (Sudafed)
- lithium
- sibutramine (Meridia)
- MDMA (ecstasy)
- zolpidem (ambien)
- dextromethorphan (cough suppressant) – increased risk of serotonin syndrome/toxidrome
- tramadol (synergistic serotoninergic effect said to increase risk of seizure or serotonin syndrome/toxidrome)
- pethidine/meperidine – increased risk of serotonin syndrome/toxidrome
- herbal Saint John's wort or yohimbe – increased risk of serotonin syndrome/toxidrome
Painkillers of the NSAIDs drug family may interfere and reduce efficiency of SSRIs:
SSRIs also directly interfere with ligands of 5-HT receptors, like the psychedelics and entactogens. SSRIs strongly diminish the effects of tryptamines (e.g. psilocybin and LSD), and phenethylamines (e.g. the 2C family), and almost completely eliminate the serotonergic effects of MDxx (e.g. MDMA). The exact mechanism that causes this interaction is still unclear. However, salvinorin A (found in Salvia divinorum) has no actions at the 5-HT2A serotonin receptor, nor is it known to have affinity for any other sites to date.
List of agents
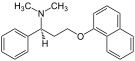
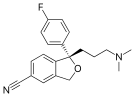
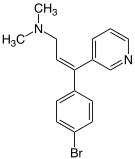
Drugs in this class include (trade names in parentheses):
- citalopram (Celexa, Cipramil, Cipram, Dalsan, Recital, Emocal, Sepram, Seropram, Citox, Cital)
- dapoxetine (Priligy)
- escitalopram (Lexapro, Cipralex, Seroplex, Esertia)
- fluoxetine (Depex, Prozac, Fontex, Seromex, Seronil, Sarafem, Ladose, Motivest, Flutop, Fluctin (EUR), Fluox (NZ), Depress (UZB), Lovan (AUS), Prodep (IND))
- fluvoxamine (Luvox, Fevarin, Faverin, Dumyrox, Favoxil, Movox, Floxyfral)
- indalpine (Upstene) (discontinued)
- paroxetine (Paxil, Seroxat, Sereupin, Aropax, Deroxat, Divarius, Rexetin, Xetanor, Paroxat, Loxamine, Deparoc)
- sertraline (Zoloft, Lustral, Serlain, Asentra, Tresleen)
- zimelidine (Zelmid, Normud) (discontinued)
| Selective serotonin reuptake inhibitors (SSRIs) | ||||
|---|---|---|---|---|

|
|
|

|

|

|
File:Paroxetine.svg | 
|
|
|
Related agents
SSRIs form a subclass of serotonin uptake inhibitors, which includes other non-selective inhibitors as well. Serotonin-norepinephrine reuptake inhibitors, serotonin-norepinephrine-dopamine reuptake inhibitors and selective serotonin reuptake enhancers are also serotonergic antidepressants.
Mechanism of action
SSRIs are believed to act by inhibiting the reuptake of serotonin after being released in synapses. How much an individual will respond to this, however, also depends on genetics. In addition, several other mechanisms are suggested for the desired effect, e.g. neuroprotection and anti-inflammatory and immunomodulatory factors. Taken together, SSRI has several advantages compared with tricyclic antidepressants (TCA)s and 5-HT-prodrugs. However, the latter might be required in addition to SSRIs in certain situations.
Basic understanding
Further information: Chemical synapseIn the brain, messages are passed between two nerve cells via a chemical synapse, a small gap between the cells. The (presynaptic) cell that sends the information releases neurotransmitters (including serotonin) into that gap. The neurotransmitters are then recognized by receptors on the surface of the recipient (postsynaptic) cell, which upon this stimulation, in turn, relays the signal. About 10% of the neurotransmitters are lost in this process; the other 90% are released from the receptors and taken up again by monoamine transporters into the sending (presynaptic) cell (a process called reuptake).
To stimulate the recipient cell, SSRIs inhibit the reuptake of serotonin. As a result, the serotonin stays in the synaptic gap longer than it normally would, and may repeatedly stimulate the receptors of the recipient cell. The current model of SSRIs (the Monoamine Hypothesis) assumes that a lower homeostatic level of serotonin is primarily responsible for depression. While this holds in cases of major depression, minor to moderate cases are not as clear cut, and may in fact be caused by excess serotonin in specific areas of the brain.
Some current research points to more than just a single type of chemical signaling - the classic synapse model - involving serotonin. Astrocytes are "helper cells" in the brain that do not participate directly in chemical signaling, but play a part in homeostasis for many chemical levels in the brain. Recent research suggests that serotonin is one of the hormones regulated by astrocytes, and that astrocytes actually uptake, package, and resend serotonin in a way similar to neuronal axons, but do not have corresponding post-synaptic terminals, therefore appearing to function only to control the local levels of serotonin in the cerebrospinal fluid.
Still more research illustrates that the current model for the antidepressant activity of SSRIs may be misdirected, as a drug that works entirely opposite to SSRIs - Tianeptine, a selective serotonin reuptake enhancer - also exhibits antidepressant activity, especially in patients resistant to SSRI therapy. The effect of an SSRE in comparison to an SSRI requires that the nature of serotonin signaling in the areas of the brain related to mood and cognition needs further elucidation. If serotonin firing is regularly phasic (related to brain waves), or rapid and discrete, then SSRIs simply compress the signal potential at affected receptors (bringing down the maximum potential and bring up the minimum) by causing a constant leftover signal (serotonin left in the synaptic gap) coupled with weaker subsequent signals (due to the decrease in presynaptic serotonin available to send new signals). By this hypothetical model, SSREs increase the signal potential separation (min to max) at affected 5-HT sites by reducing the level of free cerebrospinal serotonin and increasing the amount uptaken into axons to send new signals.
Pharmacodynamics
SSRIs inhibit the reuptake of the neurotransmitter serotonin (5-hydroxytryptamine or 5-HT) into the presynaptic cell, increasing levels of 5-HT within the synaptic cleft.
However, there is one counteracting effect: high serotonin levels will not only activate the postsynaptic receptors, but also flood presynaptic autoreceptors, which serve as a feedback sensor for the cell. Activation of the autoreceptors (by agonists like serotonin) triggers a throttling back of serotonin production. The resulting serotonin deficiency persists for some time, as the transporter inhibition occurs downstream to the cause of the deficiency and therefore, is not able to counterbalance the serotonin deficiency. The body adapts gradually to this situation by lowering (downregulating) the sensitivity of the autoreceptors.
Another adaptive process provoked by SSRIs is the downregulation of postsynaptic serotonin 5-HT2A receptors. After the use of an SSRI, since there is more serotonin available, the response is to decrease the number of postsynaptic receptors over time and in the long run, this modifies the serotonin/receptor ratio. This downregulation of 5-HT2A occurs when the antidepressant effects of SSRIs become apparent. Also, deceased suicidal and otherwise depressed patients have had more 5-HT2A receptors than normal patients. These considerations suggest that 5-HT2A overactivity is involved in the pathogenesis of depression.
Most of the serotonin receptors on the surface of the cell are coupled to a G-protein inside it. These proteins activate or inhibit second messengers, which in turn affect transcription factors. Transcription factors are proteins that fit to the beginning of a gene and tell the cell to start using it.
These (slowly proceeding) neurophysiological adaptations of the brain tissue are the reason why usually several weeks of continuous SSRI use is necessary for the antidepressant effect to become fully manifested, and why increased anxiety is a common side effect in the first few days or weeks of use.
Role in BDNF release
SSRIs act on signal pathways such as cAMP (Cyclic AMP) on the postsynaptic neuronal cell, which leads to the release of Brain Derived Neurotrophic Factor (BDNF). BDNF enhances the growth and survival of cortical neurons and synapses.
Pharmacogenetics
Further information: PharmacogeneticsLarge bodies of research are devoted to using genetic markers to predict whether patients will respond to SSRIs or have side effects that will cause their discontinuation, although these tests are not yet ready for widespread clinical use. Single-nucleotide polymorphisms of the 5-HT(2A) gene correlated with paroxetine discontinuation due to side effects in a group of elderly patients with major depression, but not mirtazapine (a non-SSRI antidepressant) discontinuation.
Neuroprotection
Studies have suggested that SSRIs may promote the growth of new neural pathways or neurogenesis in rats. Also, SSRIs may protect against neurotoxicity caused by other compounds (for instance fenfluramine) as well as from depression itself. SSRIs have been found to induce programmed cell death in Burkitt lymphoma and the brain tumors neuroblastoma and glioma with minimal effect on normal tissue.
Anti-inflammatory and immunomodulation
Recent studies show pro-inflammatory cytokine processes take place during depression, mania and bipolar disorder, in addition to somatic disease (such as autoimmune hypersensitivity) and it is possible that symptoms manifest in these psychiatric illnesses are being attenuated by pharmacological effect of antidepressants on the immune system.
SSRIs have demonstrated immunomodulatory and anti-inflammatory effects against pro-inflammatory cytokine processes, specifically on the regulation of Interferon-gamma (IFN-gamma) and Interleukin-10 (IL-10), as well as TNF-alpha and Interleukin-6 (IL-6). Antidepressants have also been shown to suppress TH1 upregulation.
Future serotonergic antidepressants may be made to specifically target the immune system by either blocking the actions of pro-inflammatory cytokines or increasing the production of anti-inflammatory cytokines.
SSRIs versus TCAs
SSRIs are described as 'selective' because they affect only the reuptake pumps responsible for serotonin, as opposed to earlier antidepressants, which affect other monoamine neurotransmitters as well, and as a result, SSRIs have fewer side effects.
There appears no significant difference in effectiveness between SSRIs and tricyclic antidepressants, which were the most commonly used class of antidepressants before the development of SSRIs. However, SSRIs have the important advantage that their toxic dose is high, and, therefore, they are much more difficult to use as a means to commit suicide. Further, they have fewer and milder side effects. Tricyclic antidepressant also have a higher risk of serious cardiovascular side effects, which SSRIs lack.
SSRIs versus 5-HT-Prodrugs
Further information: ProdrugsSerotonin cannot be administered directly because when ingested orally, it will not cross the blood–brain barrier, and therefore would have no effect on brain functions. Also, serotonin would activate every synapse it reaches, whereas SSRIs only enhance a signal that is already present, but too weak to come through. The selectivity of the membrane can be reduced for a drug by injecting it in a concentrated sugar solution. The high osmotic pressure of the sugar solution causes the endothelial cells of the capillaries to shrink, which opens gaps between their tight junctions and makes the barrier more permeable. As a result the drug can enter the brain tissue.
SSRIs together with 5-HT-Prodrugs
Biosynthetic serotonin is made from tryptophan, an amino acid. In 1989, the Food and Drug Administration made tryptophan available by prescription only, in response to an outbreak of eosinophilia-myalgia syndrome caused by impure L-tryptophan supplements sold over-the-counter. With current standards, L-tryptophan is again available over the counter in the US as well as supplement 5-HTP, which is a direct precursor to serotonin.
Society and culture
Criticism
See also: Biopsychiatry controversy and Biological psychiatryIn late 2004 media attention was given to a proposed link between SSRI use and juvenile suicide. For this reason, the use of SSRIs in pediatric cases of depression is now recognized by the United States FDA as warranting a cautionary statement to the parents of children who may be prescribed SSRIs by a family doctor. The FDA's currently required packaging insert for SSRIs includes a warning (known as a "black box warning") that a pooled analysis of placebo controlled trials of 9 antidepressant drugs (including multiple SSRIs) resulted in a risk of suicidal behavior that was twice that of placebo. At the same time, in adults SSRIs do not increase the risk of suicide.
Critics of SSRIs claim that the widely disseminated television and print advertising of SSRIs promotes an inaccurate message, oversimplifying what these medications actually do and deceiving the public.
The criticism stems from questions about the validity of claims that SSRIs work by 'correcting' chemical imbalances. Without accurately measuring patients' neurotransmitter levels to allow for continuous monitoring during treatment, it is impossible to know if one is correctly targeting a deficient neurotransmitter (i.e. correcting an imbalance), reaching a desirable level, or even introducing too much of a particular neurotransmitter. Thus it has been argued that SSRIs can actually cause chemical imbalances and abnormal brain states, as evidenced by the fact that many report problems of sexual dysfunction, whose effects last long after the medication has been discontinued. Hence, it is purported that when a patient discontinues an SSRI, they may have a chemical imbalance due to the rapid cessation of the drug that causes the discontinuation syndrome.
One possible mechanism is by inhibition of dopaminergic neurotransmission.
Biopsychiatrists believe that, among other factors, the balance of neurotransmitters in the brain is a biological regulator of mental health. In this theory, emotions within a "normal" spectrum reflect a proper balance of neurochemicals, but abnormally extreme emotions, such as clinical depression, reflect an imbalance. Psychiatrists claim that medications regulate neurotransmitters, and many if not most psychiatrists also claim they treat abnormal personalities by removing a neurochemical excess or replenishing a deficit. On the other hand, Elliot Valenstein, a psychologist and neuroscientist, claims that the broad biochemical assertions and assumptions of mainstream psychiatry are not supported by evidence.
One controversial critic of antidepressants, Peter Breggin, a physician who opposes the overuse of prescription medications to treat patients for mental health issues, predicted iatrogenic issues that SSRIs incur on a significant percentage of patients. Another prominent SSRI critic is David Healy.
A widely reported meta-analysis combined 35 clinical trials submitted to the U.S. Food and Drug Administration (FDA) before licensing of four newer antidepressants (including the SSRIs paroxetine and fluoxetine, and two non-SSRI antidepressants nefazodone and venlafaxine). The authors found that although the antidepressants were statistically superior to placebo they did not exceed the NICE criteria for a 'clinically significant' effect. For more detail, see the section "Efficacy".
A study in The New England Journal of Medicine on a possible publication bias regarding the efficacy of SSRI medications in the treatment of depression suggests that their effectiveness and risk-benefit ratios may be greatly exaggerated. Of 74 studies registered with the United States FDA, 37 with positive results were published in academic journals, while 22 studies with negative results were not published and 11 with negative results were published in a way that conveyed a positive outcome (one positive study was not published and three negative studies were published with results that were portrayed as negative). Overall, 94% of studies actually published were positive outcomes; when published and unpublished studies were included for analysis, the percentage of positive outcomes was 51%.
Although controversial, the existence of an SSRI-related withdrawal syndrome mimicking depression may inflate the therapeutic effect size reported in long-term (more than 6 months) placebo controlled trials of SSRI’s, due to a reliance on randomized discontinuation designs. Discontinuation trials are a variant of the classic 2-arm placebo controlled randomized controlled trials used in shorter placebo controlled studies of SSRI’s.
Regulation
All SSRIs are approved in the U.S. for use with psychiatric disorders as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM IV).
Approved uses for SSRIs vary by country and are determined by the overseeing branch of government in charge of regulating drugs. In the U.S., the Food and Drug Administration (FDA) approves drugs after trial results have been submitted by the pharmaceutical companies. In Europe, drugs can be approved either by the European Medicines Agency for human consumption throughout the European Union or by the regulatory agencies of individual countries for use within those countries.. In Canada, the drug approval process is carried out by Health Canada.
Lawsuits
Hundreds of lawsuits have been filed against drug manufacturers seeking compensation for harm attributed to the use of SSRIs. Suits based on product liability, for example, often allege failure to adequately warn users of potential side effects. Manufacturers have defended many suits on the merits and settled many others. In 2005, the U.S. FDA asked manufacturers to include black box warnings on antidepressant drug packaging. Though a 2007 study purportedly showed that the black box "warnings discouraged use of antidepressants in children and adolescents and... led to increases in suicide rates as a result of untreated depression" an article in the New York Times that ran two weeks later questioned the results of the study, claiming that the data did not support a causal link between the black box warning and increased rates of suicide.
See also
- Antidepressant
- Dopamine reuptake inhibitor (DRI)
- Norepinephrine reuptake inhibitor (NRI)
- Norepinephrine-dopamine reuptake inhibitor (NDRI)
- Reuptake inhibitor
- Serotonin reuptake inhibitor (SRI)
- Serotonin-norepinephrine reuptake inhibitor (SNRI)
- Serotonin-norepinephrine-dopamine reuptake inhibitor (SNDRI)
References
- Barlow, David H. Durand, V. Mark (2009). "Chapter 7: Mood Disorders and Suicide". Abnormal Psychology: An Integrative Approach (Fifth ed.). Belmont, CA: Wadsworth Cengage Learning. p. 239. ISBN 0-495-09556-7. OCLC 192055408.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Preskorn SH, Ross R, Stanga CY (2004). "Selective Serotonin Reuptake Inhibitors". In Sheldon H. Preskorn, Hohn P. Feighner, Christina Y. Stanga and Ruth Ross (ed.). Antidepressants: Past, Present and Future. Berlin: Springer. pp. 241–62. ISBN 978-3-540-43054-4.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Jay C. Fournier, MA; Robert J. DeRubeis, PhD; Steven D. Hollon, PhD; Sona Dimidjian, PhD; Jay D. Amsterdam, MD; Richard C. Shelton, MD; Jan Fawcett, MD (2010). "Antidepressant Drug Effects and Depression Severity". The Journal of the American Medical Association. 303 (1): 47–53. doi:10.1001/jama.2009.1943. PMID 20051569.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kramer, Peter (7 Sept 2011). "In Defense of Antidepressants". The New York Times. Retrieved 13 July 2011.
{{cite news}}: Check date values in:|date=(help) - ^ Ronald Pies, MD (2010). "Antidepressants Work, Sort of-Our System of Care Does Not". Journal of Clinical Psychopharmacology. 30 (2): 101–104. PMID 20520282.
{{cite journal}}: Text "doi:10.1097/JCP.0b013e3181d52dea" ignored (help) Cite error: The named reference "Pies" was defined multiple times with different content (see the help page). - Medford, Nick. "Understanding and treating depersonalization disorder". Advances in Psychiatric Treatment (2005). Retrieved 2011-11-11.
- ^ "www.nice.org.uk" (PDF).
- Depression: The NICE Guideline on the Treatment and Management of Depression in Adults (Updated Edition) (PDF). RCPsych Publications. 2010. ISBN 1-904671-85-3.
- ^ Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT (2008). "Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration". PLoS Medicine. 5 (2): e45. doi:10.1371/journal.pmed.0050045. PMC 2253608. PMID 18303940.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Horder J, Matthews P, Waldmann R (2010). "Placebo, Prozac and PLoS: significant lessons for psychopharmacology". Journal of Psychopharmacology. 25 (10): 1277–88. doi:10.1177/0269881110372544. PMID 20571143.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Fountoulakis KN, Moller H-J (2010). "Efficacy of antidepressants: a re-analysis and re-interpretation of the Kirsch data". International Journal of Neuropsychopharmacology. 14 (3): 1–8. doi:10.1017/S1461145710000957. PMID 20800012.
{{cite journal}}: Unknown parameter|month=ignored (help) - John Kelley (March 2, 2010). "Antidepressants: Do They "Work" or Don't They?". Scientific American.
- "www.nice.org.uk" (PDF).
- Coupland CA, Dhiman P, Barton G; et al. (2011). "A study of the safety and harms of antidepressant drugs for older people: a cohort study using a large primary care database". Health Technol Assess. 15 (28): 1–202, iii–iv. doi:10.3310/hta15280. PMID 21810375.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Gartlehner G, Hansen RA, Morgan LC; et al. (2011). "Comparative benefits and harms of second-generation antidepressants for treating major depressive disorder: an updated meta-analysis". Ann. Intern. Med. 155 (11): 772–85. doi:10.1059/0003-4819-155-11-201112060-00009. PMID 22147715.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "www.nice.org.uk" (PDF). Retrieved 2013-02-20. Cite error: The named reference "urlwww.nice.org.uk" was defined multiple times with different content (see the help page).
- ^ Kapczinski F, Lima MS, Souza JS, Schmitt R (2003). "Antidepressants for generalized anxiety disorder". Cochrane Database Syst Rev (2): CD003592. doi:10.1002/14651858.CD003592. PMID 12804478.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "www.nice.org.uk" (PDF).
- Arroll B, Elley CR, Fishman T; et al. (2009). "Antidepressants versus placebo for depression in primary care". Cochrane Database Syst Rev (3): CD007954. doi:10.1002/14651858.CD007954. PMID 19588448.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - "Medscape Log In".
- ^ "National Guideline Clearinghouse | Practice guideline for the treatment of patients with eating disorders".
- Flament MF, Bissada H, Spettigue W (2012). "Evidence-based pharmacotherapy of eating disorders". Int. J. Neuropsychopharmacol. 15 (2): 189–207. doi:10.1017/S1461145711000381. PMID 21414249.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Mead GE, Hsieh CF, Lee R; et al. (2012). "Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery". Cochrane Database Syst Rev. 11: CD009286. doi:10.1002/14651858.CD009286.pub2. PMID 23152272.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Waldinger MD (2007). "Premature ejaculation: state of the art". The Urologic Clinics of North America. 34 (4): 591–9, vii–viii. doi:10.1016/j.ucl.2007.08.011. PMID 17983899.
{{cite journal}}: Unknown parameter|month=ignored (help) - Waldinger MD, Zwinderman AH, Olivier B (2004). "On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment". European Urology. 46 (4): 510–5, discussion 516. doi:10.1016/j.eururo.2004.05.005. PMID 15363569.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Abdel-Hamid IA, El Naggar EA, El Gilany AH (2001). "Assessment of as needed use of pharmacotherapy and the pause-squeeze technique in premature ejaculation". International Journal of Impotence Research. 13 (1): 41–5. doi:10.1038/sj.ijir.3900630. PMID 11313839.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wang WF, Wang Y, Minhas S, Ralph DJ (2007). "Can sildenafil treat primary premature ejaculation? A prospective clinical study". International Journal of Urology. 14 (4): 331–5. doi:10.1111/j.1442-2042.2007.01606.x. PMID 17470165.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Wu Q, Bencaz AF, Hentz JG, Crowell MD (2012). "Selective serotonin reuptake inhibitor treatment and risk of fractures: a meta-analysis of cohort and case-control studies". Osteoporos Int. 23 (1): 365–75. doi:10.1007/s00198-011-1778-8. PMID 21904950.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - September 23, 2012. "SSRIs and Depression". Emedicinehealth.com. Retrieved 2012-09-23.
{{cite web}}: CS1 maint: numeric names: authors list (link) - A landmark study in the use of anti-depressants and their role in step-therapy can be found in the STAR*D trial.
- Coleman, E. (2011). "Chapter 28. Impulsive/compulsive sexual behavior: Assessment and treatment". In Grant, Jon E.; Potenza, Marc N. (eds.). The Oxford Handbook of Impulse Control Disorders. New York: Oxford University Press. p. 385.
{{cite book}}: Cite has empty unknown parameter:|nopp=(help) - Hu XH, Bull SA, Hunkeler EM; et al. (2004). "Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression: patient report versus physician estimate". The Journal of Clinical Psychiatry. 65 (7): 959–65. doi:10.4088/JCP.v65n0712. PMID 15291685.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Landén M, Högberg P, Thase ME (2005). "Incidence of sexual side effects in refractory depression during treatment with citalopram or paroxetine". The Journal of Clinical Psychiatry. 66 (1): 100–6. doi:10.4088/JCP.v66n0114. PMID 15669895.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Clayton, Anita H. (2003). "Antidepressant-Associated Sexual Dysfunction: A Potentially Avoidable Therapeutic Challenge". Primary Psychiatry. 10 (1): 55–61.
- Kanaly KA, Berman JR (2002). "Sexual side effects of SSRI medications: potential treatment strategies for SSRI-induced female sexual dysfunction". Current Women's Health Reports. 2 (6): 409–16. PMID 12429073.
{{cite journal}}: Unknown parameter|month=ignored (help) - Csoka AB, Bahrick AS, Mehtonen O-P (2008). "Persistent Sexual Dysfunction after Discontinuation of Selective Serotonin Reuptake Inhibitors (SSRIs)". J Sex Med. 5 (1): 227–33. doi:10.1111/j.1743-6109.2007.00630.x. PMID 18173768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Waldinger MD, Olivier B (2004). "Utility of selective serotonin reuptake inhibitors in premature ejaculation". Current Opinion in Investigational Drugs. 5 (7): 743–7. PMID 15298071.
{{cite journal}}: Unknown parameter|month=ignored (help) - Dording CM, Fisher L, Papakostas G; et al. (2008). "A double-blind, randomized, pilot dose-finding study of maca root (L. meyenii) for the management of SSRI-induced sexual dysfunction". CNS Neurosci Ther. 14 (3): 182–91. doi:10.1111/j.1755-5949.2008.00052.x. PMID 18801111.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Huffman, Grace Brooke (1997). "Cardiac effects in patients using SSRI antidepressants - selective serotonin reuptake inhibitor - Tips from Other Journals". American Family Physician.
{{cite web}}: Unknown parameter|month=ignored (help) - Pacher P, Kecskemeti V (2004). "Cardiovascular Side Effects of New Antidepressants and Antipsychotics: New Drugs, old Concerns?". Current Pharmaceutical Design. 10 (20): 2463–75. doi:10.2174/1381612043383872. PMC 2493295. PMID 15320756.
- Goldberg RJ (1998). "Selective serotonin reuptake inhibitors: infrequent medical adverse effects". Archives of Family Medicine. 7 (1): 78–84. doi:10.1001/archfami.7.1.78. PMID 9443704.
- FDA. "FDA Drug Safety".
- "ref2" (PDF). Retrieved 2012-09-23.
- Pacher P, Ungvari Z, Nanasi PP, Furst S, Kecskemeti V (1999). "Speculations on difference between tricyclic and selective serotonin reuptake inhibitor antidepressants on their cardiac effects. Is there any?". Current Medicinal Chemistry. 6 (6): 469–80. PMID 10213794.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - van Broekhoven F, Kan CC, Zitman FG (2002). "Dependence potential of antidepressants compared to benzodiazepines". Prog. Neuropsychopharmacol. Biol. Psychiatry. 26 (5): 939–43. doi:10.1016/S0278-5846(02)00209-9. PMID 12369270.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Stone MB, Jones ML (2006-11-17). "Clinical review: relationship between antidepressant drugs and suicidal behavior in adults" (PDF). Overview for December 13 Meeting of Psychopharmacologic Drugs Advisory Committee (PDAC). FDA. pp. 11–74. Retrieved 2007-09-22. Cite error: The named reference "FDA2" was defined multiple times with different content (see the help page).
- Levenson M, Holland C (2006-11-17). "Statistical Evaluation of Suicidality in Adults Treated with Antidepressants" (PDF). Overview for December 13 Meeting of Psychopharmacologic Drugs Advisory Committee (PDAC). FDA. pp. 75–140. Retrieved 2007-09-22.
- ^ Olfson M, Marcus SC, Shaffer D (2006). "Antidepressant drug therapy and suicide in severely depressed children and adults: A case-control study". Archives of General Psychiatry. 63 (8): 865–72. doi:10.1001/archpsyc.63.8.865. PMID 16894062.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hammad TA (2004-08-116). "Review and evaluation of clinical data. Relationship between psychiatric drugs and pediatric suicidal behavior" (PDF). FDA. pp. 42, 115. Retrieved 2008-05-29.
{{cite web}}: Check date values in:|date=(help) - Hetrick S, Merry S, McKenzie J, Sindahl P, Proctor M (2007). Hetrick, Sarah E (ed.). "Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents". Cochrane Database Syst Rev (3): CD004851. doi:10.1002/14651858.CD004851.pub2. PMID 17636776.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Meta-Analysis of Aggression and/or Hostility-Related Events in Children and Adolescents Treated with Fluoxetine Compared with Placebo Journal of Child and Adolescent Psychopharmacology. October 2007, 17(5): 713-718. doi:10.1089/cap.2006.0138.
- Gibbons RD, Hur K, Bhaumik DK, Mann JJ (2006). "The relationship between antidepressant prescription rates and rate of early adolescent suicide". The American Journal of Psychiatry. 163 (11): 1898–904. doi:10.1176/appi.ajp.163.11.1898. PMID 17074941.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Report of the CSM expert working group on the safety of selective serotonin reuptake inhibitor antidepressants" (PDF). MHRA. 2004-12-01. Retrieved 2007-09-25.
- "Selective Serotonin Reuptake Inhibitors (SSRIs): Overview of regulatory status and CSM advice relating to major depressive disorder (MDD) in children and adolescents including a summary of available safety and efficacy data". MHRA. 2005-09-29. Retrieved 2008-05-29.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - Gunnell D, Saperia J, Ashby D (2005). "Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review". BMJ. 330 (7488): 385. doi:10.1136/bmj.330.7488.385. PMC 549105. PMID 15718537.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Fergusson D, Doucette S, Glass KC; et al. (2005). "Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials". BMJ. 330 (7488): 396. doi:10.1136/bmj.330.7488.396. PMC 549110. PMID 15718539.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Rihmer Z, Akiskal H (2006). "Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries". J Affect Disord. 94 (1–3): 3–13. doi:10.1016/j.jad.2006.04.003. PMID 16712945.
{{cite journal}}: Unknown parameter|month=ignored (help) - Hall WD, Lucke J (2006). "How have the selective serotonin reuptake inhibitor antidepressants affected suicide mortality?". Aust N Z J Psychiatry. 40 (11–12): 941–50. doi:10.1111/j.1440-1614.2006.01917.x. PMID 17054562.
- "FDA Proposes New Warnings About Suicidal Thinking, Behavior in Young Adults Who Take Antidepressant Medications". FDA. 2007-05-02. Retrieved 2008-05-29.
- "www1.mhlw.go.jp" (PDF). Japanese Ministry of Health (in Japanese).
- "Questions and answers: Advice on SSRIs in children from the Committee on Safety of Medicine" (PDF). Medicines and Healthcare products Regulatory Agency.
- Gibbons RD, Brown CH, Hur K; et al. (2007). "Early evidence on the effects of regulators' suicidality warnings on SSRI prescriptions and suicide in children and adolescents". The American Journal of Psychiatry. 164 (9): 1356–63. doi:10.1176/appi.ajp.2007.07030454. PMID 17728420.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Xu J, Kochanek KD, Tejada-Vera B (2009). "Deaths: Preliminary Data for 2007" (PDF). National Vital Statistics Reports. 58 (1): 29–30. Retrieved 2009-09-20.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Heron M, Hoyert DL, Murphy SL; et al. (2009). "Deaths: Final Data for 2006" (PDF). National Vital Statistics Reports. 57 (14): 30. Retrieved 2009-09-20.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Domar, A. D. (31 October 2012). "The risks of selective serotonin reuptake inhibitor use in infertile women: a review of the impact on fertility, pregnancy, neonatal health and beyond". Human Reproduction. doi:10.1093/humrep/des383.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Rahimi, Roja (2006). "Pregnancy outcomes following exposure to serotonin reuptake inhibitors: a meta-analysis of clinical trials". Reproductive Toxicology. 22 (4): 571–575. doi:10.1016/j.reprotox.2006.03.019. PMID 16720091.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - "Breastfeeding Update: SDCBC's quarterly newsletter". Breastfeeding.org. Retrieved 2010-07-10.
- "Using Antidepressants in Breastfeeding Mothers". kellymom.com. Retrieved 2010-07-10.
- Gentile S, Rossi A, Bellantuono C (2007). "SSRIs during breastfeeding: spotlight on milk-to-plasma ratio". Archives of Women's Mental Health. 10 (2): 39–51. doi:10.1007/s00737-007-0173-0. PMID 17294355.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - USA (2012-05-24). "Antidepressant use during pregnancy and ... [Arch Gen Psychiatry. 2011] - PubMed - NCBI". Ncbi.nlm.nih.gov. Retrieved 2012-09-23.
- Medicalnewstoday.com Medical News Today - Lancet Press Release. Feb 05 2005
- Vogel G, Neill D, Hagler M, Kors D (1990). "A new animal model of endogenous depression: a summary of present findings". Neuroscience and Biobehavioral Reviews. 14 (1): 85–91. doi:10.1016/S0149-7634(05)80164-2. PMID 2183099.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Velazquez-Moctezuma J, Aguilar-Garcia A, Diaz-Ruiz O (1993). "Behavioral effects of neonatal treatment with clomipramine, scopolamine, and idazoxan in male rats". Pharmacology, Biochemistry, and Behavior. 46 (1): 215–7. doi:10.1016/0091-3057(93)90343-R. PMID 7902983.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hansen HH, Sánchez C, Meier E (1997). "Neonatal administration of the selective serotonin reuptake inhibitor Lu 10-134-C increases forced swimming-induced immobility in adult rats: a putative animal model of depression?". The Journal of Pharmacology and Experimental Therapeutics. 283 (3): 1333–41. PMID 9400008.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Popa D, Léna C, Alexandre C, Adrien J (2008). "Lasting syndrome of depression produced by reduction in serotonin uptake during postnatal development: evidence from sleep, stress, and behavior". The Journal of Neuroscience. 28 (14): 3546–54. doi:10.1523/JNEUROSCI.4006-07.2008. PMID 18385313.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Maciag D, Simpson KL, Coppinger D; et al. (2006). "Neonatal Antidepressant Exposure has Lasting Effects on Behavior and Serotonin Circuitry". Neuropsychopharmacology. 31 (1): 47–57. doi:10.1038/sj.npp.1300823. PMC 3118509. PMID 16012532.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Maciag D, Williams L, Coppinger D, Paul IA (2006). "Neonatal citalopram exposure produces lasting changes in behavior which are reversed by adult imipramine treatment". European Journal of Pharmacology. 532 (3): 265–9. doi:10.1016/j.ejphar.2005.12.081. PMC 2921633. PMID 16483567.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Holden C (2004). "Neuroscience. Prozac treatment of newborn mice raises anxiety". Science. 306 (5697): 792. doi:10.1126/science.306.5697.792. PMID 15514122.
{{cite journal}}: Unknown parameter|month=ignored (help) - Ansorge MS, Zhou M, Lira A, Hen R, Gingrich JA (2004). "Early-life blockade of the 5-HT transporter alters emotional behavior in adult mice". Science. 306 (5697): 879–81. doi:10.1126/science.1101678. PMID 15514160.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ansorge MS, Morelli E, Gingrich JA (2008). "Inhibition of serotonin but not norepinephrine transport during development produces delayed, persistent perturbations of emotional behaviors in mice". The Journal of Neuroscience. 28 (1): 199–207. doi:10.1523/JNEUROSCI.3973-07.2008. PMID 18171937.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Misri S, Reebye P, Kendrick K; et al. (2006). "Internalizing behaviors in 4-year-old children exposed in utero to psychotropic medications". The American Journal of Psychiatry. 163 (6): 1026–32. doi:10.1176/appi.ajp.163.6.1026. PMID 16741203.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Maciag D, Coppinger D, Paul IA (2006). "Evidence that the deficit in sexual behavior in adult rats neonatally exposed to citalopram is a consequence of 5-HT1 receptor stimulation during development". Brain Research. 1125 (1): 171–5. doi:10.1016/j.brainres.2006.10.009. PMC 1762094. PMID 17101120.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - FDA.gov, FDA Public Health Advisory - Treatment Challenges of Depression in Pregnancy
- , Kieler H, Artama M, Engeland A, Ericsson O, Furu K, Gissler M, Nielsen RB, Norgaard M, Stephansson O, Valdimarsdottir U, Zoega H, Haglund B." Selective serotonin reuptake inhibitors during pregnancy and risk of persistent pulmonary hypertension in the newborn: population based cohort study from the five Nordic countries" BMJ 2012;344:d8012
- ^ Weinrieb, RM (2005 Mar). "Selective serotonin re-uptake inhibitors and the risk of bleeding". Expert opinion on drug safety. 4 (2): 337–44. PMID 15794724.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - http://www.neurology.org/content/early/2012/10/17/WNL.0b013e318271f848.abstract Selective serotonin reuptake inhibitors and brain hemorrhage
- Serebruany VL (2006). "Selective serotonin reuptake inhibitors and increased bleeding risk: are we missing something?". The American Journal of Medicine. 119 (2): 113–6. doi:10.1016/j.amjmed.2005.03.044. PMID 16443409.
{{cite journal}}: Unknown parameter|month=ignored (help) - Halperin D, Reber G (2007). "Influence of antidepressants on hemostasis". Dialogues in Clinical Neuroscience. 9 (1): 47–59. PMC 3181838. PMID 17506225.
- ^ Isbister G, Bowe S, Dawson A, Whyte I (2004). "Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose". J Toxicol Clin Toxicol. 42 (3): 277–85. doi:10.1081/CLT-120037428. PMID 15362595.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Borys D, Setzer S, Ling L, Reisdorf J, Day L, Krenzelok E (1992). "Acute fluoxetine overdose: a report of 234 cases". Am J Emerg Med. 10 (2): 115–20. doi:10.1016/0735-6757(92)90041-U. PMID 1586402.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Oström M, Eriksson A, Thorson J, Spigset O (1996). "Fatal overdose with citalopram". Lancet. 348 (9023): 339–40. doi:10.1016/S0140-6736(05)64513-8. PMID 8709713.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sporer K (1995). "The serotonin syndrome. Implicated drugs, pathophysiology and management". Drug Saf. 13 (2): 94–104. doi:10.2165/00002018-199513020-00004. PMID 7576268.
- September 23, 2012. "SSRIs and Depression". Emedicinehealth.com. Retrieved 2012-09-23.
{{cite web}}: CS1 maint: numeric names: authors list (link) - "Why Painkillers Interfere with Anti-depressants". Healthcentral.com. 2011-04-20. Retrieved 2012-09-23.
- Solomon H. Snyder. "J.L. Warner-Schmidt et.al "Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans" PNAS 2011". Pnas.org. Retrieved 2012-09-23.
- Watson, Cheryl; et al. "Serotonin Regulation by Astrocytes". The FASEB Journal.
{{cite journal}}: Explicit use of et al. in:|first=(help) - Gobbi M, Crespi D, Foddi MC; et al. (1997). "Effects of chronic treatment with fluoxetine and citalopram on 5-HT uptake, 5-HT1B autoreceptors, 5-HT3 and 5-HT4 receptors in rats". Naunyn-Schmiedeberg's Archives of Pharmacology. 356 (1): 22–8. doi:10.1007/PL00005024. PMID 9228186.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eison AS, Mullins UL (1996). "Regulation of central 5-HT2A receptors: a review of in vivo studies". Behavioural Brain Research. 73 (1–2): 177–81. doi:10.1016/0166-4328(96)00092-7. PMID 8788498.
- Kolb, Bryan and Wishaw Ian. An Introduction to Brain and Behavior. New York: Worth Publishers 2006, Print.
- Rasmussen-Torvik LJ, McAlpine DD (2007). "Genetic screening for SSRI drug response among those with major depression: great promise and unseen perils". Depression and Anxiety. 24 (5): 350–7. doi:10.1002/da.20251. PMID 17096399.
- Murphy GM, Kremer C, Rodrigues HE, Schatzberg AF (2003). "Pharmacogenetics of antidepressant medication intolerance". The American Journal of Psychiatry. 160 (10): 1830–5. doi:10.1176/appi.ajp.160.10.1830. PMID 14514498.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Malberg JE, Eisch AJ, Nestler EJ, Duman RS (2000). "Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus". The Journal of Neuroscience. 20 (24): 9104–10. PMID 11124987.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Levkovitz Y, Gil-Ad I, Zeldich E, Dayag M, Weizman A (2005). "Differential induction of apoptosis by antidepressants in glioma and neuroblastoma cell lines: evidence for p-c-Jun, cytochrome c, and caspase-3 involvement". Journal of Molecular Neuroscience. 27 (1): 29–42. doi:10.1385/JMN:27:1:029. PMID 16055945.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Serafeim A, Holder MJ, Grafton G; et al. (2003). "Selective serotonin reuptake inhibitors directly signal for apoptosis in biopsy-like Burkitt lymphoma cells". Blood. 101 (8): 3212–9. doi:10.1182/blood-2002-07-2044. PMID 12515726.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - O'Brien SM, Scully P, Scott LV, Dinan TG (2006). "Cytokine profiles in bipolar affective disorder: focus on acutely ill patients". Journal of Affective Disorders. 90 (2–3): 263–7. doi:10.1016/j.jad.2005.11.015. PMID 16410025.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Obuchowicz E, Marcinowska A, Herman ZS (2005). "". Psychiatria Polska (in Polish). 39 (5): 921–36. PMID 16358592.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hong CJ, Yu YW, Chen TJ, Tsai SJ (2005). "Interleukin-6 genetic polymorphism and Chinese major depression". Neuropsychobiology. 52 (4): 202–5. doi:10.1159/000089003. PMID 16244501.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Elenkov IJ, Iezzoni DG, Daly A, Harris AG, Chrousos GP (2005). "Cytokine dysregulation, inflammation and well-being". Neuroimmunomodulation. 12 (5): 255–69. doi:10.1159/000087104. PMID 16166805.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kubera M, Maes M, Kenis G, Kim YK, Lasoń W (2005). "Effects of serotonin and serotonergic agonists and antagonists on the production of tumor necrosis factor alpha and interleukin-6". Psychiatry Research. 134 (3): 251–8. doi:10.1016/j.psychres.2004.01.014. PMID 15892984.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Diamond M, Kelly JP, Connor TJ (2006). "Antidepressants suppress production of the Th1 cytokine interferon-gamma, independent of monoamine transporter blockade". European Neuropsychopharmacology. 16 (7): 481–90. doi:10.1016/j.euroneuro.2005.11.011. PMID 16388933.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Kubera M, Lin AH, Kenis G, Bosmans E, van Bockstaele D, Maes M (2001). "Anti-Inflammatory effects of antidepressants through suppression of the interferon-gamma/interleukin-10 production ratio". Journal of Clinical Psychopharmacology. 21 (2): 199–206. doi:10.1097/00004714-200104000-00012. PMID 11270917.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Maes M (2001). "The immunoregulatory effects of antidepressants". Human Psychopharmacology. 16 (1): 95–103. doi:10.1002/hup.191. PMID 12404604.
{{cite journal}}: Unknown parameter|month=ignored (help) - Maes M, Kenis G, Kubera M, De Baets M, Steinbusch H, Bosmans E (2005). "The negative immunoregulatory effects of fluoxetine in relation to the cAMP-dependent PKA pathway". International Immunopharmacology. 5 (3): 609–18. doi:10.1016/j.intimp.2004.11.008. PMID 15683856.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - O'Brien SM, Scott LV, Dinan TG (2004). "Cytokines: abnormalities in major depression and implications for pharmacological treatment". Human Psychopharmacology. 19 (6): 397–403. doi:10.1002/hup.609. PMID 15303243.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Anderson IM (2000). "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability". Journal of Affective Disorders. 58 (1): 19–36. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555.
{{cite journal}}: Unknown parameter|month=ignored (help) - Gunnell D, Saperia J, Ashby D (2005). "Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review". BMJ. 330 (7488): 385. doi:10.1136/bmj.330.7488.385. PMC 549105. PMID 15718537.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lacasse JR, Leo J (2005). "Serotonin and Depression: A Disconnect between the Advertisements and the Scientific Literature". PLoS Medicine. 2 (12): e392. doi:10.1371/journal.pmed.0020392. PMC 1277931. PMID 16268734.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - Moncrieff J, Cohen D (2006). "Do Antidepressants Cure or Create Abnormal Brain States?". PLoS Medicine. 3 (7): e240. doi:10.1371/journal.pmed.0030240. PMC 1472553. PMID 16724872.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - Damsa C, Bumb A, Bianchi-Demicheli F; et al. (2004). "'Dopamine-dependent' side effects of selective serotonin reuptake inhibitors: a clinical review". The Journal of Clinical Psychiatry. 65 (8): 1064–8. doi:10.4088/JCP.v65n0806. PMID 15323590.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Valenstein, Elliot S. (1998). Blaming the brain: the truth about drugs and mental health. New York: Free Press. ISBN 0-684-84964-X.
- Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R (2008). "Selective publication of antidepressant trials and its influence on apparent efficacy". The New England Journal of Medicine. 358 (3): 252–60. doi:10.1056/NEJMsa065779. PMID 18199864.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Deshauer D, Moher D, Fergusson D, Moher E, Sampson M, Grimshaw J (2008). "Selective serotonin reuptake inhibitors for unipolar depression: a systematic review of classic long-term randomized controlled trials". CMAJ. 178 (10): 1293–301. doi:10.1503/cmaj.071068. PMC 2335186. PMID 18458261.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Geddes JR, Carney SM, Davies C; et al. (2003). "Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review". Lancet. 361 (9358): 653–61. doi:10.1016/S0140-6736(03)12599-8. PMID 12606176.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Center for Drug Evaluation and Research Antidepressant Use in Children, Adolescents, and Adults. Retrieved September 30, 2008.
- "Early Evidence on the Effects of Regulators' Suicidality Warnings on SSRI Prescriptions and Suicide in Children and Adolescents". Am J Psychiatry. 2007-09-01. Retrieved 2012-06-19.
- "Experts Question Study on Youth Suicide Rates". New York Times. 2007-09-14. Retrieved 2012-06-19.
External links
- PROZAC Product/Prescribing Information at Eli Lilly and Company
- Barry Yeoman Putting Science in the Dock, The Nation at barryyeoman.com
- Serotonin+uptake+inhibitors at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
| Serotonin receptor modulators | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-HT1 |
| ||||||||||||||||||||||||||||||||||||||
| 5-HT2 |
| ||||||||||||||||||||||||||||||||||||||
| 5-HT3–7 |
| ||||||||||||||||||||||||||||||||||||||