Pharmaceutical compound
 | |
| Clinical data | |
|---|---|
| Trade names | Leustatin, Mavenclad, others |
| Other names | 2-Chlorodeoxyadenosine; 2-Chloro-2'-deoxyadenosine; 2-CdA |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a693015 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intravenous, subcutaneous (liquid), by mouth (tablet) |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 100% (i.v.); 37 to 51% (orally) |
| Protein binding | 25% (range 5-50%); up to 20% (orally) |
| Metabolism | Mostly via intracellular kinases; 15-18% is excreted unchanged.
Intravenous and subcutaneous bolus injection: 15-18% is excreted unchanged After oral administration, 25% (±21%) of dose is excreted unchanged in urine and 3.8% as a metabolite. |
| Elimination half-life | Approximately 10 hours after both intravenous infusion and subcutaneous bolus injection ranging from 5.6 to 7.6 hours and 18.4 to 19.7 hours after oral administration, indicative of different elimination phases. |
| Excretion | Urinary |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.164.726 |
| Chemical and physical data | |
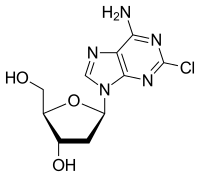
| Formula | C10H12ClN5O3 |
| Molar mass | 285.69 g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Cladribine, sold under the brand name Leustatin, among others, is a medication used to treat hairy cell leukemia (leukemic reticuloendotheliosis) and B-cell chronic lymphocytic leukemia. Cladribine, sold under the brand name Mavenclad, is used for the treatment of adults with highly active forms of relapsing-remitting multiple sclerosis.
Cladribine is a purine analogue that selectively targets and suppresses lymphocytes implicated in the underlying pathogenesis of multiple sclerosis and B-cell leukaemia. Chemically, it mimics the nucleoside deoxyadenosine. However, unlike deoxyadenosine, it is relatively resistant to breakdown by the enzyme adenosine deaminase, which causes it to accumulate in targeted cells and interfere with the cell's ability to process DNA. Cladribine is taken up by cells via transporter proteins. Once inside a cell, cladribine undergoes phosphorylation by the enzyme deoxycytidine kinase (DCK) to produce mononucleotide 2-chlorodeoxyadenosine 5’monophosphate (2-CdAMP), which is subsequently phosphorylated to the triphosphorylated active compound 2-chlorodeoxyadenosine 5’triphosphate (2-CdATP). Activated cladribine is incorporated into cellular DNA, which triggers apoptosis. Accumulation of cladribine into cells is dependent on the ratio of DCK and 5'-nucleotidase (5’-NT), which breaks down and inactivates the compound. This ratio differs between cell types, with high levels in T and B lymphocytes, resulting in selective targeting of these cells. In contrast, DCK:5'NT is relatively low in other cell types, thus sparing numerous non-haematological cells.
It is on the World Health Organization's List of Essential Medicines.
Medical uses
Cladribine is used as a first- and second-line treatment for symptomatic hairy cell leukemia and for B-cell chronic lymphocytic leukaemia, and is administered by intravenous or subcutaneous infusion. Some investigators have used the parenteral formulation orally to treat patients with hairy cell leukemia. About 37–51% of oral cladribine is bioavailable orally. It is used, often in combination with other cytotoxic agents, to treat various kinds of histiocytosis, including Erdheim–Chester disease and Langerhans cell histiocytosis.
Following EMA approval of cladribine tablets for the treatment of adult patients with highly active relapsing-remitting multiple sclerosis in 2017, as of July 2020, cladribine tablets have gained marketing authorisation in over 75 countries. In 2019, cladribine tablets were approved by the FDA for the treatment of relapsing forms of multiple sclerosis, to include relapsing-remitting disease and active secondary progressive disease, in adult patients who have had an inadequate response to, or are unable to tolerate, an alternate drug indicated for the treatment of multiple sclerosis.
Cladribine may cause foetal harm when administered to a pregnant woman and is listed by the FDA as pregnancy category D; safety and efficacy in children has not been established.
Mechanism of action
As a purine analogue, cladribine is taken up into rapidly proliferating cells, including B and T lymphocytes, to be incorporated into DNA synthesis. Chemically, it mimics nucleoside adenosine; however, unlike adenosine, cladribine has a chlorine molecule at position 2, which renders it partially resistant to breakdown by adenosine deaminase. This causes it to accumulate in cells and interfere with the targeted cell's ability to process DNA.
Cladribine is taken up by specific nucleoside transporter proteins. Once inside a cell, cladribine undergoes phosphorylation by the enzyme deoxycytidine kinase (DCK) to produce mononucleotide 2-chlorodeoxyadenosine 5’monophosphate (2-CdAMP), which is subsequently phosphorylated to the triphosphorylated active compound, 2-chlorodeoxyadenosine 5’triphosphate (2-CdATP).
Activated cladribine is incorporated into the DNA synthesis pathway, where it disrupts DNA repair and synthesis, resulting in an accumulation of DNA strand breaks This is followed by the activation of transcription factor p53, the release of cytochrome c from mitochondria and eventual programmed cell death (apoptosis). This process occurs over approximately 2 months, with a peak level of cell depletion 4–8 weeks after treatment.
Another family of enzymes, the 5'-nucleotidase (5'-NT) family, is also capable of dephosphorylating cladribine, making it inactive. The most important subtypes of this group appear to be cytosolic 5'-NT, c-5NCT1A and c-NT1B, which are cytosolically active and specific for purine analogues.
Accumulation of cladribine into cells is dependent on the ratio of DCK and 5'-NT. This ratio differs between cell types, with high levels in T and B lymphocytes, making them particularly susceptible to cell death. The cells with the highest ratios are B cells, especially germinal centre and naïve B cells. This helps to explain which B cells are more vulnerable to cladribine-mediated apoptosis. DCK is the rate-limiting enzyme for conversion of the cladribine prodrug into its active triphosphate form, leading to the selective depletion of dividing and non-dividing T and B lymphocytes. In contrast, the DCK:5'-NT ratio is relatively low in other cell types, thus sparing numerous non-hematologic cells.
In multiple sclerosis, cladribine's effectiveness may be due to depletion of B cells, in particular memory B cells. In the pivotal phase 3 clinical trial of oral cladribine in multiple sclerosis, CLARITY, cladribine selectively depleted 80% of peripheral B cells, compared to only 40–45% of CD4+ T cells and 15‒30% CD8+ T cells. More recently, cladribine has been shown to induce long term, selective suppression of certain subtypes of B cells, especially memory B cells.
Although cladribine is selective for B cells, the long-term suppression of memory B cells, which may contribute to its effect in multiple sclerosis, is not explained by gene or protein expression. Instead, cladribine appears to deplete the entire B cell department, but while naïve B cells rapidly move from lymphoid organs, the memory B cell pool repopulates slowly from the bone marrow. Both hairy cell leukemia and B-cell chronic lymphocytic leukaemia are types of B cell blood cancers.
History in hairy cell leukemia
Ernest Beutler and Dennis A. Carson had studied adenosine deaminase deficiency and recognised that because the lack of adenosine deaminase led to the destruction of B cell lymphocytes, a drug designed to inhibit adenosine deaminase might be useful in lymphomas. Carson then synthesised cladribine, and through clinical research at Scripps starting in the 1980s, Beutler tested it as intravenous infusion and found it was especially useful to treat hairy cell leukemia. No pharmaceutical companies were interested in selling the drug because hairy cell leukemia was an orphan disease, so Beutler's lab synthesised and packaged it and supplied it to the hospital pharmacy; the laboratory also developed a test to monitor blood levels. This was the first treatment that led to prolonged remission of hairy cell leukemia, which was previously untreatable.
In February 1991, Scripps began a collaboration with Johnson & Johnson to bring intravenous cladribine to market, and by December of that year, Johnson & Johnson had filed a new drug application; cladribine was approved by the FDA in 1993 for hairy cell leukemia as an orphan drug, and was approved in Europe later that year.
The subcutaneous formulation was developed in Switzerland in the early 1990s and it was commercialised by Lipomed GmbH in the 2000s.
Safety profile of cladribine in hairy cell leukemia
Injectable cladribine suppresses the body's ability to make new lymphocytes, natural killer cells, and neutrophils (called myelosuppression); data from hairy cell leukemia studies showed that about 70% of people taking the drug developed dangerously low levels of white blood cells and about 30% developed infections and some of those progressed to septic shock; about 40% of people taking the drug had fewer red blood cells and became severely anaemic; and about 10% of people had too few platelets. At the dosage used to treat hairy cell leukemia in two clinical trials, 16% of people had rashes and 22% had nausea, the nausea generally did not lead to vomiting.
History in multiple sclerosis
In the mid-1990s, Beutler, in collaboration with Jack Sipe, a neurologist at Scripps Institute, ran several clinical trials exploring the utility of cladribine in multiple sclerosis, based on the drug's immunosuppressive effects. Sipe's insight into multiple sclerosis, and Beutler's interest in multiple sclerosis due to his sister having the disease, initiated a very productive collaboration. Ortho-Clinical, a subsidiary of Johnson & Johnson, filed a new drug application for cladribine for multiple sclerosis in 1997 but withdrew it in the late 1990s after discussion with the FDA proved that more clinical data would be needed.
Ivax acquired the rights for oral administration of cladribine to treat multiple sclerosis from Scripps in 2000, and partnered with Serono in 2002. Ivax was acquired by Teva in 2006, and Merck KGaA acquired control of Serono's drug business in 2006.
An oral formulation of the drug with cyclodextrin was developed by Ivax and Serono, and then Merck KGaA conducted clinical trials. Merck KGaA submitted an application to the European Medicines Agency in 2009, which was rejected in 2010, and an appeal was denied in 2011. Likewise Merck KGaA's new drug application with the FDA rejected in 2011.
The ratio of benefit to harm was not clear to regulators, and further studies were requested to address concerns related to severe lymphopenia and cancer cases observed during pivotal trials. Clinical studies of multiple sclerosis were still ongoing at the time of the rejections, and Merck KGaA committed to completing them. A meta-analysis of data from clinical trials comparing the risk of cancer and other disease-modifying therapies showed that cladribine tablets did not increase the risk of cancer at the doses used in the initial clinical trials.
Based on the supporting data from the completed clinical trials that confirmed no increased risk of cancer, Merck announced it would again seek regulatory approval. In 2016, the EMA accepted its application for review. On 22 June 2017, the EMA's Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the treatment of relapsing forms of multiple sclerosis.
Cladribine tablets were later approved in Europe, in August 2017, for highly active relapsing-remitting multiple sclerosis, and has since been approved by the FDA for the treatment of relapsing-remitting and secondary progressive multiple sclerosis in the US.
Use in multiple sclerosis
As per the EU label, cladribine tablets are indicated for the treatment of adult patients with highly active relapsing multiple sclerosis as defined by clinical or imaging features: (i) patients with a relapse in the previous year and at least one T1 Gd+ lesion or 9 or more T2 lesions, while on another disease-modifying therapies or (ii) patients with two or more relapses in the previous year, whether on disease-modifying treatment or not.
Two main approaches to multiple sclerosis treatment maintenance therapy are used – immunomodulation and immunosuppression and alternatively, immune reconstitution therapy. Classified as the latter, cladribine tablets are administered intermittently as a short treatment course without continuous immunosuppression. In contrast to maintenance therapies, clinical efficacy extends beyond the dosing period.
Cladribine tablets are administered as 2 courses separated by 1 year (a maximum of 20 days of treatment). The recommended cumulative dose is 3.5 mg/kg weight over 2 years, administered as 1 treatment course of 1.75 mg/kg per year. Each treatment course consists of 2 treatment weeks, one at the beginning of the first month and one at the beginning of the second month of the respective treatment year. Each treatment week consists of 4 or 5 days on which a patient receives 10 mg or 20 mg (1 or 2 tablets) as a single daily dose based on body weight.
Before initiating treatment with cladribine tablets, blood tests, MRI and infection screening must be performed. Due to an increased risk of herpes zoster with cladribine tablets, patients who are antibody-negative for varicella zoster virus are recommended to be vaccinated before starting treatment. Treatment should not be initiated within 4 to 6 weeks of receiving a live or attenuated live vaccine because of a risk of active infection. Vaccination with live or attenuated live vaccines should also be avoided during and after treatment, but can be considered when lymphocyte counts have recovered to ≥1000 cells/mm.
Following completion of the two treatment courses, no further treatment or additional monitoring is required.
The use of cladribine tablets is contraindicated in pregnant women, and women of childbearing potential must use effective contraception to prevent pregnancy during treatment and 6 months after receiving the last dose.
Efficacy of cladribine tablets in multiple sclerosis
Clinical trial results have shown that cladribine tablets can be an effective treatment for highly active, relapsing forms of multiple sclerosis, with significant clinical benefits in relapse rate, disability progression, and radiological measures. Compared with placebo, patients who received cladribine tablets (3.5 mg/kg) in the CLARITY study had a 58% reduction in annualized relapse rate and 47% of patients showed no evidence of disease activity at 2 years. Clinical improvements can be observed at Week 24 of treatment, and benefits may be sustained up to 4 years, beyond the 2-year dosing period and recovery of total lymphocytes. Post-hoc analyses of clinical trial data showed that 89% of patients remained free from disability progression two years after treatment.
Further analyses of a subgroup of patients in the CLARITY study who had very active multiple sclerosis showed a 67% reduction in relapse rates and an 82% reduction in disability progression in those treated with cladribine tablets. Similarly, clinical improvements were seen in lesion burden on MRI scans in this population.
Studies evaluating the treatment effects of cladribine tablets across a spectrum of baseline demographics and disease characteristics showed that the relative risk of relapse was significantly reduced compared with placebo, irrespective of previous treatment experience.
Furthermore, treatment with cladribine tablets has been shown to significantly reduce the rate of brain atrophy in patients with highly active relapsing-remitting multiple sclerosis. This reduction correlated with a reduced risk in disability progression in a retrospective analysis.
In clinical trials, higher cumulative doses of cladribine tablets did not result in further improvement in efficacy nor did additional courses after the 2-year treatment period, but was associated with a higher incidence of Grade 3 and Grade 4 lymphopenia.
Safety profile of cladribine tablets in multiple sclerosis
Cladribine tablets target the cells of the adaptive immune system with minimal impact on innate immune cells. Although the exact mechanism by which cladribine exerts its therapeutic effect is not fully elucidated, it is proposed to have a transient effect on B and T lymphocyte depletion, interrupting the cascade of immune events central to multiple sclerosis. As a result, a reduction in lymphocyte count (lymphopenia) may be reported following treatment. In clinical trials, lymphocyte levels above Grade 0 (≥1000 cells/mm) and Grade 1 (<1000–800 cells/mm) were maintained in most patients, with levels continuing to improve after the 2-year dosing period. Less than 1% of patients developed Grade 4 lymphopenia (<200 cells/mm). It is important that patients with lymphocyte counts below 500 cells/mm should be actively monitored for signs suggestive of infection and that anti-infective treatments are given to at-risk patients.
Despite the initial reduction in lymphocyte counts following treatment, studies showed the overall risk of infection in patients receiving cladribine tablets was comparable to those who received placebo, except for herpes zoster infection. Due to this increased risk, it is recommended that patients are screened for varicella zoster virus and antibody-negative patients are vaccinated prior to receiving treatment. In an analysis of post-approval data, as of 2020, no new infection safety signals were observed in over 18,000 patients.
Progressive multifocal leukoencephalopathy has been reported in patients with hairy cell leukemia treated with parenteral cladribine. However, in up to 10 years of follow-up of patients receiving cladribine tablets for multiple sclerosis, no cases of progressive multifocal leukoencephalopathy have been observed; baseline MRI must be performed prior to initiating treatment.
In clinical trials, malignancies were observed more frequently in patients treated with cladribine tablets compared with patients who received placebo. Compared with a matched reference population from the Global Cancer Observatory database, cladribine tablets had no increased risk of malignancy in long-term real-world evidence data.
Research
Cladribine has been studied as part of a multidrug chemotherapy regimen for drug-resistant T-cell prolymphocytic leukaemia.
References
- "Cladribine". Drugs.com. 28 February 2020. Retrieved 4 March 2020.
- "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- "Neurological therapies". Health Canada. 9 May 2018. Retrieved 13 April 2024.
- "Mavenclad EPAR". European Medicines Agency (EMA). 22 August 2017. Retrieved 26 August 2024.
- Liliemark J (February 1997). "The clinical pharmacokinetics of cladribine". Clinical Pharmacokinetics. 32 (2): 120–131. doi:10.2165/00003088-199732020-00003. PMID 9068927. S2CID 32926069.
- ^ "PRODUCT INFORMATION LITAK© 2 mg/mL solution for injection" (PDF). TGA eBusiness Services. St Leonards, Australia: Orphan Australia Pty. Ltd. 10 May 2010. Retrieved 27 November 2014.
- ^ Giovannoni G (October 2017). "Cladribine to Treat Relapsing Forms of Multiple Sclerosis". Neurotherapeutics. 14 (4): 874–887. doi:10.1007/s13311-017-0573-4. PMC 5722776. PMID 29168160.
- "European Medicines Agency - - Litak". www.ema.europa.eu. 17 September 2018. Archived from the original on 3 August 2018. Retrieved 1 July 2024.
- ^ "Leustat Injection. - Summary of Product Characteristics (SPC) - (eMC)". www.medicines.org.uk. Archived from the original on 3 October 2017. Retrieved 19 August 2016.
- ^ "Mavenclad EU SmPC" (PDF). European Medicines Agency. February 2021.
- ^ Leist TP, Weissert R (2011). "Cladribine: mode of action and implications for treatment of multiple sclerosis". Clinical Neuropharmacology. 34 (1): 28–35. doi:10.1097/WNF.0b013e318204cd90. PMID 21242742. S2CID 43201228.
- Jain P, Pemmaraju N, Ravandi F (June 2014). "Update on the biology and treatment options for hairy cell leukemia". Current Treatment Options in Oncology. 15 (2): 187–209. doi:10.1007/s11864-014-0285-5. PMC 4198068. PMID 24652320.
- World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ "Cladribine- cladribine injection". DailyMed. 31 December 2019. Retrieved 4 March 2020.
- "Erdheim-Chester Disease". Histiocytosis Association. Archived from the original on 6 June 2019.
- Aricò M (June 2016). "Langerhans cell histiocytosis in children: from the bench to bedside for an updated therapy". British Journal of Haematology. 173 (5): 663–670. doi:10.1111/bjh.13955. PMID 26913480.
The combination of cytarabine and cladribine is the current standard for second-line therapy of refractory cases with vital organ dysfunction.
- ^ Rammohan K, Coyle PK, Sylvester E, Galazka A, Dangond F, Grosso M, et al. (December 2020). "The Development of Cladribine Tablets for the Treatment of Multiple Sclerosis: A Comprehensive Review". Drugs. 80 (18): 1901–1928. doi:10.1007/s40265-020-01422-9. PMC 7708385. PMID 33247831.
- Jamroz-Wiśniewska A, Bełtowski J, Wójcicka G, Bartosik-Psujek H, Rejdak K (2020). "Cladribine Treatment Improved Homocysteine Metabolism and Increased Total Serum Antioxidant Activity in Secondary Progressive Multiple Sclerosis Patients". Oxidative Medicine and Cellular Longevity. 2020: 1654754. doi:10.1155/2020/1654754. PMC 7103043. PMID 32256946.
- ^ Johnston JB (June 2011). "Mechanism of action of pentostatin and cladribine in hairy cell leukemia". Leukemia & Lymphoma. 52 (Suppl 2): 43–45. doi:10.3109/10428194.2011.570394. PMID 21463108. S2CID 207508023.
- Beutler E, Piro LD, Saven A, Kay AC, McMillan R, Longmire R, et al. (1991). "2-Chlorodeoxyadenosine (2-CdA): A Potent Chemotherapeutic and Immunosuppressive Nucleoside". Leukemia & Lymphoma. 5 (1): 1–8. doi:10.3109/10428199109068099. PMID 27463204.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Ceronie B, Jacobs BM, Baker D, Dubuisson N, Mao Z, Ammoscato F, et al. (May 2018). "Cladribine treatment of multiple sclerosis is associated with depletion of memory B cells". Journal of Neurology. 265 (5): 1199–1209. doi:10.1007/s00415-018-8830-y. PMC 5937883. PMID 29550884.
{{cite journal}}: CS1 maint: overridden setting (link) - Baker D, Marta M, Pryce G, Giovannoni G, Schmierer K (February 2017). "Memory B Cells are Major Targets for Effective Immunotherapy in Relapsing Multiple Sclerosis". eBioMedicine. 16: 41–50. doi:10.1016/j.ebiom.2017.01.042. PMC 5474520. PMID 28161400.
- Baker D, Herrod SS, Alvarez-Gonzalez C, Zalewski L, Albor C, Schmierer K (July 2017). "Both cladribine and alemtuzumab may effect MS via B-cell depletion". Neurology. 4 (4): e360. doi:10.1212/NXI.0000000000000360. PMC 5459792. PMID 28626781.
- Lichtman MA (2012). "Biographical Memoir: Ernest Beutler 1928–2008" (PDF). National Academy of Sciences.
- Staff (8 March 1993). "Ortho Biotech's Leustatin For Hairy Cell Leukemia". The Pink Sheet. Archived from the original on 3 October 2017.
- ^ "Litak EMA package: Scientific Discussion" (PDF). Europeans Medicines Agency. 2004. Archived from the original (PDF) on 24 September 2015. Retrieved 21 August 2016.
- "Litak: Background Information on the Procedure" (PDF). Europeans Medicines Agency. 2004. Archived from the original (PDF) on 21 August 2016. Retrieved 21 August 2016.
- ^ Sauter E, Ono M. "A potential new MS treatment's long and winding road". News & Views - Scripps Research Institute.
- "Ivax to Develop Cladribine for Multiple Sclerosis". Reuters. 4 December 2000.
- Sargent C (31 October 2002). "Serono Purchases Rights To Experimental MS Drug". Dow Jones Newswires in the Wall Street Journal.
- Bayot J (26 July 2005). "Teva to Acquire Ivax, Another Maker of Generic Drugs". New York Times.
- "Teva Completes Acquisition of Ivax". Teva Press Release. 2006. Archived from the original on 18 December 2019. Retrieved 21 August 2016.
- Staff (21 September 2006). "Merck KGaA to acquire Serono". First Word Pharma.
- ^ "Withdrawal Assessment Report for Movectro" (PDF). Europeans Medicines Agency. 2011. Archived from the original (PDF) on 21 August 2016. Retrieved 21 August 2016.
Procedure No. EMEA/H/C/001197
- ^ Gever J (22 June 2011). "Merck KGaA Throws in Towel on Cladribine for MS".
- Pakpoor J, Disanto G, Altmann DR, Pavitt S, Turner BP, Marta M, et al. (December 2015). "No evidence for higher risk of cancer in patients with multiple sclerosis taking cladribine". Neurology. 2 (6): e158. doi:10.1212/nxi.0000000000000158. PMC 4592538. PMID 26468472.
{{cite journal}}: CS1 maint: overridden setting (link) - "Four years after a transatlantic slapdown, Merck KGaA will once again seek cladribine OK". Fierce Biotech.
- "Merck Receives European Medicines Agency Acceptance for Review of Marketing Authorization Application for Cladribine Tablets". PR News Wire. 18 July 2016.
- Merck. "Cladribine Tablets Receives Positive CHMP Opinion for Treatment of Relapsing Forms of Multiple Sclerosis". www.prnewswire.co.uk. Retrieved 22 August 2017.
- "Cladribine approved in Europe". Merck Press Release. 25 August 2017.
- Sorensen PS, Sellebjerg F (2019). "Pulsed immune reconstitution therapy in multiple sclerosis". Therapeutic Advances in Neurological Disorders. 12: 1756286419836913. doi:10.1177/1756286419836913. PMC 6440030. PMID 30944586.
- Giovannoni G (June 2018). "Disease-modifying treatments for early and advanced multiple sclerosis: a new treatment paradigm". Current Opinion in Neurology. 31 (3): 233–243. doi:10.1097/WCO.0000000000000561. PMID 29634596. S2CID 4736668.
- Baker D, Herrod SS, Alvarez-Gonzalez C, Zalewski L, Albor C, Schmierer K (July 2017). "Both cladribine and alemtuzumab may effect MS via B-cell depletion". Neurology: Neuroimmunology & Neuroinflammation. 4 (4): e360. doi:10.1212/NXI.0000000000000360. PMC 5459792. PMID 28626781.
- ^ Giovannoni G, Soelberg Sorensen P, Cook S, Rammohan K, Rieckmann P, Comi G, et al. (October 2018). "Safety and efficacy of cladribine tablets in patients with relapsing-remitting multiple sclerosis: Results from the randomized extension trial of the CLARITY study". Multiple Sclerosis. 24 (12): 1594–1604. doi:10.1177/1352458517727603. PMID 28870107. S2CID 1910070.
{{cite journal}}: CS1 maint: overridden setting (link) - Giovannoni G, Comi G, Cook S, Rammohan K, Rieckmann P, Soelberg Sørensen P, et al. (February 2010). "A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis". The New England Journal of Medicine. 362 (5): 416–426. doi:10.1056/NEJMoa0902533. PMID 20089960.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Giovannoni G, Cook S, Rammohan K, Rieckmann P, Sørensen PS, Vermersch P, et al. (April 2011). "Sustained disease-activity-free status in patients with relapsing-remitting multiple sclerosis treated with cladribine tablets in the CLARITY study: a post-hoc and subgroup analysis". The Lancet. Neurology. 10 (4): 329–337. doi:10.1016/S1474-4422(11)70023-0. PMID 21397565. S2CID 20149620.
{{cite journal}}: CS1 maint: overridden setting (link) - Comi G, Cook SD, Giovannoni G, Rammohan K, Rieckmann P, Sørensen PS, et al. (April 2013). "MRI outcomes with cladribine tablets for multiple sclerosis in the CLARITY study". Journal of Neurology. 260 (4): 1136–1146. doi:10.1007/s00415-012-6775-0. PMID 23263473. S2CID 8934723.
{{cite journal}}: CS1 maint: overridden setting (link) - Schippling S (2018). "CLARITY: An analysis of severity and frequency of relapses in patients with RRMS treated with cladribine tablets or placebo". Ectrims: 549.
- ^ Comi G, Cook S, Giovannoni G, Rieckmann P, Sørensen PS, Vermersch P, et al. (April 2019). "Effect of cladribine tablets on lymphocyte reduction and repopulation dynamics in patients with relapsing multiple sclerosis". Multiple Sclerosis and Related Disorders. 29: 168–174. doi:10.1016/j.msard.2019.01.038. PMID 30885375. S2CID 83461539.
{{cite journal}}: CS1 maint: overridden setting (link) - Giovannoni G (2017). "Effect of cladribine tablets on relapse rates and the proportions qualified relapse-free in patients with multiple sclerosis: analysis of the CLARITY and CLARITY extension studies". EAN: 0542.
- Giovannoni G, Rammohan K, Cook S, Soelberg-Sørensen P, Vermersch P, Keller B, et al. (2018). "An exploratory analysis of the efficacy of cladribine tablets 3.5mg/kg in patients with relapsing multiple sclerosis stratified according to age above and below 45 years in the CLARITY study". Ectrims: 1204. Archived from the original on 17 July 2021. Retrieved 14 July 2021.
{{cite journal}}: CS1 maint: overridden setting (link) - Giovannoni G, Soelberg Sorensen P, Cook S, Rammohan KW, Rieckmann P, Comi G, et al. (May 2019). "Efficacy of Cladribine Tablets in high disease activity subgroups of patients with relapsing multiple sclerosis: A post hoc analysis of the CLARITY study". Multiple Sclerosis. 25 (6): 819–827. doi:10.1177/1352458518771875. PMC 6460686. PMID 29716436.
{{cite journal}}: CS1 maint: overridden setting (link) - Rammohan K, Giovannoni G, Comi G, Cook S, Rieckmann P, Soelberg Sørensen P, et al. (January 2012). "Cladribine tablets for relapsing-remitting multiple sclerosis: Efficacy across patient subgroups from the phase III CLARITY study". Multiple Sclerosis and Related Disorders. 1 (1): 49–54. doi:10.1016/j.msard.2011.08.006. PMID 25876451.
{{cite journal}}: CS1 maint: overridden setting (link) - De Stefano N, Giorgio A, Battaglini M, De Leucio A, Hicking C, Dangond F, et al. (February 2018). "Reduced brain atrophy rates are associated with lower risk of disability progression in patients with relapsing multiple sclerosis treated with cladribine tablets". Multiple Sclerosis. 24 (2): 222–226. doi:10.1177/1352458517690269. PMC 5818021. PMID 28140753.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Cook S, Leist T, Comi G, Montalban X, Giovannoni G, Nolting A, et al. (April 2019). "Safety of cladribine tablets in the treatment of patients with multiple sclerosis: An integrated analysis". Multiple Sclerosis and Related Disorders. 29: 157–167. doi:10.1016/j.msard.2018.11.021. PMID 30885374. S2CID 81873347.
{{cite journal}}: CS1 maint: overridden setting (link) - Giovannoni G (2020). "A965". Actrims-Ectrims: A965.
- Hasanali ZS, Saroya BS, Stuart A, Shimko S, Evans J, Vinod Shah M, et al. (June 2015). "Epigenetic therapy overcomes treatment resistance in T cell prolymphocytic leukemia". Science Translational Medicine. 7 (293): 293ra102. doi:10.1126/scitranslmed.aaa5079. PMC 4807901. PMID 26109102.
{{cite journal}}: CS1 maint: overridden setting (link)
| Demyelinating diseases of the central nervous system | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Signs and symptoms | |||||||||
| Investigations and diagnosis |
| ||||||||
| Approved treatment | |||||||||
| Other treatments | |||||||||
| Demyelinating diseases |
| ||||||||
| Other | |||||||||
| Merck Serono | |
|---|---|
| Products | |
| Related | |
| Immunosuppressive drugs / Immunosuppressants (L04) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intracellular (initiation) |
| ||||||||||||||
| Intracellular (reception) |
| ||||||||||||||
| Extracellular |
| ||||||||||||||
| Unsorted |
| ||||||||||||||