A 3D cell culture is an artificially created environment in which biological cells are permitted to grow or interact with their surroundings in all three dimensions. Unlike 2D environments (e.g. a Petri dish), a 3D cell culture allows cells in vitro to grow in all directions, similar to how they would in vivo. These three-dimensional cultures are usually grown in bioreactors, small capsules in which the cells can grow into spheroids, or 3D cell colonies. Approximately 300 spheroids are usually cultured per bioreactor.
Background
3D cell cultures have been used in research for several decades. One of the first recorded approaches for their development was at the beginning of the 20th century, with the efforts of Alexis Carrel to develop methods for prolonged in vitro tissue cultures. Early studies in the 80's, led by Mina Bissell from the Lawrence Berkeley National Laboratory, highlighted the importance of 3D techniques for creating accurate in vitro culturing models. This work focused on the importance of the extracellular matrix and the ability of cultures in artificial 3D matrices to produce physiologically relevant multicellular structures, such as acinar structures in healthy and cancerous breast tissue models. These techniques have been applied to in vitro disease models used to evaluate cellular responses to pharmaceutical compounds.
Eric Simon, in a 1988 NIH SBIR grant report, showed that electrospinning could be used to produce nano- and submicron-scale polystyrene and polycarbonate fibrous mats (now known as scaffolds) specifically intended for use as in vitro cell substrates. This early use of electrospun fibrous lattices for cell culture and tissue engineering showed that various cell types including Human Foreskin Fibroblasts (HFF), transformed Human Carcinoma (HEp-2), and Mink Lung Epithelium (MLE) would adhere to and proliferate upon the fibers. It was noted that as opposed to the flattened morphology typically seen in 2D culture, cells grown on the electrospun fibers exhibited a more histotypic rounded 3-dimensional morphology generally observed in vivo.
3D cell culture, by emulating essential aspects of the in vivo environment, including interactions between cells and the extracellular matrix, allows for the faithful recreation of structural architecture and specialized functions in normal tissues or tumors in a laboratory setting. This approach authentically models the conditions and processes of living tissues, producing responses akin to those observed in vivo. Since its inception in the 1970s, 3D cell culture has provided significant insights into the mechanisms regulating tissue homeostasis and cancer. Moreover, it has expedited translational research in the realms of cancer biology and tissue engineering.
Properties
In living tissue, cells exist in 3D microenvironments with intricate cell-cell and cell-matrix interactions and complex transport dynamics for nutrients and cells. Standard 2D, or monolayer, cell cultures are inadequate representations of this environment, which often makes them unreliable predictors of in vivo drug efficacy and toxicity. 3D spheroids more closely resemble in vivo tissue in terms of cellular communication and the development of extracellular matrices. These matrices help the cells to be able to move within their spheroid similar to the way cells would move in living tissue. The spheroids are thus improved models for cell migration, differentiation, survival, and growth. Furthermore, 3D cell cultures provide more accurate depiction of cell polarization, since in 2D, the cells can only be partially polarized. Moreover, cells grown in 3D exhibit different gene expression than those grown in 2D.
The third dimension of cell growth provides more contact space for mechanical inputs and for cell adhesion, which is necessary for integrin ligation, cell contraction and even intracellular signalling. Normal solute diffusion and binding to effector proteins (like growth factors and enzymes) is also reliant on the 3D cellular matrix, so it is critical for the establishment of tissue scale solute concentration gradients
For the purposes of drug toxicology screening, it is much more useful to test gene expression of in vitro cells grown in 3D than 2D, since the gene expression of the 3D spheroids will more closely resemble gene expression in vivo. Lastly, 3D cell cultures have greater stability and longer lifespans than cell cultures in 2D. This means that they are more suitable for long-term studies and for demonstrating long-term effects of the drug. 3D environments also allow the cells to grow undisturbed. In 2D, the cells must undergo regular trypsinization to provide them with sufficient nutrients for normal cell growth. 3D spheroids have been cultured in a lab setting for up to 302 days while still maintaining healthy, non-cancerous growth.
In the interdisciplinary research of biology and aerospace, the 3D printed-scaffolds are also being used for protecting cells from the effect of gravity during the launching.
Classification of 3D culture methods
There are a large number of commercially available culturing tools that claim to provide the advantages of 3D cell culture. In general, the platforms can be classified in two types of 3D culturing methods: scaffold techniques and scaffold-free techniques.
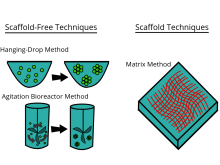
Scaffold techniques
Scaffold techniques include the use of solid scaffolds, hydrogels and other materials. In a recent study potentiality of human CD34+ stem cells explored by generating in vitro agarose gel 3D model to understand the bone ossification process. Scaffolds can be used to generate microtissue 3D model by culturing fibroblasts outside of tumour cells, mimicking the tumor stroma interaction.
The effectiveness of scaffolds in various applications, particularly in tissue engineering, is significantly impacted by factors such as pore distribution, exposed surface area, and porosity. The quantity and arrangement of these elements influence both the depth and rate at which cells penetrate the scaffold volume, the structure of the resulting extracellular matrix, and ultimately, the success of the regenerative process. Scaffolds can be produced with diverse architectures depending on the manufacturing method, leading to either random or precisely designed pore distribution. Recently, advanced computer-controlled rapid prototyping techniques have been employed to create scaffolds with well-organized geometries.
Hydrogels
As the natural extracellular matrix (ECM) is important in the survival, proliferation, differentiation and migration of the cells, different hydrogel matrices mimicking natural ECM structure are considered as potential approaches towards in vivo –like cell culturing. Hydrogels are composed of interconnected pores with high water retention, which enables efficient transport of e.g. nutrients and gases. Several different types of hydrogels from natural and synthetic materials are available for 3D cell culture, including e.g. animal ECM extract hydrogels, protein hydrogels, peptide hydrogels, polymer hydrogels, and wood-based nanocellulose hydrogel.
The approach to crafting the optimal ECM replica relies on the specific characteristics of the culture in question and typically involves employing diverse and independent chemical processes. For example, the utilization of photolabile chemistries can lead to the erosion of specific regions within a gel, and subsequently exposing these areas allows for the application of adhesive ligands, promoting cell adhesion and migration. The development of more intricate frameworks is anticipated, comprising interwoven networks of chemistries under the control of both cells and users. In essence, there is no singular network capable of faithfully emulating the intricate ECM of every tissue type. However, a thoughtful integration of bioinspired cues into synthetic gels holds the potential to yield resilient and versatile scaffolds applicable across various cell culture systems.
Scaffold-free techniques
Scaffold free techniques employ another approach independent from the use scaffold. Scaffold-free methods include e.g. the use of low adhesion plates, hanging drop plates, micropatterned surfaces, and rotating bioreactors, magnetic levitation, and magnetic 3D bioprinting.
Spheroids

Spheroids are a type of three-dimensional cell modeling that better simulate a live cell's environmental conditions compared to a two-dimensional cell model, specifically with the reactions between cells and the reactions between cells and the matrix. Spheroids are useful in the study of changing physiological characteristics of cells, the difference in the structure of healthy cells and tumor cells, and the changes cells undergo when forming a tumor. Spheroids co-cultured with tumor and healthy cells were used to simulate how cancerous cells interact with normal cells. Spheroids can also be co-cultured with fibroblasts to mimic tumor-stroma interaction. Spheroids can be grown with a few different methods. One common method is to use low cell adhesion plates, typically a 96 well plate, to mass-produce spheroid cultures, where the aggregates form in the rounded bottom of the cell plates. Spheroids can also be cultured using the hanging drop method involving forming cell aggregates in drops that hang from the surface of a cell plate. Other methods under investigation include the use of rotating wall vessel bioreactors, which spins and cultures the cells when they are constantly in free fall and forms aggregates in layers Recently, some protocols have been standardized to produce uniform and reliable spheroids. Researchers had also explored standardized, economical and reproducible methods for 3D cell culture. To improve reproducibility and transparency in spheroid experiments, an international consortium developed MISpheroID (Minimal Information in Spheroid Identity).
Clusteroids
clusteroids are a type of three-dimensional cell modeling similar to spheroids but are distinguished by their creation method; grown as clusters of cells in an aqueous two-phase system of water-in-water Pickering emulsion using interfacial tension and osmotic shrinkage to pack the cells into dense clusters which are then cultured in a hydrogel into tissues or organoids.
In the absence of blood vessels, oxygen permeability is impaired during necrotic nucleus formation and this prevents the ex vivo use of 3D cell culture. There is an emulsion template that can overcome this problem. This approach allowed researchers to adjust the cell composition to attain the ideal conditions for promoting the synthesis of diverse angiogenic protein markers within the co-cultured clusteroids. HUVEC cells exhibit a reaction to the presence of Hep-G2 cells and their derivatives by generating endothelial cell sprouts in Matrigel, all without the external introduction of vascular endothelial growth factor (VEGF) or other agents that induce angiogenesis. The replication of this cultivation technique is straightforward for generating various cell co-culture spheroids. The w/w Pickering emulsion template greatly aids in constructing 3D co-culture models, offering significant potential for applications in drug testing and tissue engineering.
Bioreactors
The bioreactors used for 3D cell cultures are small plastic cylindrical chambers that are specifically engineered for the purpose of growing cells in three dimensions. The bioreactor uses bioactive synthetic materials such as polyethylene terephthalate membranes to surround the spheroid cells in an environment that maintains high levels of nutrients. They are easy to open and close, so that cell spheroids can be removed for testing, yet the chamber is able to maintain 100% humidity throughout. This humidity is important to achieve maximum cell growth and function. The bioreactor chamber is part of a larger device that rotates to ensure equal cell growth in each direction across three dimensions.
MC2 Biotek has developed a bioreactor to incubate proto-tissue that uses gas exchange to maintain high oxygen levels within the cell chamber. This is an improvement over previous bioreactors because the higher oxygen levels help the cell grow and undergo normal cell respiration.
Collaborative efforts between tissue engineering (TE) firms, academic institutions, and industrial partners can enhance the transformation of research-oriented bioreactors into efficient commercial manufacturing systems. Academic collaborators contribute foundational aspects, while industrial partners provide essential automation elements, ensuring compliance with regulatory standards and user-friendliness. Established consortia in Europe, such as REMEDI, AUTOBONE, and STEPS, focus on developing automated systems to streamline the engineering of autologous cell-based grafts. The aim is to meet regulatory criteria and ensure cost-effectiveness, making tissue-engineered products more clinically accessible and advancing the translational paradigm of TE from research to a competitive commercial field.
Microfluidics
The utilization of microfluidic technology facilitates the generation of intricate micro-scale structures and the precise manipulation of parameters, thereby emulating the in vivo cellular milieu. The integration of microfluidic technology with 3D cell culture holds considerable potential for applications that seek to replicate in vivo tissue characteristics, notably exemplified by the evolving organ-on-a-chip system. The various cell structures in the human body must be vascularized to receive the nutrients and gas exchange in order to survive. Similarly, 3D cell cultures in vitro require certain levels of fluid circulation, which can be problematic for dense, 3D cultures where cells may not all have adequate exposure to nutrients. This is particularly important in hepatocyte cultures because the liver is a highly vascularized organ. One study cultured hepatocytes and vascular cells together on a collagen gel scaffold between microfluidic channels, and compared growth of cells in static and flowing environments, and showed the need for models with tissues and a microvascular network. Another study showed that hanging-drop based spheroid co-culture device can be useful, generating two different cell spheroids on adjacent channels of microfluidic hanging drop device, and co-culturing spheroids with merging droplets, to monitor tumor-induced angiogenesis.
Microfluidic 3D cell culture, with its potential applications in biomedical research and tissue engineering, is an area of growing interest. However, its advancement is accompanied by several formidable challenges. One such challenge pertains to the difficulty in accessing cultured cells within microsystems, coupled with the intricate nature of sample extraction for subsequent assays. Additionally, the development of methodologies and devices dedicated to in vivo-like cell metabolism and functions study, as well as drug discovery, represents a significant hurdle for microfluidic 3D cell culture devices. Another noteworthy impediment is the limited availability of microfabrication instrumentation in conventional biology laboratories. Moreover, the commercialization of mature and user-friendly microfluidic devices poses a substantial challenge, hindering their accessibility to biologists. Lastly, while biologists often seek high-throughput assay tools with optimal reproducibility, microfluidics encounters technical limitations in meeting these demands, despite the potential feasibility of parallel assays.
High-throughput screening
Advanced development of 3D models for high-throughput screening in high density formats has recently been achievable due to technological achievements related to increased microplate density. These can be found in 384 and 1536-well formats that are cell repellent, cost effective, and amenable to fully automated screening platforms. Two options that afford 1536-well formats are available from either Greiner Bio-One using the m3D Magnetic 3D bioprinting and Corning Life Sciences which incorporates an ultra-low attachment surface coating, along with a microcavity geometry and gravity to create 3D models. Due to the rapid and affordable methods and technologies that have been developed for 3D screening, parallel high-throughput screening approaches to test isogenic pairs of oncogene related mutants versus wildtype have been enabled. Moreover, High-throughput screening techniques play a pivotal role in connecting the realms of pharmacology and toxicology within the framework of 3D cell culture.
Pharmacology and toxicology
A primary purpose of growing cells in 3D scaffolds and as 3D cell spheroids in vitro is to test pharmacokinetic and pharmacodynamic effects of drugs and nanomaterials in preclinical trials. Toxicology studies have shown 3D cell cultures to be nearly on par with in vivo studies for the purposes of testing toxicity of drug compounds. When comparing LD50 values for 6 common drugs: acetaminophen, amiodarone, diclofenac, metformin, phenformin, and valproic acid, the 3D spheroid values correlated directly with those from in vivo studies. Although 2D cell cultures have previously been used to test for toxicity along with in vivo studies, the 3D spheroids are better at testing chronic exposure toxicity because of their longer life spans. The matrix in 3D Spheroids causes cells to maintain actin filaments and is more relevant physiologically in cytoskeletal organization and cell polarity and shape of human cells. The three-dimensional arrangement allows the cultures to provide a model that more accurately resembles human tissue in vivo without using animal test subjects.
The current protocols for evaluating drug candidates and assessing toxicity heavily depend on outcomes derived from early-stage in vitro cell-based assays, with the expectation that these assays faithfully capture critical aspects of in vivo pharmacology and toxicology. Various in vitro designs have been fine-tuned for high throughput to enhance screening efficiency, allowing exhaustive libraries of potential pharmacologically relevant or potentially toxic molecules to undergo scrutiny for cell signals indicative of tissue damage or aligned with therapeutic objectives. Innovative approaches to multiplexed cell-based assay designs, involving the selection of specific cell types, signaling pathways, and reporters, have become standard practice.
Despite these advancements, a considerable percentage of new chemical and biological entities (NCEs/NBEs) encounter setbacks in late-stage human drug testing. Some receive regulatory "black box" warnings, while others are withdrawn from the market due to safety concerns post-regulatory approval. This recurrent pattern underscores the inadequacy of in vitro cell-based assays and subsequent preclinical in vivo studies in furnishing comprehensive pharmacological and toxicity data or reliable predictive capacity for comprehending the in vivo performance of drug candidates.
The absence of a dependable translational assay toolkit for pharmacology and toxicology contributes to the high cost and inefficiency of transitioning from initial in vitro cell-based screens to in vivo testing and subsequent clinical approvals. Particular emphasis is placed on their capacity to retain essential cell and molecular interactions, as well as physiological parameters influencing cell phenotypes and responses to bioactive agents. The distinctive advantages and challenges associated with these models are scrutinized, with a specific focus on their suitability for cell-based assays and their predictive capabilities, crucial for establishing accurate correlations with in vivo mechanisms of drug toxicity.
While assessing safety and efficacy, these models are well equipped to model a wide range of disease states. Each of these models has advantages and limitations that require model development and data interpretation. Public-private partnerships are critical to advance and stimulate research in this area.
Criticisms
Existing 3D methods are not without limitations, including scalability, reproducibility, sensitivity, and compatibility with high-throughput screening (HTS) instruments. Cell-based HTS relies on rapid determination of cellular response to drug interaction, such as dose dependent cell viability, cell-cell/cell-matrix interaction, and/or cell migration, but the available assays are not optimized for 3D cell culturing. Another challenge faced by 3D cell culturing is the limited amount of data and publications that address mechanisms and correlations of drug interaction, cell differentiation, and cell-signalling in these 3D environments. None of the 3D methods have yet replaced 2D culturing on a large scale, including in the drug development process; although the number of 3D cell culturing publications is increasing rapidly, the current limited biochemical characterization of 3D tissue diminishes the adoption of new methods.
Drug-induced liver injury (DILI) stands as a primary cause of compound attrition in the pharmaceutical realm during the course of drug development. To preemptively assess the toxicity of compounds before embarking on laboratory animal testing, a range of in-vitro cell culture toxicity assays has been employed over the years. While two-dimensional (2D) in-vitro cell culture models are commonly utilized and have contributed significantly to our understanding, they frequently exhibit limitations in faithfully replicating the natural structures of in-vivo tissues. Although the most logical testing method involves humans, ethical constraints associated with human trials pose significant challenges. Consequently, there is a pressing need for enhanced human-relevant and predictive models to overcome these limitations.
The past decade has witnessed substantial endeavors aimed at advancing three-dimensional (3D) in-vitro cell culture models to better emulate in-vivo physiological conditions. The intrinsic advantages of 3D cell culture lie in its ability to represent cellular interactions akin to those in-vivo. When appropriately validated, 3D cell culture models can serve as a pivotal intermediary, bridging the gap between conventional 2D cell culture models and in-vivo animal models. This review endeavors to offer a comprehensive overview of the challenges associated with the sensitivity of biomarkers employed in detecting DILI during drug development. Additionally, it explores the potential of 3D cell culture models to address the existing gaps in the current paradigm, offering a promising avenue for more accurate toxicity assessments.
There are also problems using spheroids as a model for cancerous tissue. Although beneficial for 3D tissue culture, tumor spheroids have been criticized for being challenging or impossible to "manipulate gradients of soluble molecules in constructs, and to characterize cells in these complex gradients", unlike the paper-supported 3D cell culture for tissue-based bioassays explored by Ratmir et al. Further challenges associated with complex 3D cell culture techniques include: imaging due to large scaffold sizes and incompatibility with many fluorescence microscopes, flow cytometry because it requires the dissociation of spheroids into a single-cell suspension, and the automation of liquid handling.
2D models cannot study cell-cell and cell-matrix interactions. As a result of the scarcity of preclinical models relevant to 2D cultures, 3D culture provides a pathophysiological microenvironment and has the potential to play a role in cancer drug discovery.
Tissue engineering requires 3D cellular scaffolds. As biomaterials, various natural and synthetic polymer hydrogels have been used by scientists to design 3D scaffolds. Since this barrier is a structure that mimics the natural ECM microenvironment, synthetic scaffolds may be more useful for studying specific tumorigenic steps. Finally, it is suggested that the most suitable three-dimensional models should be carefully selected according to specific targets.
See also
- Cell culture
- Cell lines
- Cell culture assay
- Hydrogel
- Madin-Darby Canine Kidney cell line
- Microphysiometry
References
- ^ Fey S, Wrzesinski K (2013). "Determination of Acute Lethal and Chronic Lethal Thresholds of Valproic Acid Using 3D Spheroids Constructed From the Immortal Human Hepatocyte Cell Line HEPG2/C3A" (PDF). In Boucher A (ed.). Valproic Acid. Nova Science Publishers, Inc. pp. 141–165. ISBN 978-1-62417-952-5. Archived from the original (PDF) on 2 December 2013.
- Mapanao AK, Voliani V (June 2020). "Three-dimensional tumor models: Promoting breakthroughs in nanotheranostics translational research". Applied Materials Today. 19: 100552. doi:10.1016/j.apmt.2019.100552. S2CID 213634060.
- Carrel A (May 1912). "On the Permanent Life of Tissues Outside of the Organisms". The Journal of Experimental Medicine. 15 (5): 516–28. doi:10.1084/jem.15.5.516. PMC 2124948. PMID 19867545.
- MERIT Award Recipient: Mina J. Bissell, Ph.D. (n.d.). Retrieved 16 June 2016, from http://www.cancer.gov/research/nci-role/spotlight/merit/Bissell Archived 17 September 2020 at the Wayback Machine
- Simon, Eric M. (1988). "NIH Phase I Final Report: Fibrous Substrates for Cell Culture (R3RR03544A) (PDF Download Available)". ResearchGate. Retrieved 22 May 2017.
- Xu Q, Yan M, Tang Y (2023). "3D-Autologous Culture Method for Precision Oncology". Cancer Systems and Integrative Biology. Methods Mol Biol. Vol. 2660. pp. 61–68. doi:10.1007/978-1-0716-3163-8_5. ISBN 978-1-0716-3162-1. PMID 37191790.
- Koledova Z (2017). "3D Cell Culture: An Introduction". 3D Cell Culture. Methods Mol Biol. Vol. 1612. pp. 1–11. doi:10.1007/978-1-4939-7021-6_1. ISBN 978-1-4939-7019-3. PMID 28634931.
- Marx, Vivien (11 April 2013). "A Better Brew" (PDF). Nature. Retrieved 9 July 2013.
- Souza GR, Molina JR, Raphael RM, Ozawa MG, Stark DJ, Levin CS, et al. (April 2010). "Three-dimensional tissue culture based on magnetic cell levitation". Nature Nanotechnology. 5 (4): 291–6. Bibcode:2010NatNa...5..291S. doi:10.1038/nnano.2010.23. PMC 4487889. PMID 20228788.
- ^ Pampaloni F, Reynaud EG, Stelzer EH (October 2007). "The third dimension bridges the gap between cell culture and live tissue". Nature Reviews Molecular Cell Biology. 8 (10): 839–45. doi:10.1038/nrm2236. PMID 17684528. S2CID 23837249.
- Chun TH, Hotary KB, Sabeh F, Saltiel AR, Allen ED, Weiss SJ (May 2006). "A pericellular collagenase directs the 3-dimensional development of white adipose tissue". Cell. 125 (3): 577–91. doi:10.1016/j.cell.2006.02.050. PMID 16678100. S2CID 15822397.
- ^ Yamada KM, Cukierman E (August 2007). "Modeling tissue morphogenesis and cancer in 3D". Cell. 130 (4): 601–10. doi:10.1016/j.cell.2007.08.006. PMID 17719539. S2CID 9233152.
- Friedrich J, Seidel C, Ebner R, Kunz-Schughart LA (12 February 2009). "Spheroid-based drug screen: considerations and practical approach". Nature Protocols. 4 (3): 309–24. doi:10.1038/nprot.2008.226. PMID 19214182. S2CID 21783074.
- ^ Prestwich GD (August 2007). "Simplifying the extracellular matrix for 3-D cell culture and tissue engineering: a pragmatic approach". Journal of Cellular Biochemistry. 101 (6): 1370–83. doi:10.1002/jcb.21386. PMID 17492655. S2CID 45152239.
- ^ Griffith LG, Swartz MA (March 2006). "Capturing complex 3D tissue physiology in vitro". Nature Reviews Molecular Cell Biology. 7 (3): 211–24. doi:10.1038/nrm1858. PMID 16496023. S2CID 34783641.
- Lee J, Cuddihy MJ, Kotov NA (March 2008). "Three-dimensional cell culture matrices: state of the art" (PDF). Tissue Engineering. Part B, Reviews. 14 (1): 61–86. doi:10.1089/teb.2007.0150. hdl:2027.42/63369. PMID 18454635.
- Haycock JW (2011). "3D Cell Culture: A Review of Current Approaches and Techniques". 3D Cell Culture. Methods in Molecular Biology. Vol. 695. pp. 1–15. doi:10.1007/978-1-60761-984-0_1. ISBN 978-1-60761-983-3. PMID 21042962.
- Suuronen EJ, Sheardown H, Newman KD, McLaughlin CR, Griffith M (2005). "Building in vitro models of organs". A Survey of Cell Biology. International Review of Cytology. Vol. 244. pp. 137–73. doi:10.1016/s0074-7696(05)44004-8. ISBN 9780123646484. PMID 16157180.
- Louekari K (October 2004). "Status and prospects of in vitro tests in risk assessment". Alternatives to Laboratory Animals. 32 (4): 431–5. doi:10.1177/026119290403200416. PMID 15651929. S2CID 25708371.
- Knight B, Laukaitis C, Akhtar N, Hotchin NA, Edlund M, Horwitz AR (May 2000). "Visualizing muscle cell migration in situ". Current Biology. 10 (10): 576–85. Bibcode:2000CBio...10..576K. doi:10.1016/s0960-9822(00)00486-3. PMID 10837222. S2CID 5830501.
- Roskelley CD, Desprez PY, Bissell MJ (December 1994). "Extracellular matrix-dependent tissue-specific gene expression in mammary epithelial cells requires both physical and biochemical signal transduction". Proceedings of the National Academy of Sciences of the United States of America. 91 (26): 12378–82. Bibcode:1994PNAS...9112378R. doi:10.1073/pnas.91.26.12378. PMC 45441. PMID 7528920.
- ^ Wrzesinski K, Magnone MC, Hansen LV, Kruse ME, Bergauer T, Bobadilla M, Gubler M, Mizrahi J, Zhang K, Andreasen CM, Joensen KE (2013). "HepG2/C3A spheroids exhibit stable physiological functionality for at least 24 days after recovering from trypsinisation". Toxicol. Res. 2 (3): 163–172. doi:10.1039/C3TX20086H.
- "After trypsinisation, 3D spheroids of C3A hepatocytes need 18 days to re-establish similar levels of key physiological functions to those seen in the liver" (PDF). Archived from the original (PDF) on 2 April 2015. Retrieved 25 November 2013.
- Han, Y; Zeger, L; Tripathi, R; Egli, M; Ille, F; Lockowandt, C; Florin, G; Atic, E; Redwan, IN; Fredriksson, R; Kozlova, EN (October 2021). "Molecular genetic analysis of neural stem cells after space flight and simulated microgravity on earth". Biotechnology and Bioengineering. 118 (10): 3832–46. doi:10.1002/bit.27858. PMID 34125436. S2CID 235425528.
- Srikanth L, Sunitha MM, Kumar PS, Chandrasekhar C, Vengamma B, Sarma PV (November 2016). "+ stem cells". Molecular Biology Reports. 43 (11): 1233–42. doi:10.1007/s11033-016-4053-4. PMID 27497820. S2CID 13230517.
- Pednekar, Kunal P.; Heinrich, Marcel A.; van Baarlen, Joop; Prakash, Jai (6 October 2021). "Novel 3D µtissues Mimicking the Fibrotic Stroma in Pancreatic Cancer to Study Cellular Interactions and Stroma-Modulating Therapeutics". Cancers. 13 (19): 5006. doi:10.3390/cancers13195006. PMC 8508009. PMID 34638490.
- Wang H, van Blitterswijk CA (May 2010). "The role of three-dimensional polymeric scaffold configuration on the uniformity of connective tissue formation by adipose stromal cells". Biomaterials. 31 (15): 4322–9. doi:10.1016/j.biomaterials.2010.02.008. PMID 20199809.
- Melchels FP, Barradas AM, van Blitterswijk CA, de Boer J, Feijen J, Grijpma DW (November 2010). "Effects of the architecture of tissue engineering scaffolds on cell seeding and culturing" (PDF). Acta Biomater. 6 (11): 4208–17. doi:10.1016/j.actbio.2010.06.012. PMID 20561602.
- Carletti E, Motta A, Migliaresi C (2011). "Scaffolds for tissue engineering and 3D cell culture". 3D Cell Culture. Methods Mol Biol. Vol. 695. pp. 17–39. doi:10.1007/978-1-60761-984-0_2. ISBN 978-1-60761-983-3. PMID 21042963.
- Sadat-Shojai M (2018). "Controlled pattern of cell growth in modulated protein nanocomplexes: Regulating cells spreading in three dimensions". Materials Today. 21 (6): 686–8. doi:10.1016/j.mattod.2018.06.003. S2CID 139837561.
- Tibbitt MW, Anseth KS (July 2009). "Hydrogels as extracellular matrix mimics for 3D cell culture". Biotechnology and Bioengineering. 103 (4): 655–63. doi:10.1002/bit.22361. PMC 2997742. PMID 19472329.
- Geckil H, Xu F, Zhang X, Moon S, Demirci U (April 2010). "Engineering hydrogels as extracellular matrix mimics". Nanomedicine. 5 (3). London, England: 469–84. doi:10.2217/nnm.10.12. PMC 2892416. PMID 20394538.
- Birgersdotter A, Sandberg R, Ernberg I (October 2005). "Gene expression perturbation in vitro—a growing case for three-dimensional (3D) culture systems". Semin Cancer Biol. 15 (5): 405–12. doi:10.1016/j.semcancer.2005.06.009. PMID 16055341.
- Barralet JE, Wang L, Lawson M, Triffitt JT, Cooper PR, Shelton RM (June 2005). "Comparison of bone marrow cell growth on 2D and 3D alginate hydrogels". J Mater Sci Mater Med. 16 (6): 515–9. doi:10.1007/s10856-005-0526-z. PMID 15928866.
- ^ Tibbitt MW, Anseth KS (July 2009). "Hydrogels as extracellular matrix mimics for 3D cell culture". Biotechnol Bioeng. 103 (4): 655–63. doi:10.1002/bit.22361. PMC 2997742. PMID 19472329.
- ^ Xiang X, Phung Y, Feng M, Nagashima K, Zhang J, Broaddus VC, et al. (January 2011). "The development and characterization of a human mesothelioma in vitro 3D model to investigate immunotoxin therapy". PLOS ONE. 6 (1): e14640. Bibcode:2011PLoSO...614640X. doi:10.1371/journal.pone.0014640. PMC 3031536. PMID 21305058.
- ^ Fennema E, Rivron N, Rouwkema J, van Blitterswijk C, de Boer J (February 2013). "Spheroid culture as a tool for creating 3D complex tissues" (PDF). Trends in Biotechnology. 31 (2): 108–15. doi:10.1016/j.tibtech.2012.12.003. PMID 23336996.
- Jiang Y, Pjesivac-Grbovic J, Cantrell C, Freyer JP (December 2005). "A multiscale model for avascular tumor growth". Biophysical Journal. 89 (6): 3884–94. Bibcode:2005BpJ....89.3884J. doi:10.1529/biophysj.105.060640. PMC 1366955. PMID 16199495.
- Guttilla IK, Phoenix KN, Hong X, Tirnauer JS, Claffey KP, White BA (February 2012). "Prolonged mammosphere culture of MCF-7 cells induces an EMT and repression of the estrogen receptor by microRNAs". Breast Cancer Research and Treatment. 132 (1): 75–85. doi:10.1007/s10549-011-1534-y. PMID 21553120. S2CID 6930899.
- Kunz-Schughart LA, Heyder P, Schroeder J, Knuechel R (May 2001). "A heterologous 3-D coculture model of breast tumor cells and fibroblasts to study tumor-associated fibroblast differentiation". Experimental Cell Research. 266 (1): 74–86. doi:10.1006/excr.2001.5210. PMID 11339826.
- Priwitaningrum, Dwi L.; Blondé, Jean-Baptiste G.; Sridhar, Adithya; van Baarlen, Joop; Hennink, Wim E.; Storm, Gert; Le Gac, Séverine; Prakash, Jai (December 2016). "Tumor stroma-containing 3D spheroid arrays: A tool to study nanoparticle penetration". Journal of Controlled Release. 244 (Pt B): 257–268. doi:10.1016/j.jconrel.2016.09.004. hdl:1874/346099. PMID 27616660.
- Phung YT, Barbone D, Broaddus VC, Ho M (2011). "Rapid generation of in vitro multicellular spheroids for the study of monoclonal antibody therapy". Journal of Cancer. 2: 507–14. doi:10.7150/jca.2.507. PMC 3204399. PMID 22043235.
- Tung YC, Hsiao AY, Allen SG, Torisawa YS, Ho M, Takayama S (February 2011). "High-throughput 3D spheroid culture and drug testing using a 384 hanging drop array". The Analyst. 136 (3): 473–8. Bibcode:2011Ana...136..473T. doi:10.1039/c0an00609b. PMC 7454010. PMID 20967331.
- Xu X, Farach-Carson MC, Jia X (November 2014). "Three-dimensional in vitro tumor models for cancer research and drug evaluation". Biotechnology Advances. 32 (7): 1256–68. doi:10.1016/j.biotechadv.2014.07.009. PMC 4171250. PMID 25116894.
- Santi, Melissa; Mapanao, Ana Katrina; Cappello, Valentina; Voliani, Valerio (1 July 2020). "Production of 3D tumor models of head and neck squamous cell carcinomas for nanotheranostics assessment". ACS Biomaterials Science & Engineering. 6 (9): 4862–9. doi:10.1021/acsbiomaterials.0c00617. PMC 7735655. PMID 33395269.
- Tan, Loh Teng Hern; Low, Liang Ee; Tang, Siah Ying; Yap, Wei Hsum; Chuah, Lay Hong; Chan, Chim Kei; Lee, Learn Han; Goh, Bey Hing (2019). "A reliable and affordable 3D tumor spheroid model for natural product drug discovery: A case study of curcumin". Progress in Drug Discovery & Biomedical Science. 2. doi:10.36877/pddbs.a0000017.
- Peirsman, Arne; Blondeel, Eva; Ahmed, Tasdiq; Anckaert, Jasper; Audenaert, Dominique; Boterberg, Tom; Buzas, Krisztina; Carragher, Neil; Castellani, Gastone; Castro, Flávia; Dangles-Marie, Virginie (1 November 2021). "MISpheroID: a knowledgebase and transparency tool for minimum information in spheroid identity". Nature Methods. 18 (11): 1294–1303. doi:10.1038/s41592-021-01291-4. PMC 8566242. PMID 34725485.
- Celik; Dominici; Filby; Das; Madden; Paunov (11 July 2019). "Fabrication of Human Keratinocyte Cell Clusters for Skin Graft Applications by Templating Water-in-Water Pickering Emulsions". Biomimetics. 4 (3): 50. doi:10.3390/biomimetics4030050. PMC 6784416. PMID 31336810.
- ^ Wang A, Madden LA, Paunov VN (2020). "High-throughput fabrication of hepatic cell clusteroids with enhanced growth and functionality for tissue engineering applications". Mater. Adv. 1 (8): 3022–32. doi:10.1039/D0MA00635A.
- Chiew GG, Fu A, Perng Low K, Qian Luo K (2015). "Physical supports from liver cancer cells are essential for differentiation and remodeling of endothelial cells in a HepG2-HUVEC co-culture model". Sci. Rep. 5 (1): 10801. Bibcode:2015NatSR...510801C. doi:10.1038/srep10801. PMC 4459107. PMID 26053957.
- Lasli S, Kim HJ, Lee K, Suurmond CE, Goudie M, Bandaru P, Sun W, Zhang S, Zhang N, Ahadian S, Dokmeci MR, Lee J, Khademhosseini A (August 2019). "A Human Liver-on-a-Chip Platform for Modeling Nonalcoholic Fatty Liver Disease". Adv Biosyst. 3 (8): e1900104. doi:10.1002/adbi.201900104. PMC 7473489. PMID 32648699.
- Wang A, Weldrick PJ, Madden LA, Paunov VN (May 2021). "Biofilm-Infected Human Clusteroid Three-Dimensional Coculture Platform to Replace Animal Models in Testing Antimicrobial Nanotechnologies". ACS Appl Mater Interfaces. 13 (19): 22182–22194. doi:10.1021/acsami.1c02679. PMID 33956425.
- Wang A, Madden LA, Paunov VN (March 2022). "Vascularized Co-Culture Clusteroids of Primary Endothelial and Hep-G2 Cells Based on Aqueous Two-Phase Pickering Emulsions". Bioengineering. 9 (3): 126. doi:10.3390/bioengineering9030126. PMC 8945860. PMID 35324815.
- Du Y, Han R, Wen F, Ng San San S, Xia L, Wohland T, et al. (January 2008). "Synthetic sandwich culture of 3D hepatocyte monolayer". Biomaterials. 29 (3): 290–301. doi:10.1016/j.biomaterials.2007.09.016. PMID 17964646.
- ^ Derda R, Laromaine A, Mammoto A, Tang SK, Mammoto T, Ingber DE, Whitesides GM (November 2009). "Paper-supported 3D cell culture for tissue-based bioassays". Proceedings of the National Academy of Sciences of the United States of America. 106 (44): 18457–62. Bibcode:2009PNAS..10618457D. doi:10.1073/pnas.0910666106. PMC 2773961. PMID 19846768.
- Fey, Stephen J. "WO2012022351". European Patent Register.
- Freed LE, Vunjak-Novakovic G (2002). "Spaceflight bioreactor studies of cells and tissues". Adv Space Biol Med. Advances in Space Biology and Medicine. 8: 177–95. doi:10.1016/s1569-2574(02)08019-x. ISBN 978-0-444-50735-8. PMID 12951697.
- Wendt D, Riboldi SA, Cioffi M, Martin I (2009). "Bioreactors in tissue engineering: scientific challenges and clinical perspectives". Bioreactor Systems for Tissue Engineering. Advances in Biochemical Engineering/Biotechnology. Vol. 112. pp. 1–27. Bibcode:2009bste.book....1W. doi:10.1007/978-3-540-69357-4_1. ISBN 978-3-540-69356-7. PMID 19290495.
- Schmid J, Schwarz S, Meier-Staude R, Sudhop S, Clausen-Schaumann H, Schieker M, Huber R (October 2018). "A Perfusion Bioreactor System for Cell Seeding and Oxygen-Controlled Cultivation of Three-Dimensional Cell Cultures". Tissue Eng Part C Methods. 24 (10): 585–595. doi:10.1089/ten.TEC.2018.0204. PMC 6208160. PMID 30234443.
- Wendt D, Riboldi SA, Cioffi M, Martin I (September 2009). "Potential and bottlenecks of bioreactors in 3D cell culture and tissue manufacturing". Adv Mater. 21 (32–33): 3352–67. Bibcode:2009AdM....21.3352W. doi:10.1002/adma.200802748. PMID 20882502.
- Li XJ, Valadez AV, Zuo P, Nie Z (June 2012). "Microfluidic 3D cell culture: potential application for tissue-based bioassays". Bioanalysis. 4 (12): 1509–25. doi:10.4155/bio.12.133. PMC 3909686. PMID 22793034.
- Sudo R, Chung S, Zervantonakis IK, Vickerman V, Toshimitsu Y, Griffith LG, Kamm RD (July 2009). "Transport-mediated angiogenesis in 3D epithelial coculture". FASEB Journal. 23 (7): 2155–64. doi:10.1096/fj.08-122820. PMC 2718841. PMID 19246488.
- Rodoplu, Didem; Matahum, Jefunnie Sierra; Hsu, Chia-Hsien (29 March 2022). "A microfluidic hanging drop-based spheroid co-culture platform for probing tumor angiogenesis". Lab on a Chip. 22 (7): 1275–85. doi:10.1039/D1LC01177D. PMID 35191460. S2CID 247024765.
- Marimuthu M, Kim S (June 2011). "Microfluidic cell coculture methods for understanding cell biology, analyzing bio/pharmaceuticals, and developing tissue constructs". Anal Biochem. 413 (2): 81–9. doi:10.1016/j.ab.2011.02.027. PMID 21354094.
- Elliott NT, Yuan F (January 2011). "A review of three-dimensional in vitro tissue models for drug discovery and transport studies". J Pharm Sci. 100 (1): 59–74. doi:10.1002/jps.22257. PMID 20533556.
- Chen SY, Hung PJ, Lee PJ (August 2011). "Microfluidic array for three-dimensional perfusion culture of human mammary epithelial cells". Biomed Microdevices. 13 (4): 753–8. doi:10.1007/s10544-011-9545-3. PMID 21556741.
- Musick K, Khatami D, Wheeler BC (July 2009). "Three-dimensional micro-electrode array for recording dissociated neuronal cultures". Lab Chip. 9 (14): 2036–42. doi:10.1039/b820596e. PMC 2818679. PMID 19568672.
- Malik M, Yang Y, Fathi P, Mahler GJ, Esch MB (2021). "Critical Considerations for the Design of Multi-Organ Microphysiological Systems (MPS)". Front Cell Dev Biol. 9: 721338. doi:10.3389/fcell.2021.721338. PMC 8459628. PMID 34568333.
- Baillargeon, P; Shumate, J; Hou, S; Fernandez-Vega, V; Marques, N; Souza, G; et al. (2019). "Automating a Magnetic 3D Spheroid Model Technology for High-Throughput Screening". SLAS Technol. 24 (4): 420–8. doi:10.1177/2472630319854337. PMC 7704036. PMID 31225974.
- Hou, S; Tiriac, H; Sridharan, BP; Scampavia, L; Madoux, F; Seldin, J; et al. (2018). "Advanced Development of Primary Pancreatic Organoid Tumor Models for High-Throughput Phenotypic Drug Screening". SLAS Discov. 23 (6): 574–584. doi:10.1177/2472555218766842. PMC 6013403. PMID 29673279.
- Madoux, F; Tanner, A; Vessels, M; Willetts, L; Hou, S; Scampavia, L; et al. (2017). "A 1536-Well 3D Viability Assay to Assess the Cytotoxic Effect of Drugs on Spheroids". SLAS Discov. 22 (5): 516–524. doi:10.1177/2472555216686308. PMID 28346088.
- Quereda, V; Hou, S; Madoux, F; Scampavia, L; Spicer, TP; Duckett, D (2018). "A Cytotoxic Three-Dimensional-Spheroid, High-Throughput Assay Using Patient-Derived Glioma Stem Cells". SLAS Discov. 23 (8): 842–9. doi:10.1177/2472555218775055. PMC 6102052. PMID 29750582.
- Kota, S; Hou, S; Guerrant, W; Madoux, F; Troutman, S; Fernandez-Vega, V; et al. (2018). "A novel three-dimensional high-throughput screening approach identifies inducers of a mutant KRAS selective lethal phenotype". Oncogene. 37 (32): 4372–84. doi:10.1038/s41388-018-0257-5. PMC 6138545. PMID 29743592.
- Cassano D, Santi M, D'Autilia F, Mapanao AK, Luin S, Voliani V (2019). "Photothermal effect by NIR-responsive excretable ultrasmall-in-nano architectures". Materials Horizons. 6 (3): 531–7. doi:10.1039/C9MH00096H. hdl:11384/77439.
- Mapanao AK, Santi M, Faraci P, Cappello V, Cassano D, Voliani V (September 2018). "Endogenously Triggerable Ultrasmall-in-Nano Architectures: Targeting Assessment on 3D Pancreatic Carcinoma Spheroids". ACS Omega. 3 (9): 11796–801. doi:10.1021/acsomega.8b01719. PMC 6173554. PMID 30320273.
- Zustiak, Silviya Petrova; Dadhwal, Smritee; Medina, Carlos; Steczina, Sonette; Chehreghanianzabi, Yasaman; Ashraf, Anisa; Asuri, Prashanth (February 2016). "Three-dimensional matrix stiffness and adhesive ligands affect cancer cell response to toxins". Biotechnology and Bioengineering. 113 (2): 443–452. doi:10.1002/bit.25709. PMID 26184715. S2CID 38031281.
- Otieno, Monicah A.; Gan, Jinping; Proctor, William (2018), Chen, Minjun; Will, Yvonne (eds.), "Status and Future of 3D Cell Culture in Toxicity Testing", Drug-Induced Liver Toxicity, Methods in Pharmacology and Toxicology, New York, NY: Springer, pp. 249–261, doi:10.1007/978-1-4939-7677-5_12, ISBN 978-1-4939-7677-5
- Fey SJ, Wrzesinski K (June 2012). "Determination of drug toxicity using 3D spheroids constructed from an immortal human hepatocyte cell line". Toxicological Sciences. 127 (2): 403–11. doi:10.1093/toxsci/kfs122. PMC 3355318. PMID 22454432.
- Messner S, Agarkova I, Moritz W, Kelm JM (January 2013). "Multi-cell type human liver microtissues for hepatotoxicity testing". Archives of Toxicology. 87 (1): 209–13. doi:10.1007/s00204-012-0968-2. PMC 3535351. PMID 23143619.
- Jensen J, Hyllner J, Björquist P (June 2009). "Human embryonic stem cell technologies and drug discovery". Journal of Cellular Physiology. 219 (3): 513–9. doi:10.1002/jcp.21732. PMID 19277978. S2CID 36354049.
- Alexander F, Eggert S, Wiest J (February 2018). "A novel lab-on-a-chip platform for spheroid metabolism monitoring". Cytotechnology. 70 (1): 375–386. doi:10.1007/s10616-017-0152-x. PMC 5809666. PMID 29032507.
- Amacher DE (May 2010). "The discovery and development of proteomic safety biomarkers for the detection of drug-induced liver toxicity". Toxicol Appl Pharmacol. 245 (1): 134–42. Bibcode:2010ToxAP.245..134A. doi:10.1016/j.taap.2010.02.011. PMID 20219512.
- Zhang M, Chen M, Tong W (January 2012). "Is toxicogenomics a more reliable and sensitive biomarker than conventional indicators from rats to predict drug-induced liver injury in humans?". Chem Res Toxicol. 25 (1): 122–9. doi:10.1021/tx200320e. PMID 22122743.
- Stevens JL (November 2006). "Future of toxicology—mechanisms of toxicity and drug safety: where do we go from here?". Chem Res Toxicol. 19 (11): 1393–1401. doi:10.1021/tx060213n. PMID 17112225.
- Lee MY, Dordick JS (December 2006). "High-throughput human metabolism and toxicity analysis". Curr Opin Biotechnol. 17 (6): 619–27. doi:10.1016/j.copbio.2006.09.003. PMID 17046235.
- Houck KA, Kavlock RJ (March 2008). "Understanding mechanisms of toxicity: insights from drug discovery research". Toxicol Appl Pharmacol. 227 (2): 163–78. Bibcode:2008ToxAP.227..163H. doi:10.1016/j.taap.2007.10.022. PMID 18063003.
- Prestwich GD (January 2008). "Evaluating drug efficacy and toxicology in three dimensions: using synthetic extracellular matrices in drug discovery". Acc Chem Res. 41 (1): 139–48. doi:10.1021/ar7000827. PMID 17655274.
- Astashkina A, Mann B, Grainger DW (April 2012). "A critical evaluation of in vitro cell culture models for high-throughput drug screening and toxicity". Pharmacol Ther. 134 (1): 82–106. doi:10.1016/j.pharmthera.2012.01.001. PMID 22252140.
- Wang H, Brown PC, Chow EC, Ewart L, Ferguson SS, Fitzpatrick S, Freedman BS, Guo GL, Hedrich W, Heyward S, Hickman J, Isoherranen N, Li AP, Liu Q, Mumenthaler SM, Polli J, Proctor WR, Ribeiro A, Wang JY, Wange RL, Huang SM (September 2021). "3D cell culture models: Drug pharmacokinetics, safety assessment, and regulatory consideration". Clin Transl Sci. 14 (5): 1659–80. doi:10.1111/cts.13066. PMC 8504835. PMID 33982436.
- Chipangura JK, Ntamo Y, Mohr B, Chellan N (2023). "A review of challenges and prospects of 3D cell-based culture models used for studying drug induced liver injury during early phases of drug development". Hum Exp Toxicol. 42: 9603271221147884. Bibcode:2023HETox..4211478C. doi:10.1177/09603271221147884. PMID 36879529.
- Jiang J, Wolters JE, van Breda SG, Kleinjans JC, de Kok TM (2015). "Development of novel tools for the in vitro investigation of drug-induced liver injury". Expert Opin Drug Metab Toxicol. 11 (10): 1523–37. doi:10.1517/17425255.2015.1065814. PMID 26155718.
- Funk C, Roth A (January 2017). "Current limitations and future opportunities for prediction of DILI from in vitro". Arch Toxicol. 91 (1): 131–142. doi:10.1007/s00204-016-1874-9. PMID 27766365.
- Tutty MA, Movia D, Prina-Mello A (September 2022). "Three-dimensional (3D) liver cell models — a tool for bridging the gap between animal studies and clinical trials when screening liver accumulation and toxicity of nanobiomaterials". Drug Deliv Transl Res. 12 (9): 2048–74. doi:10.1007/s13346-022-01147-0. PMC 9066991. PMID 35507131.
- Nguyen DG, Funk J, Robbins JB, Crogan-Grundy C, Presnell SC, Singer T, Roth AB (2016). "Bioprinted 3D Primary Liver Tissues Allow Assessment of Organ-Level Response to Clinical Drug Induced Toxicity In Vitro". PLOS ONE. 11 (7): e0158674. Bibcode:2016PLoSO..1158674N. doi:10.1371/journal.pone.0158674. PMC 4936711. PMID 27387377.
- Fang Y, Eglen RM (June 2017). "Three-Dimensional Cell Cultures in Drug Discovery and Development". SLAS Discov. 22 (5): 456–472. doi:10.1177/1087057117696795. PMC 5448717. PMID 28520521.
- İpek S, Üstündağ A, Can Eke B (May 2023). "Three-dimensional (3D) cell culture studies: a review of the field of toxicology". Drug Chem Toxicol. 46 (3): 523–533. doi:10.1080/01480545.2022.2066114. PMID 35450503.
- Jensen C, Teng Y (2020). "Is It Time to Start Transitioning From 2D to 3D Cell Culture?". Frontiers in Molecular Biosciences. 7: 33. doi:10.3389/fmolb.2020.00033. PMC 7067892. PMID 32211418.
- Szot CS, Buchanan CF, Freeman JW, Rylander MN (November 2011). "3D in vitro bioengineered tumors based on collagen I hydrogels". Biomaterials. 32 (31): 7905–12. doi:10.1016/j.biomaterials.2011.07.001. PMC 3229258. PMID 21782234.
- Kim JB (October 2005). "Three-dimensional tissue culture models in cancer biology". Semin Cancer Biol. 15 (5): 365–77. doi:10.1016/j.semcancer.2005.05.002. PMID 15975824.
- Horning JL, Sahoo SK, Vijayaraghavalu S, Dimitrijevic S, Vasir JK, Jain TK, Panda AK, Labhasetwar V (2008). "3-D tumor model for in vitro evaluation of anticancer drugs". Mol Pharm. 5 (5): 849–62. doi:10.1021/mp800047v. PMID 18680382.
- Pontes Soares C, Midlej V, de Oliveira ME, Benchimol M, Costa ML, Mermelstein C (2012). "2D and 3D-organized cardiac cells shows differences in cellular morphology, adhesion junctions, presence of myofibrils and protein expression". PLOS ONE. 7 (5): e38147. Bibcode:2012PLoSO...738147S. doi:10.1371/journal.pone.0038147. PMC 3360656. PMID 22662278.
- Lei Y, Schaffer DV (December 2013). "A fully defined and scalable 3D culture system for human pluripotent stem cell expansion and differentiation". Proc Natl Acad Sci U S A. 110 (52): E5039–48. Bibcode:2013PNAS..110E5039L. doi:10.1073/pnas.1309408110. PMC 3876251. PMID 24248365.
- Chopra V, Dinh TV, Hannigan EV (June 1997). "Three-dimensional endothelial-tumor epithelial cell interactions in human cervical cancers". In Vitro Cell Dev Biol Anim. 33 (6): 432–42. doi:10.1007/s11626-997-0061-y. PMID 9201511.
- ^ Habanjar O, Diab-Assaf M, Caldefie-Chezet F, Delort L (November 2021). "3D Cell Culture Systems: Tumor Application, Advantages, and Disadvantages". International Journal of Molecular Sciences. 22 (22): 12200. doi:10.3390/ijms222212200. PMC 8618305. PMID 34830082.