| AOC3 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | AOC3, HPAO, SSAO, VAP-1, VAP1, amine oxidase, copper containing 3, amine oxidase copper containing 3 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 603735; MGI: 1306797; HomoloGene: 2770; GeneCards: AOC3; OMA:AOC3 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Amine oxidase, copper containing 3 (AOC3), also known as vascular adhesion protein (VAP-1) and HPAO is an enzyme that in humans is encoded by the AOC3 gene on chromosome 17. This protein is a member of the semicarbazide-sensitive amine oxidase (SSAO; aka primary amine oxidase) family of enzymes and is associated with many vascular diseases.
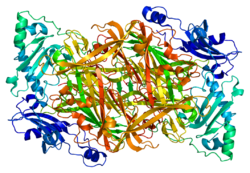
Structure
VAP-1 is a type 1 membrane-bound glycoprotein that has a distal adhesion domain and an enzymatically active amine oxidase site outside of the membrane. The AOC3 gene is mapped onto 17q21 and has an exon count of 6.
Function
Amine oxidases are a family of enzymes that catalyze the oxidation of various endogenous amines, including histamine or dopamine. VAP-1 constitutes the copper dependent class of amine oxidases, such as lysyl oxidase or lysine demethylase, and is one of the four known in humans. The other class is flavin dependent such as monoamine oxidase (MAO) A and B. VAP-1, in particular, catalyzes the oxidative conversion of primary amines (methylamine and aminoacetone) to aldehydes (formaldehyde and methylglyoxal) ammonium and hydrogen peroxide in the presence of copper and quinone cofactor.
VAP-1 is primarily localized on the cell surface on the adipocyte plasma membrane. However, circulating VAP-1 has been shown to be the main source of SSAO in human serum. Serum VAP-1 originates from many tissues. VAP-1 has adhesive properties, functional monoamine oxidase activity, and possibly plays a role in glucose handling, leukocyte trafficking, and migration during inflammation. This rise in metabolic products contributes to generating advanced glycation end-products and oxidative stress along with the monoamine detoxification in the organism.
Like monoamine oxidase (MAO), VAP-1 can deaminate short-chain primary amines, but SSAO enzymes, including VAP-1, can tolerate several selective flavin-dependent MAO-A and MAO-B inhibitors like clorgiline, pargyline, and deprenyl, but are still sensitive to semicarbazide and other hydrazines, hydroxylamine and propargylamine.
VAP-1 is found in the smooth muscle of blood vessels and various other tissues, and can mostly be found in two forms: tissue-bound and soluble isoforms. The tissue-bound SSAO is primarily located in the leukocytes, adipocytes, and the endothelium of highly vascularized tissues, including the kidney, liver, and gonads. Thus, this form participates in cellular differentiation, deposition of the ECM (extracellular matrix) in smooth muscle cells, lipid trafficking in adipocytes and control of muscular tone, by mechanisms that are not completely understood. The soluble form, which is commonly known as VAP-1, is a proinflammatory protein derived from shedding of the transmembrane protein. It is highly expressed on the endothelium of the lung and trachea, and absent from leukocytes and epithelial cells. It moderates leukocyte recruitment, is both an adhesion molecule and a primary amine oxidase, and plays a role in clinical disease.
Clinical significance
Membrane-bound VAP-1 releases an active, soluble form of the protein, which may be conducive to increased inflammation and the progression of many vascular disorders. In particular, elevation of VAP-1 activity and the increased enzymatic-mediated deamination is proposed to play a role in renal and vascular disease, oxidative stress, acute and chronic hyperglycemia, and diabetes complications.
In diabetic patients, the amine oxidase activity stimulates glucose uptake via translocation of transporters to the cell membrane in adipocytes and smooth muscle cells. This modifies hepatic glucose homeostasis and may contribute to patterns of GLUT expression in chronic disease, as insulin resistance in humans have been linked to altered expression of GLUT isoforms by granulosa cells and adipose tissues.
In particular, hydrogen peroxide, released during the deamination of SSAO, acts as a signal-transducing molecule, affecting GLUT1 and GLUT4 translocation to the plasma membrane by granulosa cells and adipose tissue. This mimics insulin and interferes with cell processes in diabetic patients. Additionally, hydrogen peroxide, along with aldehydes and glucose, is involved in generating advanced glycation end-products and oxidative stress, which leads to the development of atherosclerosis, a disease in which plaque builds up inside arteries.
Cell processes involved in insulin resistance are often associated with elevated VAP-1 expression and modified GLUT expression in patients with liver diseases. Accordingly, subjects with diabetes are often at an increased risk for the development of and mortality from various cancers, including colorectal cancer hepatocellular carcinoma. Because of hyperinsulinemia - the increased bioavailability of insulin-like growth factors-1 and hypoadiponectinemia - diabetic patients have a greater chance of developing oncogenesis and tumor progression. In one study, serum VAP-1 was shown to independently predict 10-year all-cause mortality, cardiovascular mortality, and cancer-related mortality in subjects with type 2 diabetes. This may be because VAP-1 is involved in binding TIL, lymphokine-activated killer cells, and natural killer cells to the vasculature of cancer tissue. Hence, increased serum VAP-1 activity has been repeatedly found to be associated with various vascular disorders, such as the complications of diabetes mellitus, acute and chronic hyperglycemia, congestive heart failure, atherosclerosis, and Alzheimer's disease.
The same elevation is seen in kidney disease, even when accounted for factors of age, gender, and smoking. Studies have established a strong correlation between serum VAP-1 levels and urinary albumin excretion, which supports the idea that VAP-1 may be involved in the pathogenesis of kidney damage in humans. In renal pathology, the aldehydes produced by SSAO are highly reactive and lead to the formation of protein cross-linking and oxidative stress. Additionally, VAP-1 mediates leukocyte migration and, eventually, can lead to chronic inflammatory cell accumulation and the development of kidney fibrosis.
As for stroke patients, the products from deamination induce cytotoxicity protein cross-linking and amyloid-beta (Aβ) aggregation along with oxidative stress and thus are considered a potential risk factor for stress-related angiopathy. In these patients, VAP-1 may be involved in increasing vascular damage due to increased susceptibility of endothelial cells to oxygen-glucose deprivation (OGD). In hemorrhagic stroke patients, plasmatic VAP-1 activity is increase, and in ischemic stroke patients, it can predict the appearance of parenchymal hemorrhages after tissue plasminogen activator treatment due to the transmigration of inflammatory cells into ischaemic brain. VAP-1-expression is increased in blood vessels of ischemic areas where it may be mediating neutrophil adhesion to vascular endothelium in ischemic heart. The presence of diminished expression of vascular VAP-1 in infarcted brain areas and the increased concentration of VAP-1 in serum suggests that acute cerebral ischaemia triggers early release of endothelial VAP-1 from brain vasculature.
Lastly, during pulmonary infection and airway hyper-activity, VAP-1 may also contribute to the recruitment of inflammatory cells and the transfer of neutrophils from the microvasculature. Inhibitors of VAP-1 may be effective in reducing inflammation in various vascular diseases, but more studies are needed to understand to what extent.
Whether serum VAP-1 is a good biomarker for these diseases requires further investigation. Although many studies concerning VAP-1 as a therapeutic target are becoming more frequent, it is difficult to study VAP-1 in cell or tissue systems, since the enzyme progressively loses its expression, and immortalized cell lines do not show any expression at all.
Interactions
VAP-1 has been shown to interact with:
References
- ^ GRCh38: Ensembl release 89: ENSG00000131471 – Ensembl, May 2017
- ^ GRCm38: Ensembl release 89: ENSMUSG00000019326 – Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: AOC3 Amine oxidase, copper containing 3".
- Foot JS, Yow TT, Schilter H, Buson A, Deodhar M, Findlay AD, Guo L, McDonald IA, Turner CI, Zhou W, Jarolimek W (Nov 2013). "PXS-4681A, a potent and selective mechanism-based inhibitor of SSAO/VAP-1 with anti-inflammatory effects in vivo". The Journal of Pharmacology and Experimental Therapeutics. 347 (2): 365–74. doi:10.1124/jpet.113.207613. PMID 23943052. S2CID 6164890.
- ^ Schilter HC, Collison A, Russo RC, Foot JS, Yow TT, Vieira AT, Tavares LD, Mattes J, Teixeira MM, Jarolimek W (20 March 2015). "Effects of an anti-inflammatory VAP-1/SSAO inhibitor, PXS-4728A, on pulmonary neutrophil migration". Respiratory Research. 16 (1): 42. doi:10.1186/s12931-015-0200-z. PMC 4389443. PMID 25889951.
- ^ Januszewski AS, Mason N, Karschimkus CS, Rowley KG, Best JD, O'Neal DN, Jenkins AJ (May 2014). "Plasma semicarbazide-sensitive amine oxidase activity in type 1 diabetes is related to vascular and renal function but not to glycaemia". Diabetes & Vascular Disease Research. 11 (4): 262–269. doi:10.1177/1479164114532963. PMID 24853908. S2CID 23326308.
- ^ Repessé X, Moldes M, Muscat A, Vatier C, Chetrite G, Gille T, Planes C, Filip A, Mercier N, Duranteau J, Fève B (Aug 2015). "Hypoxia inhibits semicarbazide-sensitive amine oxidase activity in adipocytes". Molecular and Cellular Endocrinology. 411: 58–66. doi:10.1016/j.mce.2015.04.011. PMID 25907140. S2CID 46505459.
- ^ Valente T, Gella A, Solé M, Durany N, Unzeta M (Oct 2012). "Immunohistochemical study of semicarbazide-sensitive amine oxidase/vascular adhesion protein-1 in the hippocampal vasculature: pathological synergy of Alzheimer's disease and diabetes mellitus". Journal of Neuroscience Research. 90 (10): 1989–96. doi:10.1002/jnr.23092. PMID 22714978. S2CID 26126297.
- ^ Hernandez-Guillamon M, Solé M, Delgado P, García-Bonilla L, Giralt D, Boada C, Penalba A, García S, Flores A, Ribó M, Alvarez-Sabin J, Ortega-Aznar A, Unzeta M, Montaner J (2012). "VAP-1/SSAO plasma activity and brain expression in human hemorrhagic stroke". Cerebrovascular Diseases. 33 (1): 55–63. doi:10.1159/000333370. PMID 22133888. S2CID 24467635.
- ^ Li HY, Jiang YD, Chang TJ, Wei JN, Lin MS, Lin CH, Chiang FT, Shih SR, Hung CS, Hua CH, Smith DJ, Vanio J, Chuang LM (Mar 2011). "Serum vascular adhesion protein-1 predicts 10-year cardiovascular and cancer mortality in individuals with type 2 diabetes". Diabetes. 60 (3): 993–9. doi:10.2337/db10-0607. PMC 3046860. PMID 21282368.
- ^ Koc-Zorawska E, Przybylowski P, Malyszko JS, Mysliwiec M, Malyszko J (Jun 2013). "Vascular adhesion protein-1, a novel molecule, in kidney and heart allograft recipients". Transplantation Proceedings. 45 (5): 2009–12. doi:10.1016/j.transproceed.2013.01.103. PMID 23769096.
- ^ Solé M, Unzeta M (Nov 2011). "Vascular cell lines expressing SSAO/VAP-1: a new experimental tool to study its involvement in vascular diseases". Biology of the Cell. 103 (11): 543–57. doi:10.1042/BC20110049. PMID 21819380. S2CID 4598444.
- ^ El-Maghrabey MH, Kishikawa N, Ohyama K, Imazato T, Ueki Y, Kuroda N (Jun 2015). "Determination of human serum semicarbazide-sensitive amine oxidase activity via flow injection analysis with fluorescence detection after online derivatization of the enzymatically produced benzaldehyde with 1,2-diaminoanthraquinone". Analytica Chimica Acta. 881: 139–47. Bibcode:2015AcAC..881..139E. doi:10.1016/j.aca.2015.04.006. hdl:10069/35501. PMID 26041530.
- ^ Wong M, Saad S, Zhang J, Gross S, Jarolimek W, Schilter H, Chen JA, Gill AJ, Pollock CA, Wong MG (Oct 2014). "Semicarbazide-sensitive amine oxidase (SSAO) inhibition ameliorates kidney fibrosis in a unilateral ureteral obstruction murine model". American Journal of Physiology. Renal Physiology. 307 (8): F908–16. doi:10.1152/ajprenal.00698.2013. PMID 25143459.
- ^ Sun P, Solé M, Unzeta M (2014). "Involvement of SSAO/VAP-1 in oxygen-glucose deprivation-mediated damage using the endothelial hSSAO/VAP-1-expressing cells as experimental model of cerebral ischemia". Cerebrovascular Diseases. 37 (3): 171–80. doi:10.1159/000357660. PMID 24503888. S2CID 11980778.
- Weston CJ, Adams DH (Jul 2011). "Hepatic consequences of vascular adhesion protein-1 expression". Journal of Neural Transmission. 118 (7): 1055–64. doi:10.1007/s00702-011-0647-0. PMID 21512782. S2CID 26073771.
- ^ Lin MS, Li HY, Wei JN, Lin CH, Smith DJ, Vainio J, Shih SR, Chen YH, Lin LC, Kao HL, Chuang LM, Chen MF (Nov 2008). "Serum vascular adhesion protein-1 is higher in subjects with early stages of chronic kidney disease". Clinical Biochemistry. 41 (16–17): 1362–7. doi:10.1016/j.clinbiochem.2008.06.019. PMID 18644360.
- ^ Karim S, Liaskou E, Fear J, Garg A, Reynolds G, Claridge L, Adams DH, Newsome PN, Lalor PF (Dec 2014). "Dysregulated hepatic expression of glucose transporters in chronic disease: contribution of semicarbazide-sensitive amine oxidase to hepatic glucose uptake". American Journal of Physiology. Gastrointestinal and Liver Physiology. 307 (12): G1180–90. doi:10.1152/ajpgi.00377.2013. PMC 4269679. PMID 25342050.
- Kaplan MA, Kucukoner M, Inal A, Urakci Z, Evliyaoglu O, Firat U, Kaya M, Isikdogan A (2014). "Relationship between serum soluble vascular adhesion protein-1 level and gastric cancer prognosis". Oncology Research and Treatment. 37 (6): 340–4. doi:10.1159/000362626. PMID 24903765. S2CID 22849102.
- Airas L, Lindsberg PJ, Karjalainen-Lindsberg ML, Mononen I, Kotisaari K, Smith DJ, Jalkanen S (Aug 2008). "Vascular adhesion protein-1 in human ischaemic stroke". Neuropathology and Applied Neurobiology. 34 (4): 394–402. doi:10.1111/j.1365-2990.2007.00911.x. PMID 18005095. S2CID 25254193.
- Li HY, Wei JN, Lin MS, Smith DJ, Vainio J, Lin CH, Chiang FT, Shih SR, Huang CH, Wu MY, Hsein YC, Chuang LM (Jun 2009). "Serum vascular adhesion protein-1 is increased in acute and chronic hyperglycemia". Clinica Chimica Acta; International Journal of Clinical Chemistry. 404 (2): 149–53. doi:10.1016/j.cca.2009.03.041. PMID 19336232.
External links
- Human AOC3 genome location and AOC3 gene details page in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: Q16853 (Membrane primary amine oxidase) at the PDBe-KB.
Further reading
- Lalor PF, Lai WK, Curbishley SM, Shetty S, Adams DH (Sep 2006). "Human hepatic sinusoidal endothelial cells can be distinguished by expression of phenotypic markers related to their specialised functions in vivo". World Journal of Gastroenterology. 12 (34): 5429–39. doi:10.3748/wjg.v12.i34.5429. PMC 4088223. PMID 17006978.
- Bustelo XR, Barbacid M (May 1992). "Tyrosine phosphorylation of the vav proto-oncogene product in activated B cells". Science. 256 (5060): 1196–9. Bibcode:1992Sci...256.1196B. doi:10.1126/science.256.5060.1196. PMID 1375396. S2CID 35071104.
- Andersson B, Wentland MA, Ricafrente JY, Liu W, Gibbs RA (Apr 1996). "A "double adaptor" method for improved shotgun library construction". Analytical Biochemistry. 236 (1): 107–13. doi:10.1006/abio.1996.0138. PMID 8619474.
- Zhang X, McIntire WS (Nov 1996). "Cloning and sequencing of a copper-containing, topa quinone-containing monoamine oxidase from human placenta". Gene. 179 (2): 279–86. doi:10.1016/S0378-1119(96)00387-3. PMID 8972912.
- Yu W, Andersson B, Worley KC, Muzny DM, Ding Y, Liu W, Ricafrente JY, Wentland MA, Lennon G, Gibbs RA (Apr 1997). "Large-scale concatenation cDNA sequencing". Genome Research. 7 (4): 353–8. doi:10.1101/gr.7.4.353. PMC 139146. PMID 9110174.
- Smith DJ, Salmi M, Bono P, Hellman J, Leu T, Jalkanen S (Jul 1998). "Cloning of vascular adhesion protein 1 reveals a novel multifunctional adhesion molecule". The Journal of Experimental Medicine. 188 (1): 17–27. doi:10.1084/jem.188.1.17. PMC 2525535. PMID 9653080.
- Lalor PF, Edwards S, McNab G, Salmi M, Jalkanen S, Adams DH (Jul 2002). "Vascular adhesion protein-1 mediates adhesion and transmigration of lymphocytes on human hepatic endothelial cells". Journal of Immunology. 169 (2): 983–92. doi:10.4049/jimmunol.169.2.983. PMID 12097405.
- Salmi M, Stolen C, Jousilahti P, Yegutkin GG, Tapanainen P, Janatuinen T, Knip M, Jalkanen S, Salomaa V (Dec 2002). "Insulin-regulated increase of soluble vascular adhesion protein-1 in diabetes". The American Journal of Pathology. 161 (6): 2255–62. doi:10.1016/S0002-9440(10)64501-4. PMC 1850919. PMID 12466139.
- Singh B, Tschernig T, van Griensven M, Fieguth A, Pabst R (May 2003). "Expression of vascular adhesion protein-1 in normal and inflamed mice lungs and normal human lungs". Virchows Archiv. 442 (5): 491–5. doi:10.1007/s00428-003-0802-6. PMID 12700900. S2CID 21175610.
- Zhang Q, Mashima Y, Noda S, Imamura Y, Kudoh J, Shimizu N, Nishiyama T, Umeda S, Oguchi Y, Tanaka Y, Iwata T (Oct 2003). "Characterization of AOC2 gene encoding a copper-binding amine oxidase expressed specifically in retina". Gene. 318: 45–53. doi:10.1016/S0378-1119(03)00753-4. PMID 14585497.
- Conklin DJ, Cowley HR, Wiechmann RJ, Johnson GH, Trent MB, Boor PJ (Feb 2004). "Vasoactive effects of methylamine in isolated human blood vessels: role of semicarbazide-sensitive amine oxidase, formaldehyde, and hydrogen peroxide". American Journal of Physiology. Heart and Circulatory Physiology. 286 (2): H667–76. doi:10.1152/ajpheart.00690.2003. PMID 14715500.
- Olivé M, Unzeta M, Moreno D, Ferrer I (Feb 2004). "Overexpression of semicarbazide-sensitive amine oxidase in human myopathies". Muscle & Nerve. 29 (2): 261–6. doi:10.1002/mus.10550. PMID 14755492. S2CID 6932766.
- Forster-Horváth C, Döme B, Paku S, Ladányi A, Somlai B, Jalkanen S, Tímár J (Apr 2004). "Loss of vascular adhesion protein-1 expression in intratumoral microvessels of human skin melanoma". Melanoma Research. 14 (2): 135–40. doi:10.1097/00008390-200404000-00010. PMID 15057044. S2CID 22397003.
- Aboulaich N, Vainonen JP, Strålfors P, Vener AV (Oct 2004). "Vectorial proteomics reveal targeting, phosphorylation and specific fragmentation of polymerase I and transcript release factor (PTRF) at the surface of caveolae in human adipocytes". The Biochemical Journal. 383 (Pt 2): 237–48. doi:10.1042/BJ20040647. PMC 1134064. PMID 15242332.
- Boomsma F, Pedersen-Bjergaard U, Agerholm-Larsen B, Hut H, Dhamrait SS, Thorsteinsson B, van den Meiracker AH (May 2005). "Association between plasma activities of semicarbazide-sensitive amine oxidase and angiotensin-converting enzyme in patients with type 1 diabetes mellitus". Diabetologia. 48 (5): 1002–7. doi:10.1007/s00125-005-1716-4. hdl:1765/73367. PMID 15830186.
- Li HY, Lee WJ, Chen MJ, Chuang LM (May 2005). "Change in vascular adhesion protein-1 and metabolic phenotypes after vertical banded gastroplasty for morbid obesity". Obesity Research. 13 (5): 855–61. doi:10.1038/oby.2005.98. PMID 15919838.
- Airenne TT, Nymalm Y, Kidron H, Smith DJ, Pihlavisto M, Salmi M, Jalkanen S, Johnson MS, Salminen TA (Aug 2005). "Crystal structure of the human vascular adhesion protein-1: unique structural features with functional implications". Protein Science. 14 (8): 1964–74. doi:10.1110/ps.051438105. PMC 2279308. PMID 16046623.