Pharmaceutical compound
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /nəˈprɒksən/ |
| Trade names | Aleve, Naprosyn, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a681029 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 95% (by mouth) |
| Protein binding | 99% |
| Metabolism | Liver (to 6-desmethylnaproxen) |
| Elimination half-life | 12–17 hours (adults) |
| Excretion | Kidney |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.040.747 |
| Chemical and physical data | |
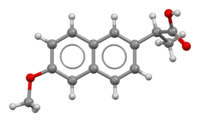
| Formula | C14H14O3 |
| Molar mass | 230.263 g·mol |
| 3D model (JSmol) | |
| Melting point | 152–154 °C (306–309 °F) |
SMILES
| |
InChI
| |
| (verify) | |
Naproxen, sold under the brand name Aleve among others, is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain, menstrual cramps, and inflammatory diseases such as rheumatoid arthritis, gout and fever. It is taken orally. It is available in immediate and delayed release formulations. Onset of effects is within an hour and lasts for up to twelve hours. Naproxen is also available in salt form, naproxen sodium, which has better solubility when taken orally.
Common side effects include dizziness, headache, bruising, allergic reactions, heartburn, and stomach pain. Severe side effects include an increased risk of heart disease, stroke, gastrointestinal bleeding, and stomach ulcers. The heart disease risk may be lower than with other NSAIDs. It is not recommended in people with kidney problems. Use is not recommended in the third trimester of pregnancy.
Naproxen is a nonselective COX inhibitor. As an NSAID, naproxen appears to exert its anti-inflammatory action by reducing the production of inflammatory mediators called prostaglandins. It is metabolized by the liver to inactive metabolites.
Naproxen was patented in 1967 and approved for medical use in the United States in 1976. In the United States it is available over the counter and as a generic medication. In 2022, it was the 88th most commonly prescribed medication in the United States, with more than 7 million prescriptions.
Medical uses
Naproxen's medical uses are related to its mechanism of action as an anti-inflammatory compound. Naproxen is used to treat a variety of inflammatory conditions and symptoms that are due to excessive inflammation, such as pain and fever (naproxen has fever-reducing, or antipyretic, properties in addition to its anti-inflammatory activity). Naproxen's anti-inflammatory properties may relieve pain caused by inflammatory conditions such as migraine, osteoarthritis, kidney stones, rheumatoid arthritis, psoriatic arthritis, gout, ankylosing spondylitis, menstrual cramps, tendinitis, and bursitis.
Naproxen sodium is used as a "bridge therapy" in medication-overuse headache to slowly take patients off other medications.
Available formulations
Naproxen sodium is available as both an immediate-release and an extended-release tablet. The extended-release formulations (sometimes called "sustained release", or "enteric coated") take longer to take effect than the immediate-release formulations and therefore are less useful when immediate pain relief is desired. Extended-release formulations are more useful for the treatment of chronic, or long-lasting, conditions, in which long-term pain relief is desirable.
-
 250 mg tablet of naproxen
250 mg tablet of naproxen
-
220 mg tablet of naproxen sodium. Imprint L490 (upside-down). Round, light blue tablet
-
 Naproxen extended release 500 mg, back and front
Naproxen extended release 500 mg, back and front
Pregnancy and lactation
As with all non-steroidal anti-inflammatory medications (NSAIDs), naproxen use should be avoided in pregnancy due to the importance of prostaglandins in vascular and renal function in the fetus. NSAIDs should especially be avoided in the third trimester. Small amounts of naproxen are excreted in breast milk. However, adverse effects are uncommon in infants breastfed from a mother taking naproxen.
Adverse effects
Common adverse effects include dizziness, drowsiness, headache, rash, bruising, and gastrointestinal upset. Heavy use is associated with an increased risk of end-stage renal disease and kidney failure. Naproxen may cause muscle cramps in the legs in 3% of people.
In October 2020, the U.S. Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid. They recommend avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.
Gastrointestinal
As with other non-COX-2 selective NSAIDs, naproxen can cause gastrointestinal problems, such as heartburn, constipation, diarrhea, ulcers and stomach bleeding. Naproxen should be taken orally with, or just after food, to decrease the risk of gastrointestinal side effects. Persons with a history of ulcers or inflammatory bowel disease should consult a doctor before taking naproxen. In U.S. markets, naproxen is sold with boxed warnings about the risk of gastrointestinal ulceration or bleeding. Naproxen poses an intermediate risk of stomach ulcers compared with ibuprofen, which is low-risk, and indometacin, which is high-risk. To reduce stomach ulceration risk, it is often combined with a proton-pump inhibitor (a medication that reduces stomach acid production) during long-term treatment of those with pre-existing stomach ulcers or a history of developing stomach ulcers while on NSAIDs.
Cardiovascular
COX-2 selective and nonselective NSAIDs have been linked to increases in the number of serious and potentially fatal cardiovascular events, such as myocardial infarctions and strokes. Naproxen is, however, associated with the smallest overall cardiovascular risks. Cardiovascular risk must be considered when prescribing any nonsteroidal anti-inflammatory drug. The drug had roughly 50% of the associated risk of stroke compared with ibuprofen and was also associated with a reduced number of myocardial infarctions compared with control groups.
A study found that high-dose naproxen induced near-complete suppression of platelet thromboxane throughout the dosing interval and appeared not to increase cardiovascular disease (CVD) risk, whereas other non-aspirin high-dose NSAID regimens had only transient effects on platelet COX-1 and were associated with a small but definite vascular hazard. Conversely, naproxen was associated with higher rates of upper gastrointestinal bleeding complications compared with other NSAIDs.
Interactions
Drug–drug interactions
Naproxen may interact with antidepressants, lithium, methotrexate, probenecid, warfarin and other blood thinners, heart or blood pressure medications, including diuretics, or steroid medicines such as prednisone.
NSAIDs such as naproxen may interfere with and reduce the efficacy of SSRI antidepressants, as well as increase the risk of bleeding greater than the individual bleeding risk of either class of agent, when taken together. Naproxen is not contraindicated in the presence of SSRIs, though concomitant use of the medications should be done with caution. Alcohol consumption increases the risk of gastrointestinal bleeding when combined with NSAIDs like naproxen in a dose-dependent manner (that is, the higher the dose of naproxen, the higher the risk of bleeding). The risk is highest for people who are heavy drinkers.
Pharmacology
Mechanism of action
Naproxen works by reversibly inhibiting both the COX-1 and COX-2 enzymes as a non-selective coxib.
Pharmacokinetics
Naproxen is a minor substrate of CYP1A2 and CYP2C9. It is extensively metabolized in the liver to 6-O-desmethylnaproxen, and both the parent drug and the desmethyl metabolite undergo further metabolism to their respective acylglucuronide conjugated metabolites. An analysis of two clinical trials shows that naproxen's time to peak plasma concentration occurs between 2 and 4 hours after oral administration, though naproxen sodium reaches peak plasma concentrations within 1–2 hours.
Pharmacogenetics
The pharmacogenetics of naproxen has been studied to better understand its adverse effects. In 1998, a small pharmacokinetic (PK) study failed to show that differences in a patient's ability to clear naproxen from the body could account for differences in a patient's risk of experiencing the adverse effect of a serious gastrointestinal bleed while taking naproxen. However, the study failed to account for differences in the activity of CYP2C9, a drug-metabolizing enzyme that is necessary for clearing naproxen. Studies on the relationship between CYP2C9 genotype and NSAID-induced gastrointestinal bleeds have shown that genetic variants in CYP2C9 that reduce the clearance of major CYP2C9 substrates (like naproxen) increase the risk of NSAID-induced gastrointestinal bleeds, especially for homozygous defective variants.
Chemistry
Naproxen is a member of the 2-arylpropionic acid (profen) family of NSAIDs. The free acid is an odorless, white to off-white crystalline substance. Naproxen free base is lipid-soluble and practically insoluble in water, while naproxen sodium and many other salts are freely soluble in water, often soluble in methanol, and sparingly soluble in alcohol; check the specific solubility of each salt before use. Naproxen has a melting point of 152–155 °C, while naproxen salts tend to have higher melting points.
Synthesis
Naproxen has been industrially produced by Syntex starting from 2-naphthol as follows:
Society and culture
Brand names
Naproxen and naproxen sodium are marketed under various brand names, including Accord, Aleve, Anaprox, Antalgin, Apranax, Feminax Ultra, Flanax, Inza, Maxidol, Nalgesin, Naposin, Naprelan, Naprogesic, Naprosyn, Narocin, Pronaxen, Proxen, and Soproxen. It is also available as the combination naproxen/esomeprazole magnesium in delayed-release tablets under the brand name Vimovo.
Access restrictions
Syntex first marketed naproxen in 1976, as the prescription drug Naprosyn. They first marketed naproxen sodium under the brand name Anaprox in 1980. It remains a prescription-only drug in much of the world. In the United States, the Food and Drug Administration (FDA) approved it as an over-the-counter (OTC) drug in 1994. OTC preparations of naproxen in the U.S. are mainly marketed by Bayer HealthCare under the brand name Aleve and generic store brand formulations in 220 mg tablets. In Australia, packets of 275 mg tablets of naproxen sodium are Schedule 2 pharmacy medicines, with a maximum daily dose of five tablets or 1375 mg. In the United Kingdom, 250 mg tablets of naproxen were approved for OTC sale under the brand name Feminax Ultra in 2008, for the treatment of primary dysmenorrhoea in women aged 15 to 50. In the Netherlands, 220 mg and 275 mg tablets are available OTC in drugstores, 550 mg is OTC only at pharmacies. Aleve became available over the counter in some provinces in Canada on 14 July 2009, but not British Columbia, Quebec or Newfoundland and Labrador; it subsequently became available OTC in British Columbia in January 2010.
Toxicology scandal
Naproxen was one of the four substances named in the prosecution of Industrial Bio-Test Laboratories (IBT) for fraudulent toxicology testing. Naproxen passed subsequent legitimate toxicology testing.
Ecological effects
Naproxen has been found in groundwater and drinking water in concentrations high enough to have adverse effects on invertebrates including fungi, algae, bacteria and fishes. Naproxen is not thoroughly removed by conventional water treatment methods, and its degradation pathways in the environment are limited. Some methods more successfully remove naproxen from wastewater, including metal-organic complexes and porous carbon. Although the levels are generally low enough to not be acutely toxic, sub-lethal effects may still occur, such as reduced photosynthetic ability.
Research
Naproxen may have antiviral activity against influenza. In laboratory research, it blocks the RNA-binding groove of the nucleoprotein of the virus, preventing the formation of the ribonucleoprotein complex—thus taking the viral nucleoproteins out of circulation.
Veterinary use
Horses
Naproxen is given by mouth to horses at a dose of 10 mg/kg and has shown to have a wide safety margin (no toxicity when given at three times the recommended dose for 42 days). It is more effective for myositis than the commonly used NSAID phenylbutazone, and has shown especially good results for treatment of equine exertional rhabdomyolysis, a disease of muscle breakdown; it is less commonly used for musculoskeletal disease.
References
- ^ "Naproxen". Drugs.com. 2017. Retrieved 7 February 2017.
- ^ "Naproxen international". Drugs.com. 7 December 2020. Retrieved 3 January 2021.
- "Naproxen Use During Pregnancy". Drugs.com. 13 August 2019. Retrieved 27 December 2019.
- "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- Gill, A, ed. (July 2013). Standard for the Uniform Scheduling of Medicines and Poisons No. 4 (PDF). Therapeutic Goods Administration. ISBN 978-1-74241-895-7.
- "Boots Period Pain Relief 250 mg Gastro-Resistant Tablets - Summary of Product Characteristics (SmPC)". (emc). 4 February 2013. Retrieved 12 February 2023.
- ^ Angiolillo DJ, Weisman SM (April 2017). "Clinical Pharmacology and Cardiovascular Safety of Naproxen". American Journal of Cardiovascular Drugs. 17 (2): 97–107. doi:10.1007/s40256-016-0200-5. PMC 5340840. PMID 27826802.
- ^ "Naproxen Monograph for Professionals". Drugs.com. AHFS. Retrieved 19 December 2018.
- Derry C, Derry S, Moore RA, McQuay HJ (January 2009). "Single dose oral naproxen and naproxen sodium for acute postoperative pain in adults". The Cochrane Database of Systematic Reviews. 2009 (1): CD004234. doi:10.1002/14651858.CD004234.pub3. PMC 6483469. PMID 19160232.
- McEvoy GK (2000). AHFS Drug Information, 2000. American Society of Health-System Pharmacists. p. 1854. ISBN 9781585280049.
- ^ "Naprosyn- naproxen tablet EC-Naprosyn- naproxen tablet, delayed release Anaprox DS- naproxen sodium tablet". DailyMed. 1 July 2019. Retrieved 27 December 2019.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 520. ISBN 9783527607495.
- "Medicines A to Z - Naproxen". NHS. National Health Service. 24 October 2018. Retrieved 11 March 2020.
- "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- "Naproxen Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- Garza I, Schwedt TJ (April 2010). "Diagnosis and management of chronic daily headache". Seminars in Neurology. 30 (2). WebMD LLC: 154–166. doi:10.1055/s-0030-1249224. PMID 20352585.
- ^ "L490 (Naproxen 220 mg)". drugs.com. Retrieved 17 May 2017.
- "LACTMED: NAPROXEN". TOXNET. NIH. Retrieved 21 July 2017.
- Perneger TV, Whelton PK, Klag MJ (December 1994). "Risk of kidney failure associated with the use of acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs". The New England Journal of Medicine. 331 (25): 1675–1679. doi:10.1056/nejm199412223312502. PMID 7969358.
- Allen RE, Kirby KA (August 2012). "Nocturnal leg cramps". American Family Physician. 86 (4): 350–355. PMID 22963024.
- ^ "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "NSAIDs may cause rare kidney problems in unborn babies". U.S. Food and Drug Administration. 21 July 2017. Retrieved 15 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "Naproxen". PubMed Health. 1 September 2008. Archived from the original on 22 July 2010.
- ^ "How to take it". NHS.Gov. 20 January 2022.
- Richy F, Bruyere O, Ethgen O, Rabenda V, Bouvenot G, Audran M, et al. (July 2004). "Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a consensus statement using a meta-analytic approach". Annals of the Rheumatic Diseases. 63 (7): 759–766. doi:10.1136/ard.2003.015925. PMC 1755051. PMID 15194568.
- Rossi S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. pp. 665, 673. ISBN 978-0-85711-084-8.
- Nissen SE, Yeomans ND, Solomon DH, Lüscher TF, Libby P, Husni ME, et al. (December 2016). "Cardiovascular Safety of Celecoxib, Naproxen, or Ibuprofen for Arthritis". The New England Journal of Medicine. 375 (26): 2519–2529. doi:10.1056/NEJMoa1611593. PMID 27959716.
- ^ Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM, et al. (January 2011). "Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis". BMJ. 342: c7086. doi:10.1136/bmj.c7086. PMC 3019238. PMID 21224324. c7086.
- ^ Bhala N, Emberson J, Merhi A, Abramson S, Arber N, Baron JA, et al. (August 2013). "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". Lancet. 382 (9894): 769–779. doi:10.1016/S0140-6736(13)60900-9. PMC 3778977. PMID 23726390.
- Warner-Schmidt JL, Vanover KE, Chen EY, Marshall JJ, Greengard P (May 2011). "Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans". Proceedings of the National Academy of Sciences of the United States of America. 108 (22): 9262–9267. Bibcode:2011PNAS..108.9262W. doi:10.1073/pnas.1104836108. PMC 3107316. PMID 21518864.
- ^ Turner MS, May DB, Arthur RR, Xiong GL (March 2007). "Clinical impact of selective serotonin reuptake inhibitors therapy with bleeding risks". Journal of Internal Medicine. 261 (3): 205–213. doi:10.1111/j.1365-2796.2006.01720.x. PMID 17305643. S2CID 41772614.
- ^ Pfau PR, Lichenstein GR (November 1999). "NSAIDs and alcohol: never the twain shall mix?". The American Journal of Gastroenterology. 94 (11): 3098–3101. doi:10.1111/j.1572-0241.1999.03098.x. PMID 10566697. S2CID 41310743.
- Duggan KC, Walters MJ, Musee J, Harp JM, Kiefer JR, Oates JA, et al. (November 2010). "Molecular basis for cyclooxygenase inhibition by the non-steroidal anti-inflammatory drug naproxen". The Journal of Biological Chemistry. 285 (45): 34950–34959. doi:10.1074/jbc.M110.162982. PMC 2966109. PMID 20810665.
- Hinz B, Cheremina O, Besz D, Zlotnick S, Brune K (April 2008). "Impact of naproxen sodium at over-the-counter doses on cyclooxygenase isoforms in human volunteers". International Journal of Clinical Pharmacology and Therapeutics. 46 (4): 180–186. doi:10.5414/CPP46180. PMID 18397691.
- Van Hecken A, Schwartz JI, Depré M, De Lepeleire I, Dallob A, Tanaka W, et al. (October 2000). "Comparative inhibitory activity of rofecoxib, meloxicam, diclofenac, ibuprofen, and naproxen on COX-2 versus COX-1 in healthy volunteers". Journal of Clinical Pharmacology. 40 (10): 1109–1120. doi:10.1177/009127000004001005. PMID 11028250. S2CID 24736336. Archived from the original on 23 February 2020. Retrieved 23 February 2020.
- Gross GJ, Moore J (July 2004). "Effect of COX-1/COX-2 inhibition versus selective COX-2 inhibition on coronary vasodilator responses to arachidonic acid and acetylcholine". Pharmacology. 71 (3): 135–142. doi:10.1159/000077447. PMID 15161995. S2CID 34018223.
- Hawkey CJ (October 2001). "COX-1 and COX-2 inhibitors". Best Practice & Research. Clinical Gastroenterology. 15 (5): 801–820. doi:10.1053/bega.2001.0236. PMID 11566042.
- Vree TB, van den Biggelaar-Martea M, Verwey-van Wissen CP, Vree JB, Guelen PJ (August 1993). "Pharmacokinetics of naproxen, its metabolite O-desmethylnaproxen, and their acyl glucuronides in humans". Biopharmaceutics & Drug Disposition. 14 (6): 491–502. doi:10.1002/bdd.2510140605. PMID 8218967. S2CID 35920001.
- ^ Rodrigues AD (November 2005). "Impact of CYP2C9 genotype on pharmacokinetics: are all cyclooxygenase inhibitors the same?". Drug Metabolism and Disposition. 33 (11): 1567–1575. doi:10.1124/dmd.105.006452. PMID 16118328. S2CID 5754183.
- el Mouelhi M, Ruelius HW, Fenselau C, Dulik DM (1987). "Species-dependent enantioselective glucuronidation of three 2-arylpropionic acids. Naproxen, ibuprofen, and benoxaprofen". Drug Metabolism and Disposition. 15 (6): 767–772. PMID 2893700.
- Harrington PJ, Lodewijk E (1997). "Twenty Years of Naproxen Technology". Org. Process Res. Dev. 1 (1): 72–76. doi:10.1021/op960009e.
- "Vimovo- naproxen and esomeprazole magnesium tablet, delayed release". DailyMed. 2 August 2019. Retrieved 27 December 2019.
- "Aleve- naproxen sodium tablet". DailyMed. 4 November 2019. Retrieved 27 December 2019.
- "Medicines regulator approves availability of a new OTC medicine for period pain" (Press release). Medicines and Healthcare products Regulatory Agency (MHRA). 1 April 2008. Archived from the original (PDF) on 21 September 2013.
- "Aleve products released in Canada".
- "Aleve – Welcome to Canada, Eh!" (PDF) (Press release). Bayer Health Care. 14 July 2009. Retrieved 24 March 2012.
- "Aleve – Helping British Columbians with Joint and Arthritis Pain Get Back to Doing the Activities They Love". newswire.ca. 28 January 2010. Archived from the original on 21 September 2013. Retrieved 27 September 2012.
- "Industry Documents Library".
- Wojcieszyńska D, Guzik U (March 2020). "Naproxen in the environment: its occurrence, toxicity to nontarget organisms and biodegradation". Applied Microbiology and Biotechnology. 104 (5): 1849–1857. doi:10.1007/s00253-019-10343-x. PMC 7007908. PMID 31925484.
- Rodríguez-Serin H, Gamez-Jara A, De La Cruz-Noriega M, Rojas-Flores S, Rodriguez-Yupanqui M, Gallozzo Cardenas M, et al. (October 2022). "Literature Review: Evaluation of Drug Removal Techniques in Municipal and Hospital Wastewater". International Journal of Environmental Research and Public Health. 19 (20): 13105. doi:10.3390/ijerph192013105. PMC 9602914. PMID 36293682.
- Moreno Ríos AL, Gutierrez-Suarez K, Carmona Z, Ramos CG, Silva Oliveira LF (March 2022). "Pharmaceuticals as emerging pollutants: Case naproxen an overview". Chemosphere. 291 (Pt 1): 132822. Bibcode:2022Chmsp.29132822M. doi:10.1016/j.chemosphere.2021.132822. hdl:11323/9007. PMID 34767851.
- Mulkiewicz E, Wolecki D, Świacka K, Kumirska J, Stepnowski P, Caban M (October 2021). "Metabolism of non-steroidal anti-inflammatory drugs by non-target wild-living organisms". The Science of the Total Environment. 791: 148251. Bibcode:2021ScTEn.79148251M. doi:10.1016/j.scitotenv.2021.148251. PMID 34139498.
- Huynh NC, Nguyen TT, Nguyen DT, Tran TV (November 2023). "Occurrence, toxicity, impact and removal of selected non-steroidal anti-inflammatory drugs (NSAIDs): A review". The Science of the Total Environment. 898: 165317. Bibcode:2023ScTEn.89865317H. doi:10.1016/j.scitotenv.2023.165317. PMID 37419350.
- Parolini M (October 2020). "Toxicity of the Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) acetylsalicylic acid, paracetamol, diclofenac, ibuprofen and naproxen towards freshwater invertebrates: A review". The Science of the Total Environment. 740: 140043. Bibcode:2020ScTEn.74040043P. doi:10.1016/j.scitotenv.2020.140043. hdl:2434/747078. PMID 32559537.
- Mojiri A, Zhou JL, Ratnaweera H, Rezania S, Nazari VM (February 2022). "Pharmaceuticals and personal care products in aquatic environments and their removal by algae-based systems". Chemosphere. 288 (Pt 2): 132580. Bibcode:2022Chmsp.28832580M. doi:10.1016/j.chemosphere.2021.132580. PMID 34687686.
- Lejal N, Tarus B, Bouguyon E, Chenavas S, Bertho N, Delmas B, et al. (May 2013). "Structure-based discovery of the novel antiviral properties of naproxen against the nucleoprotein of influenza A virus". Antimicrobial Agents and Chemotherapy. 57 (5): 2231–2242. doi:10.1128/AAC.02335-12. PMC 3632891. PMID 23459490.
Lay summary at: "Pain reliever shows anti-viral activity against flu". EurekAlert!. - McIlwraith CW, Frisbie DD, Kawcak CE (2001). "Nonsteroidal Anti-Inflammatory Drugs". Proceedings of the Annual Convention of the American Association of Equine Practitioners. 47: 182–187. ISSN 0065-7182.
- May SA, Lees P (1996). "Nonsteroidal anti-inflammatory drugs". In McIlwraith CW, Trotter GW (eds.). Joint disease in the horse. Philadelphia: WB Saunders. pp. 223–237. ISBN 0-7216-5135-6.
External links
| Non-steroidal anti-inflammatory drugs (NSAIDs) (primarily M01A and M02A, also N02BA) | |
|---|---|
| pyrazolones / pyrazolidines | |
| salicylates | |
| acetic acid derivatives and related substances | |
| oxicams | |
| propionic acid derivatives (profens) |
|
| n-arylanthranilic acids (fenamates) | |
| COX-2 inhibitors (coxibs) | |
| other | |
| NSAID combinations | |
| Key: underline indicates initially developed first-in-class compound of specific group; WHO-Essential Medicines; withdrawn drugs; veterinary use. | |
| Topical products for joint and muscular pain (M02) | |||||||
|---|---|---|---|---|---|---|---|
| Anti-inflammatory preparations, non-steroids |
| ||||||
| Capsaicin derivatives | |||||||
| Other | |||||||
| Prolactin inhibitors and anti-inflammatory products for vaginal administration (G02CB–G02CC) | |
|---|---|
| Prolactin inhibitors | |
| Anti-inflammatory products for vaginal administration | |
| Prostanoid signaling modulators | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Receptor (ligands) |
| ||||||||||||||||||||||||||
| Enzyme (inhibitors) |
| ||||||||||||||||||||||||||
| Others | |||||||||||||||||||||||||||
