| Bertolotti's syndrome | |
|---|---|
 | |
| X-ray of Bertolotti's syndrome (in this case, right transverse mega-apophysis of L5 with pseudoarticulation with the sacral ala). Woman 67 years old. |
Bertolotti's syndrome is a commonly missed cause of back pain which occurs due to lumbosacral transitional vertebrae (LSTV). It is a congenital condition but is not usually symptomatic until one's later twenties or early thirties. However, there are a few cases of Bertolotti's that become symptomatic at a much earlier age.
It is named for Mario Bertolotti, an Italian physician who first described it in 1917.
Presentation
A chronic, persistent low back pain along with buttock pain is the most important presentation. Radicular pain is observed.
Pathophysiology
Bertolotti's syndrome is characterized by sacralization of the lowest lumbar vertebral body and lumbarization of the uppermost sacral segment. It involves a total or partial unilateral or bilateral fusion of the transverse process of the lowest lumbar vertebra to the sacrum, leading to the formation of a transitional 5th lumbar vertebra. Of importance is that this syndrome will result in a pain generating 4th lumbar disc resulting in a "sciatic" type of a pain correlating to the 5th lumbar nerve root. Usually the transitional vertebra will have a "spatulated" transverse process on one side resulting in articulation or partial articulation with the sacrum or at time the ilium and in some cases with both. This results in limited / altered motion at the lumbo-sacral articulation. This loss of motion will then be compensated for at segments superior to the transitional vertebra resulting in accelerated degeneration and strain through the L4 disc level which can become symptomatic and inflame the adjacent L5 nerve root resulting in "sciatic" or radicular pain patterns. Scoliosis is frequently found to be associated.
Classification
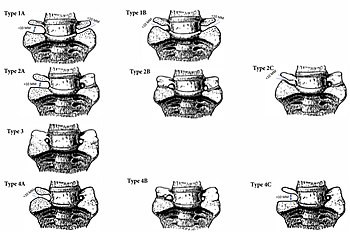
Bertolotti's Syndrome is classified via the Jenkins Classification. The Jenkins classification is separated into 4 categories: Type 1, 2, 3, and 4 with subclassifications of: L (left) or R (right) prominence, A (unilateral), B (bilateral), or C (Type 2 with Type 1 and contralateral 2 anatomy or Type 4 with a gap > 10 mm and contralateral Type 3 anatomy), + L (left) or R (right) iliac contact.
Type 1: A dysplastic transverse process that shows a gap of less than 10mm, but greater than 2mm across the lumbosacral junction.
Type 2: Pseudo-articulation between adjacent transverse processes with a gap of less than 2 mm.
Type 3: Complete fusion lateral to the facet at the ala, without spontaneous fusion of the disk or facet joints, of the lumbosacral junction.
Type 4: Presence of unilaterally fused side with varying pseudoarticulation on the contralateral side (Type 4A, 4B, or 4C).
Diagnosis
The diagnosis depends on appropriate patient history backed by imaging studies like X ray and MRI. Lumbosacral spine radiographs help in the identification of the skeletal abnormality. MRI helps in confirmation.
Treatment
Non surgical treatments include steroid injections in the lower back or radiofrequency sensory ablation. Physical therapy interventions are also helpful in early cases and are focused around mobilization, neural stretching, and core strengthening exercises. Surgical intervention is usually a last resort if all conservative methods fail. It can be treated surgically with posterolateral fusion or resection of the transitional articulation.
References
- Quinlan, JF; Duke, D; Eustace, S (30 August 2006). "Bertolotti's syndrome. A cause of back pain in young people". The Bone & Joint Journal. 88 (9): 1183–6. doi:10.1302/0301-620X.88B9.17211. PMID 16943469.
- Bertolotti M: Contributo alla conoscenza dei vizi differenzazione regionale del rachide con speciale riguardo all assimilazione sacrale della V. lombare. Radiol Med. 1917, 4: 113-144.
- ^ Jancuska, Jeffrey; Spivak, Jeffrey; Bendo, John (29 July 2015). "A Review of Symptomatic Lumbosacral Transitional Vertebrae: Bertolotti's Syndrome". International Journal of Spine Surgery. 9: 42. doi:10.14444/2042. PMC 4603258. PMID 26484005.
- Jain, Anuj; Agarwal, Anil; Jain, Suruchi; Shamshery, Chetna (2013). "Bertolotti Syndrome: A Diagnostic and Management Dilemma for Pain Physicians". The Korean Journal of Pain. 26 (4): 368–73. doi:10.3344/kjp.2013.26.4.368. PMC 3800709. PMID 24156003.
- Jenkins, Arthur L; O’Donnell, John; Chung, Richard J.; Jenkins, Sarah; Hawks, Charlotte; Lazarus, Daniella; McCaffrey, Tara; Terai, Hiromi; Harvie, Camryn (March 2023). "Redefining The Classification for Bertolotti's Syndrome: Anatomical Findings in The Lumbosacral Transitional Vertebrae Guide Treatment Selection". World Neurosurgery. 175: e303–e313. doi:10.1016/j.wneu.2023.03.077. PMID 36965661. S2CID 257733733.
- Mitra, R; Carlisle, M (23 November 2008). "Bertolotti's Syndrome: A Case Report". Pain Practice. 9 (2): 152–4. doi:10.1111/j.1533-2500.2008.00253.x. PMID 19037900. S2CID 24091334.
- Jenkins, Arthur L.; Chung, Richard J.; O’Donnell, John; Hawks, Charlotte; Jenkins, Sarah; Lazarus, Daniella; McCaffrey, Tara; Terai, Hiromi; Harvey, Camryn; Matsoukas, Stavros (2023-03-08). "Redefining the Treatment of Lumbosacral Transitional Vertebrae for Bertolotti Syndrome: Long-Term Outcomes Utilizing the Jenkins Classification to Determine Treatment". World Neurosurgery. 175: e21–e29. doi:10.1016/j.wneu.2023.03.012. ISSN 1878-8750. PMID 36898630. S2CID 257438800.
- Chung, Richard J.; Harvie, Camryn; O’Donnell, John; Jenkins, Sarah; Jenkins, Arthur L. (2023-02-13). "Surgical outcome of a patient with Bertolotti's syndrome in whom the established Castellvi classification system failed: illustrative case". Journal of Neurosurgery: Case Lessons. 5 (7): CASE22450. doi:10.3171/CASE22450. PMC 10550603. PMID 38015013. S2CID 256862124.
Further reading
Paraskevas, Georgios; Tzaveas, Alexandros; Koutras, Georgios; Natsis, Konstantinos (2009). "Lumbosacral transitional vertebra causing Bertolotti's syndrome: A case report and review of the literature". Cases Journal. 2: 8320. doi:10.4076/1757-1626-2-8320. PMC 2740102. PMID 19830065.
External links
| Classification | D |
|---|
| Congenital malformations and deformations of musculoskeletal system / musculoskeletal abnormality | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Appendicular limb / dysmelia |
| ||||||||||||||||||||||
| Axial |
| ||||||||||||||||||||||