The term human blood group systems is defined by the International Society of Blood Transfusion (ISBT) as systems in the human species where cell-surface antigens—in particular, those on blood cells—are "controlled at a single gene locus or by two or more very closely linked homologous genes with little or no observable recombination between them", and include the common ABO and Rh (Rhesus) antigen systems, as well as many others; 44 human systems are identified as of 31 December 2022.
Table of systems and classifications
| ISBT No. | System name | System symbol | Structure / function | Chromosome | Antigens | Notes |
|---|---|---|---|---|---|---|
| 001 | ABO | ABO | Carbohydrate (N-Acetylgalactosamine, galactose). | 9q34.2 | A, B, H | Mainly elicit IgM antibody reactions, although anti-H is very rare, see the Hh antigen system (Bombay phenotype, ISBT #18). |
| 002 | MNS | MNS | GPA / GPB (glycophorins A and B). | 4q31.21 | M, N, S, s | |
| 003 | P1PK | P | Glycolipid | 22q13.2 | P1, P, and P | |
| 004 | Rh | RH | Protein and glucose. | 1p36.11 | C, c, D, E, e | There is no "d" antigen; lowercase "d" indicates the absence of D. |
| 005 | Lutheran | LU | Protein (member of the immunoglobulin superfamily). | 19q13.32 | 21 antigens | |
| 006 | Kell | KEL | Glycoprotein. | 7q34 | K, k, Kp, Kp, Js and Js | |
| 007 | Lewis | LE | Carbohydrate (fucose residue). | 19p13.3 | Mainly Le and Le | Associated with tissue ABH antigen secretion. |
| 008 | Duffy | FY | Protein (chemokine receptor). | 1q23.2 | Mainly Fy and Fy | Individuals lacking Duffy antigens altogether are immune to malaria caused by Plasmodium vivax and Plasmodium knowlesi. |
| 009 | Kidd | JK | Protein (urea transporter). | 18q12.3 | Jk and Jk | |
| 010 | Diego | DI | Glycoprotein (band 3, AE 1, or anion exchange). | 17q21.31 | Positive blood is found only among East Asians and Native Americans. | |
| 011 | Yt | YT | Protein (AChE, acetylcholinesterase). | 7q22.1 | ||
| 012 | XG | XG | Glycoprotein. | Xp22.33 | ||
| 013 | Scianna | SC | Glycoprotein. | 1p34.2 | ||
| 014 | Dombrock | DO | Glycoprotein (fixed to cell membrane by GPI, or glycosyl-phosphatidyl-inositol). | 12p12.3 | ||
| 015 | Colton | CO | Aquaporin 1. | 7p14.3 | Mainly Co(a) and Co(b) | |
| 016 | Landsteiner-Wiener | LW | Protein (member of the immunoglobulin superfamily). | 19p13.2 | ||
| 017 | Chido/Rodgers | CH | C4A C4B (complement fractions). | 6p21.3 | ||
| 018 | Hh | H | Carbohydrate (fucose residue). | 19q13.33 | ||
| 019 | XK | XK | Glycoprotein. | Xp21.1 | ||
| 020 | Gerbich | GE | GPC / GPD (Glycophorins C and D). | 2q14.3 | ||
| 021 | Cromer | CROM | Glycoprotein (DAF or CD55, regulates complement fractions C3 and C5, attached to the membrane by GPI). | 1q32.2 | ||
| 022 | Knops | KN | Glycoprotein (CR1 or CD35, immune complex receptor). | 1q32.2 | ||
| 023 | Indian | IN | Glycoprotein (CD44 adhesion function?). | 11p13 | ||
| 024 | Ok | OK | Glycoprotein (CD147). | 19p13.3 | ||
| 025 | Raph | RAPH | Transmembrane glycoprotein. | 11p15.5 | ||
| 026 | JMH | JMH | Protein (fixed to cell membrane by GPI). Also known as Semaphorin 7A or CD108. | 15q24.1 | ||
| 027 | Ii | I | Branched (I) / unbranched (i) polysaccharide. | 6p24.2 | ||
| 028 | Globoside | GLOB | Glycolipid. Antigen P. | 3q26.1 | ||
| 029 | GIL | GIL | Aquaporin 3. | 9p13.3 | ||
| 030 | Rh-associated glycoprotein | RHAg | Rh-associated glycoprotein. | 6p21-qter | ||
| 031 | Forssman | FORS | Globoside alpha-1,3-N-acetylgalactosaminyltransferase 1 (GBGT1). | 9q34.13 | ||
| 032 | Langereis | LAN | ABCB6, human ATP-binding cassette (ABC) transporter, mitochondrial porphyrin transporter. | 2q36 | ||
| 033 | Junior | JR | ABCG2. Multi-drug transporter protein. | 4q22 | ||
| 034 | Vel | Vel | Human red cell antigens. | 1p36.32 | ||
| 035 | CD59 | CD59 | — | 11p13 | ||
| 036 | Augustine | AUG | Protein (transporter). | 6p21.1 | ||
| 037 | KANNO | PRNP | — | 20p13 | ||
| 038 | SID | SID | 17q21.32 | |||
| 039 | CTL2 | CTL2 | 19p13.2 | |||
| 040 | PEL | PEL | 13q32.1 | |||
| 041 | MAM | MAM | 19q13.33 | |||
| 042 | EMM | EMM | 4p16.3 | |||
| 043 | ABCC1 | ABCC1 | 16p13.11 | |||
| 044 | Er | Er | Protein | Er, Er, Er3, Er4, and Er5 | Illustrates potential antigenicity of low abundance membrane proteins and contributes to understanding of in vivo characteristics of the Piezo1 protein in transfusion biology |
Antibodies
Following is a comparison of clinically relevant characteristics of antibodies against the main human blood group systems:
| ABO | Rh | Kell | Duffy | Kidd | Lutheran | MNS | Lewis | P | Ii | |
|---|---|---|---|---|---|---|---|---|---|---|
| Most common in immediate hemolytic transfusion reactions | A | Yes | Fy | Jk | ||||||
| Most common in delayed hemolytic transfusion reactions | E,D,C | Jk | ||||||||
| Most common in hemolytic disease of the newborn | Yes | D,C | Yes | |||||||
| Commonly produce intravascular hemolysis | Yes | Yes | Yes | |||||||
| Reactive at room temperature | Yes | M,N | Le, Le | P1 | ||||||
| Nearly always clinically insignificant | Yes | M,N | Yes | P1 | ||||||
| Naturally occurring | Yes | Yes | M,N | Yes | Yes | Yes | ||||
| Enhanced by ficain and papain | Yes | Yes | Yes | Yes | P1 | Yes | ||||
| Destroyed by ficain and papain | Fy, Fy | Yes | Yes | |||||||
| Displaying dosage Further information: Blood compatibility testing | Cc, Ee | Yes | Yes | Yes |
Compatibility testing
Main article: Blood compatibility testing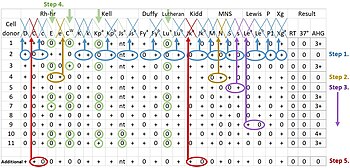
Blood compatibility testing is performed before blood transfusion, including matching of the ABO blood group system and the Rh blood group system, as well as screening for recipient antibodies against other human blood group systems. Blood compatibility testing is also routinely performed on pregnant women and on the cord blood from newborn babies, because incompatibility puts the baby at risk for developing hemolytic disease of the newborn. It is also used before hematopoietic stem cell transplantation, as it may be responsible for some cases of acute graft-versus-host disease.
Other human blood group systems than ABO and Rh have a relatively small risk of complications when blood is mixed. Therefore, in emergencies such as major hemorrhage, the urgency of transfusion can exceed the need for compatibility testing against other blood group systems (and potentially Rh as well). Also, blood compatibility testing beyond ABO and Rh is generally limited to antibody detection (not necessarily including forward typing). Still, in Europe, females who require blood transfusions are often typed for the K and extended Rh antigens to prevent sensitization to these antigens, which could put them at risk for developing hemolytic disease of the newborn during pregnancy.
When needing to give red blood cell transfusion to a patient, the presence of clinically significant antibodies produced by the patient can be detected by mixing patient serum with 2 to 4 "screening" or "control" red blood cells that together display essentially all relevant antigens. If any of these mixes display a reaction (evidence of patient antibodies binding to the screening red blood cells), a more extensive antibody panel is warranted (as imaged at right).
See also
References
- ISBT (2016). "International Society for Blood Transfusion (ISBT) Committee on Terminology for Red Cell Surface Antigens, Terminology Home Page". Archived from the original on 3 March 2016. Retrieved 20 February 2016.
- "Red Cell Immunogenetics and Blood Group Terminology". International Society of Blood Transfusion. 2023. Archived from the original on 2 February 2022. Retrieved 25 April 2023.
- ISBT (2021). "Table of Blood Group Systems v 10.0 (June 2021)" (PDF). International Society of Blood Transfusion. Archived (PDF) from the original on 15 January 2022. Retrieved 11 February 2022.
- Smart, E.; Armstrong, B. (2008). "Blood group systems". ISBT Science Series. 3 (2): 68–92. doi:10.1111/j.1751-2824.2008.00188.x. ISSN 1751-2816.
- ^ Helias, V.; Saison, C.; Ballif, B.A.; Peyrard, T.; Takahashi, J.; Takahashi, H.; Tanaka, M.; Deybach, J.C.; Puy, H.; Le Gall, M.; Sureau, C.; Pham, B.N.; Le Pennec, P.Y.; Tani, Y.; Cartron, J.P.; Arnaud, L. (2012). "ABCB6 is Dispensable for Erythropoiesis and Specifies the New Blood Group System Langereis". Nature Genetics. 44 (2, January 15): 170–173. doi:10.1038/ng.1069. PMC 3664204. PMID 22246506.
- Daniels, G.; Ballif, B. A.; Helias, V.; Saison, C.; Grimsley, S.; Mannessier, L.; Hustinx, H.; Lee, E.; et al. (20 April 2015). "Lack of the nucleoside transporter ENT1 results in the Augustine-null blood type and ectopic mineralization". Blood. 125 (23): 3651–3654. doi:10.1182/blood-2015-03-631598. PMC 4458803. PMID 25896650.
- National Center for Global Health and Medicine, Japanese Red Cross Society, Fukushima Medical University and Japan Agency for Medical Research and Development (2019-08-05) 新たなヒト血液型「KANNO」の国際認定―国立国際医療研究センターなど、日本の研究グループとして初めての登録― (in Japanese)
- "Omae, Y.; Ito, S.; Takeuchi, M.; Isa, K.; Ogasawara, K.; Kawabata, K.; Oda, A.; Kaito, S.; Tsuneyama, H.; Uchikawa, M.; Wada, I.; Ohto, H.; Tokunaga, K. (2019). "Integrative genome analysis identified the KANNO blood group antigen as prion protein" Transfusion. 2019 Jul;59(7):2429-2435. DOI:10.1111/trf.15319. Epub 2019 Apr 24.
- Karamatic Crew, Vanja; Tilley, Louise A; Satchwell, Timothy J; AlSubhi, Samah A; Jones, Benjamin; Spring, Frances A; Walser, Piers J; Martins Freire, Catarina; Murciano, Nicoletta; Rotordam, Maria Giustina; Woestmann, Svenja J; Hamed, Marwa; Alradwan, Reem; AlKhrousey, Mouza; Skidmore, Ian; Lewis, Sarah; Hussain, Shimon; Jackson, Jane; Latham, Tom; Kilby, Mark D; Lester, William Arthur; Becker, Nadine; Rapedius, Markus; Toye, Ashley Mark; Thornton, Nicole M (19 September 2022). "Missense mutations in PIEZO1, encoding the Piezo1 mechanosensor protein, define the Er red blood cell antigens". Blood. 141 (2): 135–146. doi:10.1182/blood.2022016504. PMC 10644042. PMID 36122374. S2CID 252382544.
- Mais, Daniel (2014). Quick compendium of clinical pathology. United States: American Society for Clinical Pathology Press. ISBN 978-0-89189-615-9. OCLC 895712380.
- ^ Hill, Ben C.; Hanna, Courtney A.; Adamski, Jill; Pham, Huy P.; Marques, Marisa B.; Williams, Lance A. (2017). "Ficin-Treated Red Cells Help Identify Clinically Significant Alloantibodies Masked as Reactions of Undetermined Specificity in Gel Microtubes". Laboratory Medicine. 48 (1): 24–28. doi:10.1093/labmed/lmw062. ISSN 0007-5027. PMID 28007780.
- ^ Eric Ching. "Questions and Answers on Proteolytic Enzymes Used in Blood Group Serology". Canadian Society for Transfusion Medicine. Retrieved 2021-01-28.
- American Association for Clinical Chemistry (15 November 2019). "Blood Typing". Lab Tests Online. Retrieved 27 January 2020.
- Gonsorcik, V.K. (7 August 2018). "ABO Grouping: Overview, Clinical Indications/Applications, Test Performance". Medscape. Retrieved 2 March 2020.
- Bacigalupo, A.; Van Lint, M. T.; M. Margiocco, D. Occhini; Ferrari, G.; Pittaluga, P. A.; Frassoni, F.; Peralvo, J.; Lercari, G.; Carubia, F.; Marmont, A. M. (1988). "Abo Compatibility and Acute Graft-Versus-Host Disease Following Allogeneic Bone Marrow Transplantation". Transplantation. 45 (6): 1091–1093. doi:10.1097/00007890-198806000-00018. ISSN 0041-1337. PMID 3289150. S2CID 39707395.
- ^ Goodell, Pamela P.; Uhl, Lynne; Mohammed, Monique; Powers, Amy A. (2010). "Risk of Hemolytic Transfusion Reactions Following Emergency-Release RBC Transfusion". American Journal of Clinical Pathology. 134 (2): 202–206. doi:10.1309/AJCP9OFJN7FLTXDB. ISSN 0002-9173. PMID 20660321.
- Westhoff, Connie M. (2019). "Blood group genotyping". Blood. 133 (17): 1814–1820. doi:10.1182/blood-2018-11-833954. ISSN 0006-4971. PMID 30808639.
- "Glossary: Antibody Screen - Blood Bank Guy Glossary".
Further reading
- Dean, Laura (2005). Blood Groups and Red Cell Antigens. Bethesda, MD, USA: National Center for Biotechnology Information (NCBI), National Library of Medicine, National Institutes of Health. Retrieved 19 February 2016.
- SIB-EBI-PIR (2016). "Blood group Antigen Proteins: List of Entries, 17 February version". Swiss-Prot Protein Knowledgebase. Geneva, CHE: Swiss Institute of Bioinformatic (SIB), in cooperation with the European Bioinformatics Institute (EBI, Hinxton, ENG), and the Protein Information Resource (PIR, Washington DC, USA). Retrieved 19 February 2016.
- ISBT Table of blood group antigens within systems, updated August 2008.
- BGMUT Blood Group Antigen Gene Mutation Database at NCBI, NIH.
External links
- BGvar, a comprehensive online resource for blood group associated genetic variants.
- Rophina, Mercy; Pandhare, Kavita; Jadhao, Sudhir; Nagaraj, Shivashankar H.; Scaria, Vinod (2021-02-05). "BGvar - a comprehensive resource for blood group immunogenetics". bioRxiv. 32 (3): 229–236. doi:10.1101/2021.02.04.429861. PMID 34897852. S2CID 231885707. - Human Blood Group System NIH, National Library of Medicine.
 Media related to Human blood group systems at Wikimedia Commons
Media related to Human blood group systems at Wikimedia Commons
| Blood transfusion and transfusion medicine | |
|---|---|
| Blood products | |
| General concepts | |
| Methods | |
| Tests | |
| Transfusion reactions and adverse effects | |
| Blood group systems | |