Medical condition
| Femoroacetabular impingement | |
|---|---|
| Other names | Hip impingement syndrome, |
| The three recognized types of femoroacetabular impingement. Click image to see video illustration of the three types. | |
| Specialty | Orthopedic |
Femoroacetabular impingement (FAI) is a condition involving one or more anatomical abnormalities of the hip joint, which is a ball and socket joint. It is a common cause of hip pain and discomfort in young and middle-aged adults. It occurs when the ball shaped femoral head contacts the acetabulum abnormally or does not permit a normal range of motion in the acetabular socket. Damage can occur to the articular cartilage, or labral cartilage (soft tissue, ring-shaped bumper of the socket), or both. The condition may be symptomatic or asymptomatic. It may cause osteoarthritis of the hip. Treatment options range from conservative management to surgery.
Signs and symptoms
Pain is the most common complaint in those with FAI. It is experienced in a number of areas, making the diagnosis challenging, but commonly occurs in the groin, upper buttock/lower back, the buttock or beneath the buttock, side of the affected hip and posterior upper leg. Onset of symptoms has been reported to present in both an acute and more gradual manner. The pain is often significant enough to cause a decrease in activity level and movement. Some will also describe decreased range of motion of the affected hip. Another symptom is groin pain associated with activity and no prior history of trauma. Inability to perform activities such as high hip flexion or prolong sitting can also be seen in individuals with FAI.
Cause
FAI is characterized by abnormal contact between the proximal femur and rim of the acetabulum (hip socket). In most cases, patients present with a deformity in the femoral head, or acetabulum, a poorly positioned femoral-acetabular junction, or any or all of the foregoing. The cause of FAI is currently unknown, but both congenital and acquired etiologies have been put forth. Studies have shown an increased incidence in siblings, suggesting a genetic component. At least one study has also shown a predilection in the white population. It has also been reported to be more common in males. However, there is no concrete evidence to suggest a genetic trait and instead, the most favored theory currently supports that FAI (the cam type in particular) is due to repetitive movements involving the hip (e.g. squatting) in young athletes. Aggravating activities that are commonly reported include repetitive or prolonged squatting, twisting movements of the hip, like pivoting during athletics, getting in and out of cars, and even sitting for prolonged periods. A combination of these factors may also predispose to a form of FAI; predominantly, a marginal developmental hip abnormality together with environmental factors such as recurrent motion of the legs within a supraphysiologic range.
Three types of FAI are recognized (see title image). The first involves an excess of bone along the upper surface of the femoral head, known as a cam deformity (abbreviation for camshaft, which the shape of the femoral head and neck resembles). The second is due to an excess of growth of the upper lip of the acetabular cup and is known as a 'pincer' deformity. The third is a combination of the two, generally referred to as 'mixed.' The most common type seen, approximately 70% of the time, is the mixed type. A complicating issue is that some of the radiographic findings of FAI have also been described in asymptomatic subjects.
Current literature suggests that the cam type of impingement is associated with the development of hip osteoarthritis. Thus far, no correlation has been seen between the pincer type and development of hip osteoarthritis.
Anatomy
The hip joint is classified as a ball and socket joint. This type of synovial joint allows for multidirectional movement and rotation. There are two bones that make up the hip joint and create an articulation between the femur and pelvis. This articulation connects the axial skeleton with the lower extremity. The pelvic bone, also known as the innominate bone, is formed by three bones fused together: the ilium, ischium, and pubis. The musculature of the hip is divided into anterior hip muscles and posterior hip muscles. The major nerve supply that runs through the hip joint is the femoral nerve and the sciatic nerve.
Diagnosis
Clinical evaluation is the first step in diagnosis, but will rarely lead to the diagnosis on its own, due to inconsistent and vague nature of the pain. Childhood and current activity should be inquired about. Physical exam should also involve assessing passive internal rotation of the hip during flexion, as range of motion is reduced in proportion to the size of a cam lesion. Flexing the hip to 90 degrees, adducting, and internally rotating the hip, known as the FADDIR test, should also be performed. It is positive when it causes pain. The FABER test should also be performed, this test involves flexing, abducting, and externally rotating the hip. The FABER test is useful when diagnosing concurrently with a labral pathology and is considered positive if the position elicits pain. Additional non-invasive ways to observe possible FAI is changes in gait that include a lower peak hip extension and internal rotation to compensate for bony growth.
X-ray


Projectional radiography ("X-ray")is often considered first line for FAI. Anterior-posterior pelvis and a lateral image of the hip in question should be attained. A 45-degree Dunn view is also recommended.
Other modalities
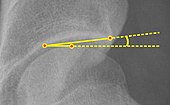
MRI imaging may follow, particularly if there is no specific evidence on radiographs, producing a three-dimensional reconstruction of the joint for better definition, to evaluate the hip cartilage, or measure hip socket angles (e.g. the alpha-angle as described by Nötzli in 2-D and by Siebenrock in 3-D). MR arthrogram had been used in the past, as it was more sensitive for picking up soft tissue lesions; however, due to improvement in technology, MRI is now considered comparable for picking up such lesions. CT is not usually used due to radiation exposure and no benefit above MRI. It is possible to perform dynamic simulation of hip motion with CT or MRI assisting to establish whether, where, and to what extent, impingement is occurring.
The diagnosis is often made in conjunction with a labral tear.
Differential Diagnosis
Source:
- Piriformis syndrome or strain
- Labral tear without FAI
- Adductor muscle strain
- Sciatica
- Athletic pubalgia
- Gluteus medius/minimus or illiopsoas tendinopathy
- Stress fracture
- Femoral head osteonecrosis
- Other impingements, including anterior inferior iliac spine, ischiofemoral and iliopsoas
- Loose body in the joint (intra-articular body)
Prevention
Prevention is currently being investigated. The goal of prevention would be to avoid joint damage and premature hip osteoarthritis. Studies are examining the effectiveness of screening adolescents in school and targeting at-risk individuals for education, physical therapy and decreasing participation in possibly harmful activities/sports as referenced in the epidemiology section.
Treatment
Treatment of FAI can be divided into those that are non-operative (conservative) and operative. Conservative treatment is often prescribed for those who have not yet received any therapy. Conservative treatment includes physical therapy, avoidance of those activities that produce pain, and nonsteroidal anti-inflammatory drugs. It may also include joint injections with cortisone or hyaluronic acid, particularly for those who wish to avoid surgery.
Physical therapy is implemented for the purpose of improving joint mobility, strengthening muscles surrounding the joint, correcting posture, and treating any other muscle or joint deficits that may be exacerbating the condition. A movement analysis may also be performed to identify specific movement patterns that may be causing injury. Studies to demonstrate the effectiveness of physical therapy are currently underway, with no conclusive results to date.
Operative treatment is generally recommended to those who continue to have symptoms. It involves the surgical correction of any bony abnormalities causing the impingement and correction of any soft tissue lesions, such as labral tears. The primary aim of surgery is to correct the fit of the femoral head and acetabulum to create a hip socket that reduces contact between the two, allowing a greater range of movement. This includes femoral head sculpting and/or trimming of the acetabular rim.
Surgery may be arthroscopic or open. A 2011 study analyzing current surgical methods for management of symptomatic femoral acetabular impingement, suggested that the arthroscopic method had surgical outcomes equal to or better than other methods with a lower rate of major complications when performed by experienced surgeons; consequently, the surgery is now rarely done open.
Outcomes of arthroscopic surgery are currently being studied, but have generally been positive. According to a 2019 meta-analysis, the risk of having surgery fail or need to be re-operated on is about 5.5% whereas the complication rate is 1.7%. Additionally, patient reported outcomes show that approximately three to six months post-operative hip arthroscopy is when pain reduction and activities of daily life are improved. For sport function this timeline is about six months to a year. Failure of hip arthroscopy is more likely to fail in older patients, females, or those who have experienced the symptoms of FAI for a long period of time.
When performed on elite athletes, most are able to return their previous level of competition. These athletes also have a higher rate of return to sport than recreational and collegiate athletes.
Long term, randomized controlled trials evaluating the efficacy of conservative and operative treatments are underway.
Epidemiology
There has been limited research on the prevalence of FAI among a general population according to a literature review by Algarni. On the other hand, there are many sources that discuss the prevalence of athletes with the condition especially those that are younger and white. Hockey, tennis, soccer, and equestrian are all sports where the prevalence of a femoral neck abnormalities are higher due to the nature of the sport to force athletes into forced, loaded flexion and internal rotation.
Cam lesions are more common in males, where pincer lesions are more common in females due to differences in anatomical development of the pelvis.
History
FAI is a relatively recent discovery. Its original description is credited to orthopedic surgeon Dr. Reinhold Ganz, who first proposed the condition as a cause for hip osteoarthritis in a publication in 2003.
While the true diagnosis of FAI can be considered a relatively recent discovery, reports of damage to the femoroaceatabular region date back over a century ago in the orthopedic realm of medicine. It was not until the development of an open surgical dislocation procedure was developed that FAI was discovered as an anatomical difference and cause of osteoarthritis. Orthopedic surgeon Dr. Reinhold Ganz can be credited with this discovery in his 2003 publication that discussed the findings and relation to hip osteoarthritis.
Society
Notable persons who have had hip impingement:
- Zach Banner (born 1993), American NFL football offensive tackle for the Pittsburgh Steelers
- Michelle Kwan, American figure skater
- Oscar Hiljemark, Swedish footballer
- Greg Holland, American baseball player
- Devin Mesoraco, American baseball player
- Charlie Morton, American baseball player
- Andy Murray, British tennis player
- Greg Norman, Australian golfer
- Alex Rodriguez, American baseball player
- Isaiah Thomas, American basketball player
Notes
- Unless otherwise specified in boxes, reference is the one marked in header.
- ^ This can also be used in children. At between 5 and 10 years, the minimum normal value is 15°.
References
- ^ Pun S, Kumar D, Lane NE (January 2015). "Femoroacetabular impingement". Arthritis & Rheumatology. 67 (1): 17–27. doi:10.1002/art.38887. PMC 4280287. PMID 25308887.
- Dooley PJ (January 2008). "Femoroacetabular impingement syndrome: Nonarthritic hip pain in young adults". Canadian Family Physician. 54 (1): 42–7. PMC 2293316. PMID 18208954.
- ^ Banerjee P, McLean CR (March 2011). "Femoroacetabular impingement: a review of diagnosis and management". Current Reviews in Musculoskeletal Medicine. 4 (1): 23–32. doi:10.1007/s12178-011-9073-z. PMC 3070009. PMID 21475562.
- Agricola R, Weinans H (February 2016). "What is femoroacetabular impingement?". British Journal of Sports Medicine. 50 (4): 196–7. doi:10.1136/bjsports-2015-094766. PMID 26130699. S2CID 12149232.
- Egger, Anthony C.; Frangiamore, Salvatore; Rosneck, James (2016). "Wolters Kluwer Health - Article Landing Page". Sports Medicine and Arthroscopy Review. 24 (4): e53–e58. doi:10.1097/jsa.0000000000000126. PMID 27811519.
- ^ Menge TJ, Truex NW (May 2018). "Femoroacetabular impingement: a common cause of hip pain". The Physician and Sportsmedicine. 46 (2): 139–144. doi:10.1080/00913847.2018.1436844. PMID 29406812. S2CID 46857494.
- ^ Chakraverty, J.K.; Snelling, N.J. (2012). "Anterior hip pain – Have you considered femoroacetabular impingement?". International Journal of Osteopathic Medicine. 15: 22–27. doi:10.1016/j.ijosm.2011.09.003.
- ^ Ghaffari A, Davis I, Storey T, Moser M (November 2018). "Current Concepts of Femoroacetabular Impingement". Radiologic Clinics of North America. 56 (6): 965–982. doi:10.1016/j.rcl.2018.06.009. PMID 30322493. S2CID 53191134.
- ^ Banerjee, Purnajyoti; Mclean, Christopher R. (March 2011). "Femoroacetabular impingement: a review of diagnosis and management". Current Reviews in Musculoskeletal Medicine. 4 (1): 23–32. doi:10.1007/s12178-011-9073-z. ISSN 1935-973X. PMC 3070009. PMID 21475562.
- ^ Egger, Anthony C.; Frangiamore, Salvatore; Rosneck, James (December 2016). "Femoroacetabular Impingement: A Review". Sports Medicine and Arthroscopy Review. 24 (4): e53–e58. doi:10.1097/JSA.0000000000000126. ISSN 1538-1951. PMID 27811519.
- ^ Kuhlman GS, Domb BG (December 2009). "Hip impingement: identifying and treating a common cause of hip pain". American Family Physician. 80 (12): 1429–34. PMID 20000305.
- Leunig M, Beaulé PE, Ganz R (March 2009). "The concept of femoroacetabular impingement: current status and future perspectives". Clinical Orthopaedics and Related Research. 467 (3): 616–22. doi:10.1007/s11999-008-0646-0. PMC 2635437. PMID 19082681.
- Beck M, Kalhor M, Leunig M, Ganz R (July 2005). "Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip". The Journal of Bone and Joint Surgery. British Volume. 87 (7): 1012–8. doi:10.1302/0301-620X.87B7.15203. PMID 15972923.
- Chakraverty JK, Sullivan C, Gan C, Narayanaswamy S, Kamath S (February 2013). "Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms". AJR. American Journal of Roentgenology. 200 (2): 389–95. doi:10.2214/AJR.12.8546. PMID 23345362. S2CID 35426349.
- ^ van Klij, Pim; Heerey, Joshua; Waarsing, Jan H.; Agricola, Rintje (April 2018). "The Prevalence of Cam and Pincer Morphology and Its Association With Development of Hip Osteoarthritis". The Journal of Orthopaedic and Sports Physical Therapy. 48 (4): 230–238. doi:10.2519/jospt.2018.7816. hdl:1765/105591. ISSN 1938-1344. PMID 29548271. S2CID 4528621.
- Prentice, William E. (November 21, 2016). Principles of athletic training : a guide to evidence-based clinical practice (Sixteenth ed.). New York, NY. ISBN 978-1-259-82400-5. OCLC 953984958.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Starkey, Chad, 1959- (2015). Examination of orthopedic & athletic injuries. Brown, Sara D. (Fourth ed.). Philadelphia. ISBN 978-0-8036-3918-8. OCLC 893974504.
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - King, Matthew G; Lawrenson, Peter R; Semciw, Adam I; Middleton, Kane J; Crossley, Kay M (May 2018). "Lower limb biomechanics in femoroacetabular impingement syndrome: a systematic review and meta-analysis". British Journal of Sports Medicine. 52 (9): 566–580. doi:10.1136/bjsports-2017-097839. ISSN 0306-3674. PMID 29439949. S2CID 4859307.
- Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB (November 2008). "A systematic approach to the plain radiographic evaluation of the young adult hip". The Journal of Bone and Joint Surgery. American Volume. 90 (Suppl 4): 47–66. doi:10.2106/JBJS.H.00756. PMC 2682767. PMID 18984718.
- Ruiz Santiago, Fernando; Santiago Chinchilla, Alicia; Ansari, Afshin; Guzmán Álvarez, Luis; Castellano García, Maria del Mar; Martínez Martínez, Alberto; Tercedor Sánchez, Juan (2016). "Imaging of Hip Pain: From Radiography to Cross-Sectional Imaging Techniques". Radiology Research and Practice. 2016: 1–15. doi:10.1155/2016/6369237. ISSN 2090-1941. PMC 4738697. PMID 26885391.
- ^ Fa, Liangguo; Wang, Qing; Ma, Xiangxing (2014). "Superiority of the modified Tönnis angle over the Tönnis angle in the radiographic diagnosis of acetabular dysplasia". Experimental and Therapeutic Medicine. 8 (6): 1934–1938. doi:10.3892/etm.2014.2009. ISSN 1792-0981. PMC 4218684. PMID 25371759.
- Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (May 2002). "The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement". The Journal of Bone and Joint Surgery. British Volume. 84 (4): 556–60. doi:10.1302/0301-620X.84B4.12014. PMID 12043778.
- Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC (November 2011). "The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity". Clinical Orthopaedics and Related Research. 469 (11): 3229–40. doi:10.1007/s11999-011-1945-4. PMC 3183218. PMID 21761254.
- Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA (January 2007). "Noninvasive three-dimensional assessment of femoroacetabular impingement". Journal of Orthopaedic Research. 25 (1): 122–31. doi:10.1002/jor.20309. PMID 17054112. S2CID 26697099.
- http://www.clinicalgraphics.com Dynamic motion simulation for hip impingement.
- Bedi, Asheesh; Chen, Neal; Robertson, William; Kelly, Bryan T. (2008). "The Management of Labral Tears and Femoroacetabular Impingement of the Hip in the Young, Active Patient". Arthroscopy: The Journal of Arthroscopic & Related Surgery. 24 (10): 1135–1145. doi:10.1016/j.arthro.2008.06.001. PMID 19028166.
- ^ Cakic, J.; Patricios, J. (July 2014). "Femoroacetabular impingement: prevention or intervention? The sports physician's quandary". British Journal of Sports Medicine. 48 (14): 1073–1074. doi:10.1136/bjsports-2014-093792. hdl:2263/42041. ISSN 1473-0480. PMID 24858362. S2CID 7104674.
- ^ Casartelli, Nicola C.; Bizzini, Mario; Kemp, Joanne; Naal, Florian D.; Leunig, Michael; Maffiuletti, Nicola A. (May 2018). "What treatment options exist for patients with femoroacetabular impingement syndrome but without surgical indication?". British Journal of Sports Medicine. 52 (9): 552–553. doi:10.1136/bjsports-2017-098059. ISSN 1473-0480. PMID 28935688. S2CID 4817032.
- Loudon, Janice K.; Reiman, Michael P. (May 2014). "Conservative management of femoroacetabular impingement (FAI) in the long distance runner". Physical Therapy in Sport. 15 (2): 82–90. doi:10.1016/j.ptsp.2014.02.004. ISSN 1873-1600. PMID 24629576.
- ^ Nasser, Rima; Domb, Benjamin (2018). "Bone & Joint". EFORT Open Reviews. 3 (4): 121–129. doi:10.1302/2058-5241.3.170041. PMC 5941972. PMID 29780619.
- Bhatia, Sanjeev; Lee, Simon; Shewman, Elizabeth; Mather, Richard C.; Salata, Michael J.; Bush-Joseph, Charles A.; Nho, Shane J. (September 2015). "Effects of acetabular rim trimming on hip joint contact pressures: how much is too much?". The American Journal of Sports Medicine. 43 (9): 2138–2145. doi:10.1177/0363546515590400. ISSN 1552-3365. PMID 26180260. S2CID 1172435.
- Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ (February 2011). "Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement". Arthroscopy. 27 (2): 252–69. doi:10.1016/j.arthro.2010.09.011. PMID 21266276.
- Kierkegaard, Signe; Langeskov-Christensen, Martin; Lund, Bent; Naal, Florian D.; Mechlenburg, Inger; Dalgas, Ulrik; Casartelli, Nicola C. (April 2017). "Pain, activities of daily living and sport function at different time points after hip arthroscopy in patients with femoroacetabular impingement: a systematic review with meta-analysis". British Journal of Sports Medicine. 51 (7): 572–579. doi:10.1136/bjsports-2016-096618. ISSN 1473-0480. PMID 27845683. S2CID 11254041.
- ^ Minkara, Anas A.; Westermann, Robert W.; Rosneck, James; Lynch, T. Sean (February 2019). "Systematic Review and Meta-analysis of Outcomes After Hip Arthroscopy in Femoroacetabular Impingement". The American Journal of Sports Medicine. 47 (2): 488–500. doi:10.1177/0363546517749475. ISSN 0363-5465. PMID 29373805. S2CID 25695274.
- Kierkegaard, Signe; Langeskov-Christensen, Martin; Lund, Bent; Naal, Florian D; Mechlenburg, Inger; Dalgas, Ulrik; Casartelli, Nicola C (April 2017). "Pain, activities of daily living and sport function at different time points after hip arthroscopy in patients with femoroacetabular impingement: a systematic review with meta-analysis". British Journal of Sports Medicine. 51 (7): 572–579. doi:10.1136/bjsports-2016-096618. ISSN 0306-3674. PMID 27845683. S2CID 11254041.
- Casartelli, Nicola C; Leunig, Michael; Maffiuletti, Nicola A; Bizzini, Mario (June 2015). "Return to sport after hip surgery for femoroacetabular impingement: a systematic review". British Journal of Sports Medicine. 49 (12): 819–824. doi:10.1136/bjsports-2014-094414. ISSN 0306-3674. PMID 25841163. S2CID 5811818.
- Wall PD, Brown JS, Parsons N, Buchbinder R, Costa ML, Griffin D (September 2014). "Surgery for treating hip impingement (femoroacetabular impingement)". The Cochrane Database of Systematic Reviews. 9 (9): CD010796. doi:10.1002/14651858.CD010796.pub2. PMC 11166468. PMID 25198064.
- ^ Algarni, Abdulrahman D. (July 1, 2013). "Femoroacetabular impingement in athletes: A review of the current literature". Saudi Journal of Sports Medicine. 13 (2): 63. doi:10.4103/1319-6308.123370. ISSN 1319-6308. S2CID 72759055.
- Mallets, Emma; Turner, Ann; Durbin, Jeremy; Bader, Alexander; Murray, Leigh (July 2019). "Short-Term Outcomes of Conservative Treatment for Femoroacetabular Impingement: A Systematic Review and Meta-Analysis". International Journal of Sports Physical Therapy. 14 (4): 514–524. doi:10.26603/ijspt20190514. ISSN 2159-2896. PMC 6670054. PMID 31440404.
- ^ Hessel, Joy A. (May 2014). "Femoroacetabular impingement in athletes". Orthopedic Nursing. 33 (3): 137–139, quiz 140–141. doi:10.1097/NOR.0000000000000045. ISSN 1542-538X. PMID 24845836. S2CID 22837401.
- Ganz, Reinhold; Parvizi, Javad; Beck, Martin; Leunig, Michael; Nötzli, Hubert; Siebenrock, Klaus A. (December 2003). "Femoroacetabular impingement: a cause for osteoarthritis of the hip". Clinical Orthopaedics and Related Research (417): 112–120. doi:10.1097/01.blo.0000096804.78689.c2. ISSN 0009-921X. PMID 14646708. S2CID 37330685.
- "Surgery now, flexibility later for Banner". USCFootball.com.
- "Hiljemark måste opereras - blir borta i tre månader". fotbollskanalen (in Swedish). Retrieved October 28, 2019.
- "Hip issue lands struggling Cardinals reliever Holland on DL". AP NEWS. May 26, 2018. Retrieved January 19, 2019.
- "Reds catcher Devin Mesoraco holding off on hip surgery for now". May 5, 2015.
- "/ccpa/". TribLIVE.com.
- Marston, Robert (January 2, 2018). "Medical opinion: Andy Murray may have degenerative arthritis, leaving hip replacement as the likely optionÂ". The Telegraph. ISSN 0307-1235. Retrieved January 19, 2019.
- "Isaiah Thomas Ruled Out for Remainder of Playoffs". NBA.com.
Further reading
- Lewis CL, Sahrmann SA (January 2006). "Acetabular labral tears". Physical Therapy. 86 (1): 110–21. doi:10.1093/ptj/86.1.110. PMID 16386066.
External links
- Femoroacetabular Impingement (FAI) on OrthoInfo
- IMPAKT-HiP (Investigations of Mobility, Physical Activity, and Knowledge in Hip Pain) Study by the Arthritis Research Centre of Canada