
Immunoglobulin A (Ig A, also referred to as sIgA in its secretory form) is an antibody that plays a role in the immune function of mucous membranes. The amount of IgA produced in association with mucosal membranes is greater than all other types of antibody combined. In absolute terms, between three and five grams are secreted into the intestinal lumen each day. This represents up to 15% of total immunoglobulins produced throughout the body.
IgA has two subclasses (IgA1 and IgA2) and can be produced as a monomeric as well as a dimeric form. The IgA dimeric form is the most prevalent and, when it has bound the Secretory component, is also called secretory IgA (sIgA). sIgA is the main immunoglobulin found in mucous secretions, including tears, saliva, sweat, colostrum and secretions from the genitourinary tract, gastrointestinal tract, prostate and respiratory epithelium. It is also found in small amounts in blood. The secretory component of sIgA protects the immunoglobulin from being degraded by proteolytic enzymes; thus, sIgA can survive in the harsh gastrointestinal tract environment and provide protection against microbes that multiply in body secretions. sIgA can also inhibit inflammatory effects of other immunoglobulins. IgA is a poor activator of the complement system, and opsonizes only weakly.
Forms
IgA1 vs. IgA2
IgA exists in two isotypes, IgA1 and IgA2. They are both heavily glycosylated proteins. While IgA1 predominates in serum (~80%), IgA2 percentages are higher in secretions than in serum (~35% in secretions); the ratio of IgA1 and IgA2 secreting cells varies in the different lymphoid tissues of the human body:
- IgA1 is the predominant IgA subclass found in serum. Most lymphoid tissues have a predominance of IgA1-producing cells.
- In IgA2, the heavy and light chains are not linked with disulfide, but with non-covalent bonds. In secretory lymphoid tissues (e.g., gut-associated lymphoid tissue, or GALT), the share of IgA2 production is larger than in the non-secretory lymphoid organs (e.g. spleen, peripheral lymph nodes).
Both IgA1 and IgA2 have been found in external secretions like colostrum, maternal milk, tears and saliva, where IgA2 is more prominent than in the blood. Polysaccharide antigens tend to induce more IgA2 than protein antigens.
Both IgA1 and IgA2 can be in membrane-bound form. (see B-cell receptor)
The heavy chain of IgA1, in contrast to IgA2, features an extended hinge region. This is thought to allow IgA1 to adapt more effectively to varying epitope spacings on multivalent antigens, while also presenting less resistance to bacterial proteases.
Serum vs. secretory IgA
It is also possible to distinguish forms of IgA based upon their location – serum IgA vs. secretory IgA.
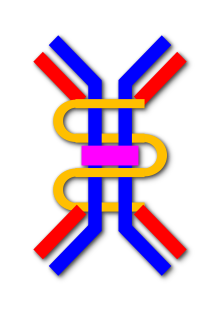
In secretory IgA, the form found in secretions, polymers of 2–4 IgA monomers are linked by two additional chains; as such, the molecular weight of slgA is 385kD. One of these is the J chain (joining chain), which is a polypeptide of molecular mass 15kD, rich with cysteine and structurally completely different from other immunoglobulin chains. This chain is formed in the IgA-secreting cells.
The oligomeric forms of IgA in the external (mucosal) secretions also contain a polypeptide of a much larger molecular mass (70 kD) called the secretory component that is produced by epithelial cells. This molecule originates from the poly-Ig receptor (130 kD) that is responsible for the uptake and transcellular transport of oligomeric (but not monomeric) IgA across the epithelial cells and into secretions such as tears, saliva, sweat and gut fluid.
Physiology
Serum IgA
In the blood, IgA interacts with an Fc receptor called FcαRI (or CD89), which is expressed on immune effector cells, to initiate inflammatory reactions. Ligation of FcαRI by IgA containing immune complexes causes antibody-dependent cell-mediated cytotoxicity (ADCC), degranulation of eosinophils and basophils, phagocytosis by monocytes, macrophages, and neutrophils, and triggering of respiratory burst activity by polymorphonuclear leukocytes. Unlike IgM and IgG, which activate complement through the classical pathway, IgA can activate complement via the alternative and lectin pathways.
Secretory IgA
The high prevalence of IgA in mucosal areas is a result of a cooperation between plasma cells that produce polymeric IgA (pIgA), and mucosal epithelial cells that express polymeric immunoglobulin receptor (pIgR). Polymeric IgA (mainly the secretory dimer) is produced by plasma cells in the lamina propria adjacent to mucosal surfaces. It binds to the pIgR on the basolateral surface of epithelial cells, and is taken up into the cell via endocytosis. The receptor-IgA complex passes through the cellular compartments before being secreted on the luminal surface of the epithelial cells, still attached to the receptor. Proteolysis of the receptor occurs, and the dimeric IgA molecule, along with a portion of the receptor known as the secretory component (SC), is free to diffuse throughout the lumen, with dimeric IgA and SC together forming the so-called secretory IgA (sIgA) In the gut, IgA can bind to the mucus layer covering the epithelial cells. In this way, a barrier capable of neutralizing threats before they reach the epithelial cells is formed.
Secretory IgA levels fluctuate diurnally, with the highest levels found in the small intestine and feces around ZT6, the middle of the light period. The regulation of IgA secretion is related to the microbiota, and IgA is known to control specific members of oscillating microbes through direct interactions. However, the underlying cause of the rhythmic secretion of IgA is not completely understood and may differ from one region of the body to another.
Production of sIgA against specific antigens depends on sampling of M cells and underlying dendritic cells, T cell activation, and B cell class switching in GALT, mesenteric lymph nodes, and isolated lymphoid follicles in the small intestine.
sIgA primarily acts by blockading epithelial receptors (e.g. by binding their ligands on pathogens), by sterically hindering attachment to epithelial cells, and by immune exclusion. Immune exclusion is a process of agglutinating polyvalent antigens or pathogens by crosslinking them with antibody, trapping them in the mucus layer, and/or clearing them peristaltically. The oligosaccharide chains of the component of IgA can associate with the mucus layer that sits atop epithelial cells. Since sIgA is a poor opsonin and activator of complement, simply binding a pathogen isn't necessarily enough to contain it—specific epitopes may have to be bound to sterically hinder access to the epithelium.
Clearance of IgA is mediated at least in part by asialoglycoprotein receptors, which recognizes galactose-terminating IgA N-glycans.
Pathology
Genetic
Decreased or absent IgA due to an inherited inability to produce IgA is termed selective IgA deficiency and can produce a clinically significant immunodeficiency.
Anti-IgA antibodies, sometimes present in individuals with low or absent IgA, can result in serious anaphylactic reactions when transfused with blood products that incidentally contain IgA. However, most persons with suspected IgA anaphylactic reactions had experienced acute generalized reactions that were from causes other than anti-IgA transfusion.
Microbial
Neisseria species including Neisseria gonorrhoeae (which causes gonorrhea), Streptococcus pneumoniae, and Haemophilus influenzae type B all release a protease that destroys IgA. Additionally, Blastocystis species have been shown to have several subtypes that generate cysteine and aspartic protease enzymes which degrade human IgA.
Autoimmune and immune-mediated
IgA nephropathy is caused by IgA deposits in the kidneys. The pathogenesis involves the production of hypoglycosylated IgA1, which accumulates and subsequently leads to the formation of immune complexes and the production of IgA-specific IgG, further leading to tissue inflammation.
Celiac disease involves IgA pathology due to the presence of IgA antiendomysial antibodies. Additional testing has been conducted using IgA trans-glutaminase autoantibodies which has been identified as a specific and sensitive for the detection of celiac disease.
Henoch–Schönlein purpura (HSP) is a systemic vasculitis caused by deposits of IgA and complement component 3 (C3) in small blood vessels. HSP occurs usually in small children and involves the skin and connective tissues, scrotum, joints, gastrointestinal tract and kidneys. It usually follows an upper respiratory infection and resolves within a couple weeks as the liver clears out the IgA aggregates.
Linear IgA bullous dermatosis and IgA pemphigus are two examples of IgA-mediated immunobullous diseases. IgA-mediated immunobullous diseases can often be difficult to treat even with usually effective medications such as rituximab.
Drug-induced
Vancomycin can induce a linear IgA bullous dermatosis in some patients.
See also
References
- Bonner A, Almogren A, Furtado PB, Kerr MA, Perkins SJ (January 2009). "Location of secretory component on the Fc edge of dimeric IgA1 reveals insight into the role of secretory IgA1 in mucosal immunity". Mucosal Immunology. 2 (1): 74–84. doi:10.1038/mi.2008.68. PMID 19079336.
- Bonner A, Almogren A, Furtado PB, Kerr MA, Perkins SJ (February 2009). "The nonplanar secretory IgA2 and near planar secretory IgA1 solution structures rationalize their different mucosal immune responses". The Journal of Biological Chemistry. 284 (8): 5077–87. doi:10.1074/jbc.M807529200. PMC 2643523. PMID 19109255.
- Făgărășan S.; Honjo T. (January 2003). "Intestinal IgA synthesis: regulation of front-line body defences". Nature Reviews. Immunology. 3 (1): 63–72. doi:10.1038/nri982. PMID 12511876. S2CID 2586305.
- Brandtzaeg P, Pabst R (November 2004). "Let's go mucosal: communication on slippery ground". Trends in Immunology. 25 (11): 570–7. doi:10.1016/j.it.2004.09.005. PMID 15489184.
- Macpherson AJ, Slack E (November 2007). "The functional interactions of commensal bacteria with intestinal secretory IgA". Current Opinion in Gastroenterology. 23 (6): 673–8. doi:10.1097/MOG.0b013e3282f0d012. PMID 17906446. S2CID 8445606.
- Junqueira LC, Carneiro J (2003). Basic Histology. McGraw-Hill. ISBN 978-0-8385-0590-8.
- Holmgren J, Czerkinsky C (April 2005). "Mucosal immunity and vaccines". Nature Medicine. 11 (4 Suppl): S45–53. doi:10.1038/nm1213. PMID 15812489.
- Janeway, C.A.; Travers, P.; Walport, M.; Shlomchik, M.J. (2001). Immunobiology: The Immune System in Health and Disease (5th ed.). New York: Garland Science. pp. 387–397. ISBN 0-8153-3642-X.
- ^ Maverakis E, Kim K, Shimoda M, Gershwin ME, Patel F, Wilken R, Raychaudhuri S, Ruhaak LR, Lebrilla CB (February 2015). "Glycans in the immune system and The Altered Glycan Theory of Autoimmunity: a critical review". Journal of Autoimmunity. 57: 1–13. doi:10.1016/j.jaut.2014.12.002. PMC 4340844. PMID 25578468.
- ^ Delacroix DL, Dive C, Rambaud JC, Vaerman JP (October 1982). "IgA subclasses in various secretions and in serum". Immunology. 47 (2): 383–5. PMC 1555453. PMID 7118169.
- ^ Simell B, Kilpi T, Käyhty H (March 2006). "Subclass distribution of natural salivary IgA antibodies against pneumococcal capsular polysaccharide of type 14 and pneumococcal surface adhesin A (PsaA) in children". Clinical and Experimental Immunology. 143 (3): 543–9. doi:10.1111/j.1365-2249.2006.03009.x. PMC 1809616. PMID 16487254.
- Macpherson AJ, McCoy KD, Johansen FE, Brandtzaeg P (January 2008). "The immune geography of IgA induction and function". Mucosal Immunology. 1 (1): 11–22. doi:10.1038/mi.2007.6. PMID 19079156.
- Hung AF, Chen JB, Chang TW (August 2008). "Alleles and isoforms of human membrane-bound IgA1". Molecular Immunology. 45 (13): 3624–30. doi:10.1016/j.molimm.2008.04.023. PMID 18538846. S2CID 26094982.
- Flajnik, M. F.; Singh, Nevil; Holland, Steven M., eds. (2023). Paul's fundamental immunology (8th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wikins. pp. 662–663. ISBN 978-1-9751-4253-7.
- ^ Snoeck V, Peters IR, Cox E (2006). "The IgA system: a comparison of structure and function in different species" (PDF). Veterinary Research. 37 (3): 455–67. doi:10.1051/vetres:2006010. PMID 16611558.
- Daha, Nina A.; Banda, Nirmal K.; Roos, Anja; Beurskens, Frank J.; Bakker, Joost M.; Daha, Mohamed R.; Trouw, Leendert A. (Aug 2011). "Complement activation by (auto-) antibodies". Molecular Immunology. 48 (14): 1656–1665. doi:10.1016/j.molimm.2011.04.024.
- Kaetzel CS, Robinson JK, Chintalacharuvu KR, Vaerman JP, Lamm ME (October 1991). "The polymeric immunoglobulin receptor (secretory component) mediates transport of immune complexes across epithelial cells: a local defense function for IgA". Proceedings of the National Academy of Sciences of the United States of America. 88 (19): 8796–800. Bibcode:1991PNAS...88.8796K. doi:10.1073/pnas.88.19.8796. PMC 52597. PMID 1924341.
- ^ Ratiner, Karina; Fachler-Sharp, Tahel; Elinav, Eran (16 January 2023). "Small Intestinal Microbiota Oscillations, Host Effects and Regulation-A Zoom into Three Key Effector Molecules". Biology. 12 (1): 142. doi:10.3390/biology12010142. PMC 9855434. PMID 36671834.
- ^ Mantis NJ, Rol N, Corthésy B (November 2011). "Secretory IgA's complex roles in immunity and mucosal homeostasis in the gut". Mucosal Immunology. 4 (6): 603–11. doi:10.1038/mi.2011.41. PMC 3774538. PMID 21975936.
- Yel L (January 2010). "Selective IgA deficiency". Journal of Clinical Immunology. 30 (1): 10–6. doi:10.1007/s10875-009-9357-x. PMC 2821513. PMID 20101521.
- Sandler SG, Mallory D, Malamut D, Eckrich R (January 1995). "IgA anaphylactic transfusion reactions". Transfusion Medicine Reviews. 9 (1): 1–8. doi:10.1016/S0887-7963(05)80026-4. PMID 7719037.
- Halter R, Pohlner J, Meyer TF (July 1984). "IgA protease of Neisseria gonorrhoeae: isolation and characterization of the gene and its extracellular product". The EMBO Journal. 3 (7): 1595–601. doi:10.1002/j.1460-2075.1984.tb02016.x. PMC 557564. PMID 6430698.
- Proctor M, Manning PJ (September 1990). "Production of immunoglobulin A protease by Streptococcus pneumoniae from animals". Infection and Immunity. 58 (9): 2733–7. doi:10.1128/IAI.58.9.2733-2737.1990. PMC 313560. PMID 2117567.
- St Geme JW, de la Morena ML, Falkow S (October 1994). "A Haemophilus influenzae IgA protease-like protein promotes intimate interaction with human epithelial cells". Molecular Microbiology. 14 (2): 217–33. doi:10.1111/j.1365-2958.1994.tb01283.x. PMID 7830568. S2CID 30615746.
- Roberts T, Stark D, Harkness J, Ellis J (2014). "Update on the pathogenic potential and treatment options for Blastocystis sp". Gut Pathogens. 6: 17. doi:10.1186/1757-4749-6-17. PMC 4039988. PMID 24883113.
- Lai, Kar Neng; Tang, Sydney C. W.; Schena, Francesco Paolo; Novak, Jan; Tomino, Yasuhiko; Fogo, Agnes B.; Glassock, Richard J. (2016). "IgA nephropathy". Nature Reviews Disease Primers. 2: 16001. doi:10.1038/nrdp.2016.1. PMID 27189177. S2CID 3989355.
- Prince HE, Norman GL, Binder WL (March 2000). "Immunoglobulin A (IgA) deficiency and alternative celiac disease-associated antibodies in sera submitted to a reference laboratory for endomysial IgA testing". Clinical and Diagnostic Laboratory Immunology. 7 (2): 192–6. doi:10.1128/cdli.7.2.192-196.2000. PMC 95847. PMID 10702491.
- Cunningham-Rundles C (September 2001). "Physiology of IgA and IgA deficiency". Journal of Clinical Immunology. 21 (5): 303–9. doi:10.1023/A:1012241117984. PMID 11720003. S2CID 13285781.
- Malamut G, Cording S, Cerf-Bensussan N (June 26, 2019). "Recent advances in celiac disease and refractory celiac disease". F1000Res. 8: 969. doi:10.12688/f1000research.18701.1. PMC 6600866. PMID 31297187.
- Cunningham-Rundles C (February 2000). "Comparison of assays for anti-endomysial and anti-transglutaminase antibodies for diagnosis of pediatric celiac disease". The Israel Medical Association Journal. 2 (2): 122–5. PMID 10804933.
- Rai A, Nast C, Adler S (December 1999). "Henoch-Schönlein purpura nephritis". Journal of the American Society of Nephrology. 10 (12): 2637–44. doi:10.1681/ASN.V10122637. PMID 10589705.
- He Y, Shimoda M, Ono Y, Villalobos IB, Mitra A, Konia T, Grando SA, Zone JJ, Maverakis E (June 2015). "Persistence of Autoreactive IgA-Secreting B Cells Despite Multiple Immunosuppressive Medications Including Rituximab". JAMA Dermatology. 151 (6): 646–50. doi:10.1001/jamadermatol.2015.59. PMID 25901938.
- Go JR, Abu Saleh OM (October 2020). "Vancomycin-Induced Linear IgA Bullous Dermatosis". The New England Journal of Medicine. 383 (16): 1577. doi:10.1056/NEJMicm2003334. PMID 33053287. S2CID 222420540.
External links
- Immunoglobulin+A at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Herich, R. (2017). "Is the role of IgA in local immunity completely known?". Food and Agricultural Immunology. 28 (2): 223–237. doi:10.1080/09540105.2016.1258547.
| Lymphocytic adaptive immune system and complement | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lymphoid |
| ||||||||
| Lymphocytes | |||||||||
| Substances | |||||||||
| Antibodies | |
|---|---|
| Main types | |
| Chains |
|