| Nissen fundoplication | |
|---|---|
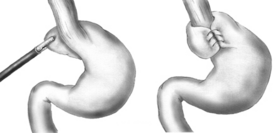 Diagram of a Nissen fundoplication. Diagram of a Nissen fundoplication. | |
| Other names | Laparoscopic Nissen fundoplication |
| ICD-9-CM | 44.66, 44.67 |
| [edit on Wikidata] | |
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal (270° anterior), Belsey (270° anterior transthoracic), Dor (anterior 180–200°), Lind (300° posterior), and Toupet fundoplications (posterior 270°) are alternative procedures with somewhat different indications and outcomes.
History
Dr. Rudolph Nissen (1896–1981) first performed the procedure in 1955 and published the results of two cases in a 1956 Swiss Medical Weekly. In 1961 he published a more detailed overview of the procedure. Nissen originally called the surgery "gastroplication". The procedure has borne his name since it gained popularity in the 1970s.
Indications
The most common indication for a fundoplication is GERD that has failed lifestyle modification and medical management. Patients that continue to have reflux symptoms or that have had uncontrolled reflux symptoms for more than 5 years are also candidates for surgical management. Complications that arise from long term GERD such as severe esophagitis, stricture formation, and ulcer development, all of which can be seen on endoscopy, warrant surgical intervention. Presence of Barrett's esophagus is not an indication, as the benefit of a fundoplication in preventing progression into adenocarcinoma is controversial. Respiratory symptoms and upper airway symptoms such as cough, asthma, hoarseness are also indications for surgical intervention. In the pediatric population, infants who fail to thrive or have inadequate weight gain despite proton-pump inhibitor (PPI) therapy may also benefit from fundoplication.
Technique

In a fundoplication, the gastric fundus (upper part) of the stomach is wrapped, or plicated, around the lower end of the esophagus and stitched in place, reinforcing the closing function of the lower esophageal sphincter (LES). The esophageal hiatus is also narrowed down by sutures to prevent or treat concurrent hiatal hernia, in which the fundus slides up through the enlarged esophageal hiatus of the diaphragm. The surgeon should begin with ligating and dividing the short gastric arteries.
In a Nissen fundoplication, also called a complete fundoplication, the fundus is wrapped the entire 360 degrees around the esophagus. In contrast, surgery for achalasia is generally accompanied by either a Dor or Toupet partial fundoplication, which is less likely than a Nissen wrap to aggravate the dysphagia that characterizes achalasia. In a Dor (anterior) fundoplication, the fundus is laid over the top of the esophagus; while in a Toupet (posterior) fundoplication, the fundus is wrapped around the back of the esophagus.
The procedure can be performed with open surgery but is now routinely performed laparoscopically, as laparoscopic surgery has decreased post-operative complications and decreased hospital stay. When used to alleviate gastroesophageal reflux symptoms in patients with delayed gastric emptying, it is frequently combined with modification of the pylorus via pyloromyotomy or pyloroplasty.
This procedure can also be completed robotically. Outcomes comparing laparoscopic fundoplication to robotic fundoplication show similar clinical outcomes, but robotic fundoplication is more likely to have an increased length of operative time and financial cost.
Mechanism of relief
Whenever the stomach contracts, it also closes off the esophagus instead of squeezing stomach acids into it. This prevents the reflux of gastric acid (in GERD). Although antacids and PPI drug therapy can reduce the effects of reflux acid, successful surgical treatment has the advantage of eliminating drug side-effects and damaging effects from other components of reflux such as bile or gastric contents. The Nissen fundoplication reduces reflux by reinforcing the LES by increasing LES pressure and increasing the LES length.
Effectiveness
Nissen (complete) fundoplication is generally considered to be safe and effective, with a mortality rate of less than 1% and many of the most common post-operative complications minimized or eliminated by the partial fundoplication procedures now more commonly used. Studies have shown that after 10 years, 89.5% of patients are still symptom-free. When compared to stand alone medical therapy with PPIs, Nissen fundoplication has been found to be superior in reducing acid reflux as well as the symptoms associated with reflux. Fundoplication was found to be better at increasing LES pressure than PPI therapy, whilst having similar risk for adverse events. In patients with non-acid reflux, a hiatal hernia, or respiratory symptoms, surgical intervention was found to be more effective at controlling symptoms than PPIs alone.
Complications
Complications include "gas bloat syndrome", dysphagia (trouble swallowing), dumping syndrome, excessive scarring, vagus nerve injury and, rarely, achalasia. The fundoplication can also come undone over time in about 5–10% of cases, leading to recurrence of symptoms. If the symptoms warrant a repeat surgery, the surgeon may use Marlex or another form of artificial mesh to strengthen the connection. Postoperative ileus, which is common after abdominal surgery, is possible.
In "gas bloat syndrome", fundoplication can alter the mechanical ability of the stomach to eliminate swallowed air by belching, leading to an accumulation of gas in the stomach or small intestine. Data varies, but some degree of gas-bloat may occur in as many as 41% of Nissen patients, whereas the occurrence is less with patients undergoing partial anterior fundoplication. Gas bloat syndrome is usually self-limiting within 2 to 4 weeks, but in some it may persist. The offending gas may also come from dietary sources (especially carbonated beverages), or involuntary swallowing of air (aerophagia). If postoperative gas-bloat syndrome does not resolve with time, dietary restrictions, counseling regarding aerophagia, medications, and correction – either by endoscopic balloon dilatation or repeat surgery to revise the Nissen fundoplication to a partial fundoplication – may be necessary.
Acute dysphagia or short term trouble swallowing is a symptom that most patients will have after having a fundoplication. Patients who have dysphagia prior to surgery are more likely to have some dysphagia post-operatively. Symptoms of dysphagia will often resolve on their own within a few months. Short term dysphagia is controlled by modifying diet to include more easily swallowed food such as liquids and soft foods. Dysphagia that persists longer than 3 months will need further evaluation, typically with a barium swallow study, esophageal manometry, or endoscopy. Structural changes such as movement of the wrap, herniation, development of stenosis or stricture may lead to persistent dysphagia. Previously undiagnosed achalasia or a wrap that is too tight may also lead to persistent dysphagia. Depending on the etiology of persistent dysphagia, a trial of PPI therapy, endoscopic dilation, or surgical revision may be necessary.
Vomiting is sometimes impossible or, if not, very painful after a fundoplication, with the likelihood of this complication typically decreasing in the months after surgery. In some cases, the purpose of this operation is to correct excessive vomiting. Initially, vomiting is impossible; however, small amounts of vomit may be produced after the wrap settles over time, and in extreme cases such as alcohol poisoning or food poisoning, the patient may be able to vomit freely with some amount of pain.
See also
References
- ^ Minjarez, Renee C.; Jobe, Blair A. (16 May 2006). "Surgical therapy for gastroesophageal reflux disease". GI Motility Online. doi:10.1038/gimo56 (inactive 1 November 2024).
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - Nissen R (1956). "Eine einfache Operation zur Beeinflussung der Refluxösophagitis" [A Simple Operation for Control of Reflux Esophagitis]. Schweizerische Medizinische Wochenschrift (in German). 86 (Suppl 20): 590–592. PMID 13337262. NAID 10008497300.
- Nissen R (1961). "Gastropexy and "Fundoplication" in Surgical Treatment of Hiatal Hernia". The American Journal of Digestive Diseases. 6 (10): 954–61. doi:10.1007/BF02231426. PMID 14480031. S2CID 29470586.
- Stylopoulos N, Rattner DW; Rattner (2005). "The History of Hiatal Hernia surgery: From Bowditch to Laparoscopy". Ann. Surg. 241 (1): 185–93. doi:10.1097/01.sla.0000149430.83220.7f. PMC 1356862. PMID 15622007.
- Frazzoni, Marzio (2014). "Laparoscopic fundoplication for gastroesophageal reflux disease". World Journal of Gastroenterology. 20 (39): 14272–14279. doi:10.3748/wjg.v20.i39.14272. ISSN 1007-9327. PMC 4202356. PMID 25339814.
- ^ Wykypiel, H.; Wetscher, G. J.; Klingler, P.; Glaser, K. (November 2005). "The Nissen fundoplication: indication, technical aspects and postoperative outcome". Langenbeck's Archives of Surgery. 390 (6): 495–502. doi:10.1007/s00423-004-0494-7. ISSN 1435-2443. PMID 15351884. S2CID 278325.
- ^ Patti, Marco G. (2016-01-01). "An Evidence-Based Approach to the Treatment of Gastroesophageal Reflux Disease". JAMA Surgery. 151 (1): 73–78. doi:10.1001/jamasurg.2015.4233. ISSN 2168-6254. PMID 26629969.
- Slater, Bethany J.; Rothenberg, Steven S. (December 2017). "Fundoplication". Clinics in Perinatology. 44 (4): 795–803. doi:10.1016/j.clp.2017.08.009. PMID 29127961. S2CID 242477061.
- Holcomb GW 3rd, St Peter SD (2019). "Error traps and safety steps when performing a laparoscopic Nissen fundoplication". Semin Pediatr Surg. 28 (3): 160–163. doi:10.1053/j.sempedsurg.2019.04.019. PMID 31171151. S2CID 150096013.
- Eshraghi, Niknam; Farahmand, Mehrdad; Soot, Scott J.; Rand-Luby, Leslie; Deveney, Clifford W.; Sheppard, Brett C. (May 1998). "Comparison of outcomes of open versus laparoscopic nissen fundoplication performed in a single practice". The American Journal of Surgery. 175 (5): 371–374. doi:10.1016/s0002-9610(98)00049-x. ISSN 0002-9610. PMID 9600280.
- Markar, S. R.; Karthikesalingam, A. P.; Hagen, M. E.; Talamini, M.; Horgan, S.; Wagner, O. J. (2010). "Robotic vs. laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease: systematic review and meta-analysis". The International Journal of Medical Robotics and Computer Assisted Surgery. 6 (2): 125–131. doi:10.1002/rcs.309. PMID 20506440. S2CID 23663135.
- Richter, Joel E.; Kumar, Ambuj; Lipka, Seth; Miladinovic, Branko; Velanovich, Vic (April 2018). "Efficacy of Laparoscopic Nissen Fundoplication vs Transoral Incisionless Fundoplication or Proton Pump Inhibitors in Patients With Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-analysis". Gastroenterology. 154 (5): 1298–1308.e7. doi:10.1053/j.gastro.2017.12.021. ISSN 1528-0012. PMID 29305934.
- Tristão, Luca Schiliró; Tustumi, Francisco; Tavares, Guilherme; Bernardo, Wanderley Marques (April 2021). "Fundoplication versus oral proton pump inhibitors for gastroesophageal reflux disease: a systematic review and meta-analysis of randomized clinical trials". Esophagus. 18 (2): 173–180. doi:10.1007/s10388-020-00806-w. ISSN 1612-9067. PMID 33527310. S2CID 231746674.
- Waring JP (1999). "Postfundoplication complications. Prevention and management". Gastroenterol. Clin. North Am. 28 (4): 1007–19, viii–ix. doi:10.1016/S0889-8553(05)70102-3. PMID 10695014.
- Curet MJ, Josloff RK, Schoeb O, Zucker KA; Josloff; Schoeb; Zucker (1999). "Laparoscopic reoperation for failed antireflux procedures". Archives of Surgery. 134 (5): 559–63. doi:10.1001/archsurg.134.5.559. PMID 10323431.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Booth, M.I. (2003). "Treatments: What Is the Current Rate of Gas-Bloat Syndrome Following Open and Laparoscopic Antireflux Surgery?". In Giuli, R.; Siewert, J.R; Couturier, D.; Scarpignato, C. (eds.). Barrett's Esophagus. Vol. 6. OESO, UNESCO.
- Herron, D. M.; Swanström, L. L.; Ramzi, N.; Hansen, P. D. (December 1999). "Factors predictive of dysphagia after laparoscopic Nissen fundoplication". Surgical Endoscopy. 13 (12): 1180–1183. doi:10.1007/PL00009616. ISSN 0930-2794. PMID 10594261. S2CID 20831084.
- ^ Wo, J. M.; Trus, T. L.; Richardson, W. S.; Hunter, J. G.; Branum, G. D.; Mauren, S. J.; Waring, J. P. (November 1996). "Evaluation and management of postfundoplication dysphagia". The American Journal of Gastroenterology. 91 (11): 2318–2322. ISSN 0002-9270. PMID 8931410.
- ^ Yadlapati, Rena; Hungness, Eric S.; Pandolfino, John E. (August 2018). "Complications of Antireflux Surgery". The American Journal of Gastroenterology. 113 (8): 1137–1147. doi:10.1038/s41395-018-0115-7. ISSN 1572-0241. PMC 6394217. PMID 29899438.
- Richter, Joel E. (May 2013). "Gastroesophageal Reflux Disease Treatment: Side Effects and Complications of Fundoplication". Clinical Gastroenterology and Hepatology. 11 (5): 465–471. doi:10.1016/j.cgh.2012.12.006. PMID 23267868.
- Spechler, Stuart Jon (March 2004). "The Management of Patients Who Have "Failed" Antireflux Surgery". American Journal of Gastroenterology. 99 (3): 552–561. doi:10.1111/j.1572-0241.2004.04081.x. ISSN 0002-9270. PMID 15056101. S2CID 6795623.