| Obesity-associated morbidity | |
|---|---|
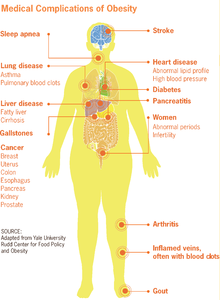 | |
| Obesity may cause a number of medical complications which negatively impact peoples' quality of life. | |
| Specialty | Endocrinology(other specialties) |
| Part of a series on |
| Human body weight |
|---|
| General concepts |
| Medical concepts |
| Measurements |
| Related conditions |
| Obesity-associated morbidity |
| Management of obesity |
| Social aspects |

Obesity is a risk factor for many chronic physical and mental illnesses.
The health effects of being overweight but not obese are controversial, with some studies showing that the mortality rate for individuals who are classified as overweight (BMI 25.0 to 29.9) may actually be lower than for those with an ideal weight (BMI 18.5 to 24.9). Health risks for those who are overweight may be decreasing because of improvements in medical care. Some obesity-associated medical conditions may be the result of stress caused by medical discrimination against people who are obese, rather than the direct effects of obesity, and some may be exacerbated by the relatively poor healthcare received by people who are obese.
Medical discrimination
Main article: Social stigma of obesity § In healthcareBecause of the social stigma of obesity, people who are obese may receive poorer healthcare than people within the normal BMI weight range, potentially contributing to the relationship between obesity and poor health outcomes. People who experience weight-related discrimination, irrespective of their actual weight status, similarly have poorer health outcomes than those who do not experience weight-related discrimination. People who are obese are also less likely to seek medical care than people who are not obese, even if the weight gain is caused by medical problems. Peter Muennig, a professor in the Department of Health Policy and Management at Columbia University, has proposed that obesity-associated medical conditions may be caused "not from adiposity alone, but also from the psychological stress induced by the social stigma associated with being obese".
Cardiological risks
See also: Cardiology
Body weight is not considered to be an independently predictive risk factor for cardiovascular disease by current (as of 2014) risk assessment tools. Mortality from cardiovascular disease has decreased despite increases in obesity, and at least one clinical trial was stopped early because the weight loss intervention being tested did not reduce cardiovascular disease.
Ischemic heart disease
Abdominal obesity is associated with cardiovascular diseases including angina and myocardial infarction. However, overall obesity (as measured by BMI) may lead to false diagnoses of myocardial infarction and may decrease mortality after acute myocardial infarction.
In 2008, European guidelines concluded that 35% of ischemic heart disease among adults in Europe is due to obesity.
Congestive heart failure
Having obesity is associated to about 11% of heart failure cases in males and 14% in females.
High blood pressure
More than 85% of those with hypertension have a BMI greater than 25, although diet is probably a more important factor than body weight. Risk estimates indicate that at least two-thirds of people with hypertension can be directly attributed to obesity. The association between obesity and hypertension has been found in animal and clinical studies, which have suggested that there are multiple potential mechanisms for obesity-induced hypertension. These mechanisms include the activation of the sympathetic nervous system as well as the activation of the renin–angiotensin–aldosterone system. As of 2007, it was unclear whether there is an association between hypertension and obesity in children, but there is little direct evidence that blood pressure has increased despite increases in pediatric overweight.
Abnormal cholesterol levels
Obesity is associated with increased levels of LDL cholesterol and lower levels of HDL cholesterol in the blood.
Deep vein thrombosis and pulmonary embolism
Obesity increases one's risk of venous thromboembolism by approximately 2.3 fold.
Dermatological risks
See also: DermatologyObesity is associated with the incidence of stretch marks, acanthosis nigricans, lymphedema, cellulitis, hirsutism, and intertrigo.
Endocrine risks
Further information: Endocrinology
Diabetes mellitus
Main article: DiabesityThe link between obesity and type 2 diabetes is so strong that researchers in the 1970s started calling it "diabesity". Excess weight is behind 64% of cases of diabetes in males and 77% of cases in females.
Gynecomastia
In some individuals, obesity can be associated with elevated peripheral conversion of androgens into estrogens.
Gastrointestinal risks
See also: Human digestive systemGastroesophageal reflux disease
Several studies have shown that the frequency and severity of GERD symptoms increase with BMI, such that people who are underweight have the fewest GERD symptoms, and people who are severely obese have the most GERD symptoms. However, most studies find that GERD symptoms are not improved by nonsurgical weight loss.
Cholelithiasis (gallstones)
Obesity causes the amount of cholesterol in bile to rise, in turn the formation of stone can occur
Reproductive system (or genital system)
See also: Human reproductive systemPolycystic ovarian syndrome (PCOS)
Due to its association with insulin resistance, the risk of obesity increases with polycystic ovarian syndrome (PCOS). In the US approximately 60% of patients with PCOS have a BMI greater than 30. It remains uncertain whether PCOS contributes to obesity, or the reverse.
Infertility
Obesity can lead to infertility in both males and females. This is primarily due to excess estrogen interfering with normal ovulation in females and altering spermatogenesis in males. It is believed to cause 6% of primary infertility. A review in 2013 came to the result that obesity increases the risk of oligospermia and azoospermia in males, with an of odds ratio 1.3. Being morbidly obese increases the odds ratio to 2.0.
Complications of pregnancy
Obesity is related to many complications in pregnancy including: haemorrhage, infection, increased hospital stays for the mother, and increased NICU requirements for the infant. Obese females also have increased risk of preterm births and low birth weight infants.
Obese females have more than twice the rate of C-sections compared to females of "normal" weight. Some have suggested that this may be due in part to the social stigma of obesity.
Birth defects
Those who are obese during pregnancy have a greater risk of having a child with a number of congenital malformations including: neural tube defects such as anencephaly and spina bifida, cardiovascular anomalies, including septal anomalies, cleft lip and palate, anorectal malformation, limb reduction anomalies, and hydrocephaly.
Intrauterine fetal death
Maternal obesity is associated with an increased risk of intrauterine fetal death.
Buried penis
See also: Buried penisExcess body fat in morbid obesity can, in some cases, completely obscure or "bury" the penis.
Neurological risks
See also: Neurology
Stroke
Ischemic stroke is increased in both men and women who are obese.
Meralgia paresthetica
Meralgia paresthetica is a neuropathic pain or numbness of the thighs, sometimes associated with obesity.
Migraines
Migraine (and headaches in general) is comorbid with obesity. The risk of migraine rises 50% by BMI of 30 kg/m and 100% by BMI of 35 kg/m. The causal connection remains unclear.
Carpal tunnel syndrome
The risk of carpal tunnel syndrome is estimated to rise 7.4% for each 1 kg/m increase of body mass index.
Dementia
One review found that those who are obese do not have a significantly higher rate of dementia than those with "normal" weight.
Idiopathic intracranial hypertension
Idiopathic intracranial hypertension, or unexplained high pressure in the cranium, is a rare condition that can cause visual impairment, frequent severe headache, and tinnitus. It is most commonly seen in obese women, and the incidence of idiopathic intracranial hypertension is increasing along with increases in the number of people who are obese.
Multiple sclerosis
Obese female individuals at 18 years of age have a greater than twofold increased risk of multiple sclerosis compared to females with a BMI between 18.5 and 20.9. Female individuals who are underweight at age 18 have the lowest risk of multiple sclerosis. However, body weight as an adult was not associated with risk of multiple sclerosis.
Cancer
Main article: Obesity and cancer
Many cancers occur at increased frequency in those who are overweight or obese. A study from the United Kingdom found that approximately 5% of cancer is due to excess weight. These cancers include:
- breast cancer
- ovarian cancer
- esophageal cancer
- colorectal cancer
- hepatocellular carcinoma
- pancreatic cancer
- gallbladder cancer
- stomach cancer
- endometrial cancer
- cervical cancer
- prostate cancer
- renal cell carcinoma
- non-Hodgkin's lymphoma
- multiple myeloma
A high body mass index (BMI) is associated with a higher risk of developing ten common cancers including 41% of uterine cancers and at least 10% of gallbladder, kidney, liver and colon cancers in the UK. For those undergoing surgery for cancer, obesity is also associated with an increased risk of major postoperative complications compared with those of "normal" weight.
Psychiatric risks
See also: Psychiatry
Depression
Obesity has been associated with depression, likely due to social factors rather than physical effects of obesity. However, it is possible that obesity is caused by depression (due to reduced physical activity or, in some people, increases in appetite). Obesity-related disabilities may also lead to depression in some people. Repeated failed attempts at weight loss might also lead to depression.
The association between obesity and depression is strongest in those who are more severely obese, those who are younger, and in women. Suicide rate however decreases with increased BMI. Similarly, weight loss through bariatric surgery is associated with increased risk of suicide.
Social stigmatization
Main article: Social stigma of obesityObese people draw negative reactions from others, and people are less willing to help obese individuals in any situation due to social stigmatization. People who are obese also experience fewer educational and career opportunities, on average earn a lesser income, and generally receive poorer health care and treatment than individuals of "normal" weight.
Respiratory system
See also: Respiratory systemObstructive sleep apnea
Obesity is a risk factor for obstructive sleep apnea.
Obesity hypoventilation syndrome

Obesity hypoventilation syndrome is defined as the combination of obesity, hypoxia during sleep, and hypercapnia during the day, resulting from hypoventilation.
Chronic lung disease
Obesity is associated with a number of chronic lung diseases, including asthma and COPD. It is believed that a systemic pro-inflammatory state induced by some causes of obesity may contribute to airway inflammation, leading to asthma.
Complications during general anaesthesia
Obesity significantly reduces and stiffens the functional lung volume, requiring specific strategies for respiratory management under general anesthesia.
Obesity and asthma
The low grade systemic inflammation of obesity has been shown to worsen lung function in asthma and increase the risk of developing an asthma exacerbation.
COVID-19
A study in England found a linear increase in severe COVID-19 resulting in hospitalisation and death for those whose BMI is above 23, and a linear increase in admission to an intensive care unit across the whole BMI spectrum. The difference in COVID-19 risk from having a high BMI was most pronounced in people aged under 40, or who were black. A study from Mexico found that obesity alone was responsible for a 2.7 times increased risk of death from COVID-19, while comorbidities with diabetes, immunosuppression or high blood pressure increased the risk further. A study from the United States found that there was an inverse correlation between age and BMI of COVID patients; the younger the age group, the higher its BMI.
Rheumatological and orthopedic risks
See also: Rheumatology
Gout
Compared to men with a BMI of 21–22.9, men with a BMI of 30–34.9 have 2.33 times more gout, and men with a BMI ≥ 35 have 2.97 times more gout. Weight loss decreases these risks.
Poor mobility
There is a strong association between obesity and musculoskeletal pain and disability.
Osteoarthritis
Increased rates of arthritis are seen in both weight-bearing and non-weight-bearing joints. Weight loss and exercise act to reduce the risk of osteoarthritis.
Low back pain
Obese individuals are twice to four times more likely to have lower back pain than their "normal" weight peers.
Traumatic injury
In females, low BMI is a risk factor for osteoporotic fractures in general. In contrast, obesity is a protective factor for most osteoporotic fractures.
Urological and nephrological risks
See also: Urology and Nephrology
Urinary incontinence
Urge, stress, and mixed incontinence all occur at higher rates in obese people. The rates of urinary incontinence are about double that found in the "normal" weight population. Urinary incontinence improves with weight loss.
Chronic kidney disease
Obesity increases one's risk of chronic kidney disease by three to four times.
Hypogonadism
In males, obesity and metabolic syndrome both increase estrogen and adipokine production. This reduces gonadotropin-releasing hormone, in turn reducing both luteinizing hormone and follicle stimulating hormone. The result is reduction of the testis' production of testosterone and a further increase in adipokine levels. This then feeds back to cause further weight gain.
Erectile dysfunction
Obese male individuals can experience erectile dysfunction, and weight loss can improve their sexual functioning.
See also
References
- Flegal, K. M.; Graubard, B. I.; Williamson, D. F.; Gail, M. H. (2005). "Excess Deaths Associated With Underweight, Overweight, and Obesity". JAMA. 293 (15): 1861–1867. doi:10.1001/jama.293.15.1861. PMID 15840860.
- ^ Malnick, S.D.H.; Knobler, H (12 August 2006). "The medical complications of obesity". QJM. 99 (9): 565–579. doi:10.1093/qjmed/hcl085. PMID 16916862.
- ^ Muennig, P (2008). "The body politic: the relationship between stigma and obesity-associated disease". BMC Public Health. 8: 128. doi:10.1186/1471-2458-8-128. PMC 2386473. PMID 18426601.
- Phelan, S. M.; Burgess, D. J.; Yeazel, M. W.; Hellerstedt, W. L.; Griffin, J. M.; van Ryn, M. (April 2015). "Impact of weight bias and stigma on quality of care and outcomes for patients with obesity". Obesity Reviews. 16 (4): 319–326. doi:10.1111/obr.12266. PMC 4381543. PMID 25752756.
- ^ Puhl, Rebecca M.; Heuer, Chelsea A. (May 2009). "The Stigma of Obesity: A Review and Update". Obesity. 17 (5): 941–964. doi:10.1038/oby.2008.636. PMID 19165161.
- Schafer, Markus H.; Ferraro, Kenneth F. (March 2011). "The Stigma of Obesity: Does Perceived Weight Discrimination Affect Identity and Physical Health?". Social Psychology Quarterly. 74 (1): 76–97. doi:10.1177/0190272511398197.
- Puhl, Rebecca M.; King, Kelly M. (2013). "Weight discrimination and bullying". Best Practice & Research Clinical Endocrinology & Metabolism. 27 (2): 117–127. doi:10.1016/j.beem.2012.12.002. PMID 23731874.
- Muennig, Peter (7 August 2018). "Policy - Peter Muennig". www.publichealth.columbia.edu. Columbia University. Archived from the original on 21 May 2022. Retrieved 22 May 2022.
- Morris (2014). "Review of Clinical Practice Guidelines for the Management of LDL-Related Risk". Journal of the American College of Cardiology. 64 (2): 196–206. doi:10.1016/j.jacc.2014.05.015. PMID 25011724.
- Flegal; Carroll; Kit; Ogden (2012). "Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010". JAMA. 307 (5): 491–497. doi:10.1001/jama.2012.39. PMID 22253363. S2CID 7396422.
- The Look AHEAD Research Group (2013). "Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes". New England Journal of Medicine. 369 (2): 145–154. doi:10.1056/NEJMoa1212914. PMC 3791615. PMID 23796131.
- Poirier P, Giles TD, Bray GA, et al. (May 2006). "Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss". Arteriosclerosis, Thrombosis, and Vascular Biology. 26 (5): 968–976. CiteSeerX 10.1.1.508.7066. doi:10.1161/01.ATV.0000216787.85457.f3. PMID 16627822. S2CID 6052584.
- ^ Yusuf S, Hawken S, Ounpuu S, et al. (2004). "Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study". The Lancet. 364 (9438): 937–952. doi:10.1016/S0140-6736(04)17018-9. hdl:10983/21615. PMID 15364185. S2CID 30811593.
- Tsigos C, Hainer V, Basdevant A, et al. (2008). "Management of obesity in adults: European clinical practice guidelines". Obesity Facts. 1 (2): 106–116. doi:10.1159/000126822. PMC 6452117. PMID 20054170. as PDF Archived 2015-10-17 at the Wayback Machine
- ^ Haslam DW, James WP (October 2005). "Obesity". The Lancet. 366 (9492): 1197–209. doi:10.1016/S0140-6736(05)67483-1. PMID 16198769. S2CID 208791491.
- Narkiewicz, Krzysztof (February 2006). "Obesity and hypertension—the issue is more complex than we thought". Nephrology Dialysis Transplantation. 21 (2): 264–267. doi:10.1093/ndt/gfi290. PMID 16311261.
- Hall, John E. (2003). "The kidney, hypertension, and obesity". Hypertension. 41 (3 Pt 2): 625–633. doi:10.1161/01.HYP.0000052314.95497.78. PMID 12623970.
- Rahmouni K, Correia ML, Haynes WG, Mark AL (January 2005). "Obesity-associated hypertension: new insights into mechanisms". Hypertension. 45 (1): 9–14. doi:10.1161/01.HYP.0000151325.83008.b4. PMID 15583075.
- Chiolero A, Bovet P, Paradis G, Paccaud F (March 2007). "Has blood pressure increased in children in response to the obesity epidemic?". Pediatrics. 119 (3): 544–553. doi:10.1542/peds.2006-2136. PMID 17332208. S2CID 46223377.
- Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW (January 2008). "Cardiovascular risk factors and venous thromboembolism: a meta-analysis". Circulation. 117 (1): 93–102. doi:10.1161/CIRCULATIONAHA.107.709204. PMID 18086925.
- Darvall KA, Sam RC, Silverman SH, Bradbury AW, Adam DJ (February 2007). "Obesity and thrombosis". European Journal of Vascular and Endovascular Surgery. 33 (2): 223–33. doi:10.1016/j.ejvs.2006.10.006. PMID 17185009.
- Yosipovitch G, DeVore A, Dawn A (June 2007). "Obesity and the skin: skin physiology and skin manifestations of obesity". Journal of the American Academy of Dermatology. 56 (6): 901–16, quiz 917–20. doi:10.1016/j.jaad.2006.12.004. PMID 17504714.
- Hahler B (June 2006). "An overview of dermatological conditions commonly associated with the obese patient". Ostomy Wound Management. 52 (6): 34–6, 38, 40 passim. PMID 16799182.
- Kopelman, Peter G.; Caterson, Ian D.; Stock, Michael J.; Dietz, William H. (2005). Clinical Obesity in Adults and Children. Blackwell. p. 493. ISBN 978-1-4051-1672-5. Archived from the original on 2023-01-12. Retrieved 2017-09-07.
- Johnson, Ruth E.; Murad, M. Hassan (November 2009). "Gynecomastia: Pathophysiology, Evaluation, and Management". Mayo Clinic Proceedings. 84 (11): 1010–1015. doi:10.1016/S0025-6196(11)60671-X. PMC 2770912. PMID 19880691.
- ^ Anand G, Katz PO (2008). "Gastroesophageal reflux disease and obesity". Reviews in Gastroenterological Disorders. 8 (4): 233–239. PMID 19107097. Archived from the original on 2016-09-18. Retrieved 2009-01-14.
- Ayazi S, Hagen JA, Chan LS, et al. (August 2009). "Obesity and gastroesophageal reflux: quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms". Journal of Gastrointestinal Surgery. 13 (8): 1440–1447. doi:10.1007/s11605-009-0930-7. PMC 2710497. PMID 19475461.
- Kjellin; Ramel; Rössner; Thor (1996). "Gastroesophageal reflux in obese patients is not reduced by weight reduction". Scandinavian Journal of Gastroenterology. 31 (11): 1047–1051. doi:10.3109/00365529609036885. PMID 8938895.
- "Gallstones". United States: National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 16 October 2016. Retrieved 13 May 2016.
- Samer El Hayek; Lynn Bitar; Layal H. Hamdar; Fadi G. Mirza; Georges Daoud (5 April 2016). "Poly Cystic Ovarian Syndrome: An Updated Overview". Frontiers in Physiology. 7: 124. doi:10.3389/fphys.2016.00124. PMC 4820451. PMID 27092084.
- Kamangar; Okhovat; Schmidt; Beshay; Pasch; Cedars; Huddleston; Shinkai (2015). "Polycystic Ovary Syndrome: Special Diagnostic and Therapeutic Considerations for Children". Pediatric Dermatology. 32 (5): 571–578. doi:10.1111/pde.12566. PMID 25787290. S2CID 2132971.
- Hammoud AO, Gibson M, Peterson CM, Meikle AW, Carrell DT (October 2008). "Impact of male obesity on infertility: a critical review of the current literature". Fertility and Sterility. 90 (4): 897–904. doi:10.1016/j.fertnstert.2008.08.026. PMID 18929048.
- ^ Arendas K, Qiu Q, Gruslin A (June 2008). "Obesity in pregnancy: pre-conceptional to postpartum consequences". Journal of Obstetrics and Gynaecology Canada. 30 (6): 477–488. doi:10.1016/s1701-2163(16)32863-8. PMID 18611299.
- ^ Sermondade, N.; Faure, C.; Fezeu, L.; et al. (2012). "BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis". Human Reproduction Update. 19 (3): 221–231. doi:10.1093/humupd/dms050. PMC 3621293. PMID 23242914. Archived from the original on 2015-12-23.
- Heslehurst N, Simpson H, Ells LJ, et al. (November 2008). "The impact of maternal BMI status on pregnancy outcomes with immediate short-term obstetric resource implications: a meta-analysis". Obesity Reviews. 9 (6): 635–683. doi:10.1111/j.1467-789X.2008.00511.x. PMID 18673307. S2CID 32714616. Archived from the original on 2019-04-01. Retrieved 2018-11-07.
- McDonald SD, Han Z, Mulla S, Beyene J (2010). "Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta-analyses". BMJ. 341: c3428. doi:10.1136/bmj.c3428. PMC 2907482. PMID 20647282.
- Poobalan AS, Aucott LS, Gurung T, Smith WC, Bhattacharya S (January 2009). "Obesity as an independent risk factor for elective and emergency caesarean delivery in nulliparous women—systematic review and meta-analysis of cohort studies". Obesity Reviews. 10 (1): 28–35. doi:10.1111/j.1467-789X.2008.00537.x. PMID 19021871. S2CID 11750524.
- DeJoy; Bittner (2015). "Obesity stigma as a determinant of poor birth outcomes in women with high BMI: a conceptual framework". Maternal and Child Health Journal. 19 (4): 693–699. doi:10.1007/s10995-014-1577-x. PMID 25047786. S2CID 24804448.
- Stothard KJ, Tennant PW, Bell R, Rankin J (February 2009). "Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis". JAMA. 301 (6): 636–650. doi:10.1001/jama.2009.113. PMID 19211471.
- Pestana IA, Greenfield JM, Walsh M, Donatucci CF, Erdmann D (2009). "Management of 'Buried' Penis in Adulthood: An Overview". Plastic and Reconstructive Surgery. 124 (4): 1186–1195. doi:10.1097/PRS.0b013e3181b5a37f. PMID 19935302. S2CID 36775257.
- Patijn J, Mekhail N, Hayek S, Lataster A, van Kleef M, Van Zundert J (May–June 2011). "Meralgia Paresthetica". Pain Practice. 11 (3): 302–308. doi:10.1111/j.1533-2500.2011.00458.x. PMID 21435164. S2CID 31291517.
- ^ Chai NC, Scher AI, Moghekar A, Bond DS, Peterlin BL (February 2014). "Obesity and headache: part I—a systematic review of the epidemiology of obesity and headache". Headache. 54 (2): 219–234. doi:10.1111/head.12296. PMC 3971380. PMID 24512574.
- Peterlin BL, Sacco S, Bernecker C, Scher AI (April 2016). "Adipokines and Migraine: A Systematic Review". Headache. 56 (4): 622–644. doi:10.1111/head.12788. PMC 4836978. PMID 27012149.
- Shiri R, Pourmemari MH, Falah-Hassani K, Viikari-Juntura E (December 2015). "The effect of excess body mass on the risk of carpal tunnel syndrome: a meta-analysis of 58 studies". Obesity Reviews. 16 (12): 1094–1104. doi:10.1111/obr.12324. PMID 26395787. S2CID 11156913.
- Beydoun MA, Beydoun HA, Wang Y (May 2008). "Obesity and central obesity as risk factors for incident dementia and its subtypes: A systematic review and meta-analysis". Obesity Reviews. 9 (3): 204–218. doi:10.1111/j.1467-789X.2008.00473.x. PMC 4887143. PMID 18331422.
- Wall M (March 2008). "Idiopathic intracranial hypertension (pseudotumor cerebri)". Current Neurology and Neuroscience Reports. 8 (2): 87–93. doi:10.1007/s11910-008-0015-0. PMID 18460275. S2CID 17285706.
- Julayanont P, Karukote A, Ruthirago D, Panikkath D, Panikkath R (19 February 2016). "Idiopathic intracranial hypertension: ongoing clinical challenges and future prospects". Journal of Pain Research. 9: 87–99. doi:10.2147/JPR.S60633. PMC 4767055. PMID 26929666.
- ^ Munger KL, Chitnis T, Ascherio A (2009). "Body size and risk of MS in two cohorts of US women". Neurology. 73 (19): 1543–1550. doi:10.1212/WNL.0b013e3181c0d6e0. PMC 2777074. PMID 19901245.
- Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D (2016). "Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study". BMJ. 335 (7630): 1134. doi:10.1136/bmj.39367.495995.AE. PMC 2099519. PMID 17986716.
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (April 2003). "Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults". New England Journal of Medicine. 348 (17): 1625–1638. doi:10.1056/NEJMoa021423. PMID 12711737. S2CID 22714795.
- Lyford, Joanna (August 2014). "Rising obesity levels in UK could result in 4,000 extra cancer cases each year". The Pharmaceutical Journal. Archived from the original on 2017-09-05. Retrieved 2014-08-17.
- STARSurg Collaborative (2016). "Multicentre prospective cohort study of body mass index and postoperative complications following gastrointestinal surgery". British Journal of Surgery. 103 (9): 1157–1172. doi:10.1002/bjs.10203. PMC 4973675. PMID 27321766.
- ^ Mukamal KJ, Rimm EB, Kawachi I, O'Reilly EJ, Calle EE, Miller M (November 2009). "Body Mass Index and Risk of Suicide Among One Million US Adults". Epidemiology. 21 (1): 82–86. doi:10.1097/EDE.0b013e3181c1fa2d. PMID 19907331. S2CID 10646644.
- ^ Dixon JB, Dixon ME, O'Brien PE (September 2003). "Depression in association with severe obesity: changes with weight loss". Archives of Internal Medicine. 163 (17): 2058–2065. doi:10.1001/archinte.163.17.2058. PMID 14504119.
- Tindle; Omalu; Courcoulas; Marcus; Hammers; Kuller (2010). "Risk of suicide after long-term follow-up from bariatric surgery". The American Journal of Medicine. 123 (11): 1036–1042. doi:10.1016/j.amjmed.2010.06.016. PMC 4296730. PMID 20843498.
- Sikorski, Claudia; Luppa, Melanie; Kaiser, Marie; Glaesmer, Heide; Schomerus, Georg; König, Hans-Helmut; Riedel-Heller, Steffi G (December 2011). "The stigma of obesity in the general public and its implications for public health - a systematic review". BMC Public Health. 11 (1): 661. doi:10.1186/1471-2458-11-661. PMC 3175190. PMID 21859493.
- "Dicke sind faul und dumm" [Fat people are lazy and stupid]. Süddeutsche Zeitung (in German). August 11, 2008. Archived from the original on June 13, 2018. Retrieved March 8, 2011.
- ^ Poulain M, Doucet M, Major GC, et al. (April 2006). "The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies". CMAJ. 174 (9): 1293–1299. doi:10.1503/cmaj.051299. PMC 1435949. PMID 16636330.
- Olson, Amy L.; Zwillich, Clifford (September 2005). "The obesity hypoventilation syndrome". The American Journal of Medicine. 118 (9): 948–956. doi:10.1016/j.amjmed.2005.03.042. PMID 16164877.
- Sutherland ER (August 2008). "Obesity and asthma". Immunology and Allergy Clinics of North America. 28 (3): 589–602, ix. doi:10.1016/j.iac.2008.03.003. PMC 2504765. PMID 18572109.
- Hodgson, Luke E.; Murphy, Patrick B.; Hart, Nicholas (May 2015). "Respiratory management of the obese patient undergoing surgery". Journal of Thoracic Disease. 7 (5): 943–952. doi:10.3978/j.issn.2072-1439.2015.03.08. PMC 4454851. PMID 26101653.
- Peters, Michael C.; McGrath, Kelly Wong; Hawkins, Gregory A.; Hastie, Annette T.; Levy, Bruce D.; Israel, Elliot; et al. (July 2016). "Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts". The Lancet Respiratory Medicine. 4 (7): 574–584. doi:10.1016/S2213-2600(16)30048-0. PMC 5007068. PMID 27283230.
- Gao, Min; Piernas, Carmen; Astbury, Nerys M.; Hippisley-Cox, Julia; O'Rahilly, Stephen; Aveyard, Paul; Jebb, Susan A. (1 June 2021). "Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study". The Lancet Diabetes & Endocrinology. 9 (6): 350–359. doi:10.1016/S2213-8587(21)00089-9. PMC 8081400. PMID 33932335.
- Vera-Zertuche, J. M.; Mancilla-Galindo, J.; Tlalpa-Prisco, M.; Aguilar-Alonso, P.; Aguirre-García, M. M.; Segura-Badilla, O.; Lazcano-Hernández, M.; Rocha-González, H. I.; Navarro-Cruz, A. R.; Kammar-García, A.; Vidal-Mayo, J. de J. (2021). "Obesity is a strong risk factor for short-term mortality and adverse outcomes in Mexican patients with COVID-19: a national observational study". Epidemiology & Infection. 149: e109. doi:10.1017/S0950268821001023. PMC 8134888. PMID 33913410. S2CID 233446019.
- Kass, David A.; Duggal, Priya; Cingolani, Oscar (16 May 2020). "Obesity could shift severe COVID-19 disease to younger ages". The Lancet. 395 (10236): 1544–1545. doi:10.1016/S0140-6736(20)31024-2. PMC 7196905. PMID 32380044.
- Choi HK, Atkinson K, Karlson EW, Curhan G (April 2005). "Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study". Archives of Internal Medicine. 165 (7): 742–748. doi:10.1001/archinte.165.7.742. PMID 15824292. S2CID 12201127.
- Tukker, A.; Visscher, T. L. S.; Picavet, H. S. J. (March 2009). "Overweight and health problems of the lower extremities: osteoarthritis, pain and disability". Public Health Nutrition. 12 (3): 359–368. doi:10.1017/S1368980008002103. PMID 18426630.
- Yu SP, Hunter DJ (August 2015). "Managing osteoarthritis". Australian Prescriber. 38 (4): 115–119. doi:10.18773/austprescr.2015.039. PMC 4653978. PMID 26648637.
- Molenaar EA, Numans ME, van Ameijden EJ, Grobbee DE (November 2008). "Aanzienlijke comorbiditeit bij volwassenen met overgewicht: resultaten uit het 'Leidsche Rijn Gezondheidsproject'" [Considerable comorbidity in overweight adults: results from the Utrecht Health Project]. Nederlands Tijdschrift voor Geneeskunde (in Dutch). 152 (45): 2457–63. PMID 19051798.
- ^ Johansson, Helena; Kanis, John A.; Odén, Anders; McCloskey, Eugene; Chapurlat, Roland D.; Christiansen, Claus; et al. (January 2014). "A Meta-Analysis of the Association of Fracture Risk and Body Mass Index in Women". Journal of Bone and Mineral Research. 29 (1): 223–233. doi:10.1002/jbmr.2017. PMID 23775829. S2CID 44761194.
- Hunskaar S (2008). "A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women". Neurourology and Urodynamics. 27 (8): 749–757. doi:10.1002/nau.20635. PMID 18951445. S2CID 20378183.
- Bart S, Ciangura C, Thibault F, et al. (September 2008). "Incontinence urinaire d'effort et obésité" [Stress urinary incontinence and obesity]. Progrès en Urologie (in French). 18 (8): 493–498. doi:10.1016/j.purol.2008.04.015. PMID 18760738.
- Subak LL, Wing R, West DS, et al. (January 2009). "Weight loss to treat urinary incontinence in overweight and obese women". New England Journal of Medicine. 360 (5): 481–490. doi:10.1056/NEJMoa0806375. PMC 2877497. PMID 19179316.
- Ejerblad E, Fored CM, Lindblad P, Fryzek J, McLaughlin JK, Nyrén O (2006). "Obesity and risk for chronic renal failure". Journal of the American Society of Nephrology. 17 (6): 1695–1702. doi:10.1681/ASN.2005060638. PMID 16641153.
- Corona G, Bianchini S, Sforza A, Vignozzi L, Maggi M (October 2015). "Hypogonadism as a possible link between metabolic diseases and erectile dysfunction in aging men". Hormones – International Journal of Endocrinology and Metabolism. 14 (4): 569–578. doi:10.14310/horm.2002.1635. hdl:2158/1090319. PMID 26732155.
- Corona, Giovanni; Rastrelli, Giulia; Filippi, Sandra; Vignozzi, Linda; Mannucci, Edoardo; Maggi, Mario (2014). "Erectile dysfunction and central obesity: an Italian perspective". Asian Journal of Andrology. 16 (4): 581–591. doi:10.4103/1008-682X.126386. PMC 4104087. PMID 24713832.
- Chitaley, Kanchan; Kupelian, Varant; Subak, Leslee; Wessells, Hunter (December 2009). "Diabetes, Obesity and Erectile Dysfunction: Field Overview and Research Priorities". Journal of Urology. 182 (6S): S45-50. doi:10.1016/j.juro.2009.07.089. PMC 2864637. PMID 19846136.
Further reading
- King, Lauren K.; March, Lyn; Anandacoomarasamy, Ananthila (2013-08-01). "Obesity & osteoarthritis". The Indian Journal of Medical Research. 138 (2): 185–193. PMC 3788203. PMID 24056594.Review
- Zhao, Lan-Juan; Jiang, Hui; Papasian, Christopher J; Maulik, Dev; Drees, Betty; Hamilton, James; Deng, Hong-Wen (2008-01-01). "Correlation of Obesity and Osteoporosis: Effect of Fat Mass on the Determination of Osteoporosis". Journal of Bone and Mineral Research. 23 (1): 17–29. doi:10.1359/jbmr.070813. PMC 2663586. PMID 17784844.
- Guh, Daphne P; Zhang, Wei; Bansback, Nick; Amarsi, Zubin; Birmingham, C Laird; Anis, Aslam H (25 March 2009). "The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis". BMC Public Health. 9 (1): 88. doi:10.1186/1471-2458-9-88. PMC 2667420. PMID 19320986.
| Malnutrition | |||||
|---|---|---|---|---|---|
| Protein-energy malnutrition | |||||
| Vitamin deficiency |
| ||||
| Mineral deficiency | |||||
| Growth | |||||
| General | |||||