P-glycoprotein 1 (permeability glycoprotein, abbreviated as P-gp or Pgp) also known as multidrug resistance protein 1 (MDR1) or ATP-binding cassette sub-family B member 1 (ABCB1) or cluster of differentiation 243 (CD243) is an important protein of the cell membrane that pumps many foreign substances out of cells. More formally, it is an ATP-dependent efflux pump with broad substrate specificity. It exists in animals, fungi, and bacteria, and it likely evolved as a defense mechanism against harmful substances.
P-gp is extensively distributed and expressed in the intestinal epithelium where it pumps xenobiotics (such as toxins or drugs) back into the intestinal lumen, in liver cells where it pumps them into bile ducts, in the cells of the proximal tubule of the kidney where it pumps them into urinary filtrate (in the proximal tubule), and in the capillary endothelial cells composing the blood–brain barrier and blood–testis barrier, where it pumps them back into the capillaries.
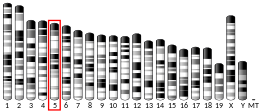
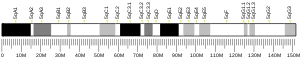
P-gp is a glycoprotein that in humans is encoded by the ABCB1 gene. P-gp is a well-characterized ABC-transporter (which transports a wide variety of substrates across extra- and intracellular membranes) of the MDR/TAP subfamily. The normal excretion of xenobiotics back into the gut lumen by P-gp pharmacokinetically reduces the efficacy of some pharmaceutical drugs (which are said to be P-gp substrates). In addition, some cancer cells also express large amounts of P-gp, further amplifying that effect and rendering these cancers multidrug resistant. Many drugs inhibit P-gp, typically incidentally rather than as their main mechanism of action; some foods do as well. Any such substance can sometimes be called a P-gp inhibitor.
P-gp was discovered in 1971 by Victor Ling.
Gene
A 2015 review of polymorphisms in ABCB1 found that "the effect of ABCB1 variation on P-glycoprotein expression (messenger RNA and protein expression) and/or activity in various tissues (e.g. the liver, gut and heart) appears to be small. Although polymorphisms and haplotypes of ABCB1 have been associated with alterations in drug disposition and drug response, including adverse events with various ABCB1 substrates in different ethnic populations, the results have been majorly conflicting, with limited clinical relevance."
Protein
P-gp is a 170 kDa transmembrane glycoprotein, which includes 10–15 kDa of N-terminal glycosylation. The N-terminal half of the protein contains six transmembrane helixes, followed by a large cytoplasmic domain with an ATP-binding site, and then a second section with six transmembrane helixes and an ATP-binding domain that shows over 65% of amino acid similarity with the first half of the polypeptide. In 2009, the first structure of a mammalian P-glycoprotein was solved (3G5U). The structure was derived from the mouse MDR3 gene product heterologously expressed in Pichia pastoris yeast. The structure of mouse P-gp is similar to structures of the bacterial ABC transporter MsbA (3B5W and 3B5X) that adopt an inward facing conformation that is believed to be important for binding substrate along the inner leaflet of the membrane. Additional structures (3G60 and 3G61) of P-gp were also solved revealing the binding site(s) of two different cyclic peptide substrate/inhibitors. The promiscuous binding pocket of P-gp is lined with aromatic amino acid side chains.
Through Molecular Dynamic (MD) simulations, this sequence was proved to have a direct impact in the transporter's structural stability (in the nucleotide-binding domains) and defining a lower boundary for the internal drug-binding pocket.
Species, tissue, and subcellular distribution
P-gp is expressed primarily in certain cell types in the liver, pancreas, kidney, colon, and jejunum. P-gp is also found in brain capillary endothelial cells.
Function
Substrate enters P-gp either from an opening within the inner leaflet of the membrane or from an opening at the cytoplasmic side of the protein. ATP binds at the cytoplasmic side of the protein. Following binding of each, ATP hydrolysis shifts the substrate into a position to be excreted from the cell. Release of the phosphate (from the original ATP molecule) occurs concurrently with substrate excretion. ADP is released, and a new molecule of ATP binds to the secondary ATP-binding site. Hydrolysis and release of ADP and a phosphate molecule resets the protein, so that the process can start again.
The protein belongs to the superfamily of ATP-binding cassette (ABC) transporters. ABC proteins transport various molecules across extra- and intra-cellular membranes. ABC genes are divided into seven distinct subfamilies (ABC1, MDR/TAP, MRP, ALD, OABP, GCN20, White). This protein is a member of the MDR/TAP subfamily. Members of the MDR/TAP subfamily are involved in multidrug resistance. P-gp is an ATP-dependent drug efflux pump for xenobiotic compounds with broad substrate specificity. It is responsible for decreased drug accumulation in multidrug-resistant cells and often mediates the development of resistance to anticancer drugs. This protein also functions as a transporter in the blood–brain barrier. Mutations in this gene are associated with colchicine resistance and Inflammatory bowel disease 13. Alternative splicing and the use of alternative promoters results in multiple transcript variants.
P-gp transports various substrates across the cell membrane including:
- Drugs such as colchicine, desloratadine, tacrolimus and quinidine.
- Chemotherapeutic agents such as topoisomerase inhibitors (i.e. etoposide, doxorubicin), microtubule-targeted drugs (i.e. vinblastine), and tyrosine kinase inhibitors (i.e. gefitinib, sunitinib).
- Lipids
- Steroids
- Xenobiotics
- Peptides
- Bilirubin
- Cardiac glycosides like digoxin
- Immunosuppressive agents
- Glucocorticoids like dexamethasone
- HIV-type 1 antiretroviral therapy agents like protease inhibitors and nonnucleoside reverse transcriptase inhibitors
Its ability to transport the above substrates accounts for the many roles of P-gp including:
- Regulating the distribution and bioavailability of drugs
- Increased intestinal expression of P-glycoprotein can reduce the absorption of drugs that are substrates for P-glycoprotein. Thus, there is a reduced bioavailability, and therapeutic plasma concentrations are not attained. On the other hand, supratherapeutic plasma concentrations and drug toxicity may result because of decreased P-glycoprotein expression
- Active cellular transport of antineoplastics resulting in multidrug resistance to these drugs
- The removal of toxic metabolites and xenobiotics from cells into urine, bile, and the intestinal lumen
- The transport of compounds out of the brain across the blood–brain barrier
- Digoxin uptake
- Prevention of ivermectin and loperamide entry into the central nervous system
- The migration of dendritic cells
- Protection of hematopoietic stem cells from toxins.
It is inhibited by many drugs, such as amiodarone, azithromycin, captopril, clarithromycin, cyclosporine, piperine, quercetin, quinidine, quinine, reserpine, ritonavir, tariquidar, and verapamil.
Regulation of expression and function of P-gp in cancer cells
At the transcriptional level, the expression of P-gp has been intensively studied, and numerous transcription factors and pathways are known to play roles. A variety of transcription factors, such as p53, YB-1, and NF-κB are involved in the direct regulation of P-gp by binding to the promoter regions of the P-gp gene. Many cell signaling pathways are also involved in transcriptional regulation of P-gp. For example, the PI3K/Akt pathway and the Wnt/β-catenin pathway were reported to positively regulate the expression of P-gp. Mitogen-activated protein kinase (MAPK) signaling includes three pathways: the classical MAPK/ERK pathway, the p38 MAPK pathway, and the c-Jun N-terminal kinase (JNK) pathway, all of which were reported to have implications in the regulation of the expression of P-gp. Studies suggested that the MAPK/ERK pathway is involved in the positive regulation of P-gp; the p38 MAPK pathway negatively regulates the expression of the P-gp gene; and the JNK pathway was reported to be involved in both positive regulation and negative regulation of P-gp.
After 2008, microRNAs (miRNAs) were identified as new players in regulating the expression of P-gp in both transcriptional and post-transcriptional levels. Some miRNAs decrease the expression of P-gp. For example, miR-200c down-regulates the expression of P-gp through the JNK signaling pathway or ZEB1 and ZEB2; miR-145 down-regulates the mRNA of P-gp by directly binding to the 3'-UTR of the gene of P-gp and thus suppresses the translation of P-gp. Some other miRNAs increase the expression of P-gp. For example, miR-27a up-regulates P-gp expression by suppressing the Raf kinase inhibitor protein (RKIP); alternatively, miR-27a can also directly bind to the promoter of the P-gp gene, which works in a similar way with the mechanism of action of transcriptional factors.
The expression of P-gp is also regulated by post-translational events, such as post-transcriptional modification, degradation, and intracellular trafficking of P-gp. Pim-1 protects P-gp from ubiquitination and the following degradation in the proteasome. Small GTPases Rab5 down-regulates the endocytotic trafficking of P-gp and thus increases the functional P-gp level on the cell membrane; while Small GTPases Rab4 work in an opposite way: Rab4 down-regulates the exocytotic trafficking of P-gp from intracellular compartments to the cell membrane, and therefore decreases the functional P-gp level on the cell membrane.
Clinical significance
Drug interactions
Some common pharmacological inhibitors of P-glycoprotein include: amiodarone, clarithromycin, ciclosporin, colchicine, diltiazem, erythromycin, felodipine, ketoconazole, lansoprazole, omeprazole and other proton-pump inhibitors, nifedipine, paroxetine, reserpine, saquinavir, sertraline, quinidine, tamoxifen, verapamil, and duloxetine. Elacridar and CP 100356 are other common P-gp inhibitors. Zosuquidar and tariquidar were also developed with this in mind. Lastly, valspodar and reversan are other examples of such agents. ABCB1 is linked to the daily dose of warfarin required to maintain the INR to a target of 2.5. Patients with the GT or TT genotypes of the 2677G>T SNP require around 20% more warfarin daily.
Common pharmacological inducers of P-glycoprotein include carbamazepine, dexamethasone, doxorubicin, nefazodone, phenobarbital, phenytoin, prazosin, rifampicin, St. John's wort, tenofovir, tipranavir, trazodone, and vinblastine.
Substrates of P-glycoprotein are susceptible to changes in pharmacokinetics due to drug interactions with P-gp inhibitors or inducers. Some of these substrates include colchicine, ciclosporin, dabigatran, digoxin, diltiazem, fexofenadine, indinavir, morphine, and sirolimus.
Diseases (non-cancer)
Decreased P-gp expression has been found in Alzheimer's disease brains.
Altered P-gp function has also been linked to inflammatory bowel diseases (IBD); however, due to its ambivalent effects in intestinal inflammation many questions remain so far unanswered. While decreased efflux activity may promote disease susceptibility and drug toxicity, increased efflux activity may confer resistance to therapeutic drugs in IBD. Mice deficient in MDR1A develop chronic intestinal inflammation spontaneously, which appears to resemble human ulcerative colitis.
Cancer
P-gp efflux activity is capable of lowering intracellular concentrations of otherwise beneficial compounds, such as chemotherapeutics and other medications, to sub-therapeutic levels. Consequently, P-gp overexpression is one of the main mechanisms behind decreased intracellular drug accumulation and development of multidrug resistance in human multidrug-resistant (MDR) cancers.
History
P-gp was first characterized in 1976. P-gp was shown to be responsible for conferring multidrug resistance upon mutant cultured cancer cells that had developed resistance to cytotoxic drugs.
The structure of mouse P-gp, which has 87% sequence identity to human P-gp, was resolved by x-ray crystallography in 2009. The first structure of human P-gp was solved in 2018, with the protein in its ATP-bound, outward-facing conformation.
Research
Radioactive verapamil can be used for measuring P-gp function with positron emission tomography.
P-gp is also used to differentiate transitional B cells from naive B cells. Dyes such as rhodamine 123 and MitoTracker dyes from Invitrogen can be used to make this differentiation.
MDR1 as a drug target
It has been suggested that MDR1 inhibitors might treat various diseases, especially cancers, but none have done well in clinical trials.
Single nucleotide polymorphism rs1045642
Single Nucleotide Polymorphism rs1045642 (3435T>C or 3435C>T) is important for the differential activity of the P-gp pump.
Homozygous subjects, identified with the TT genotype, are usually more able to extrude xenobiotics from the cell. A Homozygous genotype for the allele ABCB1/MDR1 is capable of a higher absorption from the blood vessels and a lower extrusion into the lumen. Xenobiotics are extruded at a lower rate with heterozygous (CT) alleles compared to homozygous ones.
References
- ^ GRCm38: Ensembl release 89: ENSMUSG00000040584 – Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Ueda K, Clark DP, Chen CJ, Roninson IB, Gottesman MM, Pastan I (January 1987). "The human multidrug resistance (mdr1) gene. cDNA cloning and transcription initiation". The Journal of Biological Chemistry. 262 (2): 505–8. doi:10.1016/S0021-9258(19)75806-2. PMID 3027054.
- ^ Dean, Michael (2002-11-01). "The Human ATP-Binding Cassette (ABC) Transporter Superfamily". National Library of Medicine (US), NCBI. Archived from the original on 2006-02-12. Retrieved 2008-03-02.
- Yu J, Zhou Z, Tay-Sontheimer J, Levy RH, Ragueneau-Majlessi I (September 2017). "Intestinal Drug Interactions Mediated by OATPs: A Systematic Review of Preclinical and Clinical Findings". Journal of Pharmaceutical Sciences. 106 (9): 2312–2325. doi:10.1016/j.xphs.2017.04.004. PMID 28414144.
- Wolking S, Schaeffeler E, Lerche H, Schwab M, Nies AT (July 2015). "Impact of Genetic Polymorphisms of ABCB1 (MDR1, P-Glycoprotein) on Drug Disposition and Potential Clinical Implications: Update of the Literature". Clinical Pharmacokinetics. 54 (7): 709–35. doi:10.1007/s40262-015-0267-1. PMID 25860377. S2CID 35961181.
- Franck Viguié (1998-03-01). "ABCB1". Atlas of Genetics and Cytogenetics in Oncology and Haematology. Retrieved 2008-03-02.
- ^ Aller SG, Yu J, Ward A, Weng Y, Chittaboina S, Zhuo R, et al. (March 2009). "Structure of P-glycoprotein reveals a molecular basis for poly-specific drug binding". Science. 323 (5922): 1718–22. Bibcode:2009Sci...323.1718A. doi:10.1126/science.1168750. PMC 2720052. PMID 19325113.
- Ward A, Reyes CL, Yu J, Roth CB, Chang G (November 2007). "Flexibility in the ABC transporter MsbA: Alternating access with a twist". Proceedings of the National Academy of Sciences of the United States of America. 104 (48): 19005–10. Bibcode:2007PNAS..10419005W. doi:10.1073/pnas.0709388104. PMC 2141898. PMID 18024585.
- Ferreira RJ, Ferreira MJ, Dos Santos DJ (June 2012). "Insights on P-Glycoprotein's Efflux Mechanism Obtained by Molecular Dynamics Simulations". Journal of Chemical Theory and Computation. 8 (6): 1853–64. doi:10.1021/ct300083m. PMID 26593820.
- Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC (November 1987). "Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues". Proceedings of the National Academy of Sciences of the United States of America. 84 (21): 7735–8. Bibcode:1987PNAS...84.7735T. doi:10.1073/pnas.84.21.7735. PMC 299375. PMID 2444983.
- Schinkel AH (April 1999). "P-Glycoprotein, a gatekeeper in the blood-brain barrier". Advanced Drug Delivery Reviews. 36 (2–3): 179–194. doi:10.1016/S0169-409X(98)00085-4. PMID 10837715.
- "Entrez Gene: ABCB1".
- "Desloratadine: Drug information". UpToDate. Retrieved 2019-02-01.
- "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". FDA. 26 May 2021.
- Goldsmith ME, Gudas JM, Schneider E, Cowan KH (January 1995). "Wild type p53 stimulates expression from the human multidrug resistance promoter in a p53-negative cell line". The Journal of Biological Chemistry. 270 (4): 1894–8. doi:10.1074/jbc.270.4.1894. PMID 7829527.
- ^ Bargou RC, Jürchott K, Wagener C, Bergmann S, Metzner S, Bommert K, et al. (April 1997). "Nuclear localization and increased levels of transcription factor YB-1 in primary human breast cancers are associated with intrinsic MDR1 gene expression". Nature Medicine. 3 (4): 447–50. doi:10.1038/nm0497-447. PMID 9095180. S2CID 13323149.
- Zhou G, Kuo MT (June 1997). "NF-kappaB-mediated induction of mdr1b expression by insulin in rat hepatoma cells". The Journal of Biological Chemistry. 272 (24): 15174–83. doi:10.1074/jbc.272.24.15174. PMID 9182539.
- Lim JC, Kania KD, Wijesuriya H, Chawla S, Sethi JK, Pulaski L, et al. (August 2008). "Activation of beta-catenin signalling by GSK-3 inhibition increases p-glycoprotein expression in brain endothelial cells". Journal of Neurochemistry. 106 (4): 1855–65. doi:10.1111/j.1471-4159.2008.05537.x. PMC 4303914. PMID 18624906.
- Yang JM, Vassil AD, Hait WN (October 2001). "Activation of phospholipase C induces the expression of the multidrug resistance (MDR1) gene through the Raf-MAPK pathway". Molecular Pharmacology. 60 (4): 674–80. PMID 11562428.
- Lu F, Hou YQ, Song Y, Yuan ZJ (January 2013). "TFPI-2 downregulates multidrug resistance protein in 5-FU-resistant human hepatocellular carcinoma BEL-7402/5-FU cells". Anatomical Record. 296 (1): 56–63. doi:10.1002/ar.22611. PMID 23125179. S2CID 12846258.
- ^ Sui H, Cai GX, Pan SF, Deng WL, Wang YW, Chen ZS, et al. (December 2014). "miR200c attenuates P-gp-mediated MDR and metastasis by targeting JNK2/c-Jun signaling pathway in colorectal cancer". Molecular Cancer Therapeutics. 13 (12): 3137–51. doi:10.1158/1535-7163.MCT-14-0167. PMID 25205654.
- Bark H, Choi CH (May 2010). "PSC833, cyclosporine analogue, downregulates MDR1 expression by activating JNK/c-Jun/AP-1 and suppressing NF-kappaB". Cancer Chemotherapy and Pharmacology. 65 (6): 1131–6. doi:10.1007/s00280-009-1121-7. PMID 19763573. S2CID 31179492.
- Park SM, Gaur AB, Lengyel E, Peter ME (April 2008). "The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2". Genes & Development. 22 (7): 894–907. doi:10.1101/gad.1640608. PMC 2279201. PMID 18381893.
- Sachdeva M, Liu Q, Cao J, Lu Z, Mo YY (August 2012). "Negative regulation of miR-145 by C/EBP-β through the Akt pathway in cancer cells". Nucleic Acids Research. 40 (14): 6683–92. doi:10.1093/nar/gks324. PMC 3413133. PMID 22495929.
- Li J, Wang Y, Song Y, Fu Z, Yu W (August 2014). "miR-27a regulates cisplatin resistance and metastasis by targeting RKIP in human lung adenocarcinoma cells". Molecular Cancer. 13: 193. doi:10.1186/1476-4598-13-193. PMC 4158130. PMID 25128483.
- Zhang H, Li M, Han Y, Hong L, Gong T, Sun L, et al. (September 2010). "Down-regulation of miR-27a might reverse multidrug resistance of esophageal squamous cell carcinoma". Digestive Diseases and Sciences. 55 (9): 2545–51. doi:10.1007/s10620-009-1051-6. PMID 19960259. S2CID 43382510.
- Xie Y, Burcu M, Linn DE, Qiu Y, Baer MR (August 2010). "Pim-1 kinase protects P-glycoprotein from degradation and enables its glycosylation and cell surface expression". Molecular Pharmacology. 78 (2): 310–8. doi:10.1124/mol.109.061713. PMC 11037423. PMID 20460432. S2CID 6190303.
- Fu D, van Dam EM, Brymora A, Duggin IG, Robinson PJ, Roufogalis BD (July 2007). "The small GTPases Rab5 and RalA regulate intracellular traffic of P-glycoprotein". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1773 (7): 1062–72. doi:10.1016/j.bbamcr.2007.03.023. PMID 17524504.
- Ferrándiz-Huertas C, Fernández-Carvajal A, Ferrer-Montiel A (January 2011). "Rab4 interacts with the human P-glycoprotein and modulates its surface expression in multidrug resistant K562 cells". International Journal of Cancer. 128 (1): 192–205. doi:10.1002/ijc.25310. PMID 20209493. S2CID 25335596.
- ^ Horn JR, Hansten P (December 2008). "Drug Transporters: The Final Frontier for Drug Interactions". Pharmacy Times. Retrieved 2018-11-30.
- ^ "Drug Interactions & Labeling – Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". Center for Drug Evaluation and Research. U.S. Food and Drug Administration. Retrieved 2018-11-30.
- Srivalli KM, Lakshmi PK (July 2012). "Overview of P-glycoprotein inhibitors: a rational outlook". Brazilian Journal of Pharmaceutical Sciences. 48 (3): 353–367. doi:10.1590/S1984-82502012000300002.

- Ruike Z, Junhua C, Wenxing P (November 2010). "In vitro and in vivo evaluation of the effects of duloxetine on P-gp function". Human Psychopharmacology. 25 (7–8): 553–559. doi:10.1002/hup.1152. PMID 21312289. S2CID 3516785.
- Gopisankar MG, Hemachandren M, Surendiran A. ABCB1 266G-T single nucleotide polymorphism influences warfarin dose requirement for warfarin maintenance therapy. Br J Biomed Sci 2019:76;150-152
- "Use of Non-Vitamin K Antagonist Oral Anticoagulants (NOAC) in Non-Valvular Atrial Fibrillation". Ministry of Health. Province of British Columbia. Appendix A. 2015. Archived from the original on 2018-12-01. Retrieved 2018-11-30.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - "Diltiazem: Drug information". UpToDate. Retrieved 2019-02-01.
- van Assema DM, van Berckel BN (2016). "Blood-Brain Barrier ABC-transporter P-glycoprotein in Alzheimer's Disease: Still a Suspect?". Current Pharmaceutical Design. 22 (38): 5808–5816. doi:10.2174/1381612822666160804094544. PMID 27494062.
- Ho GT, Moodie FM, Satsangi J (May 2003). "Multidrug resistance 1 gene (P-glycoprotein 170): an important determinant in gastrointestinal disease?". Gut. 52 (5): 759–66. doi:10.1136/gut.52.5.759. PMC 1773632. PMID 12692067.
- ^ Cario E (March 2017). "P-glycoprotein multidrug transporter in inflammatory bowel diseases: More questions than answers". World Journal of Gastroenterology. 23 (9): 1513–1520. doi:10.3748/wjg.v23.i9.1513. PMC 5340804. PMID 28321153.
- Wilk JN, Bilsborough J, Viney JL (2005). "The mdr1a-/- mouse model of spontaneous colitis: a relevant and appropriate animal model to study inflammatory bowel disease". Immunologic Research. 31 (2): 151–9. doi:10.1385/ir:31:2:151. PMID 15778512. S2CID 21256040.
- Sui H, Fan ZZ, Li Q (April 2012). "Signal transduction pathways and transcriptional mechanisms of ABCB1/Pgp-mediated multiple drug resistance in human cancer cells". The Journal of International Medical Research. 40 (2): 426–35. doi:10.1177/147323001204000204. PMID 22613403.
- Breier A, Gibalova L, Seres M, Barancik M, Sulova Z (January 2013). "New insight into p-glycoprotein as a drug target". Anti-Cancer Agents in Medicinal Chemistry. 13 (1): 159–70. doi:10.2174/1871520611307010159. PMID 22931413.
- Juliano RL, Ling V (November 1976). "A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants". Biochimica et Biophysica Acta (BBA) - Biomembranes. 455 (1): 152–62. doi:10.1016/0005-2736(76)90160-7. PMID 990323.
- Kim Y, Chen J (February 2018). "Molecular structure of human P-glycoprotein in the ATP-bound, outward-facing conformation". Science. 359 (6378): 915–919. Bibcode:2018Sci...359..915K. doi:10.1126/science.aar7389. PMID 29371429.
- Luurtsema G, Windhorst AD, Mooijer MP, Herscheid A, Lammertsma AA, Franssen EJ (2002). "Fully automated high yield synthesis of (R)- and (S)-[C-11]verapamil for measuring P-glycoprotein function with positron emission tomography". Journal of Labelled Compounds and Radiopharmaceuticals. 45 (14): 1199–1207. doi:10.1002/jlcr.632.
- Wirths S, Lanzavecchia A (December 2005). "ABCB1 transporter discriminates human resting naive B cells from cycling transitional and memory B cells". European Journal of Immunology. 35 (12): 3433–41. doi:10.1002/eji.200535364. PMID 16259010. S2CID 24412083.
- Inhibiting Cancer Drug Resistance Gene May Not Be Best Approach Apr 2020
- Levran O, O'Hara K, Peles E, et al. (2008). "AABCB1 (MDR1) genetic variants are associated with methadone doses required for effective treatment of heroin dependence". Hum Mol Genet. 17 (14): 2219–2227. doi:10.1093/hmg/ddn122. PMC 2599947. PMID 18424454.
Further reading
- Kumar YS, Adukondalu D, Sathish D, Vishnu YV, Ramesh G, Latha AB, et al. (2010). "P-Glycoprotein- and cytochrome P-450-mediated herbal drug interactions". Drug Metabolism and Drug Interactions. 25 (1–4): 3–16. doi:10.1515/DMDI.2010.006. PMID 21417789. S2CID 10573193.
- Kim Y, Chen J (February 2018). "Molecular structure of human P-glycoprotein in the ATP-bound, outward-facing conformation". Science. 359 (6378): 915–919. Bibcode:2018Sci...359..915K. doi:10.1126/science.aar7389. PMID 29371429.
External links
- P-Glycoprotein at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ABCB1 human gene location in the UCSC Genome Browser.
- ABCB1 human gene details in the UCSC Genome Browser.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.
| Membrane proteins, carrier proteins: membrane transport proteins ABC transporter (TC 3A1) | |
|---|---|
| A | |
| B | |
| C | |
| D | |
| E | |
| F | |
| G | |
| see also ABC transporter disorders | |
| Proteins: clusters of differentiation (see also list of human clusters of differentiation) | |
|---|---|
| 1–50 | |
| 51–100 | |
| 101–150 | |
| 151–200 | |
| 201–250 | |
| 251–300 | |
| 301–350 | |