| Part of a series on |
| Genetic engineering |
|---|
 |
| Genetically modified organisms |
| History and regulation |
| Process |
| Applications |
| Controversies |
Gene therapy is a medical technology that aims to produce a therapeutic effect through the manipulation of gene expression or through altering the biological properties of living cells.
The first attempt at modifying human DNA was performed in 1980, by Martin Cline, but the first successful nuclear gene transfer in humans, approved by the National Institutes of Health, was performed in May 1989. The first therapeutic use of gene transfer as well as the first direct insertion of human DNA into the nuclear genome was performed by French Anderson in a trial starting in September 1990. Between 1989 and December 2018, over 2,900 clinical trials were conducted, with more than half of them in phase I. In 2003, Gendicine became the first gene therapy to receive regulatory approval. Since that time, further gene therapy drugs were approved, such as alipogene tiparvovec (2012), Strimvelis (2016), tisagenlecleucel (2017), voretigene neparvovec (2017), patisiran (2018), onasemnogene abeparvovec (2019), idecabtagene vicleucel (2021), nadofaragene firadenovec, valoctocogene roxaparvovec and etranacogene dezaparvovec (all 2022). Most of these approaches utilize adeno-associated viruses (AAVs) and lentiviruses for performing gene insertions, in vivo and ex vivo, respectively. AAVs are characterized by stabilizing the viral capsid, lower immunogenicity, ability to transduce both dividing and nondividing cells, the potential to integrate site specifically and to achieve long-term expression in the in-vivo treatment. ASO / siRNA approaches such as those conducted by Alnylam and Ionis Pharmaceuticals require non-viral delivery systems, and utilize alternative mechanisms for trafficking to liver cells by way of GalNAc transporters.
Not all medical procedures that introduce alterations to a patient's genetic makeup can be considered gene therapy. Bone marrow transplantation and organ transplants in general have been found to introduce foreign DNA into patients.
Background
Gene therapy was first conceptualized in the 1960s, when the feasibility of adding new genetic functions to mammalian cells began to be researched. Several methods to do so were tested, including injecting genes with a micropipette directly into a living mammalian cell, and exposing cells to a precipitate of DNA that contained the desired genes. Scientists theorized that a virus could also be used as a vehicle, or vector, to deliver new genes into cells.
One of the first scientists to report the successful direct incorporation of functional DNA into a mammalian cell was biochemist Dr. Lorraine Marquardt Kraus (6 September 1922 – 1 July 2016) at the University of Tennessee Health Science Center in Memphis, Tennessee. In 1961, she managed to genetically alter the hemoglobin of cells from bone marrow taken from a patient with sickle cell anaemia. She did this by incubating the patient's cells in tissue culture with DNA extracted from a donor with normal hemoglobin. In 1968, researchers Theodore Friedmann, Jay Seegmiller, and John Subak-Sharpe at the National Institutes of Health (NIH), Bethesda, in the United States successfully corrected genetic defects associated with Lesch-Nyhan syndrome, a debilitating neurological disease, by adding foreign DNA to cultured cells collected from patients suffering from the disease.
The first attempt, an unsuccessful one, at gene therapy (as well as the first case of medical transfer of foreign genes into humans not counting organ transplantation) was performed by geneticist Martin Cline of the University of California, Los Angeles in California, United States on 10 July 1980. Cline claimed that one of the genes in his patients was active six months later, though he never published this data or had it verified.
After extensive research on animals throughout the 1980s and a 1989 bacterial gene tagging trial on humans, the first gene therapy widely accepted as a success was demonstrated in a trial that started on 14 September 1990, when Ashanthi DeSilva was treated for ADA-SCID.
The first somatic treatment that produced a permanent genetic change was initiated in 1993. The goal was to cure malignant brain tumors by using recombinant DNA to transfer a gene making the tumor cells sensitive to a drug that in turn would cause the tumor cells to die.
The polymers are either translated into proteins, interfere with target gene expression, or possibly correct genetic mutations. The most common form uses DNA that encodes a functional, therapeutic gene to replace a mutated gene. The polymer molecule is packaged within a "vector", which carries the molecule inside cells.
Early clinical failures led to dismissals of gene therapy. Clinical successes since 2006 regained researchers' attention, although as of 2014, it was still largely an experimental technique. These include treatment of retinal diseases Leber's congenital amaurosis and choroideremia, X-linked SCID, ADA-SCID, adrenoleukodystrophy, chronic lymphocytic leukemia (CLL), acute lymphocytic leukemia (ALL), multiple myeloma, haemophilia, and Parkinson's disease. Between 2013 and April 2014, US companies invested over $600 million in the field.
The first commercial gene therapy, Gendicine, was approved in China in 2003, for the treatment of certain cancers. In 2011, Neovasculgen was registered in Russia as the first-in-class gene-therapy drug for treatment of peripheral artery disease, including critical limb ischemia. In 2012, alipogene tiparvovec, a treatment for a rare inherited disorder, lipoprotein lipase deficiency, became the first treatment to be approved for clinical use in either the European Union or the United States after its endorsement by the European Commission.
Following early advances in genetic engineering of bacteria, cells, and small animals, scientists started considering how to apply it to medicine. Two main approaches were considered – replacing or disrupting defective genes. Scientists focused on diseases caused by single-gene defects, such as cystic fibrosis, haemophilia, muscular dystrophy, thalassemia, and sickle cell anemia. alipogene tiparvovec treats one such disease, caused by a defect in lipoprotein lipase.
DNA must be administered, reach the damaged cells, enter the cell and either express or disrupt a protein. Multiple delivery techniques have been explored. The initial approach incorporated DNA into an engineered virus to deliver the DNA into a chromosome. Naked DNA approaches have also been explored, especially in the context of vaccine development.
Generally, efforts focused on administering a gene that causes a needed protein to be expressed. More recently, increased understanding of nuclease function has led to more direct DNA editing, using techniques such as zinc finger nucleases and CRISPR. The vector incorporates genes into chromosomes. The expressed nucleases then knock out and replace genes in the chromosome. As of 2014 these approaches involve removing cells from patients, editing a chromosome and returning the transformed cells to patients.
Gene editing is a potential approach to alter the human genome to treat genetic diseases, viral diseases, and cancer. As of 2020 these approaches are being studied in clinical trials.
Classification
Breadth of definition
In 1986, a meeting at the Institute Of Medicine defined gene therapy as the addition or replacement of a gene in a targeted cell type. In the same year, the FDA announced that it had jurisdiction over approving "gene therapy" without defining the term. The FDA added a very broad definition in 1993 of any treatment that would 'modify or manipulate the expression of genetic material or to alter the biological properties of living cells'. In 2018 this was narrowed to 'products that mediate their effects by transcription or translation of transferred genetic material or by specifically altering host (human) genetic sequences'.
Writing in 2018, in the Journal of Law and the Biosciences, Sherkow et al. argued for a narrower definition of gene therapy than the FDA's in light of new technology that would consist of any treatment that intentionally and permanently modified a cell's genome, with the definition of genome including episomes outside the nucleus but excluding changes due to episomes that are lost over time. This definition would also exclude introducing cells that did not derive from a patient themselves, but include ex vivo approaches, and would not depend on the vector used.
During the COVID-19 pandemic, some academics insisted that the mRNA vaccines for COVID were not gene therapy to prevent the spread of incorrect information that the vaccine could alter DNA, other academics maintained that the vaccines were a gene therapy because they introduced genetic material into a cell. Fact-checkers, such as Full Fact, Reuters, PolitiFact, and FactCheck.org said that calling the vaccines a gene therapy was incorrect. Podcast host Joe Rogan was criticized for calling mRNA vaccines gene therapy as was British politician Andrew Bridgen, with fact checker Full Fact calling for Bridgen to be removed from the conservative party for this and other statements.
Genes present or added
Gene therapy encapsulates many forms of adding different nucleic acids to a cell. Gene augmentation adds a new protein coding gene to a cell. One form of gene augmentiation is gene replacement therapy, a treatment for monogenic recessive disorders where a single gene is not functional an additional functional gene is added. For diseases caused by multiple genes or a dominant gene, gene silencing or gene editing approaches are more appropriate but gene addition, a form of gene augmentation where new gene is added, may improve a cells function without modifying the genes that cause a disorder.
Cell types
Gene therapy may be classified into two types by the type of cell it affects: somatic cell and germline gene therapy.
In somatic cell gene therapy (SCGT), the therapeutic genes are transferred into any cell other than a gamete, germ cell, gametocyte, or undifferentiated stem cell. Any such modifications affect the individual patient only, and are not inherited by offspring. Somatic gene therapy represents mainstream basic and clinical research, in which therapeutic DNA (either integrated in the genome or as an external episome or plasmid) is used to treat disease. Over 600 clinical trials utilizing SCGT are underway in the US. Most focus on severe genetic disorders, including immunodeficiencies, haemophilia, thalassaemia, and cystic fibrosis. Such single gene disorders are good candidates for somatic cell therapy. The complete correction of a genetic disorder or the replacement of multiple genes is not yet possible. Only a few of the trials are in the advanced stages.
In germline gene therapy (GGT), germ cells (sperm or egg cells) are modified by the introduction of functional genes into their genomes. Modifying a germ cell causes all the organism's cells to contain the modified gene. The change is therefore heritable and passed on to later generations. Australia, Canada, Germany, Israel, Switzerland, and the Netherlands prohibit GGT for application in human beings, for technical and ethical reasons, including insufficient knowledge about possible risks to future generations and higher risks versus SCGT. The US has no federal controls specifically addressing human genetic modification (beyond FDA regulations for therapies in general).
In vivo versus ex vivo therapies

In in vivo gene therapy, a vector (typically, a virus) is introduced to the patient, which then achieves the desired biological effect by passing the genetic material (e.g. for a missing protein) into the patient's cells. In ex vivo gene therapies, such as CAR-T therapeutics, the patient's own cells (autologous) or healthy donor cells (allogeneic) are modified outside the body (hence, ex vivo) using a vector to express a particular protein, such as a chimeric antigen receptor.
In vivo gene therapy is seen as simpler, since it does not require the harvesting of mitotic cells. However, ex vivo gene therapies are better tolerated and less associated with severe immune responses. The death of Jesse Gelsinger in a trial of an adenovirus-vectored treatment for ornithine transcarbamylase deficiency due to a systemic inflammatory reaction led to a temporary halt on gene therapy trials across the United States. As of 2021, in vivo and ex vivo therapeutics are both seen as safe.
Gene editing
See also: CRISPR gene editing
The concept of gene therapy is to fix a genetic problem at its source. If, for instance, a mutation in a certain gene causes the production of a dysfunctional protein resulting (usually recessively) in an inherited disease, gene therapy could be used to deliver a copy of this gene that does not contain the deleterious mutation and thereby produces a functional protein. This strategy is referred to as gene replacement therapy and could be employed to treat inherited retinal diseases.
While the concept of gene replacement therapy is mostly suitable for recessive diseases, novel strategies have been suggested that are capable of also treating conditions with a dominant pattern of inheritance.
- The introduction of CRISPR gene editing has opened new doors for its application and utilization in gene therapy, as instead of pure replacement of a gene, it enables correction of the particular genetic defect. Solutions to medical hurdles, such as the eradication of latent human immunodeficiency virus (HIV) reservoirs and correction of the mutation that causes sickle cell disease, may be available as a therapeutic option in the future.
- Prosthetic gene therapy aims to enable cells of the body to take over functions they physiologically do not carry out. One example is the so-called vision restoration gene therapy, that aims to restore vision in patients with end-stage retinal diseases. In end-stage retinal diseases, the photoreceptors, as the primary light sensitive cells of the retina are irreversibly lost. By the means of prosthetic gene therapy light sensitive proteins are delivered into the remaining cells of the retina, to render them light sensitive and thereby enable them to signal visual information towards the brain.
In vivo, gene editing systems using CRISPR have been used in studies with mice to treat cancer and have been effective at reducing tumors. In vitro, the CRISPR system has been used to treat HPV cancer tumors. Adeno-associated virus, Lentivirus based vectors have been to introduce the genome for the CRISPR system.
Vectors
Main article: Vectors in gene therapyThe delivery of DNA into cells can be accomplished by multiple methods. The two major classes are recombinant viruses (sometimes called biological nanoparticles or viral vectors) and naked DNA or DNA complexes (non-viral methods).
Viruses
Main article: Viral vector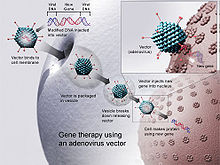
In order to replicate, viruses introduce their genetic material into the host cell, tricking the host's cellular machinery into using it as blueprints for viral proteins. Retroviruses go a stage further by having their genetic material copied into the nuclear genome of the host cell. Scientists exploit this by substituting part of a virus's genetic material with therapeutic DNA or RNA. Like the genetic material (DNA or RNA) in viruses, therapeutic genetic material can be designed to simply serve as a temporary blueprint that degrades naturally, as in a non-integrative vectors, or to enter the host's nucleus becoming a permanent part of the host's nuclear DNA in infected cells.
A number of viruses have been used for human gene therapy, including viruses such as lentivirus, adenoviruses, herpes simplex, vaccinia, and adeno-associated virus.
Adenovirus viral vectors (Ad) temporarily modify a cell's genetic expression with genetic material that is not integrated into the host cell's DNA. As of 2017, such vectors were used in 20% of trials for gene therapy. Adenovirus vectors are mostly used in cancer treatments and novel genetic vaccines such as the Ebola vaccine, vaccines used in clinical trials for HIV and SARS-CoV-2, or cancer vaccines.
Lentiviral vectors based on lentivirus, a retrovirus, can modify a cell's nuclear genome to permanently express a gene, although vectors can be modified to prevent integration. Retroviruses were used in 18% of trials before 2018. Libmeldy is an ex vivo stem cell treatment for metachromatic leukodystrophy which uses a lentiviral vector and was approved by the European medical agency in 2020.
Adeno-associated virus (AAV) is a virus that is incapable of transmission between cells unless the cell is infected by another virus, a helper virus. Adenovirus and the herpes viruses act as helper viruses for AAV. AAV persists within the cell outside of the cell's nuclear genome for an extended period of time through the formation of concatemers mostly organized as episomes. Genetic material from AAV vectors is integrated into the host cell's nuclear genome at a low frequency and likely mediated by the DNA-modifying enzymes of the host cell. Animal models suggest that integration of AAV genetic material into the host cell's nuclear genome may cause hepatocellular carcinoma, a form of liver cancer. Several AAV investigational agents have been explored in treatment of wet age related macular degeneration by both intravitreal and subretinal approaches as a potential application of AAV gene therapy for human disease.
Non-viral
| This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources in this section. Unsourced material may be challenged and removed. (April 2021) (Learn how and when to remove this message) |
Non-viral vectors for gene therapy present certain advantages over viral methods, such as large scale production and low host immunogenicity. However, non-viral methods initially produced lower levels of transfection and gene expression, and thus lower therapeutic efficacy. Newer technologies offer promise of solving these problems, with the advent of increased cell-specific targeting and subcellular trafficking control.
Methods for non-viral gene therapy include the injection of naked DNA, electroporation, the gene gun, sonoporation, magnetofection, the use of oligonucleotides, lipoplexes, dendrimers, and inorganic nanoparticles. These therapeutics can be administered directly or through scaffold enrichment.
More recent approaches, such as those performed by companies such as Ligandal, offer the possibility of creating cell-specific targeting technologies for a variety of gene therapy modalities, including RNA, DNA and gene editing tools such as CRISPR. Other companies, such as Arbutus Biopharma and Arcturus Therapeutics, offer non-viral, non-cell-targeted approaches that mainly exhibit liver trophism. In more recent years, startups such as Sixfold Bio, GenEdit, and Spotlight Therapeutics have begun to solve the non-viral gene delivery problem. Non-viral techniques offer the possibility of repeat dosing and greater tailorability of genetic payloads, which in the future will be more likely to take over viral-based delivery systems.
Companies such as Editas Medicine, Intellia Therapeutics, CRISPR Therapeutics, Casebia, Cellectis, Precision Biosciences, bluebird bio, Excision BioTherapeutics, and Sangamo have developed non-viral gene editing techniques, however frequently still use viruses for delivering gene insertion material following genomic cleavage by guided nucleases. These companies focus on gene editing, and still face major delivery hurdles.
BioNTech, Moderna Therapeutics and CureVac focus on delivery of mRNA payloads, which are necessarily non-viral delivery problems.
Alnylam, Dicerna Pharmaceuticals, and Ionis Pharmaceuticals focus on delivery of siRNA (antisense oligonucleotides) for gene suppression, which also necessitate non-viral delivery systems.
In academic contexts, a number of laboratories are working on delivery of PEGylated particles, which form serum protein coronas and chiefly exhibit LDL receptor mediated uptake in cells in vivo.
Treatment
Cancer

There have been attempts to treat cancer using gene therapy. As of 2017, 65% of gene therapy trials were for cancer treatment.
Adenovirus vectors are useful for some cancer gene therapies because adenovirus can transiently insert genetic material into a cell without permanently altering the cell's nuclear genome. These vectors can be used to cause antigens to be added to cancers causing an immune response, or hinder angiogenesis by expressing certain proteins. An Adenovirus vector is used in the commercial products Gendicine and Oncorine. Another commercial product, Rexin G, uses a retrovirus-based vector and selectively binds to receptors that are more expressed in tumors.
One approach, suicide gene therapy, works by introducing genes encoding enzymes that will cause a cancer cell to die. Another approach is the use oncolytic viruses, such as Oncorine, which are viruses that selectively reproduce in cancerous cells leaving other cells unaffected.
mRNA has been suggested as a non-viral vector for cancer gene therapy that would temporarily change a cancerous cell's function to create antigens or kill the cancerous cells and there have been several trials.
Afamitresgene autoleucel, sold under the brand name Tecelra, is an autologous T cell immunotherapy used for the treatment of synovial sarcoma. It is a T cell receptor (TCR) gene therapy. It is the first FDA-approved engineered cell therapy for a solid tumor. It uses a self-inactivating lentiviral vector to express a T-cell receptor specific for MAGE-A4, a melanoma-associated antigen.
Genetic diseases
Gene therapy approaches to replace a faulty gene with a healthy gene have been proposed and are being studied for treating some genetic diseases. As of 2017, 11.1% of gene therapy clinical trials targeted monogenic diseases.
Diseases such as sickle cell disease that are caused by autosomal recessive disorders for which a person's normal phenotype or cell function may be restored in cells that have the disease by a normal copy of the gene that is mutated, may be a good candidate for gene therapy treatment. The risks and benefits related to gene therapy for sickle cell disease are not known.
Gene therapy has been used in the eye. The eye is especially suitable for adeno-associated virus vectors. Voretigene neparvovec is an approved gene therapy to treat Leber's hereditary optic neuropathy. alipogene tiparvovec, a treatment for pancreatitis caused by a genetic condition, and Zolgensma for the treatment of spinal muscular atrophy both use an adeno-associated virus vector.
Infectious diseases
As of 2017, 7% of genetic therapy trials targeted infectious diseases. 69.2% of trials targeted HIV, 11% hepatitis B or C, and 7.1% malaria.
List of gene therapies for treatment of disease
See also: List of gene therapiesSome genetic therapies have been approved by the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and for use in Russia and China.
| INN | Brand name | Type | Manufacturer | Target | US Food and Drug Administration (FDA) approved | European Medicines Agency (EMA) authorized |
|---|---|---|---|---|---|---|
| afamitresgene autoleucel | Tecelra | Ex vitro | Adaptimmune | synovial sarcoma | August 2024 | |
| alipogene tiparvovec | Glybera | In vivo | Chiesi Farmaceutici | lipoprotein lipase deficiency | Withdrawn | |
| atidarsagene autotemcel | Libmeldy, Lenmeldy
(Arylsulfatase A gene encoding autologous CD34+ cells) |
Ex vitro | Orchard Therapeutics | metachromatic leukodystrophy | March 2024 | December 2020 |
| autologous CD34+ | Strimvelis | adenosine deaminase deficiency (ADA-SCID) | May 2016 | |||
| axicabtagene ciloleucel | Yescarta | Ex vitro | Kite pharma | large B-cell lymphoma | October 2017 | August 2018 |
| beremagene geperpavec | Vyjuvek | In vivo | Krystal Biotech | dystrophic epidermolysis bullosa (DEB) | May 2023 | |
| betibeglogene autotemcel | Zynteglo | beta thalassemia | August 2022 | May 2019 | ||
| brexucabtagene autoleucel | Tecartus | Ex vitro | Kite Pharma | mantle cell lymphoma and acute lymphoblastic leukemia | July 2020 | December 2020 |
| cambiogenplasmid | Neovasculgen | vascular endothelial growth factor peripheral artery disease | ||||
| delandistrogene moxeparvovec | Elevidys | In vivo | Catalent | Duchenne muscular dystrophy | June 2023 | |
| eladocagene exuparvovec | Kebilidi, Upstaza | In vivo | PTC Therapeutics | aromatic L‑amino acid decarboxylase (AADC) deficiency | November 2024 | July 2022 |
| elivaldogene autotemcel | Skysona | cerebral adrenoleukodystrophy | July 2021 | |||
| exagamglogene autotemcel | Casgevy | Ex vivo | Vertex Pharmaceuticals | sickle cell disease | December 2023 | |
| gendicine | head and neck squamous cell carcinoma | |||||
| idecabtagene vicleucel | Abecma | Ex vivo | Celgene | multiple myeloma | March 2021 | |
| lisocabtagene maraleucel | Breyanzi | Ex vivo | Juno Therapeutics | B-cell lymphoma | February 2021 | |
| lovotibeglogene autotemcel | Lyfgenia | Ex vivo | Bluebird Bio | sickle cell disease | December 2023 | |
| nadofaragene firadenovec | Adstiladrin | Ferring Pharmaceuticals | high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) | Yes | ||
| obecabtagene autoleucel | Aucatzyl | Autolus Therapeutics | acute lymphoblastic leukemia | November 2024 | ||
| onasemnogene abeparvovec | Zolgensma | In vivo | Novartis Gene Therapies | spinal muscular atrophy type I | May 2019 | March 2020 |
| talimogene laherparepvec | Imlygic | In vivo | Amgen | melanoma | October 2015 | December 2015 |
| tisagenlecleucel | Kymriah | B cell lymphoblastic leukemia | August 2018 | |||
| valoctocogene roxaparvovec | Roctavian | BioMarin International Limited | hemophilia A | August 2022 | ||
| voretigene neparvovec | Luxturna | In vivo | Spark Therapeutics | biallelic RPE65 mutation associated Leber congenital amaurosis | December 2017 | November 2018 |
Adverse effects, contraindications and hurdles for use
Some of the unsolved problems include:
- Off-target effects – The possibility of unwanted, likely harmful, changes to the genome present a large barrier to the widespread implementation of this technology. Improvements to the specificity of gRNAs and Cas enzymes present viable solutions to this issue as well as the refinement of the delivery method of CRISPR. It is likely that different diseases will benefit from different delivery methods.
- Short-lived nature – Before gene therapy can become a permanent cure for a condition, the therapeutic DNA introduced into target cells must remain functional and the cells containing the therapeutic DNA must be stable. Problems with integrating therapeutic DNA into the nuclear genome and the rapidly dividing nature of many cells prevent it from achieving long-term benefits. Patients require multiple treatments.
- Immune response – Any time a foreign object is introduced into human tissues, the immune system is stimulated to attack the invader. Stimulating the immune system in a way that reduces gene therapy effectiveness is possible. The immune system's enhanced response to viruses that it has seen before reduces the effectiveness to repeated treatments.
- Problems with viral vectors – Viral vectors carry the risks of toxicity, inflammatory responses, and gene control and targeting issues.
- Multigene disorders – Some commonly occurring disorders, such as heart disease, high blood pressure, Alzheimer's disease, arthritis, and diabetes, are affected by variations in multiple genes, which complicate gene therapy.
- Some therapies may breach the Weismann barrier (between soma and germ-line) protecting the testes, potentially modifying the germline, falling afoul of regulations in countries that prohibit the latter practice.
- Insertional mutagenesis – If the DNA is integrated in a sensitive spot in the genome, for example in a tumor suppressor gene, the therapy could induce a tumor. This has occurred in clinical trials for X-linked severe combined immunodeficiency (X-SCID) patients, in which hematopoietic stem cells were transduced with a corrective transgene using a retrovirus, and this led to the development of T cell leukemia in 3 of 20 patients. One possible solution is to add a functional tumor suppressor gene to the DNA to be integrated. This may be problematic since the longer the DNA is, the harder it is to integrate into cell genomes. CRISPR technology allows researchers to make much more precise genome changes at exact locations.
- Cost – alipogene tiparvovec (Glybera), for example, at a cost of $1.6 million per patient, was reported in 2013, to be the world's most expensive drug.
Deaths
Three patients' deaths have been reported in gene therapy trials, putting the field under close scrutiny. The first was that of Jesse Gelsinger, who died in 1999, because of immune rejection response. One X-SCID patient died of leukemia in 2003. In 2007, a rheumatoid arthritis patient died from an infection; the subsequent investigation concluded that the death was not related to gene therapy.
Regulations
Regulations covering genetic modification are part of general guidelines about human-involved biomedical research. There are no international treaties which are legally binding in this area, but there are recommendations for national laws from various bodies.
The Helsinki Declaration (Ethical Principles for Medical Research Involving Human Subjects) was amended by the World Medical Association's General Assembly in 2008. This document provides principles physicians and researchers must consider when involving humans as research subjects. The Statement on Gene Therapy Research initiated by the Human Genome Organization (HUGO) in 2001, provides a legal baseline for all countries. HUGO's document emphasizes human freedom and adherence to human rights, and offers recommendations for somatic gene therapy, including the importance of recognizing public concerns about such research.
United States
No federal legislation lays out protocols or restrictions about human genetic engineering. This subject is governed by overlapping regulations from local and federal agencies, including the Department of Health and Human Services, the FDA and NIH's Recombinant DNA Advisory Committee. Researchers seeking federal funds for an investigational new drug application, (commonly the case for somatic human genetic engineering,) must obey international and federal guidelines for the protection of human subjects.
NIH serves as the main gene therapy regulator for federally funded research. Privately funded research is advised to follow these regulations. NIH provides funding for research that develops or enhances genetic engineering techniques and to evaluate the ethics and quality in current research. The NIH maintains a mandatory registry of human genetic engineering research protocols that includes all federally funded projects.
An NIH advisory committee published a set of guidelines on gene manipulation. The guidelines discuss lab safety as well as human test subjects and various experimental types that involve genetic changes. Several sections specifically pertain to human genetic engineering, including Section III-C-1. This section describes required review processes and other aspects when seeking approval to begin clinical research involving genetic transfer into a human patient. The protocol for a gene therapy clinical trial must be approved by the NIH's Recombinant DNA Advisory Committee prior to any clinical trial beginning; this is different from any other kind of clinical trial.
As with other kinds of drugs, the FDA regulates the quality and safety of gene therapy products and supervises how these products are used clinically. Therapeutic alteration of the human genome falls under the same regulatory requirements as any other medical treatment. Research involving human subjects, such as clinical trials, must be reviewed and approved by the FDA and an Institutional Review Board.
Gene doping
Main article: Gene dopingAthletes may adopt gene therapy technologies to improve their performance. Gene doping is not known to occur, but multiple gene therapies may have such effects. Kayser et al. argue that gene doping could level the playing field if all athletes receive equal access. Critics claim that any therapeutic intervention for non-therapeutic/enhancement purposes compromises the ethical foundations of medicine and sports.
Genetic enhancement
Further information: Human genetic enhancement See also: Human germline engineering and Assisted reproductive technologyGenetic engineering could be used to cure diseases, but also to change physical appearance, metabolism, and even improve physical capabilities and mental faculties such as memory and intelligence. Ethical claims about germline engineering include beliefs that every fetus has a right to remain genetically unmodified, that parents hold the right to genetically modify their offspring, and that every child has the right to be born free of preventable diseases. For parents, genetic engineering could be seen as another child enhancement technique to add to diet, exercise, education, training, cosmetics, and plastic surgery. Another theorist claims that moral concerns limit but do not prohibit germline engineering.
A 2020 issue of the journal Bioethics was devoted to moral issues surrounding germline genetic engineering in people.
Possible regulatory schemes include a complete ban, provision to everyone, or professional self-regulation. The American Medical Association's Council on Ethical and Judicial Affairs stated that "genetic interventions to enhance traits should be considered permissible only in severely restricted situations: (1) clear and meaningful benefits to the fetus or child; (2) no trade-off with other characteristics or traits; and (3) equal access to the genetic technology, irrespective of income or other socioeconomic characteristics."
As early in the history of biotechnology as 1990, there have been scientists opposed to attempts to modify the human germline using these new tools, and such concerns have continued as technology progressed. With the advent of new techniques like CRISPR, in March 2015 a group of scientists urged a worldwide moratorium on clinical use of gene editing technologies to edit the human genome in a way that can be inherited. In April 2015, researchers sparked controversy when they reported results of basic research to edit the DNA of non-viable human embryos using CRISPR. A committee of the American National Academy of Sciences and National Academy of Medicine gave qualified support to human genome editing in 2017 once answers have been found to safety and efficiency problems "but only for serious conditions under stringent oversight."
History
| This section may be too long and excessively detailed. Please consider summarizing the material. (November 2018) |
1970s and earlier
In 1972, Friedmann and Roblin authored a paper in Science titled "Gene therapy for human genetic disease?". Rogers (1970) was cited for proposing that exogenous good DNA be used to replace the defective DNA in those with genetic defects.
1980s
In 1984, a retrovirus vector system was designed that could efficiently insert foreign genes into mammalian chromosomes.
1990s
The first approved gene therapy clinical research in the US took place on 14 September 1990, at the National Institutes of Health (NIH), under the direction of William French Anderson. Four-year-old Ashanti DeSilva received treatment for a genetic defect that left her with adenosine deaminase deficiency (ADA-SCID), a severe immune system deficiency. The defective gene of the patient's blood cells was replaced by the functional variant. Ashanti's immune system was partially restored by the therapy. Production of the missing enzyme was temporarily stimulated, but the new cells with functional genes were not generated. She led a normal life only with the regular injections performed every two months. The effects were successful, but temporary.
Cancer gene therapy was introduced in 1992/93 (Trojan et al. 1993). The treatment of glioblastoma multiforme, the malignant brain tumor whose outcome is always fatal, was done using a vector expressing antisense IGF-I RNA (clinical trial approved by NIH protocol no.1602 24 November 1993, and by the FDA in 1994). This therapy also represents the beginning of cancer immunogene therapy, a treatment which proves to be effective due to the anti-tumor mechanism of IGF-I antisense, which is related to strong immune and apoptotic phenomena.
In 1992, Claudio Bordignon, working at the Vita-Salute San Raffaele University, performed the first gene therapy procedure using hematopoietic stem cells as vectors to deliver genes intended to correct hereditary diseases. In 2002, this work led to the publication of the first successful gene therapy treatment for ADA-SCID. The success of a multi-center trial for treating children with SCID (severe combined immune deficiency or "bubble boy" disease) from 2000 and 2002, was questioned when two of the ten children treated at the trial's Paris center developed a leukemia-like condition. Clinical trials were halted temporarily in 2002, but resumed after regulatory review of the protocol in the US, the United Kingdom, France, Italy, and Germany.
In 1993, Andrew Gobea was born with SCID following prenatal genetic screening. Blood was removed from his mother's placenta and umbilical cord immediately after birth, to acquire stem cells. The allele that codes for adenosine deaminase (ADA) was obtained and inserted into a retrovirus. Retroviruses and stem cells were mixed, after which the viruses inserted the gene into the stem cell chromosomes. Stem cells containing the working ADA gene were injected into Andrew's blood. Injections of the ADA enzyme were also given weekly. For four years T cells (white blood cells), produced by stem cells, made ADA enzymes using the ADA gene. After four years more treatment was needed.
In 1996, Luigi Naldini and Didier Trono developed a new class of gene therapy vectors based on HIV capable of infecting non-dividing cells that have since then been widely used in clinical and research settings, pioneering lentivirals vector in gene therapy.
Jesse Gelsinger's death in 1999 impeded gene therapy research in the US. As a result, the FDA suspended several clinical trials pending the reevaluation of ethical and procedural practices.
2000s
The modified gene therapy strategy of antisense IGF-I RNA (NIH n˚ 1602) using antisense / triple helix anti-IGF-I approach was registered in 2002, by Wiley gene therapy clinical trial - n˚ 635 and 636. The approach has shown promising results in the treatment of six different malignant tumors: glioblastoma, cancers of liver, colon, prostate, uterus, and ovary (Collaborative NATO Science Programme on Gene Therapy USA, France, Poland n˚ LST 980517 conducted by J. Trojan) (Trojan et al., 2012). This anti-gene antisense/triple helix therapy has proven to be efficient, due to the mechanism stopping simultaneously IGF-I expression on translation and transcription levels, strengthening anti-tumor immune and apoptotic phenomena.
2002
Sickle cell disease can be treated in mice. The mice – which have essentially the same defect that causes human cases – used a viral vector to induce production of fetal hemoglobin (HbF), which normally ceases to be produced shortly after birth. In humans, the use of hydroxyurea to stimulate the production of HbF temporarily alleviates sickle cell symptoms. The researchers demonstrated this treatment to be a more permanent means to increase therapeutic HbF production.
A new gene therapy approach repaired errors in messenger RNA derived from defective genes. This technique has the potential to treat thalassaemia, cystic fibrosis and some cancers.
Researchers created liposomes 25 nanometers across that can carry therapeutic DNA through pores in the nuclear membrane.
2003
In 2003, a research team inserted genes into the brain for the first time. They used liposomes coated in a polymer called polyethylene glycol, which unlike viral vectors, are small enough to cross the blood–brain barrier.
Short pieces of double-stranded RNA (short, interfering RNAs or siRNAs) are used by cells to degrade RNA of a particular sequence. If a siRNA is designed to match the RNA copied from a faulty gene, then the abnormal protein product of that gene will not be produced.
Gendicine is a cancer gene therapy that delivers the tumor suppressor gene p53 using an engineered adenovirus. In 2003, it was approved in China for the treatment of head and neck squamous cell carcinoma.
2006
In March, researchers announced the successful use of gene therapy to treat two adult patients for X-linked chronic granulomatous disease, a disease which affects myeloid cells and damages the immune system. The study is the first to show that gene therapy can treat the myeloid system.
In May, a team reported a way to prevent the immune system from rejecting a newly delivered gene. Similar to organ transplantation, gene therapy has been plagued by this problem. The immune system normally recognizes the new gene as foreign and rejects the cells carrying it. The research utilized a newly uncovered network of genes regulated by molecules known as microRNAs. This natural function selectively obscured their therapeutic gene in immune system cells and protected it from discovery. Mice infected with the gene containing an immune-cell microRNA target sequence did not reject the gene.
In August, scientists successfully treated metastatic melanoma in two patients using killer T cells genetically retargeted to attack the cancer cells.
In November, researchers reported on the use of VRX496, a gene-based immunotherapy for the treatment of HIV that uses a lentiviral vector to deliver an antisense gene against the HIV envelope. In a phase I clinical trial, five subjects with chronic HIV infection who had failed to respond to at least two antiretroviral regimens were treated. A single intravenous infusion of autologous CD4 T cells genetically modified with VRX496 was well tolerated. All patients had stable or decreased viral load; four of the five patients had stable or increased CD4 T cell counts. All five patients had stable or increased immune response to HIV antigens and other pathogens. This was the first evaluation of a lentiviral vector administered in a US human clinical trial.
2007
In May 2007, researchers announced the first gene therapy trial for inherited retinal disease. The first operation was carried out on a 23-year-old British male, Robert Johnson, in early 2007.
2008
Leber's congenital amaurosis is an inherited blinding disease caused by mutations in the RPE65 gene. The results of a small clinical trial in children were published in April. Delivery of recombinant adeno-associated virus (AAV) carrying RPE65 yielded positive results. In May, two more groups reported positive results in independent clinical trials using gene therapy to treat the condition. In all three clinical trials, patients recovered functional vision without apparent side-effects.
2009
In September researchers were able to give trichromatic vision to squirrel monkeys. In November 2009, researchers halted a fatal genetic disorder called adrenoleukodystrophy in two children using a lentivirus vector to deliver a functioning version of ABCD1, the gene that is mutated in the disorder.
2010s
2010
An April paper reported that gene therapy addressed achromatopsia (color blindness) in dogs by targeting cone photoreceptors. Cone function and day vision were restored for at least 33 months in two young specimens. The therapy was less efficient for older dogs.
In September it was announced that an 18-year-old male patient in France with beta thalassemia major had been successfully treated. Beta thalassemia major is an inherited blood disease in which beta haemoglobin is missing and patients are dependent on regular lifelong blood transfusions. The technique used a lentiviral vector to transduce the human β-globin gene into purified blood and marrow cells obtained from the patient in June 2007. The patient's haemoglobin levels were stable at 9 to 10 g/dL. About a third of the hemoglobin contained the form introduced by the viral vector and blood transfusions were not needed. Further clinical trials were planned. Bone marrow transplants are the only cure for thalassemia, but 75% of patients do not find a matching donor.
Cancer immunogene therapy using modified antigene, antisense/triple helix approach was introduced in South America in 2010/11 in La Sabana University, Bogota (Ethical Committee 14 December 2010, no P-004-10). Considering the ethical aspect of gene diagnostic and gene therapy targeting IGF-I, the IGF-I expressing tumors i.e. lung and epidermis cancers were treated (Trojan et al. 2016).
2011
In 2007 and 2008, a man (Timothy Ray Brown) was cured of HIV by repeated hematopoietic stem cell transplantation (see also allogeneic stem cell transplantation, allogeneic bone marrow transplantation, allotransplantation) with double-delta-32 mutation which disables the CCR5 receptor. This cure was accepted by the medical community in 2011. It required complete ablation of existing bone marrow, which is very debilitating.
In August two of three subjects of a pilot study were confirmed to have been cured from chronic lymphocytic leukemia (CLL). The therapy used genetically modified T cells to attack cells that expressed the CD19 protein to fight the disease. In 2013, the researchers announced that 26 of 59 patients had achieved complete remission and the original patient had remained tumor-free.
Human HGF plasmid DNA therapy of cardiomyocytes is being examined as a potential treatment for coronary artery disease as well as treatment for the damage that occurs to the heart after myocardial infarction.
In 2011, Neovasculgen was registered in Russia as the first-in-class gene-therapy drug for treatment of peripheral artery disease, including critical limb ischemia; it delivers the gene encoding for VEGF. Neovasculogen is a plasmid encoding the CMV promoter and the 165 amino acid form of VEGF.
2012
The FDA approved Phase I clinical trials on thalassemia major patients in the US for 10 participants in July. The study was expected to continue until 2015.
In July 2012, the European Medicines Agency recommended approval of a gene therapy treatment for the first time in either Europe or the United States. The treatment used Alipogene tiparvovec (Glybera) to compensate for lipoprotein lipase deficiency, which can cause severe pancreatitis. The recommendation was endorsed by the European Commission in November 2012, and commercial rollout began in late 2014. Alipogene tiparvovec was expected to cost around $1.6 million per treatment in 2012, revised to $1 million in 2015, making it the most expensive medicine in the world at the time. As of 2016, only the patients treated in clinical trials and a patient who paid the full price for treatment have received the drug.
In December 2012, it was reported that 10 of 13 patients with multiple myeloma were in remission "or very close to it" three months after being injected with a treatment involving genetically engineered T cells to target proteins NY-ESO-1 and LAGE-1, which exist only on cancerous myeloma cells.
2013
In March researchers reported that three of five adult subjects who had acute lymphocytic leukemia (ALL) had been in remission for five months to two years after being treated with genetically modified T cells which attacked cells with CD19 genes on their surface, i.e. all B cells, cancerous or not. The researchers believed that the patients' immune systems would make normal T cells and B cells after a couple of months. They were also given bone marrow. One patient relapsed and died and one died of a blood clot unrelated to the disease.
Following encouraging Phase I trials, in April, researchers announced they were starting Phase II clinical trials (called CUPID2 and SERCA-LVAD) on 250 patients at several hospitals to combat heart disease. The therapy was designed to increase the levels of SERCA2, a protein in heart muscles, improving muscle function. The U.S. Food and Drug Administration (FDA) granted this a breakthrough therapy designation to accelerate the trial and approval process. In 2016, it was reported that no improvement was found from the CUPID 2 trial.
In July researchers reported promising results for six children with two severe hereditary diseases had been treated with a partially deactivated lentivirus to replace a faulty gene and after 7–32 months. Three of the children had metachromatic leukodystrophy, which causes children to lose cognitive and motor skills. The other children had Wiskott–Aldrich syndrome, which leaves them to open to infection, autoimmune diseases, and cancer. Follow up trials with gene therapy on another six children with Wiskott–Aldrich syndrome were also reported as promising.
In October researchers reported that two children born with adenosine deaminase severe combined immunodeficiency disease (ADA-SCID) had been treated with genetically engineered stem cells 18 months previously and that their immune systems were showing signs of full recovery. Another three children were making progress. In 2014, a further 18 children with ADA-SCID were cured by gene therapy. ADA-SCID children have no functioning immune system and are sometimes known as "bubble children".
Also in October researchers reported that they had treated six people with haemophilia in early 2011 using an adeno-associated virus. Over two years later all six were producing clotting factor.
2014
In January researchers reported that six choroideremia patients had been treated with adeno-associated virus with a copy of REP1. Over a six-month to two-year period all had improved their sight. By 2016, 32 patients had been treated with positive results and researchers were hopeful the treatment would be long-lasting. Choroideremia is an inherited genetic eye disease with no approved treatment, leading to loss of sight.
In March researchers reported that 12 HIV patients had been treated since 2009 in a trial with a genetically engineered virus with a rare mutation (CCR5 deficiency) known to protect against HIV with promising results.
Clinical trials of gene therapy for sickle cell disease were started in 2014.
In February LentiGlobin BB305, a gene therapy treatment undergoing clinical trials for treatment of beta thalassemia gained FDA "breakthrough" status after several patients were able to forgo the frequent blood transfusions usually required to treat the disease.
In March researchers delivered a recombinant gene encoding a broadly neutralizing antibody into monkeys infected with simian HIV; the monkeys' cells produced the antibody, which cleared them of HIV. The technique is named immunoprophylaxis by gene transfer (IGT). Animal tests for antibodies to ebola, malaria, influenza, and hepatitis were underway.
In March, scientists, including an inventor of CRISPR, Jennifer Doudna, urged a worldwide moratorium on germline gene therapy, writing "scientists should avoid even attempting, in lax jurisdictions, germline genome modification for clinical application in humans" until the full implications "are discussed among scientific and governmental organizations".
In December, scientists of major world academies called for a moratorium on inheritable human genome edits, including those related to CRISPR-Cas9 technologies but that basic research including embryo gene editing should continue.
2015
Researchers successfully treated a boy with epidermolysis bullosa using skin grafts grown from his own skin cells, genetically altered to repair the mutation that caused his disease.
In November, researchers announced that they had treated a baby girl, Layla Richards, with an experimental treatment using donor T cells genetically engineered using TALEN to attack cancer cells. One year after the treatment she was still free of her cancer (a highly aggressive form of acute lymphoblastic leukaemia ). Children with highly aggressive ALL normally have a very poor prognosis and Layla's disease had been regarded as terminal before the treatment.
2016
In April the Committee for Medicinal Products for Human Use of the European Medicines Agency endorsed a gene therapy treatment called Strimvelis and the European Commission approved it in June. This treats children born with adenosine deaminase deficiency and who have no functioning immune system. This was the second gene therapy treatment to be approved in Europe.
In October, Chinese scientists reported they had started a trial to genetically modify T cells from 10 adult patients with lung cancer and reinject the modified T cells back into their bodies to attack the cancer cells. The T cells had the PD-1 protein (which stops or slows the immune response) removed using CRISPR-Cas9.
A 2016 Cochrane systematic review looking at data from four trials on topical cystic fibrosis transmembrane conductance regulator (CFTR) gene therapy does not support its clinical use as a mist inhaled into the lungs to treat cystic fibrosis patients with lung infections. One of the four trials did find weak evidence that liposome-based CFTR gene transfer therapy may lead to a small respiratory improvement for people with CF. This weak evidence is not enough to make a clinical recommendation for routine CFTR gene therapy.
2017
In February Kite Pharma announced results from a clinical trial of CAR-T cells in around a hundred people with advanced non-Hodgkin lymphoma.
In March, French scientists reported on clinical research of gene therapy to treat sickle cell disease.
In August, the FDA approved tisagenlecleucel for acute lymphoblastic leukemia. Tisagenlecleucel is an adoptive cell transfer therapy for B-cell acute lymphoblastic leukemia; T cells from a person with cancer are removed, genetically engineered to make a specific T-cell receptor (a chimeric T cell receptor, or "CAR-T") that reacts to the cancer, and are administered back to the person. The T cells are engineered to target a protein called CD19 that is common on B cells. This is the first form of gene therapy to be approved in the United States. In October, a similar therapy called axicabtagene ciloleucel was approved for non-Hodgkin lymphoma.
In October, biophysicist and biohacker Josiah Zayner claimed to have performed the very first in-vivo human genome editing in the form of a self-administered therapy.
On 13 November, medical scientists working with Sangamo Therapeutics, headquartered in Richmond, California, announced the first ever in-body human gene editing therapy. The treatment, designed to permanently insert a healthy version of the flawed gene that causes Hunter syndrome, was given to 44-year-old Brian Madeux and is part of the world's first study to permanently edit DNA inside the human body. The success of the gene insertion was later confirmed. Clinical trials by Sangamo involving gene editing using zinc finger nuclease (ZFN) are ongoing.
In December the results of using an adeno-associated virus with blood clotting factor VIII to treat nine haemophilia A patients were published. Six of the seven patients on the high dose regime increased the level of the blood clotting VIII to normal levels. The low and medium dose regimes had no effect on the patient's blood clotting levels.
In December, the FDA approved voretigene neparvovec, the first in vivo gene therapy, for the treatment of blindness due to Leber's congenital amaurosis. The price of this treatment is US$850,000 for both eyes.
2019
In May, the FDA approved onasemnogene abeparvovec (Zolgensma) for treating spinal muscular atrophy in children under two years of age. The list price of Zolgensma was set at US$2.125 million per dose, making it the most expensive drug ever.
In May, the EMA approved betibeglogene autotemcel (Zynteglo) for treating beta thalassemia for people twelve years of age and older.
In July, Allergan and Editas Medicine announced phase I/II clinical trial of AGN-151587 for the treatment of Leber congenital amaurosis 10. This is one of the first studies of a CRISPR-based in vivo human gene editing therapy, where the editing takes place inside the human body. The first injection of the CRISPR-Cas System was confirmed in March 2020.
Exagamglogene autotemcel, a CRISPR-based human gene editing therapy, was used for sickle cell and thalassemia in clinical trials.
2020s
2020
In May, onasemnogene abeparvovec (Zolgensma) was approved by the European Union for the treatment of spinal muscular atrophy in people who either have clinical symptoms of SMA type 1 or who have no more than three copies of the SMN2 gene, irrespective of body weight or age.
In August, Audentes Therapeutics reported that three out of 17 children with X-linked myotubular myopathy participating the clinical trial of a AAV8-based gene therapy treatment AT132 have died. It was suggested that the treatment, whose dosage is based on body weight, exerts a disproportionately toxic effect on heavier patients, since the three patients who died were heavier than the others. The trial has been put on clinical hold.
On 15 October, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Libmeldy (autologous CD34+ cell enriched population that contains hematopoietic stem and progenitor cells transduced ex vivo using a lentiviral vector encoding the human arylsulfatase A gene), a gene therapy for the treatment of children with the "late infantile" (LI) or "early juvenile" (EJ) forms of metachromatic leukodystrophy (MLD). The active substance of Libmeldy consists of the child's own stem cells which have been modified to contain working copies of the ARSA gene. When the modified cells are injected back into the patient as a one-time infusion, the cells are expected to start producing the ARSA enzyme that breaks down the build-up of sulfatides in the nerve cells and other cells of the patient's body. Libmeldy was approved for medical use in the EU in December 2020.
On 15 October, Lysogene, a French biotechnological company, reported the death of a patient in who has received LYS-SAF302, an experimental gene therapy treatment for mucopolysaccharidosis type IIIA (Sanfilippo syndrome type A).
2021
In May, a new method using an altered version of HIV as a lentivirus vector was reported in the treatment of 50 children with ADA-SCID obtaining positive results in 48 of them, this method is expected to be safer than retroviruses vectors commonly used in previous studies of SCID where the development of leukemia was usually observed and had already been used in 2019, but in a smaller group with X-SCID.
In June a clinical trial on six patients affected with transthyretin amyloidosis reported a reduction the concentration of missfolded transthretin (TTR) protein in serum through CRISPR-based inactivation of the TTR gene in liver cells observing mean reductions of 52% and 87% among the lower and higher dose groups.This was done in vivo without taking cells out of the patient to edit them and reinfuse them later.
In July results of a small gene therapy phase I study was published reporting observation of dopamine restoration on seven patients between 4 and 9 years old affected by aromatic L-amino acid decarboxylase deficiency (AADC deficiency).
2022
In February, the first ever gene therapy for Tay–Sachs disease was announced, it uses an adeno-associated virus to deliver the correct instruction for the HEXA gene on brain cells which causes the disease. Only two children were part of a compassionate trial presenting improvements over the natural course of the disease and no vector-related adverse events.
In May, eladocagene exuparvovec is recommended for approval by the European Commission.
In July results of a gene therapy candidate for haemophilia B called FLT180 were announced, it works using an adeno-associated virus (AAV) to restore the clotting factor IX (FIX) protein, normal levels of the protein were observed with low doses of the therapy but immunosuppression was necessitated to decrease the risk of vector-related immune responses.
In December, a 13-year girl that had been diagnosed with T-cell acute lymphoblastic leukaemia was successfully treated at Great Ormond Street Hospital (GOSH) in the first documented use of therapeutic gene editing for this purpose, after undergoing six months of an experimental treatment, where all attempts of other treatments failed. The procedure included reprogramming a healthy T-cell to destroy the cancerous T-cells to first rid her of leukaemia, and then rebuilding her immune system using healthy immune cells. The GOSH team used BASE editing and had previously treated a case of acute lymphoblastic leukaemia in 2015 using TALENs.
2023
In May 2023, the FDA approved beremagene geperpavec for the treatment of wounds in people with dystrophic epidermolysis bullosa (DEB) which is applied as a topical gel that delivers a herpes-simplex virus type 1 (HSV-1) vector encoding the collagen type VII alpha 1 chain (COL7A1) gene that is dysfunctional on those affected by DEB . One trial found 65% of the Vyjuvek-treated wounds completely closed while only 26% of the placebo-treated at 24 weeks. It has been also reported its use as an eyedrop for a patient with DEB that had vision loss due to the widespread blistering with good results.
In June 2023, the FDA gave an accelerated approval to Elevidys for Duchenne muscular dystrophy (DMD) only for boys 4 to 5 years old as they are more likely to benefit from the therapy which consists of one-time intravenous infusion of a virus (AAV rh74 vector) that delivers a functioning "microdystrophin" gene (138 kDa) into the muscle cells to act in place of the normal dystrophin (427 kDa) that is found mutated in this disease.
In July 2023, it was reported that it had been developed a new method to affect genetic expressions through direct current.
In December 2023, two gene therapies were approved for sickle cell disease, exagamglogene autotemcel and lovotibeglogene autotemcel.
2024
In November 2024, FDA granted accelerated approval for eladocagene exuparvovec-tneq (Kebilidi, PTC Therapeutics), a direct-to-brain gene therapy for aromatic L-amino acid decarboxylase deficiency. It uses a recombinant adeno-associated virus serotype 2 (rAAV2) to deliver a functioning DOPA decarboxylase (DDC) gene directly into the putamen, increasing the AADC enzyme and restoring dopamine production. It is administered through a stereotactic surgical procedure.
List of gene therapies
- Gene therapy for color blindness
- Gene therapy for epilepsy
- Gene therapy for osteoarthritis
- Gene therapy in Parkinson's disease
- Gene therapy of the human retina
- List of gene therapies
References
- Kaji EH, Leiden JM (February 2001). "Gene and stem cell therapies". JAMA. 285 (5): 545–550. doi:10.1001/jama.285.5.545. PMID 11176856.
- Ermak G (2015). Emerging Medical Technologies. World Scientific. ISBN 978-981-4675-81-9.
- "What is Gene Therapy?". U.S. Food and Drug Administration (FDA). 9 December 2020.
- Rosenberg SA, Aebersold P, Cornetta K, Kasid A, Morgan RA, Moen R, et al. (August 1990). "Gene transfer into humans--immunotherapy of patients with advanced melanoma, using tumor-infiltrating lymphocytes modified by retroviral gene transduction". The New England Journal of Medicine. 323 (9): 570–578. doi:10.1056/NEJM199008303230904. PMID 2381442.
- ^ "Gene Therapy Clinical Trials Worldwide Database". The Journal of Gene Medicine. Wiley. June 2016. Archived from the original on 31 July 2020.
- Gorell E, Nguyen N, Lane A, Siprashvili Z (April 2014). "Gene therapy for skin diseases". Cold Spring Harbor Perspectives in Medicine. 4 (4): a015149. doi:10.1101/cshperspect.a015149. PMC 3968787. PMID 24692191.
- Zimmer C (16 September 2013). "DNA Double Take". The New York Times. Archived from the original on 2 January 2022.
- "Lorraine Kraus Obituary". The Commercial Appeal. Retrieved 7 July 2023.
- "Gene therapy". WhatIsBiotechnology.org. The Biotechnology and Medicine Education Trust (Biotechmet). Retrieved 7 July 2023.
- U.S. Congress, Office of Technology Assessment (December 1984). Human gene therapy – A background paper. DIANE Publishing. ISBN 978-1-4289-2371-3.
- Sun M (October 1982). "Martin Cline loses appeal on NIH grant". Science. 218 (4567): 37. Bibcode:1982Sci...218...37S. doi:10.1126/science.7123214. PMID 7123214.
- Lowenstein PR (2008). "Gene Therapy for Neurological Disorders: New Therapies or Human Experimentation?". In Burley J, Harris J (eds.). A Companion to Genethics. John Wiley & Sons. ISBN 978-0-470-75637-9.
- ^ Sheridan C (February 2011). "Gene therapy finds its niche". Nature Biotechnology. 29 (2): 121–128. doi:10.1038/nbt.1769. PMID 21301435. S2CID 5063701.
- O'Malley BW, Ledley FD (October 1993). "Somatic gene therapy. Methods for the present and future". Arch Otolaryngol Head Neck Surg. 119 (10): 1100–7. doi:10.1001/archotol.1993.01880220044007. PMID 8398061.
- Oldfield EH, Ram Z, Culver KW, Blaese RM, DeVroom HL, Anderson WF (February 1993). "Gene therapy for the treatment of brain tumors using intra-tumoral transduction with the thymidine kinase gene and intravenous ganciclovir". Human Gene Therapy. 4 (1): 39–69. doi:10.1089/hum.1993.4.1-39. PMID 8384892.
- ^ Richards S (6 November 2012). "Gene Therapy Arrives in Europe". The Scientist.
- ^ Maguire AM, Simonelli F, Pierce EA, Pugh EN, Mingozzi F, Bennicelli J, et al. (May 2008). "Safety and efficacy of gene transfer for Leber's congenital amaurosis". The New England Journal of Medicine. 358 (21): 2240–2248. doi:10.1056/NEJMoa0802315. PMC 2829748. PMID 18441370.
- ^ Simonelli F, Maguire AM, Testa F, Pierce EA, Mingozzi F, Bennicelli JL, et al. (March 2010). "Gene therapy for Leber's congenital amaurosis is safe and effective through 1.5 years after vector administration". Molecular Therapy. 18 (3): 643–650. doi:10.1038/mt.2009.277. PMC 2839440. PMID 19953081.
- ^ Cideciyan AV, Hauswirth WW, Aleman TS, Kaushal S, Schwartz SB, Boye SL, Windsor EA, Conlon TJ, Sumaroka A, Roman AJ, Byrne BJ, Jacobson SG (August 2009). "Vision 1 year after gene therapy for Leber's congenital amaurosis". The New England Journal of Medicine. 361 (7): 725–727. doi:10.1056/NEJMc0903652. PMC 2847775. PMID 19675341.
- ^ Bainbridge JW, Smith AJ, Barker SS, Robbie S, Henderson R, Balaggan K, et al. (May 2008). "Effect of gene therapy on visual function in Leber's congenital amaurosis". The New England Journal of Medicine. 358 (21): 2231–2239. doi:10.1056/NEJMoa0802268. hdl:10261/271174. PMID 18441371.
- ^ Ghosh P (28 April 2016). "Gene therapy reverses sight loss and is long-lasting". BBC News Online. Retrieved 29 April 2016.
- Fischer A, Hacein-Bey-Abina S, Cavazzana-Calvo M (June 2010). "20 years of gene therapy for SCID". Nature Immunology. 11 (6): 457–460. doi:10.1038/ni0610-457. PMID 20485269. S2CID 11300348.
- Ferrua F, Brigida I, Aiuti A (December 2010). "Update on gene therapy for adenosine deaminase-deficient severe combined immunodeficiency". Current Opinion in Allergy and Clinical Immunology. 10 (6): 551–556. doi:10.1097/ACI.0b013e32833fea85. PMID 20966749. S2CID 205435278.
- ^ Geddes L (30 October 2013). "'Bubble kid' success puts gene therapy back on track". New Scientist. Retrieved 2 January 2022.
- Cartier N, Aubourg P (July 2010). "Hematopoietic stem cell transplantation and hematopoietic stem cell gene therapy in X-linked adrenoleukodystrophy". Brain Pathology. 20 (4): 857–862. doi:10.1111/j.1750-3639.2010.00394.x. PMC 8094635. PMID 20626747. S2CID 24182017.
- ^ Ledford H (2011). "Cell therapy fights leukaemia". Nature. doi:10.1038/news.2011.472.
- ^ Coghlan A (26 March 2013). "Gene therapy cures leukaemia in eight days". The New Scientist. Retrieved 15 April 2013.
- ^ Coghlan A (11 December 2013). "Souped-up immune cells force leukaemia into remission". New Scientist. Retrieved 15 April 2013.
- LeWitt PA, Rezai AR, Leehey MA, Ojemann SG, Flaherty AW, Eskandar EN, et al. (April 2011). "AAV2-GAD gene therapy for advanced Parkinson's disease: a double-blind, sham-surgery controlled, randomised trial". The Lancet. Neurology. 10 (4): 309–319. doi:10.1016/S1474-4422(11)70039-4. PMID 21419704. S2CID 37154043.
- Herper M (26 March 2014). "Gene Therapy's Big Comeback". Forbes. Retrieved 28 April 2014.
- ^ Pearson S, Jia H, Kandachi K (January 2004). "China approves first gene therapy". Nature Biotechnology. 22 (1): 3–4. doi:10.1038/nbt0104-3. PMC 7097065. PMID 14704685.
- ^ "Gene Therapy for PAD Approved". 6 December 2011. Retrieved 5 August 2015.
- ^ Gallagher J (2 November 2012). "Gene therapy: Glybera approved by European Commission". BBC News. Retrieved 15 December 2012.
- "What is gene therapy?". Genetics Home Reference. 28 March 2016. Archived from the original on 6 April 2016. Retrieved 2 January 2022.
- "How does gene therapy work?". Genomics Home Reference. U.S. National Library of Medicine.
- Pezzoli D, Chiesa R, De Nardo L, Candiani G (September 2012). "We still have a long way to go to effectively deliver genes!". Journal of Applied Biomaterials & Functional Materials. 10 (2): 82–91. doi:10.5301/JABFM.2012.9707. PMID 23015375. S2CID 6283455.
- Vannucci L, Lai M, Chiuppesi F, Ceccherini-Nelli L, Pistello M (January 2013). "Viral vectors: a look back and ahead on gene transfer technology". The New Microbiologica. 36 (1): 1–22. PMID 23435812.
- Gothelf A, Gehl J (November 2012). "What you always needed to know about electroporation based DNA vaccines". Human Vaccines & Immunotherapeutics. 8 (11): 1694–1702. doi:10.4161/hv.22062. PMC 3601144. PMID 23111168.
- Urnov FD, Rebar EJ, Holmes MC, Zhang HS, Gregory PD (September 2010). "Genome editing with engineered zinc finger nucleases". Nature Reviews Genetics. 11 (9): 636–646. doi:10.1038/nrg2842. PMID 20717154. S2CID 205484701.
- ^ Bak RO, Gomez-Ospina N, Porteus MH (August 2018). "Gene Editing on Center Stage". Trends in Genetics. 34 (8): 600–611. doi:10.1016/j.tig.2018.05.004. PMID 29908711. S2CID 49269023.
- Stone D, Niyonzima N, Jerome KR (September 2016). "Genome editing and the next generation of antiviral therapy". Human Genetics. 135 (9): 1071–82. doi:10.1007/s00439-016-1686-2. PMC 5002242. PMID 27272125.
- Cross D, Burmester JK (September 2006). "Gene therapy for cancer treatment: past, present and future". Clinical Medicine & Research. 4 (3): 218–27. doi:10.3121/cmr.4.3.218. PMC 1570487. PMID 16988102.
- Maeder ML, Gersbach CA (March 2016). "Genome-editing Technologies for Gene and Cell Therapy". Molecular Therapy. 24 (3): 430–46. doi:10.1038/mt.2016.10. PMC 4786923. PMID 26755333.
- "Tests suggest scientists achieved 1st 'in body' gene editing". AP NEWS. 7 February 2019. Retrieved 17 November 2020.
- "First CRISPR therapy dosed". Nature Biotechnology. 38 (4): 382. 1 April 2020. doi:10.1038/s41587-020-0493-4. ISSN 1546-1696. PMID 32265555. S2CID 215406440.
- ^ Sherkow JS, Zettler PJ, Greely HT (December 2018). "Is it 'gene therapy'?". Journal of Law and the Biosciences. 5 (3): 786–793. doi:10.1093/jlb/lsy020. PMC 6534757. PMID 31143463.
- Asaleh A, Zhou J, Rahmanian N (November 2022). "Letter to the Editor: A Lesson for the Future-How Semantic Ambiguity Led to the Spread of Anti-Scientific Attitudes About COVID-19 mRNA Vaccines". Human Gene Therapy. 33 (21–22): 1213–1216. doi:10.1089/hum.2022.29223.aas (inactive 1 November 2024). PMID 36375123.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - "Andrew Bridgen wrong to call mRNA vaccines gene therapy". Full Fact. 12 January 2023. Retrieved 19 February 2023.
- "Fact Check-mRNA vaccines are distinct from gene therapy, which alters recipient's genes". Reuters. 10 August 2021. Retrieved 19 February 2023.
- "Joe Rogan falsely says mRNA vaccines are 'gene therapy'". PolitiFact. Retrieved 19 February 2023.
- Spencer SH (28 June 2022). "Website Peddles Old, Debunked Falsehood About COVID-19 mRNA Vaccines". FactCheck.org. Retrieved 19 February 2023.
- "These experts say Joe Rogan is 'extraordinarily dangerous' to society – here's why". The Independent. 2 February 2022. Retrieved 19 February 2023.
- "Andrew Bridgen MP's false claims put lives at risk". Full Fact. 11 January 2023. Retrieved 19 February 2023.
- ^ Nóbrega C, Mendonça L, Matos CA (2020). A handbook of gene and cell therapy. Cham: Springer. ISBN 978-3-030-41333-0. OCLC 1163431307.
- Williams DA, Orkin SH (April 1986). "Somatic gene therapy. Current status and future prospects". The Journal of Clinical Investigation. 77 (4): 1053–6. doi:10.1172/JCI112403. PMC 424438. PMID 3514670.
- Mavilio F, Ferrari G (July 2008). "Genetic modification of somatic stem cells. The progress, problems and prospects of a new therapeutic technology". EMBO Reports. 9 (Suppl 1): S64–69. doi:10.1038/embor.2008.81. PMC 3327547. PMID 18578029.
- ^ "International Law". The Genetics and Public Policy Center, Johns Hopkins University Berman Institute of Bioethics. 2010. Archived from the original on 2 September 2014.
- Strachnan T, Read AP (2004). Human Molecular Genetics (3rd ed.). Garland Publishing. p. 616. ISBN 978-0-8153-4184-0.
- Hanna K (2006). "Germline Gene Transfer". National Human Genome Research Institute.
- "Human Cloning and Genetic Modification". Association of Reproductive Health Officials. 2013. Archived from the original on 18 June 2013.
- "Gene Therapy". ama-assn.org. 4 April 2014. Archived from the original on 15 March 2015. Retrieved 22 March 2015.
- "Gene & Cell Therapy FAQs | ASGCT - American Society of Gene & Cell Therapy | ASGCT - American Society of Gene & Cell Therapy". asgct.org. Retrieved 23 July 2021.
- "Evaluation of the Clinical Success of Ex Vivo and In Vivo Gene Therapy". Journal of Young Investigators. January 2009. Retrieved 23 July 2021.
- "Challenges In Gene Therapy". learn.genetics.utah.edu. Retrieved 23 July 2021.
- Mullard A (June 2020). "Gene-editing pipeline takes off". Nature Reviews. Drug Discovery. 19 (6): 367–372. doi:10.1038/d41573-020-00096-y. PMID 32415249. S2CID 218657910.
- ^ MacLaren RE, Groppe M, Barnard AR, Cottriall CL, Tolmachova T, Seymour L, Clark KR, During MJ, Cremers FP, Black GC, Lotery AJ, Downes SM, Webster AR, Seabra MC (March 2014). "Retinal gene therapy in patients with choroideremia: initial findings from a phase 1/2 clinical trial". Lancet. 383 (9923): 1129–1137. doi:10.1016/S0140-6736(13)62117-0. PMC 4171740. PMID 24439297.
- Dever DP, Bak RO, Reinisch A, Camarena J, Washington G, Nicolas CE, et al. (November 2016). "CRISPR/Cas9 β-globin gene targeting in human haematopoietic stem cells". Nature. 539 (7629): 384–389. Bibcode:2016Natur.539..384D. doi:10.1038/nature20134. PMC 5898607. PMID 27820943.
- Gupta RM, Musunuru K (October 2014). "Expanding the genetic editing tool kit: ZFNs, TALENs, and CRISPR-Cas9". The Journal of Clinical Investigation. 124 (10): 4154–61. doi:10.1172/JCI72992. PMC 4191047. PMID 25271723.
- Sanches-da-Silva GN, Medeiros LF, Lima FM (21 August 2019). "The Potential Use of the CRISPR-Cas System for HIV-1 Gene Therapy". International Journal of Genomics. 2019: 8458263. doi:10.1155/2019/8458263. PMC 6721108. PMID 31531340.
- Patent: US7824869B2
- Bi A, Cui J, Ma YP, Olshevskaya E, Pu M, Dizhoor AM, Pan ZH (April 2006). "Ectopic expression of a microbial-type rhodopsin restores visual responses in mice with photoreceptor degeneration". Neuron. 50 (1): 23–33. doi:10.1016/j.neuron.2006.02.026. PMC 1459045. PMID 16600853.
- ^ Song, Xiangrong; Liu, Chao; Wang, Ning; Huang, Hai; He, Siyan; Gong, Changyang; Wei, Yuquan (1 January 2021). "Delivery of CRISPR/Cas systems for cancer gene therapy and immunotherapy". Advanced Drug Delivery Reviews. Delivery of Biomacromolecules for Therapeutic Genome Editing. 168: 158–180. doi:10.1016/j.addr.2020.04.010. ISSN 0169-409X. PMID 32360576. S2CID 218493473.
- Nayerossadat N, Maedeh T, Ali PA (2012). "Viral and nonviral delivery systems for gene delivery". Advanced Biomedical Research. 1 (1): 27. doi:10.4103/2277-9175.98152. PMC 3507026. PMID 23210086.
- ^ Ginn SL, Amaya AK, Alexander IE, Edelstein M, Abedi MR (May 2018). "Gene therapy clinical trials worldwide to 2017: An update". The Journal of Gene Medicine. 20 (5): e3015. doi:10.1002/jgm.3015. PMID 29575374. S2CID 4966300.
- ^ Bulcha JT, Wang Y, Ma H, Tai PW, Gao G (February 2021). "Viral vector platforms within the gene therapy landscape". Signal Transduction and Targeted Therapy. 6 (1): 53. doi:10.1038/s41392-021-00487-6. PMC 7868676. PMID 33558455.
- Jensen, Thomas Leth; Gøtzsche, Casper René; Woldbye, David P. D. (2021). "Current and Future Prospects for Gene Therapy for Rare Genetic Diseases Affecting the Brain and Spinal Cord". Frontiers in Molecular Neuroscience. 14: 695937. doi:10.3389/fnmol.2021.695937. ISSN 1662-5099. PMC 8527017. PMID 34690692.
- Manini A, Abati E, Nuredini A, Corti S, Comi GP (2022). "Adeno-Associated Virus (AAV)-Mediated Gene Therapy for Duchenne Muscular Dystrophy: The Issue of Transgene Persistence". Frontiers in Neurology. 12: 814174. doi:10.3389/fneur.2021.814174. PMC 8797140. PMID 35095747.
- ^ Sabatino DE, Bushman FD, Chandler RJ, Crystal RG, Davidson BL, Dolmetsch R, et al. (August 2022). "Evaluating the state of the science for adeno-associated virus integration: An integrated perspective". Molecular Therapy. 30 (8): 2646–2663. doi:10.1016/j.ymthe.2022.06.004. PMC 9372310. PMID 35690906.
- Campochiaro, P. A.; Avery, R.; Brown, D. M.; Heier, J. S.; Ho, A. C.; Huddleston, S. M.; Jaffe, G. J.; Khanani, A. M.; Pakola, S.; Pieramici, D. J.; Wykoff, C. C.; Van Everen, S. (2024). "Gene therapy for neovascular age-related macular degeneration by subretinal delivery of RGX-314: a phase 1/2a dose-escalation study". Lancet. 403 (10436): 1563–1573. doi:10.1016/S0140-6736(24)00310-6. PMID 38554726.
- Khanani, A. M.; Boyer, D. S.; Wykoff, C. C.; Regillo, C. D.; Busbee, B. G.; Pieramici, D.; Danzig, C. J.; Joondeph, B. C.; Major Jr, J. C.; Turpcu, A.; Kiss, S. (2024). "Safety and efficacy of ixoberogene soroparvovec in neovascular age-related macular degeneration in the United States (OPTIC): a prospective, two-year, multicentre phase 1 study". eClinicalMedicine. 67. doi:10.1016/j.eclinm.2023.102394. PMC 10751837. PMID 38152412.
- Yin H, Kanasty RL, Eltoukhy AA, Vegas AJ, Dorkin JR, Anderson DG (August 2014). "Non-viral vectors for gene-based therapy". Nature Reviews. Genetics. 15 (8): 541–555. doi:10.1038/nrg3763. PMID 25022906. S2CID 15273455.
- Krasilnikova, O.; Yakimova, A.; Ivanov, S.; Atiakshin, D.; Kostin, A.A.; Sosin, D.; Shegay, P.; Kaprin, A.D.; Klabukov, I. (2023). "Gene-Activated Materials in Regenerative Dentistry: Narrative Review of Technology and Study Results". International Journal of Molecular Sciences. 24 (22): 16250. doi:10.3390/ijms242216250. ISSN 1422-0067. PMC 10671237. PMID 38003439.
- Foldvari, M.; Chen, D.W.; Nafissi, N.; Calderon, D.; Narsineni, L.; Rafiee, A. (2016). "Non-viral gene therapy: Gains and challenges of non-invasive administration methods". Journal of Controlled Release. 240: 165–190. doi:10.1016/j.jconrel.2015.12.012. ISSN 1873-4995. PMID 26686079.
- Bertrand N, Grenier P, Mahmoudi M, Lima EM, Appel EA, Dormont F, et al. (October 2017). "Mechanistic understanding of in vivo protein corona formation on polymeric nanoparticles and impact on pharmacokinetics". Nature Communications. 8 (1): 777. Bibcode:2017NatCo...8..777B. doi:10.1038/s41467-017-00600-w. PMC 5626760. PMID 28974673.
- ^ Goswami R, Subramanian G, Silayeva L, Newkirk I, Doctor D, Chawla K, et al. (24 April 2019). "Gene Therapy Leaves a Vicious Cycle". Frontiers in Oncology. 9: 297. doi:10.3389/fonc.2019.00297. PMC 6491712. PMID 31069169.
- Wirth T, Parker N, Ylä-Herttuala S (August 2013). "History of gene therapy". Gene. 525 (2): 162–169. doi:10.1016/j.gene.2013.03.137. PMID 23618815.
- Singh V, Khan N, Jayandharan GR (May 2022). "Vector engineering, strategies and targets in cancer gene therapy". Cancer Gene Therapy. 29 (5): 402–417. doi:10.1038/s41417-021-00331-7. PMID 33859378. S2CID 233258994.
- Anguela XM, High KA (January 2019). "Entering the Modern Era of Gene Therapy". Annual Review of Medicine. 70 (1): 273–288. doi:10.1146/annurev-med-012017-043332. PMID 30477394. S2CID 53750215.
- Wang Y, Zhang R, Tang L, Yang L (February 2022). "Nonviral Delivery Systems of mRNA Vaccines for Cancer Gene Therapy". Pharmaceutics. 14 (3): 512. doi:10.3390/pharmaceutics14030512. PMC 8949480. PMID 35335891.
- ^ "FDA grants accelerated approval to afamitresgene autoleucel for unresectable or metastatic synovial sarcoma". U.S. Food and Drug Administration (FDA). 2 August 2024. Retrieved 19 September 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "FDA Approves First T-Cell Receptor Gene Therapy For Solid Tumors". AABB News & Resources. 6 August 2024. Retrieved 19 September 2024.
- Monga I, Qureshi A, Thakur N, Gupta AK, Kumar M (September 2017). "ASPsiRNA: A Resource of ASP-siRNAs Having Therapeutic Potential for Human Genetic Disorders and Algorithm for Prediction of Their Inhibitory Efficacy". G3. 7 (9): 2931–2943. doi:10.1534/g3.117.044024. PMC 5592921. PMID 28696921.
- ^ Olowoyeye A, Okwundu CI (November 2020). "Gene therapy for sickle cell disease". The Cochrane Database of Systematic Reviews. 2020 (11): CD007652. doi:10.1002/14651858.CD007652.pub7. PMC 8275984. PMID 33251574.
- Chen W, Hu Y, Ju D (August 2020). "Gene therapy for neurodegenerative disorders: advances, insights and prospects". Acta Pharmaceutica Sinica B. 10 (8): 1347–1359. doi:10.1016/j.apsb.2020.01.015. PMC 7488363. PMID 32963936.
- "FDA Approves First Gene Therapy for Children with Metachromatic Leukodystrophy". U.S. Food and Drug Administration (FDA) (Press release). 9 August 2024.
- "Orchard Therapeutics Receives EC Approval for Libmeldy for the Treatment of Early-Onset Metachromatic Leukodystrophy (MLD)" (Press release). Orchard Therapeutics. 21 December 2020. Retrieved 23 July 2021 – via GlobeNewswire.
- ^ "FDA Approves First Topical Gene Therapy for Treatment of Wounds in Patients with Dystrophic Epidermolysis Bullosa". U.S. Food and Drug Administration (FDA) (Press release). 19 May 2023. Retrieved 31 July 2023.
- "FDA Approves First Cell-Based Gene Therapy to Treat Adult and Pediatric Patients with Beta-thalassemia Who Require Regular Blood Transfusions". U.S. Food and Drug Administration (FDA) (Press release). 17 August 2022. Retrieved 31 August 2022.
- "FDA Approves First Cell-Based Gene Therapy For Adult Patients with Relapsed or Refractory MCL". U.S. Food and Drug Administration (FDA) (Press release). 24 July 2020. Retrieved 24 July 2020.
- "FDA approves brexucabtagene autoleucel for relapsed or refractory B-cell precursor acute lymphoblastic leukemia". U.S. Food and Drug Administration (FDA). 1 October 2021. Retrieved 2 October 2021.
- "Tecartus". European Medicines Agency. 13 October 2020.
- ^ "FDA Approves First Gene Therapy for Treatment of Certain Patients with Duchenne Muscular Dystrophy". U.S. Food and Drug Administration (FDA) (Press release). 23 June 2023. Retrieved 12 July 2023.
- ^ "FDA Approves First Gene Therapy for Treatment of Aromatic L-amino Acid Decarboxylase Deficiency". U.S. Food and Drug Administration (FDA) (Press release). 14 November 2024. Retrieved 17 November 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "Upstaza EPAR". European Medicines Agency (EMA). 13 April 2022. Archived from the original on 14 March 2023. Retrieved 3 March 2023. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ "Casgevy". U.S. Food and Drug Administration (FDA). 8 December 2023. Retrieved 8 December 2023.
- "Abecma (idecabtagene vicleucel)". U.S. Food and Drug Administration (FDA). 21 April 2021.
- "Breyanzi (lisocabtagene maraleucel)". U.S. Food and Drug Administration (FDA). 4 March 2021.
- ^ "Lyfgenia". U.S. Food and Drug Administration (FDA). 8 December 2023. Archived from the original on 8 December 2023. Retrieved 9 December 2023.
- "FDA Approves First Gene Therapy for the Treatment of High-Risk, Non-Muscle-Invasive Bladder Cancer". U.S. Food and Drug Administration (FDA) (Press release). 16 December 2022. Retrieved 16 December 2022.
- "FDA approves obecabtagene autoleucel for acute lymphoblastic leukemia". U.S. Food and Drug Administration (FDA). 8 November 2024. Retrieved 10 November 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "Autolus Therapeutics Announces FDA Approval of Aucatzyl (obecabtagene autoleucel – obe-cel) for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (r/r B-ALL)" (Press release). Autolus Therapeutics. 8 November 2024. Retrieved 10 November 2024 – via GlobeNewswire.
- "Zolgensma". U.S. Food and Drug Administration (FDA). 16 March 2021.
- "EMA-approved application for Zolgensma". Aetion (Press release). Retrieved 23 July 2021.
- "FDA Approves T-VEC to Treat Metastatic Melanoma". National Cancer Institute. 25 November 2015. Retrieved 23 July 2021.
- "Imlygic". European Medicines Agency (EMA). 17 September 2018.
- "First gene therapy to treat severe haemophilia A". European Medicines Agency (EMA) (Press release). 24 June 2022. Archived from the original on 26 June 2022. Retrieved 26 June 2022.
- "Roctavian: Pending EC decision". European Medicines Agency (EMA). 23 June 2022. Archived from the original on 26 June 2022. Retrieved 26 June 2022.
- "Roctavian". Union Register of medicinal products. 25 August 2022. Retrieved 6 September 2022.
- "FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss". U.S. Food and Drug Administration (FDA) (Press release). 24 March 2020. Retrieved 23 July 2021.
- "Luxturna". European Medicines Agency (EMA). 24 September 2018.
- Guo, Congting; Ma, Xiaoteng; Gao, Fei; Guo, Yuxuan (9 March 2023). "Off-target effects in CRISPR/Cas9 gene editing". Frontiers in Bioengineering and Biotechnology. 11: 1143157. doi:10.3389/fbioe.2023.1143157. ISSN 2296-4185. PMC 10034092. PMID 36970624.
- Wu, Shao-Shuai; Li, Qing-Cui; Yin, Chang-Qing; Xue, Wen; Song, Chun-Qing (15 March 2020). "Advances in CRISPR/Cas-based Gene Therapy in Human Genetic Diseases". Theranostics. 10 (10): 4374–4382. doi:10.7150/thno.43360. ISSN 1838-7640. PMC 7150498. PMID 32292501.
- Korthof G. "The implications of Steele's soma-to-germline feedback for human gene therapy".
- Woods NB, Bottero V, Schmidt M, von Kalle C, Verma IM (April 2006). "Gene therapy: therapeutic gene causing lymphoma". Nature. 440 (7088): 1123. Bibcode:2006Natur.440.1123W. doi:10.1038/4401123a. PMID 16641981. S2CID 4372110.
- Thrasher AJ, Gaspar HB, Baum C, Modlich U, Schambach A, Candotti F, et al. (September 2006). "Gene therapy: X-SCID transgene leukaemogenicity". Nature. 443 (7109): E5-6, discussion E6-7. Bibcode:2006Natur.443E...5T. doi:10.1038/nature05219. PMID 16988659. S2CID 4301764.
- Bak RO, Porteus MH (July 2017). "CRISPR-Mediated Integration of Large Gene Cassettes Using AAV Donor Vectors". Cell Reports. 20 (3): 750–756. doi:10.1016/j.celrep.2017.06.064. PMC 5568673. PMID 28723575.
- Rojahn SY (11 February 2014). "Genome Surgery". MIT Technology Review. Archived from the original on 15 February 2014. Retrieved 17 February 2014.
- "Gene therapy needs a hero to live up to the hype". New Scientist. 30 October 2013. Retrieved 2 January 2022.
- Crasto AM (7 July 2013). "Glybera – The Most Expensive Drug in the world & First Approved Gene Therapy in the West". All About Drugs. Retrieved 2 November 2013.
- "Gene Therapy". Oak Ridge National Laboratory. 20 December 2012. Archived from the original on 20 December 2012. Retrieved 2 January 2022.
- Raper SE, Chirmule N, Lee FS, Wivel NA, Bagg A, Gao GP, et al. (September 2003). "Fatal systemic inflammatory response syndrome in a ornithine transcarbamylase deficient patient following adenoviral gene transfer". Molecular Genetics and Metabolism. 80 (1–2): 148–58. doi:10.1016/j.ymgme.2003.08.016. PMID 14567964.
- Frank KM, Hogarth DK, Miller JL, Mandal S, Mease PJ, Samulski RJ, et al. (July 2009). "Investigation of the cause of death in a gene-therapy trial". The New England Journal of Medicine. 361 (2): 161–9. doi:10.1056/NEJMoa0801066. PMID 19587341.
- HUGO Ethics Committee (April 2001). "Statement on Gene Therapy Research" (PDF). Human Genome Organization. Archived from the original (PDF) on 7 September 2008.
- Isasi RM, Nguyen TM, Knoppers BM (October 2006). "National Regulatory Frameworks Regarding Human Genetic Modification Technologies (Somatic and Germline Modification)" (PDF). Genetics & Public Policy Center. Archived from the original (PDF) on 17 September 2014.
- "Home - NIH Genetic Testing Registry (GTR) - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2 May 2022.
- ^ "NIH Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules". U.S. National Institutes of Health. April 2016. Archived from the original on 28 May 2016.
- "Read the Belmont Report". HHS.gov. 15 January 2018. Retrieved 2 January 2022.
- U.S. Food and Drug Administration (14 October 1993). "Application of Current Statutory Authorities to Human Somatic Cell Therapy Products and Gene Therapy Products" (PDF). Federal Register. 58 (197). Archived (PDF) from the original on 21 June 2009.
- "Guidance for Industry: Guidance for Human Somatic Cell Therapy and Gene Therapy". U.S. Food and Drug Administration (FDA). 9 July 2009. Archived from the original on 9 July 2009. Retrieved 2 January 2022.
- "WADA Gene Doping". WADA. Archived from the original on 21 November 2009. Retrieved 27 September 2013.
- Kayser B, Mauron A, Miah A (March 2007). "Current anti-doping policy: a critical appraisal". BMC Medical Ethics. 8: 2. doi:10.1186/1472-6939-8-2. PMC 1851967. PMID 17394662.
- Powell R, Buchanan A (February 2011). "Breaking evolution's chains: the prospect of deliberate genetic modification in humans". The Journal of Medicine and Philosophy. 36 (1): 6–27. doi:10.1093/jmp/jhq057. PMID 21228084.
- Baylis F, Robert JS (2004). "The inevitability of genetic enhancement technologies". Bioethics. 18 (1): 1–26. doi:10.1111/j.1467-8519.2004.00376.x. PMID 15168695.
- Evans J (2002). Playing God?: Human Genetic Engineering and the Rationalization of Public Bioethical Debate. University of Chicago Press. ISBN 978-0-226-22262-2.
- "The Center for Health Ethics - University of Missouri School of Medicine - Gene Therapy and Genetic Engineering". ethics.missouri.edu. 3 December 2013. Archived from the original on 3 December 2013. Retrieved 2 January 2022.
- Roco MC, Bainbridge WS (2002). "Converging Technologies for Improving Human Performance: Integrating From the Nanoscale". Journal of Nanoparticle Research. 4 (4): 281–295. Bibcode:2002JNR.....4..281R. doi:10.1023/A:1021152023349. S2CID 136290217.
- Allhoff F (March 2005). "Germ-line genetic enhancement and Rawlsian primary goods" (PDF). Kennedy Institute of Ethics Journal. 15 (1): 39–56. CiteSeerX 10.1.1.566.171. doi:10.1353/ken.2005.0007. PMID 15881795. S2CID 14432440. Archived (PDF) from the original on 30 January 2012.
- Ranisch R (January 2020). "Special Issue:Human Germline Editing". Bioethics. 34 (1): 1–143.
- "Ethical issues related to prenatal genetic testing. The Council on Ethical and Judicial Affairs, American Medical Association". Archives of Family Medicine. 3 (7): 633–642. July 1994. doi:10.1001/archfami.3.7.633. PMID 7921302.
- "The Declaration of Inuyama: Human Genome Mapping, Genetic Screening and Gene Therapy". Council for International Organizations of Medical Sciences. Archived from the original on 5 August 2001.
- Smith KR, Chan S, Harris J (October 2012). "Human germline genetic modification: scientific and bioethical perspectives". Archives of Medical Research. 43 (7): 491–513. doi:10.1016/j.arcmed.2012.09.003. PMID 23072719.
- Reardon S (14 February 2017). "US science advisers outline path to genetically modified babies". Nature. doi:10.1038/nature.2017.21474.
- ^ Wade N (19 March 2015). "Scientists Seek Ban on Method of Editing the Human Genome". The New York Times. Archived from the original on 2 January 2022. Retrieved 20 March 2015.
- ^ Pollack A (3 March 2015). "A Powerful New Way to Edit DNA". The New York Times. Archived from the original on 2 January 2022. Retrieved 20 March 2015.
- ^ Baltimore D, Berg P, Botchan M, Carroll D, Charo RA, Church G, et al. (April 2015). "Biotechnology. A prudent path forward for genomic engineering and germline gene modification". Science. 348 (6230): 36–38. Bibcode:2015Sci...348...36B. doi:10.1126/science.aab1028. PMC 4394183. PMID 25791083.
- ^ Lanphier E, Urnov F, Haecker SE, Werner M, Smolenski J (March 2015). "Don't edit the human germ line". Nature. 519 (7544): 410–411. Bibcode:2015Natur.519..410L. doi:10.1038/519410a. PMID 25810189.
- Liang P, Xu Y, Zhang X, Ding C, Huang R, Zhang Z, et al. (May 2015). "CRISPR/Cas9-mediated gene editing in human tripronuclear zygotes". Protein & Cell. 6 (5): 363–372. doi:10.1007/s13238-015-0153-5. PMC 4417674. PMID 25894090.
- Kolata G (23 April 2015). "Chinese Scientists Edit Genes of Human Embryos, Raising Concerns". The New York Times. Archived from the original on 2 January 2022. Retrieved 24 April 2015.
- Harmon A (14 February 2017). "Human Gene Editing Receives Science Panel's Support". The New York Times. ISSN 0362-4331. Archived from the original on 2 January 2022. Retrieved 17 February 2017.
- Committee on Human Gene Editing: Scientific, Medical, and Ethical Considerations . "Human Genome Editing: Science, Ethics, and Governance". nationalacademies.org. National Academy of Sciences; National Academy of Medicine. Retrieved 21 February 2017.
- "Scientists OK genetically engineering babies". New York Post. Reuters. 14 February 2017. Retrieved 17 February 2017.
- Friedmann T, Roblin R (March 1972). "Gene therapy for human genetic disease?". Science. 175 (4025): 949–955. Bibcode:1972Sci...175..949F. doi:10.1126/science.175.4025.949. PMID 5061866. S2CID 19952096.
- Rogers S, New Scientist 1970, p. 194
- Cepko CL, Roberts BE, Mulligan RC (July 1984). "Construction and applications of a highly transmissible murine retrovirus shuttle vector. This Vector is used for entering a cell in the humans cell body". Cell. 37 (3): 1053–1062. doi:10.1016/0092-8674(84)90440-9. PMID 6331674. S2CID 34544709.
- "The first gene therapy". Life Sciences Foundation. 21 June 2011. Archived from the original on 28 November 2012. Retrieved 7 January 2014.
- Blaese RM, Culver KW, Miller AD, Carter CS, Fleisher T, Clerici M, et al. (October 1995). "T lymphocyte-directed gene therapy for ADA- SCID: initial trial results after 4 years". Science. 270 (5235): 475–480. Bibcode:1995Sci...270..475B. doi:10.1126/science.270.5235.475. PMID 7570001. S2CID 46339645.
- Trojan J, Johnson TR, Rudin SD, Ilan J, Tykocinski ML, Ilan J (January 1993). "Treatment and prevention of rat glioblastoma by immunogenic C6 cells expressing antisense insulin-like growth factor I RNA". Science. 259 (5091): 94–97. Bibcode:1993Sci...259...94T. doi:10.1126/science.8418502. PMID 8418502.
- ^ Trojan J, Pan YX, Wei MX, Ly A, Shevelev A, Bierwagen M, et al. (2012). "Methodology for Anti-Gene Anti-IGF-I Therapy of Malignant Tumours". Chemotherapy Research and Practice. 2012: 1–12. doi:10.1155/2012/721873. PMC 3287029. PMID 22400112.
- Abbott A (April 1992). "Gene therapy. Italians first to use stem cells". Nature. 356 (6369): 465. Bibcode:1992Natur.356..465A. doi:10.1038/356465a0. PMID 1560817. S2CID 4319842.
- Cavazzana-Calvo M, Thrasher A, Mavilio F (February 2004). "The future of gene therapy". Nature. 427 (6977): 779–781. Bibcode:2004Natur.427..779C. doi:10.1038/427779a. PMID 14985734. S2CID 4421364.
- Blakeslee S (18 May 1993). "Treatment for 'Bubble Boy Disease'". The New York Times. ISSN 0362-4331. Retrieved 9 February 2018.
- Naldini, Luigi; Blömer, Ulrike; Gallay, Philippe; Ory, Daniel; Mulligan, Richard; Gage, Fred H.; Verma, Inder M.; Trono, Didier (12 April 1996). "In Vivo Gene Delivery and Stable Transduction of Nondividing Cells by a Lentiviral Vector". Science. 272 (5259): 263–267. Bibcode:1996Sci...272..263N. doi:10.1126/science.272.5259.263. ISSN 0036-8075. PMID 8602510. S2CID 18997464.
- Stein R (11 October 2010). "First patient treated in stem cell study". The Washington Post. Retrieved 10 November 2010.
- "Death Prompts FDA to Suspend Arthritis Gene Therapy Trial". Medpage Today. 27 July 2007. Retrieved 10 November 2010.
- Stolberg SG (22 January 2000). "Gene Therapy Ordered Halted At University". The New York Times. Retrieved 10 November 2010.
- Wilson JF (18 March 2002). "Murine Gene Therapy Corrects Symptoms of Sickle Cell Disease". The Scientist – Magazine of the Life Sciences. Retrieved 17 August 2010.
- "Gene Therapy Corrects Sickle Cell Disease In Laboratory Study". St. Jude Children's Research Hospital. 4 December 2008. Retrieved 29 December 2012 – via ScienceDaily.
- Penman D (11 October 2002). "Subtle gene therapy tackles blood disorder". New Scientist. Retrieved 17 August 2010.
- "DNA nanoballs boost gene therapy". New Scientist. 12 May 2002. Retrieved 17 August 2010.
- Ananthaswamy A (20 March 2003). "Undercover genes slip into the brain". New Scientist. Retrieved 17 August 2010.
- Holmes R (13 March 2003). "Gene therapy may switch off Huntington's". New Scientist. Retrieved 17 August 2010.
- Ott MG, Schmidt M, Schwarzwaelder K, Stein S, Siler U, Koehl U, et al. (April 2006). "Correction of X-linked chronic granulomatous disease by gene therapy, augmented by insertional activation of MDS1-EVI1, PRDM16 or SETBP1". Nature Medicine. 12 (4): 401–409. doi:10.1038/nm1393. PMID 16582916. S2CID 7601162.
- Brown BD, Venneri MA, Zingale A, Sergi Sergi L, Naldini L (May 2006). "Endogenous microRNA regulation suppresses transgene expression in hematopoietic lineages and enables stable gene transfer". Nature Medicine. 12 (5): 585–591. doi:10.1038/nm1398. PMID 16633348. S2CID 11114427.
- Morgan RA, Dudley ME, Wunderlich JR, Hughes MS, Yang JC, Sherry RM, et al. (October 2006). "Cancer regression in patients after transfer of genetically engineered lymphocytes". Science. 314 (5796): 126–129. Bibcode:2006Sci...314..126M. doi:10.1126/science.1129003. PMC 2267026. PMID 16946036.
- Levine BL, Humeau LM, Boyer J, MacGregor RR, Rebello T, Lu X, et al. (November 2006). "Gene transfer in humans using a conditionally replicating lentiviral vector". Proceedings of the National Academy of Sciences of the United States of America. 103 (46): 17372–17377. Bibcode:2006PNAS..10317372L. doi:10.1073/pnas.0608138103. PMC 1635018. PMID 17090675.
- "Penn Medicine presents HIV gene therapy trial data at CROI 2009". EurekAlert!. 10 February 2009. Archived from the original on 25 August 2012. Retrieved 19 November 2009.
- "Gene therapy first for poor sight". BBC News. 1 May 2007. Retrieved 3 May 2010.
- Dolgin E (2009). "Colour blindness corrected by gene therapy". Nature. doi:10.1038/news.2009.921.
- Cartier N, Hacein-Bey-Abina S, Bartholomae CC, Veres G, Schmidt M, Kutschera I, et al. (November 2009). "Hematopoietic stem cell gene therapy with a lentiviral vector in X-linked adrenoleukodystrophy" (PDF). Science. 326 (5954): 818–823. Bibcode:2009Sci...326..818C. doi:10.1126/science.1171242. PMID 19892975. S2CID 27783.
- Komáromy AM, Alexander JJ, Rowlan JS, Garcia MM, Chiodo VA, Kaya A, et al. (July 2010). "Gene therapy rescues cone function in congenital achromatopsia". Human Molecular Genetics. 19 (13): 2581–2593. doi:10.1093/hmg/ddq136. PMC 2883338. PMID 20378608.
- Cavazzana-Calvo M, Payen E, Negre O, Wang G, Hehir K, Fusil F, et al. (September 2010). "Transfusion independence and HMGA2 activation after gene therapy of human β-thalassaemia". Nature. 467 (7313): 318–322. Bibcode:2010Natur.467..318C. doi:10.1038/nature09328. PMC 3355472. PMID 20844535.
- Galanello R, Origa R (May 2010). "Beta-thalassemia". Orphanet Journal of Rare Diseases. 5: 11. doi:10.1186/1750-1172-5-11. PMC 2893117. PMID 20492708.
- ^ Beals JK (16 September 2010). "Gene Therapy Frees Beta-Thalassemia Patient From Transfusions for 2+ Years". MedScape. Retrieved 15 December 2012.
- ^ Leboulch P (20 March 2013). "Five year outcome of lentiviral gene therapy for human beta-thalassemia, lessons and prospects". Thalassemia Reports. 3 (1s): 108. doi:10.4081/thal.2013.s1.e43.
- ^ Clinical trial number NCT01639690 for "β-Thalassemia Major With Autologous CD34+ Hematopoietic Progenitor Cells Transduced With TNS9.3.55 a Lentiviral Vector Encoding the Normal Human β-Globin Gene" at ClinicalTrials.gov
- Trojan A, Aristizabal BH, Jay LM, Castillo T, Penagos PJ, Briceño I, Trojan J (2016). "IGF-I biomarker testing in an ethical context". Adv Modern Oncol Res. 2 (4): 188–200. doi:10.18282/amor.v2.i4.58 (inactive 1 November 2024).
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - Castillo T, Trojan A, Noguera MC, Jay LM, Crane C, Alvarez A, et al. (2016). "Epistemológica experiencia en la elaboración de tecnología biomolecular para estrategia de la inmunoterapia génica" [Epistemological experience in developing of molecular biology technology for immunogene therapy strategy]. Rev Cien (in Spanish). 2 (25): 228–240. doi:10.14483//udistrital.jour.RC.2016.25.a6.
- Rosenberg T (27 May 2011). "The Man Who Was Cured of HIV and What It Means for a Cure for AIDS". New York. Retrieved 2 January 2022.
- "Letters from the Director: Remembering Timothy Ray Brown: A Champion for HIV Cure Research | NIH Office of AIDS Research". www.oar.nih.gov. Retrieved 26 June 2022.
- "Gene Therapy Turns Several Leukemia Patients Cancer Free. Will It Work for Other Cancers, Too?". Singularity Hub. 6 January 2014. Retrieved 7 January 2014.
- Yang ZJ, Zhang YR, Chen B, Zhang SL, Jia EZ, Wang LS, et al. (July 2009). "Phase I clinical trial on intracoronary administration of Ad-hHGF treating severe coronary artery disease". Molecular Biology Reports. 36 (6): 1323–1329. doi:10.1007/s11033-008-9315-3. PMID 18649012. S2CID 23419866.
- Hahn W, Pyun WB, Kim DS, Yoo WS, Lee SD, Won JH, et al. (October 2011). "Enhanced cardioprotective effects by coexpression of two isoforms of hepatocyte growth factor from naked plasmid DNA in a rat ischemic heart disease model". The Journal of Gene Medicine. 13 (10): 549–555. doi:10.1002/jgm.1603. PMID 21898720. S2CID 26812780.
- "Neovasculogen". Eurolab. Retrieved 4 August 2015.
- Deev RV, Bozo IY, Mzhavanadze ND, Voronov DA, Gavrilenko AV, Chervyakov YV, et al. (September 2015). "pCMV-vegf165 Intramuscular Gene Transfer is an Effective Method of Treatment for Patients With Chronic Lower Limb Ischemia". Journal of Cardiovascular Pharmacology and Therapeutics. 20 (5): 473–482. doi:10.1177/1074248415574336. PMID 25770117. S2CID 13443907.
- "On Cancer: Launch of Stem Cell Therapy Trial Offers Hope for Patients with Inherited Blood Disorder". Memorial Sloan-Kettering Cancer Center. 16 July 2012. Retrieved 15 December 2012.
- Pollack A (20 July 2012). "European Agency Recommends Approval of a Gene Therapy". The New York Times. Retrieved 2 January 2022.
- "First Gene Therapy Approved by European Commission". UniQure (Press release). 2 November 2012. Archived from the original on 5 November 2012. Retrieved 2 January 2022.
- "Chiesi and uniQure delay Glybera launch to add data". Biotechnology. The Pharma Letter. 4 August 2014. Retrieved 28 August 2014.
- Burger L, Hirschler B (26 November 2014). "First gene therapy drug sets million-euro price record". Reuters. Retrieved 30 March 2015.
- Whalen J (2 November 2012). "Gene-Therapy Approval Marks Major Milestone". The Wall Street Journal.
- Morrison C (3 March 2015). "$1-million price tag set for Glybera gene therapy". TradeSecrets. 33 (3): 217–218. doi:10.1038/nbt0315-217. PMID 25748892. S2CID 205266596.
- "Gene therapy approved in Europe for first time". Archived from the original on 4 January 2014.
- Regalado A (4 May 2016). "The World's Most Expensive Medicine Is a Bust". MIT Technology Review.
- Bosely S (30 April 2013). "Pioneering gene therapy trials offer hope for heart patients". The Guardian. Retrieved 28 April 2014.
- "Cardiac gene therapy news: The Physicians Clinic". thephysiciansclinic.co.uk. 8 September 2013. Archived from the original on 29 April 2014. Retrieved 2 January 2022.
- "Celladon Receives Breakthrough Therapy Designation From FDA for Mydicar, Novel, First-in-Class Therapy in Development to Treat Heart Failure". Celladon. 10 July 2015. Archived from the original on 10 July 2015. Retrieved 2 January 2022.
- Fernàndez-Ruiz I (March 2016). "Gene therapy: No improvement in outcomes with gene therapy for heart failure". Nature Reviews. Cardiology. 13 (3): 122–123. doi:10.1038/nrcardio.2016.14. PMID 26843287. S2CID 205472001.
- Biffi A, Montini E, Lorioli L, Cesani M, Fumagalli F, Plati T, et al. (August 2013). "Lentiviral hematopoietic stem cell gene therapy benefits metachromatic leukodystrophy". Science. 341 (6148): 1233158. doi:10.1126/science.1233158. PMID 23845948. S2CID 206546808.
- Aiuti A, Biasco L, Scaramuzza S, Ferrua F, Cicalese MP, Baricordi C, et al. (August 2013). "Lentiviral hematopoietic stem cell gene therapy in patients with Wiskott–Aldrich syndrome". Science. 341 (6148): 1233151. doi:10.1126/science.1233151. PMC 4375961. PMID 23845947.
- Gallagher J (21 April 2015). "Gene therapy: 'Tame HIV' used to cure disease". BBC News, Health. Retrieved 21 April 2015.
- Malech HL, Ochs HD (April 2015). "An emerging era of clinical benefit from gene therapy". JAMA. 313 (15): 1522–1523. doi:10.1001/jama.2015.2055. PMID 25898049.
- "Gene therapy cure for children with 'bubble baby' disease". Science Daily. 18 November 2014.
- "Gene therapy provides safe, long-term relief for patients with severe hemophilia B". Science Daily. 20 November 2014.
- Beali A (25 January 2014). "Gene therapy restores sight in people with eye disease". The New Scientist. Retrieved 25 January 2014.
- Tebas P, Stein D, Tang WW, Frank I, Wang SQ, Lee G, et al. (March 2014). "Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV". The New England Journal of Medicine. 370 (10): 901–910. doi:10.1056/NEJMoa1300662. PMC 4084652. PMID 24597865.
- Dvorsky G (6 March 2014). "Scientists Create Genetically Modified Cells That Protect Against HIV". io9, Biotechnology. Retrieved 6 March 2014.
- Clinical trial number NCT02247843 for "Stem Cell Gene Therapy for Sickle Cell Disease" at ClinicalTrials.gov
- Clinical trial number NCT00012545 for "Collection and Storage of Umbilical Cord Stem Cells for Treatment of Sickle Cell Disease" at ClinicalTrials.gov
- "Ten things you might have missed Monday from the world of business". Boston Globe. 3 February 2015. Retrieved 13 February 2015.
- Zimmer C (9 March 2015). "Protection Without a Vaccine". The New York Times. Archived from the original on 2 January 2022. Retrieved 30 March 2015.
- Gardner MR, Kattenhorn LM, Kondur HR, von Schaewen M, Dorfman T, Chiang JJ, et al. (March 2015). "AAV-expressed eCD4-Ig provides durable protection from multiple SHIV challenges". Nature. 519 (7541): 87–91. Bibcode:2015Natur.519...87G. doi:10.1038/nature14264. PMC 4352131. PMID 25707797.
- Wade N (3 December 2015). "Scientists Place Moratorium on Edits to Human Genome That Could Be Inherited". The New York Times. Archived from the original on 2 January 2022. Retrieved 3 December 2015.
- Walsh F (3 December 2015). "Gene editing: Is era of designer humans getting closer?". BBC News Health. Retrieved 31 December 2015.
- "Genetically Altered Skin Saves A Boy Dying Of A Rare Disease". NPR.org.
- Henry R (19 February 2017). "Leukaemia cure hopes rise as girl is gene‑edited". The Times. Retrieved 20 February 2017.
- Sample I (5 November 2015). "Baby girl is first in the world to be treated with 'designer immune cells'". The Guardian. Retrieved 6 November 2015.
- ^ "'Designer cells' reverse one-year-old's cancer". BBC News. 5 November 2015. Retrieved 11 December 2022.
- "Summary of opinion1 (initial authorisation) Strimvelis" (PDF). European Medicines Agency. 1 April 2016. pp. 1–2. Archived from the original (PDF) on 28 January 2018. Retrieved 13 April 2016.
- Hirscheler B (1 April 2016). "Europe gives green light to first gene therapy for children". Reuters. Retrieved 13 April 2016.
- Reeves R (6 June 2016). "Second gene therapy wins approval in Europe". Bionews. Archived from the original on 21 February 2017. Retrieved 20 February 2017.
- Coghlan A (9 April 2016). "Gene Therapy Approved". New Scientist. No. 3068. pp. 8–9.
- Cyranoski D (July 2016). "Chinese scientists to pioneer first human CRISPR trial". Nature. 535 (7613): 476–477. Bibcode:2016Natur.535..476C. doi:10.1038/nature.2016.20302. PMID 27466105.
- Bennett J (15 November 2016). "Chinese Scientists Become First to Use CRISPR Gene-Editing on Humans". Popular Mechanics. Retrieved 16 November 2016.
- Lee TW, Southern KW, Perry LA, Penny-Dimri JC, Aslam AA (June 2016). Southern KW (ed.). "Topical cystic fibrosis transmembrane conductance regulator gene replacement for cystic fibrosis-related lung disease". The Cochrane Database of Systematic Reviews. 2016 (6): CD005599. doi:10.1002/14651858.CD005599.pub5. PMC 8682957. PMID 27314455.
- Whipple T (1 March 2017). "New gene therapy 'shrinks tumours like ice cubes'". The Times. Retrieved 1 March 2017.
- Coghlan A (March 2017). "Gene therapy 'cures' boy of blood disease that affects millions". New Scientist.
- "FDA approval brings first gene therapy to the United States" (Press release). U.S. Food and Drug Administration (FDA). 30 August 2017.
- "FDA approves axicabtagene ciloleucel for large B-cell lymphoma". U.S. Food and Drug Administration (FDA). Retrieved 5 January 2018.
- Zayner J (6 October 2017). "DIY Human CRISPR Myostatin Knock-Out". Youtube. Archived from the original on 11 November 2017. Retrieved 20 May 2020.
- Zayner J. "The First Attempt At Human CRISPR Gene Editing". Retrieved 20 May 2020.
- "AP Exclusive: US scientists try 1st gene editing in the body". AP NEWS. 15 November 2017. Retrieved 17 November 2020.
- Kaiser J (November 2017). "A human has been injected with gene-editing tools to cure his disabling disease. Here's what you need to know". Science. doi:10.1126/science.aar5098.
- Zhang S (15 November 2017). "The First Man to Have His Genes Edited Inside His Body". The Atlantic. Retrieved 17 November 2020.
- Ledford H (5 September 2018). "First test of in-body gene editing shows promise". Nature. doi:10.1038/d41586-018-06195-6. S2CID 92840885.
- Marchione M (7 February 2019). "Tests suggest scientists achieved 1st 'in body' gene editing". AP News. Retrieved 7 February 2019.
- Staff (2 February 2019). "Ascending Dose Study of Genome Editing by the Zinc Finger Nuclease (ZFN) Therapeutic SB-913 in Subjects With MPS II". ClinicalTrials.gov. U.S. National Library of Medicine. Retrieved 7 February 2019.
- Rangarajan S, Walsh L, Lester W, Perry D, Madan B, Laffan M, et al. (December 2017). "AAV5-Factor VIII Gene Transfer in Severe Hemophilia A". The New England Journal of Medicine. 377 (26): 2519–2530. doi:10.1056/nejmoa1708483. hdl:10044/1/57163. PMID 29224506.
- van den Berg HM (December 2017). "A Cure for Hemophilia within Reach". The New England Journal of Medicine. 377 (26): 2592–2593. doi:10.1056/nejme1713888. PMID 29224412.
- "FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss". U.S. Food and Drug Administration (FDA) (Press release). 19 December 2017. Retrieved 20 December 2017.
- Herper M (2 January 2018). "Spark Therapeutics Sets Price Of Blindness-Treating Gene Therapy At $850,000". Forbes. Retrieved 4 January 2018.
- Sheridan K (19 December 2017). "The FDA approved a gene therapy to treat blindness in a groundbreaking moment for DNA-based medicine". Newsweek. Retrieved 20 December 2017.
- Stein R (24 May 2019). "At $2.1 Million, New Gene Therapy Is The Most Expensive Drug Ever". NPR. Retrieved 24 May 2019.
- Tong A (3 June 2019). "EU stamps historic OK on bluebird's gene therapy for β-thalassemia – now sit back and wait for the price". Retrieved 4 June 2019.
- "Zynteglo EPAR". European Medicines Agency (EMA). 25 March 2019. Retrieved 8 June 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "Single Ascending Dose Study in Participants With LCA10". clinicaltrials.gov. Retrieved 20 August 2019.
- "Allergan and Editas Medicine Initiate the Brilliance Phase 1/2 Clinical Trial of AGN-151587 (EDIT-101) for the Treatment of LCA10". Editas Medicine. Retrieved 20 August 2019.
- Ledford H (March 2020). "CRISPR treatment inserted directly into the body for first time". Nature. 579 (7798): 185. Bibcode:2020Natur.579..185L. doi:10.1038/d41586-020-00655-8. PMID 32157225.
- Stein, Rob (29 July 2019). "In A 1st, Doctors In U.S. Use CRISPR Tool To Treat Patient With Genetic Disorder". NPR. Retrieved 25 September 2024.
- "Zolgensma EPAR". European Medicines Agency (EMA). 24 March 2020. Retrieved 16 October 2020.
- "Audentes Therapeutics Provides Update on the ASPIRO Clinical Trial Evaluating AT132 in Patients with X-linked Myotubular Myopathy". Audentes Therapeutics. 10 August 2020. Archived from the original on 27 October 2020. Retrieved 21 September 2020.
- "Astellas' Audentes reports 3rd death in gene therapy trial". Fierce Biotech. 21 August 2020. Retrieved 21 September 2020.
- "High-dose AAV gene therapy deaths". Nature Biotechnology. 38 (8): 910. 1 August 2020. doi:10.1038/s41587-020-0642-9. ISSN 1546-1696. PMID 32760031. S2CID 220981004.
- ^ "Libmeldy: Pending EC decision". European Medicines Agency (EMA). 16 October 2020. Archived from the original on 17 October 2020. Retrieved 16 October 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "New gene therapy to treat rare genetic disorder metachromatic leukodystrophy". European Medicines Agency. 16 October 2020. Retrieved 16 October 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "Libmeldy EPAR". European Medicines Agency (EMA). 13 October 2020. Retrieved 22 December 2020.
- Lysogene (15 October 2020). "Lysogene provides update on the AAVance Clinical Trial Evaluating LYS-SAF302 in Patients with MPS IIIA – Lysogene". Archived from the original on 17 October 2020. Retrieved 17 October 2020.
- Kohn DB, Booth C, Shaw KL, Xu-Bayford J, Garabedian E, Trevisan V, et al. (May 2021). "Autologous Ex Vivo Lentiviral Gene Therapy for Adenosine Deaminase Deficiency". The New England Journal of Medicine. 384 (21): 2002–2013. doi:10.1056/NEJMoa2027675. PMC 8240285. PMID 33974366.
- Marchione M (11 May 2021). "AIDS virus used in gene therapy to fix 'bubble baby' disease". Stat. Retrieved 19 July 2021.
- "Gene therapy restores immune function in children with rare immunodeficiency". National Institutes of Health (NIH). 11 May 2021. Retrieved 19 July 2021.
- "Why Gene Therapy Caused Leukemia In Some 'Boy In The Bubble Syndrome' Patients". ScienceDaily. Retrieved 19 July 2021.
- Mamcarz E, Zhou S, Lockey T, Abdelsamed H, Cross SJ, Kang G, et al. (April 2019). "Lentiviral Gene Therapy Combined with Low-Dose Busulfan in Infants with SCID-X1". The New England Journal of Medicine. 380 (16): 1525–1534. doi:10.1056/NEJMoa1815408. PMC 6636624. PMID 30995372.
- "HIV used to cure 'bubble boy' disease". BBC News. 17 April 2019. Retrieved 19 July 2021.
- Pittman J, Ravitz JD. "These Scientists May Have Found a Cure for 'Bubble Boy' Disease". Smithsonian Magazine. Retrieved 19 July 2021.
- Rohr K (17 April 2019). "Gene therapy restores immunity in infants with rare immunodeficiency disease". National Institutes of Health (NIH). Retrieved 4 June 2020.
- Gillmore JD, Gane E, Taubel J, Kao J, Fontana M, Maitland ML, et al. (August 2021). "CRISPR-Cas9 In Vivo Gene Editing for Transthyretin Amyloidosis". The New England Journal of Medicine. 385 (6): 493–502. doi:10.1056/NEJMoa2107454. PMID 34215024. S2CID 235722446.
- "News: Clinical Trial Update: Positive Data for First Ever In Vivo CRISPR Medicine". CRISPR Medicine. Retrieved 16 December 2021.
- "The science news that shaped 2021: Nature's picks". Nature. December 2021. doi:10.1038/d41586-021-03734-6. PMID 34907370. S2CID 245144020.
- Pearson TS, Gupta N, San Sebastian W, Imamura-Ching J, Viehoever A, Grijalvo-Perez A, et al. (July 2021). "Gene therapy for aromatic L-amino acid decarboxylase deficiency by MR-guided direct delivery of AAV2-AADC to midbrain dopaminergic neurons". Nature Communications. 12 (1): 4251. Bibcode:2021NatCo..12.4251P. doi:10.1038/s41467-021-24524-8. PMC 8275582. PMID 34253733.
- Ibrahim M (14 July 2021). "Gene therapy restores missing dopamine in children with rare brain disease". Science. Retrieved 18 July 2021.
- "Gene therapy trial points to a wider window to alter course of rare disease". Stat. 12 July 2021. Retrieved 18 July 2021.
- Flotte TR, Cataltepe O, Puri A, Batista AR, Moser R, McKenna-Yasek D, et al. (February 2022). "AAV gene therapy for Tay-Sachs disease". Nature Medicine. 28 (2): 251–259. doi:10.1038/s41591-021-01664-4. PMC 10786171. PMID 35145305. S2CID 246748772.
- Sena-Esteves M (14 February 2022). "First gene therapy for Tay-Sachs disease successfully given to two children". The Conversation. Retrieved 7 March 2022.
- "Parents spark breakthrough gene therapy for children with Tay-Sachs disease". The Independent. 18 February 2022. Retrieved 7 March 2022.
- "Upstaza: Pending EC decision". European Medicines Agency. 19 May 2022. Archived from the original on 25 May 2022. Retrieved 22 May 2022.
- "PTC Therapeutics Receives Positive CHMP Opinion for Upstaza for the Treatment of AADC Deficiency". PTC Therapeutics (Press release). 20 May 2022. Retrieved 22 May 2022.
- Chowdary P, Shapiro S, Makris M, Evans G, Boyce S, Talks K, et al. (July 2022). "Phase 1-2 Trial of AAVS3 Gene Therapy in Patients with Hemophilia B". The New England Journal of Medicine. 387 (3): 237–247. doi:10.1056/NEJMoa2119913. PMID 35857660. S2CID 250697905.
- "Novel gene therapy could reduce bleeding risk for haemophilia patients". ScienceDaily. Retrieved 3 August 2022.
- "Transformational therapy cures haemophilia B". BBC News. 21 July 2022. Retrieved 3 August 2022.
- "Base editing: Revolutionary therapy clears girl's incurable cancer". BBC News. 11 December 2022. Retrieved 11 December 2022.
- "Gene therapy eyedrops restored a boy's sight. Similar treatments could help millions". AP News. 24 July 2023. Retrieved 31 July 2023.
- Huang, Jinbo; Xue, Shuai; Buchmann, Peter; Teixeira, Ana Palma; Fussenegger, Martin (16 August 2023). "An electrogenetic interface to program mammalian gene expression by direct current". Nature Metabolism. 5 (8): 1395–1407. doi:10.1038/s42255-023-00850-7. PMC 10447240. PMID 37524785.
- "PTC Therapeutics Announces FDA Approval of AADC Deficiency Gene Therapy". PTC Therapeutics, Inc. 13 November 2024. Retrieved 21 November 2024.
Further reading
- "Gene Therapy: An Overview of Approved and Pipeline Technologies" (PDF). CADTH (171). March 2018. Archived (PDF) from the original on 19 October 2018.
- Baum C, Düllmann J, Li Z, Fehse B, Meyer J, Williams DA, von Kalle C (March 2003). "Side effects of retroviral gene transfer into hematopoietic stem cells". Blood. 101 (6): 2099–2114. doi:10.1182/blood-2002-07-2314. PMID 12511419. S2CID 8489829.
- Daley J (January 2020). "Gene Therapy Arrives: After false starts, drugs that manipulate the code of life are finally changing lives". Scientific American. 322 (1): None. doi:10.1038/scientificamerican012020-2SglZYN24KkpjWDUVuCdME. PMID 39014835.
- Gardlík R, Pálffy R, Hodosy J, Lukács J, Turna J, Celec P (April 2005). "Vectors and delivery systems in gene therapy". Medical Science Monitor. 11 (4): RA110–121. PMID 15795707.
- Horn PA, Morris JC, Neff T, Kiem HP (September 2004). "Stem cell gene transfer – efficacy and safety in large animal studies". Molecular Therapy. 10 (3): 417–431. doi:10.1016/j.ymthe.2004.05.017. PMID 15336643.
- Parambi DG, Alharbi KS, Kumar R, Harilal S, Batiha GE, Cruz-Martins N, Magdy O, Musa A, Panda DS, Mathew B (October 2021). "Gene Therapy Approach with an Emphasis on Growth Factors: Theoretical and Clinical Outcomes in Neurodegenerative Diseases". Molecular Neurobiology. 59 (1): 191–233. doi:10.1007/s12035-021-02555-y. PMC 8518903. PMID 34655056.
- Salmons B, Günzburg WH (April 1993). "Targeting of retroviral vectors for gene therapy". Human Gene Therapy. 4 (2): 129–141. doi:10.1089/hum.1993.4.2-129. PMID 8494923.
- Staff (18 November 2005). "Gene Therapy". Human Genome Project Information. Oak Ridge National Laboratory. Archived from the original (FAQ) on 27 April 2006. Retrieved 28 May 2006.
- Tinkov S, Bekeredjian R, Winter G, Coester C (20 November 2000). "Polyplex-conjugated microbubbles for enhanced ultrasound targeted gene therapy" (PDF). Georgia World Congress Center, Atlanta, GA: 2008 AAPS Annual Meeting and Exposition. Archived from the original (PDF) on 7 July 2012. Retrieved 26 January 2009.
- Wang H, Shayakhmetov DM, Leege T, Harkey M, Li Q, Papayannopoulou T, Stamatoyannopolous G, Lieber A (September 2005). "A capsid-modified helper-dependent adenovirus vector containing the beta-globin locus control region displays a nonrandom integration pattern and allows stable, erythroid-specific gene expression". Journal of Virology. 79 (17): 10999–11013. doi:10.1128/JVI.79.17.10999-11013.2005. PMC 1193620. PMID 16103151.
External links
| Genetic engineering | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Genetically modified organisms |
| ||||||||||||||||||||||||||
| Processes |
| ||||||||||||||||||||||||||
| Uses |
| ||||||||||||||||||||||||||
| Related articles | |||||||||||||||||||||||||||
| Regulation | |||||||||||||||||||||||||||
| Geography | |||||||||||||||||||||||||||
| Similar fields | |||||||||||||||||||||||||||
| Biotechnology | |||||
|---|---|---|---|---|---|
| History |  | ||||
| Branches | |||||
| Biological concepts | |||||
| General concepts | |||||
| Basic techniques and tools |
| ||||
| Applications | |||||
| Interdisciplinary fields | |||||
| Lists | |||||
| Longevity | |||||||
|---|---|---|---|---|---|---|---|
| Ageing | |||||||
| Life extension | |||||||
| Lists of life expectancy |
| ||||||
| Records | |||||||
| Immortality | |||||||
| Longevity genes | |||||||
| Related | |||||||