Pharmaceutical compound
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Ultiva |
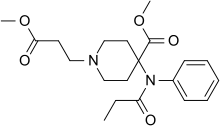
| Other names | methyl 1-(2-methoxycarbonylethyl)-4-(phenyl-propanoyl-amino)-piperidine-4-carboxylate |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 0 |
| Protein binding | 70% (bound to plasma proteins) |
| Metabolism | cleaved by non-specific plasma and tissue esterases |
| Elimination half-life | 1-20 minutes |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.211.201 |
| Chemical and physical data | |
| Formula | C20H28N2O5 |
| Molar mass | 376.453 g·mol |
| 3D model (JSmol) | |
| Melting point | 5 °C (41 °F) |
SMILES
| |
InChI
| |
| (verify) | |
Remifentanil, marketed under the brand name Ultiva is a potent, short-acting synthetic opioid analgesic drug. It is given to patients during surgery to relieve pain and as an adjunct to an anaesthetic. Remifentanil is used for sedation as well as combined with other medications for use in general anesthesia. The use of remifentanil has made possible the use of high-dose opioid and low-dose hypnotic anesthesia, due to synergism between remifentanil and various hypnotic drugs and volatile anesthetics.
Clinical use
Remifentanil is used as an opioid analgesic that has a rapid onset and rapid recovery time. It has been used effectively during craniotomies, spinal surgery, cardiac surgery, and gastric bypass surgery. While opiates function similarly, with respect to analgesia, the pharmacokinetics of remifentanil allows for quicker post-operative recovery.
Administration
It is administered in the form remifentanil hydrochloride and in adults is given as an intravenous infusion in doses ranging from 0.1 microgram per kilogram per minute to 0.5 (μg/kg)/min. Children may require higher infusion rates (up to 1.0 (μg/kg)/min). The clinically useful infusion rates are 0.025–0.1 (μg/kg)/min for sedation (rates adjusted to age of patient, severity of their illness and invasiveness of surgical procedure). Small amounts of other sedative medications are usually co-administered with remifentanil to produce sedation. Clinically useful infusion rates in general anesthesia vary but are usually 0.1–1 (μg/kg)/min.
Remifentanil can be administered as part of an anesthesia technique called TIVA (total intravenous anesthesia) using computer controlled infusion pumps in a process called TCI (target controlled infusion). A target plasma concentration is entered as ng/mL into the pump, which calculates its infusion rate according to patient factors like age and weight. Induction levels of 40 ng/mL are commonly used, but it generally varies between 3–8 ng/mL. For certain surgical procedures that produce particularly strong stimuli a level of up to 15 ng/mL might be needed. The relatively short context-sensitive half-life of remifentanil allows the desired blood plasma level to be achieved quickly, and also for the same reason, recovery occurs quickly. This allows remifentanil to be used in unique circumstances such as cesarean section.
Remifentanil's short context-sensitive half-life makes it ideal for intense pain of short duration. As such, it has been used for analgesia in labor successfully; however, it is not as effective as epidural analgesia.
In combination with propofol, remifentanil is used for anesthesia of patients undergoing electroconvulsive therapy.
Metabolism
Remifentanil is considered a metabolic soft drug, one that is rapidly metabolized to an inactive form. Unlike other synthetic opioids which are hepatically metabolized, remifentanil has an ester linkage which undergoes rapid hydrolysis by non-specific tissue and plasma esterases. This means that accumulation does not occur with remifentanil and its context-sensitive half-life remains at 4 minutes after a 4-hour infusion.
Remifentanil is metabolized to a compound (remifentanil acid) which has 1/4600th the potency of the parent compound.
Due to its quick metabolism and short effects, remifentanil has opened up new possibilities in anesthesia. When remifentanil is used together with a hypnotic (i.e. one that produces sleep) it can be used in relative high doses. This is because remifentanil is rapidly eliminated from the blood plasma on termination of the remifentanil infusion; hence the effects of the drug quickly dissipate even after very long infusions. Owing to synergism between remifentanil and hypnotic drugs (such as propofol) the dose of the hypnotic can be substantially reduced. This leads often to more hemodynamic stability during surgery and a quicker post-operative recovery time.
Side-effects
Remifentanil is a specific μ-receptor agonist. Hence, it causes a reduction in sympathetic nervous system tone, respiratory depression and analgesia. The drug's effects include a dose-dependent decrease in heart rate and arterial pressure and respiratory rate and tidal volume. Muscle rigidity is sometimes noted.
The most common side effects reported by patients receiving this medication are a sense of extreme "dizziness" (often short lived, a common side effect of other fast-acting synthetic phenylpiperidine narcotics such as fentanyl and alfentanil) and intense itching (pruritus), often around the face. These side effects are often controlled by either altering the administered dose (decreasing or in some cases, increasing the dose) or by administering other sedatives that allow the patient to tolerate or lose awareness of the side effect.
Because pruritus is partially due to excessive serum histamine levels, antihistamines such as diphenhydramine (Benadryl) are often co-administered. This is done with care, however, as excessive sedation may occur.
Nausea can occur as a side effect of remifentanil, however, it is usually transient in nature due to the drug's short half-life which rapidly removes it from the patient's circulation once the infusion is terminated.
Potency
Comparing its analgesia-sedation effect in ventilated patients, remifentanil may be superior to morphine but not to fentanyl.
Circumventing naltrexone
Remifentanil has been used with some success to circumvent naltrexone in patients who are in need of pain management.
Abuse potential
Remifentanil, being a μ-receptor agonist, functions like other μ-receptor agonists, such as morphine and codeine; it can cause euphoria and has the potential for abuse. However, due to its rapid metabolism and short-acting half-life the likelihood of abuse is quite low. Nevertheless, there have been some documentations of remifentanil abuse.
Development and marketing
Prior to the development of remifentanil, most short-acting hypnotics and amnestics faced issues with prolonged use, where accumulation would result in unfavorable lingering effects during post-operative recovery. Remifentanil was designed to serve as a strong anesthetic with an ultra-short and predictable duration that would not have accumulation issues.
Remifentanil was patented by Glaxo Wellcome Inc. and was FDA approved on July 12, 1996. Its patent ended on the 10th of September 2017.
Regulation
In Hong Kong, remifentanil is regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. It can only be used legally by health professionals and for university research purposes. The substance can be given by pharmacists under a prescription. Anyone who supplies the substance without prescription can be fined HK$10,000 (US$1,550). The penalty for trafficking or manufacturing the substance is a HK$5,000,000 (US$775,000) fine and life imprisonment. Possession of the substance for consumption without license from the Department of Health is illegal with a HK$1,000,000 (US$155,000) fine and/or 7 years of jail time.
Remifentanil is a Schedule II narcotic controlled substance in the United States with a DEA ACSCN of 9739 and a 2013 annual aggregate manufacturing quota of 3,750 grams, unchanged from the prior year.
References
- Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- "Remifentanil, IV opioid analgesic, Remi | Ultiva". www.ultiva.com. Retrieved 2015-11-30.
- Gesztesi Z, Mootz BL, White PF (November 1999). "The use of a remifentanil infusion for hemodynamic control during intracranial surgery". Anesthesia and Analgesia. 89 (5): 1282–7. doi:10.1213/00000539-199911000-00038. PMID 10553851.
- Grottke O, Dietrich PJ, Wiegels S, Wappler F (November 2004). "Intraoperative wake-up test and postoperative emergence in patients undergoing spinal surgery: a comparison of intravenous and inhaled anesthetic techniques using short-acting anesthetics". Anesthesia and Analgesia. 99 (5): 1521–1527. doi:10.1213/01.ANE.0000134684.25322.26. PMID 15502058. S2CID 45361690.
- Knapik M, Knapik P, Nadziakiewicz P, Misiołek H, Saucha W, Walaszczyk M, Dyaczyńska-Herman A (August 2006). "Comparison of remifentanil or fentanyl administration during isoflurane anesthesia for coronary artery bypass surgery". Medical Science Monitor. 12 (8): PI33–8. PMID 16865075.
- De Baerdemaeker LE, Jacobs S, Pattyn P, Mortier EP, Struys MM (September 2007). "Influence of intraoperative opioid on postoperative pain and pulmonary function after laparoscopic gastric banding: remifentanil TCI vs sufentanil TCI in morbid obesity". British Journal of Anaesthesia. 99 (3): 404–11. doi:10.1093/bja/aem164. PMID 17606479.
- Michelsen LG, Hug Jr CC (December 1996). "The pharmacokinetics of remifentanil". Journal of Clinical Anesthesia. 8 (8): 679–82. doi:10.1016/s0952-8180(96)00179-1. PMID 8982900.
- Guy J, Hindman BJ, Baker KZ, Borel CO, Maktabi M, Ostapkovich N, et al. (March 1997). "Comparison of remifentanil and fentanyl in patients undergoing craniotomy for supratentorial space-occupying lesions". Anesthesiology. 86 (3): 514–524. doi:10.1097/00000542-199703000-00002. PMID 9066316.
- Weale NK, Rogers CA, Cooper R, Nolan J, Wolf AR (February 2004). "Effect of remifentanil infusion rate on stress response to the pre-bypass phase of paediatric cardiac surgery". British Journal of Anaesthesia. 92 (2): 187–194. doi:10.1093/bja/aeh038. PMID 14722167.
- "Remifentanil Actavis" (in Swedish). Retrieved 21 Aug 2014.
- White LD, Hodsdon A, An GH, Thang C, Melhuish TM, Vlok R (November 2019). "Induction opioids for caesarean section under general anaesthesia: a systematic review and meta-analysis of randomised controlled trials". International Journal of Obstetric Anesthesia. 40: 4–13. doi:10.1016/j.ijoa.2019.04.007. hdl:10072/416502. PMID 31230994.
- Stocki D, Matot I, Einav S, Eventov-Friedman S, Ginosar Y, Weiniger CF (March 2014). "A randomized controlled trial of the efficacy and respiratory effects of patient-controlled intravenous remifentanil analgesia and patient-controlled epidural analgesia in laboring women". Anesthesia and Analgesia. 118 (3): 589–597. doi:10.1213/ANE.0b013e3182a7cd1b. PMID 24149580. S2CID 4844447.
- Ulusoy H, Cekic B, Besir A, Geze S, Hocaoglu C, Akdogan A (February 2014). "Sevoflurane/remifentanil versus propofol/remifentanil for electroconvulsive therapy: comparison of seizure duration and haemodynamic responses". The Journal of International Medical Research. 42 (1): 111–119. doi:10.1177/0300060513509036. PMID 24398757.
- Bodor N, Buchwald P (January 2000). "Soft drug design: general principles and recent applications". Medicinal Research Reviews. 20 (1): 58–101. doi:10.1002/(SICI)1098-1128(200001)20:1<58::AID-MED3>3.0.CO;2-X. PMID 10608921. S2CID 25119421.
- Hoke JF, Cunningham F, James MK, Muir KT, Hoffman WE (April 1997). "Comparative pharmacokinetics and pharmacodynamics of remifentanil, its principle metabolite (GR90291) and alfentanil in dogs". The Journal of Pharmacology and Experimental Therapeutics. 281 (1): 226–232. PMID 9103501.
- ^ Patel SS, Spencer CM (September 1996). "Remifentanil". Drugs. 52 (3): 417–27, discussion 428. doi:10.2165/00003495-199652030-00009. PMID 8875131. S2CID 265900417.
- Dahaba AA, Grabner T, Rehak PH, List WF, Metzler H (September 2004). "Remifentanil versus morphine analgesia and sedation for mechanically ventilated critically ill patients: a randomized double blind study". Anesthesiology. 101 (3): 640–646. doi:10.1097/00000542-200409000-00012. PMID 15329588. S2CID 17192694.
- Spies C, Macguill M, Heymann A, Ganea C, Krahne D, Assman A, et al. (March 2011). "A prospective, randomized, double-blind, multicenter study comparing remifentanil with fentanyl in mechanically ventilated patients". Intensive Care Medicine. 37 (3): 469–476. doi:10.1007/s00134-010-2100-5. PMID 21165734.
- Ternes JW, O'Brien CP (1990). "The opioids: Abuse liability and treatments for dependence". Advances in Alcohol & Substance Abuse. 9 (1–2): 27–45. doi:10.1300/J251v09n01_03. PMID 2198785.
- Panlilio LV, Schindler CW (May 2000). "Self-administration of remifentanil, an ultra-short acting opioid, under continuous and progressive-ratio schedules of reinforcement in rats". Psychopharmacology. 150 (1): 61–6. doi:10.1007/s002130000415. PMID 10867977. S2CID 21623038.
- Baylon GJ, Kaplan HL, Somer G, Busto UE, Sellers EM (December 2000). "Comparative abuse liability of intravenously administered remifentanil and fentanyl". Journal of Clinical Psychopharmacology. 20 (6): 597–606. doi:10.1097/00004714-200012000-00002. PMID 11106130.
- Levine AI, Bryson EO (February 2010). "Intranasal self-administration of remifentanil as the foray into opioid abuse by an anesthesia resident". Anesthesia and Analgesia. 110 (2): 524–5. doi:10.1213/ANE.0b013e3181c5f069. PMID 19917624.
- Feldman PL, Chorghade MS (July 2006). Chorghade MS (ed.). "Discovery and development of the ultrashort-acting analgesic remifentanil". Drug Discovery and Development. 18. Wiley Online Library: 339–342. doi:10.1002/0471780103. ISBN 9780471398486.
- US 5866591, Gatlin LA, Heiman SA, Lewis JS, "Stable formulations of remifentanil", issued 2 February 1999
- Orange book: approved drug products with therapeutic equivalence evaluations. Silver Spring, MD: US Food and Drug Administration. 2010.
External links
- "Remifentanil". Drug Information Portal. U.S. National Library of Medicine.
- "Remifentanil Hydrochloride". Drug Information Portal. U.S. National Library of Medicine.
| General anesthetics (N01A) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inhalational | |||||||||||||||
| Injection |
| ||||||||||||||
| |||||||||||||||
| Opioid receptor modulators | |||||
|---|---|---|---|---|---|
| μ-opioid (MOR) |
| ||||
| δ-opioid (DOR) |
| ||||
| κ-opioid (KOR) |
| ||||
| Nociceptin (NOP) |
| ||||
| Others |
| ||||