| This article may be too technical for most readers to understand. Please help improve it to make it understandable to non-experts, without removing the technical details. (September 2023) (Learn how and when to remove this message) |
| Rhinitis medicamentosa | |
|---|---|
| Other names | Rebound congestion |
 | |
| Specialty | Otorhinolaryngology |
| Symptoms | Nasal congestion |
| Usual onset | After 5–7 days of use of topical decongestant nasal sprays |
| Causes | Overuse of decongestant nasal sprays and certain oral medications |
| Prevention | Limiting use of decongestant nasal sprays and other potentially problematic medications |
| Treatment | Ceasing use of offending medications |
Rhinitis medicamentosa (or RM, also known as rebound congestion) is a condition of rebound nasal congestion suspected to be brought on by extended use of topical decongestants (e.g., oxymetazoline, phenylephrine, xylometazoline, and naphazoline nasal sprays) and certain oral medications (e.g., sympathomimetic amines and various 2-imidazolines) that constrict blood vessels in the lining of the nose, although evidence has been contradictory.
Presentation
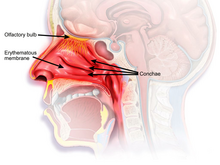
The characteristic presentation of RM involves nasal congestion without rhinorrhea, postnasal drip, or sneezing following several days of decongestant use. This condition typically occurs after 5–7 days of use of topical decongestants. Patients often try increasing both the dose and the frequency of nasal sprays upon the onset of RM, worsening the condition. The swelling of the nasal passages caused by rebound congestion may eventually result in permanent turbinate hypertrophy, which may block nasal breathing until surgically removed.

Pathophysiology
The pathophysiology of RM is unclear, although several mechanisms involving norepinephrine signaling have been proposed. RM is associated with histological changes that include: an increase in the number of lymphocytes and fibroblasts, epithelial cell denudation, epithelial edema, goblet cell hyperplasia, increased expression of the epidermal growth factor receptor, increased mucus production, nasociliary loss, inflammatory cell infiltration, and squamous cell metaplasia.
Direct acting sympathomimetic amines, such as phenylephrine, stimulate alpha adrenergic receptors, while mixed-acting agents, such as pseudoephedrine can stimulate both alpha and beta adrenergic receptors directly and indirectly by releasing norepinephrine from sympathetic nerve terminals. At first, the vasoconstrictive effect of alpha-receptors dominates, but with continued use of an alpha agonist, this effect fades first, allowing the vasodilation due to beta-receptor stimulation to emerge.
2-Imidazoline derivatives, such as oxymetazoline, may participate in negative feedback on endogenous norepinephrine production. Therefore, after cessation of prolonged use, there will be inadequate sympathetic vasoconstriction in the nasal mucosa, and domination of parasympathetic activity can result in increased secretions and nasal edema. Evidence suggests that if oxymetazoline is used only nightly for allergic rhinitis (instead of more frequent dosage as may be directed on product label), it may be used longer than one week without high risk of rhinitis medicamentosa especially with use of intranasal steroid like fluticasone furoate.
Treatment
The treatment of RM involves withdrawal of the offending nasal spray or oral medication. Both a "cold turkey" and a "weaning" approach can be used. Cold turkey is the most effective treatment method, as it directly removes the cause of the condition, yet the time period between the discontinuation of the drug and the relief of symptoms may be too long and uncomfortable for some individuals (particularly when trying to go to sleep when they are unable to breathe through their nose).
The use of over-the-counter (OTC) saline nasal sprays may help open the nose without causing RM if the spray does not contain a decongestant. Symptoms of congestion and runny nose can often be treated with corticosteroid nasal sprays under the supervision of a physician. For very severe cases, oral steroids or nasal surgery may be necessary.
A study has shown that the anti-infective agent benzalkonium chloride, which is frequently added to topical nasal sprays as a preservative, aggravates the condition by further increasing the rebound swelling.
See also
References
- Mortuaire, G.; de Gabory, L.; François, M.; Massé, G.; Bloch, F.; Brion, N.; Jankowski, R.; Serrano, E. (June 2013). "Rebound congestion and rhinitis medicamentosa: Nasal decongestants in clinical practice. Critical review of the literature by a medical panel". European Annals of Otorhinolaryngology, Head and Neck Diseases. 130 (3): 137–144. doi:10.1016/j.anorl.2012.09.005. PMID 23375990.
- ^ Ramey JT, Bailen E, Lockey RF (2006). "Rhinitis medicamentosa" (PDF). Journal of Investigational Allergology and Clinical Immunology. 16 (3): 148–155. PMID 16784007. Retrieved 29 April 2015.
- Rhinitis Medicamentosa at eMedicine
- Adams, H. Richard (2013). "Adrenergic Agonists and Antagonists". In Riviere, Jim E.; Papich, Mark G. (eds.). Veterinary Pharmacology and Therapeutics. John Wiley & Sons. pp. 125–56. ISBN 978-1-118-68590-7.
- Passàli, Desiderio; Salerni, Lorenzo; Passàli, Giulio Cesare; Passàli, Francesco Maria; Bellussi, Luisa (18 October 2006). "Nasal decongestants in the treatment of chronic nasal obstruction: efficacy and safety of use" (PDF). Expert Opinion on Drug Safety. 5 (6): 783–790. doi:10.1517/14740338.5.6.783. hdl:2108/102185. PMID 17044805. S2CID 43718145.
- Lacroix, Jean-Silvain (1989). "Adrenergic and non-adrenergic mechanisms in sympathetic vascular control of nasal mucosa". Acta Physiologica Scandinavica Supplementum. 581: 1–49. PMID 2568728.
- Elwany, Samy S.; Stephanos, Wahid M. (1983). "Rhinitis medicamentosa: An experimental histopathological and histochemical study". ORL. 45 (4): 187–194. doi:10.1159/000275642. PMID 6192384.
- ^ Baroody, Fuad M.; Brown, David; Gavanescu, Laura; DeTineo, Marcy; Naclerio, Robert M. (April 2011). "Oxymetazoline adds to the effectiveness of fluticasone furoate in the treatment of perennial allergic rhinitis". Journal of Allergy and Clinical Immunology. 127 (4): 927–934. doi:10.1016/j.jaci.2011.01.037. PMID 21377716.
- Graf, P.; Hallen, H.; Juto, J.-E. (May 1995). "Benzalkonium chloride in a decongestant nasal spray aggravates rhinitis medicamentosa in healthy volunteers". Clinical & Experimental Allergy. 25 (5): 395–400. doi:10.1111/j.1365-2222.1995.tb01069.x. PMID 7553241. S2CID 19989791.
Further reading
- Bernstein, I.Leonard (January 2000). "Is the use of benzalkonium chloride as a preservative for nasal formulations a safety concern? A cautionary note based on compromised mucociliary transport". Journal of Allergy and Clinical Immunology. 105 (1): 39–44. doi:10.1016/S0091-6749(00)90175-1. PMID 10629450.
- Remsen, K. A.; Black, M. J. (19 April 1980). "Rhinitis medicamentosa". CMAJ. 122 (8): 881–884. PMC 1801634. PMID 6154514.
- Adams, H. Richard (2013). "Adrenergic Agonists and Antagonists". In Riviere, Jim E.; Papich, Mark G. (eds.). Veterinary Pharmacology and Therapeutics. John Wiley & Sons. pp. 125–56. ISBN 978-1-118-68590-7.
- Elwany, Samy S.; Stephanos, Wahid M. (1983). "Rhinitis medicamentosa: An experimental histopathological and histochemical study". ORL. 45 (4): 187–194. doi:10.1159/000275642. PMID 6192384.
- Baldwin, R. L.; Jolly, P. A.; Mizes, J. S.; Fleece, L. (1984). "Rhinitis medicamentosa. Conceptualization, incidence, and treatment". The Alabama Journal of Medical Sciences. 21 (2): 205–208. PMID 6375416.
- Graf, Peter (October 1999). "Adverse Effects of benzalkonium chloride on the nasal mucosa: Allergic rhinitis and rhinitis medicamentosa". Clinical Therapeutics. 21 (10): 1749–1755. doi:10.1016/S0149-2918(99)80053-8. PMID 10566570.
- Graf, P.; Hallen, H.; Juto, J.-E. (May 1995). "Benzalkonium chloride in a decongestant nasal spray aggravates rhinitis medicamentosa in healthy volunteers". Clinical & Experimental Allergy. 25 (5): 395–400. doi:10.1111/j.1365-2222.1995.tb01069.x. PMID 7553241. S2CID 19989791.
- Lin, Chun-Yu; Cheng, Po-Hsu; Fang, Sheen-Yie (28 June 2016). "Mucosal Changes in Rhinitis Medicamentosa". Annals of Otology, Rhinology & Laryngology. 113 (2): 147–151. doi:10.1177/000348940411300213. PMID 14994772. S2CID 850948.
- Mabry, R. L. (1982). "Rhinitis medicamentosa: the forgotten factor in nasal obstruction". Southern Medical Journal. 75 (7): 817–819. doi:10.1097/00007611-198207000-00013. PMID 6178170. S2CID 29244245.
- Bu, G. X.; Wang, J. Q. (1991). "Studies of rhinitis medicamentosa". Chinese Medical Journal. 104 (1): 60–63. PMID 1879198.
External links
| Classification | D |
|---|---|
| External resources |
| Diseases of the respiratory system | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Upper RT (including URTIs, common cold) |
| ||||||||||||||||||||||
| Lower RT/ lung disease (including LRTIs) |
| ||||||||||||||||||||||
| Pleural cavity/ mediastinum |
| ||||||||||||||||||||||
| Other/general | |||||||||||||||||||||||