
Tubular carcinoma is a subtype of invasive ductal carcinoma of the breast. More rarely, tubular carcinomas may arise in the pancreas or kidney. Most tubular carcinomas begin in the milk duct of the breast and spread to healthy tissue around it.
Pathology
Although tubular carcinoma has been considered a special-type tumor, recent trend has been to classify it as a low-grade, invasive NOS carcinoma because there is a continuous spectrum from pure tubular carcinomas to mixed NOS carcinomas with tubular features, depending on the percentage of the lesion that displays tubular features.
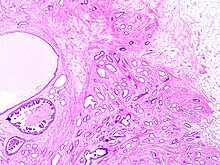
Histology
Tubular carcinomas are generally around 1 cm. or smaller, and are made up of tubules. They are usually low-grade. Elastosis has been noted as common but is not present in all cases.
Prevalence
Prevalence has previously been controversial, with contradictory reports from studies reporting either very low prevalence, or a high prevalence. With the increasing availability of screening mammography, however, tubular carcinomas are being diagnosed earlier, and more recent studies suggest tubular carcinomas represent between 8% and 27% of all breast cancers.
Prognosis
Tubular carcinoma is one of the histologic types of breast cancer with a more favorable outcome.
See also
- Breast cancer classification
- Ductal carcinoma in situ – a common precancerous or Stage 0 breast cancer
- Invasive cribriform carcinoma of the breast – a rare breast cancer that consists of >50% cribriform histopathology but commonly has small or large areas (<50%) closely resembling tubular carcinoma histopathology.
- Intraductal papillary mucinous neoplasm
- Invasive carcinoma of no special type
- Invasive lobular carcinoma
- Invasion (cancer)
Notes and references
- Notes
- Special-type tumor: such as mucinous and cribriform carcinomas.
- NOS: of type "Not Otherwise Specified".
- References
- ^ Image by Mikael Häggström, MD. Reference for typical features: Pragya Virendrakumar Jain, M.D., Julie M. Jorns, M.D. "Breast - Other invasive carcinoma subtypes, WHO classified - Tubular". Pathology Outlines.
{{cite web}}: CS1 maint: multiple names: authors list (link) Last author update: 23 March 2023 - ^ Hudis, Kenneth (22 June 2019). "IDC Type: Tubular Carcinoma of the Breast". Breastcancer.org. Retrieved 26 February 2022.
- Limaiem, Faten; Mlika, Mouna (2022). "Tubular Breast Carcinoma". StatPearls. StatPearls Publishing. PMID 31194380. Retrieved 3 March 2022.
- Chelliah, Adeline; Kalimuthu, Sangeetha; Chetty, Runjan (October 2016). "Intraductal tubular neoplasms of the pancreas: an overview". Ann Diagn Pathol. 24 (24:68–72): 68–72. doi:10.1016/j.anndiagpath.2016.04.009. PMID 27185640.
- Zhao, Ming; He, Xiang-lei; Teng, Xiao-dong (December 2015). "Mucinous tubular and spindle cell renal cell carcinoma: a review of clinicopathologic aspects". Diagnostic Pathology. 10 (1): 168. doi:10.1186/s13000-015-0402-1. PMC 4573286. PMID 26377921.
- Musser, Robert (2009). The P.I.N.K. Primer. Dog Ear Publishing. pp. 20–. ISBN 978-1-60844-176-1.
- Feng, Yixiao; Spezia, Mia; Huang, Shifeng; Yuan, Chengfu; Zeng, Zongyue; Zhang, Linghuan; Ji, Xiaojuan; Liu, Wei; Huang, Bo; Luo, Wenping; Liu, Bo; Lei, Yan; Du, Scott; Vuppalapati, Akhila; Luu, Hue H.; Haydon, Rex C.; He, Tong-Chuan; Ren, Guosheng (June 2018). "Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis". Genes & Diseases. 5 (2): 77–106. doi:10.1016/j.gendis.2018.05.001. PMC 6147049. PMID 30258937.
- "Understanding Your Pathology Report: Breast Cancer", Cancer.org, American Cancer Society, 2022, retrieved 26 February 2022
- "Farlex Partner Medical Dictionary". 2009. not otherwise specified. Retrieved 26 February 2022.
- ^ Stavros, A. Thomas (2004). Rapp, Cynthia L.; Parker, Steve H. (eds.). Breast Ultrasound. Lippincott Williams & Wilkins. pp. 647–649. ISBN 978-0-397-51624-7. OCLC 1065689596. p. 649:
A highly differentiated invasive carcinoma that forms well-defined tubules (containing epithelium, but no myoepithelium) and that have abundant desmoplastic fibrous stromal reaction between the tubules.
- Rosen, Paul Peter, ed. (2001). Rosen's Breast Pathology. Lippincott Williams & Wilkins. pp. 373–. ISBN 978-0-7817-2379-4. OCLC 1117861419.
- "Breast Cancer Treatment (Adult) (PDQ®)–Health Professional Version". National Cancer Institute. 20 January 2022. Retrieved 26 February 2022.
- Demir S, Sezgin G, Sari AA, Kucukzeybek BB, Yigit S, Etit D, Yazici A, Kucukzeybek Y (October 2021). "Clinicopathological analysis of invasive cribriform carcinoma of the breast, with review of the literature". Annals of Diagnostic Pathology. 54: 151794. doi:10.1016/j.anndiagpath.2021.151794. PMID 34325338.
Further reading
- Cserni, Gábor (March 2020). "Histological type and typing of breast carcinomas and the WHO classification changes over time". Pathologica. 112 (1): 25–41. doi:10.32074/1591-951X-1-20. PMC 8138497. PMID 32202537.
- Erber, Ramona; Hartmann, Arndt (August 2020). "Histology of Luminal Breast Cancer". Breast Care. 15 (4). Basel: 327–336. doi:10.1159/000509025. PMC 7490665. PMID 32982642.
- Sanders, Melinda A.; Mayer, Ingrid A.; Chakravarthy, Bapsi (3 March 2017). "22 Tubular Carcinoma of the Breast". In Raghavan, Derek; Ahluwalia, Manmeet S.; Blanke, Charles D.; et al. (eds.). Textbook of Uncommon Cancer (5 ed.). John Wiley & Sons. pp. 338–344. ISBN 978-1-119-19621-1. OCLC 1069570078.
- Zhang, Hanwen; Zhang, Ning (December 2020). "Special subtypes with favorable prognosis in breast cancer: A registry-based cohort study and network meta-analysis". Cancer Treatment Reviews. 91: 102–108. doi:10.1016/j.ctrv.2020.102108. PMID 33075683.
This oncology article is a stub. You can help Misplaced Pages by expanding it. |