| This article may be too technical for most readers to understand. Please help improve it to make it understandable to non-experts, without removing the technical details. (April 2023) (Learn how and when to remove this message) |
Ultrasound-triggered drug delivery using stimuli-responsive hydrogels refers to the process of using ultrasound energy for inducing drug release from hydrogels that are sensitive to acoustic stimuli. This method of approach is one of many stimuli-responsive drug delivery-based systems that has gained traction in recent years due to its demonstration of localization and specificity of disease treatment. Although recent developments in this field highlight its potential in treating certain diseases such as COVID-19, there remain many major challenges that need to be addressed and overcome before more related biomedical applications are clinically translated into standard of care.
Types of Hydrogels Used in Drug Delivery Systems
Traditional Hydrogels
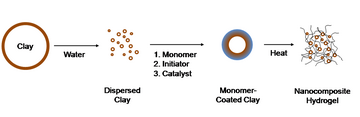
Hydrogels are three dimensional structures consisting of hydrophilic polymers (i.e., polymers, colloids, etc.) that form networks through cross-linking processes. The macromolecules involved in the formation of hydrogels are able to absorb and retain large amounts of water and other aqueous substances. Since its discovery in 1960, hydrogels have become a crucial component in biomedical research and applications. A few examples of hydrogel use include organ regeneration, wound healing, and drug delivery. Hydrogels are generally classified based on the following characteristics: material, crosslinking mechanism, physical structure, electric charge, and response to stimuli. Synthesis of hydrogels are developed from a combination or isolated forms of natural and synthetic polymers. The main examples of natural polymers used to derive hydrogels include polysaccharides, polypeptides, and polynucleotides. Several known examples of synthetic polymeric constituents include poly (vinyl alcohol) (PVA), poly (acrylic acid) (PAA), and poly (2-hydroxyethyl methacrylate) (PHEMA). The crosslinking mechanism of the hydrophilic macromolecules are driven by covalent bonding, resulting in a physical- or chemical-type hydrogel. Physical hydrogels contain reversible matrices of hydrogen and non-covalent bonds, while chemical hydrogels are composed of irreversible matrices that are molecularly held together by covalent bonds. Used as another parameter in characterizing gels, electric charge (also referred to as ionic character) describes the ability of the macromolecules to drive swelling behavior. Hydrogels classified based on this property fall under three main categories: cationic, anionic, and amphoteric. Bawa et al. demonstrated that cationic gels swell in acidic environments but remain condensed in basic environments.
Smart Hydrogel Polymers

Since traditional hydrogels were able to encapsulate and carry materials, research into drug-loaded hydrogels began to expand in the field of drug delivery. Dubbed as “smart hydrogels” or “stimuli-responsive hydrogels”, these gels are able to dynamically respond to external or internal stimuli in addition to possessing similar swelling-deswelling properties of traditional hydrogels. Various examples of external stimuli that have been used to control smart hydrogels in drug delivery systems include temperature, pH, light, ultrasound, and enzymes. Additional considerations in designing smart hydrogels involve fundamental understanding of bond strength, molecular weight, degree of polymerization, polymer structure, and molecular assembly. The bond strength describes the cross-linking strength of the hydrogel, which is considered in designing drug release mechanisms of hydrogel-based platforms. Scientific understanding of the molecular weight of gels is taken into account when loading drugs of increasing weight. Similar to conventional hydrogels, the polymeric chain (or backbone) of the smart hydrogels is derived from polysaccharides, polypeptides, and polynucleotides. Examples of natural polymers include alginate, chitosan, cellulose, gelatin, fibrin, and collagen. Hydrogel size and type are the two main properties considered in designing hydrogels when seeking the optimal delivery route for drug administration. Various examples of hydrogel type designs include nanoparticles, nanogels, and microgels. For example, El-Sherbiny et al. proposed gelatin-based hydrogel nanoparticles that were stimulated by magnetic forces. Other variables considered in hydrogel design include safety, biodegradability, drug loading capacity, and on-demand control of drug release . The main safety concerns in formulating hydrogels include bacterial infection and biocompatibility. The final parameter considered in developing hydrogels for drug delivery systems revolve around the embedded payload within the hydrogel. Cells, proteins, and therapeutic drugs are the main payloads used in hydrogel-based drug delivery platforms. In one example of payload use, Jiang et al. demonstrated the stimulated release of gallic acid from chitin-based hydrogel via ultrasound induction.
Use of Ultrasound for Drug Therapy
General Overview of Ultrasound
According to the Moyano et al., ultrasound refers to vibrational mechanical waves with frequencies greater than 20 kilohertz (kHz). Ultrasound is traditionally used for imaging, monitoring, and diagnosing a broad range of conditions in the medical field. Various examples of ultrasound modalities include Doppler ultrasound, focused ultrasound, and echocardiography. The key component of using most ultrasound devices is a transducer that consists of an array of piezoelectric crystals. The atoms within these crystals vibrate under electrical current stimulation, converting this electrical energy into mechanical, in this case, high acoustic or ultrasonic energy. When the sonicating transducer is directed at the human body, the resulting sound pressure waves produced by the transducer will pass through the dermal layer and reach the tissue where the waves are reflected (or echoed) back to the transducer and converted back into electrical signals for image reconstruction. Tissue characteristics such as density affect the intensity of the reflected sound waves. Other parameters such as beam frequency, equipment components, and imaging settings contribute towards the resolution of the ultrasound application. Ultrasound has also been used for therapeutic purposes because it is non-invasiveness, able to provide deeper tissue penetration, and safely localize application of acoustic energy.

While ultrasound modalities are generally considered safe, extreme levels of human exposure to ultrasound can increase injury risk. In the US, the Food and Drug Administration (FDA) guidelines, the maximum allowed exposure to ultrasound for use is defined by the following key parameters: mechanical index, thermal index, spatial-peak temporal-peak intensity, spatial-peak pulse-average power, and spatial-peak temporal-average power. Mechanical index (MI) is a unitless metric that is used to measure the acoustic power output from ultrasound use. Since the MI is inversely proportional to the ultrasonic beam frequency, the MI will be lower at higher frequencies. The thermal index (TI) describes the risk of increasing the temperature of the tissue being sonicated by ultrasound. A solution to decreasing TI involves the reduction of the time that the sonicating transducer is focused on the targeted area. The spatial-peak temporal-peak (SPTP) power refers to the highest intensity output of the ultrasound beam during implementation. The spatial-peak pulse-average (SPPA) power is a measure of the maximum intensity output averaged over the duration of ultrasound use in. The spatial-peak temporal-average power describes the measure of the highest intensity output generated by the repeating pulse of the ultrasound beam over a period of time.
Effects of Focused Ultrasound on Smart Hydrogels
Due to the sonication capability of ultrasound and drug-release property of smart hydrogels, there has been scientific interest in controlling the release of the payload from hydrogels. Focusing and directing acoustic energy (that can convert to thermal or mechanical energy) towards smart hydrogels, implanted within tissue at times, induces a hydrogel response that results in the release of the embedded payload. Although hydrogels that are sensitive to mechanical pressure are generally used in ultrasound-triggered drug delivery platforms, hydrogels that respond to changes in temperature have also been used for these systems. For example, Makhmalzadeh et al. proposed an ultrasound-triggered drug delivery method involving the use of thermo-responsive hydrogels loaded with silibinin, a cancer drug for treating melanoma. At low temperatures, these thermo-responsive hydrogels exist in liquid form but following ultrasonication, they transition into a gel state. Although ultrasound- and thermo-sensitive hydrogels are responsive to certain ultrasound modalities, they differ in how they respond to external stimuli. Ultrasound-responsive hydrogels are capable of being stimulated by more than one type of stimulation force through ultrasound. Conversely, thermo-responsive hydrogels, as the name specifies, can only respond to the thermal forces induced by ultrasound. Despite this, thermo-responsive hydrogels have been widely used in cancer-based drug delivery systems.

Of the existing ultrasound modalities, focused ultrasound has been used extensively in drug delivery research. High-Intensity Focused Ultrasound (HIFU) and Low-Intensity Focused Ultrasound are the two main techniques used in inducing drug release from smart hydrogels. Current HIFU applications are used for ablating tumors located at increased depths. Since HIFU is able to invoke high temperatures, they have been used for cancer therapy by stimulating drug release from smart hydrogels via thermolysis mechanisms. In regard to the use of ultrasound- and thermo-responsive hydrogels for drug delivery, HIFU is able to stimulate both types of hydrogels. In one study related to cancer therapy, HIFU exhibited high efficiency inducing nanovaccine release from hydrogel-based carriers. Although HIFU has been studied in various capacities, this technique can cause irreparable damage to healthy tissue. Therefore, LIFU has been the conventional method for use in hydrogel responsive drug delivery platforms. In other areas of the biomedical field, LIFU has been used for stimulation such as bone regeneration in tissue engineering applications. Due to its lower generated acoustic power output, LIFU is preferred over HIFU in biomedical applications involving neuromodulation and other brain-related procedures. Studies have shown that LIFU has proven to be a cost-effective and non-invasive method for hydrogel-based drug delivery.
The underlying drug-releasing mechanism induced by focused ultrasound onto ultrasound-sensitive hydrogels is based on mechanical or thermal effects. Mechanical-based ultrasound sonication mechanisms refer to the conversion of acoustic energy into mechanical energy with various types that include acoustic cavitation force, or oscillation force. Generally, applying mechanical pressure to a responsive hydrogel loaded with drugs causes the hydrogel to deform. This deformation reduces the structural integrity of the hydrophobic core, allowing for the release of the drug payload. Both ultrasound- and thermo- responsive hydrogels are capable of carrying various embedded carriers of drug payloads which include metal-organic framework, nanoparticles, and liposomes. Although many studies have demonstrated the irreversible compression of hydrogels induced under ultrasound, Goncalves et al. designed hydrogel-based nanoparticles that were capable of “self-healing”, meaning they were able to return to their original form following drug release from its depot.
Acoustic cavitation forces, specifically, have been used in conjunction with ultrasound-responsive hydrogels for drug delivery. This type of mechanical force refers to the formation, growth, and destruction of bubble occurs that results in the generation of acoustic energy. There are varying degrees of cavitation which divided into three groups: sonoporation, stable cavitation, and inertial cavitation. Sonoporation refers to the process of using ultrasound to open pores (or permeability) of cellular membranes to allow substances of interest to enter into the targeted cell. In cases where microbubbles are coated with hydrogels, these embedded carrier systems undergo stable cavitation and inertial cavitation. Stable cavitation characterizes vapor bubbles that oscillate within its own equilibrium, while inertial cavitation describes bubbles that generate a net growth each time the bubble expands and results in the bubble collapsing violently. Severe cavitation increases the risk of damage to tissue and drug degradation. Other forces generated by ultrasound that is used in several hydrogel-based platforms are hyperthermia and radiation. These forces are generally created by HIFU as they generate high levels of heat. Thus, guidelines established by the FDA help ensure the safe use of ultrasound in all biomedical applications, inclusive of drug delivery systems, based on the scientific understanding of these mechanical forces.
Drug delivery applications and effects
Tissue engineering
In regard to tissues, ultrasound is generally used for imaging and monitoring tissue pathologies. Due to its ability to penetrate through tissue easily, ultrasound has been widely studied and developed for drug delivery applications in the field of tissue engineering. In order for hydrogels to release drugs at the targeted location, they must be injected or implanted within the tissue. Injection of hydrogels is usually preferred over implantation due to its minimal invasiveness, reduced healing time following the procedure, and biocompatibility. In one study, Liu et al. proposed a novel design of injectable chemotaxis hydrogels to help promote the migration of bone marrow mesenchymal cells for cartilage repair. Other examples of using smart hydrogels and ultrasound in tissue engineering applications include cartilage repair, bone repair, and wound healing. The design of these drug delivery platforms is specific to each tissue type and its intended use.
Cancer treatment
In the field of cancer, ultrasound is commonly used for helping health care professionals detect and develop a diagnosis in affected patients. In the context of drug delivery, ultrasound has been used for a wide variety of therapeutic applications which include but are not limited to melanoma, ovarian cancer, and breast cancer. Hydrogels are generally used in designing these drug delivery platforms due to minimal invasiveness (if injected) and its ability to carry a different cancer drugs. These hydrogel-based systems are also paired with chemotherapy treatments. Cancer drugs used in this drug delivery platforms include doxorubicin, mitoxantrone, paclitaxel, silibinin, and cisplatin. In a cancer therapy study, Baghbani et al. proposed a method of pairing ultrasound with doxorubicin-loaded alginate-stabilized perfluorohexane (PFH) nanodroplets.
Gene therapy
Although it is generally used in combination with cancer therapeutic treatments, gene therapy has become a topic of interest in the drug delivery field. Gene therapy refers to the insertion of genes into a biological system in an attempt to add or modify mutated genes for therapeutic benefit. In order to attain high transgene expression, the electrostatic interaction between the gene and hydrogel polymer and the controlled release of the drug payload from the hydrogel is necessary. Several gene therapy drugs used in hydrogel-based drug delivery systems include CRISPR/Cas9, siRNA, and other RNA-based drugs. In a gene therapy study, Han et al. proposed a focused ultrasound-responsive hydrogel-based system for delivering siRNA nanoparticles to the targeted tumor site
Challenges and future development
The main challenge for future ultrasound-triggered hydrogel responsive delivery systems is to develop safer guidelines for using HIFU to take advantage of its benefits. In doing so, this will lead to improvements on FDA guidelines for ultrasound use. Therefore, the use of LIFU or lower acoustic energy intensity settings is suggested as the conventional method for decreasing injury risk, specifically damage to healthy tissue, until then. Focused ultrasound continues to be the primary type of ultrasound technique used in drug delivery systems. Another challenge presented in using ultrasound for inducing drug release from smart hydrogels in delivery platforms is inappropriate drug administration and unexpected complications. Currently, on-demand drug release from ultrasound-responsive hydrogels is still difficult to fully control when only using ultrasound. Yeingst et al. suggested that future hydrogel-based delivery platforms will be designed based on the drug payload to optimize the interaction between the ultrasound and stimuli-responsive hydrogel. Future development of drug delivery systems will continue to incorporate ultrasound and smart hydrogel designs.
References
- Wichterle, O.; Lím, D. (Jan 1960). "Hydrophilic Gels for Biological Use". Nature. 185 (4706): 117–118. Bibcode:1960Natur.185..117W. doi:10.1038/185117a0. ISSN 0028-0836. S2CID 4211987.
- ^ Jeong, Kwang-Hun; Park, Duckshin; Lee, Young-Chul (Jul 2017). "Polymer-based hydrogel scaffolds for skin tissue engineering applications: a mini-review". Journal of Polymer Research. 24 (7): 112. doi:10.1007/s10965-017-1278-4. ISSN 1022-9760. S2CID 136085690.
- ^ Chandan, Rajeet; Mehta, Sourabh; Banerjee, Rinti (2020-09-14). "Ultrasound-Responsive Carriers for Therapeutic Applications". ACS Biomaterials Science & Engineering. 6 (9): 4731–4747. doi:10.1021/acsbiomaterials.9b01979. ISSN 2373-9878. PMID 33455210. S2CID 225390128.
- Boucard, Nadège; Viton, Christophe; Agay, Diane; Mari, Eliane; Roger, Thierry; Chancerelle, Yves; Domard, Alain (Aug 2007). "The use of physical hydrogels of chitosan for skin regeneration following third-degree burns". Biomaterials. 28 (24): 3478–3488. doi:10.1016/j.biomaterials.2007.04.021. PMID 17482258.
- ^ Colangelo, Maria Teresa; Belletti, Silvana; Govoni, Paolo; Guizzardi, Stefano; Galli, Carlo (2021-05-12). "A Biomimetic Polynucleotides–Hyaluronic Acid Hydrogel Promotes Wound Healing in a Primary Gingival Fibroblast Model". Applied Sciences. 11 (10): 4405. doi:10.3390/app11104405. ISSN 2076-3417.
- ^ Wu, Chueh-Hung; Sun, Ming-Kuan; Kung, Yi; Wang, Yu-Chi; Chen, Sen-Lu; Shen, Hsin-Hsin; Chen, Wen-Shiang; Young, Tai-Horng (April 2020). "One injection for one-week controlled release: In vitro and in vivo assessment of ultrasound-triggered drug release from injectable thermoresponsive biocompatible hydrogels". Ultrasonics Sonochemistry. 62: 104875. Bibcode:2020UltS...6204875W. doi:10.1016/j.ultsonch.2019.104875. PMID 31796329. S2CID 208627036.
- ^ Zhang, Yuqi; Yu, Jicheng; Bomba, Hunter N.; Zhu, Yong; Gu, Zhen (2016-10-12). "Mechanical Force-Triggered Drug Delivery". Chemical Reviews. 116 (19): 12536–12563. doi:10.1021/acs.chemrev.6b00369. ISSN 0009-2665. PMID 27680291.
- Deligkaris, Kosmas; Tadele, Tadele Shiferaw; Olthuis, Wouter; van den Berg, Albert (June 2010). "Hydrogel-based devices for biomedical applications". Sensors and Actuators B: Chemical. 147 (2): 765–774. Bibcode:2010SeAcB.147..765D. doi:10.1016/j.snb.2010.03.083.
- ^ Bashir, Shahid; Hina, Maryam; Iqbal, Javed; Rajpar, A. H.; Mujtaba, M. A.; Alghamdi, N. A.; Wageh, S.; Ramesh, K.; Ramesh, S. (2020-11-16). "Fundamental Concepts of Hydrogels: Synthesis, Properties, and Their Applications". Polymers. 12 (11): 2702. doi:10.3390/polym12112702. ISSN 2073-4360. PMC 7697203. PMID 33207715.
- ^ Dreiss, Cécile A. (Aug 2020). "Hydrogel design strategies for drug delivery". Current Opinion in Colloid & Interface Science. 48: 1–17. doi:10.1016/j.cocis.2020.02.001. S2CID 213548223.
- ^ Peppas, N.A.; Slaughter, B.V.; Kanzelberger, M.A. (2012), "Hydrogels", Polymer Science: A Comprehensive Reference, Elsevier, pp. 385–395, doi:10.1016/b978-0-444-53349-4.00226-0, ISBN 978-0-08-087862-1, retrieved 2023-04-12
- ^ Bustamante-Torres, Moises; Romero-Fierro, David; Arcentales-Vera, Belén; Palomino, Kenia; Magaña, Héctor; Bucio, Emilio (2021-10-25). "Hydrogels Classification According to the Physical or Chemical Interactions and as Stimuli-Sensitive Materials". Gels. 7 (4): 182. doi:10.3390/gels7040182. ISSN 2310-2861. PMC 8628675. PMID 34842654.
- ^ Cascone, Sara; Lamberti, Gaetano (Jan 2020). "Hydrogel-based commercial products for biomedical applications: A review". International Journal of Pharmaceutics. 573: 118803. doi:10.1016/j.ijpharm.2019.118803. PMID 31682963. S2CID 207897947.
- Bawa, Priya; Pillay, Viness; Choonara, Yahya Essop; du Toit, Lisa Claire; Ndesendo, Valence Methaius Kessy; Kumar, Pradeep (Mar 2011). "A Composite Polyelectrolytic Matrix for Controlled Oral Drug Delivery". AAPS PharmSciTech. 12 (1): 227–238. doi:10.1208/s12249-010-9576-8. ISSN 1530-9932. PMC 3066358. PMID 21225384.
- ^ Athanassiadis, Athanasios G.; Ma, Zhichao; Moreno-Gomez, Nicolas; Melde, Kai; Choi, Eunjin; Goyal, Rahul; Fischer, Peer (2022-03-09). "Ultrasound-Responsive Systems as Components for Smart Materials". Chemical Reviews. 122 (5): 5165–5208. doi:10.1021/acs.chemrev.1c00622. ISSN 0009-2665. PMC 8915171. PMID 34767350.
- ^ Sun, Zhaoyi; Song, Chengjun; Wang, Chao; Hu, Yiqiao; Wu, Jinhui (2020-01-07). "Hydrogel-Based Controlled Drug Delivery for Cancer Treatment: A Review". Molecular Pharmaceutics. 17 (2): 373–391. doi:10.1021/acs.molpharmaceut.9b01020. ISSN 1543-8384. PMID 31877054. S2CID 209488927.
- ^ Hoare, Todd R.; Kohane, Daniel S. (Apr 2008). "Hydrogels in drug delivery: Progress and challenges". Polymer. 49 (8): 1993–2007. doi:10.1016/j.polymer.2008.01.027.
- Bordbar-Khiabani, Aydin; Gasik, Michael (2022-03-27). "Smart Hydrogels for Advanced Drug Delivery Systems". International Journal of Molecular Sciences. 23 (7): 3665. doi:10.3390/ijms23073665. ISSN 1422-0067. PMC 8998863. PMID 35409025.
- ^ Tu, Li; Liao, Zhihuan; Luo, Zheng; Wu, Yun-Long; Herrmann, Andreas; Huo, Shuaidong (Dec 2021). "Ultrasound-controlled drug release and drug activation for cancer therapy". Exploration. 1 (3): 20210023. doi:10.1002/EXP.20210023. ISSN 2766-2098. PMC 10190934. PMID 37323693. S2CID 245546824.
- Pal, Sanjay; Mehta, Devashish; Dasgupta, Ujjaini; Bajaj, Avinash (2021-03-01). "Advances in engineering of low molecular weight hydrogels for chemotherapeutic applications". Biomedical Materials. 16 (2): 024102. doi:10.1088/1748-605X/abdce1. ISSN 1748-6041. PMID 33461186. S2CID 231642961.
- ^ Baghbani, Fatemeh; Moztarzadeh, Fathollah; Mohandesi, Jamshid Aghazadeh; Yazdian, Fatemeh; Mokhtari-Dizaji, Manijhe (Dec 2016). "Novel alginate-stabilized doxorubicin-loaded nanodroplets for ultrasounic theranosis of breast cancer". International Journal of Biological Macromolecules. 93 (Pt A): 512–519. doi:10.1016/j.ijbiomac.2016.09.008. PMID 27601134.
- ^ Huebsch, Nathaniel; Kearney, Cathal J.; Zhao, Xuanhe; Kim, Jaeyun; Cezar, Christine A.; Suo, Zhigang; Mooney, David J. (2014-07-08). "Ultrasound-triggered disruption and self-healing of reversibly cross-linked hydrogels for drug delivery and enhanced chemotherapy". Proceedings of the National Academy of Sciences. 111 (27): 9762–9767. Bibcode:2014PNAS..111.9762H. doi:10.1073/pnas.1405469111. ISSN 0027-8424. PMC 4103344. PMID 24961369.
- ^ Kubota, Takeshi; Kurashina, Yuta; Onoe, Hiroaki (2021-01-25). "Ultrasound-Triggered Drug Release from Hydrogel Microspheres with Release Booster". 2021 IEEE 34th International Conference on Micro Electro Mechanical Systems (MEMS). Gainesville, FL, USA: IEEE. pp. 26–29. doi:10.1109/MEMS51782.2021.9375158. ISBN 978-1-6654-1912-3. S2CID 232317513.
- ^ Jiang, Huixin; Kobayashi, Takaomi (Jun 2017). "Ultrasound stimulated release of gallic acid from chitin hydrogel matrix". Materials Science and Engineering: C. 75: 478–486. doi:10.1016/j.msec.2017.02.082. PMID 28415488.
- ^ Vashist, Arti; Kaushik, Ajeet; Alexis, Kayla; Dev Jayant, Rahul; Sagar, Vidya; Vashist, Atul; Nair, Madhavan (2017-09-27). "Bioresponsive Injectable Hydrogels for On-demand Drug Release and Tissue Engineering". Current Pharmaceutical Design. 23 (24): 3595–3602. doi:10.2174/1381612823666170516144914. PMC 6889087. PMID 28521694.
- ^ Lynch, Courtney R.; Kondiah, Pierre P. D.; Choonara, Yahya E.; du Toit, Lisa C.; Ally, Naseer; Pillay, Viness (2020-03-20). "Hydrogel Biomaterials for Application in Ocular Drug Delivery". Frontiers in Bioengineering and Biotechnology. 8: 228. doi:10.3389/fbioe.2020.00228. ISSN 2296-4185. PMC 7099765. PMID 32266248.
- Li, Jianyu; Mooney, David J. (2016-10-18). "Designing hydrogels for controlled drug delivery". Nature Reviews Materials. 1 (12): 16071. Bibcode:2016NatRM...116071L. doi:10.1038/natrevmats.2016.71. ISSN 2058-8437. PMC 5898614. PMID 29657852.
- ^ Gonçalves, Catarina; Pereira, Paula; Gama, Miguel (2010-02-24). "Self-Assembled Hydrogel Nanoparticles for Drug Delivery Applications". Materials. 3 (2): 1420–1460. Bibcode:2010Mate....3.1420G. doi:10.3390/ma3021420. ISSN 1996-1944. PMC 5513474.
- ^ Raghuwanshi, Vikram Singh; Garnier, Gil (Dec 2019). "Characterisation of hydrogels: Linking the nano to the microscale". Advances in Colloid and Interface Science. 274: 102044. doi:10.1016/j.cis.2019.102044. PMID 31677493. S2CID 207895878.
- El-Sherbiny, Ibrahim M.; Smyth, Hugh D. C. (2011). "Smart Magnetically Responsive Hydrogel Nanoparticles Prepared by a Novel Aerosol-Assisted Method for Biomedical and Drug Delivery Applications". Journal of Nanomaterials. 2011 (2011): 1–13. doi:10.1155/2011/910539. ISSN 1687-4110. PMC 3146763. PMID 21808638.
- ^ Sun, Yi; Chen, Le-Gao; Fan, Xiao-Ming; Pang, Jian-Liang (2022-10-22). "Ultrasound Responsive Smart Implantable Hydrogels for Targeted Delivery of Drugs: Reviewing Current Practices". International Journal of Nanomedicine. 17: 5001–5026. doi:10.2147/IJN.S374247. PMC 9586127. PMID 36275483.
- Kim, Hyun Young; Chang, Rachel Yoon Kyung; Morales, Sandra; Chan, Hak-Kim (2021-01-29). "Bacteriophage-Delivering Hydrogels: Current Progress in Combating Antibiotic Resistant Bacterial Infection". Antibiotics. 10 (2): 130. doi:10.3390/antibiotics10020130. ISSN 2079-6382. PMC 7911734. PMID 33572929.
- ^ Bellotti, Elena; Schilling, Andrea L.; Little, Steven R.; Decuzzi, Paolo (Jan 2021). "Injectable thermoresponsive hydrogels as drug delivery system for the treatment of central nervous system disorders: A review". Journal of Controlled Release. 329: 16–35. doi:10.1016/j.jconrel.2020.11.049. PMID 33259851. S2CID 227251886.
- ^ Yeingst, Tyus J.; Arrizabalaga, Julien H.; Hayes, Daniel J. (2022-09-01). "Ultrasound-Induced Drug Release from Stimuli-Responsive Hydrogels". Gels. 8 (9): 554. doi:10.3390/gels8090554. ISSN 2310-2861. PMC 9498906. PMID 36135267.
- ^ Moyano, David Baeza; Paraiso, Daniel Arranz; González-Lezcano, Roberto Alonso (2022-02-24). "Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review". Healthcare. 10 (3): 423. doi:10.3390/healthcare10030423. ISSN 2227-9032. PMC 8954895. PMID 35326901.
- ^ Sirsi, Shashank R.; Borden, Mark A. (Jun 2014). "State-of-the-art materials for ultrasound-triggered drug delivery". Advanced Drug Delivery Reviews. 72: 3–14. doi:10.1016/j.addr.2013.12.010. PMC 4041842. PMID 24389162.
- ^ Seah, Brenden Cheong-Qi; Teo, Boon Mian (2018-11-20). "Recent advances in ultrasound-based transdermal drug delivery". International Journal of Nanomedicine. 13: 7749–7763. doi:10.2147/IJN.S174759. PMC 6251463. PMID 30538456.
- Azagury, Aharon; Khoury, Luai; Enden, Giora; Kost, Joseph (Jun 2014). "Ultrasound mediated transdermal drug delivery". Advanced Drug Delivery Reviews. 72: 127–143. doi:10.1016/j.addr.2014.01.007. PMID 24463344.
- Daftardar, Saloni; Neupane, Rabin; Boddu, Sai HS.; Renukuntla, Jwala; Tiwari, Amit K. (2019-06-03). "Advances in Ultrasound Mediated Transdermal Drug Delivery". Current Pharmaceutical Design. 25 (4): 413–423. doi:10.2174/1381612825666190211163948. PMID 30747058. S2CID 73427459.
- ^ Jang, Yongho; Kim, Doyeon; Lee, Hohyeon; Jang, Hyejin; Park, Suhyeon; Kim, Ga Eul; Lee, Hak Jong; Kim, Hyun Jung; Kim, Hyuncheol (Jul 2020). "Development of an ultrasound triggered nanomedicine-microbubble complex for chemo-photodynamic-gene therapy". Nanomedicine: Nanotechnology, Biology and Medicine. 27: 102194. doi:10.1016/j.nano.2020.102194. PMID 32278102. S2CID 215742067.
- Makhmalzadeh, Behzad Sharif; Molavi, Ommoleila; Vakili, Mohammad Reza; Zhang, Hai-Feng; Solimani, Amir; Abyaneh, Hoda Soleymani; Loebenberg, Raimar; Lai, Raymond; Lavasanifar, Afsaneh (2018-05-03). "Functionalized Caprolactone-Polyethylene Glycol Based Thermo-Responsive Hydrogels of Silibinin for the Treatment of Malignant Melanoma". Journal of Pharmacy & Pharmaceutical Sciences. 21 (1): 143–159. doi:10.18433/jpps29726. ISSN 1482-1826. PMID 29789104.
- Tehrani Fateh, Sepand; Moradi, Lida; Kohan, Elmira; Hamblin, Michael R; Shiralizadeh Dezfuli, Amin (2021-08-11). "Comprehensive review on ultrasound-responsive theranostic nanomaterials: mechanisms, structures and medical applications". Beilstein Journal of Nanotechnology. 12: 808–862. doi:10.3762/bjnano.12.64. ISSN 2190-4286. PMC 8372309. PMID 34476167.
- ^ Ma, Panqin; Lai, Xiyu; Luo, Zheng; Chen, Ying; Loh, Xian Jun; Ye, Enyi; Li, Zibiao; Wu, Caisheng; Wu, Yun-Long (2022). "Recent advances in mechanical force-responsive drug delivery systems". Nanoscale Advances. 4 (17): 3462–3478. Bibcode:2022NanoA...4.3462M. doi:10.1039/D2NA00420H. ISSN 2516-0230. PMC 9400598. PMID 36134346.
- Phenix, Christopher Peter; Togtema, Melissa; Pichardo, Samuel; Zehbe, Ingeborg; Curiel, Laura (2014-03-31). "High Intensity Focused Ultrasound Technology, its Scope and Applications in Therapy and Drug Delivery". Journal of Pharmacy & Pharmaceutical Sciences. 17 (1): 136–153. doi:10.18433/J3ZP5F. ISSN 1482-1826. PMID 24735765. S2CID 40538431.
- ^ Zardad, Az-Zamakhshariy; Choonara, Yahya; du Toit, Lisa; Kumar, Pradeep; Mabrouk, Mostafa; Kondiah, Pierre; Pillay, Viness (2016-10-18). "A Review of Thermo- and Ultrasound-Responsive Polymeric Systems for Delivery of Chemotherapeutic Agents". Polymers. 8 (10): 359. doi:10.3390/polym8100359. ISSN 2073-4360. PMC 6431863. PMID 30974645.
- Meng, Zhouqi; Zhang, Yaojia; She, Jialin; Zhou, Xuanfang; Xu, Jun; Han, Xiao; Wang, Chao; Zhu, Meifang; Liu, Zhuang (2021-02-10). "Ultrasound-Mediated Remotely Controlled Nanovaccine Delivery for Tumor Vaccination and Individualized Cancer Immunotherapy". Nano Letters. 21 (3): 1228–1237. Bibcode:2021NanoL..21.1228M. doi:10.1021/acs.nanolett.0c03646. ISSN 1530-6984. PMID 33522825. S2CID 231764401.
- ^ Yang, Min-Ho; Lim, Ki-Taek; Choung, Pill-Hoon; Cho, Chong-Su; Chung, Jong Hoon (2010-05-31). "Application of Ultrasound Stimulation in Bone Tissue Engineering". International Journal of Stem Cells. 3 (2): 74–79. doi:10.15283/ijsc.2010.3.2.74. ISSN 2005-3606. PMC 4021800. PMID 24855544.
- McCarthy, Colleen; Camci-Unal, Gulden (2021-11-30). "Low Intensity Pulsed Ultrasound for Bone Tissue Engineering". Micromachines. 12 (12): 1488. doi:10.3390/mi12121488. ISSN 2072-666X. PMC 8707172. PMID 34945337.
- Baek, Hongchae; Pahk, Ki Joo; Kim, Hyungmin (May 2017). "A review of low-intensity focused ultrasound for neuromodulation". Biomedical Engineering Letters. 7 (2): 135–142. doi:10.1007/s13534-016-0007-y. ISSN 2093-9868. PMC 6208465. PMID 30603160.
- Yan, Yiran; Chen, Yan; Liu, Zhongxun; Cai, Feiyan; Niu, Wanting; Song, Liming; Liang, Haifeng; Su, Zhiwen; Yu, Bo; Yan, Fei (Nov 2021). "Brain Delivery of Curcumin Through Low-Intensity Ultrasound-Induced Blood–Brain Barrier Opening via Lipid-PLGA Nanobubbles". International Journal of Nanomedicine. 16: 7433–7447. doi:10.2147/IJN.S327737. ISSN 1178-2013. PMC 8575349. PMID 34764649.
- Nikolova, Maria P.; Kumar, Enamala Manoj; Chavali, Murthy S. (2022-10-15). "Updates on Responsive Drug Delivery Based on Liposome Vehicles for Cancer Treatment". Pharmaceutics. 14 (10): 2195. doi:10.3390/pharmaceutics14102195. ISSN 1999-4923. PMC 9608678. PMID 36297630.
- Zeng, Yuqin; Zhang, Can; Du, Dou; Li, Ya; Sun, Lu; Han, Yuanyuan; He, Xiaoxiao; Dai, Jianwu; Shi, Liyang (Jun 2022). "Metal-organic framework-based hydrogel with structurally dynamic properties as a stimuli-responsive localized drug delivery system for cancer therapy". Acta Biomaterialia. 145: 43–51. doi:10.1016/j.actbio.2022.04.003. PMID 35398545. S2CID 248060272.
- Epstein-Barash, Hila; Orbey, Gizem; Polat, Baris E.; Ewoldt, Randy H.; Feshitan, Jameel; Langer, Robert; Borden, Mark A.; Kohane, Daniel S. (Jul 2010). "A microcomposite hydrogel for repeated on-demand ultrasound-triggered drug delivery". Biomaterials. 31 (19): 5208–5217. doi:10.1016/j.biomaterials.2010.03.008. hdl:1721.1/126409. PMC 3072837. PMID 20347484.
- Dimatteo, Robert; Darling, Nicole J.; Segura, Tatiana (Mar 2018). "In situ forming injectable hydrogels for drug delivery and wound repair". Advanced Drug Delivery Reviews. 127: 167–184. doi:10.1016/j.addr.2018.03.007. PMC 6003852. PMID 29567395.
- ^ Liu, Hui; Xiang, Xi; Huang, Jianbo; Zhu, Bihui; Wang, Liyun; Tang, Yuanjiao; Du, Fangxue; Li, Ling; Yan, Feng; Ma, Lang; Qiu, Li (May 2021). "Ultrasound augmenting injectable chemotaxis hydrogel for articular cartilage repair in osteoarthritis". Chinese Chemical Letters. 32 (5): 1759–1764. doi:10.1016/j.cclet.2020.12.004. S2CID 230529135.
- Veronick, James A.; Assanah, Fayekah; Piscopo, Nicole; Kutes, Yasemin; Vyas, Varun; Nair, Lakshmi S.; Huey, Bryan D.; Khan, Yusuf (Feb 2018). "Mechanically Loading Cell/Hydrogel Constructs with Low-Intensity Pulsed Ultrasound for Bone Repair". Tissue Engineering Part A. 24 (3–4): 254–263. doi:10.1089/ten.tea.2016.0547. ISSN 1937-3341. PMC 5792249. PMID 28610471.
- ^ Sonker, Muskan; Bajpai, Sushant; Khan, Mohd Ashhar; Yu, Xiaojun; Tiwary, Saurabh Kr; Shreyash, Nehil (2021-12-20). "Review of Recent Advances and Their Improvement in the Effectiveness of Hydrogel-Based Targeted Drug Delivery: A Hope for Treating Cancer". ACS Applied Bio Materials. 4 (12): 8080–8109. doi:10.1021/acsabm.1c00857. ISSN 2576-6422. PMID 35005919. S2CID 243891112.
- Chen, Zeming; Liu, Fuyao; Chen, Yanke; Liu, Jun; Wang, Xiaoying; Chen, Ann T.; Deng, Gang; Zhang, Hongyi; Liu, Jie; Hong, Zhangyong; Zhou, Jiangbing (Dec 2017). "Targeted Delivery of CRISPR/Cas9-Mediated Cancer Gene Therapy via Liposome-Templated Hydrogel Nanoparticles". Advanced Functional Materials. 27 (46): 1703036. doi:10.1002/adfm.201703036. PMC 5939593. PMID 29755309.
- ^ Das, Sabya Sachi; Bharadwaj, Priyanshu; Bilal, Muhammad; Barani, Mahmood; Rahdar, Abbas; Taboada, Pablo; Bungau, Simona; Kyzas, George Z. (2020-06-22). "Stimuli-Responsive Polymeric Nanocarriers for Drug Delivery, Imaging, and Theragnosis". Polymers. 12 (6): 1397. doi:10.3390/polym12061397. ISSN 2073-4360. PMC 7362228. PMID 32580366.
- Han, Hyounkoo; Kim, Doyeon; Jang, Yongho; Seo, Minkyu; Kim, Kwangmeyung; Lee, Jong Bum; Kim, Hyuncheol (Jun 2020). "Focused ultrasound-triggered chemo-gene therapy with multifunctional nanocomplex for enhancing therapeutic efficacy". Journal of Controlled Release. 322: 346–356. doi:10.1016/j.jconrel.2020.03.041. PMID 32243982. S2CID 214785305.