| Revision as of 12:24, 26 December 2009 edit99.191.74.146 (talk) duplicate wikilinks in intro← Previous edit | Latest revision as of 01:18, 22 December 2024 edit undoMitch Ames (talk | contribs)Autopatrolled, Extended confirmed users, Pending changes reviewers186,520 edits Sentence case, per MOS:CAPSTag: AWB | ||
| (887 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Chronic disorder related to the Gulf War}} | |||
| {{POV}} | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| {{Infobox |
{{Infobox medical condition | ||
| | name = Gulf War syndrome | |||
| | synonym = Chronic multisymptom illness<ref>{{cite web |url=http://www.nationalacademies.org/hmd/Reports/2013/Gulf-War-and-HealthTreatment-for-Chronic-Multisymptom-Illness.aspx |title=Persian Gulf War and Health: Treatment for Chronic Multisymptom Illness |department=Health and Medicine Division |website=nationalacademies.org |url-status=live |archive-url=https://web.archive.org/web/20170511120553/http://www.nationalacademies.org/hmd/Reports/2013/Gulf-War-and-HealthTreatment-for-Chronic-Multisymptom-Illness.aspx |archive-date=2017-05-11 |df=dmy-all}}</ref><ref>{{cite web |url=https://usiraq.procon.org/sourcefiles/riegle-rpt.pdf |title=U.S. Chemical and Biological Warfare-related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Persian Gulf War |quote=A Report of Chairman ], and Ranking Member ] of the ] with respect to Export Administration – ] |date=May 25, 1994 |publisher=]}}</ref> | |||
| |Image = Pyridostigmine.svg | |||
| | image = DesertStormMap v2.svg | |||
| |Caption = nerve agent antidote pyridostigmine, <br /> an implicated toxin | |||
| | image_size = 350px | |||
| |ICD9 = {{ICD9|V65.5}} (inconclusive) <br /> also nonstandard "DX111" | |||
| |
| alt = | ||
| | caption = Summary of the ] offensive ground campaign, February 24–28, 1991, by nationality | |||
| | pronounce = | |||
| | specialty = <!--from Wikidata; can be overwritten--> | |||
| | symptoms = Vary somewhat among individuals and include fatigue, headaches, cognitive dysfunction, musculoskeletal pain, insomnia,<ref name=VA_med_unexpl_ill/> and respiratory, gastrointestinal, and dermatologic complaints | |||
| | complications = | |||
| | onset = | |||
| | duration = | |||
| | types = | |||
| | causes = Toxic exposures during the 1990–91 Persian Gulf War. See Congressional records for testimony about chemical weapon disposal accident. | |||
| | risks = | |||
| | diagnosis = | |||
| | differential = ] (ME/CFS); ]; ] (MS) | |||
| | prevention = | |||
| | treatment = | |||
| | medication = | |||
| | prognosis = | |||
| | frequency = 25% to 34% of the 697,000 U.S. troops of the 1990–91 Gulf War | |||
| | deaths = | |||
| }} | }} | ||
| '''Gulf War syndrome''' ('''GWS''') also known as '''Gulf War Illness''' or '''Chronic Multi-symptom Illness''', is a chronic and multi-symptomatic disorder affecting military veterans of both sides of the ] (1990–1991).<ref name="veteranIllnesses" /><ref>{{cite journal | vauthors = Iversen A, Chalder T, Wessely S | title = Gulf War Illness: lessons from medically unexplained symptoms | journal = Clinical Psychology Review | volume = 27 | issue = 7 | pages = 842–854 | date = October 2007 | pmid = 17707114 | doi = 10.1016/j.cpr.2007.07.006 }}</ref><ref>{{cite journal | vauthors = Gronseth GS | title = Gulf war syndrome: a toxic exposure? A systematic review | journal = Neurologic Clinics | volume = 23 | issue = 2 | pages = 523–540 | date = May 2005 | pmid = 15757795 | doi = 10.1016/j.ncl.2004.12.011 }}</ref> A wide range of acute and chronic symptoms have been linked to it, including ], ], cognitive problems, insomnia,<ref name="VA_med_unexpl_ill">{{cite web |url=https://www.publichealth.va.gov/exposures/gulfwar/medically-unexplained-illness.asp |title=Persian Gulf War Veterans' Medically Unexplained Illnesses |series=Public Health |publisher=U.S. Department of Veterans Affairs |department=Veterans Health |language=en}}</ref> rashes and ].<ref>{{cite web |publisher=] |title=Gulf War Syndrome |url=http://www.healthsystem.virginia.edu/uvahealth/adult_environ/gulf.cfm |archive-url=https://web.archive.org/web/20040714014747/http://www.healthsystem.virginia.edu/UVAHealth/adult_environ/gulf.cfm |archive-date=2004-07-14 |df=dmy-all}}</ref> Approximately 250,000<ref name="www8.nationalacademies.org">{{cite web |url=http://www8.nationalacademies.org/onpinews/newsitem.aspx?RecordID=12835 |title=Gulf War service linked to post-traumatic stress disorder, multisymptom illness, other health problems, but causes are unclear |access-date=2012-05-09 |publisher=] |date=2010-04-09 | vauthors = Stencel C |url-status=live |archive-url=https://web.archive.org/web/20120314071134/http://www8.nationalacademies.org/onpinews/newsitem.aspx?RecordID=12835 |archive-date=2012-03-14 |df=dmy-all}}</ref> of the 697,000 U.S. veterans who served in the Gulf War have enduring chronic multi-symptom illness, a condition with serious consequences.<ref name=FedReport>{{cite web |url=http://www.va.gov/gulfwaradvisorycommittee/docs/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |title=Gulf War Illness and the Health of Persian Gulf War Veterans: Scientific Findings and Recommendations |author=Research Advisory Committee on Gulf War Veterans' Illnesses |access-date=2012-05-09 |date=2008-11-01 |publisher=U.S. Department of Veterans Affairs |url-status=live |archive-url=https://web.archive.org/web/20131109141703/http://www.va.gov/gulfwaradvisorycommittee/docs/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2013-11-09 |df=dmy-all}}</ref> From 1995 to 2005, the health of combat veterans worsened in comparison with nondeployed veterans, with the onset of more new chronic diseases, functional impairment, repeated clinic visits and hospitalizations, ]-like illness, ], and greater persistence of adverse health incidents.<ref>{{cite journal | vauthors = Li B, Mahan CM, Kang HK, Eisen SA, Engel CC | title = Longitudinal health study of US 1991 Gulf War veterans: changes in health status at 10-year follow-up | journal = American Journal of Epidemiology | volume = 174 | issue = 7 | pages = 761–768 | date = October 2011 | pmid = 21795757 | doi = 10.1093/aje/kwr154 | doi-access = free }}</ref> | |||
| '''Gulf War syndrome''' (GWS) or '''Gulf War illness''' (GWI) affects ] and civilians who were near conflicts during, and downwind of a ] depot demolition after, the 1991 ].<ref>Iversen A, Chalder T, Wessely S. "Gulf War Illness: lessons from medically unexplained symptoms." Clin Psychol Rev. 2007 Oct;27(7):842-54.</ref><ref>Gronseth GS. "Gulf war syndrome: a toxic exposure? A systematic review." Neurol Clin. 2005 May;23(2):523-40.</ref> A wide range of acute and chronic symptoms have included ], loss of muscle control, ]s, dizziness and loss of balance, memory problems, muscle and ], ], skin problems, and ].<ref>University of Virginia. </ref> Roughly 1 in 4 of the 697,000 veterans who served in the first Gulf War are afflicted with the disorder, a real condition with real causes and serious consequences.<ref name=FedReport></ref> | |||
| Exposure to toxic chemicals is the cause of the illness. Several specific causes have been investigated, including ] nerve gas antidote, ] pesticides, chemical weapons, and ]. Causes which have been ruled out include ], ], and ].<ref name=FedReport/> Antidote pills given to protect troops from ] and insect repellents used during deployment were most closely linked.<ref name=FedReport/> Exposure to the destruction of the ], where large quantities of the chemical weapon ] was stored, is negatively correlated with motor speed.<ref name=Toomey>Toomey ''et al'' (2009) "Neuropsychological functioning of U.S. Gulf War veterans 10 years after the war" ''J Int Neuropsychol Soc'' PMID 19640317</ref> Epidemiological evidence is consistent with increased risk of birth defects in the offspring of persons exposed to depleted uranium.<ref name="Hindin">Hindin, R. ''et al.'' (2005) ''Environmental Health,'' vol. 4, pp. 17. </ref> | |||
| While the treatment of sarin exposure has been studied,<ref name=Schecter>Schecter, WP (2004) "Cholinergic symptoms due to nerve agent attack: a strategy for management." ''Anesthesiol Clin North America'' '''22'''(3):579-90. PMID 15325720</ref> other ]s such as pyridostigmine bromide and organophosphate insect repellents may or may not involve similar management. ] can be decontaminated from steel surfaces<ref name=Francis>Francis, A.J. (2005) "Decontamination of uranium-contaminated steel surfaces by hydroxycarboxylic acid with uranium recovery." ''Environ Sci Technol'' '''39'''(13):5015-21. PMID 16053105</ref> and aquifers.<ref name=Wu>Wu, W.M. ''et al'' (2006) "Pilot-scale in situ bioremedation of uranium in a highly contaminated aquifer. 2. Reduction of u(VI) and geochemical control of u(VI) bioavailability." ''Environ Sci Technol'' '''40'''(12):3986-95. PMID 16830572</ref> Diplomatic reconciliation is a means of prevention.<ref name=Curle>Curle, A. (1997) "Public mental health. III: Hatred and reconciliation." ''Med Confl Surviv'' '''13'''(1):37-47. PMID 9080785</ref><ref name=Jentleson>Jentleson, B.W. (1996) UC Berkeley Policy Paper 27, ''Institute on Global Conflict and Cooperation''</ref> | |||
| ==Classification== | |||
| Medial ailments associated with Gulf War Syndrome has been recognized by both the US Department of Defense, Department of Veterans Affairs, and Veterans Administration.<ref></ref> Since so little concrete information was known about this condition the Veterans administrations originally classified individuals with related ailments believed to be connected to their service in the Persian Gulf a special non-ICD-9 code DX111, as well as ICD-9 code V65.5.<ref>Department of Veterans Affairs </ref> | |||
| ==Signs and symptoms== | |||
| Gulf War illness is linked to exposure to sub-lethal amounts of organophosphates, particularly ].<ref name=":7">{{cite journal | vauthors = Cruz-Hernandez A, Roney A, Goswami DG, Tewari-Singh N, Brown JM | title = A review of chemical warfare agents linked to respiratory and neurological effects experienced in Gulf War Illness | journal = Inhalation Toxicology | volume = 34 | issue = 13–14 | pages = 412–432 | date = November 2022 | pmid = 36394251 | pmc = 9832991 | doi = 10.1080/08958378.2022.2147257 | bibcode = 2022InhTx..34..412C }}</ref><ref name=":8">{{cite journal | vauthors = Weisskopf MG, Sullivan KA | title = Invited Perspective: Causal Implications of Gene by Environment Studies Applied to Gulf War Illness | journal = Environmental Health Perspectives | volume = 130 | issue = 5 | pages = 51301 | date = May 2022 | pmid = 35543506 | pmc = 9093160 | doi = 10.1289/EHP11057 }}</ref><ref name=":9">{{cite web |date=May 11, 2022 |title=UTSW genetic study confirms sarin nerve gas as cause of Gulf War illness |url=https://www.utsouthwestern.edu/newsroom/articles/year-2022/sarin-nerve-gas-gulf-war-illness.html |website=UT Southwestern Medical Center}}</ref> Exposure to pesticides containing other organophosphates and exposure to pills containing ], used as a pretreatment to protect against ] effects, has been found to be associated with the neurological effects seen in Persian Gulf War syndrome.<ref name=":0" /><ref name=":5">{{cite journal | vauthors = White RF, Steele L, O'Callaghan JP, Sullivan K, Binns JH, Golomb BA, Bloom FE, Bunker JA, Crawford F, Graves JC, Hardie A, Klimas N, Knox M, Meggs WJ, Melling J, Philbert MA, Grashow R | title = Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: Effects of toxicant exposures during deployment | journal = Cortex; A Journal Devoted to the Study of the Nervous System and Behavior | volume = 74 | pages = 449–475 | date = January 2016 | pmid = 26493934 | pmc = 4724528 | doi = 10.1016/j.cortex.2015.08.022 | df = dmy-all | series = What's your poison? Neurobehavioural consequences of exposure to industrial, agricultural and environmental chemicals }}</ref> Other potential causes that have been investigated are ] and emissions from ]s, but their relationships to the illness are not as clear.<ref name=":0" /><ref name=":5" /> Gulf War illness is not the result of combat or other stressors, and Gulf War veterans have lower rates of ] (PTSD) than veterans of other wars.<ref name="FedReport" /><ref name=":0">{{Cite book |url=https://www.va.gov/RAC-GWVI/RACReport2014Final.pdf |title=Gulf War Illness and the Health of Persian Gulf War Veterans: Research Update and Recommendations, 2009–2013: Updated Scientific Findings and Recommendations |collaboration=Research Advisory Committee on Gulf War Veterans' Illnesses |date=May 2014 |location=Washington, DC |pages=3, 9–10, 20 |publisher=U.S. Department of Veterans Affairs}}</ref> | |||
| ] offensive ground campaign, February 24-28, 1991, by nationality (click for detail).]] | |||
| The ] said research suggested up to 33,000 UK Gulf War veterans could be living with Gulf War illness,<ref>{{cite web |date=20 February 2020 |title=What is Persian Gulf War Illness? |url=https://www.britishlegion.org.uk/stories/what-is-gulf-war-illness |access-date=25 May 2021 |website=Royal British Legion}}</ref> with 1,300 claiming a war pension for conditions connected to their service.<ref>{{cite news |date=18 February 2021 |title=Gulf War syndrome 'not caused by depleted uranium' |url=https://www.bbc.co.uk/news/uk-56116101 |access-date=24 February 2021 |work=BBC News}}</ref> In 2007 the Royal British Legion produced a comprehensive report entitled ''Legacy of Suspicion'',<ref>{{cite web |title=Gulf War: a legacy of suspicion |url=https://storage.rblcdn.co.uk/sitefinity/docs/default-source/campaigns-policy-and-research/gulf_war_legacy_of_suspicion.pdf |access-date=25 May 2021 |website=Royal British Legion}}</ref> which made recommendations about necessary research and compensation. The Royal British Legion is still campaigning for the UK government to properly address symptoms experienced by veterans of the Gulf War.<ref>{{cite web |date=8 February 2019 |title=Gulf War illnesses |url=https://www.britishlegion.org.uk/get-involved/things-to-do/campaigns-policy-and-research/campaigns/gulf-war-illnesses |access-date=25 May 2021 |website=Royal British Legion}}</ref> | |||
| About one-fourth of the 697,000 U.S. servicemen and women in the first Gulf War have shown symptoms related to Gulf War Syndrome. | |||
| According to a 2013 report by the ], veterans of the U.S. wars in ] and ] may also have Gulf War illness,<ref>{{cite news |url=http://www.armytimes.com/mobile/news/2013/01/gannett-new-vets-showing-gulf-war-illness-symptoms-012313 |title=Report: New vets show Gulf War illness symptoms |author=Kennedy, Kelly |date=23 January 2013 |newspaper=Army Times |access-date=28 January 2013 |agency=USA Today}}{{dead link|date=March 2024}}</ref> though later findings identified causes that would not have been present in those wars.<ref name=":0" /><ref name=":5" /> | |||
| U.S. and UK, with the highest rates of excess illness, are distinguished from the other nations by higher rates of ] use, use of ] ], and somewhat higher rates of exposures to oil fire ] and reported chemical alerts. France, with possibly the lowest illness rates, had lower rates of pesticide use, and no use of anthrax vaccine.<ref> December 12-13, 2005 Committee Meeting Minutes (page 78)</ref> French troops also served to the North and West of all other combat troops, away and upwind of major combat engagements<ref> December 12-13, 2005 Committee Meeting Minutes (page 68)</ref> . | |||
| == Signs and symptoms == | |||
| A 2001 study of 15,000 February 1991 U.S. ] combat veterans and 15,000 control veterans found that the Gulf War veterans were 1.8 (fathers) to 2.8 (mothers) times more likely to have children with birth defects.<ref>{{cite journal | |||
| According to an April 2010 U.S. Department of Veterans Affairs (VA) sponsored study conducted by the Institute of Medicine (IOM), part of the U.S. ], 250,000<ref name="www8.nationalacademies.org" /> of the 696,842 U.S. servicemen and women in the 1991 Gulf War continue to be affected by chronic multi-symptom illness, which the IOM now refers to as ''Gulf War illness''. The IOM found that it continued to affect these veterans nearly 20 years after the war.{{citation needed|date=August 2020}} | |||
| | author = Kang, H., ''et al.' | |||
| | year = 2001 | |||
| | url = http://www.annalsofepidemiology.org/article/PIIS1047279701002459/abstract | |||
| | title = Pregnancy Outcomes Among U.S. Gulf War Veterans: A Population-Based Survey of 30,000 Veterans | |||
| | journal = ''Annals of Epidemiology'' | |||
| | volume = 11 | |||
| | issue = 7 | |||
| | pages = 504–511 | |||
| | pmid = 11557183 | doi = 10.1016/S1047-2797(01)00245-9 | |||
| }}</ref> After examination of children's medical records two years later, the birth defect rate increased by more than 20%: | |||
| According to the IOM, "It is clear that a significant portion of the soldiers deployed to the Gulf War have experienced troubling constellations of symptoms that are difficult to categorize," said committee chair Stephen L. Hauser, professor and chair, department of neurology, ] (UCSF). {{blockquote|Unfortunately, symptoms that cannot be easily quantified are sometimes incorrectly dismissed as insignificant and receive inadequate attention and funding by the medical and scientific establishment. Veterans who continue to suffer from these symptoms deserve the very best that modern science and medicine can offer to speed the development of effective treatments, cures, and—we hope—prevention. Our report suggests a path forward to accomplish this goal, and we believe that through a concerted national effort and rigorous scientific input, answers can be found.<ref name="www8.nationalacademies.org" />}} | |||
| <blockquote>"Dr. Kang found that male Gulf War veterans reported having infants with likely birth defects at twice the rate of non-veterans. Furthermore, female Gulf War veterans were almost three times more likely to report children with birth defects than their non-Gulf counterparts. The numbers changed somewhat with medical records verification. However, Dr. Kang and his colleagues concluded that the risk of birth defects in children of deployed male veterans still was about 2.2 times that of non-deployed veterans."<ref>Department of Veterans Affairs (2003) ''Gulf War Review'' '''12'''(1), p. 10.</ref></blockquote> | |||
| Questions still exist regarding why certain veterans showed, and still show, medically unexplained symptoms while others did not, why symptoms are diverse in some and specific in others, and why combat exposure is not consistently linked to having or not having symptoms. The lack of data on veterans' pre-deployment and immediate post-deployment health status and lack of measurement and monitoring of the various substances to which veterans may have been exposed make it difficult—and in many cases impossible—to reconstruct what happened to service members during their deployments nearly 20 years after the fact, the committee noted.<ref name="www8.nationalacademies.org" /> The report called for a substantial commitment to improving identification and treatment of multisymptom illness in Gulf War veterans focussing on continued monitoring of Gulf War veterans, improved medical care, examination of genetic differences between symptomatic and asymptomatic groups and studies of environment-gene interactions.<ref name="www8.nationalacademies.org" /> | |||
| In a study of U.K. troops, "Overall, the risk of any malformation among pregnancies reported by men was 50% higher in Gulf War Veterans (GWV) compared with Non-GWVs."<ref>Doyle, P., ''et al.'' (2004) ''International Journal of Epidemiology,'' '''33'''(1), pp. 74-86; PMID 15075150.</ref> | |||
| A variety of signs and symptoms have been associated with GWI: | |||
| {|class="wikitable sortable" style="font-size:97%; text-align:right;" | {|class="wikitable sortable" style="font-size:97%; text-align:right;" | ||
| |+Excess prevalence of general ]s<ref name=RAC_GWVI_Minutes_2005/>{{rp|page=70}} '''*''' | |||
| |+Excess prevalence of general ]s<ref> December 12-13, 2005 Committee Meeting Minutes (page 70), ''This table applies only to coalition forces involved in ].''</ref>'''*''' | |||
| !width="200px"| Symptom | !width="200px"| Symptom | ||
| !width="50px"| U.S. | !width="50px"| U.S. | ||
| Line 60: | Line 61: | ||
| |align="left"|Diarrhea||16%|| ||9%||13% | |align="left"|Diarrhea||16%|| ||9%||13% | ||
| |- | |- | ||
| |align="left"|Dyspepsia/indigestion||12%|| ||5%||9% | |align="left"|]/indigestion||12%|| ||5%||9% | ||
| |- | |- | ||
| |align="left"|Neurological problems||16%|| ||8%||12% | |align="left"|Neurological problems||16%|| ||8%||12% | ||
| Line 66: | Line 67: | ||
| |align="left"|Terminal tumors||33%|| ||9%||11% | |align="left"|Terminal tumors||33%|| ||9%||11% | ||
| |} | |} | ||
| ::<small>'''*''' ''This table applies only to coalition forces involved in ].''</small> | |||
| . This version from data by same author(s) in Wilcock, A.R., ed. (2004) "Uranium in the Wind" (Ontario: Pandora Press) ISBN 097361532X</ref>]] | |||
| {|class="wikitable sortable" style="font-size:97%; text-align:right;" | {|class="wikitable sortable" style="font-size:97%; text-align:right;" | ||
| |+Excess prevalence of recognized medical conditions<ref> |
|+Excess prevalence of recognized medical conditions<ref name=RAC_GWVI_Minutes_2005/>{{rp|page=71}} | ||
| !width="200px"| Condition | !width="200px"| Condition | ||
| !width="50px"| U.S. | !width="50px"| U.S. | ||
| Line 76: | Line 78: | ||
| |- | |- | ||
| |align="left"|Skin conditions | |align="left"|Skin conditions | ||
| |{{sort|20| |
|{{sort|20|20–21%}} ||21% ||{{sort|04|4–7%}} ||4% | ||
| |- | |- | ||
| |align="left"|Arthritis/joint problems | |align="left"|Arthritis/joint problems | ||
| |{{sort|06| |
|{{sort|06|6–11%}} ||10% ||{{sort|0|(-1)–3%}} ||2% | ||
| |- | |- | ||
| |align="left"|Gastro-intestinal (GI) problems | |align="left"|Gastro-intestinal (GI) problems | ||
| |{{sort|15|15%}} || ||{{sort|05| |
|{{sort|15|15%}} || ||{{sort|05|5–7%}} ||1% | ||
| |- | |- | ||
| |align="left"|Respiratory problem | |align="left"|Respiratory problem | ||
| |{{sort|04| |
|{{sort|04|4–7%}} ||2% ||{{sort|02|2–5%}} ||1% | ||
| |- | |- | ||
| |align="left"|Chronic fatigue syndrome | |align="left"|Chronic fatigue syndrome | ||
| |{{sort|01| |
|{{sort|01|1–4%}} ||3% || ||0% | ||
| |- | |- | ||
| |align="left"|Post-traumatic stress disorder | |align="left"|Post-traumatic stress disorder | ||
| |{{sort|02| |
|{{sort|02|2–6%}} ||9% ||{{sort|06|6%}} ||3% | ||
| |- | |- | ||
| |align="left"|Chronic multi-symptom illness | |align="left"|Chronic multi-symptom illness | ||
| |{{sort|13| |
|{{sort|13|13–25%}} ||26% || || | ||
| |} | |} | ||
| Birth defects have been suggested as a consequence of Gulf War deployment. However, a 2006 review of several studies of international coalition veterans' children found no strong or consistent evidence of an increase in birth defects, finding a modest increase in birth defects that was within the range of the general population, in addition to being unable to exclude ] as an explanation for the results.<ref name="DoyleReview">{{cite journal | vauthors = Doyle P, Maconochie N, Ryan M | title = Reproductive health of Gulf War veterans | journal = Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences | volume = 361 | issue = 1468 | pages = 571–584 | date = April 2006 | pmid = 16687262 | pmc = 1569619 | doi = 10.1098/rstb.2006.1817 }}</ref> A 2008 report stated that "it is difficult to draw firm conclusions related to birth defects and pregnancy outcomes in Gulf War veterans", observing that while there have been "significant, but modest, excess rates of birth defects in children of Gulf War veterans", the "overall rates are still within the normal range found in the general population".<ref name=GWV_08_p50>{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=50 (p. 60 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref> The same report called for more research on the issue. | |||
| Although Gulf War illness is the most prominent condition affecting Gulf War veterans, it is just one health issue to be addressed in the larger context of the health of Gulf War veterans. Other Gulf War-related health issues of importance include rates of diagnosable medical conditions and post-war mortality among Gulf War veterans, and questions related to the risk of birth defects and other health problems in veterans’ family members. The three studies most representative of Gulf War era veterans in the U.S. and U.K. have all indicated significant excess rates of birth defects in children of Gulf War veterans. News articles have reported that rates of cancer and birth defects in Iraq increased dramatically during the 1990s, specifically in regions where the greatest quantity of ] was used in the Gulf War. Conference reports describing an increased incidence of congenital anomalies in Basrah and increased numbers of cancer cases, both in Iraqi military personnel who served in the war and in four Iraqi hospitals, lend some support to these contentions.<ref name="FedReport" /> | |||
| === Comorbid illnesses === | |||
| ==Causes== | |||
| Persian Gulf War veterans have been identified to have an increased risk of ].<ref>{{cite web |url=http://www.va.gov/ms/documents/Wallin_MS_Cohort_Incidence_Brain_2012.pdf |title=The Gulf War era multiple sclerosis cohort: age and incidence rates by race, sex and service |website=va.gov |archive-url=https://web.archive.org/web/20161113032416/http://www.va.gov/ms/documents/Wallin_MS_Cohort_Incidence_Brain_2012.pdf |archive-date=2016-11-13 |df=dmy-all |access-date=2016-11-12 }}</ref> | |||
| The ] mandated the ] ] to provide nine reports on Gulf War Syndrome since 1998.<ref></ref> Aside from the many physical and psychological issues involving any war zone deployment, Gulf War veterans were exposed to a unique mix of hazards not previously experienced during wartime. These included ] pills given to protect troops from the effects of nerve agents, ], and ] and ] vaccines. The oil and smoke that spewed for months from hundreds of burning oil wells presented another exposure hazard not previously encountered in a warzone. Military personnel also had to cope with swarms of insects, requiring the widespread use of pesticides. | |||
| A 2017 study by the U.S. Department of Veterans Affairs found that veterans possibly exposed to chemical warfare agents at ] experienced different patterns of brain cancer mortality risk compared to the other groups, with veterans possibly exposed having a higher risk of brain cancer in the time period immediately following the Gulf War.<ref>{{cite journal | vauthors = Barth SK, Dursa EK, Bossarte RM, Schneiderman AI | title = Trends in brain cancer mortality among U.S. Gulf War veterans: 21 year follow-up | journal = Cancer Epidemiology | volume = 50 | issue = Pt A | pages = 22–29 | date = October 2017 | pmid = 28780478 | pmc = 5824993 | doi = 10.1016/j.canep.2017.07.012 }}</ref> | |||
| United States Veterans Affairs Secretary ]'s panel found that pre-2005 studies suggested the veterans' illnesses are neurological and apparently are linked to exposure to ], such as the nerve gas ], the anti-nerve gas drug ], and ]s that affect the nervous system. The review committee concluded that "Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans," the review committee said.<ref></ref> | |||
| ===Iraqi veterans=== | |||
| ===Pyridostigmine bromide nerve gas antidote=== | |||
| Although an understudied group, opposing Iraqi veterans of the ] in the Gulf War also experienced acute and chronic symptoms associated with Gulf War syndrome. A 2011 study in the U.S. Army Medical Department Journal reported Iraqi veterans of the Gulf War had a higher prevalence of somatic disorders as compared to Iraqi civilians, with risk greater in troops stationed in Kuwait.<ref name="USAMDJ2011">{{cite journal | vauthors = Jamil H, Hamdan TA, Grzybowski M, Arnetz BB | title = Health effects associated with geographical area of residence during the 1991 Gulf War: a comparative health study of Iraqi soldiers and civilians | journal = U.S. Army Medical Department Journal | pages = 87–96 | date = 2011 | pmid = 21805460 | pmc = 3159173 }}</ref> | |||
| In comparison to Allied troops, health symptoms were similar amongst Iraqi veterans: | |||
| The US military issued ] pills, PB, to protect against exposure to nerve gas agents such as ] and ]. PB was used to pretreat nerve agent poisoning and is not a vaccine however taken before exposure to nerve agents, PB was thought to increase the efficacy of nerve agent antidotes. PB had been used since 1955 for patients suffering from ] with dosed up to 1,500 mg a day, far in excess of the 90 mg given to soldiers, and was considered safe by the FDA at either level for indefinite use and its use to pretreat nerve agent exposure has recently been approved.<ref>PBS Frontline. </ref> | |||
| {| class="wikitable" | |||
| |+Risk of health symptoms<ref name=USAMDJ2011/> | |||
| |- | |||
| ! Symptom !! Odds ratios (95% CI) - Zone 1 vs Zone 3 | |||
| |- | |||
| | Headaches || 3.65 (2.51–5.31) | |||
| |- | |||
| | Respiratory disorder || 4.09 (2.60–6.43) | |||
| |- | |||
| | Genitourinary disorder || 4.06 (2.65–6.21) | |||
| |- | |||
| | Musculoskeletal disorder || 4.33 (2.96–6.33) | |||
| |- | |||
| | Chronic fatigue || 126.3 (29.9–532.8) | |||
| |- | |||
| | Skin disorders|| 1.89 (1.24–2.87) | |||
| |- | |||
| | Miscellaneous disorders || 4.43 (2.44–8.05) | |||
| |} | |||
| ::<small>'''*''' ''Zone 1 = In Kuwait, Zone 3 = 360 km from Kuwait.''</small> | |||
| == Causes == | |||
| About half of U.S. Gulf War veterans report using PB during deployment, with greatest use among Army personnel. Concerns have been raised about the possibility of increased health problems from PB when it is combined with other risk factors. | |||
| Many of the symptoms of Gulf War illness are similar to the symptoms of organophosphate, ], and ] poisoning.<ref name="Friis">{{cite book | vauthors = Friis RH, Sellers TA |url=https://archive.org/details/epidemiologyforp00robe |title=Epidemiology for Public Health Practice |publisher=Jones & Bartlett Publishers |year=2004 |isbn=978-0-7637-3170-0}}</ref><ref>{{cite book | vauthors = Spektor DM, Rettig RA, Hilborne LH, Golomb BA, Marshall GN, Davis LM, Sherbourne CD, Harley NH, Augerson WS, Cecchine G | title = A Review of the Scientific Literature as it Pertains to Gulf War Illnesses|date=1998 |publisher=] |isbn=978-0-8330-2680-4 }}</ref> Gulf War veterans were exposed to a number of sources of these compounds, including nerve gas and ]s.<ref>{{cite news |date=November 13, 2004 |title=Campaigners hail 'nerve gas link' to Gulf War Syndrome |url=http://www.scotsman.com/news/uk/campaigners_hail_nerve_gas_link_to_gulf_war_syndrome_1_1046500 |url-status=live |archive-url=https://web.archive.org/web/20120213230705/http://www.scotsman.com/news/uk/campaigners_hail_nerve_gas_link_to_gulf_war_syndrome_1_1046500 |archive-date=February 13, 2012 |access-date=November 24, 2009 |newspaper=The Scotsman |location=Edinburgh, UK |df=dmy-all}}</ref> In 2022, researchers led by Robert Haley, MD at ] found that exposure to sarin nerve gas in soldiers who had a particular genetic mutation that prevented them from breaking down the nerve gas is likely to be responsible for the syndrome.<ref name=":9" /> The findings and an editorial by two leading epidemiologists were published in '']''.<ref name=":8" /> | |||
| The ] mandated the ]' contract with the ] (NAS) to provide reports on Gulf War illnesses. Between 1998 and 2009, the NAS's Institute of Medicine (IOM) authored ten such reports.<ref>{{cite web |url=http://www.publichealth.va.gov/exposures/gulfwar/announcement.asp |title=Gulf War exposures announcement |website=publichealth.va.gov |url-status=live |archive-url=https://web.archive.org/web/20091218093021/http://www.publichealth.va.gov/exposures/gulfwar/announcement.asp |archive-date=2009-12-18 |df=dmy-all}}</ref> In addition to the many physical and psychological issues involved in any war zone deployment, Gulf War veterans were exposed to a unique mix of hazards not previously experienced during wartime. These included ] pills (given to protect troops from the effects of nerve agents), depleted uranium munitions, and multiple simultaneous vaccinations including ] and ] toxin vaccines. The oil and smoke that spewed for months from hundreds of burning oil wells presented another exposure hazard not previously encountered in a war zone. Military personnel also had to cope with swarms of insects, requiring the widespread use of pesticides. High-powered microwaves were used to disrupt Iraqi communications, and though it is unknown whether this might have contributed to the syndrome, research has suggested that safety limits for electromagnetic radiation are too lenient.<ref>{{cite report |url=http://www.veterans.senate.gov/hearings.cfm?action=release.display&release_id=a22ac85f-bc73-435f-b78b-3b107a51cf87 |title=Gulf War Illnesses |year=2007 |publisher=U.S. Senate Veterans Affairs Committee |archive-url=https://web.archive.org/web/20130227190650/http://veterans.senate.gov/hearings.cfm?action=release.display&release_id=a22ac85f-bc73-435f-b78b-3b107a51cf87 |archive-date=2013-02-27 |df=dmy-all}}, Testimony to the Senate Veterans Affairs Committee by Meryl Nass, MD on September 25, 2007</ref> | |||
| Given both the large body of epidemiological data on myasthenia gravis patients and follow up studies done on veterans it was concluded that while it was unlikely that health effects reported today by Gulf War veterans are the result of exposure solely to PB, use of PB was ] with illness.<ref name=FedReport/> | |||
| The Research Advisory Committee on Gulf War Veterans' Illnesses (RAC), a VA federal advisory committee mandated by Congress in legislation enacted in 1998,<ref name=":6" /><ref name=":4" /> found that pre-2005 studies suggested the veterans' illnesses are neurological and apparently are linked to exposure to ]s, such as the nerve gas sarin, the anti-nerve gas drug pyridostigmine bromide, and pesticides that affect the nervous system. The RAC concluded in 2004 that, "research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans."<ref>{{cite web |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/ReportandRecommendations_ScientificProgressinUnderstandingGWVI_2004.pdf |collaboration=Research Advisory Committee on Gulf War Veterans' Illnesses |date=September 2004 |title=Scientific Progress in Understanding Gulf War Veterans' Illnesses: Report and Recommendations |publisher=United States Department of Veterans Affairs |access-date=2012-05-09 |url-status=live |archive-url=https://web.archive.org/web/20120319024036/http://www.va.gov/RAC-GWVI/docs/Committee_Documents/ReportandRecommendations_ScientificProgressinUnderstandingGWVI_2004.pdf |archive-date=2012-03-19 |df=dmy-all}}</ref> | |||
| ===Organophosphate pesticides=== | |||
| The use of ] ] and ] during the first Gulf War is credited with keeping rates of pest-borne diseases low. Pesticide use is one of only two exposures consistently identified by Gulf War epidemiologic studies to be significantly associated with Gulf War illness.<ref>U.S. Department of Defense, Office of the Special Assistant to the Undersecretary of Defense (Personnel and Readiness) for Gulf War Illnesses Medical Readiness and Military Deployments. Environmental Exposure Report: Pesticides Final Report. Washington, D.C. April 17, 2003.</ref> Multisymptom illness profiles similar to Gulf War illness have been associated with low-level pesticide exposures in other human populations. In addition, Gulf War studies have identified dose-response effects, indicating that greater pesticide use is more strongly associated with Gulf War illness than more limited use.<ref>Krengel M, Sullivan K. Neuropsychological Functioning in Gulf War Veterans Exposed to Pesticides and Pyridostigmine Bromide. Fort Detrick, MD: U.S. Army Medical Research and Materiel Command; August, 2008. W81XWH-04-1-0118</ref> Pesticide use during the Gulf War has also been associated with ] deficits and ] alterations in Gulf War veterans in clinical studies conducted follownf the end of the war. The 2008 report concluded that “all available sources of evidence combine to support a consistent and compelling case that pesticide use during the Gulf War is causally associated with Gulf War illness.”<ref name=FedReport/> | |||
| The RAC concluded<ref name=":0" /> that "exposure to pesticides and/or to PB are causally associated with GWI and the neurological dysfunction in GW veterans. Exposure to ] and ] and to ] emissions are also associated with neurologically based health effects. Gene-environment interactions are likely to have contributed to development of GWI in deployed veterans. The health consequences of chemical exposures in the GW and other conflicts have been called "toxic wounds" by veterans. This type of injury requires further study and concentrated treatment research efforts that may also benefit other occupational groups with similar exposure-related illnesses."<ref name=":5" /> | |||
| ===Sarin nerve agent=== | |||
| ] | |||
| === Sarin nerve agent === | |||
| Many of the symptoms of Gulf War syndrome are similar to the symptoms of ], ], and ] poisoning.<ref name=Friis>{{cite book |title=Epidemiology for Public Health Practice |last=Friis |first=Robert H. |coauthors=Thomas A. Sellers |year=2004 |publisher=Jones & Bartlett Publishers |isbn=0763731706 }}</ref><ref>{{cite book |title=A Review of the Scientific Literature as it Pertains to Gulf War Illnesses |last=Spektor |first=Dalia M. |coauthors=Richard A. Rettig, Lee H. Hilborne, Beatrice Alexandra Golomb, Grant N. Marshall, L. M. Davis, Cathy Donald Sherbourne, Naomi H. Harley, William S. Augerson, Gary Cecchine, United States Dept. of Defense |year=1998 |publisher=Rand Corporation |isbn=0833026801 }}</ref> Gulf War veterans were exposed to a number of sources of these compounds, including ] and ].<ref>{{cite web|url=http://news.scotsman.com/topics.cfm?tid=847&id=1311632004 |title=Campaigners hail 'nerve gas link' to Gulf War Syndrome - Scotsman.com News |publisher=News.scotsman.com |date= |accessdate=2009-11-24}}</ref> | |||
| {{See also|Iraqi chemical weapons program}} | |||
| ]Low-level exposure to nerve agents has been suggested as the cause of GWI.<ref name=":7" /><ref name=":8" /><ref name=":9" /> In 1991, Chemical detection units from Czechoslovakia, France, and Britain confirmed chemical agents. French detection units detected chemical agents. Both Czech and French forces reported detections immediately to U.S. forces. U.S. forces detected, confirmed, and reported chemical agents; and U.S. soldiers were awarded medals for detecting chemical agents. The ] said that chemical alarms went off 18,000 times during the Gulf War. After the air war started on January 16, 1991, coalition forces were chronically exposed to low, nonlethal levels of chemical and biological agents released primarily by direct Iraqi attack via ]s, ]s, ], or aircraft ] and by fallout from allied bombings of Iraqi chemical warfare munitions facilities.<ref>{{citation | vauthors = Riegle DW |title=U.S. Chemical and Biological Warfare-Related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Gulf War |date=1994-02-09 |df=dmy-all |url=http://en.wikisource.org/Riegle_Report |access-date=2012-05-09 |archive-url=https://web.archive.org/web/20120706211735/http://en.wikisource.org/Riegle_Report |archive-date=2012-07-06 |url-status=live |publisher=] |author-link=Donald W. Riegle Jr.}}</ref> | |||
| In 1997, the US Government released an unclassified report that stated: | |||
| Chemical detection units from the Czech Republic, France, and Britain confirmed chemical agents. French detection units detected chemical agents. Both Czech and French forces reported detections immediately to U.S. forces. U.S. forces detected, confirmed, and reported chemical agents; and U.S. soldiers were awarded medals for detecting chemical agents. The ] said that chemical alarms went off 18,000 times during the Gulf War. After the air war started on January 16, 1991, coalition forces were chronically exposed to low but nonlethal levels of chemical and biological agents released primarily by direct Iraqi attack via ]s, ]s, ], or aircraft ] and by ] from allied bombings of Iraqi chemical warfare munitions facilities.<ref> </ref> | |||
| : "The ] (IC) has assessed that Iraq did not use chemical weapons during the Gulf war. However, based on a comprehensive review of intelligence information and relevant information made available by the United Nations Special Commission (UNSCOM), we conclude that chemical warfare (CW) agent was released as a result of US postwar demolition of rockets with chemical warheads in a bunker (called Bunker 73 by Iraq) and a pit in an area known as ]."<ref>{{cite web |author=Persian Gulf War Illnesses Task Force |date=April 9, 1997 |title=Khamisiyah: A Historical Perspective on Related Intelligence |url=https://fas.org/irp/gulf/cia/970409/cia_wp.html |archive-url=https://web.archive.org/web/20130722221240/https://fas.org/irp/gulf/cia/970409/cia_wp.html |archive-date=July 22, 2013 |access-date=March 29, 2015 |publisher=] |df=dmy-all}}</ref> | |||
| Over 125,000 U.S. troops and 9,000 U.K. troops were exposed to nerve gas and ] when the Iraqi depot in Khamisiyah was destroyed.{{citation needed|date=March 2015}} Studies have confirmed earlier suspicions that exposure to sarin, in combination with other contaminants such as pesticides and PB were related to reports of veteran illness. Estimates range from 100,000 to 300,000 individuals exposed to nerve agents.<ref name="Golomb08">{{cite journal | vauthors = Golomb BA | title = Acetylcholinesterase inhibitors and Gulf War illnesses | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 105 | issue = 11 | pages = 4295–4300 | date = March 2008 | pmid = 18332428 | pmc = 2393741 | doi = 10.1073/pnas.0711986105 | bibcode = 2008PNAS..105.4295G | doi-access = free }}</ref> | |||
| In 1997, the US Government released an unclassified report that stated, ''"The US Intelligence Community (IC) has assessed that Iraq did not use chemical weapons during the Gulf War. However, based on a comprehensive review of intelligence information and relevant information made available by the United Nations Special Commission (UNSCOM), we conclude that chemical warfare (CW) agent was released as a result of US postwar demolition of rockets with chemical warheads at several sites including ]"''. Over 125,000 U.S. troops and 9,000 UK troops were exposed to nerve gas and ] when the Iraqi depot in Khamisiyah was destroyed . | |||
| " <ref></ref> | |||
| The 2014 report by the U.S. Department of Veterans Affairs (VA) Research Advisory Committee on Gulf War illnesses (RAC) concluded that, "exposure to the nerve gas agents sarin/cyclosarin has been linked in two more studies to changes in structural magnetic resonance imaging findings that are associated with cognitive decrements, further supporting the conclusion from evidence reviewed in the 2008 report that exposure to these agents is etiologically important to the central nervous system dysfunction that occurs in some subsets of Gulf War veterans."<ref name=":0" /> | |||
| Recent studies have confirmed earlier suspicions that exposure that sarin, in combination with other contaminants such as pesticides and PB were related to reports of veteran illness. Estimates range from 100,000 to 300,000 individuals exposed to nerve agents <ref>Beatrice Alexandra Golomb.</ref><ref>Navy Times. </ref> | |||
| A 2022 study of 1,016 U.S. Gulf War veterans found evidence of a ] link between GWI and exposure to low levels of sarin, which was released into the air by coalition bombing of Iraqi chemical weapons facilities. Significantly, the study found an increased incidence of GWI not only among veterans who recounted hearing nerve agent alarms, but also among veterans with the RR or QR (as opposed to the QQ) forms of the ] gene, which produces an ] that deactivates organophosphates (including sarin) through ]. By contrast, GWI was ''inversely'' associated with higher levels of the type Q ], which is more efficient at breaking down sarin than its type R counterpart. The authors "found that the PON1 ] and hearing nerve agent alarms were independent and the findings robust to both measured and unmeasured ], supporting a mechanistic interaction. ... Moreover, the change in the combined effect from one category to the next was significantly greater than the sum of the independent effects of the environmental exposure and the genotype". Although organophosphate pesticides could have triggered the nerve agent alarms in use at the time and contributed to ] symptoms similar to GWI, Haley ''et al.'' ruled out pesticides as a primary cause of GWI, citing that pesticide use was "ubiquitous long before the approximately 10,000 alarms began sounding at the start of the air campaign when Coalition bombing of Iraqi chemical weapon facilities released the fallout cloud that reached U.S. troop concentrations just as sarin was detected at multiple sites," while "the PON1 R isoenzyme is the more efficient detoxifier of most pesticides."<ref>{{cite journal | vauthors = Haley RW, Kramer G, Xiao J, Dever JA, Teiber JF | title = Evaluation of a Gene-Environment Interaction of ''PON1'' and Low-Level Nerve Agent Exposure with Gulf War Illness: A Prevalence Case-Control Study Drawn from the U.S. Military Health Survey's National Population Sample | journal = Environmental Health Perspectives | volume = 130 | issue = 5 | pages = 57001 | date = May 2022 | pmid = 35543525 | pmc = 9093163 | doi = 10.1289/EHP9009 | publisher = ] }} cf. {{cite web |date=11 May 2022 |title=UTSW genetic study confirms sarin nerve gas as cause of Gulf War illness |url=https://www.utsouthwestern.edu/newsroom/articles/year-2022/sarin-nerve-gas-gulf-war-illness.html |access-date=11 May 2022 |publisher=] |quote=For Gulf War veterans with the QQ genotype, hearing nerve agent alarms—a proxy for chemical exposure—raised their chance of developing GWI by 3.75 times. For those with the QR genotype, the alarms raised their chance of GWI by 4.43 times. And for those with two copies of the R gene, inefficient at breaking down sarin, the chance of GWI increased by 8.91 times. Those soldiers with both the RR genotype and low-level sarin exposure were over seven times more likely to get GWI due to the interaction per se, over and above the increase in risk from both risk factors acting alone. For genetic epidemiologists, this number leads to a high degree of confidence that sarin is a causative agent of GWI.}}</ref> | |||
| ===Depleted uranium=== | |||
| === Earlier considered potential causes === | |||
| ] | |||
| ==== Depleted uranium ==== | |||
| ] (DU) was widely used in tank ] and ] ] for the first time in the ]. DU is a dense, weakly radioactive metal. Munitions made from it often burn when they impact a hard target, producing toxic ] products. Roughly 320 tons of DU were used during the February, 1991 conflict.<ref name="autogenerated6">Global Security. ````</ref> After military personnel began reporting unexplained health problems in the aftermath of the Gulf War, questions were raised about the health effect of exposure to depleted uranium. | |||
| ] | |||
| The Gulf War included the first widespread combat usage of ] (DU), in tank ] and ] ].<ref name="Globalsecurity">{{cite web |title=Depleted Uranium |publisher=GlobalSecurity.org |url=http://www.globalsecurity.org/military/systems/munitions/du.htm |date=nd |access-date=2012-05-09 |df=dmy-all |url-status=live |archive-url=https://web.archive.org/web/20120119045145/http://www.globalsecurity.org/military/systems/munitions/du.htm |archive-date=2012-01-19}}</ref> DU has been suggested as a possible cause of Gulf War syndrome.<ref name="Jiang">{{cite journal | vauthors = Jiang GC, Aschner M | title = Neurotoxicity of depleted uranium: reasons for increased concern | journal = Biological Trace Element Research | volume = 110 | issue = 1 | pages = 1–17 | date = April 2006 | pmid = 16679544 | doi = 10.1385/BTER:110:1:1 | bibcode = 2006BTER..110....1J | s2cid = 24199948 }}</ref> | |||
| The use of DU in ] is controversial because of questions about potential long-term health effects.<ref name=MillerMcClain>{{cite journal | |||
| | author = Miller AC, McClain D. | |||
| | title = A review of depleted uranium biological effects: in vitro and in vivo studies | |||
| | journal = ''Rev Environ Health'' | |||
| | year = 2007 Jan-Mar | |||
| | volume = 22 | |||
| | issue = 1 | |||
| | pages = 75–89 | |||
| | pmid = 17508699}}</ref> Normal functioning of the ], ], ], ], and numerous other systems can be affected by uranium exposure, because in addition to being weakly radioactive, uranium is a ].<ref name=Craft04>{{cite journal | |||
| | title = Depleted and natural uranium: chemistry and toxicological effects | |||
| | author = E. S. Craft, A. W. Abu-Qare, M. M. Flaherty, M. C. Garofolo, H. L. Rincavage, M. B. Abou-Donia | |||
| | journal = ''Journal of Toxicology and Environmental Health Part B: Critical Reviews'' | |||
| | year = 2004 | |||
| | volume = 7 | |||
| | issue = 4 | |||
| | pages = 297–317 | |||
| | doi = 10.1080/10937400490452714}}</ref> Because ] is a heavy metal and chemical toxicant with nephrotoxic (kidney-damaging),<ref></ref> ] (birth defect-causing),<ref>{{cite journal |author=Hindin R, Brugge D, Panikkar B |title=Teratogenicity of depleted uranium aerosols: a review from an epidemiological perspective |journal=''Environ Health'' |volume=4 |issue= |page=17 |year= 2005|pmid=16124873 |doi=10.1186/1476-069X-4-17}}</ref><ref>{{cite journal |author=Arfsten D, Still K, Ritchie G |title=A review of the effects of uranium and depleted uranium exposure on reproduction and fetal development |journal=Toxicol Ind Health |volume=17 |issue=5-10 |pages=180–91 |year=2001 |pmid=12539863 | doi = 10.1191/0748233701th111oa}}</ref> and potentially ]ic<ref>{{Dead link|date=April 2008}}</ref> properties, uranium exposure is associated with a variety of illnesses.<ref></ref> The chemical toxicological hazard posed by uranium dwarfs its radiological hazard because it is only weakly radioactive, and depleted uranium even less so. DU has recently been recognized as a ].<ref name="autogenerated3">{{cite journal |author=Jiang G, Aschner M |title=Neurotoxicity of depleted uranium: reasons for increased concern |journal=''Biol Trace Elem Res'' |volume=110 |issue=1 |pages=1–17 |year=2006 |pmid=16679544 | doi = 10.1385/BTER:110:1:1}}</ref> In 2005, depleted uranium was shown to be a neurotoxin in rats.<ref>{{cite journal |author=Anandan N, Shetty S, Patil K, Ibrahim A |title=Acute urinary retention caused by anterior urethral polyp |journal=''Br J Urol'' |volume=69 |issue=3 |pages=321–2 |year=1992 |pmid=1568112 |doi=10.1111/j.1464-410X.1992.tb15541.x}}</ref> Epidemiological evidence is consistent with increased risk of birth defects in the offspring of persons exposed to DU.<ref name="Hindin" /> | |||
| A 2008 review by the U.S. Department of Veterans Affairs found no association between DU exposure and multisymptom illness, concluding that "exposure to DU munitions is not likely a primary cause of Gulf War illness". There is some evidence that long-term exposure to high doses of DU can cause other health problems that are unrelated to GWS.<ref name="FedReport" /> Since 2011, US combat veterans may claim disability compensation for health problems related to exposure to depleted uranium.<ref>{{cite web |url=https://www.publichealth.va.gov/exposures/depleted_uranium/ |title=Depleted Uranium |department=VA Public Health |date=October 12, 2023 |url-status=live |archive-url=https://web.archive.org/web/20240328161155/https://www.publichealth.va.gov/exposures/depleted_uranium/ |archive-date= Mar 28, 2024 }}</ref> The ] decides these claims on a case-by-case basis.{{citation needed|date=February 2024}} | |||
| Early studies of depleted uranium ] exposure assumed that uranium combustion product particles would quickly settle out of the air<ref>{{dead link|date=November 2009}}</ref> and thus could not affect populations more than a few kilometers from target areas,<ref>{{cite journal |author=Mitsakou C, Eleftheriadis K, Housiadas C, Lazaridis M |title=Modeling of the dispersion of depleted uranium aerosol |journal=Health Phys |volume=84 |issue=4 |pages=538–44 |year=2003 |pmid=12705453 |doi=10.1097/00004032-200304000-00014}}</ref> and that such particles, if inhaled, would remain undissolved in the lung for a great length of time and thus could be detected in urine.<ref>{{cite journal |author=Horan P, Dietz L, Durakovic A |title=The quantitative analysis of depleted uranium isotopes in British, Canadian, and U.S. Gulf War veterans |journal=Mil Med |volume=167 |issue=8 |pages=620–7 |year=2002 |pmid=12188230}}</ref> ] ion contamination has been found on and around depleted uranium targets.<ref>{{cite journal |author=Salbu B, Janssens K, Lind O, Proost K, Gijsels L, Danesi P |title=Oxidation states of uranium in depleted uranium particles from Kuwait |journal=J Environ Radioact |volume=78 |issue=2 |pages=125–35 |year=2005 |pmid=15511555 |doi=10.1016/j.jenvrad.2004.04.001}}</ref> | |||
| A 2018 study stated that "the number of Gulf War veterans who developed the Gulf War syndrome following exposure to high quantities of DU has risen to about one-third of the 800,000 U.S. forces deployed," with 25,000 of those having had a premature death.<ref>{{cite journal | vauthors = Faa A, Gerosa C, Fanni D, Floris G, Eyken PV, Lachowicz JI, Nurchi VM | title = Depleted Uranium and Human Health | journal = Current Medicinal Chemistry | volume = 25 | issue = 1 | pages = 49–64 | year = 2018 | pmid = 28462701 | doi = 10.2174/0929867324666170426102343 | url = https://www.researchgate.net/publication/316656324 | url-status = live | type = Review article | archive-url = https://web.archive.org/web/20230605154247/https://www.researchgate.net/publication/316656324_Depleted_Uranium_and_Human_Health | archive-date = Jun 5, 2023 }}</ref> A 2021 study by a team at the ] tested urine samples of 154 US veterans, reporting that no soldiers with the syndrome were exposed to significant amounts of depleted uranium and that DU "is not and never was in the bodies of those who are ill at sufficient quantities to cause disease".<ref>{{Cite news|date=2021-02-18|title=Gulf War syndrome 'not caused by depleted uranium'|language=en-GB|work=BBC News|url=https://www.bbc.com/news/uk-56116101|access-date=2021-02-18}}</ref><ref>{{Cite web| vauthors = Cotterill T |date=18 February 2021|title=Gulf War syndrome 'not caused by depleted uranium' city scientists claim|url=https://www.portsmouth.co.uk/news/defence/gulf-war-syndrome-not-caused-depleted-uranium-portsmouth-scientists-claim-3138826|access-date=2021-02-18|website=]|language=en}}</ref> | |||
| In 2001, a study was published in Military Medicine that found DU in the urine of Gulf War veterans.<ref>{{cite journal |author=Hodge S, Ejnik J, Squibb K, McDiarmid M, Morris E, Landauer M, McClain D |title=Detection of depleted uranium in biological samples from Gulf War veterans |journal=Mil Med |volume=166 |issue=12 Suppl |pages=69–70 |year=2001 |pmid=11778443}}</ref> Another study, published by ] in 2004, also showed DU in the urine of Gulf War veterans.<ref>{{cite journal |author=Gwiazda R, Squibb K, McDiarmid M, Smith D |title=Detection of depleted uranium in urine of veterans from the 1991 Gulf War |journal=Health Phys |volume=86 |issue=1 |pages=12–8 |year=2004 |pmid=14695004 |doi=10.1097/00004032-200401000-00004}}</ref> A study of UK veterans who thought they might have been exposed to DU showed aberrations in their ] ]s.<ref name="Schröder2003">{{cite pmid|12678382}}</ref> Mice immune cells exposed to uranium exhibit abnormalities.<ref>{{cite journal |author=Wan B, Fleming J, Schultz T, Sayler G |title=In vitro immune toxicity of depleted uranium: effects on murine macrophages, CD4+ T cells, and gene expression profiles |journal=Environ Health Perspect |volume=114 |issue=1 |pages=85–91 |year=2006 |pmid=16393663}}</ref> | |||
| ==== Pyridostigmine bromide nerve gas antidote ==== | |||
| In the ] war zone where depleted uranium was also used, an absence of problems is seen by some as evidence of DU munitions' safety. "Independent investigations by the World Health Organization, European Commission, European Parliament, United Nations Environment Programme, United Kingdom Royal Society, and the Health Council of the Netherlands all discounted any association between depleted uranium and leukemia or other medical problems."<ref name="autogenerated6" /> In Italy, controversy over the health risks associated with the use of DU continues, with a Senate investigation committee was due to release its report into 'Balkan Syndrome' by the end of 2007.<ref>{{cite web |author=Anes Alic|url=http://www.isn.ethz.ch/news/sw/details.cfm?id=18290|title=Depleted uranium, depleted health concerns|publisher=ISN Security Watch|date=October 29, 2007}}</ref> Since then, there has been a resurgence of interest in the health effects of depleted uranium, especially since it has recently been linked with neurotoxicity.<ref name="autogenerated3" /> | |||
| The US military issued ] (PB) pills to protect against exposure to nerve gas agents such as sarin and ]. PB was used as a ] against nerve agents; it is not a vaccine. Taken before exposure to nerve agents, PB was thought to increase the efficiency of nerve agent antidotes. PB had been used since 1955 for patients who have ] with doses up to 1,500 mg a day, far in excess of the 90 mg given to soldiers, and was considered safe by the FDA at either level for indefinite use and its use to pre-treat nerve agent exposure had recently been approved.<ref>{{cite news |publisher=PBS |work=Frontline |access-date=2012-05-09 |date=1996-12-01 |url=https://www.pbs.org/wgbh/pages/frontline/shows/syndrome/analysis/pyribrom.html |title=Pyridostigmine bromide use in the First Gulf War |url-status=live |archive-url=https://web.archive.org/web/20121112142950/http://www.pbs.org/wgbh/pages/frontline/shows/syndrome/analysis/pyribrom.html |archive-date=2012-11-12 |df=dmy-all}}</ref> | |||
| Given both the large body of epidemiological data on myasthenia gravis patients and follow-up studies done on veterans it was concluded that while it was unlikely that health effects reported today by Gulf War veterans are the result of exposure solely to PB, use of PB was ] with illness.<ref name=FedReport /> However,{{clarify|reason=Isn't IOM in agreement with "unlikely" in the previous sentence?|date=January 2022}} a later review by the ] concluded that the evidence was not strong enough to establish a causal relationship.<ref name="iom_p13">{{cite book |page=13 |title=Gulf War and Health: Treatment for Chronic Multisymptom Illness |year=2013 |publisher=]}}</ref> | |||
| The aerosol produced during impact and combustion of depleted uranium munitions can potentially contaminate wide areas around the impact sites or can be inhaled by civilians and military personnel.<ref name="ncbi.nlm.nih.gov">Mitsakou C, Eleftheriadis K, Housiadas C, Lazaridis M 2003 Apr, Retrieved January 15, 2009</ref> During a three week period of conflict in 2003 ], 1,000 to 2,000 tonnes of DU munitions were used, mostly in cities.<ref name="gaurdian2003">Paul Brown, ''guardian.co.uk'' 25 April 2003, Retrieved February 3, 2009</ref> Depleted uranium may have been standard ordnance in the arsenals of both sides during the ]. | |||
| === |
==== Organophosphates ==== | ||
| ] (OPIDN, aka organophosphate-induced delayed polyneuropathy) may contribute to the unexplained illnesses of the Gulf War veterans.<ref>{{cite journal |doi=10.1016/j.jns.2017.08.451 |title=New insights into the organophosphate-induced delayed neuropathy |journal=Journal of the Neurological Sciences |volume=381 |pages=153–159 |year=2017 | vauthors = Qiang D, Xie X, Gao Z |s2cid=54302903 }}</ref><ref>{{cite journal | vauthors = Mackenzie Ross SJ, Brewin CR, Curran HV, Furlong CE, Abraham-Smith KM, Harrison V | title = Neuropsychological and psychiatric functioning in sheep farmers exposed to low levels of organophosphate pesticides | journal = Neurotoxicology and Teratology | volume = 32 | issue = 4 | pages = 452–459 | year = 2010 | pmid = 20227490 | pmc = 3042861 | doi = 10.1016/j.ntt.2010.03.004 | bibcode = 2010NTxT...32..452M }}</ref> | |||
| ====Anthrax vaccine==== | |||
| ===== Organophosphate pesticides ===== | |||
| Iraq had loaded ], ], and ] into ] and artillery shells in preparing for the Gulf War and that these munitions were deployed to four locations in Iraq.<ref> Anthony H. Cordesman. Iraq and the War of Sanctions: Conventional Threats and Weapons of Mass Destruction</ref> | |||
| The use of ] ] and ] during the first Gulf War is credited with keeping rates of pest-borne diseases low. Pesticide use is one of only two exposures consistently identified by Gulf War epidemiologic studies to be significantly associated with Gulf War illness.<ref>{{cite book |publisher=] |author=Office of the Special Assistant to the Undersecretary of Defense (Personnel and Readiness) for Gulf War Illnesses Medical Readiness and Military Deployments |title=Environmental Exposure Report: Pesticides Final Report |location=Washington, D.C. |date=2003-04-17 |df=dmy-all}}</ref> Multisymptom illness profiles similar to Gulf War illness have been associated with low-level pesticide exposures in other human populations. In addition, Gulf War studies have identified dose-response effects, indicating that greater pesticide use is more strongly associated with Gulf War illness than more limited use.<ref name=":2">{{cite book | vauthors = Krengel M, Sullivan K |title=Neuropsychological Functioning in Gulf War Veterans Exposed to Pesticides and Pyridostigmine Bromide |location=Fort Detrick, MD |publisher=U.S. Army Medical Research and Materiel Command |date=2008-08-01 |url=https://apps.dtic.mil/sti/pdfs/ADA491742.pdf |access-date=2012-05-09 |df=dmy-all |url-status=live |archive-url=https://web.archive.org/web/20130408132243/http://www.dtic.mil/cgi-bin/GetTRDoc?AD=ADA491742 |archive-date=2013-04-08}} W81XWH-04-1-0118</ref> Pesticide use during the Gulf War has also been associated with ] deficits and ] alterations in Gulf War veterans in clinical studies conducted following the end of the war. The 2008 report concluded that "all available sources of evidence combine to support a consistent and compelling case that pesticide use during the Gulf War is causally associated with Gulf War illness."<ref name=FedReport /> | |||
| During Operation Desert Storm, 41% of U.S. combat soldiers and 75% of UK combat soldiers were vaccinated against ].<ref> December 12-13, 2005 Committee Meeting Minutes (page 73.)</ref> Like all vaccines, the early 1990s version of the ] was a source of several ]s. Reactions included local skin irritation, some lasting for weeks or months.<ref></ref> While the ] (FDA) approved the vaccine, it never went through large scale clinical trials, unlike most other vaccines in the United States.<ref></ref> | |||
| While recent studies have demonstrated the vaccine’s is highly reactogenic <ref> Pharmacoepidemiology and Drug Safety.Short-term reactogenicity and gender effect of anthrax vaccine: analysis of a 1967-1972 study and review of the 1955-2005 medical literature</ref>, there is no clear evidence or epidemiological studies on Gulf War veterans linking the vaccine to Gulf War Syndrome. Combining this with the lack of symptoms from current deployments of individuals who have received the vaccine led the Committee on Gulf War Veterans’ Illnesses to conclude that the vaccine is not a likely cause of Gulf War illness for most ill veterans.<ref name=FedReport/> | |||
| === |
=== Less likely causes === | ||
| According to the VA's 2008 RAC report, "For several Gulf War exposures, an association with Gulf War illness cannot be ruled out. These include low-level exposure to nerve agents, close proximity to oil well fires, receipt of multiple vaccines, and effects of combinations of Gulf War exposures." However, several potential causes of GWI were deemed, "not likely to have caused Gulf War illness for the majority of ill veterans," including "depleted uranium, anthrax vaccine, fuels, solvents, sand and particulates, infectious diseases, and chemical agent resistant coating (CARC)," for which "there is little evidence supporting an association with Gulf War illness or a major role is unlikely based on what is known about exposure patterns during the Gulf War and more recent deployments."<ref name="RAC11">{{cite report |last=Research Advisory Committee on Gulf War Veterans' Illnesses, U.S. Department of Veterans Affairs|title=Gulf War Illness and the Health of Gulf War Veterans: Scientific Findings and Recommendations |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |page=1 |year=2008 |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |location=Washington, DC |publisher=U.S. Government Printing Office |archive-date=2014-06-03 |df=dmy-all}}</ref> | |||
| The VA's 2014 RAC report reinforced its 2008 report findings: "The research reviewed in this report supports and reinforces the conclusion in the 2008 RACGWVI report that exposures to pesticides and pyridostigmine bromide are causally associated with Gulf War illness. Evidence also continues to demonstrate that Gulf War illness is not the result of psychological stressors during the war." It also found additional evidence since the 2008 report for the role of ] in GWI, but inadequate evidence regarding exposures to oil well fires, vaccines, and depleted uranium to make new conclusions about them.<ref name=":0" /> | |||
| Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans, according to a ] review committee. | |||
| ====Oil well fires==== | ==== Oil well fires ==== | ||
| During the war, many ] by the retreating Iraqi army, and the smoke from those fires was inhaled by large numbers of soldiers, many of whom had acute ] and other chronic effects, including ] and ]. However, firefighters who were assigned to the oil well fires and encountered the smoke, but who did not take part in combat, have not had GWI symptoms.<ref name=RAC_GWVI_Minutes_2005/>{{rp|pages=148, 154, 156}} The 2008 RAC report states that "evidence is inconsistent or limited in important ways."<ref name="RAC11" /> | |||
| ==== Anthrax vaccine ==== | |||
| During the war, many ] by the retreating Iraqi army, and the smoke from those fires was inhaled by large numbers of soldiers, many of whom suffered acute ] and other chronic effects, including ] and ]. However, firefighters who were assigned to the oil well fires and encountered the smoke, but who did not take part in combat, have not had GWI symptoms.<ref> December 12-13, 2005 Committee Meeting Minutes (pages 148, 154, 156)</ref> | |||
| {{update|date=January 2022}} | |||
| Iraq had loaded anthrax, ] toxin, and ] into ] and artillery shells in preparing for the Gulf War and these munitions were deployed to four locations in Iraq.<ref>{{cite book | vauthors = Cordesman AH |title=Iraq and the War of Sanctions: Conventional Threats and Weapons of Mass Destruction |url=https://books.google.com/books?id=qFCkQRQApSwC |year=1999 |publisher=] |isbn=978-0-275-96528-0}}</ref> During Operation Desert Storm, 41% of U.S. combat soldiers and 75% of UK combat soldiers were vaccinated against anthrax.<ref name=RAC_GWVI_Minutes_2005/>{{rp|page=73}} Reactions included local skin irritation, some lasting for weeks or months.<ref>{{cite web |url=http://www.gao.gov/new.items/d0192t.pdf | vauthors = Chan KC |date=2000-10-11 |access-date=2012-05-09 |df=dmy-all |title=GAO-01-92T Anthrax Vaccine: Preliminary Results of GAO's Survey of Guard/Reserve Pilots and Aircrew Members |publisher=] |url-status=live |archive-url=https://web.archive.org/web/20120406120022/http://www.gao.gov/new.items/d0192t.pdf |archive-date=2012-04-06}}</ref> While the ] (FDA) approved the vaccine, it never went through large-scale clinical trials.<ref>{{cite news |url=http://www.gulfwarvets.com/anthrax11.htm |date=2001-05-16 |df=dmy-all |title=Expert: Anthrax vaccine not proven | vauthors = Burdeau C |newspaper=] |archive-url=https://web.archive.org/web/20011107182429/http://www.gulfwarvets.com/anthrax11.htm |archive-date=2001-11-07}} ({{cite news |title=original source |url=http://orig.clarionledger.com/news/0105/16/m11.html |newspaper=] |archive-url=https://archive.today/20120712043354/http://orig.clarionledger.com/news/0105/16/m11.html |archive-date=2012-07-12 |df=dmy-all }})</ref> | |||
| While recent studies have demonstrated the vaccine is highly ],<ref>{{cite journal | vauthors = McNeil MM, Chiang IS, Wheeling JT, Zhang Y | title = Short-term reactogenicity and gender effect of anthrax vaccine: analysis of a 1967-1972 study and review of the 1955-2005 medical literature | journal = Pharmacoepidemiology and Drug Safety | volume = 16 | issue = 3 | pages = 259–274 | date = March 2007 | pmid = 17245803 | doi = 10.1002/pds.1359 | s2cid = 25335669 | url = https://zenodo.org/record/1229308 }}</ref> there is no clear evidence or epidemiological studies on Gulf War veterans linking the vaccine to Gulf War illness. Combining this with the lack of symptoms from current deployments of individuals who have received the vaccine led the Committee on Gulf War Veterans' Illnesses to conclude that the vaccine is not a likely cause of Gulf War illness for most ill veterans.<ref name="FedReport" /> However, the committee report does point out that veterans who received a larger number of various vaccines in advance of deployment have shown higher rates of persistent symptoms since the war.<ref name="RAC123">{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=123 (p. 133 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref><ref name="FedReport" /> | |||
| ==Diagnosis== | |||
| However, research was done by PB Asa, Y Cao, and RF Garry on serum antibodies to squalene in Gulf War Syndrome patients. The results showed "the substantial majority (95%) of overtly ill deployed GWS patients had antibodies to squalene. All (100%) GWS patients immunized for service in Desert Shield/Desert Storm who did not deploy, but had the same signs and symptoms as those who did deploy, had antibodies to squalene. In contrast, none (0%) of the deployed Persian Gulf veterans not showing signs and symptoms of GWS have antibodies to squalene. Neither patients with idiopathic autoimmune disease nor healthy controls had detectable serum antibodies to squalene."<ref>{{cite journal | vauthors = Asa PB, Cao Y, Garry RF | title = Antibodies to squalene in Gulf War syndrome | journal = Experimental and Molecular Pathology | volume = 68 | issue = 1 | pages = 55–64 | date = February 2000 | pmid = 10640454 | doi = 10.1006/exmp.1999.2295 }}</ref> Their work of the researchers was profiled by Gary Matsumoto in "Vaccine A". | |||
| Multisymptom illness is more prevalent in Gulf War I veterans than veterans of previous conflicts, but the pattern of comorbidities is similar for actively deployed and nondeployed military personnel.<ref>Kelsall ''et al'' (2009) "Physical, psychological, and functional comorbidities of multisymptom illness in Australian male veterans of the 1991 Gulf War," ''Am J Epidemiol'' '''170'''(8):1048-56. PMID 19762370</ref> Management of potentially comorbid toxic exposures requires awareness of the toxins involved.<ref name=Schecter /> Exposure to the destruction of the ], where large quantities of the chemical weapon ] was stored, is negatively correlated with motor speed.<ref name=Toomey /> Epidemiological evidence is consistent with increased risk of birth defects in the offspring of persons exposed to depleted uranium<ref name="Hindin" /> and uranium exposure has also been associated with increased cancer rates.<ref name="ajph.org"></ref><ref></ref><ref></ref><ref> </ref><ref> </ref><ref></ref> | |||
| This research and theory was later criticized, and further research has leaned heavily against squalene in vaccinations causing GWS; Perhaps the most important points against this theory include that squalene antibodies have been detected in populations not exposed to squalene containing vaccinations, and that the anthrax vaccines used in the Gulf War did not actually contain squalene in any form.<ref>Office of the Federal Register, National Archives and Records Administration. (2004, January 7). 69 FR 1320 - Biological Products; Bacterial Vaccines and Toxoids; Implementation of Efficacy Review. . Office of the Federal Register, National Archives and Records Administration. https://www.govinfo.gov/app/details/FR-2004-01-08/C3-32255</ref><ref>{{cite journal | vauthors = Del Giudice G, Fragapane E, Bugarini R, Hora M, Henriksson T, Palla E, O'hagan D, Donnelly J, Rappuoli R, Podda A | title = Vaccines with the MF59 adjuvant do not stimulate antibody responses against squalene | journal = Clinical and Vaccine Immunology | volume = 13 | issue = 9 | pages = 1010–1013 | date = September 2006 | pmid = 16960112 | pmc = 1563566 | doi = 10.1128/CVI.00191-06 }}</ref><ref>{{Cite web | vauthors = Henig J |date=2009-10-18 |title=FactCheck: Swine Flu Vaccine Fears Greatly Exaggerated |url=https://www.newsweek.com/factcheck-swine-flu-vaccine-fears-greatly-exaggerated-81069 |access-date=2022-11-06 |website=Newsweek |language=en}}</ref> | |||
| ==Management== | |||
| ==== Combat stress ==== | |||
| Diplomatic reconciliation is one means of prevention,<ref name=Curle /><ref name=Jentleson /> beyond battlefield air quality management, which often conflicts with established tactical policy. For example, most organized armies practice "secure and hold" tactics which require occupation of areas before they can be decontaminated. | |||
| Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans, according to a ] (VA) review committee.{{citation needed|date=August 2020}} An April 2010 Institute of Medicine review found, "the excess of unexplained medical symptoms reported by deployed Gulf war veterans cannot be reliably ascribed to any known psychiatric disorder",<ref name="books.nap.edu">{{cite book |series=Gulf War and Health |volume=8 |title=Update of Health Effects of Serving in the Gulf War |collaboration=Committee on Gulf War and Health |quote=Health Effects of Serving in the Gulf War, Update 2009; Board on the Health of Select Populations; Institute of Medicine, National Academy of Sciences |publisher=] |year=2010 |isbn=978-0-309-14921-1 |location=Washington, DC |page=109 |doi=10.17226/12835 |pmid=25032373 |url=http://books.nap.edu/openbook.php?record_id=12835&page=109}}</ref> although they also concluded that "the constellation of unexplained symptoms associated with the Gulf War illness complex could result from interplay between both biological and psychological factors."<ref name="books.nap.edu_260">{{cite book |page=260 |url=http://books.nap.edu/openbook.php?record_id=12835&page=260 |collaboration=Committee on Gulf War and Health |series=Gulf War and Health |volume=8 |title=Update of Health Effects of Serving in the Gulf War | year=2010 |publisher=]| doi=10.17226/12835 | pmid=25032373 | isbn=978-0-309-14921-1 }}</ref> | |||
| == Pathobiology == | |||
| ===Acetylcholinesterase inhibitors=== | |||
| ====Nerve agent antidote and insect repellent==== | |||
| === Chronic inflammation === | |||
| In 2008, a paper published in the '']'' suggested that excess illnesses in Gulf War veterans could be explained in part by their exposure to ] and ] ]s.<ref name=Golomb>Golomb, B. (2008) ''Proc Natl Acad Sci''; ; </ref> A federal report released in November, 2008, agreed, stating that exposure to two substances "are causally associated with Gulf War illness":<ref></ref> | |||
| The 2008 VA report on ''Gulf War illness and the Health of Gulf War Veterans'' suggested a possible link between GWI and ], nonspecific ] of the ] that cause pain, fatigue and memory issues, possibly due to pathologically persistent increases in ]s and suggested further research be conducted on this issue.<ref>{{cite news |url=http://www.fight4vets.com/va-benefits-for-gulf-war-syndrome/ |title=VA Benefits for Gulf War Syndrome|work=fight4vets |access-date=25 July 2016 |archive-url=https://web.archive.org/web/20160819104709/http://www.fight4vets.com/va-benefits-for-gulf-war-syndrome/ |archive-date=19 August 2016 |url-status=live}}</ref> | |||
| *], an acetylcholinesterase inhibitor intended to protect against nerve agents,<ref> December 12-13, 2005 Committee Meeting Minutes</ref> and | |||
| *]s and ]s (often acetylcholinesterase inhibitors) | |||
| == Diagnosis == | |||
| {{expand-section}} | |||
| Clinical diagnosis of Gulf War illness has been complicated by multiple case definitions. In 2014, the ] ] (IOM)—contracted by the ] for the task—released a report concluding that the creation of a new ] for chronic multisymptom illness in Gulf War veterans was not possible because of insufficient evidence in published studies regarding its onset, duration, severity, frequency of symptoms, exclusionary criteria, and laboratory findings. Instead, the report recommended the use of two case definitions, the "Kansas" definition and the "Centers for Disease Control and Prevention (CDC)" definition, noting: "There is a set of symptoms (fatigue, pain, ]) that are reported in all the studies that have been reviewed. The CDC definition captures those three symptoms; the Kansas definition also captures them, but it also includes the symptoms reported most frequently by Gulf War veterans."<ref name=":1">{{cite book |title=Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined |department=Institute of Medicine, National Academy of Sciences |collaboration=Committee on the Development of a Consensus Case Definition for Chronic Multisymptom illness in 1990–1991 Gulf War Veterans |publisher=National Academies Press |year=2014 |isbn=978-0-309-29877-3 |location=Washington, D.C. |pages=90–99 |oclc=880456748}}</ref> | |||
| The Kansas case definition is more specific and may be more applicable for research settings, while the CDC case definition is more broad and may be more applicable for clinical settings.<ref name=":1" /> | |||
| ====Sarin==== | |||
| === Classification === | |||
| Exposure to ], a ], is a possible comorbidity. Chemical weapons classified as nerve agents are also strong ]. A 2004 review discusses symptoms, signs, and treatment of nerve agent exposure.<ref name=Schecter /> | |||
| Medical ailments associated with service in the 1990–1991 Gulf War have been recognized by both the ] and the ].<ref name=veteranIllnesses>{{cite web |url=http://www.publichealth.va.gov/exposures/gulfwar/associated_illnesses.asp |title=Gulf War Veterans' Illnesses: Illnesses Associated with Gulf War Service |date=nd |access-date=2012-05-09 |publisher=United States Department of Veterans Affairs |url-status=live |archive-url=https://web.archive.org/web/20120212190215/http://www.publichealth.va.gov/exposures/gulfwar/associated_illnesses.asp |archive-date=2012-02-12 |df=dmy-all}}</ref> | |||
| Before 1998, the terms ''Gulf War syndrome, Gulf War veterans' illness, unexplained illness'', and ''undiagnosed illness'' were used interchangeably to describe chronic unexplained symptoms in veterans of the 1991 Gulf War. The term ''chronic multisymptom illness'' (CMI) was first used following publication of a 1998 study<ref name=":2" /> describing chronic unexplained symptoms in Air Force veterans of the 1991 Gulf War.<ref name="iom_p13" /> | |||
| ===Uranium exposure=== | |||
| In a 2014 report contracted by the U.S. Department of Veterans Affairs, the ] Institute of Medicine recommended the use the term ''Gulf War illness'' rather than ''chronic multisymptom illness''.<ref name=":1" /> Since that time, relevant publications by the National Academy of Science and the U.S. Department of Defense have used only the term ''Gulf War illness'' (GWI).{{citation needed|date=December 2021}} | |||
| ] ]s such as ] should be treated with ] or other means shortly after exposure.<ref>Spagnul, A ''et al'' (2009) "Calixarene-entrapped nanoemulsion for uranium extraction from contaminated solutions." ''J Pharm Sci'' PMID 19780139</ref> Incorporated uranium becomes ] ions, which accumulate in bone, liver, kidney, and reproductive tissues. ] can be decontaminated from steel surfaces<ref name=Francis /> and aquifers.<ref name=Wu /> | |||
| The U.S. Department of Veterans Affairs (VA) confusingly still uses an array of both old and new terminology for ''Gulf War illness''. VA's specialty clinical evaluation War Related Illness and Injury Study Centers (WRIISCs) use the recommended term ''Gulf War illness'',<ref>{{Cite web |url=https://www.warrelatedillness.va.gov/WARRELATEDILLNESS/education/factsheets/gulf-war-illness-for-veterans.pdf |series=Gulf War Illness |title=Information for Veterans |website=War Related Illness and Injury Study Center}}</ref> as do VA's Office of Research and Development (VA-ORD) and many recent VA research publications.<ref>{{Cite web |url=https://www.research.va.gov/currents/1017-Evidence-of-DNA-damage-in-Vets-with-Gulf-War-illness.cfm |title=Researchers find evidence of DNA damage in Vets with Gulf War illness |last=U.S. Department of Veterans Affairs, Office of Research and Development |date=2017-10-19 |df=dmy-all}}</ref> However, VA's Public Health website still uses ''Gulf War veterans' medically unexplained illnesses'', ''chronic multi-symptom illness'' (CMI), and ''undiagnosed illnesses'', but explains that VA doesn't use the term ''Gulf War syndrome'' because of varying symptoms.<ref>{{cite web |url=http://www.publichealth.va.gov/exposures/gulfwar/medically-unexplained-illness.asp |title=Gulf War Veterans' Medically Unexplained Illnesses |series=Public Health |publisher=US Department of Veterans Affairs |department=Veterans Health Administration |website=publichealth.va.gov |archive-url=https://web.archive.org/web/20140224112435/http://www.publichealth.va.gov/exposures/gulfwar/medically-unexplained-illness.asp |archive-date=2014-02-24 |df=dmy-all |url-status=live}}</ref> | |||
| ==Epidemiology== | |||
| Epidemiologic studies have been performed evaluating many suspected factors for Gulf War illness as seen in veteran populations. Below is a summary of epidemiologic studies of veterans displaying multisymptom illness and their exposure to suspect conditions from the 2008 U.S. Veterans Administration report.<ref> (page 220-221)</ref> | |||
| The ] (VHA) originally classified individuals with related ailments believed to be connected to their service in the Persian Gulf a special non-ICD-9 code DX111, as well as ICD-9 code V65.5.<ref>{{cite web |collaboration=Department of Veterans Affairs Veterans Health Initiative |url=http://www.hanford.gov/hanford/files/VA_GuidetoGulfWarVeteransHealth.pdf |title=A Guide to Gulf War Veterans' Health |archive-url=https://web.archive.org/web/20060926215559/http://www.hanford.gov/hanford/files/VA_GuidetoGulfWarVeteransHealth.pdf |archive-date=2006-09-26 |df=dmy-all |year=2002}}</ref> | |||
| === Kansas definition === | |||
| In 1998, the State of Kansas Persian Gulf Veterans Health Initiative sponsored an epidemiological survey led by Dr. Lea Steele of deployment-related symptoms in 2,030 Gulf War veterans. The result was a "clinically based descriptive definition using correlated symptoms" in six symptom groups: fatigue and sleep problems, pain, neurologic and mood, gastrointestinal, respiratory symptoms, and skin (dermatologic) symptoms.<ref name=":1" /> | |||
| To meet the "Kansas" case definition, a veteran of the 1990–91 Gulf War must have symptoms in at least three of the six symptom domains, which during the survey were scored based on severity ("severity"). Symptom onset must have developed during or after deploying to the 1990–91 Gulf War theatre of operations ("onset") and must have been present in the year before interview ("duration"). Participants were excluded if they had a diagnosis of or were being treated for any of several conditions that might otherwise explain their symptoms ("exclusionary criteria"), including cancer, diabetes, heart disease, chronic infectious disease, lupus, multiple sclerosis, stroke, or any serious psychiatric condition.<ref name=":1" /> | |||
| Applying the Kansas case definition to the original Kansas study cohort resulted in a prevalence of Gulf War illness of 34.2% in Gulf War veterans and 8.3% in nondeployed Gulf War era veterans, or an excess rate of GWI of 26.3% in Gulf War veterans.<ref name=":1" /> | |||
| === CDC definition === | |||
| Also in 1998, a study published by Dr. Keiji Fukuda under the auspices of the ] (CDC) examined chronic multisymptom illness through a cross-sectional survey of 3,675 ill and healthy ] veterans of the 1990–91 Gulf War, including from a ]-based ] unit and three comparison Air Force units. The CDC case definition was derived from clinical data and ].<ref name=":1" /> | |||
| The result was a symptom-category approach to a case definition, with three symptom categories: fatigue, mood–cognition, and musculoskeletal. To meet the case definition, the veteran of the 1990–91 Gulf War must have symptoms in two of the three categories and have experienced the illness for six months or longer ("duration").<ref name=":1" /> | |||
| The original study also including a determination of severity of symptoms ("severity"). "Severe cases were identified if at least one symptom in each of the required categories was rated as severe. Of 1,155 participating Gulf War veterans, 6% had severe CMI, and 39% had mild to moderate CMI; of the 2,520 nondeployed era veterans, 0.7% had severe and 14% had mild to moderate CMI."<ref name=":1" /> | |||
| == Treatment == | |||
| A 2013 report by the ] reviewed the peer-reviewed published medical literature for evidence regarding treatments for symptoms associated with ''chronic multisymptom illness'' (CMI) in 1990–91 Gulf War veterans, and in other chronic multisymptom conditions. For the studies the report reviewed that were specifically regarding CMI in 1990–91 Gulf War veterans (''Gulf War illness''), the report made the following conclusions:<ref name="iom_p13" /> | |||
| * ]: "Although the study of doxycycline was found to have high strength of evidence and was conducted in a group of 1991 Gulf War veterans who had CMI, it did not demonstrate efficacy; that is, doxycycline did not reduce or eliminate the symptoms of CMI in the study population." | |||
| * ] (CBT) and exercise: "These studies evaluated the effects of exercise and CBT in combination and individually. The therapeutic benefit of exercise was unclear in those studies. Group CBT rather than exercise may confer the main therapeutic benefit with respect to physical symptoms." | |||
| The report concluded: "On the basis of the evidence reviewed, the committee cannot recommend any specific therapy as a set treatment for veterans who have CMI. The committee believes that a 'one-size-fits-all' approach is not effective for managing veterans who have CMI and that individualized health care management plans are necessary."<ref name="iom_p13" /> | |||
| By contrast, the U.S. Department of Defense (DoD) noted in a May 2018 publication that the primary focus of its Gulf War illness Research Program (GWIRP) "has been to fund research studies to identify treatment targets and test interventional approaches to alleviate symptoms. While most of these studies remain in progress, several have already shown varying levels of promise as GWI treatments." | |||
| According to the May 2018 DoD publication:<ref name=":3" />{{Long quote|date=November 2020}} | |||
| {{blockquote|'''''Published Results on Treatments'''''}} | |||
| {{blockquote|''The earliest federally funded multi-center clinical trials were VA- and DoD-funded trials that focused on antibiotic treatment (doxycycline) (Donta, 2004) and cognitive behavioral therapy with exercise (Donta, 2003). Neither intervention provided long-lasting improvement for a substantial number of Veterans.''}} | |||
| {{blockquote|''Preliminary analysis from a placebo-controlled trial showed that 100 mg of Coenzyme Q10 (known as CoQ10 or Ubiquinone) significantly improved general self-reported health and physical functioning, including among 20 symptoms, each of which was present in at least half of the study participants, with the exception of sleep. These improvements included reducing commonly reported symptoms of fatigue, dysphoric mood, and pain (Golomb, 2014). These results are currently being expanded in a GWIRP-funded trial of a "mitochondrial cocktail" for GWI of CoQ10 plus a number of nutrients chosen to support cellular energy production and defend against oxidative stress. The treatment is also being investigated in a larger, VA- sponsored Phase III trial of Ubiquinol, the reduced form of CoQ10.''}} | |||
| {{blockquote|''In a randomized, sham-controlled VA-funded trial of a nasal CPAP mask (Amin, 2011-b), symptomatic GW Veterans with sleep-disordered breathing receiving the CPAP therapy showed significant improvements in fatigue scores, cognitive function, sleep quality, and measures of physical and mental health (Amin, 2011a).''}} | |||
| {{blockquote|''Preliminary data from a GWIRP-funded acupuncture treatment study showed that Veterans reported significant reductions in pain and both primary and secondary health complaints, with results being more positive in the bi-weekly versus weekly treatment group (Conboy, 2012). Current studies funded by the GWIRP and the VA are also investigating yoga as a treatment for GWI.''}} | |||
| {{blockquote|''An amino acid supplement containing L-carnosine was found to reduce irritable bowel syndrome-associated diarrhea in a randomized, controlled GWIRP-funded trial in GW Veterans (Baraniuk, 2013). Veterans receiving L-carnosine showed a significant improvement in performance in a cognitive task, but no improvement in fatigue, pain, hyperalgesia, or activity levels.''}} | |||
| {{blockquote|''Results from a 26 week GWIRP-funded trial comparing standard care to nasal irrigation with either saline or a xylitol solution revealed that both irrigation protocols reduced GWI respiratory (chronic rhinosinusitis) and fatigue symptoms (Hayer, 2015).''}} | |||
| {{blockquote|''Administration of the glucocorticoid receptor antagonist mifepristone to GW Veterans in a GWIRP-funded randomized trial resulted in an improvement in verbal learning, but no improvement in self-reported physical health or other self-reported measures of mental health (Golier, 2016).''}}{{blockquote|'''''Ongoing Intervention Studies'''''}} | |||
| {{blockquote|''The GWIRP is currently funding many early-phase clinical trials aimed at GWI. Interventions include direct electrical nerve stimulation, repurposing FDA-approved pharmaceuticals, and dietary protocols and/or nutraceuticals. Both ongoing and closed GWIRP-supported clinical treatment trials and pilot studies can be found at .''}} | |||
| {{blockquote|''A Clinical Consortium Award was offered to support a group of institutions, coordinated through an Operations Center that will conceive, design, develop, and conduct collaborative Phase I and II clinical evaluations of promising therapeutic agents for the management or treatment of GWI. These mechanisms were designed to build on the achievements of the previously established consortia and to further promote collaboration and resource sharing.''}} | |||
| The ] has made significant and continuing investment in DoD's Gulf War illness treatment research, with $129 million appropriated for the GWIRP between federal fiscal years (FY) 2006 and 2016.<ref>{{Cite web |url=http://cdmrp.army.mil/gwirp/default |title=Gulf War Illness Research Program, Congressionally Directed Medical Research Programs |website=cdmrp.army.mil |access-date=2018-07-11 |df=dmy-all |archive-date=2018-07-11 |archive-url=https://web.archive.org/web/20180711185306/http://cdmrp.army.mil/gwirp/default }}</ref> The funding has risen from $5 million in FY2006, to $20 million each year from FY2013 through FY2017,<ref>{{Cite web |url=http://cdmrp.army.mil/gwirp/pbks/gwirppbk2018.pdf |title="Gulf War Illness Research Program", Congressionally Directed Medical Research Programs |website=cdmrp.army.mil |access-date=2018-07-11 |df=dmy-all |archive-date=2018-07-11 |archive-url=https://web.archive.org/web/20180711185302/http://cdmrp.army.mil/gwirp/pbks/gwirppbk2018.pdf }}</ref> and to $21 million for FY2018.<ref>{{Cite web |url=http://cdmrp.army.mil/funding/gwirp |title=Funding Opportunities-FY18 GWIRP, Congressionally Directed Medical Research Programs (CDMRP), US DoD |website=cdmrp.army.mil |access-date=2018-07-11 |df=dmy-all |archive-date=2018-07-11 |archive-url=https://web.archive.org/web/20180711185231/http://cdmrp.army.mil/funding/gwirp }}</ref> | |||
| == Prognosis == | |||
| According to the May 2018 DoD publication cited above, "Research suggests that the GWI symptomology experienced by Veterans has not improved over the last 25 years, with few experiencing improvement or recovery ... . Many Veterans will soon begin to experience the common co-morbidities associated with aging. The effect that aging will have on this unique and vulnerable population remains a matter of significant concern, and population-based research to obtain a better understanding of mortality, morbidity, and symptomology over time is needed."<ref name=":3" /> | |||
| == Prevalence == | |||
| The 2008 and 2014 VA (RAC) reports and the 2010 IOM report found that the chronic multisymptom illness in Gulf War veterans—Gulf War illness—is more prevalent in Gulf War veterans than their non-deployed counterparts or veterans of previous conflicts.<ref name="FedReport" /><ref name=":0" /><ref name="books.nap.edu" /> While a 2009 study found the pattern of comorbidities similar for actively deployed and nondeployed Australian military personnel, the large body of U.S. research reviewed in the VA and IOM reports showed the opposite in U.S. troops.<ref>{{cite journal | vauthors = Kelsall HL, McKenzie DP, Sim MR, Leder K, Forbes AB, Dwyer T | title = Physical, psychological, and functional comorbidities of multisymptom illness in Australian male veterans of the 1991 Gulf War | journal = American Journal of Epidemiology | volume = 170 | issue = 8 | pages = 1048–1056 | date = October 2009 | pmid = 19762370 | doi = 10.1093/aje/kwp238 | doi-access = free }}</ref> The VA's 2014 RAC report found Gulf War illness in "an excess of 26–32 percent of Gulf War veterans compared to nondeployed era veterans" in pre-2008 studies, and "an overall multisymptom illness prevalence of 37 percent in Gulf War veterans and an excess prevalence of 25 percent" in a later, larger VA study.<ref name=":0" /> | |||
| According to a May 2018 report by the ], "GWI is estimated to have affected 175,000 to 250,000 of the nearly 700,000 troops deployed to the 1990–1991 GW theater of operations. Twenty-seven of the 28 Coalition members participating in the GW conflict have reported GWI in their troops. Epidemiologic studies indicate that rates of GWI vary in different subgroups of GW Veterans. GWI affects Veterans who served in the U.S. Army and Marines Corps at higher rates than those who served in the Navy and Air Force, and U.S. enlisted personnel are affected more than officers. Studies also indicate that GWI rates differ according to where Veterans were located during deployment, with the highest rates among troops who served in forward areas."<ref name=":3">{{cite web |url=http://cdmrp.army.mil/gwirp/pdfs/GWIRP_Landscape.pdf |title=The Gulf War Illness Landscape |collaboration=Gulf War Illness Research Program |quote=Congressionally Directed Medical Research Program |publisher=U.S. Department of Defense |date=May 2018 |access-date=2018-07-11 |df=dmy-all |archive-date=2018-07-11 |archive-url=https://web.archive.org/web/20180711185414/http://cdmrp.army.mil/gwirp/pdfs/GWIRP_Landscape.pdf }}</ref> | |||
| == Research == | |||
| Epidemiologic studies have looked at many suspected causal factors for Gulf War illness as seen in veteran populations. Below is a summary of epidemiologic studies of veterans displaying multisymptom illness and their exposure to suspect conditions from the 2008 U.S. Department of Veterans Affairs report.<ref name=RAC230>{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=220 (p. 230 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref> | |||
| A fuller understanding of immune function in ill Gulf War veterans is needed, particularly in veteran subgroups with different clinical characteristics and exposure histories. It is also important to determine the extent to which identified immune perturbations may be associated with altered neurological and endocrine processes that are associated with immune regulation.<ref name=GWVI_08_p262>{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=262 (p. 272 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref> Very limited cancer data have been reported for U.S. Gulf War veterans in general, and no published research on cases occurring after 1999. Because of the extended latency periods associated with most cancers, it is important that cancer information is brought up to date and that cancer rates be assessed in Gulf War veterans on an ongoing basis. In addition, cancer rates should be evaluated in relation to identifiable exposure and location subgroups.<ref name=RAC55>{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=45 (p. 55 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref> | |||
| {| class="wikitable" <!-- this table has not been peer reviewed --> | {| class="wikitable" <!-- this table has not been peer reviewed --> | ||
| | |
|- | ||
| ! style="text-align: center;" colspan="7" | <big>Epidemiologic studies of Gulf War veterans:</big><br />association of deployment exposures with multisymptom illness<ref name=RAC222>{{cite report |year=2008 |title=Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations |publisher=U.S. Department of Veterans Affairs |page=222 (p. 232 in PDF) |url=http://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |url-status=live |archive-url=https://web.archive.org/web/20140603002651/http://www1.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf |archive-date=2014-06-03 |df=dmy-all}}</ref> | |||
| ! style="align: left;" colspan="8" | Epidemiologic Studies of Gulf War Veterans: Association of Deployment Exposures With Multisymptom Illness<ref> (page 222)</ref> | |||
| | |
|- | ||
| ! style="align: |
! style="text-align: center;" rowspan="3" |Suspected causative agent | ||
| ! style="align: |
! style="text-align: center;" colspan="2" |Preliminary analysis<br /><small>(no controls for exposure)</small> | ||
| ! style="align: |
! style="text-align: center;" colspan="3" |Adjusted analysis<br /><small>(controlled for effects of exposure)</small> | ||
| ! style="align: |
! style="text-align: center;" rowspan="3" |Clinical evaluations | ||
| | |
|- | ||
| ! style="align: left;" |
<!-- ! style="text-align: left;" | --> | ||
| ! style="align: |
! style="text-align: center;" colspan="2" |<small>GWV population in which<br /> association was ...</small> | ||
| ! style="align: |
! style="text-align: center;" colspan="3" |<small>GWV population in which<br /> association was ...</small> | ||
| ! style="align: left;" |
<!-- ! style="text-align: left;" | --> | ||
| |- | |||
| ! style="align: left;" colspan="1" |GWV population in which association was statistically significant | |||
| ! style="align: left;" |
<!-- ! style="text-align: left;" | --> | ||
| ! style="align: |
! style="text-align: right;" |assessed | ||
| ! style="text-align: right;" |statistically significant | |||
| |----- | |||
| ! style="align: |
! style="text-align: right;" |assessed | ||
| ! style="align: |
! style="text-align: right;" |statistically significant | ||
| ! style="align: |
! style="text-align: center;" |<small>Dose response effect identified?</small> | ||
| ! style="align: left;" |
<!-- ! style="text-align: left;" | --> | ||
| |- | |||
| ! style="align: left;" colspan="1" |6 | |||
| ! style="align: |
! style="text-align: right;" |Pyridostigmine bromide | ||
| | style="text-align: right;" |10 | |||
| ! style="align: left;" colspan="2" |<small>Associated with neurocognitive and HPA differences in GW vets</small> | |||
| | style="text-align: right;" |9 | |||
| |----- | |||
| | style="text-align: right;" |6 | |||
| | style="text-align: right;" |6 | |||
| | rowspan="2" style="text-align:center;" |✓ | |||
| | rowspan="2" style="text-align: left;" |<small>Associated with neurocognitive and HPA differences in GW vets</small> | |||
| |- | |||
| ! style="align: left;" colspan="1" |5 | |||
| ! style="align: |
! style="text-align: right;" |Pesticides | ||
| | style="text-align: right;" |10 | |||
| ! style="align: left;" colspan="2" |<small>Associated with neurocognitive and HPA differences in GW vets</small> | |||
| | style="text-align: right;" |10 | |||
| |----- | |||
| | style="text-align: right;" |6 | |||
| | style="text-align: right;" |5 | |||
| |- | |||
| ! style="align: left;" colspan="1" |13 | |||
| ! style="align: |
! style="text-align: right;" |Physiological stressors | ||
| | style="text-align: right;" |14 | |||
| | style="text-align: right;" |13 | |||
| | style="text-align: right;" |7 | |||
| | style="text-align: right;" |1 | |||
| |----- | |||
| | style="text-align:center;" | | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |13 | |||
| ! style="align: |
! style="text-align: right;" |Chemical weapons | ||
| | style="text-align: right;" |16 | |||
| | style="text-align: right;" |13 | |||
| | style="text-align: right;" |5 | |||
| ! style="align: left;" colspan="2" |<small>Associated with neurocognitive and HPA differences in GW vets</small> | |||
| | style="text-align: right;" |3 | |||
| |----- | |||
| | style="text-align:center;" | | |||
| | style="text-align: left;" |<small>Associated with neurocognitive and HPA differences in GW vets</small> | |||
| |- | |||
| ! style="align: left;" colspan="1" |8 | |||
| ! style="align: |
! style="text-align: right;" |Oil well<br />fires | ||
| | style="text-align: right;" |9 | |||
| | style="text-align: right;" |8 | |||
| | style="text-align: right;" |4 | |||
| | style="text-align: right;" |2 | |||
| |----- | |||
| | rowspan="2" style="text-align:center;" |✓ | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |2 | |||
| ! style="align: |
! style="text-align: right;" |Number of<br />vaccines | ||
| | style="text-align: right;" |2 | |||
| | style="text-align: right;" |2 | |||
| | style="text-align: right;" |1 | |||
| | style="text-align: right;" |1 | |||
| |----- | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |5 | |||
| ! style="align: |
! style="text-align: right;" |Anthrax<br />vaccine | ||
| | style="text-align: right;" |5 | |||
| | style="text-align: right;" |5 | |||
| | style="text-align: right;" |2 | |||
| | style="text-align: right;" |1 | |||
| | style="text-align:center;" | | |||
| |----- | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |5 | |||
| ! style="align: |
! style="text-align: right;" |Tent heater exhaust | ||
| | style="text-align: right;" |5 | |||
| | style="text-align: right;" |4 | |||
| | style="text-align: right;" |2 | |||
| | style="text-align: right;" |1 | |||
| | style="text-align:center;" | | |||
| |----- | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |3 | |||
| ! style="align: |
! style="text-align: right;" |Sand / particulates | ||
| | style="text-align: right;" |3 | |||
| | style="text-align: right;" |3 | |||
| | style="text-align: right;" |3 | |||
| | style="text-align: right;" |1 | |||
| | style="text-align:center;" | | |||
| |----- | |||
| | style="text-align: left;" | | |||
| |- | |||
| ! style="align: left;" colspan="1" |5 | |||
| ! style="align: |
! style="text-align: right;" |Depleted<br />uranium | ||
| | style="text-align: right;" |5 | |||
| | style="text-align: right;" |3 | |||
| | style="text-align: right;" |1 | |||
| | style="text-align: right;" |0 | |||
| | style="text-align:center;" | | |||
| |----- | |||
| | style="text-align: left;" | | |||
| |- | |||
| |} | |} | ||
| == |
== Controversies == | ||
| An early argument in the years following the Gulf War was that similar syndromes have been seen as an after effect of other conflicts — for example, "]" after ], and ] (PTSD) after the ].<ref>{{cite journal | vauthors = Hyams KC, Wignall FS, Roswell R | title = War syndromes and their evaluation: from the U.S. Civil War to the Persian Gulf War | journal = Annals of Internal Medicine | volume = 125 | issue = 5 | pages = 398–405 | date = September 1996 | pmid = 8702091 | doi = 10.7326/0003-4819-125-5-199609010-00007 | df = dmy-all | s2cid = 24433771 }}</ref> Cited as evidence for this argument was a review of the medical records of 15,000 ] soldiers showing that "those who lost at least 5% of their company had a 51% increased risk of later development of cardiac, gastrointestinal, or nervous disease."<ref>{{cite journal | vauthors = Pizarro J, Silver RC, Prause J | title = Physical and mental health costs of traumatic war experiences among Civil War veterans | journal = Archives of General Psychiatry | volume = 63 | issue = 2 | pages = 193–200 | date = February 2006 | pmid = 16461863 | pmc = 1586122 | doi = 10.1001/archpsyc.63.2.193 | df = dmy-all }}</ref> | |||
| Early Gulf War research also failed to accurately account for the prevalence, duration, and health impact of Gulf War illness. For example, a November 1996 article in the '']'' found no difference in death rates, hospitalization rates, or self-reported symptoms between Persian Gulf veterans and non-Persian Gulf veterans. This article was a compilation of dozens of individual studies involving tens of thousands of veterans. The study did find a statistically significant elevation in the number of traffic accidents Gulf War veterans had.<ref>{{cite journal | vauthors = Gray GC, Coate BD, Anderson CM, Kang HK, Berg SW, Wignall FS, Knoke JD, Barrett-Connor E | title = The postwar hospitalization experience of U.S. veterans of the Persian Gulf War | journal = The New England Journal of Medicine | volume = 335 | issue = 20 | pages = 1505–1513 | date = November 1996 | pmid = 8890103 | doi = 10.1056/nejm199611143352007 | df = dmy-all | doi-access = free }}</ref> An April 1998 article in '']'' similarly found no increased rate of hospitalization and better health on average for veterans of the Persian Gulf War in comparison to those who stayed home.<ref name=pmid_9621191>{{cite journal | vauthors = Knoke JD, Gray GC | title = Hospitalizations for unexplained illnesses among U.S. veterans of the Persian Gulf War | journal = Emerging Infectious Diseases | volume = 4 | issue = 2 | pages = 211–219 | year = 1998 | pmid = 9621191 | pmc = 2640148 | doi = 10.3201/eid0402.980208 }}</ref> | |||
| Similar syndromes have been seen as an after effect of other conflicts — for example, ']' after ], and ''] (PTSD)'' after the ]. A review of the medical records of 15,000 ] soldiers showed that "those who lost at least 5% of their company had a 51% increased risk of later development of cardiac, gastrointestinal, or nervous disease."<ref name="Enserink2001">{{cite doi|10.1126/science.291.5505.812}}</ref> | |||
| In contrast to those early studies, in January 2006, a study led by Melvin Blanchard published in the '']'', part of the "National Health Survey of Gulf War-Era Veterans and Their Families", found that veterans deployed in the Persian Gulf War had nearly twice the prevalence of chronic multisymptom illness, a cluster of symptoms similar to a set of conditions often at that time called Gulf War Syndrome.<ref>{{cite web |url=http://record.wustl.edu/news/page/normal/6377.html |title=Study finds multisymptom condition is more prevalent among Persian Gulf vets | vauthors = Purdy MC |date=2006-01-20 |publisher=] |archive-url=https://web.archive.org/web/20090414152555/http://record.wustl.edu/news/page/normal/6377.html |archive-date=2009-04-14 |url-status=live |access-date=2012-05-09 |df=dmy-all}}</ref> | |||
| A November 1996 article in the ] found no difference in death rates, hospitalization rates or self-reported symptoms between Persian Gulf veterans and non-Persian Gulf veterans. This article was a compilation of dozens of individual studies involving tens of thousands of veterans. The study did find a statistically significant elevation in the number of traffic accidents suffered by Gulf War veterans.<ref> New England Journal of Medicine. Disease and Suspicion after the Persian Gulf War. Volume 335:1525-1527, November 14, 1996</ref> An April, 1998 article in Emerging Infectious Diseases similarly found no increased rate of hospitalization and better health overall for veterans of the Persian Gulf War vs. Veterans who stayed home.<ref name=pmid_9621191>{{cite journal |author=Knoke JD, Gray GC |title=Hospitalizations for unexplained illnesses among U.S. veterans of the Persian Gulf War |journal=Emerging Infect. Dis. |volume=4 |issue=2 |pages=211–9 |year=1998 |pmid=9621191 |pmc=2640148 |doi= |url= http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640148/pdf/9621191.pdf}}</ref> | |||
| ]. claimed Gulf War syndrome as a defense in his murder trial]] | |||
| On November 17, 2008, the ] (VA) Research Advisory Committee on Gulf War Veterans' Illnesses (RAC), a Congressionally mandated ] composed of VA-appointed clinicians, researchers, and representative Gulf War veterans,<ref>{{cite web |url=https://www.va.gov/rac-gwvi/ |title=Research Advisory Committee on Gulf War Veterans' Illnesses home page |collaboration=Research Advisory Committee on Gulf War Veterans' Illnesses |website=va.gov |language=en |access-date=2018-07-11 |df=dmy-all}}</ref> issued a major report announcing scientific findings, in part, that "''Gulf War illness is real''", that GWI is a distinct physical condition, and that it is not psychological in nature. The 454 page report reviewed 1,840 published studies to form its conclusions identifying the high prevalence of Gulf War illness, suggesting likely causes rooted in toxic exposures while ruling out combat stress as a cause, and opining that treatments likely could be found. It recommended that Congress increase funding for treatment-focused Gulf War illness research to at least $60 million per year.<ref name="CNN">{{cite news |url=http://www.cnn.com/2008/HEALTH/11/17/gulf.war.illness.study/index.html |title=Gulf War illness is real, new federal report says |publisher=] | vauthors = Silverleib A |date=2008-12-09 |access-date=2012-05-09 |url-status=live |archive-url=https://web.archive.org/web/20121109040324/http://www.cnn.com/2008/HEALTH/11/17/gulf.war.illness.study/index.html |archive-date=2012-11-09 |df=dmy-all}}</ref><ref name="RAC11"/> | |||
| In March 2013, a hearing was held before the Subcommittee on Oversight and Investigations of the Committee on Veterans' Affairs, ], to determine not whether Gulf War illness exists, but rather how it is identified, diagnosed and treated, and how the tools put in place to aid these efforts have been used.<ref>{{cite web |url=https://purl.fdlp.gov/GPO/gpo45677 |title=Gulf War: What Kind of Care Are Veterans Receiving 20 Years Later? |quote=Hearing before the Subcommittee on Oversight and Investigations of the Committee on Veterans' Affairs, U.S. House of Representatives, One Hundred Thirteenth Congress, First Session, Wednesday, March 13, 2013. |department=Committee on Veterans' Affairs |publisher=U.S. House of Representatives}}</ref> | |||
| Despite these studies, on November 17, 2008 a congressionally appointed committee called the Research Advisory Committee on Gulf War Veterans' Illnesses, staffed with independent scientists and veterans appointed by the Department of Veterans Affairs, announced that the syndrome is a distinct physical condition. The committee recommended that Congress increase funding for research on Gulf War veterans' health to at least $60 million per year.<ref>News Services, "Gulf War Syndrome Is Real, Panel Concludes", '']'', November 18, 2008, p. 14.</ref> In January 2006, a study led by Melvin Blanchard and published by the '']'', part of the "National Health Survey of Gulf War-Era Veterans and Their Families", stated that veterans deployed in the Persian Gulf War had nearly twice the prevalence of chronic multisymptom illness, a cluster of symptoms similar to a set of conditions often called Gulf War Syndrome.<ref></ref> | |||
| By 2016, the National Academy of Sciences, Engineering, and Medicine (NASEM) concluded there was sufficient evidence of a positive association between deployment to the 1990–1991 Gulf War and Gulf War illness.<ref>{{cite book |series=Gulf War and Health |volume=10 |title=Update of Health Effects of Serving in the Gulf War | veditors = Cory-Slechta D, Wedge R, Fulco C, Liverman CT, Sox HC, Mitchell AE, Sivitz LB, Black RE |collaboration=Committee on Gulf War and Health |quote=Board on the Health of Select Populations; Institute of Medicine, National Academies of Sciences, Engineering, and Medicine |publisher=National Academy Press |year=2016 |isbn=978-0-309-07178-9 |location=Washington, D.C. |page=11 |oclc=45180227}}</ref> | |||
| ==See also== | |||
| *'']'' an 89-minute 2005 documentary that covers the Gulf War syndrome. | |||
| *] | |||
| === Jones controversy === | |||
| ==References== | |||
| Louis Jones Jr., the perpetrator of the 1995 ], stated that the Gulf War syndrome caused him to commit the crime and he sought clemency, hoping to avoid the death sentence imposed on him by a federal court.<ref name="MillerShould">{{cite news | vauthors = Miller M |url=http://www.newsweek.com/should-louis-jones-die-132259 |title=Should Louis Jones die? |archive-url=https://web.archive.org/web/20160809015628/http://www.newsweek.com/should-louis-jones-die-132259 |archive-date=2016-08-09 |df=dmy-all |magazine=] |date=March 12, 2003 |access-date=July 17, 2016}}</ref> Jones was executed in 2003.<ref name="Collins2003">{{cite news | vauthors = Collins D |url=http://www.cbsnews.com/news/gulf-war-vet-executed/ |title=Gulf War vet executed |archive-url=https://web.archive.org/web/20160819205707/http://www.cbsnews.com/news/gulf-war-vet-executed/ |archive-date=2016-08-19 |df=dmy-all |publisher=] |date=February 19, 2003 |access-date=July 17, 2016}}</ref> | |||
| {{Reflist|2}} | |||
| == Related legislation == | |||
| ==External links== | |||
| On March 14, 2014, Representative ] introduced the ] into the ], where it passed the House by unanimous consent but then died in Congress when the Senate failed to take action on it.<ref>{{cite web |url=https://www.congress.gov/bill/113th-congress/house-bill/4261/actions |title=Actions – H.R.4261 – 113th Congress (2013–2014): Gulf War Health Research Reform Act of 2014 | vauthors = Coffman M |date=2014-06-02 |website=congress.gov |access-date=2019-08-15 |df=dmy-all}}</ref> The bill would have altered the relationship between the Research Advisory Committee on Gulf War Veterans' Illnesses (RAC) and the ] (VA) under which the RAC is constituted. The bill would have made the RAC an independent organization within the VA, require that a majority of the RAC's members be appointed by Congress instead of the VA, and authorized the RAC to release its reports without needing prior approval from the VA Secretary.<ref name=CoffmanPRmar14>{{cite web | vauthors = Coffman M |title=Bipartisan Bill on Gulf War Health Research |url=http://coffman.house.gov/media-center/press-releases/bipartisan-bill-on-gulf-war-health-research|publisher=House Office of Mike Coffman |access-date=27 May 2014 |date=14 March 2014 |archive-url=https://web.archive.org/web/20140321054456/http://coffman.house.gov/media-center/press-releases/bipartisan-bill-on-gulf-war-health-research |archive-date=21 March 2014}}</ref><ref name=USAtoday14mar>{{cite news| vauthors = Kennedy K |title=Congress seeks independence for Gulf War illness board |url=https://www.usatoday.com/story/news/politics/2014/03/14/house-demands-independence-from-va-for-gulf-war-illness-advisory-board/6428299/ |access-date=27 May 2014 |newspaper=USA Today |date=14 March 2014 |url-status=live |archive-url=https://web.archive.org/web/20140530135801/http://www.usatoday.com/story/news/politics/2014/03/14/house-demands-independence-from-va-for-gulf-war-illness-advisory-board/6428299/ |archive-date=30 May 2014}}</ref> | |||
| In the year prior to the consideration of this bill, the VA and the RAC were at odds with one another.<ref name="USAtoday14mar" /> The VA replaced all but one of the members of the RAC, removed some of their supervisory tasks, tried to influence the board to decide that stress, rather than biology was the cause of Gulf War illness, and told the RAC that it could not publish reports without permission.<ref name="USAtoday14mar" /> The RAC was created after Congress decided that the VA's research into the issue was flawed, and focused on psychological causes, while mostly ignoring biological ones.<ref name="USAtoday14mar" /> | |||
| ; Research | |||
| * , publishers of the 2008 '''' (7.4 MB PDF) | |||
| * , founded in 1997 by Dr. Asaf Durakovic, M.D., formerly Chief of Professional Clinical Services in the U.S. Army's 531st Medical Detachment during the Desert Shield phase of the 1991 Gulf War and former Veteran's Administration official | |||
| The RAC was first authorized under the Veterans Programs Enhancement Act of 1998 (Section 104 of Public Law 105–368, enacted November 11, 1998, and now codified as 38 U.S.C. § 527 note).<ref name=":6">{{Cite web |url=https://www.va.gov/RAC-GWVI/docs/Committee_Documents/Legislation.pdf |title=Authorizing Legislation |last=U.S. Department of Veterans Affairs |access-date=August 15, 2019}}</ref><ref name=":4">{{Cite web|url=https://www.congress.gov/105/plaws/publ368/PLAW-105publ368.pdf |title=Veterans Programs Enhancement Act of 1998, Public Law 105–368 Section 104, 112 STAT. 3315 |last=U.S. Government Printing Office |access-date=August 15, 2019}}</ref> While the law directing its creation mandated that it be established not later than January 1, 1999,<ref name=":4" /> the RAC's first charter was not issued until January 23, 2002, by VA Secretary ].<ref>{{Cite web |url=https://www.va.gov/RAC-GWVI/Committee_Documents_Archived_Charters.asp |title=Archived Committee Charters, Research Advisory Committee on Gulf War Veterans' Illnesses |last=U.S. Department of Veterans Affairs |access-date=August 15, 2019}}</ref> The RAC convened for its first meetings on April 11–12, 2002.<ref name=RAC_GWVI_Minutes_2005>{{cite web |url=https://www.va.gov/RAC-GWVI/Pre_2014_Committee_Documents.asp |title=Pre 2014 Archived Meetings and Minutes, Research Advisory Committee on Gulf War Veterans' Illnesses |publisher=U.S. Department of Veterans Affairs |access-date=August 15, 2019}}</ref> | |||
| ; Associations | |||
| * | |||
| * | |||
| * | |||
| == See also == | |||
| ; Video | |||
| * ] | |||
| * ''Conspiracy Test: Gulf War Illness'' investigative report by the ] - , , , , | |||
| * ] | |||
| * ] | |||
| * ], an activist for those affected by Gulf War illness | |||
| * ]s | |||
| == References == | |||
| {{Reflist|25em}} | |||
| == External links == | |||
| {{Medical resources | |||
| | ICD9 = {{ICD9|V65.5}} (inconclusive) <br /> also nonstandard "DX111" | |||
| | MeshID = D018923 | |||
| | SNOMED CT = 95877004 | |||
| }} | |||
| {{Gulf War}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Gulf War Syndrome}} | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 01:18, 22 December 2024
Chronic disorder related to the Gulf WarMedical condition
| Gulf War syndrome | |
|---|---|
| Other names | Chronic multisymptom illness |
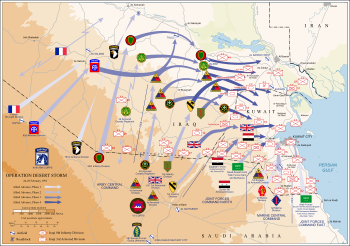 | |
| Summary of the Operation Desert Storm offensive ground campaign, February 24–28, 1991, by nationality | |
| Symptoms | Vary somewhat among individuals and include fatigue, headaches, cognitive dysfunction, musculoskeletal pain, insomnia, and respiratory, gastrointestinal, and dermatologic complaints |
| Causes | Toxic exposures during the 1990–91 Persian Gulf War. See Congressional records for testimony about chemical weapon disposal accident. |
| Differential diagnosis | myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS); fibromyalgia; multiple sclerosis (MS) |
| Frequency | 25% to 34% of the 697,000 U.S. troops of the 1990–91 Gulf War |
Gulf War syndrome (GWS) also known as Gulf War Illness or Chronic Multi-symptom Illness, is a chronic and multi-symptomatic disorder affecting military veterans of both sides of the Gulf War (1990–1991). A wide range of acute and chronic symptoms have been linked to it, including fatigue, muscle pain, cognitive problems, insomnia, rashes and diarrhea. Approximately 250,000 of the 697,000 U.S. veterans who served in the Gulf War have enduring chronic multi-symptom illness, a condition with serious consequences. From 1995 to 2005, the health of combat veterans worsened in comparison with nondeployed veterans, with the onset of more new chronic diseases, functional impairment, repeated clinic visits and hospitalizations, myalgic encephalomyelitis/chronic fatigue syndrome-like illness, post-traumatic stress disorder, and greater persistence of adverse health incidents.
Gulf War illness is linked to exposure to sub-lethal amounts of organophosphates, particularly sarin. Exposure to pesticides containing other organophosphates and exposure to pills containing pyridostigmine bromide, used as a pretreatment to protect against nerve agent effects, has been found to be associated with the neurological effects seen in Persian Gulf War syndrome. Other potential causes that have been investigated are cyclosarin and emissions from oil well fires, but their relationships to the illness are not as clear. Gulf War illness is not the result of combat or other stressors, and Gulf War veterans have lower rates of post-traumatic stress disorder (PTSD) than veterans of other wars.
The Royal British Legion said research suggested up to 33,000 UK Gulf War veterans could be living with Gulf War illness, with 1,300 claiming a war pension for conditions connected to their service. In 2007 the Royal British Legion produced a comprehensive report entitled Legacy of Suspicion, which made recommendations about necessary research and compensation. The Royal British Legion is still campaigning for the UK government to properly address symptoms experienced by veterans of the Gulf War.
According to a 2013 report by the Iraq and Afghanistan Veterans of America, veterans of the U.S. wars in Iraq and Afghanistan may also have Gulf War illness, though later findings identified causes that would not have been present in those wars.
Signs and symptoms
According to an April 2010 U.S. Department of Veterans Affairs (VA) sponsored study conducted by the Institute of Medicine (IOM), part of the U.S. National Academy of Sciences, 250,000 of the 696,842 U.S. servicemen and women in the 1991 Gulf War continue to be affected by chronic multi-symptom illness, which the IOM now refers to as Gulf War illness. The IOM found that it continued to affect these veterans nearly 20 years after the war.
According to the IOM, "It is clear that a significant portion of the soldiers deployed to the Gulf War have experienced troubling constellations of symptoms that are difficult to categorize," said committee chair Stephen L. Hauser, professor and chair, department of neurology, University of California, San Francisco (UCSF).
Unfortunately, symptoms that cannot be easily quantified are sometimes incorrectly dismissed as insignificant and receive inadequate attention and funding by the medical and scientific establishment. Veterans who continue to suffer from these symptoms deserve the very best that modern science and medicine can offer to speed the development of effective treatments, cures, and—we hope—prevention. Our report suggests a path forward to accomplish this goal, and we believe that through a concerted national effort and rigorous scientific input, answers can be found.
Questions still exist regarding why certain veterans showed, and still show, medically unexplained symptoms while others did not, why symptoms are diverse in some and specific in others, and why combat exposure is not consistently linked to having or not having symptoms. The lack of data on veterans' pre-deployment and immediate post-deployment health status and lack of measurement and monitoring of the various substances to which veterans may have been exposed make it difficult—and in many cases impossible—to reconstruct what happened to service members during their deployments nearly 20 years after the fact, the committee noted. The report called for a substantial commitment to improving identification and treatment of multisymptom illness in Gulf War veterans focussing on continued monitoring of Gulf War veterans, improved medical care, examination of genetic differences between symptomatic and asymptomatic groups and studies of environment-gene interactions.
A variety of signs and symptoms have been associated with GWI:
| Symptom | U.S. | UK | Australia | Denmark |
|---|---|---|---|---|
| Fatigue | 23% | 23% | 10% | 16% |
| Headache | 17% | 18% | 7% | 13% |
| Memory problems | 32% | 28% | 12% | 23% |
| Muscle/joint pain | 18% | 17% | 5% | 2% (<2%) |
| Diarrhea | 16% | 9% | 13% | |
| Dyspepsia/indigestion | 12% | 5% | 9% | |
| Neurological problems | 16% | 8% | 12% | |
| Terminal tumors | 33% | 9% | 11% |
- * This table applies only to coalition forces involved in combat.
| Condition | U.S. | UK | Canada | Australia |
|---|---|---|---|---|
| Skin conditions | 20–21% | 21% | 4–7% | 4% |
| Arthritis/joint problems | 6–11% | 10% | (-1)–3% | 2% |
| Gastro-intestinal (GI) problems | 15% | 5–7% | 1% | |
| Respiratory problem | 4–7% | 2% | 2–5% | 1% |
| Chronic fatigue syndrome | 1–4% | 3% | 0% | |
| Post-traumatic stress disorder | 2–6% | 9% | 6% | 3% |
| Chronic multi-symptom illness | 13–25% | 26% |
Birth defects have been suggested as a consequence of Gulf War deployment. However, a 2006 review of several studies of international coalition veterans' children found no strong or consistent evidence of an increase in birth defects, finding a modest increase in birth defects that was within the range of the general population, in addition to being unable to exclude recall bias as an explanation for the results. A 2008 report stated that "it is difficult to draw firm conclusions related to birth defects and pregnancy outcomes in Gulf War veterans", observing that while there have been "significant, but modest, excess rates of birth defects in children of Gulf War veterans", the "overall rates are still within the normal range found in the general population". The same report called for more research on the issue.
Comorbid illnesses
Persian Gulf War veterans have been identified to have an increased risk of multiple sclerosis.
A 2017 study by the U.S. Department of Veterans Affairs found that veterans possibly exposed to chemical warfare agents at Khamisiyah experienced different patterns of brain cancer mortality risk compared to the other groups, with veterans possibly exposed having a higher risk of brain cancer in the time period immediately following the Gulf War.
Iraqi veterans
Although an understudied group, opposing Iraqi veterans of the Iraqi Army in the Gulf War also experienced acute and chronic symptoms associated with Gulf War syndrome. A 2011 study in the U.S. Army Medical Department Journal reported Iraqi veterans of the Gulf War had a higher prevalence of somatic disorders as compared to Iraqi civilians, with risk greater in troops stationed in Kuwait.
In comparison to Allied troops, health symptoms were similar amongst Iraqi veterans:
| Symptom | Odds ratios (95% CI) - Zone 1 vs Zone 3 |
|---|---|
| Headaches | 3.65 (2.51–5.31) |
| Respiratory disorder | 4.09 (2.60–6.43) |
| Genitourinary disorder | 4.06 (2.65–6.21) |
| Musculoskeletal disorder | 4.33 (2.96–6.33) |
| Chronic fatigue | 126.3 (29.9–532.8) |
| Skin disorders | 1.89 (1.24–2.87) |
| Miscellaneous disorders | 4.43 (2.44–8.05) |
- * Zone 1 = In Kuwait, Zone 3 = 360 km from Kuwait.
Causes
Many of the symptoms of Gulf War illness are similar to the symptoms of organophosphate, mustard gas, and nerve gas poisoning. Gulf War veterans were exposed to a number of sources of these compounds, including nerve gas and pesticides. In 2022, researchers led by Robert Haley, MD at University of Texas Southwestern Medical Center found that exposure to sarin nerve gas in soldiers who had a particular genetic mutation that prevented them from breaking down the nerve gas is likely to be responsible for the syndrome. The findings and an editorial by two leading epidemiologists were published in Environmental Health Perspectives.
The United States Congress mandated the U.S. Department of Veterans Affairs' contract with the National Academy of Sciences (NAS) to provide reports on Gulf War illnesses. Between 1998 and 2009, the NAS's Institute of Medicine (IOM) authored ten such reports. In addition to the many physical and psychological issues involved in any war zone deployment, Gulf War veterans were exposed to a unique mix of hazards not previously experienced during wartime. These included pyridostigmine bromide pills (given to protect troops from the effects of nerve agents), depleted uranium munitions, and multiple simultaneous vaccinations including anthrax and botulinum toxin vaccines. The oil and smoke that spewed for months from hundreds of burning oil wells presented another exposure hazard not previously encountered in a war zone. Military personnel also had to cope with swarms of insects, requiring the widespread use of pesticides. High-powered microwaves were used to disrupt Iraqi communications, and though it is unknown whether this might have contributed to the syndrome, research has suggested that safety limits for electromagnetic radiation are too lenient.
The Research Advisory Committee on Gulf War Veterans' Illnesses (RAC), a VA federal advisory committee mandated by Congress in legislation enacted in 1998, found that pre-2005 studies suggested the veterans' illnesses are neurological and apparently are linked to exposure to neurotoxins, such as the nerve gas sarin, the anti-nerve gas drug pyridostigmine bromide, and pesticides that affect the nervous system. The RAC concluded in 2004 that, "research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans."
The RAC concluded that "exposure to pesticides and/or to PB are causally associated with GWI and the neurological dysfunction in GW veterans. Exposure to sarin and cyclosarin and to oil well fire emissions are also associated with neurologically based health effects. Gene-environment interactions are likely to have contributed to development of GWI in deployed veterans. The health consequences of chemical exposures in the GW and other conflicts have been called "toxic wounds" by veterans. This type of injury requires further study and concentrated treatment research efforts that may also benefit other occupational groups with similar exposure-related illnesses."
Sarin nerve agent
See also: Iraqi chemical weapons program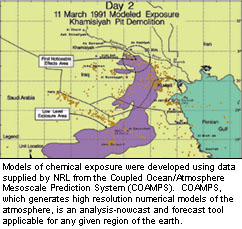
Low-level exposure to nerve agents has been suggested as the cause of GWI. In 1991, Chemical detection units from Czechoslovakia, France, and Britain confirmed chemical agents. French detection units detected chemical agents. Both Czech and French forces reported detections immediately to U.S. forces. U.S. forces detected, confirmed, and reported chemical agents; and U.S. soldiers were awarded medals for detecting chemical agents. The Riegle Report said that chemical alarms went off 18,000 times during the Gulf War. After the air war started on January 16, 1991, coalition forces were chronically exposed to low, nonlethal levels of chemical and biological agents released primarily by direct Iraqi attack via missiles, rockets, artillery, or aircraft munitions and by fallout from allied bombings of Iraqi chemical warfare munitions facilities.
In 1997, the US Government released an unclassified report that stated:
- "The US Intelligence Community (IC) has assessed that Iraq did not use chemical weapons during the Gulf war. However, based on a comprehensive review of intelligence information and relevant information made available by the United Nations Special Commission (UNSCOM), we conclude that chemical warfare (CW) agent was released as a result of US postwar demolition of rockets with chemical warheads in a bunker (called Bunker 73 by Iraq) and a pit in an area known as Khamisiyah."
Over 125,000 U.S. troops and 9,000 U.K. troops were exposed to nerve gas and mustard gas when the Iraqi depot in Khamisiyah was destroyed. Studies have confirmed earlier suspicions that exposure to sarin, in combination with other contaminants such as pesticides and PB were related to reports of veteran illness. Estimates range from 100,000 to 300,000 individuals exposed to nerve agents.
The 2014 report by the U.S. Department of Veterans Affairs (VA) Research Advisory Committee on Gulf War illnesses (RAC) concluded that, "exposure to the nerve gas agents sarin/cyclosarin has been linked in two more studies to changes in structural magnetic resonance imaging findings that are associated with cognitive decrements, further supporting the conclusion from evidence reviewed in the 2008 report that exposure to these agents is etiologically important to the central nervous system dysfunction that occurs in some subsets of Gulf War veterans."
A 2022 study of 1,016 U.S. Gulf War veterans found evidence of a causal link between GWI and exposure to low levels of sarin, which was released into the air by coalition bombing of Iraqi chemical weapons facilities. Significantly, the study found an increased incidence of GWI not only among veterans who recounted hearing nerve agent alarms, but also among veterans with the RR or QR (as opposed to the QQ) forms of the PON1 gene, which produces an enzyme that deactivates organophosphates (including sarin) through hydrolysis. By contrast, GWI was inversely associated with higher levels of the type Q isozyme, which is more efficient at breaking down sarin than its type R counterpart. The authors "found that the PON1 genotype and hearing nerve agent alarms were independent and the findings robust to both measured and unmeasured confounding, supporting a mechanistic interaction. ... Moreover, the change in the combined effect from one category to the next was significantly greater than the sum of the independent effects of the environmental exposure and the genotype". Although organophosphate pesticides could have triggered the nerve agent alarms in use at the time and contributed to neurotoxic symptoms similar to GWI, Haley et al. ruled out pesticides as a primary cause of GWI, citing that pesticide use was "ubiquitous long before the approximately 10,000 alarms began sounding at the start of the air campaign when Coalition bombing of Iraqi chemical weapon facilities released the fallout cloud that reached U.S. troop concentrations just as sarin was detected at multiple sites," while "the PON1 R isoenzyme is the more efficient detoxifier of most pesticides."
Earlier considered potential causes
Depleted uranium

The Gulf War included the first widespread combat usage of depleted uranium (DU), in tank kinetic energy penetrator and autocannon rounds. DU has been suggested as a possible cause of Gulf War syndrome.
A 2008 review by the U.S. Department of Veterans Affairs found no association between DU exposure and multisymptom illness, concluding that "exposure to DU munitions is not likely a primary cause of Gulf War illness". There is some evidence that long-term exposure to high doses of DU can cause other health problems that are unrelated to GWS. Since 2011, US combat veterans may claim disability compensation for health problems related to exposure to depleted uranium. The Veterans Administration decides these claims on a case-by-case basis.
A 2018 study stated that "the number of Gulf War veterans who developed the Gulf War syndrome following exposure to high quantities of DU has risen to about one-third of the 800,000 U.S. forces deployed," with 25,000 of those having had a premature death. A 2021 study by a team at the University of Portsmouth tested urine samples of 154 US veterans, reporting that no soldiers with the syndrome were exposed to significant amounts of depleted uranium and that DU "is not and never was in the bodies of those who are ill at sufficient quantities to cause disease".
Pyridostigmine bromide nerve gas antidote
The US military issued pyridostigmine bromide (PB) pills to protect against exposure to nerve gas agents such as sarin and soman. PB was used as a prophylactic against nerve agents; it is not a vaccine. Taken before exposure to nerve agents, PB was thought to increase the efficiency of nerve agent antidotes. PB had been used since 1955 for patients who have myasthenia gravis with doses up to 1,500 mg a day, far in excess of the 90 mg given to soldiers, and was considered safe by the FDA at either level for indefinite use and its use to pre-treat nerve agent exposure had recently been approved.
Given both the large body of epidemiological data on myasthenia gravis patients and follow-up studies done on veterans it was concluded that while it was unlikely that health effects reported today by Gulf War veterans are the result of exposure solely to PB, use of PB was causally associated with illness. However, a later review by the Institute of Medicine concluded that the evidence was not strong enough to establish a causal relationship.
Organophosphates
Organophosphate-induced delayed neuropathy (OPIDN, aka organophosphate-induced delayed polyneuropathy) may contribute to the unexplained illnesses of the Gulf War veterans.
Organophosphate pesticides
The use of organophosphate pesticides and insect repellents during the first Gulf War is credited with keeping rates of pest-borne diseases low. Pesticide use is one of only two exposures consistently identified by Gulf War epidemiologic studies to be significantly associated with Gulf War illness. Multisymptom illness profiles similar to Gulf War illness have been associated with low-level pesticide exposures in other human populations. In addition, Gulf War studies have identified dose-response effects, indicating that greater pesticide use is more strongly associated with Gulf War illness than more limited use. Pesticide use during the Gulf War has also been associated with neurocognitive deficits and neuroendocrine alterations in Gulf War veterans in clinical studies conducted following the end of the war. The 2008 report concluded that "all available sources of evidence combine to support a consistent and compelling case that pesticide use during the Gulf War is causally associated with Gulf War illness."
Less likely causes
According to the VA's 2008 RAC report, "For several Gulf War exposures, an association with Gulf War illness cannot be ruled out. These include low-level exposure to nerve agents, close proximity to oil well fires, receipt of multiple vaccines, and effects of combinations of Gulf War exposures." However, several potential causes of GWI were deemed, "not likely to have caused Gulf War illness for the majority of ill veterans," including "depleted uranium, anthrax vaccine, fuels, solvents, sand and particulates, infectious diseases, and chemical agent resistant coating (CARC)," for which "there is little evidence supporting an association with Gulf War illness or a major role is unlikely based on what is known about exposure patterns during the Gulf War and more recent deployments."
The VA's 2014 RAC report reinforced its 2008 report findings: "The research reviewed in this report supports and reinforces the conclusion in the 2008 RACGWVI report that exposures to pesticides and pyridostigmine bromide are causally associated with Gulf War illness. Evidence also continues to demonstrate that Gulf War illness is not the result of psychological stressors during the war." It also found additional evidence since the 2008 report for the role of sarin in GWI, but inadequate evidence regarding exposures to oil well fires, vaccines, and depleted uranium to make new conclusions about them.
Oil well fires
During the war, many oil wells were set on fire in Kuwait by the retreating Iraqi army, and the smoke from those fires was inhaled by large numbers of soldiers, many of whom had acute pulmonary and other chronic effects, including asthma and bronchitis. However, firefighters who were assigned to the oil well fires and encountered the smoke, but who did not take part in combat, have not had GWI symptoms. The 2008 RAC report states that "evidence is inconsistent or limited in important ways."
Anthrax vaccine
| This article needs to be updated. Please help update this article to reflect recent events or newly available information. (January 2022) |
Iraq had loaded anthrax, botulinum toxin, and aflatoxin into missiles and artillery shells in preparing for the Gulf War and these munitions were deployed to four locations in Iraq. During Operation Desert Storm, 41% of U.S. combat soldiers and 75% of UK combat soldiers were vaccinated against anthrax. Reactions included local skin irritation, some lasting for weeks or months. While the Food and Drug Administration (FDA) approved the vaccine, it never went through large-scale clinical trials.
While recent studies have demonstrated the vaccine is highly reactogenic, there is no clear evidence or epidemiological studies on Gulf War veterans linking the vaccine to Gulf War illness. Combining this with the lack of symptoms from current deployments of individuals who have received the vaccine led the Committee on Gulf War Veterans' Illnesses to conclude that the vaccine is not a likely cause of Gulf War illness for most ill veterans. However, the committee report does point out that veterans who received a larger number of various vaccines in advance of deployment have shown higher rates of persistent symptoms since the war.
However, research was done by PB Asa, Y Cao, and RF Garry on serum antibodies to squalene in Gulf War Syndrome patients. The results showed "the substantial majority (95%) of overtly ill deployed GWS patients had antibodies to squalene. All (100%) GWS patients immunized for service in Desert Shield/Desert Storm who did not deploy, but had the same signs and symptoms as those who did deploy, had antibodies to squalene. In contrast, none (0%) of the deployed Persian Gulf veterans not showing signs and symptoms of GWS have antibodies to squalene. Neither patients with idiopathic autoimmune disease nor healthy controls had detectable serum antibodies to squalene." Their work of the researchers was profiled by Gary Matsumoto in "Vaccine A".
This research and theory was later criticized, and further research has leaned heavily against squalene in vaccinations causing GWS; Perhaps the most important points against this theory include that squalene antibodies have been detected in populations not exposed to squalene containing vaccinations, and that the anthrax vaccines used in the Gulf War did not actually contain squalene in any form.
Combat stress
Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans, according to a U.S. Department of Veterans Affairs (VA) review committee. An April 2010 Institute of Medicine review found, "the excess of unexplained medical symptoms reported by deployed Gulf war veterans cannot be reliably ascribed to any known psychiatric disorder", although they also concluded that "the constellation of unexplained symptoms associated with the Gulf War illness complex could result from interplay between both biological and psychological factors."
Pathobiology
Chronic inflammation
The 2008 VA report on Gulf War illness and the Health of Gulf War Veterans suggested a possible link between GWI and chronic, nonspecific inflammation of the central nervous system that cause pain, fatigue and memory issues, possibly due to pathologically persistent increases in cytokines and suggested further research be conducted on this issue.
Diagnosis
Clinical diagnosis of Gulf War illness has been complicated by multiple case definitions. In 2014, the National Academy of Sciences Institute of Medicine (IOM)—contracted by the U.S. Department of Veterans Affairs for the task—released a report concluding that the creation of a new case definition for chronic multisymptom illness in Gulf War veterans was not possible because of insufficient evidence in published studies regarding its onset, duration, severity, frequency of symptoms, exclusionary criteria, and laboratory findings. Instead, the report recommended the use of two case definitions, the "Kansas" definition and the "Centers for Disease Control and Prevention (CDC)" definition, noting: "There is a set of symptoms (fatigue, pain, neurocognitive) that are reported in all the studies that have been reviewed. The CDC definition captures those three symptoms; the Kansas definition also captures them, but it also includes the symptoms reported most frequently by Gulf War veterans."
The Kansas case definition is more specific and may be more applicable for research settings, while the CDC case definition is more broad and may be more applicable for clinical settings.
Classification
Medical ailments associated with service in the 1990–1991 Gulf War have been recognized by both the U.S. Department of Defense and the U.S. Department of Veterans Affairs.
Before 1998, the terms Gulf War syndrome, Gulf War veterans' illness, unexplained illness, and undiagnosed illness were used interchangeably to describe chronic unexplained symptoms in veterans of the 1991 Gulf War. The term chronic multisymptom illness (CMI) was first used following publication of a 1998 study describing chronic unexplained symptoms in Air Force veterans of the 1991 Gulf War.
In a 2014 report contracted by the U.S. Department of Veterans Affairs, the National Academy of Sciences Institute of Medicine recommended the use the term Gulf War illness rather than chronic multisymptom illness. Since that time, relevant publications by the National Academy of Science and the U.S. Department of Defense have used only the term Gulf War illness (GWI).
The U.S. Department of Veterans Affairs (VA) confusingly still uses an array of both old and new terminology for Gulf War illness. VA's specialty clinical evaluation War Related Illness and Injury Study Centers (WRIISCs) use the recommended term Gulf War illness, as do VA's Office of Research and Development (VA-ORD) and many recent VA research publications. However, VA's Public Health website still uses Gulf War veterans' medically unexplained illnesses, chronic multi-symptom illness (CMI), and undiagnosed illnesses, but explains that VA doesn't use the term Gulf War syndrome because of varying symptoms.
The Veterans Health Administration (VHA) originally classified individuals with related ailments believed to be connected to their service in the Persian Gulf a special non-ICD-9 code DX111, as well as ICD-9 code V65.5.
Kansas definition
In 1998, the State of Kansas Persian Gulf Veterans Health Initiative sponsored an epidemiological survey led by Dr. Lea Steele of deployment-related symptoms in 2,030 Gulf War veterans. The result was a "clinically based descriptive definition using correlated symptoms" in six symptom groups: fatigue and sleep problems, pain, neurologic and mood, gastrointestinal, respiratory symptoms, and skin (dermatologic) symptoms.
To meet the "Kansas" case definition, a veteran of the 1990–91 Gulf War must have symptoms in at least three of the six symptom domains, which during the survey were scored based on severity ("severity"). Symptom onset must have developed during or after deploying to the 1990–91 Gulf War theatre of operations ("onset") and must have been present in the year before interview ("duration"). Participants were excluded if they had a diagnosis of or were being treated for any of several conditions that might otherwise explain their symptoms ("exclusionary criteria"), including cancer, diabetes, heart disease, chronic infectious disease, lupus, multiple sclerosis, stroke, or any serious psychiatric condition.
Applying the Kansas case definition to the original Kansas study cohort resulted in a prevalence of Gulf War illness of 34.2% in Gulf War veterans and 8.3% in nondeployed Gulf War era veterans, or an excess rate of GWI of 26.3% in Gulf War veterans.
CDC definition
Also in 1998, a study published by Dr. Keiji Fukuda under the auspices of the U.S. Centers for Disease Control and Prevention (CDC) examined chronic multisymptom illness through a cross-sectional survey of 3,675 ill and healthy U.S. Air Force veterans of the 1990–91 Gulf War, including from a Pennsylvania-based Air National Guard unit and three comparison Air Force units. The CDC case definition was derived from clinical data and statistical analyses.
The result was a symptom-category approach to a case definition, with three symptom categories: fatigue, mood–cognition, and musculoskeletal. To meet the case definition, the veteran of the 1990–91 Gulf War must have symptoms in two of the three categories and have experienced the illness for six months or longer ("duration").
The original study also including a determination of severity of symptoms ("severity"). "Severe cases were identified if at least one symptom in each of the required categories was rated as severe. Of 1,155 participating Gulf War veterans, 6% had severe CMI, and 39% had mild to moderate CMI; of the 2,520 nondeployed era veterans, 0.7% had severe and 14% had mild to moderate CMI."
Treatment
A 2013 report by the Institute of Medicine reviewed the peer-reviewed published medical literature for evidence regarding treatments for symptoms associated with chronic multisymptom illness (CMI) in 1990–91 Gulf War veterans, and in other chronic multisymptom conditions. For the studies the report reviewed that were specifically regarding CMI in 1990–91 Gulf War veterans (Gulf War illness), the report made the following conclusions:
- Doxycycline: "Although the study of doxycycline was found to have high strength of evidence and was conducted in a group of 1991 Gulf War veterans who had CMI, it did not demonstrate efficacy; that is, doxycycline did not reduce or eliminate the symptoms of CMI in the study population."
- Cognitive behavioral therapy (CBT) and exercise: "These studies evaluated the effects of exercise and CBT in combination and individually. The therapeutic benefit of exercise was unclear in those studies. Group CBT rather than exercise may confer the main therapeutic benefit with respect to physical symptoms."
The report concluded: "On the basis of the evidence reviewed, the committee cannot recommend any specific therapy as a set treatment for veterans who have CMI. The committee believes that a 'one-size-fits-all' approach is not effective for managing veterans who have CMI and that individualized health care management plans are necessary."
By contrast, the U.S. Department of Defense (DoD) noted in a May 2018 publication that the primary focus of its Gulf War illness Research Program (GWIRP) "has been to fund research studies to identify treatment targets and test interventional approaches to alleviate symptoms. While most of these studies remain in progress, several have already shown varying levels of promise as GWI treatments."
According to the May 2018 DoD publication:
Published Results on Treatments
The earliest federally funded multi-center clinical trials were VA- and DoD-funded trials that focused on antibiotic treatment (doxycycline) (Donta, 2004) and cognitive behavioral therapy with exercise (Donta, 2003). Neither intervention provided long-lasting improvement for a substantial number of Veterans.
Preliminary analysis from a placebo-controlled trial showed that 100 mg of Coenzyme Q10 (known as CoQ10 or Ubiquinone) significantly improved general self-reported health and physical functioning, including among 20 symptoms, each of which was present in at least half of the study participants, with the exception of sleep. These improvements included reducing commonly reported symptoms of fatigue, dysphoric mood, and pain (Golomb, 2014). These results are currently being expanded in a GWIRP-funded trial of a "mitochondrial cocktail" for GWI of CoQ10 plus a number of nutrients chosen to support cellular energy production and defend against oxidative stress. The treatment is also being investigated in a larger, VA- sponsored Phase III trial of Ubiquinol, the reduced form of CoQ10.
In a randomized, sham-controlled VA-funded trial of a nasal CPAP mask (Amin, 2011-b), symptomatic GW Veterans with sleep-disordered breathing receiving the CPAP therapy showed significant improvements in fatigue scores, cognitive function, sleep quality, and measures of physical and mental health (Amin, 2011a).
Preliminary data from a GWIRP-funded acupuncture treatment study showed that Veterans reported significant reductions in pain and both primary and secondary health complaints, with results being more positive in the bi-weekly versus weekly treatment group (Conboy, 2012). Current studies funded by the GWIRP and the VA are also investigating yoga as a treatment for GWI.
An amino acid supplement containing L-carnosine was found to reduce irritable bowel syndrome-associated diarrhea in a randomized, controlled GWIRP-funded trial in GW Veterans (Baraniuk, 2013). Veterans receiving L-carnosine showed a significant improvement in performance in a cognitive task, but no improvement in fatigue, pain, hyperalgesia, or activity levels.
Results from a 26 week GWIRP-funded trial comparing standard care to nasal irrigation with either saline or a xylitol solution revealed that both irrigation protocols reduced GWI respiratory (chronic rhinosinusitis) and fatigue symptoms (Hayer, 2015).
Administration of the glucocorticoid receptor antagonist mifepristone to GW Veterans in a GWIRP-funded randomized trial resulted in an improvement in verbal learning, but no improvement in self-reported physical health or other self-reported measures of mental health (Golier, 2016).
Ongoing Intervention Studies
The GWIRP is currently funding many early-phase clinical trials aimed at GWI. Interventions include direct electrical nerve stimulation, repurposing FDA-approved pharmaceuticals, and dietary protocols and/or nutraceuticals. Both ongoing and closed GWIRP-supported clinical treatment trials and pilot studies can be found at .
A Clinical Consortium Award was offered to support a group of institutions, coordinated through an Operations Center that will conceive, design, develop, and conduct collaborative Phase I and II clinical evaluations of promising therapeutic agents for the management or treatment of GWI. These mechanisms were designed to build on the achievements of the previously established consortia and to further promote collaboration and resource sharing.
The U.S Congress has made significant and continuing investment in DoD's Gulf War illness treatment research, with $129 million appropriated for the GWIRP between federal fiscal years (FY) 2006 and 2016. The funding has risen from $5 million in FY2006, to $20 million each year from FY2013 through FY2017, and to $21 million for FY2018.
Prognosis
According to the May 2018 DoD publication cited above, "Research suggests that the GWI symptomology experienced by Veterans has not improved over the last 25 years, with few experiencing improvement or recovery ... . Many Veterans will soon begin to experience the common co-morbidities associated with aging. The effect that aging will have on this unique and vulnerable population remains a matter of significant concern, and population-based research to obtain a better understanding of mortality, morbidity, and symptomology over time is needed."
Prevalence
The 2008 and 2014 VA (RAC) reports and the 2010 IOM report found that the chronic multisymptom illness in Gulf War veterans—Gulf War illness—is more prevalent in Gulf War veterans than their non-deployed counterparts or veterans of previous conflicts. While a 2009 study found the pattern of comorbidities similar for actively deployed and nondeployed Australian military personnel, the large body of U.S. research reviewed in the VA and IOM reports showed the opposite in U.S. troops. The VA's 2014 RAC report found Gulf War illness in "an excess of 26–32 percent of Gulf War veterans compared to nondeployed era veterans" in pre-2008 studies, and "an overall multisymptom illness prevalence of 37 percent in Gulf War veterans and an excess prevalence of 25 percent" in a later, larger VA study.
According to a May 2018 report by the U.S. Department of Defense, "GWI is estimated to have affected 175,000 to 250,000 of the nearly 700,000 troops deployed to the 1990–1991 GW theater of operations. Twenty-seven of the 28 Coalition members participating in the GW conflict have reported GWI in their troops. Epidemiologic studies indicate that rates of GWI vary in different subgroups of GW Veterans. GWI affects Veterans who served in the U.S. Army and Marines Corps at higher rates than those who served in the Navy and Air Force, and U.S. enlisted personnel are affected more than officers. Studies also indicate that GWI rates differ according to where Veterans were located during deployment, with the highest rates among troops who served in forward areas."
Research
Epidemiologic studies have looked at many suspected causal factors for Gulf War illness as seen in veteran populations. Below is a summary of epidemiologic studies of veterans displaying multisymptom illness and their exposure to suspect conditions from the 2008 U.S. Department of Veterans Affairs report.
A fuller understanding of immune function in ill Gulf War veterans is needed, particularly in veteran subgroups with different clinical characteristics and exposure histories. It is also important to determine the extent to which identified immune perturbations may be associated with altered neurological and endocrine processes that are associated with immune regulation. Very limited cancer data have been reported for U.S. Gulf War veterans in general, and no published research on cases occurring after 1999. Because of the extended latency periods associated with most cancers, it is important that cancer information is brought up to date and that cancer rates be assessed in Gulf War veterans on an ongoing basis. In addition, cancer rates should be evaluated in relation to identifiable exposure and location subgroups.
| Epidemiologic studies of Gulf War veterans: association of deployment exposures with multisymptom illness | ||||||
|---|---|---|---|---|---|---|
| Suspected causative agent | Preliminary analysis (no controls for exposure) |
Adjusted analysis (controlled for effects of exposure) |
Clinical evaluations | |||
| GWV population in which association was ... |
GWV population in which association was ... | |||||
| assessed | statistically significant | assessed | statistically significant | Dose response effect identified? | ||
| Pyridostigmine bromide | 10 | 9 | 6 | 6 | ✓ | Associated with neurocognitive and HPA differences in GW vets |
| Pesticides | 10 | 10 | 6 | 5 | ||
| Physiological stressors | 14 | 13 | 7 | 1 | ||
| Chemical weapons | 16 | 13 | 5 | 3 | Associated with neurocognitive and HPA differences in GW vets | |
| Oil well fires |
9 | 8 | 4 | 2 | ✓ | |
| Number of vaccines |
2 | 2 | 1 | 1 | ||
| Anthrax vaccine |
5 | 5 | 2 | 1 | ||
| Tent heater exhaust | 5 | 4 | 2 | 1 | ||
| Sand / particulates | 3 | 3 | 3 | 1 | ||
| Depleted uranium |
5 | 3 | 1 | 0 | ||
Controversies
An early argument in the years following the Gulf War was that similar syndromes have been seen as an after effect of other conflicts — for example, "shell shock" after World War I, and post-traumatic stress disorder (PTSD) after the Vietnam War. Cited as evidence for this argument was a review of the medical records of 15,000 American Civil War soldiers showing that "those who lost at least 5% of their company had a 51% increased risk of later development of cardiac, gastrointestinal, or nervous disease."
Early Gulf War research also failed to accurately account for the prevalence, duration, and health impact of Gulf War illness. For example, a November 1996 article in the New England Journal of Medicine found no difference in death rates, hospitalization rates, or self-reported symptoms between Persian Gulf veterans and non-Persian Gulf veterans. This article was a compilation of dozens of individual studies involving tens of thousands of veterans. The study did find a statistically significant elevation in the number of traffic accidents Gulf War veterans had. An April 1998 article in Emerging Infectious Diseases similarly found no increased rate of hospitalization and better health on average for veterans of the Persian Gulf War in comparison to those who stayed home.
In contrast to those early studies, in January 2006, a study led by Melvin Blanchard published in the Journal of Epidemiology, part of the "National Health Survey of Gulf War-Era Veterans and Their Families", found that veterans deployed in the Persian Gulf War had nearly twice the prevalence of chronic multisymptom illness, a cluster of symptoms similar to a set of conditions often at that time called Gulf War Syndrome.

On November 17, 2008, the Department of Veterans Affairs (VA) Research Advisory Committee on Gulf War Veterans' Illnesses (RAC), a Congressionally mandated federal advisory committee composed of VA-appointed clinicians, researchers, and representative Gulf War veterans, issued a major report announcing scientific findings, in part, that "Gulf War illness is real", that GWI is a distinct physical condition, and that it is not psychological in nature. The 454 page report reviewed 1,840 published studies to form its conclusions identifying the high prevalence of Gulf War illness, suggesting likely causes rooted in toxic exposures while ruling out combat stress as a cause, and opining that treatments likely could be found. It recommended that Congress increase funding for treatment-focused Gulf War illness research to at least $60 million per year.
In March 2013, a hearing was held before the Subcommittee on Oversight and Investigations of the Committee on Veterans' Affairs, U.S. House of Representatives, to determine not whether Gulf War illness exists, but rather how it is identified, diagnosed and treated, and how the tools put in place to aid these efforts have been used.
By 2016, the National Academy of Sciences, Engineering, and Medicine (NASEM) concluded there was sufficient evidence of a positive association between deployment to the 1990–1991 Gulf War and Gulf War illness.
Jones controversy
Louis Jones Jr., the perpetrator of the 1995 murder of Tracie McBride, stated that the Gulf War syndrome caused him to commit the crime and he sought clemency, hoping to avoid the death sentence imposed on him by a federal court. Jones was executed in 2003.
Related legislation
On March 14, 2014, Representative Mike Coffman introduced the Gulf War Health Research Reform Act of 2014 (H.R. 4261; 113th Congress) into the United States House of Representatives, where it passed the House by unanimous consent but then died in Congress when the Senate failed to take action on it. The bill would have altered the relationship between the Research Advisory Committee on Gulf War Veterans' Illnesses (RAC) and the United States Department of Veterans Affairs (VA) under which the RAC is constituted. The bill would have made the RAC an independent organization within the VA, require that a majority of the RAC's members be appointed by Congress instead of the VA, and authorized the RAC to release its reports without needing prior approval from the VA Secretary.
In the year prior to the consideration of this bill, the VA and the RAC were at odds with one another. The VA replaced all but one of the members of the RAC, removed some of their supervisory tasks, tried to influence the board to decide that stress, rather than biology was the cause of Gulf War illness, and told the RAC that it could not publish reports without permission. The RAC was created after Congress decided that the VA's research into the issue was flawed, and focused on psychological causes, while mostly ignoring biological ones.
The RAC was first authorized under the Veterans Programs Enhancement Act of 1998 (Section 104 of Public Law 105–368, enacted November 11, 1998, and now codified as 38 U.S.C. § 527 note). While the law directing its creation mandated that it be established not later than January 1, 1999, the RAC's first charter was not issued until January 23, 2002, by VA Secretary Anthony Principi. The RAC convened for its first meetings on April 11–12, 2002.
See also
- Organophosphate-induced delayed neuropathy
- Ukrainian syndrome
- Environmental issues with war
- Michael Donnelly, an activist for those affected by Gulf War illness
- Burn pits
References
- "Persian Gulf War and Health: Treatment for Chronic Multisymptom Illness". Health and Medicine Division. nationalacademies.org. Archived from the original on 11 May 2017.
- "U.S. Chemical and Biological Warfare-related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Persian Gulf War" (PDF). United States Senate Committee on Banking, Housing, and Urban Affairs. May 25, 1994.
A Report of Chairman Donald W. Riegle Jr., and Ranking Member Alfonse M. D'Amato of the Committee on Banking, Housing, and Urban Affairs with respect to Export Administration – United States Senate
- ^ "Persian Gulf War Veterans' Medically Unexplained Illnesses". Veterans Health. Public Health. U.S. Department of Veterans Affairs.
- ^ "Gulf War Veterans' Illnesses: Illnesses Associated with Gulf War Service". United States Department of Veterans Affairs. nd. Archived from the original on 12 February 2012. Retrieved 9 May 2012.
- Iversen A, Chalder T, Wessely S (October 2007). "Gulf War Illness: lessons from medically unexplained symptoms". Clinical Psychology Review. 27 (7): 842–854. doi:10.1016/j.cpr.2007.07.006. PMID 17707114.
- Gronseth GS (May 2005). "Gulf war syndrome: a toxic exposure? A systematic review". Neurologic Clinics. 23 (2): 523–540. doi:10.1016/j.ncl.2004.12.011. PMID 15757795.
- "Gulf War Syndrome". University of Virginia. Archived from the original on 14 July 2004.
- ^ Stencel C (9 April 2010). "Gulf War service linked to post-traumatic stress disorder, multisymptom illness, other health problems, but causes are unclear". National Academy of Sciences. Archived from the original on 14 March 2012. Retrieved 9 May 2012.
- ^ Research Advisory Committee on Gulf War Veterans' Illnesses (1 November 2008). "Gulf War Illness and the Health of Persian Gulf War Veterans: Scientific Findings and Recommendations" (PDF). U.S. Department of Veterans Affairs. Archived (PDF) from the original on 9 November 2013. Retrieved 9 May 2012.
- Li B, Mahan CM, Kang HK, Eisen SA, Engel CC (October 2011). "Longitudinal health study of US 1991 Gulf War veterans: changes in health status at 10-year follow-up". American Journal of Epidemiology. 174 (7): 761–768. doi:10.1093/aje/kwr154. PMID 21795757.
- ^ Cruz-Hernandez A, Roney A, Goswami DG, Tewari-Singh N, Brown JM (November 2022). "A review of chemical warfare agents linked to respiratory and neurological effects experienced in Gulf War Illness". Inhalation Toxicology. 34 (13–14): 412–432. Bibcode:2022InhTx..34..412C. doi:10.1080/08958378.2022.2147257. PMC 9832991. PMID 36394251.
- ^ Weisskopf MG, Sullivan KA (May 2022). "Invited Perspective: Causal Implications of Gene by Environment Studies Applied to Gulf War Illness". Environmental Health Perspectives. 130 (5): 51301. doi:10.1289/EHP11057. PMC 9093160. PMID 35543506.
- ^ "UTSW genetic study confirms sarin nerve gas as cause of Gulf War illness". UT Southwestern Medical Center. May 11, 2022.
- ^ Gulf War Illness and the Health of Persian Gulf War Veterans: Research Update and Recommendations, 2009–2013: Updated Scientific Findings and Recommendations (PDF). Washington, DC: U.S. Department of Veterans Affairs. May 2014. pp. 3, 9–10, 20.
- ^ White RF, Steele L, O'Callaghan JP, Sullivan K, Binns JH, Golomb BA, et al. (January 2016). "Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: Effects of toxicant exposures during deployment". Cortex; A Journal Devoted to the Study of the Nervous System and Behavior. What's your poison? Neurobehavioural consequences of exposure to industrial, agricultural and environmental chemicals. 74: 449–475. doi:10.1016/j.cortex.2015.08.022. PMC 4724528. PMID 26493934.
- "What is Persian Gulf War Illness?". Royal British Legion. 20 February 2020. Retrieved 25 May 2021.
- "Gulf War syndrome 'not caused by depleted uranium'". BBC News. 18 February 2021. Retrieved 24 February 2021.
- "Gulf War: a legacy of suspicion" (PDF). Royal British Legion. Retrieved 25 May 2021.
- "Gulf War illnesses". Royal British Legion. 8 February 2019. Retrieved 25 May 2021.
- Kennedy, Kelly (23 January 2013). "Report: New vets show Gulf War illness symptoms". Army Times. USA Today. Retrieved 28 January 2013.
- ^ "Pre 2014 Archived Meetings and Minutes, Research Advisory Committee on Gulf War Veterans' Illnesses". U.S. Department of Veterans Affairs. Retrieved August 15, 2019.
- Doyle P, Maconochie N, Ryan M (April 2006). "Reproductive health of Gulf War veterans". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 361 (1468): 571–584. doi:10.1098/rstb.2006.1817. PMC 1569619. PMID 16687262.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 50 (p. 60 in PDF). Archived (PDF) from the original on 3 June 2014.
- "The Gulf War era multiple sclerosis cohort: age and incidence rates by race, sex and service" (PDF). va.gov. Archived from the original (PDF) on 13 November 2016. Retrieved 12 November 2016.
- Barth SK, Dursa EK, Bossarte RM, Schneiderman AI (October 2017). "Trends in brain cancer mortality among U.S. Gulf War veterans: 21 year follow-up". Cancer Epidemiology. 50 (Pt A): 22–29. doi:10.1016/j.canep.2017.07.012. PMC 5824993. PMID 28780478.
- ^ Jamil H, Hamdan TA, Grzybowski M, Arnetz BB (2011). "Health effects associated with geographical area of residence during the 1991 Gulf War: a comparative health study of Iraqi soldiers and civilians". U.S. Army Medical Department Journal: 87–96. PMC 3159173. PMID 21805460.
- Friis RH, Sellers TA (2004). Epidemiology for Public Health Practice. Jones & Bartlett Publishers. ISBN 978-0-7637-3170-0.
- Spektor DM, Rettig RA, Hilborne LH, Golomb BA, Marshall GN, Davis LM, et al. (1998). A Review of the Scientific Literature as it Pertains to Gulf War Illnesses. RAND Corporation. ISBN 978-0-8330-2680-4.
- "Campaigners hail 'nerve gas link' to Gulf War Syndrome". The Scotsman. Edinburgh, UK. 13 November 2004. Archived from the original on 13 February 2012. Retrieved 24 November 2009.
- "Gulf War exposures announcement". publichealth.va.gov. Archived from the original on 18 December 2009.
- Gulf War Illnesses (Report). U.S. Senate Veterans Affairs Committee. 2007. Archived from the original on 27 February 2013., Testimony to the Senate Veterans Affairs Committee by Meryl Nass, MD on September 25, 2007
- ^ U.S. Department of Veterans Affairs. "Authorizing Legislation" (PDF). Retrieved August 15, 2019.
- ^ U.S. Government Printing Office. "Veterans Programs Enhancement Act of 1998, Public Law 105–368 Section 104, 112 STAT. 3315" (PDF). Retrieved August 15, 2019.
- "Scientific Progress in Understanding Gulf War Veterans' Illnesses: Report and Recommendations" (PDF). United States Department of Veterans Affairs. September 2004. Archived (PDF) from the original on 19 March 2012. Retrieved 9 May 2012.
- Riegle DW (9 February 1994), U.S. Chemical and Biological Warfare-Related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Gulf War, Wikisource, archived from the original on 6 July 2012, retrieved 9 May 2012
- Persian Gulf War Illnesses Task Force (9 April 1997). "Khamisiyah: A Historical Perspective on Related Intelligence". Federation of American Scientists. Archived from the original on 22 July 2013. Retrieved 29 March 2015.
- Golomb BA (March 2008). "Acetylcholinesterase inhibitors and Gulf War illnesses". Proceedings of the National Academy of Sciences of the United States of America. 105 (11): 4295–4300. Bibcode:2008PNAS..105.4295G. doi:10.1073/pnas.0711986105. PMC 2393741. PMID 18332428.
- Haley RW, Kramer G, Xiao J, Dever JA, Teiber JF (May 2022). "Evaluation of a Gene-Environment Interaction of PON1 and Low-Level Nerve Agent Exposure with Gulf War Illness: A Prevalence Case-Control Study Drawn from the U.S. Military Health Survey's National Population Sample". Environmental Health Perspectives. 130 (5). National Institute of Environmental Health Sciences: 57001. doi:10.1289/EHP9009. PMC 9093163. PMID 35543525. cf. "UTSW genetic study confirms sarin nerve gas as cause of Gulf War illness". University of Texas Southwestern Medical Center. 11 May 2022. Retrieved 11 May 2022.
For Gulf War veterans with the QQ genotype, hearing nerve agent alarms—a proxy for chemical exposure—raised their chance of developing GWI by 3.75 times. For those with the QR genotype, the alarms raised their chance of GWI by 4.43 times. And for those with two copies of the R gene, inefficient at breaking down sarin, the chance of GWI increased by 8.91 times. Those soldiers with both the RR genotype and low-level sarin exposure were over seven times more likely to get GWI due to the interaction per se, over and above the increase in risk from both risk factors acting alone. For genetic epidemiologists, this number leads to a high degree of confidence that sarin is a causative agent of GWI.
- "Depleted Uranium". GlobalSecurity.org. nd. Archived from the original on 19 January 2012. Retrieved 9 May 2012.
- Jiang GC, Aschner M (April 2006). "Neurotoxicity of depleted uranium: reasons for increased concern". Biological Trace Element Research. 110 (1): 1–17. Bibcode:2006BTER..110....1J. doi:10.1385/BTER:110:1:1. PMID 16679544. S2CID 24199948.
- "Depleted Uranium". VA Public Health. October 12, 2023. Archived from the original on Mar 28, 2024.
- Faa A, Gerosa C, Fanni D, Floris G, Eyken PV, Lachowicz JI, et al. (2018). "Depleted Uranium and Human Health". Current Medicinal Chemistry (Review article). 25 (1): 49–64. doi:10.2174/0929867324666170426102343. PMID 28462701. Archived from the original on Jun 5, 2023.
- "Gulf War syndrome 'not caused by depleted uranium'". BBC News. 2021-02-18. Retrieved 2021-02-18.
- Cotterill T (18 February 2021). "Gulf War syndrome 'not caused by depleted uranium' city scientists claim". The News (Portsmouth). Retrieved 2021-02-18.
- "Pyridostigmine bromide use in the First Gulf War". Frontline. PBS. 1 December 1996. Archived from the original on 12 November 2012. Retrieved 9 May 2012.
- ^ Gulf War and Health: Treatment for Chronic Multisymptom Illness. National Academies Press. 2013. p. 13.
- Qiang D, Xie X, Gao Z (2017). "New insights into the organophosphate-induced delayed neuropathy". Journal of the Neurological Sciences. 381: 153–159. doi:10.1016/j.jns.2017.08.451. S2CID 54302903.
- Mackenzie Ross SJ, Brewin CR, Curran HV, Furlong CE, Abraham-Smith KM, Harrison V (2010). "Neuropsychological and psychiatric functioning in sheep farmers exposed to low levels of organophosphate pesticides". Neurotoxicology and Teratology. 32 (4): 452–459. Bibcode:2010NTxT...32..452M. doi:10.1016/j.ntt.2010.03.004. PMC 3042861. PMID 20227490.
- Office of the Special Assistant to the Undersecretary of Defense (Personnel and Readiness) for Gulf War Illnesses Medical Readiness and Military Deployments (17 April 2003). Environmental Exposure Report: Pesticides Final Report. Washington, D.C.: United States Department of Defense.
- ^ Krengel M, Sullivan K (1 August 2008). Neuropsychological Functioning in Gulf War Veterans Exposed to Pesticides and Pyridostigmine Bromide (PDF). Fort Detrick, MD: U.S. Army Medical Research and Materiel Command. Archived from the original on 8 April 2013. Retrieved 9 May 2012. W81XWH-04-1-0118
- ^ Research Advisory Committee on Gulf War Veterans' Illnesses, U.S. Department of Veterans Affairs (2008). Gulf War Illness and the Health of Gulf War Veterans: Scientific Findings and Recommendations (PDF) (Report). Washington, DC: U.S. Government Printing Office. p. 1. Archived (PDF) from the original on 3 June 2014.
- Cordesman AH (1999). Iraq and the War of Sanctions: Conventional Threats and Weapons of Mass Destruction. Greenwood Publishing Group. ISBN 978-0-275-96528-0.
- Chan KC (11 October 2000). "GAO-01-92T Anthrax Vaccine: Preliminary Results of GAO's Survey of Guard/Reserve Pilots and Aircrew Members" (PDF). Government Accountability Office. Archived (PDF) from the original on 6 April 2012. Retrieved 9 May 2012.
- Burdeau C (16 May 2001). "Expert: Anthrax vaccine not proven". The Clarion-Ledger. Archived from the original on 7 November 2001. ("original source". The Clarion-Ledger. Archived from the original on 12 July 2012.)
- McNeil MM, Chiang IS, Wheeling JT, Zhang Y (March 2007). "Short-term reactogenicity and gender effect of anthrax vaccine: analysis of a 1967-1972 study and review of the 1955-2005 medical literature". Pharmacoepidemiology and Drug Safety. 16 (3): 259–274. doi:10.1002/pds.1359. PMID 17245803. S2CID 25335669.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 123 (p. 133 in PDF). Archived (PDF) from the original on 3 June 2014.
- Asa PB, Cao Y, Garry RF (February 2000). "Antibodies to squalene in Gulf War syndrome". Experimental and Molecular Pathology. 68 (1): 55–64. doi:10.1006/exmp.1999.2295. PMID 10640454.
- Office of the Federal Register, National Archives and Records Administration. (2004, January 7). 69 FR 1320 - Biological Products; Bacterial Vaccines and Toxoids; Implementation of Efficacy Review. . Office of the Federal Register, National Archives and Records Administration. https://www.govinfo.gov/app/details/FR-2004-01-08/C3-32255
- Del Giudice G, Fragapane E, Bugarini R, Hora M, Henriksson T, Palla E, et al. (September 2006). "Vaccines with the MF59 adjuvant do not stimulate antibody responses against squalene". Clinical and Vaccine Immunology. 13 (9): 1010–1013. doi:10.1128/CVI.00191-06. PMC 1563566. PMID 16960112.
- Henig J (2009-10-18). "FactCheck: Swine Flu Vaccine Fears Greatly Exaggerated". Newsweek. Retrieved 2022-11-06.
- ^ Update of Health Effects of Serving in the Gulf War. Gulf War and Health. Vol. 8. Washington, DC: National Academies Press. 2010. p. 109. doi:10.17226/12835. ISBN 978-0-309-14921-1. PMID 25032373.
Health Effects of Serving in the Gulf War, Update 2009; Board on the Health of Select Populations; Institute of Medicine, National Academy of Sciences
- Update of Health Effects of Serving in the Gulf War. Gulf War and Health. Vol. 8. National Academies Press. 2010. p. 260. doi:10.17226/12835. ISBN 978-0-309-14921-1. PMID 25032373.
- "VA Benefits for Gulf War Syndrome". fight4vets. Archived from the original on 19 August 2016. Retrieved 25 July 2016.
- ^ Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined. Institute of Medicine, National Academy of Sciences. Washington, D.C.: National Academies Press. 2014. pp. 90–99. ISBN 978-0-309-29877-3. OCLC 880456748.
- "Information for Veterans" (PDF). War Related Illness and Injury Study Center. Gulf War Illness.
- U.S. Department of Veterans Affairs, Office of Research and Development (19 October 2017). "Researchers find evidence of DNA damage in Vets with Gulf War illness".
- "Gulf War Veterans' Medically Unexplained Illnesses". Veterans Health Administration. publichealth.va.gov. Public Health. US Department of Veterans Affairs. Archived from the original on 24 February 2014.
- "A Guide to Gulf War Veterans' Health" (PDF). 2002. Archived from the original (PDF) on 26 September 2006.
- ^ "The Gulf War Illness Landscape" (PDF). U.S. Department of Defense. May 2018. Archived from the original (PDF) on 11 July 2018. Retrieved 11 July 2018.
Congressionally Directed Medical Research Program
- "Gulf War Illness Research Program, Congressionally Directed Medical Research Programs". cdmrp.army.mil. Archived from the original on 11 July 2018. Retrieved 11 July 2018.
- ""Gulf War Illness Research Program", Congressionally Directed Medical Research Programs" (PDF). cdmrp.army.mil. Archived from the original (PDF) on 11 July 2018. Retrieved 11 July 2018.
- "Funding Opportunities-FY18 GWIRP, Congressionally Directed Medical Research Programs (CDMRP), US DoD". cdmrp.army.mil. Archived from the original on 11 July 2018. Retrieved 11 July 2018.
- Kelsall HL, McKenzie DP, Sim MR, Leder K, Forbes AB, Dwyer T (October 2009). "Physical, psychological, and functional comorbidities of multisymptom illness in Australian male veterans of the 1991 Gulf War". American Journal of Epidemiology. 170 (8): 1048–1056. doi:10.1093/aje/kwp238. PMID 19762370.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 220 (p. 230 in PDF). Archived (PDF) from the original on 3 June 2014.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 262 (p. 272 in PDF). Archived (PDF) from the original on 3 June 2014.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 45 (p. 55 in PDF). Archived (PDF) from the original on 3 June 2014.
- Gulf War Illness and the Health of Gulf War Veterans, Scientific Findings and Recommendations (PDF) (Report). U.S. Department of Veterans Affairs. 2008. p. 222 (p. 232 in PDF). Archived (PDF) from the original on 3 June 2014.
- Hyams KC, Wignall FS, Roswell R (September 1996). "War syndromes and their evaluation: from the U.S. Civil War to the Persian Gulf War". Annals of Internal Medicine. 125 (5): 398–405. doi:10.7326/0003-4819-125-5-199609010-00007. PMID 8702091. S2CID 24433771.
- Pizarro J, Silver RC, Prause J (February 2006). "Physical and mental health costs of traumatic war experiences among Civil War veterans". Archives of General Psychiatry. 63 (2): 193–200. doi:10.1001/archpsyc.63.2.193. PMC 1586122. PMID 16461863.
- Gray GC, Coate BD, Anderson CM, Kang HK, Berg SW, Wignall FS, et al. (November 1996). "The postwar hospitalization experience of U.S. veterans of the Persian Gulf War". The New England Journal of Medicine. 335 (20): 1505–1513. doi:10.1056/nejm199611143352007. PMID 8890103.
- Knoke JD, Gray GC (1998). "Hospitalizations for unexplained illnesses among U.S. veterans of the Persian Gulf War". Emerging Infectious Diseases. 4 (2): 211–219. doi:10.3201/eid0402.980208. PMC 2640148. PMID 9621191.
- Purdy MC (20 January 2006). "Study finds multisymptom condition is more prevalent among Persian Gulf vets". Washington University in St. Louis. Archived from the original on 14 April 2009. Retrieved 9 May 2012.
- "Research Advisory Committee on Gulf War Veterans' Illnesses home page". va.gov. Retrieved 11 July 2018.
- Silverleib A (9 December 2008). "Gulf War illness is real, new federal report says". CNN. Archived from the original on 9 November 2012. Retrieved 9 May 2012.
- "Gulf War: What Kind of Care Are Veterans Receiving 20 Years Later?". Committee on Veterans' Affairs. U.S. House of Representatives.
Hearing before the Subcommittee on Oversight and Investigations of the Committee on Veterans' Affairs, U.S. House of Representatives, One Hundred Thirteenth Congress, First Session, Wednesday, March 13, 2013.
- Cory-Slechta D, Wedge R, Fulco C, Liverman CT, Sox HC, Mitchell AE, Sivitz LB, Black RE, eds. (2016). Update of Health Effects of Serving in the Gulf War. Gulf War and Health. Vol. 10. Washington, D.C.: National Academy Press. p. 11. ISBN 978-0-309-07178-9. OCLC 45180227.
Board on the Health of Select Populations; Institute of Medicine, National Academies of Sciences, Engineering, and Medicine
- Miller M (12 March 2003). "Should Louis Jones die?". Newsweek. Archived from the original on 9 August 2016. Retrieved 17 July 2016.
- Collins D (19 February 2003). "Gulf War vet executed". CBS News. Archived from the original on 19 August 2016. Retrieved 17 July 2016.
- Coffman M (2 June 2014). "Actions – H.R.4261 – 113th Congress (2013–2014): Gulf War Health Research Reform Act of 2014". congress.gov. Retrieved 15 August 2019.
- Coffman M (14 March 2014). "Bipartisan Bill on Gulf War Health Research". House Office of Mike Coffman. Archived from the original on 21 March 2014. Retrieved 27 May 2014.
- ^ Kennedy K (14 March 2014). "Congress seeks independence for Gulf War illness board". USA Today. Archived from the original on 30 May 2014. Retrieved 27 May 2014.
- U.S. Department of Veterans Affairs. "Archived Committee Charters, Research Advisory Committee on Gulf War Veterans' Illnesses". Retrieved August 15, 2019.
External links
| Classification | D |
|---|
| Gulf War | |
|---|---|
| Participants | |
| Background | |
| Invasion of Kuwait | |
| Coalition intervention | |
| Battles | |
| Air campaign | |
| Impact on Israel | |
| Aftermath | |
| Memorials | |
| Military technology | |